Patient-Centered Communication and Shared Decision Making
The committee’s conceptual framework for a high-quality cancer care delivery system highlights the critical importance of engaged patients. Patients are at the center of the framework (see Figure S-2), which conveys the most important goal of a high-quality cancer care delivery system: meeting the needs of patients with cancer and their families. Such a system should support all patients and families in making informed health care decisions that are consistent with their needs, values, and preferences. This will require a delivery system and workforce oriented to the provision of patient-centered care, defined as “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions” (IOM, 2001, p. 40). Patient-centered care includes fostering good communication between patients and their cancer care team; developing and disseminating evidence-based information to inform patients, caregivers, and the cancer care team about treatment options; and practicing shared decision making. Although patient-centered communication and shared decision making were not a major focus of the Institute of Medicine’s (IOM’s) Ensuring Quality Cancer Care report (IOM and NRC, 1999), several concepts from that report are relevant to the committee’s recommendations on both topics: the importance of developing a cancer care plan; managing pain, other symptoms, and side effects; as well as the timely referral to hospice care at the end of life.
Currently, patient-centered communication and shared decision making in oncology are suboptimal (Aiello Bowles et al., 2008; Ayanian et al., 2005, 2010; Wagner et al., 2010). In a study of 1,057 patient encounters with
3,552 clinical decisions, only 9 percent resulted in what was defined as an informed medical decision (Braddock et al., 1999). More recently, studies have found that clinicians ask for patient preferences in medical decisions only about half the time (Lee et al., 2012; Zikmund-Fisher et al., 2010). A number of obstacles prevent patient-centered communication and shared decision making among patients, their family, caregivers, and the cancer care team. The emotional, financial, and logistical repercussions of a cancer diagnosis and the complexity of treatment options, together with patients’ limitations in health literacy and lack of experience with the health care system, can make it difficult for patients and their families to actively engage in making health care decisions. The current reimbursement system does not incentivize clinicians to engage in patient-centered communication and shared decision making. In addition, clinicians often lack training in communication, leading to difficulties in recognizing and responding to patients’ informational and emotional needs. A lack of understandable and easily available information on prognosis, treatment options, likelihood of treatment responses, palliative care, psychosocial support, and the costs of cancer care contribute to communication problems, which are exacerbated in patients with advanced cancer.1
This chapter describes the benefits, challenges, and characteristics of patient-centered communication and shared decision making; presents approaches and tools to facilitate patient-centered communication and shared decision making; and discusses the importance of advance care planning, the provision of palliative care and psychosocial support across the cancer continuum, and timely referral to hospice when patients near the end of life. The evidence base for this chapter is primarily derived from the National Cancer Policy Forum’s workshop summaries on Patient-Centered Cancer Treatment Planning: Improving the Quality of Oncology Care, Assessing and Improving Value in Cancer Care, and Delivering Affordable Cancer Care in the 21st Century, and the National Cancer Institute’s (NCI’s) monograph Patient-Centered Communication in Cancer Care (Epstein and Street, 2007; IOM, 2009a, 2011b, 2013). The committee identifies two recommendations to improve patient-centered communication and shared decision making.
DEFINING PATIENT-CENTERED COMMUNICATION
AND SHARED DECISION MAKING
The concept of patient-centeredness as an important attribute of high-quality health care gained national prominence with the IOM report
____________________
1 Cancer that has spread to other places in the body and usually cannot be cured or controlled with treatment (NCI, 2013b).
Crossing the Quality Chasm: A New Health System for the 21st Century (IOM, 2001). The IOM defines patient-centeredness as “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions” (IOM, 2001, p. 40).2 Over time, other organizations and individuals have elaborated on the attributes of patient-centered care (Bechtel and Ness, 2010; Berwick, 2009; Epstein et al., 2010; Picker Institute, 2013). In the cancer setting, some of the attributes of patient-centered care highlighted at an IOM National Cancer Policy Forum workshop included (IOM, 2011a)
• patient education and empowerment;
• patient-centered communication, which involves the patient, family, and friends; explains treatment options; and includes patients in treatment decisions to reflect patients’ values, preferences, and needs;
• coordination and integration of care; and
• provision of emotional support as needed, such as relieving fear and anxiety and addressing mental health issues.
Effective patient-clinician communication and shared decision making are key components of patient-centered care. These components require that informed, activated, and participatory patients and family members interact with a patient-centered care team that has effective communication skills and is supported by an accessible, well-organized, and responsive health care system (see Figure 3-1) (Epstein and Street, 2007). As described by the NCI’s monograph Patient-Centered Communication in Cancer Care, the primary functions of patient-centered communication are to (1) foster healing relationships, (2) exchange information, (3) respond to emotions, (4) manage uncertainty, (5) make decisions, and (6) enable patient self-management (see Table 3-1) (Epstein and Street, 2007). These six functions dynamically interact to influence the quality of patient-clinician interactions and may ultimately influence patients’ health outcomes (Epstein and Street, 2007). They are skills that need to be developed, utilized, and maintained across the cancer care continuum.
Sepucha and colleagues (2004, p. 57) argued that the “quality of a clinical decision, or its patient-centeredness, is the extent to which it reflects the considered needs, values, and expressed preferences of a well-informed patient and is thus implemented.” Rather than relying on clinician-directed decision making, over the past few decades patients
____________________
2 Needs generally refer to a patient’s physical or emotional requirements. Values and preferences represent a patient’s concerns, expectations, and choices regarding health care, based on a full and accurate understanding of care options (adapted from IOM, 2001, 2003).
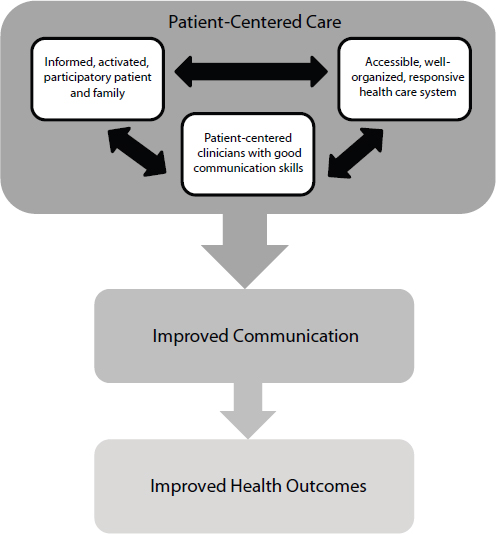
FIGURE 3-1 Model of patient-centered care. The patient, clinicians, and health care system dynamically interact to influence patient-centered care. The delivery of patient-centered care has the potential to improve communication and health outcomes.
SOURCE: Adapted from Epstein and Street, 2007.
have individually and collectively pushed for a greater role in medical decision making (Clancy, 2008) (see Figure 3-2). Health researchers, advocacy organizations, and the Agency for Healthcare Research and Quality (AHRQ) have also encouraged patients to play a larger role in making medical decisions. Research indicates that when patients are involved in their own care, they are more satisfied with the care they receive and
TABLE 3-1 Important Functions of Patient-Clinician Communication
| Function | Description |
| Fostering Healing Relationships | Developing a patient-clinician relationship that is characterized by trust and rapport is critical to patient-centered communication and shared decision making. This involves mutual understanding of patient and clinician roles, as well as clinician self-awareness and provision of emotional support, guidance, and understanding. |
| Exchanging Information | The cancer care team should ascertain patients’ informational needs. Conveying information to patients can be facilitated through the ask-tell-ask method, an approach described in the section on prioritizing clinician training in communication. The exchange includes the cancer care team’s provision of accurate prognostic information and treatment options, realistic expectations for response to treatment, and the cost of cancer care to inform patients’ decisions. |
| Responding to Emotions | The cancer care team should recognize and respond to patients’ emotions, which involves verbally expressing understanding, legitimizing feelings, and providing empathy and support. This also includes the development of a psychosocial care plan and linking patients to psychosocial care if they experience high levels of emotional distress, anxiety, and depressive symptoms. |
| Managing Uncertainty | Clinicians play an important role in reducing and managing the uncertainty associated with cancer care. This can include cognitive-behavioral interventions to help patients cope with this uncertainty and, if possible, improve understanding. |
| Making Decisions | Shared decision making involves three processes—information exchange, deliberation, and reaching a final decision. A patient’s decision often extends beyond medical issues, and includes factors such as finances and the expense of treatment, and impact on employment and family. The logistics of scheduling and receiving cancer treatment can be an enormous strain for patients, families, and caregivers; disrupt family life; and require negotiations with employers for time off or flexible work schedules. |
| Enabling Patient Self-Management | The cancer care team should provide individuals with resources to be proactive in their care. Examples of self-management tools and enablers include cancer care plans, survivorship care plans, and patient navigators who assist patients to overcome health care system barriers and facilitate timely access to health care services. |
SOURCES: C-Change, 2005; Epstein and Street, 2007; Lauria et al., 2001.
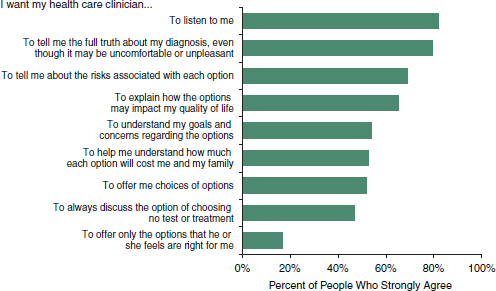
FIGURE 3-2 People want to be involved in understanding evidence and making decisions about their care. The IOM surveyed a nationally representative sample of 1,068 U.S. adults who had seen at least one health care clinician in the previous year. The majority of adults strongly agreed that they should be actively involved in understanding and making decisions about their care.
SOURCE: Alston et al., 2012.
often experience better health outcomes (Alston et al., 2012; CFAH, 2010; Hibbard and Greene, 2013; Lantz et al., 2005; Maurer et al., 2012; Roseman et al., 2013). Thus, shared decision making is a critical feature of patient-centered communication, and is defined as “the process of negotiation by which physicians and patients arrive at a specific course of action, based on a common understanding of the goals of treatment, the risks and benefits of the chosen treatment versus reasonable alternatives, and each other’s values and preferences” (IOM, 2011a, p. 8; adapted from Sheridan et al., 2004).
Patients with cancer and their families are often required to manage greater portions of their cancer care due to advances in cancer treatment, as well as changes in the practice of health care, such as earlier discharge from the hospital (CFAH, 2010; McCorkle et al., 2011). These duties may include drug management, wound care, rehabilitation, and lifestyle changes (CFAH, 2010). Clinicians help patients engage in self-management, which involves managing the medical and psychological aspects of cancer care, as well as adapting to changes in roles that result from cancer diagnosis (McCorkle et al., 2011). Promoting patient self-management can facilitate shared decision making and improve cancer care.
THE IMPORTANCE OF PATIENT-CENTERED COMMUNICATION AND SHARED DECISION MAKING IN CANCER
A number of factors related to cancer care necessitate a patient-centered approach to communication: (1) cancer care is extremely complex and patients’ treatment choices have serious implications for their health outcomes and quality of life; (2) the evidence supporting many decisions in cancer care is limited or incomplete; and (3) trade-offs in the risks and benefits of cancer treatment choices may be weighed differently by individual patients, and clinicians need to elicit patient needs, values, and preferences in these circumstances. Each of these factors is discussed below.
Complexity of Cancer Care
Cancer care is complex. It may involve multiple treatment modalities, including chemotherapy, radiation, and surgery, all of which need to be coordinated among different cancer care specialists. Treatment regimens can also be time intensive, debilitating, and often result in serious and sometimes long-term complications (IOM, 2011a). In addition, patients must often choose from multiple cancer treatment options, requiring patients and their families to decide on the goals of treatment (e.g., prioritizing survival time vs. maximizing quality of life), whether to participate in clinical trials, and to weigh evidence of the risks and benefits of different treatment approaches. These decisions often need to be revisited at various points along the cancer care continuum. A patient’s goals or preferences at the time of initial diagnosis, for example, may be very different from a patient who has advanced cancer.
Limitations in the Evidence Base
As described in Chapter 5, the committee recommends that researchers improve the breadth and depth of information collected in clinical research. Studies indicate that there is a lack of evidence to support many medical decisions (El Dib et al., 2007; IOM, 2008b, 2012; Villas Boas et al., 2012). Evidence supporting patients’ medical decisions can be especially limited for older adults and individuals with comorbidities, as these individuals are often underrepresented or excluded from clinical trials (IOM, 2009b, 2010). While comparative effectiveness research (CER) and learning health care systems aim to fill these evidence gaps, they have limitations. Clinicians should fully communicate gaps in the evidence base to their patients during the medical decision-making process. When
evidence is sparse, patient preferences should be a particularly important consideration in the health care decision-making process.
Preference-Sensitive Decisions
Some decisions in cancer care are particularly sensitive to patient preferences. For example, women with breast cancer can often choose from different courses of treatment—mastectomy versus lumpectomy followed by radiation—and expect equivalent survival outcomes (Fisher et al., 2002). Women may choose mastectomy, or the removal of the entire breast, for peace of mind or to avoid radiation therapy, while women who choose lumpectomy followed by radiation may do so to conserve their breasts (Collins et al., 2009). Women with BRCA 1 and 2 gene mutations are at higher risk for developing breast and ovarian cancer, and may face difficult decisions about breast cancer screening, as well as consideration of prophylactic mastectomy or oophorectomy to reduce the risk of cancer3 (Jolie, 2013; Schwartz et al., 2009). These decisions can have a major impact on an individual’s future. Thus, patients’ preferences need to inform medical decisions. Patients’ preferences are also particularly important when they consider their treatment goals, such as choosing a less aggressive treatment strategy in order to maintain a high quality of life (Berman, 2012; Epstein and Street, 2007; Gruman, 2013). Preferences may also change over time and clinicians need to revisit these throughout the cancer care continuum. For example, women considering second line chemotherapy may prefer to take a more active role in decision making compared to women who are considering first line chemotherapy (Grunfeld et al., 2006).
CHALLENGES TO PATIENT-CENTERED COMMUNICATION AND SHARED DECISION MAKING IN CANCER
There are a number of challenges to patient-centered communication and shared decision making. This section discusses patient, clinician, and health care system challenges.
Challenges for Patients
A cancer diagnosis can lead to a state of crisis for an individual and his or her family because most people are not immediately equipped to understand their diagnosis or how to identify options for moving forward (NCCS, 2012a). Because treatment and its side effects, as well as recovery
____________________
3 Oophrectomy is surgery to remove one or both ovaries (NCI, 2013b).
and the worry about recurrence, can result in a series of crises for a patient, the crisis does not end once the shock of initial diagnosis wears off (NCCS, 2012a).
The emotional repercussions of a cancer diagnosis can prevent patients from engaging in effective communication with their clinicians about their diagnosis and treatment. Patients can become anxious; feel vulnerable, alone, and fearful; and experience feelings of losing control when receiving a cancer diagnosis. Given these emotions, patients may be unable to retain important information regarding their treatment when speaking with their care team (IOM, 2011a).
Patients’ lack of assertiveness may also create communication challenges. Ideally, patients are active communicators, asking questions, assertively stating their opinions, introducing new topics of conversation, and discussing their concerns, feelings, or preferences when communicating with their clinicians (Epstein and Street, 2007). Patients’ lack of experience with the health care delivery system and illness, however, can impede their active participation (IOM, 2011a).
Research indicates that the average patient asks five or fewer questions during a 15-minute doctor’s visit (IOM, 2008a), and an AHRQ public service announcement noted that people ask more questions when buying a cell phone or ordering a meal than they do during medical appointments. Patients may refrain from asking questions because some clinicians are not receptive or because patients fear they will be considered difficult and receive worse care (Frosch et al., 2012; Gruman, 2013).
Patients who only participate in their care on a limited basis risk poor health outcomes because they may fail to express their needs, fears, expectations, and preferences, which are important to their health care decisions. These patients may also feel dissatisfied when interacting with their clinicians (Epstein and Street, 2007), a problem exacerbated by patients’ awe of their clinicians or lack of self-confidence (Hoffman, 2004). Older adults may be more reluctant to question their clinicians’ authority because they may think it is impolite or inappropriate to ask questions or make decisions about their own care (Busari, 2013; Hoffman, 2004; IOM, 2008a). Research has also linked patients’ level of participation in clinical encounters with their level of education, ethnicity, gender, personality, and the orientation of patient-clinician relationships (shared control versus physician control) (Epstein and Street, 2007). Box 3-1 lists a number of questions that patients with cancer can discuss with their clinicians.
In addition, a patient’s level of health literacy and numeracy can affect patient-centered communication and shared decision making (Peters et al., 2007). More than 90 million adults in the United States have poor reading and writing skills and only 38 percent of high school seniors are proficient in reading (Kutner et al., 2007; NAEP, 2010; NRC, 2012).
BOX 3-1
Questions That Patients with Cancer Can Discuss with Their Clinicians
Questions About Prognosis
• What is the goal of treatment? Is it directly treating the cancer or improving my symptoms, or both?
• How long does the average person with this cancer live? (ask for a window and the most likely scenario)
• How will I feel?
• What is my likelihood of a cure?
• If I cannot be cured, will I live longer with treatment? How much longer?
• Will I feel better or worse?
• Can I receive palliative care focused on maintaining the quality of my and my family’s life during my cancer treatment?
• What options do I have if I don’t want to continue my cancer treatment?
• When should I think about hospice? Can I meet with hospice now, when I am well?
• How often should we check in about my care plan?
Questions About Treatment
• What are my treatment options?
• Why do I need this treatment?
• How does this treatment compare with other treatment options?
• What things are likely to happen to me?
• Am I healthy enough to undergo the treatment?
• What are the risks and benefits of treatment?
• Are there any side effects?
Furthermore, many individuals have inadequate health literacy, which is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (IOM, 2004a, p. 32; Ratzan and Parker, 2000). AHRQ estimated that 36 percent of the adult population, or approximately 80 million individuals, have poor health literacy, with low health literacy more prevalent in certain subgroups, including older adults, racial and ethnic minority populations, adults who spoke a language other than English prior to starting school, individuals who have not completed high school, and people living in poverty (Berkman et al., 2011). Poor health literacy can hinder patients’ ability to receive health care, including their ability to communicate with their clinicians and man-
• Will treatment make me feel better or worse?
• How many times have you done this procedure?
• What is the cost of this treatment?
• What clinical trials are available?
![]() What are the potential benefits of clinical trials?
What are the potential benefits of clinical trials?
![]() Am I eligible to participate?
Am I eligible to participate?
![]() How do I enroll?
How do I enroll?
• Which hospital is best for my needs?
• Which clinician(s) will coordinate my care?
• How do you spell the name of that drug?
• Will this medicine interact with medicines that I’m already taking?
Questions About Advance Care Planning
• Are there things I should be doing to plan ahead?
![]() Draft a will?
Draft a will?
![]() Participate in advance care planning and decide on my advance directives?
Participate in advance care planning and decide on my advance directives?
![]() Choose a health care proxy who can speak for me if I am unable?
Choose a health care proxy who can speak for me if I am unable?
![]() Address financial or family legal issues?
Address financial or family legal issues?
![]() Appoint a durable power of attorney for financial affairs?
Appoint a durable power of attorney for financial affairs?
![]() Write notes or create DVDs for loved ones?
Write notes or create DVDs for loved ones?
Questions About Family, Psychosocial, and Spiritual Needs
• Will you help me talk with my children?
• Who is available to help me cope with this situation?
SOURCES: Adapted from AHRQ, 2013b; ASCO and Cancer.Net, 2012; Harrington and Smith, 2008.
age chronic illnesses (IOM, 2011b). Poor health literacy is associated with increased hospitalizations, greater use of emergency room services, and lower probability of receiving preventive care (Berkman et al., 2011). Poor health literacy is especially concerning for older adults, as Berkman and colleagues (2011) found that lower health literacy in this group was associated with a higher risk of mortality and a worse overall health status.
Even if a patient has good health literacy, he or she may experience information overload when interacting with clinicians, which can be exacerbated by clinicians’ use of unfamiliar terminology or jargon (Hoffman, 2004; IOM, 2011a). Patients may not retain important information if they feel overwhelmed with new terminology while grappling with all of the information clinicians are trying to impart. Moreover, patients have very
different expectations regarding the amount of information they need in order to make shared decisions about their care; while many patients want to know as much as possible, some patients do not want information (Epstein and Street, 2007; IOM, 2011a). Additionally, a patient’s informational needs may vary substantially from those of the patient’s family and caregivers.
There are a number of special considerations when the cancer care team communicates with older adults who have cancer. Older patients may be less technologically savvy and may need alternate options for communicating (such as large print brochures, plain language, and more repetition). Likewise, family members may have to make medical decisions for some older patients with cancer due to a patient’s’ cognitive status, further complicating the communication and shared decision-making processes. In addition, it may be more difficult for the care team to communicate treatment options to older adults, as multiple comorbid chronic diseases are more prevalent in this population, making the options for cancer treatment especially complex.
Challenges for Clinicians
A number of factors can prevent clinicians from engaging in patient-centered communication and shared decision making, including clinicians’ lack of training in communication (see section below on prioritizing clinician training in communication) and insensitivity to patients’ informational, cultural, and emotional needs. Clinician characteristics, such as age, gender, and training, may influence the provision of patient-centered communication (Epstein and Street, 2007; Porter-O’Grady and Malloch, 2007). For example, some older clinicians may use authoritative communication styles rather than more collaborative approaches (Busari, 2013; Frosch et al., 2012).
Epstein and Street (2007) noted that some clinicians fail to appreciate the range of patient and family needs, explaining, in part, patients and their families’ dissatisfaction with the timing and amount of information given to them by clinicians. As mentioned previously, clinicians need to be aware of the differing informational needs of patients and adapt their communication approach accordingly (Epstein and Street, 2007; IOM, 2011a). A clinician’s level of comfort discussing specific aspects of cancer care can also impede patient-centered communication and shared decision making. Research shows that clinicians are often uncomfortable discussing poor prognoses, psychosocial and emotional aspects of care, and sexuality (Epstein and Street, 2007; IOM, 2008a; Mack and Smith, 2012). Furthermore, clinicians may not recognize patients’ emotional
cues and may be unfamiliar with resources and services designed to meet patients’ psychosocial health needs (Epstein and Street, 2007; IOM, 2008a).
Clinicians can also misjudge patient preferences. For example, clinicians may expect women with early stage breast cancer to prefer to keep their breast, given that mastectomy and lumpectomy followed by radiation can be equally effective treatment options for some patients. A study of breast cancer patients who were provided comprehensive information about both treatment options, however, found that approximately one-third of women chose to have a mastectomy (Collins et al., 2009). Other patients may prioritize quality of life rather than length of life as a primary goal (Berman, 2012; IOM, 2011a). In addition, patients with cancer may assess the benefits and risks of chemotherapy differently than their clinicians, and may be more willing to undergo chemotherapy with small benefits and high risks of toxicity (Matsuyama et al., 2006).
Differences between patients’ and clinicians’ culture and language may influence clinicians’ ability to engage in patient-centered communication and shared decision making. Surbone (2010, p. 4) emphasized that language and cultural barriers can be a major source of stress for patients, family members, and clinicians, especially if “linguistic, health literacy, and cultural differences combined render mutual understanding especially difficult.” Clinicians’ and patients’ mutual misunderstanding can result in frustration and mistrust, negatively impacting the care received by patients with cancer (Surbone, 2010). Epstein and Street (2007) noted that cultural beliefs will affect communication between clinicians and patients, influence how patients and clinicians interpret their interaction, and impact communication outcomes. Given the growing diversity of the U.S. population (see Chapter 2), it is imperative for clinicians and the health care system to overcome cultural and language barriers to ensure that all patients with cancer receive patient-centered care. In 2013, the U.S. Department of Health and Human Services (HHS) released a blueprint that aims to ensure culturally and linguistically appropriate health care (HHS, 2013a). To address barriers in language, the American Cancer Society’s National Cancer Information Center works with interpreter-services to provide cancer information assistance for the public in 160 languages (see Annex 8-1).
Clinicians’ lack of time may also limit the provision of patient-centered communication and shared decision making. The reimbursement system fails to adequately compensate clinicians for the time it takes to facilitate patient-centered care (IOM, 2009a, 2011b). Smith and Hillner (2011) argued that many of the responsibilities of oncologists are
reimbursed poorly or not at all. Cognitive care4—which can include discussions with patients about prognosis and likely response to treatment, referrals to clinical trials, development of advanced medical directives, and family conferences—is not reimbursed as well as the administration of chemotherapy. Chapter 8 further discusses the perverse incentives of the current reimbursement system and new models of payment that have the potential to improve patient-centered communication and shared decision making in cancer.
System-Level Challenges
The fragmented nature of the cancer care system can prohibit patient-centered communication and shared decision making (IOM and NRC, 1999). Epstein and Street (2007) emphasized that patient-centered communication and shared decision making relies on more than the patient-clinician interactions; it also includes the physical and procedural characteristics of the health care system. Patients who find it difficult to navigate the health care system are likely to experience lower quality patient-clinician communication and shared decision making, which could contribute to underutilization of high-quality care, overuse of care that is unlikely to improve patient outcomes, and higher costs.
Fragmentation of the cancer care delivery system also contributes to communication problems between patients and their care teams. Patients with cancer may need to coordinate care among multiple clinicians on their cancer care team and other care teams. Jessie Gruman, a four-time cancer survivor, pointed out that in 1 year, eight physicians cared for her, and yet only once did two of those physicians communicate directly with each other; she was primarily responsible for sharing her medical information among the different clinicians (Gruman, 2013). It can be especially difficult for care team members to share information and communicate effectively with patients if the care team members’ electronic health records (EHRs) are not interoperable (see Chapter 7 on additional information technology challenges). With system problems such as these, it can be unclear to patients and care teams who is responsible for each aspect of care and who needs to be contacted to address a treatment complication (IOM, 2011a). New models of care and reimbursement, such as accountable care organizations (ACOs) or oncology patient-centered medical homes, may address some of these system challenges (see Chapter 8).
________________
4 Cognitive care refers to evaluation and management services, which entails time spent discussing, for example, prognosis and treatment options (Smith and Hillner, 2011).
IMPROVING PATIENT-CENTERED COMMUNICATION AND SHARED DECISION MAKING IN CANCER
This section discusses strategies for improving patient-centered communication and shared decision making, including (1) making more comprehensive and understandable information available to patients and their families; (2) developing decision aids to facilitate patient-centered communication and shared decision making; (3) prioritizing clinician training in communication; (4) preparing cancer care plans; and (5) using new models of payment to incentivize patient-centered communication and shared decision making.
Making More Comprehensive Information Available
The availability of easily understood, accurate information on cancer prognosis, treatment benefits and harms, palliative care, psychosocial support, and likelihood of treatment response can improve patient-centered communication and shared decision making. A number of trusted organizations have developed print, electronic, and social resources to inform patients and their families about cancer, such as the NCI, the American Cancer Society, the Centers for Disease Control and Prevention, the Mayo Clinic, the National Coalition for Cancer Survivorship, American Society of Clinical Oncology, LIVESTRONG, and the Susan G. Komen Foundation (see Table 3-2 for examples of patient resources).5 However, there are some serious limitations with the type of information included in the available resources on cancer. In addition, there are a number of other websites that may contain inaccurate or outdated information. Thus, finding accurate, useful cancer information online can be a major challenge for patients and their families (Chan et al., 2012; IOM, 2011a; Irwin et al., 2011; Lawrentschuk et al., 2012; Quinn et al., 2012; Shah et al., 2013).
Information that is readily available on cancer often does not answer all of the questions that are important to patients. Some organizations do not provide detailed information on prognosis for various cancers or on the likelihood that treatments will cure cancer or prolong life (IOM, 2009a). Without this information, patients may have poorly informed or unrealistic expectations about the benefit of certain interventions or their likelihood of survival (IOM, 2009a, 2013; Smith and Hillner, 2010). These inaccurate perceptions could result in care that is not aligned with a patient’s goals, such as futile chemotherapy near the end of life. Around 70 to 80 percent of patients with metastatic lung and colorectal cancer in a
________________
5 See http://www.cancer.gov; http://www.cancer.org; http://www.cdc.gov/cancer; http://www.mayoclinic.com/health-information; http://www.canceradvocacy.org; http://www.cancer.net; http://www.livestrong.org; and http://ww5.komen.org (accessed March 28, 2013).
TABLE 3-2 Examples of Web-Based Information, Resources, and Tools for Patients
| Resource | Description |
| AARP Medicare Starter Kit | This kit provides individuals who are approaching age 65 with information on Medicare, including information on choosing a health insurance plan and a timeline for making decisions. It explains in detail issues related to coverage, costs, options, enrollment deadlines, and eligibility. The kit also identifies resources where individuals can find further information on the program. |
| American Society of Clinical Oncology’s (ASCO’s) Advanced Cancer Care Planning Booklet | This booklet offers patients with advanced cancer information about treatment options, clinical trial participation, palliative care and hospice care, the role of family in the decision-making process, and end-of-life planning (e.g., creating an advanced directive, developing a living will, and how to find religious or spiritual support if desired). It includes a blank sheet on which patients can write questions and answers from their clinicians. It also provides additional resources for caregiving, end-of-life care planning, grief and bereavement, cancer treatment, and general patient support. |
| ASCO’s Cancer.Net Mobile | This application helps patients plan and manage their cancer treatment and care, including tools to assemble questions for clinicians and record their responses, track symptoms and side effects during treatment, among other resources. |
| Cancer Support Community | This organization provides a variety of online support groups and discussion boards. The support groups meet in a chat room for 90 minutes per week and are led by licensed mental health professionals. Support groups are organized based on issues, such as caregiving and dealing with bereavement. The discussion boards allow patients to connect with others in order to receive and offer advice and support from those with similar cancer experiences. |
| Center for Advancing Health | This organization runs the Prepared Patient Forum, an interactive website where individuals can read about other patients’ experiences with the health care system and share their own experiences. It also publishes the latest research related to health care decisions and provides links to trusted and helpful resources. |
| Resource | Description |
| John M. Eisenberg Center for Clinical Decisions and Communications Science | This center translates comparative effectiveness research findings into plain language that patients can understand. It creates a variety of products, ranging from research summaries to decision aids and other materials, for use by patients, clinicians, and policy makers. It also runs a conference series to discuss state-of-the-art in communication and medical decision making. |
| Leukemia & Lymphoma Society’s Acute Myeloid Leukemia (AML) Guide | This guide provides detailed information about the biology of AML, considerations in treatment planning (e.g., choosing a specialist, risks and benefits of various treatment options, clinical trial participation, follow-up care), and general strategies for maintaining health (e.g., maintaining a healthy diet and seeing a doctor regularly). It also includes definitions of medical terms. |
| National Coalition for Cancer Survivorship’s (NCCS’s) Cancer Survival Toolbox | This toolbox is a free, self-learning audio program composed of various scenarios cancer patients and survivors commonly face during their cancer journey. The goal of the program is to help patients develop the skills needed to better face and understand the challenges of their illness. It emphasizes developing communication skills, finding information, making decisions, and solving problems. It also includes links to cancer-specific programs that teach patients more about their disease. The NCCS Pocket Cancer Care Guide, a cell phone application, helps patients build question lists, and record and play back office visit conversations, among other features. |
| Patient Advocate Foundation | This organization has a list of resources to help patients find assistance in addressing a variety of medical-related issues. Resources include the National Financial Resource Directory (provides information on financial relief for all areas in life, such as housing, utilities, and food), the National Uninsured Resource Directory & Financial Resource (provides information on available organizations and resources that may help with access to care), National Underinsured Resource Directory & Financial Resource (provides information for patients whose insurance plan does not provide full coverage), and InsureUStoday (provides information on the Affordable Care Act). |
SOURCES: AHRQ, 2012; ASCO, 2011; ASCO and Cancer.Net, 2012; Cancer Support Community, 2012; CFAH, 2012; Finch, 2011; Leukemia & Lymphoma Society, 2012; NCCS, 2012c; Patient Advocate Foundation, 2012.
recent survey, for example, did not understand that their chemotherapy was unlikely to result in a cure (Weeks et al., 2012). In another survey, 64 percent of patients with metastatic lung cancer did not understand that radiation therapy was unlikely to result in a cure (Chen et al., 2013). To inform patients’ expectations about therapy, Smith and Hillner suggested that the NCI revise www.cancer.gov to summarize the available information from clinical research on various cancers’ curability, average lifespan, average treatment benefit, most common side effects, and available clinical trials (Smith and Hillner, 2010).
There is a dearth of information on the patient experience with cancer and its treatment. Oftentimes, available information focuses on survival but neglects other outcomes that matter to patients and their families (Fleurence et al., 2013). Patients are often interested in how they are going to feel during treatment or how long it will take before they can go back to work (Basch, 2013; IOM, 2008a, 2011a). The concept of providing patients with this type of information is consistent with the aims of the Patient-Centered Outcomes Research Institute (PCORI) to support research that aligns with a patient’s experience with treatment (PCORI, 2013b). In its first round of funded projects, PCORI focused largely on addressing questions that are critical to patients and clinicians when making health care decisions (Fleurence et al., 2013). PCORI has also prioritized communication and dissemination of research results, including comparing approaches to disseminate CER, engaging people to ask for information from CER, and supporting shared decision making (PCORI, 2012). In Chapter 5, the committee recommends that the NCI, other federal agencies, PCORI, and researchers work to develop a common set of data elements in research studies that will capture patient-reported outcomes, relevant patient characteristics, and health behaviors to address the need for better clinical information.
Patients and families also lack access to information about the cost of cancer care. In this report, the committee defines the total cost of cancer care as all direct medical costs resulting from the provision of cancer care,6 including payment reimbursed by insurance companies to hospitals and clinicians as well as out-of-pocket costs. Out-of-pocket costs are expenses for medical care that are paid for by the patient and can include deductibles, coinsurance, and copayments for covered services, as well as services that are not covered by insurance (HealthCare.gov, 2013).
The complexity of calculating costs from the multiple perspectives of cancer care (i.e., society, health care system, payer, or patients) presents a
________________
6 This definition varies from other uses of total cost of care, which factor in direct nonmedical costs (such as transportation and parking associated with the receipt of care) and indirect costs (such as lost productivity due to disease morbidity or premature death).
major challenge to making the cost of cancer care more transparent. The price that a clinician or hospital charges for care is often different from the amount collected for that care. Hospitals and clinician practices, for example, usually have a chargemaster that consists of a comprehensive listing of charges for each billable item associated with the care they provide. This chargemaster serves as a starting point for negotiating reimbursement with payers. Thus, the amount that payers reimburse clinicians and hospitals likely varies by payer and is almost always less than what is listed in the chargemaster. In addition, differences in patients’ health insurance benefit plan designs, including variations in the benefits covered and cost-sharing requirements, mean that individual patients can pay different out-of-pocket amounts for the same care. Uninsured patients, who do not have a payer to negotiate the price on their behalf, may pay much more than a well-insured patient for the same care. According to Reinhardt, “this situation has resulted in an opaque system in which payers with market power force weaker payers to cover disproportionate shares of providers’ fixed costs—a phenomenon sometimes termed cost shifting—or providers simply succeed in charging higher prices when they can” (Reinhardt, 2011, p. 2125).
The system’s lack of price transparency is very problematic for patients and clinicians who want to be cost conscious when making decisions about care (Gruman, 2013). A recent study found that only 16 percent of a randomly selected group of U.S. hospitals were able to provide a cost estimate for a hospital stay that included both hospital charges and physician fees for a common surgical procedure (Rosenthal et al., 2013).
A growing number of stakeholders, however, have recognized the importance of price transparency in health care, including state and federal government leaders, private-sector trade groups, and health payers (Rosenthal et al., 2013). The Government Accountability Office concluded that a number of health care and legal factors make it difficult for consumers to obtain price information and recommended that HHS assess the feasibility of estimating complete costs of health care available to consumers through its ongoing and future price transparency efforts (GAO, 2011).
The Patient Protection and Affordable Care Act (ACA)7 requires hospitals to annually publish and update a list of standard charges for their services. In 2014, Health Insurance Marketplaces will require participating health plans to create communication tools where patients can research anticipated out-of-pocket costs for specific services. Private companies are also utilizing proprietary software that analyzes claims data to estimate the costs of common medical procedures (Hostetter and Klein, 2012). As
________________
7 Patient Protection and Affordable Care Act, Public Law 111-148, 111th Congress, 2nd Sess. (March 23, 2010).
of February 2013, at least 30 states had signed laws or proposed legislation focusing on health care price transparency (NCSL, 2013). Several states have also created all-payer claims databases, which collect health insurance claims information from all payers into a single database, including information on charges and payments, the clinicians/hospitals receiving payment, clinical diagnosis and procedure codes, and patient demographics (APCD, 2013; NCSL, 2013).
As depicted in the committee’s conceptual framework (see Figure S-2), publicly reported quality measurement will facilitate better information about the cost of cancer care. The Centers for Medicare & Medicaid Services (CMS) may be in the best position to provide this information. In 2013, HHS released average Medicare charges for 100 common inpatient hospital procedures and 30 outpatient procedures in an effort to improve the affordability and accountability of the health care system (CMS, 2013b; HHS, 2013b). In addition, a U.S. federal judge has lifted an injunction preventing public access to a database that provides information on Medicare insurance claims by individual clinicians (Tamman, 2013). Clinical practice guidelines could also include cost information for different chemotherapy regimens (IOM, 2013; Ramsey and Shankaran, 2012). One study found that when cost information was included in laboratory test ordering forms, it led to a decrease in the number of tests clinicians ordered and reduced hospital charges by more than $400,000 over the 6-month intervention (Feldman et al., 2013). In addition, the decision-support software eviti® provides clinicians with cost data based on average wholesale price for more than 1,100 different cancer care regimens (Licking, 2012). Although one study found that eviti® reduced nonstandard treatment in lung cancer, its impact on the cost of care was not assessed (Ganz, 2013; Grund et al., 2012).
Given patients’ needs for more comprehensive information about cancer care, the committee recommends that the NCI, CMS, PCORI, as well as patient advocacy organizations, professional organizations, and other public and private stakeholders, improve the development of clinical and cost information and make it available through print, electronic, and social media. This information should be easily accessible to patients and their families. Access to more comprehensive information on cancer care will enable patients to make better informed decisions about their care.
Improving Shared Decision Making Using Decision Aids
One of the important functions of communication in cancer care is ensuring that patients make decisions that are consistent with their needs, preferences, and values. Clinicians have an important role in improving
patient-centered communication and shared decision making by listening actively, assessing a patient’s understanding of treatment options, validating a patient’s participation in the decision-making process, and communicating empathy both verbally and nonverbally (Epstein and Street, 2007). In addition, decision making can be improved through use of decision aids that facilitate patient understanding of treatment options and enable patients to take a more active role in decision making. A decision aid is a “tool that provides patients with evidence-based, objective information on all treatment options for a given condition. Decision aids present the risks and benefits of all options and help patients understand how likely it is that those benefits or harms will affect them” (MedPAC, 2010, p. 195). Decision aids can include written material, Web-based tools, videos, and multimedia programs (MedPAC, 2010). Some decision aids are designed for patient use and others are designed for clinicians to use with patients.
Decision aids have rapidly been developed by organizations such as AHRQ, the NCI, the Informed Medical Decisions Foundation, Healthwise, and many others (MedPAC, 2010). Estimates suggest that there are more than 500 decision aids currently available (Elwyn et al., 2006; OHRI, 2013). In the cancer setting, one of the most recognized decision aids is Adjuvant! Online. Clinicians and patients use Adjuvant! Online to assess the risk of an individual patient developing a recurrence and/or dying from breast cancer within 10 years of their diagnosis in order to guide decisions about adjuvant treatment for breast cancer (chemotherapy, endocrine therapy, or none) (Gribbin and Dewis, 2009). The Informed Medical Decisions Foundation’s website includes a number of decision aids relevant to cancer, including those for breast cancer, prostate cancer, and end-of-life decisions, as well as screening aids for colorectal cancer and prostate cancer (Informed Medical Decisions Foundation, 2012b). PCORI also supports research on decision aids (PCORI, 2013a). Oshima Lee and Emanuel (2013) have suggested that PCORI’s research on the effectiveness of shared decision-making techniques could be broadly disseminated to improve the development of future decision aids.
There are a number of ongoing efforts to improve shared decision making. The University of California, San Francisco, and the Dartmouth-Hitchcock Medical Center, for example, offer decision support programs for patients with breast cancer (see Box 3-2), and in 2007, Washington state became the first state to enact legislation promoting the use of shared decision making and decision aids in practice (Armstron and Arterburn, 2013). Group Health recently implemented a demonstration project using 12 video-based decision aids for elective surgical procedures and has since distributed more than 31,000 decision aids to participating patients. More
BOX 3-2
Examples of Decision Support Programs
University of California, San Francisco, Carol Franc Buck Breast Care Center
This program provides patients with information packets and decision aids to review prior to their medical appointments, as well as an intern who accompanies them throughout their consultation and treatment planning process. The interns generate a prioritized list of questions for the patients to ask their clinicians. They may also accompany patients to their medical appointments to record the discussion and write down answers doctors provide to their questions. The written answers are reviewed by the clinicians, put in the medical chart, and sent home with the patient, along with an audio recording of the visit.
Dartmouth-Hitchcock Medical Center
At this center, every breast cancer patient is referred to the Center for Shared Decision Making when first diagnosed. Patients complete online surveys to capture their medical and family history, how important it is to them to keep their breasts and avoid radiation, and other personal treatment-related preferences. The patients also watch a video with a decision aid that is appropriate for their situation. Following the video, patients are asked what treatment they prefer, how certain they are in their decision, and if they understand the survival and recurrence rates associated with their various treatment options. The collected information is entered into a clinical decision support system, which will alert the center’s clinicians to different actions based on the patients’ responses.
SOURCES: Informed Medical Decisions Foundation, 2012a; IOM, 2011a; UCSF Carol Franc Buck Breast Cancer Center, 2012.
than 65 percent of patients who undergo elective surgery at Group Health now use a decision aid (Armstron and Arterburn, 2013).
A Cochrane systematic review of 86 studies found that individuals who used decision aids had improved knowledge about their care options and more accurate expectations about potential benefits and harms, made decisions more consistent with their values, and were more engaged in their care compared to individuals who did not use decision aids (Stacey et al., 2011). In cancer care, a systematic review of 23 randomized clinical trials of cancer decision aids found that decision aids improved patient participation in decision making and resulted in higher-quality medical decisions (Stacey et al., 2008). For example, a randomized controlled trial found that Adjuvant! Online made a difference in patients’ decisions on whether or not to take adjuvant therapy and resulted in treatment decisions that were more tailored to patient preferences (Siminoff et al., 2006). Video decision aids have also been effective in the cancer setting in pro-
moting patients’ understanding of end-of-life care options (El-Jawahri et al., 2010; Volandes et al., 2013). Decision aids that provide information on prognosis are acceptable and desired among patients with metastatic cancer (Chiew et al., 2008; Smith et al., 2011), and these decision aids improve knowledge without creating anxiety (Leighl et al., 2011) or diminishing hope (Smith et al., 2010).
In addition, decision aids may reduce the cost of care (The Commonwealth Fund, 2007; Oshima Lee and Emanuel, 2013). One study found that individuals who used decision aids had 5.3 percent lower overall medical costs compared to individuals who had received standard of care (Veroff et al., 2013). Some savings from shared decision making could result from patients opting for less aggressive interventions that are more aligned with their needs, values, and preferences (Covinsky et al., 2000; El-Jawahri et al., 2010; Oshima Lee and Emanuel, 2013; Veroff et al., 2013). Because of these benefits, the committee recommends that the NCI, CMS, PCORI, as well as patient advocacy organizations, professional organizations, and other public and private stakeholders, improve the development of decision aids and make them available through print, electronic, and social media.
To ensure the development and dissemination of high-quality decision aids, it may be beneficial to have a mechanism for quality control. Oshima Lee and Emanuel (2013) called upon CMS to begin certifying patient decision aids in order to (1) promote an ideal approach to patient-clinician decision making, (2) improve the quality of health care decisions, and (3) reduce the cost of health care. Other groups have also developed criteria to evaluate decision aids (Elwyn et al., 2006). This mechanism for quality control may be met by Section 3506 of the ACA, which calls for HHS to establish a program that would facilitate shared decision making. Although this program would be responsible for developing, certifying, and disseminating patient decision aids, it has not yet been funded (Informed Medical Decisions Foundation, 2013).
The cancer community could also promote more widespread use of high-quality decision aids by addressing barriers in uptake among patients and clinicians. Clinicians lack incentives to use decision aids in their practices and have limited training in their use (Lin et al., 2013). King and Moulton (2013) noted that the Group Health demonstration project overcame clinician reluctance to using decision aids by changing institutional culture, presenting patient satisfaction data to clinicians, and providing decision aid training. Additional research on patient use of decision aids could inform interventions designed to broaden the reach of these decision aids (Belkora et al., 2011; Partin et al., 2006).
Prioritizing Clinician Training in Communication
Communication is a core responsibility for clinicians and the Accreditation Council for Graduate Medical Education expects medical residents to demonstrate competency in communication (ACGME, 2008; Moore et al., 2013). As discussed previously, clinicians need to communicate effectively with patients to build patient-clinician relationships focused on trust and rapport, as well as to exchange information, respond to patient emotions, manage the uncertainty associated with a cancer diagnosis and treatment, participate in shared decision making, and enable patient self-management (Epstein and Street, 2007). Effective communication is associated with patients experiencing faster recovery, improved pain control, and better psychological functioning; ineffective communication is associated with patient anxiety, uncertainty, and dissatisfaction with cancer care (reviewed in Moore et al., 2013). In addition, the availability of clinical and cost information is insufficient to assist patients in making decisions consistent with their needs, preferences, and values. It is also critically important for clinicians to provide patients with the opportunity to discuss this information in real time with members of the cancer care team. Technology-enabled approaches, such as telemedicine, may increase the opportunity for patients to have these interactions (see Chapter 4).
Many clinicians, however, are not trained to communicate well and many patients with cancer have unmet communication needs (Hack, 2005). Kissane et al. (2012) noted that medical schools teach generic communication skills, but the cancer setting requires specialty communication skills training, including breaking bad news, discussing prognosis and risk, using shared decision making to make care plans, responding to emotions, dealing with recurrence, changing treatment goals, running a family meeting, and discussing death and dying. Because cancer is a life-threatening condition, giving bad news, such as discussing a poor prognosis, recurrence, or progression, is a common clinician task. But clinicians are rarely trained to have these difficult conversations with patients (Baile et al., 2000; Oncotalk, 2002; Orlander et al., 2002; Quill and Townsend, 1991; Wittenberg-Lyles et al., 2013). A survey of oncologists found that less than 10 percent reported formal training in breaking bad news and only 32 percent had the opportunity during training to regularly observe other clinicians break bad news to patients (Baile et al., 2000).
Given the importance of communication in the cancer setting, the committee recommends that professional educational programs for members of the cancer care team should provide comprehensive and formal training in communication. A Cochrane systematic review assessing communication skills training in cancer found that this training is effective and improves clinician empathy and use of open-ended questions
(Moore et al., 2013). Additional research will be needed to understand the link between clinician communication training and improved patient outcomes (Moore et al., 2013; Uitterhoeve et al., 2010). However, there is some evidence on how to train clinicians most effectively.
Many clinicians learn communication skills by watching mentors communicate with patients or through didactic approaches, but research indicates that there are more effective methods of improving communication skills (Back et al., 2009a, 2010; Berkhof et al., 2010). Key attributes of effective communication skills training include (1) recognition and definition of the essential skills in communication (for example, demonstrating empathy, using open-ended questions, and assessing psychosocial care needs); (2) opportunities for clinicians to practice communication skills through role-playing; (3) thoughtful feedback from skilled communicators; (4) self-reflection through video and audio recordings; and (5) continued practice of communication skills (Back et al., 2009a; Moore et al., 2013).
Communication skills training has been delivered in a number of formats, including sessions integrated into a degree program, as well as multi-day workshops (Moore et al., 2013). Epstein and Street (2007) suggested that communication training should be introduced as early as possible in medical and nursing education, because clinicians immediately start establishing routines for interacting with patients. Additional research is necessary to assess the duration of effectiveness of this training (Moore et al., 2013).
There are a number of challenges to implementing communication skills training. Compared to other types of clinician training that test knowledge to assess improvement, it is more difficult to measure improvements in communication skills. The diversity of settings in which communication skills training occurs (i.e., medical and nursing schools, residency programs, and clinical practice), along with the various levels of exposure that clinicians have to communication skills training, may also make it difficult to implement. In addition, communication skills training needs to be reinforced over time, but there is a lack of information regarding how often this should occur. There is also uncertainty regarding the scalability of current communication programs, given the resources needed to establish a communication skills training program, measure performance, and evaluate outcomes. Additional communication training could be supported through the NCI R25 mechanism (NCI, 2013a), but Kissane et al. (2012) argued that this funding is unlikely to sustain these programs over time. The importance of communication to new models of payment, however, may spur investment in communication skills training (see Chapter 8).
In addition, a number programs and models are available to improve
clinician communication skills in the cancer setting. Oncotalk®8 uses a series of learning modules (e.g., fundamental communication skills, giving bad news, discussing treatment options, and informed consent, etc.) to teach clinicians about specific communication tasks, provide suggestions for implementing these skills, and review recommended sources for more information. One of the communication approaches advocated by Oncotalk is the ask-tell-ask method, which has clinicians ask their patients to describe their understanding of an issue by using prompts such as, “to make sure we are on the same page, can you tell me what your understanding of your disease is?” The process of asking for this information can improve the patient-clinician relationship, demonstrate a clinician’s willingness to listen, and help direct the conversation. Next, clinicians tell their patients the information that needs to be conveyed in straightforward language, breaking down the information so that it is not overwhelming to the patient. In the final step, clinicians ask patients if they understand the information, which acts as a check to see if patients received the information the clinician tried to impart and provides an opportunity for patients to ask questions (Back et al., 2009b). An evaluation of Oncotalk found that the program was a successful teaching model for improving communication skills in postgraduate medical trainees (Back et al., 2007).
Another approach to communication emphasized in the palliative care setting for nurses is the COMFORT model (Communicate, Orientation and opportunity, Mindful presence, Family, Openings, Relating, and Team) (Goldsmith et al., 2013; Wittenberg-Lyles et al., 2013). This approach builds a number of communication skills, including practicing empathy, engaging in interdisciplinary collaboration, gauging health literacy, and recognizing the patient and family in palliative care interactions.
Communicating Information and Preparing Cancer Care Plans
To achieve high-quality cancer care, the cancer care team needs to effectively communicate and engage in shared decision making with patients to ensure that patients understand their disease, know their care options, and develop a plan for care. The committee recommends that the cancer care team provide patients and their families with understandable information on cancer prognosis, treatment benefits and harms, palliative care, psychosocial support, and estimates of the total and out-of-pocket costs of cancer care. The cancer care team should communicate and personalize this information for their patients at key decision points along the continuum of cancer care, using decision aids
________________
8 See http://depts.washington.edu/oncotalk (accessed January 3, 2013).
when available. The American Board of Internal Medicine’s (ABIM’s) Charter for medical professionalism highlights the fundamental importance of communication with patients such that “patients are completely and honestly informed … [and] empowered to decide on the course of therapy” (ABIM, 2013).
The cancer care team personalizes this information for patients by ensuring that the communication approach takes into account a patient’s language, health literacy, and informational and emotional needs. Health literacy toolkits may help clinicians more effectively convey understandable information to their patients (AMA, 2013; DeWalt et al., 2010; LINCS, 2013). In addition, several IOM workshops highlighted some methods that clinicians could use to present complicated information to patients in a format that facilitates comprehension (see Table 3-3).
Patient-clinician communication is especially important when patients and their families need to make specific decisions about their care. This includes key decision points, such as at the time of initial diagnosis, when patients experience cancer progression or recurrence, following treatment, or when the goals of care or patient preferences change.
Cancer care plans facilitate clinicians’ communication of this information because they provide patients and their families with a roadmap to navigate their cancer care. They can also facilitate coordinated care by summarizing all relevant information into a single location that can be shared among members of the cancer care team, the primary care/ geriatrics care team, and other clinicians involved in a patient’s care. Additionally, cancer care plans can encourage patient participation in decisions about their care and help patients retain important information by providing a summary of key information (IOM, 2011a).
The IOM report Ensuring Quality Cancer Care recommended that patients with cancer have “an agreed-upon care plan that outlines the goals of care” (IOM and NRC, 1999, p. 7). The IOM also recommended care plans for cancer survivors completing primary treatment (IOM and NRC, 2005). More recently, an IOM workshop highlighted the importance of care planning for promoting patient-centered communication and shared decision making (IOM, 2011a). Thus, the committee recommends that the cancer care team collaborate with their patients to develop a care plan that reflects their patients’ needs, values, and preferences, and considers palliative care needs and psychosocial support across the cancer care continuum. Involvement of patients’ primary/geriatrics and specialist care teams may also be helpful in developing a care plan, especially for patients with comorbidities.
Currently, the evidence base for care plans is limited and primarily related to survivorship care plans rather than care plans for ongoing cancer care. The IOM report From Cancer Patient to Cancer Survivor: Lost in Transi-
| Strategy | Description |
| Absolute risk | Patients and caregivers are better at comprehending absolute risk than relative risk. Relative risk compares risk in two different populations. For example, people who smoke are about 15 to 30 times more likely to develop lung cancer or die from lung cancer compared to people who do not smoke. In contrast, absolute risk represents an individual’s overall risk. For example, the risk that a woman who is 40 years old will be diagnosed with breast cancer during the next 10 years is 1.47 percent (or 1 in 68 women). |
| Graphical formats | Graphs can help patients and caregivers comprehend risk. Some graphical formats are easier for patients and caregivers to interpret. For example, pictographs (or diagrams representing statistical data in pictorial form) improve patients’ and caregivers’ comprehension compared to bar graphs or pie charts. |
| Rare events | Comparing the likelihood of a medical event to the likelihood of a commonly understood rare event can help patients and caregivers understand risk. For example, “an individual has a 1 in 10,000,000 chance of getting struck by lightning, and about a 1 in 100 chance of dying if they smoke 10 cigarettes a day for one year.” |
| Multiple formats | Presenting patients and caregivers with complicated information in multiple formats improves comprehension. For example, clinicians can present information as both percentages and as frequencies, and numerical information can be presented both orally and visually (e.g., in a graph). |
| Read back | When clinicians ask their patients to repeat back the information they heard, rather than just ask whether they understood the information, comprehension improves. Repetition requires patients to demonstrate to the clinicians that they understand the information. It also gives clinicians the opportunity to clarify information or emphasize necessary details. |
| Videos | Clinicians can use videos to provide realistic visual images of various treatment options and outcomes. For example, a study evaluating the effect of a video on the cardiopulmonary resuscitation (CPR) preferences of patients with advanced cancer found that patients who watched the video had improved knowledge of CPR and more confidence in their health care decisions, compared to patients who did not watch the video. |
SOURCES: CDC, 2013; El-Jawahri et al., 2010; Gigerenzer and Edwards, 2003; IOM, 2009a, 2011b; NCI, 2012; Peters et al., 2007; Volandes et al., 2013.
tion argues that even though there is limited evidence to support survivorship care plans, “some elements of care simply make sense—that is, they have strong face validity and can reasonably be assumed to improve care” (IOM and NRC, 2005). Only one randomized clinical trial on survivorship care planning has been published (Grunfeld et al., 2011), which found that survivorship care plans were not beneficial for improving patient-reported outcomes. However, the validity and generalizability of this study has been questioned (Parry et al., 2013). Moreover, the relevance of this finding on care plans in the treatment setting is unknown. CMS recognizes the promise of care planning and is in the process of implementing a new Medicare payment policy to reward care planning delivered in the context of a patient-centered medical home for patients with complex chronic conditions (Bindman et al., 2013). Bindman and colleagues note that the “care plan is based on a physical, mental, cognitive, psychosocial, and functional and environmental (re)assessment of the patient and on an inventory of resources and supports available to the patient.” The need to consider multiple treatment modalities, facilitate shared decision making, and coordinate care in the cancer treatment setting suggests that care plans may prove especially beneficial there.
Documenting information in a patient’s care plan is insufficient to ensure patient-centered communication and shared decision making. Parry and colleagues (2013) noted that “much like electronic health records, care plans are vehicles for communication and coordination of care, nothing more. We cannot expect a document to do the work of a process, and we certainly cannot expect it to fix a flawed process” (p. 2651). The care plan is a tool to facilitate communication and shared decision making, care coordination, and retention of the path of care. Equally important to the care plan itself are the conversations that a patient and clinician have regarding a patient’s cancer care. Improving clinician training in communication will be essential to implementing the committee’s recommendation on cancer care planning.
Progress on implementing cancer care planning is under way. CMS has established two new Healthcare Common Procedure Coding System codes for cancer treatment planning and care coordination related to initial treatment and change of treatment (NCCS, 2012b). In June 2013, the Planning Actively for Cancer Treatment (PACT) Act of 2013 was introduced in the U.S. House of Representatives.9 This bill would provide Medicare coverage for cancer care planning and coordination services, including the development of a written plan for cancer treatment. A number of cancer organizations have endorsed the PACT Act of 2013,
________________
9 H.R. 2477. Planning Actively for Cancer Treatment (PACT) Act of 2013. 113th Cong. 1st. sess. (June 25, 2013).
including the American Cancer Society Cancer Action Network, ASCO, LIVESTRONG, the National Coalition for Cancer Survivorship, and the National Comprehensive Cancer Network (NCCS, 2013).
Care Plan Components
Cancer care plans document information about a patient’s diagnosis and prognosis, the planned path of care, and who is responsible for each portion of that care. Box 3-3 lists examples of typical features of cancer care plans, and the section below elaborates on a number of critical fea-
BOX 3-3
Information in a Cancer Care Plan
Utilizing patient-centered communication and shared decision making, the cancer care team should collaborate with patients to develop a cancer care plan. Examples of components in a patient-specific cancer care plan include
• Patient information (e.g., name, date of birth, medication list, and allergies)
• Diagnosis, including specific tissue information, relevant biomarkers, and stage
• Prognosis
• Treatment goals (curative, life-prolonging, symptom control, palliative care)
• Initial plan for treatment and proposed duration, including specific chemotherapy drug names, doses, and schedule as well as surgery and radiation therapy (if applicable)
• Expected response to treatment
• Treatment benefits and harms, including common and rare toxicities and how to manage these toxicities, as well as short-term and late effects of treatment
• Information on quality of life and a patient’s likely experience with treatment
• Who will take responsibility for specific aspects of a patient’s care (e.g., the cancer care team, the primary care/geriatrics care team, or other care teams)
• Advance care plans, including advanced directives and other legal documents
• Estimated total and out-of-pocket costs of cancer treatment
• A plan for addressing a patient’s psychosocial health needs, including psychological, vocational, disability, legal, or financial concerns and their management
• Survivorship plan, including a summary of treatment and information on recommended follow-up activities and surveillance, as well as risk reduction and health promotion activities
SOURCES: IOM, 2011a; IOM and NRC, 2005.
tures, including clinical and cost information, palliative care, psychosocial support, and advance care planning. Care plans should be updated when new information becomes relevant, such as changes in treatment response or patient preferences. Further research on care plans will also be needed, including the optimal presentation of this information and the relationship between care plans and patient-clinician communication and shared decision making, among other topics. Table 3-4 illustrates an example of a care plan for cancer, which could be imported into electronic health records (EHRs) and shared with patients.
Clinical information. The clinical information that the cancer care team discusses with patients should include all relevant information for patients to make decisions about their care options, including cancer prognosis, likelihood of treatment response, treatment benefits and harms, and likely experience with a treatment. The prognostic information should include specifics about curability, response rates for various treatment options, and a treatment’s impact on survival as well as quality of life.
Palliative care. Palliative care is defined as “patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and facilitating patient autonomy, access to information, and choice” (NQF, 2006, p. 3).
Palliative care has the following characteristics:
• Care is provided and services are coordinated by an interdisciplinary team;
• Patients, families, and palliative and non-palliative health care clinicians collaborate and communicate about care needs;
• Services are available concurrently with or independent of curative or life-prolonging care; and
• Clinicians respect their patients and families’ dignity throughout the course of illness, during the dying process, and after death.
Despite the importance of palliative care in improving the quality of patients’ lives, clinicians often fail to address patients’ palliative care needs in their care plans. Clinicians often equate palliative care with end-of-life care and consider it an alternative, rather than a complement, to curative or life-extending treatment (see Box 3-4). However, palliative care services may be introduced at any point along the continuum of cancer care as a critical layer of support that is delivered concurrently
TABLE 3-4 Example of a Written Plan for Communication
| Plan component | Purpose |
| Name_____ | Lets the cancer care team personalize each patient’s plan; make a copy for the medical record. |
| Medical Record No._____ Date_____ |
|
| 1. Diagnosis:_____ | Gives the disease a name so the patient can look it up. |
| 2. Stage (where it has spread):_____ (list all areas) |
Allows discussion of prognosis. Showing metastases to the brain and liver quickly points out the seriousness of the illness. |
| 3. Prognosis:_____ List whether curable or not curable and expected average lifespan |
Allows the cancer care team to ask first if patients want to know the full details of their illness! Allows open communication about goals, rest-of-life planning. Some patients will persist in denial, but this allows open dialogue with the family. |
| 4. Treatment Goals:_____ List cure, long-or short-term control, pain relief, hospice care |
Makes explicit what the cancer care team can and cannot do; for curable disease, this reinforces the patient’s goal, and that cure is possible. The cancer care team can use this to bring up do-not-resuscitate and cardiopulmonary resuscitation issues. Allows the cancer care team to emphasize that hospice care does not mean “no treatment,” but a different set of treatment goals. |
| 5. Treatment Options:_____ List all that apply |
The cancer care team should list treatments, response rates, and common toxicities. The cancer team should specifically mention vomiting and hair loss, the two most feared symptoms. If the cancer care team cannot define a real benefit then there is no justification for treatment. |
| 6. Call the doctor if:_____ List the threshold for fever, pain, and other symptoms |
Gives patients explicit reasons to call their cancer care team and gives explicit permission to call. |
| 7. How to reach me:_____ List the phone numbers during office and off-hours |
The cancer care team should tell patients to keep this handy. They will call, and for real events. Emails for nonemergency purposes work well for prescription refills, questions about new drugs, encouragement, etc. |
| 8. Signed:_____, MD | Personalizes the plan as well as making it a part of the medical record. |
SOURCE: Adapted from Smith, T.: J Clin Oncol 21(9 Suppl), 2003: 12s-16s. Reprinted with permission. © 2003 American Society of Clinical Oncology. All rights reserved.
BOX 3-4
Challenges to the Delivery of Palliative Care Across the Cancer Care Continuum
In this report, the committee utilizes the term palliative care and adopts the National Quality Forum’s definition: “patient-and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and facilitating patient autonomy, access to information, and choice” (NQF, 2006, p. 3). The committee conceptualizes palliative care as an added layer of support that can be delivered concurrently with other therapeutic treatment modalities to improve quality of life for cancer patients.
A lack of awareness about palliative care and definitional challenges reduce patients’ access to palliative care across the cancer care continuum. A recent survey found that 70 percent of the public had no knowledge about palliative care, but once informed, 95 percent of respondents agreed that patients with serious illness should be informed about palliative care (Center to Advance Palliative Care, 2011).
Although the general public has little knowledge about palliative care, clinicians often conflate palliative care with hospice care (Center to Advance Palliative Care, 2011; Meier, 2012). Thus, clinicians often neglect recommending palliative care until late in the cancer care continuum. Studies suggest that some oncology clinicians prefer the term supportive care as opposed to palliative care, and if the name were changed, clinicians would be more likely to refer patients earlier in the cancer care continuum (Dalal et al., 2011; Hui et al., 2013; Wentlandt et al., 2012). However, others have asserted that changing the name risks even more confusion: “Rather than changing the name from ‘palliative care,’ risking ambiguity and confusion, we believe that improved communication is key to appropriate engagement with palliative care services” (Milne et al., 2013).
with therapeutic treatment modalities to improve quality of life for cancer patients (Ferris et al., 2009; Hennessy et al., 2013; Spinks et al., 2012). In a provisional clinical opinion, ASCO endorsed the provision of palliative care concurrent with usual cancer care (Smith et al., 2012). This concept is illustrated in Figure 3-3, showing palliative and life-prolonging care being delivered simultaneously. Generally, the majority of a patient’s care is initially focused on life-prolonging therapy, but as a patient’s disease progresses, palliative care takes on a more prominent role. However, individuals’ need for palliative care may vary throughout their disease trajectory. For example, a patient may require more palliative care early in treatment (during chemotherapy or following surgery or radiation treatment) and then have lower palliative care needs during periods of remission.
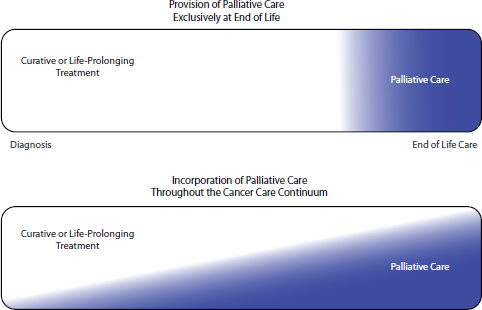
FIGURE 3-3 Relationship of curative or life-prolonging treatment to palliative care for cancer. In current practice, there is often a single focus on curative or life-prolonging treatment, with palliative care provided only near the end of life. The committee’s framework of high-quality cancer care incorporates palliative care throughout the cancer continuum, becoming more intensive toward the end of life.
SOURCE: Adapted from IOM, 1997.
There is strong evidence to support the provision of palliative care throughout the cancer care continuum. Early palliative care referral has been associated with bitmapped improved uneditable, symptom with type management patches (Bandieri et al., landscape 2012; Temel et al., 2010), increased survival time (Temel et al., 2010), lower utilization of aggressive end-of-life care (Greer et al., 2012; Temel et al., 2010), and more accurate patient expectations regarding long-term prognoses (Temel et al., 2011). Despite these benefits, clinicians often do not refer their patients to palliative care until the last 2 months of life (Cheng et al., 2005; Osta et al., 2008). At one comprehensive cancer center, fewer than half of patients received a palliative care consultation before they died, and palliative care consultations occurred late in the disease process (Hui et al., 2012).
Inclusion of palliative care in the cancer care plan will help improve patient access to palliative care across the cancer continuum. Addressing palliative care needs is also critical for high-quality end-of-life care. This is discussed in greater depth in the sections below on Emphasizing Palliative Care and Psychosocial Support and Providing Timely Referred Hospice Care.
Psychosocial support. Care plans should address a patient’s psychosocial health needs (see Table 3-5). Many patients with cancer have unmet psychosocial needs, and patients with cancer report that their clinicians often do not understand their psychosocial needs; do not consider psychological support as a component of cancer care; and fail to recognize, treat, or refer patients to psychosocial services (IOM, 2008a). The committee endorses the recommendations in the IOM report Cancer Care for the Whole Patient, which stated that the cancer care team should identify each patient’s psychosocial health needs and design and implement a care plan that (1) links the patient and family with psychosocial services; (2) coordinates biomedical and psychosocial care; and (3) engages and supports patients in managing their illness and health (IOM, 2008a).The psychosocial care plan should be revisited across the cancer care continuum, as these needs are likely to change depending on a patient’s circumstances. Meeting psychosocial health needs in end-of-life care is especially important, as discussed below. Chapter 4 elaborates on the workforce providing psychosocial support to patients with cancer.
Cost. The cancer care team should discuss the total and out-of-pocket cost of cancer care with patients. There is a growing recognition of the role of care teams in discussing cost with their patients as a critical aspect of patient-centered communication and shared decision making (Moriates, et al., 2013). The American Society of Clinical Oncology’s (ASCO’s) policy statement states that “communication with patients about the cost of care is a key component of high quality care” (Meropol et al., 2009, p. 3871). Discussing costs “openly, in a way that allows patients an opportunity to hear the justification for cost-conscious decisions and to be active agents in thinking through treatment choices when feasible, is consistent with physicians’ ethical duties to be transparent with patients and provide patient-centered care” (Sommers et al., 2013, p. 344). Additional experts have asserted that “‘financial toxicity’ as a result of disease or treatment decisions might be considered analogous to physical toxicity and might be considered a relevant variable in guiding cancer management” (Zafar et al., 2013, p. 381).
Because cancer treatment can be a large financial burden, cost is an important issue for many patients and families (Bernard et al., 2011; IOM, 2013; Stump et al., 2013). A survey found that more than a third of individuals reported that medical problems were the reason for bankruptcy, even though three out of four families studied had insurance at the onset of illness (Himmelstein et al., 2009). Cancer patients, especially those under 65 years, have a higher bankruptcy rate compared to people who do not have cancer (Ramsey et al., 2013). Another study of patients undergoing adjuvant treatment for regional colon cancer found that 38
TABLE 3-5 Psychosocial Needs and Formala Services to Address Them
| Psychosocial Need | Health Services |
| Information about illness, treatments, health, and services |
• Provision of information (e.g., on illness, treatments, effects on health, and psychosocial services) and help to patients/families in understanding and using the information |
| Help in coping with emotions accompanying illness and treatment |
• Peer support programs • Counseling/psychotherapy to individuals or groups • Pharmacological management of mental symptoms |
| Help in managing illness |
• Comprehensive illness self-management/self-care programs |
| Assistance in changing behaviors to minimize impact of disease |
• Behavioral/health promotion interventions, such as:
|
| Material and logistical resources, such as transportation |
• Provision of resources |
| Help in managing disruptions in work, school, and family life |
• Family caregiver education • Assistance with activities of daily living (ADLs), instrumental ADLs, chores • Legal protections and services (e.g., under Americans with Disabilities Act and Family and Medical Leave Act) • Cognitive testing and educational assistance |
| Financial advice and/or assistance |
• Financial planning/counseling, including management of day-to-day activities such as bill paying • Insurance (e.g., health, disability) counseling • Eligibility assessment/counseling for other benefits (e.g., Supplemental Security Income, Social Security Disability Income) • Supplemental financial grants |
aFamily members and friends and other informal sources of support are key providers of psychosocial health services. This table includes only formal sources of psychosocial support—those that must be secured through the assistance of an organization or agency that in some way enables the provision of needed services (sometimes at no cost or through volunteers).
SOURCE: Adapted from IOM, 2008a.
percent of patients reported at least one treatment-related financial hardship (Shankaran et al., 2012).
The committee recognizes that there are a number of challenges to discussing the cost of care. Both clinicians and patients can be reluctant to broach the subject of cancer care costs (Neumann et al., 2010; Sommers et al., 2013). For example, a survey of oncologists found that only 43 percent always or frequently discuss the cost of cancer care with patients (Neumann et al., 2010). Clinicians may not explain the potential cost implications for different cancer care options because these discussions are time consuming and not prioritized under the current reimbursement system (see Chapter 8). In addition, some clinicians may not know the total costs involved in cancer care or the out-of-pocket costs for which patients may be responsible, given the variable insurance plans with differing benefit packages. However, a recent survey found that 76 percent of physicians were “aware of the costs of the tests/treatments [they] recommend” (Tilburt et al., 2013), and oncologists have reported that their incomes increase when they administer chemotherapy and growth factors (Malin et al., 2013). Because exact information may not always be available, the cancer care team should provide patients with estimates of the total and out-of-pocket costs of cancer care.
Another challenge to discussing cost information with patients is the possibility that some patients may reject potentially beneficial cancer care due to cost concerns. However, this information is important for patients to make informed decisions about their care. Patients may not be aware of their out-of-pocket costs until after care is provided, but discussing these costs prior to cancer care could facilitate more fully informed decisions. If patients have multiple treatment options to consider, the cancer care team should provide patients with information that compares the relative costs of these different options. In addition, providing information on the total cost of care can enable cost-conscious patients to consider equally effective, lower cost cancer care options.
Given time constraints for clinicians, nonclinician practice staff, such as financial counselors or other administrative practice staff, may be helpful in communicating with patients about the cost of cancer care. Some oncology practices have already started employing financial counselors who inform patients about the total costs of cancer treatment, their insurance benefits, and anticipated out-of-pocket costs for treatment (Gesme and Wiseman, 2011). New models of payment may also help facilitate this change.
Advance care planning. Advance care planning is defined by the National Hospice and Palliative Care Organization as “making decisions about the care you would want to receive if you happen to become unable to speak
for yourself” (NHPCO, 2013, p. 1). The cancer care team should discuss advance care planning with patients and document these preferences in the care plan. Advance care planning should begin early in the cancer care continuum and be revisited under changing circumstances, such as when patients’ cancers progress, or they change their preferences. It may be helpful for the cancer care team to work with the primary care/geriatrics care team in advance care planning, because the primary care/geriatrics care team may have a more established relationship with a patient and be better suited to eliciting their patients’ preferences. The cancer care team should then implement their patients’ advance care plans if their patients lose decisional capacity at any point in the course of illness. (Also see the section below on “Implementing Advance Care Planning.”)
Advancing New Payment Models
The committee recommends that CMS and other payers design, implement, and evaluate innovative payment models that incentivize the cancer care team to discuss information on cancer prognosis, treatment benefits and harms, palliative care, psychosocial support, and estimates of the total and out-of-pocket costs of cancer care with their patients and document their discussions in each patient’s care plan. As mentioned previously, the current fee-for-service reimbursement system does not compensate the cancer care team well for providing cognitive care to their patients, such as having conversations about prognosis, likelihood of treatment responses, and support services for patients. Because it can result in care that is misaligned with their preferences and contribute to unnecessary or harmful interventions, the current reimbursement system is detrimental to the quality of care that patients with cancer receive. In Chapter 8, the committee elaborates on new delivery and payment models that could incentivize better patient-clinician communication and shared decision making, including oncology patient-centered medical homes, ACOs, and bundled payments. These models reward the cancer care team for the quality, patient-centeredness, and efficiency of care they provide. Effective patient-clinician communication will be necessary in these models to avert potentially costly complications. In addition, these models are designed to disincentivize clinicians from using more (or more costly) interventions when they are unlikely to benefit a patient.
Financial incentives in fee-for-service reimbursement can also hinder the provision of palliative care and psychosocial support across the cancer continuum. The current system incentivizes clinicians to provide highly interventional care, because interventional care is reimbursed more generously than palliative care and psychosocial support. A previous IOM committee highlighted the deficiencies of fee-for-service reimburse-
ment in the provision of palliative care and recommended that new payment models be considered (IOM, 1997). This committee makes a similar recommendation.
IMPROVING PATIENT-CENTERED COMMUNICATION AND SHARED DECISION MAKING AT THE END OF LIFE
Patients with advanced cancer confront “complex physical, psychological, social, and spiritual consequences of disease and its treatment” (Peppercorn et al., 2011, p. 755). And, too often, patients with advanced cancer receive suboptimal care. This section describes challenges and opportunities to improve cancer care for individuals approaching the end of life, including the importance of palliative care, psychosocial support, advance care planning, end-of-life communication, and timely referral to hospice.
A related activity is an IOM consensus committee on transforming end-of-life care. That committee is currently examining issues in end-of-life care, including advance care planning, patient-clinician communication of values and preferences, and health care financing and reimbursement. The report is expected to be released in 2014.
Implementing Advance Care Planning
Advance care planning is “making decisions about the care you would want to receive if you happen to become unable to speak for yourself” (NHPCO, 2013, p. 1). Ideally, all patients should have an advance care plan in place, prior to diagnosis, as a routine part of medical care. Advance care planning is also a part of a patient’s care plan. The cancer care team should discuss advance care planning early in the course of a patient’s care and implement the plan when needed. The ASCO policy statement on advanced cancer recommends that “[a]ll patients must have a regular opportunity to make their preferences about how to live their final weeks and months clear to their oncologist. Only through these discussions do we have an opportunity to match patients’ goals with the actual care delivered” (Peppercorn et al., 2011, p. 757).
Components of advance care planning include consideration of what types of life-sustaining treatments align with a patient’s preferences, preparation of advance directives, and identification of a health care proxy. Advance directives are “formal legal documents specifically authorized by state laws that allow patients to continue their personal autonomy and that provide instructions for care in case they become incapacitated and cannot make decisions” (AHRQ, 2013a, p. 1). A health care proxy is a document that “allows the patient to designate a surrogate, a person who
will make treatment decisions for the patient if the patient becomes too incapacitated to make such decisions” (AHRQ, 2013a, p. 1).
Advance care planning is an opportunity for cancer care teams to engage with their patients to make more informed decisions about care that is aligned with a patient’s needs, values, and preferences and can help maximize quality of life for the time a patient has left (IOM, 2011a). Patients who discuss advance care planning with their clinicians are more likely to receive end-of-life care that is consistent with their preferences (Detering et al., 2010; Mack et al., 2010; Silveira et al., 2010).
Advance care planning, however, is currently underutilized. Many discussions with patients about advance care planning occur during acute hospital care with clinicians other than oncologists late in the course of disease (Mack et al., 2012a). In addition, estimates suggest that only around half of individuals have an advance directive in their medical record (reviewed in AHRQ, 2003; Wilson et al., 2013; Yung et al., 2010). As a result, clinicians may provide end-of-life care that is not aligned with their patients’ preferences. For example, 70 percent of people say they want to die at home, but 70 percent of people die in hospitals or nursing homes (Goodman, 2012). A study found that the patients’ expressed preferences for end-of-life care and documentation of this information in the medical record matched only 30 percent of the time (Heyland et al., 2013). Surveys also suggest that many patients, particularly older patients, would prefer care focused on comfort over life-extending care (see the sections below on Emphasizing Palliative Care and Psychosocial Support and Providing Timely Referred Hospice Care) (Barnato et al., 2007; Maida et al., 2010; Rose et al., 2004), but end-of-life care for cancer patients is often intensive (Morden et al., 2012). Allison and Sudore (2013) assert that failure to discuss and document patient preferences for end-of-life care is tantamount to a medical error. Thus, the committee recommends that in the setting of advanced cancer, the cancer care team should revisit and implement their patients’ advance care plans to provide patients with end-of-life care consistent with their needs, values, and preferences (Recommendation 2).
Many efforts to improve advance care planning are under way. In 2013, the Personalize Your Care Act was introduced in the U.S. House of Representatives.10 This act would provide Medicare and Medicaid patients with coverage for voluntary advance care planning consultations. It would also direct the Secretary of HHS to develop standards for EHR documentation of the result of advance care planning discussions. Currently, EHRs often do not record patients’ decisions made during advance care planning in an actionable format (Tai-Seale et al., 2012). Although this
________________
10 Personalize Your Care Act of 2013, H.R. 1173, 113th Cong., 1st Sess. (March 14, 2013).
act would greatly improve the availability of advance care planning, its likelihood of passing Congress is unknown. Previous Congressional efforts to improve advance care planning have been very controversial and failed to become law (Tinetti, 2012).
The most evidence-based and widespread model of advance care planning is Respecting Choices®, which was developed by health care organizations in La Crosse, Wisconsin. This model incorporates six goals into routine care: (1) patients are invited to understand and discuss plans for future health care; (2) patients are supported by trained nonclinicians in the planning process; (3) patients develop plans that are specific and understandable to all stakeholders; (4) plans are accessible wherever a patient is treated; (5) plans are updated and become more specific as a patient’s illness progresses, and (6) clinicians review and honor plans at the right time (Hammes et al., 2010). After 2 years of implementation, a retrospective analysis found that 85 percent of all adult decedents in La Crosse had an advance directive; 95 percent of the advance directives were in the patient’s medical record; and in 98 percent of the cases, instructions in the advance directive were consistent with care near the end of life (Hammes and Rooney, 1998). More recent data from La Crosse found even greater prevalence and accessibility of advance directives (Hammes et al., 2010).
There are also a number of grassroots educational campaigns, such as the Conversation Project and Honoring Choices Minnesota®, which are encouraging people to have honest conversations about their preferences for end-of-life care with their families (Bisognano and Goodman, 2013; Wilson and Schettle, 2013). The Conversation Project is also collaborating with the Institute for Healthcare Improvement to ensure that the health care delivery system is well prepared to elicit and respect patient preferences for end-of-life care (Bisognano and Goodman, 2013). Similarly, ASCO and Cancer.Net have prepared a booklet for patients and families about advance care planning for people with cancer (ASCO and Cancer.Net, 2012). As mentioned previously, videos may also assist patients in making more informed decisions about their care options at the end of life. For example, Volandes et al. (2013) found that patients with advanced cancer who viewed a video of cardiopulmonary resuscitation (CPR) were less likely to opt for CPR than those who listened to a verbal description of CPR.
Improving Clinician Training in End-of-Life Communication
The advanced cancer care setting presents a number of added challenges to patient-centered communication and shared decision making, particularly because conversations about the end of life are understandably difficult for both clinicians and patients (Harrington and Smith,
2008; IOM, 2009a; The et al., 2000). Clinicians, concerned that patients will become depressed or lose hope, are often reluctant to discuss realistic prognostic information with patients, despite evidence that patients want their clinicians to be honest and truthful (IOM, 2011a; Mack and Smith, 2012; Smith and Longo, 2012). Good communication about prognosis is especially important because a patient’s understanding of his or her illness is strongly linked to the treatment choices the patient makes. Patients with advanced cancer who understand that their disease is incurable are more likely to prefer symptom-directed care, while patients who overestimate their prognosis are more likely to receive disease-focused care with unclear benefit (Greer et al., 2013). The ASCO policy statement on advanced cancer care estimated that clinicians have realistic conversations with fewer than 40 percent of their patients with advanced cancer (Peppercorn et al., 2011). Clinicians often delay conversations about advance directives until there are no longer any curative or life-prolonging treatment options available to patients (Keating et al., 2010). One study found that as many as half of all non-small-cell lung cancer patients had not discussed hospice with any of their doctors 2 months prior to their deaths (Huskamp et al., 2009).
Given the need for better communication at the end of life and the effectiveness of communication training programs, the committee recommends that professional educational programs for members of the cancer care team provide comprehensive and formal training in end-of-life communication. These professional education programs need to be available both during initial training as well as for clinicians currently practicing. All clinicians working in oncology should be proficient at discussing these difficult issues.
Aligned with this recommendation, the IOM report Approaching Death: Improving Care at the End of Life (1997) recommended that educators and health professionals make changes to undergraduate, graduate, and continuing education programs to ensure that clinicians are well equipped to provide high-quality end-of-life care. The committee emphasized a number of interpersonal skills and attitudes that clinicians should develop, including listening to patients, families, and other members of the care team; conveying difficult news; understanding and managing patient and family responses to illness; providing information and guidance on prognosis and care options; practicing shared decision making and conflict resolution; recognizing and understanding the clinician’s own feelings and anxieties about dying and death; and demonstrating empathy and sensitivity to religious, ethnic, and other personal characteristics.
Emphasizing Palliative Care and Psychosocial Support
As discussed previously, high-quality cancer care includes the provision of palliative care and psychosocial support throughout the cancer continuum. In addition, the committee recommends that in the setting of advanced cancer, the cancer care team should place a primary emphasis on providing cancer patients with palliative care and psychosocial support for end-of-life care. Palliative care can be provided by a number of clinicians in a variety of settings, including the outpatient setting and inpatient hospital units (GPC, 2013a). Given the limited supply of palliative care clinicians and recognition that some palliative care tasks are routine aspects of care (see Chapter 4), Quill and Abernethy (2013) suggested a model of care that includes primary and specialty palliative care. In this model, the cancer care team would provide primary palliative care, including basic management of pain, symptoms, depression, and anxiety, as well as basic discussions about prognosis, goals of treatment, suffering, and advance directives. If patients require more complex palliative care needs, the cancer care team would refer patients to palliative care specialists, who would manage refractory pain, more complex psychosocial needs, and conflict resolution regarding the goals or methods of treatment (Quill and Abernethy, 2013).
Patients with advanced cancer and their families may have a number of psychosocial health needs (see Table 3-5). Compared to patients with earlier stage disease, patients with advanced cancer may have different needs, such as greater concern about religion and spirituality, as well as coping with existential suffering (Balboni et al., 2007; IOM, 2004b; Kissane, 2012). They are also more likely to experience distress. Estimates suggest that one-third to one-half of patients with cancer experience considerable distress, and those who are diagnosed with cancers associated with poorer prognoses experience greater distress (Zabora et al., 2001). Family caregivers also report considerable distress that may interfere with their ability to provide emotional or logistical support and exacerbate patients’ emotional distress (Braun et al., 2007; IOM, 2008a; Siegel et al., 1996). Thus, in the advanced cancer setting, it is especially important for the cancer care team to identify the psychosocial health needs of patients and their families, and to develop a care plan that addresses these needs.
Providing Timely Referral to Hospice Care
Hospice care is a form of palliative care and occurs at the end of life. It is defined by the National Quality Forum as “a service delivery system that provides palliative care for patients who have a limited life expectancy and require comprehensive biomedical, psychosocial, and spiritual
support as they enter the terminal stage of an illness or condition. It also supports family members coping with the complex consequences of illness, disability, and aging as death nears. Hospice care further addresses the bereavement needs of the family following the death of the patient” (NQF, 2006, p. 3). The Medicare hospice benefit is available for patients who have 6 months or less to live (prognosis must be agreed upon by two physicians) and who agree to forgo Medicare-covered benefits to treat their terminal illness (Medicare will still pay for covered benefits for any health problems that are not related to the terminal illness) (CMS, 2013a). Hospice care is often provided to patients in their homes, but it can also be delivered in freestanding hospice facilities, hospitals, nursing homes, and other long-term care facilities (GPC, 2013b).
The benefits of hospice care have been well documented in terms of improved quality of life, reductions in symptom distress, better outcomes for family caregivers, and patient and family satisfaction with care (Black et al., 2011; Shepperd et al., 2011; Teno et al., 2004; Wright et al., 2010). Unfortunately, these services are often underutilized by patients and their cancer care teams. In 2011, the median length of hospice care for patients in the United States was only 19.1 days and the average length of hospice care for patients was 69.1 days (NHPCO, 2012). More than one-third of patients with hospice care had a length of stay less than 7 days (NHPCO, 2012). Because access to hospice care improves the quality of cancer care, the committee recommends that the cancer care team provide cancer patients with timely referral to hospice care for end-of-life care.
Not all patients will opt for hospice care (Goodman, 2012; Matsuyama et al., 2006). The majority of patients with advanced cancer, however, would likely choose to transition to hospice care if a clinician or knowledgeable person had an honest conversation with them about their prognosis at the end of life. However, patients with advanced cancer are often treated aggressively near the end of their lives (Earle et al., 2004; Morden et al., 2012). In an analysis of Medicare claims data, more than 15 percent of cancer patients who received chemotherapy were treated within 2 weeks of their deaths (Earle et al., 2004).
Several studies have found that when a physician discusses a prognosis and end-of-life care preferences with the patient, that patient is less likely to want aggressive measures; for example, they are three times more likely to complete “do not resuscitate” forms and twice as likely to choose hospice care than are patients who do not have this discussion (Mack et al., 2012b; Wright et al., 2008). In a randomized clinical trial, Casarett and colleagues (2005) conducted structured interviews with nursing home residents to identify residents whose goals for care, treatment preferences, and palliative care needs indicated that hospice care would be the preferred course. They then notified these residents’ physicians and asked
them to authorize a hospice informational visit. The result of this intervention was a 20-fold increase in the number of patients choosing hospice care. Similarly, at the Ireland Cancer Center in Cleveland, all patients with advanced lung cancer met with a chaplain, a social worker, and an advanced practice nurse from a nearby hospice facility to discuss their care needs and goals. These conversations increased hospice use from 13 percent to 80 percent and the length of stay in hospice from an average of 10 to 44 days (Ford Pitorak et al., 2003). Thus, it is important that these services be discussed with and be accessible to patients.
Advancing New Payment Models
The current fee-for-service reimbursement system can impede high-quality communication and care for patients with advanced cancer. The ASCO statement on advanced cancer highlights time as a major barrier to clinicians’ provision of high-quality advanced cancer care, noting that discussions of prognosis, treatment options, and the patient’s goals and preferences require substantially more time than a standard followup visit (Peppercorn et al., 2011). Thus, ASCO recommends that payers reimburse clinicians for care planning to support the time and effort required to provide individualized care for individuals with advanced cancer (Peppercorn et al., 2011). The committee endorses this concept and recommends that CMS and other payers design, implement, and evaluate innovative payment models that incentivize the cancer care team to counsel their patients about advance care planning. As discussed previously, new models of payment may better support clinicians for having these important conversations compared to fee-for-service reimbursement.
In addition, insurance policies that prevent the dual use of hospice services and active treatment are a challenge to clinicians’ delivery of hospice care. Patients who use the Medicare hospice benefit must agree to forgo disease-directed treatment (MedPAC, 2012). The Medicare Payment Advisory Commission (MedPAC) has said that shorter hospice stays are not the result of benefit design but, rather, reluctance among clinicians, patients, and families to recognize that a patient’s condition is incurable and clinicians’ financial incentives to continue to treat a patient with active therapy (MedPAC, 2009). A number of stakeholders in oncology have suggested, however, that the requirement to forgo anti-cancer treatment when entering hospice care is problematic for patients with cancer (Harrington and Smith, 2008; Peppercorn et al., 2011). The ASCO statement on advanced cancer recommended that pilot programs evaluate the potential for providing concurrent anti-cancer treatment with hospice care (Peppercorn et al., 2011).
The committee recommends that in the setting of advanced cancer, CMS and other payers design, implement, and evaluate innovative payment models that incentivize the cancer care team to provide cancer patients with timely referral to hospice care for end-of-life care. A number of innovative palliative and hospice care models can inform payers in implementing this recommendation (see Table 3-6). In addition, the ACA directed the Secretary of HHS to establish a demonstration program that evaluates whether hospice care provided concurrently with disease-
TABLE 3-6 Examples of Hospice Care Models
| Program | Description |
| Aetna’s Compassionate Care Program | A care management program involving nurses trained in managing the care of terminally ill patients. Care managers identify patients’ needs through a comprehensive assessment and through consults with the patient, family, and clinicians involved with the patient’s care. Care managers provide patients and their families with education, support, and assistance with pain medications, psychosocial needs, and advance directives. An “enhanced hospice access” arm of this program has expanded patients’ access to hospice care by changing the definition of terminal illness to 12 months of life expectancy and allowing patients to access both hospice benefits and disease-directed therapy simultaneously. In this program, hospice election has been associated with patient satisfaction and a decrease in the use of acute care, intensive care, and emergency services. In the commercially insured population, patients’ hospice election has resulted in a net medical cost decrease of approximately 22 percent. |
| Sutter’s Advanced Illness Management (AIM) Program | The AIM program is an integrated system of care for individuals with advanced disease that provides home-based transitional and palliative care services. The AIM program provides patients and families with counseling with the goal of increasing hospice use and decreasing the use of unwanted acute care. Preliminary data suggest that AIM improves patient, family, and clinician satisfaction with care and increases use of hospice. AIM is associated with decreased hospitalizations and an average savings of $2,000 per patient a month. |
SOURCES: Aetna, 2013; Krakauer et al., 2009; Meyer, 2011.
directed care improves patient care, quality of life, and cost-effectiveness for Medicare beneficiaries. CMS has not yet initiated the demonstration project (Rau, 2013). Chapter 8 discusses different payment models that may offer improved care for patients with advanced cancer, including patient-centered medical homes, ACOs, and bundled payments.
Patients are at the center of the committee’s conceptual framework (see Figure S-2), which conveys the most important goal of a high-quality cancer care delivery system: meeting the needs of patients with cancer and their families. Such a system should support all patients in making informed medical decisions that are consistent with their needs, values, and preferences. In the current system, information to help patients understand their cancer prognoses, treatment benefits and harms, palliative care, psychosocial support, and costs of care is often unavailable or not regularly communicated. Additionally, patient-clinician communication and shared decision making is often less than optimal, impeding the delivery of patient-centered, high-quality cancer care. For example, several recent studies found that approximately 65 to 80 percent of cancer patients with poor prognoses incorrectly believed their treatments could result in a cure.
Recommendation 1: Engaged Patients
Goal: The cancer care team should provide patients and their families with understandable information on cancer prognosis, treatment benefits and harms, palliative care, psychosocial support, and estimates of the total and out-of-pocket costs of cancer care.
To accomplish this:
• The National Cancer Institute, the Centers for Medicare & Medicaid Services, the Patient-Centered Outcomes Research Institute, as well as patient advocacy organizations, professional organizations, and other public and private stakeholders should improve the development of this information and decision aids and make them available through print, electronic, and social media.
• Professional educational programs for members of the cancer care team should provide comprehensive and formal training in communication.
• The cancer care team should communicate and personalize this information for their patients at key decision points along the continuum of cancer care, using decision aids when available.
• The cancer care team should collaborate with their patients to develop a care plan that reflects their patients’ needs, values, and preferences, and considers palliative care needs and psychosocial support across the cancer care continuum.
• The Centers for Medicare & Medicaid Services and other payers should design, implement, and evaluate innovative payment models that incentivize the cancer care team to discuss this information with their patients and document their discussions in each patient’s care plan.
Patients with advanced cancer face specific communication and decision-making needs. Clinicians should discuss these patients’ options, such as implementing advance care plans, emphasizing palliative care, and psychosocial support, and maximizing quality of life by providing timely use of hospice care. These difficult conversations do not occur as frequently or as timely as they should, resulting in care that may not be aligned with patient preferences.
Recommendation 2: Engaged Patients
Goal: In the setting of advanced cancer, the cancer care team should provide patients with end-of-life care consistent with their needs, values, and preferences.
To accomplish this:
• Professional educational programs for members of the cancer care team should provide comprehensive and formal training in end-of-life communication.
• The cancer care team should revisit and implement their patients’ advance care plans.
• The cancer care team should place a primary emphasis on providing cancer patients with palliative care, psychosocial support, and timely referral to hospice care for end-of-life care.
• The Centers for Medicare & Medicaid Services and other payers should design, implement, and evaluate innovative payment models that incentivize the cancer care team to counsel their patients about advance care planning and timely referral to hospice care for end-of-life care.
ABIM (American Board of Internal Medicine). 2013. Physician charter. http://www.abimfoundation.org/Professionalism/Physician-Charter.aspx (accessed July 31, 2013).
ACGME (Accreditation Council for Graduate Medical Education). 2008. Educational program. http://www.acgme.org/acgmeweb/Portals/0/PDFs/commonguide/IVA5d_EducationalProgram_ACGMECompetencies_IPCS_Documentation.pdf (accessed August 7, 2013).
Aetna. 2013. Aetna Compassionate Care SM Program. http://www.aetna.com/individuals-families-health-insurance/sas/compassionate-care/program-description.html (accessed June 20, 2013).
AHRQ (Agency for Healthcare Research and Quality). 2003. Advance care planning, preferences for care at the end of life: Research in action. www.ahrq.gov/research/findings/factsheets/aging/endliferia/index.html (accessed June 20, 2013).
———. 2012. About the Eisenberg Center. http://effectivehealthcare.ahrq.gov/index.cfm/who-is-involved-in-the-effective-health-care-program1/about-the-eisenberg-center (accessed January 4, 2013).
———. 2013a. Advance care planning, preferences for care at the end of life. http://www.ahrq.gov/research/findings/factsheets/aging/endliferia/index.html (accessed April 1, 2013).
———. 2013b. Questions are the answer. Better communication. Better care. http://www.ahrq.gov/legacy/questions/index.html (accessed April 1, 2013).
Aiello Bowles, E. J., L. Tuzzio, C. J. Wiese, B. Kirlin, S. M. Greene, S. B. Clauser, and E. H. Wagner. 2008. Understanding high-quality cancer care: a summary of expert perspectives. Cancer 112(4):934-942.
Allison, T. A., and R. L. Sudore. 2013. Disregard of patients’ preferences is a medical error. JAMA Internal Medicine 173(9):787-788.
Alston, C., L. Paget, G. C. Halvorson, B. Novelli, J. Guest, P. McCabe, K. Hoffman, C. Koepke, M. Simon, S. Sutton, S. Okun, P. Wicks, T. Undem, V. Rohrbach, and I. V. Kohorn. 2012. Communicating with patients on health care evidence: Discussion paper. http://www.iom.edu/~/media/Files/Perspectives-Files/2012/Discussion-Papers/VSRT-Evidence.pdf (accessed March 28, 2013).
AMA (American Medical Association). 2013. Health literacy resources. http://www.ama-assn.org/ama/pub/about-ama/ama-foundation/our-programs/public-health/health-literacy-program/health-literacy-kit.page? (Accessed August 7, 2013).
APCD (All-Payer Claims Database). 2013. Interactive state report map. http://www.apcdcouncil.org/state/map (accessed April 30, 2013).
Armstron, S., and D. Arterburn. 2013. Creating a culture to promote shared decision making at Group Health. http://www.iom.edu/Global/Perspectives/2013/SharedDecisionMaking.aspx (accessed May 2, 2013).
ASCO (American Society of Clinical Oncology). 2011. ASCO launches Cancer.Net mobile, a new app for iPhone, iPad, and iPod Touch that puts cancer care in the hands of patients and caregivers. http://www.asco.org/press-center/asco-launches-cancernet-mobile-new-app-iphone-ipad-and-ipod-touch-puts-cancer-care (accessed May 2, 2013).
ASCO and Cancer.Net. 2012. Advanced cancer care planning: What patients and families need to know about their choices when facing serious illness. http://www.cancer.net/patient/Coping/Advanced%20Cancer%20Care%20Planning/Advanced_Cancer_Care_Planning.pdf (accessed May 2, 2012).
Ayanian, J. Z., A. M. Zaslavsky, E. Guadagnoli, C. S. Fuchs, K. J. Yost, C. M. Creech, R. D. Cress, L. C. O’Connor, D. W. West, and W. E. Wright. 2005. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. Journal of Clinical Oncology 23(27):6576-6586.
Ayanian, J. Z., A. M. Zaslavsky, N. K. Arora, K. L. Kahn, J. L. Malin, P. A. Ganz, M. van Ryn, M. C. Hornbrook, C. I. Kiefe, Y. He, J. M. Urmie, J. C. Weeks, and D. P. Harrington. 2010. Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. Journal of Clinical Oncology 28(27):4154-4161.
Back, A. L., R. M. Arnold, W. F. Baile, K. A. Fryer-Edwards, S. C. Alexander, G. E. Barley, T. A. Gooley, and J. A. Tulsky. 2007. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Archives of Internal Medicine 167(5):453-460.
Back, A. L., R. M. Arnold, W. F. Baile, J. A. Tulsky, G. E. Barley, R. D. Pea, and K. A. Fryer-Edwards. 2009a. Faculty development to change the paradigm of communication skills teaching in oncology. Journal of Clinical Oncology 27(7):1137-1141.
Back, A. L., R. M. Arnold, W. F. Baile, J. A. Tulsky, and K. A. Fryer-Edwards. 2009b. Approaching difficult communication tasks in oncology. CA: A Cancer Journal for Clinicians 55(3):164-177.
Back, A. L., R. M. Arnold, J. A. Tulsky, W. F. Baile, and K. Fryer-Edwards. 2010. “Could I add something?” Teaching communication by intervening in real time during a clinical encounter. Academic Medicine 85(6): 1048-1051.
Baile, W. F., R. Buckman, R. Lenzi, G. Glober, E. A. Beale, and A. P. Kudelka. 2000. SPIKES—A six-step protocol for delivering bad news: Application to the patient with cancer. Oncologist 5(4):302-311.
Balboni, T. A., L. C. Vanderwerker, S. D. Block, M. E. Paulk, C. S. Lathan, J. R. Peteet, and H. G. Prigerson. 2007. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. Journal of Clinical Oncology 25(5):555-560.
Bandieri, E., D. Sichetti, M. Romero, C. Fanizza, M. Belfiglio, L. Buonaccorso, F. Artioli, F. Campione, G. Tognoni, and M. Luppi. 2012. Impact of early access to a palliative/ supportive care intervention on pain management in patients with cancer. Annals of Oncology 23(8):2016-2020.
Barnato, A. E., M. B. Herndon, D. L. Anthony, P. M. Gallagher, J. S. Skinner, J. P. Bynum, and E. S. Fisher. 2007. Are regional variations in end-of-life care intensity explained by patient preferences?: A study of the U.S. Medicare population. Medical Care 45(5):386-393.
Basch, E. 2013. Toward patient-centered drug development in oncology. New England Journal of Medicine 369(5):397-400.
Bechtel, C., and D. L. Ness. 2010. If you build it, will they come? Designing truly patient-centered health care. Health Affairs (Millwood) 29(5):914-920.
Belkora, J. K., A. Teng, S. Volz, M. K. Loth, L. J. Esserman. 2011. Expanding the reach of decision and communication aids in a breast care center: A quality improvement study. Patient Education and Counseling 83(2):234-239.
Berkhof, M., H. J. van Rijssen, A. J. M. Schellart, J. R. Anema, and A. J. van der Beek. 2010. Effective training strategies for teaching communication skills to physicians: An overview of systematic reviews. Patient Education and Counseling 84(2):152-162.
Berkman, N. D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, A. Viera, K. Crotty, A. Holland, M. Brasure, K. N. Lohr, E. Harden, E. Tant, I. Wallace, and M. Viswanathan. 2011. Health literacy interventions and outcomes: An updated systematic review, Evidence Report/ Technology Assessment: Number 199. Rockville, MD: Agency for Healthcare Research and Quality.
Berman, A. 2012. Living life in my own way—and dying that way as well. Health Affairs (Millwood) 31(4):871-874.
Bernard, D. S., S. L. Farr, and Z. Fang. 2011. National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. Journal of Clinical Oncology 29(20):2821-2826.
Berwick, D. M. 2009. What “patient-centered” should mean: Confessions of an extremist. Health Affairs (Millwood) 28(4):w555-w565.
Bindman, A. B., J. D. Blum, and R. Kronick. 2013. Medicare payment for chronic care delivered in a patient-centered medical home. Journal of the American Medical Association. (epub ahead of print).
Bisognano, M., and E. Goodman. 2013. Engaging patients and their loved ones in the ultimate conversation. Health Affairs (Millwood) 32(2):203-206.
Black, B., K. Herr, P. Fine, S. Sanders, X. Tang, K. Bergen-Jackson, M. Titler, and C. Forcucci. 2011. The relationships among pain, nonpain symptoms, and quality of life measures in older adults with cancer receiving hospice care. Pain Medicine 12(6):880-889.
Braddock, C. H., 3rd, K. A. Edwards, N. M. Hasenberg, T. L. Laidley, and W. Levinson. 1999. Informed decision making in outpatient practice: Time to get back to basics. Journal of the American Medical Association 282(24):2313-2320.
Braun, M., M. Mikulincer, A. Rydall, A. Walsh, and G. Rodin. 2007. Hidden morbidity in cancer: spouse caregivers. Journal of Clinical Oncology 25(30):4829-4834.
Busari, J. O. 2013. The discourse of generational segmentation and the implications for postgraduate medical education. Perspectives on Medical Education. (epub ahead of print).
Cancer Support Community. 2012. Online Support. http://www.cancersupportcommunity.org/MainMenu/Cancer-Support/Online-Support-Groups.html (accessed January 4, 2013).
Casarett, D., J. Karlawish, K. Morales, R. Crowley, T. Mirsch, and D. A. Asch. 2005. Improving the use of hospice services in nursing homes: A randomized controlled trial. Journal of the American Medical Association 294(2):211-217.
C-Change. 2005. Cancer patient navigation overview. http://cancerpatientnavigation.org (accessed September 26, 2012).
CDC (Centers for Disease Control and Prevention). 2013. Lung cancer risk factors. http://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm (accessed April 24, 2013).
Center to Advance Palliative Care. 2011. 2011 public opinion research on palliative care: A report based on research by Public Opinion Strategies. New York: Center to Advance Palliative Care.
CFAH (Center for Advancing Health). 2010. Snapshot of people’s engagement in their health care. http://www.cfah.org/file/CFAH_Snapshot_2010_Full.pdf (accessed September 25, 2012).
———. 2012. Prepared Patient Forum. http://www.preparedpatientforum.org/preparedpatient/index.cfm (accessed January 4, 2013).
Chan, D. S., A. Willicombe, T. D. Reid, C. Beaton, D. Arnold, J. Ward, I. L. Davies, and W. G. Lewis. 2012. Relative quality of internet-derived gastrointestinal cancer information. Journal of Cancer Education 27(4):676-679.
Chen, A,. B., A. Cronin, J. C. Weeks, E. A. Chrischilles, J. Malin, J. A. Hayman, and D. Schrag. 2013. Expectations about the effectiveness of radiation therapy among patients with incurable lung cancer. Journal of Clinical Oncology 31(21):2730-2735.
Cheng, W. W., J. Willey, J. L. Palmer, T. Zhang, and E. Bruera. 2005. Interval between palliative care referral and death among patients treated at a comprehensive cancer center. Journal of Palliative Medicine 8(5):1025-1032.
Chiew, K. S., H. Shepherd, J. Vardy, M. H. Tattersall, P. N. Butow, and N. B. Leighl. 2008. Development and evaluation of a decision aid for patients considering first-line chemotherapy for metastatic breast cancer. Health Expectations 11(1):35-45.
Clancy, C. M. 2008. How patient-centered healthcare can improve quality. http://www.psqh.com/marapr08/ahrq.html (accessed September 25, 2012).
CMS (Centers for Medicare & Medicaid Services). 2013a. Medicare hospice benefits. http://www.medicare.gov/Pubs/pdf/02154.pdf (accessed May 2, 2013).
———. 2013b. Medicare provider charge data. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data (accessed July 31, 2013).
Collins, E. D., C. P. Moore, K. F. Clay, S. A. Kearing, A. M. O’Connor, H. A. Llewellyn-Thomas, J. R. J. Barth, and K. R. Sepucha. 2009. Can women with early-stage breast cancer make an informed decision for mastectomy? Journal of Clinical Oncology 27(4):519-525.
The Commonwealth Fund. 2007. Bending the curve: Options for achieving savings and improving value in U.S. health spending. New York: The Commonwealth Fund.
Covinsky, K. E., J. D. Fuller, K. Yaffe, C. B. Johnston, M. B. Hamel, J. Lynn, J. M. Teno, and R. S. Phillips. 2000. Communication and decision-making in seriously ill patients: Findings of the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Journal of the American Geriatrics Society 48(5 Suppl): S187-S193.
Dalal, S., S. Palla, D. Hui, L. Nguyen, R. Chacko, Z. Li, N. Fadul, C. Scott, V. Thornton, B. Coldman, Y. Amin, and E. Bruera. 2011. Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. Oncologist 16(1):105-111.
Detering, K. M., A. D. Hancock, M. C. Reade, and W. Silvester. 2010. The impact of advance care planning on end of life care in elderly patients: Randomized controlled trial. British Medical Journal 340:c1345.
DeWalt, D. A., L. F. Callahan, V. H. Hawk, K. A. Broucksou, A. Hink, R. Rudd, and C. Brach. 2010. Health literacy universal precautions toolkit. AHRQ Publication No. 10-0046-EF. Rockville, MD: Agency for Healthcare Research and Quality.
Earle, C. C., B. A. Neville, M. B. Landrum, J. Z. Ayanian, S. D. Block, and J. C. Weeks. 2004. Trends in the aggressiveness of cancer care near the end of life. Journal of Clinical Oncology 22(2):315-321.
El Dib, R. P., A. N. Atallah, and R. B. Andriolo. 2007. Mapping the Cochrane evidence for decision making in health care. Journal of Evaluation in Clinical Practice 13:689-692.
El-Jawahri, A., L. M. Podgurski, A. F. Eichler, S. R. Plotkin, J. S. Temel, S. L. Mitchell, Y. Chang, M. J. Barry, and A. E. Volandes. 2010. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. Journal of Clinical Oncology 28(2):305-310.
Elwyn, G., A. O’Connor, D. Stacey, R. Volk, A. Edwards, A. Coulter, R. Thomson, A. Barratt, M. Barry, S. Bernstein, P. Butow, A. Clarke, V. Entwistle, D. Feldman-Stewart, M. Holmes-Rovner, H. Llewellyn-Thomas, N. Moumjid, A. Mulley, C. Ruland, K. Sepucha, A. Sykes, and T. Whelan. 2006. Developing a quality criteria framework for patient decision aids: Online international Delphi consensus process. BMJ 333(7565):417.
Epstein, R. M., and R. L. Street, Jr. 2007. Patient-centered communication in cancer care: Promoting healing and reducing suffering. National Cancer Institute, NIH Publication No. 07-6225.
Bethesda, MD: National Cancer Institute.
Epstein, R. M., K. Fiscella, C. S. Lesser, and K. C. Stange. 2010. Why the nation needs a policy push on patient-centered health care. Health Affairs (Millwood) 29(8):1489-1495.
Feldman, L. S., H. M. Shihab, D. Thiemann, H. C. Yeh, M. Ardolino, S. Mandell, and D. J. Brotman. 2013. Impact of providing fee data on laboratory test ordering: A controlled clinical trial. Journal of the American Medical Association Internal Medicine 1-6. doi: 10.1001./jamainternmed.2013.232. (epub ahead of print).
Ferris, F. D., E. Bruera, N. Cherny, C. Cummings, D. Currow, D. Dudgeon, N. Janjan, F. Strasser, C. F. von Gunten, and J. H. Von Roenn. 2009. Palliative cancer care a decade later: accomplishments, the need, next steps—from the American Society of Clinical Oncology. Journal of Clinical Oncology 27(18):3052-3058.
Finch, C. 2011. AARP Launches Free Medicare Starter Kit Guide for Boomers. Suite101, http://suite101.com/article/aarp-launches-free-medicare-starter-kit-guide-for-boomers-a363274 (accessed January 4, 2013).
Fisher, B., S. Anderson, J. Bryant, R. G. Margolese, M. Deutsch, E. R. Fisher, J.-H. Jeong, and N. Wolmark. 2002. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. New England Journal of Medicine 347(16):567-575.
Fleurence, R., J. V. Selby, K. Odom-Walker, G. Hunt, D. Meltzer, J. R. Slutsky, and C. Yancy. 2013. How the Patient-Centered Outcomes Research Institute is engaging patients and others in shaping its research agenda. Health Affairs (Millwood) 32(2):393-400.
Ford Pitorak, E., M. Beckham Armour, and H. D. Sivec. 2003. Project safe conduct integrates palliative goals into comprehensive cancer care. Journal of Palliative Medicine 6(4):645-655.
Frosch, D. L., S. G. May, K. A. Rendle, C. Tietbohl, and G. Elwyn. 2012. Authoritarian physicians and patients’ fear of being labeled “difficult” among key obstacles to shared decision making. Health Affairs (Millwood) 31(5):1030-1038.
Ganz, P. A. 2013. Identifying tools and strategies to provide quality oncology care. Journal of Oncology Practice 9(3):125-127.
GAO (Government Accountability Office). 2011. Meaningful price information is difficult for consumers to obtain prior to receiving care. http://www.gao.gov/products/GAO-11-791 (accessed March 29, 2013).
Gesme, D. H., and M. Wiseman. 2011. A financial counselor on the practice staff: A win-win. Journal of Oncology Practice 7(4):273-275.
Gigerenzer, G., and A. Edwards. 2003. Simple tools for understanding risks: From innumeracy to insight. BMJ 327(7417):741-744.
Goldsmith, J., B. Ferrell, E. Wittenberg-Lyles, and S. L. Ragan. 2013. Palliative care communication in oncology nursing. Clinical Journal of Oncology Nursing 17(2):163-167.
Goodman, E. 2012. Die the way you want to. Harvard Business Review January-February 2012., http://hbr.org/2012/01/tackling-social-problems/ar/1 (accessed April 25, 2013).
GPC (Get Palliative Care). 2013a. Frequently asked questions. http://www.getpalliativecare.org/whatis/faq/#who-provides-palliative-care (accessed August 8, 2013).
———. 2013b. Glossary. http://www.getpalliativecare.org/whatis/glossary (accessed August 8, 2013).
Greer, J. A., W. F. Pirl, V. A. Jackson, A. Muzikansky, I. T. Lennes, R. S. Heist, E. R. Gallagher, and J. S. Temel. 2012. Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. Journal of Clinical Oncology 30(4):394-400.
Greer, J. A., V. A. Jackson, D. E. Meier, and J. S. Temel. 2013. Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA: A Cancer Journal for Clinicians. (epub ahead of print).
Gribbin, J., and R. Dewis. 2009. Appendix 1 Adjuvant! Online: Review of evidence concerning its validity, and other considerations relating to its use in the NHS. In NICE treatment guidelines, No. 80. Cardiff, UK: National Collaborating Centre for Cancer.
Gruman, J. C. 2013. An accidental tourist finds her way in the dangerous land of serious illness. Health Affairs (Millwood) 32(2):427-431.
Grund, S. H., A. A. Forastiere, W. A. Flood, E. Whyler, V. Kozlovski, and Y.-N. Wong. 2012. A Web-based decision support platform to reduce non-evidence-based treatment of non-small cell lung cancer. Journal of Clinical Oncology 30(Suppl 34):abstr 71.
Grunfeld, E. A., E. J. Maher, S. Browne, P. Ward, T. Young, B. Vivat, G. Walker, C. Wilson, H. W. Potts, A. M. Westcombe, M. A. Richards, and A. J. Ramirez. 2006. Advanced breast cancer patients’ perceptions of decision making for palliative chemotherapy. Journal of Clinical Oncology 24(7):1090-1098.
Grunfeld, E., J. A. Julian, G. Pond, E. Maunsell, D. Coyle, A. Folkes, A. A. Joy, L. Provencher, D. Rayson, D. E. Rheaume, G. A. Porter, L. F. Paszat, K. I. Pritchard, A. Robidoux, S. Smith, J. Sussman, S. Dent, J. Sisler, J. Wiernikowski, and M. N. Levine. 2011. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. Journal of Clinical Oncology 29(36):4755-4762.
Hack, T. F., L. F. Degner, P. A. Parker, and SCRN Communication Team. 2005. The communication goals and needs of cancer patients: A review. Psychooncology 14(10):831-845.
Hammes, B. J., and B. L. Rooney. 1998. Death and end-of-life planning in one midwestern community. Archives of Internal Medicine 158(4):383-390.
Hammes, B. J., B. L. Rooney, and J. D. Goodman. 2010. A comparative, retrospective, observational study of the prevalence, availability, and specificity of advance care plans in a county that implemented an advance care planning microsystem. Journal of the American Geriatrics Society 58(7):1249-1255.
Harrington, S. E., and T. J. Smith. 2008. The role of chemotherapy at the end of life: “When is enough, enough?” Journal of the American Medical Association 299(22):2667-2678.
HealthCare.gov. 2013. Out-of-pocket costs. http://www.healthcare.gov/glossary/O/oopcosts.html (accessed April 22, 2013).
Hennessy, J. E., B. A. Lown, L. Landzaat, and K. Porter-Williamson. 2013. Practical issues in palliative and quality-of-life care. Journal of Oncology Practice 9(2):78-80.
Heyland, D. K., D. Barwich, D. Pichora, P. Dodek, F. Lamontagne, J. J. You, C. Tayler, P. Porterfield, T. Sinuff, and J. Simon. 2013. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Internal Medicine: 1-10. doi: 10.1001/ jamainternmed.2013.180. (epub ahead of print).
HHS (U.S. Department of Health and Human Services). 2013a. National standards for culturally and linguistically appropriate services in health and health care: A blueprint for advancing and sustaining CLAS policy and practice. Washington, DC: Office of Minority Health.
———. 2013b. Administration offers consumers an unprecedented look at hospital charges. http://www.hhs.gov/news/press/2013pres/05/20130508a.html (accessed July 31, 2013).
Hibbard, J. H., and J. Greene. 2013. What the evidence shows about patient activation: Better health outcomes and care experiences; fewer data on costs. Health Affairs (Millwood) 32(2):207-214.
Himmelstein, D. U., D. Thorne, E. Warren, and S. Woolhandler. 2009. Medical bankruptcy in the United States, 2007: results of a national study. American Journal of Medicine 122(8):741-746.
Hoffman, B., ed. 2004. A cancer survivor’s almanac: Charting your journey. Hoboken, NJ: John Wiley & Sons, Inc.
Hostetter, M., and S. Klein. 2012. Quality matters. Health care price transparency: Can it promote high-value care ? http://www.commonwealthfund.org/Newsletters/Quality-Matters/2012/April-May/In-Focus.aspx (accessed March 29, 2013).
Hui, D., S. H. Kim, J. H. Kwon, K. C. Tanco, T. Zhang, J. H. Kang, W. Rhondali, G. Chisholm, and E. Bruera. 2012. Access to palliative care among patients treated at a comprehensive cancer center. Oncologist 17(12):1574-1580.
Hui, D., M. De La Cruz, M. Mori, H. A. Parsons, J. H. Kwon, I. Torres-Vigil, S. H. Kim, R. Dev, R. Hutchins, C. Liem, D. H. Kang, and E. Bruera. 2013. Concepts and definitions for “supportive care,” “best supportive care,” “palliative care,” and “hospice care” in the published literature, dictionaries, and textbooks. Supportive Care Cancer 21(3):659-685.
Huskamp, H. A., N. L. Keating, J. L. Malin, A. M. Zaslavsky, J. C. Weeks, C. C. Earle, J. M. Teno, B. A. Virnig, K. L. Kahn, Y. He, and J. Z. Ayanian. 2009. Discussions with physicians about hospice among patients with metastatic lung cancer. Archives of Internal Medicine 169(10):954-962.
Informed Medical Decisions Foundation. 2012a. Dartmouth-Hitchcock Medical Center. http://informedmedicaldecisions.org/imdf_demo_site/dartmouth-hitchcock-medicalcenter/ (accessed January 4, 2013).
———. 2012b. How the foundation develops decision aids. http://informedmedicaldecisions.org/shared-decision-making-in-practice/decision-aids (accessed January 4, 2013).
———. 2013. Affordable Care Act. http://informedmedicaldecisions.org/shared-decision-making-policy/federal-legislation/affordable-care-act (accessed March 20, 2013).
IOM (Institute of Medicine). 1997. Approaching death: Improving care at the end of life. Washington, DC: National Academy Press.
———. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
———. 2003. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press.
———. 2004a. Health literacy: A prescription to end confusion. Washington, DC: The National Academies Press.
———. 2004b. Meeting psychosocial needs of women with breast cancer. Washington, DC: The National Academies Press.
———. 2008a. Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press.
———. 2008b. Knowing what works in health care: A roadmap for the nation. Washington, DC: The National Academies Press.
———. 2009a. Assessing and improving value in cancer care. Washington, DC: The National Academies Press.
———. 2009b. Initial national priorities for comparative effectiveness research. Washington, DC: The National Academies Press.
———. 2010. A national cancer clinical trials system for the 21st century: Reinvigorating the NCI Cooperative Group Program. Washington, DC: The National Academies Press.
———. 2011a. Patient-centered cancer treatment planning: Improving the quality of oncology care: Workshop summary. Washington, DC: The National Academies Press.
———. 2011b. Promoting health literacy to encourage prevention and wellness: Workshop summary. Washington, DC: The National Academies Press.
———. 2012. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
———. 2013. Delivering affordable cancer care in the 21st century: Workshop summary. Washington, DC: The National Academies Press.
IOM and NRC (National Research Council). 1999. Ensuring quality cancer care. Washington, DC: National Academy Press.
———. 2005. From cancer patient to cancer survivor: Lost in transition. Washington, DC: The National Academies Press.
Irwin, J. Y., T. Thyvalikakath, H. Spallek, T. Wali, A. R. Kerr, and T. Schleyer. 2011. English and Spanish oral cancer information on the internet: a pilot surface quality and content evaluation of oral cancer web sites. Journal of Public Health Dentistry 71(2):106-116.
Jolie, A. 2013. My medical choice. New York Times, May 14, A25.
Keating, N. L., M. B. Landrum, S. O. Rogers, Jr., S. K. Baum, B. A. Virnig, H. A. Huskamp, C. C. Earle, and K. L. Kahn. 2010. Physician factors associated with discussions about end-of-life care. Cancer 116(4):998-1006.
King, J., and B. Moulton. 2013. Group Health’s participation in a shared decision-making demonstration yielded lessons, such as role of culture change. Health Affairs (Millwood) 32(2):294-302.
Kissane, D. W. 2012. The relief of existential suffering. Archives of Internal Medicine 172(19): 1501-1505.
Krakauer, R., C. M. Spettell, L. Reisman, and M. J. Wade. 2009. Opportunities to improve the quality of care for advanced illness. Health Affairs (Millwood) 28(5):1357-1359.
Kutner, M., E. Greenberg, Y. Jin, B. Boyle, Y. Hsu, and E. Dunleavy. 2007. Literacy in everday life: Results from the 2003 National Assessment of Adult Literacy (NCES 2007-480). Washington, DC: National Center for Education Statistics.
Lantz, P. M., N. K. Janz, A. Fagerlin, K. Schwartz, L. Liu, I. Lakhani, B. Salem, and S. J. Katz. 2005. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Services Research 40(3):745-767.
Lauria, M. M., E. J. Clark, J. F. Hermann, and N. M. Stearns, eds. 2001. Social work in oncology: Supporting survivors, families, and caregivers. Atlanta, GA: American Cancer Society.
Lawrentschuk, N., D. Sasges, R. Tasevski, R. Abouassaly, A. M. Scott, and I. D. Davis. 2012. Oncology health information quality on the Internet: A multilingual evaluation. Annals of Surgical Oncology 19(3):706-713.
Lee, C. N., Y. Chang, N. Adimorah, J. K. Belkora, B. Moy, A. H. Partridge, D. W. Ollila, and K. R. Sepucha. 2012. Decision making about surgery for early-stage breast cancer. Journal of the American College of Surgeons 214(1):1-10.
Leighl, N. B., H. L. Shepherd, P. N. Butow, S. J. Clarke, M. McJannett, P. J. Beale, N. R. Wilcken, M. J. Moore, E. X. Chen, D. Goldstein, L. Horvath, J. J. Knox, M. Krzyzanowska, A. M. Oza, R. Feld, D. Hedley, W. Xu, and M. H. Tattersall. 2011. Supporting treatment decision making in advanced cancer: A randomized trial of a decision aid for patients with advanced colorectal cancer considering chemotherapy. Journal of Clinical Oncology 29(15):2077-2084.
Leukemia & Lymphoma Society. 2012. The AML guide: Information for patients and caregivers acute myeloid leukemia. http://www.lls.org/content/nationalcontent/resourcecenter/freeeducationmaterials/leukemia/pdf/amlguide.pdf (accessed January 4, 2013).
Licking, E. 2012. As new tools offer explicit cost data on cancer treatments, will payers push for their use? http://realendpoints.com/2012/02/as-new-tools-offer-explicit-cost-data-on-cancer-treatments-will-payers-push-for-their-use (accessed April 22, 2013).
Lin, G. A., M. Halley, K. A. Rendle, C. Tietbohl, S. G. May, L. Trujillo, and D. L. Frosch. 2013. An effort to spread decision aids in five California primary care practices yielded low distribution, highlighting hurdles. Health Affairs (Millwood) 32(2):311-320.
LINCS (Literacy Information and Communication System). 2013. Resource collection topics. http://lincs.ed.gov/professional-development/resource-collections (accessed August 7, 2013).
Mack, J. W., and T. J. Smith. 2012. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. Journal of Clinical Oncology 30(22):2715-2117.
Mack, J. W., J. C. Weeks, A. A. Wright, S. D. Block, and H. G. Prigerson. 2010. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. Journal of Clinical Oncology 28(7):1203-1208.
Mack, J. W., A. Cronin, N. Taback, H. A. Huskamp, N. L. Keating, J. L. Malin, C. C. Earle, and J. C. Weeks. 2012a. End-of-life care discussions among patients with advanced cancer: A cohort study. Annals of Internal Medicine 156(3):204-210.
Mack, J. W., A. Cronin, N. L. Keating, N. Taback, H. A. Huskamp, J. L. Malin, C. C. Earle, and J. C. Weeks. 2012b. Associations between end-of-life discussion characteristics and care received near death: A prospective cohort study. Journal of Clinical Oncology 30(35):4387-4395.
Maida, V., J. Peck, M. Ennis, N. Brar, and A. R. Maida. 2010. Preferences for active and aggressive intervention among patients with advanced cancer. BMC Cancer 10:592.
Malin, J. L., J. C. Weeks, A. L. Potosky, M. C. Hornbrook, and N. L. Keating. 2013. Medical oncologists’ perceptions of financial incentives in cancer care. Journal of Clinical Oncology 31(5)L530-535.
Matsuyama, R., S. Reddy, and T. J. Smith. 2006. Why do patients choose chemotherapy near the end of life? A review of the perspective of those facing death from cancer. Journal of Clinical Oncology 24(21):3490-3496.
Maurer, M., P. Dardess, K. L. Carman, K. Frazier, and L. Smeeding. 2012. Guide to patient and family engagement: Environmental scan report. (Prepared by American Institutes for Research under contract HHSA 290-200-600019). AHRQ Publication No. 12-0042-EF. Rockville, MD: Agency for Healthcare Research and Quality.
McCorkle, R., E. Ercolano, M. Lazenby, D. Schulman-Green, L. S. Schilling, K. Lorig, and E. H. Wagner. 2011. Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA: A Cancer Journal for Clinicians 6(1):50-62.
MedPAC (Medicare Payment Advisory Commission). 2009. Report to the Congress: Medicare payment policy. http://www.medpac.gov/documents/mar09_entirereport.pdf (accessed April 1, 2013).
———. 2010. Report to the Congress: Aligning incentives in Medicare. http://www.medpac.gov/documents/jun10_entirereport.pdf (accessed March 28, 2013).
———. 2012. Hospice services payment system. http://www.medpac.gov/documents/MedPAC_Payment_Basics_12_hospice.pdf (accessed April 1, 2013).
Meier, D. 2012. Learning from Amy Berman: Barriers to palliative care and how to overcome them. http://healthaffairs.org/blog/2012/04/30/learning-from-amy-berman-barriers-to-palliative-care-and-how-we-might-overcome-them/ (accessed August 8, 2013).
Meropol, N. J., D. Schrag, T. J. Smith, T. M. Mulvey, R. M. Langdon, Jr., D. Blum, P. A. Ubel, and L. E. Schnipper. 2009. American Society of Clinical Oncology guidance statement: The cost of cancer care. Journal of Clinical Oncology 27(23):3868-3874.
Meyer, H. 2011. Changing the conversation in California about care near the end of life. Health Affairs (Millwood) 30(3):390-393.
Milne, D., M. Jefford, P. Schofield, and S. Aranda. 2013. Appropriate, timely referral to palliative care services: a name change will not help. Journal of Clinical Oncology 31(16):2055.
Moore, P. M., S. R. Mercado, M. G. Artigues, and T. A. Lawrie. 2013. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database of Systematic Reviews 3: CD003751.
Morden, N. E., C. H. Chang, J. O. Jacobson, E. M. Berke, J. P. Bynum, K. M. Murray, and D. C. Goodman. 2012. End-of-life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health Affairs (Millwood) 31(4):786-796.
Moriates, C., N. T. Shah, and V. M. Arora. 2013. First, do no (financial) harm. Journal of the American Medical Association (epub ahead of print).
NAEP (National Assessment of Educational Progress). 2010. The nation’s report card: Grade 12 reading and mathematics 2009 national and pilot state results. Washington, DC: U.S. Department of Education.
NCCS (National Coalition for Cancer Survivorship). 2012a. Cancer is a crisis. http://www.canceradvocacy.org/resources/remaining-hopeful/cancer-is-a-crisis (accessed September 24, 2012).
———. 2012b. NCCS applauds establishment of cancer treatment planning and care coordination reimbursement codes. http://www.canceradvocacy.org/news/nccs-applauds-establishment-treatment-care-reimbursement-codes.html (accessed September 24, 2012).
———. 2012c. Cancer survivor toolbox. http://www.canceradvocacy.org/toolbox (accessed January 4, 2013).
———. 2013. Support the PACT Act. http://www.canceradvocacy.org/pact-act (accessed August 1, 2013).
NCI (National Cancer Institute). 2012. Breast cancer risk in American women. http://www.cancer.gov/cancertopics/factsheet/detection/probability-breast-cancer (accessed April 24, 2013).
———. 2013a. Cancer Education and Career Development Program (R25T). http://www.cancer.gov/researchandfunding/cancertraining/outsidenci/R25T (accessed May 2, 2013).
———. 2013b. NCI dictionary of cancer terms. http://www.cancer.gov/dictionary (accessed July 19, 2013).
NCSL (National Conference of State Legislatures). 2013. State and federal actions related to transparency and disclosure of health charges and provider payments. http://www.ncsl.org/issues-research/health/transparency-and-disclosure-health-costs.aspx#State_Efforts (accessed April 30, 2013).
Neumann, P. J., J. A. Palmer, E. Nadler, C. Fang, and P. Ubel. 2010. Cancer therapy costs influence treatment: A national survey of oncologists. Health Affairs (Millwood) 29(1):196-202.
NHPCO (National Hospice and Palliative Care Organization). 2012. NHPCO facts and figures: Hospice care in America. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf (accessed April 30, 2013).
———. 2013. Advance care planning. http://www.nhpco.org/advance-care-planning (accessed April 1, 2013).
NQF (National Quality Forum). 2006. A national framework and preferred practices for palliative and hospice care quality. http://www.qualityforum.org/Publications/2006/12/A_National_Framework_and_Preferred_Practices_for_Palliative_and_Hospice_Care_Quality.aspx (accessed May 22, 2013).
NRC (National Research Council). 2012. Improving adult literacy instruction: Options for practice and research. Washington, DC: The National Academies Press.
OHRI (Ottawa Hospital Research Institute). 2013. A to Z inventory of decision aids. http://decisionaid.ohri.ca/AZinvent.php (accessed March 29, 2013).
Oncotalk. 2002. Learning module 2: Giving bad news. http://depts.washington.edu/oncotalk/learn/modules.html (accessed May 15, 2013).
Orlander, J. D., B. G. Fincke, D. Hermanns, and G. A. Johnson. 2002. Medical residents’ first clearly remembered experiences of giving bad news. Journal of General Internal Medicine 17(11):825-831.
Oshima Lee, E., and E. J. Emanuel. 2013. Shared decision making to improve care and reduce costs. New England Journal of Medicine 368(1):6-8.
Osta, B. E., J. L. Palmer, T. Paraskevopoulos, B. L. Pei, L. E. Roberts, V. A. Poulter, R. Chacko, and E. Bruera. 2008. Interval between first palliative care consult and death in patients diagnosed with advanced cancer at a comprehensive cancer center. Journal of Palliative Medicine 11(1):51-57.
Parry, C., E. E. Kent, L. P. Forsythe, C. M. Alfano, and J. H. Rowland. 2013. Can’t see the forest for the care plan: A call to revisit the context of care planning. Journal of Clinical Oncology 31(21):2651-2653.
Partin, M. R., D. Nelson, A. B. Flood, G. Friedemann-Sanchez, and T. J. Wilt. 2006. Who uses decision aids? Subgroup analyses from a randomized controlled effectiveness trial of two prostate cancer screening decision support interventions. Health Expectations 9(3):285-295.
Patient Advocate Foundation. 2012. Resources. http://www.patientadvocate.org/resources.php (accessed January 4, 2013).
PCORI (Patient-Centered Outcomes Research Institute). 2012. National priorities for research and research agenda. http://www.pcori.org/assets/PCORI-National-Priorities-and-Research-Agenda-2012-05-21-FINAL.pdf (accessed May 2, 2013).
———. 2013a. Development and pilot of three patient decision aids for implanted defibrillators. http://www.pcori.org/pilot-projects/development-and-pilot-of-three-patient-decision-aids-for-implanted-defibrillators (accessed May 2, 2013).
———. 2013b. Patient-centered outcomes research. http://www.pcori.org/research-we-support/pcor (accessed March 29, 2013).
Peppercorn, J. M., T. J. Smith, P. R. Helft, D. J. Debono, S. R. Berry, D. S. Wollins, D. M. Hayes, J. H. Von Roenn, and L. E. Schnipper. 2011. American Society of Clinical Oncology statement: Toward individualized care for patients with advanced cancer. Journal of Clinical Oncology 29(6):755-760.
Peters, E., J. Hibbard, P. Slovic, and N. Dieckmann. 2007. Numeracy skill and the communication, comprehension, and use of risk-benefit information. Health Affairs (Millwood) 26(3):741-748.
Picker Institute. 2013. Principles of patient-centered care. http://pickerinstitute.org/about/picker-principles (accessed July 17, 2013).
Porter-O’Grady, T., and K. Malloch. 2007. Quantum leadership: A resource for healthcare innovation, second edition. Sudbury, MA: Jones and Bartlett Publishers.
Quill, T. E., and A. P. Abernethy. 2013. Generalist plus specialist palliative care—creating a more sustainable model. New England Journal of Medicine 368(13):1183-1174.
Quill, T. E., and P. Townsend. 1991. Bad news: Delivery, dialogue, and dilemmas. Archives of Internal Medicine 151(3):463-468.
Quinn, E. M., M. A. Corrigan, S. M. McHugh, D. Murphy, J. O’Mullane, A. D. Hill, and H. P. Redmond. 2012. Breast cancer information on the internet: Analysis of accessibility and accuracy. Breast 21(4):514-517.
Ramsey, S., and V. Shankaran. 2012. Managing the financial impact of cancer treatment: The role of clinical practice guidelines. Journal of the National Comprehensive Cancer Network 10(8):1037-1042.
Ramsey, S. D., D. Blough, A. Kirchhoff, K. Kreizenbeck, C. R. Fedorenko, K. S. Snell, P. Newcomb, W. Hollingworth, and K. Overstreet. 2013. Washington state cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Affairs (Millwood) 10.1377/hlthaff.2012.1263. (epub ahead of print).
Ratzan, S. C., and R. M. Parker. 2001. Introduction. In National Library of Medicine Current Bibliographies in Medicine: Health Literacy. NLM Pub. No. CBM 2000-1, edited by C. R. Selden, M. Zorn, S. C. Ratzan, and R. M. Parker. Bethesda, MD: National Institutes of Health.
Rau, J. 2013. Medicare lags in project to expand hospice. http://www.kaiserhealthnews.org/Stories/2013/May/09/Medicare-delays-experiment-on-hospice-and-curative-care.aspx (accessed May 14, 2013).
Reinhardt, U. E. 2011. The many different prices paid to providers and the flawed theory of cost shifting: Is it time for a more rational all-payer system? Health Affairs (Millwood) 30(11):2125-2133.
Rose, J. H., E. E. O’Toole, N. V. Dawson, R. Lawrence, D. Gurley, C. Thomas, M. B. Hamel, and H. J. Cohen. 2004. Perspectives, preferences, care practices, and outcomes among older and middle-aged patients with late-stage cancer. Journal of Clinical Oncology 22(24):4907-4917.
Roseman, D., J. Osborne-Stafsnes, C. Helwig, S. Boslaugh, and K. Slate-Miller. 2013. Early lessons from four “Aligning Forces for Quality” communities bolster the case for patient-centered care. Health Affairs (Millwood) 32(2):232-241.
Rosenthal, J. A., X. Lu, and P. Cram. 2013. Availability of consumer prices from U.S. hospitals for a common surgical procedure. Journal of the American Medical Association Internal Medicine 173(6):427-432.
Schwartz, M. D., H. B. Valdimarsdottir, T. A. DeMarco, B. N. Peshkin, W. Lawrence, J. Rispoli, K. Brown, C. Isaacs, S. O’Neill, R. Shelby, S. C. Grumet, M. M. McGovern, S. Garnett, H. Bremer, S. Leaman, K. O’Mara, S. Kelleher, and K. Komaridis. 2009. Randomized trial of a decision aid for BRCA1/BRCA2 mutation carriers: impact on measures of decision making and satisfaction. Health Psychology 28(1):11-19.
Sepucha, K. R., J. F. J. Fowler, and J. A. G. Mulley. 2004. Policy support for patient-centered care: The need for measurable improvements in decision quality. Health Affairs (Millwood) Suppl Variation: VAR54-62.
Shah, A., J. J. Paly, J. A. Efstathiou, and J. E. Bekelman. 2013. Physician evaluation of internet health information on proton therapy for prostate cancer. International Journal of Radiation Oncology, Biology, Physics 85(4):e173-e177.
Shankaran, V., S. Jolly, D. Blough, and S. D. Ramsey. 2012. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: A population-based exploratory analysis. Journal of Clinical Oncology 30(14):1608-1614.
Shepperd, S., B. Wee, and S. E. Strauss. 2011. Hospital at home: home-based end of life care. Cochrane Database of Systematic Reviews 7: CD009231.
Sheridan, S. L., R. P. Harris, and S. H. Woolf. 2004. Shared decision making about screening and chemoprevention: A suggested approach from the U. S. Preventive Services Task Force. American Journal of Preventive Medicine 26(1):56-66.
Siegel, K., D. G. Karus, V. H. Raveis, G. H. Christ, and F. P. Mesagno. 1996. Depressive distress among the spouses of terminally ill cancer patients. Cancer Practice 4(1):25-30.
Silveira, M. J., S. Y. H. Kim, and K. M. Langa. 2010. Advance directives and outcomes of surrogate decision making before death. New England Journal of Medicine 362(13): 1211-1218.
Siminoff, L. A., N. H. Gordon, P. Silverman, T. Budd, and P. M. Ravdin. 2006. A decision aid to assist in adjuvant therapy choices for breast cancer. Psycho-Oncology 15(11):1001-1013.
Smith, T. J. 2003. Tell it like it is. Journal of Clinical Oncology 21(9 Suppl):12s-16s.
Smith, T. J., and B. E. Hillner. 2010. Concrete options and ideas for increasing value in oncology care: The view from one trench. Oncologist (15 Suppl 1):65-72.
———. 2011. Bending the cost curve in cancer care. New England Journal of Medicine 364(21): 2060-2065.
Smith, T. J., and D. L. Longo. 2012. Talking with patients about dying. New England Journal of Medicine 367(17):1651-1652.
Smith, T. J., L. A. Dow, E. Virago, J. Khatcheressian, L. J. Lyckholm, and R. Matsuyama. 2010. Giving honest information to patients with advanced cancer maintains hope. Oncology (Williston Park) 24(6):521-525.
Smith, T. J., L. A. Dow, E. A. Virago, J. Khatcheressian, R. Matsuyama, and L. J. Lyckholm. 2011. A pilot trial of decision aids to give truthful prognostic and treatment information to chemotherapy patients with advanced cancer. Journal of Supportive Oncology 9(2):79-86.
Smith, T. J., S. Temin, E. R. Alesi, A. P. Abernethy, T. A. Balboni, E. M. Basch, B. R. Ferrell, M. Loscalzo, D. E. Meier, J. A. Paice, J. M. Peppercorn, M. Somerfield, E. Stovall, and J. H. Von Roenn. 2012. American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. Journal of Clinical Oncology 30(8):880-887.
Sommers, R., S. D. Goold, E. A. McGlynn, S. D. Pearson, and M. Danis. 2013. Focus groups highlight that many patients object to clinicians’ focusing on costs. Health Affairs (Millwood) 32(2):338-346.
Spinks, T., H. W. Albright, T. W. Feeley, R. Walters, T. W. Burke, T. Aloia, E. Bruera, A. Buzdar, L. Foxhall, D. Hui, B. Summers, A. Rodriguez, R. Dubois, and K. I. Shine. 2012. Ensuring quality cancer care: A follow-up review of the Institute of Medicine’s 10 recommendations for improving the quality of cancer care in America. Cancer 118(10):2571-2582.
Stacey, D., R. Samant, and C. Bennett. 2008. Decision making in oncology: A review of patient decision aids to support patient participation. CA: A Cancer Journal of Clinicians 58(5):293-304.
Stacey, D., C. L. Bennett, M. J. Barry, N. F. Col, K. B. Eden, M. Holmes-Rovner, H. Llewellyn-Thomas, A. Lyddiatt, F. Légaré, and R. Thomson. 2011. Decision aids to help people who are facing health treatment or screening decisions. Cochrane Database of Systematic Reviews (10): CD001431.
Stump, T. K., N. Eghan, B. L. Egleston, O. Hamilton, M. Pirollo, J. S. Schwartz, K. Armstron, J. R. Beck, N. J. Meropol, and Y.-N. Wong. 2013. Cost concerns of patients with cancer. Journal of Oncology Practice (epub ahead of print).
Surbone, A. 2010. Cultural competence in oncology: Where do we stand? Annals of Oncology 21(1):3-5.
Tai-Seale, M., C. Wilson, S. Tapper, P. Cheng, S. Lai, F. Wu, and J. Newman. 2012. CC1-03: Documentations of advanced health care directives in the electronic health record: Where are they? Clinical Medicine & Research 10(3):167.
Tamman, M. 2013. U.S. federal judge lifts ban on public access to Medicare data. http://www.reuters.com/article/2013/05/31/medicare-lawsuit-idUSL2N0EC25U20130531 (accessed July 31, 2013).
Temel, J. S., J. A. Greer, A. Muzikansky, E. R. Gallagher, S. Admane, V. A. Jackson, C. M. Dahlin, C. D. Blinderman, J. Jacobsen, W. F. Pirl, J. A. Billings, and T. J. Lynch. 2010. Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine 363(8):733-742.
Temel, J. S., J. A. Greer, S. Admane, E. R. Gallagher, V. A. Jackson, T. J. Lynch, I. T. Lennes, C. M. Dahlin, and W. F. Pirl. 2011. Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: Results of a randomized study of early palliative care. Journal of Clinical Oncology 29(17):2319-2326.
Teno, J. M., B. R. Clarridge, V. Casey, L. C. Welch, T. Wetle, R. Shield, and V. Mor. 2004. Family perspectives on end-of-life care at the last place of care. Journal of the American Medical Association 291(1):88-93.
The, A.-M., T. Hak, G. Koeter, and G. van Der Wal. 2000. Collusion in doctor-patient communication about imminent death: An ethnographic study. BMJ 321(7273):1376-1381.
Tilburt, J. C., M. K. Wynia; R. D. Sheeler, B. Thorsteinsdottir, K. M. James, J. S. Egginton, M. Liebow, S. Hurst, M. Danis, and S. D. Goold. 2013. Journal of the American Medical Association 310(4):380-388.
Tinetti, M. E. 2012. The retreat from advanced care planning. Journal of the American Medical Association 307(9):915-916.
UCSF Carol Franc Buck Breast Cancer Center. 2012. Decision services. http://www.decisionservices.ucsf.edu (accessed January 4, 2013).
Uitterhoeve, R. J., J. M. Bensing, R. P. Grol, P. H. Demulder, and T. van Achterberg. 2010. The effect of communication skills training on patient outcomes in cancer care: A systematic review of the literature. European Journal of Cancer Care 19(4):442-457.
Veroff, D., A. Marr, and D. E. Wennberg. 2013. Enhanced support for shared decision making reduced costs of care for patients with preference-sensitive conditions. Health Affairs (Millwood) 32(2):285-293.
Villas Boas, P. J., R. S. Spagnuolo, A. Kamegasawa, L. G. Braz, A. Polachini do Valle, E. C. Jorge, H. H. Yoo, A. J. Cataneo, I. Correa, F. B. Fukushima, P. do Nascimento, N. S. Modolo, M. S. Teixeira, E. I. de Oliveira Vidal, S. R. Daher, and R. El Dib. 2012. Systematic reviews showed insufficient evidence for clinical practice in 2004: What about in 2011? The next appeal for the evidence-based medicine age. Journal of Evaluating Clininical Practice 19(4):633-637.
Volandes, A. E., M. K. Paasche-Orlow, S. L. Mitchell, A. El-Jawahri, A. D. Davis, M. J. Barry, K. L. Hartshorn, V. A. Jackson, M. R. Gillick, E. S. Walker-Corkery, Y. Chang, L. López, M. Kemeny, L. Bulone, E. Mann, S. Misra, M. Peachey, E. D. Abbo, A. F. Eichler, A. S. Epstein, A. Noy, T. T. Levin, and J. S. Temel. 2013. Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. Journal of Clinical Oncology 31(3):380-386.
Wagner, E. H., E. J. Aiello Bowles, S. M. Greene, L. Tuzzio, C. J. Wiese, B. Kirlin, and S. B. Clauser. 2010. The quality of cancer patient experience: perspectives of patients, family members, providers and experts. Quality and Safety in Health Care 19(6):484-489.
Weeks, J. C., P. J. Catalano, A. Cronin, M. D. Finkelman, J. W. Mack, N. L. Keating, and D. Schrag. 2012. Patients’ expectations about effects of chemotherapy for advanced cancer. New England Journal of Medicine (17):1616-1625.
Wentlandt, K., M. K. Krzyzanowska, N. Swami, G. M. Rodin, L. W. Le, and C. Zimmermann. 2012. Referral practices of oncologists to specialized palliative care. Journal of Clinical Oncology 30(35):4380-4386.
Wilson, C. J., J. Newman, S. Tapper, S. Lai, P. H. Cheng, F. M. Wu, and M. Tai-Seale. 2013. Multiple locations of advance care planning documentation in an electronic health record: Are they easy to find? Journal of Palliative Medicine 16(9):1089-1094.
Wilson, K., and S. Schettle. 2013. A grassroots initiative for end-of-life planning. Health Affairs (Millwood) 34(4):823-824.
Wittenberg-Lyles, E., J. Goldsmith, B. Ferrell, and S. L. Ragan. 2013. Communication in palliative nursing. New York: Oxford University Press.
Wright, A. A., A. Ray, B. Zhang, J. W. Mack, S. L. Mitchell, M. E. Nilsson, E. T. Trice, S. D. Block, P. K. Maciejewski, and H. G. Prigerson. 2008. Medical care and emotional distress associated with advanced cancer patients’ end-of-life discussions with their physicians. Journal of Clinical Oncology (May 20 Suppl):abstr 6505.
Wright, A. A., N. L. Keating, T. A. Balboni, U. A. Matulonis, S. D. Block, and H. G. Prigerson. 2010. Place of death: Correlations with quality of life of patients with cancer and predictors of bereaved caregivers’ mental health. Journal of Clinical Oncology 28(29):4457-4464.
Yung, V. Y., A. M. Walling, L. Min, N. S. Wenger, and D. A. Ganz. 2010. Documentation of advance care planning for community-dwelling elders. Journal of Palliative Medicine 13(7):861-867.
Zabora, J., K. BrintzenhofeSzoc, B. Curbow, C. Hooker, and S. Piantadosi. 2001. The prevalence of psychological distress by cancer site. Psychooncology 10(1):19-28.
Zafar, S. Y., J. M. Peppercorn, D. Schrag, D. H. Taylor, A. M. Goetzinger, X. Zhong, and A. P. Abernethy. 2013. The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18(4):381-390.
Zikmund-Fisher, B. J., M. P. Couper, E. Singer, P. A. Ubel, S. Ziniel, F. J. Fowler, Jr., C. A. Levin, and A. Fagerlin. 2010. Deficits and variations in patients’ experience with making 9 common medical decisions: The DECISIONS survey. Medical Decision Making 30(5 Suppl):85S-95S.






























































