4
Equity-Focused Approaches to Obesity Prevention in Workplaces
Important Points Made by Speakers
• The number of workplace wellness programs has been growing as employers increasingly recognize their potential to reduce medical spending, absenteeism, and employee turnover. (Crawford)
• New tools and approaches used to improve the health of employees should be tailored to the needs, belief systems, and histories of particular groups. (Baxter)
• Wellness programs can be kept quite low in cost while generating large health benefits. (Anthony)
Goal 4 in Accelerating Progress in Obesity Prevention (IOM, 2012a), directed at health care providers, insurers, and employers (see Box 4-1), was discussed during two different sessions at the workshop: the first, summarized in this chapter, looked at workplace environments; the second, summarized in the next chapter, examined the role of health care providers and insurers in obesity prevention.
As noted in Accelerating Progress in Obesity Prevention, many jobs have become more sedentary in recent decades, and the resulting decrease in energy expended at work has been associated with increased obesity. Increased obesity, in turn, raises employers’ costs through greater use of sick leave, more absenteeism, greater use of disability benefits, more workplace injuries, and higher health care costs. Obesity prevention can reduce these costs, leaving both employers and employees better off.
Three speakers examined the workplace as a venue for increasing employee wellness and decreasing health disparities. Standing committee
BOX 4-1
Goal 4 from Accelerating Progress in Obesity Prevention
Goal: Expand the role of health care providers, insurers, and employers in obesity prevention.
Recommendation: Health care and health service providers, employers, and insurers should increase the support structure for achieving better population health and obesity prevention.
member Patricia Crawford, cooperative extension nutrition specialist in the Department of Nutritional Science and Toxicology and adjunct professor in the School of Public Health at the University of California, Berkeley, described the rapid expansion of workplace wellness programs and their potential to improve health. Ray Baxter, Kaiser Permanente’s senior vice president for community benefit, research, and health policy, summarized the approaches being used by his company to improve the health of its employees and customers. Finally, Sharen Anthony, with the Public Health Foundation Enterprises Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), discussed how the benefits of an employee wellness program can extend beyond individual employees.
THE POTENTIAL OF EMPLOYEE WELLNESS PROGRAMS
Summary of Remarks by Patricia Crawford
More than 60 percent of Americans are in the workforce, and employed adults spend a quarter of their lives at their worksite, noted Crawford. Work can have both negative and positive effects on health. Sedentary jobs can contribute to decreased fitness and increased body mass index (BMI) levels (Choi et al., 2010; Church et al., 2011). In addition, foods available at worksites may not contribute to a healthy diet. But worksites also can offer wellness programs, and in recent years the number of such programs has been growing (Stoltzfus, 2009). Today, 77 percent of large manufacturers have some type of worksite wellness program, as do 22 percent of small businesses (Baicker et al., 2010; MetLife, 2010). Worksite wellness is a $6 billion business, and hundreds of vendors offer such programs to employers (Forbes, 2013).
The majority of worksite wellness programs have focused on preventing weight gain and changing the environment, whether by making physical activity opportunities or healthy foods more available (Salinardi et al., 2013). Some target high-risk behaviors such as smoking. Some include obesity management or weight loss programs at the worksite, while others focus on obesity prevention. Crawford explained that workplaces can help reduce the overconsumption of sugar-sweetened beverages, deliver messages about physical activity and nutrition, ensure proper labeling of foods, and promote breastfeeding-friendly environments. The field is evolving rapidly, she said, driven partly by the needs of organizations and partly by external policies such as the Patient Protection and Affordable Care Act of 2010.1
Research results have been mixed on the effectiveness of worksite wellness programs. Some have found little change in measures of health (Salinardi et al., 2013). On the other hand, others have found that such programs create a culture of health within organizations (Anderko et al., 2012). This culture of health in the workplace may have effects that are difficult to document in the short term but in the longer term may yield such benefits as lower employee turnover (Isaac, 2010). Studies also have shown that wellness programs are associated with lowered medical costs, reduced absenteeism, and improved work productivity (Goetzel and Ozminkowski, 2008; Heinen and Darling, 2009; Merrill et al., 2011).
The presentations at the workshop focused on the particular strategy from Accelerating Progress in Obesity Prevention of creating or expanding healthy environments by establishing, implementing, and monitoring policy initiatives that support wellness. Crawford concluded, however, by noting that obesity prevention efforts in the workplace inevitably overlap and merge with those implemented in other settings.
“The workplace can be a microcosm for society.” —Patricia Crawford
___________________
1Patient Protection and Affordable Care Act, Public Law 111-148, 111th Cong. (March 23, 2010).
CASE STUDY: TOTAL HEALTH AT KAISER PERMANENTE
Summary of Remarks by Ray Baxter
Kaiser Permanente, a prepaid fully integrated health care delivery system that began about 70 years ago in the shipyards of Oakland, California, has a diverse workforce that is scattered throughout the San Francisco Bay Area. Baxter explained that although all members of its workforce have access to the same health care system, their health conditions mirror those of the neighborhoods in which they live, reflecting the influence of social and environmental factors on peoples’ choices and behaviors.
Recognizing the influence of these factors, Kaiser Permanente has been taking an integrated approach to four diseases—cardiovascular disease, diabetes, cancer, and chronic respiratory disease—and four modifiable risk factors that play a role in these diseases—unhealthy diet, inactivity, the use of tobacco, and the harmful use of alcohol (see Figure 4-1). These risk factors can be difficult to change because they involve behaviors that are easy to adopt and are accepted by society, Baxter said. At the same time, however, these risk factors also can be modified by a wide range of interventions. Stairways, sidewalks, and traffic features that protect pedestrians can help increase physical activity, for example, while marketing can promote healthy instead of unhealthy products. No one approach alone is sufficient, said Baxter. But a combination involving individuals, families, schools, worksites, neighborhoods, communities, and society in general—which Kaiser Permanente has termed “Total Health”—can make a difference (see Figure 4-2).
Powerful tools now are available with which to engage with patients and help them change their behaviors, Baxter pointed out. Online health coaching, mobile apps, social media, and other applications of new media can engage many consumers. Clinical care can include reference to optimal resources and support; for example, any patient seen by a Kaiser Permanente provider is asked about smoking and physical activity. Support for healthy pregnancies can include support for breastfeeding. Prediabetics can receive interventions to keep them from converting to full-blown diabetics.
Baxter emphasized that all of these tools and approaches can be used for obesity prevention and treatment. To be most effective, however, they need to be tailored to the needs, belief systems, and histories of
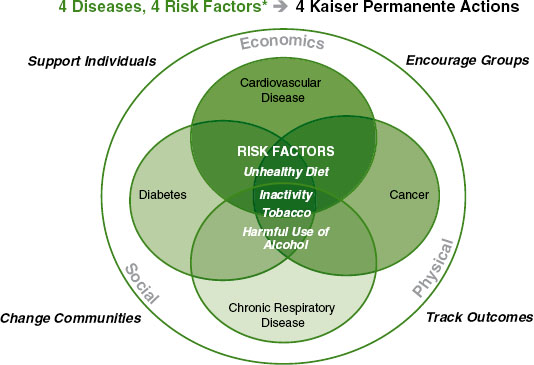
FIGURE 4-1 Kaiser Permanente is taking an integrated approach to diseases and risk factors.
*Aligns with the World Health Organization’s framework for monitoring noncommunicable diseases.
SOURCE: Recreated from the World Health Organization (http://www.who.int/ncdnet/about/4diseases/en).
particular groups. For example, culturally grounded health education might include cooking classes or translations of health education materials, while tapping into traditions such as dance or foods can resonate with particular groups. Community partners can bring to bear competencies and models that health care providers may lack. The real challenge, said Baxter, is to scale up successful culturally appropriate programs to promote equity.
Last year Kaiser Permanente reached a labor agreement2 with the coalition of unions that represents nearly 100,000 of its workers. That agreement includes a collective incentive program to achieve a 5 percent improvement in BMI, smoking, blood pressure, and cholesterol by the end of 2016. Rewards recognize the collective achievement of groups, not changes in individual employees, thereby taking advantage of the
___________________
2See http://www.lmpartnership.org/what-is-partnership/national-agreements/2012-national-agreement.
social mechanisms that drive behavior change. (Baxter noted in the discussion session that more research on incentives and behaviors would help companies structure such programs.)
The company also is making its Total Health approaches available to its customers. It offers a portfolio of services to help organizations improve the health of their workforce, including lifestyle health coaching, communications, analytics, and reporting. The company is bringing workforce health resources to almost 500 cities in California.3 Beyond working with employers, the company is working with more than 40 communities to support local groups (Kaiser Permanente, 2011). And in this work it is focusing on individuals and communities with the least access to healthy foods and activities and engaging them in the design of solutions.
During the discussion period, Baxter noted some of the specific ways in which Kaiser Permanente has addressed disparity issues. Rather than adopting what Baxter called “peanut butter programs,” in which the same approach is applied universally, the company uses unit-based teams— small groups working on problems that are aligned with its priorities.
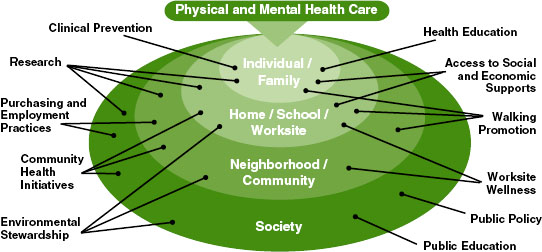
FIGURE 4-2 Changing deep-seated behaviors requires deploying a wide range of assets.
SOURCE: Kaiser Permanente, internal graphic used to outline Total Health efforts.
___________________
3See http://www.cacities.org/Top/Partners/Cities-for-Workforce-Health.
These small groups can adopt ideas used elsewhere and tailor those ideas for their own purposes. For example, a group with particularly inflexible schedules might work on ways to increase physical activity.
“We have to engage everyone in the organization in changing behavior and in changing the culture of the organization in a fundamental way. And to do that we have to support each other. We have to do it collectively, not as a payment or punishment on an individual basis but on a collective basis. This is a grand experiment in doing things differently.” —Ray Baxter
IMPROVING THE HEALTH OF WIC EMPLOYEES
Summary of Remarks by Sharen Anthony
The California WIC program is the nation’s largest, with 3,500 staff serving almost 1.4 million mothers and children each month (National WIC Association, 2013). The California WIC Association, a nonprofit organization formed by the directors of local WIC agencies, has a WIC Worksite Wellness program whose motto is “work well, be well, live well.” To become a wellness worksite, a WIC agency needs to make a commitment to the program, designate a wellness coordinator and team, conduct a staff wellness preprogram survey, complete a 10-step workplan, and request to be certified. The workplan covers the following elements:
• healthy foods,
• community building,
• physical activity,
• wellness coordinator,
• general health,
• wellness communication,
• mental health support,
• senior-level and board support,
• lactation accommodation, and
• periodic evaluation.
At the time of the workshop, 30 WIC agencies were certified as wellness worksites.4
Anthony described the activities of the local WIC agency with which she works, the Public Health Foundation Enterprises WIC Program, which has more than 650 employees. Building on the WIC food package changes made in 2009, the wellness program, known as Health is Wealth, promotes and reinforces healthy eating and active lifestyles among WIC employees. Staff members track health indicators such as blood pressure, glucose levels, and BMI in a health passport. Staff also submit ideas for the program and vote on suggested options. A “Health is Wealth” link on the internal intranet provides staff success stories, local opportunities for fitness, and other information.
The program is run on a shoestring budget, said Anthony, but the WIC agency has worked hard to get staff buy-in and support. A Health is Wealth advisory board comprising administrative and front-line support staff oversees the program, and the program has enlisted allies to further the agency’s wellness activities. According to Anthony, experience with the program has shown that inexpensive steps, such as canvas bags with wellness messages, pedometers, and exercise DVDs for Instant Recess®, can make a difference in helping staff be more active and make better dietary choices.
The cost of the wellness program for the agency is about $100 per employee per year, or about $2 per employee per week, and the benefits to employees are immense, Anthony said. Furthermore, although change cannot happen overnight, the program’s impacts go well beyond individual employees. Behavior changes made by one employee can have a ripple effect, extending to coworkers, WIC clients, families, friends, and the community. For example, some staff in the agency have championed Kaiser Permanente’s “Everybody Walk” program, and employees are now walking 6 to 7 miles daily. Such activities do not have a direct cost to the agency but can have major health benefits, Anthony explained.
Anthony had one recommendation that would increase the benefits of the WIC employee wellness program. Nutrition services and administrative expenditures under WIC should be expanded, she said, to allow for evidence-based training and interventions and for materials and tools to engage WIC employees in healthy habits and active living.
___________________
4See http://www.calwic.org/focus-areas/wic-worksite-wellness/certified-well-wicworksites for a list of certified agencies.
By meeting the wellness needs of their employees, WIC agencies can better meet the wellness needs of the people they serve, Anthony said, including people affected by disparities. In addition, as she noted in the discussion session, documenting this effect through research could help generate support and additional funding for such efforts.
“We knew that we needed to walk the talk so that we could be role models and cheerleaders for our WIC participants. Therefore, we needed to develop a strategic plan that could have an impact on our staff.” —Sharen Anthony










