3
A Comprehensive Framework
for Ensuring the Health of an
Operational Workforce
When Congress passed the Occupational Safety and Health Act of 19701 with the intent of ensuring safe and healthful working conditions in the United States, it found that “personal injuries and illnesses arising out of work situations impose a substantial burden upon, and are a hindrance to, interstate commerce in terms of lost production, wage loss, medical expenses, and disability compensation payments” (Sec. 2). In recent years, the impacts of poor health and injuries on productivity, profit, and the readiness of a workforce to accomplish its basic mission have been strong driving forces for new workplace initiatives designed to improve employee health and safety. Beyond that motivation, however, the committee asserts that safe and healthful working conditions are a matter not only of workforce effectiveness but also of basic civil rights and expectations.
As described in previous chapters, a significant proportion of the Department of Homeland Security (DHS) workforce operates outside of conventional workspaces on a routine or recurring basis, creating challenges to protecting employee health not encountered in most other federal agencies. A comprehensive approach to workforce health protection at DHS must be responsive to these challenges. This chapter delineates a comprehensive framework for ensuring the health of an operational workforce. It then details in turn the key functions that support the two pillars of this framework—medical readiness and medical support for operations. The final section addresses the integration of essential workforce health
__________________
129 USC 651.
protection functions that underpins the entire framework and is vital if the functions are to be carried out successfully.
WORKFORCE HEALTH PROTECTION AND MISSION SUCCESS
Former DHS Deputy Secretary Lute (2013), addressing the Institute of Medicine (IOM) Committee on Department of Homeland Security Workforce Resilience, said that homeland security is not about unity of command but unity of effort. The DHS workforce, although highly diverse, is united by its common mission—to create a safe, secure, resilient homeland where the American way of life can thrive (Lute, 2013). The ability to fulfill that mission depends on the mission readiness of the DHS workforce. A workforce that is mission ready is physically capable, mentally prepared, trained, equipped, and adequately supported for the job. Protecting the homeland can be physically and mentally demanding, with many inherent risks. Consequently, mission readiness depends, in part,2 on
- a workforce that is medically ready (free of health-related conditions that would impede the ability to participate fully in operations and achieve the goals of its mission); and
- the capability to provide medical support to the workforce during planned and contingency operations.
Workforce health protection, as an overarching strategy for promoting, protecting, and restoring the physical and mental well-being of the workforce, addresses both of these requirements. It encompasses a broad set of activities focused on promotion, prevention, surveillance, detection, early intervention, treatment, recovery, and reintegration. The health protection program must be more, however, than the sum of its parts. Like the agency itself, workforce health protection must be about unity of effort if it is to be effective.
A FRAMEWORK FOR ENSURING THE HEALTH OF AN OPERATIONAL WORKFORCE
In its statement of task, the committee was asked to identify the key functions of an integrated occupational health and operational medicine infrastructure. It did so by examining and identifying commonalities in the major elements of employee health protection and promotion programs of public and private organizations. While recognizing the limitations of
__________________
2There are many other determinants of mission readiness that are beyond the scope of this report.
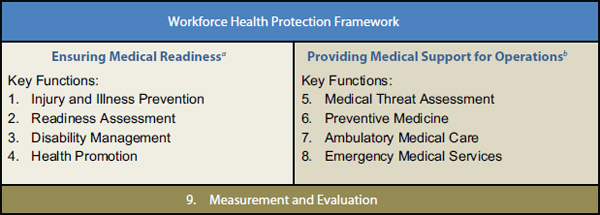
FIGURE 3-1 A two-pillar framework with nine essential functions that support the health of an operational workforce.
aMedical readiness is the extent to which members of the operational workforce are free of health-related conditions that would impede their ability to participate fully in operations and achieve the goals of their mission.
bMedical support for operations consists of preventive and responsive medical and health support services provided outside of conventional workplaces during routine, planned, and contingency operations to employees and others under the organization’s control.
applying Department of Defense (DoD) models to a civilian government agency, the committee found the DoD force health protection concept (DoD, 2004) useful in framing the key functions of workforce health protection for DHS. The committee therefore adapted the DoD force health protection model to derive a framework for ensuring the health of a civilian operational workforce (see Figure 3-1).
The two pillars of this framework reflect the two medical requirements for mission readiness: medical readiness and operational medical support. In total, as shown in Figure 3-1, the committee identified nine essential and interconnected functions of workforce health protection that support an operational workforce. Measurement and evaluation spans both pillars and serves as a foundation for the framework. Without measurement and evaluation, the medical readiness and medical response capability of the DHS workforce cannot be assessed, reported, or improved.
A unified strategy for workforce health protection will integrate and therefore ensure coordination of the nine key functions, resulting in
- a prevention-focused approach to workplace injury and illness that creates a safe, supportive working environment;
- ongoing readiness assessment to ensure an individual’s continued ability to carry out his/her responsibilities fully and safely;
- proactive medical case management to restore employees to a state of health and readiness as rapidly as possible;
- adequate and effective preventive and responsive medical support services available when needed;
- promotion of physical fitness and healthy lifestyle choices to optimize human performance and readiness; and
- ongoing measurement and evaluation for decision making, accountability, situational awareness, and continuous quality improvement.
The underlying infrastructure that serves to integrate these functions includes the doctrine (plans, policies, and standards), organizational constructs (reporting structures, governance mechanisms), and resources (qualified personnel, budgets, information management systems) that enable mission capability.
The subsections below provide a description of the four key functions for ensuring medical readiness that form the first pillar of the workforce health protection framework presented above (see Figure 3-1) and explain their importance. The remainder of the framework is discussed later in the chapter.
Injury and Illness Prevention
In the Occupational Safety and Health Act of 1970, “Congress declares it to be its purpose and policy … to assure so far as possible every working man and woman in the Nation safe and healthful working conditions … by encouraging employers and employees in their efforts to reduce the number of occupational safety and health hazards at their places of employment, and to stimulate employers and employees to institute new and to perfect existing programs for providing safe and healthful working conditions.” To achieve this purpose, it has since 1970 been customary and expected practice for all but the smallest public and private employers to establish and implement comprehensive occupational safety and health programs.
Occupational safety and health programs facilitate risk management—a continuous, multistep process designed to reduce risks to health, mission, and property. The three main elements of risk management are (1) hazard identification, (2) risk assessment, and (3) risk control. Hazards are identified by observation (through workplace inspections and job hazard analyses) or from past experiences (e.g., root cause and trend analyses following injuries and illnesses). Once a hazard has been identified, a risk assessment process is used to determine the likelihood that the hazard
will cause a mishap and the severity (human health and property damage) should a mishap occur. This information is used in the assignment of risk assessment categories, which indicate the level to which risks from a hazard should be managed. Risks can be controlled through (1) engineering controls, (2) administrative procedures/work practices (e.g., training, standard operating procedures, posted signs, vaccination), and (3) the use of personal protective and other safety equipment (USCG, 2013). In operational settings, tension can exist between occupational safety and health objectives and mission requirements. Operational risk management enables risk-based decision making, the goal of which is to control risks to acceptable levels consistent with the organization’s mission—minimizing risk without compromising mission success.
Occupational safety professionals are often focused on the prevention of traumatic injuries and workplace fatalities through mitigation of safety hazards, whereas industrial hygienists provide expertise on the identification and control of health hazards from acute or chronic exposure to chemical, biological, and physical agents. Ergonomists are concerned with ensuring that the design of workspaces, equipment, and work tasks suits the individual worker so as to prevent disorders resulting from cumulative trauma, most notably musculoskeletal disorders (NRC, 2000). Although occupational safety and health program staff have an important role to play in providing guidance and performing evaluations to ensure compliance with policy and regulations, risk management is considered a primary responsibility of those most familiar with their workplace hazards—individuals and operational units at the local level (The Conference Board, 2003). A centralized oversight entity cannot predict safety and health risks for each worksite and so must provide employees with the tools and information to make sound risk management decisions.
Requirements for Federal Agency Occupational Safety and Health Programs
Section 19 of the Occupational Safety and Health Act of 1970 requires that all federal employees be provided with “safe and healthful places and conditions of employment.” To this end, the act assigns responsibility for establishing and maintaining “an effective and comprehensive occupational safety and health program” to heads of federal agencies. Further roles and responsibilities for federal agency occupational safety and health programs are delineated in Federal Executive Order 121963—Occupational Safety and Health Programs for Federal Employees (1980)—which requires
__________________
3Executive Order 12196—Occupational Safety and Health Programs for Federal Employees, 45 FR 12769, 3 CFR, 1980 Comp., p. 145. Feb. 26, 1980.
federal agencies to apply occupational safety and health practices that are required of nongovernmental activities regulated by the Occupational Safety and Health Administration (OSHA) and outlines several basic administrative controls to support this compliance. All of the items delineated in that executive order bear on the subject of the present analysis, but two specific requirements placed on federal agencies merit special mention: “designate an agency official with sufficient authority to represent the interest and support of the agency head to be responsible for the … program,” and “operate an occupational safety and health management information system.” As required by Executive Order 12196, the Code of Federal Regulations, Title 29, part 1960 (29 CFR 1960) specifies the basic program elements that all federal agency occupational safety and health programs should encompass. Provisions built into those elements give agencies the flexibility needed to implement programs tailored to their organizational and mission requirements.
Federal agencies must submit annual reports of occupational injuries and illnesses to the Bureau of Labor Statistics and OSHA. The Bureau of Labor Statistics uses this information to generate aggregated injury and illness data from across the federal government; OSHA uses it to target federal agencies for compliance inspections (29 CFR 1960). OSHA administers citations but does not fine federal agencies for failure to comply with regulations and standards (OSHA, 2013).
Despite the above regulations, tens of thousands of injuries and illnesses, many of which are preventable, continue to occur each year in federal workplaces. The annual government-wide workers’ compensation costs associated with these events total almost $3.0 billion (OWCP, 2013). To address this burden, President Obama established a 4-year Protecting Our Workers and Ensuring Reemployment (POWER) initiative in July 2010 (Obama, 2010). The POWER initiative requires all executive departments and agencies, through aggressive performance targets, root cause analysis, and adoption of proven safety and health management programs, to improve their performance in workplace safety and health in seven areas:
- reducing total injury and illness case rates,
- reducing lost time injury and illness case rates,
- analyzing lost time injury and illness data,
- increasing the timely filing of workers’ compensation claims,
- increasing the timely filing of wage-loss claims,
- reducing lost production day rates, and
- speeding employees’ return to work in cases of serious injury or illness.
Through these objectives, the POWER initiative places shared responsibility for employee health on the occupational safety and health programs designed to prevent injury and illness and on disability management programs responsible for helping injured and ill employees return to work as quickly as possible.
Best Practices in Occupational Safety and Health
Best practices in occupational safety and health can be viewed as features of a systematic approach that leads to highly effective control of injuries, illnesses, and disability and thereby to a healthier workforce. Such a systematic approach—called by some an occupational safety and health management system or, in OSHA’s terms, an injury and illness prevention program—provides a “flexible, commonsense, proven tool to find and fix hazards before injuries, illnesses, or deaths occur” (Hagemann, 2013). OSHA has identified six core elements essential to an injury and illness prevention program: management leadership, employee participation, hazard identification, hazard prevention and control, education and training, and program evaluation and improvement (Hagemann, 2013). The importance of these elements to the effectiveness of occupational safety and health programs is supported by research on the characteristics of an occupational safety and health management system that appear to lead to the greatest improvement in safety and health outcomes (Shannon et al., 1997).
Medical Countermeasures Programs
Medical countermeasures programs, which span the fields of occupational medicine and occupational safety and health, are critical not only to ensuring public health but also to preventing illness among federal employees who serve in operational capacities. The anthrax mailings in 2001, the severe acute respiratory syndrome (SARS) epidemic in 2003, and the H1N1 influenza pandemic in 2009 highlighted the importance of preparedness planning for large-scale chemical, biological, radiological, and nuclear events that can threaten both public health and business operations across the globe. Workplace plans to ensure continuity of business operations are particularly important for those members of the workforce who are considered mission-essential personnel; strategies for distribution and dispensing of medical countermeasures4 to prevent and mitigate the health effects of
__________________
4Medical countermeasures include biologics (e.g., vaccines, antimicrobials, antibody preparations), nonbiologic materials and devices (e.g., ventilators, diagnostic devices, personal protective equipment such as face masks and gloves), and public health interventions (e.g., contact and transmission interventions, social distancing, community shielding).
chemical, biological, radiological, and nuclear hazards are critical elements of such contingency plans. Agencies that play a key role in the federal response to chemical, biological, radiological, and nuclear events, including the Department of Health and Human Services and DHS, are required by executive order (Obama, 2009) to have in place programs that enable the capability to dispense medical countermeasures to their workforce rapidly following such an attack to ensure that mission-essential functions of federal agencies are not disrupted.
Readiness Assessment
Workers in many occupations may, in the course of their daily operations, be required to perform work that is arduous and/or hazardous in nature. Not only must they be capable of performing those duties, but they must be able to so without posing a threat to their own health and wellbeing or that of others. Key to ensuring this capability is readiness assessment, which includes developing medical and physical ability standards and conducting fitness-for-duty and fitness-for-deployment evaluations.
Medical and Physical Ability Standards
There is no one accepted method for the development of medical and physical ability standards; however, two criteria (i.e., fitness-for-duty drivers) generally are considered: (1) essential job tasks, and (2) the environmental conditions and circumstances under which those tasks must be performed. These criteria are identified through a job task analysis, which can be conducted internally or contracted out and ideally involves human resources and medical personnel, as well as individuals currently employed in that occupation. The California Commission on Peace Officer Standards and Training recommends a variety of techniques for conducting job task analyses, including “review of current job descriptions, interviews with supervisors and employees, development and administration of questionnaires, use of daily job diaries by employees, [and] review of records (e.g., police reports, critical incident reports).” Also recommended is the use of someone experienced in conducting such analyses and consultation with “several employees under a range of conditions” whenever possible (Goldberg et al., 2004, p. 23). Generally, the resulting list of essential job functions is not comprehensive but focuses on those tasks that impact a physician’s determination of an individual’s ability to do the job.
The development of medical and physical ability standards from the results of a job task analysis is not a simple process of identifying disqualifying medical and physical conditions. For most conditions, simply having the condition does not preclude an individual from being able to perform
essential job tasks, as the condition’s impact can depend on its degree or severity. Generally, medical and physical ability standards provide guidance to physicians on how to conduct a thorough examination (by body system) and how to quantify safety risks associated with having a given condition. The standards are subject to much interpretation, and individualized assessments are always required. Additionally, the standards and guidance for fitness for duty need to be maintained as living documents, reviewed and updated periodically, because the evidence base (research and experience) changes over time.
For legal defensibility, medical and physical ability standards need to be closely linked to the essential tasks of a job; consequently, standards developed by one organization cannot necessarily be applied to the jobs of another. For example, the American College of Occupational and Environmental Medicine’s consensus guidance developed for medical evaluation of patrol officers may not be universally applicable across all law enforcement officer positions given the diversity of their functions. Essential job tasks for special weapons and tactics (SWAT) team members may be very different from those for patrol officers. Similarly, medical standards for 1811 series5 criminal investigators at the Federal Bureau of Investigation (FBI) may or may not be applicable to 1811 series investigators at Immigration and Customs Enforcement (ICE) if they are performing different tasks or operating under different conditions. At the same time, however, sharing of medical standards for the purpose of adaptation, particularly for those agencies with employees under the same job series, could reduce the burden (financial and labor) of setting standards and lead to increased uniformity. For example, the FBI and the National Park Service have already developed medical standards for federal law enforcement officers that could be adapted by other agencies. Given that the FBI’s process for developing these standards cost approximately $3.5 million (Wade, 2013), this represents a valuable opportunity for interagency collaboration to improve efficiency across the government.
Medical and physical qualification for federal positions The authority for federal agencies to establish medical evaluation and clearance programs is accorded by Title 5, part 339 of the Code of Federal Regulations (5 CFR 339). Such programs are justified under the regulation as a means of protecting the health of employees whose work poses significant health and safety risks to themselves or others due to occupational or environmental exposures or other demands. The regulation does impose some constraints
__________________
5The 1811 series is the Office of Personnel Management job series for criminal investigators in the federal government.
on federal agencies to ensure that fitness for duty is evaluated on a case-by-case basis:
- The agency is required to grant a waiver when the evidence indicates that an applicant or employee who does not meet the medical or physical standards can, with or without reasonable accommodation, perform the essential functions of the job without endangering him/herself or others.
- Applicants cannot be disqualified from a position based on medical history alone; medical history may be disqualifying only if (1) the medical condition is disqualifying, (2) there is a possibility of its recurrence, and (3) recurrence poses a significant risk of harm to themselves or others.
The Office of Personnel Management (OPM) is responsible for establishing or approving medical standards for government-wide occupations (5 CFR 339). However, when a job series is associated predominantly with a single federal agency (i.e., more than half of all those employed under that job series are employed within a single agency), that agency may establish medical standards for the position without OPM approval. An example of the latter is the border patrol agent job series (GL-1896), which is exclusive to CBP. Agencies do not need OPM approval to establish physical standards, but in accordance with 5 CFR 339, the requirements must be supported by the essential duties of the position and clearly articulated in the position description.
Waivers As noted above, 5 CFR 339 requires that agencies grant a waiver when an individual does not meet medical or physical standards but demonstrates evidence of being able to perform the essential functions of the job safely. Employers can grant waivers but impose restrictions on duty as part of a risk management solution that keeps people on the job who have demonstrated their performance capability. For example, someone diagnosed with major depressive disorder may be granted a waiver on condition of demonstrating active treatment and submitting to annual evaluations (McMillan, 2013)—an important accommodation as the incidence of mental health disorders continues to increase. Waiver processes grant employing agencies considerable flexibility and can help address concerns about how to handle medical issues uncovered during periodic evaluations—concerns that may deter employers from instituting regular medical evaluations. A fair waiver process also can help build trust if employees understand that a diagnosis will not necessarily mean the loss of their job. As described above, line personnel who are intimately familiar with the requirements of the job ideally are involved in decisions regarding waivers, in
consultation with knowledgeable medical authorities. A waiver guide, as is used in some DoD agencies, can help ensure consistency in waiver decisions.
Fitness-for-Duty Evaluations
Fitness-for-duty evaluations compare an individual’s medical status and physical abilities against established medical and physical qualifications. Standards and guidance materials ensure that such practices are transparent, fair, and evidence based. For example, the National Fire Protection Association 1582 Standard on Comprehensive Occupational Medical Program for Fire Departments6 requires that candidates undergo a medical evaluation (to include a medical history, medical examination, and laboratory testing) prior to employment and annually thereafter, the purpose of which is to identify medical conditions that may interfere with the individual’s ability to perform the essential job tasks safely. The standard divides medical conditions into two categories—those that would preclude a team member from safely performing essential job tasks in training or operational environments, and those that could do so, depending on the degree or severity of the condition. The ability of applicants and incumbents with medical conditions in the latter category to perform essential job tasks safely must be assessed before a determination regarding employment can be made.
Similar guidance materials for medical evaluation of law enforcement officers have been issued by the American College of Occupational and Environmental Medicine (ACOEM, 2010)7 and the California Commission on Peace Officer Standards and Training (Goldberg et al., 2004). Commonalities among such standards and guidance include
- ensuring compliance with applicable law and regulations, most notably the Americans with Disabilities Act;
- linking medical conditions with the ability to perform essential job tasks safely;
- promoting individualized assessments (as opposed to stipulating categorical exclusionary criteria); and
- clarifying the roles of the medical review officer and the hiring authority.
Fitness-for-duty evaluation is a risk management process; evidence regarding the immediacy, severity, and likelihood of a risk must be considered.
__________________
6Because fire departments are completely decentralized and there is no central authority over local jurisdictions, adoption of the standard cannot be enforced.
7The American College of Occupational and Environmental Medicine’s guidance is still under development and currently addresses only a few of the planned medical evaluation topics.
However, a determination that a candidate is unable to perform an essential job function because of a disability is not sufficient grounds for an unfit determination. The Americans with Disabilities Act requires that reasonable accommodations be considered on a case-by-case basis. Such accommodations could include “restructuring a job by reallocating or redistributing marginal job functions; altering when or how an essential function is performed; permitting use of accrued paid leave or unpaid leave for necessary treatment; modifying examinations, training materials or policies; [and] acquisition or modification of equipment and devices” (Goldberg et al., 2004, p. 10). To evaluate risk and the potential for its mitigation effectively, evaluating physicians need to be familiar with the essential tasks and demands of the job. This requirement necessitates highly detailed position descriptions, particularly if the medical evaluation is outsourced to someone unfamiliar with the job requirements.
Fitness-for-duty evaluations for positions with medical or physical qualifications may be conducted prior to employment (postoffer but preplacement), periodically throughout employment, or on an as-needed basis during employment. In the latter case, such evaluations may be performed when indicated by noted declines or failures in on-the-job performance, following notification by an employee of a change in health status (e.g., a new diagnosis), and after occupational or personal injury or illness that may temporarily or permanently affect an employee’s ability to perform essential job functions safely. The latter case provides a good reason for ensuring that fitness-for-duty and disability management activities are integrated. When an individual who is required to meet medical qualification standards is injured (on or off the job), it is necessary to assess whether the injury will result in permanent, partial, or total disability. In the case of personal illness, extended leave of absence (as permitted under the Family and Medical Leave Act) may also indicate a need for fitness-for-duty evaluation (McMillan, 2013).
When a potentially problematic medical condition is identified during a fitness-for-duty evaluation, a common next step is follow-up with the individual’s treating physician regarding medical records related to management of the condition. If the individual is an employee, he/she may be placed on restricted duty until a determination is made. The amount of time an individual is allowed to remain on limited duty before the case is sent for a determination will likely vary depending on the circumstances. In the military, up to 2 years may pass before someone on limited duty is sent before a medical review board. In the FBI, the average interval is closer to 3 years (Wade, 2013).
There is no standardized clearance process for fitness for duty. The party that makes determinations regarding reasonable accommodation and employability varies across organizations. In some cases, it may be
an occupational health nurse or a medical review officer (internal or outsourced), and in other cases, a medical review board. A medical review board is used by DoD, the FBI (which calls it a Medical Mandates Evaluation Board), and the Secret Service to make determinations on reasonable accommodation and employability. Notably, medical personnel frequently advise such boards, but voting members often are senior line officers and administrative personnel. It is important to note that fitness-for-duty determination is a process that spans human resources and medical responsibilities, and consequently it requires significant coordination between these two entities.
Concerns Regarding Medical Standards and Fitness-for-Duty Evaluations
Throughout its information-gathering process, the committee heard of several concerns regarding fitness-for-duty evaluations from both organization and employee perspectives. Medical and administrative personnel often are concerned about the constraints and liabilities associated with the Americans with Disabilities Act (ADA) or the Rehabilitation Act (for federal agencies). Both laws prohibit discrimination against those with handicaps or disabilities and have significantly impacted fitness-for-duty evaluations. For example, ADA prohibits preemployment evaluations; instead, employers must make a job offer contingent on meeting medical and/or physical qualifications. ADA also requires an employer to consider whether reasonable accommodations can be made for otherwise qualified individuals with disabilities (employees or applicants) without causing undue hardship for agency operations. ADA and the Rehabilitation Act allow employees to sue8 federal agencies if they are removed from their position on medical grounds, and if the agency fails to meet the burden of proof demonstrating that the employee has a disqualifying medical condition and that the condition poses a reasonable probability of substantial harm.9 These concerns were discussed with the committee by FBI Medical Director Dr. David Wade (2013), who noted that to protect the agency from that litigious environment, a solid job task analysis must be implemented with rigor and with a scientific methodology.
Employees are concerned about protection of their personal medical information and the application of fitness-for-duty evaluation for punitive purposes. For example, psychological fitness-for-duty evaluations sometimes
__________________
8The Equal Employment Opportunity Commission is the entity responsible for enforcing federal laws against employment discrimination. Equal employment opportunity suits can be filed if employees feel they have been subjected to discrimination based on their disability status (EEOC, 2013).
9Slater v. DHS, 2008 MSPB 73 (U.S. Merit Systems Protection Board, 2008).
are ordered as a means of dealing with disruptive behavior (Spottswood, 2013). Union representatives from the Border Patrol and the Federal Protective Service expressed concern about the potential for uneven application of fitness-for-duty evaluation based solely on performance (Shigg, 2013; Wright, 2013). However, they agreed that performance-based standards are necessary to ensure that an employee can capably perform on the job when decreased performance is noticed or upon return to duty following an injury. Both also expressed concern that regular medical examinations have led to systematic abuses in the past and do not accurately gauge an employee’s ability to do the job; from the union’s perspective, they stated, regular medical examination would be a nonstarter. Acknowledging psychological fitness-for-duty evaluations as a serious intrusion into employees’ privacy, Dr. Wade (2013) indicated that policies have been put in place at the FBI prohibiting the use of psychological fitness-for-duty evaluations for punitive purposes.
Consistent, transparent processes, detailed position descriptions, and clear policies that set expectations from the start of employment can help address concerns regarding uneven or punitive use of fitness-for-duty evaluations. More important, to build trust and employee engagement, it is critical that fitness-for-duty programs be designed and promoted as part of an overarching strategy for protecting the health and safety of the workforce and ensuring mission success.
Fitness-for-Deployment Evaluations
Given the health and safety risks faced by workers during deployment to remote and/or hazardous settings (e.g., disaster sites), 5 CFR 339 grants federal agencies the authority to require medical evaluation and clearance prior to deployment for disaster response and recovery work and other planned or contingency operations. For some positions, medical clearance may be a condition of employment, but predeployment clearance programs can also be instituted and applied to employees whose positions are not subject to medical standards.10 The Department of State, for example, has a medical clearance program that determines the posts to which members of the Foreign Service can deploy, but does not have medical standards per se (Rosenfarb, 2013). Predeployment evaluations are particularly critical for volunteers or those in positions not subject to medical standards because no prior information on the health status of such individuals may be known. Multiple organizations examined by the committee, including the Texas Task Force One urban search and rescue team (Minson, 2013) and
__________________
10A relevant example at DHS is predeployment screening and clearance for federal employees who volunteer to deploy as part of the DHS Surge Capacity Force.
the American Red Cross (Smith, 2013), conduct predeployment health assessments using questionnaires.
To mitigate health risks to volunteers, the American Red Cross has developed a system for prescreening volunteer responders. During the application process, potential responders provide an overview of their general health by completing a health status record, which is reviewed and compared with a Physical Capacity Grid that details the capacities necessary for successfully performing 30 different basic tasks entailed in relief operations (Smith, 2013). This process determines the type of job a volunteer can do. The American Red Cross also has developed 15 hardship codes describing common physical, environmental, and emotional situations that may affect individuals on a relief operation. Specific assignments that match the responder’s hardship code need to be discussed with the individual before assignment. Medical restrictions also may be applied that limit the types of disasters for which the responder can be deployed (Smith, 2013). Prior to deployment, a preassignment health questionnaire, consisting of yes/no questions, is completed to ensure that health status records are up to date. Any “yes” response is referred to a reviewer who conducts a health interview with the responder; the responder may then be cleared for deployment or denied for medical reasons.
In May 2010, Federal Occupational Health (FOH)11 proposed a similar program for the Federal Emergency Management Agency (FEMA) to address medical clearance for deployment. Viewing deployment readiness as a safety issue as opposed to an accommodation/employability issue, FOH asserted that environmental conditions (including medical infrastructure at disaster sites, power status, accessibility for those with handicaps, expected ambient temperature, and international sites/ability to medically evacuate) should serve as the major determining factors in clearance for specific deployments. FOH proposed a color-coded system as a means of indicating the types of environmental conditions under which a person can deploy based on the results of a health assessment (FOH, 2010). The proposed system takes into account environmental changes that can occur at disaster sites, enabling employees who may not be cleared to deploy under harsh environmental conditions to deploy later when the environment is more suitable to their status. FOH (2010, p. 1) believes that this approach “would satisfy ADA concerns while helping to ensure we are safely using all skilled employees.” To date, such a program has not been implemented.
__________________
11FOH is a nonappropriated agency within the U.S. Department of Health and Human Services. It is the largest provider of occupational health and wellness services to the federal government.
Disability Management
Disability management has been defined as “a set of practices designed to minimize the disabling impact of injuries and health conditions that arise during the course of employment” (Hunt, 2009, p. 1). Emerging as a tactic for combating rising workers’ compensation costs, disability management has two primary goals: ensuring continued employment for workers with disabilities and lowering employers’ disability costs (Hunt, 2009). Whereas the provision of workers’ compensation benefits addresses the administrative process of ensuring the financial protection of employees who acquire a disability in the course of performing their job, disability management focuses on preventing the worsening of an injury or illness and turnover for disability reasons (Hunt, 2009). The ultimate goal is to ensure timely reintegration of employees into the workforce (return to work). Since the introduction of this concept in the 1970s, principles of disability management have become increasingly commonplace in existing workers’ compensation programs to help organizations meet these goals.
The Federal Employees’ Compensation Act (FECA) provides workers’ compensation benefits (including wage-loss benefits and vocational rehabilitation) to all civilian federal employees who are injured or become ill in the course of performing their job. The act is administered by the Office of Workers’ Compensation Programs (OWCP) in the Department of Labor (DOL), which is the sole entity with the authority to approve or deny a workers’ compensation claim. For traumatic injuries, claims generally are adjudicated by OWCP within 45 days of receipt; this 45-day period is called the continuation-of-pay (COP) period. During this time, employing agencies are responsible for continuing to pay an employee’s salary without requiring the employee to charge sick or annual leave. COP does not apply to occupational disease or recurrence cases (DFEC, 2012). Employing agencies are responsible for advising employees on the process for completing and submitting claims.12
In addition to the administrative aspects of helping injured and ill employees navigate the workers’ compensation claims process, employing agencies are responsible for those aspects of the medical case management process focused on limiting disability and reintegrating injured and recovering employees into the workforce. Support for reintegration may entail providing “light”-duty work when possible or helping to find a new position for employees that are unable to continue carrying out the duties of their old position. OWCP roles in this area include assigning a nurse case manager to ensure provision of appropriate medical care and assist
__________________
12Many agencies have begun using eCOMP, a free, Web-based portal provided by DOL, for the electronic filing of FECA claim forms.
in return to work, providing referral to a medical specialist for a second opinion as necessary, and providing referral for vocational rehabilitation services when an employee is unable to return to his/her previous position (DFEC, 2013).
Return to work can prove difficult under FECA, and more so the longer an employee is away from work. As explained to the committee, FECA “was set up intentionally to be ‘non-adversarial,’ but in return gives enormously generous benefits to the injured worker” (Crowley, 2013), in most cases providing 75 percent of the worker’s date-of-injury salary tax free, with no cap on the amount of compensation or the time for which it is provided. Under FECA, employees have the right to choose their own physician, who determines their ability to work. While an agency can request that DOL refer an injured worker for a second opinion with a physician of DOL’s choosing, it is up to DOL to determine whether doing so is warranted. When a second opinion contradicts the initial determination and is contested by the primary physician, it must then go to an independent medical examiner—a process that can take years (Crowley, 2013). Additionally, following a “total person concept,” if workers have not returned to work and suffer a non-work-related injury, they are eligible to remain on workers’ compensation (Crowley, 2013).
As described earlier, President Obama’s POWER initiative was established to help address the burden of occupational injuries and illnesses on employees, agencies, and the federal government as a whole, in part through return-to-work efforts. The last four of the seven performance areas under POWER relate to workers’ compensation and return to work: increasing the timely filing of workers’ compensation claims, increasing the timely filing of wage-loss claims, reducing lost production day rates, and speeding employees’ return to work in cases of serious injury or illness (Obama, 2010). Although the first two of these areas would appear to be solely administrative in nature, early filing of workers’ compensation claims may translate to earlier intervention to support return-to-work efforts (Tritz, 2013).
The 14 agencies subject to the speeding return to work POWER goal (including DHS) must participate as members in the POWER Return To Work Council, which was chartered to assist OWCP in identifying strategies that could help federal agencies increase return-to-work rates. Council members generally are senior officials with oversight of agency workers’ compensation programs. As part of these efforts, DOL initiated a study on best practices in return to work. The Council reviewed the results of that study, and the following five practices it deemed useful to the
greatest number of agencies were developed into a DOL (2013) guidance document13:
- [have] early contact with injured workers,
- provide modified work positions for short-term injuries,
- communicate within the agency,
- review periodic roll cases and discuss with OWCP, and
- present disability costs to directors and operational managers.
Increasing evidence from the literature shows that early intervention programs can improve return-to-work outcomes for injured workers (Carroll et al., 2010; DOL, 2013; Hoefsmit et al., 2012). In a quantitative study of FECA cases from 2005 to 2010, Maxwell and colleagues (2013, p. x) found that “injured workers who did not return to work quickly (without wage loss relative to their pre-injury earnings) were unlikely to return to work within three years of the reported date of the injury or illness.” The Washington State Department of Labor and Industries found that while most injured workers return from disability within 6 weeks, those who remain on disability at 3 months are already 50 percent more likely to remain on disability at 1 year (Franklin, 2013).
Different agencies have established different methods for ensuring early intervention, including 24-hour hotlines for reporting and the use of agency nurse case managers who initiate contact with an injured or ill employee weeks before a DOL nurse case manager is assigned to the case. Agency nurse case managers may be able to help identify limited-duty positions, which can reduce the COP period and associated workers’ compensation costs (Mitchell, 2013). In Chapter 4, a case study of the Federal Air Marshal Service expands on how agency nurse case managers can also serve to integrate workers’ compensation, medical, safety, and operational programs.
Health Promotion
A medically ready workforce must start with employees who are fit and healthy, both physically and mentally. The process of ensuring a fit and healthy operational workforce begins prior to employment with the setting of expectations and, when appropriate, through physical fitness testing, and continues until retirement through organizational health and wellness programs. For most civilian jobs, participation in health promotion programs is voluntary, but mandatory periodic fitness testing and health
__________________
13Additional information on return to work is available at http://www.dol.gov/odep/returnto-work/index.htm (accessed January 22, 2014).
screening may be justified and legally defensible for certain safety- and security-sensitive positions.14
Elements of Workplace Health Promotion Programs
Workplace health promotion programs often are tailored to the needs of the workforce, and consequently their elements may vary. However, a comprehensive worksite health promotion program is described in Healthy People 2010 (HHS, 2000) as including the following elements:
- health education that focuses on skill development and lifestyle behavior change in addition to information dissemination and awareness building, preferably tailored to employees’ interests and needs;
- supportive social and physical work environments, including established norms for healthy behavior and policies that promote health and reduce the risk of disease, such as worksite smoking policies, healthy nutrition alternatives in the cafeteria and vending services, and opportunities for obtaining regular physical activity;
- integration of the worksite program into the organization’s administrative structure;
- related programs, such as employee assistance programs; and
- screening programs, preferably linked to medical care service delivery to ensure follow-up and appropriate treatment as necessary and to encourage adherence.
Health screening programs, which may include a health risk assessment,15 identify an individual’s health risks based on physiological data (e.g., weight, blood pressure, cholesterol) and lifestyle factors (e.g., smoking, alcohol intake, exercise, diet). Educational materials, recommendations for lifestyle changes, and implementation plans can then be developed based on those risks, taking into consideration the person’s current life circumstances.
__________________
14Safety- and security-sensitive positions include “positions that involve law enforcement, national security, the protection of life and property, public health or safety, or other functions requiring a high degree of trust and confidence” (Executive Order 12564).
15A health risk assessment is a tool or process for “the assessment of personal health habits and risk factors (which may be supplemented by biomedical measurements of physiologic health); a quantitative estimation or qualitative assessment of future risk of death and other adverse health outcomes; and provision of feedback in the form of educational messages and counseling that describe ways in which changing one or more behavioral risk factors might alter the risk of disease or death” (Soler et al., 2010, p. s238).
TABLE 3-1 Individual- and Organization-Level Impacts of Workplace Health Promotion Programs
| Individual-Level Impacts | Organization-Level Impacts |
|
• Improve fitness, health, and resilience • Decrease disease risk factors (e.g., body mass index, blood pressure, cholesterol) • Prevent occupational injuries • Decrease recovery time from injury and illness • Increase job satisfaction |
• Improve mission readiness • Reduce absenteeism and increase productivity • Reduce health-related costs • Reduce turnover for medical reasons • Improve morale |
Although often neglected, mental health promotion is of critical importance. According to the Substance Abuse and Mental Health Services Administration, an estimated 19.6 percent of U.S. adults suffer from mental illness16 each year (SAMHSA, 2012). Mental health disorders affect the workplace, and the workplace can affect mental health; such disorders are increasingly becoming a cause of reduced productivity, morale, and engagement (Harnois and Gabriel, 2000; IOM, 2013). A 2009 survey of 34,622 employees from 6 American companies found depression (first) and anxiety (fifth) to be among the top five most costly health conditions to employers in terms of annual medical, drug, absenteeism,17 and presenteeism18 costs (Loeppke et al., 2009). The suffering caused by mental disorders can be exacerbated by the additional burden of stigma associated with such disorders, which may prevent affected individuals from seeking help (IOM, 2013). The workplace also can be a major source of stress on employees. Although stress is not considered a mental health disorder, it, too, can impact productivity, morale, and engagement. Employee stress or work-life management and resilience programs, including employee assistance programs, can help employees manage stress and find additional professional help as needed.19
__________________
16The Substance Abuse and Mental Health Services Administration (SAMHSA, 2012) defines mental illness as “currently or at any time in the past year having had a diagnosable mental, behavioral, or emotional disorder (excluding developmental and substance use disorders) of sufficient duration to meet diagnostic criteria specified within the Diagnostic and Statistical Manual of Mental Disorders.”
17Absenteeism is defined as habitual absence from work (IOM, 2005).
18Presenteeism is defined as “on-the-job productivity loss that is illness related; for example, problems such as allergies, asthma, chronic back pain, migraines, arthritis, and depression; also related to productivity loss resulting from caregiving, lack of job satisfaction, and organizational culture” (IOM, 2005).
19For additional information on such programs and their importance, see IOM, 2013.
Benefits of Workplace Health Promotion Programs
Health promotion programs can provide benefits at both the individual and organizational levels (see Table 3-1). At the individual level, physical fitness and a healthy lifestyle can reduce risk factors, such as high body mass index, blood pressure, and cholesterol, associated with chronic disease. These benefits may be especially important for individuals in occupations associated with higher-than-average rates of chronic illness, such as law enforcement. Healthier workers also may be less likely to be injured on the job, and when occupational injuries do occur, they may be less severe and take less time to resolve in healthy individuals (Musich, 2001). At the organizational level, programs that improve the health of the workforce can reduce occupational injury and illness rates and improve productivity by reducing use of sick leave, presenteeism, and turnover for medical reasons (Chapman, 2012). In addition to the reductions in associated costs (e.g., direct health care, workers’ compensation, and disability costs, as well as costs associated with recruitment and training of replacement staff), the end result is high-functioning personnel who are available for mission duties. An additional potential benefit of workplace health promotion programs—one that is less easily measured but equally important—is improved morale: when employees feel valued and taken care of by their employer, job satisfaction and engagement may increase, driving cohesion, loyalty, and esprit de corps (Berry et al., 2011; Lowe et al., 2003).
Financial constraints often are cited as a major barrier to the establishment of workplace health promotion and wellness programs, but such rationales are short-sighted; the return on investment in worker health can more than justify the costs. Return-on-investment estimates vary across studies and are difficult to derive because of the challenges integrating savings data from multiple cost sources (e.g., absenteeism, presenteeism, health care plan costs, and workers’ compensation and disability costs). Nonetheless, a recent meta-analysis by researchers at Harvard University showed that on average, employers saved $3.27 on health care costs for every $1 spent on health promotion programs (Baicker et al., 2010).
The benefits of health promotion programs may be even greater when such programs target employees in jobs that are physically demanding and inherently hazardous. For example, a study by Leffer and Grizzell (2010) showed that establishment of a physician-organized wellness regime at a county fire department was associated with a statistically significant 40 percent reduction in the injury rate relative to the baseline period during the first 9-month intervention period, and by the second intervention year,
this reduction reached 60 percent.20 Firefighters were encouraged to perform 30 minutes of cardiovascular exercise 4 or 5 days a week (using plans developed according to their life circumstances) and received individualized recommendations for addressing health risks identified during counseling or indicated by biometric data.
Workplace Health Promotion Programs in Federal Government Settings
Federal employees can choose from among more than 200 health plans under the Federal Employees Health Benefits (FEHB) Program. Under FEHB law,21 the Office of Personnel Management (OPM) has the authority to negotiate contracts with private health insurance carriers for the entire federal government. As part of this negotiation process, premiums and benefits are set annually, so federal employers cannot offer such incentives as reduced health plan rates to employees participating in health promotion programs. Although OPM has encouraged contracted carriers to offer health promotion and wellness programs, including health risk assessments (OPM, 2011), such programs may vary significantly among carriers and are neither targeted to specific agency employee populations nor integrated into operations at federal worksites—shortcomings that may diminish their effectiveness. Many agencies therefore are supplementing health plan wellness benefits with worksite health promotion programs. These programs may or may not be comprehensive and can be developed and implemented internally or outsourced. For example, some agencies have established interagency agreements with FOH for an integrated health, wellness, and work-life program called FedStrive. In other cases, agencies outsource specific elements of wellness programs, such as employee assistance program services.
Another important difference between federal health promotion programs and their counterparts in private industry relates to data access. Utilization data on health benefits commonly are used to identify top health risks and cost contributors in employee populations; this information can then be used to target interventions and to measure program impacts. Although OPM recently started collecting health care utilization data from carriers and has created a data warehouse as an initial step in the analysis of such data (OPM, 2010), this information currently is not made available
__________________
20The intervention, which was compliant with National Fire Protection Association (NFPA) Standard 1582 on a Comprehensive Occupational Medical Program for Fire Departments, entailed a stress test, collection of biometric data (e.g., body mass index, blood pressure, cholesterol), and one-on-one counseling with the consulting physician.
21Public Law 86-382.
to individual federal agencies.22 Thus, federal agencies cannot use metrics related to health care utilization to target interventions or evaluate the performance of prevention programs. However, return-on-investment models may still be developed from estimated savings associated with changes in population risk profiles (Goetzel, 2013).
PROVIDING MEDICAL SUPPORT FOR OPERATIONS
The second pillar of a comprehensive workforce health protection framework is the capability to provide medical support to the workforce during operations. Activities of the employees of an agency or private organization that are conducted in areas remote from conventional medical support raise the issue of how to provide those services in the event of a work-related illness or injury. Operational medicine programs make occupational safety and health and medical services available to workers operating outside conventional workspaces, and they are essential to mission readiness.
The concept of embedding medical support within operational units stems from practices long used by the military to render initial essential stabilizing medical care for battle injuries during the critical few minutes after an injury occurs so as to preserve life and limb. The military also has long recognized the value of having medical support available to prevent and treat disease and nonbattle injuries in order to maintain the operational status of deployed forces. Although battle injuries are the leading cause of deaths in theater, most hospital admissions in deployed operational settings are associated with disease and nonbattle injuries (DoD, 2004). Thus preventive medicine, urgent care, and emergency or tactical medical services are all essential functions of embedded medical support for force sustainment.
The laws and regulations that govern medical practice in civilian settings differ substantially from the authorities that can be granted in the military. Military combat medics such as 18 Deltas23 have wide latitude in rendering medical care, whereas civilian emergency medical technicians (EMTs) and paramedics must be licensed and work under a directing physician using approved protocols. Despite these differences, the strategy of
__________________
22In the future, agencies may be able to access separate databases containing their own health care utilization and health risk data (Goetzel, 2013).
2318 Delta is the DoD designation for a U.S. Army Special Forces Medical Specialist, a corpsman who can work independently in austere environments and is trained and authorized to perform advanced procedures and provide care. These personnel receive approximately 1 year of additional training; civilian emergency medical services (EMS) personnel typically do not receive this type of training.
BOX 3-1
Operational Medicine at the Federal
Bureau of Investigation (FBI)
The FBI’s operational medical program is housed within the Office of Medical Services’ Health Care Programs Unit. Originally based on the military special forces model, the program was created to provide support to FBI tactical operations. The FBI currently employs approximately 400 operational medicine personnel, with a ratio of 4:1 basic life support to advanced life support capabilities. FBI operational medicine covers three broad classifications of operations:
- Tactical medical operations: The majority of operational medicine activity supports FBI SWAT teams in all 56 field offices and the Hostage Rescue Team based in Quantico, Virginia.
- Specialized team support: A number of teams require embedded medical treatment capabilities, either by statute or by bureau policy (e.g., teams that collect evidence in hazardous environments; teams that deal with chemical, biological, radiological, and nuclear agents; aviation assets that transport subjects by aircraft; technical dive team units).
- Baseline capacities: Over the last 3 years, the FBI has instituted a baseline capacity that mirrors the Department of Defense tactical combat casualty care program through the creation of the Care Under Fire course. All new agents receive this training, and an effort currently is under way to provide this training for the remaining 11,000 FBI Special Agents.
The FBI’s operational medical program operates similarly to a low-call-volume emergency medical services department, dependent on a high level of oversight, simulation, and skills currency training. While the Office of Medical Services provides general program oversight, quality assurance for the program is provided through a variety of means. Credentialing of all operational medical staff is documented and monitored through the use of a centralized electronic credentialing system. All medical encounters are recorded on paper, scanned, and reviewed; in the future, an electronic patient care record may be used for this purpose. Reports that involve an employee become part of the employee’s health record; there are separate repositories for nonemployees, depending on whether they are bystanders or subjects of an investigation (Fabbri, 2013).
embedding medical support within operational units has been adopted in several civilian settings, most notably law enforcement.
Characterizations of operational medicine often center on one of its functions—tactical medicine, defined as “the provision of field medical care during high-risk, extended duration and mission-driven law enforcement operations, often rendered under functionally austere conditions” (Tang,
2013). Such care is similar to that delivered by conventional emergency medical services (EMS) personnel, “modified for the realities of the tactical environment” (Heck and Pierluisi, 2001, p. 403). How this support is provided varies; although some organizations employ personnel whose sole job is to provide medical support during an operation, others utilize law enforcement officers who are able to provide medical support as a collateral duty. Within the federal government, the FBI has developed an extensive program for providing operational medical support to its law enforcement workforce, as outlined in Box 3-1.
Operational medicine is not restricted to the practice of embedding medical practitioners in deployable tactical law enforcement teams, and the elements of an operational medicine program can vary substantially depending on the mission requirements. Like tactical law enforcement teams, rescue teams may have embedded staff to provide medical support to team members and members of the public in emergency situations (see, for example, the description of the National Park Service’s operational medicine program in Box 3-2). Physicians, nurses, and physician assistants stationed in fixed facilities in remote duty outposts may also provide operational medical support. GE Energy, for example, has employees stationed in some of the most remote parts of the world and is responsible for their health and safety (see Appendix E for additional details). In such cases, the distinction between operational medicine and travel medicine as part of an occupational medicine program can become blurred and may be merely a matter of semantics.
Although embedded medical personnel generally are employees of the organization in which they are embedded, fixed facilities and the associated medical staff may be owned by the organization or outsourced (to medical services contractors or through agreements with local health system providers). To achieve their mission, some organizations have created advanced-scope positions requiring additional specialized training to fulfill specific needs; examples include the National Park Service’s Parkmedic and Remote Emergency Medical Responder and the Secret Service’s Emergency Services Specialist (Ross, 2013; Stair, 2013). Despite the variability in the composition of operational medicine programs, the key functions are generally the same—threat assessment, preventive medicine, ambulatory medical support, and emergency medical support.
Medical Threat Assessment
As discussed in relation to occupational safety and health, risk management is a continuous, multistep process designed to reduce risks to health, mission, and property. Management of risk also is important in the context of operational medicine and is achieved in part through medical threat
BOX 3-2
Operational Medicine in the National Park Service
The National Park Service (NPS) manages 9.2 percent of U.S. lands, spanning a wide variety of ecosystems, biomes, and climates. Each year, its 28,000 employees and 120,000 volunteers work not only to conserve and protect these lands but also to protect the 280-300 million visitors to U.S. national parks. To the latter end, the NPS Organic Act (16 USC 1-4) grants NPS the authorities to provide emergency services to visitors and employees. Approximately 75 percent of NPS law enforcement personnel are rangers, whose official job duties include not only law enforcement but also search and rescue and emergency medical services (EMS).
To exercise these authorities, NPS has created an EMS system consisting of 137 EMS programs and 2,286 EMS providers, overseen by four national medical directors that provide overall guidance. Within this system, NPS has created six levels of practice—Emergency Medical Responder, Remote Emergency Medical Responder, Emergency Medical Technician, Advanced Emergency Medical Technician, Parkmedic, and Paramedic—with differing scopes of practice. NPS provides specialized training programs for advanced-scope positions—Remote Emergency Medical Responder and Parkmedic—carried out in high-altitude locations, similar to conditions these personnel will face, and all skills testing is conducted out in the elements. Additionally, NPS operates three medical clinics, providing both emergency care for visitors and employees and routine care for visitors; owns 117 ambulances, 290 intercept vehicles, and more than 4,000 automated external defibrillators; and manages more than 290 memorandums of understanding and memorandums of agreement with local hospitals. Each year, NPS responds to approximately 90,000 calls, about 15,000 of which become patient encounters, providing basic and advanced life support and cardiac, trauma, and medical support, and conducts more than 10,000 patient transports via ground, air, and vessel.
In 2008, NPS implemented an electronic patient care record to create a more evidence-based practice. This system has enabled quality assurance and improvement, refinement of existing and creation of new protocols and procedures, epidemiological surveillance, risk management, and increased notification and communication abilities. NPS also engages in operational leadership—its term for risk management—whereby a green-amber-red model is used to help determine risks associated with operations.
While the program is not congressionally funded, Department of the Interior leadership has found it to be an important, indeed necessary component of the agency’s operations. Each year, money is shifted from other operations to ensure consistent funding. In addition, although technically the government is not allowed to bill, the three NPS clinics function as a Blue Cross Blue Shield preferred provider organization, enabling them to seek cost recovery.
SOURCE: Ross, 2013.
BOX 3-3
Medical Care of In-Custody Individuals
In addition to ensuring the health of those conducting missions and bystanders caught in the mission’s perimeter, medical support during operations extends to ensuring the health and welfare of those taken into custody. This is an ethical imperative, as assuming custody for an individual transfers responsibility for safety from that individual to the agency assuming custody. U.S. legal requirements recognize and safeguard this imperative. Federal courts have held that pretrial medical care, whether in prison or other custody, is required by the Fourteenth Amendment (Wagner v. Bay City, 227 F.3d 316 [5th Circuit 2000]). Further, Mulry and colleagues (2008, pp. 123-124) contend that “the withholding of adequate medical care may be viewed as excessive force, an unconstitutional act in violation of the Fourth Amendment right to be free of unconstitutional seizure.”
NOTE: The definition of operational medicine adopted by the committee encompasses health and medical support provided to persons in DHS care and custody during routine, planned, and contingency operations. However, assessment of health care provided to detainees within Immigration and Customs Enforcement detainment facilities, as well as the adequacy of the facilities themselves, was not considered to be within the scope of this study.
assessment, which involves the creation of a comprehensive mission preplan. The California Commission on Peace Officer Standards and Training (CA POST, 2010, p. 12) recommends that medical threat assessment “be conducted based on available intelligence and information on the nature of the response … [and] incorporated into the tactical plan for the specific mission,” serving as a significant resource for the operations commander. At the committee’s second meeting, Dr. Nelson Tang, Medical Director for ICE and the Secret Service,24 suggested that threat assessment should include examination of a variety of issues, including expected contingencies, expected responses, source of resources, and the destination for casualties resulting from the event (Tang, 2013). Answering such questions prior to an operation will assist in the development of both preventive and responsive medical support plans, protecting the health of the workforce and those affected by operations, including individuals in custody (see Box 3-3).
__________________
24Dr. Tang is Director of the Division of Special Operations and Chief Medical Officer at the Johns Hopkins Center for Law Enforcement Medicine. Several federal agencies, including ICE and the Secret Service, have contracts with this center to provide medical direction for operational medicine programs.
Preventive Medicine and Ambulatory Medical Care
The goal of operational medicine is to support the operational workforce in successful completion of the mission. Operational units often are small, so that illness or injury of members can adversely impact the unit’s mission; thus, the preventive medicine and ambulatory medical care functions are critical to mission success. Preventive medicine functions begin before the mission occurs (e.g., administering predeployment vaccinations, promoting understanding of nutrition issues and sleep/rest cycles), but also continue throughout operations (e.g., food and water hygiene, field sanitation, control of disease vectors). Preventive medicine requirements can be influenced by preoperation threat assessments.
Operational medicine programs often include specialized training in preventive and nonemergency medical care functions because EMS providers traditionally are not trained in these areas. Routine medical problems such as gastrointestinal illnesses, bronchitis, and sports-type injuries (e.g., sprains and strains) usually would be handled through outpatient clinics or hospital visits in traditional work settings, but during operations or when members of the workforce are operating in austere environments, it may be that such resources are absent or cannot be utilized for security reasons.
Emergency Medical Support
Emergency medical support during operations commonly, though not always, is provided by EMTs (basic life support) and paramedics (advanced life support). Notable differences between EMS in conventional settings and during operations include challenging environmental conditions, the length of time until patients can be transferred to definitive care, and in some cases, the requirement to work while “under fire.” Both additional training and expanded protocols are required to provide medical support beyond the conventional role of EMS personnel. Some agencies, including the National Park Service, the FBI, the Secret Service, and Customs and Border Protection (CBP), have developed advanced-capability paramedic positions to ensure the availability of properly trained medical support personnel for the unique challenges and demands associated with their operational missions. This additional training typically includes both simple outpatient treatment skills and more advanced measures to support seriously ill or injured persons when evacuation to a conventional medical facility is delayed. In some programs, all operational team members are trained in “self-care” to provide initial life- and limb-saving treatment prior to evacuation to a definitive hospital facility.
Measurement is critical to understanding organizational needs. However, data collection alone is not enough; the data must be used to drive individual and organizational performance. If impact is not measured, success cannot be distinguished from failure.
Spanning both pillars of the framework outlined in this chapter, measurement and evaluation is essential to developing, implementing, and continuously improving programs designed to address the other eight key functions of an integrated workforce health protection framework (see Figure 3-1). According to the World Health Organization (WHO), “a healthy workplace is one in which workers and managers collaborate to use a continual improvement process to protect and promote the health, safety and well-being of workers and the sustainability of the workplace” (Burton, 2010, p. 61). Measurement and evaluation is essential to this process. A system for measurement and evaluation supports multiple key organizational functions, including
- decision making,
- accountability,
- quality improvement, and
- surveillance.
These functions have been termed the “four faces of measurement” (IOM, 2005, p. 151). Processes for measurement and evaluation should be integral to any intervention program, health-related or otherwise. The objective to be met by the measurement will drive the approach to data collection, aggregation, analysis, and reporting.
Needs Assessments
First and foremost, creation and implementation of any new policy or program, including those related to workforce health protection, should be based on a comprehensive understanding of the issues involved; such understanding should be derived from a detailed needs assessment of the current situation. Developing a comprehensive picture of workforce health status and needs will require integration of information from diverse data sets that may include
- human resources data (e.g., absenteeism records or number of resignations);
- occupational health and safety data (e.g., accidents or risk assessments);
- financial data (e.g., the cost of replacing employees who are on long-term disability leave); and
- health data (e.g., common health problems among the workforce) (WHO, 2005).
In addition to enabling the creation of policy and programs based on organizational needs, data derived from such assessments will establish baselines against which program outcomes can be compared to evaluate success and drive continuous improvement.
Approaches to Measurement
The recent IOM report on DHS workforce resilience25 includes the recommendation that DHS “design and implement an ongoing measurement and evaluation process … [which] will support planning, assessment, execution, evaluation, and continuous quality improvement” (IOM, 2013, p. 153). A chapter devoted to measurement and evaluation focuses on the Donabedian (1966) model as an organizing framework for DHS. This model encompasses measurements of structure, process, and outcome and has long served as a standard model for evaluating and assessing health services and quality of care. Structural measures address basic program architecture and critical components, including leadership engagement, policies and procedures, and environmental support; process measures help assess how well the program is being implemented (e.g., utilization and satisfaction); and outcome measures examine the extent to which objectives and goals are achieved within a given period. The present committee identified three primary types of outcome measures that should be monitored in a metric-driven health protection system: health, financial, and productivity. Examples of potential outcomes of interest in each of these categories are provided in Box 3-4.
Within the field of occupational safety and health, a common approach to measurement has focused on lagging and leading indicators. Lagging indicators are retrospective measurements of system performance linked to outcomes; these are the traditional measures of safety performance, such as OSHA statistics and costs (Manuele, 2013). These indicators, however, have a key limitation: “While lagging indicators give information of direct concern to management, the workforce, and the public, they can only be used for improvement after the fact” (NRC, 2009, p. 8). Recent years have seen a shift toward what have been termed leading indicators—in the safety
__________________
25For additional information, see http://www.iom.edu/Reports/2013/A-Ready-and-ResilientWorkforce-for-the-Department-of-Homeland-Security-Protecting-Americas-Front-Line.aspx (accessed January 22, 2014).
BOX 3-4
Outcome Measures for an Integrated Workforce
Health Protection Infrastructure
Health Outcomes
- Injury and illness rates
- Health risk reduction
- Health care utilization
Financial Outcomes
- Workers’ compensation costs
- Health care costs
- Disability costs
Productivity Outcomes
- Absenteeism (sick leave utilization)
- Presenteeism
- Mission opportunities lost
- Employee turnover
context, prospective measures linked to actions taken to prevent accidents (Manuele, 2013).
The importance of using leading indicators to evaluate individual performance cannot be overstated. Attempts to evaluate individual performance based on lagging indicators may create perverse incentives, encouraging individuals to make outcomes look good and not necessarily to improve underlying performance (for example, an objective to decrease the number of workers’ compensation claims may lead to claim suppression). The use of leading indicators allows for evaluation of what individuals are doing to address an issue, while lagging indicators enable program evaluation and inform continuous improvement processes.
Workforce Perceptions of Safety
Measures of organizational climate examine workforce perceptions of organizational practices, such that those most familiar with the work environment are involved in its evaluation (Rousseau, 2011). Surveys of organizational climate focus on a wide variety of issues affecting the workforce and workplace. They take the pulse of the organization, providing insight into potential problem areas and creating opportunities for soliciting employee input and targeting interventions. Each year, OPM administers
the Federal Employee Viewpoint Survey to measure “employees’ perceptions of whether, and to what extent, conditions characterizing successful organizations are present in their agencies” (OPM, 2012, p. 2). Responses to the survey are grouped into several indices—including leadership and knowledge management, results-oriented performance culture, talent management, job satisfaction, employee engagement, and global satisfaction—providing useful information to agency leaders on challenges within their organizations that must be addressed to improve performance (OPM, 2012). However, the survey contains few items related to workforce perceptions of health and safety. Likewise, DHS reported to the committee that it currently conducts no medical and health climate surveys (Polk, 2013). Nonetheless, measures do exist with which to gauge workforce perceptions of safety and health in the workplace. Safety climate surveys such as the Zohar (1980) scale, which has been widely used and validated over the past 30 years, provide an important leading indicator and encourage the development of preventive interventions.
INTEGRATION OF ESSENTIAL WORKFORCE HEALTH PROTECTION FUNCTIONS
Most large employers have programs that address many of the key functions discussed in this chapter. Often, however, these programs operate in silos, divorced from each other both organizationally and strategically. Consequently, in the face of the numerous challenges associated with employee health (e.g., rising health care costs associated with chronic diseases, workers’ compensation costs, injury rates), employers may not know where to direct resources and interventions, and important information may not flow from one silo to another. With such fragmented systems, the result often is the introduction of multiple independent solutions that do not benefit from the synergy generated by a unified strategy (Goetzel, 2005). The solution is “strategic and systematic integration of distinct environmental, health, and safety policies and programs into a continuum of activities that enhances the overall health and well-being of the workforce, and prevents work-related injuries and illnesses” (Hymel et al., 2011, p. 695).
Characteristics of Integrated Health Systems
In a recent study on integrating employee health activities at DoD, Cecchine and colleagues (2009) define an integrated employee health system as “an infrastructure that would support all employee health activities except health care delivery, provide a way to link information about all aspects of the health of employees, and make this information available to leadership across all departments within DoD for the purposes of decision-making,
accountability, improvement, surveillance, and other questions related to health.” Through an examination of integrated workforce health systems (described in the sections below), the committee identified four beneficial characteristics of such systems:
- Harmonization: Through the creation of common standards, processes, and metrics, integration helps ensure consistency across large, complex organizations.
- Interoperability: Integration encourages interoperability, enabling the individual components of the system to work together and take advantage of components of other systems, including people, equipment, technology, and information.
- Efficiency: As with most workplace programs, health services face resource constraints. Integrated systems can lead to greater efficiency by creating economies of scale and reducing duplication of effort.
- Synergy: When programs work in concert, their overall effectiveness often surpasses their individual effects.
Models for Integrating Workforce Health Protection Functions
Integration of relevant systems is one of the “essential elements of effective workplace programs and policies for improving worker health and well-being” identified by the National Institute for Occupational Safety and Health (NIOSH, 2008). According to the NIOSH framework, “programs should reflect a comprehensive view of health,” and the integration of relevant systems is one of the keys to creating this view (NIOSH, 2008, p. 2). As a first step toward integration, NIOSH suggests creating an inventory and evaluating existing programs and policies to determine their worth and potential connections. NIOSH (2008, p. 2) recommends “integrat[ing] separately managed programs into a comprehensive health-focused system and coordinat[ing] them with an overall health and safety management system.” In recent years, several organizations—including the National Business Group on Health, NIOSH, and the Harvard Center for Work, Health, and Well-being—have released documented approaches to integrating employee health programs.
National Business Group on Health’s Employer Toolkit and Guide
In 2005, the IOM released a report in response to a National Aeronautics and Space Administration (NASA) request for recommendations on options for future worksite preventive health programs and ways to create healthier workplace environments that are conducive to more active
BOX 3-5
Recommendations for Integrating Employee Health
To disseminate the recommendations of an Institute of Medicine (IOM) report on integrating employee health programs at NASA (IOM, 2005) to a wider audience, the National Business Group on Health published an employer toolkit for improving employee health. The following keys to success were generalized from the IOM committee’s recommendations:
- Make health a core value, linked to your overall mission.
- Realize the goal by offering tangible, well-supported, integrated programs.
- Encourage consistency across all programs, in all locations, with consistent data and evaluation.
- Develop a data-based approach to policy, planning, and programming; create a standardized “health and performance” full-cost accounting; incorporate essential elements of integrated health programs in contracting requirements.
- Recruit supervisors and managers to help make the links for employees between health, productivity, and the success of the organization.
- Obtain, understand, and apply health care cost and utilization data to optimize programs.
- Offer a basic health assessment tool, like a health risk appraisal (HRA), to all employees.
- Coordinate and integrate all individual and organization-wide health policies and programs.
- Promote, then provide or make available, health screenings to minimize risks.
- Evaluate every program to ensure it’s effective and has enough resources.
- Employ a framework for measurement offering direct access to the data you collect.
- Collaborate across departments, divisions, regions, and job types.
- Assemble a data management team from key areas for ongoing measurement and evaluation.
- Establish system-wide data architecture and technology.
- Learn from your mistakes and successes. View all of your health promotion efforts as opportunities to gather research on what does and doesn’t work.
SOURCE: NBGH, 2006.
lifestyles. The IOM Committee to Assess Worksite Preventive Health Program Needs for NASA Employees recommended that NASA adopt an integrated management systems approach to employee health to support the agency’s missions and goals. The National Business Group on Health, seeking to share the key findings and recommendations from that report
so that other employers could benefit from the study results, published its Improving Health: An Employer Toolkit, in 2006. The toolkit recommendations, adapted from those made by the IOM committee to NASA, are presented in Box 3-5. More recently, the National Business Group on Health published an employer guide on Integrating Wellness and Occupational Health and Safety in the Workplace, which provides a rationale and strategies for an integrated approach (NBGH, 2013).
NIOSH’s Total Worker Health™
Stemming from the earlier Steps to a Healthier U.S. Workforce initiative, which focused on improving worker health by integrating health protection and health promotion functions, NIOSH’s Total Worker Health (TWH) program was launched in 2011 based on three seminal papers that grew out of the previous initiative. In 2012, these seminal papers were updated and published in a research compendium aimed at reviewing the current evidence base and establishing a scientific rationale for using an integrated approach to the protection and promotion of worker health (NIOSH, 2012). NIOSH defines TWH as a “strategy integrating occupational safety and health protection with health promotion to prevent worker injury and illness and to advance health and well-being” (CDC, 2013). Whereas workplace health promotion and safety programs have traditionally been compartmentalized, the goal of TWH is to promote integration and “support the development and adoption of ground-breaking research and best practices of integrative approaches that address health risk from both the work environment (physical and organizational) and individual behavior” (CDC, 2013). As part of this initiative, the Centers for Disease Control and Prevention (CDC) created an extensive website providing a wealth of information on integration, including peer-reviewed literature and other resources, guidelines for implementation, promising practices, scorecards and measurement tools, and links to Centers of Excellence funded by NIOSH.26
Harvard Center for Work, Health, and Well-being’s SafeWell Practice Guidelines
In collaboration with Dartmouth-Hitchcock Health Care, the Harvard Center for Work, Health, and Well-being created the SafeWell Practice Guidelines “to provide a model and resources for comprehensive approaches to worker health that integrate and coordinate efforts to promote
__________________
26Additional information on TWH and online resources are available at http://www.cdc.gov/niosh/TWH (accessed January 22, 2014).
healthy behaviors, ensure a safe and healthy work environment, and provide resources for balancing work and life” (McLellan et al., 2012, p. 1). Identifying a link between employee health and well-being and organizational success, the guidelines promote a vision of an integrated workforce health system, positing that “effective workplace health programs implement programs, policies, practices, and benefits designed to promote health among individual workers in healthy, safe, and productive workplaces” (McLellan et al., 2012, p. 5). In creating an integrated approach, McLellan and colleagues (2012) recommend adherence to three important principles:
- a systems-level approach that coordinates programs, policies, and practices;
- coordination of occupational safety and health, worksite health promotion, and human resources; and
- programs, policies, and practices that address the work environment/organization and worker health and well-being.
Essential to this endeavor is a foundation of organizational leadership and commitment and a strategy for evaluation and continuous improvement.
Real-World Models from Public- and Private-Sector Organizations
Throughout the course of this study, the committee examined a number of successful organizational workforce health protection programs in both the public and private sectors. The committee found that the implementation of workforce health programs varied, encompassing completely decentralized, completely centralized, and hybrid approaches. See Appendix E for brief descriptions of the organizations examined, including the Smithsonian Institution, NASA, DoD, the Department of the Interior, the Department of State, Johns Hopkins University and Medical Institutions, Johnson & Johnson (J&J), Procter & Gamble (P&G), and Superior Energy Services. Because of similarities in organizational and operational challenges faced by DHS and the Department of the Interior, the committee examined in particular detail the means by which integration of workforce health protection functions across Department of the Interior bureaus is achieved; this case study is presented in Box 3-6.
Requirements for Successful Integrated Employee Health Programs
The committee was asked to examine occupational health and operational medicine infrastructures established within and outside of government; to identify key functions of an integrated infrastructure; and ultimately to provide recommendations on how infrastructures within
BOX 3-6
Integrating Workforce Health Across a Diverse Federal
Organization: A Case Study of the Department of the Interior
Though significantly smaller than DHS, the Department of the Interior (DOI) is constructed in a similar fashion, with eight bureaus carrying out widely diverse missions, housed under a centralized headquarters entity. At the headquarters level, the Office of Occupational Safety and Health is responsible for “ensur[ing] the health, safety, and well-being of [DOI] employees and visitors” (DOI, 2008). To achieve this mission, the Office of Occupational Safety and Health developed the Safety and Health Strategic Plan, outlining overarching goals and strategies intended to provide broad direction to the bureaus and used to hold managers and executives accountable for ensuring the health and safety of the workforce. The six goals are as follows:
- Enhance the Role of Leadership and Management in Promoting a Culture of Safety.
- Enhance Employee Inclusion, Participation, and Engagement in Achieving Safety and Health Commitments.
- Prevent Exposure to Hazards and Mitigate Risk through Recognition and Prevention Programs and Processes.
- Enhance Internal Evaluation and Analysis Processes to Validate the Effectiveness of the Safety and Health Program.
- Improve Occupational Safety and Health Training and Awareness throughout the Department.
- Implement and Continuously Improve the Occupational Safety and Health Program.
DOI has taken multiple steps to ensure integration, both among bureaus and between the bureaus and headquarters. To ensure vertical integration between headquarters and the bureaus, Designated Agency Safety and Health Officials (DASHOs) within each bureau, together with the departmental DASHO, make up the department’s DASHO Council, which meets “in an ad hoc fashion to discuss appropriate activities, actions and initiatives to further the Departmental Safety and Health Program” (DOI, 1996). Additionally, DOI formed the Safety and Occupational Health Council, bringing together bureau safety and health managers to coordinate bureau activities and “serve as an advisory body on program matters to the Departmental DASHO and the DASHO Council” (DOI, 2012, p. 2).
DOI also has taken steps to ensure horizontal alignment of all workforce health protection functions at the headquarters level, including placement of the Occupational Health and Medical Programs Division under the Office of Occupational
Safety and Health, organizationally aligning these functions within a single reporting structure. The department’s medical functions are centralized within this headquarters division, which focuses on overarching policy concerns and program development, advocating for a team approach to decision making and implementation within the bureaus (Garbe, 2013). Although primary responsibilities for workforce health functions have been aligned within the Office of Occupational Safety and Health, the Office of Human Resources continues to play a supporting role by maintaining employee occupational health records and ensuring that appropriate workers’ compensation forms are completed and processed (DOI, 2009).
Implementation of workforce health programs is left to the discretion of each bureau, within broad guidelines established by the headquarters-level program. All of the department’s occupational medicine, health, and safety procedures are outlined in the Occupational Medicine Program Handbook, including information on establishing or changing physical qualification standards, conducting preplacement and periodic examinations for the purpose of medical clearance, carrying out medical surveillance processes, and implementing specific standards for various classes of positions (DOI, 2009). Also included is detailed guidance on medical employability determinations and medical examination procedures, including preplacement medical evaluations and ongoing medical surveillance.
A primary example of how DOI has approached integration across diverse components, and especially relevant to DHS, is the creation and enforcement of overarching medical standards and clearance processes. Similar to DHS, DOI employs a wide variety of operational staff, including approximately 7,000 law enforcement officers and 15,000 wildland firefighters. Other operational staff include onshore and offshore inspectors (e.g., surface mining, offshore oil and gas operations), large vessel crews, divers, pilots/aviators, and drill rig operators, among others. For each of these positions, DOI has published Office of Personnel Management (OPM)-approved medical standards.* These standards were developed through a team approach, which included subject-matter experts in safety, human resources, and medicine at both the department and bureau levels, as well as individuals working in the positions for which standards were being developed and union representation as appropriate (Garbe, 2013). The process involved not only discussion of the areas of interest, including accident and illness statistics, but also real-time observation of employment conditions and job duty performance in the operational setting.
Implementation of position-specific standards and of programs designed to ensure that such standards are being met is left to the bureaus, allowing for wide
component agencies can be better integrated into a coordinated, DHS-wide system. In this chapter, the committee has identified nine key functions essential to ensuring workforce health. Integration of these functions, as demonstrated by many of the organizations examined, has helped achieve success in ensuring workforce health.
As noted by the WHO (2008, p. 1), “integration is best seen as a continuum rather than as two extremes of integrated/not integrated.” With this point in mind, the committee viewed integration of health systems from the perspective of alignment—“the degree to which an organization’s design, strategy, and culture are cooperating to achieve the same desired goals”
discretion and creativity based on the bureau’s needs and capacities within the boundaries of good medical practice (Garbe, 2013). DOI headquarters steps in only when implementation in one bureau may jeopardize the legal defensibility of the standard in another bureau. Dr. Bob Garbe (2013), Chief of the Division of Occupational Health and Medical Programs, provided the committee with two examples of alternative approaches to implementation. The National Park Service, which employs approximately 5,000 law enforcement officers, operates a centralized medical clearance program with a single national contract medical provider. Every NPS law enforcement officer undergoes periodic medical clearance examinations through contracted examiners, the results of which are reviewed by a small group of physicians also employed by the contractor. Results are sent to the agency as cleared or not cleared. Alternatively, the Fish and Wildlife Service, many of whose operational employees are dispersed in rurally remote areas, uses a voucher system. Employees are provided with a clearance form that they bring to a local physician of their choice who conducts the examination and provides the clearance. The former approach, which has been in effect for more than 10 years, is viewed as highly successful. The latter approach, though taken out of necessity, is seen as potentially problematic, as it increases the risk for errors of omission or commission and the potential for data of lesser quality.
Because DOI, like DHS, is a loose amalgam of diverse bureaus, largely independently funded and with their own leadership, the headquarters-level program has found it difficult to ensure consistent implementation of comprehensive programs across bureaus. However, the headquarters office has played a strong coordinating and integrating role, bringing together individuals from all levels in the development of department-wide standards, ensuring that bureau-specific standards meet departmental standards, advocating for strengthening of programs based on best practices, and assisting bureaus in the design of their programs.
________________
*All of DOI’s standards can be found in Tab 12 of the Occupational Medicine Program Handbook, available at http://elips.doi.gov/ELIPS/DocView.aspx?id=3478 (accessed January 22, 2014).
(Semler, 1997, p. 23). When applied to workforce health functions, this perspective can help organizations achieve their goals for a healthy, safe, and ultimately high-functioning and productive workforce. In its examination of the organizations discussed in this chapter and in Appendix E, the committee identified four elements that are essential for successful integration of workforce health programs: leadership commitment to workforce health, organizational alignment and coordination, functional alignment, and information management. As further discussed in Chapter 4, these four elements served as the organizing framework for the recommendations presented in Chapters 5-8.
Leadership Commitment to Workforce Health
Creating a common core culture focused on health and safety (discussed in the next section) has been key to the success of many of the programs examined for this study. The creation of such a culture begins with a vision of a healthy, safe, and resilient workforce, put forth by organizational leadership committed to achieving this vision and ultimately reaching down to every employee in the organization (Cecchine et al., 2009). Leadership commitment is crucial to the creation, expansion, and sustainability of workforce health programs; without vocal and active leadership, such programs may not be viewed as a priority by management or the workforce as a whole. For example, the successful workforce health program at the Smithsonian Institution began in 2007, when then Secretary Lawrence Small set a zero-injury goal for the organization, articulating the importance of safety to its leadership. In 2009, Secretary G. Wayne Clough institutionalized leadership’s commitment to workforce health by specifically including related goals in the Smithsonian’s strategic plan for fiscal years 2010-2015.27 Each year, Dr. Clough serves as the opening speaker at the kickoff event for the Smithsonian’s National Safety Month (Duval, 2013), thereby demonstrating visible commitment to the health of his employees.
In addition to providing support, leadership involvement in the creation, implementation, and improvement of programs and policies related to employee health and safety can be invaluable to building a lasting program with significant impact. This point is demonstrated by P&G, which recognized the importance of creating a health and wellness program (Vibrant Living) that was integrated with the rest of the organization (Christensen, 2013). Key leaders from human resources, manufacturing, and research and development, as well as regional officers, were involved during every step of the program design, fostering not only leadership buy-in but also ownership of the program and its goals. Leadership commitment and involvement do not begin and end with top-tier leadership. For example, Vibrant Living, whose vision for the workforce is “the healthiest, most engaged people in the world,” continues to engage leadership at all levels through its steering team, whose members include both functional (medical, human resources, manufacturing, research and development) and regional business leaders.
Finally, creating avenues for communication is critical. As discussed above, communication with leaders at all levels helped foster a sense of ownership in P&G’s health and wellness program from the start. Organizations
__________________
27The strategic plan includes an objective to “attract, maintain, and optimize a productive, motivated, and creative workforce,” with one of the strategies for meeting this goal being to “encourage and maintain an organizational culture that embraces safety, health, and wellness” (Smithsonian Institution, 2010, p. 20).
can spend much time and effort on creating and implementing a program, but even the best programs are worth little if employees do not participate. P&G is working to brand its health programs globally with inviting names, such as Vibrant Living, that encourage their utilization (Christensen, 2013). Similarly, Superior Energy communicates its commitment to employee health through both words and actions, constantly promoting its wellness program, offering time allowances for health-related activities, and creating an incentive program. As a result, the company has seen a strong and growing interest in its wellness program in recent years (Minson, 2013).
Organizational Alignment and Coordination
All of the organizations the committee examined took steps to ensure coordination of essential workforce health protection functions, although the approaches taken to these ends varied. The Smithsonian Institution, the Department of the Interior, and Johns Hopkins all combined workforce health protection functions into a single reporting structure, while other organizations, such as NASA, P&G, and J&J, housed functions in separate reporting structures and instituted measures to ensure alignment through systematic communication and coordination.
Successfully integrated programs provide avenues for ensuring appropriate communication and coordination. Communication is especially critical in organizations where the workforce health functions are not organizationally aligned into a single reporting structure. For example, while the P&G Global Medical program is located within human resources, the industrial hygiene, safety, and environment program is housed separately under manufacturing; however, systems are in place to ensure timely information sharing between the two and coordination as necessary (Christensen, 2013). J&J is similarly organized and created the Environmental Health and Safety Leadership Council to bring Global Health and occupational safety and health leadership together to address high-level issues related to the creation of organizational policies and standards. Similar teams operate at the business unit level, bringing together occupational health physicians and/or nurses; site safety managers; and wellness, employee assistance, and industrial hygiene professionals (Isaac, 2013).
Functional Alignment
Standards and global policies are necessary in decentralized organizations to ensure that operational units are meeting established requirements for workforce health throughout the organization (Isaac, 2013). It is also critical for organizations, especially those that are decentralized, to monitor their components’ adherence to such standards. J&J currently has
27 global standards, 2 of which are related directly to employee health and 3 to safety. It also has created globally harmonized procedures, such as tobacco-free sites, wellness programs, occupational health programs, and an employee assistance program, to ensure that its operating companies can meet these standards. Auditing processes, such as the Management Action and Assessment Review System, help ensure that standards are being met and identify areas for improvement within business units. Sites are required to conduct an annual self-assessment against J&J standards, with a joint assessment being performed by Global Health Services every 3 years.
Through its global framework, P&G has instituted an employee health and wellness policy designed to ensure that all of its employees will have access to occupational health services locally, wherever they are located, either directly through P&G clinics or through a contracted provider (Christensen, 2013). Consistent standards, procedures, and training exist across all P&G subsidiaries and worksites. From evidence-based standards of practice built on guidance from best-in-class global health organizations, P&G has created 20 health-related standards spanning six domains. P&G uses an audit tool to ensure that its sites are meeting its standards and a global medical scorecard to track outcomes, allowing for measures of overall organizational health and return on investment.
It is important to note that the establishment of overarching standards does not necessarily imply a heavy-handed approach from the top with respect to how component organizations and worksites implement programs to meet the standards. For example, the Department of the Interior provided standards and guidance to its eight component bureaus but, in so doing, recognized the wide variety of their responsibilities and missions. Therefore, program implementation is left to each bureau, with broad latitude in how the standards are met.
Information Management
Consistent with findings from previous studies (Cecchine et al., 2009; IOM, 2005), information management has been critical to the success of the integrated employee health programs examined by the committee. The development of any new program should be based on organizational needs, as determined by metric-based assessments, so that programs and interventions can be appropriately designed and targeted. This process may entail collecting health risk data through voluntary health risk assessments, as was done prior to the development of intervention strategies at the Smithsonian Institution (Duval, 2013). For an operational workforce, data on patient encounters in the field may be needed to guide agency medical programs—an approach taken by the National Park Service to address injury prevention and risk management activities (Ross, 2013).
Once a program is in place, measurement and evaluation, discussed earlier, helps ensure program effectiveness and drive continuous improvement. Continuous improvement processes across large, decentralized organizations require standardized metrics and data collection tools. J&J has developed several metrics and tools for evaluating program effectiveness. The Global Health Assessment Tool, for example, enables tracking whether business units are meeting program goals and objectives (Isaac, 2013). In 2012, J&J instituted the Occupational Health Index, which examines compliance, quality, satisfaction, and efficiencies on a quarterly and annual basis (Isaac, 2013). J&J currently is developing the Health and Productivity Index, which combines health, productivity, well-being, and “culture of health” and program sustainability measures. Upon implementation, it will generate a scorecard allowing for benchmarking against other companies and correlations with business and financial value (Isaac, 2013).
Although necessary, metrics and data collection tools are not sufficient to support a comprehensive measurement and evaluation framework. Given the multidisciplinary nature of workforce health protection programs and the complexity of the data that must be integrated to inform decision making, information management systems designed for interoperability are needed to drive coordination among functions and ultimately provide a means for managing and integrating organizational knowledge. For example, the National Park Service’s electronic patient care record allows for system-wide epidemiological surveillance and real-time communication with other entities (e.g., public health, risk management) (Ross, 2013). The Smithsonian, by combining its workers’ compensation and injury reporting forms into a single automated system, enabled the immediate sharing of information between human resources and safety components. This system has facilitated case management, allowing for early involvement of nurse case managers in potential workers’ compensation cases (Duval, 2013). Prior to implementation of this system, more than 7 months may have been required for full injury/illness reports to reach the medical office. Similarly, at the Johns Hopkins Institution, an integrated workers’ compensation claims management system promoting a collaborative approach among safety professionals, adjusters, and medical and nursing professionals resulted in a 73 percent reduction in lost time claims over a 10-year period (Bernacki and Tsai, 2003).
A Common Core Culture Dedicated to Health
Ultimately, the commitment to workforce health must be ingrained throughout an organization, from high-level leadership to the frontline workforce. The four requirements for successful integrated employee health programs outlined in the preceding section—leadership commitment to
BOX 3-7
Case Study:
Creating a Culture of Health at Johnson & Johnson (J&J)
J&J has long recognized the importance of protecting its employees’ health, first installing an employee health clinic and gym at its original facility in 1886. As the company has grown and become increasingly decentralized—currently operating more than 275 companies in 60 countries with approximately 128,700 employees (J&J, 2013)—its focus on ensuring employee health has remained. In 1995, J&J began to centralize health services in its U.S.-based companies, bringing employee health, wellness, occupational medicine, disability management, benefit plan design, and employee assistance activities under a single umbrella: the J&J Health and Wellness Program (Isaac, 2013; Ozminkowski et al., 2002). Realizing success with this model, J&J currently is working to centralize global health services under the corporate umbrella as well (Isaac, 2013). J&J believes such centralization will help the company reach its ultimate goal of reducing the burden of disease and creating a competitive advantage.
J&J leadership understood that creation of programs was not enough to ensure sustainable organizational change; it was necessary to change the way workforce health is viewed throughout the organization, to create a “culture of health” (Isaac, 2013). The first step was not simply to bring programs together, but to integrate three primary functions:
- protection: keeping people safe, ensuring compliance with required regulations, and providing quality care to all employees;
- prevention: keeping the well well and managing the ill and injured; and
- performance: linking health-related processes and programs to overarching operational success.
Linking protection, prevention, and performance was the key, J&J believed, to building a sustainable culture focused on the health and well-being of its workforce, and therefore creating lasting change. To achieve such change, J&J’s health strategy focused on five pillars—leadership commitment, enterprise programs, policy and procedures, engagement and participation, and measurement and outcomes—deemed essential to creation of such a culture:
- Leadership commitment: The importance of leadership to the establishment, integration, and maintenance of any long-term strategy cannot be overstated. Senior leadership set goals for health programs, to be pursued by all operational units. These goals, updated every 5 years, are functionally integrated into the organization and evaluated as part of overall organizational performance through inclusion in the company’s annual public report. However, the importance of leadership to creating a culture does not begin and end with senior leadership, but relies on leaders at all levels. Accordingly, J&J instituted mandatory 1-day training for senior and high-potential leaders focused on demonstrating the importance of health
-
not only to the individual but also to unit productivity and the company as a whole. J&J also recruited middle managers to be “health champions” on the ground, acting as “ambassadors to health” in the workplace.
- Enterprise programs: Workforce health must be viewed coherently and as part of the overall organizational strategic plan. To this end, J&J integrated service delivery with innovative solutions that focus on prevention, behavior modification, and linkage to benefit design. The result was a single system that brings together occupational health and disease management, mental health and well-being, healthy lifestyle programs, and health education and awareness programs. J&J’s integrated health program takes a multimodal approach, providing face-to-face support at the worksite or close to home, Web-based and telephonic tools and resources, and environmental support, thus offering a choice of value-added services that meet people where they are in the health continuum.
- Policy and procedures: Centralized policies and procedures that allow for a standardized approach throughout the enterprise were deemed integral to J&J’s program. J&J currently has 27 global standards, two of which are directly related to health. Standardized procedures, or “toolkits,” support worldwide program implementation. To ensure that operating companies are maintaining these global standards, an auditing process has been put in place. Each business unit must complete an annual self-assessment, and Global Health Services visits each unit every 3 years for a joint assessment.
- Engagement and participation: A program is valuable only if it is being used. Program design at J&J is based on a variety of factors relating to need, from employee input to medical surveillance data. Communication strategies are developed to ensure that the workforce knows of their availability. Utilization rates are tracked to determine the success of communication strategies and to support decisions on which programs should be expanded or terminated.
- Measurement and outcomes: Recognizing the importance of the final result, J&J’s approach is to “measure outcomes, not effort.” To enable an in-depth look at the effectiveness of its approach to workforce health, J&J developed the Global Health Assessment Tool. Through this tool, each unit completes an annual self-assessment of how it is meeting the goals and objectives of J&J’s health programs. Based on this assessment, each site receives an action plan, a recommendation, or a certification of success in meeting each goal. In 2012, J&J instituted another ongoing measurement tool, the Occupational Health Index, to examine on a quarterly and annual basis compliance, quality, satisfaction, and efficiencies). Currently under development, the Health and Performance Index combines health, productivity, well-being, and culture of health and program sustainability measures, generating a scorecard that will allow for benchmarking against other companies and correlations to business and financial value.
The results of J&J’s integrated approach are encouraging. In an early study examining the impact of the program on health care utilization and expenditures, Ozminkowski and colleagues (2002) followed employees for up to 5 years prior to program implementation and 4 years after. They found that the program had resulted in fewer inpatient hospital days, mental health visits, and outpatient and doctor’s office visits, yielding savings of approximately $224.66 in medical expenditures per employee per year. An examination of trends over time demonstrated substantial overall increases in savings in years 3 and 4 after implementation, attributable primarily to fewer outpatient and doctor’s office visits and inpatient days. A more recent study examining health care costs from 2002 to 2008 found that J&J spent approximately $565 (in 2009 dollars) less per employee per year on medical costs (inpatient, outpatient, and pharmaceutical) than 16 other similar companies with and without health and wellness programs (Henke et al., 2011). In the first quarter of 2013, 88 percent of occupational injuries and illnesses at J&J were treated in house, enabling workers’ compensation claim costs for those incidents to be avoided (Isaac, 2013). During this time, 20 recordable cases, 19 restricted-work-day cases, and 17 lost-work-day cases were avoided as a result of case management, yielding a savings of nearly $1.4 million based on J&J’s average salary.
workforce health, organizational alignment and coordination, functional alignment, and information management—can help create a common core culture dedicated to maintaining and improving employee health and safety across an organization. Such a culture will unite a workforce in striving toward a common goal: a safe, healthy, and resilient workforce that is physically capable, mentally prepared, trained, equipped, and adequately supported to achieve its mission. The case study in Box 3-7 describes how a culture of health was achieved at J&J through successful integration of its health system and summarizes the measured impacts in terms of cost savings.
ACOEM (American College of Occupational and Environmental Medicine). 2010. Guidance for the medical evaluation of law enforcement officers. Elk Grove Village, IL: ACOEM.
Baicker, K., D. Cutler, and Z. Song. 2010. Workplace wellness programs can generate savings. Health Affairs (Millwood) 29(2):304-311.
Bernacki, E., and S. Tsai. 2003. Ten years’ experience using an integrated workers’ compensation management system to control workers’ compensation costs. Journal of Occupational and Environmental Medicine 45(5):508-516.
Berry, L. L., A. M. Mirabito, and W. B. Baun. 2011. What’s the hard return on employee wellness programs? Harvard Business Review 89(3):20-21.
Burton, J. 2010. WHO healthy workplace framework and model: Background and supporting literature and practices. Geneva, Switzerland: WHO.
CA POST (California Commisssion on Peace Officer Standards and Training). 2010. Tactical medicine: Operational programs and standardized training recommendations. Sacramento: CA POST.
Carroll, C., J. Rick, H. Pilgrim, J. Cameron, and J. Hillage. 2010. Workplace involvement improves return to work rates among employees with back pain on long-term sick leave: A systematic review of the effectiveness and cost-effectiveness of interventions. Disability and Rehabilitation 32(8):607-621.
CDC (Centers for Disease Control and Prevention). 2013. Total worker health. http://www.cdc.gov/niosh/programs/totalworkerhealth (accessed December 22, 2013).
Cecchine, G., E. M. Sloss, C. Nelson, G. Fisher, P. R. Sama, A. Pathak, and D. M. Adamson. 2009. Foundation for integrating employee health activities for active duty personnel in the Department of Defense. Santa Monica, CA: RAND Corporation.
Chapman, L. S. 2012. Meta-evaluation of worksite health promotion economic return studies: 2012 update. American Journal of Health Promotion 26(4):TAHP-1-TAHP-12.
Christensen, C. 2013. Occupational medicine at P&G. Presentation at IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
The Conference Board. 2003. Driving toward “0”: Best practices in corporate safety and health. New York: The Conference Board.
Crowley, D. 2013. Workers’ compensation: Lessons from other organizations: Department of Defense. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
DFEC (Division of Federal Employees’ Compensation). 2012. Procedure manual: Group 2–Payment of compensation and schedule awards. http://www.dol.gov/owcp/dfec/regs/compliance/DFECfolio/FECA-PT2/group2.htm#listofchapters (accessed December 22, 2013).
DFEC. 2013. About our program. http://www.dol.gov/owcp/dfec/about.htm (accessed December 22, 2013).
DoD (Department of Defense). 2004. Force health protection. Arlington, VA: DoD. http://fhp.osd.mil/pdfs/fhp2004.pdf (accessed January 22,2014).
DOI (Department of the Interior). 1996. Appendix 1: Designated agency safety and health official council charter. 485 DM 9 DOI. http://www.doi.gov/safetynet/information/councils/charters/DASHO_Council_charter.pdf (accessed December 23, 2013).
DOI. 2008. About safetynet. http://www.doi.gov/safetynet/about/index.html (accessed December 23, 2013).
DOI. 2009. Occupational medicine program handbook. Washington, DC: DOI.
DOI. 2012. Department safety and occupational health councils, committees, and working groups. In The departmental manual. Part 485: Safety and Occupational Health Program, safety management. Washington, DC: DOI. http://elips.doi.gov/ELIPS/DocView.aspx?id=1652&dbid=0 (accessed December 17, 2013).
DOL (Department of Labor). 2013. Best practices in return to work for federal employees who sustain workplace injury or illness: A guide for agencies. Washington, DC: DOL.
Donabedian, A. 1966. Evaluating the quality of medical care. The Milbank Memorial Fund Quarterly 44(3):166-206.
Duval, J. 2013. Smithsonian Institution occupational health services. Presentation at IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
EEOC (Equal Employement Opportunity Commission). 2013. About EEOC. http://www.eeoc.gov/eeoc (accessed December 22, 2013).
Fabbri, W. 2013. Operational medicine in other organizations: FBI. Presentation at IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, 2013, Washington, DC.
FOH (Federal Occupational Health). 2010. Medical clearance exams for the Department of Homeland Security employees. Washington, DC: FOH.
Franklin, G. M. 2013. Disability prevention, health care cost control and innovation in health care delivery: Historic changes in WA workers’ compensation. Presentation at IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Garbe, B. 2013. Department of the Interior medical clearance programs. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Goetzel, R. Z. 2005. Examining the value of integrating occupational health and safety and health promotion programs in the workplace. Rockville, MD: U.S. Department of Health and Human Services, CDC, NIOSH.
Goetzel, R. Z. 2013. A strategic measurement and evaluation framework to support worker health. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Goldberg, R. L., S. G. Weyers, and S. W. Spilberg. 2004. Medical screening manual for California law enforcement. Sacramento: CA POST.
Hagemann, M. 2013. OSHA injury and illness prevention programs (I2P2). Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Harnois, G., and P. Gabriel. 2000. Mental health and work: Impact, issues and good practices. Geneva, Switzerland: WHO.
Heck, J. J., and G. Pierluisi. 2001. Law enforcement special operations medical support. Prehospital Emergency Care 5(4):403-406.
Henke, R. M., R. Z. Goetzel, J. McHugh, and F. Isaac. 2011. Recent experience in health promotion at Johnson & Johnson: Lower health spending, strong return on investment. Health Affairs (Millwood) 30(3):490-499.
HHS (Department of Health and Human Services). 2000. Healthy people 2010: Understanding and improving health. Washington, DC: HHS.
Hoefsmit, N., I. Houkes, and F. J. Nijhuis. 2012. Intervention characteristics that facilitate return to work after sickness absence: A systematic literature review. Journal of Occupational Rehabilitation 22(4):462-477.
Hunt, H. A. 2009. The evolution of disability management in North American workers’ compensation programs. Kalamazoo, MI: W.E. Upjohn Institute.
Hymel, P. A., R. R. Loeppke, C. M. Baase, W. N. Burton, N. P. Hartenbaum, T. W. Hudson, R. K. McLellan, K. L. Mueller, M. A. Roberts, C. M. Yarborough, D. L. Konicki, and P. W. Larson. 2011. Workplace health protection and promotion: A new pathway for a healthier—and safer—workforce. Journal of Occupational and Environmental Medicine 53(6):695-702.
IOM (Institute of Medicine). 2005. Integrating employee health: A model program for NASA. Washington, DC: The National Academies Press.
IOM. 2013. A ready and resilient workforce for the Department of Homeland Security: Protecting America’s front line. Washington, DC: The National Academies Press.
Isaac, F. 2013. Work, health, and productivity: The Johnson & Johnson story. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
J&J (Johnson & Johnson). 2013. About Johnson & Johnson. http://www.jnj.com/about-jnj (accessed November 12, 2013).
Leffer, M., and T. Grizzell. 2010. Implementation of a physician-organized wellness regime (POWR) enforcing the 2007 NFPA standard 1582: Injury rate reduction and associated cost savings. Journal of Occupational and Environmental Medicine 52(3):336-339.
Loeppke, R., M. Taitel, V. Haufle, T. Parry, R. C. Kessler, and K. Jinnett. 2009. Health and productivity as a business strategy: A multiemployer study. Journal of Occupational and Environmental Medicine 51(4):411-428.
Lowe, G. S., G. Schellenberg, and H. S. Shannon. 2003. Correlates of employees’ perceptions of a healthy work environment. American Journal of Health Promotion 17(6):390-399.
Lute, J. 2013. Keynote address. Presentation to Committee on DHS Workforce Resilience: Meeting 2, February 4, Washington, DC.
Manuele, F. A. 2013. On the practice of safety. Hoboken, NJ: John Wiley & Sons.
Maxwell, N., A. Liu, N. Wozny, and C. M. Francis. 2013. Addressing return-to-work issues in the Federal Employees’ Compensation Act with administrative data. Princeton, NJ: Mathematica Policy Research.
McLellan, D., E. Harden, P. Markkanen, and G. Sorensen. 2012. Safewell practice guidelines: An integrated approach to worker health, version 1.0. Boston, MA: Harvard School of Public Health Center for Work, Health and Well-being.
McMillan, D. 2013. Medical standards and clearances at DHS, ICE. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Minson, M. 2013. Operational medical program/Texas engineering extension service. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Mitchell, M. 2013. Facts to know about TSA’s workers’ compensation program. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Mulry, R. F., A. M. Silverstein, and W. Fabbri. 2008. Medical care of in-custody individuals. In Tactical emergency medicine, edited by R. B. Schwartz, J. G. McManus and R. E. Swienton. Philadelphia, PA: Lippincott Williams & Wilkins. Pp. 123-129.
Musich, S., D. Napier, and D. W. Edington. 2001. The association of health risks with workers’ compensation costs. Journal of Occupational and Environmental Medicine 43(6):534-541.
NBGH (National Business Group on Health). 2006. Improving health: An employer toolkit. Washington, DC: NBGH.
NBGH. 2013. Integrating wellness and occupational health & safety in the workplace. Washington, DC: NBGH.
NIOSH (National Institute for Occupational Safety and Health). 2008. Essential elements of effective workplace programs and policies for improving worker health and wellbeing. Washington, DC: NIOSH.
NIOSH. 2012. Research compendium: The NIOSH Total Worker Health program: Seminal research papers 2012. Publication No. 2012-146. Washington, DC: NIOSH.
NRC (National Research Council). 2000. Safe work in the 21st century: Education and training needs for the next decade’s occupational safety and health personnel. Washington, DC: National Academy Press.
NRC. 2009. Evaluation of safety and environmental metrics for potential application at chemical agent disposal facilities. Washington, DC: The National Academies Press.
Obama, B. 2009. Executive order 13527—medical countermeasures following a biological attack. http://www.whitehouse.gov/the-press-office/executive-order-medical-countermeasures-following-a-biological-attack (accessed November 22, 2013).
Obama, B. 2010. Presidential memorandum—the presidential POWER initiative: Protecting Our Workers and Ensuring Reemployment. http://www.whitehouse.gov/the-press-office/presidential-memorandum-presidential-power-initiative (accessed November, 22, 2013).
OPM (Office of Personnel Management). 2010. FEHB program carrier letter: The health data warehouse. Washington, DC: OPM.
OPM. 2011. FEHB program carrier letter: Federal employees health benefits program call letter. Letter No. 2011-05. Washington, DC: OPM.
OPM. 2012. Federal Employee Viewpoint Survey results: Governmentwide management report. Washington, DC: OPM.
OSHA (Occupational Safety and Health Administration). 2013. All about OSHA. OSHA 3302-01R 2013. Washington, DC: DOL.
OWCP (Office of Workers’ Compensation Programs). 2013. OWCP annual report to Congress FY 2011. Washington, DC: DOL.
Ozminkowski, R. J., D. Ling, R. Z. Goetzel, J. A. Bruno, K. R. Rutter, F. Isaac, and S. Wang. 2002. Long-term impact of Johnson & Johnson’s health & wellness program on health care utilization and expenditures. Journal of Occupational and Environmental Medicine 44(1):21-29.
Polk, J. D. 2013. The charge to the committee. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 1, March 5, Washington, DC.
Rosenfarb, C. 2013. Other agency practices for medical standards and clearances: Department of State. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Ross, D. 2013. National Park Service operational and emergency medical services. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Rousseau, D. M. 2011. Organizational climate and culture. In Encyclopedia of occupational health and safety, edited by J. M. Stellman. Geneva, Switzerland: International Labour Organization. http://www.ilo.org/oshenc/part-v/psychosocial-andorganizational-factors/macro-organizational-factors/item/29-organizational-climate-andculture?tmpl=component&print=1 (accessed December 17, 2013).
SAMHSA (Substance Abuse and Mental Health Services Administration). 2012. Results from the 2011 national survey on drug use and health: Mental health findings. Washington, DC: HHS.
Semler, S. W. 1997. Systematic agreement: A theory of organizational alignment. Human Resource Development Quarterly 8(1):23-40.
Shannon, H., J. Mayr, and T. Haines. 1997. Overview of the relationship between organizational and workplace factors and injury rates. Safety Science 26(3):201-217.
Shigg, T. 2013. Occupational safety and health at DHS: Union perspectives. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Smith, N. 2013. American Red Cross disaster services: Deploying and maintaining a healthy workforce. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Smithsonian Insitution. 2010. Strategic plan FY 2010-2015. Washington, DC: Smithsonian Institution.
Soler, R. E., K. D. Leeks, S. Razi, D. P. Hopkins, M. Griffith, A. Aten, S. K. Chattopadhyay, S. C. Smith, N. Habarta, R. Z. Goetzel, N. P. Pronk, D. E. Richling, D. R. Bauer, L. R. Buchanan, C. S. Florence, L. Koonin, D. MacLean, A. Rosenthal, D. Matson Koffman, J. V. Grizzell, and A. M. Walker. 2010. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. American Journal of Preventive Medicine 38(2 Suppl.):S237-S262.
Spottswood, P. 2013. Medical evaluation and clearance programs. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 1, March 5-6, Washington, DC.
Stair, R. 2013. Operational medicine at DHS: Secret Service. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Tang, N. 2013. Academic model of medical direction and operational support for law enforcement. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Tritz, J. 2013. Workers’ compensation for federal employees. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
USCG (U.S. Coast Guard). 2013. Safety and environmental health manual. COMDTINST M5100.47 Washington, DC: DHS.
Wade, D. 2013. Medical structures and functions in the FBI. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
WHO (World Health Organization). 2005. Mental health policies and programmes in the workplace. Geneva, Switzerland: WHO.
WHO. 2008. Integrated health services—what and why. Geneva, Switzerland: WHO.
Wright, D. 2013. Occupational safety and health at DHS: Union perspectives. Presentation to IOM Committee on DHS Occupational Health and Operational Medicine Infrastructure: Meeting 2, June 10-11, Washington, DC.
Zohar, D. 1980. Safety climate in industrial organizations: Theoretical and applied implications. Journal of Applied Psychology 65(1):96.




















































