3
UNDERSTANDING PSYCHOLOGICAL HEALTH IN THE MILITARY
This chapter provides information essential to understanding the psychological health of military service members and their families. The chapter is divided into five sections. It begins with an overview of the demographic characteristics of U.S. armed forces personnel, both for the total force and for the deployed population. The second section provides a description of the major psychological health consequences experienced by service members deployed in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF). That discussion includes the definitions and prevalence data of the various conditions as well as details about the associated risk factors and protective factors associated with these health consequences. The third section examines the effects of deployments on the psychological well-being of spouses and children of service members deployed to OEF and OIF. Where possible, those effects are discussed in the context of the phases of deployment. The fourth section summarizes the processes that the Department of Defense (DOD) uses to assess psychological health risks in the military as part of its effort to provide prevention and treatment services. The fifth section is an overview of the psychological health services that the military makes available to service members and their families.
In this chapter the committee has summarized and included relevant information from three recent IOM reports: Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families (IOM, 2013a), Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment (IOM, 2012), and Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b).
The focus of this chapter is on military personnel and their families, many of the same psychological health issues that affect service members persist in veterans or can manifest themselves after separation from military service. For more information about the scope of these problems in the veteran population, see Returning Home from Iraq and Afghanistan (IOM, 2013a).
As with that previous report, this report generally does not include comparisons to the civilian population because the military members are likely to differ from civilians in observable and unobservable dimensions. For example, the military is a highly selected population, and applicants must meet a range of eligibility criteria and have a desire to take on the duties of military service. To the extent that these differences may themselves be associated with a health outcome, direct comparisons between the civilian and military populations will be misleading. That said, some civilian studies are included here, specifically when they are useful for interpreting key findings or when research on a particular issue is scant in the military population.
CHARACTERISTICS OF THE ARMED FORCES
The Total Force
At the end of 2011 there were nearly 2.4 million total service members in the armed forces (1.5 million in the active component and 856,000 in the reserve component). The Army is the largest branch, with 38.6 percent of the active component. The Marine Corps, the smallest branch, makes up 13.8 percent of the active force. In the reserve component, the Army National Guard is the largest branch (42.2 percent), followed by the Army Reserve (23.9 percent). The Marine Corps Reserve is the smallest branch in the reserve component (4.6 percent) (DOD, 2012a).
Sociodemographically, the active and reserve components are, by most characteristics, similar (see Table 3-1). For example, in 2011 the active component was 69.8 percent white, 16.9 percent African American, and 11.2 percent Hispanic, while the reserve component was 75.7 percent white, 15.0 percent African American, and 9.8 percent Hispanic. Similarly, 85.5 percent of the active component was male, and 14.5 percent was female, while in the reserve component 82.0 percent was male, and 18.0 percent was female. Additionally, both components have similar distributions for educational achievement and pay grade. Just over 44 percent of the active component and 43 percent of the reserve component has children (DOD, 2012a).
Some characteristics of the two components are different. The active component is younger, for instance, with 43.2 percent of the force under 25, compared to 33.5 percent of the reserve component. Among those from 26 to 40 years of age, the two components are similar in makeup; however, 8.8 percent of active-duty service members are 41 or older, compared to 23.8 percent of the reserve component. More than half (56.6 percent) of the active component is married, compared to 47.7 percent of the reserve component (DOD, 2012a).
TABLE 3-1 Sociodemographic Characteristics of Active-Duty and Reserve Component Personnel, Fiscal Year 2011
|
|
||
|
Sociodemographic Characteristic |
Reserve Component |
Active-Duty Component |
|
|
||
|
Service Branch |
|
|
|
Army |
24.1 |
39.8 |
|
Army National Guard |
42.6 |
|
|
Navy |
7.6 |
22.7 |
|
Marine Corps |
4.7 |
14.2 |
|
Air Force |
8.4 |
23.3 |
|
Air National Guard |
12.4 |
|
|
Gender |
|
|
|
Male |
82.0 |
85.5 |
|
Female |
18.0 |
14.5 |
|
Race |
|
|
|
White |
75.7 |
69.8 |
|
African American |
15.0 |
16.9 |
|
Asian |
3.1 |
3.8 |
|
American Indian or Alaska Native |
0.9 |
1.6 |
|
Native Hawaiian or Other Pacific Islandera |
0.6 |
0.6 |
|
Multiraciala |
0.8 |
2.5 |
|
Other/Unknown |
4.0 |
4.9 |
|
|
||
|
|
||
|
Sociodemographic Characteristic |
Reserve Component |
Active-Duty Component |
|
|
||
|
Ethnicity |
|
|
|
Hispanic |
9.8 |
11.2 |
|
Education |
|
|
|
No high school diploma |
2.4 |
0.5 |
|
Less than a bachelor’s degreeb |
76.8 |
79.1 |
|
Bachelor’s degree |
14.3 |
11.3 |
|
Advanced degree |
5.5 |
7.0 |
|
Unknown |
1.0 |
2.1 |
|
Age |
|
|
|
25 or younger |
33.5 |
43.2 |
|
26-30 |
19.0 |
22.8 |
|
31-35 |
12.8 |
14.3 |
|
36-40 |
11.3 |
10.9 |
|
41 or older |
23.8 |
8.8 |
|
Marital Status |
|
|
|
Not marriedc |
52.0 |
43.4 |
|
Married |
47.7 |
56.6 |
|
Dual military marriagesd |
2.6 |
6.5 |
|
Family Status |
|
|
|
With children |
43.3 |
44.2 |
|
Without children |
56.7 |
55.8 |
|
Pay Gradee |
|
|
|
E1-E3 |
19.1 |
23.8 |
|
E4-E6 |
54.5 |
49.8 |
|
E7-E9 |
11.7 |
9.4 |
|
W1-W5 |
1.4 |
1.4 |
|
O1-O3 |
6.7 |
9.2 |
|
O4-O10 |
6.8 |
6.3 |
|
|
||
NOTE: Reserve component refers to the Selected Reserve of DOD, which comprises traditional drilling Reservists and excludes Department of Homeland Security’s Coast Guard Reserve. Percentages may not total 100 due to rounding.
a The Army does not report “Native Hawaiian or Other Pacific Islander” or “Multiracial.”
b Includes individuals with at least a high-school diploma and possibly additional education less than a bachelor’s degree (e.g., associate’s degree).
c Includes never married, divorces, annulled, widowed, and unknown cases.
d A dual-military marriage refers to an active-duty or reserve component member who is married to another active-duty or reserve component member. The Army National Guard does not report dual military marriages.
e Pay grades are divided into three groups: Enlisted (E), Warrant Officer (W), and Officer (O). Within each group, 1 is the lowest pay grade.
SOURCE: DOD, 2012a.
The Deployed
More than 2.6 million service members have been deployed in support of OEF/OIF since September 11, 2001 (IOM, 2012). As of December 31, 2010, more than half of those deployed were in the Army (including active and reserve components). Nearly one-third of those deployed were in the active-component Army. National Guard and reserves across branches constituted
one-third of those deployed. More than 85 percent of those deployed were enlisted, and 12 percent were women. However, deployed women were not evenly distributed across services and pay grades. For example, deployed women were only 3.2 percent of E1–E4 in the Marine Corps, but 20.5 percent of O1–O3 in the Air Force. The average age of those deployed was 33.4 years. Deployed Marine Corps were the youngest on average (29.5 years) and deployed Air Force were the oldest (35.8 years). Those deployed from the reserves and National Guard were older on average (36 years) than active-component service members (32 years). More than two-thirds of the deployed had a high-school degree or equivalent, and more than 30 percent had at least some college education. Nearly 60 percent of those deployed were married, and nearly half had dependent children, 1.97 on average (IOM, 2013a).
By the end of 2010, deployed service members had been deployed an average of 1.7 times: 57 percent once, 27 percent twice, 10 percent three times, and 6 percent four or more times. Those in the National Guard and reserves had fewer multiple deployments than those in the active component. The average length of deployments was 7.7 months, with the average length in the various services ranging from 4.5 months in the Air Force to 9.4 months in the Army. The average cumulative length of deployments for those who deployed multiple times was 16.9 months. The average dwell time between deployments was 21 months.
Military Families
Military families are more diverse than most statistics or research might suggest. For example, many families do not meet the criteria used for official counts of military families and, therefore, are not included in the data (for example, common-law spouses). As a result, this chapter reports information on only a subset of military families: those of service members in heterosexual marriages and parents with dependent children or adult dependents who live with them at least part of the time. The committee views the military’s definition of family as narrow and out of step with the diversity in family arrangements in modern society. The committee did not find demographic data about parents or siblings of service members (who are sometimes relied upon for important caregiving responsibilities), unmarried partners, stepfamilies, children who are not legal dependents (for example, stepchildren or nonresidential children), gay families, service members acting as substitute parents, or other nontraditional family configurations. All DOD demographic data on military families and nearly all published studies focus on heterosexual, married military families. This section summarizes the limited family data reported by the 2011 DOD Demographics Profile of the Military Community (DOD, 2012a).
Table 3-2 summarizes the available demographic data on military families. At the end of 2011, the country’s 1,411,425 active-duty service members had 1,984,450 family members, and the country’s 847,934 reserve members had 1,146,358 family members. As stated above, 44.2 percent of active-duty members and 43.3 percent of reserves have children, and those in both components who have children have an average of 2.0. Among active-duty members, 5.3 percent are single with children, and among reserves, 9.4 percent are single with children. Many military children (42.6 percent), of active-duty members are under 5 years old. Among children of reserve members, 28.8 percent are under age 5, which is logical considering that the reserve component is an older population than the active component (DOD, 2012a).
There are 726,500 spouses of active-duty service members, more than half of whom are under age 30. The unemployment rate among spouses of active-duty service members is higher
than the national unemployment rate: 15 percent of spouses of active-duty members report that they are not currently in the labor force but are looking for work (DOD, 2012a). The committee was unable to find employment statistics for spouses of reserve component members.
TABLE 3-2 Summary of Selected Family Demographic Characteristics for DOD Active-Duty and Selected Reserve Members
|
|
||
|
Demographic Characteristic |
Active-Duty Component |
Reserve Component |
|
|
||
|
Percent married |
56.6% |
47.7% |
|
Percent in dual-military marriages |
6.5%a |
2.6%b |
|
Percent of married members in dual-military marriage |
11.5% |
5.5% |
|
Percent with children (overall) |
44.2% |
43.3%d |
|
Percent married to civilian, with children |
36.1% |
32.5% |
|
Percent dual-military with children |
2.8% |
1.5% |
|
Percent single with children |
5.3% |
9.4% |
|
Average number of children of members with children |
2.0 |
2.0 |
|
Percent of children ages 0 to 5 |
42.6% |
28.8% |
|
Percent married to civilian with no children |
14.0% |
12.7% |
|
Percent dual-military with no children |
3.7% |
1.2% |
|
Percent single with no children |
38.1% |
42.9% |
|
Percent with family responsibilitiesc |
59.0% |
56.4% |
|
Average number of dependents of members with dependents |
2.4 |
2.4 |
|
|
||
NOTE: Children category includes minor dependents age 20 or younger or age 22 or younger who are enrolled as full-time students.
a Of these, 81.8 percent are enlisted members and 18.2 percent are officers.
b Of these, 76.1 percent are enlisted members and 23.9 percent are officers.
c Members are classified as having family responsibilities if they have a dependent (spouse, children, other dependents) registered in the Defense Enrollment and Eligibility Reporting System.
d N=855,867 (includes Coast Guard).
SOURCE: DOD, 2012a.
PSYCHOLOGICAL HEALTH CONSEQUENCES OF DEPLOYMENT
Service Members
Compared with previous conflicts, during OEF and OIF the all-volunteer military has experienced more numerous deployments of individual service members; has seen increased deployments of women, parents of young children, and reserve and National Guard troops; and in some cases has been subject to longer deployments and shorter times at home between deployments. Many of those who have served in OEF and OIF have readjusted with few difficulties, but others have had problems in returning home, reconnecting with family members, finding employment, and returning to school. Lingering health problems related to combat, including traumatic brain injury (TBI) and posttraumatic stress disorder (PTSD), can make reintegration more difficult.
Although the vast majority of OEF and OIF veterans felt proud of their service (96 percent), felt they became more mature as a result of their service (93 percent), and built selfconfidence while serving (90 percent), 44 percent have reported readjustment difficulties, 48 percent strains on family life, 47 percent outbursts of anger, 49 percent posttraumatic stress, and 32 percent an occasional loss of interest in daily activities (Pew Research Center, 2011).
As early as 2004 it was estimated that over one-fourth of troops returning from OEF and OIF were suffering from psychological health disorders (Hoge et al., 2004). Later estimates suggested that one-fifth of the troops reported symptoms of PTSD or depression, and about the same fraction reported a probable TBI during deployment (Tanielian and Jaycox, 2008). Recent RAND Corporation reports note that a full one-third of returning OEF and OIF service members reported symptoms of psychological health or cognitive problems (Hosek, 2011; Tanielian and Jaycox, 2008). RAND reports that 18.5 percent of a representative sample of returning service members met the diagnostic criteria for PTSD or depression, 19.5 percent reported a probable TBI during deployment, and 7 percent met the criteria for a psychological health problem and TBI (Tanielian and Jaycox, 2008).
This section discusses the leading health consequences of deployment, including TBI, PTSD, major depression, substance use disorder, and suicide. The committee focused on these conditions because many of the DOD prevention programs are intended to prevent these particular conditions or to mitigate negative outcomes that may be associated with them. Although this chapter is organized by condition, the committee recognizes that the conditions discussed often do not occur in isolation. Many conditions addressed in this report share the same risk factors, are risk factors themselves for other conditions, and frequently co-occur. For example, PTSD has common risk factors with depression, is a risk factor for depression, and commonly co-occurs with depression and TBI (IOM, 2013a). Likewise, suicidality is higher among individuals with all of these disorders than in those without them. Tobacco use and nicotine addiction, although not addressed in this report, are also more common in individuals with depression, PTSD, substance use disorders, and other psychological conditions than in individuals without them (IOM, 2009a).
Based on the literature of psychological health disorders in OEF and OIF active-duty members and veterans, the 2013 IOM report Returning Home from Iraq and Afghanistan concluded that our understanding of the health consequences of service in Iraq and Afghanistan remains incomplete; even simple questions such as prevalence rates of physical and psychologic morbidity after military service in Iraq or Afghanistan continue to lack precision. For example, the literature reviewed by the committee that prepared that report found PTSD prevalence rates ranging from approximately 1 percent to 30 percent in different studies. Those widely varying prevalence estimates have added to the public’s confusion, have not been informative for health care planning, and fail to assist in projecting long-term reintegration needs. The committee noted that these differences might be explained by variations in study design factors, including population sampling strategy; data collection instruments and methods, deployment characteristics (e.g., combat exposure; length of deployment, number of deployments, and time elapsed after deployment), and demographic and service-related characteristics (e.g., active-duty versus reserves and National Guard, military training and occupation, and service branch). In particular, variations in assessment strategies, such as measuring documented psychological health diagnoses among those seeking health care versus anonymous screening, can yield vastly different results, which highlights some of the challenges to accurate identification of those who
may benefit from intervention. It has proved difficult to account for, understand, and reconcile those differences in order to provide the insights and answers needed for effective public policy, prevention, treatment, and reintegration.
Traumatic Brain Injury
Although not mentioned in the committee’s charge, TBI is a common injury among the military population—particularly among the deployed—and it frequently co-occurs with PTSD and depression (IOM, 2013a). The DOD and the Veterans Brain Injury Center estimate that brain injuries account for 22 percent of all OEF and OIF combat casualties, whereas in Vietnam brain injuries accounted for only 12 percent of combat casualties (Summerall, 2012). Furthermore, only a fraction of TBIs in the military are attributable to combat. Although several definitions of TBI exist, the committee will use the definition developed by DOD and the Department of Veterans Affairs (VA) as it focuses on service members and veterans.
The DOD–VA common definition of TBI is
A traumatically induced structural injury and/or physiological disruption of brain function as a result of an external force that is indicated by new onset or worsening of at least one of the following clinical signs, immediately following the event (DOD, 2009a):
• any period of loss of or a decreased level of consciousness;
• any loss of memory for events immediately before or after the injury;
• any alteration in mental state at the time of the injury (confusion, disorientation, slowed thinking, etc.);
• neurological deficits (weakness, loss of balance, change in vision, praxis, paresis/plegia, sensory loss, aphasia, etc.) than may or may not be transient; and
• intracranial lesion.
TBI is often classified according to severity: mild, moderate, or severe. “Mild TBI” and “concussion” are often used interchangeably. This section will focus on mild TBI, which accounts for the overwhelming majority of all TBIs sustained by the armed forces. Between 2000 and August 2013, of the 280,734 TBIs sustained in the armed forces, 231,386 (82.4 percent) were mild TBIs (Defense and Veterans Brain Injury Center, 2013).
Prevalence
Three recent studies have attempted to measure the prevalence of mild TBI in OEF and OIF service members. The RAND Corporation completed a telephone survey of 1,938 soldiers to determine probable TBI and other psychological health outcomes. Probable TBI was assessed using the Brief Traumatic Brain Injury Screen. If a soldier reported that he or she was injured during deployment and experienced “being dazed, confused, or seeing stars,” “not remembering the injury,” or “losing consciousness,” he or she was considered to have a probable TBI. The weighted results showed that 19.5 percent had a probable TBI (Tanielian and Jaycox, 2008).
In another study, all 3,973 members of a combat brigade returning from a 1 year deployment to Iraq were screened for TBI using the Warrior Administered Retrospective Casualty Assessment Tool (WARCAT). The WARCAT is a self-administered tool that asks detailed questions about sustained injuries. It asks about common injuries that cause TBI, altered mental states, and symptoms following the injury (physical and psychological). The WARCAT
results are triangulated with medical records and witnesses. In all, the results from this study indicate that 22.8 percent of the brigade had probably sustained a mild TBI while deployed (Terrio et al., 2009).
A longitudinal study of a National Guard Brigade found a lower rate of mild TBI than in the above-mentioned studies (Polusny et al., 2011). The researchers used an adapted version of the Defense and Veterans Brain Injury Center screening tool to determine mild TBI in a large group of National Guardsmen. The screen was administered in Iraq 1 month before the soldiers returned from deployment and again 1 year after their return. At the initial assessment, 9 percent of soldiers were found to have a mild TBI. The follow-up assessment, however, revealed that 22 percent of soldiers had mild TBI. It was not clear if the dramatic increase after 1 year was due to recall bias or to soldiers filtering their responses to ensure they remained with their unit and were not delayed in returning home, or possibly to the poor reliability of the screening tool (Polusny et al., 2011).
Comorbid Conditions
Depression
Depression and symptoms of depression are often found in those who have brain injury. In a study of OEF and OIF veterans, 31.8 percent of those with a TBI diagnosis suffered from major depression (Tanielian and Jaycox, 2008). In another study of 2,525 Army infantry soldiers 3 to 4 months following their return from a year-long deployment to Iraq, Hoge et al. (2008) found that among those who had experienced loss of consciousness, 22.9 percent also suffered from major depression. Among those who experienced an altered mental state due to an injury (but remained conscious), 8.4 percent also suffered from major depression.
Substance Use Disorders
It is unclear if survivors of mild TBI are at increased risk for substance use disorders. Returning Home from Iraq and Afghanistan (IOM, 2013a) summarizes the conflicting evidence and notes that most studies that look at the association between substance use and brain injury, examine all brain injuries and either do not indicate the severity of the injury or include injuries of all severities. A 2009 IOM report, Gulf War and Health, Volume 7: Long-Term Consequences of Traumatic Brain Injury (IOM, 2009b), concludes that there is limited but suggestive evidence of an association between TBI (of all severities) and decreased drug and alcohol use, relative to pre-injury use, in the 1 to 3 years following the TBI. A civilian study of TBI found that drinking and reported problems with alcohol were less 1 month after the injury than they had been before the injury but that they had increased somewhat after 1 year (although not to pre-injury levels). Those with more severe TBI decreased their alcohol use significantly more than those who had milder TBIs (Dikmen et al., 1995).
Suicide
In a study using Danish hospitalization data on civilians admitted to a hospital with a concussion, cranial fracture, or a cerebral contusion or traumatic intracranial hemorrhage, Teasdale and Engberg (2001) looked at how suicide incidence among these civilians compared with the rate in the general population. The authors screened the patients in the national death register and found an increased incidence of suicide in the TBI groups, including those with mild
TBI, when compared to the general population. In a study of active-duty service members, however, Skopp et al. (2012b) failed to find such an association between mild TBI and suicide. Those authors suggested that the difference in results between their study and that of Teasdale and Engberg may be due to a difference in the nature of the TBI experienced by the different populations in the two studies. In civilians TBIs are often associated with risky behaviors, whereas in the military mild TBIs often occur as the result of unpredictable incidents during training or combat.
Posttraumatic Stress Disorder
Although the 2009 IOM report found limited or suggestive evidence of an association between mild TBI and PTSD, the overlapping symptomology of TBI and PTSD complicates the relationship between the two conditions. Returning Home from Iraq and Afghanistan (IOM, 2013a) reported that multiple studies have shown that OEF and OIF veterans often display signs of PTSD (Carlson et al., 2010; Hill et al., 2009; Hoge et al., 2008; Kennedy et al., 2010; Schneiderman et al., 2008). A RAND study of 1,965 OEF and OIF participants found that 19.5 percent had probable TBI and 13.8 percent had probable PTSD. Of those with TBI, 33.8 percent screened positive for PTSD (Tanielian and Jaycox, 2008). Hoge et al. (2008) also found a significant association between TBI and PTSD, with 44 percent of soldiers with loss of consciousness meeting criteria for PTSD.
Posttraumatic Stress Disorder
PTSD is a psychiatric disorder that can develop after the direct personal experience of or the witnessing of an event that poses a perceived threat of death or serious injury. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) now categorizes PTSD symptoms occurring in response to a trauma in four clusters: intrusion symptoms (reexperiencing symptoms such as flashbacks, nightmares, and reactivity to trauma reminders); avoidance (of trauma-related thoughts, feelings, or external trauma reminders); negative alterations in cognitions and mood (e.g., negative beliefs and emotions, self-blame and constricted affect); and arousal and reactivity (e.g., hypervigilance, irritability, startle response, sleep disturbance, and concentration difficulties). According to the DSM-5, if the symptoms persist for 3 days to 4 weeks, the diagnosis is acute stress disorder, while if the symptoms endure for more than 1 month, the diagnosis is PTSD. The manual states that the onset of PTSD usually begins within 3 months of exposure to the traumatic event but that it may occur months later. “Delayed expression” refers to cases in which some symptoms appear soon after the trauma but take months (or even years) to meet the full diagnostic criteria (APA, 2013). Military-related traumatic events that may trigger PTSD include exposure to war, threatened or actual physical assault, threatened or actual sexual assault, being taken hostage, torture, incarceration as a prisoner of war, and motor vehicle accidents (APA, 2013). DSM-5 also considers certain indirect exposures through professional duties such as clearing body parts, first-responder activities, and accidental or violent death of a friend or relative to be exposures.
Individuals with PTSD often display a heightened startle response in reaction to unexpected stimuli (such as a loud noise or unexpected movement). Additionally, many with PTSD have difficulty remembering daily events and have difficulty concentrating or staying focused on tasks (APA, 2013). PTSD can be chronic and have no remission, or it can be recurrent and have periods of remission and recurrence (Friedman, 2003).
Prevalence
PTSD is one of the disorders most commonly diagnosed in U.S. combat troops after their deployment to Afghanistan and Iraq. In a review of the literature, the IOM (2013a) reported that PTSD prevalence estimates range from 5 percent to 30 percent among service members deployed in OEF or OIF (Booth-Kewley et al., 2010; Hoge et al., 2004, 2007; MHAT-III, 2006; Smith et al., 2008; Thomas et al., 2010). The estimates depend on when the evaluation was conducted, the diagnostic method used (for example, self-reported symptoms versus diagnosis by a health care professional), and the definition used for PTSD. Among service members with injuries sustained in OEF or OIF combat, reported PTSD prevalences range from 16.2 percent to 43.9 percent, depending on the injury. Among those who saw combat but were not injured, prevalence was 9.1 percent (Hoge et al., 2008). The prevalence may also vary according to whether the assessment method included a determination of whether the full DSM criteria for PTSD diagnosis were met as opposed to a briefer positive screen for PTSD.
The figures cited above clearly indicate variability in estimates of PTSD prevalence in the OEF and OIF military populations. Ramchand et al. (2010) reviewed 29 studies of OIF and OEF service members to characterize the variability in PTSD estimates and look for possible sources of the variability. The researchers found that the studies could be divided into studies of military personnel who were seeking treatment (for any injury) and those who were not seeking treatment. Studies of non-treatment-seeking service members generally provided PTSD prevalence estimates of about 5 to 20 percent, while studies of treatment-seeking service members yielded estimates as high as 50 percent on the basis of screening, although rates were typically lower when actual diagnoses were made. Recent research indicates that 23 percent of those seeking treatment receive a PTSD diagnosis. The authors found that the variability in PTSD estimates was probably related to representativeness and case definitions. A further factor may be the level of anonymity, which affects the PTSD estimates through a combination of factors such as concerns about stigma and worries about how a PTSD diagnosis and treatment could affect one’s standing with peers and command, influence deployment decisions, and damage one’s military career. Most studies have used post-deployment convenience samples that likely missed those service members most likely to have psychological health problems, such as those with serious injuries or those who have separated from service. The healthiest service members would also likely be excluded in many of the post-deployment studies because they are more likely to deploy multiple times and be in theater and thus unavailable for study participation. Furthermore, the studies used different definitions of PTSD (Tanielian and Jaycox, 2008). Returning Home from Iraq and Afghanistan (IOM, 2013a) concluded that using different definitions most likely contributes to much of the variability observed in the various studies and that improving the estimates of prevalence will require the use of a consistent set of criteria for PTSD and a standardized assessment.
Risk Factors
Many factors are associated with an increased likelihood of PTSD. Specifically, the IOM (2013a) reported that being under age 25, being single, and being of junior rank are risk factors for PTSD in OEF and OIF service members and veterans (Lapierre et al., 2007; Phillips et al., 2010; Seal et al., 2009). On the other hand, National Guardsmen over age 40 had significantly higher risks of PTSD (adjusted relative risk [ARR] =1.18; 95% confidence interval [CI] = 1.11–1.27) than National Guard and reserve veterans under age 25 (adjusted for gender, age group,
race/ethnicity, marital status, rank, service branch, multiple deployments, and time period) (Seal et al., 2009). Among those that deployed, the IOM (2013a) found that certain deployment-related stressors (such as troubles at home, lack of privacy, and problems with leadership), combat exposure, prior traumatic exposure, military sexual trauma, a history of psychological health conditions, and severe physical injury were all risk factors for PTSD. These are discussed individually below.
Combat Exposure
As expected, combat exposure and PTSD are linked. In their review of 29 studies of OIF and OEF military personnel, Ramchand et al. (2010) found that the only factor that was consistently significantly associated with PTSD was combat exposure and that other factors that often appear to be associated with PTSD may simply be surrogates of combat exposure.
The types of combat experiences that are associated with PTSD include killing someone (Maguen et al., 2011), the threat of personal harm (Kolkow et al., 2007; Peterson et al., 2010; Phillips et al., 2010), witnessing someone from one’s unit or an ally unit being seriously wounded or killed (Pietrzak et al., 2011), and experiencing “friendly” fire (Pietrzak et al., 2011).
Deployment-Related Stressors
Deployment and deployment-related stressors, including concerns back home, issues with leadership, and lack of privacy, have been associated with increased risk of PTSD (Booth-Kewley et al., 2010; Seal et al., 2009). Vasterling et al. (2010) found that deployed soldiers who had high combat exposure (according to the Deployment Risk and Resilience Inventory scale) showed the greatest increase in PTSD symptoms. Moreover, some investigations have indicated that National Guard soldiers suffer disproportionately from deployment (Milliken et al., 2007; Thomas et al., 2010). Deployment-related factors associated with National Guardsmen and PTSD (and depression) include financial hardship, job loss, and lack of employer support (Riviere et al., 2011).
Traumatic Exposures
Prior to military Veterans who have had prior traumatic experiences appear to be more likely to develop PTSD than those who do not have such a history. Phillips et al. (2010) found that two or more exposures to violence before entering the military also increased the likelihood of screening positive for PTSD. Multiple studies have found an association between adverse childhood experiences—such as physical, sexual, and psychological abuse or exposure to a person in the home who was mentally ill, alcoholic, or violent—and psychiatric symptoms of PTSD, anxiety, or depression (Cabrera et al., 2007; Dedert et al., 2009; Fritch et al., 2010; Gahm et al., 2007).
Military sexual trauma Military sexual trauma (MST) is defined as severe or threatening sexual harassment and sexual assault that occurs while serving in the military (Kimerling et al., 2007). MST appears to be an important risk factor for PTSD (Dutra et al., 2011; Himmelfarb et al., 2006; Maguen et al., 2012; Suris and Lind, 2008). After reviewing electronic medical records of 108,149 male and 17,580 female OEF and OIF veterans, Kimerling et al. (2010) found that those who were victims of MST were significantly more likely to have received a PTSD diagnosis and to have other psychological health disorders, including depression, other anxiety disorders, and substance use disorders than those who did not have a
history of abuse. Odds ratios remained significant after adjustment for other significant associations, and the effect sizes in women were substantially greater than those in men, indicating that MST has a greater impact on women than on men.
A representative survey of DOD service members found that in 2012, 6.1 percent of active-duty women and 1.2 percent of active-duty men experienced unwanted sexual contact, defined as sexual touching only, attempted or completed intercourse, or attempted or completed anal or oral sex (DOD, 2013a). Sixty-seven percent of women and 73 percent of men reported that the unwanted sexual contact occurred at their military installations, while 19 percent of women and 26 percent of men reported that the unwanted contact occurred while they were deployed to a combat zone. Forty-seven percent of women and 19 percent of men reported that the perpetrator was using alcohol during the incident. Thirty-eight percent of women and 17 percent of men indicated the perpetrator was of higher rank/pay grade but not in their chain of command, while 25 percent of women and 27 percent of men indicated that the perpetrator was in their chain of command. Among suspected perpetrators investigated, 90 percent were male, 2 percent were female, and 8 percent were not identified.
Thirty-three percent of the women and 10 percent of the men who experienced unwanted sexual contact reported the incident to a DOD authority (DOD, 2013a). Of the women who did not report the incident, 51 percent did not do so because they felt that their report would not be kept confidential, and 47 percent feared retaliation from the offender (DOD, 2013a). Among the men who did not report the incident, 22 percent did not do so because they thought that individuals not directly involved with the incident might get in trouble, 17 percent thought they would not be believed, and 16 percent thought their performance evaluation or chance of being promoted would suffer (DOD, 2013a).
LeardMann et al. (2013a) examined the risk factors associated with sexual assault or harassment in a cohort of 13,262 active- and reserve-component women. The authors found that women who were deployed and experienced combat reported the highest cumulative 3-year incidence of sexual harassment (19.9 percent) and assault (4.0 percent). Being born in 1980 or later, prior sexual stressors, being recently divorced, and having prior psychological health disorders were also associated with increased risk of experiencing sexual assault or harassment (or both).
History of psychological health conditions Military personnel who have been previously diagnosed with a psychological health condition, particularly PTSD, are at greater risk for a repeat diagnosis in theater (Larson et al., 2011). Using self-report data, Sandweiss et al. (2011) assessed the relationship between post-deployment PTSD and pre-deployment (baseline) psychiatric conditions and injury severity among 22,630 military personnel who had been deployed to Iraq or Afghanistan. PTSD was significantly associated with baseline psychiatric conditions; service members who had one or more baseline psychiatric conditions were 2.52 times more likely to report PTSD symptoms than those who had no baseline psychiatric conditions.
Injury severity and neurologic dysfunction Grieger et al. (2006) evaluated seriously injured soldiers and found that severe physical problems were significantly associated with PTSD. MacGregor et al. (2009) also observed a positive association between injury severity and PTSD and other psychological health diagnoses.
Protective Factors
Although it has been mostly retrospective in nature, some research has been conducted on factors that might protect soldiers from PTSD and other psychological health disorders. Gulf War and Health, Volume 6: Physiologic, Psychologic, and Psychosocial Effects of Deployment-Related Stress (IOM, 2008) reviewed studies of veterans of such past conflicts as World War II, the Gulf War, and the Vietnam War and noted that psychological resilience—often characterized by hardiness, personal control, and positive coping strategies—is inversely related to the risk of PTSD after traumatic or stressful events. Studies have indicated that strong social support is protective against the onset of PTSD. Returning Home from Iraq and Afghanistan (IOM, 2013a) reviewed recent studies of OIF and OEF veterans and found that those with PTSD had significantly lower resilience scores1 than those who did not have PTSD (Pietrzak et al., 2009a,b). Furthermore, unit support and post-deployment support were inversely related to PTSD and depressive symptoms. Additional protective factors cited in Returning Home from Iraq and Afghanistan included positive appraisals of military service, having five or more close confidants, and longer dwell times (MacGregor et al., 2012; Phillips et al., 2010; Skopp et al., 2011).
Comorbid Conditions
PTSD is often comorbid with other psychiatric conditions, including substance use disorders. The 2008 IOM report Gulf War and Health, Volume 6 (IOM, 2008) noted that the temporal relationship between PTSD and these other conditions is complex. PTSD increases the likelihood of other psychiatric disorders, and the other disorders increase the likelihood of PTSD.
That report reviewed the research on psychiatric disorders in veteran populations and concluded that PTSD is highly comorbid with generalized anxiety disorder and major depressive disorder. Alcohol and drug use, sleep disorders, an increased report of general symptoms, and a variety of psychosocial problems (including relationship problems, legal problems, violence and aggression, employment problems, and decreased quality of life) were associated with PTSD. Veterans with PTSD were not more likely to be homeless compared to veterans without PTSD, although veterans with prior combat exposure were more likely to be homeless than those without such exposure (IOM, 2008). The review of the literature in Gulf War and Health, Volume 6 (IOM, 2008) found that the association between PTSD and cardiovascular disease and PTSD and digestive disorders was mixed. No association was found between PTSD and endocrine diseases and PTSD and neurocognitive and neurobehavioral effects.
Major Depression
Mood disorders are a cluster of psychological disorders that are characterized by mood swings or an abnormally depressed (low) mood or a manic mood or irritability. The most common mood disorder is depression, and the clinically most important form is major depression, which is characterized by a depressed mood most of the day (nearly every day) or a loss of interest or pleasure, or both, accompanied by several of the following symptoms: marked unintentional weight loss or weight gain, insomnia or hypersomnia, psychomotor agitation or retardation observable by others, fatigue nearly every day, diminished concentration or increased indecisiveness, recurrent thoughts of death, or suicidal ideation (APA, 2013). Like PTSD,
____________________
1 Based on the Connor-Davidson Resilience Scale (CD-RISC) (Connor and Davidson, 2003).
depression may be defined by strict criteria, such as the DSM criteria for major depression, or by self-assessment of depression symptoms. To meet the diagnostic criteria, major depressive disorder symptoms must be present for a 2-week period. It is the second-most common psychological-health diagnosis in veterans after PTSD (Seal et al., 2009).
Prevalence
There have been no population-based studies of U.S. service members deployed to war zones in which investigators used structured diagnostic interviews, which permit more direct estimation of major depression and have an advantage over the screening instruments that are commonly used in epidemiologic surveys. According to RAND (Tanielian and Jaycox, 2008), the extant studies may substantially underestimate the prevalence of depression in the post-deployment samples. Furthermore, most studies use convenience samples, which may not be representative of the entire population deployed to war zones.
RAND reviewed 12 studies that assessed the prevalence of depression in service members who served in OEF or OIF (Tanielian and Jaycox, 2008). Estimates of prevalence in active-duty service members ranged from 5 percent (Hoge et al., 2006; Kolkow et al., 2007; MHAT-II, 2005) to 37 percent (Lapierre et al., 2007). Thomas et al. (2010) also estimated the prevalence of depression in active-duty and National Guard troops at 3 and 12 months after deployment to Iraq. They used three case definitions of depression, each reflecting a level of functional impairment. At 3 months, the prevalence ranged from 16 percent (no functional impairment) to 8.3 percent (serious impairment) in active-duty soldiers and from 11.5 percent (no impairment) to 5.0 percent (serious impairment) in National Guard soldiers. At 12 months, the rates were similar to those at 3 months in active-duty soldiers but substantially increased in National Guard soldiers.
Gadermann et al. (2012) completed a meta-analysis of 25 epidemiological studies that looked at depression among U.S. military personnel according to the DSM-IV definition of major depression. The authors’ best estimate for total prevalence of major depression was 12 percent among the currently deployed, 13.1 percent among the previously deployed, and 5.7 percent among the never deployed.
Risk Factors
Among U.S. military personnel, Gadermann et al. (2012) found that being female, young (17 to 25 years old), unmarried, and with less than a college education increased the likelihood of depression. Other risk factors for depression reported in literature include military sexual trauma, childhood physical abuse, and other adverse childhood experience (Cabrera et al., 2007; Fritch et al., 2010; Kimerling et al., 2010; Suris and Lind, 2008).
Deployment is also associated with a diagnosis of depression (Gadermann et al., 2012; IOM, 2013a). Furthermore, deployed OEF and OIF service members exposed to combat had a higher rate of new-onset depression (men, 5.7 percent; women, 15.7 percent) than those who deployed but did not see combat (men, 2.3 percent; women, 5.1 percent) (Wells et al., 2010).
Investigators have shown that depression is a major contributor to health dissatisfaction (Rauch et al., 2010) and to psychological health and physical health outcomes (Pittman et al., 2012). In fact, Kinder et al. (2008) found a positive association between depression and all-cause mortality. Additionally, among service members who attempted suicide in 2010, 17.7 percent of
them had a diagnosis of major depressive disorder (DCOE, 2011). More information about the link between suicide and depression appears in the suicide section of this chapter.
Substance Use Disorders
Substance use disorders include the misuse of intoxicating substances (including illicit drugs, prescription drugs, alcohol, and other toxic agents). According to DSM-5 (APA, 2013), a major feature of substance use disorders is “an underlying change in brain circuits that may persist beyond detoxification, particularly in individuals with severe disorders. The behavioral effects of these brain changes may be exhibited in the repeated relapses and intense drug craving when the individuals are exposed to drug-related stimuli. These persistent drug effects may benefit from long-term approaches to treatment” (APA, 2013, p. 483). Diagnosis of substance use disorders is based on an individual’s pattern of behavior and usage of the substance and is marked by a cluster of cognitive, behavioral, and physiological symptoms. An individual with a substance use disorder will continue using the substance despite the presence of substance-related symptoms and the problems they cause. According to DSM-5, symptoms may include taking more of a substance or taking it for a longer time than originally intended; the inability, despite a desire, to reduce the consumption of a substance; spending significant time obtaining a substance, using it, and recovering from its use; the failure to fulfill work, school, or family obligations because of substance use; recurrent social and interpersonal problems because of substance use; withdrawal from social occupational or family activities because of substance use; and continued use despite repeated physical and psychological health problems (APA, 2013).
Although previous definitions of substance use disorders for which most prevalence data is currently available made the distinction between “abuse” and “dependence,” DSM-5 abandoned this dichotomy and classifies the disorder by severity: mild substance use disorder (two to three symptoms), moderate substance use disorder (four to five symptoms), or severe substance use disorder (six or more symptoms).
Prevalence
Alcohol
Milliken et al. (2007) found that, based on results from the health assessment conducted after deployment, problem alcohol use (as determined by a positive response to at least one question on a two-item conjoint screen for alcohol use) among service members ranged from 11.8 percent (active duty) to 15.0 percent (National Guard and reserve). Heavy alcohol use (five or more drinks for males and four or more for females per occasion, at least once per week, for the past 30 days) in the active-duty military remained mostly constant between 2002 (18.1 percent) and 2008 (20.0 percent). By service, adjusted for demographic differences, heavy alcohol use is highest in the Marine Corps (25.2 percent), followed by the Army (21.6 percent), Navy (17.9 percent), and finally the Air Force (15.9 percent) (Bray et al., 2009).
Compared to civilians, a greater percentage of service members are heavy alcohol users overall (19.7 percent [95% CI 18.2–21.2 percent] versus 13.6 percent [95% CI 13.3–13.9 percent]). The difference varies by age group, however. Older service members (aged 46 to 64) are less likely to be heavy drinkers than civilians of the same age (3.9 percent [95% CI 2.8–4.0 percent] versus 8.5 percent [95% CI 7.4–9.6 percent]). Military personnel aged 18 to 25, however, exhibit significantly higher rates of heavy drinking than their civilian counterparts
(25.7 percent [95% CI 23.4–28.0 percent] versus 16.4 percent [95% CI 15.9–16.9 percent]) (Bray et al., 2009).
Although the rate of heavy drinking has remained mostly constant, binge drinking (five or more drinks for males, or four or more drinks for females, on a single occasion at least once in the past 30 days) among active-duty service members increased from 34.9 percent in 1998 to 47.1 percent in 2008. There are signs that this increase may have slowed, however, because between 2005 and 2008 there was no significant change in binge drinking across all services. The binge drinking rate in the Navy increased from 41.7 percent to 47.8 percent between 2005 and 2008 and from 33.9 percent to 39.0 percent in the Air Force, but no other service saw a significant change in binge drinking between 2005 and 2008. In 2008 the Marine Corps had the highest rate of binge drinking (57.6 percent) (Bray et al., 2009).
Compared to civilians, military personnel binge drink at a higher rate (45.8 percent versus 40.6 percent), and the difference is slightly more pronounced among those 18 to 25 years old (52.4 percent [95% CI 49.6–55.2 percent] in the military versus 44.9 percent [95% CI 44.2–45.6 percent] among civilians). Civilians aged 46 to 64, however, binge drink at a higher rate than service members of the same age (24.6 percent [95% CI 22.9–26.3 percent] versus 18.0 percent [95% CI 15.9–20.1 percent) (Bray et al., 2009).
In the Army, incidents of drug and alcohol abuse in soldiers increased from 28,740 offenses in 2006 to 34,586 in 2009 and then decreased by 9.1 percent to 31,617 offenses in 2010 and by another 4 percent to 29,708 in 2011 (Department of the Army, 2012). Those recent decreases were coupled with increased rates of referral for drug and alcohol treatment. In fiscal year (FY) 2010, there were more than 24,000 referrals of soldiers to the Army Substance Abuse Program; about 50 percent of those referred were enrolled. Forty-three percent of active-duty Army personnel reported binge drinking within the preceding month. Although 12 percent of soldiers reported alcohol problems on the Post Deployment Health Re-Assessment (see Appendix F), only 2 percent have been referred for further evaluation or treatment. Alcohol abuse is associated with several risk factors related to combat service, such as exposure to the threat of death or injury, witnessing atrocities, depression and PTSD symptoms, and a diagnosis of PTSD (Burnett-Zeigler et al., 2011; Department of the Army, 2012; Spera et al., 2011; Wilk et al., 2012).
Illicit Drugs
According to self-report data, the illicit drug use rate (excluding prescription drugs) among active-duty military was 2.2 percent in 2008 and has remained unchanged since 2002 (Bray et al., 2009). Across services, usage rates range from 3.2 percent (Army and Marine Corps) to 0.07 percent (Air Force). Deployment seems to be a factor in illicit drug usage rates. In the Army, Marine Corps, and Air Force, rates of illicit drug use (excluding prescription drugs) were significantly higher in personnel deployed to combat theaters other than OEF and OIF than in those deployed to OEF and OIF or those not deployed. Illicit drug use, including prescription drugs, among active-duty personnel increased from 5.0 percent in 2005 to 12.0 percent in 2008 (Bray et al., 2009).
Status of Drug Use in the Department of Defense Personnel: Fiscal Year 2008 Drug Testing Statistical Report (DOD, 2009a) indicates that, according to DOD drug testing data, from FY 2004 to FY 2008 illicit drug use rates were below 2 percent in active-duty forces. Rates were
also below 2 percent in reserve personnel not on active duty, but they exceeded 2 percent in National Guard personnel not on active duty. Drugs tested for included amphetamines, cocaine, ecstasy, marijuana, MDA (methylenedioxyamphetamine), opioids, and phencyclidine.
Illicit drug usage (excluding prescriptions) is lower among active-duty service members than among civilians for all age groups and overall (2.2 percent among active-duty versus 12.0 percent among civilians) (Bray et al., 2009).
Prescription Drugs
A recent Army report, Army 2020 Generating Health and Discipline in the Force Ahead of the Strategic Reset (Department of the Army, 2012), notes that pain is a leading cause of disability and states that 47 percent of soldiers returning from OEF and OIF have reported problems associated with pain. About 14 percent of U.S. soldiers have been prescribed opiate pain medications, and about 25 percent to 35 percent of wounded soldiers are addicted to prescription pain medications or illegal drugs. The report defines polypharmacy as the use of four or more prescription medications of which at least one is a psychotropic drug or a controlled substance, and it notes that the number of soldiers receiving polypharmacy increased in FY 2010–2011 from 141,199 to 160,175.
Since 2002 prescription drug misuse has increased dramatically across services—from 2 percent in 2002 to 4 percent in 2005 to nearly 12 percent in 2008 (Bray et al., 2009). Bray et al. (2009) found much higher rates of prescription drug misuse among active duty military personnel (11.7 percent) than among 18- to 65-year-old civilians (4.4 percent). By service, the Army had the highest rate of prescription drug misuse (15.7 percent), and Air Force had the lowest (7.7 percent).
Risk Factors
In reviewing the literature on alcohol misuse among active-duty service members, Returning Home from Iraq and Afghanistan (IOM, 2013a) found that heavy alcohol use was higher among those deployed to any operational theater than among the non-deployed. Other risk factors for increased alcohol use or misuse among active-duty service members include perceived high work stress, being younger, being male, experiencing the threat of death or injury, higher frequency of deployment, greater cumulative time deployed, and diagnosis of PTSD.
Among Army service members, being age 45 or older, male, smoking cigarettes, having a substance use disorder, being a victim of preadolescent sexual abuse (among women), having a major psychiatric disorder, prior legal problems, a history of motor vehicle accidents, and poor family support were all risk factors for misuse of opioids (Department of the Army, 2012).
Among recently returned National Guardsmen, Burnett-Zeigler et al. (2011) found that being male, being younger, and reporting symptoms of depression and PTSD were risk factors for meeting the criteria of alcohol misuse. National Guardsmen frequently reported that stigma and concerns about their military careers were barriers to their seeking treatment. Looking at risk factors by deployment phase, Ferrier-Auerbach et al. (2009) found that among the National Guard prior to deployment, younger, single soldiers drank and binged with more frequency and drank greater quantities than older, married Guardsmen. However, psychological health status was not a predictor of drinking among the pre-deployed National Guard. Among post-deployed National Guardsmen, Kehle et al. (2012) reported that at 3 to 6 months following deployment,
about 13 percent had alcohol use disorder diagnoses; 38 percent of these were diagnosed after returning from deployment. PTSD symptom severity was a predictor for alcohol-use disorder in the study population.
Substance Use Disorders and Comorbid Conditions
Substance use disorders (SUDs) frequently appear together with other psychological health conditions. Seal et al. (2011) found that among veterans with an alcohol use disorder, a drug use disorder, or both disorders, more than 80 percent had at least one other co-occurring psychological health diagnosis (PTSD, depression, anxiety, or adjustment disorder). Additionally, Stecker et al. (2010) found that alcohol misuse or abuse, sleep problems, pain, and aggression commonly co-occurred with PTSD or depression among OEF/OIF vets and service members deployed to Iraq. Nazarian et al. (2012) reported that among 62,496 men and 11,224 women who were OEF OIF veterans, more than half of those with substance use disorders (12.5 percent for men, 6.2 percent for women) were comorbid with PTSD (8.1 percent for men, 3.8 percent for women).
Suicide and Suicidal Ideation
Suicide is a lethal self-inflicted action, a suicide attempt is a nonfatal action, and suicidal ideation refers to suicidal thoughts, such as wishing to commit suicide. Suicide is a leading—as well as a growing—cause of death among U.S. service members (Ramchand et al., 2011; Trofimovich et al., 2012). DOD’s suicide rate in 2011 was 18.03 deaths per 100,000, up from 11.3 per 100,000 in 2005, a 60 percent increase (DCOE, 2012a). The Army, with 22.90 suicides per 100,000 in 2011, has the highest rate among the services. In the U.S. general population, the age-adjusted suicide rate in 2011 was 12.0 deaths per 100,000 (Hoyert and Xu, 2012).
It is difficult to determine the percentage of people who have suicidal ideation who go on to attempt or complete suicide. However, in a 2010 study of suicidal ideation and suicide attempts in a large number (52,780) of active-duty members of the Air Force, Snarr et al. (2010) found that 3 percent of the male and 5.2 percent of the female study participants reported suicidal ideation in the previous year, and 8.7 percent of those who reported suicidal ideation also reported a recent suicide attempt.
Risk Factors
Risk factors for suicidal ideation among active-duty male personnel in the Air Force include not being married, being non-Christian, being junior enlisted, being employed as medical personnel, having alcohol problems, working longer hours, having poor social support, being dissatisfied with relationships, having poor coping ability, having experienced interpersonal violence, and being dissatisfied with the Air Force way of life. Among Air Force women, risk factors include lower rank, financial stress, alcohol problems, relationship dissatisfaction, interpersonal violence, poor social support, and being non-Christian. Among both sexes, depression was the strongest predictor of suicidal ideation. Reservists deployed to OEF/OIF were more likely to report more severe psychological health issues, suicidal ideation, and suicide attempts than those who were not deployed or those who were deployed to other theaters (IOM, 2013a).
Langhinrichsen-Rohling et al. (2011) examined risk factors for suicidal ideation at four ecological levels (individual, family, workplace, and community) among a large cohort (N=52,780) of active-duty Air Force men and women. At the individual level, depressive symptoms and alcohol problems were both risk factors for suicidal ideation. For mothers in the study population, however, alcohol problems actually decreased the risk of suicidal ideation. At the family level, relationship satisfaction reduced the risk of suicidal ideation, and interpersonal violence victimization increased the risk. For mothers, parent–child relationship satisfaction also reduced the risk for suicidal ideation. At the workplace level, dissatisfaction with the Air Force way of life was a strong predictor of suicidal ideation among men, and satisfaction with workplace relationships reduced the risk of suicidal ideation among women. At the community level, social support reduced the risk of suicidal ideation among both men and women. A perception of community unity was protective for men. The authors suggest that focusing on the non-individual and less-stigmatizing risk and protective factors at the workplace and community levels may be an effective strategy for the military’s suicide prevention efforts (Langhinrichsen-Rohling et al., 2011).
At least 90 percent of people who die by suicide have a psychological illness at the time of their death. The most common is major depressive disorder, followed by SUD (Moœcicki, 2001). Risk factors for completed suicide among service members include being male, white, under the age of 25 years, junior enlisted or high-school educated, and divorced. (The suicide rate in divorced service members was 55 percent higher than that in married service members.) Active-duty service members had a 70 percent higher risk of suicide than did deployed reserves and National Guard members. Firearms accounted for 62 percent of all suicides, and drug overdose was the most frequent method of suicide attempts (57 percent) (DCOE, 2011).
DOD data illustrate the relationship between psychological health disorders and suicide attempts. Among service members who attempted suicide in 2011, a majority (64.6 percent) had a history of psychological illness (DCOE, 2012a). Among suicide attempters, 34.4 percent reported a mood disorder; 26 percent had an anxiety disorder, most frequently PTSD; and 27 percent had a history of substance use (DCOE, 2012a).
A new study points to a similar pattern among suicide completers. Among the Millennium Cohort, a large longitudinal sample of service members, the leading risk factors for suicide were depression, manic depressive disorder, and heavy or binge drinking or alcohol-related problems (LeardMann et al., 2013b). The study did not find an association between suicide and combat experience, cumulative days deployed, or number of deployments; however, the study did have some limitations, such as its self-report methodology, its definition of combat exposure, and a 31 percent participation rate. The risk factors identified in this study suggest that the treatment of underlying psychiatric disorders, even though these disorders are not the only risk factor, is nonetheless a critical component of suicide prevention (Engel, 2013) and that service members who have not deployed are also at elevated risk, so they should be considered in screening and prevention efforts. The overwhelming majority of civilians who die by suicide had untreated psychiatric disorders (Henriksson et al., 2001).
An analysis of the health care experiences that preceded suicide and suicide attempts in U.S. service members during the 2001–2010 period found that 45 percent of those who died of suicide, 73 percent of those who had self-inflicted injuries, and 76 percent of the likely self-harm cohort had outpatient visits within 30 days preceeding these events. The authors speculated that there might be “triggering” events that lead to seeking health care and that people might be
screened for suicide risk in primary care (Trofimovich et al., 2012). See Chapter 4 for a description of DOD’s RESPECT–Mil program, which screens for suicide in primary care.
Protective Factors
Protective factors that make suicide less likely are not as well studied as risk factors, and most of the research on them has been carried out in civilian populations. The most recognized protective factors are social support, including strong interpersonal bonds to family/unit members and responsibility to one’s family; psychological factors, such as resilience, good impulse control, and good problem-solving skills; and psychological health treatment (Bryan and Hernandez, 2013; Nock et al., 2013; VA and DOD, 2013). In military populations, unit cohesion is one example of social support that buffers against the adverse effects of stress, the development of PTSD, and potentially suicidal behavior (Brailey et al., 2007). In a 3-year longitudinal study of veterans, resilience was found to protect against suicidal thoughts and suicide attempts (Youssef et al., 2013a). Resilience in the study was measured by the well-validated Connor-Davidson Resilience Scale, which defines resilience as being able to thrive in the face of adversity. In a related study of Iraq/Afghanistan-era military and veterans, resilience was found to be negatively associated with depressive symptoms and suicidal ideation (Youssef et al., 2013b).
PSYCHOLOGICAL HEALTH AMONG MILITARY FAMILIES2
Military family members play an integral role in the readiness and well-being of the military force. Recognizing this role, Returning Home from Iraq and Afghanistan (IOM, 2013a) examined the evidence demonstrating that military family members have to deal with impairments in psychological and physical well-being, relationship problems, responsibilities as caregivers of children or wounded service members, and overwhelming household duties. This section summarizes the findings from that report about the psychological health challenges and interpersonal violence affecting military spouses and children.
Evidence suggests that military service by itself does not appear to significantly raise the probability of negative outcomes but that the likelihood of negative consequences for families rises with the amount of the service members’ exposure to traumatic or life-altering experiences (MacLean and Elder, 2007). In contrast, deployment to combat zones has been found to significantly predict a variety of negative outcomes, including marital conflict and intimate partner violence (IOM, 2008). When service members display negative psychological symptoms, the likelihood of negative consequences for families rises substantially (de Burgh et al., 2011), and families who experience the injury or death of service members are almost certain to experience at least some negative consequences.
Family members of the National Guard and reserves face unique challenges in the degree to which they are adequately prepared for deployment, supported during deployment, assisted following deployment, and prepared for subsequent deployments, which may have an impact on their psychological health. Relative to active-duty families, members of the National Guard and
____________________
2 As stated earlier in this chapter, research on families in the literature is generally limited to heterosexual married couples and their dependent children and does not reflect the true diversity of family arrangements in modern society.
reserves and their families have limited access to military chaplains, family support programs, and all the other parts of the military landscape designed to support psychological health. Moreover, community providers may not be sufficiently aware of or sufficiently trained to fulfill their needs (DOD Task Force on Mental Health, 2007).
Psychological Health of Spouses
Every deployment consists of a before-deployment, during-deployment, and afterdeployment period, and some researchers have attempted to examine what implications each of these deployment stages has for families, particularly spouses. The duration and content of these phases vary widely, however—suggesting caution about the confidence with which predictions can be made about the implications of these stages for families. Nonetheless, for the sake of clarity it is helpful to organize the discussion on the psychological health of families according to pre-deployment, during deployment, and post-deployment.
Pre-Deployment
Before deployment, families must make legal, logistical, and emotional preparations for separation and for the possible injury or death of the deployed service member. Although it is logical that families would find this process difficult and stressful, few prospective studies of family members have been published. Returning Home from Iraq and Afghanistan (IOM, 2013a) found in the limited existing research that spouses of service members expecting deployment reported substantially elevated stress levels and depressive symptoms, although baseline levels of these problems in this population are not well documented. Warner and colleagues (2009) reported that nearly one-quarter of spouses reported mild depressive symptoms, one-half reported symptoms consistent with depression, and one-tenth reported severe depressive symptoms. Nearly all spouses (90 percent) reported “feeling lonely” and were concerned with the “safety of the deployed spouse.” Spousal communication and parenting while the spouse is deployed were also commonly cited as concerns (Warner et al., 2009).
In addition, service members who are anticipating separation expect their spouses will have difficulty coping at home during the forthcoming deployment. Approximately one-third of junior-enlisted members and members married less than 3 years indicated that their spouse would have a serious or very serious problem dealing with the deployment (Spera, 2009).
During Deployment
Several studies have examined the prevalence of psychological symptoms among military spouses in relation to deployment-related stressors. In its review of the literature, Returning Home from Iraq and Afghanistan (IOM, 2013a) found that deployment to a war theater is associated with increased psychological health problems, particularly depression and anxiety, among military spouses. The length of the deployment and the cumulative months of deployment predict increases in the likelihood of distress, but the number of deployments does not. Additionally, a service member’s psychological issues are related to increases in marital distress, relationship problems, and disruptions to family life.
Eaton et al. (2008) studied more than 700 spouses of active-duty service members who sought primary care at military facilities. The spouses and service members reported similar levels of major depression or generalized anxiety disorders (19.5 percent and 15.6 percent,
respectively). Spouses were more likely than service members, however, to seek care (70 percent versus 40 percent) and less likely to be impeded in doing so by worries about stigma.
Mansfield et al. (2010), in an analysis of medical records of more than 250,000 military wives found that wives whose husbands were deployed were significantly more likely to have diagnoses of depression, anxiety, acute stress reaction, adjustment disorders, and sleep disorders than wives whose husbands had not been deployed. Compared with wives of non-deployed partners, spouses of deployed service members also used psychological health services at higher rates, which increased with deployment length. The likelihood of any psychological health diagnosis was 19 percent higher among women whose husbands had been deployed from 1 to 11 months (41.3 excess cases/1,000) and 27 percent higher among women whose husbands had been deployed longer than 11 months (60.7 excess cases/1,000).
A study by SteelFisher et al. (2008) revealed similar patterns. Spouses who experienced deployment extension reported increased levels of psychological health problems relative to those who did not. Half of the spouses reported frequent feelings of anxiety, and almost half reported frequent feelings of depression. In a sample of 332 National Guard members and 212 partners, Gorman et al. (2011) found that 40 percent and 34 percent, respectively, met screening criteria for one or more psychological health problems. Two small studies focused on spouses’ stress and on coping with the demands of their service members’ military duties. In one of these, spouses evaluated their partners’ deployment as one of the most stressful experiences of recent years in their lives (Dimiceli et al., 2010). In turn, spouses’ perceived stress was negatively related to their levels of well-being (Padden et al., 2011) and their psychological symptoms (Dimiceli et al., 2010). Consistent with the broader literature on stress, coping strategies focused on problem solving, and taking action appeared to predict better psychological health (Dimiceli et al., 2010; Padden et al., 2011).
Post-Deployment
Just as families must adjust to life with one spouse deployed, so too must they readjust when the service member returns from deployment. Adjustments and readjustments can include the reassignment of parental duties and roles, financial management, and household chores (Bowling and Sherman, 2008; Pincus et al., 2001). Sahlstein et al. (2009) found that communication between spouses was helpful in returning the family structure to its predeployment state. Couples who maintained open communication and offered mutual support during the deployment returned to normal more quickly than those who did not.
Psychological Health of Military Children
Children in military families have the advantage of a number of resources that help to buffer them from risks that many non-military children might experience (Sheppard et al., 2010). Resources for military families can include access to child care and health services, housing, schools, sports and recreation facilities, and support services. (The specific resources available depend on whether the service member is in the active component, National Guard, or reserves.) On the other hand, military children may also have to cope with circumstances specific to military families, such as frequent relocations, parents leaving for and returning from deployments (which can be unexpected, prolonged, and repeated), and the medical, psychological, and economic consequences of deployment without access to enhanced services.
Overall, psychological health visits for military children rose dramatically from 2003 to 2008. Inpatient days for military children rose 50 percent, and appointments for psychological health problems rose by more than 85 percent per capita during that period (IOM, 2010). Gorman et al. (2010) reported that psychological health clinical visits for military children rose when the father was deployed. When the mother was deployed, however, psychological health–related visits declined. The older the child was, the more likely he or she was to seek psychological health treatment. This was true no matter which parent was deployed.
During a parent’s deployment, military children make more outpatient and well-child visits to TRICARE providers. However, children of young single parents had fewer visits to TRICARE during deployment than during pre-deployment (Eide et al., 2010). The authors of that study speculate that, during deployment, children of single parents may be with non-military caretakers who are not familiar with or do not have easy access to the military health care system.
Research on OEF and OIF and previous conflicts suggests that deployment is associated with a variety of internalizing (e.g., sadness, depression, and anxiety) and externalizing (such as aggressiveness and irritability) symptoms in military children which in many cases are not clinically significant (Cozza et al., 2005; Lincoln et al., 2008; Sheppard et al., 2010). Longer cumulative deployment time has been associated with more problems. Some research suggests that children of deployed parents experience emotional and behavioral symptoms at a greater rate than the population as a whole and at a greater rate than military children whose parents are not deployed. Much of this research, however, is limited in design (convenience samples, serviceseeking samples, cross-sectional), and further investigation is needed to understand the full impact of deployment on children’s psychological health (Chandra et al., 2010a; Chartrand et al., 2008; Lester et al., 2010; Mansfield et al., 2011).
Children may also have psychological symptoms when the well-being of their custodial parent is compromised. Research has consistently found that the impact of parental wartime deployments on military child adjustment is related to family functioning, perceived support, and parent–child relationships (e.g., communication, parenting) (Chandra et al., 2010a; Gewirtz et al., 2011) in addition to the well-being of both the at-home caregiver (Chandra et al., 2010b) and the service member during reintegration (Lester et al., 2010). Chartrand et al. (2008) found that not only did spouses of deployed service members with children have significantly higher depression scores than spouses of non-deployed personnel, but their young children also exhibited increased behavioral symptoms compared to their peers without a deployed parent. Children with one deployed parent also have reported that helping their caregiver “deal with life” without their deployed parent was one of the most difficult aspects of the deployment (Chandra et al., 2011). Similarly, parents having difficulty coping emotionally with deployment were more likely to report that their children were having emotional problems as well. Families who access military support services, however, report fewer child psychological problems than those who do not seek services.
Reed et al. (2011) looked at risky behaviors among adolescents with military parents. The authors found that adolescents with one deployed parent were more likely to report binge drinking than their counterparts without military parents. Older boys (10th and 12th grade) with military parents (deployed or not deployed) were more likely to report thoughts of suicide. Older boys and older girls with deployed parents were more likely to report a depressed mood than boys and girls of the same age without military parents. Similarly, Gilreath et al. (2013) found
that adolescents with a parent that had deployed at least once in the previous 10 years were more likely to report using alcohol, tobacco, marijuana, and other drugs in their lifetime or in the previous 30 days.
Using community-based survey data, Cederbaum et al. (2013) compared the psychological health of adolescents with parents or siblings in the military to the psychological health of adolescents without a family military connection. The study was conducted as a special module of the biennial state-wide California Healthy Kids Survey of public school students. Of 14,299 7th-, 9th-, and 11th-grade adolescents, more than 13 percent had a parent or sibling in the military. This group was more likely than those without a military connection to experience depressive symptoms and suicidal ideation. Deployment, in particular, had a noticeable impact. Multivariate analyses found a higher likelihood of feeling sad or hopeless for those with one family member deployed (odds ratio [OR] = 1.40, 95% CI, 1.24–1.59) or two or more family members deployed (OR = 1.56, 95% CI, 1.34–1.83) versus those with no family deployments. Likewise, there was an increased likelihood of depressive symptoms among those reporting one deployment (OR = 1.15, 95% CI, 1.00–1.33) and two or more deployments (OR = 1.41, 95% CI, 1.26–1.58). The study concluded that there is a need to screen military-connected adolescents for psychological health issues, especially during times of warfare.
In a meta-analysis, Card et al. (2011) reviewed 16 studies that examined maladjustment among children of deployed parents. Of those, five reported associations between parental deployment and academic adjustment. Overall, the analysis revealed that parental deployment is associated with slightly poorer academic outcomes among pre-adolescent children. However, the authors were unable to confidently comment on the strength of that association, due to the heterogeneity of the reviewed research.
Parental injury can take a toll on a child’s emotional well-being; however, families with a high level of stress before the injury tend to be more distressed following the injury than those with lower levels of pre-injury distress (Cozza et al., 2010). Research is sparse on the impact of military death on military children; however, available data indicate that a bereaved child is at increased risk for psychiatric disorder and behavioral and emotional problems. Parental death that occurs during a long deployment can trigger maladaptive cognitions or omens, regret, and self-blame. In cases of suicide, the feelings of guilt, anger, shame, confusion, and rejection can be magnified (Cohen and Mannarino, 2011).
Family Violence
This section addresses the problem of interpersonal violence within military families, which includes intimate partner violence and child maltreatment.
Intimate Partner Violence
In 2011 the rate of substantiated incidents3 of spousal abuse in DOD was 11.1 per 1,000 couples (DOD, 2012b). This rate extends an upward trend that began in FY 2009. Before then, from FY 2001 to FY 2008 the rate had been declining. The data are compiled annually by DOD’s Family Advocacy Program (FAP), which was created in 1984 to identify, prevent, and treat family violence in the military. Because each report of spousal abuse reflects a single
____________________
3 A “substantiated incident” is one that the DOD Family Advocacy Program believes to have occurred.
incident, there can be more than one report for a single victim. The abuser can be an active-duty service member or a civilian.
Physical abuse accounts for 90 percent of spousal abuse cases, emotional abuse accounts for 6 to 8 percent, sexual abuse accounts for 0.5 percent, and neglect accounts for 0.4 percent (Rentz et al., 2006). Two-thirds (67 percent) of abusers are male, and one-third (33 percent) are female (DOD, 2012b). In FY 2011 there were 18 fatalities tied to spousal abuse (DOD, 2012b). The occurrence of spousal abuse, as compiled by the FAP, is probably an underestimate: Incidents often go unreported out of concern for the career implications for the active-duty service member or because of the victim’s concerns about his or her physical safety. The figures are also underestimated because the DOD database of law-enforcement cases of abuse—the Defense Incident-Based Reporting System—includes only the minority of cases that rise to the level of a crime.
In a recent report the Centers for Disease Control and Prevention (CDC) assessed the prevalence of sexual and physical violence by an intimate partner among active-duty women and the wives of active-duty men and compared these groups with the general population (Black and Merrick, 2013). Women in the general population were more likely to experience lifetime sexual violence by an intimate partner (20.0 percent) than were active-duty women (12.5 percent) or wives of active-duty men (13.3 percent). Women who were deployed at least once in the 3 years prior to the survey were no more likely to be the victims of contact sexual violence by an intimate partner than those who were not deployed. Similarly, wives whose husbands had deployed at least once within the previous 3 years were no more likely to have experienced contact sexual violence by an intimate partner than wives whose husbands had not deployed.
According to the CDC report, in the general population nearly 36 percent of women aged 18 to 59 have experienced physical violence by an intimate partner at some time in their lives. Active-duty women and wives of active-duty men had lower rates of physical violence by an intimate partner, according to the study (28.4 percent and 26.9 percent, respectively). Women deployed in the 3 years prior to the survey were significantly more likely to have experienced lifetime physical violence by an intimate partner than those who had not deployed (32.2 percent and 23.9 percent, respectively) (Black and Merrick, 2013).
Risk Factors
In its review of the literature, Returning Home from Iraq and Afghanistan (IOM, 2013a) found that deployment and substance use were risk factors for spousal aggression among activeduty military service members (Martin et al., 2010; Merrill et al., 2004). Substance abusers were more likely to be physically violent and to exert more severe spousal abuse than those who were not substance abusers. That committee also found that deployment length was a factor. Deployments shorter than 6 months did not increase the risk of spousal aggression, but longer deployments did (McCarroll et al., 2010). Research has shown that among veterans and Navy recruits, PTSD is a risk factor for spousal violence or (Merrill et al., 2004; Taft et al., 2009).
In a review of intimate partner violence research among military veterans and active-duty service members, Marshall et al. (2005) found that alcohol use problems, depressive symptoms, having experienced childhood trauma, and low relationship satisfaction were all correlates of intimate partner violence perpetration.
In the only study reported in Returning Home from Iraq and Afghanistan (IOM, 2013a) that looked at spousal abuse specifically among OIF and OEF service members, experiential avoidance—a coping strategy that seeks to avoid emotionally painful events—was associated with physical aggression perpetration and victimization among 49 male National Guard members who had returned from deployment to Iraq (Reddy et al., 2011).
Child Maltreatment
Although it has been increasing since 2009, the rate of child maltreatment among military children stood at only 5.8 per 1,000 children in 2011, which is approximately half the rate of the general population (DOD, 2012b). Emotional abuse accounted for 71 percent of all cases, physical abuse for 23 percent, and sexual abuse for 6 percent. More than half (54 percent) of the abusers were male; 45 percent were female. In FY 2011, 33 military children died from child maltreatment. Although rates are not as high as in the general population, Gibbs et al. (2007) suggest that the overall rates of child maltreatment (notably neglect) by the non-deployed parent appear to rise during deployment. In that study the rate of child maltreatment was 42 percent higher during a deployment cycle with one parent absent then when both parents were home. Another study by Rentz et al. (2007) found that the risk for child maltreatment during reintegration was elevated to the same degree as during deployment.
SCREENING AND SURVEILLANCE IN THE MILITARY
Risk identification in the military occurs in different ways at various points in the military life cycle. (The military life cycle is explained in Chapter 2; see Figure 2-3.) The approaches by which the military assesses the psychological health of its service members—universal screening, strategies for psychological health integration, and self-assessment—are described below. This section includes a discussion of the evidence for the effectiveness of these strategies, which are important because they set the stage for interventions that can prevent or mitigate negative psychological health outcomes. The section concludes with an overview of new clinical practice guidelines for the assessment and management of individuals at risk for suicide which are intended to encourage optimal evidence-based care.
Screening
The screening of service members for psychological health problems occurs during four different phases: accession, pre-deployment, post-deployment, and reintegration (see Figure 2-3 in Chapter 2). Although it is less focused on psychological health, the Periodic Health Assessment is discussed at the end of this section.
Accession
Accession—that is, entrance into the uniformed services—provides an opportunity to screen potential service members for potential psychological health issues. Certain learning, behavioral, and psychological conditions are considered disqualifying for military service. As part of the medical examination of applicants that is conducted at Military Entrance Processing Stations (MEPS), two screening questionnaires are used to identify potential markers of psychological and behavioral dysfunction that would be incompatible with military service. Applicants complete the Report of Medical History (DD 2807-1) and the Supplemental Health
Screening Questionnaire (USMEPCOM Form 40-1-15-1-E) (see Appendix C), which are reviewed by DOD clinicians in making determinations about the acceptability of applicants for military service. To augment the limited number of psychological health questions on the Report of Medical History, the Supplemental Health Screening Questionnaire includes12 questions regarding the enlistee’s psychological health history. The form contains questions about recent and lifetime depression, alcohol use (using the AUDIT-C screener), self-harm history, suicidal ideation, sleep patterns, and arrest history. In addition to these screens, lab tests for drugs and alcohol are performed.
The latest screening tool used in the medical assessment, the Omaha 5, is a set of questions regarding certain key behavioral areas that MEPS providers ask during brief interviews with applicants. The Omaha 5 questionnaire includes questions about encounters with law enforcement, school authority, and psychological health professionals; self-mutilation; and home environment. These questions have not been independently validated as predictors of psychological health problems, military success, or any other endpoint (DOD, 2013e). After the applicant interview, the provider determines whether to recommend a psychological health consult based on the applicant’s answers.
Applicants with conditions that do not meet DOD standards for enlistment as outlined in DOD Instruction 6130.03 are disqualified from service. Disqualifying psychological conditions include (with exceptions in some cases) attention deficit disorder, developmental disorders, bipolar disorder, depressive disorder, speech disorders, obsessive-compulsive disorders, schizophrenic disorders, a history of suicidal behavior, eating disorders, alcohol or drug dependence or abuse, and other psychological disorders not mentioned that the examining clinician feels may interfere with satisfactory performance of military duties. The services have the authority to waive medical standards on a case-by-case basis (DOD, 2010). In FY 2009, of 296,000 accessions into service there were 1,178 psychological health waivers granted—127 for anxiety, 32 for depression, 182 for personality disorder, and 19 for PTSD (DOD, 2010).
The committee believes it is important to recognize the potential unintended consequence of elevated risk and the potential for adverse outcomes for cases in which psychological health waivers are granted. In addition, it is unclear to the committee whether information collected through the accession screening process about an enlistee’s non-disqualifying psychological issues is in any way used to target prevention interventions if an enlistee’s responses suggest a heightened risk for any negative psychological health outcomes.
Preexisting Psychological Conditions
DOD’s accession process for assessing the psychological health of recruits relies on the applicants’ knowledge of and willingness to disclose symptoms and conditions. Applicants have a strong incentive to appear qualified and therefore may withhold information, which has resulted in frequent psychological health conditions presenting during recruit training (DOD, 2013e; Gubata et al., 2012). That said, DOD’s reliance on self-report screens for psychological health history and symptoms is not unique, as practitioners and health systems rely on the same screens with the same shortcomings in the civilian world.
Studies conducted by the DOD’s Accession Medical Standards Analysis and Research Activity have shown that the majority of discharges for conditions that existed prior to service (EPTS) are for medical conditions that were not disclosed at the time of application for service.
EPTS records for active-duty, reserves, and National Guard members show that psychiatric discharges were the most common cause of EPTS discharges in the Army and in the Marine Corps, accounting for 29.6 percent and 43.3 percent of all EPTS discharges, respectively. Psychiatric discharges are the second most common cause of EPTS discharge in the Navy, accounting for 11.1 percent of discharges, while they accounted for less than 1 percent of all EPTS discharges from the Air Force. The authors note any comparisons across services should be made cautiously as these differences in EPTS discharge rates may be due in part to differences in how each service categorizes and reports EPTS discharges for psychiatric conditions (DOD, 2013e).
There is debate over the relationship between preexisting psychological conditions and an individual’s vulnerability to negative outcomes in times of stress (Warner et al., 2011b). Research into the effects of prior psychological health issues on successful military service is ongoing. Screening tools have been and are being piloted; however, to date there are insufficient data to determine whether these tools have any predictive value in determining the ability of a recruit to complete a successful tour of duty (Blakeley and Jansen, 2013).
Although research has been limited, studies have revealed that enlistees may enter the military with elevated rates of some psychological health disorders. Warner et al. (2007) examined a sample of about 1,000 Army service members in basic training and found higher depression levels than in the general population. More than one-third of all participants reported at least some depressive symptoms, with 16 percent of all participants reporting depressive symptoms consistent with a diagnosis of major depressive disorder. In the general population, lifetime depression prevalence is 7 to 12 percent. More than 25 percent of participants reported a history of verbal abuse (22.4 percent male; 46.7 percent female), and nearly 6 percent reported a history of sexual abuse (3.2 percent male; 24.4 percent female). Histories of verbal abuse and of psychiatric treatment were found to significantly increase the risk of moderate depression among participants (Warner et al., 2007). The study suggests that enlistees may have higher rates of depression than is found in the general population and may be entering the military with an elevated risk for depression or other psychological health outcomes.
As discussed earlier in the chapter, service members with depression are at increased risk for suicide. Although it did have some methodological limitations (see suicide section), a recently published study of 151,560 current and former service members in the Millennium Cohort found no association between deployment, combat, cumulative days deployed, or number of deployments and an increase in the risk of dying by suicide (LeardMann et al., 2013b). Indeed, the risk factors for suicide in this population were found to be quite similar to those in the general population: being male, being depressed, having manic depressive disorder, and having alcohol-related problems. The authors speculate the increased rate of suicide among service members may be the product of an increased prevalence of psychological disorders caused by general occupational stress in the military (deployment or otherwise). The study did not, however, investigate the timing of the onset of risk factors and symptoms. It is therefore plausible that psychological health disorders or other risk factors for suicide were present in some service members at enlistment. Regardless of when the risk factors arise, the authors suggest that the current DOD and VA prevention initiatives with the greatest potential to mitigate suicide risk are those “that address previous psychological health disorders and involve screening and facilitation of high-quality treatment for psychological and substance use disorders in primary care, specialty psychological health care, and postdeployment settings” (LeardMann et
al., 2013b, p. 503). The Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS), a study of suicide risk and resilience factors in the military being carried out through the National Institute of Mental Health, is the largest and most comprehensive such study to date, and it should provide additional insights into the issue of risk stratification in the coming years.
In a study of 4,529 male soldiers who had not deployed to Iraq and 2,392 male soldiers who had, Cabrera et al. (2007) looked at how well adverse childhood experiences predicted future psychological health outcomes. For the purposes of the study, adverse childhood experiences included exposure to a psychologically ill person in the home, exposure to an alcoholic adult in the home, sexual abuse, physical abuse, psychological abuse, and violence directed against the respondent’s mother. Approximately 53 percent of soldiers who had not deployed reported at least one adverse childhood experience, and 29 percent reported exposure to two or more. Deployed soldiers reported similar rates: 54 percent reported at least one adverse childhood experience, and 31 percent reported two or more. It is unclear if these rates are significantly different from those in the civilian population. For pre- and post-deployment samples, the authors found that the individuals who reported two or more traumatic childhood experiences were more likely to screen positive for depression and PTSD. Regression analysis results showed that although both adverse childhood experiences and combat were predictors of PTSD and depression, adverse childhood experiences were the stronger predictor of the two (Cabrera et al., 2007).
These findings further support the suggestion that pre-military experiences can affect psychological health outcomes in individuals after they join the military, indicating that these experiences should be among the risk factors considered for screening and prevention.
Pre-Deployment
All DOD service members expected to deploy for 30 days or longer must complete the Pre-Deployment Health Assessment (PreDHA) (see Appendix D). This assessment evaluates current physical and psychological health status, health behaviors, and treatment history. In the first stage of the PreDHA the service member completes an initial questionnaire, which includes several psychological health screening questions: the PC–PTSD screen for PTSD, the PHQ-2 for depression, and the AUDIT-C for alcohol use. If the service member screens positive for PTSD on the PC–PTSD tool or positive for depression according to the PHQ-2, he or she is required to complete expanded assessment tools for those conditions: the PTSD Checklist–Civilian Version (PCL–C) for PTSD and the PHQ-8 for depression. Finally, the service member meets with a health care provider to review and discuss the completed assessments face-to-face. The provider scores the completed screens and asks follow-up questions regarding suicidal ideation and violence. Based on the scores, the provider can provide brief counseling or consider referring the service member to appropriate care if he or she is not already receiving it. Based on the service member’s answers and history, the provider assesses symptom severity and determines if the service member is deployable or not, in accordance with DOD policy (DOD, 2006a).
DOD policy dictates that individuals being treated for psychotic or bipolar disorders are not deployable. Those with other psychiatric conditions are evaluated based on symptom severity, duration of treatment, stability of the condition, and level of care required. Service members taking antipsychotic medications for bipolar disorder, chronic insomnia, or psychotic conditions are not deployable. Service members taking medications that require constant laboratory monitoring (such as lithium) are also not deployable, and although some medications
for psychiatric illnesses are allowed, service members must be stable for at least 90 days prior to deployment unless a waiver is granted (Warner et al., 2011b).
One potential problem with this approach is that Nevin (2009) found the PreDHA to have low validity for identifying service members with diagnosed psychological health disorders. Using Defense Medical Surveillance System data, Nevin examined a cohort of 11,179 service members who had completed the PreDHA, 4.2 percent of whom had a recent psychological health disorder diagnosis. However, only 48.2 percent of those with a recent psychological health diagnosis answered “yes” to the PreDHA question “During the past year, have you sought counseling or care for your mental health?” This suggests the self-report nature of the PreDHA fails to accurately assess the psychological health profile of service members planning to deploy. A more accurate screen could identify service members with psychological health diagnoses and service members who are at risk of developing full-blown conditions. As an alternative to the PreDHA psychological health screening, Nevin (2009) suggests that screening the service members’ existing electronic health records for psychological health histories—rather than relying on the apparently unreliable self-reports of the service members—may offer a more accurate way to screen for psychological health disorders before deployment. This committee, however, recognizing the need to balance risk, recommends careful consideration of this approach as it could discourage service members from seeking psychological health services for fear that doing so could lead to them being deemed not-deployable. Nevin (2009) supports the suggestion that stigma associated with psychological health conditions may be driving much of the false self-reporting of service members with recent diagnoses.
Despite the apparent low validity of the psychological health screening of the PreDHA, Warner et al. (2011b) found that the psychological health screening does reduce the occurrence of psychological health problems in theater by screening out service members unfit for deployment and by identifying service members who are fit but at risk for psychological health problems and thus making it possible to monitor them while they are in theater. The authors compared three brigades that completed the PreDHA screening to three brigades that were not screened prior to deployment. The unscreened brigades were combined with a division from other posts and were not screened because of the complexity of that process, a staggered deployment schedule, and time constraints. The brigades were of comparable size, deployment history, deployment location, and combat exposure. In the first 6 months of deployment, compared to the unscreened brigades the screened brigades had fewer occurrences of combat operational stress reactions (15.7 percent versus 22.0 percent; p<0.001); psychiatric disorders (2.9 percent versus 13.2 percent; p<0.001), suicidal ideation (0.4 percent versus 0.9 percent; p<0.001), occupational duty restrictions (0.6 percent versus 1.8 percent; p<0.001), and air evacuation for psychological health reasons (0.1 percent versus 0.3 percent; p<0.05). However, the Nevin (2009) study cited above suggests that a more accurate screening tool may reduce psychological health problems in theater even further.
DOD has taken considerable steps to improve resilience and to help service members better deal with military stresses. Comprehensive Soldier Fitness, an Army-wide program designed to improve psychological health and resilience, and the Marine Corps’ Operational Stress Control and Resilience (OSCAR) are two examples of programs designed to help service members deal with stress and to help prevent negative psychological health outcomes. These programs and others, as well as the evidence of their effectiveness, are described in detail in Chapter 4.
Post-Deployment
Service members returning from deploymentmust complete a Post-Deployment Health Assessment (PDHA) (see Appendix E) in a face-to-face session with a health care provider either during in-theater medical out-processing or within 30 days following the end of a deployment. The purpose of the PDHA is to document whether the service member has developed any of the physical and psychological health issues that are common following a deployment, to document possible exposures, to identify psychological health symptoms or conditions, and to discuss any deployment-related health concerns. Positive assessments for some conditions require the use of follow-up assessment tools or referrals for further consultation.
The PDHA screens for PTSD using the four-question PC–PTSD screening tool. Whereas the PreDHA uses both the PHQ-2 and the PHQ-8 to screen for depression, the PDHA uses the two-item PHQ-2. Both tools are validated and are considered to have good sensitivity and specificity for detecting depressive disorders (Kroenke et al., 2010; Lowe et al., 2005; Smith et al., 2010). To assess alcohol use, the PDHA includes the AUDIT-C screen.
Warner et al. (2011a) found that service members are often not honest with their answers on the PDHA. Following their completion of the self-report portion of the PDHA, 2,500 Army soldiers, out of a sample of 3,502, were invited to complete an anonymous survey that included the same psychological health questions as the PDHA, demographic questions, and questions about honest reporting on the PDHA. Using demographic data from the survey (number of deployments, age, rank, sex), the researchers were able to compare the answers of the anonymous survey to the PDHA. For PTSD, 7.7 percent screened positive in the anonymous group versus 3.3 percent of the PDHA group. For depression, 7.0 percent of the anonymous group screened positive versus 1.9 percent of the PDHA group. In terms of seeking care, 8.9 percent of the anonymous group was interested versus 4.3 percent of the PDHA group. Regarding suicidal ideation, 4.7 percent of the anonymous group reported having thoughts of suicide versus 1.2 percent of the PDHA group. Although having the entire sample complete both the PDHA and the anonymous survey would have strengthened the evidence, the study suggests that some individuals filter their responses to the PDHA to conceal psychological health problems. Despite the PDHA using valid, evidence-based measures, the self-report nature of the assessment, the well-documented stigma of psychological health issues (Ben-Zeev et al., 2012; Caetano et al., 2013; Gould et al., 2007; Momen et al., 2012), and the effects that negative psychological health outcomes may have on deployment may limit DOD’s ability to identify individuals with risk factors for psychological health disorders or even to identify those individuals who have already developed full-blown psychological health disorders.
Reintegration
The Post-Deployment Health Re-Assessment (PDHRA) (see Appendix F) is completed by all deployed service members between 90 and 180 days after they have returned to their home stations. The current PDHRA, in use since September 2012, more closely resembles the PreDHA than the PDHA in that its PTSD assessment includes both the PC–PTSD and PCL-C and its depression assessment includes the PHQ-2 and PHQ-8. The alcohol abuse screening instrument is the AUDIT-C. The procedures for the PreDHA, the PDHA, and PDHRA are the same; that is, the first part is completed by the service member, and this is followed by a face-to-face session with a health care provider who asks follow-up questions, scores the assessment, and provides brief counseling or referrals, as needed.
Skopp et al. (2012a) assessed the diagnostic efficiency of the PDHRA screens for alcohol abuse, PTSD, and depressive disorder. However, the study looked at the pre–September 2012 version of the PDHRA, which used only the PHQ-2 screen for depression and the PC–PTSD screen for PTSD. The alcohol abuse screen (AUDIT-C) is the same in the current version of the PDHRA as it was in the previous version. A sample of 148 soldiers completed both the PDHRA and SCID-I diagnostic interviews (using DSM-IV criteria). Overall, the authors found the alcohol abuse, depression, and PTSD screens to have excellent negative predictive values, meaning that they were highly efficient at ruling out cases of the three conditions. The positive predictive values for the screens were low, but the authors felt that was appropriate considering the low prevalence of the conditions in the population. The authors do note, however, that the face-toface portion of the PDHRA was not evaluated and that it presents an opportunity for a health care provider to assess whether a condition is present (Skopp et al., 2012a).
Periodic Health Assessment
In addition to the above-mentioned screens, since 2006 all service members must annually complete the periodic health assessment (DOD, 2006b). Before meeting with a health care provider for the periodic health assessment, service members complete a self-administered Health Risk Appraisal (HRA). Health care providers use the completed HRA to complete the face-to-face periodic health assessment. Regarding psychological health, the HRA used by the Navy and Marine Corps includes questions on alcohol use; however, the questions differ slightly from the validated AUDIT-C screen for alcohol. Similarly, while the HRA does include a question about depression, it does not use the validated PHQ screen. The HRA does not include questions about PTSD, suicide, or any other psychological health conditions4 (Navy and Marine Corps Public Health Center, 2013) and health care providers are not required to ask follow-up questions about these conditions during the Periodic Health Assessment; however, health care providers are supposed to document any unresolved health concerns identified by previously completed Post-Deployment Health Assessments or Post-Deployment Health Reassessments (DOD, 2008).
Strategies for Integrating Psychological Health Screening
DOD is implementing structural interventions that support the improved integration of line, non-medical caregivers, and clinicians in an effort to provide early recognition and early intervention that meet the psychological health needs of service members and their families. The three efforts described below—Re-Engineering Systems of Primary Care Treatment in the Military (RESPECT–Mil), embedded mental health providers, and Patient-Centered Medical Home—represent collaborative and integrated systems of care that are intended to improve access and care coordination.
RESPECT–Mil
The U.S. Army Medical Command implemented RESPECT–Mil, which provides primary care–based screening, assessment, treatment, and referral of active-duty personnel who have PTSD or depression. DOD is implementing a tri-service expansion of the program (DCOE,
____________________
4 The committee was only able to locate the Navy and Marine Corps Health Risk Appraisal form. It is unclear to the committee if the Health Risk Appraisal form used by the other services differs from the Navy and Marine Corps Health Risk Appraisal form.
2012b). Service members who present in RESPECT–Mil clinics are screened for depression and PTSD at every visit to a primary-care provider. To screen for PTSD, the RESPECT–Mil program uses the PC–PTSD screening questions. Those who screen positive are evaluated further with the PCL–C (Department of the Army, 2010; Vythilingam et al., 2010). To screen for depression, RESPECT–Mil uses the PHQ-2 screening questions. Service members who screen positive are evaluated further with the nine-item PHQ-9 (Department of the Army, 2010; Vythilingam et al., 2010).
Data from the RESPECT–Mil program show that from February 2007, when the program began, through the end of FY 2011, 76 clinics at 31 active RESPECT–Mil sites hosted more than 1.6 million primary care visits by active-duty service members, of which 1.3 million visits—almost 80 percent—included screening for PTSD and depression. Of visits that included screening, nearly 13 percent (168,519) resulted in positive screens; 49 percent of positive screens resulted in primary care diagnoses of depression, possible PTSD, or both (DCOE, 2012b). See the section on suicide in Chapter 4 for more information about this program.
Tollison et al. (2012), citing evidence that 90 percent of patients with SUD do not seek specialty care (for which they need a referral), suggest that a similar approach of integrating SUD treatment within existing primary care systems may be helpful. DOD does not currently offer such an approach.
Embedded Mental Health Providers
In theater there are no routine required psychological health screenings, although DOD is making an effort to identify service members who display signs of psychological stress during deployment and is improving access to psychological health care. Based on a recommendation from the DOD Task Force on Mental Health (2007), all branches employ the concept of embedded behavioral health by bringing psychological health clinicians closer to service members to improve access to care, increase mission readiness, identify service members with psychological challenges as early as possible, and improve communication between psychological health professionals and operational unit leaders (Cho–Stutler, 2013). In the Marine Corps, for example, the OSCAR program attaches psychological health providers directly to units throughout the training and deployment cycles. For a more detailed description of OSCAR, see Chapter 4 of this report. As of August 2013, the Army’s Embedded Behavioral Health program had 45 embedded teams in place at U.S. and European installations with plans to expand to all deployable units by 2016 (U.S. Army, 2013).
Patient-Centered Medical Home
The Patient-Centered Medical Home (PCMH) is a team-based model that provides continuous, accessible, family-centered, comprehensive, compassionate, and culturally sensitive health care in order to achieve the best possible health outcomes. A PCMH practice is responsible for all of a patient’s health care needs and for coordinating and integrating specialty health care and other professional services. In 2008 DOD adopted the concepts of PCMH as the framework for a new primary care model in the military health system. The model focuses on the “whole person” concept, preventive care, and early intervention and management of health problems (DOD, 2011).
In August 2013 DOD released Instruction 6490.15, Integration of Behavioral Health Personnel (BHP) Services Into Patient-Centered Medical Home (PCMH) Primary Care and
Other Primary Care Service Settings (DOD, 2013b), which sets inter-service standards for adult psychological health care in primary care across the direct care system. Each military department is to establish a primary care services program that integrates psychological health personnel within 12 months of the instruction’s effective date. The instruction defines competencies, roles, and responsibilities for primary care managers (PCMs), internal psychological health consultants, and psychological health care facilitators, who work together to provide screening, assessment, treatment, and monitoring for patients at risk of, or diagnosed with, a psychological health disorder. The instruction also specifies the service delivery standards for psychological health in primary care. These include minimum screening requirements for major depressive disorder and PTSD using evidence-based screening instruments. PCMs will conduct depression screening when a new patient enters the practice, will conduct annual screening for all patients, and will screen any patient who is scored as being at a higher risk for depression as defined by the VA/DOD clinical practice guidelines on major depressive disorder. For PTSD, PCMs will screen all new patients, will screen each patient annually, and, if clinically indicated due to clinical suspicion, will screen patients with recent trauma exposure (e.g., major disaster, sexual trauma, combat) or a history of PTSD.
Self-Assessment Tools
Military Pathways
Military Pathways provides free, anonymous psychological health and alcohol self-assessments for family members and service personnel in all branches, including the National Guard and reserve (Military Pathways, 2013). The self-assessments are a series of questions that, when linked together, are designed to create a picture of how an individual is feeling and whether he or she could benefit from talking to a health professional. Military Pathways is available online, over the phone, and at special events held at installations worldwide.
According to the Military Pathways website, the primary goals of the program are to reduce stigma, raise awareness about psychological health, and connect those in need to available resources. The self-assessments address depression, PTSD, generalized anxiety disorder, alcohol use, and bipolar disorder. After an individual completes a self-assessment, he or she is provided with referral information including services provided through DOD and VA. The committee did not examine the instruments used by Military Pathways, nor did it assess the thresholds used by the program to trigger psychological health referrals. Trials to evaluate the effectiveness of the self-screening and youth program components are ongoing (Weinick et al., 2011), but the committee is not aware of published outcome or utilization data on the alcohol, PTSD, or psychological health screening components. For more about Military Pathways, see Chapter 4.
Clinical Practice Guidelines
Under the auspices of the VA/DOD Evidence-Based Practice-Guidelines Work Group, representatives of DOD and VA serve on committees for developing, updating, and implementing joint clinical practice guidelines for a number of physical health and psychological health conditions. The guidelines document evidence-based procedures for screening, assessment, diagnosis, and treatment of adults who are seen in any DOD or VA clinical setting. VA/DOD joint guidelines have been in existence for several years for TBI, PTSD, major
depressive disorder, and SUD, but the first guidelines for the assessment and management of patients at risk for suicide were not released until 2013 (VA and DOD, 2013). A summary of these new guidelines is offered below. A review of VA/DOD joint guidelines for TBI, PTSD, major depressive disorder, and SUD can be found in Returning Home from Iraq and Afghanistan (IOM, 2013a).
The committee acknowledges that the presence of clinical guidelines does not ensure that people receive optimal evidence-based care. Poor dissemination practices, the lack of uniform or quality training, and other barriers affect the extent to which clinicians use clinical practice guidelines and the fidelity of their implementation (Stein et al., 2009).
The VA/DOD guidelines addressing patients at risk for suicide are divided into four different modules: the assessment and determination of risk for suicide, including assessment of risk factors and protective factors; the initial management of the patient at risk for suicide, including determination of appropriate care setting and securing the patient’s safety, especially through restriction of lethal means; the treatment of the patient at risk for suicide, including suicide-focused psychotherapy, psychotherapy for co-occurring psychological disorders, and pharmacotherapy; and follow-up and monitoring of the patient at risk for suicide, including adherence to treatment and follow-up care strategies and continuity of care. Under each of these modules the guidelines rank the strength of the evidence.
In the assessment of suicide risk, the guidelines specific three levels—high acute risk, intermediate acute risk, and low acute risk—and advise on what action should be taken for each level. For patients with high acute risk, the guidelines advise maintaining direct observational control of patients, transferring or escorting the patient to and urgent or emergency care setting for evaluation of need for hospitalization, and documenting risk assessment.
From the VA/DOD guidelines, Figure 3-1 shows the process for assessing the risk of suicide in a primary care setting. Any person who is identified as being at possible suicide risk should be formally assessed for suicidal ideation, plans, intent and behavior, the availability of lethal means, and the presence of risk factors and warning signs. A clinical judgment that is based on all this information should include a determination of the level of suicide risk and a formulation of the care setting.
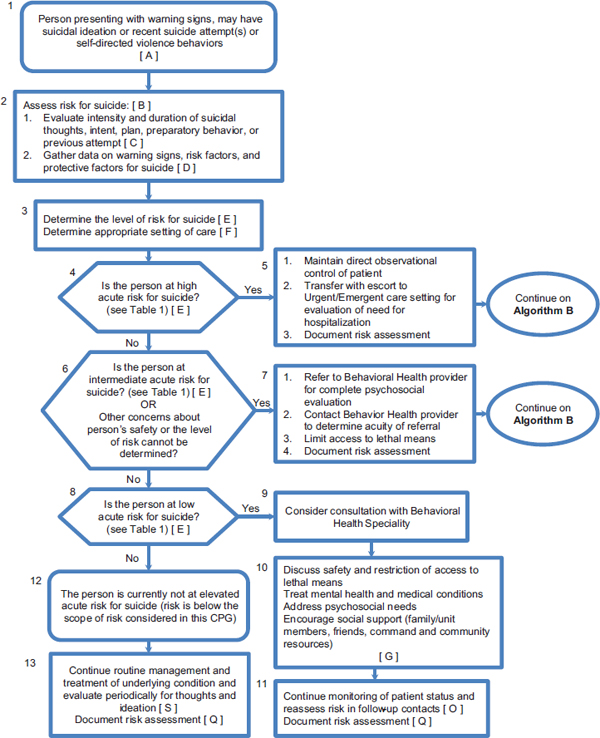
FIGURE 3-1 Algorithm A—assessment and management of risk for suicide in primary care.
SOURCE: VA and DOD, 2013.
Figure 3-2, which is taken from the VA/DOD guidelines, shows the process for the initial management of individuals identified as being at risk of suicide. The patient and provider should develop a collaboratively designed safety plan before the patient is discharged from acute care. This development should include inquiring about access to lethal means and, if possible, devising plans to restrict access to these means. The person at risk should be placed in an appropriate setting of care that provides the necessary supervision to ensure safety. Based on the assessment described, providers should implement the treatment protocol outlined in Algorithm C for high-risk suicide patients (see VA and DOD, 2010).
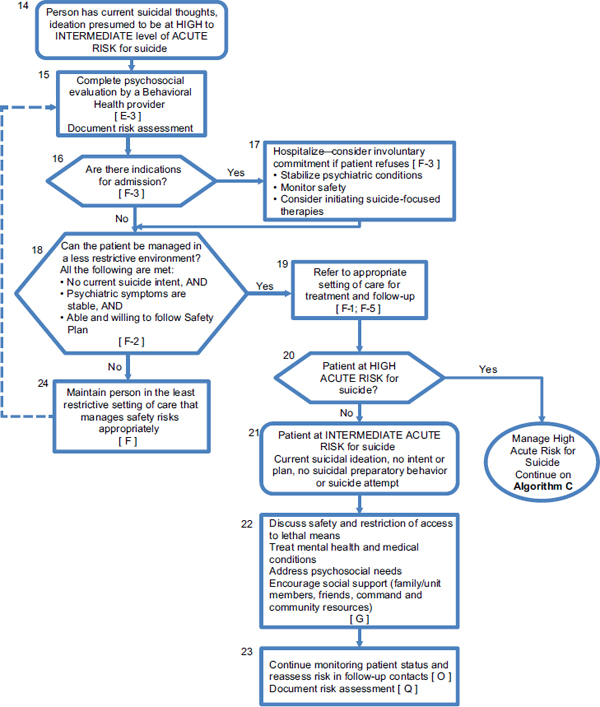
FIGURE 3-2 Algorithm B—initial management of patient at risk for suicide.
SOURCE: VA and DOD, 2013.
The new guidelines are a major step forward in suicide prevention; however, the committee is not aware of how DOD intends to promote the use of the guidelines or train clinicians on the recommendations.
PSYCHOLOGICAL HEALTH SERVICES IN THE MILITARY
Psychological health services are provided under DOD’s Military Health System, which serves 9.7 million service members, retirees, and family members. There are two broad types of care: direct care at military treatment facilities, and contract care sponsored under DOD’s TRICARE insurance plans (IOM, 2013b). Service members in a war theater have the additional benefit of an embedded psychological health professional who can perform the initial treatment for combat stress and PTSD in theater. Having embedded psychological health professionals also serves to reduce the stigma that deters soldiers from seeking and receiving psychological health care.
Under TRICARE, all of the main types of inpatient and outpatient psychological health services are available, including psychotherapy (individual, family, and groups), suicide
prevention, psychological testing, medication management, tele-mental health, acute inpatient psychiatric care, psychiatric partial hospitalization, and residential treatment. To receive psychological health services through TRICARE, active-duty service members must obtain referrals from their military hospital or clinic (DOD, 2013c). Family members and other TRICARE beneficiaries do not need referrals or prior authorization for the first eight outpatient sessions per fiscal year (DOD, 2013c). Prior authorization and limits on the number of annual days of care apply to acute inpatient care, residential treatment, and partial hospitalization (DOD, 2013c).
The costs of psychological health services vary according to the type of TRICARE plan that is selected by the service member and family. For example, TRICARE’s Prime plan functions like an HMO (health maintenance organization): TRICARE Prime has no costs using a civilian health care provider if subscribers go through their primary care provider; TRICARE’s Extra plan sponsors a preferred provider network from which subscribers can choose their providers. If the subscriber elects to use an authorized provider outside the network, additional fees and special authorizations are often required. TRICARE’s Standard plan is like a fee-for-service civilian policy, and it affords the greatest flexibility in choice of TRICARE-certified providers. Although this plan does not have premiums, the fees are higher than those of other TRICARE plans.
National Guard and reserve soldiers, when activated for at least 30 days, are eligible for the same health benefits as active-duty service members and their families (DOD, 2013d). When deactivated, National Guard and reserve soldiers and their families are eligible for only one type of plan under TRICARE. Known as TRICARE Reserve Select, the plan has monthly premiums and cost-sharing arrangements similar to those of civilian employer plans, although often at lower cost. Some members of Congress have called for having psychological health professionals embedded where National Guard and reserve troops train one weekend per month, but DOD opposes this policy as unnecessary and logistically difficult because of a shortage of psychological health providers (Zoroya, 2011).
Psychological health services provided or funded by DOD have not been without controversy. The National Defense Authorization Act for FY 2006 directed the Secretary of Defense to establish a task force to review and make recommendations about improving the efficacy of psychological health services. The task force found that psychological health professionals are not sufficiently accessible to service members and their families; that there are significant gaps in the continuum of care; that the military system does not have enough resources, funding, or personnel to sufficiently support psychological health of service members and their families in peace and during conflicts; and that psychological health stigma remains pervasive. The task force’s main recommendations were to build a culture of support for psychological health, ensure a full continuum of care for service members and families, provide sufficient resources and allocate them according to requirements (including a recommendation to ensure TRICARE networks fulfill beneficiaries’ psychological health needs), and empower leadership to advocate for psychological health (DOD Task Force on Mental Health, 2007). The committee could not find information regarding TRICARE’s implementation of these recommendations.
Being deployed to a war zone can result in numerous adverse psychological health conditions. As directed by the statement of task, the committee focused on PTSD, depression, SUDs, suicide, and interpersonal violence. Any one of these conditions can in turn have numerous sequelae and associated comorbidities that can have significant impacts on health, quality of life, and family functioning. Some of these comorbidities are complicated in nature—particularly the relationship between PTSD and TBI—and require further study to be fully understood. Others, such as chronic pain due to physical injury and its treatment, can further complicate psychological health conditions. DOD currently screens for many of these conditions at numerous points during the military life cycle. The committee is not aware, however, of any DOD health screening procedures that occur at separation. Additionally, stigma and service-related consequences, such as deployability associated with psychological health conditions and their treatment in the military, limit the usefulness of the screening instruments as many service members may not be reporting truthfully. RESPECT–Mil and embedded mental health providers are two efforts to help improve access to psychological health care and lessen the stigma associated with seeking care, but more needs to be done in this area to balance disincentives for care seeking and reporting with identifying and intervening for those at greatest risk for negative deployment-related outcomes and function.
The committee’s review of risk and protective factors in military and family populations suggests that prevention strategies are needed at multiple levels—individual, interpersonal, institutional, community, and societal—to address the influence that these factors have on psychological health. For example, there are different experiences and conditions associated with the societal environment to which members of the reserve component return as compared to the active component. Reserve component members must immediately reintegrate into civilian work places and neighborhoods, environments which may have little comprehension of the military member’s deployment experience. Active-duty members on the other hand return to a knowledgeable and relatively supportive societal environment, the military base. Thus, prevention strategies specific to this specific adjustment (risk factor) for reservists might be appropriate. For example, a program of third location decompression with additional concentrated social and psychological support for members of returning reserve units might be developed and tested.
At the institutional level, some risk and protective factors have their influence primarily at the military unit level (e.g., company, battalion). For example, service members and families who have chronic pain may be are exposed to different institutional-level risks for developing opioid addiction. A clinic within a “protective” institutional environment would be one that minimizes opioid dependence by adopting safe opioid prescribing practices that are promulgated in clinical practice guidelines and educational programs. Alternatively, other clinics may have patterns of over-reliance on opioid medications as the first-order treatment of chronic pain, and little or no adoption of safe prescribing practices. Finally, perceptions of stigma associated with having acute psychological symptoms, or a psychological disorder, and seeking professional help, is an example of an influence that operates at the relationship, social, and institutional level. Policies and strategies to change stigma could affect expression of all disorders not simply one disorder in terms of inhibiting early discussions of symptoms and distress, or early treatment seeking.
APA (American Psychiatric Association). 2013. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Publishing.
Ben-Zeev, D., P. W. Corrigan, T. W. Britt, and L. Langford. 2012. Stigma of mental illness and service use in the military. Journal of Mental Health 21(3):264–273.
Black, C. M., and M. T. Merrick. 2013. Prevalence of Intimate Partner Violence, Stalking, and Sexual Violence Among Active Duty Women and Wives of Active Duty Men—Comparisons with Women in the U.S. General Population, 2010. Atlanta, GA: Centers for Disease Control and Prevention.
Blakeley, K., and D. J. Jansen. 2013. Post-Traumatic Stress Disorder and Other Mental Health Problems in the Military: Oversight Issues for Congress. Washington, DC: Congressional Research Service.
Booth-Kewley, S., G. E. Larson, R. M. Highfill-McRoy, C. F. Garland, and T. A. Gaskin. 2010. Correlates of posttraumatic stress disorder symptoms in Marines back from war. Journal of Traumatic Stress 23(1):69–77.
Bowling, U. B., and M. D. Sherman. 2008. Welcoming them home: Supporting service members and their families in navigating the tasks of reintegration. Professional Psychology Research and Practice 39(4):451–458.
Brailey, K., J. J. Vasterling, S. P. Proctor, J. I. Constans, and M. J. Friedman. 2007. PTSD symptoms, life events, and unit cohesion in U.S. Soldiers: Baseline findings from the neurocognition deployment health study. Journal of Traumatic Stress 20(4):495–503.
Bray, R. M., M. R. Pemberton, L. L. Hourani, M. Witt, K. L. Olmstead, J. M. W. Brown, B., M. E. Lance, M. E. Marsden, and S. Scheffer. 2009. 2008 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel. Research Triangle Park, NC: RTI International.
Bryan, C. J., and A. M. Hernandez. 2013. The functions of social support as protective factors for suicidal ideation in a sample of Air Force personnel. Suicide and Life-Threatening Behavior 43(5):562–573.
Burnett-Zeigler, I., M. Ilgen, M. Valenstein, K. Zivin, L. Gorman, A. Blow, S. Duffy, and S. Chermack. 2011. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive Behaviors 36(8):801–806.
Cabrera, O. A., C. W. Hoge, P. D. Bliese, C. A. Castro, and S. C. Messer. 2007. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. American Journal of Preventive Medicine 33(2):77–82.
Caetano, R., M. S. Kaplan, N. Huguet, B. H. McFarland, K. Conner, N. Giesbrecht, and K. B. Nolte. 2013. Acute alcohol intoxication and suicide among United States ethnic/racial groups: Findings from the National Violent Death Reporting System. Alcoholism: Clinical and Experimental Research 37(5):839–846.
Card, N. A., L. Bosch, D. M. Casper, C. B. Wiggs, S. A. Hawkins, G. L. Schlomer, and L. M. Borden. 2011. A meta-analytic review of internalizing, externalizing, and academic adjustment among children of deployed military service members. Journal of Family Psychology 25(4):508–520.
Carlson, K. F., D. Nelson, R. J. Orazem, S. Nugent, D. X. Cifu, and N. A. Sayer. 2010. Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. Journal of Traumatic Stress 23(1):17–24.
Cederbaum, J. A., T. D. Gilreath, R. Benbenishty, R. A. Astor, D. Pineda, K. T. Depedro, M. C. Esqueda, and H. Atuel. 2013. Well-being and suicidal ideation of secondary school students from military families. Journal of Adolescent Health (in press).
Chandra, A., S. Lara-Cinisomo, L. H. Jaycox, T. Tanielian, R. M. Burns, T. Ruder, and B. Han. 2010a. Children on the homefront: The experience of children from military families. Pediatrics 125(1):16–25.
———. 2011. Views from the Homefront: The Experiences of Youth and Spouses from Military Families. Santa Monica, CA: RAND Corporation.
Chandra, A., L. T. Martin, S. A. Hawkins, and A. Richardson. 2010b. The impact of parental deployment on child social and emotional functioning: Perspectives of school staff. Journal of Adolescent Health 46(3):218–223.
Chartrand, M. M., D. A. Frank, L. F. White, and T. R. Shope. 2008. Effect of parents’ wartime deployment on the behavior of young children in military families. Archives of Pediatric and Adolescent Medicine 162(11):1009–1014.
Cho-Stutler, L. 2013. Staff Voices: Q & A on the Army’s Embedded Behavioral Health (EBH) Program. http://www.deploymentpsych.org/blog/staff-voices-q-army%E2%80%99s-embedded-behavioral-health-ebh-program (accessed August 29, 2013).
Cohen, J. A., and A. P. Mannarino. 2011. Trauma-focused CBT for traumatic grief in military children. Journal of Contemporary Psychotherapy 41(4):219–227.
Collins, E. M. 2012. Bringing Behavioral Health to the Troops. http://soldiers.dodlive.mil/2012/09/bringing-behavioral-health-to-the-troops (accessed August 30, 2013).
Connor, K. M., and J. R. Davidson. 2003. Development of a new resilience scale: The Connor- Davidson resilience scale (CD-RISC). Depression and Anxiety 18(2):76-82.
Cozza, S. J., R. S. Chun, and J. A. Polo. 2005. Military families and children during Operation Iraqi Freedom. Psychiatric Quarterly 76(4):371–378.
Cozza, S. J., J. M. Guimond, J. B. McKibben, R. S. Chun, T. L. Arata-Maiers, B. Schneider, A. Maiers, C. S. Fullerton, and R. J. Ursano. 2010. Combat-injured service members and their families: The relationship of child distress and spouse-perceived family distress and disruption. Journal of Traumatic Stress 23(1):112–115.
DCOE (Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury). 2011. Department of Defense Suicide Event Report: Calendar Year 2010 Annual Report. Washington, DC: National Center for Telehealth and Technology, Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury.
———. 2012a. Department of Defense Suicide Event Report: Calendar Year 2011 Annual Report. Washington, DC: National Center for Telehealth and Technology, Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury.
———. 2012b. RESPECT–Mil: Re-engineering Systems of Primary Care Treatment in the Military. Washington, DC: Defense Centers of Excellence for Psychological Health & Traumatic Brain Injury.
de Burgh, H. T., C. J. White, N. T. Fear, and A. C. Iversen. 2011. The impact of deployment to Iraq or Afghanistan on partners and wives of military personnel. International Review of Psychiatry 23(2):192–200.
Dedert, E. A., K. T. Green, P. S. Calhoun, R. Yoash-Gantz, K. H. Taber, M. M. Mumford, L. A. Tupler, R. A. Morey, C. E. Marx, R. D. Weiner, and J. C. Beckham. 2009. Association of trauma exposure with psychiatric morbidity in military veterans who have served since September 11, 2001. Journal of Psychiatric Research 43(9):830–836.
Defense and Veterans Brain Injury Center. 2013. DOD Numbers for Traumatic Brain Injury Worldwide—Totals. Silver Spring, MD: Defense and Veterans Brain Injury Center.
Department of the Army. 2010. Re-engineering Systems of the Primary Care Treatment (of Depression and Post-Traumatic Stress Disorder) in the Military Documentation Form. Sam Houston, TX: U.S. Army Medical Command.
———. 2012. Army 2020: Generating Health and Discipline in the Force Ahead of the Strategic Reset. Washington, DC: Department of Defense.
Dikmen, S. S., J. E. Machamer, D. M. Donovan, H. R. Winn, and N. R. Temkin. 1995. Alcohol use before and after traumatic head injury. Annals of Emergency Medicine 26(2):167–176.
Dimiceli, E. E., M. A. Steinhardt, and S. E. Smith. 2010. Stressful experiences, coping strategies, and predictors of health-related outcomes among wives of deployed military servicemen. Armed Forces &Society 36(2):351–373.
DOD (Department of Defense). 2006a. Memorandum: Policy Guidance for Deployment-Limiting Psychiatric Conditions and Medications. Washington, DC: Department of Defense.
———. 2006b. Periodic Health Assessment Policy for Active Duty and Selected Reserve Members. Washington, DC: Department of Defense.
———. 2008. Periodic Health Assessment NavyMed 6120/4. http://www.med.navy.mil/directives/ExForms/NAVMED%206120-4%20(Rev.%2003-2008).pdf (accessed January 7, 2014).
———. 2009a. Status of Drug Use in Department of Defense Personnel: Fiscal Year 2008 Drug Testing Statistical Report. Falls Church, VA: Office of the Assistant Secretary of Defense for Health Affairs.
———. 2009b. DOD/VA Code Proposal Final. http://www.cdc.gov/nchs/data/icd9/Sep08TBI.pdf (accessed October 30, 2013).
———. 2010. Medical Standards for Appointment, Enlistment, or Induction in the Military Services. Washington, DC: Department of Defense.
———. 2011. Military Health System Patient Centered Medical Home Guide. Washington, DC: Department of Defense.
———. 2012a. 2011 Demographics: Profile of the Military Community. Washington, DC: Department of Defense.
———. 2012b. Department of Defense Family Advocacy Program Child Abuse/Neglect (CAN) Data FY11 Report. Washington, DC: Department of Defense.
———. 2013a. Department of Defense Annual Report on Sexual Assault in the Military: Fiscal Year 2012 Volume II. Washington, DC: Department of Defense.
———. 2013b. Integration of Behavioral Health Personnel (BHP) Services into Patient-Centered Medical Home (PCMH) Primary Care and Other Primary Care Service Settings. Washington, DC: Department of Defense.
———. 2013c. TRICARE Behavioral Health Care Services Fact Sheet. Washington, DC: Department of Defense.
———. 2013d. TRICARE National Guard and Reserve Member Families. http://www.tricare.mil/reserve (accessed November 1, 2013).
———. 2013e. AMSARA: Attrition & Morbidity Data for 2012 Accessions Annual Report 2013. Washington, DC: Department of Defense.
DOD Task Force on Mental Health. 2007. An Achievable Vision: Report of the Department of Defense Task Force on Mental Health. Falls Church, VA: Defense Health Board.
Dutra, L., K. Grubbs, C. Greene, L. L. Trego, T. L. McCartin, K. Kloezeman, and L. Morland. 2011. Women at war: Implications for mental health. Journal of Trauma and Dissociation 12(1):25–37.
Eaton, K. M., C. W. Hoge, S. C. Messer, A. A. Whitt, O. A. Cabrera, D. McGurk, A. Cox, and C. A. Castro. 2008. Prevalence of mental health problems, treatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military Medicine 173(11):1051–1056.
Eide, M., G. Gorman, and E. Hisle-Gorman. 2010. Effects of parental military deployment on pediatric outpatient and well-child visit rates. Pediatrics 126(1):22–27.
Engel, C. C. 2013. Suicide, mental disorders, and the US military: Time to focus on mental health service delivery. JAMA 310(5):484–485.
Ferrier-Auerbach, A. G., S. M. Kehle, C. R. Erbes, P. A. Arbisi, P. Thuras, and M. A. Polusny. 2009. Predictors of alcohol use prior to deployment in National Guard soldiers. Addictive Behaviors 34(8):625–631.
Friedman, M. 2003. Post Traumatic Stress Disorder. Kansas City, MO: Compact Clinicals.
Fritch, A. M., M. Mishkind, M. A. Reger, and G. A. Gahm. 2010. The impact of childhood abuse and combat-related trauma on postdeployment adjustment. Journal of Traumatic Stress 23(2):248–254.
Gadermann, A. M., C. C. Engel, J. A. Naifeh, M. K. Nock, M. Petukhova, P. N. Santiago, B. Wu, A. M. Zaslavsky, and R. C. Kessler. 2012. Prevalence of DSM-IV major depression among U.S. military personnel: Meta-analysis and simulation. Military Medicine 177(8 Suppl):47–59.
Gahm, G. A., B. A. Lucenko, P. Retzlaff, and S. Fukuda. 2007. Relative impact of adverse events and screened symptoms of posttraumatic stress disorder and depression among active duty soldiers seeking mental health care. Journal of Clinical Psychology 63(3):199–211.
Gewirtz, A. H., C. R. Erbes, M. A. Polusny, M. S. Forgatch, and D. S. DeGarmo. 2011. Helping military families through the deployment process: Strategies to support parenting. Professional Psychology Research and Practice 42(1):56–62.
Gibbs, D. A., S. L. Martin, L. L. Kupper, and R. E. Johnson. 2007. Child maltreatment in enlisted soldiers’ families during combat-related deployments. JAMA 298(5):528–535.
Gilreath, T. D., J. A. Cederbaum, R. A. Astor, R. Benbenishty, D. Pineda, and H. Atuel. 2013. Substance use among military-connected youth: The California Healthy Kids Survey. American Journal of Preventive Medicine 44(2):150–153.
Gorman, G. H., M. Eide, and E. Hisle-Gorman. 2010. Wartime military deployment and increased pediatric mental and behavioral health complaints. Pediatrics 126(6):1058–1066.
Gorman, L. A., A. J. Blow, B. D. Ames, and P. L. Reed. 2011. National Guard families after combat: Mental health, use of mental health services, and perceived treatment barriers. Psychiatric Services 62(1):28–34.
Gould, M., N. Greenberg, and J. Hetherton. 2007. Stigma and the military: Evaluation of a PTSD psychoeducational program. Journal of Trauma Stress 20(4):505–515.
Grieger, T. A., S. J. Cozza, R. J. Ursano, C. Hoge, P. E. Martinez, C. C. Engel, and H. J. Wain. 2006. Posttraumatic stress disorder and depression in battle-injured soldiers. American Journal of Psychiatry 163(10):1777–1783.
Gubata, M. E., A. A. Oetting, N. S. Weber, X. Feng, D. N. Cowan, and D. W. Niebuhr. 2012. A noncognitive temperament test to predict risk of mental disorders and attrition in U.S. Army recruits. Military Medicine 177(4):374–379.
Henriksson, S., G. Boethius, and G. Isacsson. 2001. Suicides are seldom prescribed antidepressants: Findings from a prospective prescription database in Jamtland County, Sweden, 1985–1995. Acta Psychiatrica Scandanavica 103(4):301–306.
Hill, J. J., 3rd, B. H. Mobo, Jr., and M. R. Cullen. 2009. Separating deployment-related traumatic brain injury and posttraumatic stress disorder in veterans: Preliminary findings from the Veterans Affairs traumatic brain injury screening program. American Journal of Physical Medicine and Rehabilitation 88(8):605–614.
Himmelfarb, N., D. Yaeger, and J. Mintz. 2006. Posttraumatic stress disorder in female veterans with military and civilian sexual trauma. Journal of Traumatic Stress 19(6):837–846.
Hoge, C. W., A. Terhakopian, C. A. Castro, S. C. Messer, and C. C. Engel. 2007. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry 164(1):150–153.
Hoge, C. W., C. A. Castro, S. C. Messer, D. McGurk, D. I. Cotting, and R. L. Koffman. 2004. Combat duty in Iraq and Afghanistan, mental health problems and barriers to care. New England Journal of Medicine 351(1):13–22.
Hoge, C. W., J. L. Auchterlonie, and C. S. Milliken. 2006. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 295(9):1023–1032.
Hoge, C. W., D. McGurk, J. L. Thomas, A. L. Cox, C. C. Engel, and C. A. Castro. 2008. Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine 358(5):453–463.
Hosek, J. 2011. How Is Deployment to Iraq and Afghanistan Affecting US Service Members and Their Families? An Overview of Early RAND Research on the Topic. Santa Monica, CA: RAND Corporation.
Hoyert, D. L., and J. Xu. 2012. Deaths: Preliminary data for 2011. National Vital Statistics Reports 61(6):1–51.
IOM (Institute of Medicine). 2008. Gulf War and Health, Volume 6: Physiologic, Psychologic, and Psychosocial Effects of Deployment-Related Stress. Washington, DC: The National Academies Press.
———. 2009a. Combatting Tobacco Use in Military and Veteran Populations. Washington, DC: The National Academies Press.
———. 2009b. Gulf War and Health, Volume 7: Long-Term Consequences of Traumatic Brain Injury. Washington, DC: The National Academies Press.
———. 2010. Returning Home from Iraq and Afghanistan: Preliminary Assessment of Readjustment Needs of Service Members, Veterans, and Their Families. Washington, DC: The National Academies Press.
———. 2012. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Washington, DC: The National Academies of Press.
———. 2013a. Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington, DC: The National Academies Press.
———. 2013b. Substance Use Disorders in the U.S. Armed Forces. Washington, DC: The National Academies Press.
J-MHAT- 7 (Joint Mental Health Advisory Team 7). 2011. Operation Enduring Freedom 2010. Washington, DC: Department of Defense.
Kehle, S. M., A. G. Ferrier-Auerbach, L. A. Meis, P. A. Arbisi, C. R. Erbes, and M. A. Polusny. 2012. Predictors of postdeployment alcohol use disorders in National Guard soldiers deployed to Operation Iraqi Freedom. Psychology of Addictive Behaviors 26(1):42–50.
Kennedy, J. E., F. O. Leal, J. D. Lewis, M. A. Cullen, and R. R. Amador. 2010. Posttraumatic stress symptoms in OIF/OEF service members with blast-related and non-blast-related mild TBI. NeuroRehabilitation 26(3):223–231.
Kimerling, R., K. Gima, M. W. Smith, A. Street, and S. Frayne. 2007. The Veterans Health Administration and military sexual trauma. American Journal of Public Health 97(12):2160–2166.
Kimerling, R., A. E. Street, J. Pavao, M. W. Smith, R. C. Cronkite, T. H. Holmes, and S. M. Frayne. 2010. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. American Journal of Public Health 100(8):1409–1412.
Kinder, L. S., K. A. Bradley, W. J. Katon, E. Ludman, M. B. McDonell, and C. L. Bryson. 2008. Depression, posttraumatic stress disorder, and mortality. Psychosomatic Medicine 70(1):20–26.
Kolkow, T. T., J. L. Spira, J. S. Morse, and T. A. Grieger. 2007. Post-traumatic stress disorder and depression in health care providers returning from deployment to Iraq and Afghanistan. Military Medicine 172(5):451–455.
Kroenke, K., R. L. Spitzer, J. B. Williams, and B. Lowe. 2010. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. General Hospital Psychiatry 32(4):345–359.
Langhinrichsen-Rohling, J., J. D. Snarr, A. M. Slep, R. E. Heyman, and H. M. Foran. 2011. Risk for suicidal ideation in the U.S. Air Force: An ecological perspective. Journal of Consulting and Clinical Psychology 79(5):600–612.
Lapierre, C. B., A. F. Schwegler, and B. J. Labauve. 2007. Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. Journal of Traumatic Stress 20(6):933–943.
Larson, G. E., P. S. Hammer, T. L. Conway, E. A. Schmied, M. R. Galarneau, P. Konoske, J. A. Webb-Murphy, K. J. Schmitz, N. Edwards, and D. C. Johnson. 2011. Predeployment and in-theater diagnoses of American military personnel serving in Iraq. Psychiatric Services 62(1):15–21.
LeardMann, C. A., A. Pietrucha, K. M. Magruder, B. Smith, M. Murdoch, I. G. Jacobson, M. A. Ryan, G. Gackstetter, and T. C. Smith. 2013a. Combat deployment is associated with sexual harassment or sexual assault in a large, female military cohort. Womens Health Issues 23(4):e215–e223.
LeardMann, C. A., T. M. Powell, T. C. Smith, M. R. Bell, B. Smith, E. J. Boyko, T. I. Hooper, G. D. Gackstetter, M. Ghamsary, and C. W. Hoge. 2013b. Risk factors associated with suicide in current and former US military personnel. JAMA 310(5):496–506.
Lester, P., K. Peterson, J. Reeves, L. Knauss, D. Glover, C. Mogil, N. Duan, W. Saltzman, R. Pynoos, K. Wilt, and W. Beardslee. 2010. The long war and parental combat deployment: Effects on military children and at-home spouses. Journal of the American Academy of Child and Adolescent Psychiatry 49(4):310–320.
Lincoln, A., E. Swift, and M. Shorteno-Fraser. 2008. Psychological adjustment and treatment of children and families with parents deployed in military combat. Journal of Clinical Psychology 64(8):984–992.
Lowe, B., K. Kroenke, and K. Grafe. 2005. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research 58(2):163–171.
MacGregor, A. J., R. A. Shaffer, A. L. Dougherty, M. R. Galarneau, R. Raman, D. G. Baker, S. P. Lindsay, B. A. Golomb, and K. S. Corson. 2009. Psychological correlates of battle and nonbattle injury among Operation Iraqi Freedom veterans. Military Medicine 174(3):224–231.
MacGregor, A. J., P. P. Han, A. L. Dougherty, and M. R. Galarneau. 2012. Effect of dwell time on the mental health of US military personnel with multiple combat tours. American Journal of Public Health (102 Suppl 1):S55–S59.
MacLean, A., and G. H. Elder. 2007. Military service in the life-course. Annual Review of Sociology 33:175–196.
Maguen, S., D. S. Vogt, L. A. King, D. W. King, B. T. Litz, S. J. Knight, and C. R. Marmar. 2011. The impact of killing on mental health symptoms in Gulf War veterans. Psychological Trauma: Theory, Research, Practice, and Policy 3(1):21–26.
Maguen, S., D. D. Luxton, N. A. Skopp, and E. Madden. 2012. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. Journal of Psychiatric Research 46(3):311–316.
Mansfield, A. J., J. S. Kaufman, S. W. Marshall, B. N. Gaynes, J. P. Morrissey, and C. C. Engel. 2010. Deployment and the use of mental health services among U.S. Army wives. New England Journal of Medicine 362(2):101–109.
Mansfield, A. J., J. S. Kaufman, C. C. Engel, and B. N. Gaynes. 2011. Deployment and mental health diagnoses among children of US Army personnel. Archives of Pediatric and Adolescent Medince 165(11):999–1005.
Marshall, A. D., J. Panuzio, and C. T. Taft. 2005. Intimate partner violence among military veterans and active duty servicemen. Clinical Psychology Review 25(7):862–876.
Martin, S. L., D. A. Gibbs, R. E. Johnson, K. Sullivan, M. Clinton-Sherrod, J. L. Walters, and E. D. Rentz. 2010. Substance use by soldiers who abuse their spouses. Violence Against Women 16(11):1295–1310.
McCarroll, J. E., R. J. Ursano, X. Liu, L. E. Thayer, J. H. Newby, A. E. Norwood, and C. S. Fullerton. 2010. Deployment and the probability of spousal aggression by U.S. Army soldiers. Military Medicine 175(5):352–356.
Merrill, L. L., J. L. Crouch, C. J. Thomsen, and J. M. Guimond. 2004. Risk for intimate partner violence and child physical abuse: Psychosocial characteristics of multirisk male and female Navy recruits. Child Maltreatment 9(1):18–29.
MHAT-II (Mental Health Advisory Team II). 2005. Mental Health Advisory Team (MHAT–II): Operation Iraqi Freedom (OIF–11). Washington, DC: Office of the Surgeon General, United States Army Medical Command, Office of the Surgeon Multimational Force-Iraq.
MHAT-III (Mental Health Advisory Team III). 2006. Mental Health Advisory Team (MHAT–III): Operation Iraqi Freedom 04–06. Washington, DC: Office of the Surgeon General, United States Army Medical Command, Office of the Surgeon Multinational Force-Iraq.
Military Pathways. 2013. About Military Pathways: Mental Health Screening and Info. http://www.militarymentalhealth.org/about.aspx (accessed October 2, 2013).
Milliken, C. S., J. L. Auchterlonie, and C. W. Hoge. 2007. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA 298(18):2141–2148.
Momen, N., C. P. Strychacz, and E. Viirre. 2012. Perceived stigma and barriers to mental health care in Marines attending the Combat Operational Stress Control program. Military Medicine 177(10):1143–1148.
Moœcicki, E. K. 2001. Epidemiology of completed and attempted suicide: Toward a framework for prevention. Clinical Neuroscience Research 1(5):310–323.
Navy and Marine Corps Public Health Center. 2013. Fleet and Marine Corps Health Risk Assessment Annual Report, 2012. Washington, DC: Department of the Navy.
Nazarian, D., R. Kimerling, and S. M. Frayne. 2012. Posttraumatic stress disorder, substance use disorders, and medical comorbidity among returning U.S. veterans. Journal of Traumatic Stress 25(2):220–225.
Nevin, R. L. 2009. Low validity of self-report in identifying recent mental health diagnosis among U.S. service members completing pre-deployment health assessment (PreDHA) and deployed to Afghanistan, 2007: A retrospective cohort study. BMC Public Health 9(376).
Nock, M. K., C. A. Deming, C. S. Fullerton, S. E. Gilman, M. Goldenberg, R. C. Kessler, J. E. McCarroll, K. A. McLaughlin, C. Peterson, M. Schoenbaum, B. Stanley, and R. J. Ursano. 2013. Suicide among soldiers: A review of psychosocial risk and protective factors. Psychiatry: Interpersonal and Biological Processes 76(2):97–125.
Padden, D. L., R. A. Connors, and J. G. Agazio. 2011. Stress, coping, and well-being in military spouses during deployment separation. Western Journal of Nursing Research 33(2):247–267.
Peterson, A. L., V. Wong, M. F. Haynes, A. C. Bush, and J. E. Schillerstrom. 2010. Documented combatrelated mental health problems in military noncombatants. Journal of Traumatic Stress 23(6):674–681.
Pew Research Center. 2011. The military-civilian gap: War and sacrifice in the post-9/11 era. Washington, DC: Pew Social and Demographic Trends.
Phillips, C., C. LeardMann, G. Gumbs, and B. Smith. 2010. Risk factors for posttraumatic stress disorder among deployed U.S. male Marines. BMC Psychiatry 10(1):1–11.
Pietrzak, R. H., D. C. Johnson, M. B. Goldstein, J. C. Malley, A. J. Rivers, C. A. Morgan, and S. M. Southwick. 2009a. Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and postdeployment social support. Journal of Special Operations Medicine 9(3):74–78.
Pietrzak, R. H., D. C. Johnson, M. B. Goldstein, J. C. Malley, and S. M. Southwick. 2009b. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety 26(8):745–751.
Pietrzak, R. H., J. M. Whealin, R. L. Stotzer, M. B. Goldstein, and S. M. Southwick. 2011. An examination of the relation between combat experiences and combat-related posttraumatic stress disorder in a sample of connecticut OEF-OIF veterans. Journal of Psychiatric Research 45(12):1579–1584.
Pincus, S. H., R. House, J. Christenson, and L. E. Adler. 2001. The emotional cycle of deployment: A military family perspective. US Army Medical Department Journal (April/June):15–23.
Pittman, J. O., A. A. Goldsmith, J. A. Lemmer, M. T. Kilmer, and D. G. Baker. 2012. Post-traumatic stress disorder, depression, and health-related quality of life in OEF/OIF veterans. Quality of Life Research 21(1):99–103.
Polusny, M. A., S. M. Kehle, N. W. Nelson, C. R. Erbes, P. A. Arbisi, and P. Thuras. 2011. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in National Guard soldiers deployed to Iraq. Archives of General Psychiatry 68(1):79–89.
Ramchand, R., T. L. Schell, B. R. Karney, K. C. Osilla, R. M. Burns, and L. B. Caldarone. 2010. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: Possible explanations. Journal of Traumatic Stress 23(1):59–68.
Ramchand, R., J. D. Acosta, R. M. Burns, L. H. Jaycox, and C. G. Pernin. 2011. The War Within: Preventing Suicide in the U.S. Military. Santa Monica, CA: RAND Corporation.
Rauch, S. A., T. Favorite, N. Giardino, C. Porcari, E. Defever, and I. Liberzon. 2010. Relationship between anxiety, depression, and health satisfaction among veterans with PTSD. Journal of Affective Disorders 121(1–2):165–168.
Reddy, M. K., L. A. Meis, C. R. Erbes, M. A. Polusny, and J. S. Compton. 2011. Associations among experiential avoidance, couple adjustment, and interpersonal aggression in returning Iraqi War veterans and their partners. Journal of Consulting and Clinical Psychology 79(4):515–520.
Reed, S. C., J. F. Bell, and T. C. Edwards. 2011. Adolescent well-being in Washington state military families. American Journal of Public Health 101(9):1676–1682.
Rentz, E. D., S. L. Martin, D. A. Gibbs, M. Clinton-Sherrod, J. Hardison, and S. W. Marshall. 2006. Family violence in the military: A review of the literature. Trauma Violence Abuse 7(2):93–108.
Rentz, E. D., S. W. Marshall, D. Loomis, C. Casteel, S. L. Martin, and D. A. Gibbs. 2007. Effect of deployment on the occurrence of child maltreatment in military and nonmilitary families. American Journal of Epidemiology 165(10):1199–1206.
Riviere, L. A., A. Kendall-Robbins, D. McGurk, C. A. Castro, and C. W. Hoge. 2011. Coming home may hurt: Risk factors for mental ill health in US reservists after deployment in Iraq. British Journal of Psychiatry 198(2):136–142.
Sahlstein, E., K. C. Maguire, and L. Timmerman. 2009. Contradictions and praxis contextualized by wartime deployment: Wives’ perspectives revealed through relational dialectics. Communication Monographs 76(4):421–442.
Sandweiss, D. A., D. J. Slymen, C. A. LeardMann, B. Smith, M. R. White, E. J. Boyko, T. I. Hooper, G. D. Gackstetter, P. J. Amoroso, and T. C. Smith. 2011. Preinjury psychiatric status, injury severity, and postdeployment posttraumatic stress disorder. Archives of General Psychiatry 68(5):496–504.
Schneiderman, A. I., E. R. Braver, and H. K. Kang. 2008. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology 167(12):1446–1452.
Seal, K. H., T. J. Metzler, K. S. Gima, D. Bertenthal, S. Maguen, and C. R. Marmar. 2009. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. American Journal of Public Health 99(9):1651–1658.
Seal, K. H., G. Cohen, A. Waldrop, B. E. Cohen, S. Maguen, and L. Ren. 2011. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence 116(1–3):93–101.
Sheppard, S. C., J. W. Malatras, and A. C. Israel. 2010. The impact of deployment on U.S. military families. American Psychologist 65(6):599–609.
Skopp, N. A., M. A. Reger, G. M. Reger, M. C. Mishkind, M. Raskind, and G. A. Gahm. 2011. The role of intimate relationships, appraisals of military service, and gender on the development of posttraumatic stress symptoms following Iraq deployment. Journal of Traumatic Stress 24(3):277–286.
Skopp, N. A., R. Swanson, D. D. Luxton, M. A. Reger, L. Trofimovich, M. First, J. Maxwell, and G. A. Gahm. 2012a. An examination of the diagnostic efficiency of post-deployment mental health screens. Journal of Clinical Psychology 68(12):1253–1265.
Skopp, N. A., L. Trofimovich, J. Grimes, L. Oetjen-Gerdes, and G. A. Gahm. 2012b. Relations between suicide and traumatic brain injury, psychiatric diagnoses, and relationship problems, active component, U.S. armed forces, 2001-2009. Medical Surveillence Monthly Report 19(2):7–11.
Smith, M. V., N. Gotman, H. Lin, and K. A. Yonkers. 2010. Do the PHQ-8 and the PHQ-2 accurately screen for depressive disorders in a sample of pregnant women? General Hospital Psychiatry 32(5):544–548.
Smith, T. C., M. A. Ryan, D. L. Wingard, D. J. Slymen, J. F. Sallis, and D. Kritz-Silverstein. 2008. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: Prospective population based US military cohort study. British Medical Journal 336(7640):366–371.
Snarr, J. D., R. E. Heyman, and A. M. Slep. 2010. Recent suicidal ideation and suicide attempts in a large-scale survey of the U.S. Air Force: Prevalences and demographic risk factors. Suicide and Life Threatening Behavior 40(6):544–552.
Spera, C. 2009. Spouses’ ability to cope with deployment and adjust to Air Force family demands: Identification of risk and protective factors. Armed Forces and Society 35(2):286–306.
Spera, C., R. K. Thomas, F. Barlas, R. Szoc, and M. H. Cambridge. 2011. Relationship of military deployment recency, frequency, duration, and combat exposure to alcohol use in the Air Force. Journal of Studies on Alcohol and Drugs 72(1):5–14.
Stecker, T., J. Fortney, R. Owen, M. P. McGovern, and S. Williams. 2010. Co-occurring medical, psychiatric, and alcohol-related disorders among veterans returning from Iraq and Afghanistan. Psychosomatics 51(6):503–507.
SteelFisher, G. K., A. M. Zaslavsky, and R. J. Blendon. 2008. Health-related impact of deployment extensions on spouses of active duty army personnel. Military Medicine 173(3):221–229.
Stein, D. J., J. Ipser, and N. McAnda. 2009. Pharmacotherapy of posttraumatic stress disorder: A review of meta-analyses and treatment guidelines. CNS Spectrums 14(1 Suppl 1):25–31.
Summerall, E. L. 2012. Traumatic Brain Injury and PTSD. http://www.ptsd.va.gov/professional/pages/traumatic-brain-injury-ptsd.asp (accessed October 30, 2013).
Suris, A., and L. Lind. 2008. Military sexual trauma: A review of prevalence and associated health consequences in veterans. Trauma, Violence, and Abuse 9(4):250–269.
Taft, C. T., R. P. Weatherill, H. E. Woodward, L. A. Pinto, L. E. Watkins, M. W. Miller, and R. Dekel. 2009. Intimate partner and general aggression perpetration among combat veterans presenting to a posttraumatic stress disorder clinic. American Journal of Orthopsychiatry 79(4):461–468.
Tanielian, T., and L. H. Jaycox. 2008. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corporation.
Teasdale, T. W., and A. W. Engberg. 2001. Suicide after traumatic brain injury: A population study. Journal of Neurology, Neurosurgery, and Psychiatry 71(4):436–440.
Terrio, H., L. A. Brenner, B. J. Ivins, J. M. Cho, K. Helmick, K. Schwab, K. Scally, R. Bretthauer, and D. Warden. 2009. Traumatic brain injury screening: Preliminary findings in a US Army brigade combat team. Journal of Head Trauma and Rehabilitation 24(1):14–23.
Thomas, J. L., J. E. Wilk, L. A. Riviere, D. McGurk, C. A. Castro, and C. W. Hoge. 2010. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry 67(6):614–623.
Tollison, S. J., R. C. Henderson, J. S. Baer, and A. J. Saxon. 2012. Next steps in addressing the prevention, screening, and treatment of substance use disorder in active duty and veteran Operation Enduring Freedom and Operation Iraqi Freedom populations. Military Medicine 177(8 Suppl):39–46.
Trofimovich, L., N. A. Skopp, D. D. Luxton, and M. A. Reger. 2012. Health care experiences prior to suicide and self-inflicted injury, active component, U.S. armed forces, 2001-2010. Medical Surveillence Monthly Report 19(2):2–6.
U.S. Army. 2013. Ready and Resilient Campaign: Embedded Behavioral Health. http://www.army.mil/standto/archive_2013-08-13 (accessed January 7, 2013).
VA (Department of Veterans Affairs) and DOD . 2013. VA/DoD Clinical Practice Guideline for Assessment and Management of Patients at Risk for Suicide. Washington, DC: Department of Veterans Affairs and Department of Defense.
Vasterling, J. J., S. P. Proctor, M. J. Friedman, C. W. Hoge, T. Heeren, L. A. King, and D. W. King. 2010. PTSD symptom increases in Iraq-deployed soldiers: Comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress 23(1):41–51.
Vythilingam, M., J. Davison, C. Engel, and H. V. Ritschard. 2010. Training to Administer DOD Deployment Mental Health Assessments. Washington, DC: Department of Defense.
Warner, C. M., C. H. Warner, J. Breitbach, J. Rachal, T. Matuszak, and T. A. Grieger. 2007. Depression in entry-level military personnel. Military Medicine 172(8):795–799.
Warner, C. H., G. N. Appenzeller, C. M. Warner, and T. Grieger. 2009. Psychological effects of deployments on military families. Psychiatric Annals 39(2):54–63.
Warner, C. H., G. N. Appenzeller, T. Grieger, S. Belenkiy, J. Breitbach, J. Parker, C. M. Warner, and C. Hoge. 2011a. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Archives of General Psychiatry 68(10):1065–1071.
Warner, C. H., G. N. Appenzeller, J. R. Parker, C. M. Warner, and C. W. Hoge. 2011b. Effectiveness of mental health screening and coordination of in-theater care prior to deployment to Iraq: A cohort study. American Journal of Psychiatry 168(4):378–385.
Weinick, R. M., E. B. Beckjord, C. M. Farmer, L. T. Martin, E. M. Gillen, J. D. Acosta, M. P. Fisher, J. Garnett, G. C. Gonzalez, T. C. Helmus, L. H. Jaycox, K. A. Reynolds, N. Salcedo, and D. M. Scharf. 2011. Programs Addressing Psychological Health and Traumatic Brain Injury Among U.S. Miliary Service Members and Their Families. Santa Monica, CA: RAND Corporation.
Wells, T. S., C. A. LeardMann, S. O. Fortuna, B. Smith, T. C. Smith, M. A. Ryan, E. J. Boyko, and D. Blazer. 2010. A prospective study of depression following combat deployment in support of the wars in Iraq and Afghanistan. American Journal of Public Health 100(1):90–99.
Wilk, J. E., R. K. Herrell, G. H. Wynn, L. A. Riviere, and C. W. Hoge. 2012. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: Association with postdeployment symptoms. Psychosomatic Medicine 74(3):249–257.
Youssef, N. A., K. T. Green, J. C. Beckham, and E. B. Elbogen. 2013a. A 3-year longitudinal study examining the effect of resilience on suicidality in veterans. Annals of Clinical Psychiatry 25(1):59–66.
Youssef, N. A., K. T. Green, E. A. Dedert, J. S. Hertzberg, P. S. Calhoun, M. F. Dennis, and J. C. Beckham. 2013b. Exploration of the influence of childhood trauma, combat exposure, and the resilience construct on depression and suicidal ideation among U.S. Iraq/Afghanistan era military personnel and veterans. Archives of Suicide Research 17(2):106–122.
Zoroya, G. 2011. Pentagon opposes mental health program for guard. USA Today, December 8.


















































