4
EVIDENCE FOR DEPARTMENT OF DEFENSE INTERVENTIONS FOR PREVENTING PSYCHOLOGICAL DISORDERS
The committee was charged with conducting a systematic review and critique of Department of Defense (DOD) resilience and reintegration programs and prevention strategies related to the psychological health of service members and their families. This chapter discusses various DOD policies, programs, and services intended to enhance psychological health and prevent psychological disorders among service members and their families. It describes the nature of the interventions and reports on empirical studies that provide evidence concerning their effectiveness. Given the fast-track nature of the committee’s work, the committee conducted a literature review sufficient to highlight some of the interventions that address the psychological health concerns identified in the statement of task. It did not attempt to create a catalog of all of the DOD prevention interventions in those areas.
The chapter begins with an overview of DOD prevention interventions. It includes findings from a recent comprehensive assessment of DOD psychological health and traumatic brain injury (TBI) programs. The overview also summarizes the interventions that are the subject of this committee’s review. The sections that follow describe those interventions and their evidence and are organized by topical areas defined by the statement of task: resilience-related programs, posttraumatic stress disorder (PTSD), suicide (and depression), substance use disorders (including recovery support), reintegration, military sexual assault, and family-focused programs. The organizational structure aligns with the committee’s statement of task, but it is imperfect as some interventions address more than one health concern. For example, RESPECT–Mil, a primary care program designed to encourage early identification of depression and PSTD, is discussed in the section on suicide prevention as depression and PTSD are both risk factors for suicide.
OVERVIEW OF DOD PREVENTION INTERVENTIONS
Recent Review of DOD Psychological Health Programs
In an effort to develop a systematic list of DOD’s numerous programs that address various components of psychological health along the resilience, prevention, and treatment continuum, the RAND Corporation created a comprehensive catalogue of programs currently sponsored or funded by DOD to address psychological health and TBI. The catalogue, which is available in hardcopy and in an online searchable database, provides detailed descriptions of each program. As of November 2013, the electronic database contained 226 programs (RAND Corporation, 2013). Of the 226 programs, RAND classifies 94 as addressing the area of prevention (which includes resilience) (RAND Corporation, 2013). Appendix H shows RAND’s list of prevention/resilience programs and three classification elements reported by RAND: the
phase of deployment the intervention pertains to, whether it is a family-related intervention, and whether the intervention is based on evidence, as reported by program staff interviewed. RAND did not independently review or assess the strength of the evidence base employed. Fewer than half of the prevention programs shown are reported to be based on evidence.
RAND’s assessment (Weinick et al., 2011) found no centralized mechanism to catalogue all these programs and track which are effective, whether they meet the needs of the target audience, whether there are any gaps in program activity areas covered, and whether the programs need more resources. Furthermore, while there are many programs addressing a wide array of outcomes, many are duplicative in nature (both within and across service branches), few are based on evidence, and few measure outcomes. Programs are evaluated infrequently—according to interviews with program staff, fewer than one-third of the programs in any branch of service had had an outcome evaluation in the previous 12 months. For those programs conducting an evaluation, there was variation in the rigor of the evaluation, including such things as whether it was conducted internally or by an independent party, whether it had a control group, whether it examined both processes and outcomes, and the appropriateness of the metrics used. RAND emphasized that the negative consequences of not having a process to systematically develop, track, and evaluate programs include the proliferation of untested programs that are developed without an evidence base, inefficient use of resources, added cost and administrative inefficiencies, and the increased likelihood of failing to identify a potentially harmful program. Similarly, Meredith et al. (2011), in a monograph on resilience programs in DOD, found no standard measure of resilience or outcomes across programs, a situation that makes it difficult to compare programs and approaches that share a common goal.
The Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCOE) was established in 2007 to “assess, validate, oversee and facilitate prevention, resilience, identification, treatment, outreach, rehabilitation, and reintegration programs for psychological health and traumatic brain injury” (DOD, 2010a) for DOD. The committee did not assess DCOE’s role in psychological health programming across the department.
Selecting a Sample of Programs for Assessment
Deciding that there was little value in duplicating RAND’s efforts and considering the fast-track nature of this study, the committee concentrated its assessment on a sample of DOD prevention programs and interventions. The committee focused on interventions with strong relevance to the targeted areas of this study and for which significant information and research findings were available in the literature. As such, the interventions discussed in the section should not be considered representative of all DOD prevention interventions.
There is no consensus on exactly how “resilience” should be defined (Meredith et al., 2011). Echoing the recent RAND report Promoting Psychological Health in the U.S. Military (Meredith et al., 2011), this committee defines psychological resilience as the ability to cope with or overcome exposure to adversity or stress. However, the use of the term “resilience” in the report reflects the inconsistencies in the state of the evidence within the field and differences across DOD programs.
The capacity for resilience can be supported and enhanced across multiple systems, including within individuals, families, communities and cultural contexts, including the military unit or larger community. Resilience can occur along the continuum of response to stress, from the lack of development of psychological conditions such as PTSD and depression in response to trauma, through the ability to recover from a resultant psychological condition such as PTSD without developing a chronic condition with associated additional comorbidities (such as depression and substance abuse) and chronic functional impairment. Thus, enhancing resilience as a means of prevention can occur prior to exposure to stressors (either at a universal or selective level for those at higher risk), to decrease the development of persistent distress and psychological conditions, or can occur after initial symptoms occur to prevent chronic conditions (e.g., intervening for acute stress disorder to prevent PTSD) or can occur along the early treatment pathways (to prevent chronic disability and comorbid conditions and promote rapid recovery once PTSD has developed). As such, resilience is a concept that potentially comes into play in all phases of the deployment cycle.
In Promoting Psychological Health in the U.S. Military, Meredith et al. (2011) first examined the evidence base for resilience and then looked at the extent to which specific factors were reflected in DOD resilience-promotion programs. They reported that factors promoting psychological resilience can operate at various levels: the individual (positive coping and affect, positive thinking, realism, behavioral control, physical fitness, and altruism), the family (communication support, nurturing, emotional ties, and adaptability), the organization or unit (positive command climate, cohesion, and teamwork), and the community (cohesion, connectedness, belonging, and collective efficacy). Meredith et al. (2011) also reported that, generally speaking, most programs in the military emphasize factors with the strongest evidence in the literature. The resilience-promotion factors found in DOD programs at the individual level are positive thinking, positive coping, behavioral control, positive affect, and realism training. At the unit level a majority of programs incorporate positive command climate and teamwork. Many of the programs use enhancing family communication to promote resilience; however, there is more empirical evidence for the effectiveness of enhancing family support than for the effectiveness of enhancing family communication. Belongingness (which includes social integration and group membership) was the community factor most widely used by programs.
Concerning measures of effectiveness, Meredith et al. (2011) found no standard measures of resilience or outcomes used across DOD resilience programs. Moreover, although some of the programs have been widely disseminated and shown by research to be effective in non-military populations, by and large there is little evidence that these military programs truly build resilience. Meredith and colleagues reviewed 270 documents and found only 11 with a randomized controlled design. Three programs—Battlemind, Comprehensive Soldier Fitness, and Combat Operational Stress Control—are discussed in more detail below. See Chapter 5, What Should Be Measured?, for additional discussion about measuring the concept of resilience.
Battlemind
Battlemind, which is now called Resilience Training, is an Army program designed to foster resilience by teaching self-confidence and mental toughness in the context of deployment and transitioning home. The term “battlemind” is defined as the soldier’s inner capacity to face fear and adversity with courage. Developed by researchers at Walter Reed Army Institute of Research, Battlemind is a psycho-educational intervention that uses a cognitive and skills-based
approach to normalize reactions to operational stress, to build resilience, to ease the transition to home, and to promote self-recognition of psychological problems, help seeking, and identification of difficulties in others (Adler et al., 2009a,b). Prior to the widespread implementation of the program, randomized trials showed that the intervention had a positive effect on soldiers’ adjustment from combat, although the effect sizes were small (Adler et al., 2009b). Battlemind was launched in 2007 and mandated Army-wide.
There are several Battlemind modules,1 the most prominent of which are Battlemind Debriefing and Battlemind Training. Battlemind Debriefing is used at various intervals during combat deployment and sometimes post-deployment to deal with deployment’s cumulative effects. Among its goals are to identify the traumatic events that have placed a significant demand on unit members; to normalize thoughts and reactions; to discuss anger, withdrawal, and sleep problems; and to emphasize what individuals can do for themselves and their comrades. The debriefing seeks to restore a sense of duty and honor to the participants in order to enable them to proceed with their mission (Orsingher et al., 2008). Unlike other types of psychological debriefing, Battlemind Debriefing minimizes the degree to which traumatic events are recounted in order to avoid re-traumatization (Adler et al., 2009a).
Battlemind Training, on the other hand, is expressly designed for the post-deployment period. Based on Walter Reed Army Institute research (Adler et al., 2009a), it is a 1-hour psycho-educational intervention led by a psychological health professional which takes a cognitive and skills-based approach to informing military personnel about the post-deployment transition. It reinforces the point that specific skills that serve individuals well in combat need to be reframed and adapted for the transition home.
Several studies have evaluated the effectiveness of Battlemind. A randomized controlled trial involving 2,297 soldiers looked at Battlemind Debriefing and Battlemind Training interventions that were held 1 month post-deployment. The study found that Battlemind had positive effects on psychological health when compared to stress education, but only for those with high levels of combat exposure. More specifically, the study found that at 4 months followup both modules of Battlemind led to fewer symptoms of PTSD, less depression, and fewer sleep problems in those with high levels of combat exposure (Adler et al., 2009a). Another controlled trial of a 1-hour Battlemind training module carried out at 1 to 6 months post-deployment found fewer PTSD and depression symptoms at the 6-month follow-up; these benefits applied to participants as a whole, were of a small to medium effect size for PTSD symptoms (d=0.3 for PTSD Checklist (PCL) change score compared to a survey-only control condition), and were not restricted to those with high levels of combat exposure, although there was a high rate of loss to follow-up at 6 months (67 percent), which limited conclusions (Castro et al., 2012). The study also found less stigma surrounding help seeking immediately after the Battlemind session but not at follow-up. A UK version of Battlemind Training, described as more didactic in nature and lasting about 45 minutes, was studied in a cluster randomized controlled trial and showed no difference in PTSD and other psychiatric symptoms, although it did find a modest lowering of self-reported binge drinking (Mulligan et al., 2012). The control group was a standard postdeployment stress and homecoming brief and thus was more active than the survey-only condition used in the Castro et al. (2012) study; limitations of the study included relatively
____________________
1 Modules have been created for delivery at different stages of deployment (e.g., pre- or post-deployment) and for different personnel (e.g., soldiers, leaders, spouses).
minimal PTSD symptoms overall (mean PCL 23.6) and some crossover between the conditions. Some of the Battlemind modules have been converted from a standalone program into components of Comprehensive Soldier Fitness.
Comprehensive Soldier Fitness
In 2009 the Army launched the $125 million Comprehensive Soldier Fitness program (U.S. Army, 2009), the largest universal prevention program of its kind. At present it has already reached 1 million soldiers (Lester et al., 2011b). The goals of the Comprehensive Soldier Fitness (CSF) program are to prevent adverse psychological health consequences of trauma exposure—most notably, PTSD and depression—by increasing resilience in service members before deployment. The CSF program is based, in part, on the Penn Resiliency Program, which was developed by Martin Seligman at the University of Pennsylvania (Cornum et al., 2011). The Penn Resiliency Program is based on positive psychology as well as on cognitive behavioral theories of depression, and it includes training in assertiveness, negotiation, social skills, creative problem solving, the use of optimism and positive explanatory approaches, and decision making.
The CSF resilience-building program has four components that are designed to enhance service members’ mental, spiritual, physical, and social capabilities: (1) master resilience training, a 10-day, hands-on, face-to-face training course that includes the principles of positive psychology (Reivich et al., 2011); (2) comprehensive resilience modules (formerly known as Battlemind), which are training modules that focus on specific resilience skills using precepts of positive psychology, cognitive restructuring, mindfulness, and research on posttraumatic stress, unit cohesion, occupational health models, organizational leadership, and deployment in order to prepare service members for military life, combat, and transitioning home; (3) the global assessment tool (GAT), a confidential online 105-question survey that must be taken annually; and (4) institutional resilience training, which is expected to occur at every level of the Noncommissioned Officer Education System and the Officer Education System (U.S. Army, 2013b). Master resilience training for noncommissioned officers and mid-level supervisors is a “train the trainer” component of CSF for sergeants to use with their troops. Versions of the program are also available for military families and Army civilians, although this committee found no evidence of their implementation with these groups. The CSF GAT measures psychosocial well-being in four domains: emotional fitness, social fitness, family fitness, and spiritual fitness. Results of the GAT are used to refer soldiers to programs aimed at enhancing their strengths and addressing their weaknesses, for example, training in flexible thinking if scores in this area are lower than the norm. A similar instrument, the Family GAT, is being developed for soldiers’ spouses and partners to provide advice about possible resources for building emotional assets.
Internal Evaluation of CSF
Although evaluations that were conducted by CSF staff and were not subject to peer review have demonstrated statistically significant improvement in some GAT subscale scores, the effect sizes have been very small, with no clinically meaningful differences in pre- and posttest scores. Accordingly, it is difficult to argue there has been any meaningful change in GAT scores as a result of participation. For example, in The Comprehensive Soldier Fitness Program Evaluation Report #3: Longitudinal Analysis of the Impact of Master Resilience Training on Self-Reported Resilience and Psychological Health Data (Lester et al., 2011b), in a pre–post
comparison the maximum effect size (partial η2) of any outcome measured by the GAT was found to be 0.002 after exposure to the intervention. The only resilience or psychological health measures that saw significant improvement post-exposure were emotional fitness (a 1.31 percent improvement; 0.002 partial η2) and social fitness (a 0.66 percent improvement; 0.000 partial η2) (Lester et al., 2011b).
While Lester et al. (2011b) cite these figures as evidence of CSF’s effectiveness for prevention, this committee does not find these results meaningful, given the low level of improvement and the very small effect size. External reviews, discussed below, have raised similar questions concerning the effect sizes of reported findings and related problems in accurate interpretation of the impact.
More recently, in another internal non–peer-reviewed report, The Comprehensive Soldier and Family Fitness Program Evaluation Report #4: Evaluation of Resilience Training and Mental and Behavioral Health Outcomes, Harms et al. (2013) examined psychological health diagnosis outcomes for 7,230 soldiers who received the GAT before Master Resiliency Training was initiated (October 2010) and again approximately 6 months later (about April 2011) and who consented to use of their data for research. The researchers compared five psychological health diagnoses recorded in the U.S. Army Medical Department’s Patient Administration Systems and Biostatistics Activity (anxiety, depression, PTSD, alcohol abuse, and drug abuse) 3 months after return from deployment or completion of the second GAT for the 4,983 who had received the training (80 percent of whom had deployed) versus the 2,247 who had not (72 percent of whom had deployed). Findings revealed no change in the GAT factors and no difference in diagnosis among those receiving the intervention. Therefore, the subsequent mediation analysis performed by the authors cannot be interpreted as evidence of intervention/program impact.
External Reviews of CSF
In their review of CSF, Steenkamp et al. (2013) observed that the program that served as the blueprint for CSF, the Penn Resiliency program, did not, according to a meta-analysis, produce powerful effects in its own target, preventing depression in civilian adolescents and schoolchildren. The meta-analysis found that although the program reduced symptoms of depression, the effect size was small, and the program did not prevent, delay, or lessen “the intensity or duration of future psychological disorders” (Brunwasser et al., 2009, p. 1051). Prevention trials in adolescents and children find that an improvement in subclinical levels of depression is a more likely outcome than the prevention of a depression diagnosis in the future (Stice et al., 2009). With regard to the prevention of PTSD, Steenkamp and colleagues assert that no data at all support the effectiveness of the Penn Resiliency Program for adults; instead, they say, the best evidence for PTSD prevention can be found not in universal prevention programs like CSF, but in selective and indicated prevention programs, whose strongest effects are in preventing chronic PTSD in those who are already self-reporting clinically diagnosable stressrelated symptoms (Bryant et al., 1998). Steenkamp and colleagues also criticized the GAT as not being designed to assess PTSD symptoms; it assesses only strengths and problems in emotional, social, family, and spiritual domains. “Thus the program evaluation could not adequately assess CSF’s success in preventing PTSD” (Steenkamp et al., 2013, p. 509). Steenkamp and colleagues also question the underlying assumption of the program that increasing resilience prevents onset of PTSD, noting that “it is possible to be psychologically high functioning and still develop PTSD” (p. 510).
In their article “The Dark Side of Comprehensive Soldier Fitness,” Eidelson and colleagues (2011) emphasize that CSF was initiated without the use of pilot testing to determine program effectiveness. Like Steenkamp and colleagues, they criticize the application of the Penn Resiliency program in the face of the small effect sizes found in the meta-analysis by Brunwasser et al. (2009). Eidelson and colleagues also criticized the lack of CSF review by an independent ethics board, especially in light of the mandatory nature of the program. They assert that resilience training may “harm our soldiers by making them more likely to engage in combat actions that adversely affect their psychological health” (Eidelson et al., 2011, p. 643).
Smith (2013) critiques the CSF program as potentially causing harm. She observes that CSF’s emphasis on positive emotions and reducing the frequency of negative emotions could be detrimental. Service members experiencing negative feelings could feel “marginalized and demoralized for failing to cope using CSF’s strategies” (p. 244). To support this view, Smith cites a study by Norem and Illingworth (2004) finding that when a positive mood is induced, individuals who are pessimists display decreased ability to problem-solve. Smith also argues that CSF shifts responsibility for psychological health away from external causes, such as multiple deployments and prolonged periods of combat stress, and onto the individuals, who blame themselves for not preventing their own disorder. She points out that service members who experience self-blame are at risk for further mood disturbances and poorer quality of life (Smith, 2013).
Combat Operational Stress Control
During the past decade the Marine Corps has pioneered the development of the Combat Operational Stress Control (COSC) program whose goals are to prevent, identify, and treat combat and operational stress problems. Although the COSC program is being implemented in the Marine Corps and Navy, the generic concept of combat operational stress control informs activities in other service branches, albeit with different approaches. This section describes the Marine Corps and Navy program only. The program is taught and reinforced at multiple points during careers and deployment cycles. Its three major components are
1. The perception of stress as a continuum, according to a model that uses a color-coded tool to identify who is ready (green zone), reacting (yellow zone), injured (orange zone) and ill (red zone) (Nash, 2011). See Figure 5-1. The goal of COSC is to keep soldiers in the green zone or to treat them so they can return to the green zone.
2. The promotion of five core leadership functions: to strengthen service members; mitigate stressors; identify stress reactions, injuries, and illnesses; treat stress injuries and illnesses; and reintegrate stress casualties (Nash, 2011).
3. The oversight of combat operational stress first aid, a toolkit for non-medical care of stress injuries.
The Marine Corps requires that a percentage of leadership personnel in each operational unit be trained and certified in all three components of COSC under the related OSCAR (Operational Stress Control and Readiness) program. OSCAR is carried out by three different types of trained individuals: OSCAR “mentors,” leaders who are strong role models and are ready to intervene and mentor other Marines with stress problems; OSCAR “extenders,” who are chaplains, medical staff, and religious support specialists who can spot operational stress and provide a bridge to treatment by the third type of trained individual; and OSCAR psychological
health personnel, who are embedded in operational units to provide formal psychological health services to troops and to provide training, oversight, and consultation to commanders. OSCAR is not an intervention per se, but rather the use of trained professional and leadership teams that promote healthy social norms and facilitate access to treatment.
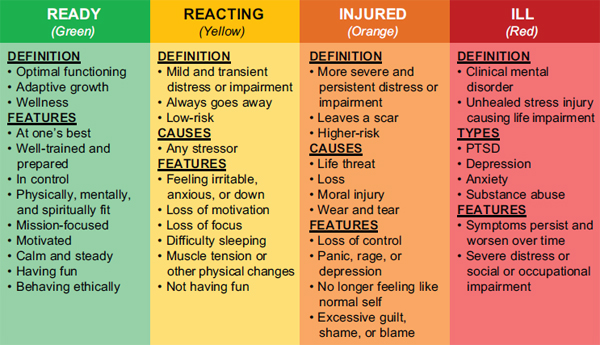
FIGURE 4-1 Stress continuum model sponsored by the Marine Corps.
SOURCE: Nash, 2011.
The only formal study of the COSC program is a baseline assessment of 553 Marines from 4 different bases who were participating in COSC (Momen et al., 2012). In this baseline assessment, 43.5 percent of the sample reported that their most recent deployment was still causing stress, and 31 percent reported that the stress affected their job performance. The most common views of combat stress reactions were that they are treatable (70.5 percent), normal (68.2 percent), can be managed (57.4 percent), and are harmful to career (46.7 percent). The survey also reported on attitudes toward help seeking and the treatment of stress-related disorders and found that fears of treatment seeking included a lack of confidentiality, a loss of trust from their unit or being treated differently by members of their unit, harming their careers, and having a preference to solve their own problems. A formal evaluation of COSC/OSCAR, including its impact on Marine mission readiness, unit cohesion, stigma, and stress burden, is being conducted by the RAND Corporation and will be published in Spring 2014.
BOOT STRAP
BOOT STRAP (Bootcamp Survival Training for Navy Recruits—A Prescription) is a program designed to help recruits cope with the emotional challenges of training. There are two studies that have examined the effectiveness of BOOT STRAP. Interestingly, one study (Williams et al., 2004) randomly assigned delivery of a psychologist-led weekly 45-minute group intervention for only half of the 25 percent of recruits who scored at higher risk based on the Perceived Stress Scale (30 or above) or the Beck Depression Inventory (18 or above) at baseline. The manual uses a cognitive behavior therapy (CBT) approach to enhance coping skills, belonging, team building, and stress management and to reduce the thought distortions associated with depression. The remaining high- and low-risk recruits participated in a control condition with weekly education (e.g., on personal hygiene) but lacking CBT strategies or a focus on support. Among the high-risk group, a greater proportion of the intervention group (86
percent) than the control group (74 percent) completed basic training; the completion rate among the intervention group was comparable to the 84 percent completion rate among the remaining 75 percent of recruits who had been deemed lower risk (Williams et al., 2004). In a follow-up study (Williams et al., 2007) of 1,199 Navy recruits cluster-randomized to either intervention or control status, the researchers did not find significantly different separation rates at 2 years or significantly different symptoms by the end of basic training (with differences in rate but not endpoint change in both studies), but they did find that those who trained in the more competitive summer “surge” recruitment months completed basic training at a significantly higher rate (10.3 versus 5.2 percent separation) (Williams et al., 2007). This program does show some feasibility and potential efficacy for the targeting of skills for those identified at risk upon initial entry into the military.
This section summarizes a body of research on several clinical interventions designed to prevent the onset of PTSD after the traumatic exposure has occurred, some of which interventions have been demonstrated to be effective. These interventions can resolve PTSD symptoms effectively, possibly decreasing the likelihood of chronic and disabling outcomes in service members.
After exposure to a traumatic event, although rates vary based on many factors—approximately one-third of men and one-half of women—develop PTSD (North et al., 2005). Although symptoms may begin in the immediate aftermath of exposure to the traumatic event, PTSD is not diagnosed until at least 1 month later, most typically in the 1 to 3 months posttrauma. Frequently, PTSD is preceded by acute stress disorder (ASD), which can be diagnosed in the first 4 weeks post-trauma, after which PTSD criterion may be met (APA, 2013). This time separation is meant to separate those for whom symptoms are transitory from those who develop PTSD, which can become more chronic, and it affords the opportunity for early intervention to prevent PTSD in trauma-exposed individuals. Most prevention trials have tested interventions in trauma-exposed civilians. The main outcome measures have been either prevention of PTSD diagnosis or a reduction in PTSD symptomatology. This section evaluates the evidence for psychotherapy or pharmacotherapy interventions for the prevention of PTSD. For more information about PTSD prevention and treatment programs in DOD and VA, see Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations (IOM, 2012). A second volume of that report, which will include an assessment of PTSD programs, will be released in summer 2014.
Psycho-Social Interventions
The strongest evidence for prevention of PTSD comes from studies of individuals with ASD who are given trauma-focused cognitive behavioral therapy. Eighty percent of individuals with ASD proceed to develop PTSD (Harvey and Bryant, 1998). Three randomized controlled trials in Australia by Bryant and colleagues (Bryant et al., 1998, 2003a, 2005) found that CBT prevents onset of PTSD in trauma-exposed individuals2 who meet the criteria for ASD. The CBT
____________________
2 Individuals were civilians who had experienced motor vehicle accidents, industrial accidents, nonsexual assault, or mild traumatic brain injury.
consisted of five to six sessions of individual therapy that included education about trauma reactions, progressive muscle relaxation training, exposure to traumatic events, cognitive restructuring of fear-related beliefs, and graded exposure to avoided situations. Individuals were started on CBT within 2 weeks of trauma and were followed until 6 months post-trauma, at which point structured diagnostic interviews were conducted. In the first study Bryant and colleagues found fewer cases of PTSD in the CBT group (17 percent) than in the supportive counseling group (67 percent) (Bryant et al., 1998). Similar findings were reported in the second study, with fewer cases of PTSD in the CBT group (17 percent) than in the supportive counseling group (58 percent) (Bryant et al., 2003a). In the third study, subjects were randomized to supportive counseling, CBT, or CBT with hypnosis (including focused attention and muscle relaxation) for 15 minutes just prior to the imagined exposure exercises, the purpose of which was to help patients engage fully in the trauma exposure (Bryant et al., 2005). Although not significantly different at end of treatment or at 6 months post-treatment in the intent to treat analysis, fewer subjects in the CBT and CBT–hypnosis groups developed PTSD than subjects given supportive counseling; the findings were limited by a small sample size and a higher dropout rate in the CBT conditions. CBT–hypnosis yielded greater reduction than CBT in reexperiencing symptoms at post-treatment. These studies figured prominently in a meta-analysis by the Cochrane Collaboration, which concluded that individual trauma-focused CBT was effective at PTSD prevention for individuals with acute traumatic stress symptoms (Roberts et al., 2012). Still, the authors suggested additional study in the form of larger, high-quality trials with longer follow-up intervals. Other types of psychotherapy, such as trauma-focused group therapy, eye movement desensitization, and non-trauma-focused CBT, were not found effective in prevention of PTSD.
Two subsequent studies by the Australian research team are noteworthy. A 4-year followup of patients studied in an earlier trial (Bryant et al., 1998) found that PTSD rates continued to be lower in patients treated with trauma-focused CBT than those treated with supportive therapy (Bryant et al., 2003b). A separate randomized controlled trial compared the efficacy of the two main elements of trauma-focused CBT—exposure therapy and cognitive therapy—and found exposure therapy to be superior in preventing cases of PTSD in subjects with ASD (Bryant et al., 2008). In contrast, another study comparing exposure therapy and cognitive therapy found them to be similarly effective in reducing the prevalence of PTSD (Shalev et al., 2012). One difference between these two studies is that Bryant and colleagues (2008) required ASD at the time of recruitment, while Shalev et al. did not require dissociation or avoidance, but rather required at least two of the three DSM-IV PTSD diagnosis clusters without the 1-month time criterion.
Psychotherapy for civilians exposed to trauma—a group composed of people with and without ASD—shows less impressive results than psychotherapy for patients with ASD. In a meta-analysis for the Cochrane Collaboration, Roberts and colleagues (2010) evaluated eight randomized controlled trials of multi-session psychotherapies and found no evidence of PTSD prevention. In fact, they found that a trend for increased PTSD symptoms at 3- to 6-month follow-ups. Because of the potential for harm and the lack of evidence of a main effect, the authors concluded that no psychotherapy intervention can be recommended for routine use. The psychotherapies under study were trauma-focused CBT individual therapy, stress management/relaxation, trauma-focused CBT group therapy, eye movement desensitization, and non-trauma-focused CBT group therapy.
Psychological debriefing, including critical incident stress debriefing (CISD), was created for use with rescue workers in the aftermath of potentially traumatic events. It includes a variety of single-session individual and group interventions that involve revisiting the trauma for the purpose of encouraging trauma-exposed persons to talk about their experiences during the trauma; to recognize and express their thoughts, emotions, and physical reactions during and since the event; and to learn coping methods. Specially trained debriefers lead the sessions, which usually focus on normalization of symptoms, group support, and provision of psychoeducation and information about resources (IOM, 2012). Most randomized controlled trials that have examined psychological debriefing for the prevention of PTSD have used onetime debriefings of victims of motor vehicle accidents or crimes, such as rape. Numerous reviews and meta-analyses of these studies have determined that this treatment is ineffective and occasionally harmful because it can cause re-traumatization or secondary exposure to trauma through forced discussion of trauma details experienced by the individual or others in group format (McNally et al., 2003; Rose et al., 2002). A more recent study (Adler et al., 2008) randomized 1,050 soldiers who served in Kosovo as peacekeepers into 62 groups that were subjected to 3 conditions: critical incident stress debriefing (the most common form of psychological debriefing), stress education, and wait list. No differences were found between groups in any of the measured psychological health outcomes, although it should be noted that soldiers in the study experienced relatively few traumas. In summary, psychological debriefing has not been shown to prevent PTSD, and the VA/DOD guidelines (VA and DOD, 2010) and the Cochrane review of this topic (Rose et al., 2002) have stated that compulsory psychological debriefing is contraindicated.
A different approach, prolonged exposure therapy, is based on fear-extinction models of PTSD and combines imagined and situational exposure through repeated confrontation of traumatic memories and avoided reminders to allow processing of the trauma, fear extinction (reduction in fear responses to trauma memories and reminders), and reduction in overgeneralization of fear contexts over time (e.g., learning that darkness alone does not mean another attack will occur) (VA, 2013). A key difference between this and psychological debriefing is that the exposures are repeated and maintained until anxiety diminishes. Rothbaum et al. (2012) examined whether an early intervention with a three-session modified version of prolonged exposure therapy following a traumatic event could reduce the onset of PTSD. Participants were trauma survivors found in an emergency department and were assigned to receive either prolonged exposure therapy or a symptom assessment only within 12 hours of experiencing the traumatic event. At 4 weeks following the intervention, there was no statistical difference in PTSD diagnosis (using the PTSD Symptom Scale Interview, PSS-I) between the two groups: 54 percent of the intervention group and 49 percent of the assessment-only group did not meet the criteria for PTSD at 4 weeks (p=.60). A treatment difference did emerge over time, however, as 74 percent of the intervention group and 53 percent of the assessment-only group (p=.04) did not meet the criteria for PTSD at 12 weeks. The effectiveness of the intervention varied according to the type of trauma. Those in the prolonged exposure group who had experienced sexual trauma saw significantly more improvement at both four (p=.004) and 12 weeks (p=.05) compared to the assessment-only group. Among those who experienced a transportation trauma or a physical assault, the prolonged exposure group did not see a significantly better outcome than the assessment only group at either 4 or 12 weeks (Rothbaum et al., 2012). These data provide a preliminary indication that the evidence-based approach of prolonged exposure therapy for PTSD may also be helpful as an early intervention strategy to
prevent chronic PTSD development; additional research is needed to clarify the optimal length of treatment and target population for this approach.
Patients often take months or years to seek treatment for their PTSD (Kessler et al., 1995). Thus Zatzick and colleagues (2013) sought to deliver psychiatric care soon after the traumatic injury occurred in order to determine the ameliorative effects of such immediate treatment. Their study, which looked at 207 hospitalized injury survivors, was a stepped-care intervention trial of psychopharmacology and cognitive behavioral therapy. The CBT component included psychoeducation, muscle relaxation, cognitive restructuring, and graded exposure. Stepped care consists of case management targeted to the intensity of need and coordinated across different care settings by a team of psychological health professionals, including those with a master’s degree in social work and nurse practitioners. Participants were initially screened in the hospital by the PTSD Checklist Civilian version (PCL–C). Patients with a score of at least 35 on the PCL–C were rescreened with a second PCL–C in the days and weeks post-discharge. Patients who again scored at least 35 were randomly assigned to stepped care or usual care. Symptoms of PTSD and functional impairment were assessed at 1, 3, 6, 9, and 12 months postinjury. At the 6-, 9-, and 12-month assessments, recipients of stepped care had clinically and significantly reduced symptoms of PTSD as determined by the Clinician-Administered PTSD Scale. Recipients of stepped care also exhibited significant improvements in physical function as measured by the Medical Outcomes Study Short Form 36 Physical Component Summary. The study concluded that a stepped-care intervention lowers PTSD symptoms and improves physical functioning during the first year post-injury, and provides an example of systematically adapting interventions based on screening.
Pharmacotherapy
The beta-adrenergic antagonist propranolol has been tested as a preventive intervention under the rationale that excessive noradrenergic activity is associated with PTSD. Although initial data in a small randomized trial of propranolol compared to placebo led to some suppression of physiologic reactivity to trauma cues when delivered in the emergency department 6 to 12 hours post-trauma and continued for the next 10 days, propranolol showed no significant reduction in PTSD symptoms 1 and 3 months thereafter (Pitman et al., 2002). Furthermore, a follow-up randomized controlled trial by the same group (Hoge et al., 2012) with propranolol dose maximized up to 240 mg/day for 19 days failed to find a significant difference in PTSD diagnosis, symptoms, or physiologic reactivity at 4 and 12 weeks post-trauma, and the authors concluded that propranolol could not be recommended as a PTSD prevention strategy in the acute aftermath of trauma. These findings were consistent with Stein and colleagues (2007), who also failed to find evidence for efficacy in PTSD prevention of 14 days of propranolol or gabapentin administered within 48 hours of traumatic injury compared to placebo in a small randomized controlled trial.
Hydrocortisone also has been tested under the rationale that low cortisol levels are associated with PTSD. Two small clinical trials found lower rates of PTSD at long-term followup (Schelling et al., 2001, 2004). In a third study by the same group, hydrocortisone given over a 4-day taper resulted in better postoperative adjustment after cardiac surgery, on the basis of measures of quality of life, stress, and PTSD (Weis et al., 2006). A small placebo-controlled randomized control trial (RCT) of 25 civilians with acute stress symptoms found the best results
at 1-month and 3-month follow-up with a single high intravenous dose (100–400 mg) of hydrocortisone given within 6 hours of trauma (Zohar et al., 2011).
Selective serotonin reuptake inhibitors (SSRIs) also have been proposed to prevent PTSD by virtue of their established efficacy for PTSD and their anti-anxiety affects. Shalev and colleagues (2012) tested the SSRI escitalopram versus placebo given over 8 weeks, initiated within 1 month post-trauma. There was no difference between escitalopram and placebo in PTSD rates. The study also randomized patients to exposure therapy and cognitive therapy, which were found similarly effective in preventing PTSD in initially symptomatic patients, and more effective than medication, suggesting that CBT approaches may be more effective for PTSD prevention than this class of medication.
In a medical record study, the use of morphine during early resuscitation and trauma care of 696 wounded soldiers in Iraq was significantly associated with a lower risk of PTSD (odds ratio 0.47; p <0.001) (Holbrook et al., 2010). The association continued to be significant after controlling for injury severity. The study was not randomized and was not designed to determine if the effect stemmed from pain reduction, antagonism of noradrenergic activity, or both. Another non-randomized study of trauma patients admitted to a hospital found that patients who met criteria for PTSD 3 months later received significantly less morphine at the time of hospitalization than those who did not develop PTSD (Bryant et al., 2009). The predictors of PTSD severity at 3 months were acute pain and mild traumatic brain injury after adjusting for injury severity, gender, age, and type of injury. The authors concluded that administration of morphine may attenuate fear conditioning. It is unclear whether morphine would be effective in the absence of physical injury and pain, although some animal data support attenuation of fear conditioning after a severe stressor (Szczytkowski-Thomson et al., 2013); additional randomized controlled trials are needed.
It should be noted that many patients receive benzodiazepines acutely, and there was early interest in benzodiazepines as an anxiolytic to prevent PTSD. Available data, however, suggest that benzodiazepines may impair extinction learning, lack efficacy for PTSD, and may even increase rates of PTSD when administered in the aftermath of trauma (Gelpin et al., 1996), leading the 2010 VA/DOD guidelines to list them as contraindicated.
Summary
PTSD may be preventable in patients at greatest risk—those with ASD or acute symptoms—who are given trauma-focused individual CBT, and one recent study suggests intervention starting within the first day post-trauma may be beneficial. It is less clear whether patients who are less symptomatic can have significant benefit from these types of early intervention strategies. Psychological debriefing is ineffective and possibly harmful; it is believed that required single-session debriefing with a review of trauma details is contraindicated and should be avoided. Although SSRI antidepressants have demonstrated efficacy for PTSD, a recent randomized controlled trial failed to show efficacy of escitalopram for PTSD prevention. The most promising pharmacotherapies with positive preliminary support are hydrocortisone and morphine given around the time of trauma, but large randomized clinical trials targeting individuals with a range of traumas, including trauma that does not include physical pain due to injury, are needed before definitive conclusions may be drawn.
The types of DOD suicide prevention interventions profiled here include crisis lines, gatekeeper training, primary care training and services, restricting access to lethal means, and a comprehensive suicide prevention program. When efficacy data are not available from DOD, the committee draws on efficacy data from similar programs in civilians. This section also describes a large-scale research effort that aims to inform ongoing health promotion, risk reduction, and suicide prevention efforts.
Suicide Crisis Lines
Each of the services prominently posts on its suicide prevention website the 800 number for the Military Crisis Line. Renamed the Military Crisis Line in 2012, the Veterans Suicide Crisis Line was launched in 2007 as a toll-free, confidential resource that links service members in crisis (or families and friends) to qualified responders. Two years after being launched, the Crisis Line added an anonymous online chat service and, in 2011, a text messaging service. The Military Crisis Line is a joint undertaking of DOD, VA, and the Substance Abuse and Mental Health Services Administration. The rationale for a suicide prevention crisis line is that suicide is often associated with stressful life events, and it is surrounded by psychological ambivalence; those surviving a suicide attempt often claim that their wish to die coexists with a wish to be rescued (Shaffer et al., 1988).
While the committee is aware of an National Institute of Mental Health–funded project to assess the feasibility of evaluating the Military Crisis Line (NIH RePORT, 2013), to date, the efficacy of the Military Crisis Line has not been evaluated. However, a descriptive study of the crisis call centers reported that the call volume to this national veterans crisis line, which is available 24 hours per day, 7 days per week, reached 171,000, with 70 percent of callers being male. It is worth noting that this service’s advertising has been targeted at overcoming stigma and the resistance among service members to seeking help, with slogans such as “It takes the courage and strength of a soldier to ask for help.” Over several years of implementation, the calls generated 16,000 referrals to care as well as referrals to services for homelessness and substance abuse (Knox et al., 2012).
The committee is aware of limited research in the biomedical literature that evaluate the efficacy of civilian crisis lines. Gould et al. (2007b) completed a study of 1,085 callers to a civilian hotline targeting suicidal adults in 2003–2004. This study assessed suicidality not only during the call, but also an average of 2 weeks afterward. It found that 50 percent of callers were indeed suicidal—they had a plan in place—and 8.1 percent had already taken some action to harm themselves immediately before calling the crisis line. The study also found a significant reduction, over the course of the call, in intent to die, hopelessness, and psychological pain. In the subsequent weeks hopelessness and psychological pain continued to decrease. The caller’s intent to die by the conclusion of the call was the strongest predictor of subsequent suicidality (i.e., suicidal thinking, plan, or attempt). The findings underestimated the effects of the hotline because they screened out callers whose suicide risk status was deemed by the counselor to be “too high,” according to their clinical criteria, to participate in the study. A subsequent study by the same team of investigators found that 50 percent of suicidal callers subsequently utilized psychological health referrals obtained by calling the crisis line (Gould et al., 2007a). A study of
a suicide prevention program for adolescents succeeded in reducing the suicidality of callers over the course of the consultation (King et al., 2003).
In a study of 14 call centers in the 1-800-SUICIDE network, Mishara et al. (2007) found great variability in adherence to protocol among volunteers receiving the calls. Most volunteers did not ask the most basic questions about suicidal ideation, such as how the caller intended to commit suicide or if the caller had the means to complete the suicide. Similarly, in 10 observed cases when a suicide appeared to be in process, the volunteer failed to follow protocol and send an ambulance to the caller’s location. The authors suggest establishing a routine monitoring system would help ensure that minimum standards are met by suicide call centers (Mishara et al., 2007).
Gatekeeper Training
Gatekeeper training is a generic approach that teaches specific groups of people to identify those around them who are at high risk for suicide and then to refer those people for treatment. The two most prominent gatekeeper training programs are sponsored by the Army: Ask, Care, Escort (ACE) and Applied Suicide Intervention Skills Training (ASIST). The former uses peers as gatekeepers, while the latter is generally reserved for health professionals, clergy, or officers.
The ACE program aims to use peers to target at-risk soldiers. Developed by the U.S. Army Center for Health Promotion and Preventive Medicine, the program includes 1.5 hours of formal training with DVDs, PowerPoint files, handouts, and training tip cards. Its specific aims are to
• Train soldiers to recognize suicidality in fellow soldiers, including warning signs;
• Target soldiers who are reluctant to seek care because of stigma;
• Enhance the gatekeeper’s confidence to ask whether a peer is contemplating suicide;
• Train soldiers in active listening; and
• Encourage gatekeepers to take peers directly to the chain of command, a chaplain, or a behavioral health clinician (Ramchand et al., 2011).
The efficacy of the ACE program has not been evaluated, but according to a major review of DOD programs by the RAND Corporation (Ramchand et al., 2011), the program has been reviewed by a panel of three suicide prevention experts and “found to meet standards of accuracy, safety, and programmatic guidelines.”
The ASIST program for gatekeepers uses a 2-day training workshop. Its specific aims are to
• Identify soldiers who have suicidal ideation;
• Comprehend how gatekeepers’ beliefs and attitudes affect suicide intervention;
• Search for a shared understanding of reasons for suicidal ideation and reasons for living;
• Assess risk and develop a plan to increase safety from suicidal behavior for an agreed amount of time; and
• Follow up on safety commitments and ascertain whether additional help is needed (Ramchand et al., 2011).
The Army’s goal is to have at least two ASIST-trained gatekeepers for each installation, camp, state, territory, and reserve support center. The Army’s policy requires training for chaplains and their assistants, psychological health professionals, and Army Community Service staff members. ASIST was founded in 1983 by researchers at the University of Calgary and a decade later was taken over by the company LivingWorks Education. ASIST is being used by the U.S. Army, U.S. Air Force, Canadian armed forces, and many civilian agencies (U.S. Army, 2013c).
The efficacy of ASIST has not been investigated by the Army. The RAND study of military suicide prevention programs identified five evaluations of civilian ASIST programs, but only one was published in the peer-reviewed literature. It was a survey of gatekeeper-trained staff members of a two-site health care facility serving over 1 million residents in Ontario, Canada (McAuliffe and Perry, 2007). The survey, which was conducted before and 2 years after gatekeeper training, found an annual increase of 14 to 21 percent in identification of suicidal risk by patients in the emergency department. It also found a 14.5 percent reduction in the length of stay for admitted patients. Respondents’ knowledge of what steps to take after assessing suicide risk increased from 87 to 97 percent. The percentage of staff endorsing the statement “I am provided with adequate ongoing training in how to assess and respond to patients with suicide risk” increased from 30 to 80 percent. The survey was not designed to evaluate the program’s impact on suicide rates or suicidality.
A systematic review of seven other gatekeeper programs (not including ASIST) found that the programs produced a significant improvement in gatekeeper’s attitudes, skills, and general knowledge of suicide prevention (Isaac et al., 2009). One of the seven programs being reviewed was for the Department of Veterans Affairs. That review found significant improvement in counseling center clinical and administrative staff (n=602) in staff knowledge, self-efficacy, and three gatekeeper skills from pre- to post-training (Matthieu et al., 2008). None of the gatekeeper programs, whether military or civilian, has been evaluated for their impact on rates of suicidality or suicide.
Primary Care Training and Services
Although not expressly intended to prevent suicides, one widespread DOD program designed to encourage recognition and high-quality treatment of depression and PTSD in primary care (using existing evidence-based screens), RESPECT–Mil,3 does have ingredients of effective suicide prevention. That is because the program requires that soldiers who are identified as having depression or PTSD symptoms be screened for suicide risk. Primary care provider education is one of only two effective types of suicide prevention programs according to an influential review article (Mann et al., 2005). Primary care offers a valuable opportunity for suicide prevention because most suicidal patients have contact with their primary care providers in the months before their death (Andersen et al., 2000; Luoma et al., 2002) and because entering primary care is considered less stigmatizing than entering specialty care. No patient outcome data are available for the RESPECT–Mil program, but a research psychologist is working with the program to implement a continuous program evaluation effort (RAND Corporation, 2013). A
____________________
3 RESPECT–Mil stands for Re-Engineering Systems of Primary Care Treatment in the Military. The program trains primary care providers in detection and treatment of PTSD and depression, relies on a nurse facilitator to ensure continuity of care, and has a behavioral health specialist review each case and consult with the nurse facilitator. For details of the program and reporting of efficacy, see Engel et al. (2008).
2009 internal evaluation of the RESPECT–Mil program found that among a convenience sample of service members previously deployed, RESPECT–Mil appeared to detect depression and PTSD problems in up to 5 percent of returning service members who were not detected as having problems during their post-deployment health assessment screening,4 a population-based screening process performed immediately following return from deployment (Military Health System Clinical Quality Management, 2009b). Among a different sample of RESPECT–Mil participants, 43 percent of service members who screened positive for PTSD or depression or received a diagnosis for either condition contacted psychological health services within 30 days (Military Health System Clinical Quality Management, 2009a).
Two of the most prominent primary care programs for civilians give primary care providers depression education or extra support, or both. On the Swedish island of Gotland, a program in primary care education led to a reduction in the suicide rate (Rutz et al., 1989). In the United States, a program5 using a depression care manager in primary care to provide algorithmbased care and monitoring of symptoms, adverse effects of drugs, and adherence to treatment was associated in a randomized controlled trial with less depression, less suicidal ideation, and less mortality (Alexopoulos et al., 2009; Bruce et al., 2004; Gallo et al., 2013). All-cause mortality was studied because the sample size (20 primary care practices) was too small to have the power to detect changes in the suicide rate.
Restricting Access to Lethal Means
Research shows unequivocal evidence of an association between firearm possession and increased risk of suicide (Freeman et al., 2003). Guns are the primary method of suicide by service members and veterans; these groups are known to have high rates of gun ownership (Claassen and Knox, 2011). A recent population-based study of veterans found that they were twice as likely as non-veterans to die by suicide and 58 percent more likely than non-veterans to use firearms rather than other suicide methods to end their lives (Kaplan et al., 2007). According to the DOD Suicide Event Report program, of the 301 military members in all services who died by suicide in 2011, 172 (60 percent) used firearms to kill themselves. Of those who used firearms, 141 (82 percent) used non-military-issue firearms and only 31 (18 percent) used military-issue firearms (DCOE, 2012a). That underscores the importance of assessing and addressing the access to non-military-issue firearms as well as military-issue firearms by people who are at risk for suicide.
International experts who reviewed the literature on suicide prevention interventions concluded that the restriction of access to lethal means is one of the few suicide prevention policies with proven effectiveness (Mann et al., 2005). In the United States, legislation aimed at tightening handgun control in the general population has been shown to reduce suicide deaths by firearms among some subgroups (Loftin et al., 1991; Ludwig and Cook, 2000).
DOD gun-safety protocols for military-issue weapons exist, but the guidance on lethalmeans counseling and restricting gun access is vague. Current DOD policy does not have provisions for restricting access to privately owned firearms for those believed to be at risk for suicide. In fact, the fiscal year (FY) 2011 National Defense Authorization Act (PL 111-383, Section 1062) prohibits the Secretary of Defense from issuing any regulation or policy on legally
____________________
4 See Chapter 4 for a description of the post-deployment health assessment.
5 The PROSPECT trial (Prevention of Suicide in Primary Care Elderly: Collaborative Trial).
owned personal firearms or ammunition kept by troops or civilian employees off base as well as from collecting any information on their guns or ammunition.6 More recently, however, DOD military leaders have been quoted in the popular press as stating that they are considering a policy that “will allow separation of privately owned firearms from those believed to be at risk of suicide” (Jordan, 2012). After the Israeli military restricted access to military-issue firearms,7 the suicide rate among adolescents (defined as ages 18 to 21) declined by 40 percent (Lubin et al., 2010). The VA/DOD Clinical Practice Guideline for the Assessment and Management of Patients at Risk for Suicide (VA and DOD, 2013) advocates restriction of lethal means for the suicidal patient.
In a study of National Violent Death Reporting System data, Caetano et al. (2013) found that in the general population alcohol was present in between 23 percent and 47 percent of people who died by suicide, with the percentage varying by race/ethnicity. Among those of Asian/Pacific Islands ancestry, 23 percent had positive blood alcohol, compared with 26 percent of blacks, 33 percent of whites, 38 percent of Hispanics, and 47 percent of American Indians and Alaskan Natives. The authors reported that the percentage of suicides with positive blood alcohol was lower in veterans than in non-veterans, although they did not present that data (Caetano et al., 2013).
In a study for DOD, Luxton et al. (2012) found that among active-duty service members who died by suicide in 2011, 21.3 percent had positive blood alcohol, and 8.7 percent tested positive for drugs. Among active-duty service members who attempted suicide, 64 percent showed evidence of drug or alcohol use. Prescription drugs, largely antidepressants and antianxiety medications, were the most frequently misused psychotropic drugs among service members with known drug use who completed or attempted suicide (Luxton et al., 2012). Restriction of medications commonly used in suicide is an effective method of suicide prevention, according to the systematic review by Mann and colleagues (2005). The military does not have any specific policy on restrictions on prescription drug availability.
Comprehensive Suicide Prevention Program
Responding to a spike in its suicide rate, in 1997 the U.S. Air Force (USAF) leadership implemented a multifaceted suicide prevention program consisting of 11 initiatives (see Box 5-1) (Knox et al., 2003). The broad-based initiatives were aimed at removing the stigma of seeking psychological health care, enhancing understanding of psychological health, and changing policies and social norms to encourage psychological health care and help individuals avoid negative career consequences from seeking help. The innovators who developed the program described it as a shift from viewing suicide as a medical problem to viewing suicide as a community-wide problem. During the program’s first 5 years, investigators found a 33 percent reduction in the rate of suicide, from approximately 12.1 per 100,000 to 8.3 per 100,000. They also found reductions in severe and moderate family violence (54 percent and 30 percent, respectively) and decreased rates for accidental death and homicides. A second report published in 2010 indicated that the lower suicide rates had continued in the years following 2003, except for 2004 when the program was implemented less rigorously (Knox et al., 2003). This USAF
____________________
6 PL 111-383: 111th Congress, Jan. 7, 2011.
7 The study restricted access by preventing soldiers who were going home for the weekend from taking their military-issue firearms with them.
program stands out among all other military prevention efforts for its comprehensiveness and for its evidence-based approach to reducing the suicide rate.
BOX 5–1
Initiatives of USAF Suicide Prevention Program
1. Leadership participation in suicide prevention activities
2. Provision of suicide prevention education in all formal training
3. Education of commanders to encourage help-seeking by subordinates
4. Increasing preventive functions performed by mental health personnel
5. Annual suicide prevention training for all military and civilian employees
6. Changes in policies to ensure that individuals under investigation for legal problems are assessed for suicide potential
7. Trauma stress response teams established to respond to terrorist attacks, serious accidents, or suicide
8. Establishment of a seamless system of services and Community Action Information Board to achieve a synergistic impact on community problems and reduce risk of suicide
9. Increased confidentiality when seen by mental health providers
10. Use of the IDS (Integrated Delivery System) Consultation Assessment Tool to enable commanders to assess unit strength and areas of vulnerability
11. Reliance on Suicide Event Surveillance System that tracks suicide events and facilitates analysis of potential risk factors
SOURCE: Knox et al., 2003.
Army STARRS
Although it is not a program intervention per se, Army STARRS (Study To Assess Risk and Resilience in Servicemembers) is a 5-year research study of risk and protective factors for suicide whose objective is to better understand psychological resilience, psychological health, and risk for self-harm among soldiers. Launched in 2009 through a partnership between the Army and the National Institute of Mental Health, Army STARRS supports an interdisciplinary team of investigators working on five separate study components: the Historical Administrative Data Study, New Soldier Study, All Army Study, Soldier Health Outcomes Study, and Special Studies (NIMH, 2013; U.S. Army, 2013a). Findings from these studies will be used to inform ongoing health promotion, risk reduction, and suicide prevention efforts.
Summary
DOD sponsors numerous types of suicide prevention programs, most of which vary by service (Ramchand et al., 2011). The USAF has the strongest program, and it is the only comprehensive program. Although it is commendable that DOD supports many programs, few have been evaluated. From the civilian literature it is clear that many programs being used by the military—involving gatekeepers, educational campaigns, and hotlines—have some limited evidence of effectiveness. The type of suicide prevention with the strongest evidence of effectiveness—restricting access to lethal means such as firearms and psychotropic medications—is not being undertaken by the military, in spite of the fact that firearms,
particularly non-military-issue firearms, are used in 60 percent of military suicide deaths and psychotropic medications are frequently used in suicide attempts. DOD is sponsoring a largescale research study to better understand psychological resilience, psychological health, and risk for self-harm among soldiers, which may further inform targets for future prevention efforts.
A 2013 IOM committee—the Committee on Prevention, Diagnosis, Treatment, and Management of Substance Use Disorders in the U.S. Armed Forces—completed a comprehensive assessment of DOD policies and programs to prevent, identify, diagnose, and treat substance use disorders (SUDs) in active-duty service members, members of the National Guard and reserves, and military dependents. That committee’s report, Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b), and other recent literature provide the basis for the following discussion of military policies, programs, and services for SUD prevention and the evidence base for SUD prevention interventions. Appendix G includes a full descriptive analysis of the SUD programs that committee reviewed. This section is organized by the types of DOD substance abuse prevention interventions profiled in that committee’s report—drug testing, community-level education and outreach, service member education and training, screening and brief intervention, environmental strategies—and discusses the available evidence for these interventions.
Drug Testing
DOD and branch-specific policy emphasize drug testing as a SUD prevention strategy. The Military and Civilian Drug Testing Program requires all active-duty members to undergo a urinalysis at least once per year to test for illicit drug use (DOD, 2012b). All urinalyses test for marijuana, cocaine, and amphetamines, but testing for other drugs (LSD, opiates, barbiturates, PCP) is not done uniformly (Miech et al., 2013). Under the current zero-tolerance policy, a positive urinalysis result leads to separation from service. In 2012 DOD expanded the urinalysis drug testing programs to screen for some of the most commonly abused prescription medications, such as hydrocodone and benzodiazepines. Service members who have approved prescriptions will not be subject to disciplinary action for using them within the prescribed dosages and times.
Until recently, none of the branches tested for alcohol. In February 2013 the Navy rolled out an alcohol breath-testing program. Random breath testing is being conducted aboard Navy ships, and positive tests may be used to identify individual who receive assistance through the drug and alcohol program advisor and the Navy Alcohol Abuse Prevention Program (U.S. Navy, 2013).
As a prevention strategy, drug testing has a presumed deterrent effect by increasing awareness of the consequences of testing positive for illicit drug use (i.e., separation from the military). There is no research, however, showing that drug testing is an effective prevention strategy for service members and their dependents. As argued in Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b), reports that cite decreasing rates of illicit drug use as evidence of the effectiveness of drug testing (Bray and Hourani, 2007; Bray et al., 2010; Miech et al.,
2013) do not take into account causality, secular trends, or other factors that affect rates of illicit drug use.
However, results from a recent study suggest that stringent military drug policy and programs may lead to a lifelong reduction in illegal drug use. Using a life-course perspective, Miech and colleagues (2013) examined long-term trends in past-year hallucinogen use among veterans and non-veterans by analyzing self-reported data from the National Survey of Drug Use and Health for 1985–2010. The results indicate that among a subgroup of respondents who reported a history of illegal drug use before the age of 18, the prevalence of hallucinogen use was lower among veterans than among non-veterans. The authors concluded that this finding suggests that the policies had their greatest effect by altering substance use trajectories that had already started.
Community-Level Education and Outreach
Aside from drug testing, DOD relies heavily on campaign-style prevention programs, including That Guy and the national Red Ribbon campaign. The That Guy campaign uses online and offline public service announcements, a website with animated risk scenarios and modeling of prevention techniques, and prevention marketing. The overall aims are to increase awareness about the hazards of excessive drinking and to change attitudes about this behavior. Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b) reviewed the campaign and found that it uses evidence-based practices of modeling, rehearsal, discussion, and practice and focuses primarily on negative perceived consequences, negative social consequences, and peer pressure. The committee is not aware, however, of any evaluation of the That Guy campaign.
Red Ribbon Week is an annual campaign conducted every October on military bases and in communities nationwide to raise awareness about SUD prevention and risk factors (National Family Partnership, 2013). The program is a universal prevention campaign aimed at addressing peer pressure and prosocial bonding in youth, as well as parent monitoring. In its review of the program, IOM (2013b) found no published information on Red Ribbon’s theoretical basis and concluded that the program varies in campaign implementation across branches and bases and suffers from a lack of specification of participation requirements.
IOM (2013b) could not determine whether the That Guy or Red Ribbon programs are effective at preventing risky drinking and alcohol misuse among service members. There are at present no published peer-reviewed studies on formal outcome evaluations of these campaigns. Research on media campaigns to prevent drug use in youth has found that theory-based and evidence-based media campaigns can be effective in that population (Crano and Burgoon, 2002). However, the effectiveness of campaign activities within the military is unknown.
There are several notable population-based and community outreach initiatives sponsored by the Air Force. The Culture of Responsible Choices (CoRC) is a commander’s program with emphasis on leadership and individual-, base-, and community-level involvement—underscoring responsible behaviors, including avoiding alcohol and drug abuse; the prevention of accidents; tobacco cessation; decreasing obesity and increasing fitness, health, and wellness; prevention of sexually transmitted diseases; and so on. The program includes annual training of leadership (i.e., commanders and health care providers) in prevention programs. Program implementation targets, in order, service members and their families, military bases, and, finally, surrounding communities. It specifies a clear chain of command regarding leadership, training, responsibility
for implementation, and dissemination from the base to the surrounding community. Although there are no published studies on the efficacy of CoRC, the IOM (2013b) concluded that CoRC provides a good model for standardizing prevention training and delivery across the military branches and that it should be evaluated to determine its efficacy.
The New Orientation to Reduce Threats to Health from Secretive Problems That Affect Readiness (NORTH STAR) program is a community-based framework for the prevention of substance problems, family maltreatment, and suicide. It is an integrated delivery system involving commanders and providers partnered with Air Force community action and information boards at each of the 10 major commands (Heyman et al., 2011). The partners at each command selected the programs that matched their specific risk and protective factor profiles using a guide on evidence-based programs that called for rating the programs according to evaluation outcomes and targeted risk and protective factors. The guide also includes training, implementation, and survey evaluation protocols. The use of a framework, delivery system, and guide to select prevention programs that fit a particular base’s risk and protective factor profile is based on extensive community-based prevention research strategies that have been evaluated in civilian populations (Heyman and Smith Slep, 2001; Pentz, 2003; Riggs et al., 2009). Studies of the effectiveness of the NORTH STAR program indicate that the program is promising. A randomized controlled trial of the program involving 24 Air Force bases and more than 50,000 active-duty military members found reductions in alcohol abuse and prescription drug use (as well as suicidality and partner physical abuse), after controlling for the level of integrated delivery system functioning and command support (Heyman et al., 2011).
In addition to the CoRC and NORTH STAR programs, Enforcing Underage Drinking Laws (EUDL) is another promising Air Force program. EUDL is a pilot program designed to reduce drinking and associated alcohol-related misconduct among underage active-duty Air Force members. The program funds the development of broad-based community coalitions to implement environmental prevention strategies that reduce the availability and consumption of alcoholic beverages by underage service members. The strategies employed include (1) enforcement aimed at reducing the social availability of alcohol, (2) compliance checks at alcohol establishments, (3) driving-under-the-influence checks, (4) education of state legislatures and development of local policies, (5) a media awareness campaign, and (6) provision of alternative activities to alcohol use. (See the section about environmental strategies below for more information about this type of SUD prevention.) Evaluation results from the five sites showed significant reductions in arrest rates for minors in possession of alcohol and for driving under the influence, both within sites and compared with control communities (Spera et al., 2010, 2012). Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b) reported that there are currently no plans to expand it to all Air Force bases; however, some of its components will be implemented within other Air Force–wide initiatives.
Service Member Education and Training
DOD-wide policies (DODD 1010.1 and DODD 1010.4) call for the provision of education to ensure that personnel understand the implications of not adhering to DOD policies concerning the use of alcohol and other drugs. However, the policies provide little or no guidance for prevention strategies involving large-scale efforts to educate individuals on the risks and health consequences of the use of alcohol and other drugs.
Each service has specific policies for providing education and training. Alcohol and other drug abuse prevention curricula are included in the general military training provided by the services. The nature of the information and the frequency with which it is provided vary by service, but generally training entails providing service members with information about substance use policies, responsible behavior, risks and consequences of use, and available SUD programs and services.
In addition, each of the services has policies that focus specifically on training individuals in leadership roles to identify early substance abuse problems among their personnel (IOM, 2013b). These training programs vary among the services but can include the training of commanders and supervisors to recognize risk factors, serve as role models, and provide support for prevention. For example in the Navy, senior Navy personnel act as alcohol and drug control officers and provide guidance to drug and alcohol program advisors (DAPAs). DAPAs manage substance abuse prevention programs and conduct prevention education courses, including Alcohol-AWARE, Personal Responsibility and Values Education and Training, Alcohol and Drug Abuse Management Seminar for Leaders/Supervisors, and Skills for Life. In the Air Force, Airman Leadership School or Non-Commissioned Officer Academy students receive education and training that emphasize leadership in delivering prevention, the identification and referral of substance abusers, and education and counseling processes.
Research emphasizes the importance of training military leaders to identify at-risk personnel as early as possible in order to reduce risk of alcohol-related problems (Bray et al., 2013; IOM, 2013b). Leadership skill building should focus on how best to approach military personnel in a way that encourages help-seeking behavior and reduces defensiveness, negative attitudes, and stigma (Bray et al., 2013). Little is known about the quality of the SUD training and education provided in the military. The committee authoring Returning Home from Iraq and Afghanistan (IOM, 2013b) did not receive data or information about the theoretical underpinnings of the training and education programs, effects and outcomes, the proportion of service members who receive the education and training, or methods of delivery.
Screening and Brief Intervention
Routine screening and brief interventions for alcohol misuse within primary care settings are two effective approaches used by the military to deal with alcohol abuse. The Screening, Brief Intervention and Referral to Treatment (SBIRT) model is an evidence-based, comprehensive psychological health approach for the prevention of and intervention in risky alcohol use. The model includes screening for at-risk drinking, providing a brief intervention, and providing referrals to specialty substance use treatment for those who have alcohol dependence (IOM, 2013a). Evidence supporting the efficacy of the SBIRT model is not yet as plentiful or compelling for drug misuse as it is for alcohol misuse. It is also important to note that the effectiveness of SBIRT programs can depend on their fidelity, application, and comprehensiveness, and significant staff training and continuing monitoring are needed to maintain their effectiveness (IOM, 2013a).
Environmental Strategies
In addition to efforts aimed at affecting individual behavior, there are also system-level or environmental prevention strategies that target the community at large. Environmental
prevention strategies are directed at community norms, institutions, attitudes, and policy regulation and can be highly effective (SAMHSA, 2012). For example, during the past several decades, anti-smoking campaigns have resulted in major reductions in smoking initiation and tobacco use through a combination of higher prices (i.e., taxation), restrictions on where use is permitted, and changed social norms about smoking. In Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b), the committee concluded that the military has a unique opportunity to communicate consistent messages about drinking, illicit drug use, and non-medical use of prescription drugs and to control environmental factors driving heavy drinking and prescription drug misuse. Such controls include restricting availability, increasing cost, and limiting permitted times and locations for the use of legal drugs.
Until recently, the military had few control measures directed at changing environmental factors that contribute to alcohol misuse. However, in August 2013 reports in the Military Times announced that commanders in four major Army garrisons were, or were considering, restricting sales of liquor at post exchange stores operated by the Army and Air Force Exchange Service. The types of restrictions would vary by garrison and would include halting the sale of hard liquor (not beer and wine) or the sale of all alcohol at certain store locations and limiting the hours that liquor is sold (Gould, 2013). At this time, the committee is not aware of any DOD-wide effort along these lines, but it sees this as a positive development. It is a first step in addressing problem drinking and the military’s inconsistent messaging surrounding alcohol, which includes having a zero-tolerance policy while promoting the availability of alcohol.
In response to the growing problem of prescription drug abuse in the military, DOD has taken steps to foster a military medical practice environment that reduces the risk of prescription drug abuse (IOM, 2013b). For example, DOD’s Pharmacoeconomic Center (PEC) developed systems and tools for monitoring the use of controlled substances prescribed for individuals. Despite noting some limitations,8Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b) found PEC’s activities and reporting tools to be comprehensive. The Army recently set limits on the length of prescriptions for controlled substances as well as on the quantity dispensed (U.S. Army, 2011). Service members who need ongoing treatment with controlled substances will have greater contact with their prescribing physician, and those who are prescribed these medications on a short-term basis will not be allowed to use them beyond 30 days.
The environmental control measures taken by DOD to reduce misuse of alcohol and prescription drugs are consistent with research in this area. For alcohol, Babor and colleagues (2010b) discuss four environmental policy approaches that are appropriate in the military context: strategies controlling affordability through pricing and taxation, restricting the availability of alcohol for purchase, altering the context in which alcohol is consumed (e.g., requiring and implementing age identification), and preventing impaired driving through, for example, sobriety checkpoints and random breath tests. Partnerships within the larger communities in which military bases are located are also integral to a solid environmental prevention strategy (Spoth et al., 2011).
____________________
8 The PEC data systems do not include in-theater pharmacy data in settings where there are no electronic medical records. Nor are they equipped to assess illicit activity on the part of service members who obtain prescriptions from civilian providers and retail pharmacies.
For preventing illicit drug use and abuse of prescription drugs, Babor and colleagues (2010a) discuss three environmental, population-level approaches that are pertinent to the military. The first is supply control, which involves disrupting the production, distribution, and sale of drugs. Military commands can work with the communities around the bases to help implement actions (e.g., the arrest of traffickers and dealers) that disrupt local drug markets at the street level. A second approach involves the criminalization or decriminalization of drug use. Evidence on the effectiveness of both criminalization and decriminalization comes from U.S. and international studies (Hughes and Stevens, 2010), none of which has been based on military populations. Criminalization of drug use in the military is driven in part by the need for combat readiness, which is not an imperative in civilian populations. The use of prescription regimens is the third approach. Such regimens focus on controlling the safety, storage, and distribution of prescription drugs. Some of these measures entail tight regulation of prescription dispensing and control and over-the-counter sales, physician education, and increased enforcement of prescription regulations.
In addition, the Office of National Drug Control Policy has environmental prevention strategies that correspond with the prescription regimes of Babor and colleagues (Babor et al., 2010a; ONDCP, 2013). These include education for parents, children, patients, and providers; prescription drug monitoring programs; responsible prescription drug disposal programs; and proper implementation and enforcement of related policies and laws.
Recovery
Navy MORE (My Ongoing Recovery Experience) is the only DOD recovery program that the committee is aware of. Established in 2010, Navy MORE is targeted to substance abusers in their recovery period 12 to 18 months after the conclusion of formal substance use treatment. It is a Web- and phone-based program run by a contractor for the Navy Bureau of Medicine and Surgery. Each Navy MORE recipient is assigned a recovery coach who is a licensed alcohol and drug counselor trained in relapse prevention. Coaches are connected to clients via phone and the Internet. Clients in Navy MORE are given 7 online assessments over the course of 12 months. After filling out the assessment, clients receive a tailored educational recovery program designed according to their own unique needs in recovery. Navy MORE also sponsors workbook activities designed to enable clients to explore the challenges of recovery through hypothetical situations. Furthermore, the program’s website has a “commitment tool” with which clients are able to track and report on their commitments and goals for recovery. The website also has an online library of more than 160 articles, fact sheets and videos and also a “serenity” tab that helps clients manage stress through meditation, prayer, affirmations, sober fun ideas, inspiring movies, and humor. Clients can remain connected with the recovery community through online tools, including an alumni bulletin board. The design of Navy MORE is based on evidence-based practices and milestones of recovery originating from the Butler Center for Research at Hazelden. Navy MORE is planning to perform an evaluation of its effectiveness (Hazelden Foundation, 2013; RAND Corporation, 2013).
Summary
By focusing on drug testing as prevention, DOD and the different military branches may fail to implement more evidence-based prevention strategies that have proven effectiveness, such as environmental strategies (e.g., reducing availability or raising the price of alcohol on bases).
DOD policies provide little or no guidance for other prevention strategies, such as large-scale efforts to educate individuals on the risks and health consequences of alcohol and other drug use, indicated prevention programs for those identified as being at risk, prevention efforts aimed at military families, and environmental prevention strategies. Although some branches have policies that address these additional prevention strategies, DOD’s delegation of SUD prevention to the individual branches results in the inconsistent availability of SUD prevention services for service members and their families (IOM, 2013b; Weinick et al., 2011).
As described in a previous committee’s review (IOM, 2013b), programs exist that appear to meet prevention needs in that they are appropriate to the populations served, are theory based, address multiple risk factors, and have evaluated psychological outcomes. However, many of these programs adapted materials and concepts from civilian prevention programs and have not been tested with military populations. Furthermore, many of the prevention efforts appear to be focused on campaigns, Internet games, and camps or events with no research evidence that they affect substance use.
Reintegration has been defined as the process of transitioning a service member back into personal and organizational roles following deployment (DCOE, 2012b). This period includes positive events, such as reunions with family and friends and a return to one’s pre-deployment life, but it is also a time during which the service member faces increased tension at the personal, family, and work levels and exacerbation of deployment-related stress conditions.
Characteristics of the service member and his or her military status influence the length and nature of the reintegration period (DCOE, 2012b). The reintegration period for active-duty service members is generally a defined time-frame that occurs before, or concurrent with, preparations for a new mission or deployment. Veterans who transition out of active-duty status and members of the National Guard and reserve components may experience a more extended reintegration period as they transition back into a permanent civilian life. A significant concern for National Guard members and reservists is that they may not have ready access to reintegration resources at military facilities following their return from a deployment (DCOE, 2012b). Wounded service members experience additional reintegration challenges and may have unique needs for reintegration support. Studies have concluded that the current understanding of reintegration is extremely limited and should be expanded upon with significant research (Currie et al., 2011). This understanding is important to the development of interventions targeted at facilitating the reintegration process.
Currently, each service has its own distinct approach to the deployment cycle, and each defines the process of reintegration slightly differently, making it difficult to develop DOD-wide programs and initiatives for returning service members and their families (DCOE, 2012b). Moreover, although many resources to support reintegration exist, very few have well-defined policies, procedures, and metrics for assessing the needs and outcomes of the populations they serve (DCOE, 2012b).
The sections below describe four programs—third location decompression, Real Warriors, Yellow Ribbon Reintegration Program, and Wounded Warrior Programs—that are
intended to support reintegration following deployment. The discussion includes what the committee has found in the literature about the evidence and effectiveness of these programs.
Third Location Decompression
Third location decompression (TLD) is a program held at the end of deployment and before reentry to home in a comfortable and relaxing stopover of 1 to 5 days in duration. The rationale for the program stems from research showing that Vietnam veterans with difficult homecoming experiences were more likely to have prolonged psychopathology (e.g., Borus, 1973; Koenen et al., 2003). While widely implemented by UK and Canadian Armed Forces, the U.S. military has used TLD in a more limited manner for specific units, such as the Marine Special Operations Command (Military Suicide Report, 2012) and some personnel in the Air Force and in the Naval Special Warfare Command (Garber and Zamorski, 2012).
The TLD program of the Canadian Armed Forces has two goals: to minimize distress and offer guidance on how to manage common problems related to the transition; and to promote help-seeking for psychological health and transition problems by reviewing personal signs and symptoms and refuting common misperceptions. Those goals are addressed by 3 hours of psychoeducation over the course of a 5-day stay at a resort in Cyprus. One hour is devoted to Battlemind Training, and the other 2 hours are spent on two electives on such topics as “Coping with Stress and Anger,” “Healthy Relationships,” and “Post-Deployment Reintegration From the Veteran’s Perspective.” Veterans’ perceptions of the program, measured at program completion and 4 to 6 months later, were studied by Garber and Zamorski (2012). They found that 95 percent of the 3,300 participants endorsed the statement that “some form of TLD is a good idea,” 74 percent endorsed the statement that TLD “made reintegration easier for me,” and 60 percent endorsed the statement that TLD “made reintegration easier for my family.”
Another evaluation compared the original Canadian TLD program with a new one (Zamorski et al., 2012). The purposes remain the same, but the new program scuttled Battlemind Training in favor of a review of the difficulties and accomplishments of the mission, a greater focus on assessing the severity of transition and psychological health problems, and a focus on the physiology of the human stress response. The evaluation of 22,113 Canadian personnel returning from Afghanistan found that the new program was superior to the old in terms of perceptions of the program’s value, in confidence of psychological health knowledge and abilities, psychological health literacy, and sense of responsibility toward others. It was also found superior in self-management of psychological health problems and more positive attitudes about psychological health care. Neither of the evaluations assessed psychological health symptoms or mental functioning.
The UK Armed Forces sponsors a 24- to 36-hour TLD program with two distinct psychoeducational briefings dealing with identification and management of psychological health problems and with easing reintegration with family and friends. In an evaluation of TLD attendees (n=1,407) and non-attendees (n=1,664), Jones and colleagues (2013) found a positive effect on psychological health. The TLD group was less likely to report PTSD symptoms than those in the control group (3.0 percent versus 4.5 percent, AOR 0.57, 95% CI = 0.36–0.91). Those in the TLD group were also less likely to report multiple physical symptoms than the controls (6.6 percent versus 9.4 percent, AOR 0.65, 95% CI = 0.45–0.95), and less likely to report harmful levels of alcohol use (16.8 percent versus 19.5 percent of controls, AOR 0.74,
95% CI = 0.54–1.00). There were no differences in readjustment as measured by a special selfreport scale and no differences on the General Health Questionnaire, which assesses common psychological disorders. Attendees with medium combat exposure were less likely than controls with medium combat exposure to report PTSD symptoms and multiple physical symptoms. Attendees with low combat exposure were less likely to report symptoms on the General Health Questionnaire. The findings with respect to combat exposure were counterintuitive, as one would expect high combat exposure to carry the largest effects. One possible explanation suggested by the study authors is that a high combat exposure and high PTSD symptomatology may limit the service member’s ability to engage in the TLD process. The authors concluded that TLD should continue to be used for deployed military personnel.
Real Warriors
Real Warriors is a high-profile multimedia DOD education campaign that employs public service announcements, social media, podcasts, a website, fact sheets, and press releases. The campaign’s stated purposes are to build resilience, facilitate recovery, and support reintegration from deployment. The campaign is sponsored by the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury. The campaign features real stories of service members who reached out for help and had beneficial outcomes, such as learning coping skills, maintaining security clearances, and succeeding in their careers. In one of the campaign’s takehome messages, the Army declared that “Real Warriors are proving through their example that reaching out is a sign of strength that benefits the entire military community” (Department of the Army, 2013).
The utility of the Real Warriors campaign has been assessed by the RAND Corporation (Acosta et al., 2012). RAND conducted a literature search to discern best practices and empirically defined features of effective psychological health media campaigns, it convened an expert panel, and it performed a content analysis of the Real Warriors website, among other methods. RAND’s assessment found that the campaign’s core messages, while appropriate and relevant, were not articulated anywhere on the Real Warriors’ website. The assessment also found that the video profiles of personal stories of service members coping with psychological illness were compelling and constituted the heart of the campaign. However, the website was found to be so overwhelming that it caused “information overload.” RAND’s assessment also found that while most of the campaign’s social media tools were viewed as useful, use of the tools was still fragmentary and not all partner organizations were actively involved in the campaign's dissemination. The RAND assessment was limited insofar as it did not perform an evaluation of the effectiveness of the campaign in terms of achieving health outcomes, such as gains in knowledge, symptom reductions, or changes in perspectives on seeking help. Although public education campaigns are a standard method of encouraging help seeking and promoting resilience, systematic reviews of similar campaigns for other populations find that they have only modest effects in curtailing suicidal behavior, increasing help seeking, or increasing use of antidepressants (Fountoulakis et al., 2011; Mann et al., 2005).
Yellow Ribbon Reintegration Program
The Yellow Ribbon Reintegration Program (YRRP) provides support to reserve component service members and their families before, during, and after mobilization. This population is eligible for an array of services and benefits at the different phases of mobilization;
however, the resources are often difficult to navigate and many are located on or near active military installations—away from where many reserve component service members live. Through one-on-one meetings and workshops, the YRRP helps reserve component service members and their families connect to the health, financial, and employment services to which they are entitled (DCOE, 2012b).
The program activities are structured by deployment phase: pre-deployment, deployment, demobilization, and post-deployment. To find program activities, users can search the YRRP online event portal. Service members (or family members) using the portal can filter events by location, service branch, and deployment phase to find events that are relevant to them. Some, but not all, of the activities are mandatory (Yellow Ribbon Reintegration Program, 2013a).
One recent notable reintegration component of the YRRP is Hero2Hired, a Web-based comprehensive career services program that seeks out employers committed to hiring reserve component service members. Using the Hero2Hired website, reserve component service members and veterans can search for positions in private industry that match well to their military specialties. The program also provides resume assistance, interview preparation, and skills assessment tools to help reserve component service members match their skills and interests with potential careers (Yellow Ribbon Reintegration Program, 2013b).
In FY 2012, YRRP provided information and resources to 248,252 individuals—106,468 of which were family members—at 2,028 events. Based on event participant survey data, 80 percent of respondents were satisfied with the programming, and 91 percent reported that the YRRP event helped increase their knowledge of available support programs and resources. Nearly 80 percent of those surveyed noted an increase in their ability to communicate with their families, manage deployment-related stress and anxiety, manage finances and employment issues, and prepare for their continued military service (Yellow Ribbon Reintegration Program, 2013b).
Wounded Warrior Programs
The DOD Office of Wounded Warrior Care and Transition Policy, which was established in 2008, seeks to ensure that wounded, ill, injured, and transitioning service members obtain high-quality care (both medical and non-medical) and experience a seamless transition back to active duty or to civilian life. The office supports the programs offered by each military service’s Wounded Warrior program and provides assistance and guidance to these programs. However, the office does not have the authority to direct the service-specific programs (GAO, 2012). The office developed and distributes several handbooks, among them a compensation and benefits handbook that covers recovery resources, medical care, DOD pay, the disability evaluation system, and reintegration. Another handbook addresses the resources available to caregivers, who are eligible for receipt of DOD compensation for their efforts on behalf of a catastrophically afflicted service member. The office also sponsors an education and employment initiative designed to assist recovering service members identify their skills and assist them in matching those skills with education and career opportunities. Finally, the office sponsors Operation Warfighter, which supports internships that place wounded warriors in real-world jobs and provides special supports to help them remain employed (DOD, 2013e).
In an evaluation report of DOD’s and VA’s progress in implementing policies on care, management, and transition of recovering service members and veterans, the Government
Accountability Office (GAO) found that the DOD Wounded Warrior programs were not always accessible to those who needed them (GAO, 2012). The two main reasons were inconsistent methods for referrals and inconsistent eligibility criteria. For example, some Wounded Warrior programs restrict eligibility to those who only have combat-related injuries or illnesses, while others allow non-combat injuries as well. Additionally, GAO found that the Office of Wounded Warrior Care and Transition Policy lacked sufficient leadership and authority over the individual services. Currently, the office cannot direct how the services implement their Wounded Warrior programs. GAO identifies this as the main reason for program inconsistencies across the servicespecific programs (GAO, 2012). Furthermore, GAO found, there is currently no body that collects information regarding the performance of the programs.
GAO recommended that DOD create an office to oversee and monitor activities of the wounded warrior programs. Among its tasks, the office should ensure uniform eligibility criteria and create a common mechanism to monitor the performance of Wounded Warrior programs. GAO also recommended more vigorous leadership to resolve the challenges with care coordination, disability evaluations, and electronic sharing of medical records (GAO, 2012). The Office of Wounded Warrior Transition Policy is currently conducting a Wounded Warrior program assessment at six sites (RAND Corporation, 2013).
As discussed in Chapter 4, sexual assault in the military is a significant problem that is associated with various psychological health disorders among victims, including PTSD, depression, and SUDs. The Sexual Assault Prevention Response (SAPR) program, which was established in 2005, oversees DOD policy and programs pertaining to military sexual assault (DOD, 2013f). A recent DOD directive instructs all military services to align their sexual assault prevention policies with the central SAPR program (DOD, 2013a). The SAPR program is mandated to focus on prevention, education and training, response capability, victim support, and reporting procedures (DOD, 2013c). DOD policy requires that sexual assault awareness and prevention training occurs at accession, as part of all professional military education activities, and during pre-command training.
A core tenet of the SAPR program is prevention at six levels of military culture and society. Those six levels are (1) strengthening individual knowledge and skills, (2) promoting community education, (3) educating providers, (4) fostering coalitions and networks, (5) changing organizational practices, and (6) influencing policy and legislation. The aim of this approach is to engage members of the military at all levels to do their part to help reduce sexual assault (DOD, 2013a).
Although each service branch must adhere to the central SAPR policy, there is some flexibility for branches to adapt programs to reflect their own individual cultures and structures. One of the primary strategies for preventing sexual assault in the military is to encourage service members to look out for each other, recognize potentially harmful situations, and intervene if they suspect unwanted sexual contact is likely to occur. This behavior is encouraged using a variety of methods. In the Army, for example, the I.A.M. Strong (Intervene. Act. Motivate.) campaign trains soldiers at all levels to create a shift in culture in which precursors to sexual assault are rejected and soldiers continually look out for each other. The program uses the Army’s existing warrior ethos of “never leaving another comrade behind” to encourage this shift
(DOD, 2013d). Additionally, commanders are trained to help create an environment of respect that encourages soldier intervention, reporting, and rejection of sexual innuendo and suggestion. The Army’s sexual assault prevention program also has a website with training materials, policies, and video content (DOD, 2013d). Programs in other branches have a less visible online presence, but all encourage a combination of bystander intervention and the training of leaders to help foster a culture that rejects attitudes and behavior conducive to sexual assault, creates an environment of respect, and encourages the reporting of sexual assault after it occurs.
Because sexual assault is often unreported (and a goal of the SAPR program is to increase reporting), looking at the reported cases of sexual assault in the military is not necessarily a good indicator of the program’s effectiveness at reducing sexual assaults. That said, reported sexual assaults among women rose significantly from 4.4 percent in fiscal year (FY) 2010 to 6.1 percent in FY 2012. Among men, there was no significant change between FY 2010 (0.9 percent) and FY 2012 (1.2 percent). However, SAPR also looks at other measurable outcomes, such as changes in knowledge, skills, and behaviors (DOD, 2013a). Overall, the military achieved nearly universal training of its service members in 2012 (96 percent of activeduty women and 97 percent of active-duty men received training). Service members also generally rated the training highly: 94 percent of men and women thought the training effectively explained what is considered sexual assault; 94 percent of men and women agreed the training communicated that alcohol may increase the likelihood of sexual assault; 93 percent of men and women felt the training taught them how to avoid situations that may be conducive to being a victim of sexual assault; and 92 percent of women and 93 percent of men agreed that the training taught them how to intervene when they witnessed a potential “risky situation” (DOD, 2013a).
In January 2012 the SAPR completed a rapid assessment of the commander training provided by the branches of service to officers (in pay grades O-4 through O-7) before they assumed command (DOD Sexual Assault Prevention and Response Office, 2012). This exercise was directed by (and delivered to) the Secretary of Defense. Although the training does appear to reach most service members, this exercise arose out of the concern that some of the servicespecific elements of the SAPR program are not standardized across the services, are inconsistent in their application, and are missing critical evaluation components needed to measure their effectiveness (DOD Sexual Assault Prevention and Response Office, 2012). The assessment found that most of the program’s messages were consistently presented and that the training appeared to be fully integrated into the pre-command curriculum. It also found, however, that the content varied across the services and that certain core SAPR messages were missing from some training programs. Additionally, the report noted that there were no assessments of training participants to ensure that they had mastered the core SAPR concepts, and it suggested that data should be collected and assessed to assist in validating the training curriculum (DOD Sexual Assault Prevention and Response Office, 2012). SAPR recommended that the Secretary of Defense direct the services to ensure that the core concepts of SAPR training are incorporated into the services’ training materials and also that the revised training curricula be submitted to the Under Secretary of Defense to ensure they are in compliance with SAPR standards (DOD Sexual Assault Prevention and Response Office, 2012). DOD Instruction 6495.02 directs the services to comply with this recommendation (DOD, 2013c). That instruction also requires the services to submit to the Under Secretary of Defense quarterly and annual reports that assess the implementation of policies and procedures, advocacy activities (planned and completed), and data on restricted and unrestricted reports of sexual assault within the given service (DOD, 2013c).
The care and support of military families is considered a national security policy priority because of the integral role that family members have in supporting service members and, therefore, the mission of the military. This section describes some of the DOD interventions for preventing psychological health problems among families and reviews what the committee has found in the literature concerning the evidence and effectiveness of these programs.
There are hundreds of family-related programs (DOD-wide and service-specific), and the policy and management responsibilities for them range across the DOD enterprise. The Annual Report to Congress on Plans for the Department of Defense for the Support of Military Family Readiness (DOD, 2011) contains a descriptive list of military family-readiness programs and activities for each of the military services and for the Office of the Secretary of Defense (OSD); however, it is not readily apparent which ones are considered prevention programs. OSD offices with family-related programs and activities include
• Office of the Deputy Assistant Secretary of Defense for Health Affairs;
o Force Health Protection and Readiness
o TRICARE Management Agency
o Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury
o Uniformed Services University of the Health Sciences’ School of Medicine
• Office of the Assistant Secretary of Defense for Reserve Affairs
• Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy
• Office of the Deputy Under Secretary of Defense for Wounded Warrior Care and Transition Policy
The Office of the Assistant Deputy Secretary of Defense for Military Community and Family Policy (MC&FP) is responsible for family support policies and programs. Program areas include family center operations, child care, youth programs, family advocacy, relocation, transition support services, and support during mobilization and deployment. MC&FP has responsibilities for dependents’ education programs, community programs, and coordination of the services of nonprofit agencies. In 2008 MC&FP launched the Joint Family Support Assistance Program to provide services solely to National Guard and reserve families, particularly those who live beyond the reach of services available on military installations (Blaisure et al., 2012). A major MC&FP program includes Military OneSource and Military and Family Life Counselor services, which are discussed later in the section on non-medical counseling services.
Recent Reviews of Family Programs
The committee examined several reviews that assess military family programs. A common finding is that there are gaps in the evidence supporting the effectiveness of interventions for military families. As mentioned in the beginning of this chapter, the RAND Corporation compiled a list of DOD programs that address psychological health and traumatic brain injury (Weinick et al., 2011). Of the 94 programs classified as prevention/resilience
programs, 47 serve families in some capacity, and fewer than half (21) of those include an evidence-based intervention (see Appendix H) (RAND Corporation, 2013).
Similarly, the committee authoring the 2013 IOM report Returning Home from Iraq and Afghanistan (2013a) assessed family-focused programs and found a lack of information on the effectiveness of broad-based, universal prevention efforts targeting military families and children. It found that many interventions for family members have been developed and tested in civilian communities but not in military populations (see also Lester and Flake, 2013). That committee recommended that DOD increase its efforts to identify, develop, and test new prevention (and treatment) interventions targeted toward military families, including interventions directed specifically at children and adolescents. It also recommended that DOD include nontraditional families (e.g., same sex couples, non-married domestic partners, families with stepchildren, etc.) in its research and policies. This committee echoes that sentiment.
The DOD Military Family Readiness Council9 annually provides to Congress an assessment of the adequacy and effectiveness of the military family readiness programs and activities. The Council’s 2012 report (DOD, 2012c) made the following recommendations about strengthening program evaluation for family support programs:
1. Review existing programs and prepare them for program evaluation.
2. Include evaluation components when a new program is developed and implemented. When possible, these programs should be modeled on research-based programs.
3. Include funding for assessment in the program’s budget.
The next section describes some of DOD’s efforts to address gaps in program evidence and evaluation that were identified by the recent reviews of family programs.
Program Evaluation Projects
OSD recently launched a large-scale 5-year (FY 2013-FY 2017) program evaluation of DOD-wide family support programs (DOD, 2012c). It builds on a program review project started by MC&FP, in collaboration with the Penn State University Clearinghouse for Military Family Readiness, to assess the effectiveness of military family support programs. The objective of this effort is to measure the impact of family support programs across DOD and to move the portfolio of family support programs from being assessed with performance measures toward being assessed with outcome measures. The evaluation plan calls for the evaluation of two major OSD-sponsored programs including the non-medical counseling program that involves face-to-face counseling from Military OneSource and Military and Family Life Counselor services, and the Spouse Education and Career Opportunities program.
IOM (2013a) reported on an evaluation tool developed by Miller and her colleagues at the RAND Corporation (2011) that measures the performance of military family readiness programs.10 Rather than developing program-specific evaluation instruments, they developed an adaptable survey instrument to measure five aspects of family readiness programs: (1) the problems and needs of service members and their families, (2) the actions families take to address their needs, (3) their satisfaction with the resources they use to meet their needs, (4) why
____________________
9 Established in 2008 under section 1781a of title 10, U.S. Code, and the Federal Advisory Committee Act of 1972.
10 The research was sponsored by the Under Secretary of Defense for Personnel and Readiness.
certain resources were used and others were not (either military, civilian, formal, or informal resources), and (5) the effectiveness of the resources on retention and readiness. The authors noted that by measuring these issues rather than focusing on the individual programs, service providers and military leadership at all levels can better understand the needs of their service members, identify unmet needs among specific demographic groups and locations, and adjust service provision as needed to more effectively meet their needs (Miller et al., 2011). It is not known whether DOD has used or plans to use the survey instrument in any capacity.
Selecting a Sample of Family-Focused Programs for Assessment
In the sections that follow, the committee describes a sample of family-focused prevention programs administered by DOD. The committee did not conduct an exhaustive review of family prevention programs given the fast-track nature of this study and a determination that there was little value in duplicating the program reviews discussed above. The committee concentrated its assessment on a sample of DOD prevention programs and interventions with strong relevance to the targeted areas of this study and for which significant information and research findings were available in the literature. As such, the interventions discussed in the section should not be considered representative of all DOD prevention interventions. The programs are organized into the following areas: family-centered resiliency, non-medical counseling, couples education, military children, SUD prevention for military families, and family violence.
Family-Centered Resiliency
Families OverComing Under Stress (FOCUS) is a family-centered resiliency training program developed by researchers at the University of California, Los Angeles, and Harvard University and implemented under contract with the Navy. Adapted from an evidence-based family-centered preventive intervention for civilian families, the FOCUS program is designed to meet the specific needs of military families facing combat operational stress associated with wartime deployments, reintegration issues, and combat-related physical and psychological injuries. FOCUS is a selective prevention program, as families entering the program may be proactively seeking to enhance coping in the face of increased challenges or may already be experiencing deployment distress (Lester et al., 2012).
Designed to enhance resiliency—defined as “engagement in adaptive behaviors and achieving developmental milestones in the face of stressful or traumatic life events” (Lester et al., 2011a, p. 19)—FOCUS entails a series of integrated prevention services and employs a family narrative approach. Among these are eight structured family-training sessions that are designed to increase resiliency skills in the domains of communication, emotion regulation, managing trauma or loss reminders, problem solving, managing traumatic stress, and goal setting (Lester et al., 2011a). In addition, FOCUS uses a standardized psychological health assessment to customize service delivery and screens for a range of psychological health problems (e.g., PTSD, depression, suicidal ideation) in adults and children, supporting referrals to psychological health or other social support services for family members with an untreated significant psychological health problem or ongoing domestic violence or active substance abuse problems. Between 2008 and 2011, FOCUS delivered family resiliency training and parent child skillbuilding groups to more than 5,000 military children, spouses, and service members and also
provided family-centered consultations, briefings, and educational workshops to more than 100,000 family members, providers, and other community members (Lester et al., 2013).
Lester and colleagues (2012) conducted a pre–post evaluation at the time of the program’s initial implementation period which included 331 families with a mean of 4.5 servicemember deployments. Post-intervention findings showed improved family function11 and adaptation among FOCUS participants (p<0.001). There were significant reductions in symptoms of anxiety and depression among parents (p<0.001) and significant reductions in emotional and behavioral problems for boys and girls in all age groups (p<0.001).
A subsequent study on the impact of FOCUS by Lester and colleagues (2013) in 280 families with at least 1 active-duty military parent and at least 1 child aged 3 or older had two goals: to develop an understanding of how different type of distress (deployment-related stress, posttraumatic distress, family functioning, child adjustment, spousal adjustment) are related among families that participated in the program; and to evaluate the pathways of program impact on child psychological health symptoms using longitudinal assessment data following program participation. The findings confirmed the researchers’ theory that psychological stress in military families reverberates throughout the family. In addition, the findings showed that at the time that families entered the program, distress levels among the service-member parent, civilian/caretaking parent, and children were all significantly related. Consistent with the initial evaluation, this study demonstrated that FOCUS improved family functioning, which can be expected to have helped reduce child distress. The authors acknowledge the limitations of conclusions drawn due to the open nature of these service evaluations and note that additional data from a randomized design with a control condition would offer more definitive support for the intervention.
Another resiliency program for families is Military Pathways, a multi-component program that uses universal and selective prevention approaches designed to help educate and support military families in coping with deployment stress, recognizing signs and symptoms of psychological health problems, and building resiliency and to help service members reconnect with their children. Program components include educational materials and anonymous, psychological health and alcohol-use self-assessments accessible online, via the phone, and through special events held at installations (Military Pathways, 2013). The self-assessments address PTSD, depression, generalized anxiety disorder, alcohol use, and bipolar disorder. After completing the self-assessment, individuals receive referral information, including information about services provided by TRICARE Health Program, Military OneSource, and Vet Centers. In addition, the family resiliency kit and a special program for youth (Signs of Suicide, or SOS) are special components aimed directly at military family members; trained paraprofessionals deliver the family kit, and school professionals (not specified) deliver the SOS program to youth in schools. A theoretical basis is implied by program content that includes empowerment building and social and family support seeking (IOM, 2013b).
Military Pathways targets active-duty service members and their families primarily at entry into the military and pre-deployment; however, the online, telephone, and video components can be accessed at any stage of military life. The program reaches more than 305,000 active-duty service members and their families each year (Weinick et al., 2011). Trials to evaluate the effectiveness of the self-screening and youth program components are ongoing
____________________
11 Measured with the McMaster Family Assessment Device.
(Weinick et al., 2011), but the committee is not aware of published outcome data on the alcohol, PTSD, or psychological health screening components.
Non-Medical Counseling
Non-medical counseling refers to short-term, problem-focused counseling designed to address general conditions of living; it addresses such issues as stress management, marital problems, parenting issues, grief, and crisis intervention. (Medical counseling, by contrast, is designed to address long-term, medically diagnosable issues, such as substance abuse, psychological illness, or PTSD.) DOD offers confidential, free non-medical counseling sessions to all active-duty, National Guard, and reserve members and their families. Services are available through Military OneSource and the Military and Family Life Consultant (MFLC) program. In FY 2011, Military OneSource provided more than 313,000 in-person counseling sessions (DOD, 2012a). Data regarding the number of telephone or online counseling sessions completed by Military OneSource were not reported. The MFLC program provides services, including evidence-based problem solving–focused behavioral and short-term counseling to active-duty service members and families on or off military installations. Support is provided to the reserve components for mobilization, deployment, and reunion activities as requested by reserve unit commands. In FY 2011 the MFLC program completed 6.9 million face-to-face contacts (DOD, 2012a).
DOD sponsored two studies assessing the effectiveness of the counseling services (DOD, 2012a). In one study, conducted in 2010 in collaboration with Virginia Polytechnic University, researchers collected data from an assessment tool completed by counseling participants in order to measure the impact of counseling through the MFLC program. The study found that 98 percent of respondents reported that the counseling sessions helped them deal more effectively with their problems and that they would use the service again. Virtually all (99 percent) reported that they received the kind of counseling service they wanted and that they would recommend MFLC services to a friend (DOD, 2012a). In the second study, DOD included questions on the use of non-medical counseling in the May 2010 Military Family Life Survey for military spouses and a paired subset of active-duty personnel. Spouses reported that MilitaryOne Source counseling was the second most utilized source of counseling. More than half found it to be “very useful” (Defense Manpower Data Center, 2011). (The most utilized source is medical counseling sponsored under TRICARE.)
Couples Education
The Prevention and Relationship Enhancement Program (PREP) for Strong Bonds is a scientifically based educational program for couples designed to address the stress on military couples posed by long separations, frequent relocations, and deployment. The program is based on research that shows that couples education is effective at improving couple functioning (Stanley et al., 2010). Its goal is to strengthen the family and prevent divorce by teaching couples skills, principles, and strategies associated with healthy relationships. The program, which is led by trained Army chaplains, includes a 1-day weekday training on post, followed by a weekend retreat at a hotel off post.
Program modules address such topics as communication and effective management skills, deployment and reintegration issues, fun and friendship, and relationship dynamics. An
RCT found that the divorce rate for Army couples assigned to participate in PREP for Strong Bonds was one-third of that for control couples (2.03 percent for Army couples versus 6.2 percent for the control group) when assessed 1 year after the intervention. The study authors concluded that couples education—at least in the short run—can reduce the risk of divorce (Stanley et al., 2010).
It is also worth noting that couples-based cognitive behavioral therapy interventions specifically targeting PTSD are now available. For example, Cognitive Behavioral Couple Therapy (Monson et al., 2012) for PTSD is an evidence-based intervention designed to target both PTSD symptoms and couple functioning; in a randomized controlled trial it was found to lead to a significantly greater reduction in PSTD symptoms and significantly greater relationship satisfaction when compared with a waitlist control.
Military Children
Established in 2010 and funded by the Department of Defense Educational Activity, the Building Capacity Consortium project aims to make civilian school systems more aware of and responsive to the needs of military children. The project serves approximately 117,000 students in 140 schools in 8 school districts in San Diego and Riverside counties in Southern California. Approximately 10 percent of the students served by the program are from military families. The project has three primary aims:
1. Enable public schools to create military-friendly school environments that improve students’ social, behavioral, and academic outcomes;
2. Build each local education agency’s capacity to sustain the initiative long after grant funding ends; and
3. Create an infrastructure for replication and scaling up nationwide (Benbenishty and Esqueda, 2012).
A core component of the project is the placement of University of Southern California master’s of social work students as interns in participating military-connected schools. In this way future social workers are trained about the needs of military children and military-connected schools, and the participating schools are provided with social work services (Astor et al., 2011).
In addition, the project has worked with the state of California, as part of the state’s school-based health survey, to identify and collect data on military children for the first time. This information will help schools track psychological health trends and the needs of military children (Astor et al., 2011). The project also identifies and implements existing evidence-based programs that serve military children. This involves either adapting an existing program that serves military families to work in a school environment or adapting a school-based program that is not military focused to address the needs of military children. Some of the programs the Building Capacity Consortium has scaled up within participating schools include FOCUS, Family Readiness Express, Partners at Learning, A STEM, and Support for Students Exposed to Trauma (Astor et al., 2011).
The project released evaluation reports in 2011 and 2012 that offered project achievements, assessments of intern performance, and feedback from the interns on their training. Also reported were data from the California Health Kids Survey that include behavioral health information on substance use, violence, victimization, school performance, weapons, and
gang membership in the participating schools. Trend data from 2000 to 2011 (the first year of the program) are reported, but no comparison data from non-participating schools are presented (Benbenishty and Esqueda, 2012).
SUD Prevention for Military Families
While some SUD-prevention resources target military spouses and children, no single uniform DOD program provides comprehensive SUD-prevention programming for dependents, and the committee authoring Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b) was not aware of any reports on the effectiveness of prevention resources for this population. Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b) did identify the following programs that exemplify SUD-prevention resources for military family members.
The Red Ribbon campaign is a universal prevention campaign aimed at addressing peer pressure and prosocial bonding in youth as well as parental monitoring. Thus, it is most developmentally appropriate for young military members with families. Red Ribbon Week is an annual campaign that is conducted nationwide in the United States every October both at the community level and on military bases. There is no evidence on this program’s effectiveness, and both military bases and communities vary widely in the activities they sponsor under the auspices of the campaign.
Drug Education for Youth, or DEFY, is a comprehensive prevention program offered by the Air Force, Navy, and Marine Corps. It is aimed at adolescents and consists of a summer leadership camp and a school-year mentoring program. The program’s curriculum includes a variety of topics, including substance abuse prevention and other vital life skills, such as conflict resolution, self-management skills, study skills, leadership, and community service. Substance Use Disorders in the U.S. Armed Forces (IOM, 2013b) did not find any formal outcome evaluations that have been conducted with military dependent participants, so it is unknown whether the program is effective at preventing SUDs for military dependents or at building any of its other targeted life skills.
As discussed earlier in the section on substance use disorders, the EUDL program is a pilot program that showed significant reductions in drinking among underage airmen (Spera et al., 2010). Its aims include making environmental changes in the community that may benefit spouses and child dependents. There are currently no plans to expand it to all Air Force bases; however, some of its components will be implemented as part of other Air Force–wide initiatives.
In studies of the effectiveness of prevention programs with civilian adolescent populations, SUD-prevention programs that focus only on increasing knowledge or changing attitudes have had fewer effects on substance use behaviors than programs that focus on building resistance skills as well as social and life skills (Botvin et al., 1995). The social resistance skills approach to drug use prevention recognizes the role of various social influences. These programs promote ways to avoid high-risk situations—where there is pressure to smoke, drink, or use drugs—and teach knowledge and skills needed to handle social pressure in such situations (Botvin and Griffin, 2004). Evidence-based SUD-prevention programs often address skills that are particularly relevant to military members and their families, such as resisting peer pressure, avoiding high-risk situations, identifying and bonding with individuals who provide social support and a non-use norm, and practicing emotional regulation and impulse control.
Family Violence
In its review of family-focused programs, Returning Home from Iraq and Afghanistan (IOM, 2013a) found little information about the prevention of family violence or abuse in the military. In 2010 GAO concluded that, despite some improvements subsequent to the mandate to establish a DOD Task Force on Domestic Violence that was included in the National Defense Authorization Act for Fiscal Year 2000, “DOD lacks the sustained leadership and oversight of its efforts to prevent and treat domestic abuse that would enable the department to accurately assess the effectiveness of these efforts” (GAO, 2010, p. 23).
In studies of civilian populations, there is evidence supporting the restriction of access to lethal means in cases of domestic violence. The Federal Domestic Violence Gun Ban (the Lautenberg Amendment, in the Omnibus Consolidated Appropriations Act for FY 1997, P.L. 104-208) prohibits persons convicted of misdemeanor crimes of domestic violence from possessing firearms and ammunition (Krouse, 2012). There is no exception for law enforcement or military personnel. However, studies suggest that in cases of domestic violence other types of gun restrictions are more effective than misdemeanor laws, which is the only type of gun restriction implemented by the military in cases of domestic violence. Vigdor and Mercy (2006) examined the impact of three types of state law on intimate partner homicides in the civilian sector: (1) laws that prevent individuals who have been convicted of domestic violence misdemeanors from owning or purchasing a firearm, (2) laws preventing those individuals subject to a current restraining order from owning or purchasing a firearm, and (3) laws that allow law enforcement officers to confiscate firearms at the scene of an alleged domestic violence incident. They found that laws restricting access to firearms by individuals subject to a restraining order are an effective way to reduce interpersonal homicide rates. They find no evidence of an effect from domestic violence misdemeanor laws or laws that allow police to confiscate firearms at a domestic violence scene. The committee is not aware of whether DOD collects data on the numbers of service members with restraining orders.
Every military installation has a Family Advocacy Program (FAP) in place to provide an array of services dealing with sexual, physical, or emotional abuse of a family member (DOD, 2010b). Every service has an accreditation process with standards for counseling, record keeping, quality measurement, and staff credentials (DOD, 2013b). One prominent component of the program, the New Parent Support Program (NPSP), is a voluntary home visitation program targeting active-duty parents with children under age 3 identified as being at risk for family violence. Families can self-refer or be referred by a health provider. From 2005, when the program assessment began, to 2011, at least 85 percent of families who received intensive NPSP services for at least 6 months were not reported for child abuse or neglect within 1 year of completing the program (DOD, 2011, 2012a). No control group data were presented.
In regard to spousal abuse in FY 2009, 90 percent of service members who completed FAP treatment had not been reported for spousal abuse (physical, sexual, or emotional) within 1 year of program completion (DOD, 2010b); in FY 2010 that figure rose to 96 percent of service members who had completed a FAP treatment program (DOD, 2011) and in FY 2011 to 97 percent of participating service members (DOD, 2012a). Again, no control group data were presented, but DOD cited evidence indicating that abusers who complete a treatment program are less likely to repeat abuse than those who drop out of the program (DOD, 2012a). DOD noted, however, that spousal abusers are a heterogeneous group (for example, men or women who are
emotional or physical abusers) and that the treatment for the various types of abuser differs greatly. The outcome data do not stratify by treatment type, so some treatments may be more effective than others (DOD, 2010b). The FAP is working toward capturing treatment-specific outcome data, but DOD did not report on the specifics of those efforts (DOD, 2010b).
A community-based program designed to address family violence as well as substance problems and suicidality is the NORTH STAR program (see the substance use disorder section for program details). Results from an RCT of more than 50,000 active-duty military members from 24 Air Force bases found that the program resulted in reductions in partner physical abuse (as well as suicidality, alcohol abuse, and prescription drug use) after controlling for the level of integrated delivery system functioning and command support (Heyman et al., 2011).
DOD has implemented numerous resilience and prevention programs that address various aspects of psychological health. The committee identified some programs that are based on evidence and that have demonstrated effectiveness; however, comprehensive assessments of DOD programs show that a majority of the programs are not based on evidence and that programs are evaluated infrequently. Programs tend focus on individual-level interventions, with few exceptions. There is a lack of a process within DOD to systematically develop, track, and evaluate programs; among those that are evaluated, there is wide variability in the rigor of the evaluation. Similarly, although some of the evidence that DOD cites as justification for some of its programs may be statistically significant, it is not always clinically meaningful. The committee is also concerned DOD does not systematically consider the cost-effectiveness of its programs to ensure that resources are directed to programs that see the greatest results per dollar spent.
For military families, the committee found no DOD universal prevention programs for which there is an evidence base. Many programs for military families originate in the civilian world and are not tested with military populations before they are implemented. Given the exceptional demands that deployments to Iraq and Afghanistan have placed on military families and the impact that family concerns have on soldiers’ well-being, there continues to be a need for military leaders to gain a better understanding of the needs of families and to use that understanding to implement more effective coordinated programs and services for the good of military families and, thus, for the military as a whole.
DOD’s delegation of prevention efforts to the individual branches results in inconsistent availability of prevention services for service members and their families. However, because many are not evaluated, inconsistent application of programs allows for piloting and experimentation, although currently there is not a systematic process for DOD or the individual branches to monitor or share best practices.
Acosta, J. D., L. T. Martin, M. P. Fisher, R. Harris, and R. M. Weinick. 2012. Assessment of the Content, Design, and Dissemination of the Real Warriors Campaign. Santa Monica, CA: RAND Corporation.
Adler, A. B., B. T. Litz, C. A. Castro, M. Suvak, J. L. Thomas, L. Burrell, D. McGurk, K. M. Wright, and P. D. Bliese. 2008. A group randomized trial of critical incident stress debriefing provided to U.S. Peacekeepers. Journal of Traumatic Stress 21(3):253–263.
Adler, A. B., P. D. Bliese, D. McGurk, C. W. Hoge, and C. A. Castro. 2009a. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: Randomization by platoon. Journal of Consulting and Clinical Psychology 77(5):928–940.
Adler, A. B., C. A. Castro, and D. McGurk. 2009b. Time-driven Battlemind psychological debriefing: A group-level early intervention in combat. Military Medicine 174(1):21–28.
Alexopoulos, G. S., C. F. Reynolds, 3rd, M. L. Bruce, I. R. Katz, P. J. Raue, B. H. Mulsant, D. W. Oslin, and T. Ten Have. 2009. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. American Journal of Psychiatry 166(8):882–890.
Andersen, U. A., M. Andersen, J. U. Rosholm, and L. F. Gram. 2000. Contacts to the health care system prior to suicide: A comprehensive analysis using registers for general and psychiatric hospital admissions, contacts to general practitioners and practicing specialists and drug prescriptions. Acta Psychiatrica Scandinavica 102(2):126–134.
APA (American Psychiatric Association). 2013. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Publishing.
Astor, R. A., R. Benbenishty, and M. Wong. 2011. Building Capacity in Military Schools: Annual Report, Year 1. Los Angeles, CA: University of Southern California School of Social Work.
Babor, T., J. Caulkins, G. Edwards, B. Fischer, D. Foxcroft, K. Humphreys, I. Obot, J. Rehm, P. Reuter, R. Room, I. Rossow, and J. Strang. 2010a. Drug Policy and the Public Good. Oxford, England: Oxford University Press.
Babor, T. F., R. Caetano, S. Casswell, G. Edwards, N. Giesbrecht, K. Graham, J. Grube, L. Hill, H. Holder, R. Homel, M. Livingston, E. Osterberg, J. Rehm, R. Room, and I. Rossow. 2010b. Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford, England: Oxford University Press.
Benbenishty, R., and M. Esqueda. 2012. Building Capacity in Military Connected Schools Consortium Technical and Evaluation Report, Year 2. University of Southern California.
Blaisure, K. R., T. Saathoff-Wells, A. Pereira, S. MacDermid Wadsworth, and A. L. Dombro. 2012. Serving Military Families in the 21st Century. New York: Routledge/Taylor & Francis Group.
Borus, J. F. 1973. Reentry. I. Adjustment issues facing the Vietnam returnee. Archives of General Psychiatry 28(4):501–506.
Botvin, G., and K. Griffin. 2004. Life skills training: Empirical findings and future directions. Journal of Primary Prevention 25(2):211–232.
Botvin, G. J., E. Baker, L. Dusenbury, E. M. Botvin, and T. Diaz. 1995. Long-term follow-up results of a randomized drug abuse prevention trial in a white middle-class population. JAMA 273(14):1106–1112.
Bray, R. M., and L. L. Hourani. 2007. Substance use trends among active duty military personnel: Findings from the United States Department of Defense health related behavior surveys, 1980–2005. Addiction 102(7):1092–1101.
Bray, R. M., M. R. Pemberton, M. E. Lane, L. L. Hourani, M. J. Mattiko, and L. A. Babeu. 2010. Substance use and mental health trends among U.S. military active duty personnel: Key findings from the 2008 DoD Health Behavior Survey. Military Medicine 175(6):390–399.
Bray, R. M., J. M. Brown, and J. Williams. 2013. Trends in binge and heavy drinking, alcohol-related problems, and combat exposure in the U.S. Military. Substance Use & Misuse 48(10):799–810.
Bruce, M. L., T. R. Ten Have, C. F. Reynolds, 3rd, Katz, II, H. C. Schulberg, B. H. Mulsant, G. K. Brown, G. J. McAvay, J. L. Pearson, and G. S. Alexopoulos. 2004. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA 291(9):1081–1091.
Brunwasser, S. M., J. E. Gillham, and E. S. Kim. 2009. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. Journal Consulting and Clinical Psychology 77(6):1042–1054.
Bryant, R. A., A. G. Harvey, S. T. Dang, T. Sackville, and C. Basten. 1998. Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology 66(5):862–866.
Bryant, R. A., M. Moulds, R. Guthrie, and R. D. Nixon. 2003a. Treating acute stress disorder following mild traumatic brain injury. American Journal of Psychiatry 160(3):585–587.
Bryant, R. A., M. L. Moulds, and R. V. Nixon. 2003b. Cognitive behaviour therapy of acute stress disorder: A four-year follow-up. Behaviour Research and Therapy 41(4):489–494.
Bryant, R. A., M. L. Moulds, R. M. Guthrie, and R. D. Nixon. 2005. The additive benefit of hypnosis and cognitive-behavioral therapy in treating acute stress disorder. Journal of Consulting and Clinical Psychology 73(2):334–340.
Bryant, R. A., J. Mastrodomenico, K. L. Felmingham, S. Hopwood, L. Kenny, E. Kandris, C. Cahill, and M. Creamer. 2008. Treatment of acute stress disorder: A randomized controlled trial. Archives of General Psychiatry 65(6):659–667.
Bryant, R. A., M. Creamer, M. O’Donnell, D. Silove, and A. C. McFarlane. 2009. A study of the protective function of acute morphine administration on subsequent posttraumatic stress disorder. Biological Psychiatry 65(5):438–440.
Caetano, R., M. S. Kaplan, N. Huguet, B. H. McFarland, K. Conner, N. Giesbrecht, and K. B. Nolte. 2013. Acute alcohol intoxication and suicide among United States ethnic/racial groups: Findings from the National Violent Death Reporting System. Alcoholism: Clinical and Experimental Research 37(5):839–846.
Castro, C. A., A. B. Adler, D. McGurk, and P. D. Bliese. 2012. Mental health training with soldiers four months after returning from Iraq: Randomization by platoon. Journal of Traumatic Stress 25(4):376–383.
Claassen, C. A., and K. L. Knox. 2011. Assessment and management of high-risk suicidal states in postdeployment Operation Enduring Freedom and Operation Iraqi Freedom military personnel. In Caring for Veterans with Deployment-Related Stress Disorders: Iraq, Afghanistan, and Beyond, edited by J. I. Ruzek, P. P. Schnurr, J. J. Vasterling and M. J. Friedman. Washington, DC: American Psychological Association. Pp. 109–127.
Cornum, R., M. D. Matthews, and M. E. P. Seligman. 2011. Comprehensive Soldier Fitness: Building resilience in a challenging institutional context. American Psychologist 66(1):4–9.
Crano, W. D., and M. Burgoon. 2002. Mass Media and Drug Prevention: Classic and Contemporary Theories and Research. Mahwah, NJ: Lawrence Erlbaum Associates.
Currie, S. L., A. Day, and E. Kelloway. 2011. Bringing the troops back home: Modeling the postdeployment reintegration experience. Journal of Occupational Health Psychology 16(1):38–47.
DCOE (Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury). 2012a. Department of Defense Suicide Event Report: Calendar Year 2011 Annual Report. Washington, DC: National Center for Telehealth and Technology, Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
———. 2012b. Review of Post-Deployment Reintegration: Evidence, Challenges, and Strategies for Program Development. Arlington, VA: Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury.
Defense Manpower Data Center. 2011. 2010 Military Family Life Project. Arlington, VA: Department of Defense.
Department of the Army. 2013. Real Warriors. http://realwarriors.net/aboutus (accessed October 2, 2013).
DOD (Department of Defense). 2010a. DOD Appoints New Director of the Defense Center of Excellence for Psychological Health and Traumatic Brain Injury. http://www.defense.gov/releases/release.aspx?releaseid=14077 (accessed January 15, 2014).
———. 2010b. Plans for the Department of Defense for the Support of Military Family Readiness: Report to the Congressional Defense Committees Pursuant to Section 1782b of Title 10, United States Code. Washington, DC: Department of Defense.
———. 2011. Annual Report to Congress on Plans for the Department of Defense for the Support of Military Family Readiness. Washington, DC: Department of Defense.
———. 2012a. Annual Report to Congress on Plans for the Department of Defense for the Support of Military Family Readiness. Washington, DC: Department of Defense.
———. 2012b. Department of Defense Instruction 1010.01: Military Personnel Drug Abuse Testing Program (MPDATP). Washington, DC: Department of Defense.
———. 2012c. Annual Report to the Congressional Defense Committees on the Department of Defense Military Family Readiness Council. Washington, DC: Department of Defense.
———. 2013a. Department of Defense Annual Report on Sexual Assault in the Military: Fiscal Year 2012, Volume II. Washington, DC: Department of Defense.
———. 2013b. Department of Defense Directive: Sexual Assault Prevention and Response (SAPR) Program. Washington, DC: Department of Defense.
———. 2013c. Department of Defense Instruction 6495.02: Sexual Assault Prevention and Response (SAPR) Program Procedures. Washington, DC: Department of Defense.
———. 2013d. How Do We Implement I. A. M. Strong. http://www.preventsexualassault.army.mil/howdo.cfm (accessed September 20, 2013).
———. 2013e. Office of Warrior Care Policy. Office of Warrior Care Policy. http://warriorcare.dodlive.mil/about (accessed November 4, 2013).
———. 2013f. Sexual Assault Prevention and Response Office. http://www.sapr.mil/index.php/about/mission-and-history (accessed September 19, 2013).
DOD Sexual Assault Prevention and Response Office. 2012. Evaluation of Pre-Command Sexual Assault Prevention and Response Training. Washington, DC: Department of Defense.
Eidelson, R., M. Pilisuk, and S. Soldz. 2011. The dark side of Comprehensive Soldier Fitness. American Psychologist 66(7):643–644.
Engel, C. C., T. Oxman, C. Yamamoto, D. Gould, S. Barry, P. Stewart, K. Kroenke, J. W. Williams, Jr., and A. J. Dietrich. 2008. RESPECT–Mil: Feasibility of a systems-level collaborative care approach to depression and post-traumatic stress disorder in military primary care. Military Medicine 173(10):935–940.
Fountoulakis, K. N., X. Gonda, and Z. Rihmer. 2011. Suicide prevention programs through community intervention. Journal of Affective Disorders 130(1–2):10–16.
Freeman, T. W., V. Roca, and T. Kimbrell. 2003. A survey of gun collection and use among three groups of veteran patients admitted to Veterans Affairs hospital treatment programs. Southern Medical Journal 96(3):240–243.
Gallo, J. J., K. H. Morales, H. R. Bogner, P. J. Raue, J. Zee, M. L. Bruce, and C. F. Reynolds, 3rd. 2013. Long term effect of depression care management on mortality in older adults: Follow-up of cluster randomized clinical trial in primary care. BMJ 346:f2570.
GAO (Government Accountability Office). 2010. Sustained Leadership and Oversight Needed to Improve DOD's Prevention and Treatment of Domestic Abuse. Washington, DC: Government Accountability Office.
———. 2012. Recovering Servicemembers and Veterans: Sustained Leadership Attention and Systematic Oversight Needed to Resolve Persistent Problems Affecting Care and Benefits. Washington, DC: Government Accountability Office.
Garber, B. G., and M. A. Zamorski. 2012. Evaluation of a third-location decompression program for Canadian forces members returning from Afghanistan. Military Medicine 177(4):397–403.
Gelpin, E., O. Bonne, T. Peri, D. Brandes, and A. Y. Shalev. 1996. Treatment of recent trauma survivors with benzodiazepines: A prospective study. Journal of Clinical Psychiatry 57(9):390–394.
Gewirtz, A. H., C. R. Erbes, M. A. Polusny, M. S. Forgatch, and D. S. DeGarmo. 2011. Helping military families through the deployment process: Strategies to support parenting. Professional Psychology Research & Practice 42(1):56–62.
Gould, J. 2013. Alcohol Sales Face Restrictions on Posts. http://www.militarytimes.com/article/20130826/BENEFITS07/308260004/Alcohol-sales-face-restrictions-posts (accessed August 27, 2013).
Gould, M., N. Greenberg, and J. Hetherton. 2007a. Stigma and the military: Evaluation of a PTSD psychoeducational program. Journal of Traumatic Stress 20(4):505–515.
Gould, M. S., J. Kalafat, J. L. Harrismunfakh, and M. Kleinman. 2007b. An evaluation of crisis hotline outcomes. Part 2: Suicidal callers. Suicide and Life-Threatening Behavior 37(3):338–352.
Harms, P. D., M. N. Herian, D. V. Krasikova, A. Vanhove, and P. B. Lester. 2013. The Comprehensive Soldier and Family Fitness Program Evaluation Report #4: Evaluation of Resilience Training and Mental and Behavioral Health Outcomes. Washington, DC: Department of Defense.
Harvey, A. G., and R. A. Bryant. 1998. The relationship between acute stress disorder and posttraumatic stress disorder: A prospective evaluation of motor vehicle accident survivors. Journal of Consulting and Clinical Psychology 66(3):507–512.
Hazelden Foundation. 2013. Navy MORE. http://www.hazelden.org/web/public/pr091001.page (accessed November 11, 2013).
Heyman, R. E., and A. M. Smith Slep. 2001. Risk factors for family violence: Introduction to the special series. Aggression and Violent Behavior 6(2–3):115–119.
Heyman, R. E., A. M. Smith Slep, and J. P. Nelson. 2011. Empirically guided community intervention for partner abuse, child maltreatment, suicidality, and substance misuse. In Risk and Resilience in U.S. Military Families, edited by S. M. Wadsworth and D. Riggs. New York: Springer. Pp. 85–107.
Hoge, E. A., J. J. Worthington, J. T. Nagurney, Y. Chang, E. B. Kay, C. M. Feterowski, A. R. Katzman, J. M. Goetz, M. L. Rosasco, N. B. Lasko, R. M. Zusman, M. H. Pollack, S. P. Orr, and R. K. Pitman. 2012. Effect of acute posttrauma propranolol on PTSD outcome and physiological responses during script-driven imagery. CNS Neuroscience & Therapeutics 18(1):21–27.
Holbrook, T. L., M. R. Galarneau, J. L. Dye, K. Quinn, and A. L. Dougherty. 2010. Morphine use after combat injury in Iraq and post-traumatic stress disorder. New England Journal of Medicine 362(2):110–117.
Hughes, C. E., and A. Stevens. 2010. What can we learn from the Portuguese decriminalization of illicit drugs? British Journal of Criminology 50(6):999–1022.
IOM (Institute of Medicine). 2012. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Washington, DC: The National Academies Press.
———. 2013a. Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington, DC: The National Academies Press.
———. 2013b. Substance Use Disorders in the U.S. Armed Forces. Washington, DC: The National Academies Press.
Isaac, M., B. Elias, L. Y. Katz, S. L. Belik, F. P. Deane, M. W. Enns, and J. Sareen. 2009. Gatekeeper training as a preventative intervention for suicide: A systematic review. Canadian Journal of Psychiatry 54(4):260–268.
Jones, N., M. Jones, N. T. Fear, M. Fertout, S. Wessely, and N. Greenberg. 2013. Can mental health and readjustment be improved in UK military personnel by a brief period of structured postdeployment rest (third location decompression)? Occupational and Environmental Medicine 70(7):439–445.
Jordan, B. 2012. DoD Could Renew Push to Restrict Personal Weapons. http://www.military.com/dailynews/2012/06/21/dod-could-renew-push-to-restrict-personal-weapons.html (accessed October 1, 2012).
Kaplan, M. S., N. Huguet, B. H. McFarland, and J. T. Newsom. 2007. Suicide among male veterans: A prospective population-based study. Journal of Epidemiology and Community Health 61(7):619–624.
Kessler, R. C., A. Sonnega, E. Bromet, M. Hughes, and C. B. Nelson. 1995. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry 52(12):1048–1060.
King, R., B. Nurcombe, L. Bickman, L. Hides, and W. Reid. 2003. Telephone counselling for adolescent suicide prevention: Changes in suicidality and mental state from beginning to end of a counselling session. Suicide and Life Threatening Behavior 33(4):400–411.
Knox, K. L., D. A. Litts, G. W. Talcott, J. C. Feig, and E. D. Caine. 2003. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the U.S. Air Force: Cohort study. BMJ 327(7428):1376.
Knox, K. L., J. Kemp, R. McKeon, and I. R. Katz. 2012. Implementation and early utilization of a suicide hotline for veterans. American Journal of Public Health 102(Suppl 1):S29–S32.
Koenen, K. C., J. M. Stellman, S. D. Stellman, and J. F. Sommer, Jr. 2003. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychol 71(6):980–986.
Krouse, W. J. 2012. Gun Control Legislation. Washington, DC: Congressional Research Service.
Lester, P., and Lieutenant Colonel E. Flake. 2013. How wartime military service affects children and families. The Future of Children 23(2):121–141.
Lester, P., C. Mogil, W. Saltzman, K. Woodward, W. Nash, G. Leskin, B. Bursch, S. Green, R. Pynoos, and W. Beardslee. 2011a. Families Overcoming Under Stress: Implementing family-centered prevention for military families facing wartime deployments and combat operational stress. Military Medicine 176(1):19–25.
Lester, P. B., P. D. Harms, M. N. Herian, D. V. Krasikova, and S. J. Beal. 2011b. The Comprehensive Soldier Fitness Program Evaluation Report #3: Longitudinal Analysis of the Impact of Master Resilience Training on Self-Reported Resilience and Psychological Health Data. Washington, DC: Department of Defense.
Lester, P., W. R. Saltzman, K. Woodward, D. Glover, G. A. Leskin, B. Bursch, R. Pynoos, and W. Beardslee. 2012. Evaluation of a family-centered prevention intervention for military children and families facing wartime deployments. American Journal of Public Health 102 (Suppl 1):S48–S54.
Lester, P., J. A. Stein, W. Saltzman, K. Woodward, S. W. Macdermid, N. Milburn, C. Mogil, and W. Beardslee. 2013. Psychological health of military children: Longitudinal evaluation of a familycentered prevention program to enhance family resilience. Military Medicine 178(8):838–845.
Loftin, C., D. McDowall, B. Wiersema, and T. J. Cottey. 1991. Effects of restrictive licensing of handguns on homicide and suicide in the District of Columbia. New England Journal of Medicine 325(23):1615–1620.
Lubin, G., N. Werbeloff, D. Halperin, M. Shmushkevitch, M. Weiser, and H. Y. Knobler. 2010. Decrease in suicide rates after a change of policy reducing access to firearms in adolescents: A naturalistic epidemiological study. Suicide and Life-Threatening Behavior 40(5):421–424.
Ludwig, J., and P. J. Cook. 2000. Homicide and suicide rates associated with implementation of the Brady Handgun Violence Prevention Act. JAMA 284(5):585–591.
Luoma, J. B., C. E. Martin, and J. L. Pearson. 2002. Contact with mental health and primary care providers before suicide: A review of the evidence. American Journal of Psychiatry 159(6):909–916.
Luxton, D. D., J. E. Osenbach, M. A. Reger, D. J. Smolenski, N. A. Skopp, N. E. Bush, and G. A. Gahm. 2012. Department of Defense Suicide Event Report: Calendar Year 2011 Annual Report. Washington, DC: Department of Defense.
Mann, J. J., A. Apter, J. Bertolote, A. Beautrais, D. Currier, A. Haas, U. Hegerl, J. Lonnqvist, K. Malone, A. Marusic, L. Mehlum, G. Patton, M. Phillips, W. Rutz, Z. Rihmer, A. Schmidtke, D. Shaffer, M. Silverman, Y. Takahashi, A. Varnik, D. Wasserman, P. Yip, and H. Hendin. 2005. Suicide prevention strategies: A systematic review. JAMA 294(16):2064–2074.
Matthieu, M. M., W. Cross, A. R. Batres, C. M. Flora, and K. L. Knox. 2008. Evaluation of gatekeeper training for suicide prevention in veterans. Archives of Suicide Research 12(2):148–154.
McAuliffe, N., and L. Perry. 2007. Making it safer: A health centre’s strategy for suicide prevention. Psychiatric Quarterly 78(4):295–307.
McNally, R. J., R. A. Bryant, and A. Ehlers. 2003. Does early psychological intervention promote recovery from posttraumatic stress? Psychological Science in the Public Interest 4(2):45–79.
Meredith, L. S., C. D. Sherbourne, S. Gaillot, L. Hansell, H. V. Ritschard, A. M. Parker, and G. Wrenn. 2011. Promoting Psychological Resilience in the U.S. Military. Santa Monica, CA: RAND Corporation.
Miech, R. A., A. S. London, J. M. Wilmoth, and S. Koester. 2013. The effects of the military’s antidrug policies over the life course: The case of past-year hallucinogen use. Substance Use & Misuse 48(10):837–853.
Military Health System Clinical Quality Management. 2009a. Evaluation of the RESPECT–Mil Program: Phase II Study #2: Mental Health Services Following Initial RESPECT–Mil Assessment. Falls Church, VA: Military Health System Clinical Quality Management.
———. 2009b. Evaluation of the RESPECT-Mil Program: Phase II Study #4: Post-Deployment Health Assessment and RESPECT–Mil Assessment. Falls Church, VA: Military Health System Clinical Quality Management.
Military Pathways. 2013. About Military Pathways: Mental Health Screening and Info. http://www.militarymentalhealth.org/about.aspx (accessed October 2, 2013).
Military Suicide Report. 2012. Marine Corps Sending Most Elite to “Special” Decompression, Psychological Screening Center After War Duty. http://themilitarysuicidereport.wordpress.com/tag/post-deployment-decompression (accessed August 15, 2013).
Miller, L. L., B. D. Rostker, R. M. Burns, D. Barnes-Proby, S. Lara-Cinisomo, and T. R. West. 2011. A New Approach for Assessing the Needs of Service Members and Their Families. Santa Monica, CA: RAND Corporation.
Mishara, B. L., F. Chagnon, M. Daigle, B. Balan, S. Raymond, I. Marcoux, C. Bardon, J. K. Campbell, and A. Berman. 2007. Comparing models of helper behavior to actual practice in telephone crisis intervention: A silent monitoring study of calls to the U.S. 1-800-Suicide Network. Suicide and Life Threatening Behavior 37(3):291–307.
Momen, N., C. P. Strychacz, and E. Viirre. 2012. Perceived stigma and barriers to mental health care in Marines attending the Combat Operational Stress Control Program. Military Medicine 177(10):1143–1148.
Monson, C. M., S. J. Fredman, A. Macdonald, N. D. Pukay-Martin, P. A. Resick, and P. P. Schnurr. 2012. Effect of cognitive-behavioral couple therapy for PTSD: A randomized controlled trial. JAMA 308(7):700–709.
Mulligan, K., N. T. Fear, N. Jones, H. Alvarez, L. Hull, U. Naumann, S. Wessely, and N. Greenberg. 2012. Postdeployment Battlemind training for the U.K. armed forces: A cluster randomized controlled trial. Journal of Consulting & Clinical Psychology 80(3):331–341.
Nash, W. P. 2011. US Marine Corps and Navy combat and operational stress continuum model: A tool for leaders. In Combat and operational behavioral health, edited by Walter Reed Army Medical Center Borden Institute. Washington, DC: Department of the Army.
National Family Partnership. 2013. Red Ribbon Fact Sheet. http://www.nfp.org/default.asp?PageNum=617 (accessed September 28, 2013).
NIMH (National Institute of Mental Health). 2013. Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS): A Partnership Between NIMH and the U.S. Army. http://www.nimh.nih.gov/health/topics/suicide-prevention/suicide-prevention-studies/army-study-to-assess-risk-and-resilience-in-servicemembers-army-starrs-a-partnership-between-nimh-and-the-usarmy.shtml (accessed October 10, 2013).
NIH RePORT (National Institute of Health Research Portfolio Online Reporting Tools). 2013. Outcomes in Callers to the VA’s 24/7 Veterans Crisis Line. http://projectreporter.nih.gov/project_info_description.cfm?aid=8443620&icde=18798938 (accessed January 6, 2013).
Norem, J. K., and K. S. S. Illingworth. 2004. Mood and performance among defensive pessimists and strategic optimists. Journal of Research in Personality 38(4):351–366.
North, C. S., B. Pfefferbaum, P. Narayanan, S. Thielman, G. McCoy, C. Dumont, A. Kawasaki, N. Ryosho, Y. S. Kim, and E. L. Spitznagel. 2005. Comparison of post-disaster psychiatric disorders after terrorist bombings in Nairobi and Oklahoma City. British Journal of Psychiatry 186:487–493.
ONDCP (Office of National Drug Control Policy). 2013. Prescription Drug Abuse. http://www.whitehouse.gov/ondcp/prescription-drug-abuse (accessed October 3, 2013).
Orsingher, J. M., A. T. Lopez, and M. E. Rinehart. 2008. Battlemind training system: “Armor for your mind.” US Army Medical Department Journal:66–71.
Pentz, M. A. 2003. Evidence-based prevention: Characteristics, impact, and future direction. Journal of Psychoactive Drugs 35(Suppl 1):143–152.
Pitman, R. K., K. M. Sanders, R. M. Zusman, A. R. Healy, F. Cheema, N. B. Lasko, L. Cahill, and S. P. Orr. 2002. Pilot study of secondary prevention of posttraumatic stress disorder with propranolol. Biological Psychiatry 51(2):189–192.
Ramchand, R., J. D. Acosta, R. M. Burns, L. H. Jaycox, and C. G. Pernin. 2011. The War Within: Preventing Suicide in the U.S. Military. Santa Monica, CA: RAND Corporation.
RAND Corporation. 2013. Catalog of Psychological Health and Traumatic Brain Injury Programs. http://smapp.rand.org/multi/military/innovative-practices/catalog (accessed September 22, 2013).
Reivich, K. J., M. E. P. Seligman, and S. McBride. 2011. Master resilience training in the U.S. Army. American Psychologist 66(1):25–34.
Riggs, N. R., C. P. Chou, and M. A. Pentz. 2009. Preventing growth in amphetamine use: Long-term effects of the Midwestern Prevention Project (MPP) from early adolescence to early adulthood. Addiction 104(10):1691–1699.
Roberts, N. P., N. J. Kitchiner, J. Kenardy, and J. I. Bisson. 2010. Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic Reviews (3):CD006869.
———. 2012. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews (3):CD007944.
Rose, S., J. Bisson, R. Churchill, and S. Wessely. 2002. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews (2):CD000560.
Rothbaum, B. O., M. C. Kearns, M. Price, E. Malcoun, M. Davis, K. J. Ressler, D. Lang, and D. Houry. 2012. Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry 72(11):957–963.
Rutz, W., L. von Knorring, and J. Walinder. 1989. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatrica Scandinavica 80(2):151–154.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2012. CAPT Webinars Help Practitioners Implement Environmental Prevention Strategies. http://captus.samhsa.gov/accessresources/capt-webinars-help-practitioners-implement-environmental-prevention-strategies (accessed October 18, 2013).
Schelling, G., J. Briegel, B. Roozendaal, C. Stoll, H. B. Rothenhausler, and H. P. Kapfhammer. 2001. The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors. Biological Psychiatry 50(12):978–985.
Schelling, G., B. Roozendaal, and D. J. De Quervain. 2004. Can posttraumatic stress disorder be prevented with glucocorticoids? Annals of the New York Academy of Science 1032:158–166.
Shaffer, D., A. Garland, M. Gould, P. Fisher, and P. Trautman. 1988. Preventing teenage suicide: A critical review. Journal of the American Academy of Child & Adolescent Psychiatry 27(6):675–687.
Shalev, A. Y., Y. Ankri, Y. Israeli-Shalev, T. Peleg, R. Adessky, and S. Freedman. 2012. Prevention of posttraumatic stress disorder by early treatment: Results from the Jerusalem Trauma Outreach and Prevention study. Archives of General Psychiatry 69(2):166–176.
Smith, S. L. 2013. Could comprehensive soldier fitness have iatrogenic consequences?: A commentary. Journal of Behavioral Health Services and Research 40(2):242–246.
Spera, C., K. Franklin, K. Uekawa, J. F. Kunz, R. Z. Szoc, R. K. Thomas, and M. H. Cambridge. 2010. Reducing drinking among junior enlisted Air Force members in five communities: Early findings of the EUDL program’s influence on self-reported drinking behaviors. Journal of Studies on Alcohol and Drugs 71(3):373–383.
Spera, C., F. Barlas, R. Z. Szoc, J. Prabhakaran, and M. H. Cambridge. 2012. Examining the influence of the Enforcing Underage Drinking Laws (EUDL) program on alcohol-related outcomes in five communities surrounding Air Force bases. Addictive Behaviors 37(4):513–516.
Spoth, R. L., L. L. Schainker, and S. Hiller-Sturmhoefel. 2011. Translating family-focused prevention science into public health impact. Alcohol Research and Health 34(2):188–203.
Stanley, S. M., E. S. Allen, H. J. Markman, G. K. Rhoades, and D. L. Prentice. 2010. Decreasing divorce in Army couples: Results from a randomized controlled trial using PREP for Strong Bonds. Journal of Couple & Relationship Therapy 9(2):149–160.
Steenkamp, M. M., W. P. Nash, and B. T. Litz. 2013. Post-traumatic stress disorder: Review of the Comprehensive Soldier Fitness Program. American Journal of Prentive Medicine 44(5):507–512.
Stein, M. B., C. Kerridge, J. E. Dimsdale, and D. B. Hoyt. 2007. Pharmacotherapy to prevent PTSD: Results from a randomized controlled proof-of-concept trial in physically injured patients. Journal of Traumatic Stress 20(6):923–932.
Stice, E., H. Shaw, C. Bohon, C. N. Marti, and P. Rohde. 2009. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology 77(3):486–503.
Szczytkowski-Thomson, J. L., C. L. Lebonville, and D. T. Lysle. 2013. Morphine prevents the development of stress-enhanced fear learning. Pharmacology, Biochemistry, and Behavior 103(3):672–677.
U.S. Army. 2009. Comprehensive Soldier Fitness: Strong Minds, Strong Bodies. http://www.army.mil/article/28194/Comprehensive_Soldier_Fitness___Strong_Minds__Strong_Bodies/ (accessed November 21, 2013).
———. 2011. ALARACT 062/2011: Changes to Length of Authorized Duration of Controlled Substance Prescriptions in MEDCOM Regulation 40-51. Washington, DC: Office of the Army Surgeon General.
———. 2013a. Army STARRS. http://www.armystarrs.org (accessed October 10, 2013).
———. 2013b. Comprehensive Soldier Fitness. http://csf.army.mil (accessed August 15, 2013).
———. 2013c. Suicide Prevention Training. www.armyg1.army.mil/hr/suicide/training.asp (accessed December 17, 2013).
U.S. Navy. 2013. NAVYADMIN 012/13. Washington, DC: Department of the Navy.
VA (Department of Veterans Affairs). 2013. Prolonged Exposure Therapy. http://www.ptsd.va.gov/public/pages/prolonged-exposure-therapy.asp (accessed October 20, 2013).
VA and DOD. 2010. VA/DOD Clinical Practice Guideline for Management of Post-Traumatic Stress. Washington, DC: VA and DOD.
———. 2013. VA/DOD Clinical Practice Guideline for Assessment and Management of Patients at Risk for Suicide. Washington, DC: VA and DOD.
Vigdor, E. R., and J. A. Mercy. 2006. Do laws restricting access to firearms by domestic violence offenders prevent intimate partner homicide? Evaluation Review 30(3):313–346.
Weinick, R. M., E. B. Beckjord, C. M. Farmer, L. T. Martin, E. M. Gillen, J. D. Acosta, M. P. Fisher, J. Garnett, G. C. Gonzalez, T. C. Helmus, L. H. Jaycox, K. A. Reynolds, N. Salcedo, and D. M. Scharf. 2011. Programs Addressing Psychological Health and Traumatic Brain Injury Among U.S. Miliary Service Members and Their Families. Santa Monica, CA: RAND Corporation.
Weis, F., E. Kilger, B. Roozendaal, D. J. de Quervain, P. Lamm, M. Schmidt, M. Schmolz, J. Briegel, and G. Schelling. 2006. Stress doses of hydrocortisone reduce chronic stress symptoms and improve health-related quality of life in high-risk patients after cardiac surgery: A randomized study. Journal of Thoracic and Cardiovascular Surgery 131(2):277–282.
Williams, A., B. M. Hagerty, S. M. Yousha, J. Horrocks, K. S. Hoyle, and D. Liu. 2004. Psychosocial effects of the boot strap intervention in Navy recruits. Military Medicine 169(10):814–820.
Williams, A., B. M. Hagerty, A. C. Andrei, S. M. Yousha, R. A. Hirth, and K. S. Hoyle. 2007. Stars: Strategies to assist Navy recruits’ success. Military Medicine 172(9):942–949.
Yellow Ribbon Reintegration Program. 2013a. Yellow Ribbon Events Plus. https://www.yellowribbonevents.org/default.aspx (accessed November 5, 2013).
———. 2013b. Annual Advisory Board Report to Congress. Arlington, VA: Yellow Ribbon Reintegration Program.
Zamorski, M. A., K. Guest, L. S. Bailey, and B. G. Garber. 2012. Beyond Battlemind: Evaluation of a new mental health training program for Canadian forces personnel participating in third-location decompression. Military Medicine 177(11):1245–1253.
Zatzick, D., G. Jurkovich, F. P. Rivara, J. Russo, A. Wagner, J. Wang, C. Dunn, S. P. Lord, M. Petrie, S. O’Connor S, and W. Katon. 2013. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery 257(3):390–399.
Zohar, J., H. Yahalom, N. Kozlovsky, S. Cwikel-Hamzany, M. A. Matar, Z. Kaplan, R. Yehuda, and H. Cohen. 2011. High dose hydrocortisone immediately after trauma may alter the trajectory of PTSD: Interplay between clinical and animal studies. European Neuropsychopharmacology 21(11):796–809.


















































