Clinician-Patient Communication and Advance Care Planning
There are many barriers to clear communication on people’s preferences for end-of-life care. Albeit well intentioned, past efforts to ensure that patients’ wishes are known and followed have fallen short, even when codified into legislation and regulation, as a result of multiple factors:
- the natural reluctance of patients, families, and clinicians to explore death and dying;
- a fragmented health care system that can make the discussion of end-of-life preferences “someone else’s problem”;
- poor-quality communication in the conversations that are held, often in hurried or crisis situations; and
- inadequate structural supports for advance care planning, including clinician training, payment, and record keeping.
The “living will”—conceived as a document designed to protect people’s legal right to have the amount and kinds of medical treatment they want even if they can no longer express that choice themselves—was perceived as the solution for Americans’ concerns about being “hooked up to machines” for long periods or, conversely, being protected against premature “pulling of the plug.” Nonetheless, this legal approach has been disappointingly ineffective in improving the care people nearing the end of life receive and in ensuring that this care accords with their informed preferences.
This chapter describes some of the reasons for that failure and the evolution of new and potentially more effective approaches to advance care planning. These approaches share the following features:
- They do not consider advance care planning a one-time activity, but instead emphasize discussion of goals, values, and care preferences among individuals, family, health care agents, and care providers over the life span. Ideally, these discussions would start early in adulthood, addressing global values and the identification of potential surrogate decision makers, and focusing on more specific treatment preferences for older persons and those facing serious illness. With changes in health status, they would take on increasing specificity. “Putting it in writing” remains important but does not substitute for the discussion.
- They emphasize appointment of a health care agent1; encourage adequate preparation of that agent for future decision making; and support discussions of care choices among individuals, the agent, and the primary clinician.
- They respect and accommodate the different cultural, ethnic, and spiritual values of the diverse U.S. population.
A measure of control over the final phase of life appears achievable in most situations today if patients, families, and clinicians have these essential conversations. The best experiences occur when there are reliable systems for eliciting, recording, and using information about patients’ preferences; when clinicians are trained to carry out these tasks effectively and are properly compensated for doing so; and when, regardless of care setting—home, nursing home, hospital, intensive care, rehabilitation facility, or under hospice care—patients’ wishes are known and respected to the extent possible. Instead, however, there are strong professional, cultural, and financial incentives for continuing treatment beyond the point where it benefits patients.
This chapter examines the current state of advance care planning—who participates and the ways in which it affects clinical care, patient and caregiver outcomes, and the costs of care. It then describes the way age, disability, and personal background may affect attitudes about and experiences with advance care planning. Next, fundamental to the advance care planning process is clear empathetic communication between clinicians and patients, which can lead to shared decision making. Accordingly, the chapter explores the elements of good communication in this process. This is followed by discussion of several model advance care planning programs
_______________
1These individuals are variously called surrogates, proxies, or agents. A health care agent is an individual designated in an advance directive, while a health care proxy is any designated substitute decision maker, including a guardian or conservator. A surrogate is a person who, by default, becomes the decision maker for an individual who has no appointed proxy (HHS, 2008). In this report, the term “health care agent” is generally used. The form that names the agent is often called a durable power of attorney for health care.
and the committee’s proposed life cycle model for advance care planning. The chapter ends by outlining research needs and presenting the committee’s findings, conclusions, and recommendations on alignment of care with patient preferences.
Americans express strong views when asked about the kinds of care they want when they are seriously ill and approaching death. As noted in earlier chapters, in general they prefer to die at home, and they want to remain in charge of decisions about their care (CHCF, 2012; Fischer et al., 2013; Gruneir et al., 2007; Tang, 2003). However, evidence suggests these wishes are not likely to be fulfilled:
- In 2009, one in four adults aged 65 and older died in an acute care hospital, 28 percent died in a nursing home, and one in three died at home (Teno et al., 2013). Among all decedents, 30 percent were in an intensive care unit (ICU) in the month preceding death.
- An estimated 40 percent of all adult medical inpatients are incapable of making their own treatment decisions because of unconsciousness, cognitive impairment, or inability to express a choice (Raymont et al., 2004).
- Among nursing home residents, 44-69 percent cannot make their own medical decisions (Kim et al., 2002).
- Fully 70 percent of decedents participating in the Health and Retirement Study who were aged 60 and older at death and who faced treatment decisions in the final days of their lives were incapable of participating in these decisions (Silveira et al., 2010).
- The vast majority of critically ill patients cannot participate directly in decision making (Nelson et al., 2006), nor are they likely even to have met the intensivist physicians caring for them (Gay et al., 2009).
The Institute of Medicine (IOM) report Approaching Death (IOM, 1997) reviews many of the then-recognized shortcomings of the advance directive approach:
- patients’ and families’ lack of awareness of or interest in completing forms;
- clinicians’ unwillingness to adhere to patients’ wishes;
- difficulties in having meaningful family conversations about patients’ wishes and in making choices in the face of prognostic uncertainty;
- lack of institutional support and processes for completing advance directives; and
- cultural and legal factors, including resistance within the medical culture as well as differences in families’ cultural traditions.
A study of public views conducted around the same time that report was published reinforced these concerns (American Health Decisions, 1997). Respondents noted that there are many reasons why they or their loved ones avoid talking about death, including that it is upsetting or depressing or is an issue to be addressed in the future. They also felt that the medical system’s emphasis on achieving cure and sustaining life “even when death is inevitable—can ironically result in treatments that prolong life ‘unnaturally’ and cause unnecessary suffering.”
Some of the problems identified 17 years ago have since diminished or been remedied, while others have become more acutely apparent. The mischaracterization of advance care planning as “death panels” during debates about the Affordable Care Act (see Chapter 6) suggests that misunderstandings about the process have persisted and, indeed, intensified.
The remainder of this section reviews the four-decade history of advance directives/advance care planning. Before proceeding, however, a note about these two terms is in order. Approaching Death draws a useful distinction between advance directives (documents written or completed by patients) and the broader concept of advance care planning. As Box 3-1 describes, advance care planning is a process for setting goals and plans with respect to medical treatments and other clinical considerations. It brings together patients, families, and clinicians “to develop a coherent care plan that meets the patients’ goals, values, and preferences” (Walling et al., 2008, p. 3896). It can begin at any point in a person’s life, regardless of his or her current health state; is revisited periodically; and becomes more specific as changing health status warrants.
As anticipated in Approaching Death, the current emphasis has evolved considerably from a debate about specific legal forms and living wills to acceptance of the more general concept of advance care planning (Sabatino, 2010). Because much of the large body of research in this area focuses on advance directives (a tangible product) rather than the broader and more difficult to document topic of advance care planning, this chapter likewise talks about directives. It should be noted, however, that while the committee consistently found shortcomings in advance directives, it is more optimistic about the potential benefits of advance care planning.
The following historical review draws on a report prepared by the U.S. Department of Health and Human Services (HHS, 2008) titled Advance Directives and Advance Care Planning. That report resulted from a request
by Congress in 2006 that HHS conduct a study of advance directives and how to promote their use.
For decades, people with advanced serious illnesses relied almost unquestioningly on their physicians’ judgment regarding treatment matters, trusting that physicians would act in their patients’ best interests as a matter of professional and personal ethics. As technology and medicine advanced, increasingly intensive interventions could keep people alive with breathing tubes and feeding tubes and high doses of powerful drugs. In many cases, people recovered and resumed their former lives, but in other cases, the lives these technologies sustained were not optimal.
Around the time public awareness of the darker potential of “heroic measures” was growing, so was the consumer rights movement. In that context, Americans sought to assert their right to control whether life-sustaining treatments were used in their care, especially when the outcome was doubtful. Among the earliest attempts to codify this new right was the California Natural Death Act of 19762 (Towers, 1978), which made the written advance directives of terminally ill patients binding on their physicians. The California law was quickly followed by similar actions in other states and upheld in state and federal courts. In 1990, Congress passed the Patient Self-Determination Act,3 which required all health care facilities receiving reimbursement from Medicare or Medicaid “to ask patients whether they have advance directives, to provide information about advance directives, and to incorporate advance directives into the medical record” (HHS, 2008, p. x), setting the stage for subsequent emphasis on this type of form.
Public concern about advance directives increased in the wake of several well-publicized legal cases that centered on the right to withdraw treatment from people lacking decision-making capacity. At the same time, new state laws outlined do-not-resuscitate protocols—medical orders signed by a clinician—for use outside as well as within the hospital. Building on this concept of having medical orders in place to guide treatment, a new model was pioneered in Oregon for recording a broader range of preferences. These Physician Orders for Life-Sustaining Treatment (POLST), now being approved in an increasing number of states (see Box 3-1 and Annex 3-2) and described later in this chapter, are actionable in and out of the hospital, even in emergency situations.
Regional and national efforts to encourage advance care planning have
_______________
2Natural Death Act, Ch. 1439, 1976 Cal. Stat. 6478 (enacting Cal. Health & Safety Code § 7188 (repealed 2000)).
3The Patient Self-Determination Act, Omnibus Budget Reconciliation Act of 1990, Public Law 101-508 §§ 4206 and 4751, 104 Stat. 1388-155 and 1388-204 (1991).
BOX 3-1
Terms Related to Advance Care Planning
Advance care planning entails a number of different kinds of instruments. In this report, the committee has tried to maintain the distinctions among them, but the medical literature reviewed does not always do so, and there is confusion even in the field. Terms appearing in this report with respect to advance care planning are defined as follows, with the understanding that in discussing particular studies, the committee uses the terms employed by their authors.
Advance care planning refers to the whole process of discussion of end-of-life care, clarification of related values and goals, and embodiment of preferences through written documents and medical orders. This process can start at any time and be revisited periodically, but it becomes more focused as health status changes. Ideally, these conversations (1) occur with a person’s health care agent and primary clinician, along with other members of the clinical team; (2) are recorded and updated as needed; and (3) allow for flexible decision making in the context of the patient’s current medical situation.
Advance directive refers to several types of patient-initiated documents, especially living wills and documents that name a health care agent. People can complete these forms at any time and in any state of health that allows them to do so.
- Living will—a written (or video) statement about the kinds of medical care a person does or does not want under certain specific conditions (often “terminal illness”) if no longer able to express those wishes.
- Durable power of attorney for health care—identifies the person (the health care agent) who should make medical decisions in case of the patient’s incapacity.
Medical orders are created with and signed by a health professional, usually a physician (in some states, a nurse practitioner or physician assistant), for someone who is seriously ill. Because they are actual doctor’s orders, other health professionals, including emergency personnel, are required to follow them.
evolved. Community Conversations on Compassionate Care (CCCC),4 operating in Upstate New York, was launched with a press conference of spiritual leaders in Rochester, New York, in 2002 to encourage everyone aged 18 and older to start early advance care planning discussions. The Center for Practical Bioethics works extensively in the Midwest and throughout the
_______________
4See https://www.compassionandsupport.org/index.php/for_patients_families/advance_care_planning/community_conversations (accessed December 16, 2014).
- Physician Orders for Life-Sustaining Treatment (POLST)a—physician orders covering a range of topics likely to emerge in care of a patient near the end of life, an innovation that began in Oregon in the early 1990s, gradually spread to a few states, and is increasingly being adopted nationwide. The orders cross care settings and are honored in the community in an emergency. As of December 2013, the POLST Paradigm Task Force had endorsed the POLST programs of 16 states,b and another 12 states were developing POLST implementation plans (National POLST, 2012f).
- Do-not-resuscitate,c do-not-intubate, do-not-hospitalize orders—medical orders covering specific treatments that are written in a health care facility, but do not cross care settings and are not necessarily honored in the community. An out-of-hospital do-not-resuscitate is a do-not-resuscitate medical order that pertains when a patient is outside of a health care facility setting (for example, a hospital or nursing home), and is intended to ensure that a patient will not be resuscitated against his or her wishes by emergency medical personnel.
____________
aThe names of similar forms in different states vary. They include MOLST (Medical Orders for Life-Sustaining Treatment), MOST (Medical Orders for Scope of Treatment), POST (Physician Orders for Scope of Treatment), COLST (Clinical Orders for Life-Sustaining Treatment), SMOST or SPOST (Summary of Physician Orders for Scope of Treatment), and TPOPP (Transportable Physician Order for Patient Preference). The approach is referred to as the POLST paradigm, and the state organizations or coalitions that oversee the implementation of these medical order programs are referred to as POLST paradigm programs. Program names vary among the states overseeing these forms as well. This chapter uses POLST to apply to all these variations unless the text is referring to a specific program with a different name. See also http://www.polst.org.
bCalifornia, Colorado, Georgia, Hawaii, Idaho, Louisiana, Montana, New York, North Carolina, Oregon, Pennsylvania, Tennessee, Utah, Washington, West Virginia, and Wisconsin (Wisconsin has been endorsed only regionally).
cBecause of the high likelihood that resuscitation near death will be unsuccessful and will only cause injury and distress, the term “do not attempt resuscitation” is also used. It has been suggested that “allow natural death” may be a less threatening term than “do-not-resuscitate” (Venneman et al., 2008).
United States to effectively engage various population groups through religious, veterans, and other organizations with which they are connected and makes advance directives and related resources available through its Caring Conversations® initiative.5 Nationally, the American Bar Association Commission on Law and Aging6 has produced a comprehensive “Consumer’s
_______________
5See https://www.practicalbioethics.org/resources/caring-conversations (accessed December 16, 2014).
6See http://www.americanbar.org/groups/law_aging.html (accessed December 16, 2014).
Toolkit for Health Care Advance Planning” covering important issues such as selecting a health care agent and weighing odds of survival, as well as state-specific advance care planning information (American Bar Association, 2005). National Healthcare Decisions Day7 has been held on or near April 16 since 2008. This 50-state public awareness campaign is designed to motivate people to select a health care agent and prepare a living will, to advise them where to obtain these documents, and to link them to resources that can help in having difficult conversations. More recently, The Conversation Project8 was launched by author Ellen Goodman in 2010 as a grassroots public campaign designed to change and increase the conversation around end-of-life care long before a medical crisis occurs (see Chapter 6 for more detail on these and other initiatives).
Medicare covers a one-time initial preventive physical examination (the Welcome to Medicare Preventive Visit) that includes end-of-life planning as a required service for Medicare beneficiaries who desire it (CMS, 2012a). Although this is a one-time service for which the physician is paid, it is seldom used. Of the millions of beneficiaries newly enrolled in 2011, Medicare paid for preventive visits for only approximately 240,000 (CMS, 2012b); the number who chose to receive the advance care planning information is unknown, but was undoubtedly smaller.
At present, all 50 U.S. states and the District of Columbia have laws supporting advance directives and the appointment of a health care agent (through what is often called a durable power of attorney for health care; see Box 3-1) (Gillick, 2010). An examination of policies regarding advance directives in a dozen large nations around the world9 found that “the U.S. stands alone in terms of attention paid to advance directives, perhaps due to the emphasis on individual rights and [a] highly litigant system” (Blank, 2011, p. 210). This chapter examines what the U.S. effort in this area over the past 40 years has accomplished. (For a discussion of the 2009 controversy over death panels, see Chapter 6.)
THE CURRENT STATE OF ADVANCE CARE PLANNING AND WHAT IT ACHIEVES
The ethical principle of autonomy underlies much of the thinking about advance care planning in the United States. But the principle of autonomy—particularly with a growing segment of the population that highly values
_______________
7See http://www.nhdd.org/public-resources (accessed December 16, 2014).
8See http://theconversationproject.org (accessed December 16, 2014).
9The other countries in this review were Brazil, China, Germany, India, Israel, Japan, Kenya, Netherlands, Taiwan, Turkey, and the United Kingdom. Usage of advance directives is low in other countries, even in those whose legal systems allow them (Blank, 2011).
other principles, such as family cohesion—is showing signs of stress. Trying to determine in advance how one might want to be treated in some hypothetical future state is highly problematic (Loewenstein, 2005). Moreover, according to the President’s Council on Bioethics (2005, p. xix), the process gives “major ethical weight to personal autonomy and choice and personal pride in self-sufficiency. But in so doing, it deliberately ignores the truth of human interdependence and of our unavoidable need for human presence and care.” And human presence and care are exactly what is needed by the overwhelming proportion of people unable to make their own decisions near the end of life.
Who Have Made Their Wishes Clear?
It’s always too early, until it’s too late.
—The Conversation Project, 2013
Most people have no documentation of their wishes regarding end-of-life care, and few have talked with either their family or physician about the subject (Clements, 2009). (See also the subsequent discussion of specific population groups.) A 2013 national survey of nearly 2,100 Americans aged 18 and older found that, while 90 percent believe having family conversations about wishes at the end of life is important, fewer than 30 percent have done so (The Conversation Project, 2013).
I have served as a clinical chaplain in home health hospices and as an independent health care ethics consultant and educator for community-based organizations over the past 10 years. I have learned over this time that it is extremely difficult for patients and their families and caregivers to address end-of-life decisions. Changes in the patient’s physical, mental, and spiritual states, the news of the diagnosis, the impact on family, friends, caregivers, and even the community at large, all contribute to the emotional stress of decision making at this point in a person’s life.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
According to results of a 2012 survey (CHCF, 2012), the demographic groups most likely to have had a discussion about end-of-life issues with a loved one were those aged 65 and older, whites, people with higher education and income, and those with one or more chronic conditions (see the
next section for discussion of differences among population groups). And while 42 percent of respondents reported having such a discussion, only 23 percent had put their wishes in writing. More than three-quarters of respondents said they would “definitely” or “probably” want to talk with their doctor about their wishes for medical treatment toward the end of life if they were seriously ill (47 and 32 percent, respectively); however, more than 90 percent said a doctor had never asked them about those issues. Among respondents aged 65 or older—the prime age group for having chronic illnesses—84 percent had not been asked.
The older people are, the more likely they are to have participated in some kind of advance care planning activity, as shown in Table 3-1. Other factors that increase the likelihood of having an advance directive include more education, having a close family member or confidant, recent hospital admission, and having a close family member who died with pain or suffering (Carr and Khodyakof, 2007). Although marital status and number of children did not affect the likelihood of having an advance directive in the study by Carr and Khodyakof (2007), those with dependent children were significantly less likely than those without dependent children to have any advance care planning documents in place (Nilsson et al., 2009).
According to the HHS (2008) review, advance care planning is least likely to take place in hospitals and intensive care settings, perhaps because of patients’ physical, mental, or cognitive state or because the overriding impulse is to provide what the authors call aggressive treatment. By contrast, nursing home residents are more likely than individuals in other care settings to complete advance directives.
Why People Do Not Participate in Advance Care Planning
Many factors contribute to whether people complete some sort of advance directive form. For example, people who believe doctors, not patients, should make decisions about health care and those who have a greater fear of death are significantly less likely to complete a form (Carr and Khodyakov, 2007). However, when people reluctant to complete advance directives hear the personal stories of others who have had to make end-of-life decisions for a loved one without any guidance, the desire to save their family from these painful experiences can become a prime motivator for putting their own wishes in writing (Halpern, 2012a; Steinhauser et al., 2000a).
The many and varied requirements embedded in state laws covering advance directives also discourage their completion. Problems include poor readability and lack of clarity in some state-mandated forms; restrictions on who can serve as health care agents and limitations on their authority; procedural requirements, including the need for witness signatures or no-
TABLE 3-1 Participation in Advance Care Planning Activities, U.S. Adults
| Associated Press-National Opinion Research Center (AP-NORC),a 2013 (people 40+) (%) | National Council on Aging (NCOA)-United Healthcare-USA Today,b 2013 (people 60+) (%) | California HealthCare Foundation (CHCF),c 2012 (all ages) (%) | Excellus BlueCross BlueShield Upstate New York,d 2013 (working-age population) (%) | |
| Have an advance directive | 47 | 54 | 23 | |
| Discussed care preferences with a loved one | 41 | 62 | 42 (higher among those 65 and older) | |
| Designated a health care power of attorney (or equivalent) | 49 | — | 58 | |
SOURCES:
aTompson et al., 2013: telephone survey conducted by the AP-NORC Center for Public Affairs Research from February 21 through March 27, 2013, among a nationally representative sample of 1,019 American adults aged 40 and older.
bNCOA et al., 2013: telephone survey conducted by Penn Schoen Berland from April 4 through May 3, 2013, among a national sample of adults, including 1,007 respondents aged 60 or older, and an oversample of low-income adults aged 60 and older, including those with three or more chronic health conditions and those living in Birmingham (Alabama), Indianapolis (Indiana), Los Angeles (California), Orlando (Florida), and San Antonio (Texas).
cCHCF, 2012: statewide survey conducted by Lake Research Partners from October 26 through November 3, 2011, among a representative sample of 1,669 Californians aged 18 and older, including 393 respondents who had lost a loved one in the previous 12 months.
dPersonal communication, P. Bomba, Community Conversations on Compassionate Care and employer groups, March 1, 2014. Upstate New York data were collected as part of a serial data collection on advance care planning among ~6,000 employees of Excellus BlueCross BlueShield and other subsidiaries in Upstate New York since 2002. Results reflect a 2013 data update. (http://www.compassionandsupport.org/pdfs/research/2006_Employee_Health_Care_Decisions_Survey_Results_Report.pb.092406.FINAL.pdf [accessed December 16, 2014]).
tarization; inadequate reciprocity across states; and inadequate reflection of different religious, cultural, and social characteristics of individuals and families (Castillo et al., 2011).
According to Fried and colleagues (2010, p. 2329), advance care planning “may best be understood as a health behavior, for which individuals have highly varied motivation, barriers and facilitators, and self-efficacy regarding their participation.” It may be efficacious to tailor information to the readiness of individuals to participate in specific advance care planning activities, an approach similar to how the stages of change model has been used to help people adopt health-promoting behaviors, such as smoking cessation (Orleans and Cassidy, 2011).10 A stages of change strategy for advance care planning would approach people differently depending on whether they needed help in completing an advance directive, naming a health care agent, or communicating their preferences to their physician or family members (Fried et al., 2010). Individuals vary greatly in their readiness to participate in each of these activities.
A 2012 California survey (CHCF, 2012) asked adults (all ages) whether they had spoken with a loved one about their wishes for end-of-life medical treatment. Among those who had not, the most important reasons given were
- too many other things to worry about right now (41 percent);
- don’t want to think about death or dying (26 percent), cited by 38 percent of Latinos and 26 percent of Asians and Pacific Islanders, but only 15 percent of African Americans and of non-Latino whites; and
- family member did not want to discuss it (13 percent).
Another reported reason patients (versus the public) do not participate in advance care planning is that they “would rather concentrate on staying alive than talk about death” (Ganti et al., 2007; Knauft et al., 2005, p. 2190).
Reluctance to engage in advance care planning sometimes originates in patients’ sense that the initiative to do so should come from clinicians—hence “the importance of clinicians bringing up advance care planning with their patients who may be fearful of discussing the topic with family or be waiting for some one else to initiate discussion” (Phipps et al., 2003,
_______________
10In the Orleans and Cassidy (2011) review, the stages of change are specified as precontemplation (not thinking about participating in the activity yet), contemplation (thinking about participating in the next 6 months), preparation (planning to complete the activity in the next 30 days), action (participated in the activity within the past 6 months), and maintenance (participated in the activity more than 6 months ago).
p. 553). Finally, people often do not realize they have a terminal disease, what that disease is, or that they are dying (Gardiner et al., 2009).
My mother died in January 2012. She was in a nursing home for the last 7 weeks of her life and in a hospital for 2 weeks prior to that. At no time did a doctor or nurse say to me, “I’m sorry, but there is nothing we can do for your mother—let’s plan for her to have an easy death.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
The Choice of a Health Care Agent
With respect to the choice of a health care agent, the following general points apply:
- Married people overwhelmingly choose their spouse (Carr and Khodyakov, 2007). Spousal proxies have been found to be more accurate than adult children in their assessment of an elder’s wishes (Parks et al., 2011; but see the quote below for a counterexample), with wives being more accurate than husbands (Zettel-Watson et al., 2008).
- Unmarried and widowed parents choose a child and rarely some other relative, friend, or professional, although in families with only one or two children, a child is less likely to be selected (Carr and Khodyakov, 2007).
- People without a spouse or children choose another relative, such as a sister or a brother or perhaps a friend or a colleague (Carr and Khodyakov, 2007).
The above pattern is not universal, however, and “individuals will innovate to meet their own needs and the presumed needs of their loved ones” (Carr and Khodyakov, 2007, p. 188)—for example, when they believe decision making would be too stressful. Being a health care agent is a difficult job and an extra burden on an already stressed spouse, partner, parent, or child. Close family members may be unable to separate their feelings from the needs of the situation, be unwilling to face the prognosis or talk through the patient’s wishes, or be unable to handle conflicts that arise among family members or with clinical staff. Family members who can answer yes to the following questions are less likely to struggle with the agent role: Do
My mother was 99 when she fell, fractured her hip, had a mild heart attack, and became unconscious. EMTs [emergency medical technicians] took her to the hospital. The surgeon there said she needed a hip operation to relieve the pain. I knew Mom would not want that. For several years, she had told me and my stepfather that she “was ready to go” and didn’t care about living to 100. Her quality of life had clearly deteriorated.
When I saw Mom in the ICU, she was surrounded by beeping monitors and tubes, with nurses running in and out. Her head thrashed from side to side, and she couldn’t recognize anyone. She kept repeating, “I already died once, why am I still here?” and “Let me go, let me go.” It was heartbreaking.
Some years earlier, Mom told me she had assigned me her health care durable power of attorney. I never asked to see the documents, because I thought it would be “impolite.” The day of Mom’s crisis, I found out that my stepfather, who was devastated and grieving, had health care power of attorney for Mom, and I was merely the backup. Shockingly, he agreed to the operation, which was scheduled to begin in 3 hours, and I had no legal power to stop it.
I had a hard talk with my stepfather and reminded him of Mom’s wishes. An hour before the operation, he agreed to talk to a hospice representative, who said Mom was eligible for hospice at their facility. Three hours later, Mom was in a quiet, machine-free hospice room, on increased pain medication, looking much more tranquil, with calm, relaxed breathing. She died 10 hours later, in that peaceful state. I know we did what she wanted.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
you have prior experience as someone’s health care agent, and have you had prior conversations with the patient about treatment preferences? (Majesko et al., 2012). Box 3-2 lists some of the key considerations in an individual’s choice of a health care agent.
An obvious and important consideration is the availability of the agent. In a survey of almost 300 physicians regarding their recent experiences with
BOX 3-2
What to Keep in Mind When Choosing a Health Care Agent
The person you select as an agent must:
- Meet legal criteria (for example, be a competent adult and at least age 18 years)
- Be willing to speak on your behalf
- Be willing to act on your wishes
- Be able to separate his/her own feelings from yours
- Live close by or be willing to come
- Know you well
- Understand what is important to you
- Be willing to talk with you now about sensitive wishes
- Be willing to listen to your wishes
- Be able to work with those providing your care to carry out your wishes
- Be available in the future
- Be able to handle potential conflicts between your family, close friends
SOURCE: Compassion and Support, 2010, p. 7.
patient decision making, most (73 percent) reported having to make major decisions for patients, for various reasons. One in five reported difficulty contacting agents, and one in four reported never having talked to agents personally (Torke et al., 2009).
Most states have established default systems for authorizing surrogates. Thus, even if a proxy form is not signed or if the chosen health care agent is not reasonably available, a priority list of people who can make decisions if the patient cannot is generally in place. State laws vary, but such lists generally start with the immediate family. In some states, lists include domestic partners or close friends or senior officials in religious organizations, and in some, they include physicians, often in consultation with an ethics committee or other physician (in other states, physicians cannot take on this role). To the extent possible, default surrogates are charged with making decisions (substituted judgment) reflecting to the extent possible the patient’s likely decisions, best interests, instructions if any, or personal values (American Bar Association, 2009; Kohn and Blumenthal, 2008).11 If patients have not thoroughly discussed their wishes, however, it is unlikely that surrogates,
_______________
11Ostensibly, these laws provide the maximum feasible protection of the wishes of the incapacitated person and “the fundamental right to make health care decisions for oneself” (Kohn and Blumenthal, 2008, p. 9) (as expressed in the laws of Illinois, Louisiana, and Utah, for example).
even family members, can accurately gauge what those preferences would be despite believing to the contrary (Kohn and Blumenthal, 2008).
Although surrogacy laws meet most situations, they fall short, for example, in serving families in which intergenerational and group decision making are highly valued or cultural groups more likely to select a non-family member as health care agent (Kohn and Blumenthal, 2008). Further, the underlying presumption of health care proxy statutes is that people will have a spouse, child, sibling, or close friend whom they can name as their agent. Many people, especially among the elderly, have no such person. While data on the number of such people are lacking, they may represent 3 to 4 percent of the nursing home population alone (Karp and Wood, 2003). In many states, should they become unable to make or communicate their own health care decisions, no one has the authority to make those decisions unless a court deems them legally incompetent and appoints a guardian. Because such guardians may be strangers with little or no evidence of the patient’s prior wishes, there is no assurance their decisions will be what the patient would have chosen. In the absence of clear guidance from the patient and in light of the consequent uncertainty, the default decision often is to treat the patient’s various conditions regardless of likely benefit.
Do Clinicians Follow Patients’ Previously Expressed Wishes?
Data on the impact of advance directives on the treatment received by patients suggest that directives are not always followed. In one large study, for example, 92 percent of people had recorded a preference for what the authors call comfort-focused care in their living will, but this desire was “poorly correlated with treatment delivered” (Kelley et al., 2011, p. 240). In a study of advanced cancer patients, 13 percent received life-extending treatment in the last week of life despite a stated preference for treatment focused on relieving pain and discomfort (Mack et al., 2010b).
While the predominant conversation about advance care planning focuses on people who want to avoid intensive and nonbeneficial medical interventions, the recent controversy over “death panels” (see Chapter 6) makes clear that many Americans worry about being denied care, and some clinicians believe patients may fear they will give up on care too soon (Gutierrez, 2012). Yet while some people, at least in the abstract, do want every treatment the health system can offer (Pew Research Center, 2013; Veysman, 2010), a study of people aged 60 and older at the time of death revealed that fewer than 2 percent (10 subjects) of those with a living will wanted “all care possible” (Silveira et al., 2010). In another study, involving people with advanced cancer who were aware they were terminally ill, just 17 percent wanted supposed life-extending treatment (Mack et al., 2010b). If patients with serious advanced illness receive less intensive treat-
ment than desired, the difference may reflect a lack of treatment options. For example, one study found more frequent mismatches between desire for intensive treatment and services received for patients with cancer than for those with congestive heart failure or chronic obstructive pulmonary disease. The authors conclude that “it is probable that many [cancer] patients reached a point in the course of their illness where treatment options were limited regardless of the patient’s preferences” (Cosgriff et al., 2007, p. 1570).
Physician Concerns
Several studies have explored the extent to which physicians comply with directives such as living wills and what factors may influence their actions in this regard. One such study found that most primary care physicians would honor a patient’s advance directive even if it were 5 years old (80 percent) or even if the patient’s spouse requested continued resuscitative care (74 percent).12 Fear of legal liability was a concern, including for one-third and one-half of respondents in these situations, respectively (Burkle et al., 2012), and for a large percentage of emergency physicians (58 percent) (Marco et al., 2009). In general, physicians believe their liability risk is greater if they, mistakenly, do not attempt resuscitation than if they provide it against patient wishes (Burkle et al., 2012). As in so many other instances, the default is to treat.
Burkle and colleagues (2012) found that almost 60 percent of the physicians in their study were not likely to honor the wishes of patients whose advance directives indicated they wanted to “pass away in peace” if such patients were in a sudden acute situation (ventricular fibrillation) and likely to be treated successfully (including 45 percent who considered it unlikely that they would honor the advance directive and 14 percent who were unsure). The fact that the remainder would honor patients’ directives in such a situation suggests that, despite several decades of experience, some 40 percent of physicians remain confused about the purpose and interpretation of advance directives. This is true even among emergency medical personnel and hospital residents likely to be called upon under urgent circumstances. Several small studies have shown that some clinicians assume a living will’s instructions apply even if the patient does not have the requisite terminal condition or persistent unconsciousness (Mirarchi et al., 2008, 2009, 2012).
_______________
12By contrast, a survey involving more than 10,000 physicians found that more than half (55 percent) would not consider halting life-sustaining therapy because the family demanded it; for 29 percent, that decision would depend on circumstances (Kane, 2010).
System/Logistical Challenges
Patients’ advance care preferences cannot be followed if the record of those preferences cannot be found and/or is not up to date. People’s preferences change over time and with hospitalization (Chochinov et al., 1999; Ditto et al., 2006; Fried et al., 2007), which may partially explain why the actual preferences of patients differ from what is documented in their medical record (Volandes et al., 2012a,b). Yung and colleagues (2010) found that advance directives for 53 percent of patients (aged 75 and older and in fragile health) who said they gave them to their health care provider were not in their medical record, nor was there any indication of their existence. This percentage was much higher—83 percent—for a separate cohort of patients aged 65 and older and also in fragile health. For patients who said they had not provided an advance directive to their provider but had communicated information about their health care agent, that person’s name and contact information was in the medical record zero percent of the time for patients under age 75 and 16 percent of the time for those aged 75 and older.
Even if the clinician remembers the conversation and the patient’s wishes, recording those preferences is critical “in a health-care system that relies on teams of providers in different settings” (Yung et al., 2010, p. 866) and in which frequent care transitions occur near the end of life (Lakin et al., 2013). Researchers attempting to track the continuity of advance care planning documentation across care settings found that when patients transitioned from provider office to hospital or emergency department, the likelihood that advance care planning documentation would be available and/or in concordance “was no greater than chance” (Yung et al., 2010, p. 865). As discussed in detail in the section on electronic health records later in this chapter, data standards for electronic health records that help promote document portability, availability, and agreement do not require robust documentation of advance care planning.
The implementation of advance directives for pediatric patients entails several particular barriers. For example, emergency department personnel are uncomfortable honoring them, schools may not accept them, and parents seeking to honor their children’s wishes encounter negative reactions from others (Lotz et al., 2013).
Conflicting Views
There are two schools of thought regarding how binding advance directive instructions should be: one is that they should be followed strictly, and the other holds that “it is simply not possible for people to anticipate [their future] decisions about life-preserving treatment with any degree of
accuracy” (Bomba et al., 2012; Sahm et al., 2005, p. 297). Further, prior instructions may not fit the current situation or reflect advances in treatment options. These problems, it is said, are compounded by the lack of clarity in the wording of many advance planning documents. The question is not just what they mean in some abstract sense but what they meant to the person who completed them, who now can no longer amplify or explain and whose mind may have changed with time and altered circumstances.
A German study found that nonclinicians had a much more flexible approach than clinical personnel to interpreting advance directives (Sahm et al., 2005). The authors conclude that the uncertainties around decision making are a strong argument for employing sound clinical judgment in the final phases of a patient’s life. They suggest that a preferable alternative to rigid advance directives is comprehensive advance care planning, which can take into account a broader array of issues and social relationships and can include spiritual and cultural matters, as well as practical concerns.
Taking this argument a step further are those who recommend that advance care planning’s main objective should not be to make advance treatment decisions, but “to prepare patients and surrogates to work with their clinicians to make the best possible in-the-moment medical decisions” (Sudore and Fried, 2010, p. 259). It is suggested that health care agents need this flexibility because they will have to live with the decisions they make (Vig et al., 2006). In one study, the majority of patients (55 percent) gave their surrogates leeway to consider the benefits and burdens of treatment and “specify processes rather than outcomes in their preferences for end-of-life care” (Shapiro, 2012, p. 226).
Conflicts in the implementation of advance directives occur in certain typical situations: when the directive requests a type or intensity of care that, at the time of the event, is judged by clinicians or family not to be in the patient’s best interest, and when the health care agent disagrees with the patient’s request. State laws differ regarding the circumstances under which families can override advance directives. In addition, many hospitals have nonbeneficial care policies and/or refer such cases to the ethics committee for resolution.
Does Advance Care Planning Affect Patient and Caregiver Outcomes?
Advance care planning influences the quality of care and patient and family satisfaction in several ways:
- People who participate in advance care planning generally but not always choose treatment focused on relieving pain and discomfort over life-extending treatments and enroll in hospice earlier, thereby
- avoiding many physical and psychological stresses (Mack et al., 2010b; Wright et al., 2008).
- Advance care planning gives patients and families the opportunity to start preparing mentally and emotionally for death (Martin et al., 1999; Steinhauser et al., 2000a).
- Advance care planning supports several of the primary concerns of people with life-limiting illnesses: involvement, clear communication, shared decision making (Steinhauser et al., 2000b), and a sense of control (Edwards et al., 2010; Martin et al., 1999).
- By stating the kind of care they want in advance, patients may alleviate the burden of decision making on family members (Billings, 2012; Detering et al., 2010).
- Among children and youth, participation in systematic advance care planning programs may enhance positive emotions and facilitate communication, lead to treatment modifications (for example, withdrawal of ventilator support and addition of opioid analgesia), and support having death occur at home (Lotz et al., 2013).
Comparing the survival of patients with and without advance care planning13 before stem cell transplant therapy revealed that those without such documents were significantly more likely to die within 1 year of transplant than those who had them (Ganti et al., 2007). This finding led researchers to conclude that the discussions were not deleterious to patients and that those “who did not engage in [advance care planning] were the most likely to face a situation in which [it] might have helped” (p. 5647). Another study found that discussions of do-not-resuscitate orders did not result in worse psychosocial functioning, including greater anxiety or depression, among either patients or caregivers (Stein et al., 2013).
The impact of advance care planning for the elderly has been studied, and the results parallel those found in other population groups. Elders do engage in such discussions, most often with family present, if given an opportunity to reflect on their goals, values, and beliefs; to articulate and document their treatment preferences; and to choose a health care agent. Those who have these discussions are almost three times as likely to have their end-of-life wishes both known and followed, and their family members suffer significantly less stress, anxiety, and depression after their loved one’s death (Detering et al., 2010).14
_______________
13Advance care planning is defined in this study as having one or more of the following: a living will, a power of attorney for health care, or life support instructions (Ganti et al., 2007). No distinction is drawn between completion of such a document with and without comprehensive discussion with the physician.
14Of those receiving the advance care planning intervention, 10 percent of patients’ wishes were unknown; 3 percent of patients’ wishes were known but not followed.
Research related specifically to advance care planning among people with heart failure, chronic obstructive pulmonary disease, cancer, and dementia, discussed in Annex 3-1 at the end of this chapter, provides many insights into the role of advance care planning in several of the most common causes of death in the United States. It reveals that for each of these conditions, high-quality palliative care, which includes the goal-setting activities of advance care planning, would be an important parallel focus of treatment, but in each case is not the current standard of care.
What Are the Effects of Advance Care Planning on Health Care Agents and Families?
Health care agents and surrogates (including those who are family members) are critically important for the 44 to 69 percent of nursing home residents with decisional impairment (Kim et al., 2002). Agents may also make decisions for large numbers of geriatric patients who retain decisionmaking capacity yet defer decisions to family members (Vig et al., 2007).
Even when patients’ preferences are clear to health care agents—which too often they are not (Fried and O’Leary, 2008)—the decisions these agents must make do not come without difficulty (Schenker et al., 2012). Moreover, “surrogates are not perfect ambassadors of patient preferences” (Vig et al., 2006, p. 1688). Often, caregivers (usually family members) want life-sustaining measures used even when patients do not (Phipps et al., 2003). At times, health care agents may be required to make a decision at odds with patients’ expressed wishes (to die at home, for example) when clinical circumstances evolve differently than anticipated.
Health care agents’ decisions inevitably are colored by their own wishes and care preferences, feelings of overwhelming responsibility, religious beliefs, and the desire for family consensus (Fritch et al., 2013; Schenker et al., 2012). Interviews with health care agents have revealed the broad range of bases on which they make their decisions: conversations with patients, the agents’ own beliefs and preferences, input from others close to the family, shared values and life experiences, and written documents (Vig et al., 2006).
When health care agents cannot meet patients’ requests, they feel regret or guilt that may lead to complicated grief and bereavement (Fried and O’Leary, 2008; Topf et al., 2013).15 Family decision making can have a significant and sometimes long-term negative psychological impact, including stress, guilt, doubt, grief, and even increased thoughts of suicide, especially among spouses (Abbott et al., 2013; Wendler and Rid, 2011). Wendler and
_______________
15Complicated grief is long-lasting and shares elements of both depression and posttraumatic stress disorder. For a full description, see http://www.health.harvard.edu/fhg/updates/Complicated-grief.shtml (accessed December 16, 2014).
TABLE 3-2 Stresses on Health Care Agents and Examples of Potential Remedies
| Stressor | Potential |
| Uncertainty about patient preferences | Remedy More thorough advance care planning |
| Uncertainty about prognosis | Conversation about key decision points |
| Discomfort with the hospital environment | Familiarizing family members with the hospital; explaining why certain procedures are followed, who directs various aspects of care, and whom to ask for what |
| Discomfort with the logistics of making decisions | Ensuring that information is conveyed in a thorough and unhurried manner; use of a shared decision-making model |
| Poor communication by clinicians | Targeted communication training for clinical staff; limiting the number of clinicians with whom the health care agent must deal |
| Uncertainty and guilt | Providing support and positive reinforcement for health care agent decisions and adequate subsequent counseling |
SOURCES: Majesko et al., 2012; Vig et al., 2007; Wendler and Rid, 2011.
Rid (2011) reviewed the literature on health care agent stressors and identified a number of problems commonly reported by agents, some of which appear to be at least partly remediable (see Table 3-2).
Risk factors for complicated grief among bereaved caregivers include fewer years of education, younger age of the deceased, and lower satisfaction with social support (Allen et al., 2013). The care provided by hospices may lead to positive health outcomes, including survival, among the bereaved and may help some people avoid long-term depression and other consequences of complicated grief (Christakis and Iwashyna, 2003). A hospital-based family support specialist who maintains connections with health care agents can provide emotional, communication, decision, and anticipatory grief support (White et al., 2012).
Negative mental health effects among family members of ICU patients in one study were markedly higher (reaching 82 percent) if family members believed the information received from the staff to be too rushed, unclear, or incomplete or if they shared in end-of-life decision making (Azoulay et al., 2005). Having an advance directive reduces bereaved family members’ concerns about physician communication or lack of information (Teno et al., 2007). Health care agents may also be helped by previous decision-
making experiences; effective coping strategies; supportive life circumstances; a belief that their decisions will result in a “good” outcome; and having a clinician who is available and who provides frank information, recommendations, and respect (Back et al., 2010; Vig et al., 2007).
An approach to working with families that supports both emotional reasoning and medical requirements has been suggested, allowing patients, families, and physicians to “expand their medical focus to include disease-modifying and symptomatic treatments and attend to underlying psychological, spiritual, and existential issues” (Back et al., 2003, p. 439). Health care agents who have been well prepared, who have the support of other family members and the clinical team, and who have been given some reasonable leeway in carrying out their role will be able to do so with fewer long-lasting negative effects. Effective preparation has been shown to be best achieved when the patient-agent discussion is guided by a trained facilitator (or other knowledgeable person), when there is an opportunity to discuss concerns, and when patient misconceptions regarding the likely outcomes of treatment are corrected (Fried et al., 2002; Jezewski et al., 2007; Kirchhoff et al., 2010). Grief and bereavement are a natural corollary to losing a loved one; unrelieved stress-related problems are not.
Does Advance Care Planning Affect Health Care Costs?
The purpose of comprehensive advance care planning is to ensure that people receive the care they desire and minimize the burden on their families. In doing so, an additional benefit may be lower health care costs. This is useful to know given that proposals to expand and improve advance care planning programs will almost certainly be met with the argument that they are “too expensive.” The evidence presented in this section suggests just the contrary.
Several large studies have attempted to assess the impact of advance care planning on health care costs. One found no association between advance care planning (either reported completion of an advance directive or discussion of care preferences) and Medicare expenditures in the last 6 months of life (Kelley et al., 2011). Another study compared costs for people who had “treatment-limiting advance directives” and those who did not (Nicholas et al., 2011). People with such directives had lower rates of life-sustaining treatment (34 percent versus 39 percent), were less likely to die in the hospital (37 percent versus 43 percent), and were more likely to use hospice (40 percent versus 26 percent). All these care differences were statistically significant. But again, median fee-for-service Medicare spending in the last 6 months of life was not significantly different for the two groups ($21,008 for the treatment-limiting group versus $21,614 for the group without a treatment-limiting advance directive).
Another analysis of this study compares spending for decedents in low-spending regions of the country (who were significantly more likely to have a treatment-limiting advance directive) with spending for decedents in higher-spending regions (Nicholas et al., 2011). Although the two groups had similar cause-of-death and comorbidity patterns, the costs of care in the last 6 months were substantially different. The largest differential was between spending for people with a treatment-limiting advance directive in low-spending regions ($14,153) and spending for those without a directive in high-spending regions ($26,616). These data further suggest that having an advance directive made no statistically significant difference in predicted spending in the low- and medium-spending regions; in the high-spending regions, however, a treatment-limiting advance directive might save $5,585 per death, primarily as a result of lower hospital utilization rates. Thus, this study demonstrates “a statistically and economically significant relationship between advance directives and regional practice patterns” (Nicholas et al., 2011, p. 1452).
A large portion of hospital costs at the end of life is associated with ICU care. One study found that among Americans who died, the cost of a terminal hospitalization with an ICU stay was an estimated $38,000, compared with $13,000 if ICU care was not included (both of these figures are in 2010 dollars) (Zilberberg and Shorr, 2012).
Assessing patients’ end-of-life preferences and providing care congruent with their values, along with coordinating the care provided by different clinicians and institutions, produces important improvements in clinical care. In one such model program, the Sutter Health Advanced Illness Management program, this combination of approaches appeared to save about $2,000 per month per patient in direct care costs (Meyer, 2011).
Lower rates of hospital deaths and higher rates of hospice enrollment occur when the care team pays attention to more than patients’ physical condition—specifically, to their religious and spiritual concerns (Flannelly et al., 2012). Such whole-person care “may assist patients in recognizing less aggressive [end-of-life] care options that remain consistent with their religious/spiritual beliefs” (Balboni et al., 2011, p. 5389). In this study, the estimated care costs in the last week of life for cancer patients who reported high spiritual support were $2,441 less than costs for those who reported less spiritual support.16
Finally, in a cohort of 603 advanced cancer patients, 188 reported discussing their end-of-life care preferences with their physicians (Zhang et al., 2009). Costs of care in the last week of life were 36 percent lower among
_______________
16These findings were adjusted to take into account potential confounders such as advance directives and advance care planning.
patients who had the care discussion, amounting to savings of $1,041 per patient in 2008 dollars.
ADVANCE CARE PLANNING AND TREATMENT PREFERENCES AMONG SPECIFIC POPULATION GROUPS
This section describes what is known about advance care planning and treatment preferences among people in specific groups described by age, disability state, religious affiliation, ethnicity, and literacy level. An important caveat is that all of these groups include individuals with a full range of attitudes and preferences, and the generalities that may be derived from population studies may not apply at all to a specific patient and family. Chapter 1 of this report notes the importance of patient-centered care for people nearing the end of life; the wide variation in preferences that exists in any group reinforces the need for end-of-life care that approaches each individual and family as unique.
Children and the Elderly
Children
The typical barriers to conducting advance care planning in adult populations—reluctance to discuss dying, cultural norms that support family-level decisions, clinician time constraints, unpredictable disease trajectories, and insufficient clinician preparation to conduct such discussions—also are present when the patient is a child.17 In addition, the process is made more difficult by concerns regarding the child’s cognitive and emotional development and both the child’s and parents’ readiness to participate in such conversations; the emotional burden on parents and caregivers; differences in understanding of prognosis between clinician and child/parent; unrealistic expectations among parents; and the need for a three-way conversation and communication among parents, children, and clinicians (Durall et al., 2012).
Nonetheless, advance care planning models suitable for children and adolescents have been developed. Even suitable adult advance directives have been used successfully with younger people. When combined with in-depth counseling (such as Gundersen Health System’s Respecting Choices model, discussed later in this chapter), they have greatly increased the proportion of adolescent patients who give their families the leeway to “do what is best at the time,” increased information available to the patient and family and improved patient understanding about end-of-life decisions, and
_______________
17The term “child” here encompasses adolescents.
I am a pediatrician, specializing in care of children living with HIV. Discussions regarding end-of-life care of children are always difficult. Many family members (and health professionals) shy away from the issue. Speaking directly with the child or adolescent is both extremely important and extremely difficult. Spiritual care is often neglected, as it is kept separate from medical discussions.
There is great need to treat the child as a child—a complex, multifaceted individual—and not as an impersonal medical case. Children have much greater insight into their own conditions and realities than they are given credit. The death of a child is and should be heart-breaking. However, end-of-life care should not be treated as a taboo subject, especially when speaking directly with the child/adolescent. Successes in end-of-life care for children come from strong, supportive relationships with health care providers, counselors, spiritual leaders, and family members.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
increased patient and family agreement about decisions to limit treatment (Lyon et al., 2009, 2013).
Five Wishes,18 an advance directive written in nontechnical language, includes identification of a health care agent, as well as choices about medical and nonmedical treatment and comfort. Wish 5—“what I want my loved ones to know”—lets patients describe how they want to be remembered and in a group of adolescents and young adults, was deemed the most helpful part of the document (Wiener et al., 2008). Five Wishes is available in child and adolescent/young adult versions (Wiener et al., 2012).
Available guidelines for making end-of-life treatment decisions for pediatric patients tend to be broad, and research has yet to fully establish their usefulness in clinical settings (Hinds et al., 2010). Making decisions that will not forestall the death of a terminally ill child and involving the child in the decision that will end his or her life “are startling concepts,” say Hinds and colleagues (2010, p. 1049). From these authors’ vantage point of working in pediatric oncology, enabling a peaceful death is part of providing care of the highest quality. The way these decisions are made and a respectful reaction to parents’ decisions “can color all of their pre-
_______________
18See http://www.agingwithdignity.org/five-wishes.php (accessed December 16, 2014).
ceding treatment-related interactions, and may influence how well parents emotionally survive the dying and death of their child” (Hinds et al., 2010, p. 1049).
The capacity or incapacity of children to participate in end-of-life decision making cannot be assumed and must be individually determined at each decision point (Hinds et al., 2010). This capacity begins at least by age 10 and in some cases by age 6, and depends in part on children’s own appraisal of their health and well-being. Because of their experiences, many children are perceptive judges of the balance between the burdens and benefits of treatment. Even children aged 5-6 can be capable of remarkably insightful abstract leaps and often express their views in drawings and stories, for example.
Few studies of pediatric advance care planning have been conducted, and those generally have involved small numbers of patients and families. A recent review found three reports of systematic advance care planning programs specifically for children, all in the United States (Lotz et al., 2013).19 Although the three program models had similar overall designs, they differed in care setting, target population, participants, and advance directive used. These programs increased completion of advance directives and parents’ initiation of discussions about treatment, and both patients and physicians made increasing use of the programs over time.
The importance of involving children in these discussions is illustrated by research among 24 pairs of adolescents with AIDS and their family decision makers, which found that family members did not recognize when their child wanted to have an end-of-life conversation (Garvie et al., 2012). The great majority of the adolescents (90 percent) wanted to talk about end-of-life issues before entering the dying phase, including 48 percent who thought the best timing for end-of-life decisions was before getting sick and another 24 percent who wanted to have conversations throughout the illness trajectory: before getting sick, when first diagnosed, when first sick, and when dying. While parents may be reluctant to have end-of-life discussions when their child’s health is relatively stable (Edwards et al., 2012), most clinicians (71 percent in the Durall et al. [2012] study) believe advance care planning discussions often happen too late in the course of disease. Anticipatory guidance and reflection on the goals of care during times of both stability and worsening illness are useful (Edwards et al., 2012). Families are more likely to take advantage of palliative care options when they and the care team recognize earlier in the clinical course that a cure is unrealistic and focus instead on reducing suffering (Wolfe et al., 2000).
From the sparse research available, it is clear that parents of children
_______________
19They are the FACE Intervention (Lyon et al., 2009), the Footprints Model (Toce and Collins, 2003), and Respecting Choices (Hammes et al., 2005).
who will not survive need time for making decisions and preparing for their child’s death. Understanding parents’ end-of-life decision making for their children necessitates consideration of the reason, understanding, and emotion they bring to their responsibilities and their roles as parents and as decision makers (Bluebond-Langner et al., 2007). Factors that help parents improve their decision-making capability are opportunities to make decisions that accord with the family’s traditions and values, clear and complete understanding of the child’s condition, and opportunities within each clinical encounter to build trust and reinforce parents’ competence (Hinds et al., 2010; Lannen et al., 2010). In sum, believing “they have acted as ‘good parents’ in such a situation is likely to be very important to their emotional recovery from the dying and death of their child” (Hinds et al., 2010, p. 1058).
The Elderly
Older Americans are more likely than those who are younger to have thought about their end-of-life preferences or completed an advance directive (CHCF, 2012; Pew Research Center, 2013; Tompson et al., 2013). The higher rate of any kind of consideration of end-of-life care reflects age-related increases in the prevalence of chronic illnesses, dementia, other cognitive impairments, frailty, and disability. In one large study,20 the proportion of people with one or more disabilities increased from 28 percent 2 years before death to more than half (56 percent) in the last month of life (Smith et al., 2013a).
In one study of more than 5,000 65-year-old individuals, most were able to articulate their preferences for end-of-life care, and most said they would reject life-extending treatment if they had a terminal illness involving either cognitive impairment or severe physical pain (Carr and Moorman, 2009). That these survey respondents were more likely to avoid life-sustaining treatments in the case of cognitive impairment than in the case of physical pain may indicate the relative importance of these experiences. A separate study, however, found that while pain control was ranked as the most important attribute among both patients and physicians, mental awareness was ranked lower in importance among physicians than among patients (Steinhauser et al., 2000a). “This discrepancy between what patients value and what physicians rate as important could lead physicians to advocate for (or encourage the patient’s family to select)
_______________
20In this study of 8,232 people over age 50 who died while enrolled in the Health and Retirement Study between 1995 and 2010, disability was defined as needing help with at least one of the following activities of daily living: dressing, bathing, eating, getting in or out of bed, walking across the room, and using the toilet.
treatments that do not mesh with the patient’s preferences” (Carr and Moorman, 2009, p. 769).
Infrequently considered is that an older person’s net financial worth is positively associated with participating in any type of advance care planning, regardless of demographic, health, and psychological characteristics. People with higher incomes are more likely to engage in estate and financial planning,21 an activity that frequently includes or otherwise may trigger some aspects of health-related planning, such as establishing a durable power of attorney for health care (Carr, 2012b).
Differences Across Disability Groups
People with Cognitive Impairments
Determining whether an individual patient has the cognitive capacity to participate meaningfully in decisions about end-of-life treatments is a challenge to clinicians, and “physicians regularly fail to recognize incapacity” (Sessums et al., 2011, p. 420). Such a determination is especially challenging when it involves people who live in community group homes and other community settings (rather than in state institutions), especially if they have no family, guardian, or health care agent. Challenges further emerge because of a “lack of clear standards and regulatory guidelines protecting these individuals when institutionalized that do not transfer to the more independent, ‘least-restrictive’ environments of privatized group homes” (Artnak, 2008, p. 240).
Determining capacity generally requires tests of whether patients can understand, retain, and use information about proposed treatment in the decision-making process; appreciate the significance of the decision and use reason in making it; and communicate their choice (Raymont et al., 2004; Sessums et al., 2011). Capacity is task specific. People who lack the decision-making capacity to make certain medical decisions—especially high-risk or exceedingly complex ones—may nevertheless retain the capacity to make simpler decisions and even to choose a health care agent they trust. However, determinations of capacity are not standardized, and although many different instruments for assessing capacity exist, their precision and suitability for different clinical settings vary considerably.22
_______________
21An intriguing recent report found in four analyses that saving money, in itself, is a buffer against anxiety about death by providing a sense of control over one’s fate and protecting people from existential fears (Zaleskiewicz et al., 2013).
22Sessums and colleagues (2011) recommend three capacity-assessing instruments suitable for use in a physician office visit: the Aid to Capacity Evaluation (ACE), the Hopkins Competency Assessment Test (HCAT), and Understanding Treatment Disclosure (UTD). These instruments have robust likelihood ratios (sensitivity/specificity) and moderate to strong levels of evidence.
In some situations, physicians may rely heavily on the views of family members as well as their own knowledge of the fragile health of their patients with intellectual disabilities (Wagemans et al., 2013). Clear communication—verbal and nonverbal—and efforts to avoid possible misunderstandings by using language free of jargon are vital for clinicians serving such patients (Tuffrey-Wijne and McEnhill, 2008).
A study of factors influencing parents’ resuscitation decisions for their institutionalized children with severe developmental disabilities found that a concerted effort to explain treatment options and end-of-life issues resulted in some families’ making a change from full-resuscitation to do-not-resuscitate status (Friedman and Gilmore, 2007). Family members, religious leaders, and discussions with physicians had the greatest influence on those who chose full resuscitation. Families’ perceptions of the child’s quality of life or discomfort did not appear to affect the decision.
Homeless or “Unbefriended” Patients
“Unbefriended” patients who have neither decision-making capacity nor a surrogate decision maker are at particular risk of not having their wishes known or followed. Physicians and institutions need clear guidance on how to handle the care of such patients, with the Veterans Health Administration’s “detailed and transparent process . . . [being] a model for other institutions” (Berlinger et al., 2013, p. 51). That policy describes a collaborative approach that involves the hospital’s senior leadership and guides professionals on how to collaborate with legal counsel if a court-appointed guardian is needed.
Homeless people might be assumed to be a quintessential “unbefriended” population, with high rates of cognitive challenges due in part to underlying mental health problems, substance abuse, and isolation (Karp and Wood, 2003). A test of whether homeless people can and will complete a counseling session on advance care planning and an advance directive was conducted in Minneapolis (Song et al., 2010). More than one-quarter of the subjects completed an advance directive, with a higher rate of completion (38 percent) being seen among those who received guidance from a counselor. About one-third of the group had someone (often a family member) whom they wanted to make decisions about their care in specific clinical situations.
Having a single health professional make unilateral decisions for an unbefriended patient is ethically unsatisfactory in terms of protecting patient autonomy and establishing transparency. Equally troublesome is “waiting until the patient’s medical condition worsens into an emergency so that consent to treat is implied” (Berlinger et al., 2013, p. 51), which compro-
mises patient care and prevents any thorough and thoughtful consideration of patient preferences or best interests.
People with Physical Disabilities
People are not well able to foresee their own (or others’) capacity to adapt to a disability (Stein, 2003), which means that others’ assessments of quality of life, a fundamentally subjective judgment, are not necessarily in accord with those of people with disabilities. The “paradox” of high perceived quality of life despite serious and persistent disabilities has been acknowledged for some time (Albrecht and Devlieger, 1999; King et al., 2012).
People with severe neuromuscular diseases, such as Duchenne’s muscular dystrophy or amyotrophic lateral sclerosis, are not necessarily well served by advance directive language that refers to “extreme disability” as a reason to withhold or withdraw treatment because of the lack of context provided (Stein, 2003). The core definition of quality of life for many people with disabilities is “living well,” and the underlying factors contributing to living well are consistent across disabilities: health status, social connectedness, being oneself (that is, able to continue doing things important to the person), and financial security (Murphy et al., 2009). The possibility of quality of life for people with disabilities nearing the end of life often is ignored (Gill, 2010). Even health care providers familiar with people with disabilities and their lives may hold negative views about their quality of life. According to disability rights advocate Diane Coleman in testimony provided to the committee, “Unfortunately, the disability community . . . has a lot of experience with devaluation by physicians and other health care providers, devaluation that leads to pressure to forego life-sustaining treatment” (Coleman, 2013).
One approach suggested to improve the relevance and suitability of advance care planning to people with disabilities is to reconsider including disabling conditions as a reason for limiting treatment in living wills and make greater efforts to help health care agents understand the complex choices involved when a medical condition or injury might lead to substantial disability (Stein, 2003).
Differences Among Religious Groups
The majority of patients at the end of their lives find religion to be important; however, these needs are supported only minimally or not at all by the current health care system (Balboni et al., 2007). Research has documented a strong role of religious affiliation, although not necessarily denominational affiliation, in both advance care planning and the
nature of treatment preferences at the end of life. In a large survey of mostly white, non-Hispanic individuals aged 64-65, those from traditionally defined religious groups (categorized as conservative, moderate, or liberal Protestant; Catholic; other; and no religion) had similar treatment preferences given two end-of-life scenarios, and the majority of people in all religious subcategories “would reject life-sustaining treatments if faced with an incurable terminal illness” (Sharp et al., 2012, p. 288). However, people holding fundamentalist views,23 regardless of denomination, were significantly more likely to want life-sustaining treatments than their non-fundamentalist counterparts, even after controlling for sociodemographic factors and health status. Two specific attitudes accounted for this difference: fundamentalists were less likely to believe that quality of life is more important than just staying alive and more likely to say that their religious or spiritual beliefs would guide their medical decisions. Similarly, in another study, conservative Protestants and those attributing great importance to religion/spirituality had a lower likelihood of engaging in advance care planning (Garrido et al., 2013). Beliefs about God’s control of life’s length and adherence to values supporting the use of all available treatments were the main factors accounting for the relationships between religiosity and advance care planning.
Additional spiritual beliefs that influence both treatment choices and how those choices are made relate to the origin of illness and well-rooted confidence that miracle cures can occur or that “those who believe in God do not have to plan for end-of-life care” (Balboni et al., 2013; Johnson et al., 2008, p. 1956). For instance, in a prospective, multicenter cohort study, researchers found that positive religious coping (constructive reliance on faith, e.g., through seeking God’s love and care) was associated with receipt of intensive life-prolonging medical care near the end of life (Phelps et al., 2009). Positive religious coping among patients remained a strong predictor of intensive life-prolonging care despite statistically accounting for known demographic (age and race) and psychosocial confounders, including patients’ acknowledgment of terminal illness and completion of advance directives. Thus, the choice of life-prolonging therapies near the end of life among “religious copers” may be driven by their belief in God’s divine healing or hope for a miraculous cure through intensive medical care.
The research literature also identifies a strong interaction between religiosity/spirituality and certain racial/ethnic group membership (Buck and Meghani, 2012; Johnson et al., 2005; Winter et al., 2007). Recent data from the Pew Research Religion and Public Life Project (reported in
_______________
23Defined as “agreeing or agreeing strongly with both of the two statements: (1) the Bible is God’s word and everything happened or will happen exactly as it says and (2) the Bible is the answer to all important human problems” (Sharp et al., 2012, p. 283).
more detail in Chapter 6) reveal that most white mainline Protestants (72 percent), white Catholics (65 percent), and white evangelical Protestants (62 percent) would stop medical treatment if they had an incurable disease and were suffering a great deal of pain. Most black Protestants (61 percent) and Hispanic Catholics (57 percent), by contrast, would tell their physician to “do everything possible to save their lives” (Pew Research Center, 2013, p. 16).
Despite this well-documented relationship between race/ethnicity and preference for intensive life-sustaining treatment at the end of life, mechanisms explaining this relationship are not fully understood. In a large, single-site study with a predominantly African American sample, those who were highly religious and/or spiritual were more likely to have a designated decision maker for end-of-life decisions (Karches et al., 2012). In this study, religious characteristics were not significantly associated with the likelihood of having an advance directive or do-not-resuscitate order. In another study, the effect of race on end-of-life decisions was only partially mediated by a measure of guidance by God’s will (Winter et al., 2007). The authors conclude that other dimensions of spirituality or unique constructs not pertaining to spirituality and religiosity may operate simultaneously in explaining end-of-life preferences among racial subgroups. Thus, pathways to the use of intensive measures to extend life are multifactorial and may go beyond religious beliefs (see the following subsection).
Differences Across Racial, Ethnic, and Cultural Groups24
Patients’ backgrounds, culture, ethnicity, and race influence their perceptions about life, illness, suffering, dying, and death and the meaning they ascribe to these events. These perceptions in turn affect preferences for the kinds of care people want, how much they want to know about their situation and choices, whether and how they want to make treatment choices, whom they want to make those choices if they cannot, and the role of the family in the entire process (Blank, 2011; Kagawa-Singer and Blackhall, 2001).
In the coming years, rapid growth in the proportion of U.S. elderly that are members of racial/ethnic minority groups will challenge clinicians to communicate more effectively with people of many cultural traditions. Between 2010 and 2030, the U.S. white, non-Hispanic population aged 65 and older is expected to increase by 59 percent, whereas the minority population of the same age group will increase by 160 percent (Greenberg, 2011). It is vital, therefore, that clinicians be aware of common differences
_______________
24The terms used to describe population groups in this section vary and are generally those used by the authors cited.
in perception among racial, ethnic, and cultural groups so that at the very least, they can ask the right probing questions and have a firmer basis for individualized understanding of patients and their families.
As noted above, although there are many differences among individual perspectives and actions within groups, the general pattern in minority populations is one of a lack of advance care planning and a preference for more intensive treatments; poorer communication with clinicians is part of this pattern. Although patients and families may not follow clinicians’ advice and recommendations, “avoiding such communication increases the likelihood of poor end-of-life decision making” (Curtis and Engelberg, 2011, p. 283).
In many cultures, collective family decision making—and even sometimes the paternalistic decisions of the family patriarch—is considered as important or more so than patient autonomy (Blank, 2011). Having made reference to the collective wisdom of the family in every other aspect of their lives to that point, dying individuals cannot realistically be expected to make decisions completely on their own or to name a single health care agent. In a presentation to the committee, Rebecca Dresser, a member of the President’s Council on Bioethics (2002-2009), suggested that bioethics has had an unintended and at times negative consequence by focusing on autonomy and ignoring guidance and support (Dresser, 2013).
The fact that racial and ethnic minority individuals are less likely to use advance directives or choose hospice care has been noted in numerous studies in different population groups (Johnson et al., 2008; Ko and Berkman, 2010; Ko and Lee, 2013; Muni et al., 2011; Phipps et al., 2003; Waite et al., 2013; Zaide et al., 2013). At the same time, many authors have found associations between minority race or ethnicity and the receipt of more intensive end-of-life care (see, for example, Barnato et al., 2007; Mitchell and Mitchell, 2009; Muni et al., 2011). This pattern may result from a lack of information about advance planning documents and hospice (Wicher and Meeker, 2012) or from lower levels of general or health literacy (Volandes et al., 2008b). However, Volandes and colleagues (2008a) warn that “while attention to patients’ culture is important, it is also important to avoid ascribing choices to culture that may actually reflect inadequate comprehension” (p. 700). Despite the often high-pressure, complex situations in which end-of-life decisions must be made, clinicians cannot make assumptions about preferences or take communication shortcuts without jeopardizing the quality of care.
The available body of evidence suggests that multiple factors are at work in forming patient and family preferences and in translating those preferences into care (see Table 3-3). As Ko and Lee (2013, p. 6) state, “Taken together, race/ethnicity can be thought of as a proxy for personal, cultural, and social contexts, so that an individual’s values, beliefs, and per-
TABLE 3-3 Summary of Patient and Family Factors in End-of-Life Decision Making Among Individuals of Different Races, Ethnicities, and Cultures
| Factor | Selected Source(s) |
| A combination of beliefs, preferences, and values | Johnson et al., 2008 |
| Spiritual beliefs | Wicher and Meeker, 2012 |
| Knowledge about advance directives | Wicher and Meeker, 2012 |
| Historical mistrust of the health care system | Kagawa-Singer and Blackhall, 2001; Wicher and Meeker, 2012 |
| Cultural beliefs about family involvement | Blank, 2011; Kagawa-Singer and Blackhall, 2001; Ko and Berkman, 2010; Yennurajalingam et al., 2013a,b |
| Desire to avoid emotional distress for self or family by discussing death, fear, denial | West and Hollis, 2012 |
| “Don’t want to think about dying” or family already aware of care preferences | Carr, 2012a |
| Disagreement between patient and family preferences for treatment | Muni et al., 2011; Phipps et al., 2003 |
| Patients and physicians each waiting for the other to initiate the discussion | Phipps et al., 2003 |
| Extent to which family engages in estate planning | Carr, 2011, 2012b |
| Literacy level | Waite et al., 2013 |
| Socioeconomic status* | Carr, 2012b |
*Although racial/ethnic differences in ICU care were found after controlling for socioeconomic status, once a patient is in the ICU, socioeconomic status may not make a difference (Muni et al., 2011).
sonal circumstances are necessary for [understanding] his or her [advance care planning].”
A relative lack of advance care planning is seen among black, Hispanic, and Asian patients across socioeconomic groups. It is seen as well across care settings, including hospitals and nursing homes and even in intensive care, where patients are least likely to be able to make their own decisions and the need for such planning is greatest (Frahm et al., 2012; Muni et al., 2011; Reynolds et al., 2008). “Advance directives, which are generally accepted in western civilization, hold little or no relevance within the [black and minority ethnic] population” (Cox et al., 2006, p. 20), including Asian
cultures, in which family decision making predominates (Blank, 2011), and American Indian cultures, which hold different views from those typical of the white, non-Hispanic population regarding autonomy and informed consent (Colclough and Brown, 2013).
Asians
Whereas one U.S. study of patients with head and neck cancers found that more than 81 percent did not want anyone else present at the time of diagnosis (Kim and Alvi, 1999), patients from family-centered cultures such as the Japanese are more likely to want a relative present for such difficult conversations (Fujimori and Uchitomi, 2009). A review of the literature indicates that Asian patients in general may be less likely than patients of other cultural backgrounds to want an estimate of life expectancy and more likely to have family present when receiving bad news (Fujimori and Uchitomi, 2009). In a separate study of more than 500 Japanese cancer patients, Fujimori and colleagues (2007) found that married patients, those with less helplessness/hopelessness, and those with more formal education preferred to discuss life expectancy. Still, the majority of these patients preferred to have their physician explain the status of their illness, break bad news honestly and in a way that is easy to understand, and explain the treatment plan.
African Americans
As noted, African Americans are less likely than white non-Hispanics to express any treatment wishes or to have written advance care planning documents. Compared with whites, they also are more likely to report inadequate or problematic communication with physicians (Trice and Prigerson, 2009), to have greater concerns about staying informed about the illness, and to give the care their family member received a lower rating (Welch et al., 2005). In response, some efforts have been made to carefully tailor the messages regarding advance care planning to African American (as well as other cultural) communities. One example is the comprehensive approach of Gloria Anderson called “What Y’all Gon’ Do With Me?: The African-American Spiritual and Ethical Guide to End of Life Care” (Anderson, 2006).
A study involving New York State nursing homes found lower rates of hospice use and higher rates of in-hospital deaths among blacks than whites: 40 percent of black patients and 24 percent of white patients died in hospitals, a differential accounted for largely by a higher use of feeding tubes and a lower use of do-not-resuscitate and do-not-hospitalize orders among black patients (Zheng et al., 2011). Overall, according to the au-
thors (p. 996), “Other conditions being equal, residents from facilities with higher concentrations of blacks have higher risk of in-hospital death and lower probability of using hospice.” Further examination is needed of why differentials in use occur by diagnosis and type of nursing home, and especially how these differentials may affect quality of care and outcomes.
Some evidence suggests that the gap between African American and white patients in the use of hospice has been shrinking. Between 1992 and 2000, the hospice use rate for whites doubled and for African Americans increased almost four-fold (Han et al., 2006). Differences by race and ethnicity still are seen, however (see Table 3-4). Blacks are underrepresented in the proportion of deaths that occur in hospice, which has been attributed, at least in part, to the Medicare Hospice Benefit’s requirement that enrollees give up curative efforts (Wicher and Meeker, 2012).
The well-documented historical abuse of African Americans in medical research, dating back more than 150 years, continues to ripple throughout the health care enterprise in many parts of the United States. The author of the award-winning book Medical Apartheid says people tried to discourage her from writing the book, claiming that “any acknowledgment of abuse will drive African Americans from sorely needed medical care. However, a steady course of lies and exploitation has already done this” (Washington, 2006, pp. 386-387). This history and profound lack of trust may be one
TABLE 3-4 Race and Ethnicity of U.S. Decedents, and Hospice Patients, 2011
| White, non-Hispanic (%) | African American, non-Hispanic (%) | Hispanic (%) | Multiracial (%) | Asian, Hawaiian, Other Pacific Islander (%) | |
| Race and ethnicity of U.S. decedents aged 35 and over (2011, preliminary)a | 80.9 | 10.9 | 5.5 | N/A | 2.1 |
| Race and ethnicity of U.S. hospice patients (2011) | 82.8 | 8.5 | 6.2b | 6.1 | 2.4 |
aFully 99 percent of hospice patients were aged 35 and older in 2011.
bThe National Hospice and Palliative Care Organization (NHPCO) reports Hispanic ethnicity separately from race.
SOURCES: Hoyert and Xu, 2012; NHPCO, 2013.
reason why African Americans may prefer intensive life-sustaining treatment near the end of life and believe that advance care planning and hospice may deny them wanted services (Johnson et al., 2008, 2011; Lepore et al., 2011; West and Hollis, 2012).
Some believe that poor physician communication skills contribute to this lack of trust (Gordon et al., 2006). In a study of physician-patient relationships, however, the issue on which African American and white respondents were in closest agreement was whether they had complete trust in their physician; African American respondents rated all other measures of relationship quality significantly lower compared with white respondents (Smith et al., 2007).
Hispanics/Latinos
Compared with other minority populations, less research has been done among Hispanics/Latinos on end-of-life preferences and decision making. The available studies suggest, however, that they follow the general pattern seen among cultural and ethnic minority populations as previously described (Carr, 2012a). Extent of knowledge about and attitudes toward advance directives are strong predictors of whether such directives are completed among both Hispanics and whites, and disparities in rates of completion may be due to differences in these factors (Ko and Lee, 2013). Greater acculturation was found to increase the likelihood of having an advance directive among older Latinos (Kelley et al., 2010).
Interviews with 147 Latinos aged 60 and older from Los Angeles–area senior centers found that most (84 percent) would prefer care focused on relieving pain and discomfort if they became seriously ill, yet nearly half (47 percent) had never discussed these preferences with either their family or their physicians (Kelley et al., 2010). Interviewees expressed a strong preference for family involvement in decision making about end-of-life care, whether or not they were incapacitated. In another study, 71 percent of hospitalized Latinos had not had a discussion about advance directives with clinical personnel (Fischer et al., 2012). Latinos who had had such a discussion were just as likely as any other population group members to have an advance directive on file, suggesting that the primary barrier to overcome is the low rate of such discussions.
System Factors in Decision Making
Mack and colleagues (2010a, p. 1537) conclude that “wider issues within the health care system . . . could explain the major disparity we identified. . . . White patients may have greater continuity of providers and sites of care, with the confirmation of [do-not-resuscitate] orders and docu-
mentation of preferences, for example, at every encounter. Alternatively, racial bias on the part of health care providers about patient preferences could have a role.”
Several potential system barriers to advance care planning and completion of advance directives have been identified. For example, doctors’ belief that African American patients “are more likely to prefer intensive, life-sustaining treatment” (Barnato et al., 2011, p. 1663) may lead to an overestimation of an African American individual’s preference for such treatment. This may be one reason black patients tend to receive life-extending measures even when they have stated a preference for symptom-directed care (Mack et al., 2010a) and why the hospital care they receive is more likely to involve intensive services (Barnato et al., 2006, 2007).
Some patients may simply need more information about advance directives, the advance care planning process, and hospice and palliative care options (Johnson et al., 2008; Wicher and Meeker, 2012; Zaide et al., 2013). As a practical matter, health care providers need to be sure that the relevant discussions with all patients, regardless of race, ethnicity, language, and health literacy level, are unhurried, culturally appropriate, free of confusing medical terms and concepts, and adequately understood by the patient and family. Physicians can be part of that discussion, but may not in all cases be the most appropriate person to lead a lengthy conversation; bicultural and bilingual patient navigators or other trained laypersons may be helpful in talking to patients and their families about advance care planning. Materials in languages other than English and designed for low-literacy populations may also improve knowledge, understanding, and rates of advance care planning (Fischer et al., 2012).
Differences Across Literacy Levels
Levels of both general literacy and health literacy—defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (Ratzan and Parker, 2000, p. vi)—affect engagement in advance care planning and the preparation of advance directives.
General Literacy
Most advance directives (which often contain complex legal constructions and descriptions of medical technologies and procedures) require at least a 12th-grade reading level (Castillo et al., 2011). The 2003 National Assessment of Adult Literacy found that 14 percent of the total U.S. population aged 16 and older have below-basic prose literacy, and adults 65 and older account for more than one-quarter of these individuals (Baer et al.,
2009). And while adults with income below 125 percent of the poverty level accounted for 24 percent of the adult population in 2003, they represented 56 percent of those with below-basic prose literacy.
Predictions are that the general English literacy of the U.S. population will decline as a result of several factors, including continued low high school graduation rates; continued low reading and math performance among U.S. schoolchildren, particularly blacks and Hispanics; and the increasing number of immigrants (Kirsch et al., 2007; Parker et al., 2008). In 2011, almost 61 million U.S. residents aged 5 and older spoke a language other than English at home, and 7 percent of those residents—4.3 million people—spoke English “not at all.” For 38 million Americans, the language spoken at home is Spanish, and for 23 million more, it is something else—with Chinese, French, German, Korean, Tagalog, and Vietnamese each being spoken by more than 1 million people (Ryan, 2013).
Health Literacy
According to an IOM (2004) report, approximately 90 million people have low health literacy. As a result, they would be likely to have significant difficulty navigating the health care system and/or completing a range of tasks key to self-managing complex chronic conditions successfully. In general, people with low health literacy experience more hospitalizations, use more emergency care, and are less able to interpret medication labels and health messages appropriately than those with higher health literacy (Berkman et al., 2011). Low-literacy seniors have poorer health status than their more health-literate counterparts. Such difficulties are likely to escalate near the end of life.
Health literacy “is not simply the ability to read. It requires a complex group of reading, listening, analytical, and decision-making skills, and the ability to apply these skills to health situations” (NNLM, 2013). Frequently measured and highly correlated health literacy components are “the ability to interpret documents, read and write prose (print literacy), use quantitative information (numeracy), and speak and listen effectively (oral literacy)” (Berkman et al., 2011, p. ES-1), with oral literacy being less frequently assessed. Numeracy skills are especially important in understanding prognoses, risks of treatment, and the expression of clinical uncertainty.
The 2003 National Assessment of Adult Literacy assessed the health literacy of U.S. adults using multiple measures. The test content encompassed clinical and prevention topics, as well as navigation of the health care system (Kutner et al., 2006). Key results (all statistically significant at the 0.05 level) mirror those for general literacy:
- The health literacy of 36 percent of U.S. adults was basic or below and was “proficient” for only 12 percent.
- White (non-Hispanic) and Asian/Pacific Islander adults had higher average health literacy than other groups.
- Those aged 65 and older had lower average health literacy than younger adults, and 29 percent of adults aged 65 and older had below-basic health literacy.
Low health literacy affects certain population subgroups disproportionately: people of lower socioeconomic status, racial and ethnic minorities, people with disabilities, those with psychiatric and other cognitive disorders, and the elderly. Nevertheless, “people of all ages, races, incomes, and education levels—not just people with limited reading skills or people for whom English is a second language—are affected by limited health literacy” (ODPHP, 2010, p. 4).
Multiple studies have shown that health literacy affects health care utilization, outcomes, and costs (Berkman et al., 2011). Individuals with low health literacy whose difficulties are compounded by the emotional stress and debilitation of an advanced disease may have difficulty reading, comprehending, and/or signing insurance forms or complicated advance directive documents. In one study of almost 800 patients aged 55 to 74, almost one-half of those with adequate literacy, just more than one-quarter of those with marginal literacy, and only one-eighth of those with low literacy reported having an advance directive (Waite et al., 2013). Uncertainties about care preferences among less health-literate groups suggest a need for culturally sensitive decision-making tools that take literacy into account (Sudore et al., 2010).
ELEMENTS OF GOOD COMMUNICATION IN ADVANCE CARE PLANNING
Elements of good communication in advance care planning include open, clear, and respectful communication between clinician and patient; good communication with families and health care agents; and shared decision making and patient-centered care.
Clinician-Patient Communication
Open, clear, and respectful communication between health care professional and patient is a precondition for effective advance care planning. It also is critical to developing a therapeutic relationship and negotiating and carrying out a treatment plan. Moreover, it is professionally rewarding and
personally satisfying for clinicians, and reduces anxiety and uncertainty for patients (Dias et al., 2003).
A National Cancer Institute (NCI) monograph on improving patient-centered communication is organized around six major goals:
- fostering healing relationships,
- exchanging information,
- responding to emotions,
- managing uncertainty,
- making decisions, and
- enabling patient self-management (Epstein and Street, 2007).
Several of these goals are major topics in this report and in this chapter in particular. Authors of the NCI monograph point out the interrelationships among these goals and the variability in information about each of them.
After-death interviews with 205 families of adult decedents included several questions related to advance care planning. Although total “quality of dying and death scores” were not influenced by whether the patient had an advance directive, “higher scores were associated with communication about treatment preferences, compliance with treatment preferences, and family satisfaction regarding communication with the health care team” (Curtis et al., 2002, p. 17). Specific components of communication associated with a better-quality dying experience included how well the health care team listened to the family25 and explained the patient’s condition “in language they can understand and in terms that are meaningful in their lives” (Curtis et al., 2002, p. 27).
While in-the-moment decision making may provide the most accurate reflection of patients’ wishes at the time a decision is needed, this approach entails numerous barriers. For example, considering all the implications of a decision—medical, psychological, logistical, financial, caregiving—may be nearly impossible for patients and health care agents under such circumstances; many of them may not want to think about these issues and the current trajectory of a serious advanced illness, and clinicians may not have the time to discuss them. Nevertheless, clinicians—especially those who do not have a lengthy previous relationship with the patient—need this input.
According to Sudore and Fried (2010, p. 257), what matters most to patients “is the potential outcomes of treatment.” Asking patients about the outcomes they most hope for or fear is a way to identify values and prefer
_______________
25Previous research indicated that when physicians talked to patients about advance directives, they spent two-thirds of the time talking; discussed attitudes toward uncertainty only 55 percent of the time; and asked about patients’ values, goals, and reasons for treatment preferences 34 percent of the time (Tulsky et al., 1998).
ences in a way that may be more actionable than asking whether they want or do not want specific interventions. And because opinions change over time, discussions of this type need to be repeated. Good questions include “What information would you like to know?,” “Who else should be given the information and be involved in decision making?,” and “How should that information be presented?” (Russell and Ward, 2011). A review of the international literature26 suggests that cancer patients’ information preferences are affected by four factors: setting, manner of communicating bad news, what and how much information is provided, and emotional support (Fujimori and Uchitomi, 2009).
Despite the importance of good clinician-patient communication, many impediments to such communication exist. Some are inherent in the previously discussed issues concerning specific populations. Others relate to physicians themselves, including a lack of training, insufficient time, competing needs, and personal discomfort in discussing terminal prognoses and death. Walling and colleagues (2008) identify the following reasons for a lack of the effective clinician-patient communication needed for advance care planning:
- reluctance to give patients bad news, with doctors’ physiological responses to breaking bad news showing that it is stressful for them to do so;
- physicians’ avoidance of discussions of negative prognoses because of some combination of uncertainty and not wanting to engender hopelessness;
- lack of evidence about the best timing for discussions of future treatment options and the above-noted changing concerns of patients over the course of illness that may warrant repeat discussions;
- reluctance on the part of patients to discuss these matters; and
- time constraints and distractions (pagers, for example).
“There is too little time during our appointments to discuss everything we should” was the most common barrier to advance care planning mentioned by almost two-thirds of 56 physicians responding to one survey, with wanting to maintain patients’ hope being the next most frequently cited (by 23 percent) (Knauft et al., 2005).
Lack of time to identify patients’ preferences can contribute to misunderstandings if doctors rely instead on their own instincts and experience. Two studies found that even specially trained palliative care physicians who
_______________
26This systematic review of English-language research papers was conducted by investigators in Japan, but they note that most of the research they found reported on experiences in Western countries.
had had lengthy initial consultations with their patients most commonly assessed the patients’ medical decision-making preferences (how actively they wanted to participate in making treatment decisions) incorrectly (Bruera et al., 2001, 2002).
The following sections look at four topics that exemplify the challenges of end-of-life communications: discussing prognosis, handling emotional encounters, nurturing patients’ hope, and addressing spirituality and religion.
Discussing Prognosis
Shortcomings in existing prognostic tools and methods contribute to a lack of clarity about disease prognosis that weighs on physicians and clouds communication (Smith et al., 2013b; see also Chapter 2). Population-based estimates of the course of disease do not exclude the possibility that an individual patient will be an exception at the short or long tail of longevity. Not only is estimating prognosis difficult, but so, too, as noted above, is the process of communicating it to patients and families (Lamont and Christakis, 2003). Numerous studies have shown that to compensate, physicians tend to provide prognosis estimates infrequently or to give overly optimistic estimates of survival. The more long-standing the physician-patient relationship, the more likely it is that the physician will make an inaccurate, overpessimistic prediction of prognosis (Christakis and Lamont, 2000). It is not surprising, then, that interviews with terminally ill patients and their caregivers reveal considerable uncertainty about life expectancy among both groups, even within a few weeks of death (Fried et al., 2006).
A study involving palliative care specialists found that almost all of their consultations (93 percent) included some prognostic information and more pessimistic than optimistic cues, gave greater emphasis to quality of life than to length of survival, focused on the situation of the particular patient rather than population-based estimates as the patient neared death, and tended to provide more pessimistic views when talking to family members without the patient present (perhaps because the patient was too ill to participate) (Gramling et al., 2013).
Often family members and health care agents do not understand, have not been made aware of, or cannot accept their loved one’s serious prognosis (see also the discussion of good communication with families and health care agents below). Both patients and family members frequently “don’t hear” negative messages about prognosis (Fried et al., 2003) and tend to interpret even negative information optimistically—not because physicians are unclear or families do not understand numerical risk information, but because of psychological factors and belief in the power of positive thinking (Wachterman et al., 2013; Zier et al., 2012). On the other hand, even
a single pessimistic statement from an oncologist can reduce patients’ unchecked optimism (Robinson et al., 2008).
Bringing physician and patient views into greater alignment is necessary to give patients the best opportunity to make realistic and informed choices about their care. One strategy is to make clear that the plan of treatment may go well, but that it may not effect a cure of the underlying disease. Oncologists make such statements in less than half of patient visits (46 percent) (Robinson et al., 2008), and even so, patients often do not understand them (Weeks et al., 2012).
Handling Emotional Encounters
Patients living with advanced serious illnesses experience significant distress, and their need to make difficult decisions about treatment contributes to this suffering. These treatment decisions can be fraught with uncertainty and are often clouded by a fear of death. Such distress is known to be highly prevalent among cancer patients in particular, with up to 60 percent of selected populations acknowledging emotional difficulties (Carlson et al., 2010, 2012; Gao et al., 2010; Zabora et al., 2001). Many factors contribute to this distress, including managing physical symptoms, adjusting to changes in social or occupational roles, and navigating the emotional ups and downs of cancer remission and progression (Anderson et al., 2008). In addition, most patients face multiple decisions about treatment throughout the course of their illness. These decisions vary from discrete choices about surgery to more general decisions about philosophies of treatment and balances between risk and reward.
Much of the research on clinician management of emotional encounters comes from studies of cancer patients, and it has found that clinicians do not consistently handle patients’ and families’ expressions of emotions well (Loewenstein, 2005; Pollak et al., 2007). In fact, research suggests that empathetic responses by physicians to patients’ expressed emotions are relatively rare, despite physicians’ high confidence in being able to address patients’ concerns and the frequency with which such concerns are expressed. Analysis of audiotapes from almost 400 conversations between oncologists and 270 patients with advanced cancer27 revealed that opportunities for the oncologists to show empathy arose in patients’ remarks some 292 times in 398 conversations (Pollak et al., 2007). Some 68 percent of these remarks were direct (e.g., “I have been really depressed lately”), and one-third were indirect (e.g., “Oh, no. What do we do now?”).
Emotions can arise in patients in response to several broad categories of issues: symptoms, diagnosis, and treatment; social issues; the health care
_______________
27Most of these 270 patients had at least a 6-month relationship with their oncologist.
system, and death and dying (Anderson et al., 2008). Common words used to express such emotion are “concern,” “scared,” “worried,” “depressed,” and “nervous,” which would appear to be patently emotion laden. Yet “when clinicians repeatedly miss patients’ expressions of emotion, patients eventually cease to express emotion,” and an important opportunity to relieve patient distress is foregone (Anderson et al., 2008, p. 808).
In these situations, clinicians can respond with statements or questions that are “continuers” (those that name the patient’s emotion, express understanding, show respect or support, or seek to explore the emotion further) or with “terminators” (statements that seek to cut off the discussion). Pollak and colleagues (2007) found that oncologists responded with terminators 73 percent of the time. Patients learn not to raise these issues when met with such responses (see also Butow et al., 2002).
Gender is a predictor of the use of more empathetic language, with women using more such language. In addition, the extent to which oncologists self-identified as more socioemotional than technical-scientific in their orientation also predicted the use of empathetic language (Pollak et al., 2007). In this connection, a survey of oncologists (48), oncology physician assistants (26), and oncology nurses (22) found that most of the physicians (70 percent) described themselves as “technological and scientific,” while substantial majorities of the nurses (82 percent) and physician assistants (68 percent) described themselves as “social and emotional” (Morgan et al., 2010). Because the nurses and physician assistants also reported more comfort with psychosocial talk, the authors of this study suggest that the differences across professions in responding to patient emotion “could have important implications for the design of future oncology care teams” (p. 16), as well as for health professions education.
Dealing with patients’ emotions is one of the more challenging tasks of the already difficult job of caring for people likely to die. Care and support for the clinicians who do this work may reduce clinician stress and burnout and make an important contribution to improving the care they provide (Mack and Smith, 2012).
Nurturing Patients’ Hope
As suggested above, a primary reason physicians are not more candid about discussing prognosis is that they believe “discussing end-of-life care will take away the patient’s hope,” which might affect treatment outcomes (Ganti et al., 2007, p. 5647). However, research suggests that honest conversations do not rob patients and families of hope or lead to depression, and that being truthful does not hasten death (Shockney and Back, 2013). By adopting a communication approach that simultaneously emphasizes “hoping for the best and preparing for the worst,” doctors allow for im-
portant opportunities to learn from patients and families what they need, what they fear, and what is possible (Back et al., 2003, p. 439).
Ways to encourage hope in a context of greater candor do exist. Certainly, clinicians can emphasize what can be done (managing pain and symptoms, providing emotional support and care, maintaining dignity, and providing practical assistance); explore realistic goals of care; and discuss the priorities for day-to-day living (Clayton et al., 2005). The importance of the latter topic is suggested by research showing that patients and caregivers are sometimes reluctant to discuss the future because they are so focused on the here and now (Knauft et al., 2005).
Addressing Spirituality and Religion
Attention to patients’ spiritual needs can improve the quality of communication among clinicians, patients, and families and reduce the gap between the health care patients want and expect and what they receive (Edwards et al., 2010). Findings from numerous studies indicate that some patients feel that a lack of spiritual support is an important communication gap (e.g., Curtis et al., 2004; Peteet and Balboni, 2013). Many clinicians, too, believe that spiritual support is an important aspect of care (Puchalski and Ferrell, 2010). These findings parallel the goals of palliative care, with its attention to body, mind, and spirit, and of patient-centeredness, which encompasses “compassion, empathy, and responsiveness to the needs, values, and expressed preferences of the individual patient” (IOM, 2001, p. 48). As physician and ethicist Daniel Sulmasy (2009, p. 1635) puts it:
if physicians and other healthcare professionals have sworn to treat patients to the best of their ability and judgment, and the best care treats patients as whole persons, then to treat patients in a way that ignores the fundamental meaning that the patient sees in suffering, healing, life, and death is to treat patients superficially and to fall short of the best ability and judgment.
A final general consideration is that, although spirituality and religion may be powerful forces for relief of suffering for certain individuals, this does not mean physicians should encourage patients toward religious practices “as something ‘medically indicated’ for health” (Sulmasy, 2009, p. 1636). The healing benefits of spiritual practice may not be achievable through external exhortation in any case, and may be possible only when they form part of a person’s intrinsic belief system.
Good Communication with Families and Health Care Agents
Family involvement is an essential feature of advance care planning, and the family’s understanding of the illness and its treatment and likely course can help reinforce—or undermine—the work of the care team. In unexpected situations, when a sudden devastating illness or injury occurs, the same need for careful communication and family involvement occurs. These situations are made more difficult by the likelihood that no prior relationships exist among patient, family, and clinicians and when the patient’s condition requires redirecting efforts from resuscitative treatment to palliative care (Limehouse et al., 2012a,b). When there is conflict within the family, moreover, a health care agent is less likely to make decisions in agreement with the patient’s wishes (Parks et al., 2011).
Much experience with communication in family meetings has been gained in the long-term care setting. There, individuals may experience significant mental as well as physical declines during their residence, and family meetings are an important component of care. Family meetings have been found to be most successful when they occur at times other than crises and are used to share information, manage emotions, establish goals, and support decision making (Ceronsky and Weissman, 2011). Well-established guidelines exist for conducting such meetings effectively, and opportunities for improving family meetings through cross-learning across care settings may be useful (Hudson et al., 2008; McCusker et al., 2013). In the intensive care setting, conferences in which family members are given opportunities to speak and share their concerns reduce conflict with the doctor over care decisions and family dissatisfaction with the process of making those decisions (McDonagh et al., 2004).28
Physicians have avoided such conversations for various reasons—perhaps an unwillingness to reveal the limits of medical knowledge; a desire to avoid causing patients and families undue distress; or, as discussed above, concern about causing a loss of hope. Avoiding these conversations may be misguided, however, because it denies families and health care agents the opportunity to prepare emotionally and logistically for their loved one’s death (Apatira et al., 2008; Evans et al., 2009, p. 52).
Families’ and health care agents’ perceptions of prognosis may be affected by patients’ physical appearance, how they have handled previous illnesses, their strengths, and their will to live, as well as by the family members’ and agents’ own optimism, intuition, and faith. Thus, families attempt to meld and balance these factors with the information provided by the clinician. For example, as Boyd and colleagues (2010, p. 1274) note,
______________
28In this study, audiotapes of 51 family conferences, involving 214 family members and led by 36 different physicians, were made and analyzed. On average, clinicians spoke more than 70 percent of the time.
“discussing prognosis in terms of outcomes of populations of ‘similar’ patients may fall short if physicians do not also recognize and appreciate that surrogates also view unique attributes of the patient as relevant.”
Interviews with 179 health care agents for ICU patients at an academic medical center revealed that most (87 percent) wanted physicians to discuss an uncertain prognosis, and only 12 percent preferred to avoid such a discussion in case the prognosis was incorrect (Evans et al., 2009). Health care agents wanted to discuss prognosis despite uncertainty because they believed uncertainty is unavoidable. They also felt that discussing uncertainty leaves room for realistic rather than false hope (some noting that they looked for hope elsewhere) and that physicians were the best and only source for this information. Sharing information during such discussions increases trust in the physician. In addition, having this information allows health care agents to better support the patient and other family members, gives them time to prepare to make difficult life support decisions, and allows time to say good-bye and prepare for possible bereavement (Apatira et al., 2008; Evans et al., 2009). Rather than avoiding discussion of the likelihood of death, some health care agents want physicians to practice “complete honesty,” although there is a range of receptivity to this information (Evans et al., 2009).
My father had progressive bladder cancer and also was an Alzheimer’s patient who lived at home with our mother. As our father’s disease progressed, both his physical and mental health deteriorated. Our mother also passed away quite unexpectedly, so his care was completely transferred to my sister and me. We became frustrated by the lack of communication between the doctor’s office and us. It did not appear the treatments our father was receiving were working, and he had difficulty understanding why he had to go to the doctor’s for a treatment that caused immediate pain and then prolonged discomfort. Phone calls, faxes, and e-mails were not answered. We found the only way we could obtain information or answers to questions was to physically enter the doctor’s office and request a face-to-face meeting. Since I lived 5 hours away, it was necessary to schedule the meetings during my half of the week at our father’s home. The doctor even scheduled a surgery for our father near the end of his life.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
Conversations involving withdrawal of life support are inevitably difficult for all parties. Health care agents themselves are divided as to whether they want the physician to make a recommendation in such situations. In one study of 169 agents, 56 percent preferred to receive the physician’s recommendation, while 42 preferred not to (2 percent had no preference) (White et al., 2009). This differential was not related to health care agents’ demographic characteristics. These findings suggested to the authors that physicians should not routinely provide recommendations about withdrawing life support and instead be flexible in their approach to advising surrogates in such situations, taking into consideration whether such advice is appropriate, desired by the surrogate, and necessary “to ensure that decisions reflect the patient’s values and preferences” (White et al., 2009, p. 324).
Shared Decision Making and Patient-Centered Care
Increasingly, informing and involving patients regarding the decisions about their care is recognized as a standard for good care (Fowler et al., 2013). This evolution in thinking has occurred in recent decades with respect to patient-clinician communication around care decisions broadly and is particularly relevant in the context of advance care planning. “Shared decision making emerged as a compromise in the longstanding debate about the relative role of patient autonomy and provider beneficence in medical decision-making” (Stark and Fins, 2013, p. 13).
In May 2013, an editorial in the British Medical Journal called for an equal-footing partnership between patients and doctors. The editorial also acknowledged that “achieving such a partnership is a challenge. Years of paternalism have left doctors and patients unprepared for a different type of interaction” (Godlee, 2013, p. 1).29
Shared decision making is neither clearly nor consistently defined in the research literature, and more robust research methods are needed to gauge its effects more precisely (Lipkin, 2013). Nonetheless, it clearly shares characteristics and a development path with the notion of patient-centered care. Indeed, shared decision making is one aspect of patient-centeredness, an essential component of quality care. Shared decision making encompasses
- eliciting and understanding the patient’s perspective;
- understanding the patient’s psychosocial and emotional context;
_______________
29A number of articles on the topic of shared decision making from the British Medical Journal have been collected at http://www.bmj.com/specialties/shared-decision-making (accessed December 16, 2014).
- developing a shared understanding of the clinical problem and its appropriate treatment, given the patient’s goals, preferences, and values; and
- empowering patients, which is achieved through active involvement of patients in decision making (LeBlanc and Tulsky, in press).
For patients with advanced serious illnesses, shared decision making is intended to create a context in which future decisions can be made that remain true to patients’ preferences. This approach eschews the idea of specific, checkbox-style advance directives, and emphasizes participation by patients and, importantly, their families, as well as their health care agents (who may be family members), whose thoughtful selection is strongly endorsed by current practice. According to Gillick (2013, p. 575), “For frail elders and patients with advanced illness, many of whom have multiple chronic diseases, patient-centered care is impossible without caregiver involvement . . . [and] . . . the critical role of caregivers deserves considerably more attention from clinicians.”
A narrative synthesis of some 37 articles on shared decision making in palliative care identifies several important themes (Bélanger et al., 2010). Although patients prefer shared decision making (preferred by 40-73 percent of patients surveyed in five studies) and it is important to them, they often are not afforded the chance to participate. In addition, the effects of participation on patient outcomes (anxiety and depression, patient satisfaction, and life expectancy) are not yet clear, and both barriers to and facilitators of shared decision making have been identified. Barriers include patients’ and families’ unrealistic expectations of treatment; the way options are framed for patients; delaying decisions to follow predetermined patterns of care; and providing information too gradually so that when a decision is needed all the information is not in hand. Facilitators include clinicians providing sufficient, realistic information; presenting choices; and using tools to aid patients in decision making.
How Patients Make Decisions
Advance care planning is founded on the expectation that people, once presented with evidence and facts, will make rational choices based on well-established views and preferences (Swindell et al., 2011). The growing field of behavioral economics is challenging both the notion of “rational choice” and the presence of “well-established views.” Clinicians assisting patients benefit from understanding of biases and “rules of thumb” by which patients make decisions (Swindell et al., 2010). Examples of these decisionmaking methods as they might emerge in end-of-life situations include
- being unduly influenced by a memorable event (such as news reports of the extremely rare cases in which someone in a coma for many years “miraculously” returns to consciousness);
- believing that some exceptional factor will prevent a patient’s disease from following its usual course;
- being influenced by unrelated past occurrences (such as a relative’s successful recovery from a serious disease or difficult, painful death); and
- preferring inaction to avoid harm (such as declining opioid drugs early in the illness so that “they will work when I need them”), even though this inaction may cause greater harm than action.
Such biases and heuristics can unintentionally thwart what patients themselves see as their best interest and goals (Swindell et al., 2010). Clinicians who understand the ways in which patients’ decision making is not always rational can help patients reflect on their biases and to see whether doing so changes their expressed preferences (Halpern, 2012a; Swindell et al., 2011).
Insights into the psychology of human decision making can be used “to develop, test, and implement scalable interventions that improve the quality of the health decisions made by patients, family members, and providers” (Halpern, 2012b, p. 2789). “Choice architecture” takes into account the ways “choices are presented and the environment in which decisions are made,” adjusting them so that better decisions result (Halpern, 2012b, p. 2789).
Gaps between people’s intentions and their behavior are a prominent theme in the end-of-life field. A prime example is the gap between people believing in the importance of advance directives and discussions about end-of-life wishes and their taking action in accordance with that belief (CHCF, 2012; The Conversation Project, 2013). Certainly patients have been shown to vary a great deal in the extent to which they want to be involved in decisions about their end-of-life care, and it may be possible to encourage and support good decision making without relying on unrealistic expectations about patient engagement.
Choice architecture employs a number of key strategies designed to improve the decision environment, including use of defaults and precommitment (Nease et al., 2013). The precommitment approach takes into account that most people place a higher value on present or imminent events than on events that will occur in the future. Advance care planning is an example of an action that has fairly steep immediate costs (contemplation of one’s mortality and the possibility of being unable to make decisions) and benefits that may appear only theoretical. The younger and healthier the person is, the more theoretical those benefits may seem. Default or “opt-
out” choices assign patients a provisional decision; if they want to make a different decision, they can, but must actively do so.30 All default options in the health care system (for example, aggressive care unless stated otherwise) carry biases. Choice architecture seeks to make these biases explicit and, in some cases, encourage changing the default to one that is generally preferred by patients and clinicians. By doing so, biases that currently drive decisions may be undone, and patient choice may be enhanced. According to Halpern and colleagues (2013, p. 412), “A hallmark of defaults is that they lead gently, without restricting any options.” A randomized study of patients with incurable lung cancer found that when the patients were presented with an advance directive in which the default was palliative care, they were significantly more likely to elect that option than were patients given a standard advance directive or one that defaulted to life-extending treatment (Halpern, 2012b; Halpern et al., 2013). In studies in which a hypothetical advance directive used forgoing life-sustaining interventions as the default, many more study participants indicated that this was their preference than was the case if they had to actively choose that option (Kressel and Chapman, 2007; Kressel et al., 2007).
The important implication of the research by Kressel and colleagues is that “people might not have well-formulated, strongly held views on what forms of care at the end of life will best promote their values” (Halpern et al., 2013, p. 409). Rather than reflecting deeply ingrained preferences, their responses to advance directive document choices may be constructed at the time they are asked to provide them, similar to what has been observed with respect to other health care choices (Halpern et al., 2007). This hypothesis was tested with 132 patients having incurable lung disease and no prior directive (Halpern et al., 2013). Patients were randomly assigned to be presented with one of three advance directives that differed only in their embedded default options. While most of the patients chose what the authors called comfort-oriented care, the proportion making that choice was much higher in the group receiving the “comfort default” directive. When, subsequently, the study design was explained to patients along with the data showing how defaults had affected the choices of the patient groups, only 2.1 percent of participants reconsidered their selections, and no patients revised their original choices. This result suggests that changes to the way advance directives are structured that make it simple for patients to choose the kind of care most patients prefer (always with the option to
_______________
30An early successful application of “opt-out” decision making was designed to encourage people to participate in an employer-subsidized 401(k) savings plan. Automatically enrolling employees unless they actively opted out “materially increase[d] participation while maintaining a high level of employee satisfaction” (Nease et al., 2013, p. 245).
choose otherwise) might “provide a novel way to improve end-of-life care for large populations of seriously ill patients” (Halpern et al., 2013, p. 414).
Decision Aids
Decision aids have been developed to guide discussion, support patients, and make discussion of difficult issues easier.31 Recognizing that patients nearing the end of life are likely to be in a state of decline, the designers of these aids generally attempt to make their completion as low burden as possible. Many of these tools have been tested and used in the palliative care setting or with cancer patients, and many of them apply to a single decision, such as whether to place a feeding tube in a cognitively impaired patient.
Even an apparently simple open-ended question such as “What is your understanding of your illness?”—certainly fundamental to a discussion of choices—can have significant clinical utility. A study of patient responses to this question found substantial differences among patient groups: 77 percent of patients with cancer could name or describe their condition, sometimes using precise biomedical terms; 39 percent of patients with congestive heart failure and 41 percent with chronic obstructive pulmonary disease could do so; and some patients (particularly those with limited education) had little knowledge or understanding of their illness (Morris et al., 2012). Patients’ responses to this question may, therefore, signal the opportunity for clinicians to provide more information about the illness, discuss how it may affect the patients’ lives, and describe its likely course, as well as reveal whether patients have unmet emotional needs.
Decision aids are of three general types: those used in face-to-face encounters; those designed for use outside clinical encounters (take-home materials, for example); and those that use some intervening medium, such as telephone or video (Elwyn et al., 2010). Results of randomized trials of video decision aids, reported in Table 3-5, show that across the board, participants were comfortable with the decision aids and found them useful. According to the authors of one of these studies, “Physicians often underestimate the emotional resilience of patients and their desire to be involved in this decision-making process” (El-Jawahri et al., 2010, p. 309).
A research team at the forefront of developing and evaluating decision aids defines them as follows:
Decision support interventions help people think about choices they face: they describe where and why choice exists; they provide information about
_______________
31For example, the question “Are you at peace?” may be a sufficient screening question to identify patients for whom fuller spiritual assessment or specialized services are needed (Steinhauser et al., 2006).
options, including, where reasonable, the option of taking no action. These interventions help people to deliberate, independently or in collaboration with others, about options, by considering relevant attributes; they support people to forecast how they might feel about short, intermediate and long-term outcomes which have relevant consequences, in ways which help the process of constructing preferences and eventual decision making, appropriate to their individual situation. (Elwyn et al., 2010, p. 705)
Video is not the only effective medium for decision aids. In another recent study involving 120 patients with metastatic cancer who were no longer receiving curative therapy (55 intervention patients, 65 control
TABLE 3-5 Effects of Video Materials on Health Care Decisions Among Selected Audiences
| Video Content | Result | Audience |
| Patient with advanced dementia (Deep et al., 2010) | Proportion choosing comfort care* increased from 50% to 89% | General population over age 40 |
| Goals of care (life-prolonging, basic, or comfort care*) (Volandes et al., 2012a) | 80% of viewers chose comfort care,* compared with 57% in control group | Patients in skilled nursing facilities |
| Goals of care (El-Jawahri et al., 2010) | 91% of viewers chose comfort care,* compared with 22% in control group | People with advanced cancer |
| Cardiopulmonary resuscitation (CPR) (Volandes et al., 2013) | 20% of viewers wanted CPR, compared with 48% in control group | People with advanced cancer |
| CPR (Epstein et al., 2013) | 40% of viewers had their advance care plans documented 1 month after the intervention, compared with 15% in control group; viewers’ preferences for CPR changed significantly postintervention, with 24% no longer wanting CPR | People with pancreatic or hepatobiliary cancer |
| Goals of care (Volandes et al., 2012b) | Statistically significant decreases in proportion who wanted CPR or ventilation | People with advanced cancer |
*The phrase “comfort care” was used by the authors and described as care that maximizes comfort and alleviates pain or suffering.
patients), the intervention group received a pamphlet (“Living with Advanced Cancer”) and a discussion with a psychologist about preferences and values (Stein et al., 2013). Those receiving the intervention had do-not-resuscitate orders placed earlier and were less likely to die in the hospital than patients in the control group. Previous research had indicated that providing the pamphlet alone caused patients distress; with the addition of the discussion with a psychologist, no negative impact on patients or caregivers was found.
The timing of the use of decision aids also is important. By the time a patient is admitted to a hospital palliative care unit, for example, many of the most significant decisions may have been made, or patients may be too sick or preoccupied to participate (Matlock et al., 2011).
MODEL ADVANCE CARE PLANNING INITIATIVES
The National Quality Forum’s National Framework and Preferred Practices for Palliative and Hospice Care Quality includes seven preferred practices related to advance care planning (NQF, 2006). They reflect many of the issues raised in this chapter, and many build on positive experiences with model advance care planning initiatives that have improved the effectiveness of the process or its reach in the population. The seven practices are as follows:
- Document the designated surrogate/decision maker in accordance with state law for every patient in primary, acute, and long-term care and in palliative and hospice care.
- Document the patient/surrogate preferences for goals of care, treatment options, and setting of care at first assessment and at frequent intervals as conditions change.
- Convert the patient treatment goals into medical orders, and ensure that the information is transferable and applicable across care settings, including long-term care, emergency medical services [EMS], and hospital care, through a program such as the Physician Orders for Life-Sustaining Treatment (POLST) program.
- Make advance directives and surrogacy designations available across care settings, while protecting patient privacy and adherence to Health Insurance Portability and Accountability Act (HIPAA) of 1996 regulations, for example, by using Internet-based registries or electronic personal health records.
- Develop health care and community collaborations to promote advance care planning and the completion of advance directives
- for all individuals, for example, the Respecting Choices and Community Conversations on Compassionate Care programs.
- Establish or have access to ethics committees or ethics consultation across care settings to address ethical conflicts at the end of life.
- For minors with decision-making capacity, document the children’s views and preferences for medical care, including assent for treatment, and give them appropriate weight in decision making. Make appropriate professional staff members available to both the child and the adult decision maker for consultation and intervention when the child’s wishes differ from those of the adult decision maker (NQF, 2006, pp. 42-45).
These standards reflect several innovations in advance care planning that have occurred since Approaching Death (IOM, 1997) was published. These innovations overcome some of the difficulties experienced with conventional advance directives related to timing, relevance, lack of support, and unavailability when needed.
Physician Orders for Life-Sustaining Treatment
The POLST paradigm is an approach to advance care planning designed to ensure that seriously ill or frail patients can choose the treatments they want or do not want and that their wishes are documented and will be honored in an emergency (National POLST, 2012a). POLST is a clinical process designed to facilitate communication between health care professionals and patients, their families, their health care agents, or their designated surrogates. The process encourages shared, informed medical decision making. The result is a set of portable medical orders, POLST forms (see Annex 3-2), that respects the patient’s goals for care with regard to the use of cardiopulmonary resuscitation; artificially administered nutrition; and other medical interventions, such as intubation and future hospitalization (Bomba et al., 2012; National POLST, 2012a). Medical intervention options generally are described as “comfort measures only,” “limited additional interventions,” and “full treatment” and align with the intensity of the desired interventions. “Comfort measures only” indicates that the primary goal for care is maximizing comfort. If comfort needs cannot be met in the patient’s location, the patient is transported to a clinical care setting where those needs can be met. “Comfort measures” are medical care and treatment provided with the primary goal of relieving pain and other symptoms and reducing suffering, and may include offering food and fluids by mouth; turning the patient in bed; providing wound care; and providing oxygen, suctioning, and other manual treatment of airway obstruction for comfort. “Limited additional interventions” includes
comfort measures plus some medical interventions, such as administration of antibiotics and intravenous fluids. “Full treatment” includes measures provided in the other two categories, as well as use of additional medical interventions, such as intubation or mechanical ventilation.32
These medical orders support the person’s preferences with respect to treatment, preferred site for receiving care, and death, and can be reviewed and revised as needed (Bomba et al., 2012; National POLST, 2012a). They are intended to stay with patients near the end of life as they are transferred from home to hospital or any other type of care facility and to be in force wherever patients may be. POLST are followed in all care settings and by all health care professionals, including emergency medical services personnel, who in an emergency, cannot interpret a living will or take orders from a health care agent (Bomba et al., 2012; National POLST, 2012b,c).
POLST are not intended for everyone; they are for people with serious illnesses or frailty whose health care professionals would not be surprised if they died within the next year, based on their current health status and prognosis. POLST also are appropriate for patients who reside in a long-term care facility or receive long-term services at home as a result of frailty, and for persons of advanced age who want to avoid or receive any or all life-sustaining treatment. Among vulnerable populations, including persons with disabilities, POLST are intended only for seriously ill or frail patients facing end of life, not the entire population (Bomba et al., 2012; National POLST, 2012a).
The POLST process begins with the clinician’s preparing for the discussion by first reviewing the patient’s current health status and prognosis to ensure that POLST are appropriate for that patient. The second step entails retrieving and reviewing completed advance directives and prior do-not-resuscitate and/or POLST forms; the third, determining the patient’s capacity to make POLST decisions; and the fourth, educating the decision maker about POLST. A conversation or series of conversations between the patient and trained clinicians helps define the patient’s values, beliefs, and goals for care that will drive the choice of interventions. The discussion can occur in all clinical care settings, including the physician’s office, the long-term care facility, the hospital, or the patient’s home. If the patient lacks the capacity to make medical decisions outlined on the POLST form, discussion occurs with the health care agent or the appropriate surrogate, identified under state law. The clinician reviews possible treatment options on the entire POLST form and ensures shared, informed medical decision making. The POLST form is signed by the physician, because it represents
_______________
32Each state POLST paradigm program is responsible for developing that state’s POLST form; therefore, the forms vary from state to state. Forms from various states are available at http://www.polst.org/educational-resources/resource-library (accessed December 16, 2014).
a set of medical orders; in some states, nurse practitioners are authorized to sign the form. The conversation should also be documented in the patient’s medical record (Bomba et al., 2012).
The POLST form typically is printed in a bright, neon color so it is difficult to overlook on the patient’s home refrigerator or in an inches-thick medical chart. It is written in plain language, avoiding both medical and legal jargon, and intended to be based on conversations among the clinician, the patient, and the health care agent (Bomba et al., 2012; National POLST, 2012d).
The physician (or nurse practitioner, if state scope-of-practice regulations allow) should review the POLST form periodically as required by law, and also if
- the patient is transferred from one care setting or care level to another,
- there is a substantial change in the patient’s health status (for better or worse), or
- the patient or other decision maker changes his or her mind about treatment.
The advantages of POLST forms are such that their use is supported by the American Hospital Association, AARP, the National Hospice and Palliative Care Organization, and other groups. At the community level, a project sponsored by Excellus BlueCross and BlueShield in Upstate New York has worked to educate the community about that state’s POLST program (called Medical Orders for Life-Sustaining Treatment [MOLST]) (Compassion and Support, 2014a). The project has engaged employers, insured members, and clinicians in efforts to increase advance care planning and adherence to patients’ informed preferences (see also Chapter 6).
The POLST form is neither an advance directive nor a replacement for advance directives (Bomba et al., 2012; National POLST, 2012e). Both advance directives and the POLST form are helpful advance care planning documents for communicating patient wishes when appropriately used. As discussed in this chapter, one of the principal problems with the “living will” type of advance directive is that it may have been completed when a person was in relatively good health. At that point, it is almost impossible for people to predict the kind of care they would want in some future, more compromised state. Another problem is that clinicians often are unaware of the existence of the advance directive and do not always follow it if they are, if only because they believe patients’ former wishes are not relevant in their current situation. Finally, advance directives often do not accompany patients as they transfer between care settings. The POLST form is designed to overcome these limitations. Salient features of the POLST form
TABLE 3-6 Differences Between POLST and Advance Directives
| Characteristics | POLST | Advance Directives |
| Intended for | People who are seriously ill | All adults |
| Applies to | Current care | Future care |
| Form completed by | Health care professionals, based on in-depth discussion with their patients | Patients |
| Resulting form | Medical orders | Advance directive |
| Health care agent or surrogate role | Can engage in discussion if patient lacks capacity | Cannot complete |
| Portability | Clinician responsibility | Patient/family responsibility |
| Periodic review | Clinician responsibility | Patient/family responsibility |
SOURCE: Adapted from Bomba et al., 2012.
and the ways in which it differs from advance directives are summarized in Table 3-6.
Like advance directives, POLST forms allow patients to choose a range of intensities of care, from comfort measures only to full treatment, and to indicate whether they want emergency medical services personnel to attempt resuscitation. In one study of more than 700 patients with POLST in place, 42 percent specified comfort measures only, 47 percent specified limited interventions, and 12 percent specified full treatment (Hickman et al., 2010).
Effects of POLST on Patient Care
The developers of the POLST paradigm have conducted a number of studies to document its effects. These studies have yielded the following findings:
- The treatment preferences of nursing home residents without a POLST form were less likely to be reflected in medical orders, and their preferences for treatment other than cardiopulmonary resuscitation were less likely to be recorded (Hickman et al., 2010).
- Nursing home residents with POLST comfort measures only orders were less likely to receive life-prolonging treatments than those with POLST limited treatment or full treatment orders and those with traditional do-not-resuscitate and traditional full-code orders (Hickman et al., 2010).
- Having a POLST form made no difference in the amount of symptom care patients received (Hickman et al., 2010).
- Treatments provided to nursing home residents were highly consistent with POLST orders for resuscitation (98 percent), medical interventions including hospitalization (91 percent), and antibiotic administration (93 percent), but less consistent with orders regarding use of feeding tubes (64 percent) (Hickman et al., 2011).
- Patients whose POLST orders specified higher levels of medical treatment received that treatment (Hammes et al., 2012; Hickman et al., 2011).
- Care diverged from that specified in POLST orders only rarely (Hammes et al., 2012).
- One-half to three-quarters of patients with a POLST form specifying no resuscitation attempt nevertheless had orders for limited additional interventions or full treatment, which can include other medical interventions or life-sustaining treatments (Fromme et al., 2012; Hickman et al., 2009).
New York authorized the statewide use of MOLST in all care settings in 2008 after a successful 3-year community pilot was conducted to ensure that emergency medical services personnel could read and follow do-not-resuscitate and do-not-intubate orders on the MOLST form (Compassion and Support, 2008). Standardized professional training and community education materials, policies and procedures, and a quality assurance program were developed. Community-wide quality and implementation data were collected from emergency medical services, hospitals, nursing homes, hospices, assisted living facilities, enriched housing facilities, and Program of All-inclusive Care for the Elderly (PACE) programs in two Upstate New York counties (Caprio and Gillespie, 2008; Compassion and Support, undated-b).
California authorized the use of POLST in 2009, and efforts have been made to encourage facilities in the state, including nursing homes, to adopt their use. Among 283 respondents to a survey of state nursing homes, 69 percent reported that they had admitted a resident who had a POLST form (Wenger et al., 2012). Overall, 54 percent of nursing home residents had a POLST form. Fewer than 10 percent of nursing homes reported any difficulties in following the POLST orders or having emergency personnel follow them; however, problems that reportedly did arise with more frequency included
- difficulty in retrieving original POLST forms from other facilities (62 percent of respondents),
- difficulty in getting physicians to complete (38 percent) and sign (34 percent) the forms,
- family disagreement with the content of the forms (28 percent), and
- difficulty in interpreting POLST orders to make treatment decisions (21 percent).
Oregon researchers conducted a small survey of emergency medical services personnel to learn the impact of POLST on their work. They found that POLST orders affected both treatment and decisions regarding whether to transport patients to a hospital (Schmidt et al., 2013). Another recent study of 58,000 decedents in Oregon found that nearly 31 percent had POLST forms entered in Oregon’s POLST registry. Among those whose completed POLST forms stated a preference for comfort measures only (“Patient prefers no transfer to hospital for life-sustaining treatments. Transfer if comfort needs cannot be met in current location.”), that preference was highly likely to be honored (Fromme et al., 2014, p. 2). Only 6.4 percent of these decedents died in a hospital, compared with 34.2 percent of decedents without a POLST form in the registry. This suggests that such forms can be effective in limiting unwanted life-sustaining treatment.
New POLST programs in many states have carried out substantial community engagement efforts with diverse audiences. These efforts are intended to provide education about the program, especially how the POLST form differs from conventional advance directives; to obtain consumer and professional input; and to build momentum for statewide adoption (examples include the efforts of New York, described at http://www.compassionandsupport.org, and those of the Massachusetts Department of Public Health [2011]).
Challenges to POLST
Although many states have or are working to implement POLST, opposition to the paradigm has emerged in some communities, in some cases as a result of confusion between POLST and advance directives. For example, disability rights advocates successfully lobbied against Connecticut’s effort to enact POLST legislation in spring 2013 because they felt POLST limited rather than expanded patient options (Hargrave, 2013). Some Catholic theologians and organizations, including the Catholic Medical Association, have also raised objections to POLST (Brugger et al., 2013; Nienstedt et al., 2013), while others have endorsed them when used properly (Catholic Bishops of New York State, 2011). In a letter to the committee, the Catholic Health Association, which takes the view that portable medical documents such as POLST forms can be useful, emphasized the importance of “attending to some of the identified shortcomings and risks of these documents”
(Rodgers and Picchi, 2013, p. 2). Their concerns related to POLST include the following:
- The definition of whom POLST are for—The core idea is that POLST are for people who are seriously ill and near the end of life, but deviations from that notion have been seen.33
- Relevant training of health professionals—People who work with POLST, especially emergency personnel and staff of long-term care facilities, need training in the POLST process; effective communications regarding its use; and other skills, such as an understanding of the applicability of a POLST form in a given situation so they do not deny treatment for remediable problems that are not imminently life-threatening.
- Potential lack of meaningful conversation—Clinicians may simply check off the boxes on the POLST form without having the necessary conversations with patients and health care agents. In New York State, an eight-step protocol has been developed to guide clinician-patient/family interactions so as to ensure thoughtful MOLST discussions (Bomba et al., 2012).
- Significance of the clinician’s signature—Physicians or other clinicians sign the form, but attest only that the orders are to the best of their knowledge consistent with the patient’s current medical condition and preferences, not that they participated in the discussion of the orders. But the POLST form cannot be viewed as “simply another form to be completed by the health care professional, separated from the context of the advance care planning that is essential to the POLST paradigm” (Rodgers and Picchi, 2013, p. 2), because physicians are accountable for the medical orders in the form when they sign it.
- Voluntary nature of POLST—Perhaps especially in long-term care facilities and other institutional settings, the fundamental voluntary nature of POLST, in whole or in part, must be safeguarded, and completion of a POLST form should not be a requirement.
Respecting Choices
One of the best-known advance directive initiatives is Respecting Choices, a community-wide effort begun in 1991 in LaCrosse, Wisconsin.
_______________
33For example, Delaware’s Division of Public Health asked medical providers to discontinue using the state’s MOLST form until it could be revised because the agency determined it was being used for non–terminally ill patients, which is “beyond the legal parameters set forth in regulation 4304” (Delaware Health and Social Services, 2012).
Initially working with the city’s major health systems, the program was aimed not only at encouraging people to complete advance directives, although that is a challenging task in itself, but also at changing the institutional and professional culture and routines to promote and respect advance care planning in a comprehensive way (AHRQ, 2010; Gundersen Health System, 2014a,b). The program produces educational materials for patients; trains facilitators to discuss end-of-life questions with patients and prepare them for the end of life; and ensures that advance directives are available in patients’ medical records, now electronically. The project has also adopted the POLST paradigm (Hammes et al., 2012). Each health system promised to
- initiate advance care planning for each patient long before a medical crisis occurs,
- skillfully assist each willing patient with an individualized planning process,
- ensure that any plans created are clear and complete,
- have plans available to the health professionals who may participate in decision making when the patient is incapacitated, and
- follow plans appropriately and respect the values and preferences of the patient as allowed by law and organizational policy (Hammes, 2003, p. 2).
Making such a program work effectively requires embedding advance care planning in the community’s larger health system to enable professionals to communicate and collaborate on making improvements, creating ongoing monitoring and feedback loops for quality improvement, and sustaining the effort with ongoing financial support and staff training (Hammes, 2003). Two years after the implementation of the Respecting Choices program, a study found that among 540 decedents, 85 percent had a written advance directive, which in almost all cases (95 percent) was found in the patient’s medical record (Hammes and Rooney, 1998). In general, treatment preferences captured in the directives were followed when end-of-life treatment decisions were made. Accomplishing all this requires “nothing less than a cultural shift in the health care sector” (in der Schmitten et al., 2011, p. 8).
An early review of Respecting Choices describes six ways in which this program differs from conventional advance care planning initiatives, which help account for its success in achieving care in greater accord with patient wishes:
- It treats advance care planning as an ongoing process, not as an event designed to produce a product.
- It shifts the focus of end-of-life decision making away from document completion and toward facilitating discussion of values and preferences.
- It shifts the locus of planning from hospitals and physicians to the community and family.
- It does not assume the physician is crucial to the process, but promotes extensive training of nonphysician community volunteers.
- It refocuses discussion of preferences away from autonomy and toward personal relationships, for example, by asking the question, “How can you guide your loved ones to make the best decisions for you?”.
- It works with hospitals and area physician offices to ensure that completed advance directives are available in patients’ charts (Prendergast, 2001, p. N37).
The LaCrosse initiative has been used as a model for advance care planning programs for specific settings and populations, such as nursing homes (in der Schmitten et al., 2011), and for patients with advanced chronic illnesses, such as heart failure, who may be experiencing disease complications or frequent hospitalizations (Schellinger et al., 2011; see also Annex 3-1). Respecting Choices leader Bernard Hammes (2003) describes several barriers to implementation that must be overcome if the program is to be successfully replicated. First is the need to allow sufficient time to train health professionals and discussion facilitators. At the time Hammes was writing, the program recommended a 14-hour training program for facilitators and had found efforts to shorten this time unsuccessful. Hammes (2003) also cites as barriers the need to make the necessary system changes that establish advance care planning as the routine way to offer care and the need for funding for the costs of the program. Hammes acknowledges as well that transferring this model to more culturally diverse regions of the United States would be a challenge because a highly diverse population makes it more difficult to normalize the advance care planning conversation. In addition, many older people are accustomed to thinking of advance directives as “living wills”—a one-time recording of their wishes intended solely to preserve autonomy. They need to understand the new program’s more organic, discussion-based approach that evolves over time with clinical situations and health status.
Electronic Health Records
Electronic storage of advance directives, statements of wishes, health care proxies, or other relevant materials—either in the patient’s electronic
BOX 3-3
New York State’s eMOLST
New York State’s eMOLST program is an example of well-coordinated electronic documentation of advance care choices. eMOLST is a secure Web-based application that clinicians can use with patients. The application’s standardized clinical process emphasizes shared, informed decision making in completing the eMOLST form. In addition, a Chart Documentation Form provides details about the eMOLST discussion, including information on patients’ values, beliefs, and goals for care; capacity determination; and the framework for making MOLST decisions, based on who makes the decision and where it is made, in accordance with New York State’s Public Health Law.
eMOLST forms are created as pdf documents, which can be printed out for patients to keep and for insertion in paper-based medical records. The forms can also be stored or linked in electronic health records. Thus, the forms and supporting documentation are accessible regardless of whether an electronic health record is in use.
In addition, the forms become part of the state’s eMOLST registry, an electronic database that allows for ready round-the-clock availability of eMOLST forms and the detailed Chart Documentation Form. With this system, health care providers, including emergency personnel, can have access to eMOLST forms and supporting documentation at any time or place.
SOURCES: Compassion and Support, 2013, 2014b, undated-a.
health record or an external database—holds promise for solving some current problems with these documents. An example is described in Box 3-3.
A 2013 telephone survey of New York nursing homes found that almost 58 percent had implemented eMOLST, while 61 percent indicated interest in the program. A similar survey of hospices in the state found that 38 percent had implemented eMOLST, while 44 percent were interested. A similar survey of hospitals is under way.34
In theory, electronic systems should facilitate finding advance planning documents when critical decisions must be made. If records use a standard template, it may be easier to locate the relevant information to determine whether current care preferences are reflected in the medical record (Yung et al., 2010). According to Wilson and colleagues (2013, p. 1093), “Standardization is a fundamental prerequisite for efficient production and effective delivery of services,” and electronic systems can—although they do
_______________
34Personal communication, P. A. Bomba, Community Conversations on Compassionate Care, 2013.
not always—achieve standardization. Another potential advantage of having advance directives in electronic health records is that they can remind clinicians to inquire whether patients’ care preferences have changed and whether they wish to update the identity and contact information for their health care agent. For example, Partners Health System has pioneered an innovative and complete electronic health record module that supports appropriate discussion and documentation of end-of-life planning (Block, 2013). The module includes areas for documenting individuals’ preferences for receiving information about their illness, their understanding of their illness, and their goals and fears. Some of the other diverse and innovative ways in which clinicians and institutions are using electronic means to support advance care planning are described in Table 3-7.
Currently, however, there are some gaps in practice. Not all advance directive registries are linked to patients’ electronic health records. In addition, while electronic health records have increased the documentation of advance directives, they have resulted in “an increase in inaccurate
TABLE 3-7 Selected Examples of the Use of Electronic Health Records and Other Technologies to Support End-of-Life Planning
| Example | Outcome |
| Discharge summary template in the electronic health record to include care wishes expressed and health care agent (Lakin et al., 2013) | Given a modest incentive payment and feedback, clinicians recorded this information for more than 90% of patients discharged, compared with 12% of clinicians not offered these inducements. |
| Various models providing an electronic registry for 24-hour access to POLST forms and related documents (Zive and Schmidt, 2012) | Some models (such as New York’s eMOLST) also enable completion of standardized forms that can be integrated into patients’ electronic health records. |
| Web-based systems for education about end-of-life choices, forms and assistance in their completion, and document storage (Klugman and Usatine, 2012) | A Nevada pilot ended because of low usage and budget cuts; more than 5,000 accounts were created for a Texas repository in its first 3 years, and it was appreciated for its “ease of use.” |
| Interactive computer program that helps users clarify values and goals and record care preferences (Schubart et al., 2012) | In preliminary stages; a pilot shows the computer program had good reliability in representing patients’ general wishes and preferences. |
| Advance directive module in patient portals, alongside modules encouraging personal management of health (Bose-Brill and Pressler, 2012) | In preliminary stages; there is growing interest in and use of portals by patients. |
advance directive documentation from labeling errors made in transfer of information to the [electronic health record],” and systems of advance care planning and electronic health records have not yet been well coordinated (Bose-Brill and Pressler, 2012, p. 286). For example, EpicCare is one of the principal electronic health record systems adopted by U.S. health care providers. A study of the availability of advance care planning documents (including living wills, POLST forms, information about health care agents, and do-not-resuscitate orders) was conducted among active patients in EpicCare’s ambulatory care electronic health record system (Wilson et al., 2013). The study found that, while 51 percent of those aged 65 and older had such a document, only about one-third of their records included a scanned document—the only type that includes signatures, which are required to make them legally valid. Minority patients were less likely to have a scanned document. Additional problems included a lack of standardization in where in the record advance care planning information is recorded, thwarting easy retrieval, and a time lag between completion of advance care planning documents and their appearance in the electronic record.
Under the Health Information Technology for Economic and Clinical Health (HITECH) Act,35 Medicare and Medicaid have provided significant financial incentives for hospitals and physicians to engage in “meaningful use” of certified electronic health record technology (CMS, 2014). To receive these payments, physicians and hospitals must show they are “meaningfully using” electronic records to achieve certain specific objectives established by the Centers for Medicare & Medicaid Services. Thus far, the data standards related to advance care planning have been minimal, applying only to hospital patients aged 65 and older, but the evolution of meaningful use offers possibilities for expansion in various core areas, such as patient education and patient engagement. As noted earlier in this chapter, the ACA’s meaningful use provisions for electronic health records do not require, and the major commercial electronic health records do not provide for, robust documentation of advance care planning, including advance directives, POLST, or information about designation of and contact information for a health care agent. Meaningful use stage 2 includes as an objective only to “record whether a patient 65 years old or older has an advance directive” (CMS, 2012c, p. 1); further, this is not considered a “core” objective, and it is relevant only for eligible hospitals and critical access hospitals, not for eligible professionals (CMS, 2012d,e). Final recommendations from the Health Information Technology Policy Committee for meaningful use stage 3 maintained this stage 2 objective; however, the policy committee is now
_______________
35Health Information Technology for Economic and Clinical Health (HITECH) Act, Title XIII of Division A and Title IV of Division B of the American Recovery and Reinvestment Act of 2009 (ARRA), Public Law 111-5, 111th Cong., 1st sess. (February 17, 2009).
recommending that it be a core objective for eligible hospitals and a menu objective for eligible professionals (HHS, 2014). (See also the discussion of research needs related to electronic health records in Chapter 5, as well as that chapter’s recommendation.)
A PROPOSED LIFE CYCLE MODEL OF ADVANCE CARE PLANNING
As reflected in the standards of the National Framework and Preferred Practices for Palliative and Hospice Care Quality (NQF, 2006), discussed earlier, good advance care planning is not a one-time event, but should occur at appropriate decision points throughout life, roughly as detailed below (Benson and Aldrich, 2012; Bomba, 2005). The following life cycle model of advance care planning is based on these standards and practices, findings from the extant literature reviewed in this chapter, and the committee’s expertise and expert judgment. Considering the aspects of advance care planning throughout the life cycle continuum normalizes the process and aims to avoid the emotional burden sometimes experienced by patients, families, and loved ones who have not adequately prepared for making end-of-life care decisions. This proposed model has implications for quality improvement programs, clinician training, public and patient education, and payment systems.
Milestone-Specific
Under the life cycle model proposed by the committee, an initial conversation about values and life goals is held at some key maturation point—such as obtaining a driver’s license, turning 18, leaving home to go to school or into the military, or marriage (milestones when risks may change or the locus of responsibility shifts):
- The presumption is that the person is generally healthy and mentally competent, but like everyone is at risk for acute illness or injury and sudden (and possibly temporary) loss of capacity to make medical decisions.
- The purpose of the conversation at this point is to help normalize the advance care planning process by starting it early, to identify a health care agent, and to obtain guidance in the event of a rare catastrophic event.
- The consultation might be performed by a trained counselor, advanced practice nurse, physician assistant, or social worker.
Situation-Specific
Additional discussion of values and life goals is held, for example, with people in high-risk occupations; those involved in high-risk activities, including military training or deployment; and those with major genetic or congenital issues:
- Again, the presumption is that the person is in good health.
- The purpose is to ensure that a health care agent has been designated and to take into consideration any family issues (e.g., spouse, children).
- The consultation might be performed by a trained counselor, advanced practice nurse, physician assistant, or social worker.
As Part of Primary Care
Regular and periodic conversations are held with patients who do not have a serious disease regarding their values, goals, and preferences:
- This conversation can be led by a nonphysician.
- The choice of health care agent should be reviewed.
Initial Diagnosis of Chronic Illness (Disease Management)
Further discussion takes place at the initial diagnosis of a chronic life-limiting illness (although the end-point still may be years out):
- A physician should explain the diagnosis, the likely course of the illness, complications to watch for, and ways to slow the disease’s progression.
- A nonphysician can ensure that a health care agent is named and encourage a conversation about what it means to be an agent and what patient-agent discussions should take place.
As Health Worsens (Case Management)
Discussion also takes place at turning points in the disease (major treatment changes; significant side effects or “turns for the worse”; onset of comorbidities):
- Members of the care team can participate in these discussions, which should also include the designated health care agent. As the
- disease worsens, family members may benefit from counseling and practical advice. Spiritual counseling can be offered.
- Patient and family should be asked how much information they want about prognosis and what to expect.
In the Final Year of Expected Life
Discussion takes place again when death would not be a surprise if it occurred in the next year:
- The opportunity for thoughtful POLST discussions is offered to increase the likelihood that preferences for care and treatment are accessible and honored.
- A “palliative care time out”—a required family meeting after a patient has been in intensive care for a certain number of days—is held so that everyone stops and reconsiders what is being done and why.
- Members of the interdisciplinary health care team work with the family and health care agent to support their role and potentially forestall complicated bereavement.
- Members of the interdisciplinary health care team obtain help for the family with practical matters.
Special Considerations for Seriously Ill Children
Children transitioning from childhood to adulthood should choose a health care agent. For minors with decision-making capacity near the end of life, according to the NQF standard, the child’s views and preferences for medical care, including assent for treatment, should be documented and given appropriate weight in decision making (NQF, 2006; Dahlin, 2013). When the child’s wishes differ from those of the adult decision maker, appropriate professional staff members should be made available for consultation and intervention.
A large body of research exists on advance directives—whether they have been created, whether they have been followed, and what impact they have on important outcomes of care. This literature is a principal reason that the usefulness of simple checkbox-style documents has come into question. Much less research has been conducted on the effectiveness of more thorough advance care planning conducted over time and tailored to immediate decisions as needed, as in the life cycle model de-
scribed above. Also needed is further investigation into how advances in thinking about shared decision making and behavioral economics can be applied specifically in end-of-life situations. A focus on preparing people for in-the-moment decision making, rather than specifying exact treatment preferences, holds promise as well. With respect to the POLST paradigm and other community-wide efforts to encourage advance care planning, the research challenge is one of developing and validating best practices to ensure the integrity of these program models as they are diffused to other settings. Likewise, investigations should be initiated to determine the most effective ways in which electronic health records can support advance care planning.
Decision-making theory points to the various means used by individuals to arrive at important decisions; the stages of change theory described in this chapter is one such model. A better understanding of patient and family decision-making styles might help clinicians work with their patients more effectively and lead to decisions most relevant and appropriate to each patient. In addition, more information is needed on the way the care system respects, responds to, and sometimes shapes the decisions of patients and whether or in what ways this is affected by race, gender, income, literacy, insurance status, or other factors. Findings from such research should be useful in improving communication between clinicians and the full range of patients they serve. This type of research might lead to the development of appropriate decision supports as well.
Specific research needs include investigation into the effectiveness of strategies for advance care planning (versus advance directives) and their effects on achieving concordance with patients’ informed preferences and quality of care. Specific needs relate also to
- the development of guidelines for pediatric and adolescent advance care planning;
- continued research toward understanding children’s involvement in end-of-life decision making and comparative effectiveness studies of different approaches to decision support and communication;
- understanding of racial, ethnic, and cultural differences in advance care planning among nursing home residents;
- best practices and needs for different Asian, Hispanic, and South Asian populations;
- ways to improve shared decision making;
- the significance of and strategies for implementing choice architecture in advance care planning programs; and
- the most effective and cost-effective designs for financial incentives and reimbursement for clinicians to participate in advance care
- planning, recognizing that doing so takes time and may require repeated consultations.
FINDINGS, CONCLUSIONS, AND RECOMMENDATION
Findings and Conclusions
This study yielded the following findings and conclusions on alignment of the care patients receive with the care they want.
Decision-Making Capacity
Most people nearing the end of life are not physically, mentally, or cognitively able to make their own decisions about care. Approximately 40 percent of adult medical inpatients, 44-69 percent of nursing home residents, and 70 percent of older adults facing treatment decisions are incapable of making those decisions themselves. Furthermore, the majority of these patients will receive acute hospital care from physicians who do not know them. As a result, advance care planning is essential to ensure that people receive care that reflects their values, goals, and preferences (Kim et al., 2002; Nelson et al., 2006; Raymont et al., 2004; Silveira et al., 2010).
Comfort-Focused Care Versus Acute Care
People who capture their preferences for care near the end of life most commonly, but not always, choose care that is focused on alleviating pain and suffering. Because the default mode of treatment is acute care in the hospital, however, a higher prevalence of advance care planning and medical orders will be more likely to achieve patient preferences (Billings, 2012; Mack et al., 2010b; Wright et al., 2008).
Implementation of Patient Wishes
Most people, even those who are older and have serious illnesses, do not complete advance directives, and even when these documents are completed, they rarely affect treatment decisions. They often are unavailable or difficult to interpret, and they may contradict the preferences of the family or clinicians. On the other hand, people who have had conversations about end-of-life care values, goals, and preferences (although they may not have completed formal advance directive documents) are less likely to receive unwanted treatment. Advance care planning should be considered a lifelong process. Health care agents should be identified early in this process, and for people with advanced serious illnesses, POLST forms should be
used (Ditto et al., 2006; Fried et al., 2007; Hammes et al., 2012; Hickman et al., 2011; Kelley et al., 2011; NQF, 2006). However, most people—particularly younger, poorer, minority, and less educated individuals—do not have conversations about end-of-life care. Clinicians need to recognize the multiple barriers to effective communication on these issues, initiate the conversation themselves, and take time and make the effort to ensure that patient and family decisions are made with adequate information and understanding (Clements, 2009; Curtis and Engelberg, 2011; Phipps et al., 2003; Sudore et al., 2010; Volandes et al., 2008a; Waite et al., 2003).
Lack of Clinician Communication Skills
The quality of communication between clinicians and patients who have advanced serious illnesses or are nearing death falls far short of the ideal, particularly with respect to discussing prognosis, dealing with emotional and spiritual concerns, and finding the right balance between hoping for the best and preparing for the worst. Advance care planning will not succeed without improved communication generally. Incentives, quality standards, and system support for the time required to conduct such conversations are necessary to promote improved communication that meets the standards expected by patients and families (Anderson et al., 2008; Back et al., 2003; Dias et al., 2003; Epstein and Street, 2007; NQF, 2006; Smith et al., 2013b).
Recommendation 2. Professional societies and other organizations that establish quality standards should develop standards for clinician-patient communication and advance care planning that are measurable, actionable, and evidence-based. These standards should change as needed to reflect the evolving population and health system needs and be consistent with emerging evidence, methods, and technologies. Payers and health care delivery organizations should adopt these standards and their supporting processes, and integrate them into assessments, care plans, and the reporting of health care quality. Payers should tie such standards to reimbursement, and professional societies should adopt policies that facilitate tying the standards to reimbursement, licensing, and credentialing to encourage
- all individuals, including children with the capacity to do so, to have the opportunity to participate actively in their health care decision making throughout their lives and as they approach death, and receive medical and related social services consistent with their values, goals, and informed preferences;
- clinicians to initiate high-quality conversations about advance care
- planning, integrate the results of these conversations into the ongoing care plans of patients, and communicate with other clinicians as requested by the patient; and
- clinicians to continue to revisit advance care planning discussions with their patients because individuals’ preferences and circumstances may change over time.
Abbott, C. H., H. G. Prigerson, and P. K. Maciejewski. 2013. The influence of patients’ quality of life at the end of life on bereaved caregivers’ suicidal ideation. Journal of Pain and Symptom Management [epub ahead of print].
AHRQ (Agency for Healthcare Research and Quality). 2010. Service delivery innovation profile: Community-wide education, trained facilitators, and improved processes lead to more advance care planning, consistency between plans and end-of-life decisions, and low care costs. http://www.innovations.ahrq.gov/content.aspx?id=2713 (accessed June 1, 2014).
Albrecht, G. L., and P. J. Devlieger. 1999. The disability paradox: High quality of life against all odds. Social Science & Medicine 48(8):977-988.
Allen, J. Y., W. E. Haley, B. J. Small, R. S. Schonwetter, and S. C. McMillan. 2013. Bereavement among hospice caregivers of cancer patients one year following loss: Predictors of grief, complicated grief, and symptoms of depression. Journal of Palliative Medicine 16(7):745-751.
American Bar Association. 2005. Consumer’s tool kit for health care advance planning. 2nd ed. Washington, DC: American Bar Association Commission on Law and Aging.
American Bar Association. 2009. Default surrogate consent statutes. http://www.americanbar.org/content/dam/aba/migrated/aging/PublicDocuments/famcon_2009.authcheckdam.pdf (accessed June 30, 2014).
American Health Decisions. 1997. The quest to die with dignity: An analysis of Americans’ values, opinions and attitudes concerning end-of-life care. Executive summary. http://www.ahd.org/The_Quest_to_Die_With_Dignity.html (accessed August 1, 2013).
American Lung Association. 2013. Trends in COPD (chronic bronchitis and emphysema): Morbidity and mortality. http://www.lung.org/finding-cures/our-research/trend-reports/copd-trend-report.pdf (accessed June 2, 2014).
Anderson, G. T. 2006. What y’all gon’ do with me?: The African-American spiritual and ethical guide to end of life care. http://www.stu.ca/~spirituality/GloriaThomasAnderson-TheAfricanAmericanSpiritualandEthicalEndofLifeCareGuidepresentation2006.pdf (accessed June 2, 2014).
Anderson, W. G., S. C. Alexander, K. L. Rodriguez, A. S. Jeffreys, M. K. Olsen, K. I. Pollak, J. A. Tulsky, and R. M. Arnold. 2008. “What concerns me is…” Expressions of emotion by advanced cancer patients during outpatient visits. Supportive Care in Cancer 16(7):803-811.
Apatira, L., E. A. Boyd, G. Malvar, L. R. Evans, J. M. Luce, B. Lo, and D. B. White. 2008. Hope, truth, and preparing for death: Perspectives of surrogate decision makers. Annals of Internal Medicine 149(12):861-868.
Artnak, K. E. 2008. Ethics consultation in dual diagnosis of mental illness and mental retardation: Medical decision-making for community-dwelling persons. Cambridge Quarterly of Healthcare Ethics 17:239-246.
Azoulay, E., F. Pochard, N. Kentish-Barnes, S. Chevret, J. Aboab, C. Adrie, D. Annane, G. Bleichner, P. E. Bollaert, M. Darmon, T. Fassier, R. Galliot, M. Garrouste-Orgeas, C. Goulenok, D. Goldgran-Toledano, J. Hayon, M. Jourdain, M. Kaidomar, C. Laplace, J. Larché, J. Liotier, L. Papazian, C. Poisson, J. Reignier, F. Saidi, and B. Schlemmer. 2005. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. American Journal of Respiratory and Critical Care Medicine 171(9):987-994.
Back, A. L., R. M. Arnold, and T. E. Quill. 2003. Hope for the best, and prepare for the worst. Medical writings. Annals of Internal Medicine 138(5):439-443.
Back, A. L., R. M. Arnold, W. F. Baile, K. A. Edwards, and J. A. Tulsky. 2010. When praise is worth considering in a difficult conversation. Perspectives. Lancet 376(9744):866-867.
Baer, J., M. Kutner, J. Sabatini, and S. White. 2009. Basic reading skills and the literacy of America’s least literate adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2009-481. Washington, DC: National Center for Education Statistics. http://nces.ed.gov/pubs2009/2009481.pdf (accessed February 10, 2014).
Balboni, T. A., L. C. Vanderwerker, S. D. Block, M. E. Paulk, C. S. Lathan, J. R. Peteet, and H. G. Prigerson. 2007. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. Journal of Clinical Oncology 25(5):555-560.
Balboni, T., M. Balboni, M. E. Paulk, A. Phelps, A. Wright, J. Peteet, S. Block, C. Lathan, T. VanderWeele, and H. Prigerson. 2011. Support of cancer patients’ spiritual needs and associations with medical care costs at the end of life. Cancer 117(23):5383-5391.
Balboni, T. A., M. Balboni, A. C. Enzinger, K. Gallivan, E. Paulk, A. Wright, K. Steinhauser, T. J. VanderWeele, and H. G. Prigerson. 2013. Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Internal Medicine 173(12):1109-1117.
Barclay, S., N. Momen, S. Case-Upton, I. Kuhn, and E. Smith. 2011. End-of-life care conversations with heart failure patients: A systematic literature review and narrative synthesis. British Journal of General Practice 61(582):e49-e62.
Barnato, A. E., Z. Berhane, L. A. Weissfeld, C-C. H. Chang, W. T. Linde-Zwirble, and D. C. Angus. 2006. Racial variation in end-of-life intensive care use: A race or hospital effect? Health Services Research 41(6):2219-2237.
Barnato, A. E., C-C. H. Chang, O. Saynin, and A. M. Garber. 2007. Influence of race on inpatient treatment intensity at the end of life. Journal of General Internal Medicine 22(3):338-345.
Barnato, A. E., D. Mohan, J. Downs, C. L. Bryce, D. C. Angus, and R. M. Arnold. 2011. A randomized trial of the effect of patient race on physicians’ intensive care unit and life-sustaining treatment decisions for an acutely unstable elder with end-stage cancer. Critical Care Medicine 39(7):1663-1669.
Bélanger, E., C. Rodríguez, and D. Groleau. 2010. Shared decision-making in palliative care: A systematic mixed studies review using narrative synthesis. Palliative Medicine 25(3):242-261.
Benson, W. F., and N. Aldrich. 2012. Advance care planning: Ensuring your wishes are known and honored if you are unable to speak for yourself, critical issue brief. Atlanta, GA: CDC. http://www.cdc.gov/aging/pdf/advanced-care-planning-critical-issue-brief.pdf (accessed June 1, 2014).
Berkman, N. D., S. L. Sheridan, K. E. Donahue, D. J. Halpern, A. Viera, K. Crotty, A. Holland, M. Brasure, K. N. Lohr, E. Harden, E. Tant, I. Wallace, and M. Viswanathan. 2011. Health literacy interventions and outcomes: An updated systematic review. Evidence Report/Technology Assessment No. 199. AHRQ Publication No. 11-E006. Rockville, MD: AHRQ.
Berlinger, N., B. Jennings, and S. M. Wolf. 2013. The Hastings Center guidelines for decisions on life-sustaining treatment and care near the end of life. 2nd ed. New York: Oxford University Press.
Billings, J. A. 2012. The need for safeguards in advance care planning. Journal of General Internal Medicine 27(5):595-600.
Blank, R. H. 2011. End-of-life decision making across cultures. The Journal of Law, Medicine & Ethics 39(2):201-214.
Block, S. D. 2013. Assuring safe passage: Moving conversations about the end of life upstream. Chicago, IL: The University of Chicago Department of Medicine Grand Rounds. http://medicine.uchicago.edu/grandrounds/assuring%20safe%20passage%20101513.ppt (accessed May 26, 2014).
Bluebond-Langner, M., J. B. Belasco, A. Goldman, and C. Belasco. 2007. Understanding parents’ approaches to care and treatment of children with cancer when standard therapy has failed. Journal of Clinical Oncology 25(17):2414-2419.
Bomba, P. A. 2005. Advance care planning along the continuum. The Case Manager 16(2):68-72.
Bomba, P. A., and D. Vermilyea. 2006. Integrating POLST into palliative care guidelines: A paradigm shift in advance care planning in oncology. Journal of the National Comprehensive Cancer Network 4(8):819-829.
Bomba, P. A., M. Kemp, and J. S. Black. 2012. POLST: An improvement over traditional advance directives. Cleveland Clinic Journal of Medicine 79(7):457-464.
Bose-Brill, S., and T. R. Pressler. 2012. Commentary: Opportunities for innovation and improvement in advance care planning using a tethered patient portal in the electronic health record. Journal of Primary Care & Community Health 3(4):285-288.
Boyd, E. A., B. Lo, L. R. Evans, G. Malvar, L Apatira, J. M. Luce, and D. B. White. 2010. “It’s not just what the doctor tells me”: Factors that influence surrogate decision-makers’ perceptions of prognosis. Critical Care Medicine 38(5):1270-1275.
Bruera, E., C. Sweeney, K. Calder, L. Palmer, and S. Benisch-Tolley. 2001. Patient preferences versus physician perceptions of treatment decisions in cancer care. Journal of Clinical Oncology 19(11):2883-2885.
Bruera, E., J. S. Willey, J. L. Palmer, and M. Rosales. 2002. Treatment decisions for breast carcinoma: Patient preferences and physician perceptions. Cancer 94(7):2076-2080.
Brugger, C., L. C. Breschi, E. M. Hart, M. Kummer, J. I. Lane, P. T. Morrow, F. L. Smith, W. L. Toffler, M. Beffel, J. F. Brehany, S. Buscher, and R. L. Marker. 2013. The POLST paradigm and form: Facts and analysis. The Linacre Quarterly 80(2):103-138.
Buck, H. G., and S. H. Meghani. 2012. Spiritual expressions of African Americans and whites in cancer pain. Journal of Holistic Nursing 30(2):107-116.
Burkle, C. M., P. S. Mueller, K. M. Swetz, C. C. Hook, and M. T. Keegan. 2012. Physician perspectives and compliance with patient advance directives: The role external factors play on physician decision making. BMC Medical Ethics 13:31.
Butow, P. N., R. F. Brown, S. Cogar, M. H. Tattersall, and S. M. Dunn. 2002. Oncologists’ reactions to cancer patients’ verbal cues. Psycho-Oncology 11(1):47-58.
Byock, I. 2013. This is personal! In Trends in cancer care near the end of life: A Dartmouth Atlas of Health Care Brief, edited by D. C. Goodman, N. E. Morden, C.-H. Chang, E. S. Fisher, and J. E. Wennberg. Lebanon, NH: The Dartmouth Atlas of Health Care. Pp. 5-8. http://www.dartmouthatlas.org/downloads/reports/Cancer_brief_090413.pdf (accessed September 6, 2013).
Caprio, T., and S. Gillespie. 2008. Update on MOST facility implementation and quality improvement audits. Presentation to the Monroe County MOLST Quality Forum. http://www.compassionandsupport.org/pdfs/news/MC_MOLST_Quaity_Forum_QI_Presentation.FINAL.ppt (accessed March 22, 2014).
Carlson, L. E., S. L. Groff, O. Maciejewski, and B. D. Bultz. 2010. Screening for distress in lung and breast cancer outpatients: A randomized controlled trial. Journal of Clinical Oncology 28(33):4884-4491.
Carlson, L. E., A. Waller, and A. J. Mitchell. 2012. Screening for distress and unmet needs in patients with cancer: Review and recommendations. Journal of Clinical Oncology 30(11):1160-1177.
Carr, D. 2011. Why don’t older adults prepare for the end of life? The social stratification of advance care planning. Paper presented at Living in a High Inequality Regime Conference, Stanford University, Stanford, CA, November.
Carr, D. 2012a. Racial and ethnic differences in advance care planning: Identifying subgroup patterns and obstacles. Journal of Aging and Health 24(6):923-947.
Carr, D. 2012b. The social stratification of older adults’ preparations for end-of-life health care. Journal of Health and Social Behavior 53(3):297-312.
Carr, D., and D. Khodyakov. 2007. Health care proxies: Whom do young old adults choose and why? Journal of Health and Social Behavior 48(2):180-194.
Carr, D., and S. M. Moorman. 2009. End-of-life treatment preferences among older adults: An assessment of psychosocial influences. Sociological Forum 24(4):754-778.
Castillo, L. S., B. A. Williams, S. M. Hooper, C. P. Sabatino, L. A. Weithorn, and R. L. Sudore. 2011. Lost in translation: The unintended consequences of advance directive law on clinical care. Annals of Internal Medicine 154(2):121-128.
Catholic Bishops of New York State. 2011. Now and at the hour of our death: A Catholic guide to end-of-life decision-making. http://www.nyscatholic.org/wp-content/uploads/2011/11/End-of-Life-booklet-final.pdf (accessed February 5, 2013).
CDC (Centers for Disease Control and Prevention). 2011. Alzheimer’s disease. http://www.cdc.gov/aging/aginginfo/alzheimers.htm (accessed February 5, 2014).
CDC. 2012. Chronic obstructive pulmonary disease among adults—United States, 2011. Morbidity and Mortality Weekly Report 61(46):938-943.
CDC. 2013a. Heart failure fact sheet. http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_heart_failure.htm (accessed November 21, 2013).
CDC. 2013b. Leading causes of death. http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm (accessed June 2, 2014).
Ceronsky, L., and D. E. Weissman. 2011. Helping families in long-term care facing complex decisions: Applying the evidence about family meetings from other settings. Annals of Long Term Care 19(2):27-32.
CHCF (California HealthCare Foundation). 2012. Final chapter: Californians’ attitudes and experiences with death and dying. http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/F/PDF%20FinalChapterDeathDying.pdf (accessed August 7, 2013).
Chochinov, H. M., D. Tataryn, J. J. Clinch, and D. Dudgeon. 1999. Will to live in the terminally ill. Lancet 354(9181):816-819.
Christakis, N. A., and T. J. Iwashyna. 2003. The health impact of health care on families: A matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses. Social Science & Medicine 57(3):465-475.
Christakis, N. A., and E. B. Lamont. 2000. Extent and determinants of error in physicians’ prognoses in terminally ill patients: Prospective cohort study. British Medical Journal 320:469-473.
Clayton, J. M., P. N. Butow, R. M. Arnold, and M. H. N. Tattersall. 2005. Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers. Cancer 103(9):1965-1975.
Clements, J. M. 2009. Patient perceptions on the use of advance directives and life prolonging technology. American Journal of Hospice & Palliative Medicine 26(4):270-276.
CMS (Centers for Medicare & Medicaid Services). 2012a. Quick reference information: The ABCs of providing the initial preventive physical examination. http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/MPS_QRI_IPPE001a.pdf (accessed October 17, 2013).
CMS. 2012b. Medicare preventive services national provider call: The initial preventive physical exam and the annual wellness visit. Presented on the MLN Connect National Provider Call, March 28. http://www.cms.gov/Outreach-and-Education/Outreach/NPC/Downloads/IPPE-AWV-NPC-Presentation.pdf (accessed November 22, 2013).
CMS. 2012c. Stage 2 eligible hospital and critical access hospital meaningful use menu set measures: Measure 1 of 6. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/Stage2_MeaningfulUseSpecSheet_TableContents_EPs.pdf (accessed June 2, 2014).
CMS. 2012d. Stage 2 eligible hospital and critical access hospital (CAH) meaningful use core and menu objectives. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/Stage2_MeaningfulUseSpecSheet_TableContents_EligibleHospitals_CAHs.pdf (accessed June 2, 2014).
CMS. 2012e. Stage 2 eligible professional (EP) meaningful use core and menu objectives. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/Stage2_MeaningfulUseSpecSheet_TableContents_EPs.pdf (accessed June 2, 2014).
CMS. 2014. The official web site for the Medicare and Medicaid electronic health records (EHR) incentives programs. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms (accessed June 1, 2014).
Colclough, Y. Y., and G. M. Brown. 2013. End-of-life treatment decision making: American Indians’ perspective. American Journal of Hospice & Palliative Medicine [epub ahead of print].
Coleman, D. 2013. Full written public comment: Disability related concerns about POLST. http://www.notdeadyet.org/full-written-public-comment-disability-related-concerns-about-polst#_edn10 (accessed September 6, 2013).
Collins, S. P., P. S. Pang, G. C. Fonarow, C. W. Yancy, R. O. Bonow, and M. Gheorghiade. 2013. Is hospital admission for heart failure really necessary?: The role of the emergency department and observation unit in preventing hospitalization and rehospitalization. Journal of the American College of Cardiology 61(2):121-126.
Compassion and Support. 2008. Medical Orders for Life-Sustaining Treatment (MOLST) Program: A POLST Paradigm Program: A Community-Wide End-of-Life/Palliative Care Initiative Project. Poster presented to the Blue Cross Association Conference. http://www.compassionandsupport.org/pdfs/MOLST-poster.pdf (accessed May 29, 2014).
Compassion and Support. 2010. Advance care planning: Know your choices, share your wishes. Maintain control, achieve peace of mind, and assure your wishes are honored. http://www.compassionandsupport.org/pdfs/about/B-1576_Excellus_2010_Complete.pdf (accessed May 15, 2014).
Compassion and Support. 2013. eMOLST program manual. Vol. 10. http://www.compassionandsupport.org/pdfs/professionals/molst/eMOLSTProgramManual.pdf (accessed June 1, 2014).
Compassion and Support. 2014a. About us. https://www.compassionandsupport.org/index.php/about_us (accessed May 29, 2014).
Compassion and Support. 2014b. eMOLST: Electronic Medical Orders for Life-Sustaining Treatment in New York State. http://www.compassionandsupport.org/index.php/for_professionals/molst_training_center/emolst (accessed June 1, 2014).
Compassion and Support. undated-a. EMS and MOLST pilot results. http://www.compassionandsupport.org/pdfs/molst-training/ems-molst-pilot-results.pdf (accessed March 22, 2014).
Compassion and Support. undated-b. eMOLST form completion (clinical) screenshots. http://www.compassionandsupport.org/pdfs/professionals/molst/eMOLSTFormCompletionScreenshots.pdf (accessed June 1, 2014).
The Conversation Project. 2013. New survey reveals “conversation disconnect”: 90 percent of Americans know they should have a conversation about what they want at the end of life, yet only 30 percent have done so. News release. http://theconversationproject.org/wp-content/uploads/2013/09/TCP-Survey-Release_FINAL-9-18-13.pdf (accessed September 18, 2013).
Cosgriff, J. A., M. Pisani, E. H. Bradley, J. R. O’Leary, and T. R. Fried. 2007. The association between treatment preferences and trajectories of care at the end-of-life. Journal of General Internal Medicine 22(11):1566-1571.
Cox, C., E. Cole, T. Reynolds, M. Wandrag, S. Breckenridge, and M. Dingle. 2006. Implications of cultural diversity in Do Not Attempt Resuscitation (DNAR) decision making. Journal of Multicultural Nursing and Health 12(1):20.
Curtis, J. R., and R. A. Engelberg. 2011. What is the “right” intensity of care at the end of life and how do we get there? Editorial. Annals of Internal Medicine 154(4):283-284.
Curtis, J. R., D. L. Patrick, R. A. Engelberg, K. Norris, C. Asp, and I. Byock. 2002. A measure of the quality of dying and death: Initial validation using after-death interviews with family members. Journal of Pain and Symptom Management 24(1):17-31.
Curtis, J. R., R. A. Engelberg, E. L. Nielsen, D. H. Au, and D. L Patrick. 2004. Patient-physician communication about end-of-life care for patients with severe COPD. European Respiratory Journal 24:200-205.
Dahlin, C., ed. 2013. Clinical practice guidelines for quality palliative care. 3rd ed. Pittsburgh, PA: National Consensus Project for Quality Palliative Care. http://www.hpna.org/multimedia/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf (accessed August 5, 2013).
Deep, K. S., A. Hunter, K. Murphy, and A. Volandes. 2010. “It helps me see with my heart”: How video informs patients’ rationale for decisions about future care in advanced dementia. Patient Education and Counseling 81(2):229-234.
Delaware Health and Social Services. 2012. Medical Orders for Life-Sustaining Treatments (MOLST) form. http://www.patientsrightscouncil.org/site/wp-content/uploads/2012/12/Delaware_MOLST_11_12.pdf (accessed September 25, 2013).
Dellefield, M. E., and R. Ferrini. 2011. Promoting excellence in end-of-life care: Lessons learned from a cohort of nursing home residents with advanced Huntington Disease. Journal of Neuroscience Nursing 43(4):186-192.
DesHarnais, S., R. E. Carter, W. Hennessy, J. E. Kurent, and C. Carter. 2007. Lack of concordance between physician and patient: Reports on end-of-life care discussions. Journal of Palliative Medicine 10(3):728-740.
Detering, K. M., A. D. Hancock, M. C. Reade, and W. Silvester. 2010. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. British Medical Journal 340:c1345.
Dias, L., B. A. Chabner, T. J. Lynch, Jr., and R. T. Penson. 2003. Breaking bad news: A patient’s perspective. The Oncologist 8:587-596.
Ditto, P. H., J. A. Jacobson, W. D. Smucker, J. H. Danks, and A. Fagerlin. 2006. Context changes choices: A prospective study of the effects of hospitalization on life-sustaining treatment preferences. Medical Decision Making 26(4):313-322.
Dresser, R. 2013. Taking care: Ethical caregiving in our aging society. Presentation at meeting of the IOM Committee on Approaching Death: Addressing Key End-of-Life Issues, Houston, TX, July 22.
Durall, A., D. Zurakowski, and J. Wolfe. 2012. Barriers to conducting advance care discussions for children with life-threatening conditions. Pediatrics 129(4):e975-e982.
Edwards, A., N. Pang, V. Shiu, and C. Chan. 2010. Review: The understanding of spirituality and the potential role of spiritual care in end-of-life and palliative care: A meta-study of qualitative research. Palliative Medicine 24(8):753-770.
Edwards, J. D., S. S. Kun, R. J. Graham, and T. G. Keens. 2012. End-of-life discussions and advance care planning for children on long-term assisted ventilation with life-limiting conditions. Journal of Palliative Care 28(1):21-27.
El-Jawahri, A., L. J. Podgurski, A. F. Eichler, S. R. Plotkin, J. S. Temel, S. L. Mitchell, Y. Chang, M. J. Barry, and A. E. Volandes. 2010. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. Journal of Clinical Oncology 28(2):305-310.
Elwyn, G., D. Frosch, A. E. Volandes, A. Edwards, and V. M. Montori. 2010. Investing in deliberation: A definition and classification of decision support interventions for people facing difficult health decisions. Medical Decision Making 30(6):701-711.
Epstein, A. S., A. E. Volandes, L. Y. Chen, K. A. Gary, Y. Li, P. Agre, T. T. Levin, D. L. Reidy, R. D. Meng, N. H. Segal, K. H. Yu, G. K. Abou-Alfa, Y. Y. Janjigian, D. P. Kelsen, and E. M. O’Reilly. 2013. A randomized controlled trial of a cardiopulmonary resuscitation video in advance care planning for progressive pancreas and hepatobiliary cancer patients. Journal of Palliative Medicine 16(6):623-631.
Epstein, R. M., and R. L. Street, Jr. 2007. Patient-centered communication in cancer care: Promoting healing and reducing suffering. NIH No. 07-6225. Bethesda, MD: National Cancer Institute.
Evans, L. R., E. A. Boyd, G. Malvar, L. Apatira, J. M. Luce, B. Lo, and D. B. White. 2009. Surrogate decision-makers’ perspectives on discussing prognosis in the face of uncertainty. American Journal of Respiratory and Critical Care Medicine 179:48-53.
Fischer, S. M., A. Sauaia, S-J. Min, and J. Kutner. 2012. Advance directive discussions: Lost in translation or lost opportunities? Journal of Palliative Medicine 15(1):86-92.
Fischer, S. M., S. J. Min, L. Cervantes, and J. Kutner. 2013. Where do you want to spend your last days of life? Low concordance between preferred and actual site of death among hospitalized adults. Journal of Hospital Medicine 8(4):178-183.
Flannelly, K. J., L. L. Emanuel, G. F. Handzo, K. Galek, N. R. Silton, and M. Carlson. 2012. A national study of chaplaincy services and end-of-life outcomes. BMC Palliative Care 11:10.
Fowler, F. J., Jr., B. S. Gerstein, and M. J. Barry. 2013. How patient centered are medical decisions? Results of a national survey. JAMA Internal Medicine 173(13):1215-1221.
Frahm, K. A., L. M. Brown, and K. Hyer. 2012. Racial disparities in end-of-life planning and services for deceased nursing home residents. Journal of the American Medical Directors Association 13(9):819.e7-819.e11.
Fried, T. R., and J. R. O’Leary. 2008. Using the experiences of bereaved caregivers to inform patient- and caregiver-centered advance care planning. Journal of General Internal Medicine 23(10):1602-1607.
Fried, T. R., E. H. Bradley, V. R. Towle, and H. Allore. 2002. Understanding the treatment preferences of seriously ill patients. New England Journal of Medicine 346(14):1061-1066.
Fried, T. R., E. H. Bradley, and J. O’Leary. 2003. Prognosis communication in serious illness: Perceptions of older patients, caregivers, and clinicians. Journal of the American Geriatrics Society 51(10):1398-1403.
Fried, T. R., E. H. Bradley, and J. O’Leary. 2006. Changes in prognostic awareness among seriously ill older persons and their caregivers. Journal of Palliative Medicine 9(1):61-69.
Fried, T. R., J. O’Leary, P. Van Ness, and L. Fraenkel. 2007. Inconsistency over time in the preferences of older persons with advanced illness for life-sustaining treatment. Journal of the American Geriatrics Society 55(7):1007-1014.
Fried, T. R., C. Redding, M. Robbins, A. Palva, J. O’Leary, and L. Iannone. 2010. Stages of change for the component behaviors of advance care planning. Journal of the American Geriatrics Society 58(12):2329-2336.
Friedman, S., and D. Gilmore. 2007. Factors that impact resuscitation preferences for young people with severe developmental disabilities. Intellectual and Developmental Disabilities 45(2):90-97.
Fritch, J., S. Petronia, P. R. Helft, and A. Torke. 2013. Making decisions for hospitalized older adults: Ethical factors considered by family surrogates. Journal of Clinical Ethics 24(2):125-134.
Fromme, E. K., D. Zive, T. A. Schmidt, E. Olszewski, and S. W. Tolle. 2012. POLST registry do-not-resuscitate orders and other patient treatment preferences. Research letter. Journal of the American Medical Association 307(1):34-35.
Fromme, E. K., Zive, D., Schmidt, T. A., Cook, J. N. B., and Tolle, S. W. 2014. Association between Physician Orders for Life-Sustaining Treatment for scope of treatment and in-hospital death in Oregon. Journal of the American Geriatrics Society [epub ahead of print].
Fujimori, M., and Y. Uchitomi. 2009. Preferences of cancer patients regarding communication of bad news: A systematic literature review. Journal of Clinical Oncology 39(4):201-216.
Fujimori, M., T. Akechi, T. Morita, M. Inagaki, N. Akizuki, Y. Sakano, and Y. Uchitomi. 2007. Preferences of cancer patients regarding the disclosure of bad news. Psycho-Oncology 16:573-581.
Ganti, A. K., S. J. Lee, J. M. Vose, M. P. Devetten, R. G. Bociek, J. O. Armitage, P. J. Bierman, L. J. Maness, E. C. Reed, and F. R. Loberiza, Jr. 2007. Outcomes after hematopoietic stem-cell transplantation for hematologic malignancies in patients with or without advance care planning. Journal of Clinical Oncology 25(35):5643-5648.
Gao, W., M. I. Bennett, D. Stark, S. Murray, and I. J. Higginson. 2010. Psychological distress in cancer from survivorship to end of life care: Prevalence, associated factors and clinical implications. European Journal of Cancer 46(11):2036-2044.
Gardiner, C., M. Gott, N. Small, S. Payne, D. Seamark, S. Barnes, D. Halpin, and C. Ruse. 2009. Living with advanced chronic obstructive pulmonary disease: Patients concerns regarding death and dying. Palliative Medicine 23(8):691-697.
Garrido, M. M., E. L. Idler, H. Leventhal, and D. Carr. 2013. Pathways from religion to advance care planning: Beliefs about control over length of life and end-of-life values. The Gerontologist 53(5):801-816.
Garvie, P. A., J. He., J. Wang, L. J. D’Angelo, and M. E. Lyon. 2012. An exploratory survey of end-of-life attitudes, beliefs, and experiences of adolescents with HIV/AIDS and their families. Journal of Pain and Symptom Management 44(3):373-385.e29.
Gay, E. B., P. J. Pronovost, R. D. Bassett, and J. E. Nelson. 2009. The intensive care unit family meeting: Making it happen. Journal of Critical Care 24(4):629.e1-629.12.
Gill, C. J. 2010. No, we don’t think our doctors are out to get us: Responding to the straw man distortions of disability rights arguments against assisted suicide. Disability and Health Journal 3:31-38.
Gillick, M. R. 2010. Reversing the code status of advanced directives? Editorial. New England Journal of Medicine 362(13):1239-1240.
Gillick, M. R. 2013. The critical role of caregivers in achieving patient-centered care. Viewpoint. Journal of the American Medical Association 310(6):575-576.
Go, A. S., D. Mozaffarian, V. L. Roger, E. J. Benjamin, J. D. Berry, W. B. Borden, D. M. Bravata, S. Dai, E. S. Ford, C. S. Fox, S. Franco, H. J. Fullerton, C. Gillespie, S. M. Hailpern, J. A. Heit, V. J. Howard, M. D. Huffman, B. M. Kissela, S. J. Kittner, D. T. Lackland, J. H. Lichtman, L. D. Lisabeth, D. Magid, G. M. Marcus, A. Marelli, E. R. Mohler, C. S. Moy, M. E. Mussolino, G. Nichol, N. P. Paynter, P. J. Schreiner, P. D. Sorlie, J. Stein, T. N. Turan, S. S. Virani, N. D. Wong, D. Woo, and M. B. Turner. 2013. Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation 127:e6-e245.
Godlee, F. 2013. Partnering with patients. British Medical Journal 346:f3153.
Goodman, D. C., N. E. Morden, C.-H. Chang, E. S. Fisher, and J. E. Wennberg. 2013. Trends in cancer care near the end of life: A Dartmouth Atlas of Health Care Brief. http://www.dartmouthatlas.org/downloads/reports/Cancer_brief_090413.pdf (accessed September 6, 2013).
Gordon, H. S., R. L. Street, Jr., B. F. Sharf, P. A. Kelly, and J. Souchek. 2006. Racial differences in trust and lung cancer patients’ perceptions of physician communication. Journal of Clinical Oncology 24(6):904-909.
Gott, M., C. Gardiner, N. Small, S. Payne, D. Seamark, S. Barnes, D. Halpin, and C. Ruse. 2009. Barriers to advance care planning in chronic obstructive pulmonary disease. Palliative Medicine 23(7):642-648.
Gramling, R., S. A. Norton, S. Ladwig, M. Metzger, J. DeLuca, D. Gramling, D. Schatz, R. Epstein, T. Quill, and S. Alexander. 2013. Direct observation of prognosis communication in palliative care: A descriptive study. Journal of Pain and Symptom Management 45(2):202-212.
Greenberg, S. 2011. A profile of older Americans: 2011. http://www.aoa.gov/aoaroot/aging_statistics/Profile/2011/docs/2011profile.pdf (accessed October 4, 2013).
Gruneir, A., V. Mor, S. Weitzen, R. Truchil, J. Teno, and J. Roy. 2007. Where people die: A multilevel approach to understanding influences on site of death in America. Medical Care Research and Review 64(4):351-378.
Gundersen Health System. 2014a. Respecting choices: Advance care planning. http://www.gundersenhealth.org/respecting-choices (accessed June 1, 2014).
Gundersen Health System. 2014b. Respecting choices history/overview. http://www.gundersenhealth.org/respecting-choices/about-us/history-and-overview (accessed June 1, 2014).
Gutierrez, K. M. 2012. Advance directives in an intensive care unit: Experiences and recommendations of critical care nurses and physicians. Critical Care Nursing Quarterly 35(4):396-409.
Halpern, S. D. 2012a. Shaping end-of-life care: Behavioral economics and advance directives. Seminars in Respiratory and Critical Care Medicine 33(4):393-400.
Halpern, S. D. 2012b. Young leaders: Employing behavioral economics and decision science in crucial choices at end of life. Health Affairs 31(12):2789-2790.
Halpern, S. D., P. A. Ubel, and D. A. Asch. 2007. Harnessing the power of default options to improve health care. Sounding board. New England Journal of Medicine 357(13): 1340-1344.
Halpern, S. D., G. Loewenstein, K. G. Volpp, E. Cooney, K. Vranas, C. M. Quill, M. S. McKenzie, M. O. Harhay, N. B. Gabler, T. Silva, R. Arnold, D. C. Angus, and C. Bryce. 2013. Default options in advance directives influence how patients set goals for end-of-life care. Health Affairs 32(2):408-417.
Hammes, B. J. 2003. Update on respecting choices: Four years on. Innovations in End-of-Life Care 5(2):1-6. http://www.rpctraining.com.au/module06/mod06_toolkit/Additional%20references/Reference-4-3.pdf (accessed October 1, 2013).
Hammes, B. J., and B. L. Rooney. 1998. Death and end-of-life planning in one Midwestern community. Archives of Internal Medicine 158(4):383-390.
Hammes, B. J., J. Klevan, M. Kempf, and M. S. Williams. 2005. Pediatric advance care planning. Journal of Palliative Medicine 8(4):766-773.
Hammes, B. J., B. L. Rooney, J. D. Gundrum, S. E. Hickman, and N. Hager. 2012. The POLST program: A retrospective review of the demographics of use and outcomes in one community where advance directives are prevalent. Journal of Palliative Medicine 15(1):77-85.
Han, B., R. E. Remsburg, and T. J. Iwashyna. 2006. Differences in hospice use between black and white patients during the period 1992 through 2000. Medical Care 44(8):731-737.
Hargrave, B. 2013. New form adds some teeth to end-of-life care preferences. USA Today, August 5. http://www.usatoday.com/story/news/nation/2013/08/04/polst-paradigm-end-of-life-care-form-expanding-reach/2595889 (accessed June 2, 2014).
Heffner, J. E. 2011. Advance care planning in chronic obstructive pulmonary disease: Barriers and opportunities. Current Opinion in Pulmonary Medicine 17:103-109.
HHS (U.S. Department of Health and Human Services). 2008. Advance directives and advance care planning: Report to Congress. http://aspe.hhs.gov/daltcp/reports/2008/adcongrpt.htm (accessed August 7, 2013).
HHS. 2014. Meaningful use stage 3 final recommendations. http://www.healthit.gov/facas/sites/faca/files/HITPC_MUWG_Stage3_Recs_2014-04-01.pdf (accessed June 2, 2014).
Hickman, S. E., C. A. Nelson, A. H. Moss, B. J. Hammes, A. Terwilliger, A. Jackson, and S. W. Tolle. 2009. Use of the Physician Orders for Life-Sustaining Treatment (POLST) paradigm program in the hospice setting. Journal of Palliative Medicine 12(2):133-141.
Hickman, S. E., C. A. Nelson, N. A. Perrin, A. H. Moss, B. J. Hammes, and S. W. Tolle. 2010. A comparison of methods to communicate treatment preferences in nursing facilities: Traditional practices versus the Physician Orders for Life-Sustaining Treatment program. Journal of the American Geriatrics Society 58(7):1241-1248.
Hickman, S. E., C. A. Nelson, A. H. Moss, S. W. Tolle, N. A. Perrin, and B. J. Hammes. 2011. The consistency between treatments provided to nursing facility residents and orders on the Physician Orders for Life-Sustaining Treatment (POLST) form. Journal of the American Geriatrics Society 59(11):2091-2099.
Hinds, P. S., L. Oakes, and W. L. Furman. 2010. End-of-life decision-making in pediatric oncology. In Oxford textbook of palliative nursing, 3rd ed., edited by B. R. Ferrell and N. Coyle. New York: Oxford University Press. Pp. 1049-1063.
Hoyert, D. L., and J. Xu. 2012. Deaths: Preliminary data for 2011. National Vital Statistics Reports 61(6):1-52.
Hudson, P., K. Quinn, B. O’Hanlon, and S. Aranda. 2008. Family meeting in palliative care: Multidisciplinary clinical practice guidelines. BMC Palliative Care 7:12.
in der Schmitten, J., S. Rothärmel, C. Mellert, S. Rixen, B. J. Hammes, L. Briggs, K. Wegscheider, and G. Marckmann. 2011. A complex regional intervention to implement advance care planning in one town’s nursing homes: Protocol of a controlled inter-regional study. BMC Health Services Research 11(14):1-9. http://www.biomedcentral.com/content/pdf/1472-6963-11-14.pdf (accessed October 1, 2013).
IOM (Institute of Medicine). 1997. Approaching death: Improving care at the end of life. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: Improving the 21st century health care system. Washington, DC: National Academy Press.
IOM. 2004. Health literacy: A prescription to end confusion. Washington, DC: The National Academies Press.
Jezewski, M. A., M. A. Meeker, L. Sessanna, and D. S. Finnell. 2007. The effectiveness of interventions to increase advance directive completion rates. Journal of Aging and Health 19(3):519-536.
Johnson, K. S., K. I. Elbert-Avila, and J. A. Tulsky. 2005. The influence of spiritual beliefs and practices on the treatment preferences of African Americans: A review of the literature. Journal of the American Geriatrics Society 53(4):711-719.
Johnson, K. S., M. Kuchibhatla, and J. A. Tulsky. 2008. What explains racial differences in the use of advance directives and attitudes toward hospice care? Journal of the American Geriatrics Society 56(10):1953-1958.
Johnson, K. S., M. Kuchibhatla, and J. A. Tulsky. 2011. Racial differences in location before hospice enrollment and association with hospice length of stay. Journal of the American Geriatrics Society 59(4):732-737.
Kagawa-Singer, M., and L. J. Blackhall. 2001. Negotiating cross-cultural issues at the end of life: “You got to go where he lives.” Journal of the American Medical Association 286(23):2993-3001.
Kane, L. 2010. Exclusive ethics survey results: Doctors struggle with tougher-than-ever dilemmas. http://www.medscape.com/viewarticle/731485 (accessed September 6, 2013).
Karches, K. E., G. S. Chung, V. Arora, D. O. Meltzer, and F. A. Curlin. 2012. Religiosity, spirituality, and end-of-life planning: A single-site survey of medical inpatients. Journal of Pain and Symptom Management 44(6):843-851.
Karp, N., and E. Wood. 2003. Incapacitated and alone: Health care decision making for unbefriended older people. http://www.americanbar.org/content/dam/aba/administrative/law_aging/2003_Unbefriended_Elderly_Health_Care_Descision-Making7-11-03.authcheckdam.pdf (accessed February 10, 2014).
Kelley, A. S., N. S. Wenger, and C. A. Sarkisian. 2010. Opiniones: End of life care preferences and planning among older Latinos. Journal of the American Geriatrics Society 58(6):1109-1116.
Kelley, A. S., S. L. Ettner, S. Morrison, Q. Du, N. S. Wenger, and C. A. Sarkisian. 2011. Determinants of medical expenditures in the last 6 months of life. Annals of Internal Medicine 154(4):235-242.
Kim, M. K., and A. Alvi. 1999. Breaking the bad news of cancer: The patient’s perspective. Laryngoscope 109(7, Pt. 1):1064-1067.
Kim, S. Y. H., J. H. T.Karlawish, and E. D. Cain. 2002. Current state of research on decisionmaking competence of cognitively impaired elderly persons. American Journal of Geriatric Psychiatry 10:151-165.
King, J., L. Yourman, C. Ahalt, C. Eng, S. J. Knight, E. J. Pérez-Stable, and A. K. Smith. 2012. Quality of life in late-life disability: “I don’t feel bitter because I am in a wheelchair.” Journal of the American Geriatrics Society 60(3):569-576.
Kirchhoff, K. T., B. J. Hammes, K. A. Kehl, L. A. Briggs, and R. L. Brown. 2010. Effect of a disease-specific planning intervention on surrogate understanding of patient goals for future medical treatment. Journal of the American Geriatrics Society 58(7):1233-1240.
Kirkpatrick, J. N., C. J. Guger, M. F. Arnsdorf, and S. E. Fedson. 2007. Advance directives in the cardiac care unit. American Heart Journal 154(3):477-481.
Kirsch, I., H. Braun, K. Yamamoto, and A. Sum. 2007. America’s perfect storm: Three forces changing our nation’s future. Princeton, NJ: Educational Testing Service. https://www.ets.org/Media/Research/pdf/PICSTORM.pdf (accessed July 14, 2014).
Klugman, C. M., and R. P. Usatine. 2012. An evaluation of two online advance directive programs. American Journal of Hospice and Palliative Medicine 30(7):657-663.
Knauft, E., E. L. Nielsen, R. A. Engelberg, D. L. Patrick, and J. R. Curtis. 2005. Barriers and facilitators to end-of-life care communication for patients with COPD. Chest 127(6):2188-2196.
Ko, E., and C. S. Berkman. 2010. Role of children in end-of-life treatment planning among Korean American older adults. Journal of Social Work in End-of-Life & Palliative Care 6(3-4):164-184.
Ko, E., and J. Lee. 2013. Completion of advance directives among low-income older adults: Does race/ethnicity matter? American Journal of Hospice and Palliative Medicine 31(3): 247-253.
Kohn, N. A., and J. A. Blumenthal. 2008. Designating health care decision-makers for patients without advance directives: A psychological critique. Georgia Law Review 42:1-40.
Kressel, L. M., and G. B. Chapman. 2007. The default effect in end-of-life medical treatment preferences. Medical Decision Making 27(3):299-310.
Kressel, L. M., G. B. Chapman, and E. Leventhal. 2007. The influence of default options on the expression of end-of-life treatment preferences in advance directives. Journal of General Internal Medicine 22:1007-1010.
Kutner, M., E. Greenberg, Y. Jin, C. Paulsen, and S. White. 2006. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. Washington, DC: National Center for Education Statistics. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483 (accessed November 18, 2013).
Lakin, J. R., E. Le, M. Mourad, H. Hollander, and W. G. Anderson. 2013. Incentivizing residents to document inpatient advance care planning. Research letter. JAMA Internal Medicine 173(17):1652-1654.
Lamont, E. B., and N. A. Christakis. 2003. Complexities in prognostication in advanced cancer: “To help them live their lives the way they want to.” Journal of the American Medical Association 290(1):98-104.
Lannen, P., J. Wolfe, J. Mack, E. Onelov, U. Nyberg, and U. Kreicbergs. 2010. Absorbing information about a child’s incurable cancer. Oncology 78:259-266.
LeBlanc, T. W., and J. A. Tulsky. in press. Communication with the patient and family. In Oxford textbook of palliative medicine, 5th ed., edited by N. Cherney, M. Fallon, S. Kaasa, R. Portenoy, and D. Currow. Oxford, England: Oxford University Press.
Lepore, M. J., S. C. Miller, and P. Gozalo. 2011. Hospice use among urban black and white U.S. nursing home decedents in 2006. The Gerontologist 51(2):251-260.
Limehouse, W. E., V. R. Feeser, K. J. Bookman, and A. Derse. 2012a. A model for emergency department end-of-life communications after acute devastating events—Part I: Decisionmaking capacity, surrogates, and advance directives. Academic Emergency Medicine 19(9):1068-1072.
Limehouse, W. E., V. R. Feeser, K. J. Bookman, and A. Derse. 2012b. A model for emergency department end-of-life communications after acute devastating events—Part II: Moving from resuscitative or end-of-life palliative treatment. Academic Emergency Medicine 19(11):1300-1308.
Lindqvist, G., and L. R. Hallberg. 2010. “Feelings of guilt due to self-inflicted disease”: A grounded theory of suffering from chronic obstructive pulmonary disease (COPD). Journal of Health Psychology 15(3):456-466.
Lipkin, M. 2013. Shared decision making. Invited commentary. JAMA Internal Medicine 173(13):1204-1205.
Loewenstein, G. 2005. Hot-cold empathy gaps and medical decision making. Health Psychology 24(4):S49-S56.
Lotz, J. D., R. J. Jox, G. D. Borasio, and M. Führer. 2013. Pediatric advance care planning: A systematic review. Pediatrics 131(3):e873-e880.
Lyon, M. E., P. A. Garvie, R. McCarter, L. Briggs, J. He, and L. J. D’Angelo. 2009. Who will speak for me? Improving end-of-life decision-making for adolescents with HIV and their families. Pediatrics 123(2):e199-e206.
Lyon, M. E., S. Jacobs, L. Briggs, Y. I. Cheng, and J. Wang. 2013. Family-centered advance care planning for teens with cancer. JAMA Pediatrics 167(5):460-467.
Mack, J. W., and T. J. Smith. 2012. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. Journal of Clinical Oncology 30(22):2715-2717.
Mack, J. W., E. Paulk, K. Viswanath, and H. G. Prigerson. 2010a. Racial disparities in the outcomes of communication on medical care received near death. Archives of Internal Medicine 170(17):1533-1540.
Mack, J. W., J. C. Weeks, A. A. Wright, S. D. Block, and H. G. Prigerson. 2010b. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. Journal of Clinical Oncology 28(7):1203-1208.
Mack, J. W., A. Cronin, N. Taback, H. A. Huskamp, N. L. Keating, J. L. Malin, C. C. Earle, and J. C. Weeks. 2012. End-of-life care discussions among patients with advanced cancer: A cohort study. Annals of Internal Medicine 156(3):204-210.
Majesko, A., S. Y. Hong, L. Weissfeld, and D. B. White. 2012. Identifying family members who may struggle in the role of surrogate decision maker. Critical Care Medicine 40(8):2281-2286.
Marco, C. A., E. S. Bessman, and G. D. Kelen. 2009. Ethical issues of cardiopulmonary resuscitation: Comparison of emergency physician practices from 1995 to 2007. Academic Emergency Medicine 16(3):270-273.
Martin, D. K., E. C. Thiel, and P. A. Singer. 1999. A new model of advance care planning: Observations from people with HIV. Archives of Internal Medicine 159:86-92.
Massachusetts Department of Public Health. 2011. MOLST demonstration program: Recommendations for statewide expansion. Pilot results 2011. http://www.mass.gov/eohhs/docs/dph/quality/healthcare/molst-final-results-2011.pdf (accessed October 1, 2013).
Matlock, D. D., T. A. E. Keech, M. B. McKenzie, M. R. Bronsert, C. T. Nowels, and J. S. Kutner. 2011. Feasibility and acceptability of a decision aid designed for people facing advanced or terminal illness: A pilot randomized trial. Health Expectations 1-11.
McCusker, M., L. Ceronsky, C. Crone, H. Epstein, B. Greene, J. Halvorson, K. Kephart, E. Mallen, B. Nosan, M. Rohr, E. Rosenberg, R. Ruff, K. Schlecht, and L. Setterlund. 2013. Health care guideline: Palliative care for adults. Bloomington, MN: Institute for Clinical Systems Improvement. https://www.icsi.org/_asset/k056ab/PalliativeCare.pdf (accessed May 29, 2014).
McDonagh, J. R., T. B. Elliott, R. A. Engelberg, P. D. Treece, S. E. Shannon, G. D. Rubenfeld, D. L. Patrick, and J. R. Curtis. 2004. Family satisfaction with family conferences about end-of-life care in the intensive care unit: Increased proportion of family speech is associated with increased satisfaction. Critical Care Medicine 32(7):1484-1488.
Meyer, H. 2011. Changing the conversation in California about care near the end of life. Health Affairs 30(3):390-393.
Mirarchi, F. L., L. A. Hite, T. E. Cooney, T. M. Kisiel, and P. Henry. 2008. TRIAD I: The realistic interpretation of advanced directives. Journal of Patient Safety 4(4):235-240.
Mirarchi, F. L., S. Kalantzis, D. Hunter, E. McCracken, and T. Kisiel. 2009. TRIAD II: Do living wills have an impact on pre-hospital lifesaving care? Journal of Emergency Medicine 36(2):105-115.
Mirarchi, F. L., E. Costello, J. Puller, T. Cooney, and N. Kottkamp. 2012. TRIAD III: Nationwide assessment of living wills and do not resuscitate orders. Journal of Emergency Medicine 42(5):511-520.
Mitchell, B. L., and L. C. Mitchell. 2009. Review of the literature on cultural competence and end-of-life treatment decisions: The role of the hospitalist. Journal of the National Medical Association 101(9):920-926.
Mitchell, S. L., J. M. Teno, D. K. Kiely, M. L. Shaffer, R. N. Jones, H. G. Prigerson, L. Volicer, J. L. Givens, and M. B. Hamel. 2009. The clinical course of advanced dementia. New England Journal of Medicine 361(16):1529-1538.
Morgan, P. A., J. S. de Oliveira, S. C. Alexander, K. I. Pollak, A. S. Jeffreys, M. K. Olsen, R. M. Arnold, A. P. Abernethy, K. L. Rodriguez, and J. A. Tulsky. 2010. Comparing oncologist, nurse, and physician assistant attitudes toward discussions of negative emotions with patients. Journal of Physician Assistant Education 21(3):13-17.
Morris, D. A., K. S. Johnson, N. Ammarell, R. M. Arnold, J. A. Tulsky, and K. E. Steinhauser. 2012. What is your understanding of your illness? A communication tool to explore patients’ perspectives of living with advanced illness. Journal of General Internal Medicine 27(11):1460-1466.
Muni, S., R. A. Engelberg, P. D. Treece, D. Dotolo, and J. R. Curtis. 2011. The influence of race/ethnicity and socioeconomic status on end-of-life care in the ICU. Chest 139(5):1025-1033.
Murphy, K., A. Cooney, E. O. Shea, and D. Casey. 2009. Determinants of quality of life for older people living with a disability in the community. Journal of Advanced Nursing 65(3):606-615.
National POLST. 2012a. About the National POLST Paradigm. http://www.polst.org/about-the-national-polst-paradigm (accessed March 20, 2014).
National POLST. 2012b. FAQ. http://www.polst.org/advance-care-planning/faq (accessed June 1, 2014).
National POLST. 2012c. How does POLST work? http://www.polst.org/advance-care-planning/how-does-polst-work (accessed June 1, 2014).
National POLST. 2012d. What is POLST? http://www.polst.org/about-the-national-polstparadigm/what-is-polst (accessed June 1, 2014).
National POLST. 2012e. POLST and advance directives. http://www.polst.org/advance-care-planning/polst-and-advance-directives (accessed June 1, 2014).
National POLST. 2012f. Programs in your state. http://www.polst.org/programs-in-your-state (accessed June 1, 2014).
NCCN (National Comprehensive Cancer Network). 2013. Clinical practice guidelines in oncology—palliative care. Version 2.2013. Fort Washington, PA: NCCN.
NCOA (National Council on Aging), United Healthcare, and USA Today. 2013. The United States of aging survey. http://www.ncoa.org/improve-health/community-education/united-states-of-aging/usa-survey-2013.html (accessed August 5, 2013).
Nease, R. F., S. G. Frazee, L. Zarin, and S. B. Miller. 2013. Choice architecture is a better strategy than engaging patients to spur behavior change. Health Affairs 32(2):242-249.
Nelson, J. E., D. C. Angus, L. A. Weissfeld, K. A. Puntillo, M. Danis, D. Deal, M. M. Levy, and D. J. Cook. 2006. End-of-life care for the critically ill: A national intensive care unit survey. Critical Care Medicine 34(10):2547-2553.
NHPCO (National Hospice and Palliative Care Organization). 2013. Facts and figures: Hospice care in America. Alexandria, VA: NHPCO.
Nicholas, L. H., K. M. Langa, T. J. Iwashyna, and D. R. Weir. 2011. Regional variation in the association between advance directives and end-of-life Medicare expenditures. Journal of the American Medical Association 306(13):1447-1453.
Nienstedt, J. C., J. F. Kinney, J. M. LeVoir, J. M. Quinn, P. D. Sirba, M. J. Hoeppner, and L. A. Piché. 2013. Stewards of the gift of life. Minnesota Catholic Conference. http://www.mncc.org/wp-content/uploads/2013/01/POLSTBrochure2013-21.pdf (accessed October 3, 2013).
Nilsson, M. E., P. K. Maciejewski, B. Zhang, A. A. Wright, E. D. Trice, A. C. Muriel, R. J. Friedlander, K. M. Fasciano, S. D. Block, and H. G. Prigerson. 2009. Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer 115(2):399-409.
NNLM (National Network of Libraries of Medicine). 2013. Health literacy. http://nnlm.gov/outreach/consumer/hlthlit.html (accessed August 13, 2013).
NQF (National Quality Forum). 2006. A national framework and preferred practices for palliative and hospice care quality. http://www.qualityforum.org/Publications/2006/12/A_National_Framework_and_Preferred_Practices_for_Palliative_and_Hospice_Care_Quality.aspx (accessed August 5, 2013).
ODPHP (Office of Disease Prevention and Health Promotion). 2010. National action plan to improve health literacy. Washington, DC: HHS. http://www.health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf (accessed February 20, 2014).
Orleans, T., and E. F. Cassidy. 2011. Health and behavior. In Health care delivery in the United States, 10th ed., Ch. 7, edited by A. R. Kovner and J. R. Knickman. New York: Springer Publishing Company. Pp. 125-149.
Parker, R. M., M. S. Wolf, and I. Kirsch. 2008. Preparing for an epidemic of limited health literacy: Weathering the perfect storm. Journal of General Internal Medicine 23(8): 1273-1276.
Parks, S. M., L. Winter, A. J. Santana, B. Parker, J. J. Diamond, M. Rose, and R. E. Myers. 2011. Family factors in end-of-life decision-making: Family conflict and proxy relationship. Journal of Palliative Medicine 14(2):179-184.
Patel, K., D. J. A. Janssen, and R. J. Curtis. 2012. Advance care planning in COPD. Respirology 17(1):72-78.
Peteet, J. R., and M. J. Balboni. 2013. Spirituality and religion in oncology. CA: A Cancer Journal for Clinicians 63(4):280-289.
Pew Research Center. 2013. Views on end-of-life medical treatments. http://www.pewforum.org/2013/11/21/views-on-end-of-life-medical-treatments (accessed January 16, 2014).
Phelps, A. C., P. K. Maciejewski, M. Nilsson, T. A. Balboni, A. A. Wright, M. E. Paulk, E. Trice, D. Schrag, J. R. Peteet, S. D. Block, and H. G. Prigerson. 2009. Religious coping and use of intensive life-prolonging care near death in patients with advanced cancer. Journal of the American Medical Association 301(11):1140-1147.
Phipps, E., G. True, D. Harris, U. Chong, W. Tester, S. I. Chavin, and L. E. Braitman. 2003. Approaching the end of life: Attitudes, preferences, and behaviors of African-American and white patients and their family caregivers. Journal of Clinical Oncology 21(3):549-554.
Pollak, K. I., R. M. Arnold, A. S. Jeffreys, S. C. Alexander, M. K. Olsen, A. P. Abernethy, C. S. Skinner, K. L. Rodriguez, and J. A. Tulsky. 2007. Oncologist communication about emotion during visits with patients with advanced cancer. Journal of Clinical Oncology 25(36):5748-5752.
Prendergast, T. J. 2001. Advance care planning: Pitfalls, progress, promise. Critical Care Medicine 29(Suppl. 2):N34-N39.
President’s Council on Bioethics. 2005. Taking care: Ethical caregiving in our aging society. https://bioethicsarchive.georgetown.edu/pcbe/reports/taking_care (accessed February 10, 2014).
Puchalski, C., and B. Ferrell. 2010. Making health care whole: Integrating spirituality into patient care. West Conshohocken, PA: Templeton Press.
Ratzan, S. C., and R. M. Parker. 2000. Introduction. In National Library of Medicine current bibliographies in medicine: Health literacy, edited by C. R. Selden, M. Zorn, S. C. Ratzan, and R. M. Parker. Bethesda, MD: National Institutes of Health. Pp. v-vi. http://www.nlm.nih.gov/archive//20061214/pubs/cbm/hliteracy.pdf (accessed February 10, 2014).
Raymont, V., W. Bingley, A. Buchanan, A. S. David, P. Hayward, S. Wessely, and M. Hotopf. 2004. Prevalence of mental incapacity in medical inpatients and associated risk factors: Cross-sectional study. Lancet 364(9443):1421-1427.
Reynolds, K. S., L. C. Hanson, M. Henderson, and K. E. Steinhauser. 2008. End-of-life care in nursing home settings: Do race or age matter? Palliative and Supportive Care 6(1):21-27.
Robinson, T. M., S. C. Alexander, M. Hays, A. S. Jeffreys, M. K. Olsen, K. L. Rodriguez, K. I. Pollak, A. P. Abernethy, R. Arnold, and J. A. Tulsky. 2008. Patient-oncologist communication in advanced cancer: Predictors of patient perception of prognosis. Support Care Cancer 16(9):1049-1057.
Rodgers, M., and T. Picchi. 2013. Testimony submitted on behalf of the Catholic Health Association to the IOM Committee on Approaching Death: Addressing Key End-of-Life Issues, Washington, DC.
Russell, B. J., and A. M. Ward. 2011. Deciding what information is necessary: Do patients with advanced cancer want to know all the details. Cancer Management and Research 3:191-199.
Ryan, C. 2013. Language use in the United States: 2011. https://www.census.gov/prod/2013pubs/acs-22.pdf (accessed May 29, 2014).
Sabatino, C. P. 2010. The evolution of health care advance planning law and policy. Milbank Quarterly 88(2):211-239.
Sahm, S., R. Will, and G. Hommel. 2005. Would they follow what has been laid down? Cancer patients’ and healthy controls’ views on adherence to advance directives compared to medical staff. Medicine, Health Care and Philosophy 8:297-305.
Schellinger, S., A. Sidebottom, and L. Briggs. 2011. Disease specific advance care planning for heart failure patients: Implementation in a large health system. Journal of Palliative Medicine 14(11):1224-1230.
Schenker, Y., M. Crowley-Matoka, D. Dohan, G. A. Tiver, R. M. Arnold, and D. B. White. 2012. I don’t want to be the one saying “we should just let him die”: Intrapersonal tensions experienced by surrogate decision makers in the ICU. Journal of General Internal Medicine 27(12):1657-1665.
Schmidt, T. A., E. A. Olszewski, D. Zive, E. K. Fromme, and S. W. Tolle. 2013. The Oregon Physician Orders for Life-Sustaining Treatment registry: A preliminary study of emergency medical services utilization. Journal of Emergency Medicine 44(4):796-805.
Schubart, J. R., B. H. Levi, F. Camacho, M. Whitehead, E. Farace, and M. J. Green. 2012. Reliability of an interactive computer program for advance care planning. Journal of Palliative Medicine 15(6):637-642.
Sessums, L. L., H. Zembrzuska, and J. L. Jackson. 2011. Does this patient have medical decision-making capacity. Journal of the American Medical Association 306(4):420-427.
Shah, A. B., R. P. Morrissey, A. Baraghoush, P. Bharadwaj, A. Phan, M. Hamilton, J. Kobashigawa, and E. R. Schwarz. 2013. Failing the failing heart: A review of palliative care in heart failure. Reviews in Cardiovascular Medicine 14(1):41-48.
Shapiro, S. P. 2012. Advance directives: The elusive goal of having the last word. NAELA Journal 8(2):205-232.
Sharp, S., D. Carr, and C. Macdonald. 2012. Religion and end-of-life treatment preferences: Assessing the effects of religious denomination and beliefs. Social Forces 91(1):275-298.
Shockney, L. D., and A. Back. 2013. Communicating with patients on treatment options for advanced disease. Journal of the National Comprehensive Cancer Network 11(5.5): 684-686.
Silveira, M. J., S. Y. H. Kim, and K. M. Langa. 2010. Advance directives and outcomes of surrogate decision making before death. New England Journal of Medicine 362(13): 1211-1218.
Smith, A. K., R. B. Davis, and E. L. Krakauer. 2007. Differences in the quality of the patient-physician relationship among terminally ill African-American and white patients: Impact on advance care planning and treatment preferences. 2007. Journal of General Internal Medicine 22(11):1579-1582.
Smith, A. K., L. C. Walter, Y. Miao, W. J. Boscardin, and K. E. Covinsky. 2013a. Disability during the last two years of life. JAMA Internal Medicine 173(16):1506-1513.
Smith, A. K., D. B. White, and R. M. Arnold. 2013b. Uncertainty—the other side of prognosis. New England Journal of Medicine 368(26):2448-2450.
Song, J., E. R. Ratner, M. M. Wall, D. M. Bartels, N. Ulvestad, D. Petroskas, M. West, A. M. Weber-Main, L Grengs, and L. Gelberg. 2010. Effect of an end-of-life planning intervention on the completion of advance directives in homeless persons: A randomized trial. Annals of Internal Medicine 153(2):76-84.
Stark, M., and J. J. Fins. 2013. What’s not being shared in shared decision-making? The Hastings Center Report 43(4):13-16.
Stein, J. 2003. The ethics of advance directives: A rehabilitation perspective. American Journal of Physical Medicine & Rehabilitation 82(2):152-157.
Stein, R. A., L. Sharpe, M. L. Bell, F. M. Boyle, S. M. Dunn, and S. J. Clarke. 2013. Randomized controlled trial of a structured intervention to facilitate end-of-life decision making in patients with advanced cancer. Journal of Clinical Oncology 31(27):3403-3410.
Steinhauser, K. E., N. A. Christakis, E. C. Clipp, M. McNeilly, L. McIntyre, and J. A. Tulsky. 2000a. Factors considered important at the end of life by patients, family, physicians, and other care providers. Journal of the American Medical Association 284(19):2476-2482.
Steinhauser, K. E., E. C. Clipp, M. McNeilly, N. A. Christakis, L. McIntyre, and J. A. Tulsky. 2000b. In search of a good death: Observations of patients, families, and providers. Annals of Internal Medicine 132(10):825-832.
Steinhauser, K. E., C. I. Voils, E. C. Clipp, H. B. Bosworth, N. A. Christakis, and J. A. Tulsky. 2006. “Are you at peace?”: One item to probe spiritual concerns at the end of life. Archives of Internal Medicine 166:101-105.
Sudore, R. L., and T. R. Fried. 2010. Redefining the “planning” in advance care planning: Preparing for end-of-life decision making. Annals of Internal Medicine 153:256-261.
Sudore, R. L., D. Schillinger, S. J. Knight, and T. R. Fried. 2010. Uncertainty about advance care planning treatment preferences among diverse older adults. Journal of Health Communication 15(Suppl. 2):159-171.
Sulmasy, D. P. 2009. Spirituality, religion, and clinical care. Chest 135(6):1634-1642.
Swindell, J. S., A. L. McGuire, and S. D. Halpern. 2010. Beneficent persuasion: Techniques and ethical guidelines to improve patients’ decisions. Annals of Family Medicine 8(3):260-264.
Swindell, J. S., A. L. McGuire, and S. D. Halpern. 2011. Shaping patients’ decisions. Chest 139(2):424-429.
Tang, S. T. 2003. When death is imminent: Where terminally ill patients with cancer prefer to die and why. Cancer Nursing 26(3):245-251.
Temel, J. S., J. A. Greer, A. Muzikansky, E. R. Gallagher, S. Admane, J. A. Jackson, C. M. Dahlin, C. D. Blinderman, J. Jacobsen, W. F. Pirl, J. A. Billinbs, and T. J. Lynch. 2010. Early palliative care for patients with metastatic non-small-cell lung cancer. New England Journal of Medicine 363(8):733-742.
Teno, J. M., A. Gruneir, Z. Schwartz, A. Nanda, and T. Wetle. 2007. Association between advance directives and quality of end-of-life care: A national study. Journal of the American Geriatrics Society 55(2):189-194.
Teno, J. M., P. L. Gozalo, J. P. Bynum, N. E. Leland, S. C. Miller, N. E. Morden, T. Scupp, D. C. Goodman, and V. Mor. 2013. Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. Journal of the American Medical Association 309(5):470-477.
Toce, S., and M. A. Collins. 2003. The FOOTPRINTS model of pediatric palliative care. Journal of Palliative Medicine 6(6):989-1000.
Tompson, T. J. Benz, J. Agiesta, D. Junius, K. Nguyen, and K. Lowell. 2013. Long-term care: Perceptions, experiences, and attitudes among Americans 40 or older. http://www.apnorc.org/PDFs/Long%20Term%20Care/AP_NORC_Long%20Term%20Care%20Perception_FINAL%20REPORT.pdf (accessed August 7, 2013).
Topf, L., C. A. Robinson, and J. L. Bottorff. 2013. When a desired home death does not occur: The consequences of broken promises. Journal of Palliative Medicine 16(8):875-880.
Torke, A. M., M. Siegler, A. Abalos, R. M. Moloney, and G. C. Alexander. 2009. Physicians’ experience with surrogate decision making for hospitalized adults. Journal of General Internal Medicine 24(9):1023-1028.
Towers, B. 1978. The impact of the California Natural Death Act. Journal of Medical Ethics 4(2):96-98.
Trice, E. D., and H. G. Prigerson. 2009. Communication in end-stage cancer: Review of the literature and future research. Journal of Health Communication 14(Suppl. 1):95-108.
Tuffrey-Wijne, I., and L. McEnhill. 2008. Communication difficulties and intellectual disability in end-of-life care. International Journal of Palliative Nursing 14(4):189-194.
Tulsky, J. A., G. S. Fischer, M. R. Rose, and R. M. Arnold. 1998. Opening the black box: How do physicians communicate about advance directives? Annals of Internal Medicine 129(6):441-449.
Venneman, S. S., P. Namor-Harris, M. Perish, and M. Hamilton. 2008. “Allow natural death” versus “do not resuscitate”: Three words that can change a life. Journal of Medical Ethics 34:2-6.
Veysman, B. 2010. Shock me, tube me, line me. Health Affairs 29(2):324-326.
Vig, E. K., J. S. Taylor, H. Starks, E. K. Hopley, and K. Fryer-Edwards. 2006. Beyond substituted judgment: How surrogates navigate end-of-life decision-making. Journal of the American Geriatrics Society 54(11):1688-1693.
Vig, E. K., H. Starks, J. S. Taylor, E. K. Hopley, and K. Fryer-Edwards. 2007. Surviving surrogate decision-making: What helps and hampers the experience of making medical decisions for others. Journal of General Internal Medicine 22(9):1274-1279.
Volandes, A. E., M. Ariza, E. D. Abbo, and M. Paasche-Orlow. 2008a. Overcoming educational barriers for advance care planning in Latinos with video images. Journal of Palliative Medicine 11(5):700-706.
Volandes, A. E., M. Paasche-Orlow, M. R. Gillick, E. F. Cook, S. Shaykevich, E. D. Abbo, and L. Lehmann. 2008b. Health literacy not race predicts end-of-life care preferences. Journal of Palliative Medicine 11(5):754-762.
Volandes, A. E., G. H. Brandeis, A. D. Davis, M. K. Paasche-Orlow, M. R. Gillick, Y. Chang, E. S. Walker-Corkery, E. Mann, and S. L. Mitchell. 2012a. A randomized controlled trial of a goals-of-care video for elderly patients admitted to skilled nursing facilities. Journal of Palliative Medicine 15(7):805-811.
Volandes, A. E., T. T. Levin, S. Slovin, R. D. Carvajal, E. M. O’Reilly, M. L. Keohan, M. Theodoulou, M. Dickler, J. F. Gerecitano, M. Morris, A. S. Epstein, A. Naka-Blackstone, E. S. Walker-Corkery, Y. Chang, and A. Noy. 2012b. Augmenting advance care planning in poor prognosis cancer with a video decision aid: A pre-post study. Cancer 118(17):4331-4338.
Volandes, A. E., M. K. Paasche-Orlow, S. L. Mitchell, A. El-Jawahri, A. D. Davis, M. J. Barry, K. L. Hartshorn, V. A. Jackson, M. R. Gillick, E. S. Walker-Corkery, Y. Chang, L. López, M. Kemeny, L. Bulone, E. Mann, S. Misra, M. Peachey, E. D. Abbo, A. F. Eichler, A. S. Epstein, A. Noy, T. T. Levin, and J. S. Temel. 2013. Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. Journal of Clinical Oncology 31(3):380-386.
Wachterman, M. W., E. R. Marcantonio, R. B. Davis, R. A. Cohen, S. S. Waikar, R. S. Phillips, and E. P. McCarthy 2013. Relationship between the prognostic expectations of seriously ill patients undergoing hemodialysis and their nephrologists. JAMA Internal Medicine 173(13):1206-1214.
Wagemans, A., H. van Schrojenstein Lantman-de Valk, I Proot, J. Metsemakers, I. Tuffrey-Wijne, and L. Curfs. 2013. The factors affecting end-of-life decision-making by physicians of patients with intellectual disabilities in the Netherlands: A qualitative study. Journal of Intellectual Disability Research 57(4):380-389.
Waite, K. R., A. D. Federman, D. M. McCarthy, R. Sudore, L. M. Curtis, D. W. Baker, E. A. Wilson, R. Hasnain-Wynia, M. S. Wolf, and M. K. Paasche-Orlow. 2013. Literacy and race as risk factors for low rates of advance directives in older adults. Journal of the American Geriatrics Society 61(3):403-406.
Walling, A., K. A. Lorenz, S. M. Dy, A. Naeim, H. Sanati, S. M. Asch, and N. S. Wenger. 2008. Evidence-based recommendations for information and care planning in cancer care. Journal of Clinical Oncology 26(23):3896-3902.
Washington, H. A. 2006. Medical apartheid: The dark history of medical experimentation on black Americans from colonial times to the present. New York: Anchor Books.
Weeks, J. C., P. J. Catalano, A. Cronin, M. D. Finkelman, J. W. Mack, N. L. Keating, and D. Schrag. 2012. Patients’ expectations about effects of chemotherapy for advanced cancer. New England Journal of Medicine 367(17):1616-1625.
Welch, L. C., J. M. Teno, and V. Mor. 2005. End-of-life care in black and white: Race matters for medical care of dying patients and their families. Journal of the American Geriatrics Society 53(7):1145-1153.
Wendler, D., and A. Rid. 2011. Systematic review: The effects on surrogates of making treatment decisions for others. Annals of Internal Medicine 154(5):336-346.
Wenger, N. S., J. Citko, K. O’Malley, A. Diamant, K. Lorenz, V. Gonzalez, and D. M. Tarn. 2012. Implementation of physician orders for life sustaining treatment in nursing homes in California: Evaluation of a novel statewide dissemination mechanism. Journal of General Internal Medicine 28(1):51-57.
West, S. K., and M. Hollis. 2012. Barriers to completion of advance care directives among African Americans ages 25-84: A cross-generational study. Omega (Westport) 65(2): 125-137.
White, D. B., L. R. Evans, C. A. Bautista, J. M. Luce, and B. Lo. 2009. Are physicians’ recommendations to limit life support beneficial or burdensome? Bringing empirical data to the debate. American Journal of Respiratory and Critical Care Medicine 180:320-325.
White, D. B., S. M. Cua, R. Walk, L. Pollice, L. Weissfeld, S. Hong, C. S. Landefeld, and R. M. Arnold. 2012. Nurse-led intervention to improve surrogate decision making for patients with advanced critical illness. American Journal of Critical Care 21(6):396-409.
WHO (World Health Organization). 2014. Chronic respiratory diseases: Burden of COPD. http://www.who.int/respiratory/copd/burden/en (accessed June 2, 2014).
Wicher, C. P., and M. A. Meeker. 2012. What influences African American end-of-life preferences? Journal of Health Care for the Poor and Underserved 23(1):28-58.
Wiener, L., E. Ballard, T. Brennan, H. Battles, P. Martinez, and M. Pao. 2008. How I wish to be remembered: The use of an advance care planning document in adolescent and young adult populations. Journal of Palliative Medicine 11(10):1309-1313.
Wiener, L., S. Zadeh, H. Battles, K. Baird, E. Ballard, J. Osherow, and M. Pao. 2012. Allowing adolescents and young adults to plan their end-of-life care. Pediatrics 130(5):897-905.
Wilson, C. J., J. Newman, S. Tapper, S. Lai, P. H. Cheng, F. M. Wu, and M. Tai-Seale. 2013. Multiple locations of advance care planning documentation in an electronic health record: Are they easy to find? Journal of Palliative Medicine 16(9):1089-1094.
Winter, L., M. P. Dennis, and B. Parker. 2007. Religiosity and preferences for life-prolonging medical treatments in African-American and white elders: A mediation study. Omega 56(3):273-288.
Wolfe, J., N. Klar, H. E. Grier, J. Duncan, S. Salem-Schatz, E. J. Emanuel, and J. C. Weeks. 2000. Understanding of prognosis among parents of children who died of cancer: Impact on treatment goals and integration of palliative care. Journal of the American Medical Association 284(19):2469-2475.
Wright, A. A., B. Zhang, A. Ray, J. W. Mack, E. Trice, T. Balboni, S. L. Mitchell, V. A. Jackson, S. D. Block, P. K. Maciejewski, and H. G. Prigerson. 2008. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Journal of the American Medical Association 300(14):1665-1673.
Yennurajalingam, S., A. Noguera, H. A. Parsons, I. Torres-Vigil, E. R. Duarte, A. Palma, S. Bunge, L. L. Palmer, M. O. Delgado-Guay, and E. Bruera. 2013a. A multicenter survey of Hispanic caregiver preferences for patient decision control in the United States and Latin America. Palliative Medicine 27(7):692-698.
Yennurajalingam, S., H. A. Parsons, S., E. R. Duarte, A. Palma, S. Bunge, L. L. Palmer, M. O. Delgado-Guay, J. Allo, and E. Bruera. 2013b. Decisional control preferences of Hispanic patients with advanced cancer from the United States and Latin America. Journal of Pain and Symptom Management 46(3):376-385.
Yung, V. Y., A. M. Walling, L. Min, N. S. Wenger, and D. A. Ganz. 2010. Documentation of advance care planning for community-dwelling elders. Journal of Palliative Medicine 13(7):861-867.
Zabora, J., K. BrintzenhofeSzoc, B. Curbow, C. Hooker, and S. Piantadosi. 2001. The prevalence of psychological distress by cancer site. Psychooncology 10(1):19-28.
Zaide, G. B., R. Pekmezaris, C. N. Nouryan., T. P. Mir, C. P. Sison, T. Liberman, M. L. Lesser, L. B. Cooper, and G. P. Wolf-Klein. 2013. Ethnicity, race, and advance directives in an inpatient palliative care consultation service. Palliative and Supportive Care 11(1):5-11.
Zaleskiewicz, T., A. Gasiorowska, and P. Kesebir. 2013. Saving can save from death anxiety: Mortality salience and financial decision-making. PLoS ONE 8(11):e79407.
Zettel-Watson, L., P. H. Ditto, J. H. Danks, and W. D. Smucker. 2008. Actual and perceived gender differences in the accuracy of surrogate decisions about life-sustaining medical treatment among older spouses. Death Studies 32(3):273-290.
Zhang, B., A. A. Wright, H. A. Huskamp, M. E. Nilsson, M. L. Maciejewski, C. C. Earle, S. D. Block, P. K. Maciejewski, and H. G. Prigerson. 2009. Health care costs in the last week of life: Associations with end of life conversations. Archives of Internal Medicine 169(5):480-488.
Zheng, N. T., D. B. Mukamel, T. Caprio, S. Cai, and H. Temkin-Greener. 2011. Racial disparities in in-hospital death and hospice use among nursing home residents at the end-of-life. Medical Care 49(11):992-998.
Zier, L. S., P. D. Sottile, S. Y. Hong, L. A. Weissfeld, and D. B. White. 2012. Surrogate decision makers’ interpretation of prognostic information: A mixed-methods study. Annals of Internal Medicine 156(5):360-366.
Zilberberg, M. D., and A. F. Shorr. 2012. Economics at the end of life: Hospital and ICU perspectives. Seminars in Respiratory and Critical Care Medicine 33(4):362-369.
Zive, D. M., and T. A. Schmidt. 2012. Pathways to POLST registry development: Lessons learned. http://www.polst.org/wp-content/uploads/2012/12/POLST-Registry.pdf (accessed October 2, 2013).
ANNEX 3-1:
ADVANCE CARE PLANNING IN THE CONTEXT
OF COMMON SERIOUS CONDITIONS
For each of the four common serious conditions described in this appendix, all of which are leading causes of death in the United States, the failure to provide palliative care—important components of which are the setting of treatment goals and effective communication among patient, family, and clinicians—is a major shortcoming in the quality of care.
Heart Failure
Heart failure was the primary cause of more than 56,000 deaths in the United States in 2009 and was a contributing cause in 1 of every 9 deaths (274,000 deaths) (Go et al., 2013). About half of people who have heart failure die within 5 years of diagnosis (CDC, 2013a). The condition accounts for some 800,000 hospital admissions through the emergency department each year (Collins et al., 2013).36
Patients and families need good counseling so they understand the specific end-of-life quandaries raised by heart failure. These include the disease’s unpredictability and the considerable risk of sudden death, which heightens the need to designate a health care agent and specify the circumstances under which permanent pacemakers or defibrillators should be deactivated (Shah et al., 2013).
A comprehensive review of almost 25 years of medical literature found little evidence of discussions between health care professionals and heart failure patients regarding care preferences, disease progression, or future care options (Barclay et al., 2011). The authors note the frequent lack of agreement between doctors and patients/family members regarding whether such discussions had occurred and the information that was exchanged (see also DesHarnais et al., 200737; Kirkpatrick et al., 2007). Although some of these studies involved relatively small numbers of patients, consistent findings were that heart failure patients
- have mixed views about having these conversations, with some wanting a great deal of information and some wanting no details about their condition; and
_______________
36Heart failure hospitalizations are considered an ambulatory care–sensitive condition by the federal Agency for Healthcare Research and Quality: http://www.qualitymeasures.ahrq.gov/content.aspx?id=38562 (accessed December 16, 2014).
37The study by DesHarnais and colleagues (2007) involved 30 patients with heart failure (42 percent of the study population), as well as 41 patients with terminal cancer diagnoses.
- are most likely to want such conversations when they are unwell and in the hospital (a time when they may be least able to process information effectively).
In addition, health care professionals
- find establishing a diagnosis and prognosis for heart failure difficult, which complicates the task of explaining the condition to patients in a way that is not frightening and determining the appropriate timing for the discussion (Barclay et al., 2011);
- do not know patient preferences for pain control and place of death and the financial/religious considerations that factor into those preferences (DesHarnais et al., 2007); and
- tend to focus on immediate concerns of disease management, instead of viewing heart failure as a terminal illness (Barclay et al., 2011).
The articles reviewed by Barclay and colleagues (2011) indicate that patients value clinicians’ communication skills, although many cardiology professionals believe they lack such skills. Clinicians’ time pressures and manner and patients’ reluctance to ask questions are among the identified barriers to conversation on these issues.
A heart failure–specific advance care planning model was tested in a Midwest health system (Schellinger et al., 2011). The model used the Respecting Choices program, discussed earlier in this chapter, and included a facilitated, in-depth interview with patients and their family/health care agents. Discussion tools completed during the disease-specific advance care planning interviews were scanned into patients’ electronic health records. The study found no significant difference between patients among whom the model was used and a control group with respect to inpatient and emergency department admissions, although among patients who died, those who had completed their advance care planning were more than twice as likely to have been enrolled in hospice. The health system’s management was sufficiently encouraged by this study’s effectiveness in recruiting patients and achieving completion of advance directives to expand training in the model, improve the visibility of advance care planning information in the electronic health record, and continue implementation efforts.
Chronic Obstructive Pulmonary Disease (COPD)
COPD is the cause of significant morbidity and mortality worldwide (WHO, 2014). In the United States, it is the third leading cause of death (CDC, 2012), and accounted for 715,000 hospitalizations in 2011, ap-
proximately 65 percent of which were among adults aged 65 and older (American Lung Association, 2013). Like heart failure, COPD is a frequent cause of emergency hospitalizations, is progressive, has frightening and disabling symptoms (principally severe shortness of breath and anxiety), has an unpredictable trajectory, is associated with multiple comorbidities, and is a not infrequent cause of sudden death.
Few patients with COPD have discussed their end-of-life preferences with their physician (Heffner, 2011; Patel et al., 2012), and many do not know they have a life-limiting illness or even what that illness is (Gardiner et al., 2009). The barriers to greater advance care planning discussions resemble those for other medical conditions, with the added difficulty of multiple COPD phenotypes and multiple associated comorbid conditions that can affect the disease’s course (Heffner, 2011; Patel et al., 2012).
Patients with COPD have given physicians low marks with respect to discussing the specific issues of prognosis, what dying might be like, and spirituality and religion, while at the same time acknowledging their general communication skills (willingness to listen and address patients’ questions and concerns) (Curtis et al., 2004). Communication about care planning typically occurs in the crisis situation of an intensive care unit rather than in the primary care physician’s office, with each discipline believing the conversation is someone else’s responsibility (Gott et al., 2009).
COPD’s acute exacerbations followed by partial recovery “lull physicians into thinking [advance care planning] can wait until a future date and clouds the definition of what constitutes ‘end of life’ because points of transition are so poorly recognizable” (Heffner, 2011, p. 105). In this unpredictable disease, models for in-the-moment decision making may be more useful than discussions about future preferences based on hypothetical outcomes (Patel et al., 2012).
Mental health issues that characterize COPD (and many other chronic, progressive conditions) further complicate advance care planning discussions. The link between cigarette smoking and COPD stimulates feelings of remorse, shame, and guilt, which decrease patients’ motivation for engaging in advance care planning and suggest a need for psychological support and possible psychotherapeutic treatment (Heffner, 2011; Lindqvist and Hallberg, 2010).
Depression and anxiety are relatively common in chronic diseases, and are linked to increased health care utilization and higher disability rates. Depression also affects patients’ choices about care and “leads to social isolation and loneliness, which are also experienced by patients’ family caregivers,” who may stop encouraging them to engage in advance care planning (Heffner, 2011, p. 106).
Cancer
Most of the research on advance care planning for patients with specific diseases has been conducted among patients with cancer, which is responsible for more than 500,000 U.S. deaths per year (CDC, 2013b). “Cancer is an emotionally laden, often disruptive, and sometimes tumultuous experience for patients, families and providers” (Walling et al., 2008, p. 3896). For that reason alone, an essential aspect of good oncology care is good communication about the disease, its path, and choices for treatment (Trice and Prigerson, 2009). (See also the section of this chapter on handling emotional encounters.)
Advance care planning is recommended for patients with cancer at several specific points: at diagnosis, at any subsequent key time when goal-oriented discussions are appropriate (e.g., when invasive procedures or new chemotherapy regimens are contemplated, when neurological symptoms or brain metastases appear, or upon admission to an intensive care unit), and before an expected death (Walling et al., 2008). Guidelines from the National Comprehensive Cancer Network and the National Consensus Project for Quality Palliative Care recommend that physicians have an advance care planning discussion with any patients who have “incurable” cancer and an expected life span of less than 1 year (Bomba and Vermilyea, 2006; Dahlin, 2013; NCCN, 2013).
Treatment preferences of patients with advanced cancer often are unexpressed and undiscussed (Mack et al., 2010b), and care often reflects “the prevailing styles of treatment in the regions and health care systems where they happen to receive cancer treatment” (Goodman et al., 2013, p. 1). If these discussions occur, evidence from large studies suggests they tend to occur late in the disease trajectory, when patients already are in decline, and during acute hospital admissions, whereas they might better be accomplished during less stressful outpatient visits (Mack et al., 2012).
However, patients who have end-of-life discussions of any kind are more likely than those who do not to receive care in accordance with their wishes, especially when those discussions take place relatively early in the course of the illness (Goodman et al., 2013). Compared with patients who do not have these discussions, those who do, as well as patients who understand they are terminally ill, are more likely to receive end-of-life care consistent with their preferences (Mack et al., 2010b). Those who have end-of-life discussions also have lower rates of ventilation, resuscitation, and admission to the intensive care unit and are more likely to enroll in hospice earlier; early hospice enrollment is associated with improved patient and caregiver quality of life (Wright et al., 2008).
Despite these benefits, while some people “set limits on the amount of discomfort and treatments they will accept,” others “want all possible
treatments to prolong life, regardless of discomfort” (Byock, 2013, p. 7). Ironically, it is possible that choosing intensive or life-extending treatment in the face of advanced disease does not always increase longevity (e.g., Mack et al., 2010b). In a highly regarded randomized controlled trial of early introduction of palliative care in metastatic lung cancer,38 survival was actually longer in the patients who received palliative care and less chemotherapy (Temel et al., 2010).
The degree to which patients want to discuss end-of-life matters varies among individuals and families, over time, and in the face of changing circumstances, so that “the information preferences of a particular patient cannot be reliably predicted by demographic, cultural, or cancer-specific factors” (Russell and Ward, 2011, p. 191). Doctors are not accurate at guessing what those preferences will be; they must ask, although evidence suggests that this does not occur systematically. Mack and colleagues (2012) found that medical oncologists documented end-of-life discussions with only about one-quarter of their patients.
Dementias
Alzheimer’s disease is the sixth leading cause of death in the United States and was the direct cause of more than 83,000 deaths in 2010 (CDC, 2013b), although pneumonia or other manifestations of frailty often are listed as the cause of death for people with Alzheimer’s disease and dementia. Estimates are that nearly one-half of Americans aged 85 and older have Alzheimer’s disease (CDC, 2011). More than one-half of patients with Alzheimer’s disease (54 percent) lack decision-making capacity, and decisions about their care eventually end up being made by their health care agents or surrogates (Sessums et al., 2011).
Dementia differs from many other cognitive impairments in that the people afflicted went through a lifetime of making decisions and acquired the inability to continue doing so only with advancing age or the appearance of other chronic conditions. Thus, there presumably was a period of many years during which people with dementia would have been capable of expressing preferences for treatment.
Dementias are also different from many other conditions in that they typically are progressive. Huntington’s disease, for example, is a progressive neurodegenerative disorder for which there is no disease-altering treatment and that eventually results in institutionalization. Because of the pattern of erratic and impulsive behavior early in the disease, those afflicted often
_______________
38In the Temel et al. (2010) study, palliative care specifically included the advance care planning activities of establishing goals of care and assisting with decision making regarding treatment.
lose the support of friends or family, and patients have difficulty expressing themselves verbally. In a study involving 53 specialized nursing home residents with Huntington’s disease, one-quarter of the patients (or their representatives) requested cardiopulmonary resuscitation (Dellefield and Ferrini, 2011). By contrast, a study of 323 nursing home residents found that when health care agents understood the patient’s poor prognosis and the clinical complications typical in advanced dementia, they were much less likely to authorize burdensome interventions, such as hospitalization, emergency room visits, tube feeding, or intravenous therapy (Mitchell et al., 2009). In this study, fewer than one in three of the health care agents had been counseled by a physician about these complications; even fewer (18 percent) had received prognostic information from a physician.
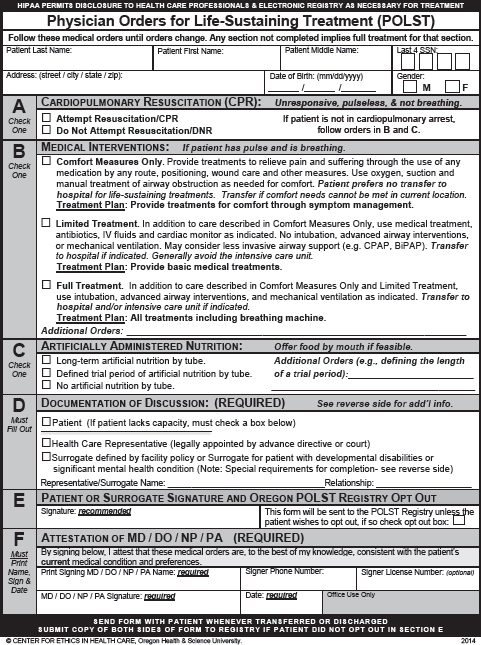
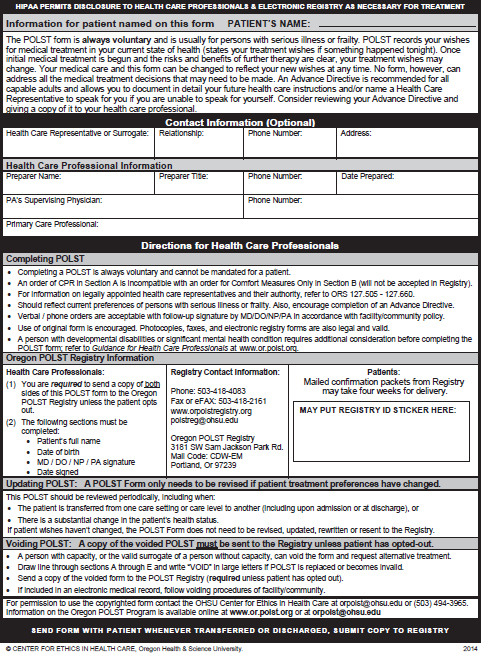
This page intentionally left blank.








































































































