Every American has a stake in improving care for people nearing the end of life. For patients and their families, that stake is immediate and personal, and no care decisions are more profound. For the millions of Americans who work with or within the health care sector—clinicians, clergy, other direct care providers, and support staff—the stake is a matter of professional commitment and responsibility. Health system managers, payers, and policy makers also have a professional stake in the provision of end-of-life care that is not only high quality but also affordable and sustainable. All Americans should be able to expect that they and their loved ones will receive the care and services they need at the end of their lives. Meanwhile, the number of Americans with some combination of aging, frailty, dependence, and multiple chronic conditions is rising, placing growing pressure on the health system at every level and on every stakeholder group.
As this report shows, the advances in medicine and health care that today help people survive advanced illnesses and serious injuries have been accompanied by several collateral effects:
- growing frustration among health care professionals at the mismatch between their training and the complex needs of the people they serve;
- a high—and escalating—financial price, which includes costs for interventions that many people near the end of life do not want and that may be unlikely to benefit them; and
- a perception among many Americans that the health care system is not designed to meet their most pressing needs and priorities, many of which involve not medical care but social services.
This study was conducted by the Institute of Medicine (IOM) Committee on Approaching Death: Addressing Key End-of-Life Issues. While opinions vary regarding many dimensions of the nation’s health care system, the committee reached the conclusion that substantially higher-quality, compassionate, yet affordable and sustainable care for people with advanced illnesses is a goal within reach. We recognize the broad agreement across many political fronts that the nation must stabilize expenditures on health care. In the end-of-life context, however, we believe that goal must be achieved in tandem with the provision of quality care that offers patients and families both compassion and choice.
This is a challenging agenda; however, this report makes clear that effective, evidence-based strategies for improving care for people nearing the end of life are already known. For the most part, money currently in the health care system can be reallocated to implement those strategies and even add some of the much-needed social supports now unavailable. In short, the committee envisions an approach to care for people near the end of life that is both high quality and compassionate; delivers value to patients, families, and the health system; and is sustainable and affordable.
Much has been written about the high costs of care in the last year of life. Persuasive arguments have been made, however, that it is misleading to look back at these expenditures and attribute them all to “the high cost of dying.” Methodologically, it is difficult to define the “end of life”—which, generally entailing acute illness, necessarily involves intense treatment—until the patient has died. People who survive these serious episodes do not appear in these calculations (Neuberg, 2009). Worse, such arguments imply that the sickest and most vulnerable people in society (some of whom will die, but many of whom will not) are somehow unworthy of investment. Moreover, costs of care in the final phase of life vary from one hospital region to another by large amounts. Yet people treated in high-cost locales live no longer than people who are equally ill but whose care costs considerably less (Dartmouth Institute for Health Policy and Clinical Practice, undated; see also Appendix E).
The key question for health care policy makers and analysts, however, should center not on costs, but on whether people nearing the end of life are receiving high-quality, effective health and supporting services and whether the mix of services available to them reflects their needs and preferences. As detailed in this report, evidence suggests a mismatch between the services most readily available to people near the end of life (acute care) and what they most often say they want (supportive services) (Gruneir et al., 2007).
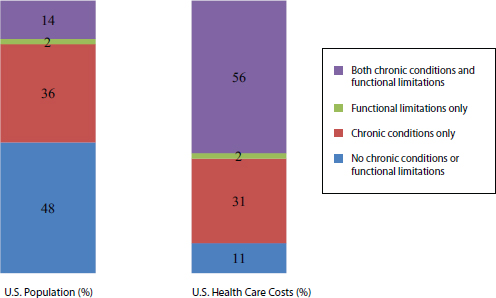
FIGURE 1-1 Population and health care costs for people with chronic conditions and functional limitations, 2010-2011.
SOURCE: Appendix E, Table E-1.
Meanwhile, a large number of Americans have chronic conditions or functional limitations—or both—which are associated with higher needs and, as a result, health care costs (see Figure 1-1). The important message of this figure is that the nearly one-half of Americans (48 percent) who have no chronic condition or functional limitation account for only 14 percent of U.S. health care costs, whereas the 14 percent of Americans who have both chronic conditions and functional limitations account for 56 percent of these costs. Two-thirds of the population with the highest health care costs (top 5 percent spenders) are under age 65 and therefore not part of the Medicare population; further, according to an analysis commissioned for this study (see Appendix E, Figure E-12), the proportion of Medicare spending in the year prior to death remained stable from 1978 to 2006 (most recent comparable data) despite rapidly rising health care costs overall.
Physicians might be assumed to be in a better position than the average nonclinician to judge the likely value of services provided near the end of life.1 It is therefore telling that when it comes to their own care, many
_______________
1“Value should always be defined around the customer, and in a well-functioning health care system, the creation of value for patients should determine the rewards for all other actors in the system. Since value depends on results, not inputs, value in health care is measured by the outcomes achieved, not the volume of services delivered” (Porter, 2010, p. 2477).
physicians choose much less aggressive treatments than they offer their patients. A 1997 study comparing 78 primary care faculty and residents with 831 of their patients found that the physicians were much less likely than the patients to want five of six specific treatments if they were terminally ill (Gramelspacher et al., 1997). Fifty-nine percent of the physicians had “least aggressive” treatment preferences, while 31 percent had “moderate” treatment preferences.
Although few scientific studies have addressed the subject, a personal essay by Kenneth Murray, M.D., suggests that doctors “don’t die like the rest of us. What’s unusual about them is not how much treatment they get compared to most Americans, but how little”2 (Murray, 2011). In a survey of some 765 physicians, most (more than 80 percent) wanted pain medications, one-quarter to one-third wanted antibiotics or intravenous (IV) hydration, and fewer than 10 percent wanted cardiopulmonary resuscitation or mechanical ventilation (Gallo et al., 2003). Likewise, a 2011 survey of some 500 board-certified U.S. physicians found that 96 percent believed “it is more important to enhance the quality of life for seriously ill patients, even if it means a shorter life,” while only 4 percent believed it is more important to extend life “through every medical intervention possible” (Regence Foundation and National Journal, 2011, p. 2).
Because people understand the world largely in terms of personal experience, families that have suffered the painful loss of a loved one tend to attribute any aspects of care that went wrong or needed improvement to factors of which they have direct knowledge—the drastic turn of the illness, the conflicting requirements of various care settings, confusion about what clinicians were telling them, the decisions they made when events felt out of control. People in these situations may not recognize that their difficulties resulted largely from systemic problems in need of fundamental solutions. Addressing such systemic factors is the aim of this report.
WHY THIS STUDY IS IMPORTANT NOW
In contemplating an addition to the considerable body of existing work on this topic, the IOM took note of a number of contextual factors that make this new study particularly timely:
_______________
2Dr. Murray is a retired clinical assistant professor of family medicine at the University of Southern California. His essay, first published in Zócalo Public Square (Murray, 2011), has been republished in The Best American Essays 2012 and widely excerpted and republished in the popular media.
- the increasing number of elderly Americans, including those with some combination of frailty, significant physical and cognitive disabilities, multiple chronic illnesses, and functional limitations;
- growing cultural diversity of the U.S. population, which makes it ever more important for clinicians to approach all patients as individuals, without assumptions about the care choices they might make;
- structural barriers in access to care that disadvantage certain population groups;
- a mismatch between the services patients and families need most and the services they can readily obtain;
- palliative care services that do not keep pace with the growing demand;
- wasteful and costly systemic problems, including perverse financial incentives, a fragmented care delivery system, time pressures that limit communication, and a lack of service coordination across programs; and
- the resulting unsustainable growth in costs of the current system over the past several decades.
To conduct this study, the IOM assembled a 21-member committee comprising experts in clinical care, aging and geriatrics, hospice and palliative care, pediatrics, consumer advocacy, spirituality, ethics, communications, clinical decision making, health care financing, law, and public policy (see Appendix G for biographical sketches of the committee members). Co-chairs of the committee were Philip A. Pizzo, M.D., former dean of the Stanford University School of Medicine, and David M. Walker, former U.S. comptroller general. The charge to the committee is presented in Box 1-1.
This study was supported by a donor that wishes to remain anonymous and whose identity was unknown to the committee. The sponsor played no role in the selection of the co-chairs or members of the committee or in the committee’s work.
The committee’s recommendations are based on both scientific evidence and expert judgment. In preparing its recommendations, the committee reviewed the most recent, powerful, and salient evidence that should reshape the U.S. approach to care near the end of life. Because so many aspects of the nation’s health care system are undergoing often dramatic changes, in part as a result of the Patient Protection and Affordable Care Act of 2010, the committee had to rely in some cases on preliminary evidence rather than definitive reports. The committee also sought to achieve a deeper understanding of the evidence through the voices and stories of people willing
BOX 1-1
Study Charge
The Institute of Medicine (IOM) will conduct a consensus study that will produce a comprehensive report on the current state of medical care for persons of all ages with a serious illness or medical condition who may be approaching death and who require coordinated care, appropriate personal communication (or communication with parents or guardians for children), and individual and family support. The committee will assess the delivery of medical care, social, and other supports to both the person approaching death and the family; person-family-provider communication of values, preferences, and beliefs; advance care planning; health care costs, financing, and reimbursement; and education of health professionals, patients, families, employers, and the public at large. The study will also explore approaches to advance the field. Specifically, the committee will:
- Review progress since the 1997 IOM report Approaching Death: Improving Care at the End of Life and the 2003 IOM report When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families. The committee will assess major subsequent events and recommendations that have been implemented as well as those that were not implemented along with remaining challenges and opportunities.
- Evaluate strategies to integrate care of those with serious illness or medical condition who may be approaching death into a person- and family-centered, team-based framework. Demographic shifts, cultural changes, fiscal realities, and the needs of vulnerable populations will be considered as will advances in technology that affect the provision of care in different settings, most notably in the home. Families are a vital component of the health care team, and the financial and other ramifications for families and society will be considered.
- Develop recommendations for changes in policy, financing mechanisms and payment practices, workforce development, research and measurement, and clinical and supportive care. These recommendations will align care with individual values, preferences, and beliefs and promote high-quality, cost-effective care for persons with serious illness or medical condition who may be approaching death, as well as with their families.
- Develop a dissemination and communication strategy to promote public engagement understanding, and action. This strategy will need to consider the fears and anxieties surrounding care for patients who may be approaching death as well as functional dependency, aging and death, and cultural diversity in values, preferences and beliefs.
to share their current, direct experiences. Thus, in addition to holding six meetings among its members, the committee received input from patients, family members, clinicians, and advocates through public workshops and additional activities and through an active Web portal to which 578 comments were submitted (see Appendix A).
In conducting this study, the committee used the definitions for basic palliative care, end-of-life care, hospice, palliative care, and specialty palliative care shown in Box 1-2. Additional definitions relevant to this study are provided in the glossary following Chapter 6. This study also was guided by the principles listed in Box 1-3.
The findings and recommendations presented in this report are intended first and foremost to address the needs of patients and families. They should also assist policy makers, clinicians in various disciplines and their educational and credentialing bodies, leaders of health care delivery and financing organizations, researchers, public and private funders, religious and community leaders, advocates for better care, journalists, and members
BOX 1-2
Key Definitions
- Basic palliative care: Palliative care that is delivered by health care professionals who are not palliative care specialists, such as primary care clinicians; physicians who are disease-oriented specialists (such as oncologists and cardiologists); and nurses, social workers, pharmacists, chaplains, and others who care for this population but are not certified in palliative care.
- End-of-life care: Refers generally to the processes of addressing the medical, social, emotional, and spiritual needs of people who are nearing the end of life. It may include a range of medical and social services, including disease-specific interventions as well as palliative and hospice care for those with advanced serious conditions who are near the end of life.
- Hospice: “A service delivery system that provides palliative care for patients who have a limited life expectancy and require comprehensive biomedical, psychosocial, and spiritual support as they enter the terminal stage of an illness or condition. It also supports family members coping with the complex consequences of illness, disability, and aging as death nears” (NQF, 2006, p. 3).
- Palliative care: Care that provides relief from pain and other symptoms, supports quality of life, and is focused on patients with serious advanced illness and their families. Palliative care may begin early in the course of treatment for a serious illness and may be delivered in a number of ways across the continuum of health care settings, including in the home, nursing homes, long-term acute care facilities, acute care hospitals, and outpatient clinics. Palliative care encompasses hospice and specialty palliative care, as well as basic palliative care.
- Specialty palliative care: Palliative care that is delivered by health care professionals who are palliative care specialists, such as physicians who are board certified in this specialty; palliative-certified nurses; and palliative care–certified social workers, pharmacists, and chaplains.
BOX 1-3
Guiding Principles for This Study
- All people with advanced illness who may be approaching the end of life are entitled to access to high-quality, compassionate, evidence-based care, consistent with their wishes, that can reasonably be expected to protect or improve the quality and length of their life. Ensuring that access and delivering that care humanely and respectfully is a central clinical and ethical obligation of health care professionals and systems.
- “All people with advanced illness” encompasses all age groups—from neonates, to children, to adolescents, to adults, to the elderly.
- “Patient-centered” and “family-oriented” care is designed to meet physical, cognitive, social, emotional, and spiritual needs, regardless of a patient’s age or infirmity; it takes into account culture, traditions, values, beliefs, and language; and it evolves with patient and family needs.
- In this report, “family” means not only people related by blood or marriage but also close friends, partners, companions, and others whom patients would want as part of their care team. As palliative care leader Ira Byock expresses it, family includes all those “for whom it matters.”*
- This report’s use of the term “vulnerable populations” goes beyond the conventional usage, which applies to people from ethnic, cultural, and racial minorities; people with low educational attainment or low health literacy; and those in prisons or having limited access to care for geographic or financial reasons. Here it includes people with serious illnesses, multiple chronic diseases, and disabilities (physical, mental, or cognitive); the frail elderly; and those without access to needed health services. In this latter sense, almost all people nearing the end of life can rightly be considered a “vulnerable population.”
- Near the end of life, clinical care is not a person’s sole priority. Patients and families may be deeply concerned with existential or spiritual issues, including bereavement, and with practical matters of coping. Appropriate support in these areas is an essential component of good care.
- The knowledge and skills that enable effective care and communication with patients and families are needed across many different health professions, among generalists as well as specialists. Honest and transparent communication about death and dying—between loved ones, between patients and clinicians, and between policy makers/media and the public—is essential to creating a truly compassionate context for high-quality end-of-life care.
- Measurement of the quality of care for the sickest and most vulnerable patients and their families is necessary to ensure access to and receipt of the highest-quality care, especially given current intense pressures to contain costs. Measurement systems should be transparent and foster accountability of services and programs.
- Innovative, well-designed biomedical, clinical, behavioral, organizational, and health policy research is needed to further improve patient-centered outcomes and ensure system sustainability.
____________
*See http://www.dyingwell.org/springer.htm (accessed December 16, 2014).
of the interested public in learning more about what constitutes good care for people nearing the end of life and the steps necessary to achieve such care for more patients and families.
In taking on this issue at this time, the committee follows in the path of many compassionate and thoughtful people, including the members of past IOM committees whose work resulted in the following reports:
- Approaching Death: Improving Care at the End of Life (IOM, 1997);
- Ensuring Quality Cancer Care (IOM, 1999);
- Improving Palliative Care for Cancer (IOM, 2001b);
- When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families (IOM, 2003);
- Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research (IOM, 2011); and
- Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis (IOM, 2013).
In addition, the IOM’s series of reports on improving the quality of care (especially Crossing the Quality Chasm [IOM, 2001a] and the work of the Roundtable on Value & Science-Driven Health Care) provide guidance and inspiration for working toward a system that provides the right care—as determined by patients and families together with their health care team—when and where it is needed at a price that is affordable and sustainable. This committee’s aim was to build on this past work and to bring compassionate and pragmatic new thinking to bear on the persistent problems affecting care for Americans living with advanced illnesses and nearing the end of life.
This committee’s charge (see Box 1-1) was to examine “medical care for persons of all ages with a serious illness or medical condition who may be approaching death.” While this may appear to be a clearly defined assignment, establishing parameters for the study was actually rather complicated. On the one hand, it was obviously infeasible for the committee to examine the entire spectrum of care for chronic illnesses from their earliest stages and manifestations or the full dimensions of frailty. This constraint imposed one limitation on the scope of the study, even though subsets of individuals with progressive chronic and debilitating conditions are highly relevant to the consideration of care in the final phase of life. On the other hand, the committee did not want to define the population of interest too narrowly or arbitrarily and thereby exclude people—or their families or
clinicians—who do not consider themselves to be “approaching death.” Further, overly narrow definitions of “who is dying” fail any pragmatic test, as the uncertainties of making prognoses amply attest.
In 1982, the Medicare Hospice Benefit set an eligibility criterion of a 6-month prognosis if the disease runs its normal course. The legislation never defined whether this meant median life expectancy or that all persons must be dead within 6 months. Given the inherent limitations of prognostication, health care providers are hard pressed to say which individual patients will live 6 months or less. If the policy that all persons who enter hospice must have illnesses that are certain to be fatal within 6 months is strictly enforced, access to hospice will be extremely limited. On the other hand, expanding hospice services to include persons who would live for years would have important financial implications. Thirty years ago, the 6-month limit might have had some, although weak, medical justification because hospices served primarily people with cancer whose disease progression could be projected fairly accurately. Today hospices serve people with many different diagnoses that follow various and often unpredictable trajectories. With good care, even people who are very ill may survive for many months or several years. The time frame for illnesses or conditions that ultimately will prove fatal is often considerably longer than 6 months and proceeds at a different pace for different individuals.
Assigning people to an “end-of-life” or “terminally ill” category—especially given prognostic uncertainty—also creates undesirable social and personal challenges. Although patients, families, and clinicians may not consider particular individuals—or themselves—to be “dying” (thus, the often preferred formulation “living with cancer” or “living with heart disease”), they still need the kinds of intense management of pain and other symptoms, psychological support, ancillary services, and family supports provided by hospice and palliative care programs. The committee believes the timing of death is a much less important consideration than whether the person is living with a set of conditions that are now causing distress or disability and thus needs services that address those problems, as determined in the context of need and not prognosis. The real challenge is to design models of quality and affordable care that fit the variable trajectories and needs of seriously ill people who are nearing the end of life and their family caregivers.
The same definitional quandary faced the authors of the 1997 IOM study Approaching Death, among many others (Hui et al., 2012). That committee, like this one, recognized that its recommendations applied to people “for whom death is imminent and those with serious, eventually fatal illnesses who may live for some time” (IOM, 1997, p. 7). That committee’s sense however, was that “those referred to as dying are often thought to be likely to die within a few days to several months,” and it
generally focused its attention on that group, rather than on people with “an incurable, terminal or fatal illness . . . whose deaths are less predictable and might not come for years” (IOM, 1997, p. 27).
The present committee’s resolution of this definitional dilemma is different in character from that of the practicing clinician, confronted with an increasing number of patients with not one but several serious and debilitating conditions that have uncertain prognoses and trajectories. For clinicians, the principle of patient-centeredness must remain paramount. Even though clinicians may be unable to predict the precise course of an individual patient’s illnesses,3 they can nevertheless demonstrate “qualities of compassion, empathy, and responsiveness to the needs, values, and expressed preferences” of the individuals and families in their care (IOM, 2001a, p. 48).
This report similarly concentrates on the population whose medical condition puts them at risk of death in some loosely defined “near future.” The committee recognizes that many of the actions and systemic changes that would improve care for people nearing the end of life would be of broad benefit to many other patient groups, especially those with advanced illnesses and the functional limitations that accompany frailty, helping them retain the highest possible degree of functioning and quality of life in their remaining lifetimes, however long they may be. Examples of the improvements the committee recommends that would affect large numbers of patients are those supporting evidence-based services, strengthened patient-clinician relationships, coordination of services, patient-centered and family-oriented care, and the free flow of information, as well as other system features considered hallmarks of high-quality care (IOM, 2001a). However, the charge to the committee did not encompass this broader patient population.
Finally, although the constellation of health challenges leading to death commonly confront people of advancing age, the committee understood the problem of end-of-life care to be relevant throughout the life cycle: infants die, most often of heritable or congenital disorders or sudden infant death syndrome; injuries are the leading cause of death for children; by adolescence and young adulthood, accidents and violence cause more than 70 percent of deaths; by age 45, cancers are the leading cause of death; and by age 65, heart disease is the leading killer (Heron, 2013). No age group is immune from death. The improvements in care and communication that would help population groups most commonly facing the end of life must, therefore, be extended to those of all ages.
_______________
3A recent review of the supportive and palliative care oncology literature found 386 articles (from either 2004 or 2009) that used the term “end of life,” but not one provided a definition (Hui et al., 2012).
While much more progress is needed to achieve the vision of an end-of-life care system characterized by high-quality care, compassion, economic value, sustainability, and affordability, the committee wishes to acknowledge and even celebrate the progress made over the past decade and a half. When the Approaching Death and When Children Die reports were published in 1997 and 2003, respectively, they contained a total of 19 recommendations. These recommendations are summarized in Appendix B, along with information on subsequent progress and remaining gaps.
A great many improvements in end-of-life care resulted from aggressive public- and private-sector efforts. Notable among these was the work of two large foundations—the Robert Wood Johnson Foundation (RWJF)4 and the Soros Foundation through its Project on Death in America (PDIA)5—which together provided millions of dollars to support professional education; research on health services delivery; the creation of models of care and their diffusion; and public engagement, media, and policy initiatives. Dozens of national and regional foundations made important contributions as well. The results of the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) galvanized many of these efforts (Connors et al., 1995). In brief, this large and rigorous multiyear project demonstrated unequivocally that the “solutions” to the problem of end-of-life care that had been promoted for years would not change clinical practice or the experiences of dying people, in part because of the powerful incentives aligned against them. New approaches were needed.
Major professional and provider organizations, advocacy organizations, and local coalitions have actively supported care improvements and public awareness. For example, in a policy statement released in November 2013, the American Public Health Association (APHA) addressed care for people near the end of life from a public health perspective, calling the burden experienced by those with advanced life-limiting conditions a “public health problem” (APHA, 2013). APHA recommended that the needs of these individuals be addressed through improvements in pain management, advance care planning, use of hospice and palliative
_______________
4RWJF’s 10-year, $170 million investment in improving end-of-life care relied on a three-part strategy: improving clinicians’ knowledge of and skills in care for the dying, encouraging institutional and policy changes that would facilitate the provision of good end-of-life care, and engaging a broad range of social institutions and leaders in creating a supportive environment for change (http://www.rwjf.org/content/dam/farm/reports/reports/2011/rwjf69582 [accessed December 16, 2014]).
5“The mission of PDIA is to understand and transform the culture and experience of dying through initiatives in research and scholarship, the arts and humanities, through innovations in provision of care, through public and professional education and through public policy” (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1282198 [accessed December 16, 2014]).
care, care coordination, health professional education and training (at both the generalist and specialty levels), and improvements to hospice and palliative care financing and policy. As another example, RWJF’s Last Acts campaign involved more than 800 partner organizations, from individual religious congregations and hospices, to the National Association for the Advancement of Colored People (NAACP), to the American Medical Association (De Milto, 2002). Thousands of individual clinicians, researchers, and community leaders worked to move the field forward. State government offices and agencies, many of them participants in the RWJF-funded Community-State Partnerships to Improve End-of-Life Care, achieved various policy advances, as did the federal government, especially through the Health Care Financing Administration (now the Centers for Medicare & Medicaid Services [CMS]), the Agency for Healthcare Research and Quality, and the National Institute of Nursing Research within the National Institutes of Health (NIH).
Several key aspects of dying in America today should be noted as context for this study.
Site of Death
“Death is not what it used to be,” the Approaching Death report observed in 1997. “In the United States, death at home in the care of family has been widely superseded by an institutional, professional, and technological process of dying” (IOM, 1997, p. 33). Although the proportion of people who die in hospitals has declined in recent years, the last few months of life are characterized by frequent hospital and intensive care stays; as noted, enrollment in hospice often occupies just the last few days of life. Among Medicare fee-for-service beneficiaries, the percentage who died in acute care hospitals declined from 33 percent in 2000 to 25 percent in 2009 (Goodman et al., 2013; Teno et al., 2013). Also in 2009, one-third of Medicare deaths occurred in private residences, 28 percent in nursing homes, and approximately 14 percent elsewhere (Teno et al., 2013).
These percentages vary from one locale to another, depending on local conditions and the availability of nonhospital services, such as nursing homes (Gruneir et al., 2007). The growing number of deaths in nursing homes—approaching 40 percent in Minnesota and Rhode Island as of 2007—is difficult to track, because many studies omit these residents. Nevertheless, the pattern of institution-based death appears to have changed to a considerable extent, in part because of the increased availability of hospice services, which help families provide appropriate care at home near
the end of life. Dying at home remains a consistent preference in population surveys and patient interviews (Teno et al., 2013).
Epidemiologic Patterns
Two and a half million Americans died in 2011, according to the most recent data from the Centers for Disease Control and Prevention (Hoyert and Xu, 2012). The nation continues to make progress on key mortality figures since the 1997 Approaching Death report was released (see Table 1-1). In general, the dramatic gains in life expectancy that began around 1900 have continued. Life expectancy was 4.8 years longer for women than for men in 2011, although the gap between the sexes has been shrinking (Hoyert and Xu, 2012). Life expectancy for whites (non-Hispanic) was 2.4 years less than that for Hispanics and 3.7 years more than that for blacks.
Table 1-2 presents information about deaths among U.S. children. Infant mortality remains a serious national public health concern: 54 of the world’s 224 countries have lower estimated 2013 infant mortality rates than the rate in the United States (CIA, 2014). Still, the U.S. rate fell 12 percent between 2005 and 2011, partly because of a decline in premature births (MacDorman et al., 2013). In general, the number of pediatric deaths due to trauma and other acute causes has declined, while the number attributable to complex chronic conditions has risen. One-third of pediatric deaths are among children with one or more complex chronic conditions. Overall, children and adolescents “live with and die from a wide array of often-rare diseases that require specialized care”; as noted earlier, many of these conditions are different from those that affect adults (see Appendix F).
The 10 leading causes of deaths in the United States are shown in Table 1-3. Heart disease and cancer together account for approximately half of the total. The leading causes vary among different population groups defined by age, race/ethnicity, and other factors.
At least seven of the causes of death listed in Table 1-3 are chronic conditions, the exceptions being unintentional injuries, influenza and
TABLE 1-1 Improvements in U.S. Life Expectancy, 1995-2011
| Indicator | 1995 | 2011 | Overall Improvement (%) |
| Average life expectancy at birth | 75.8 years | 78.7 years | 3.8 |
SOURCES: For 1995: IOM, 1997, citing Anderson et al., 1997; for 2011: Hoyert and Xu, 2012.
TABLE 1-2 Deaths Among U.S. Infants and Children, Rates and Causes, 2009-2010
| Indicator | Infants | Ages 1-4 | Ages 5-9 | Ages 10-14 |
| Number of deaths | 24,586 | 4,316 | 2,330 | 2,949 |
| Crude death rate | 614.7 per 100,000 live births | 26.5 per 100,000 | 11.5 per 100,000 | 14.3 per 100,000 |
| Leading causes of death | Prematurity and low birthweight, congenital problems, pregnancy complications, sudden infant death syndrome | Accidents (unintentional njuries), congenital problems, homicide | Accidents (unintentional injuries), cancer, congenital problems, homicide | Accidents (unintentional injuries), cancer, suicide, homicide |
SOURCE: Heron, 2013.
pneumonia, and suicide. Nonetheless, taking into account that influenza and pneumonia are most deadly among people whose health is already compromised in some way, as well as the contribution of alcohol use, depression, and other such factors to suicide and unintentional injuries (e.g., fires, falls, drownings, vehicle and pedestrian accidents), all 10 causes are linked in some way to chronic health problems.
The Changing U.S. Population
Dying in America today reflects the overall aging and growing diversity of the U.S. population, as well as the particular vulnerability of certain individuals.
Aging
An increase in the number and proportion of Americans aged 65 and older has been a dominant demographic trend since long before Medicare came into being. Three times the percentage of Americans pass their 65th birthday today as was the case in 1900, and the proportion of the population reaching age 85 is 48 times larger than a century ago (AoA, 2012). Indeed, the percentage of Americans over age 65 is on an upward trajectory from 9 percent in 1960 to a projected 20 percent in 2050 (see Table 1-4).
Greater longevity comes at a cost. With increases in life expectancy, the
TABLE 1-3 Leading Causes of Death, United States, 2010
| Cause | Percentage of Deaths |
| Heart disease | 24.2 |
| Cancer (malignant neoplasms) | 23.3 |
| Chronic lower respiratory diseases | 5.6 |
| Cerebrovascular diseases (e.g., stroke) | 5.2 |
| Unintentional injuries | 4.9 |
| Alzheimer’s disease | 3.4 |
| Diabetes mellitus | 2.8 |
| Influenza and pneumonia | 2.0 |
| Kidney diseases (e.g., nephritis) | 2.0 |
| Suicide | 1.6 |
SOURCE: Heron, 2013.
burden of serious illnesses among the nation’s Medicare-eligible (65 and older) and old-old (85 and older) populations has risen markedly. Two-thirds of people aged 65 and older suffer from serious, multiple chronic conditions (CDC, 2013). By contrast, 31 percent of those aged 45 to 64 and only 6 percent of those aged 18 to 44 were treated for two or more chronic conditions in 2009 (Machlin and Soni, 2013).
Table 1-5 shows the impact of having multiple chronic conditions on health care costs. In general, Medicare spending rises dramatically with increases in the number of chronic conditions. Beneficiaries with five or more such conditions accounted for nearly two-thirds of Medicare dollars spent in 2007 (Anderson, 2010).
In the future, the aging U.S. population is likely to experience large increases in certain diseases that are costly to treat. Without more effective methods for prevention and early treatment, conditions such as cardio-
TABLE 1-4 Growth in the U.S. Elderly Population, 1960-2050 (projection)
| Age Group | 1960 | 2000 | 2010 | 2050 (est.) |
| 65+: number | 16.6 million | 35 million | 40.3 million | 88.5 million |
| (% of total population) | (9.2) | (12.4) | (13.0) | (19.8) |
| 85+: number | 929,000 | 4.2 million | 5.5 million | 19 million |
| (% of total population) | (0.5) | (1.5) | (1.7) | (4.2) |
SOURCES: For 1960 and 2000: He et al., 2005; for 2010: Bureau of the Census, 2010; for 2050: Bureau of the Census, 2008.
TABLE 1-5 Average Medicare Expenditures per Fee-for-Service Beneficiary, by Number of Chronic Conditions, 2010
| Number of Chronic Conditions | Average Expenditure ($) |
| 0-1 | 2,025 |
| 2-3 | 5,698 |
| 4-5 | 12,174 |
| 6 or more | 32,658 |
NOTE: The 15 chronic conditions included in this analysis are high blood pressure, high cholesterol, ischemic heart disease, arthritis, diabetes, heart failure, chronic kidney disease, depression, chronic obstructive pulmonary disease, Alzheimer’s disease, atrial fibrillation, cancer, osteoporosis, asthma, and stroke.
SOURCE: CMS, 2012.
vascular disease (Pandya et al., 2013) and cancer are likely to consume an increasingly large share of health care resources because even with stable or slightly falling rates of illness, the growing number of people in the higher-risk age groups means the number of cases will grow. Thus, the number of new cases of cancer is expected to increase by 45 percent between 2010 and 2030 (IOM, 2013).
The number of Americans with Alzheimer’s disease and related dementias also is rising rapidly, expected to grow from 5.5 million in 2010 to 8.7 million in 2030 (HHS, 2013), and the prevalence of Parkinson’s disease is expected to double in the next 30 years. In 2010, the annual costs of caring for Americans with dementia, including both medical and nursing home care and unpaid care (mostly by family members), were estimated at $157-$215 billion, depending on how informal care was valued (Hurd et al., 2013); for Parkinson’s disease, the estimated direct and indirect costs totaled almost $21 billion (Kowal et al., 2013). These high costs can accumulate over a number of years of declining health, despite the tendency for the intensity of medical care to decrease among the oldest members of the population in the last year of life (see Appendix E).
Functional limitations and disabilities likewise increase with age and as death approaches (Chaudhry et al., 2013; Smith et al., 2013). One result is a growing need for nursing home and other long-term care placements. The number of Americans needing long-term care is expected to more than double, reaching 27 million, by 2050 (Senate Commission on Long-Term Care, 2013).
Living for extended periods with serious disease and disability need not be inevitable features of aging, however. Data from the National Long-Term Care Survey show that disability rates can be decreased (NIA, 2010), while
data from the Survey of Income and Program Participation show these rates stabilizing since 2000 (Kaye, 2013). In addition, evidence from the Health and Retirement Study indicate that the probability of being cognitively impaired declined from the mid-1990s up until at least 2004, and there is reason for cautious optimism that better control of stroke and heart disease will contribute to reductions in new cases of dementia as well (Rocca et al., 2011). Factors behind these improvements include not only better clinical treatment but also behavioral changes, assistive technologies, and improvements in socioeconomic status that suggest a need for a broad array of interventions—beyond health care—to reduce the burden of disability on older Americans. These improvements are masked, however, by the rapidly increasing number of older adults, which will result in increased need for services despite stable or lower disability rates.
Growing Diversity
The ethnic and cultural composition of the U.S. population is changing. Much has been said about the rapidity with which some U.S. cities and states are becoming “majority minority” places. Many clinicians today and certainly those of the future will care for people of differing ethnic, cultural, religious, and language backgrounds and literacy/health literacy levels; differing traditions and rituals around dying; differing levels of comfort with making critical decisions; differing expectations of the health care system; and differing family compositions, roles, and responsibilities. The strengths, weaknesses, and resilience of families are especially important factors, given the long-term trend to move ever more complex care to the home. Such factors can increase particular risks—in the present context, the risk of poor-quality, high-cost care in the final phase of life—for population groups, or even particular individuals.
Vulnerable Individuals
Many people are among those at heightened risk of poor-quality, high-cost end-of-life care. Beyond the demographic factors discussed above, the following individuals are particularly vulnerable:
- infants and children with congenital disorders, genetic diseases, or cancer;
- people of any age with complex chronic conditions;
- the elderly who have multiple chronic conditions, functional limitations, and frailty;
- people who have mental disorders or cognitive impairments, such as stroke, Alzheimer’s disease, or other dementias; and
- people with inadequate access to health services because of geography, immigration status, low income and lack of health insurance, incarceration, and structural features of the health care system.
Areas in which additional research is needed are cited in Chapters 2, 3, and 5. In 2013, the National Institute of Nursing Research—the lead institute within NIH for research on end-of-life care—published a summary of research trends and funding in end-of-life and palliative care for the years 1997-2010 (NINR, 2013). This summary was based on published research supported by both public and private entities. While the report notes that the scientific literature in this area has tripled since 1997 and totaled more than 3,000 publications as of 2010, it cites gaps as well.
In 1997, most research in end-of-life and palliative care was privately funded. While the amount of federal funding for such research has increased dramatically since 1997—from $4.2 million to $61.55 million in 2010—it still represents a very small proportion of the nation’s annual investment in biomedical research. Researchers who want to study end-of-life and palliative care topics face an ongoing difficulty in obtaining NIH funding. To evaluate the significance of these proposals adequately, the various NIH institutes would need approval bodies (study sections) devoted to end-of-life questions or larger numbers of people with end-of-life and palliative care expertise serving on existing study sections.
Despite considerable progress, significant problems remain in providing end-of-life care for Americans that is high quality and compassionate and preserves their choice while being affordable and sustainable. Many of these same challenges apply generally to individuals with chronic and complex medical and mental disorders and reflect the current fragmentation and limitations of the U.S. health care system—a system currently undergoing profound change.
Significant opportunities exist to improve and align financial and programmatic incentives across health and social services programs, develop incentives to implement program models that have demonstrated how to achieve better care at lower cost, better target complex care interventions and tailor resources to individual needs, and use social services to ease the burden on families and enhance quality of life. In some cases, additional research is needed, especially toward improving clinicians’ ability to identify individuals at risk of a “bad death.” In addition, greater oversight is
needed to ensure quality care, control costs, increase transparency, and ensure accountability.
A national strategy for accomplishing the needed changes in the current health care delivery system would necessarily be broad-based, taking into account features of the health care system as it is currently evolving, the way care is provided and the improvements needed, the way health care providers are trained and what they are taught to do, and the awareness and knowledge that would cause the public at large to support and advocate for these changes. Fundamental to this strategy is the need for—and difficult work of—breaking down a range of silos, for example, between “curative” and palliative care, between professional groups so as to foster interdisciplinary practice, and between traditional medical and social services. Development of a specific strategy, therefore, would require the broad engagement of multiple actors in the health care field and social and supporting services sector, as well as the organizations and institutions on which Americans rely for practical assistance, spiritual support, information, and advice as caregivers and as people with life-limiting illnesses. Designing such a complex, multipart strategy involving so many essential participants is beyond the scope of this study, particularly given that the U.S. health system is undergoing so many changes. However, the insights offered in this report regarding problems, challenges, and strengths of the system may be a foundation on which many other efforts can build. These challenges and opportunities are discussed in detail in the following chapters.
This report provides a detailed description of important aspects of the current U.S. health care system as they affect Americans nearing the end of life. As noted, the system is changing substantially at present, meaning that the following chapters, which rely heavily on published evidence and analysis, are to some extent a snapshot taken yesterday. An accurate picture of U.S. health care today has not yet developed, and what the system will be tomorrow is not clearly in focus. Nevertheless, much has been learned to date that should enable the implementation of high-quality, cost-effective care that patients and families find compassionate and supportive of their values, goals, and preferences at the end of life.
Chapter 2 describes end-of-life services as they are currently delivered, focusing especially on the role of palliative care. The importance of comprehensive advance care planning and improvements in traditional advance directives is discussed in Chapter 3. Chapter 4 examines the workforce and educational needs of health professionals who care for people nearing the
end of life. Chapter 5 reviews the policies and payment systems, particularly those of Medicare and Medicaid, that shape current patterns of care. Finally, public attitudes and beliefs about topics in end-of-life care and elements of potential public education programs are reviewed in Chapter 6.
Anderson, G. 2010. Chronic care: Making the case for ongoing care. Princeton, NJ: Robert Wood Johnson Foundation. http://www.rwjf.org/content/dam/farm/reports/reports/2010/rwjf54583 (accessed July 3, 2013).
Anderson, R. N., K. D. Kochanek, and S. L. Murphy. 1997. Report of final mortality statistics, 1995. Monthly Vital Statistics Reports 45(11):1-80.
AoA (Administration on Aging). 2012. A profile of older Americans: 2012. http://www.aoa.gov/AoAroot/Aging_Statistics/Profile/index.aspx (accessed January 4, 2014).
APHA (American Public Health Association). 2013. APHA policy #20134—Supporting public health’s role in addressing unmet needs in serious illness and at the end of life. Washington, DC: APHA. http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1450 (accessed August 5, 2014).
Bureau of the Census. 2008. Projections of the population by age and sex for the United States: 2010 to 2050. NP2008-T12. Washington, DC: Bureau of the Census.
Bureau of the Census. 2010. The older population: 2010. 2010 Census briefs. http://www.census.gov/prod/cen2010/briefs/c2010br-09.pdf (accessed July 30, 2013).
CDC (Centers for Disease Control and Prevention). 2013. The state of aging and health in America—2013. http://www.cdc.gov/aging/pdf/state-aging-health-in-america-2013.pdf (accessed November 12, 2013).
Chaudhry, S. I., T. E. Murphy, E. Gahbauer, L. S. Sussman, H. G. Allore, and T. M. Gill. 2013. Restricting symptoms in the last year of life: A prospective cohort study. JAMA Internal Medicine 173(16):1534-1540.
CIA (Central Intelligence Agency). 2014. Country comparison: Infant mortality rate. The World Factbook. https://www.cia.gov/library/publications/the-world-factbook/rankorder/2091rank.html (accessed February 6, 2014).
CMS (Centers for Medicare & Medicaid Services). 2012. Chronic conditions among Medicare beneficiaries. Baltimore, MD: CMS.
Connors, A. F., N. V. Dawson, N. A. Desbiens, W. J. Fulkerson, L. Goldman, W. A. Knaus, J. Lynn, and D. Ransohoff. 1995. A controlled trial to improve care for seriously ill hospitalized patients: The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT). Journal of the American Medical Association 274(20):1591-1598.
Dartmouth Institute for Health Policy and Clinical Practice. undated. Inpatient days per decedent during the last six months of life, by gender and level of care intensity, 2007. http://www.dartmouthatlas.org/data/topic/topic.aspx?cat=18 (accessed July 16, 2013).
De Milto, L. 2002. Assessment of Last Acts program provides recommendations for future direction: Assessing progress and opportunities for the Last Acts initiative. http://www.rwjf.org/content/dam/farm/reports/program_results_reports/2002/rwjf65521 (accessed June 23, 2014).
Gallo, J. J., J. B. Straton, M. J. Klag, L. A. Meoni, D. P. Sulmasy, N. Wang, and D. E. Ford. 2003. Life-sustaining treatments: What do physicians want and do they express their wishes to others? Journal of the American Geriatrics Society 51(7):961-969.
Goodman, D. C., E. S. Fisher, J. E. Wennberg, J. S. Skinner, S. Chasan-Taber, and K. K. Bonner. 2013. Tracking improvement in the care of chronically ill patients: A Dartmouth Atlas brief on Medicare beneficiaries near the end of life. http://www.dartmouthatlas.org/downloads/reports/EOL_brief_061213.pdf (accessed March 10, 2014).
Gramelspacher, G. P., X.-H. Zhou, M. P. Hanna, and W. M. Tierney. 1997. Preferences of physicians and their patients for end-of-life care. Journal of General Internal Medicine 12(6):346-351.
Gruneir, A., V. Mor, S. Weitzen, R. Truchil, J. Teno, and J. Roy. 2007. Where people die: A multilevel approach to understanding influences on site of death in America. Medical Care Research and Review 64(4):351-378.
He, W., M. Sengupta, V. A. Velkoff, and K. A. DeBarros. 2005. 65+ in the United States. http://www.census.gov/prod/2006pubs/p23-209.pdf (accessed July 30, 2013).
Heron, M. 2013. Deaths: Leading causes for 2010. National Vital Statistics Reports 62(6):1-97. http://www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_06.pdf (accessed February 5, 2014).
HHS (U.S. Department of Health and Human Services). 2013. National plan to address Alzheimer’s Disease—2013 update. http://aspe.hhs.gov/daltcp/napa/NatlPlan2013.shtml#intro (accessed November 12, 2013).
Hoyert, D. L., and J. Xu. 2012. Deaths: Preliminary data for 2011. National Vital Statistics Reports 61(6):1-52.
Hui, D., M. Mori, H. A. Parsons, S. H. Kim, Z. Li, S. Damani, and E. Bruera. 2012. The lack of standard definitions in the supportive and palliative oncology literature. Journal of Pain and Symptom Management 43(3):582-592.
Hurd, M. D., P. Martorell, A. Delavande, K. J. Mullen, and K. M. Langa. 2013. Monetary costs of dementia in the United States. New England Journal of Medicine 368(14):1326-1334.
IOM (Institute of Medicine). 1997. Approaching death: Improving care at the end of life. Washington, DC: National Academy Press.
IOM. 1999. Ensuring quality cancer care. Washington, DC: National Academy Press.
IOM. 2001a. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2001b. Improving palliative care for cancer. Washington, DC: National Academy Press.
IOM. 2003. When children die: Improving palliative and end-of-life care for children and their families. Washington, DC: The National Academies Press.
IOM. 2011. Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press.
IOM. 2013. Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: The National Academies Press.
Kaye, H. S. 2013. Disability rates for working-age adults and for the elderly have stabilized, but trends for each mean different results for costs. Health Affairs 32(1):127-134.
Kowal, S. L., T. M. Dall, R. Chakrabarti, M. V. Storm, and A. Jain. 2013. The current and projected economic burden of Parkinson’s disease in the United States. Movement Disorders 28(3):311-318.
MacDorman, M. F., D. L. Hoyert, and T. J. Mathews. 2013. Recent declines in infant mortality in the United States, 2005-2011. NCHS Data Brief 120. http://www.cdc.gov/nchs/data/databriefs/db120.htm (accessed February 5, 2014).
Machlin, S. R., and A. Soni. 2013. Health care expenditures for adults with multiple treated chronic conditions: Estimates from the Medicare Expenditure Panel Survey, 2009. Washington, DC: CDC. http://www.cdc.gov/pcd/issues/2013/12_0172.htm (accessed February 5, 2014).
Murray, K. 2011. How doctors die: It’s not like the rest of us, but it should be. Zocalo Public Square. http://www.zocalopublicsquare.org/2011/11/30/how-doctors-die/ideas/nexus (accessed March 1, 2014).
Neuberg, G. W. 2009. The cost of end-of-life care: A new efficiency measure falls short of AHA/ACC standards. Circulation: Cardiovascular Quality and Outcomes 2:127-133.
NIA (National Institute on Aging). 2010. Disability in older adults. Fact sheet. http://report.nih.gov/nihfactsheets/Pdfs/DisabilityinOlderAdults%28NIA%29.pdf (accessed January 4, 2014).
NINR (National Institute of Nursing Research). 2013. Building momentum: The science of end-of-life and palliative care. A review of research trends and funding, 1997-2010. http://www.ninr.nih.gov/sites/www.ninr.nih.gov/files/NINR-Building-Momentum-508.pdf (accessed March 12, 2014).
NQF (National Quality Forum). 2006. A national framework and preferred practices for palliative and hospice care quality: A consensus report. Washington, DC: NQF.
Pandya, A., T. A. Gaziano, M. C. Weinstein, and D. Cutler. 2013. More Americans living longer with cardiovascular disease will increase costs while lowering quality of life. Health Affairs 32(10):1706-1714.
Porter, M. E. 2010. What is value in health care? Perspective. New England Journal of Medicine 363(26):2477-2481.
Regence Foundation and National Journal. 2011. Living well at the end of life: A national conversation. http://syndication.nationaljournal.com/communications/NationalJournalRegenceDoctorsToplines.pdf (accessed June 23, 2014).
Rocca, W. A., R. C. Petersen, D. S. Knopman, L. E. Hebert, D. A. Evans, K. S. Hall, S. Gao, F. W. Unverzagt, K. M. Langa, E. B. Larson, and L. R. White. 2011. Trends in the incidence and prevalence of Alzheimer’s disease, dementia, and cognitive impairment in the United States. Alzheimer’s & Dementia 7(1):80-93.
Senate Commission on Long-Term Care. 2013. Report to the Congress. http://www.chhs.ca.gov/OLMDOC/Agenda%20Item%206-%20Commission%20on%20Long-Term%20Care-%20Final%20Report%209-26-13.pdf (accessed December 2, 2013).
Smith, A. K., L. C. Walter, Y. Miao, W. J. Boscardin, and K. E. Covinsky. 2013. Disability during the last two years of life. JAMA Internal Medicine 173(16):1506-1513.
Teno, J. M., P. L. Gozalo, J. P. Bynum, N. E. Leland, S. C. Miller, N. E. Morden, T. Scupp, D. C. Goodman, and V. Mor. 2013. Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. Journal of the American Medical Association 309(5):470-477.
























