Policies and Payment Systems to Support High-Quality End-of-Life Care
Financial incentives built into the programs that most often serve people with advanced serious illnesses—Medicare and Medicaid—encourage providers to render more services and more intensive services than are necessary or beneficial, and the lack of coordination among programs leads to fragmented care, with all its negative consequences. In short, the current health care system increases risks to patients and creates avoidable burdens on them and their families. Meanwhile, the practical but essential day-to-day support services, such as caregiver training, nutrition services, and medication management, that would allow people near the end of life to live in safety and comfort at home—where most prefer to be—are not easily arranged or paid for.
The U.S. health care system is in a state of rapid change. The impact of these shifting programs and incentives—and both their beneficial and unintended negative consequences—on Americans nearing the end of life should not be overlooked. Appropriate measurement and accountability structures are needed to ensure that people nearing the end of life will benefit under changing program policies. In assessing how the U.S. health care system affects Americans near the end of life, the committee focused on evidence that the current system is characterized by fragmentation and inefficiency, inadequate treatment of pain and other distressing symptoms, frequent transitions among care settings, and enormous and growing care responsibilities for families.
While the committee focused on improving the quality of care for people with serious advanced illnesses who may be approaching death, it also was attentive to the need to control spending throughout the U.S.
health care system. Likewise, most new health program proposals for the last several decades, up to and including the 2010 Patient Protection and Affordable Care Act (ACA), have tried to balance increasing access and improving the quality of care with managing costs. Indeed, decades of experience with the nation’s flagship health care programs—Medicaid for low-income Americans (including those who “spend down” their life savings to become eligible) and Medicare for those aged 65 and older and persons with disabilities—suggest that improving the quality of care can reduce costs.
For those nearing the end of life, better quality of care through a range of new delivery models has repeatedly been shown to reduce the need for frequent 911 calls, emergency department visits, and unnecessary urgent hospitalizations. Evidence suggests that palliative care, hospice, and various care models that integrate health care and social services may provide high-quality end-of-life care that can reduce the use of expensive hospital- and institution-based services, and have the potential to help stabilize and even reduce health care costs for people near the end of life. The resulting savings could be used to fund highly targeted and carefully tailored social services for both children and adults (Komisar and Feder, 2011; Unroe and Meier, 2013), improving patient care while protecting and supporting families. This chapter describes those opportunities.
The U.S. health care system is a complex mix of individual professionals, acute and long-term care facilities, dozens of ancillary services, payers, vendors, and many other components. Making a potentially cost-saving change in one area, regardless of how theoretically sound it may be, may create a response elsewhere in the system that prevents overall savings from being achieved. For that reason, piecemeal reforms will not work, and comprehensive approaches are needed.
The committee notes that many positive aspects of the nation’s current evolving health care system—the opportunities it affords for patients to choose providers and treatments, the growing number of quality initiatives, its investment in research and technology, and the commitment of large numbers of professionals and institutions to care for the frailest and sickest Americans—could be lost in draconian or ill-considered cost-containment measures, such as stinting on needed and beneficial care. For that reason, the committee focused on the system changes that would not only serve the needs of the sickest patients and their families but also, as a result of better quality, lead to more efficient, affordable, and sustainable practices. To this end, much can be learned from existing successful programs and care delivery models that could be applied more widely.
In May 2013 testimony before the House Committee on Ways and
Means Subcommittee on Health, Alice Rivlin1 began with an interesting question and arrived at an even more interesting answer:
Why reform Medicare? The main reason for reforming Medicare is not that the program is the principal driver of future federal spending increases, although it is. The main reason is not that Medicare beneficiaries could be receiving much better coordinated and more effective care, although they could. The most important reason is that Medicare is big enough to move the whole American health delivery system away from fee-for-service reimbursement, which rewards volume of services, toward new delivery structures, which reward quality and value. Medicare can lead a revolution in health care delivery that will give all Americans better health care at sustainable cost. (Rivlin, 2013)
Rivlin’s remarks highlight the two issues facing Medicare and the U.S. health sector as a whole—costs and quality. These two intertwined issues pervaded this study.
The poorer quality of care and higher costs that result from lack of service coordination, risky and repeated transitions across settings and programs, and fragmented and siloed delivery and payment systems affect large numbers of Americans, including those nearing the end of life. Although it is too early to predict the ultimate effects of the ACA, it is not too soon to start calling for accountability and transparency in care near the end of life to ensure that the goals of health care reform are realized for the most vulnerable and sickest beneficiaries.
This chapter describes systemic shortcomings in U.S. health care that hinder high-quality, compassionate, and cost-effective care for people of all ages near the end of life and their families. The chapter begins by summarizing the quality and cost challenges that must be faced in efforts to redesign policies and payment systems to support high-quality end-of-life care. It then provides background information on the most important programs responsible for financing and organizing U.S. health care and the perverse incentives in those programs that affect people near the end of life. Next, the chapter examines the gap between the services these programs pay for and what patients nearing the end of life and their families want and need. The chapter then turns to opportunities and initiatives to address the shortfalls and gaps in the current system and the concomitant need to establish greater transparency and accountability in the delivery of care near the end of life. After outlining research needs, the chapter ends with the commit-
_______________
1Alice Rivlin is Leonard D. Schaeffer chair in health economics at the Brookings Institution, a visiting professor at the Public Policy Institute of Georgetown University, and director of Brookings’ Engelberg Center for Health Care Reform. She recently served as a member of the President’s Debt Commission, was founding director of the Congressional Budget Office, served as Office of Management and Budget director, and was Federal Reserve vice-chair.
tee’s findings, conclusions, and recommendations on policies and payment systems to support high-quality end-of-life care.
Americans of any age who have a serious and potentially life-limiting medical condition—from infants with a devastating genetic disorder, to young adults brain-injured in an automobile crash, to frail older people with multiple chronic diseases—can experience a system that is structured and financed to provide costly interventions, high-tech services, and crisis and emergency care. This system is experienced by many thousands of people. What requires close examination and reform is how those resources are spent and whether they are well matched to the values, goals, wishes, and needs of patients and families. Current evidence suggests they are not.
The health care payment system in the United States is different from that in other wealthy, industrialized nations and has resulted from the nation’s unique politics and history. The U.S. system rewards the volume of medical procedures and therapies provided, and typically neither recognizes nor pays for the day-to-day, long-term services and supports—such as a companion to help with dressing, bathing, and eating—that are needed by people with advanced serious illnesses and their families (Feder et al., 2000; MedPAC, 2011; Rivlin, 2013). As noted in Chapter 2, given an informed choice, most people would prefer to have these ongoing needs met in their homes and communities. Because they often cannot, they routinely and repeatedly resort to 911 calls, emergency department visits, and hospitalizations that are neither beneficial nor wanted (Meier, 2011). This is poor-quality care, and it is extremely expensive.
People with advanced serious illnesses and multiple chronic conditions share certain needs independent of their diagnosis, stage of illness, or age. They have a high prevalence of pain and other distressing symptoms that adversely affect function and quality of life. They are at high risk of functional dependency, and the majority, like more than 60 percent of the costliest 5 percent of Medicare beneficiaries, require help from another person in meeting basic needs on a daily basis. Many suffer from cognitive impairments, such as dementia or delirium, and from other mental health problems, such as depression and anxiety—problems that require specialized attention and intervention. Meeting such needs places enormous burdens—physical, emotional, practical, and financial—on their families and especially, as discussed in Chapter 2, on family caregivers.
In this context, the committee believes a major reorientation of Medicare and Medicaid is needed to craft a system of care that is properly designed to address the central needs of nearly all Americans nearing the end
of life. This reorientation will require recognizing the root causes of high utilization of the system (such as exhausted family caregivers); designing services to address those causes (such as round-the-clock access to advice by telephone); reallocating funding away from preventable or unwanted acute/specialist/emergency care to support more appropriate services; and reducing the financial incentives that drive reliance on the riskiest, least suitable, and most costly care settings—the emergency department, the hospital, and the intensive care unit. Fundamentally, services must be tailored to the evolving needs of seriously ill individuals and families so as to provide a positive alternative to costly acute care and to help these patients remain safely at home, if that is their preference. Such tailoring of services would benefit far more people than attempting to reduce services for those in predictably imminent danger of dying.
Forty years ago, U.S. national health care expenditures totaled $75 billion, or 7.2 percent of the nation’s gross domestic product (GDP); by 1990, they totaled 10 times that amount—$724 billion—or 12.5 percent of GDP; and just 22 years later, in 2012, they totaled $2.8 trillion, or about 17.2 percent of GDP, having risen some $100 billion between 2011 and 2012 (Martin et al., 2014).2
With by far the largest budget of any department in the federal government and a program scope that “touches the lives of virtually every American” (IOM, 2009, pp. 21-23), the U.S. Department of Health and Human Services (HHS) exerts enormous influence over health care in America. That influence is exerted chiefly through Medicare and Medicaid, and the cost challenges in the Medicare and Medicaid programs are of urgent and longstanding concern to policy analysts across the political spectrum (Altman and Shactman, 2011, p. 345; Moffit and Senger, 2013; Robillard, 2013).
The National Commission on Fiscal Responsibility and Reform called federal health spending the nation’s “single largest fiscal challenge over the long run” (National Commission on Fiscal Responsibility and Reform, 2010, p. 36). Medicare and Medicaid have grown exponentially since their establishment almost 50 years ago, and their rules and structure have done much to shape care for the seriously ill and those who are dying. Financial pressure on federal health spending has several causes:
_______________
2The $2.79 trillion figure includes expenditures for personal health care ($2.36 trillion), government administration ($33 billion), net cost of health insurance ($164 billion), and government public health activities ($75 billion), as well as $160 billion in noncommercial research, structures, and equipment.
- Medicare and Medicaid are expensive. The two programs cost a combined $994 billion in 2012,3 or about 36 percent of total U.S. national health expenditures, and are projected to cost $1.125 trillion in 2014 (Cuckler et al., 2013). By consuming a large and growing portion of public spending, Medicare and Medicaid may crowd out needed investments in education, the environment, housing, infrastructure such as roads and bridges, alleviation of poverty, and other areas, which together arguably have a greater effect than medical care on population health.
- Expenditures for the two programs continue to rise and are projected to account for an increasing share of the economy. Although overall growth in U.S. health expenditures has slowed in recent years, spending on Medicare grew by almost one-third between 2007 and 2012 (from $432.8 billion to $572.5 billion) and on Medicaid by about 30 percent (from $326.2 billion to $421.2 billion) (Martin et al., 2014). Medicare trustees project that the cost of the program will grow from 3.6 percent of the nation’s GDP in 2012 to 5.6 percent in 2035 (Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds, 2013), while Medicaid expenditures are expected to more than double between 2013 and 2022, from $265 billion to $536 billion, especially with expansions in eligibility under the ACA (Elmendorf, 2013).
- The population is changing. The aging of baby boomers (those born between 1946 and 1964) and the growing number of Americans who are living longer but with substantial burdens of chronic disease put pressure on both Medicare (health services) and Medicaid (long-term care). Older people are the population group most likely to have chronic conditions leading to functional dependency, and spending on patients of all ages with chronic conditions accounts for 84 percent of health care costs (Moses et al., 2013).4
- Family caregiving has its limits. Older Americans’ reliance on family members—whose care was valued at $450 billion in 2009—to serve as caregivers may be difficult to sustain (Feinberg et al., 2011). About one-half (45 percent) of American women aged 75 and older live alone, and their children, if they have any, may be unable to leave their own jobs to take on the caregiving role (AoA, 2013). A loss of family caregiving capacity would increase demand for services paid for by both Medicare and Medicaid.
_______________
3The sum of Medicare ($572.5 billion); Medicaid, federal ($237.9 billion); and Medicaid, state and local ($183.3 billion) (Martin et al., 2014).
4The Medicare-eligible population is 14 percent of the U.S. population and 40 percent of the population incurring high health care costs (see Appendix E).
- The proportional tax base for the programs is shrinking. The ratio of elderly Americans to working-age Americans, who pay the taxes that fund Medicare and Medicaid, is shifting. In 1990, there were 21 Americans aged 65 and older for every 100 working-age Americans (Bureau of the Census, 2013); the projection for 2030 is 38 Americans 65 and older for every 100 of working age. An ever-smaller proportion of working Americans will be asked to contribute to health care for people at all income levels, including those with large incomes and substantial financial assets.5
- The pay-as-you-go system has its limits. Despite popular misconceptions, Medicare is funded by current contributions and revenues. In general, beneficiaries have not fully “paid in” during their working years for the benefits they later “take out” (Jacobson, 2013). In 2010, for example, a one-income, average-wage couple took out more than $6.00 in Medicare benefits for every $1.00 paid in (Steuerle and Quakenbush, 2012).
Analysts differ in their views on the relative importance of the various factors implicated in the rise in federal expenditures on health care:
- One recent analysis suggests that most increases in health care costs since 2000 have not been the result of population factors, such as aging or demand for services, but of high prices (especially for hospital care), the cost of drugs and medical devices, and administrative costs (Moses et al., 2013). These authors conclude that higher prices accounted for some 91 percent of the increase between 2000 and 2011. Average prices for everything from pharmaceuticals to surgeries are dramatically higher in the United States than in other countries (Klein, 2013).
- Other analyses attribute growth in health care costs to a larger mix of factors. The Bipartisan Policy Center (2012), for example, cites 13 major contributors to costs,6 emphasizing that none of them exists in isolation and that policy interventions must address multiple cost drivers.
_______________
5Although higher-income beneficiaries pay somewhat more for their Part B (physician) coverage.
6The 13 cost contributors are fee-for-service reimbursement; fragmentation in care delivery; administrative burden; population aging, rising rates of chronic disease, and comorbidities; advances in medical technology; tax treatment of health insurance; insurance benefit design; lack of transparency about cost and quality to inform consumer choice; cultural biases that influence care utilization; changing trends in market consolidation; high unit prices of medical services; the legal and regulatory environment; and the structure and supply of the health professional workforce.
- Based on a series of workshops on lowering health care costs and improving outcomes, an Institute of Medicine (IOM) committee concluded that almost 31 percent of 2009’s total health care costs could have been avoided by eliminating unnecessary services, inefficiently delivered services, excess administrative costs, prices that were too high, missed prevention opportunities, and fraud (IOM, 2010a, Box S-2).
Because of these economic realities, recommendations simply to increase total Medicare or Medicaid expenditures—say, to add new benefits for people with advanced serious illnesses without reducing costs elsewhere—are unlikely to be accepted. Conversely, proposals that demonstrably reduce costs as a result of improving the quality of care may be far better received by policy makers of all political persuasions.
U.S. health spending has grown more slowly than expected since the recent recession, a trend that has persisted. The slowdown has been attributed to a number of factors, including less new technology, greater patient cost sharing, and increased efficiency of providers (Ryu et al., 2013). If the trend continues, public-sector health care spending through 2021 will be substantially lower than projected, some analysts believe, and “bring much-needed relief throughout the economy” (Cutler and Sahni, 2013, p. 848). Others are less optimistic and believe the fundamental structural, marketplace, pricing, and demographic causes of cost growth remain unchanged (Bipartisan Policy Center, 2012).
Despite the above analyses, people in their last year of life are widely believed to be a main driver of excess health care spending. As described in the background paper prepared for this study by Aldridge and Kelley (see Appendix E), however, people in the last year of life account for just under 13 percent of total annual U.S. health care spending.7 Although the top 5 percent of health care spenders account for 60 percent of all health care costs, almost 90 percent of that costliest 5 percent are not in their last year of life. Since 1978, expenditures for Medicare beneficiaries in the last year of life—many of whom have multiple chronic conditions and dementia—have held steady at just over one-quarter of all Medicare expenditures (see Appendix E). In light of this analysis, the oft-expressed concern about “excess spending in the last year of life” distracts from the real drivers of U.S. health care expenditures overall, such as those described above, or those
_______________
7This estimate is based on 2011 Health and Retirement Study data on cost of care in the last year of life paid by Medicare, adjusted to account for costs paid by other sources (Medicaid, 10 percent; out of pocket, 18 percent; other, including private payers, 11 percent). The per person estimate that resulted was then applied to all 2011 deaths to arrive at a total. A limitation of this approach is that it excludes information on the non-Medicare population; however, the majority of costs in the last year of life are covered by Medicare.
of the Medicare program in particular. Those drivers include the system incentives described in this chapter, which not only push people toward use of the expensive acute care system as a substitute for inadequate community and social services but also, by being so costly, inhibit expansion of those services.
FINANCING AND ORGANIZATION OF END-OF-LIFE CARE
The IOM reports Approaching Death (1997) and When Children Die (2003) acknowledge the importance of the U.S. health care system in securing the care needed by dying adults and children and the “complex and often confusing organizational, financial, and regulatory arrangements that link health care professionals and institutions with each other and with governments, insurers, and other organizations” (IOM, 2003, p. 181). The present report revisits many of these entrenched problems. (Appendix B provides an overview of progress on the two previous reports’ recommendations.)
Over the past five decades, Congress has established an array of programs intended to meet the health care needs of older and low-income Americans:
- Medicare, the largest program, covers Americans aged 65 and older, people with permanent disabilities receiving Social Security Disability Income, and those with one of several specific life-threatening conditions. As noted, Medicare is federally funded by current revenue.
- Medicaid covers pregnant women, children, adults with dependent children, people with disabilities, the low-income elderly, and in some states the “medically needy”8 (KFF, 2013a). Although people commonly think of Medicaid as a program for poor children and their parents, fully 30 percent of the program’s 2011 expenditures (approximately $125 billion) was for long-term care. Medicaid is financed jointly by the federal government and the states. The federal government allows the states wide administrative latitude, which results in great variability in benefits and eligibility among states.
- The nearly 10 million Americans who receive both Medicare and Medicaid benefits are termed “dual-eligible.” A recent study of 10 years of data on the extent and causes of people “spending down”
______________
8States that have “medically needy” programs allow people whose income exceeds usual Medicaid eligibility thresholds to enroll if their income minus medical expenses meets the eligibility standard (http://www.medicare.gov/your-medicare-costs/help-paying-costs/medicaid/medicaid.html [accessed December 16, 2014]).
- their assets to become eligible for Medicaid found that almost 10 percent of the non-Medicaid population aged 50 and older became Medicaid eligible by the end of the study. Almost two-thirds of Medicaid recipients became eligible by spending down, and people who spent down had substantially lower incomes and fewer assets to begin with—a finding “inconsistent with the common assumption that . . . people who spend down are predominantly middle class” (Wiener et al., 2013, p. ES-2).
The dual-eligible population faces special challenges because the separately created and managed health and social programs under Medicare and Medicaid are not coordinated and contain perverse eligibility and coverage incentives. These financial incentives create waste and result in patients moving back and forth between care settings (and payment options) not for medical reasons, but to maximize provider reimbursements. The result is care that is both poor quality and very costly. The ACA created a new Medicare-Medicaid Coordination Office, described later in this chapter, in an attempt to address these challenges.
Table 5-1 briefly summarizes the principal programs available to meet the needs of people with serious advanced illnesses and their families. The paper by Huskamp and Stevenson in Appendix D provides additional detail, as does the series of “Payment Basics” papers available on the website of the Medicare Payment Advisory Commission (MedPAC, an independent congressional agency, http://www.medpac.gov). The detailed regulations
TABLE 5-1 Major Health and Social Programs Available to People with Serious Advanced Illnesses
| Program | Number of Americans Who Benefit | Principal Services Covereda | Program Payments (FY 2012 unless noted) |
|
Traditional Medicareb (federal) |
|||
| Medicare Part A | 49.4 million (2012) | Primarily acute inpatient hospital care (90 days per illness episode), skilled nursing facility stays, and other services | $139 billion |
| Medicare Part B | 44 million (2010) | Physician visits and other health professional services | $102 billion |
| Program | Number of Americans Who Benefit | Principal Services Covereda | Program Payments (FY 2012 unless noted) |
| Medicare Advantage Program | 14.4 million (2013) | Part A and Part B benefits managed by local and regional health plans, with other services (hospice, drug coverage) optional, often for an additional premium | $123 billion |
| Medicare Part D | 36 million (2013) | Outpatient drug expenses through prescription drug plans (deductibles and cost sharing apply, except for low-income Americans) | $54 billion |
| Medicare Hospice Benefit (under Part A) | 1.2 million (2011) | Hospice-provided services related to a terminal illness | $14 billion (2011) |
| Medicare Home Health Care (under Parts A and B) | 3.4 million (2011) | Skilled care at home: nursing; physical, occupational, or speech therapy; medical social work; home health aide services | $21 billion |
|
Medicaid (federal and state) |
|||
| Medicaid Health Insurance | 14.8 million elderly people and people with disabilities (2013) | Inpatient and outpatient hospital care, physician and other professional services, and laboratory and radiology; all states except Oklahoma cover hospice care | $272 billion (2011) |
| Long-Term Care Assistance | 4.4 million adults (2011) | Nursing home and home health care | $125 billion (2011) |
| Assistance to Medicare Beneficiaries | 9.4 million Medicare beneficiaries | Medicare premiums and cost sharing, as well as uncovered services (especially long-term care) for “dual-eligible” people | $115 billion (2011) |
| Program | Number of Americans Who Benefit | Principal Services Covereda | Program Payments (FY 2012 unless noted) |
|
U.S. Department of Veterans Affairs (VA)c |
|||
| Medical Care | 5.6 million veteran patients | Medical care, including long-term care, home care, respite care, and hospice/palliative care | $46 billion (2012) |
|
Private Insurance |
|||
| Usually through Employment-Related Plans for Employees and Retirees | 149 million nonelderly | Wide variation in coverage; almost 8 percent of hospice patients’ care is paid for by private insurance, compared with 84 percent paid for by the Medicare Hospice Benefit | $917 billion |
| Medicare Supplemental Insurance | 10.2 million | Mostly costs not covered by Medicare, such as deductibles, co-insurance, and co-payments | Information not available |
| Long-Term Care Insurance | 10 percent of the elderly | Nursing home and other long-term care services, depending on the policy | 4 percent of long-term care expenses |
NOTES:
aDoes not include some services, administration, public health, and investment.
bSome people receive benefits under more than one program.
cThe VA’s medical care category includes costs of medical services, medical administration, facility maintenance, educational support, research support, and other overhead items, but does not include costs of construction or other nonmedical support (http://www.va.gov/vetdata/Expenditures.asp [accessed December 16, 2014]).
SOURCES: MedPAC (payment basics): http://www.medpac.gov; Huskamp and Stevenson (see Appendix D); Medicare Part A and Medicaid enrollees: Kaiser Family Foundation, State Health Facts (KFF, 2014); Medicare Part B: CMS “Medicare Enrollment: National Trends” (CMS, undated-a; KFF, 2013a); Medicaid Long-Term Care Assistance: AARP Public Policy Institute (2013), KFF (2013a); Private insurance: Martin et al. (2014); Medicare Supplemental Insurance: AHIP (2013); Long-Term Care Insurance: NBER (undated).
pertaining to these programs run to thousands of pages, and many of their key features are changing as a result of the ACA. As an example, the number of enrollees in the Medicaid program will rise substantially under the act as many states extend coverage to newly eligible residents (most of whom formerly lacked health insurance).
Medicare is the chief payer of care for people aged 65 and older with advanced serious illnesses and those who elect hospice. The committee calculated that in 2009, approximately 80 percent of U.S. deaths occurred among people covered by Medicare. This share has grown since the publication of Approaching Death (IOM, 1997), when Medicare covered approximately 70 percent of deaths (IOM, 1997, p. 155).
Medicaid is the most significant payer for care of low-income children with life-limiting conditions, and it paid more than two-fifths of the nation’s total bill for nursing home and other long-term care services in 2010 (KFF, 2013a,b). Additional funding for long-term care services comes from Medicare (for post-acute care), the Social Services Block Grant, the VA, Older Americans Act programs, the U.S. Department of Housing and Urban Development, other state programs, private insurance, and out-of-pocket spending. Families pay out of pocket for many expenses incurred in the last years of life. In a study of 3,209 Medicare beneficiaries, total health care expenditures in the 5 years before death not covered by insurance plans amounted to $38,688 for individuals and $51,030 for couples in which one spouse dies. For one-quarter of the families studied, these expenditures amounted to more than total household assets (Kelley et al., 2013b). Note that high out-of-pocket costs and severe financial impacts are not limited to families with elderly decedents. Recent research has highlighted the economic hardship—including work disruptions, income loss, and increased poverty—among families of children who have advanced cancer and those who die (Bona et al., 2014; Dussel et al., 2011).
One way or another, however, Medicare and Medicaid cover the great majority of people in the last years of life, present identifiable problems, and are clearly amenable to change through federal action. Consequently, this chapter focuses on these two programs.
PERVERSE INCENTIVES AND PROGRAM MISALIGNMENT
At the system level, the financial incentives driving the volume of services delivered and leading to fragmentation in the nation’s health care system are among the most significant contributors to unnecessarily high costs (Kamal et al., 2013). According to Elhauge (2010, p. 8), “The current payment system perversely provides disincentives for any provider to invest in coordination or care that might lessen the need of patients for health care, because . . . such investments result in fewer payments for medical or
hospital services.” These perverse incentives have led to a series of disconnected, siloed service programs, each with different payment, eligibility, and benefit rules and requirements.
Rigid silos of covered services are difficult for program managers, health care facilities, clinicians, and families to overcome when trying to meet the needs of a particular patient. In fact, one of the most burdensome problems patients and family caregivers face is the lack of coordination and communication among different components of the health care system. Not knowing whom to call or who is in charge of a patient’s care is deeply frustrating and adds unnecessary stress to already difficult situations (National Direct Service Workforce Resource Center, 2011). Default reliance on the emergency care system and on 911 calls adds risk of harm, burden, and cost. Table 5-2 summarizes how the financial incentives of public programs affect people with serious advanced illnesses.
Absent incentives and mechanisms for true integration across program eligibility, benefits, and financing, it will be impossible to achieve an effectively functioning continuum of care for people with advanced serious illnesses. This situation is in sharp contrast to the IOM’s “new rules to redesign and improve care,” which emphasize customization based on patient needs, with the patient, not the health system, as the source of control (IOM, 2001, pp. 61-62). Technical, political, and attitudinal barriers must be overcome to integrate funding streams and end cost shifting among programs. Whether recent health care reforms will be able to sufficiently realign current incentives remains to be seen.
Payer Policies and Costs of Care
Since Medicare’s inception nearly half a century ago, doctors and hospitals have been reimbursed for the care they provide on the basis of fees for services performed. (Figure 5-1 shows a breakdown of Medicare benefit payments by type of service for 2012.) Fee-for-service payments reward the volume, not the quality, of services delivered. They remain the dominant financing model in U.S. health care despite a rising proportion of Americans in capitated health plans, including Medicare managed care (Medicare Advantage), and the growing number of salaried physicians (Kane and Emmons, 2013).
Generous fee-for-service payments give physicians incentives to—even in the final weeks of life—provide high-intensity, high-cost services, consult multiple subspecialties, order tests and procedures, and hospitalize patients. And because referring patients to hospice reduces the income of some other providers, the fee-for-service system discourages timely referrals to hospice. A study of more than 286,000 randomly selected fee-for-service Medicare beneficiaries who died in 2009 found that although 42 percent
TABLE 5-2 How Financial Incentives in Public Programs Affect People with Serious Advanced Illnesses
| Program | General Payment Approach | Financial Incentives | Effects on People with Serious Advanced Illnesses |
| Medicare Part A (hospitals) | Fee-for-service, based on patient’s diagnosis and hospital’s cost experience | (1) Higher payments for more intensive services are an incentive to provide services and procedures; (2) fixed, diagnosis-based payments for an inpatient stay encourage early discharge, often to a skilled nursing facility | (1) May encourage overuse of services, even when nonbeneficial; (2) frail, very sick people experience multiple transfers from one care setting to another and increased rehospitalization rates |
| Medicare Part A (skilled nursing facilities) | Payment of a fixed per diem based on the seriousness of a resident’s condition | Patients cannot receive both skilled nursing and hospice care for the same condition; basing payment on patient acuity in theory encourages providers to capture the entirety of patients’ needs (although quality concerns remain) | 30 percent of Medicare beneficiaries receive “rehabilitative” care in a skilled nursing facility in the last 6 months of life, almost always after a hospital discharge |
| Medicare Part A (Medicare Hospice Benefit) | For 97 percent of days, hospices receive an all-inclusive per diem payment, not adjusted for case mix or setting or for outlier cases | (1) The hospice benefit is limited to people who have an expected prognosis of 6 months or less if the disease runs the expected course and who agree to forgo curative treatment for the terminal condition; (2) the program was designed mainly for care in the home (where room and board are not an issue) and does not take into account variable needs over time | (1) Survival is difficult to predict, and the limit creates “an artificial distinction between potentially life-prolonging and palliative therapies” (see Appendix D) as well as a psychological barrier to accepting hospice care; (2) if care is too complex for the home, transfer to a hospital and discharge to skilled nursing may appear to be the best option unless patients also have Medicaid (which pays for nursing homes) |
| Program | General Payment Approach | Financial Incentives | Effects on People with Serious Advanced Illnesses |
| Medicare Part B (physicians) | Fee-for-service | Encourages clinicians to provide more services and treatments | Excessive, high-intensity, and burdensome care that may not be wanted is provided in the last months and weeks of life |
| Medicare Part C (Medicare Advantage) | Capitation | (1) Plans are rewarded for efforts to manage chronic diseases effectively; (2) when patients enroll in hospice, they revert to fee-for-service Medicare | (1) Unnecessary and unwanted treatments, services, and hospitalizations may be reduced; (2) plans may be encouraged to promote hospice enrollment among high-need, high-cost patients |
| Medicare Part D (drugs) | Administered prices | Prescription drug costs are controlled | Less expensive products, often generic forms, are used when available |
| Medicaid Long-Term and Nursing Home Care | Acuity score assigned to each resident | (1) The acuity score method reduces incentives to avoid people with costly conditions; (2) Medicaid’s lower reimbursement for nursing home care is an incentive to hospitalize dual-eligible residents and return them to the facility under the higher-paying Medicare skilled nursing benefit | (1) Unknown (2) Individuals discharged from the hospital back to the nursing home under the skilled nursing benefit cannot receive hospice care concurrently for the same condition; a 2011 analysis suggested one-quarter of the hospitalizations for dual-eligible beneficiaries in the year studied (2005) were preventable, being due largely to the financial incentives for nursing homes to make these transfers (Segal, 2011) |
| Program | General Payment Approach | Financial Incentives | Effects on People with Serious Advanced Illnesses |
| Medicaid Home Health | For people eligible for nursing facility services; benefits vary | Intended to prevent excessively long periods of nursing home care | Unknown |
| Administration for Community Living (ACL) | $1.34 billion budget in 2013 for programs addressing health and independence, caregiver support, and Medicare improvements | Examples include elder rights services, the Alzheimer’s Disease Supportive Services Program, long-term care information, a family caregiver support program, nutrition services, and some support services | ACL’s goal is to increase access to community supports for older Americans and people with disabilities; it administers programs authorized under the Older Americans Act and Developmental Disabilities Assistance and Bill of Rights Act |
SOURCES: Appendix D; effects of skilled nursing facility benefit: Aragon et al. (2012), Segal (2011); ACL: http://www.acl.gov/About_ACL/Organization/Index.aspx (accessed December 16, 2014).
were enrolled in hospice at the time of their death, fully 28 percent were under hospice care for 3 days or less. More than 40 percent of late enrollments in hospice were preceded by an intensive care unit stay (Teno et al., 2013). The authors further compared these 2009 rates with patterns of care for similar numbers of Medicare beneficiaries in 2000 and 2005. Over the decade, the tendency to provide hospital and intensive care near the end of life appeared to be increasing.
Both liberals and conservatives find fault with the fee-for-service payment system (Capretta, 2013). The National Commission on Physician Payment Reform, established by the Society of General Internal Medicine in 2012, concluded that fee-for-service reimbursement is the most important cause of high health care costs and expenditures. The first of the commission’s 12 recommendations says, “Over time, payers should largely eliminate stand-alone fee-for-service payment to medical practices because of its inherent inefficiencies and problematic financial incentives” (Schroeder and Frist, 2013, p. 2029).
Nevertheless, fee-for-service is expected to remain a continuing and significant payment approach for many years to come (Wilensky, 2014). While Medicare and other payers will reimburse accountable care organizations (ACOs) established under the ACA through a graduated capitation
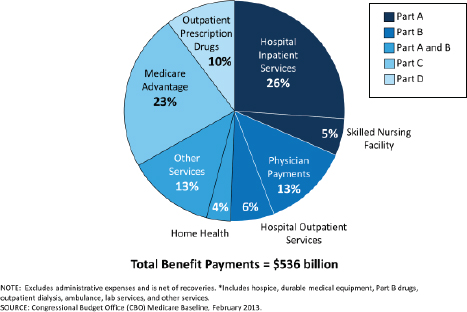
FIGURE 5-1 Medicare benefit payments by type of service, 2012.
SOURCE: KFF, 2012. Reprinted with permission from The Henry J. Kaiser Family Foundation.
approach, ACOs in turn will use fee-for-service methods to pay many physicians. The act therefore includes provisions to improve the fee-for-service system, revising the physician fee schedule and better reflecting the relative value of resources expended (Ginsburg, 2012).
The Hospital Environment
Hospital Care
As noted in Approaching Death (IOM, 1997, p. 96), “curing disease and prolonging life are the central missions of [hospitals]. Hospital culture often regards death as a failure.” While hospital and intensive care undoubtedly saves the lives of a great many otherwise healthy people, it is not necessarily useful—and is, to the contrary, harmful—for people with advanced and irreversible chronic illnesses. Yet it is hospital care, not community- or home-based care, that consumes the largest share of Medicare spending for patients in the final phase of life: fully 82 percent of all 2006 Medicare spending during the last 3 months of life was for hospital
care, despite the known risks and costs of such care and despite widespread patient preferences, noted in earlier chapters of this report, for less intensive and more home-based services (Lakdawalla et al., 2011).
The transitions between care sites—from hospital to home or nursing home and back again—encouraged, as discussed earlier in this chapter, by the current payment system, put patients at risk (Davis et al., 2012). Resulting higher rates of infection, medical errors, delirium, and falls are collectively captured by the term “burdensome transitions” (see Chapter 2), and they are increasingly common near the end of life. Earlier death may also result from these transitions. The average (mean) number of transitions from one site of care to another in the last 90 days of life increased from 2.1 per decedent in 2000 to 3.1 in 2009, and more than 14 percent of these took place in the last 3 days of life (Teno et al., 2013). This high rate of transitions between care settings is costly and inconsistent with high-quality care.
Emergency Services
When emergency medical services (EMS) providers respond to a 911 call for a Medicare patient, they are required under current Centers for Medicare & Medicaid Services (CMS) policies (generally followed by private insurers as well) to transport the patient to a hospital as a condition for being paid for their response. As a result, patients who might better be served by a palliative care home visit or a trip to a primary care clinician, if such services were available, end up being treated in an emergency department (Alpert et al., 2013).9 Pain and other unmanaged symptoms prompt many of these visits.
Fifty percent of older Americans visit the emergency department in their last month of life, and 75 percent do so in the last 6 months of life; in 77 percent of cases, the visit results in hospitalization (Smith et al., 2012). Approximately 1.1 million EMS transports are covered by Medicare annually, at a cost of some $1.3 billion.
Unnecessary and burdensome EMS transports represent poor-quality care for people with advanced serious illnesses. When they present at the emergency department, they may be admitted to inpatient care because of an unclear diagnosis; the severity of symptom distress; caregiver concerns; and, most important, a lack of prior clarification of achievable goals for care. Emergency departments are experiencing a growing number of visits by elderly patients whose mix of serious medical conditions, cognitive impairments, functional dependencies, complex medication regimens, and
_______________
9Recent growth in hospital admissions has been attributed entirely to emergency department admissions, which increased by 2.7 million between 2003 and 2009 (Kellermann et al., 2013).
caregiver exhaustion make high-quality emergency care extremely difficult (Hwang et al., 2013).
Many terminally ill patients return to the emergency department because they have not been informed and do not know that they are dying or that there are no effective treatments for their underlying disease (Mitchell et al., 2009). They may be unaware of care alternatives, such as physician house calls, community-based palliative care, or hospice. If EMS providers had more options available to them—other than not being paid—when they respond to overwhelmed caregivers who have panicked and called 911, emergency transfers to hospitals might be avoided. Communities are testing new approaches to training and paying EMS personnel to assess and intervene with soluble problems at home, such as a fall without evidence of injury, rather than routinely transporting all patients who call 911 to the emergency department. Improved “geriatric emergency services” and other models for providing more in-home care and forestalling 911 calls are being tested (Hwang et al., 2013).
The use of emergency services near the end of life is not limited to elderly individuals. Parents of uninsured or publicly insured children with serious illnesses often face delays in obtaining physician appointments and end up seeking care in the emergency department, or they may be referred there by their primary care clinician (Rhodes et al., 2013). In some parts of the country, critically ill children are stabilized at a general emergency department, where experience in recognizing a rapidly worsening condition may be lacking, before transfer to a specialized children’s hospital for further care (Chamberlain et al., 2013).
Medicaid reimbursement policies, such as lesser payment for ambulatory versus emergency department care, give hospitals incentives that favor care in the emergency department instead of the hospital’s primary care or pediatric clinic (Chamberlain et al., 2013). Finally, once a child is in the care system, fee-for-service reimbursement and the greater malpractice litigation concerns associated with pediatric care may create incentives to overtest and overtreat (Greve, 2011).
The Ambulatory Care Environment
Physician Services
As the gatekeepers for almost all other services, physicians are among the most important players in end-of-life care. Under Medicare, beneficiaries may see a physician as many times as they wish during a year. However, they may be responsible for a 20 percent co-payment for every visit after paying the deductible of $147 (as of 2014). Part B Medicare imposes no
restrictions on the type or number of physicians a beneficiary may visit (CMS, undated-c).
Physicians’ end-of-life care often fails to meet the needs of patients and families because some clinicians may
- provide care that is overly specialized and does not address the multiplicity of a patient’s diseases or the emotional, spiritual, family, practical, and support service needs of patients and their caregivers;
- continue disease treatments beyond the point when they are likely to be effective;
- fail to adequately address pain and other discomfort that often accompanies serious chronic illnesses and the dying process; and
- fail to have compassionate and caring communication with patients and family members about what to expect and how to respond as disease progresses (Weiner and Cole, 2004; Yabroff et al., 2004).
These problems have numerous causes. Shortcomings in physician education regarding end-of-life care are covered in Chapter 4. In addition, the overall culture of medicine is focused on curing acute medical problems. Reflecting and reinforcing this tendency, the financing structure of Medicare and other insurance programs rewards the performance of a high volume of services and the administration of well-reimbursed treatments and procedures rather than encouraging the provision of palliative and comfort care.
As noted earlier, the general financial incentive within fee-for-service is to see as many patients as possible and to perform multiple procedures. In addition, Congress in 1989 created a physician fee structure of “relative value scales” that takes into account primarily physician time, intensity of service, malpractice insurance, and a geographic factor. Medicare, Medicaid, and many private insurers use this system, which also financially rewards more complex specialty procedures without regard to patient benefit or cost (MedPAC, 2011). At the same time, the system undervalues the evaluation and management services necessary to help patients and families understand what to expect, to explain the pros and cons of treatment options, and to establish goals for care as a disease evolves (Kumetz and Goodson, 2013).
Annual increases in Medicare’s reimbursements to physicians are, in theory, tied to growth in the nation’s GDP. This adjustment method, established by Congress via the Balanced Budget Act of 1997 and called the “sustainable growth rate” (SGR), was intended to be cost-saving. Opposition to limiting physician fee increases has been so strong, however, that
Congress has not imposed these controls since 2002.10 Medicare payment rates for physicians already are about one-fifth lower than private insurance rates (Hackbarth, 2009), and any large additional reduction could lead many physicians to stop accepting new Medicare beneficiaries into their practices (MedPAC, 2011). Because the SGR approach could jeopardize older Americans’ access to care, it is politically unpalatable, and because it fails to incentivize higher-quality care or control health care spending, it is deemed unrealistic and outmoded (Guterman et al., 2013; Hackbarth, 2013; MedPAC, 2011). Discussion of its repeal continues.
Other Services
Although Medicare does not cap beneficiaries’ hospital admissions or medical and surgical procedures, it does cap payments for ancillary services that might substantially benefit certain people nearing the end of life—often more so than acute care and procedures. Such services may forestall hospitalizations, help people better manage daily activities, and improve both health status and quality of life (Eva and Wee, 2010; Farragher and Jassal, 2012). Limitations on rehabilitation services (including those that aid in mobility, swallowing, and communication) may therefore have unintended adverse consequences for both quality of care and health care costs if patients’ remediable problems are not addressed.
Depression, anxiety, and other mental health issues are a significant concern at the end of life and may combine with cognitive problems to cloud a person’s last months. Federal rules implementing mental health parity legislation have erased most long-standing differences between coverage of mental health and other health services for patients with Medicaid and those covered by large group health insurance plans (SAMHSA, 2013); Medicare will reimburse outpatient mental health treatment (therapy and medication management) at parity with other Part B services beginning in 2014.11 Whether mental health services will actually become available re-
_______________
10The SGR distorts the Congressional Budget Office’s (CBO’s) estimates of future health care costs. CBO is required to base its estimates on current law, and the SGR is current law, even though it is unenforced. In discussing future federal health spending, the Simpson-Bowles commission said, “These projections likely understate [the] true amount, because they count on large phantom savings—from a scheduled 23 percent cut in Medicare physician payments [in 2012; larger thereafter] that will never occur” (National Commission on Fiscal Responsibility and Reform, 2010, p. 36). The commission made reforming the SGR its first recommendation in the health arena.
11In addition, drug plans operating under Medicare Part D must cover certain classes of drugs, including antidepressants and antipsychotics. Certain intensive mental health services—such as psychiatric rehabilitation and psychiatric case management—are not covered (Bazelon Center for Mental Health Law, 2012).
mains to be seen, however, as many mental health care providers (including psychiatrists) do not accept insurance at all (Bishop et al., 2014).
The Managed Care Environment
Managed care was developed and tested in the early 1970s as a way of improving the quality and affordability of health care through capitated, integrated provider networks; an emphasis on disease prevention; utilization review for high-cost services; and other means. In the approach’s simplest formulation, managed care organizations receive capitated payments—that is, an annual fixed dollar amount for each individual enrolled in the plan (i.e., per capita).12 For that fee, enrollees receive all their physician care, hospital care, emergency services, and many other covered benefits, depending on what is included in a specific plan. The managed care organization negotiates with providers to achieve reasonable charges and contracts with (or even hires) physicians. Capitation, in theory, switches incentives toward keeping enrollees healthy and avoiding costly overtreatment.
Medicare Part C (Medicare Advantage) plans are managed care plans offered by private insurance companies that cover all Part A and Part B services. In 2012, Medicare Advantage accounted for 23 percent of all Medicare expenditures (see Figure 5-1). Unlike Medicare fee-for-service, Medicare Advantage gives physicians a financial incentive to recommend hospice for patients nearing the end of life because when plan members enroll in hospice, fee-for-service Medicare becomes the payer. This hospice “carve-out” makes it attractive for a plan to shift patients likely to be high-cost from its rolls to the Medicare Hospice Benefit, but also decreases the incentive for the plan to develop high-quality palliative care services (see Appendix D).
In general, health insurance, including managed care programs, may contain disincentives to enroll people who are the very sickest and costliest. Such initiatives require careful risk stratification and monitoring to ensure adequate access and protection for these beneficiaries.
Just as Medicare, through Medicare Advantage, has embraced managed care partly as a way to avoid the costs of unnecessary hospitalizations, Medicaid has embraced managed care partly to avoid unnecessary nursing home admissions. Ideally, these capitated environments should provide models of care and financing that best meet the needs of program beneficiaries, especially those eligible for both Medicare and Medicaid
_______________
12Payments might include some adjustments, such as for patient age and health status or local cost of living. The Balanced Budget Act of 1997 included risk adjustment, based on patients’ diagnoses, to encourage managed care organizations to enroll the sickest Medicare beneficiaries.
(CMS, 2013b). However, the development of policies for implementing and ensuring the quality of managed care options for the dual-eligible population is hampered by significant data limitations, including a lack of timely Medicaid data and comprehensive information about dual eligibles enrolled in Medicare Advantage plans (Gold et al., 2012).
An evaluation of nine state programs of integrated care for dually eligible beneficiaries, performed for MedPAC, identified several additional barriers to the development of managed care programs:
- Enrolling beneficiaries in managed care is problematic because of a lack of awareness of such programs, which may contribute to opposition from providers, beneficiary advocates, and others.
- Structural design problems include administrative leadership (through Medicare Advantage rather than state Medicaid programs), complications in providing patients with social supports and behavioral health services, and uncertainty regarding whether to create separate programs for people under age 65.
- Conflicting Medicare and Medicaid eligibility, coverage, and provider rules complicate state efforts to initiate such programs (Verdier et al., 2011).
Despite these barriers, models of managed care for dually eligible individuals have shown promise, even if they have not been widely replicated. The Evercare model, implemented in five nursing homes (Atlanta, Baltimore, Boston, Colorado [Denver/Colorado Springs], and Tampa) and involving more than 3,600 patients (half enrolled in Evercare, half receiving usual care), offered a capitated package of Medicare-covered services and intensive primary care by nurse practitioners for long-stay, frail, chronically ill nursing home patients. Services included customized care planning, coordination, and delivery. Evercare paid nursing homes an extra fee for “intensive service days” to handle cases that might otherwise have required hospitalization; this measure contributed to a 50 percent reduction in the hospitalization rate for enrollees compared with the usual care group. For those who were hospitalized, stays were shorter for the Evercare group. Evercare enrollees also had one-half the rate of emergency room visits of the usual care group and received more physician visits and mental health services (Kane et al., 2002).
Similarly, an 18-month cohort study of 323 residents with advanced dementia in 22 Boston-area nursing homes found that managed care enrollees had higher rates of do-not-hospitalize orders, primary care visits, and nurse practitioner visits and lower rates of burdensome transitions and hospitalizations for acute illnesses compared with traditional fee-for-service Medicare beneficiaries—all suggesting higher-quality care. Rates of
survival, comfort, and other outcomes did not differ significantly between the two groups (Goldfeld et al., 2013).
Finally, the Program of All-inclusive Care for the Elderly (PACE) offers a comprehensive service package designed to avoid nursing home placements. The program was established as a type of provider for Medicare and Medicaid through the Balanced Budget Act of 1997. PACE serves primarily dual-eligible individuals with chronic illnesses who are aged 55 and older. It uses a centralized, nonprofit provider model rather than a looser network of independent practitioners to provide medical and other clinical services along with the kinds of supportive and personal care services discussed later in this chapter—such as meals, transportation to day centers or other facilities, and in-home modifications.
In 2014, 31 states offered the PACE program. Data from 95 of the nation’s 103 PACE projects indicate they serve a total of slightly more than 31,000 people (National PACE Association, 2014). Thus, the PACE program remains small, and its effectiveness in serving the specific needs of the population requiring palliative care or those nearing the end of life has not been established (Huskamp et al., 2010; see also Appendix D). Moreover, a recent analysis found that, although PACE improves quality by effectively integrating acute care and long-term community supports and reducing hospitalizations, it has not reduced Medicare expenditures for beneficiaries with substantial long-term care needs, perhaps because capitation rates have been set too high (Brown and Mann, 2012).
The slow rate of PACE expansion has been attributed to regulatory and financial constraints, poor understanding of the program among referral sources, competition, and rigid structural characteristics of the program model (Gross et al., 2004). PACE is a comprehensive approach, and it requires a sophisticated infrastructure. Enabling PACE to be implemented more widely might require designing ways to expand it to the non-Medicaid population, as well as other measures (Hirth et al., 2009).
The Palliative Care and Hospice Environment
A full description of the services involved in and benefits of palliative care, including hospice, is provided in Chapter 2. This section addresses the costs of palliative care and hospice compared with usual care and the policies that regulate the organization and provision of palliative care and hospice services.
Palliative Care
Palliative care programs focus on relieving the medical, emotional, social, practical, and spiritual problems that arise in the course of a serious
illness. Many seriously ill people—not just those nearing the end of life—can benefit from palliative care, and it can be provided in many settings, including the home and the nursing home. In hospitals, palliative care teams work alongside treating physicians to provide an added layer of support for patients and their families, focusing on expert symptom management, skilled communication about what to expect, and planning for care beyond the hospital. As discussed in Chapter 2, hospital-based palliative care has grown significantly in the past two decades (CAPC, 2011, 2013).
Palliative care is sometimes viewed as an alternative to what has been termed “futile care”—that is, interventions that are unlikely to help patients or be of marginal benefit and may harm them. Although identifying which treatments are of marginal benefit may be subjective, a study conducted in one academic medical center found that critical care clinicians themselves believed almost 20 percent of their patients received care that was definitely (10.8 percent) or probably (8.6 percent) futile (Huynh et al., 2013). These opinions were based on four principal rationales: the burden on the patient greatly outweighed the benefits, the treatment could never achieve the patient’s goals, death was imminent, and the patient would never be able to survive outside the critical care unit. The total annual cost of futile treatment for the 123 (10.8 percent of) patients who received futile care was estimated at $2.6 million.
At the age of 84, my mother arrived at the emergency room [ER] in significant pain. During the preceding 3 weeks, she had contacted her health care provider several times about nausea and been assured it was not significant. Within 36 hours of arriving at the hospital, she was diagnosed with severely metastasized cancer, especially the liver and including her bones. Even though the source of the cancer had not yet been identified and no one had discussed the reasonableness of pursuing treatment, a port was installed in her chest for chemotherapy, “just in case.” In the next couple of days, as further testing was done, she had an instance of unstable heartbeat and was taken to ICU, where she was given medication and her heart rate returned to normal. The hospital cardiologist assured us her heart was not a problem, but that he would see her every day while she remained in the hospital. Why? All medical staff consistently pushed ahead with an attitude that chemotherapy WOULD be pursued, that they would get her well enough to go home and return for outpatient chemo, and no one ever raised the issue of whether such an approach would be futile. My sister and I had to press the doctor intensely to get him to acknowledge that even with chemo, her life expectancy was well less than a year.
Her condition did not improve over her stay, and 1 week later she decided not to pursue treatment (after several bouts of explosive diarrhea and an inability to get out of bed) and went home in hospice care. She died 2 weeks to the day after going to the ER. Even when leaving the hospital, they did not suggest the end was imminent. She had a great deal of testing, implantation of a PIC [peripherally inserted central catheter] line, and yet no reasonable analysis of the value of further care from anyone.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
The committee agrees with Parikh and colleagues’ (2013, p. 2348) opinion that while “cost savings are never the primary intent of providing palliative care to patients with serious illnesses . . . it is necessary to consider the financial consequences of serious illness.” Much of the spending on the sickest Medicare beneficiaries is attributable to hospital care. Hospitals with specialty palliative care services have been able to reduce their expenditures through shorter lengths of stay in the hospital and in intensive care and lower expenditures on imaging, laboratory tests, and costly pharmaceuticals. In addition, patients receiving hospital-based palliative care have been shown to have longer median hospice stays than patients receiving usual care (Gade et al., 2008; Morrison et al., 2008; Starks et al., 2013).
Most studies comparing the costs of palliative and usual care have been conducted in the hospital setting, but the differing approaches, methods, and rigor of these studies make their findings difficult to compare. Nevertheless, research using robust methods to assess many of the more mature U.S. palliative care programs shows a pattern of savings and demonstrates the substantial excess costs associated with usual care (see Tables 5-3 and 5-4). A 2012 Canadian literature review13 similarly found that hospital-based palliative care teams reduce hospital costs by $7,000 to $8,000 per patient and reduce the cost of end-of-life care by 40 percent or more (Hodgson, 2012).
Palliative care provided in nonhospital settings has also been found to yield cost savings. A systematic review examined studies of palliative care—cohort studies (34), randomized controlled trials (5), nonrandomized trials (2), and others (5)—published between 2002 and 2011 and conducted variously in hospital-based, home-based, and other program settings. Two-
_______________
13In 2012, the Canadian government allocated $3 million over 3 years to support the development and implementation of a framework for community integrated hospice and palliative care models. The Way Forward initiative is led by the Quality End-of-Life Care Coalition of Canada and managed by the Canadian Hospice Palliative Care Association.
TABLE 5-3 Randomized Controlled Trials Comparing the Costs of Palliative and Usual Care
| Study (Period Studied) | Number of Patients and Setting | Excess Cost of Usual Care | Other Findings |
| Gade et al., 2008 (2002-2003) | 517 patients in three hospitals receiving interdisciplinary palliative care services (275 patients) or usual care (237) | Excess 6-month post-hospital discharge costs of $4,855 for each usual care patient (p = 0.001) | Greater patient satisfaction with the care experience and provider communication in the palliative care than in the usual care group; also median hospice stays of 24 versus 12 days, respectively |
| Brumley et al., 2007 (2002-2004) | 145 late-stage patients who received in-home palliative care versus 152 who received usual care in two group-model health maintenance organizations in two states | Excess costs of $7,552 for each usual care group member (p = 0.03) | Palliative care recipients were 2.2 times more likely than usual care recipients to die at home and had fewer emergency department visits and hospitalizations; survival differences between the two groups disappeared after data were adjusted for diagnosis, demographics, and severity of illness (Personal communication, S. Enguidanos, University of Southern California, February 25, 2014) |
| Greer et al., 2012 (2006-2009) | 151 patients with metastatic non-small-cell lung cancer receiving usual outpatient oncologic care with or without early palliative care comanagement | Excess overall costs of $2,282 per patient among those receiving usual care only | Patients receiving early palliative care had significantly higher quality of life, experienced fewer depressive symptoms, were less likely to receive chemotherapy within 2 weeks of death, had earlier hospice enrollment, and survived 2.7 months longer |
TABLE 5-4 Observational Studies Comparing the Costs of Palliative and Usual Care
| Study (Period Studied) | Number of Patients and Setting | Excess Cost of Usual Care | Other Findings |
| Morrison et al., 2008 (observational study using propensity score matching, 2002-2004) | 4,908 patients who received palliative care consultations and 20,551 who received usual care in eight geographically and structurally diverse hospitals | Excess total costs of $2,642 for each usual care patient discharged alive (p = 0.02) and $6,896 for each who died in the hospital (p = 0.001) | Intensive care unit (ICU), imaging, laboratory, and pharmacy costs were higher among the usual care patients |
| Morrison et al., 2011 (observational study using propensity score matching, Medicaid-only patients, 2004-2007) | 475 patients who received palliative care consultations and 1,576 who received usual care in four diverse urban New York State hospitals | Excess costs of $4,098 for each usual care patient discharged alive (p <0.05) and $7,563 for each who died in the hospital (p <0.05) | Patients receiving palliative care consultation were more likely than usual care patients to be discharged to hospice (30 percent versus 1 percent) and less likely to die in intensive care (34 percent versus 58 percent) |
| Starks et al., 2013 (observational study using propensity score matching, 2005-2008) | 1,815 patients who received palliative care consultation and 1,790 comparison patients from two academic medical center hospitals | Excess costs of $2,141 for usual care patients with lengths of stay of 1-7 days (p = 0.001) and $2,870 for usual care patients with lengths of stay of 8-30 days (p = 0.012) | Some differences between palliative care and usual care groups remained |
| Penrod et al., 2010 (observational study, 2004-2006) | 606 veterans who received palliative care and 2,715 who received usual care in five U.S. Department of Veterans Affairs (VA) hospitals | Excess costs of $464 per day for usual care patients (p = 0.001) | Instrumental variables method used to account for unmeasured selection into treatment bias (Stukel et al., 2007) |
thirds of the studies were based in the United States, and the remainder were conducted internationally, in widely differing health systems. The authors found that, although the studies used a broad variety of utilization, cost, and outcome measures and employed different specialist palliative care models, palliative care was “most frequently found to be less costly relative to comparator groups, and in most cases, the difference in cost is statistically significant” (Smith et al., 2014, p. 1).
A recent review of published, peer-reviewed outcomes research on nonhospice outpatient palliative care, which included four randomized interventions and a number of nonrandomized studies, concluded that outpatient palliative care produced overall health care savings resulting from avoidance of expensive interventions. The authors suggest that such savings are “especially important in systems of shared cost/risk, integrated health systems, and accountable care organizations” (Rabow et al., 2013, p. 1546).
Community-based pediatric palliative care has also been found to produce positive patient and family outcomes, as well as cost savings (Gans et al., 2012), or at least to be relatively low cost (Bona et al., 2011).
These data across varying types of studies and care settings indicate potential savings from palliative care consultation and comanagement in hospitals and suggest savings in other settings as well. Additional research is needed before firm conclusions can be drawn on the impact of palliative care delivery on total health care spending.
Hospice Care
The Medicare Hospice Benefit is the one public insurance program intended specifically to serve beneficiaries within the last few months of life. Under this benefit, the enrolled beneficiary pays no charge for services received except for small deductibles for drugs and respite care. Most services are provided in the patient’s home by visiting nurses, with variable additional support from physicians, social workers, personal care aides, and others. For fiscal year 2014, Medicare’s daily hospice reimbursement rates were as follows: for routine home care, $156.06; for continuous home care, $910.78; for general inpatient care, $694.19; and for inpatient respite care, $161.42 (HHS and CMS, 2013).14 In addition, the total amount of Medicare payments a hospice provider is allowed to receive in a single year is capped according to a defined formula.
As described in Chapter 2, hospice services produce many benefits for patients and families. Matched cohort studies demonstrate that hospice
_______________
14Minus a two percentage point reduction to the market basket update for hospices that fail to submit the required quality data.
care enhances the quality of care, helps patients avoid hospitalizations and emergency visits, prolongs life in certain groups of patients, improves caregivers’ well-being and recovery, and in some reports appears to reduce total Medicare spending for patients with a length of hospice service of under 105 days (Kelley et al., 2013a).15
Enrollment disincentives Built into the Medicare Hospice Benefit and its payment rules are several policies that are intended to manage program costs but may work against the needs of patients with advanced serious illnesses and their families. Two eligibility requirements meant to limit the number of people who qualify for the hospice benefit are
- an expected prognosis of 6 months or less if the disease runs the expected course, as certified by two physicians16; and
- an agreement, signed by the beneficiary, to give up Medicare coverage for further treatments aimed at achieving a cure.
For many patients, these criteria have discouraged use of the benefit until the final days or hours of life and, according to Approaching Death, exclude “many [people] who might benefit from hospice services” (IOM, 1997, p. 169). The ban on “curative” treatments may also disadvantage patients with organ failure, for whom life-prolonging and palliative treatments—such as diuretics for people with heart failure—often are the same. In addition, physicians, patients, and family members alike may be unwilling to accept a prognosis of a few months—particularly given the uncertainty in predicting mortality for diseases other than cancer—or to abandon cure-oriented treatment (Fishman et al., 2009). These factors contribute to the brevity of hospice stays: the median length of stay in hospice is 18 days, and fully 30 percent of hospice beneficiaries are enrolled for less than 1 week. Still, the number of Medicare beneficiaries enrolling in the Medicare Hospice Benefit more than doubled between 2000 and 2011, from 0.5 million to more than 1.2 million (MedPAC, 2013).
Some hospice champions contend that the 6-month limit and the ban on cure-oriented treatments make the Medicare Hospice Benefit “a legal barrier to improving integration and collaboration across the health system” (Jennings and Morrissey, 2011, p. 304). In a survey of nearly 600
_______________
15Methodological difficulties in analyses of hospice savings include the lack of controlling for selection bias (that is, people who choose hospice care may be different in some way from those who do not) and the impact on the data of both very-long-stay patients and those discharged alive after very long stays, who may have been more appropriate candidates for long-term care programs rather than hospice.
16In reality, patients are able to receive hospice services for longer than 6 months if, at the end of the period, they receive a physician recertification of the 6-month prognosis.
hospices, 78 percent were found to restrict enrollment in some way, such as by declining to admit patients with ongoing disease treatment needs or without a family caregiver at home (Aldridge Carlson et al., 2012). Small hospices are especially likely to restrict enrollment (Wright and Katz, 2007).
I am a registered nurse case manager, certified in palliative nursing, working with hospice patients in their homes. I think the single most effective change that could be brought about would be to extend the hospice benefit to a 1-year prognosis rather than the current 6 months. This may allow for a strengthening of the role of palliative care much earlier in the trajectory of life-limiting illnesses, particularly those for which the expected course is more certain, such as some cancers. I think the earlier the concept of palliative care is introduced, the less intimidating the “end-of-life” connotation of hospice will be. A patient’s course would feel more of a continuum, rather than the abrupt shift from treatment to “hopelessness” that now exists. Just last week, I had a visit with a woman who had been referred to hospice by her oncologist, and she was very frightened that her death was imminent, even though it is not. Her family was equally upset with the physician for frightening the patient so.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
Payment policies The flat daily rate allowed for by the Medicare Hospice Benefit—which means the hospice receives the same amount regardless of how many, or how few, services it provides on a given day—is coming under scrutiny. The methodology and mix of services used to calculate the daily rate “have not been recalibrated since initiation of the benefit in 1983” (MedPAC, 2013, p. 263), and are inadequate for some hospice programs to cover important services (e.g., palliative radiation, intrathecal delivery of opiates).
Lengths of stay Hospice services have evolved toward serving the two tails of the longevity curve: a large number of beneficiaries enrolled only a few days before death and a large number of very-long-stay patients, with hospice, in effect, serving as an alternative (and one more generously reimbursed) to the provision of long-term care in other settings. In some cases,
long stays occur because patients improve under hospice care and outlive their original 6-month prognosis.
The high proportion of short stays in hospice is troubling on quality-of-care grounds, while growth in very long hospice stays is troubling on cost management grounds. The concern arises that incentives in the payment system may be encouraging some providers “to pursue business models that maximize profit by enrolling patients more likely to have long stays,” some of whom may not meet hospice eligibility criteria (MedPAC, 2013, p. 265). This pattern, which is more common among for-profit hospice providers (Aldridge Carlson et al., 2012), is also believed to explain some hospices’ high rates of “live discharges” for long-stay patients as the facility approaches its aggregate annual cap on Medicare reimbursements.
A concern is the enrollment in hospice of cognitively impaired nursing home residents. As a result of this trend, the mean length of stay for Medicare hospice patients, which was 48 days in 1998, was 86 days in 2011 (CMS, 2013a; MedPAC, 2013). In 2009, the longest average stays were for patients with Alzheimer’s disease (106 days) and Parkinson’s disease (105 days). By comparison, patients with lung cancer had average stays of 45 days and those with breast cancer 59 days (CMS, 2013a). Among the 10 percent of patients with stays longer than 6 months, the average length of stay in 2011 was 241 days (MedPAC, 2013).
The dominant and countervailing trend of notable concern, however—affecting at least 30 percent of all hospice beneficiaries—is stays that are too short. According to hospice industry figures, the median length of stay in hospice has steadily fallen, from 21.3 days in 2008 to 18.7 days in 2012 (NHPCO, 2009, 2013), which means that half of hospice patients have stays shorter than 18.7 days.
To the extent that the Medicare Hospice Benefit is being used for people with questionable eligibility as a de facto palliative care supplement to long-term care benefits under state Medicaid programs, the costs of the Medicare Hospice Benefit are raised artificially, and the costs of this care are transferred to the federal government. MedPAC has recommended closer program monitoring to forestall this potential misuse, and greater scrutiny is occurring (U.S. Department of Justice, 2013). Oversight is considered especially appropriate for the approximately 10 percent of hospices that exceed their benefit cap (MedPAC, 2013, p. 275).
The background paper prepared for this study by Huskamp and Stevenson (see Appendix D) reviews several potential or proposed changes to the Medicare Hospice Benefit that would affect hospice-related financial incentives and realign hospice services. Some of these changes were included in the ACA (see also Huskamp et al., 2010).
The Long-Term Care Environment
People with multiple chronic diseases and frailty need a variety of long-term services and supports that can improve the quality of their lives, potentially forestall the need for emergency visits and hospitalizations, and reflect individual and family desires for care at home for as long as possible.
Someone turning age 65 today has almost a 70 percent chance of needing some type of long-term care services and supports in their remaining years (HHS, 2014), yet few (only about 10 percent of the elderly) have private long-term care insurance. The low uptake of existing private long-term care insurance options may be attributable in part to the availability of Medicaid, which provides means-tested “public insurance to many households . . . who could otherwise afford and would be interested in private insurance coverage” (Senate Commission on Long-Term Care, 2013, p. 23), and the lack of long-term care insurance requires many people to deplete their assets to become Medicaid eligible.17 The need for new public and private long-term care insurance options that would stabilize the financial future of Americans—a neglected corollary to addressing long-term care services and their financing (IOM, 2013e; Wiener et al., 2013)—is beyond the scope of this report.
Only one-third of elderly Americans have sufficient assets to pay for 1 year of nursing home care, which in 2012 averaged $81,030 for a semiprivate room and $90,520 for a private room (National Health Policy Forum, 2013). Home-based care is less expensive, but still costly. Four hours per day of homemaker and home health aide services, 7 days per week, costs from $28,000 to $31,000 per year, and such services are not always available. It is no wonder, then, that long-term care has been called “the largest uninsured risk faced by the older population” (Norton, 2013; Spillman, 2012, p. 239).
Many families are caught in the middle: they are too “well off” for Medicaid, but unable to pay out of pocket to meet their personal care needs. This is another reason for relying on the acute care system of 911 calls, emergency departments, and hospitals when care needs become overwhelming. Unlike long-term services and supports, these much more costly acute care services are covered by Medicare.
Medicare’s benefit structure reflects patients’ health care needs as generally understood when the program was created nearly a half-century ago. Today, health and the use of health care services are understood as being influenced by a broad range of factors beyond those addressed by health professionals or traditionally covered by health insurers. There are many
_______________
17These assets do not include a person’s home. As long as a house serves as the “principal place of residence” of a Medicaid applicant (or spouse or certain other close relatives), it is not factored into the Medicaid eligibility determination, regardless of its value (HHS, 2005, p. 2).
ways to improve quality of life and comfort for people with advanced serious illnesses and lessen the burden on their family caregivers (Topf et al., 2013) while preventing predictable crises. The resulting savings in costly emergency visits, hospitalizations, and even long-term nursing home care could be redirected toward underfunded and badly needed long-term services and supports (Unroe and Meier, 2013).
We got hospice when my mother-in-law died, but only for 2 weeks. She declined steadily for 2 years before her death, as we bounced back and forth between hospital, nursing home, and home (with private-paid caregivers). It was a bad way to go, with much pain, suffering, and expense for her and our family. There were too many barriers to getting the care she needed. Medicare pays for all types of care that is unbeneficial (911 trips to the hospital, certain tests, treatments, medications, surgeries, and skilled nursing home stays for rehab, etc.). But it will not pay for the care people actually need during chronic, progressive illness—custodial care, comfort care, nursing care. We need to fix this.*
____________
*Quotation from a response submitted through the online public testimony questionnaire for this study. See Appendix C.
Institutional Long-Term Care
Medicare provides little payment for long-term services and supports, including personal assistance with activities of daily living (e.g., bathing, dressing, toileting, eating, transferring, and medication management). Medicare’s sole contribution to nursing home care is in paying for short-term skilled nursing services aimed at rehabilitation following hospitalization and for short-term home health care for the homebound with a “skilled need.” Post-acute care accounts for about 21 percent of all spending on long-term services and supports (KFF, 2013b), and its goal is to return beneficiaries to the highest possible level of functioning. In one analysis, almost one-third of Medicare beneficiaries used the skilled nursing benefit in their last 6 months of life, and 1 in 11 died while enrolled in that benefit. Many such patients may be too frail or ill to return home and would be well served if the benefit included a stronger palliative care component and allowed concurrent hospice care (Aragon et al., 2012).
The rehabilitation mission of skilled nursing facilities may conflict with patients’ medical condition and goals, especially in the last months of life, when hospice or palliative care may be better matched to their needs. The
decision to place a patient in a skilled nursing program may be based not on a clinical need for rehabilitative services or patient preferences but on built-in financial incentives. Some families are unable to provide home care for a patient in rapidly deteriorating health, but at hospital discharge they must make a difficult choice. They can choose Medicare payment for 100 days of room and board and “rehabilitative” care in a skilled nursing facility, but if they want hospice care and do not qualify for Medicaid, they will have to pay out of pocket for nursing home room and board (Aragon et al., 2012).
People covered by the skilled nursing facility benefit cannot be enrolled simultaneously in hospice unless the two services are treating totally unrelated medical conditions. Nursing homes and skilled nursing facilities have an incentive to keep people in post-acute care as long as possible instead of enrolling them in hospice because once patients are referred to hospice, they must shift from the generously reimbursed (by Medicare) skilled nursing benefit to the poorly reimbursed (by Medicaid) long-term care benefit.
Nursing homes have an incentive to hospitalize residents repeatedly so as to make them eligible once again for the higher-paying skilled nursing facility program. Indeed, there is some evidence of disproportionately high rates of potentially avoidable hospitalizations among dual-eligible residents in skilled nursing facilities and nursing homes (942 per 1,000 person years for skilled nursing facility residents and 338 per 1,000 person years for nursing home residents). By contrast, people living in the community had markedly lower rates of potentially avoidable hospitalization (250 per 1,000 person years for those receiving Medicaid-paid home- and community-based services, and only 88 per 1,000 person years for those not receiving those services) (Segal, 2011). A growing literature is finding that many hospitalizations for patients with dementia, in particular, are avoidable and a potential source of system savings (Grabowski and O’Malley, 2014).18 As noted earlier, moreover, frequent transitions between the nursing home and hospital and back again are burdensome to patients and have been associated with increased rates of feeding tube insertions, intensive care unit stays, pressure ulcers, and late enrollment in hospice for residents with advanced cognitive and functional impairments (Gozalo et al., 2011).
From the standpoint of financially strapped state Medicaid programs and providers, the cost shift to Medicare and the transfer of patients back and forth between skilled nursing facilities and hospitals has obvious appeal. From the standpoint of the quality of care for patients and families and the nation’s total health care spending, it reflects both poor quality and enormous costs.
_______________
18For example, the Evercare managed care demonstration program enhanced advance care planning, provided nurse practitioner care, and altered financial incentives, producing fewer preventable hospitalizations and improved survival with no diminution in the quality of care (Kane et al., 2004).
Home- and Community-Based Care
Because state rules governing Medicaid do not universally draw Medicare’s line between health services and support services, Medicaid is the main source of payment for the latter. Additional funding for these services comes through Medicaid’s Home and Community Based Services program.
By 2009, 3.3 million people were participating in Medicaid’s Home and Community Based Services program, a 60 percent increase in participation since 2000 (National Health Policy Forum, 2013). AARP policy analysts are among those who have encouraged states to invest in this program, making their case primarily on the grounds of cost-effectiveness (AARP Public Policy Institute, 2008). As more people age into their 70s, 80s, and 90s and need daily help, the demand for long-term care services, including in-home home health services, will continue to rise (Employment Benefit Research Institute, 2012). In this context, state Medicaid programs are giving increasing attention to “rebalancing” efforts aimed at reducing their long-standing institutional bias (Kassner, 2013)—that is, shifting long-term services and supports from expensive institutional settings, mainly nursing homes, to people’s homes. As illustrated in Box 5-1, however, while such shifts may make sense from the standpoint of both patient desires and program integrity, they need to be undertaken with some caution.
“During the late 1970s and early 1980s, the federal government sponsored a series of randomized, controlled . . . demonstrations to test the cost-effectiveness of home and community-based services as a substitute for nursing home care” (ASPE, 2000, p. 10). The National Channeling Demonstration, funded by the Health Care Financing Administration (HCFA),19 Administration on Aging (AoA), and the Office of the Assistant Secretary for Planning and Evaluation (ASPE), tested two models for financing and delivering home- and community-based services (Kemper, 1988). HCFA and the National Center for Health Services Research (NCHSR)20 sponsored more than a dozen state- or region-specific demonstrations. Major findings from these projects were as follows:
- Targeting program enrollment to those at highest risk of nursing home placement saves money.
- Home- and community-based services programs can achieve budget neutrality with narrow targeting to the highest-risk groups, low average benefit levels (taking into account the availability of informal supports), and an emphasis on high-quality services.
_______________
19HCFA is now the Centers for Medicare & Medicaid Services.
20NCHSR was a predecessor to the Agency for Healthcare Research and Quality.
BOX 5-1
Learning from Past Institution-to-Community Shifts
Experience with the community mental health services movement of several decades ago suggests that the shift from institutional to community care should be closely monitored. In the 1960s and 1970s, the nation’s large, old-fashioned, and underperforming mental hospitals were closed or greatly reduced in size, and responsibility for former residents’ continuing service needs was shifted to community service providers that were neither adequately prepared nor funded to assume this responsibility (Lyons, 1984). Setting these former patients adrift without appropriate support was a largely avoidable tragedy that contributed significantly to poor-quality care, high incarceration and hospitalization rates, and the rise of substance abuse and homelessness (Baum and Burnes, 1993; Yoon et al., 2013).
- Data limitations make designing and conducting research that truly measures cost-effectiveness—as distinct from “cost shifting” from one program to another, from state to federal funds, and from formal to informal care—nearly impossible. Cost-effectiveness studies of these programs typically use only Medicaid expenditure data and do not consider the impacts of other programs such as Medicare and Social Security Insurance.
A recent report summarizing analyses from 38 states, conducted between 2005 and 2012, found consistently lower average costs for home- and community-based care than for institutional long-term care. In 2008 in California, for example, “per recipient spending on nursing facilities was three times higher than for HCBS [home- and community-based services] ($32,406 for nursing facility care versus $9,129 for HCBS)” (Fox-Grage and Walls, 2013, pp. 6-7). However, many states cap the number of people who can enroll in the Home and Community Based Services program, and some states maintain waiting lists for the program; testimony to the Senate Commission on Long-Term Care suggests that nearly half a million people are on these lists (Senate Commission on Long-Term Care, 2013, p. 16). While the state studies varied in approach and should be replicated by independent researchers, they are important in contributing to state decisions about program policy.
The cost impact of home- and community-based services is almost always measured only in terms of Medicaid expenditures. However, analysts have repeatedly observed the need for a broader analytic framework along several dimensions. For example, capturing the true cost side of the equation requires consideration of the services’ impact on other pub-
lic programs, such as Medicare, Supplemental Security Income, and the Supplemental Nutrition Assistance Program (SNAP). These comprehensive analyses of expenditures and savings have not been carried out because acquiring the necessary data is too difficult and expensive. In addition, cost estimates need to take into account the dollar value of unpaid care provided by family caregivers.21 Even if it were possible to assess costs adequately, estimating the benefits (effectiveness) and quality gains of these programs reliably presents an additional set of methodological challenges.
Movement toward alternatives to nursing homes is also supported by federal policy makers. In its 2013 report, the Senate Commission on Long-Term Care, established in 2012, urged a shift away from nursing homes and toward home care (Senate Commission on Long-Term Care, 2013). Likewise, the Administration for Community Living, an HHS agency that includes the Administration on Aging and Administration on Intellectual and Developmental Disabilities, emphasizes community options for the elderly (Administration for Community Living, 2013).
Yet while a wide variety of community-based providers try to help people needing long-term services and supports, the financing and organization of these services and supports create barriers to access. “The network of providers to deliver this support is complex, multifaceted, specialized, isolated from other services providers, and confusing to the average consumer,” reported the Senate Commission on Long-Term Care (2013, p. 14). Rarely do service providers assess a patient’s and family’s overall needs so that they can arrange for the right set of services; instead, patients and families have access to what is funded by some mix of federal, state, and local sources, each with its own eligibility rules, limits, and procedures. Just finding out about available services and resources is a significant challenge.
An especially serious problem is the structural and financial isolation of the system for long-term services and supports from the health services sector. As a result, the planning and organization of the two are separate when patients are in transition across settings, and there are few incentives to integrate or streamline the two sets of services, despite their obvious interdependence and potential synergies.
One possible way to bridge the gap between these two service sectors for some patients and families is through community-based palliative care programs. As Huskamp and Stevenson (see Appendix D) note, “palliative care can be introduced at any point during the course of a serious advanced illness when a patient and family needs [sic] help to manage symptoms and maximize quality of life.” Insurance coverage for hospice—under Medi-
_______________
21For example, a study of family caregiving for community-dwelling elders in the last year of life estimated the value of these services as between $22,500 and $42,400 (in 2002), which the authors note equaled the cost of a home aide (Rhee et al., 2009).
care, Medicaid, and many commercial insurance plans—is the dominant financing mechanism for community-based palliative care. Models aimed at bridging the gap, such as community-based palliative care, medical homes, house calls or home-based primary care programs, and PACE, have demonstrated effectiveness in improving value (improved quality leading to lower acute care spending) (Grabowski, 2006; Kamal et al., 2013; Komisar and Feder, 2011; Unroe and Meier, 2013).
Finally, if efforts to rebalance nursing home and home- and community-based care are to succeed and more seriously ill people are to be cared for in their homes, home- and community-based care will need to encompass certain medical and quasi-medical services. These services include
- case management;
- round-the-clock access to a clinician for advice;
- mental health services;
- respite care;
- comprehensive interdisciplinary primary care;
- medication management; and
- support for basic activities of daily living—eating, bathing, dressing, toileting, and transferring (into and out of bed, a chair, a wheelchair)—through personal care aides.
Matching Services to Needs for Dual-Eligible Individuals
The nearly 10 million Americans who are dually eligible for both Medicare and Medicaid present a particular challenge to the current care system. These individuals tend to make up the sickest, frailest, poorest, and highest-cost population served by the two programs (Brown and Mann, 2012).
Because dual-eligible individuals are either 65 and older or permanently disabled and because they are poorer than the general population, they often have significant long-term care needs (CBO, 2013). As Table 5-5 shows, they account for a significant proportion (roughly one-third) of expenditures for each program. Some 65 percent of Medicaid spending for this group is for long-term care (Young et al., 2013). Over the years, a
TABLE 5-5 Dual-Eligible People in Medicare and Medicaid, 2010
| Indicator | Medicare | Medicaid |
| Share of beneficiaries who are eligible for both programs | 1 in 5 | 1 in 6 |
| Program expenditures for people eligible for both | 33% | 36% |
SOURCE: Young et al., 2013.
number of initiatives, including a new effort under the ACA described later in this chapter, have been aimed at improving both quality of care and efficiency for this high-risk population by encouraging care in the community rather than in nursing homes.
Health care spending by dual-eligible individuals varies considerably. Two in five people receiving both Medicare and Medicaid generated lower expenditures than other Medicare beneficiaries, while one in five accounted for three-fifths of all dual-eligible spending. Fewer than 1 percent of individuals cost both Medicare and Medicaid high amounts; most individuals are high cost for only one of the programs (Coughlin et al., 2012). These findings suggest that dual-eligible individuals living in nursing homes might be good candidates for palliative care and care management intended to prevent avoidable hospitalizations, while others, living in the community, would be good candidates for a medical home or other entity that coordinates and integrates social and medical supports. Program savings resulting from such interventions are most likely to occur among people who have functional dependencies, frailty, and/or dementia in the context of one or more chronic diseases.
Efforts to produce Medicare and Medicaid savings in covering dually eligible people have centered on the twin strategies of enrollment in managed care programs, such as PACE, and use of care management to coordinate care (as discussed further below). However, many of these efforts have failed to target those at highest risk and as a result, have not produced the desired savings, although they “provide strong evidence that care management might be effective at reducing costs for some subgroups of dual eligibles, such as those with severe chronic illnesses or at high risk for hospitalization” [emphasis added] (Brown and Mann, 2012, p. 4).
Organization of Services
As described in Chapter 2, significant problems and burdens accompany each transfer of a seriously ill patient from one care setting to another, and the large number of such transfers as patients near the end of life has been documented (Teno et al., 2013). Each such transfer runs the risk of
- poor communication between settings and inadequate transfer of records, including advance directives (which results in, for example, inadequate information about self-care or perplexing changes in instructions; redundant tests; duplicate, confusing, or conflicting prescriptions and medication errors; and increased risk of falls, infection, and delirium—any of which can harm patients and lead to additional hospitalizations) (Press et al., 2013);
- poor communication between providers across settings, impeding primary physicians’ ability to properly manage patients under their care; and
- confusion among patients and family members regarding what to do, which provider is responsible for what, and whom to consult when things go wrong.
Better coordination of care is widely perceived as essential to improving patient outcomes. Not only are people nearing the end of life often treated in several settings, but also they (and their families) interact with numerous physicians and other health professionals, are prescribed multiple medications and treatments that may interact in undesirable ways or be difficult to administer properly, and face logistical problems in accessing care when they need such basic services as transportation. In a conclusion still valid today, the 2001 IOM report Crossing the Quality Chasm notes that one serious consequence of the poorly organized U.S. health system is the “layers of processes and handoffs that patients and families find bewildering and clinicians view as wasteful” (IOM, 2001, p. 28). A renewed focus on discharge planning, continued access to care and support after discharge, medication reconciliation, and avoidance of rehospitalizations could improve continuity across settings in a patient-centered, family-oriented way (Coleman et al., 2006).
Conversely, inadequate care coordination results in avoidable medical complications and unnecessary hospital readmissions, which by themselves cost Medicare some $15 billion per year (Tilson and Hoffman, 2012). In the case of seriously ill children, for example, the lack of after-hours coverage in physician offices impels some working parents to seek whatever care is available, and that is found in costly hospital emergency departments (Chamberlain et al., 2013).
To the extent any organized attempt at coordination takes place outside of hospice, it is typically through “disease management” or more comprehensive “care management” programs. Often these programs entail assignment of a specially trained nurse or other health professional to help a patient with complex needs navigate the system across service providers. The success of these programs is highly variable, depending on their ability to select the most appropriate patients, meet needs around the clock, align supportive and medical services, and flexibly adjust the intensity of service to changing patient and family needs. Additional key program features are assessment of and support for family caregiver needs; round-the-clock access by phone; consistent relationships and communication among the care coordination team staff, patients, families, and medical providers; integrated assessment and delivery of both medical and social services; and generation and mobilization of needed long-term services and sup-
ports (Bass et al., 2013; Brown et al., 2012; Peikes et al., 2012) (see also the discussion of social services below). If care management initiatives that include such support services can produce savings when serving people with severe chronic illnesses or a high probability of hospital admission, they may also be well suited to people in the final phase of life before they become eligible for hospice.
A 15-program randomized controlled trial of the Medicare Coordinated Care Demonstration identified six features that appeared to be central to the limited number of coordination efforts that saved money:
- frequent face-to-face contact between the patient and the care coordinator;
- occasional face-to-face contact between the patient’s physicians and the care coordinator;
- the care coordinator’s functioning as the “communications hub” for the patient’s practitioners;
- use of evidence-based patient education interventions;
- comprehensive medication management; and
- a timely, comprehensive response to transitions between care settings, such as discharge from a hospital to post-acute care (Brown et al., 2012).
A review of studies on the effectiveness of disease management efforts within the Medicaid program reveal additional themes:
- Disease management programs were most effective in improving quality of care and achieving cost-effectiveness for the sickest patients, including those with comorbidities, underscoring the importance of targeting interventions to those most likely to benefit from them.
- Although in-person care management was the costliest intervention, it also was the most effective with high-risk patients, while less intensive management was appropriate for lower-risk patients.
- Projects that used data mining and predictive modeling to stratify patients by disease severity and risk were “particularly successful in designing and delivering [disease management] programs across chronic disease groups” (Freeman et al., 2011, p. 35).
The studies reviewed varied greatly in the medical conditions and program designs addressed and in the kinds and quality of data collected. Nor were they specifically looking at the needs of patients near the end of life. However, the general profile of patients with functional dependency, with multiple chronic diseases and comorbidities, and at risk of hospitalization
and emergency visits was relatively consistent across studies and mirrors the circumstances of people who may be nearing the end of life.
Beneficial outcomes of successful care coordination found in these studies included improved medication adherence, reduced hospitalizations and readmissions, reduced emergency visits, and fewer unnecessary medications. And disease management programs that reduced hospitalizations by only 10 percent were able to cover their associated program costs (Freeman et al., 2011). Other meta-analyses have likewise noted improvements in the quality of care but have produced less persuasive evidence on reduced health care utilization, except successes in lowering the risk of hospitalization, and on health care savings (Mattke et al., 2007). However, improvements in quality of care that are achieved without increasing costs can be considered successes when such high-risk, high-need recipients are being served.
In summary, clinician engagement and targeting and tailoring of social services and their integration with the medical care delivery system appear to be essential elements of successful disease and care management models (Freeman et al., 2011; Meyer and Smith, 2008).
Geographic Variations in Service Utilization and Costs
Studies of the costs of care in the last months of life have revealed marked differences in the utilization and costs of treatments from one geographic area to another and from one hospital to another. These differences are attributable in part to local variations in the supply and prices of medical resources (e.g., doctors, nursing home rehabilitation, home care agencies, hospitals, drugs, medical devices, and procedures) (Commonwealth Fund Commission on a High Performance Health System, 2013) and to a lesser extent to patient and family characteristics and preferences (Prigerson and Maciejewski, 2012).
Medicare payments vary widely among and within localities. Per capita Medicare spending (that is, the average amount Medicare pays out per beneficiary) varies more than two-fold among different regions of the country, mainly as the result of differences in the volume of services provided. The greatest influences on volume differences are the regional supply of physicians and available hospital beds (Dartmouth Atlas of Health Care, 2013).
An IOM committee recently determined that variation in Medicare spending across and within geographic areas is explained mainly by differences in spending for post-acute care, including subacute rehabilitation in skilled nursing facilities, long-term acute care facilities for ventilator-dependent Medicare beneficiaries, and home health agencies. If these spending variations were eliminated, overall spending variation would drop by 73 percent (IOM, 2013a). This finding has important implications for the care
of people with serious advanced illnesses. The management of transitions from one setting to another may be a more important cost driver than has previously been recognized, and “a growing body of evidence leads to the conclusion that clinical and financial integration best positions health care systems to manage the continuum of care for their complex populations efficiently” (IOM, 2013a, p. 18).
Financial incentives for nursing homes to hospitalize dually eligible residents (and then to obtain Medicare’s higher post-acute care skilled nursing benefit) are similar nationwide; however, state-level data reveal dramatic variations in preventable hospitalizations for nursing home residents. The lowest rate of such hospitalizations (65 per 1,000 person years) is found in Alaska, and the highest (231 per 1,000 person years) in Louisiana, although this analysis does not control for differences in population health across states (Segal, 2011). In one consensus of experts, expressed as a percentage of hospitalizations, a median of 19 percent of hospitalizations of all long-stay nursing home residents are considered potentially avoidable, with a range across states of 7-31 percent (Commonwealth Fund, 2013).
Variation in spending does not appear to be related to differences in quality of care provided or in care outcomes. After an extensive review of the literature, the IOM committee studying geographic variation in Medicare spending found no relationship between quality-of-care indicators and what Medicare paid for services. If people with chronic illnesses who live in higher-spending areas had better outcomes in terms of survival or quality of life, one could argue that similar resources should be expended in other locales; however, this is not the case (Dartmouth Atlas of Health Care, 2013; Wennberg et al., 2008).
To the extent that excessive services do not benefit (and may harm) patients, they represent wasteful and unnecessary expenditures, and therefore significant opportunities for both better-quality care and cost savings. Clearly, in the current environment, with abundant evidence of poor-quality care and national health expenditures continuing to rise, marked geographic and interinstitutional variations in expenditures may be a good focus for analysis of both shortfalls in quality and excess service provision.
THE GAP BETWEEN SERVICES PAID FOR AND WHAT PATIENTS AND FAMILIES WANT AND NEED
As noted throughout this report, an approach that enabled more people to remain in their homes or home-like settings in the final stages of life would better align with the preferences of many patients and families than the current system. And a significant barrier to improving the quality of end-of-life care and controlling costs is that the mix of services currently delivered and paid for fails to provide for precisely those needs that drive
repeated reliance on the emergency and acute care systems: round-the-clock access to meaningful help, house calls and home care, caregiver support, and long-term services and supports. Although some states have used the demonstration and waiver authorities under Medicare and Medicaid to create a more comprehensive continuum of services for the elderly and people who have disabilities, the nation is far from achieving an easily accessible, reliable system of care for people who have advanced serious illnesses and are nearing the end of life. Clearly, significant changes in the approach to service delivery would be needed to effectively integrate traditional medical care and social services.
Impact of Social Services on Health Outcomes
Abundant evidence reveals the powerful role of social and behavioral factors in health and health spending in contexts other than end-of-life care (Farley, 2009; Marmor et al., 1994; McGinnis and Foege, 1993; U.S. Burden of Disease Collaborators, 2013). Research conducted over several decades has established that health care in itself plays a much smaller role in the health of a population than a range of other factors related to behavior and socioeconomic status. Indeed, recent analyses attribute the paradoxically high rate of health care spending and inferior health outcomes in the United States relative to other developed countries to the lack of integration of health and social support programs (Bradley and Taylor, 2013; Shier et al., 2013). Despite its position roughly in the middle in terms of total social22 and medical spending per capita, the United States ranks 27th out of 40 nations in life expectancy, according to data from the Organisation for Economic Co-operation and Development (OECD). And while the United States is roughly in the middle relative to other OECD countries in total health and social services spending as a percentage of GDP,23 the ratio of social services spending to health services spending is markedly lower relative to other nations. These different spending patterns may reflect countries’ different histories, cultures, attitudes toward social spending, and political milieus.
In a changing health care landscape, new tools, approaches, and payment models are making it easier and more advantageous than ever for
_______________
22The OECD social expenditure database includes nations’ expenditures for such programs as pensions and retirement, home health, and other benefits for the elderly; pensions, sick leave, residential care, and rehabilitation for people with disabilities; and family allowances and maternity leave (OECD, 2014).
23The figure for the United States is 25.4 percent. By comparison, the figure for Sweden is 33.2 percent and for Ireland is 18.2 percent. At the bottom for spending in these two categories are Chile, Estonia, Korea, Mexico, and Turkey, each of which spends a total of 15 percent of GDP or less in these two categories.
providers and health systems to meet the social needs of their patients (Bachrach et al., 2014). Interventions that address patients’ social needs have been shown to positively impact patient outcomes and satisfaction with care.
The committee supports the expansion of social support for people with advanced chronic illnesses with functional debility and careful assessment of ongoing pilot programs focused on doing so (Shier et al., 2013). Much can be learned from those efforts about the impact of these services on health, as well as the means chosen to determine clients’ service needs, establish eligibility, manage costs, and ensure quality, all of which can guide future programming.
The Importance of Social Services
In this report, the term “social services” refers to a rather modest but essential set of services not generally considered part of health care. A core list of commonly needed services includes the following:
- caregiver training and support,
- retrofitting of the home for safety and mobility,
- meals and nutrition services,
- family respite, and
- transportation.
Some of these services are provided through Medicare Advantage plans and through Medicaid. Some could be provided through expansion of the Older Americans Act, which currently is underfunded to meet its potential. And some could be provided through relatively low-cost, volunteer-staffed efforts if they were implemented effectively with training, oversight, and coordination with a person’s needs. For example, health insurance counseling, legal and financial counseling, and bill payment services currently are offered by many community organizations through volunteers, consumer credit counseling programs, and representative payee programs. Volunteerism is a long-standing component of hospice.
Social services may be especially important for the sickest and most vulnerable individuals in a population, whose multiple chronic conditions, pain and other serious symptoms, functional dependency, cognitive impairment and other mental illnesses, frailty, and high family caregiver burden (Smith et al., 2010; Walke et al., 2006) converge to drive the high use of health care services (Komisar and Feder, 2011). Adequate and relatively inexpensive social services could lower demand for expensive health care services for some people nearing the end of life. For example, providing adequate caregiver training, eliminating safety risks in the home, or provid-
ing nutrition services could prevent many situations that lead to 911 calls, emergency department visits, and hospitalizations (Bachrach et al., 2014; Shier et al., 2013). In addition, sufficient support for caregivers at home might prevent the burnout that leads to those calls, visits, and hospitalizations, as well as to long-term institutionalization (AoA, undated; Reinhard et al., 2012).
Some social services could be provided through replication of successful private-sector models in populations served by managed care organizations and, eventually under the ACOs encouraged under the ACA. In this way, as different approaches to providing, tailoring, and targeting social services demonstrated their effectiveness, successful models could be expanded to cover additional population groups and to include additional services. At present, one of the most promising groups in which to expand these models is the dual-eligible population, for whom both great need and funding mechanisms exist.
How would such a service expansion be paid for? The potential savings that would result in the areas of hospital care and emergency services could exceed the cost of expanded social services. In addition, some social services themselves might produce net savings. For example, providing an elderly person daily meals is much less costly than the medical crisis and nursing home placement that result from the consequences of malnutrition (Thomas and Mor, 2013); likewise, providing an air conditioner for an elderly person with asthma is much less expensive than repeat hospitalizations.
Whatever menu of social services is available, at the top of the list should be an assessment of patient and family needs, resources, home environment, and receptivity to assistance (Feinberg, 2012), as well as aid in accessing appropriate benefits. The Senate Commission on Long-Term Care recommended “development and implementation of a standardized assessment tool that can produce a single care plan across care settings for an individual with cognitive or functional limitations” (Senate Commission on Long-Term Care, 2013, p. 43). This approach is the essence of patient-centeredness.
Many of the services listed above (and discussed in the following subsections) may not be needed every day, and they support the caregiver as well as the patient. Keeping the family confident, rested, informed about what to expect and how to handle it, and emotionally supported is essential to maintaining a seriously ill patient in the home. Through the grants to states provided by the National Family Caregiver Support Program under the Older Americans Act, social services are received by only about 700,000 caregivers annually. States work in partnership with area agencies on aging and other local community-service providers to offer information about and assistance in obtaining available services; individual counseling, organization of support groups, and evidence-based caregiver training; respite care;
and limited supplemental services. The Administration on Aging’s national caregiver surveys indicate that these services improve caregiving and “can reduce caregiver depression, anxiety, and stress and enable them to provide care longer, thereby avoiding or delaying the need for costly institutional care” (AoA, undated).
Caregiver Training and Support
As described in Chapter 2, family caregivers are essential in managing the health and social service needs of patients still living at home and bear a strong burden in doing so. Training in the responsibilities of caregiving can help. In a large online survey of a nationally representative sample of almost 1,700 people caring for family members with multiple health problems, almost half of respondents said the training they received had positive effects on the care recipient, including avoiding nursing home placement (p <0.05). Yet such training is, at best, scanty. Some 47 percent of caregivers had never received any training regarding medication management24; 42 percent reported they had to learn wound care on their own; and 37 percent believed more training would be helpful. (These data apply to all caregivers, not just those caring for a family member near the end of life.)
Retrofitting of the Home for Safety and Mobility
Publicly funded health programs generally do not cover home modifications for safety and wheelchair access, for example. The home can be a dangerous place for patients who are frail or at risk of injuries and for the growing number of patients with progressive cognitive disorders. (Fully 80 percent of the care of people with Alzheimer’s disease is provided “free” by family and friends [Horvath et al., 2013].) A randomized controlled efficacy trial of an intervention designed to give informal caregivers easy-to-read information and resources to minimize home injuries found significantly less risky behavior and fewer injuries (p ≤0.000) among members of the intervention group compared with controls. Because of the high costs of care for frail elders who experience falls, wandering, injuries in fires, and so on, even “small effect sizes translate into clinically relevant findings” (Horvath et al., 2013, p. 6).25
_______________
24Medication management included administering intravenous fluids and injections. Most care recipients took several medications: almost half took 5-9 different prescription medications, almost 20 percent took 10 or more prescription medications, and almost three-quarters took one or more over-the-counter drugs or supplements as well (Reinhard et al., 2012).
25The intervention was designed to require little, if any, professional staff time, and not counting the occasional need for a piece of specialized equipment, such as a tub transfer bench, the cost per family of the Home Safety Toolkit booklet and sample items was $210.
Meals and Nutrition Services
Buying food, cooking, and preparing meals are essential daily activities that become more difficult when one is caring for someone with an advanced serious illness living at home. Forty-one percent of caregivers in the AARP survey cited above were involved in preparing food for special diets, suggesting a need for nutrition counseling. This task involves more than “help with meals” and may include meal planning and cooking, more complicated and expensive food shopping, precise measurement, and laborious feeding for patients who have trouble swallowing. More than one-half of family caregivers surveyed found mealtime tasks difficult to carry out (Reinhard et al., 2012).
As a striking example of the impact of social services, results of a recent study suggest that among ostensibly “low-need” people aged 60 and older, home-delivered meals could mean the difference between living at home and needing nursing home placement (Thomas and Mor, 2013).26 For almost 60 percent of the study subjects, home-delivered meals provided at least half of their daily food intake. The analysis revealed that if every state increased the number of seniors receiving home-delivered meals by a mere 1 percent, the resultant decline in the number of nursing home residents would yield initial savings to state Medicaid programs overall of more than $109 million per year. Ten states would save more than $3 million, and half would save at least $1 million.
The fragility of the nation’s food programs for the elderly was demonstrated by the 2013 cuts to the nutrition programs under the Older Americans Act resulting from the federal budget sequestration. These programs expected to lose $41 million in federal funding, equivalent to the cost of 19 million meals (MOWAA, undated).
Family Respite
The shift to encouraging care at home cannot be accomplished successfully without addressing the concomitant need to support family caregivers. Burnout “is the point at which caregivers are often no longer able to continue in their caring roles and care recipients are at greatest risk of institutionalization” (Lilly et al., 2012, p. 104). Much has been written about the problem of caregiver burden and burnout, but the programmatic changes and investments that would prevent and ameliorate the problem fall short. The Senate Commission on Long-Term Care made detailed
_______________
26Among those included in this study, 70 percent were at least 75; 40 percent needed help with bathing, dressing, eating, using the toilet, and transferring into or out of a bed or chair; and 85 percent needed help with light housework, taking medications, managing money, and shopping for groceries.
recommendations about ways to strengthen supports for family caregivers (Senate Commission on Long-Term Care, 2013, p. 51).
Transportation
The accretion of family needs not adequately addressed in the community can influence the decision to admit a person to long-term care. An analysis of factors affecting that decision, conducted within the Connecticut Home Care Program for Elders (which serves approximately 14,000 state residents aged 65 and older), identified a lack of transportation for both medical and nonmedical purposes as one of these factors (Robison et al., 2012). Existing programs for meeting this need often have limitations, such as not transporting people across county or other jurisdictional lines, not providing assistance in lifting or transferring the patient from home to vehicle along with the transportation, or permitting patients to be accompanied by only certain categories of support personnel.
A proven approach to meeting this fundamental need was tested in the Cash and Counseling demonstration program, which directed cash to disabled beneficiaries with which to hire and direct their own workers.27 The program served Medicaid recipients with a range of disabilities across the age spectrum, not specifically the end-of-life population. In a randomized trial, this program showed that moderate to large reductions in unmet transportation needs could be accomplished and that participants were highly satisfied with the transportation assistance received (Carlson et al., 2007). The Cash and Counseling program is now active in 15 states.
Comprehensive Approaches
A review of seven innovative U.S. care models suggests ways in which social issues facing people with complex medical needs can be addressed (Shier et al., 2013).28 The individual projects used different designs and collected different data, yet all showed a number of positive outcomes, including “encouraging indications that greater attention to social supports may benefit patients and payers alike” (Shier et al., 2013, p. 547). All of
_______________
27The Cash and Counseling program allowed participants to purchase a range of services. Under the program, participants “appeared to receive care at least as good as that provided by agencies, in that they had the same or an even lower incidence of care-related health problems” (Carlson et al., 2007, p. 481).
28The models are the Vermont Blueprint for Health, Senior Care Options (Boston), HealthCare Partners Comprehensive Care Program (California), Mercy Health System (Pennsylvania), Geriatric Resources for Assessment and Care of Elders (GRACE) (Indianapolis, Indiana), Care Management Plus (Utah), and the Enhanced Discharge Planning Program (Chicago, Illinois).
the programs conducted baseline health and social assessments, developed individualized care plans, and made referrals to or arranged for social services. They used interdisciplinary care teams, closely involved primary care clinicians, and used electronic records. Most also used standardized intervention protocols, provided specialized training for service providers, and conducted ongoing monitoring. As these models and others develop under the ACA, their impact on both the quality and costs of care may provide insights to inform the development of new programs.
THE CHANGING HEALTH CARE SYSTEM: FINANCING AND ORGANIZATION
The financing and organization of the U.S. health care system are undergoing significant changes that have major implications for end-of-life care. These changes are resulting from the ACA, as well as from private-sector payment initiatives and state policies.
Changes Under the Affordable Care Act
Changes in financial incentives and organizational arrangements resulting from the ACA could have wide-ranging effects on Americans nearing the end of life. Specific opportunities arise from the new arrangements that involve risk sharing by Medicare providers, including ACOs, patient-centered medical homes, and bundled payments, as well as recently instituted penalties for 30-day readmissions, hospital mortality, and poor patient experience scores. These and other innovations under the ACA have spurred interest, discussed earlier, in meeting the needs of the nation’s sickest and most vulnerable patients in their own homes and communities as an alternative to costly emergency department visits, hospital stays, and institutional care.29
In addition, the new CMS Innovation Center has the broad goal of working toward better care for patients, healthier communities, and lower costs through improvements in the system of care. The center’s priorities are testing new payment and service delivery models, evaluating results and promoting best practices, and working with diverse stakeholders to develop new models for testing.
_______________
29For a detailed list of the ACA provisions affecting a related area—cancer care—see IOM (2013d, pp. 85-90). For detailed information that includes citations of specific statutory provisions, see Meier (2011, pp. 367-369).
Expansion of Home- and Community-Based Services
To accelerate the long-term trend of expanding home- and community-based services, described earlier, the ACA originally included a Community Living Assistance Services and Supports (CLASS) Act, which would have instituted a voluntary, national, federally administered long-term care insurance program. Implementation of this program was abandoned in 2011 because of persistent concerns about its costs and sustainability (Appleby and Carey, 2011).
Nevertheless, the ACA attempts to counter Medicaid’s continuing institutional bias by supporting home- and community-based services (Miller, 2012). For example, the Balancing Incentive Payments program provides grants to states for increasing access to noninstitutional care. The “Money Follows the Person” Rebalancing Demonstration Grants program has been strengthened and expanded. By the end of 2012, it had helped only a small number of people—around 31,000—with chronic conditions and disabilities transition from institutions to the community. It now has the participation of 44 states and the District of Columbia (CMS, undated-b).
The Financial Alignment Initiative
Among the most important provisions of the ACA with the potential to effect major changes in care for people with serious advanced illnesses and to generate cost savings is the establishment of the federal Medicare-Medicaid Coordination Office. This office is charged with facilitating the integration and alignment of federal Medicare and state Medicaid funding into a single source of financial support (CMS, 2013c). The office’s State Demonstrations to Integrate Care for Dual Eligible Individuals program, starting in 15 states, is aimed at breaking down payment silos by providing funds from both programs to an insurer or provider group that agrees to accept risk or participate in shared savings, and that may then match these dollars to patients’ social and medical needs (CMS, 2012; Gore and Klebonis, 2012). This merging of funding streams creates an opportunity and an incentive for state Medicaid programs to seek efficiencies in care delivery for dual-eligible individuals, as opposed to the problematic cost and care shifting that currently occurs.
In a separate Financial Alignment Initiative, CMS will test two models that can be used by states to better integrate primary, acute, behavioral health, and long-term services and supports for Medicare-Medicaid beneficiaries:
- Under the capitated model, a state, CMS, and a health plan enter into a three-way contract, and the plan receives a prospective
- blended Medicare and Medicaid payment to provide comprehensive, coordinated care.
- Under the managed fee-for-service model, a state and CMS enter into an agreement by which the state can benefit from savings resulting from initiatives designed to improve quality and reduce costs for both Medicare and Medicaid (CMS, 2014a).
Not all states are expected to participate in this program, and those that do may find it difficult to coordinate medical and long-term services and supports for the highest-risk participants. At present, individuals who enroll in hospice are excluded from these alignment projects.
Bundled Payments
Another policy trend is the development and promotion of alternatives to fee-for-service reimbursement so as to “maximize good clinical outcomes, enhance patient and physician satisfaction and autonomy, and provide cost-effective care,” as well as to promote evidence-based care (Rich et al., 2012; Schroeder and Frist, 2013, p. 2029). A prime example is the development of bundled payment approaches that cover episodes of care. Instead of reimbursing each provider separately, bundled payment systems pay a single price for a bundle of defined and related services from multiple providers associated with a single episode of care. In theory, bundled payments eliminate incentives to maximize reimbursement that were artifacts of the siloed payment system. Depending on which community-based services are included in the bundle, they may reduce cost shifting between Medicare and Medicaid. They are also expected to provide new incentives for greater care coordination and increased efficiency.
At present, CMS’s Bundled Payments for Care Improvement Initiative specifically excludes hospice services (CMS, 2013d). These services may eventually be included in appropriate bundles if ways can be found to risk-adjust for the hospice population (Dobson et al., 2012).
The committee notes that new payment approaches have almost always been accompanied by unintended consequences as those affected seek to maximize revenues under the different rules and arrangements. Bundled payments could create perverse incentives affecting health care expenditures, such as incentives to increase the volume of bundled episodes and to make greater use of services not included in the bundle. They could also lead to problems in quality and access, such as stinting on care or selecting against patients with higher likely costs (Feder, 2013; Weeks et al., 2013; Wilensky, 2014). Various strategies for forestalling these potential negative effects are being discussed (see Appendix D).
Accountable Care Organizations
The ACA encourages the development of ACOs, which CMS describes as
groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high quality care to their Medicare patients. The goal of coordinated care is to ensure that patients, especially the chronically ill, get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors. (CMS, 2013e)
Under the Shared Savings Program, Medicare will continue to pay individual providers and suppliers for specific items and services as it currently does under the Medicare fee-for-service payment system. In addition, CMS will develop a performance measurement benchmark for each ACO to determine whether it qualifies to receive shared savings (or, for “pioneer” ACOs [see below] that have elected to accept responsibility for losses, whether the ACO will be held accountable for those losses). The benchmark is an estimate of what the total Medicare Parts A and B fee-for-service expenditures would have been absent the ACO and will take into account beneficiary characteristics and other factors that may affect health care service needs (the benchmark does not take into account the social environment or functional status of the patient, except that he or she is eligible for Medicaid) (CMS, 2013e). This feature is complicated by the fact that ACOs cannot prevent enrollees from seeking care from providers that are not part of the ACO.
ACOs update the original health maintenance organization concept and could prove extremely helpful to people with advanced serious illnesses given the importance of effective care coordination to high-quality care, as discussed earlier (Berwick, 2011). Medicare offers several ACO programs:
- As of December 2013, the Medicare Shared Savings Program included more than 360 ACOs serving more than 5.3 million Medicare beneficiaries. ACOs and Medicare share any savings they achieve by lowering the growth in health care costs and must meet established standards for high-quality care.
- The Advance Payment ACO Model is a supplementary incentive program for selected participants in the Shared Savings Program. It involves 35 smaller ACOs (rural and physician based) that lack access to capital for investing in infrastructure and care coordination. These ACOs receive an advance on the shared savings they are expected to earn that reflects both fixed and variable start-up costs.
- Beginning in 2012, the Medicare program initiated demonstrations that entailed contracting with a subset of pioneer ACOs, enabling them to move more rapidly from a shared savings to a population-based payment model (see Appendix D). These pioneer ACOs must assume the risk for any losses they incur (that is, if their cost increases exceed those of regular fee-for-service Medicare in their locale); however, if their cost increases fall below those of fee-for-service Medicare by a statistically significant amount, they share those savings with the Medicare Trust Fund in the form of bonus payments.
In 2011, almost one-third of patients in the full complement of ACOs were aged 80 or older, and the average (mean) age was 73.5. Sixteen to 17 percent of enrollees were eligible for Medicaid. Diabetes was their most common chronic condition, affecting around 30 percent (Epstein et al., 2014).
In their first year of operations, the 32 pioneer ACO plans did achieve some measurable quality improvements and had mixed financial results. Overall, they saw a 0.3 percent cost growth for their nearly 670,000 beneficiaries, compared with a 0.8 percent cost growth in fee-for-service Medicare in the same local markets. Savings were not evenly distributed across plans, with 18 achieving below-budget spending and 14 experiencing above-budget spending (Patel and Lieberman, 2013). Seven of the plans abandoned participation in the pioneer program and switched to the regular Medicare Shared Savings Program, and two abandoned their ACO efforts entirely, in part because of their objections to the program’s quality metrics and administrative complexity.
Because these programs and markets are in transition, it is too early to make more than a preliminary judgment about the impact of ACOs on health care quality and costs. Nonetheless, experience to date suggests that the ACO model remains attractive to many providers, and that most are achieving both quality improvements and some reductions in cost growth. Overall first-year savings for the nearly 670,000 beneficiaries participating in the pioneer ACO program were estimated at $155.4 million (L&M Policy Research, 2013). These gains were made despite the program’s being “incredibly ambitious, even for the most advanced health systems” (Damore and Champion, 2013).
Proposed ACO improvements include new CMS policies to encourage more physicians and Medicare beneficiaries to participate, perhaps by raising Medicare premiums for nonparticipating beneficiaries, and improving ACOs’ ability to manage care (Lieberman, 2013). A specific problem for people with advanced serious illnesses is that beneficiaries placed in postacute care or institutional settings following hospitalization may no longer
belong (or be “attributable”) to the ACO if those settings are not participants in the ACO. As a result, ACA-related efforts to coordinate care could omit a vulnerable and costly population.
Other Provisions of the Affordable Care Act
Hospice and home care Changes to hospice under the ACA include a demonstration program on value-based purchasing and a demonstration program to study concurrent care for Medicare beneficiaries. CMS announced in March 2014 that it will allow up to 30 hospices to participate in a 3-year concurrent care program starting in summer 2014 (CMS, 2014b). “Concurrent care” would allow Medicare hospice patients to continue receiving cure-oriented treatments. Under one provision of the act that has been implemented, children enrolled in hospice and covered by Medicaid now can obtain simultaneous disease treatment (Rau, 2013).
Medicare payments for both hospice and home care are being reduced. Hospice payments will decline by 11.8 percent over the next decade—this despite the claims of advocates that hospice’s highly labor-intensive model does not lend itself to the productivity (and savings) gains possible in other components of the health care system.30 For home care, reductions have been instituted for standard episode payments, unusually costly “outlier” cases, and annual updates. Reduced payments to these community providers may have implications for access to and quality of care for beneficiaries as smaller programs close and larger ones gain incentives to stint on costly treatments.
Pay-for-performance In accordance with the principle of pay-for-performance, the ACA penalizes hospitals that experience higher-than-expected readmission rates within 30 days of patient discharge. This policy places a premium on discharge planning and coordination of posthospitalization care, but it also could hurt inner-city public hospitals that treat sicker and poorer patients with fewer family or community resources (Press et al., 2013). Physicians, too, are under greater pressure to provide value, as defined by conformance with both quality measures and cost controls.
Gaps in the Affordable Care Act
From the standpoint of care of patients with advanced serious illnesses, the ACA has several noteworthy gaps:
_______________
30This cut is in addition to a phase-out of the Budget Neutrality Adjustment Factor used to calculate the Medicare hospice wage index, and will result in an additional reduction in hospice reimbursement of approximately 4.2 percent (NHPCO, undated).
- It does not measure or reward greater access to coordinated, compassionate care for people with advanced serious illnesses. At present, moreover, it specifically excludes hospice beneficiaries from some of the major innovations under the act, which means opportunities to learn from—and improve—their care experiences are being lost.
- MedPAC has explored carving in hospice care under Medicare Advantage plans, thereby making them responsible for hospice costs (Harrison and Neuman, 2013). Doing so might pave the way for concurrent care, which at present remains a gap under the ACA.
- The act is not required to include home-based palliative care as a covered service.
- The act does not improve prospects for a more effective or financially stable long-term care system that better matches patient and family needs with social services.
- The act establishes no mechanism for reimbursing clinicians for the extensive and repeated conversations necessary to engage in advance care planning with patients and families or for requiring that they honor patients’ preferences regarding end-of-life care.31
The ACA is not the last word in this round of health care reform, just as Medicare was not the last word in health care financing for the elderly in 1966 (Skocpol, 2010). Even since the new law’s enactment, health policy experts have proposed changes,32 some of which could have a positive effect on care at the end of life if they
- were flexible and comprehensive, tailoring the mix and intensity of services to patient and family needs as they evolve over time;
- improved accessibility, reaching underserved populations and enabling early palliative care for those not imminently dying by
_______________
31Excellus BlueCross BlueShield has established an enhanced reimbursement program for physicians trained to conduct more thorough advance care planning discussions for seriously ill patients. This program recognizes the amount of time needed for such discussions and the fact that more than a single discussion may be required (http://www.compassionandsupport.org/index.php/for_professionals/molst_training_center/provider_training [accessed December 16, 2014]).
32One proposal would create a new Medicare option called “Medicare Essential.” This proposal would combine Medicare Parts A, B, and D and supplemental “Medigap” coverage to save costs, improve coordination of care, and promote shared decision making (Davis et al., 2013). Another proposal, developed by the Bipartisan Policy Center’s Health Care Cost Containment Initiative, would establish Medicare Networks as a more full-service alternative to ACOs (Daschle et al., 2013). A new Medicare Comprehensive Care program would be established under another major reform proposal, which would also seek to make Medicaid more “person-focused” (Antos et al., 2013).
- establishing required standards for accreditation and participation in Medicare or Medicaid;
- provided for high-quality medical care in the community, through, for example, telemonitoring, round-the-clock access to a nurse, and medication management;
- provided nonmedical support services, including those described earlier in this chapter; and
- entailed measurement of quality of care for those with advanced serious illnesses, multiple chronic conditions, frequent transitions, and functional impairments to ensure accountability and transparency.
Private-Sector Payment Initiatives
Many reform efforts focused on care of people with advanced serious illnesses are taking place in the private sector. Private insurers and managed care plans are free to experiment broadly with strategies for reducing their costs by affecting the behavior of both enrollees and providers, whereas government programs generally focus only on the latter. A frequent shortcoming is the lack of rigorous independent evaluation of these private initiatives in terms of access, quality, and costs.
One of the most promising initiatives coming out of the private sector—one that meets at least the first three principles on the above list—is concurrent care, a model that allows patients to receive hospice-like services and disease treatments at the same time. This model avoids the perceived “terrible choice” between conventional treatment and comfort measures. Examples of the concurrent care approach include the following:
- Highmark, Inc. (Pittsburgh, Pennsylvania) has a program titled Advanced Illness Services: Enhancing Care at End of Life, which serves very ill Medicare Advantage beneficiaries who live at home, use outpatient department services, and wish to receive palliative care. Patients with an approximately 1-year prognosis receive up to 10 mainly consultative home or outpatient visits by hospice or palliative care professionals concurrently with disease treatment.
- Blue Cross Blue Shield of Michigan expanded hospice eligibility to patients with a life expectancy of up to 12 months rather than the usual 6, and permits concurrent care (BCBSM, 2009).
- Kaiser-Permanente deploys an interdisciplinary in-home palliative care team to provide concurrent care. The team includes physicians, nurses, and social workers, supplemented as needed by chaplains (if desired); bereavement coordinators; home health aides; pharmacists; dietitians; physical, occupational, and speech therapists; and
- volunteers. A study of the impact of this model found that patients were satisfied with the care they received, and the likelihood of dying at home increased, while emergency department visits and hospitalizations declined. The result was significantly lower costs, after controlling for survival, age, severity of illness, and primary disease (Brumley et al., 2007).33
- Sutter Health, based in northern California, has developed an Advanced Illness Management program to coordinate palliative care across settings, including hospitals, physician offices, and patients’ homes. The program also seeks to boost hospice utilization and duration. Initial evaluation results included improved satisfaction on the part of patients, families, and physicians, as well as substantial savings. In this program, African American and white patients were equally likely to choose hospice (Meyer, 2011). The Sutter approach retains fee-for-service reimbursement (AHRQ, 2013).
- Aetna’s concurrent care model, which has been in place for about a decade, uses a comprehensive case management approach. Nurse care managers with special training in palliative care work with Medicare Advantage and commercially insured beneficiaries having a prognosis of about 12 months. They coordinate care, provide education and support, and help in symptom management. Beneficiary and family satisfaction is high. Hospice utilization was more than double for the case management group (70 percent) compared with a control group of patients (30 percent) (Spettell et al., 2009). Medical costs for people in the program were approximately $17,161—22 percent less than costs for a matched historical control population ($22,030) (Krakauer et al., 2009).
State Policies
The committee did not review in detail opportunities for states to improve systems of care for people nearing the end of life. Clearly, however, state actions in a number of domains can affect the quality, availability, and costs of care for people with advanced serious illnesses and nearing death (Christopher, 2003). Many states have initiated coalitions to contribute to policy reform at the state level and have engaged in a variety of activities
_______________
33In this study, researchers found a strong trend toward shorter survival in the palliative care group (196 days versus 242 days), potentially attributable to undetected problems with randomization between the palliative care and usual care groups, how patient preferences may have changed over time, or closer adherence to patient preferences in the palliative care group. This result is in conflict with other research indicating longer survival in palliative care programs (Temel et al., 2010; see Chapter 2), and further evaluation of the program model may be necessary to explain this finding.
to improve clinical care, program administration, and professional education; increase access to quality end-of-life care; increase the proportion of people in the state who have engaged in advance care planning; and support a range of public policies to further these efforts. Twenty-four state and local coalitions were funded under the Robert Wood Johnson Foundation’s Community-State Partnerships to Improve End-of-Life Care program (RWJF, 2004).
Other examples of state policies that can have a significant effect on end-of-life care include
- rules affecting Medicaid eligibility and benefits;
- rules governing state Medicaid managed care programs;
- low Medicaid reimbursements that make it difficult for recipients to obtain physician care;
- regulation and oversight of health facilities (for example, nursing homes, hospice, home health programs, and hospitals), including certificate-of-need programs;
- regulation of emergency medical services;
- scope-of-practice laws that limit the roles and responsibilities of, for example, nurse practitioners;
- programs and policies that support patients at home and their caregivers;
- laws enabling Physician Orders for Life-Sustaining Treatment (POLST; see Chapter 3) or otherwise covering advance care planning; and
- approaches to malpractice enforcement conveying the impression that providers must “do everything for a patient.”
Although there is evidence that concerns about malpractice liability affect physician practices, including, for example, their adherence to patients’ advance directives (see Chapter 3), some physicians’ anxiety about being sued may not be based in fact. A Congressional Budget Office study estimated that broad malpractice reforms would reduce national health care spending by only 0.5 percent (CBO, 2009). To encourage physicians to honor informed patient and family preferences for care at home, states could establish “safe harbors” protecting clinicians from liability in cases in which unwanted treatments are avoided in accordance with advance care plans. In general, fear of malpractice litigation should not be a compelling practical reason to refuse to honor patients’ preferences. Family lawsuits against physicians who honored a patient’s preference for less aggressive care are virtually nonexistent (Meisel, 2013), and to the contrary, are most likely to occur when a patient or family does not feel respected or heard by a physician.
THE NEED FOR GREATER TRANSPARENCY AND ACCOUNTABILITY
The IOM report HHS in the 21st Century (IOM, 2009) includes the recommendation that the agency improve accountability, which the report describes as requiring a systematic approach encompassing the establishment of critical, measurable goals and clear lines of responsibility; regular reporting and assessment to gauge progress; and corrective action as needed. The report suggests that this management approach is relevant across HHS, within a framework that defines who is accountable to whom and for what purpose. At no time is attention to these tasks more important than when a fundamental overhaul of policy has been initiated, as has occurred with the passage and implementation of the ACA.
As this chapter has shown, past policy initiatives embedded in Medicare, Medicaid, and other federal programs have had many unintended negative consequences—mainly in the forms of perverse and misaligned incentives and uncoordinated services—that have hampered high-quality care for people who have advanced serious illnesses and are nearing the end of life. A time of change is a time to attempt to do better—to establish whether the system is providing value for current patients and to support continued improvements in care for patients in the future. The urgency of undertaking this effort rests on the confluence of three major trends impelling change: the rising complexity and fragmentation of modern health care, unsustainable cost increases, and outcomes that do not reflect the system’s potential (IOM, 2013b).
The concept of value reflects a relationship between quality and costs. A high-value health care intervention is one that is that markedly improves quality at low cost (for example, immunizations). A low-value intervention is one that is of little to no benefit (or even harmful) and is high cost. In the current context, it is clear that recurrent hospitalizations for nursing home residents with advanced dementia are of low value. Improving value in health care is of growing importance to federal and state policy makers in light of the demonstrably poor quality of care despite high Medicare, Medicaid, and other health care expenditures.
Value improvement for clinicians often means having diagnostic and treatment tools and strategies that increase confidence in the effectiveness of their services. To communities and employers, improving value may mean keeping workers who are family caregivers and their care recipients healthier and more productive at lower cost, freeing up funds for infrastructure, education, and other important community activities. And for patients and families, improving value often involves helping them avoid bankruptcy and meeting their personal goals for care and for living as independently as possible, even with a serious chronic condition (IOM, 2010b). The value of
a particular service or program is also important to these groups because spending a great deal on one form of care may leave few resources for other services or programs that might be more beneficial.
Although different actors in the health care system define value differently, the fundamental calculus for value in health care is the health outcome achieved per dollar spent to achieve it:
If all [health] system participants have to compete on value, value will improve dramatically. As simple and obvious as this seems to be, however, improving value has not been the central goal of the participants in the system. The focus instead has been on minimizing short-term costs and battling over who pays what. The result is that many of the strategies, organizational structures, and practices of the various actors in the system are badly misaligned with value for the patient. (Porter and Teisberg, 2006, p. 4)
Many health policy experts are comfortable speaking in terms of benefit-cost ratios, cost-effectiveness, and comparative effectiveness, but clinicians usually are not trained to think in these terms.34 Simply making clinicians more aware of the cost implications of their clinical recommendations for individual patients may be unlikely to affect their decision making without addition support from clinical guidelines that incorporate a value perspective (Ubel et al., 2012).
In the context of value and the desire of policy makers, professionals, and the public to close the gap between the health system’s potential performance and its current shortcomings, “accurate, reliable, and valid measurements are a prerequisite for achieving and assessing progress in areas such as improving the quality of health care delivered to patients, reporting on the status of the health care system, and developing payment policies and financial incentives that reward improvement” (IOM, 2013c, p. 2). In general, “quality measures provide objective descriptors of the consequences of care and transform the nebulous concept of ‘good medicine’ into a measurable discipline” (IOM, 2013d, p. 272). A number of important quality measures relevant to end-of-life care already exist, as discussed in Chapter 2. The National Quality Measures Clearinghouse contains almost 200 measures coded as related to end-of-life care. Despite the number and scope of the existing measures relating to palliative and end-of-life care, there remain important omissions and limitations to existing measures. Most of the listed measures are either disease- or setting-specific; good measures that apply to the highest-cost, highest-risk individuals—those
_______________
34The quality-adjusted life-years (QALYs) metric commonly used to assess the benefits of an intervention must be used with care in the end-of-life context (Yang and Mahon, 2011, p. 1197).
with multiple chronic conditions and/or functional decline who receive care across many settings—are lacking. Few of these quality measures, however, have been integrated into CMS’s value-based purchasing programs, so they as yet have no role in improving care. It would be valuable to assess other ways, aside from value-based purchasing, of effecting improvements in care, as well as the extent to which CMS’s value-based purchasing programs improve care. Public reporting mechanisms for quality measures related to end-of-life care would be useful as well.
Improving the quality of care for Americans nearing the end of life, then, will require the development and implementation of new measures that, for example,
- are more patient-oriented and include population groups with multiple conditions receiving care across multiple settings;
- include demographic groups that are typically underserved;
- measure quality for a broader spectrum of patients, including people enrolled in Medicare Advantage, Medicaid managed care, and hospice and those residing in nursing homes;
- take into account a broader array of patient and family needs, particularly those related to the social services discussed in this chapter;
- measure the adequacy of support for informed choice by patients and families;
- enable assessment of system performance with respect to advance care planning, shared decision making, and provision of spiritual support, all now defined variably across programs and research efforts;
- track whether care provided accords with patients’ values, goals, and informed preferences; and
- capture the full array of costs of care near the end of life, including out-of-pocket expenditures and those associated with informal caregiving.
Prioritization among existing and new quality measures and indicators is likely to be an important future endeavor (Meltzer and Chung, 2014).
Learning health care organizations generate and use accurate, timely, and up-to-date evidence that helps ensure that patients receive the care they need when they need it (IOM, 2007). System learning can take place—and is needed—at the level of the individual clinical practice, the health care institution, the payer, and various levels of government, from entities as small
as a neighborhood health center to those as large as CMS. The measures described above are essential for conducting research that can provide actionable feedback to clinicians, payers, and managers and create a learning health care organization.
In advocating more effective and meaningful efficiency measures and incentives, Neuberg (2009, p. 132) says, “It is not sufficient to simply reward savings and hope that quality and outcomes are maintained.” With good measures of quality of care for people nearing the end of life, important research questions such as the following can be answered:
- How can models of end-of-life care whose effectiveness has been demonstrated be diffused and adopted more widely?
- Do the savings in hospital costs achieved by palliative care hold true for total health care costs? Do they do so if social services are added to the mix?
- How are changes in the organization and financing of the health care system affecting the nature, quality, and costs of care for patients near the end of life? Are there unintended negative consequences, and especially, has the risk of undertreatment increased?
- What are the out-of-pocket expenses, costs, and economic impact for caregivers for people near the end of life, and what social services could help minimize and manage those costs?
- How can geographic variation in intensity of services be reduced to promote access to the best care without under- or overtreatment?
- What are the experiences of patients with advanced serious illnesses enrolled in Medicare Advantage and Medicaid managed care programs, and how do they compare with those of patients having fee-for-service coverage?
- What meaningful-use criteria relating to end-of-life care need to be developed so that emerging electronic health records will collect adequate data on this care?
- What are the most effective ways to tailor and target support services to specific patients and families to meet both their evolving needs and the requirement for program sustainability?
- How can patients, families, and the public best contribute to decisions about the design of end-of-life services, and are their views taken into account?
- Why is the risk for a malpractice action still feared by some clinicians when it is so low?
Moving forward in these areas will require efforts beyond what the ACA has accomplished. In some unintended ways, the ACA may even worsen care for people with serious advanced illnesses if it launches demon-
strations involving bundled payments for discrete episodes of care without integrating long-term services and supports, or if it focuses on transitional care programs that are hospital-centric rather than truly community based (Naylor et al., 2012).
Health services research is needed to help organizations learn how to effect better transitions between hospitals; post-acute care settings, especially nursing homes; and homes. For example, it would be useful to determine the relative contribution of financial incentives, communication gaps, and resource shortages to the care provided to nursing home residents with dementia and to the causes of multiple hospitalizations for preventable conditions.
Other areas worthy of serious investigation that would directly benefit health care organizations, as suggested by the discussion in this chapter, would document the contribution of social services to quality care, and reimbursement approaches that support palliative care at home and in the hospital with full continuity between them. Benefiting patients, families, and providers would be research on approaches for attracting more members of vulnerable minority populations to hospice and ways to improve services for dual-eligible people.
Because of the profound realignment in the U.S. health care system currently under way, meaningful research is needed that is both timely and actionable. Such research can identify important modifications and refinements to these evolving financial and organizational strategies before they become firmly established and more difficult to change. The growing availability of data from electronic health records should facilitate these research efforts.
Finally, information about key end-of-life measures and the results of research need to be made broadly available so that all interested parties can learn from them; can maintain accountability; and can maximize efforts to ensure that end-of-life care is compassionate, high-quality, and affordable for all.
FINDINGS, CONCLUSIONS, AND RECOMMENDATION
Findings
This study yielded the following findings on policies and payment systems to support high-quality end-of-life care.
Fundamental Redesign of Medicare and Medicaid
Incentives under fee-for-service Medicare result in more use of services (for example, hospital days, intensive care, emergency care), more transi-
tions among care settings that are a burden on patients, and late enrollment in hospice, all of which jeopardize the quality of end-of-life care and add to its costs. In addition, payment silos contribute to fragmentation of care, hinder coordination across providers, and encourage inappropriate utilization (Aragon et al., 2012; Davis et al., 2012; Gozalo et al., 2011; Grabowski and O’Malley, 2014; Segal, 2011; Teno et al., 2013).
Integration of Health Care and Social Services
Evaluations of programs that integrate health care and long-term social services indicate that the additional supports may reduce hospitalizations and health care costs while improving enrollees’ quality of life. What makes such programs financially sustainable is an appropriate reimbursement level, along with careful targeting of services to individuals at highest risk of health care utilization (including hospitalization and nursing home placements) and tailoring of the services to individual/family needs as they evolve over time. Successful existing models need to be implemented more widely (Brown and Mann, 2012; Brown et al., 2012; Senate Commission on Long-Term Care, 2013; Unroe and Meier, 2013).
Expansion of Palliative Care
Palliative care interventions, including hospice, are effective in improving important patient outcomes, providing care more consonant with most patients’ and families’ informed preferences, and potentially reducing the costs for both public and private payers by avoiding unnecessary hospitalizations and use of intensive care. Changes throughout the health care system are needed to increase incentives for providing comprehensive palliative care (Brumley et al., 2007; Gade et al., 2008; Krakauer et al., 2009; Meyer, 2011; Morrison et al., 2008, 2011; Penrod et al., 2010; Rabow et al., 2013).
Increased Transparency and Accountability
Changes in the payment system under the ACA, as well as any future changes specifically affecting Americans nearing the end of life, need to be carefully monitored for their effects—intended and unintended—on this highly vulnerable population. To this end, relevant quality standards and actionable measures are needed (IOM, 2013b,c; Naylor et al., 2012).
Conclusions
At present, the U.S. health care system is ill designed to meet the needs of patients near the end of life and their families. The system is geared to providing acute care aimed at curing disease, but not at providing the comfort care most people near the end of life prefer. The financial incentives built into the programs that most often serve people with advanced serious illnesses—Medicare and Medicaid—are not well coordinated, and the result is fragmented care that increases risks to patients and creates avoidable burdens on them and their families. From a system perspective, fragmented, uncoordinated care and unwanted and unnecessary acute care services—which in the current system constitute “default care”—are extremely costly. At the same time, many of the practical, day-to-day social services that would allow people near the end of life to live in safety and comfort at home, where most prefer to be—such as caregiver training and support, meals and nutrition services, and family respite—are not easily arranged or paid for. The palliative care model and other care models that integrate health and social services, when properly implemented, may improve quality of care and reduce the use of expensive services, and could potentially help stabilize and even reduce increases in health care costs for people near the end of life.
Many aspects of the U.S. health care system are changing, and these and future changes may have both beneficial and unintended negative consequences for Americans of all ages near the end of life. For that reason, efforts to ensure the transparency and accountability of the programs that serve this population will need to be scrupulously monitored. Much can be learned from existing successful programs and care delivery models—such as palliative care—that merit rapid expansion.
Recommendation 4. Federal, state, and private insurance and health care delivery programs should integrate the financing of medical and social services to support the provision of quality care consistent with the values, goals, and informed preferences of people with advanced serious illness nearing the end of life. To the extent that additional legislation is necessary to implement this recommendation, the administration should seek and Congress should enact such legislation. In addition, the federal government should require public reporting on quality measures, outcomes, and costs regarding care near the end of life (e.g., in the last year of life) for programs it funds or administers (e.g., Medicare, Medicaid, the U.S. Department of Veterans Affairs). The federal government should encourage all other payment and health care delivery systems to do the same.
Specifically, actions should
-
provide financial incentives for
- − medical and social support services that decrease the need for emergency room and acute care services,
- − coordination of care across settings and providers (from hospital to ambulatory settings as well as home and community), and
- − improved shared decision making and advance care planning that reduces the utilization of unnecessary medical services and those not consistent with a patient’s goals for care;
- require the use of interoperable electronic health records that incorporate advance care planning to improve communication of individuals’ wishes across time, settings, and providers, documenting (1) the designation of a surrogate/decision maker, (2) patient values and beliefs and goals for care, (3) the presence of an advance directive, and (4) the presence of medical orders for life-sustaining treatment for appropriate populations; and
- encourage states to develop and implement a Physician Orders for Life-Sustaining Treatment (POLST) paradigm program in accordance with nationally standardized core requirements.
Medical and social services provided should accord with a person’s values, goals, informed preferences, condition, circumstances, and needs, with the expectation that individual service needs and intensity will change over time. High-quality, comprehensive, person-centered, and family-oriented care will help reduce preventable crises that lead to repeated use of 911 calls, emergency department visits, and hospital admissions, and if implemented appropriately, should contribute to stabilizing aggregate societal expenditures for medical and related social services and potentially lowering them over time.
AARP Public Policy Institute. 2008. A balancing act: State long-term care reform. In Brief 161. http://assets.aarp.org/rgcenter/il/inb161_ltc.pdf (accessed January 29, 2013).
AARP Public Policy Institute. 2013. Medicaid: A program of last resort for people who need long-term services and supports. http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/2013/medicaid-last-resort-insight-AARP-ppi-health.pdf (accessed August 19, 2014).
Administration for Community Living. 2013. New models of community care for older adults and people with disabilities. http://www.acl.gov/About_ACL/FederalInitiatives/CommunityCare.aspx (accessed November 29, 2013).
AHIP (America’s Health Insurance Plans). 2013. Trends in Medigap coverage and enrollment. http://ahip.org/Trends-Medigap-Coverage-Enroll2012 (accessed August 19, 2014).
AHRQ (Agency for Healthcare Research and Quality). 2013. Effective palliative care programs require health system change. http://www.innovations.ahrq.gov/content.aspx?id=3742 (accessed July 16, 2013).
Aldridge Carlson, M. D., C. L. Barry, E. J. Cherlin, R. McCorkle, and E. H. Bradley. 2012. Hospices’ enrollment policies may contribute to underuse of hospice care in the United States. Health Affairs 31(12):2690-2697.
Alpert, A., K. G. Morganti, G. S. Margolis, J. Wasserman, and A. L. Kellermann. 2013. Giving EMS flexibility in transporting low-acuity patients could generate substantial Medicare savings. Health Affairs 32(12):2142-2148.
Altman, S., and D. Shactman. 2011. Power, politics, and universal health care. Amherst, NY: Prometheus Books.
Antos, J., K. Baicker, M. Chernew, D. Crippen, D. Cutler, T. Daschle, F. de Brantes, D. Goldman, G. Hubbard, B. Kocher, M. Leavitt, M. McClellan, P. Orszag, M. Pauly, A. Rivlin, L. Schaeffer, D. Shalala, and S. Shortell. 2013. Bending the curve: Person-centered health care reform: A framework for improving care and slowing health care cost growth. Washington, DC: The Brookings Institution.
AoA (Administration on Aging). 2013. A profile of older Americans: 2013. http://www.aoa.gov/AoARoot/Aging_Statistics/Profile/2013/docs/2013_Profile.pdf (accessed August 6, 2014).
AoA. undated. National Family Caregiver Support Program (OAA Title IIIE). http://www.aoa.gov/aoa_programs/hcltc/caregiver/index.aspx (accessed February 3, 2014).
Appleby, J., and M. A. Carey. 2011. CLASS dismissed: Obama administration pulls plug on long-term care program. Kaiser Health News, October 14. http://www.kaiserhealthnews.org/Stories/2011/October/14/CLASS-Act-Implementation-Halted-By-Obama-Administration.aspx (accessed January 5, 2014).
Aragon, K., K. Covinsky, Y Miao, W. J. Boxcardin, L. Flint, and A. Smith. 2012. Medicare post-hospitalization skilled nursing benefit in the last six months of life. Archives of Internal Medicine 172(20):1573-1579.
Bachrach, D., Pfister, H., Wallis, K., and Lipson, M. 2014. Addressing patients’ social needs: An emerging business case for provider investment. Washington, DC: Manatt Health Solutions. http://www.commonwealthfund.org/~/media/files/publications/fund-report/2014/may/1749_bachrach_addressing_patients_social_needs_v2.pdf (accessed May 29, 2014).
Bass, D. M., K. S. Judge, A. L. Snow, N. L. Wilson, R. Morgan, W. J. Looman, C. A. McCarthy, K. Maslow, J. A. Moye, R. Randazzo, M. Garcia-Maldonado, R. Elbein, G. Odenheimer, and M. E. Junik. 2013. Caregiver outcomes of partners in dementia care: Effect of a care coordination program for veterans with dementia and their family members and friends. Journal of the American Geriatrics Society 61(8):1377-1386.
Baum, A. S., and D. W. Burnes. 1993. A nation in denial: The truth about homelessness. Boulder, CO: Westview Press.
Bazelon Center for Mental Health Law. 2012. Medicare. http://www.bazelon.org/Where-We-Stand/Access-to-Services/Medicare.aspx (accessed December 5, 2013).
BCBSM (Blue Cross Blue Shield of Michigan). 2009. Blue Cross Blue Shield of Michigan expands hospice services. News release. August 26. Detroit, MI: BCBSM. http://www.bcbsm.com/content/microsites/blue-cross-blue-shield-of-michigan-news/en/index/news-releases/2009/august-2009/blue-cross-blue-shield-of-michigan-expands-hospice-services.html (accessed July 15, 2013).
Berwick, D. M. 2011. Making good on ACOS’ promise—The final rule for the Medicare Shared Savings Program. New England Journal of Medicine 365(19):1753-1756.
Bipartisan Policy Center. 2012. What is driving U.S. health care spending? America’s unsustainable health care cost growth. http://bipartisanpolicy.org/sites/default/files/BPC%20Health%20Care%20Cost%20Drivers%20Brief%20Sept%202012.pdf (accessed December 2, 2013).
Bishop, T. F., M. J. Press, S. Keyhani, and H. A. Pincus. 2014. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry 71(92):176-181.
Boards of Trustees, Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. 2013. 2013 annual report of the boards of trustees of the federal hospital insurance and supplementary medical insurance trust funds. http://downloads.cms.gov/files/TR2013.pdf (accessed August 12, 2014).
Bona, K., J. Bates, and J. Wolfe. 2011. Massachusetts’ Pediatric Palliative Care Network: Successful implementation of a novel state-funded pediatric palliative care program. Journal of Palliative Medicine 14(11):1217-1223.
Bona, K., V. Dussel, L. Orellana, T. Kang, R. Geyer, C. Feudtner, and J. Wolfe. 2014. Economic impact of advanced pediatric cancer on families. Journal of Pain and Symptom Management 47(3):594-603.
Bradley, E. H., and L. A. Taylor. 2013. The American health care paradox: Why spending more is getting us less. New York: Public Affairs.
Brown, R., and D. R. Mann. 2012. Best bets for reducing Medicare costs for dual eligible beneficiaries: Assessing the evidence. Issue Brief. Menlo Park, CA: KFF.
Brown, R. S., D. Peikes, G. Peterson, J. Schore, and C. M. Razafindrakoto. 2012. Six features of Medicare coordinated care demonstration programs that cut hospital admissions of high-risk patients. Health Affairs 31(6):1156-1165.
Brumley, R., S. Enguidanos, P. Jamison, R. Seitz, N. Morgenstern, S. Saito, J. McIlwane, K. Hillary, and J. Gonzalez. 2007. Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. Journal of the American Geriatrics Society 55(7):993-1000.
Bureau of the Census. 2013. Aging in the United States: Past, present, and future. http://www.census.gov/population/international/files/97agewc.pdf (accessed July 4, 2013).
CAPC (Center to Advance Palliative Care). 2011. America’s care of serious illness: A state-by-state report card on access to palliative care in our nation’s hospitals. New York: CAPC. http://reportcard.capc.org/pdf/state-by-state-report-card.pdf (accessed September 19, 2013).
CAPC. 2013. Growth of palliative care in U.S. hospitals: 2013 snapshot. http://www.capc.org/capc-growth-analysis-snapshot-2013.pdf (accessed January 27, 2014).
Capretta, J. C. 2013. The role of Medicare fee-for-service in inefficient health care delivery. Washington, DC: American Enterprise Institute. http://www.aei.org/papers/health/entitlements/medicare/the-role-of-medicare-fee-for-service-in-inefficient-health-care-delivery (accessed July 1, 2013).
Carlson, B. L., L. Foster, S. B. Dale, and R. Brown. 2007. Effects of Cash and Counseling on personal care and well-being. Health Services Research 42(1, Part 2):467-487.
CBO (Congressional Budget Office). 2009. Letter to the Honorable Orrin G. Hatch. http://www.cbo.gov/sites/default/files/cbofiles/ftpdocs/106xx/doc10641/10-09-tort_reform.pdf (accessed July 11, 2013).
CBO. 2013. Dual-eligible beneficiaries of Medicare and Medicaid: Characteristics, health care spending, and evolving policies. http://www.cbo.gov/sites/default/files/cbofiles/attachments/44308_DualEligibles.pdf (accessed July 7, 2013).
Chamberlain, J. M., S. Krug, and K. N. Shaw. 2013. Emergency care for children in the United States. Health Affairs 32(12):2109-2115.
Christopher, M. 2003. Championing end-of-life care policy change. http://www.rwjf.org/content/dam/files/legacy-files/article-files/2/State_Initiatives_EOL19.pdf (accessed January 9, 2014).
CMS (Centers for Medicare & Medicaid Services). 2012. State demonstrations to integrate care for dual eligible individuals. http://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/StateDemonstrationstoIntegrateCareforDualEligibleIndividuals.html (accessed December 2, 2013).
CMS. 2013a. Medicare hospice data trends, 1998-2009. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice/Medicare_Hospice_Data.html (accessed May 30, 2014).
CMS. 2013b. Guidance to states using 1115 demonstrations or 1915(b) waivers for managed long-term services and supports programs. http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Delivery-Systems/Downloads/1115-and-1915b-MLTSS-guidance.pdf (accessed July 5, 2013).
CMS. 2013c. About the Medicare-Medicaid Coordination Office. http://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office (accessed December 2, 2013).
CMS. 2013d. Bundled payments for care improvement initiative: General information. http://innovation.cms.gov/initiatives/Bundled-Payments (accessed January 30, 2014).
CMS. 2013e. Accountable care organizations. Baltimore, MD: CMS. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/index.html?redirect=/aco (accessed May 17, 2013).
CMS. 2014a. Financial alignment initiative. http://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/FinancialAlignmentInitiative/FinancialModelstoSupportStatesEffortsinCareCoordination.html (accessed January 30, 2014).
CMS. 2014b. Medicare Care Choices Model. http://innovation.cms.gov/initiatives/Medicare-Care-Choices (accessed August 12, 2014).
CMS. undated-a. Medicare enrollment: National trends, 1966-2010. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareEnrpts/index.html?redirect=/MedicareEnRpts (accessed January 31, 2014).
CMS. undated-b. Money follows the person. http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Long-Term-Services-and-Support/Balancing/Money-Follows-the-Person.html (accessed January 30, 2014).
CMS. undated-c. Medicare 2014 costs at a glance. http://www.medicare.gov/your-medicare-costs/costs-at-a-glance/costs-at-glance.html#collapse-4809 (accessed May 14, 2014).
Coleman, E. A., C. Parry, S. Chalmers, and S. Min. 2006. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine 166(17):1822-1828.
Commonwealth Fund. 2013. Potentially avoidable hospital admissions among vulnerable Medicare beneficiaries. http://www.commonwealthfund.org/Charts/Report/Low-Income-Scorecard/Potentially-Avoidable-Hospital-Admissions-among-Vulnerable-MedicareBeneficiaries.aspx (accessed January 4, 2014).
Commonwealth Fund Commission on a High Performance Health System. 2013. Confronting costs: Stabilizing U.S. health spending while moving toward a high performance health care system. New York: Commonwealth Fund Commission on a High Performance Health System. http://www.commonwealthfund.org/~/media/Files/Publications/Fund%20Report/2013/Jan/1653_Commission_confronting_costs_web_FINAL.pdf (accessed February 22, 2014).
Coughlin, T. A., T. A. Waidmann, and L. Phadera. 2012. Among dual eligibles, identifying the highest-cost individuals could help in crafting more targeted and effective responses. Health Affairs 31(5):1083-1091.
Cuckler, G. A., A. M. Sisko, S. P. Keehan, S. D. Smith, A. J. Madison, J. A. Poisal, C. J. Wolfe, J. M. Lizonitz, and D. A. Stone. 2013. National health expenditure projections, 2012-22: Slow growth until coverage expands and economy improves. Health Affairs 32(10):1820-1831.
Cutler, D. M., and N. R. Sahni. 2013. If slow rate of health care spending growth persists, projections may be off by $770 billion. Health Affairs 32(5):841-850.
Damore, J., and W. Champion. 2013. The Pioneer ACO first year results: A fuller picture. http://healthaffairs.org/blog/2013/07/17/the-pioneer-aco-first-year-results-a-fuller-picture (accessed November 26, 2013).
Dartmouth Atlas of Health Care. 2013. Reflections on variations. Lebanon, NH: Dartmouth College, The Dartmouth Institute for Health Policy and Clinical Practice. http://www.dartmouthatlas.org/keyissues/issue.aspx?con=1338 (accessed June 27, 2013).
Daschle, T., P. Domenici, W. Frist, and A. Rivlin. 2013. Prescription for patient-centered care and cost containment. New England Journal of Medicine 369(5):471-474.
Davis, K., C. Schoen, and S. Guterman. 2013. Medicare essential: An option to promote better care and curb spending growth. Health Affairs 32(5):900-909.
Davis, M. M., M. Devoe, D. Kansagara, C. Nicolaidis, and H. Englander. 2012. “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. Journal of General Internal Medicine 27(12):1649-1656.
Dobson, A., J. E. DaVanzo, S. Heath, M. Shimer, G. Berger, A. Pick, K. Reuter, A. El-Gamil, and N. Manolov. 2012. Medicare payment bundling: Insights from claims data and policy implications. Vienna, VA: Dobson/DaVanzo & Associates, LLC.
Dussel, V., K. Bona, J. A. Heath, J. M. Hilden, J. C. Weeks, and J. Wolfe. 2011 Unmeasured costs of a child’s death: Perceived financial burden, work disruptions, and economic coping strategies used by American and Australian families who lost children to cancer. Journal of Clinical Oncology 29(8):1007-1013.
Elhauge, E., ed. 2010. The fragmentation of U.S. health care: Causes and solutions. New York: Oxford University Press.
Elmendorf, D. 2013. How have CBO’s projections of spending for Medicare and Medicaid changed since the August 2012 baseline? http://www.cbo.gov/publication/43947 (accessed November 26, 2013).
Employment Benefit Research Institute. 2012. Effects of nursing home stays on household portfolios. Issue Brief 372. Washington, DC: Employment Benefit Research Institute. http://www.ebri.org/publications/ib/index.cfm?fa=ibDisp&content_id=5078 (accessed July 6, 2013).
Epstein, A. M., A. K. Jha, E. J. Orav, D. L. Liebman, A. J. Audet, M. A. Zezza, and S. Guterman. 2014. Analysis of early accountable care organizations defines patient, structural, cost and quality-of-care characteristics. Health Affairs 33(1):95-102.
Eva, G., and B. Wee. 2010. Rehabilitation in end-of-life management. Current Opinion in Supportive and Palliative Care 4(3):158-162.
Farley, T. A. 2009. Reforming health care or reforming health? Editorial. American Journal of Public Health 99(4):588-590.
Farragher, J., and S. V. Jassal. 2012. Rehabilitation of the geriatric dialysis patient. Seminars in Dialysis 25(6):649-656.
Feder, J. 2013. Bundle with care—Rethinking Medicare incentives for post-acute care services. New England Journal of Medicine 369(5):400-401.
Feder, J., H. L. Komisar, and N. Niefeld. 2000. Long-term care in the United States: An overview. Health Affairs 19(3):40-56.
Feinberg, L. 2012. Assessing family caregiver needs: Policy and practice considerations. Washington, DC: AARP Public Policy Institute.
Feinberg, L., S. C. Reinhard, A. Houser, and R. Choula. 2011. Valuing the invaluable: 2011 update—The growing contribution and costs of family caregiving. Washington, DC: AARP, Public Policy Institute. http://assets.aarp.org/rgcenter/ppi/ltc/i51-caregiving.pdf (accessed August 27, 2013).
Fishman, J., P. O’Dwyer, H. L. Lu, H. Henderson, D. A. Asch, and D. J. Casarett. 2009. Race, treatment preferences, and hospice enrollment: Eligibility criteria may exclude patients with the greatest needs for care. Cancer 115(3):689-697.
Fox-Grage, W., and Walls, J. 2013. State studies find home and community-based services to be cost-effective. http://www.aarp.org/content/dam/aarp/research/public_policy_institute/ltc/2013/state-studies-find-hcbs-cost-effective-spotlight-AARP-ppi-ltc.pdf (accessed December 2, 2013).
Freeman, R., K. M. Lybecker, and D. W. Taylor. 2011. The effectiveness of disease management programs in the Medicaid population. Hamilton, Ontario, Canada: The Cameron Institute. http://www.fightchronicdisease.org/sites/fightchronicdisease.org/files/docs/Main%20Report%20-%20The%20effectiveness%20of%20DMPs%20in%20the%20Medicaid%20Pop%202011.pdf (accessed December 5, 2013).
Gade, G., I. Venohr, D. Conner, K. McGrady, J. Beane, R. H. Richardson, M. P. Williams, M. Liberson, M. Blum, and R. Della Penna. 2008. Impact of an inpatient palliative care team: A randomized control trial. Journal of Palliative Medicine 11(2):180-190.
Gans, D. G. Kominski, D. H. Roby, A. L. Diamant, X. Chen, W. Lin, and N. Hohe. 2012. Better outcomes, lower costs: Palliative care program reduces stress, costs of care for children with life-threatening conditions. Policy Brief UCLA Center for Health Policy Research PB2012-3:1-8.
Ginsburg, P. B. 2012. Fee-for-service will remain a feature of major payment reforms, requiring more changes in Medicare physician payment. Health Affairs 31(9):1977-1983.
Gold, M. R., G. A. Jacobson, and R. L. Garfield. 2012. There is little experience and limited data to support policy making on integrated care for dual eligibles. Health Affairs 31(6):1176-1184.
Goldfeld, K. S., D. C. Grabowski, D. J. Caudry, and S. L. Mitchell. 2013. Health insurance status and the care of nursing home residents with advanced dementia. JAMA Internal Medicine 173(22):2047-2053.
Gore, S., and J. Klebonis. 2012. Financial alignment models for Medicare-Medicaid enrollees: Considerations for reimbursement. Technical Assistance Brief. http://www.chcs.org/usr_doc/Payment_and_Reimbursement_FINAL.pdf (accessed January 28, 2014).
Gozalo P., J. Teno, S. L. Mitchell, J. Skinner, J. P. Bynum, D. Tyler, and V. Mor. 2011. End-of-life transitions among nursing home residents with cognitive issues. New England Journal of Medicine 365(13):1212-1221.
Grabowski, D. C. 2006. The cost-effectiveness of noninstitutional long-term care services: Review and synthesis of the most recent evidence. Medical Care Research and Review 63(1):3-28.
Grabowski, D. C., and A. J. O’Malley. 2014. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for Medicare. Health Affairs 33(2):244-250.
Greer, J., P. McMahon, A. Tramontano, E. Gallagher, W. F. Pirl, V. Jackson, and J. S. Temel. 2012. Effect of early palliative care on health care costs in patients with metastatic NSCLC. Journal of Clinical Oncology 30(Suppl., abstract 6004).
Greve, P. 2011. Pediatrics: A unique and volatile risk. Journal of Healthcare Risk Management 31(2):19-29.
Gross, D. L., H. Temkin-Greener, S. Kunitz, and D. B. Mukamel. 2004. The growing pains of integrated health care for the elderly: Lessons from the expansion of PACE. Milbank Quarterly 82(2):257-282.
Guterman, S., M. A. Zezza, and C. Schoen. 2013. Paying for value: Replacing Medicare’s sustainable growth rate formula with incentives to improve care. New York: Commonwealth Fund. http://www.commonwealthfund.org/Publications/Issue-Briefs/2013/Mar/Paying-for-Value-Replacing-Medicares-Sustainable-Growth-Rate.aspx (accessed July 1, 2013).
Hackbarth, G. M. 2009. Report to the Congress: Medicare payment policy. Statement before the Subcommittee on Health, Committee on Ways and Means, House of Representatives. Washington, DC: MedPAC. http://www.medpac.gov/documents/Mar09_March%20report%20testimony_WM%20FINAL.pdf (accessed July 29, 2013).
Hackbarth, G. M. 2013. Moving forward from the sustainable growth rate system. Washington, DC: MedPAC. http://www.medpac.gov/documents/04102013_MedPAC_updated_SGR_letter.pdf (accessed July 1, 2013).
Harrison, S., and K. Neuman. 2013. Medicare managed care topics. http://www.medpac.gov/transcripts/MA_topics11_13l.pdf (accessed January 9, 2014).
HHS (U.S. Department of Health and Human Services). 2000. Cost-effectiveness of home and community based services. http://aspe.hhs.gov/daltcp/reports/2000/costeff.htm (accessed August 29, 2013).
HHS. 2005. Medicaid treatment of the home: Determining eligibility and repayment for long-term care. http://aspe.hhs.gov/daltcp/reports/hometreat.htm (accessed February 21, 2014).
HHS. 2014. Long term care: The basics. http://longtermcare.gov/the-basics/how-much-care-will-you-need (accessed August 13, 2014).
HHS and CMS. 2013. Medicare program; FY 2014 hospice wage index and payment rate update; hospice quality reporting requirements; and updates on payment reform; final rule. Federal Register 78:152. http://www.gpo.gov/fdsys/pkg/FR-2013-08-07/pdf/2013-18838.pdf (accessed January 31, 2014).
Hirth, V., J. Baskins, and M. Dever-Bumba. 2009. Program of All-Inclusive Care (PACE): Past, present, and future. Journal of the American Medical Directors Association 10(3): 155-160.
Hodgson, C. 2012. Cost-effectiveness of palliative care: A review of the literature. http://www.hpcintegration.ca/media/36290/TWF-Economics-report-Eng-final-webmar7.pdf (accessed May 17, 2014).
Horvath, K. J., S. A. Trudeau, J. L. Rudolph, P. A. Trudeau, M. E. Duffy, and D. Berlowitz. 2013. Clinical trial of a home safety toolkit for Alzheimer’s disease. International Journal of Alzheimer’s Disease 1-11. http://www.hindawi.com/journals/ijad/2013/913606 (accessed November 27, 2013).
Huskamp, H. A., D. G. Stevenson, M. E. Chernew, and J. P Newhouse. 2010. A new Medicare end-of-life benefit for nursing home residents. Health Affairs 29(1):130-135.
Huynh, T. N., E. C. Kleerup, J. F. Wiley, T. D. Savitsky, D. Guse, B. J. Garber, and N. S. Wenger. 2013. The frequency and cost of treatment perceived to be futile in critical care. JAMA Internal Medicine 173(20):1887-1894.
Hwang, U., M. N. Shah, J. H. Han, C. R. Carpenter, A. L. Siu, and J. G. Adams. 2013. Transforming emergency care for older adults. Health Affairs 32(12):2116-2121.
IOM (Institute of Medicine). 1997. Approaching death: Improving care at the end of life. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2003. When children die: Improving palliative and end-of-life care for children and their families. Washington, DC: The National Academies Press.
IOM. 2007. The learning healthcare system: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2009. HHS in the 21st century: Charting a new course for a healthier America. Washington, DC: The National Academies Press.
IOM. 2010a. The healthcare imperative: Lowering costs and improving outcomes. Washington, DC: The National Academies Press.
IOM. 2010b. Value in health care: Accounting for cost, quality, safety, outcomes, and innovation. Washington, DC: The National Academies Press.
IOM. 2013a. Variation in health care spending: Target decision making, not geography. Washington, DC: The National Academies Press.
IOM. 2013b. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
IOM. 2013c. Core measurement needs for better care, better health, and lower costs: Counting what counts. Washington, DC: The National Academies Press.
IOM. 2013d. Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: The National Academies Press.
IOM. 2013e. Financing long-term services and supports for individuals with disabilities and older adults. Washington, DC: The National Academies Press.
Jacobson, L. 2013. Medicare and Social Security: What you paid in compared with what you get. PolitiFact, February 1. http://www.politifact.com/truth-o-meter/article/2013/feb/01/medicare-and-social-security-what-you-paid-what-yo (accessed July 5, 2013).
Jennings, B., and M. B. Morrissey. 2011. Health care costs in end-of-life and palliative care: The quest for ethical reform. Journal of Social Work in End-of-Life and Palliative Care 7:300-317.
Kamal, A. H., D. C. Currow, C. S. Ritchie, J. Bull, and A. P. Abernethy. 2013. Community-based palliative care: The natural evolution for palliative care delivery in the U.S. Journal of Pain and Symptom Management 46(2):254-264.
Kane, C. K., and D. W. Emmons. 2013. New data on physician practice arrangements: Private practice remains strong despite shifts toward hospital employment. Chicago, IL: American Medical Association. http://www.ama-assn.org/resources/doc/health-policy/prp-physician-practice-arrangements.pdf (accessed February 22, 2014).
Kane, R. L., G. Keckhafer, and J. Robst. 2002. Evaluation of the Evercare Demonstration Program: Final report. http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads/Evercare_Final_Report.pdf (accessed February 22, 2014).
Kane, R. L., S. Flood, B. Bershadsky, and G. Keckhafer. 2004. Effect of an innovative Medicare managed care program on the quality of care for nursing home residents. Gerontologist 44(1):95-103.
Kassner, E. 2013. Home- and community-based services: The right place and the right time. http://blog.aarp.org/2013/08/19/home-and-community-based-services-the-right-place-and-the-right-time (accessed December 2, 2013).
Kellermann, A. L., R. Y. Hsia, C. Yeh, and K. G. Morgani. 2013. Emergency care: Then, now, and next. Health Affairs 32(12):2069-2074.
Kelley, A. S., Deb, P., Du, Q., Carlson, M. D. A., and Morrison, R. S. 2013a. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Affairs 32(3):552-561.
Kelley, A. S., K. McGarry, S. Fahle, S. M. Marshall, Q. Du, and J. S. Skinner. 2013b. Out-of-pocket spending in the last five years of life. Journal of General Internal Medicine 28(2):304-309.
Kemper, P. 1988. The evaluation of the National Long Term Care Demonstration. 10. Overview of the findings. Health Services Research 23(1):161-174.
KFF (The Henry J. Kaiser Family Foundation). 2012. Medicare at a glance. http://kff.org/medicare/fact-sheet/medicare-at-a-glance-fact-sheet (accessed July 2, 2013).
KFF. 2013a. Medicaid: A primer. Key information on the nation’s health coverage program for low-income people. Menlo Park, CA: KFF, Kaiser Commission on Medicaid and the Uninsured. http://kaiserfamilyfoundation.files.wordpress.com/2010/06/7334-05.pdf (accessed August 7, 2014).
KFF. 2013b. A short look at long-term care for seniors. Journal of the American Medical Association 310(8):786.
KFF. 2014. State health facts. http://kff.org/medicare/state-indicator/total-medicare-beneficiaries (accessed January 31, 2014).
Klein, E. 2013. 21 graphs that show America’s health-care prices are ludicrous. Wonkblog. The Washington Post, March 26. http://www.washingtonpost.com/blogs/wonkblog/wp/2013/03/26/21-graphs-that-show-americas-health-care-prices-are-ludicrous (accessed November 27, 2013).
Komisar, H. L., and J. Feder. 2011. Transforming care for Medicare beneficiaries with chronic conditions and long-term care needs: Coordinating care across all services. Washington, DC: Georgetown University. http://www.cahpf.org/docuserfiles/georgetown_trnsfrming_care.pdf (accessed December 2, 2013).
Krakauer, R., C. M. Spettell, L. Reisman, and M. J. Wade. 2009. Opportunities to improve the quality of care for advanced illness. Health Affairs 28(5):1357-1359.
Kumetz, E. A., and J. D. Goodson. 2013. The undervaluation of evaluation and management professional services: The lasting impact of current procedural terminology code deficiencies on physician payment. Chest 144(3):740-745.
L & M Policy Research. 2013. Evaluation of CMMI Accountable Care Organization Initiatives. Washington, DC: L & M Policy Research.
Lakdawalla, D. N., D. P. Goldman, A. B. Jena, and D. B. Agus. 2011. Medicare end-of-life counseling: A matter of choice. Washington, DC: American Enterprise Institute. http://www.aei.org/article/health/entitlements/medicare/medicare-end-of-life-counseling-a-matter-of-choice (accessed July 2, 2013).
Lieberman, S. M. 2013. Reforming Medicare through “Version 2.0” of accountable care. Health Affairs 32(7):1258-1264.
Lilly, M. B., C. A. Robinson, S. Holtzman, and J. L. Botorff. 2012. Can we move beyond burden and burnout to support the health and wellness needs of family caregivers to persons with dementia? Health and Social Care in the Community 20(1):103-112.
Lyons, R. D. 1984. How release of mental patients began. The New York Times. http://www.nytimes.com/1984/10/30/science/how-release-of-mental-patients-began.html?pagewanted=1 (accessed December 3, 2013).
Marmor, T. R., M. L. Barer, and R. G. Evans. 1994. Why are some people healthy and others not? The determinants of health of populations. Piscataway, NJ: Aldine Transaction.
Martin, A. B., M. Hartman, L. Whittle, A. Catlin, and the National Health Expenditure Accounts Team. 2014. National health spending in 2012: Rate of health spending growth remained low for the fourth consecutive year. Health Affairs 33(1):67-77.
Mattke, S., M. Seid, and S. Ma. 2007. Evidence for the effect of disease management: Is $1 billion a year a good investment? American Journal of Managed Care 13(12):670-676. http://www.allhealth.org/briefingmaterials/AJMC-Mattke-1131.pdf (accessed February 22, 2014).
McGinniss, J. M., and W. H. Foege. 1993. Actual causes of death in the United States. Journal of the American Medical Association 270(18):2207-2212.
MedPAC (Medicare Payment Advisory Commission). 2011. The sustainable growth rate system: Policy considerations for adjustments and alternatives. http://www.medpac.gov/chapters/jun11_ch01.pdf (accessed May 15, 2014).
MedPAC. 2013. Report to Congress: Medicare payment policy. http://www.medpac.gov/documents/Mar13_entirereport.pdf (accessed December 1, 2013).
Meier, D. E. 2011. Increased access to palliative care and hospice services: Opportunities to improve value in health care. Milbank Quarterly 89(3):343-380.
Meisel, A. 2013. Presentation at Meeting of the IOM Committee on Approaching Death: Addressing Key End-of-Life Issues, Houston, TX, July 22.
Meltzer, D., and J. W. Chung. 2014. The population value of quality indicator reporting: A framework for prioritizing health care performance measures. Health Affairs 33(1):132-139.
Meyer, H. 2011. Changing the conversation in California about care near the end of life. Health Affairs 30(3):390-393.
Meyer, J., and B. M. Smith. 2008. Chronic disease management: Evidence of predictable savings. http://www.idph.state.ia.us/hcr_committees/common/pdf/clinicians/savings_report.pdf (accessed January 30, 2014).
Miller, E. A. 2012. The Affordable Care Act and long-term care: Comprehensive reform or just tinkering around the edges? Journal of Aging & Social Policy 24(2):101-117.
Mitchell, S. L., J. M. Teno, D. K. Kiely, M. L. Shaffer, R. N. Jones, H. G. Prigerson, L. Volicer, J. L. Givens, and M. B. Hamel. 2009. The clinical course of advanced dementia. New England Journal of Medicine 361(16):1529-1538.
Moffit, R. E., and A. Senger. 2013. Medicare’s rising costs—and the urgent need for reform. Washington, DC: The Heritage Foundation. http://www.heritage.org/research/reports/2013/03/medicares-rising-costsand-the-urgent-need-for-reform (accessed July 25, 2013).
Morrison, R. S., J. D. Penrod, B. Cassel, M. Caust-Ellenbogen, A. Litke, L. Spragens, D. E. Meier. 2008. Cost savings associated with U.S. hospital palliative care consultation programs. Archives of Internal Medicine 168(16):1783-1790.
Morrison, R. S., J. Dietrich, S. Ladwig, T. Quill, J. Sacco, J. Tangeman, and D. E. Meier. 2011. Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Affairs 30(3):454-463.
Moses, H., D. H. M. Matheson, E. R. Dorsey, B. P. George, D. Sadoff, S. Yoshimura. 2013. The anatomy of health care in the United States. Journal of the American Medical Association 310(18):1947-1963.
MOWAA (Meals on Wheels Association of America). undated. Federal cuts hurt our nation’s most vulnerable seniors. http://www.mowaa.org/document.doc?id=533 (accessed May 15, 2014).
National Commission on Fiscal Responsibility and Reform. 2010. The moment of truth: Report of the National Commission on Fiscal Responsibility and Reform. http://www.momentoftruthproject.org/sites/default/files/TheMomentofTruth12_1_2010.pdf (accessed February 7, 2014).
National Direct Service Workforce Resource Center. 2011. Building capacity and coordinating support for family caregivers and the direct service workforce. White Paper. http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Long-Term-Services-and-Support/Workforce/Downloads/cms-leadership-summit-on-family-white-paper.pdf (accessed February 7, 2014).
National Health Policy Forum. 2013. The basics: National spending for long-term services and supports (LTSS), 2011. Washington, DC: The George Washington University. https://www.nhpf.org/uploads/announcements/Basics_LTSS_02-01-13.pdf (accessed July 30, 2013).
National PACE Association. 2014. PACE in the states. http://www.npaonline.org/website/download.asp?id=1741&title=PACE_in_the_States (accessed May 7, 2014).
Naylor, M. D., E. T. Kurtzman, D. C. Grabowski, C. Harrington, M. McClellan, and S. C. Reinhard. 2012. Unintended consequences of steps to cut readmissions and reform payment may threaten care of vulnerable older adults. Health Affairs 31(7):1623-1631.
NBER (National Bureau of Economic Research). undated. The market for long-term care insurance. http://www.nber.org/bah/winter05/w10989.html (accessed August 19, 2014).
Neuberg, G. W. 2009. The cost of end-of-life care: A new efficiency measure falls short of AHA/ACC standards. Circulation: Cardiovascular Quality and Outcomes 2:127-133.
NHPCO (National Hospice and Palliative Care Organization). 2009. NHPCO facts and figures: Hospice care in America. Alexandria, VA: NHPCO.
NHPCO. 2013. NHPCO’s facts and figures: Hospice care in America. Alexandria, VA: NHPCO.
NHPCO. undated. The Medicare hospice benefit. http://www.nhpco.org/sites/default/files/public/communications/Outreach/The_Medicare_Hospice_Benefit.pdf (accessed November 27, 2013).
Norton, A. 2013. Many Americans worry about cost of long-term care: Poll. http://health.usnews.com/health-news/news/articles/2013/09/30/many-americans-worry-about-cost-of-long-term-care-poll (accessed December 3, 2013).
OECD (Organisation for Economic Co-operation and Development). 2014. Social expenditure—aggregated data. http://stats.oecd.org/Index.aspx?DataSetCode=SOCX_AGG (accessed August 19, 2014).
Parikh, R. B., R. A. Kirch, T. J. Smith, and J. S. Temel. 2013. Early specialty palliative care—translating data in oncology into practice. New England Journal of Medicine 369(24):2347-2351.
Patel, K., and S. Lieberman. 2013. Taking stock of initial year one results for Pioneer ACOs. http://healthaffairs.org/blog/2013/07/25/taking-stock-of-initial-year-one-results-for-pioneer-acos (accessed November 26, 2013).
Peikes, D., G. Peterson. R. S. Brown, S. Graff, and J. P. Lynch. 2012. How changes in Washington University’s Medicare Coordinated Care Demonstration pilot ultimately achieved savings. Health Affairs 31(6):1216-1226.
Penrod, J. D., P. Deb, C. Dellenbaugh, J. F. Burgess, C. W. Zhu, C. L. Christiansen, C. A. Luhrs, T. Cortez, E. Livote, V. Allen, and R. S. Morrison. 2010. Hospital-based palliative care consultation: Effects on hospital cost. Journal of Palliative Medicine 13(8):973-979.
Porter, M. E., and E. O. Teisberg. 2006. Redefining health care: Creating value-based competition on results. Boston, MA: Harvard Business School Press.
Press, M. J., D. P. Scanlon, A. M. Ryan, J. Zhu, A. S. Navathe, J. N. Mittler, and K. G. Volpp. 2013. Limits of readmission rates in measuring hospital quality suggest the need for added metrics. Health Affairs 32(6):1083-1091.
Prigerson, H. G., and P. K. Maciejewski. 2012. Dartmouth Atlas: Putting end-of-life care on the map, but missing psychosocial detail. Journal of Supportive Oncology 10(1):25-28.
Rabow, M., E. Kvale, L. Barbour, J. B. Cassel, S. Cohen, V. Jackson, C. Luhrs, V. Nguyen, S. Rinaldi, D. Stevens, L. Spragens, and D. Weissman. 2013. Moving upstream: A review of the evidence of the impact of outpatient palliative care. Journal of Palliative Medicine 16(12):1540-1549.
Rau, J. 2013. Medicare lags in project to expand hospice. Kaiser Health News, May 9. http://www.kaiserhealthnews.org/stories/2013/may/09/medicare-delays-experiment-on-hospice-and-curative-care.aspx (accessed January 7, 2014).
Reinhard, S. C., C. Levine, and S. Samis. 2012. Home alone: Family caregivers providing complex chronic care. Washington, DC: AARP Public Policy Institute. http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/home-alone-family-caregivers-providing-complex-chronic-care-rev-AARP-ppi-health.pdf (accessed February 22, 2014).
Rhee, Y., H. B. Degenholtz, A. T. Lo Sasso, and L. L. Emanuel. 2009. Estimating the quantity and economic value of family caregiving for community-dwelling older persons in the last year of life. Journal of the American Geriatrics Society 57(9):1654-1659.
Rhodes, K. V., J. Bisgaier, C. C. Lawson, D. Soglin, S. Krug, and M. Van Haitsma. 2013. “Patients who can’t get an appointment go to the ER”: Access to specialty care for publicly insured children. Annals of Emergency Medicine 61(4):394-403.
Rich, E. C., T. Lake, and C. S. Valenzano. 2012. Paying wisely: Reforming incentives to promote evidence-based decisions at the point of care. Princeton, NJ: Mathematica Policy Research, Inc.
Rivlin, A. K. 2013. Why reform Medicare? The President’s and other bipartisan proposals to reform Medicare. Testimony before the U.S. House of Representatives Committee on Ways and Means, Subcommittee on Health, May 21. http://www.brookings.edu/research/testimony/2013/05/21-bipartisan-medicare-reform-rivlin (accessed December 6, 2013).
Robillard, K. 2013. Report: New Alan Simpson-Erskine Bowles plan. POLITICO, February 19. http://www.politico.com/story/2013/02/report-new-simpson-bowles-plan-87769.html (accessed July 25, 2013).
Robison, J., N. Shugrue, M. Porter, R. Fortinsky, L. A. Curry. 2012. Transition from home care to nursing home: Unmet needs in a home-and community-based program for older adults. Journal of Aging and Social Policy 24(3):251-270.
RWJF (Robert Wood Johnson Foundation). 2004. Community-state partnerships to improve end-of-life care: An RWJF national program. Princeton, NJ: RWJF. http://www.rwjf.org/content/dam/farm/reports/program_results_reports/2004/rwjf69596 (accessed June 2, 2014).
Ryu, A. J., T. B. Gibson, M. R. McKellar, and M. E. Chernew. 2013. The slowdown in health care spending in 2009-11 reflected factors other than the weak economy and thus may persist. Health Affairs 32(5):835-840.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2013. Mental health parity and addiction equity. http://beta.samhsa.gov/health-reform/parity (accessed December 5, 2013).
Schroeder, S. A., and W. Frist. 2013. Phasing out fee-for-service payment. New England Journal of Medicine 368(21):2029-2031.
Segal, M. 2011. Dual eligible beneficiaries and potentially avoidable hospitalizations. Policy Insight Brief. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Insight-Briefs/downloads/PAHInsightBrief.pdf (accessed January 4, 2014).
Senate Commission on Long-Term Care. 2013. Report to the Congress. http://www.chhs.ca.gov/OLMDOC/Agenda%20Item%206-%20Commission%20on%20Long-Term%20Care-%20Final%20Report%209-26-13.pdf (accessed December 2, 2013).
Shier, G., M. Ginsburg, J. Howell, P. Volland, and R. Golden. 2013. Strong social support services, such as transportation and help for caregivers, can lead to lower health care use and costs. Health Affairs 32(3):544-550.
Skocpol, T. 2010. The political challenges that may undermine health reform. Health Affairs 29(7):1288-1292.
Smith, A. K., I. S. Cenzer, S. J. Knight, K. A. Puntillo, E. Widera, B. A. Williams, W. J. Boscardin, and K. E. Covinsky. 2010. The epidemiology of pain during the last two years of life. Annals of Internal Medicine 153(9):563-569.
Smith, A. K., E. McCarthy, E. Weber, I. S. Cenzer, J. Boscardin, J. Fisher, and K. Covinsky. 2012. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there. Health Affairs 31(6):1277-1285.
Smith, S., A. Brick, S. O’Hara, and C. Normand. 2014. Evidence on the cost and cost-effectiveness of palliative care: A literature review. Palliative Medicine 28(2):130-150.
Spettell, C. M., W. S. Rawlins, R. Krakauer, J. Fernandes, M. E. S. Breton, W. Gowdy, S. Brodeur, M. MacCoy, and T. A. Brennan. 2009. A comprehensive case management program to improve palliative care. Journal of Palliative Medicine 12(9):827-832.
Spillman, B. 2012. Financial preparedness for long-term care needs in old age. In Consumer knowledge and financial decisions: Lifespan perspectives, edited by D. J. Lamdin. New York: Springer. Pp. 239-253.
Starks, H., S. Wang, S. Farber, D. A. Owens, and J. R. Curtis. 2013. Cost savings vary by length of stay for inpatients receiving palliative care consultation services. Journal of Palliative Medicine 16(10):1215-1220.
Steuerle, C. E., and C. Quakenbush. 2012. Social Security and Medicare taxes and benefits over a lifetime: 2012 update. Washington, DC: Urban Institute. http://www.urban.org/UploadedPDF/412660-Social-Security-and-Medicare-Taxes-and-Benefits-Over-a-Lifetime.pdf (accessed August 15, 2014).
Stukel, T. A., E. S. Fisher, D. E. Wennberg, D. A. Alter, D. J. Gottlieb, and M. J. Vermeulen. 2007. Analysis of observational studies in the presence of treatment selection bias: Effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. Journal of the American Medical Association 297(3):278-285.
Temel, J. S., J. A. Greer, A. Muzikansky, E. R. Gallagher, S. Admane, V. A. Jackson, C. M. Dahlin, C. D. Blinderman, J. Jacobsen, W. F. Pirl, J. A. Billings, and T. J. Lynch. 2010. Early palliative care for patients with metastatic non small-cell lung cancer. New England Journal of Medicine 363(8):733-742.
Teno, J. M., P. L. Gozalo, J. P. Bynum, N. E. Leland, S. C. Miller, N. E. Morden, T. Scupp, D. C. Goodman, and V. Mor. 2013. Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. Journal of the American Medical Association 309(5):470-477.
Thomas, K. S., and V. Mor. 2013. Providing more home-delivered meals is one way to keep older adults with low care needs out of nursing homes. Health Affairs 32(10):1796-1802.
Tilson, S., and G. J. Hoffman. 2012. Addressing Medicare hospital readmissions (R42546). Washington, DC: Congressional Research Service.
Topf, L., C. A. Robinson, and J. L. Bottorff. 2013. When a desired home death does not occur: The consequences of broken promises. Journal of Palliative Medicine 16(8):875-880.
Ubel, P. A., S. R. Berry, E. Nadler, C. M. Bell, M. A. Kozminski, J. A. Palmer, W. K. Evans, E. L. Strevel, and P. J. Neumann. 2012. In a survey, marked inconsistency in how oncologists judged value of high-cost cancer drugs in relation to gains in survival. Health Affairs 31(4):709-717.
Unroe, K. T., and D. E. Meier. 2013. Quality of hospice care for individuals with dementia. Journal of the American Geriatrics Society 61:1212-1214.
U.S. Burden of Disease Collaborators. 2013. The state of U.S. health, 1990-2010: Burden of diseases, injuries, and risk factors. Journal of the American Medical Association 310(6):591-608.
U.S. Department of Justice. 2013. Hospice of Arizona and related entities pay $12 million to resolve False Claims Act allegations. News release. March 20. http://www.justice.gov/opa/pr/2013/March/13-civ-326.html (accessed July 25, 2013).
Verdier, J. M., M. Au, and J. Gillooly. 2011. Managing the care of dual eligible beneficiaries: A review of selected state programs and special needs plans. Washington, DC: MedPAC.
Walke, L. M., A. L. Byers, R. McCorkle, T. R. Fried. 2006. Symptom assessment in community-dwelling older adults with advanced chronic disease. Journal of Pain and Symptom Management 31(1):31-37.
Weeks, W. B., S. S. Rauh, E. B. Wadsworth, and J. N. Weinstein. 2013. The unintended consequences of bundled payments. Annals of Internal Medicine 158(1):62-64.
Weiner, J. S., and S. A. Cole. 2004. Three principles to improve clinician communication for advance care planning: Overcoming emotional, cognitive, and skill barriers. Journal of Palliative Medicine 7(6):817-829.
Wennberg, J. E., E. S. Fisher, D. C. Goodman, and J. S. Skinner. 2008. Tracking the care of patients with severe chronic illness: The Dartmouth Atlas of Health Care 2008. Lebanon, NH: Dartmouth Medical School. http://www.dartmouth.edu/~jskinner/documents/2008_Chronic_Care_Atlas.pdf (accessed February 22, 2014).
Wiener, J. M., W. Anderson, G. Khatutsky, Y. Kaganova, J. O’Keeffe. 2013. Medicaid spend down: New estimates and implications for long-term services and supports financing reform. Final report. http://www.rti.org/pubs/rti_medicaid-spend-down_3-20-13_1.pdf (accessed February 1, 2014).
Wilensky, G. 2014. Developing a viable alternative to Medicare’s physician payment strategy. Health Affairs 33(1):153-160.
Wright, A. A., and I. T. Katz. 2007. Letting go of the rope: Aggressive treatment, hospice care, and open access. New England Journal of Medicine 357(4):324-327. http://www.nejm.org/doi/full/10.1056/NEJMp078074 (accessed February 22, 2014).
Yabroff, K. R., J. S. Mandelblatt, and J. Ingham. 2004. The quality of medical care at the end-of-life in the USA: Existing barriers and examples of process and outcome measures. Palliative Medicine 18(3):202-216.
Yang, Y. T., and M. M. Mahon. 2011. Considerations of quality-adjusted life-year in palliative care for the terminally ill. Letter. Journal of Palliative Medicine 14(11):1197.
Yoon, J., M. E. Domino, E. C. Norton, G. S. Cuddeback, J. P. Morrissey. 2013. The impact of changes in psychiatric bed supply on jail use by persons with severe mental illness. Journal of Mental Health Policy and Economics 16(2):81-92.
Young, K., R. Garfield, M. Musumeci, L. Clemans-Cope, and E. Lawton. 2013. Medicaid’s role for dual eligible beneficiaries. Menlo Park, CA: KFF, Kaiser Commission on Medicaid and the Uninsured. http://kaiserfamilyfoundation.files.wordpress.com/2013/08/7846-04-medicaids-role-for-dual-eligible-beneficiaries.pdf (accessed February 22, 2013).


















































































