Pediatric End-of-Life and Palliative Care: Epidemiology and Health Service Use
Chris Feudtner, M.D., Ph.D., M.P.H.1,2
Wenjun Zhong, Ph.D.1
Jen Faerber, Ph.D.1
Dingwei Dai, Ph.D.1
James Feinstein, M.D., M.P.H.3
Each year in the United States, just over 45,000 infants, children, and adolescents die, with another 18,500 deaths among young adults aged 20 to 24. These deaths, while representing only a small proportion of all deaths in America, are nevertheless vitally important when considering how the U.S. health care system can better meet the needs of patients approaching the end of life. Pediatric patients who die are widely acknowledged to present many challenges that distinguish them from adult patients: they live with and die from a wide array of often-rare diseases that require specialized care; the trajectory of their illness experiences is often either much shorter or far longer than that of adult patients; the child is always cared for in the context of a family, which also needs support and often care; the mechanism of financing health care in general and palliative care specifically is different for the young versus older adults; and serious pediatric illness and death during childhood present emotional and even spiritual challenges to those who love and care for these patients.
The past decade has witnessed remarkable changes in the care that can be provided to children with life-threatening conditions and their families. The field of interdisciplinary pediatric palliative care has become a well-recognized specialty, with an ever-increasing number of children’s hospitals creating and developing interdisciplinary pediatric palliative care teams. Pediatric hospice has likewise advanced with the development and
_______________
1The Children’s Hospital of Philadelphia.
2The Perelman School of Medicine at the University of Pennsylvania.
3The Children’s Hospital of Colorado and the University of Colorado School of Medicine.
promulgation of practice standards, and with the increased possibility of pediatric patients with serious illness receiving hospice care concurrent with other modes of disease treatment. At the same time, all the challenges outlined above remain, and in certain ways as the opportunities to improve care for dying children have increased, the urgency of doing so has likewise increased. This appendix is intended to clarify the epidemiology and health service use of those receiving pediatric end-of-life and palliative care.
The analysis offered here is much more at the level of populations of patients as opposed to individual patients. Many of the most important aspects of pediatric end-of-life care can be understood only with what might be called the “3-foot view,” obtained by sitting with patients and parents and care providers and listening to and learning from their experiences. This appendix, by contrast, is based on national mortality and health service data that offer a 3,000-foot view whereby general trends of disease and care can be seen, and on clinically detailed hospital data that allow a more specific 300-foot view of the ways in which groups of patients have received care.
DEFINITIONS
Before proceeding, we define and discuss key terms and concepts used throughout this appendix.
End of life: An ambiguous yet important period of time prior to death.
The end of life is perhaps best thought of as beginning when an illness, injury, or condition progresses to the point where the health status of the patient is diminished below a level that would make it possible to live in a way that is meaningful or acceptable to that individual and ends with the patient’s death. This time period may represent the flash of a second (as is the case for patients who die instantly from trauma) or extend for several weeks or longer (as is the case for patients with progressive cancer who experience a mounting symptom burden).
The start of this time period, when the health status of the patient is judged to have descended below a threshold beyond which meaningful or acceptable quality of life is no longer possible, is subjective: seemingly similar patients and their families will make different judgments about what this threshold is, and thus when this time period starts. Because the start of this end-of-life period is a combination of both a biological process and value judgments, a change in either the patient’s biology (such as physiologic organ failure) or a value judgment about the patient’s health status (such as living with severe impairments that require technology support) can mark the beginning of the end of life.
Because this definition requires individual-level clarity about biology
and value judgments, it cannot be applied in most large population datasets, which lack such data elements. As an approximation, then, epidemiologic and health services research can focus on a defined period of time prior to the day and time of death as the “end of life.” This is a useful and often illuminating retrospective analytic strategy for population-level studies, but such uniform definitions should not be confused with the individual-level definition that is required for individual-level care and that is the required basis of any prospective study.
Care at the end of life: All forms of care—including medical, surgical, nursing, psychosocial, spiritual, and hospice—received by patients during the end-of-life period prior to death.
For the reasons discussed above, this period of time may vary substantially at the individual level across otherwise similar patients. During this period, moreover, the care received also can vary substantially depending upon the individual-level goals of care and available resources.
Palliative care: Care for patients with serious illness that is intended to palliate symptoms, enhance comfort, and improve quality of life.
Palliative care is compatible with other modes of care, such as disease-directed, cure-seeking, or life-prolonging care. Palliative care for patients with serious illness can begin long before they enter their end-of-life phase and can continue after they die, in the form of bereavement care for those who loved them. Palliative care is not synonymous with end-of-life care given the longer time frame in which it can be provided and the fact that the goals of end-of-life care often differ from those that guide palliative care, such as ongoing health maintenance interventions (for example, vaccinations), attendance at school, or involvement in other “normal” family and life activities.
Serious pediatric illness and life-threatening conditions: Illnesses and conditions that pose a significant risk of death and typically impose physical, emotional, and other forms of distressing symptoms upon patients at some point in the illness trajectory.
The distress caused by serious pediatric illness and life-threatening conditions can often be alleviated to varying degrees by the receipt of palliative care. Serious pediatric illness and life-threatening conditions are not prerequisites for the appropriate receipt of pediatric palliative care; patients with less severe forms of disease can also benefit from such care.
Pediatric age range: The range of ages at which patients with serious illness and life-threatening conditions are often treated by pediatric-oriented health care providers and hospitals.
The pediatric age range is not defined by a legal or administrative threshold (such as the 18th birthday, when individuals are granted some but not all rights and privileges of adulthood, or the 21st birthday, which is defined by the National Institutes of Health as the demarcation between
children and adults). Rather, the pediatric age range is observed to extend from the prenatal period (when consultations about fetal health are provided by perinatologists) through young adulthood. At various points during the late teen years or early 20s, patients typically transition to adult-oriented health care providers (and indeed, for patients cared for by family physicians, the transition is one not of clinical provider but instead of the nature of the patient-clinician interaction). For pediatric patients with serious illness and life-threatening conditions, however, this transition is often delayed or avoided entirely because of concerns regarding continuity of care for very ill patients, or the need for specialized knowledge about disease processes or treatments that resides predominantly in pediatric clinicians and children’s hospitals. While many of the studies and analyses discussed in this appendix are restricted to persons and patients below age 18 or 20, others extend the age range covered to 24 and even beyond, making it possible to see how the pediatric health care system is used to serve the needs of certain young adult patients.
DATA SOURCES
In addition to reviewing the published literature, we used the datasets described below in preparing this appendix.
Mortality Data
Centers for Disease Control and Prevention (CDC) mortality data (http://wonder.cdc.gov) are produced by the CDC’s National Center for Health Statistics (NCHS). Currently, the dataset spans 1968 to 2010 and comprises a county-level national mortality file and a corresponding county-level national population file.
CDC mortality data based on the NCHS annual detailed mortality files include a record for every death of a U.S. resident recorded in the United States. The annual detailed mortality files contain an extensive set of variables derived from the death certificates. For the Compressed Mortality data, the source data records are condensed with only a subset of variables being retained: (1) state and county of residence; (2) year of death; (3) race; (4) sex; (5) for 1999-2010, Hispanic origin (not Hispanic or Latino, Hispanic or Latino); (6) age group at death (specific age recoded to 16 age groups); (7) underlying cause of death (1968-1978 with International Classification of Diseases [ICD]-8 codes, 1979-1998 with ICD-9 codes, and 1999-2010 with ICD-10 codes).
For the detailed mortality file or Multiple Cause of Death data, the data are based on death certificates for U.S. residents. Currently the data span the years 1999-2010. Each death certificate contains a single underly-
ing cause of death, up to 20 additional multiple causes, and demographic data. The number of deaths, crude death rates or age-adjusted death rates, and 95 percent confidence intervals and standard errors for death rates can be obtained by place of residence (total United States, region, state, and county), age group (single year of age, 5-year age groups, 10-year age groups, and infant age groups), race, Hispanic ethnicity, gender, year, month and weekday of death, and cause of death (four-digit ICD-10 code or group of codes). Data are also available for injury intent and injury mechanism, drug/alcohol-induced causes, and urbanization categories, as well as place of death and whether an autopsy was performed.
The CDC mortality data are publicly available, and researchers need to agree to data use restrictions.
National Inpatient and Emergency Department Data
The Kids’ Inpatient Dataset (KID, http://www.hcup-us.ahrq.gov/kidoverview.jsp) is part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ).
The KID, compiled every 3 years, is composed of hospitalization discharge data from approximately 3 million hospitalizations of patients under age 21. Versions exist for 1997, 2000, 2003, 2006, and 2009. Over the years, more states have been represented, with data from 44 states being included in 2009. The sample is constructed in a manner that allows weighted analyses to generate national estimates, equivalent in 2009 to approximately 7 million hospitalizations.
The KID contains more than 100 clinical and nonclinical variables for each hospital stay, including ICD-9, Clinical Modification (ICD-9-CM) diagnosis and external cause of injury codes; ICD-9-CM and Current Procedural Terminology, Fourth Edition (CPT®-4) procedure codes; admission and discharge status; patient demographic characteristics (e.g., sex, age, urban-rural designation of residence, national quartile of median household income for patient’s zip code); expected payment source; total hospital charges; and hospital characteristics (e.g., region, trauma center indicator, urban-rural location, teaching status).
The Nationwide Emergency Department Sample (NEDS, http://www.hcup-us.ahrq.gov/nedsoverview.jsp) is also part of the HCUP. It is the largest all-payer emergency department (ED) database in the United States, yielding national estimates of hospital-based ED visits. In 2011, 28 HCUP states participated in the 2011 NEDS, providing data on 29 million ED visits at 951 hospitals.
The NEDS contains clinical and nonclinical variables regarding the ED encounter as well as linked data for any subsequent hospitalization, as
described above for the KID. The dataset also identifies injury-related ED visits, including mechanism, intent, and severity of injury; total ED charges (for ED visits); and total hospital charges (for inpatient stays for ED visits that result in admission).
Both the KID and NEDS data are available for purchase through the HCUP Central Distributor. All users of the KID and NEDS must complete the online Data Use Agreement training, sign a Data Use Agreement, and send a copy to AHRQ.
Clinically Detailed Administrative Hospitalization Data
The Pediatric Health Information System (PHIS, http://www.chca.com/index_flash.html) is maintained by the Child Hospital Association (Kansas City, Kansas). It contains clinically detailed administrative discharge data on more than 18 million patient encounters from 43 not-for-profit, tertiary children’s hospitals in the United States, representing most of the major metropolitan areas nationwide. The data are updated on a quarterly basis. The quality and reliability of the data are assured through a joint effort of the Child Hospital Association, the data manager (Thomson-Reuters, Durham, North Carolina), and participating hospitals. Data are accepted into the PHIS database only when classified errors occur in less than 2 percent of a hospital’s quarterly data.
The Premier Perspective Database (PPD) is the product of a consortium of U.S. not-for-profit hospitals and health systems, maintained by Premier, Inc. (San Diego, California) (http://www.premierinc.com). It currently serves a broad array of academic medical centers, community-based hospitals, and other health care sites, distributed throughout the urban and rural United States. The PPD represents hospitals that admit both children and adults. It compiles hospital data from approximately one-sixth of all hospitalizations in the United States and contains information on more than 130 million patient discharges. About two-thirds of the member hospitals update their data monthly, and the rest update quarterly. Upon receiving data from participating hospitals, the PPD undertakes an extensive multiphase data validation and correction process.
PHIS and PPD data elements are largely the same. They include patient characteristics (e.g., age, sex, admission and discharge dates, All Patient Refined-Diagnosis Related Groups [APR-DRGs]); diagnoses (e.g., discharge diagnosis based on ICD-9, order of diagnoses); pharmacy data (e.g., medications, route, date of administration, pharmacy charge); procedures (based on ICD-9 codes and date of procedure); supply (supply ordered, day supply delivered, and supply charge); laboratory tests (test ordered, date laboratory result delivered, but not actual results); radiologic imaging (imaging procedure, utilization of contrast media, date ordered, but not results);
and clinical services (including date provided and charge for the service). Researchers interested in using PHIS or PPD data should inquire with the respective data management organizations.
Other Data Sources and Data Needs
For the sake of thoroughness, we mention other large data sources not used in this appendix—in particular, Medicaid claims data and data from either health maintenance organizations (such as Kaiser Permanente and Group Health Cooperative) or commercial insurance plans. To date, only a limited number of epidemiologic and health services research studies regarding pediatric mortality and pediatric end-of-life and palliative care have used these data sources.
There is a compelling need for data that would provide a longitudinal “all services” perspective on the health care experience of pediatric patients with serious illness. By “all services,” we mean to include hospital care; outpatient care; inpatient and outpatient pharmacy services; and home nursing, hospice, respite, and other services. Ideally, these data would be both “all payer” and “all services,” providing a population-level perspective, so that any differences or confounding bias between patients covered, for example, by government versus commercial payers could be identified and accounted for. If not “all payer,” a data source representing the various types of payers would be a major advance. Additionally, these data need to be organized such that individual patient experiences, while being appropriately deidentified, could be analyzed over time to discern patterns of care. Many data sources, such as the KID and NEDS, do not enable such longitudinal analyses. The development of a data source with these characteristics would represent a major advance for pediatric end-of-life and palliative care research.
Finally, a data source is needed that includes indicators of the goals of care, such as the occurrence of a “goals of care” discussion between the patient/parent and the medical team, or the initiation of “do not attempt resuscitation” orders, with timestamps regarding when such markers of goals of care occur. These data would enable analysis of how care changes in response to such occurrences and whether care provided is congruent with care goals. Because of practical considerations concerning how such data on goals of care would be obtained, these data sources would likely be much smaller than those outlined above.
FINDINGS AND INTERPRETATIONS
Annual Number of Deaths and Trends Over Time
In 2010, there were 45,068 deaths in the United States among persons aged 19 or younger and another 18,664 deaths among persons aged 20-24. Combining these groups, there were 63,732 deaths.
Historically, as depicted in Figure F-1a, the number of deaths has declined remarkably since 1968, especially among those in the infant age range. This decline in numbers is not due to a decline in the overall size of the population in this age range; in a corresponding manner, the rates of death (per person in each age range) have also plummeted (see Figure F-1b).
Age Distribution of Pediatric Deaths
The peak age of pediatric mortality, by far, is during the first year of life (see Figure F-2a). Accordingly, pediatric palliative care must be designed to address the needs of neonates and infants, as well as their parents and families.
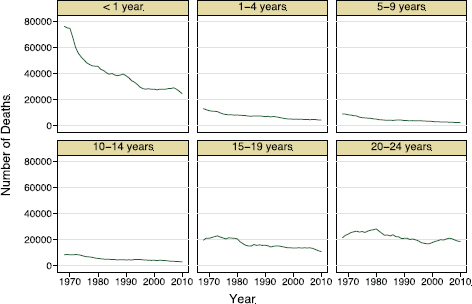
FIGURE F-1a Annual number of pediatric deaths in the United States, 1968-2010.
SOURCE: Based on Multiple Cause of Death data 1968-2010 from CDC WONDER online database.
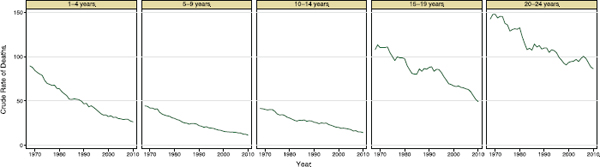
FIGURE F-1b Annual rates of pediatric deaths in the United States, 1968-2010.
NOTE: Omits infants, whose rate declined from 2,178 to 623 per 10,000 persons.
SOURCE: Based on Multiple Cause of Death data 1968-2010 from CDC WONDER online database.
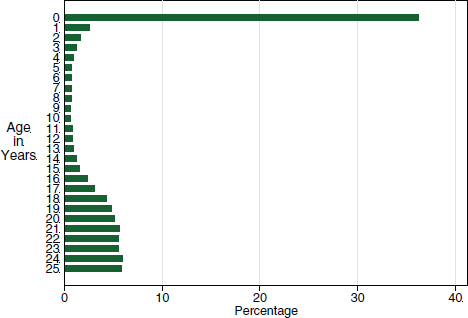
FIGURE F-2a Age distribution of pediatric deaths by year of age.
SOURCE: Based on Multiple Cause of Death data 2010 from CDC WONDER online database.
A closer look at the age distribution of pediatric deaths within the first year of life reveals the prominence of deaths within the first hours of life (see Figure F-2b). These rapid demises require that palliative care for these infants and their parents be close at hand, which is to say in places where infants are born (and antenatally as well, for prenatal visits and potentially the development of palliative care birth plans) and in newborn nurseries and neonatal intensive care units.
Causes of Pediatric Death
The single most important cause of pediatric and young adult deaths is trauma and other external causes, followed by conditions arising in the perinatal period (as underscored in the previous figures) and congenital malformations and chromosomal abnormalities (see Figure F-3).
Prevalence of Children with Conditions Warranting Palliative Care
Estimating the prevalence or number of children with conditions warranting palliative care is a difficult task for at least four reasons.
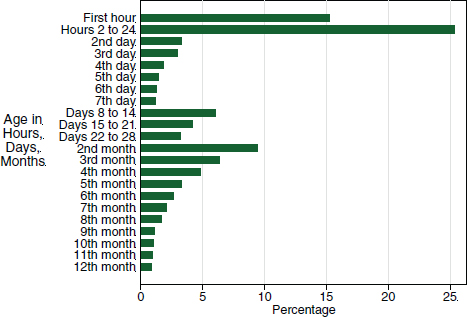
FIGURE F-2b Age distribution of infant deaths by month, day, and hours of age.
SOURCE: Based on Multiple Cause of Death data 2010 from CDC WONDER online database.
First, the case definition of “children with conditions warranting palliative care” is not clear-cut and is based to some degree on perspectives and values. At one end of a spectrum, case definition might be cases of children who are actively dying and in pain or suffering because of a symptom other than pain, and for whom palliative care is clearly needed and warranted (as part of end-of-life care). Near the middle of the spectrum are cases of children who are not actively dying but are likely to die in the ensuing months or next few years as a result of either the progressive worsening of their underlying condition or their medical fragility (what are termed here “life-threatening conditions”), and these cases are also likely to benefit from the receipt of palliative care. Toward the other end of the spectrum are cases of children who are unlikely to live out a normal life span, can be expected to live with significant impairments, and may or may not currently have symptoms that could be ameliorated with palliative care interventions (so-called life-limiting conditions).
Second, imbedded in the definitions of both life-threatening and life-limiting conditions are probability statements regarding the prognosis for how long the children will live and the likelihood that they have symptoms that could be ameliorated (or more generally, that their quality of life
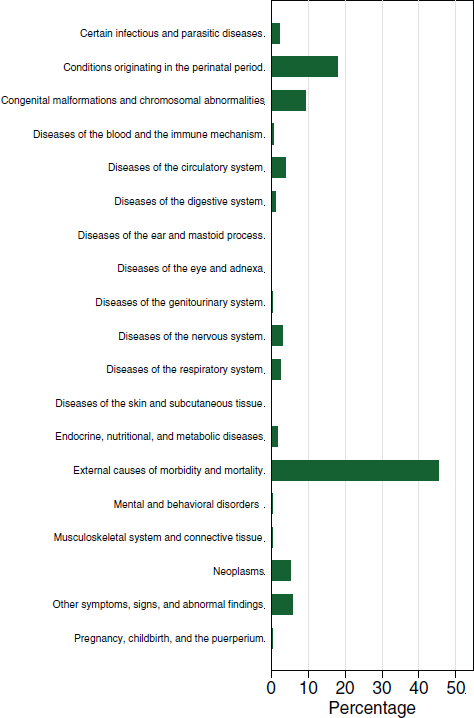
FIGURE F-3 Major causes of pediatric death.
SOURCE: Based on Multiple Cause of Death data 2010 from CDC WONDER online database.
or that of their parents or family could be improved). How large these probabilities need to be is largely a value-based decision. For example, would a patient with the following characteristics qualify as having a life-threatening condition that warrants palliative care: a combination of a 10 percent chance of dying in the next week, a 50 percent chance of dying sometime this coming year, and a 20 percent chance that symptom management could be improved with a palliative care approach?
Third, it is necessary to clarify the differences between point prevalence and period prevalence and their relevance for program development and policy considerations. Point prevalence refers to the number of cases at a given moment in time. Point prevalence is important for the design of clinical service programs, because it provides guidance on how much capacity these programs should have to take care of a specific number of patients. Period prevalence refers to the number of cases over a period of time, most often 1 year. For pediatric palliative care, period prevalence will be larger than point prevalence, because during the time period of 1 year, many cases will have both entered into the case definition (that is, developed the underlying condition) and died. Period prevalence is also relevant to program and policy development—not to understand the required daily capacity of palliative care teams but to understand the total palliative care workload of these teams. To clarify this distinction, consider two simplified scenarios. First, if the point prevalence were only 1 patient in a particular population but all the cases cared for by this team died within 1 day, then the annual period prevalence would be 365. By contrast, if the point prevalence were 20 but patients typically survived for 6 months or longer, then the annual period prevalence might be only 40. These two scenarios clarify how these two metrics—point prevalence and period prevalence—capture different perspectives on the nature and volume of the workload that a palliative care team would have to manage.
Fourth and finally, there is a relative lack of population-level data. There are to our knowledge no population-based assessments in the United States specifically designed to gather this information. A study based on primary data collection in the region around Bath, England, found an annual period prevalence of 1.2/1,000 children for conditions with a 50 percent chance or greater of causing death before age 40 while omitting patients with cancer or conditions that typically cause death within a month (Lenton et al., 2001). Another study, of all of England, based on analysis of health claims records and identifying cases on the basis of having diagnostic codes for conditions that are often the underlying conditions in patients receiving palliative care services, found an annual period prevalence of 3.2/1,000 children (Fraser et al., 2012).
With these caveats in mind, what can be offered as a range of estimates regarding the point and annual period prevalence of children with
conditions that warrant palliative care? At one extreme, the data presented above regarding both the causes of death and age at the time of death strongly suggest that the point prevalence of pediatric patients living with life-threatening conditions on any given day is approximately equal to the annual number of deaths, or about 45,000. Why? Consider first the high proportion of all pediatric deaths represented by neonatal deaths and the short life span of many infants who die (1 day or 1 week). Consider second the high proportion of deaths beyond the neonatal period due to trauma (which often results in death immediately or within hours). Together, as stated above, these two observations imply that the point prevalence of infants and children living with life-threatening and life-shortening conditions may not be more than the annual cumulative incidence of pediatric deaths. The other end of the range of estimates—but also shifting from point prevalence to annual period prevalence—would be based on the English study of claims data, applying an annual prevalence of 3.2/1,000 to the population of infants, children, and adolescents in the United States (73.9 million) to estimate 236,480 potential pediatric palliative care patients over the course of 1 year (while also acknowledging that patients with these conditions might not warrant or want palliative care). A mid-range estimate would be based on the Bath study, adjusting a point prevalence of 1.2/1,000 upward by 100 percent to account for the omission of cancer patients and patients who died from acute conditions that typically cause death within 1 month, and so apply an estimated annual period prevalence of 2.4/1,000 to the U.S. pediatric age population. This approach would yield an annual period prevalence estimate of 177,360 children (but acknowledging that only 60 percent of the patients identified in the Bath study had pain).
Complex Chronic Conditions as a Cause of Pediatric Death
Amid the vast diversity of causes of pediatric deaths, a distinction can be drawn between life-threatening conditions that arise suddenly and most often unexpectedly (such as extreme premature birth, serious infections, and trauma) and complex chronic conditions (CCCs) that can be lethal. While many pediatric deaths are unexpected, those deaths attributed to these chronic conditions may have been foreseeable, providing an opportunity to provide palliative care and plan for end-of-life care.
CCCs have been defined as conditions likely to last 6 months or longer (unless death intervenes) and requiring care by pediatric subspecialists and often a period of hospital care. In turn, this definition can be used to classify ICD-9 codes indicative of CCC status, subcategorizing these diagnoses into organ- or system-based groups (Feudtner et al., 2000).
Among pediatric patients who died with a CCC diagnosis, the modal CCC categories are neonatal diagnoses, followed by cardiovascular and
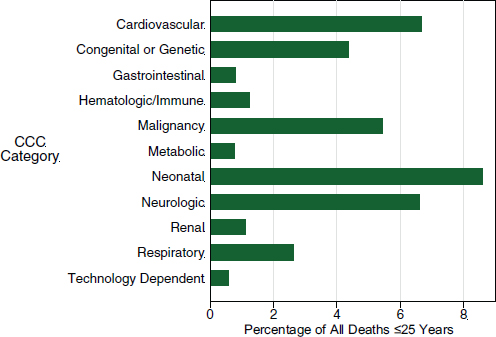
FIGURE F-4 Pediatric deaths involving complex chronic conditions.
SOURCE: Based on Multiple Cause of Death data 2010 from CDC WONDER online database.
neurologic conditions, and then malignancies (see Figure F-4). In other work, we have found that the proportion of all deaths due to CCCs is increasing because of the sharp declines in deaths due to trauma and other acute causes and the relative stability of rates of deaths due to CCCs.
Multiple Complex Chronic Condition Categories and Pediatric Deaths
In previous research, pediatric patients with a higher number of different categories of CCCs (e.g., cardiovascular and respiratory CCCs) have been found to have a heightened risk of readmission, more extensive health care utilization, and death. Among all pediatric deaths, one-third have CCCs, with 4.5 percent having two different categories of CCCs and 0.57 percent having three or more different categories (see Figure F-5).
Locations of Pediatric Deaths
Among all pediatric deaths (including trauma), the most common place of death for all persons aged 14 and younger is the hospital; this is the case
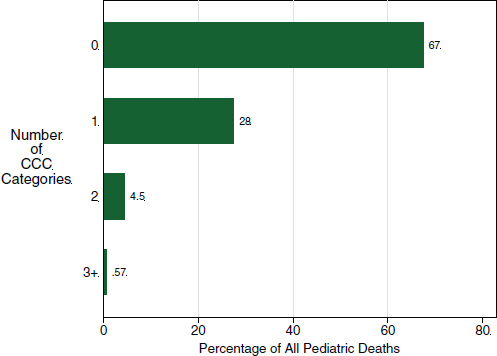
FIGURE F-5 Pediatric deaths involving multiple complex chronic conditions.
SOURCE: Based on Multiple Cause of Death data 2010 from CDC WONDER online database.
especially for infants (74 percent of whom die in hospitals) (see Figure F-6). EDs are also important sites of dying, as are homes.
Trajectories or Patterns of Experience of the Pediatric Dying Process
Based on the preceding data, as well as clinical experience, pediatric patients who die typically experience one of four different patterns of illness trajectory: (1) sudden death (e.g., trauma, meningo-coccemia), (2) a steady inexorable decline (e.g., unresectable brain tumor or Tay-Sachs), (3) fluctuating decline (e.g., progressive diseases with intermittent crises, such as worsening heart failure), and (4) constant medical fragility (e.g., “static” neurologic impairment predisposing to crises due to infections or metabolic decompensations) (see Figure F-7).
Good end-of-life care (illustrated by the shifts in the trajectories for panels B, C, and D in Figure F-7, from black into the purple trajectories) aims to improve quality of life and to prevent it from becoming so dominated by suffering that the patient descends to being in a worse-than-dead
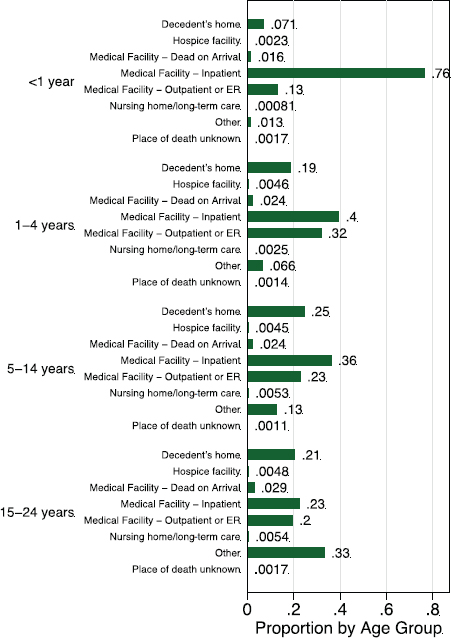
FIGURE F-6 Locations of pediatric deaths by age range.
SOURCE: Based on Multiple Cause of Death data 2010 from CDC WONDER online database.
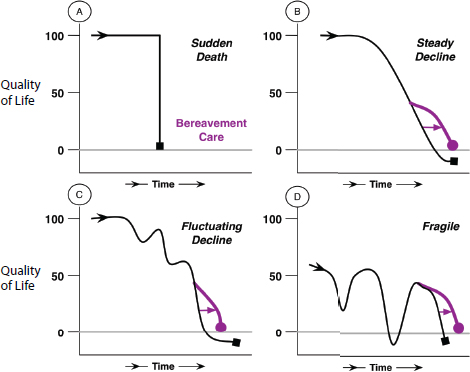
FIGURE F-7 Trajectories of pediatric dying.
SOURCE: A version of this figure appears in Feudtner, 2007. Reprinted with permission from Elsevier.
state (illustrated by the trajectories in the figure that fall below the grey line at zero quality of life). Interventions to improve or safeguard quality of life may have no impact on the patient’s life span (as illustrated in panel B) or may shorten life span (panel C, illustrating the often-discussed “double effect” whereby medications designed to improve comfort may shorten life span) or lengthen life span (panel D, the “win-win effect”). Data with which to estimate which of these possibilities is most common are not available.
Although there are no precise epidemiologic data regarding the proportion of deaths that follow each trajectory, because many pediatric deaths follow trajectories A, C, or D, predicting death is either not appropriate (for trajectory A) or exceedingly imprecise (trajectories C and D). Furthermore, for trajectories C and D, patients and parents have often experienced previous serious medical crises from which the patient survived, which affects (accurately or inaccurately) the way they perceive a current health crisis.
Deaths Attributed to Complex Chronic Conditions and Locations of Death
Again focusing on pediatric deaths attributed to CCCs (which is to say, deaths that may have been foreseeable and due to long-standing medical illness as opposed to trauma or sudden infectious illnesses), the number of such deaths declined overall from 1989 to 2006 (as shown previously for all pediatric deaths). Here we note a change in the locations of these deaths over time, with an increase in the number of deaths occurring at home (see Figure F-8).
Rising Proportion of Home Deaths Among Deaths Attributed to Complex Chronic Conditions
The decline in deaths occurring in hospitals, combined with the rise in deaths occurring at home, has resulted in a significant increase in the proportion of all pediatric CCC-related deaths occurring at home (see Figure F-9). This increase may be due to a desire to have home be the place of death or to inadvertent deaths occurring to children who are medically
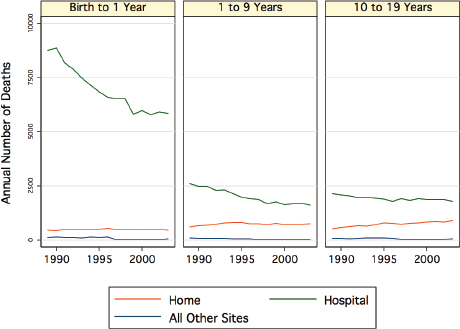
FIGURE F-8 Locations of death among deceased pediatric patients with complex chronic conditions.
SOURCE: Based on Multiple Cause of Death data from CDC; see Feudtner et al., 2007.
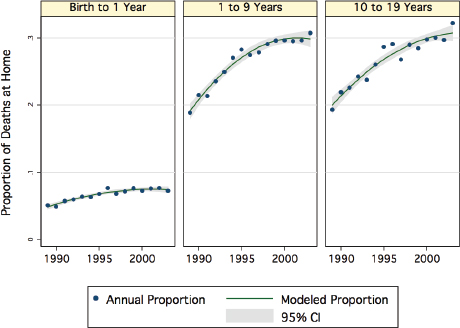
FIGURE F-9 Home deaths among pediatric patients with complex chronic conditions who died.
SOURCE: Based on Multiple Cause of Death data from CDC; see Feudtner et al., 2007.
fragile as a result of illness or dependence upon medical technology. Either way, this shift in location of death underscores the importance of having sufficient community-based capacity to provide care in the home for pediatric patients with CCCs, in the mode of either hospice or home nursing services, as well as the need for community-based bereavement services for families (parents, siblings, and others).
Rising Proportion of Home Deaths Beyond Infancy for Deceased Patients with Complex Chronic Conditions
The rise in the proportion of CCC-associated deaths that have occurred at home is observed for most of the CCC categories, with a much larger proportion and increase over time seen in patients beyond infancy (see Figure F-10).
Differences Across Race and Ethnicity in Location of Death
Across race and ethnicity categories, there are striking differences in the probability of dying at home among pediatric deaths attributed to CCCs
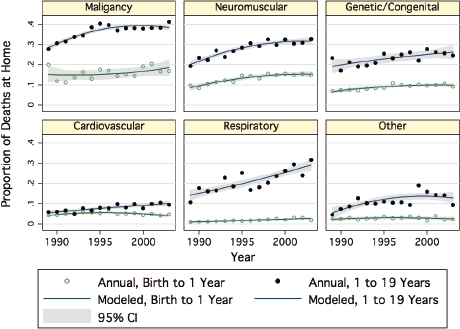
FIGURE F-10 Proportion of home deaths by age group for different complex chronic condition categories.
SOURCE: Based on Multiple Cause of Death data from CDC; see Feudtner et al., 2007.
(see Figure F-11). In other work focused on hospital care received by dying pediatric patients, we have not found such differences. This suggests that once a pediatric patient is hospitalized, care is fairly uniform across race and ethnicity categories, but access to home-based care (hospice or home nursing) may be limited because of either referral or supply or as the result of a culturally based preference not to be at home when death occurs.
State-Level Variation in Race and Ethnicity Disparities in Location of Death
The differences noted above also appear to depend upon where individuals reside. Examining the five largest states of residence in the United States (as illustrated in Figure F-12), marked state-level variation is evident even after stratification for specific underlying causes of death and specific age ranges: among these states, the baseline rates of death at home within each stratified group differ significantly. New York is observed to have had the lowest proportion of home deaths for all groups. White/non-Hispanic
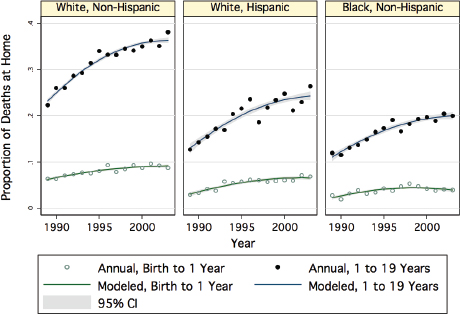
FIGURE F-11 Proportion of home deaths by age group for different race and ethnicity categories.
SOURCE: Based on Multiple Cause of Death data from CDC; see Feudtner et al., 2007.
children are observed to be more likely to have died at home than black/non-Hispanic and white/Hispanic children (with the exception of Florida for deaths due to neurologic CCCs among those aged 10-19). This geographic variability suggests that access to home-based services, in addition to any potential difference across race/ethnicity in preferences regarding palliative or end-of-life care, may be a major influence generating these differences.
Hospitalization During the Last Year of Life for Decedents with Complex Chronic Conditions
Hospitals are operationally important places in which to locate pediatric palliative care services. In multiple studies, the majority of patients whose deaths were attributed to a CCC were noted to have been hospitalized at some point during the last year of life. A study of Washington State data found that among deaths of pediatric patients with CCCs, 100 percent of infants and 84 percent of patients older than 1 year of age had been hospitalized prior to death, and many of these hospitalizations had
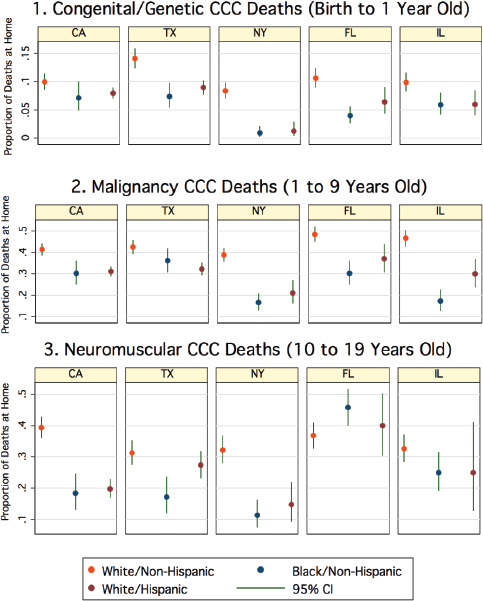
FIGURE F-12 State-level variation regarding location of death among patients with complex chronic conditions.
SOURCE: Based on Multiple Cause of Death data from CDC; see Feudtner et al., 2007.
occurred months prior to death (Feudtner et al., 2003). Hospital-based pediatric palliative care teams are thus positioned to introduce these patients and their parents to palliative care during a hospitalization, including but not limited to terminal hospitalizations.
At the same time, most patients spent the majority of their time outside of the hospital. From the same study mentioned above, focusing on children with CCCs who were 1 year of age or older at the time of their death, Figure F-13 shows the day-by-day prevalence of hospitalization among this population of patients: as patients move closer to the time of death, a larger proportion are residing in the hospital, but not until the final days are half of the patients hospitalized. Thus, a robust system of pediatric palliative care should be able to provide services both in hospitals and in homes. Because the vast majority of time during the last year of life is spent outside of hospitals, mostly at home (and settings such as schools), the development of community-based hospice or palliative care services for the delivery of care in homes is vitally important.
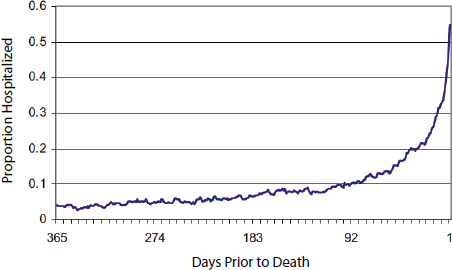
FIGURE F-13 Proportion hospitalized during the last year of life for pediatric patients >1 year of age with complex chronic conditions.
SOURCE: Based on data from Washington State; see Feudtner et al., 2003.
Terminal Hospitalization Lengths of Stay
Among pediatric patients who die during what proves to be a terminal hospitalization, the typical length of stay is a week or less, but with a very long tail of prolonged lengths of stay (see Figure F-14). Length of terminal hospitalizations does not vary substantially by patient age or race/ethnicity, but does vary based on the underlying diagnoses: these long lengths of stay are most common among patients with multiple CCCs, diagnosed either during that terminal hospitalization or during a previous hospitalization.
Intensity and Invasiveness of Terminal Hospitalization Care
Given that hospitals are where most pediatric deaths occur, examining the interventions received during terminal hospitalizations helps in assembling a portrait of pediatric end-of-life care (see Figure F-15). Most hospital deaths occur in intensive care unit (ICU) settings. Patients with no CCCs either quickly enter the ICU setting or remain outside of the ICU setting for the duration of their hospitalization. By contrast, patients with CCCs
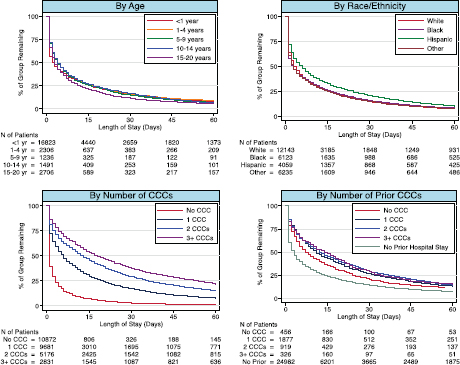
FIGURE F-14 Length of stay among pediatric patients who died in hospitals.
SOURCE: Based on PHIS and Premier data, 2007-2012.
appear to often decompensate during the course of a longer hospitalization and frequently require escalation of interventions and repeated transfers between the floor and the ICU. A similar pattern is observed for starting mechanical ventilation and undergoing the first surgery of a hospitalization
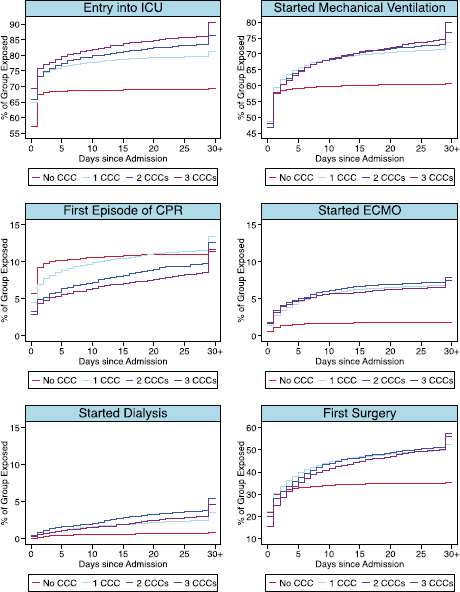
FIGURE F-15 Procedures to which pediatric patients who died in hospitals were exposed.
NOTE: ECMO = extracorporeal membrane oxygenation.
SOURCE: Based on PHIS and Premier data, 2007-2012.
(both of which are common interventions), as well as for the first episode of renal dialysis, cardiopulmonary resuscitation (CPR), or extracorporeal membranous oxygenation (ECMO).
Emergency Departments and Pediatric Deaths
As noted above, in addition to homes and hospitals, EDs are important locations of pediatric end-of-life care, with approximately 22 percent of pediatric deaths occurring in EDs in 2010 (Figure F-16 shows the age distribution of these deaths). Among an estimated (weighted sample) 29.6 million ED visits by pediatric patients (with a mean charge of $1,278), there were 9,699 deaths in EDs (with mean charges of $4,765), with another 4,449 deaths during a subsequent hospitalization (with mean ED charges for this group of $3,019). Among the ED deaths, 9.3 percent had CCCs. Among the ED patients who subsequently died in the hospital, 45 percent had CCCs. This suggests that most rapid demises that occur in EDs are due to acute processes, such as trauma or unexpected overwhelming infection, while patients with serious CCCs are stabilized in EDs and admitted to the
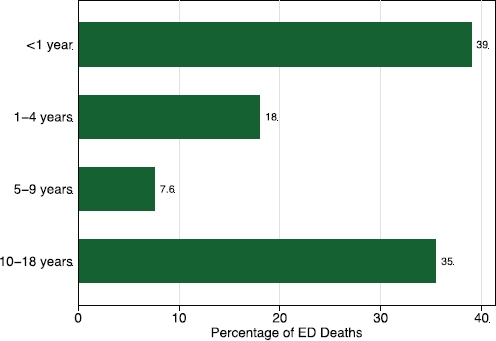
FIGURE F-16 Age distribution of pediatric deaths in emergency departments.
SOURCE: Based on data from NEDS, 2010.
hospital. Importantly, the care received by patients who died in EDs has not been characterized.
Pain and Symptoms Among Pediatric Patients Receiving Pediatric Palliative Care
In 2008, a 1-year cohort study conducted by six major hospital-based pediatric palliative care programs described the characteristics of pediatric patients receiving palliative care services (Feudtner et al., 2011). These patients experienced a broad array of impairments and symptoms, the most common being cognitive and speech impairment, fatigue and sleep problems, enteral intake, seizures, somatic pain, and dyspnea. While pain and dyspnea are prominent symptoms reported near the end of life for patients with cancer, this population includes many patients who are not near the end of life and who have conditions other than cancer, including many with neurologic or genetic conditions. Pediatric palliative care symptom management thus requires an extensive toolkit and considerable expertise. Unfortunately, research regarding pediatric symptom management is woefully lacking. This may be the single most important research priority.
Patterns of Survival Among Pediatric Palliative Care Patients
Pediatric patients receiving palliative care services have long (relative to common assumptions) life expectancies. In the cohort of 515 patients discussed in the previous section, 1-year survival was above 70 percent (Feudtner et al., 2011). This relatively long duration of survival (compared with adult patients receiving palliative care) means that pediatric palliative care services provide chronic care to patients with serious illness and are not limited to end-of-life care. Because many of these patients are hospitalized repeatedly, this also means that pediatric palliative care services often have very high daily census levels, consisting of new and ongoing patients.
Conceptual Models of Pediatric Palliative Care
Based on the findings presented thus far, with pediatric palliative care revealed as chronic care for pediatric patients with a broad array of serious and often complex illnesses, the ideal model of pediatric palliative care is not incompatible with so-called curative care (which often is not capable of effecting a cure as much as substantial life extension), nor does curative care have to be titrated down for palliative care to be titrated up (see Figure F-17). Instead, pediatric palliative care seeks to promote several modes of care simultaneously, including cure-seeking or life-extending care and
quality-of-life and comfort-maximizing care, as well as support for family members and for health care staff.
Core Tasks of Pediatric Palliative Care
The core tasks of pediatric palliative care include the provision of effective interventions to enhance the well-being or comfort of patients, family, and staff; to assist in the logistical coordination of care across a variety of settings, including the hospital, home, and other facilities; and to support problem solving and decision making for patients, their surrogate decision makers, and health care staff (see Figure F-18).
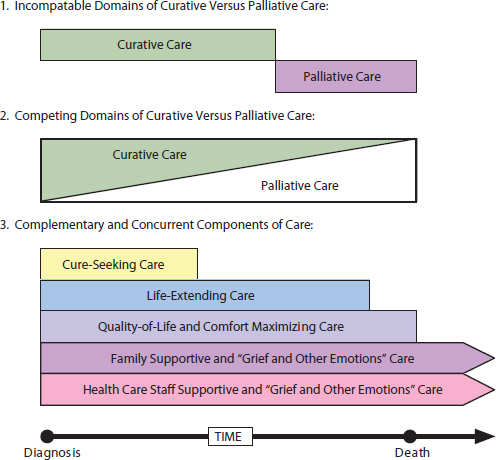
FIGURE F-17 Palliative care as patient-centered complementary and concurrent modes of care.
SOURCE: A version of this figure appears in Feudtner, 2007. Reprinted with permission from Elsevier.
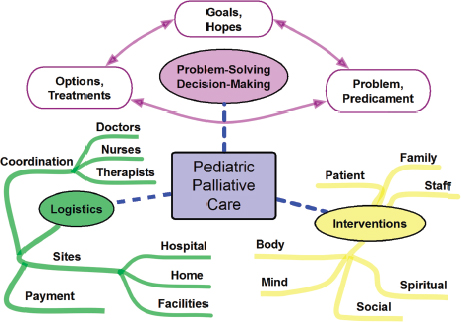
FIGURE F-18 Pediatric palliative care’s three major tasks.
SOURCE: A version of this figure appears in Feudtner, 2007. Reprinted with permission from Elsevier.
Hospital-Based Pediatric Palliative Care Programs
Hospital-based pediatric palliative care programs are more common than was previously the case, arising across the United States. Figure F-19 shows programs identified by a 2012 survey of children’s hospitals (Feudtner et al., 2013).
Establishment of New Hospital-Based Pediatric Palliative Care Programs
Most hospital-based pediatric palliative care programs are of recent vintage, having been established sometime after 2005; 12 new programs were established in 2008 alone, and another 10 were created in 2011 (Feudtner et al., 2013). These programs typically require substantial financial support from their hospital, given the relatively low rates of reimbursement for the kinds of services they provide. Ensuring the financial security of these programs is a major priority.

FIGURE F-19 Locations of hospital-based pediatric palliative care programs.
SOURCE: Feudtner et al., 2013. Reproduced with permission from Journal Pediatrics, Vol. 132, Page 1065, Coypright © 2013 by the AAP.
Staffing of Hospital-Based Pediatric Palliative Care Programs
Hospital-based pediatric palliative care programs are remarkably diverse in terms of staffing. Many programs subsist with a minimal staff, most commonly having less than a full-time equivalent (FTE) of physician time (Feutner et al., 2013). In the above-referenced survey of children’s hospitals, more than half of surveyed programs had only one physician; of programs with more than one physician on staff, many had total physician staffing of less than one full-time equivalent. Staffing by nurses ranged from 0 to 6.6 FTE (with a mean overall FTE 0.8, and for advanced practice nurses in particular, a mean FTE of 0.4). While 66 percent of programs reported
having a social worker, the mean social work FTE was only 0.29. All other members of the interdisciplinary team (including chaplains, child life specialists, bereavement specialists, music and art therapists, and psychologists) had mean FTE levels of 0.16 or less. This survey also demonstrated substantial differences in the clinical services provided by these programs. A major priority for both research and program development is to define and advance hospital-based pediatric palliative care program standards.
Hospital Charges for Pediatric Hospitalizations
We now turn to the financial aspects of pediatric end-of-life care. Ideally, we would be able to analyze cost data, including costs borne by patients, families, hospitals, and payers, but such data do not exist. We therefore focus here on hospital charges to illustrate and examine certain key issues, believing that this analysis can illuminate the financial aspects of pediatric end-of-life care.
We start with all pediatric hospitalizations. Among 8.6 million pediatric hospitalizations (which includes newborns) from 2007 to 2012 in the PHIS and Premier data, the median total charge was $8,167, and the mean was $28,654. The distribution of these charges fits the “Pareto principle” power law distribution almost exactly (see Figure F-20), with 78 percent of all hospital charges being concentrated among the top 20 percent of hospitalizations. Among the 0.5 percent of hospitalizations that ended with the death of the patient, the median charge was $68,279, and the mean was $290,416.
Correlation of Hospital Charges with Length of Stay in Children’s Hospitals
Among all the above pediatric hospitalizations, the median length of stay was 2 days, with a mean of 3.6 days. The range of length of stay was from 0 to 877 days, with the 99th percentile at 35 days. Length of stay is the primary driver of total charges, with a correlation of 0.75 (see Figure F-21).
Long Lengths of Stay and Large Average Charges in Children’s Hospitals
Reinforcing the fact that length of stay is a key driver of pediatric hospitalization charges, the average length of stay skyrockets among those patients with the largest hospital charges (see Figure F-22).
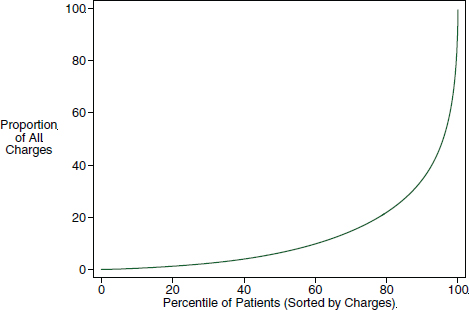
FIGURE F-20 Cumulative distribution of charges among hospitalized pediatric patients.
SOURCE: Based on data from PHIS and the Premier Perspective Database.
Prognosis and Predicted Probability of Death Among Hospitalized Pediatric Patients
Based on previous work, we implemented a prediction of mortality model, which we used as a tool for the subsequent analysis. In these data, the model is reasonably well calibrated. For example, patients with a predicted probability of dying of 0.5 were observed to have a proportion of death between 0.3 and 0.4 (see Figure F-23). Note that the calibration curve demonstrates that the predicted probability is biased upward, with those with the highest predicted probabilities of death never having an observed proportion of death as high as the predicted values.
Average Hospital Charges Across Predicted Probability of Death
Hospital charges are also associated with the probability of death, in a U-shaped function: some patients who die very soon after hospitalization incur relatively small charges, and patients with the largest charges have a much higher than average probability of having died (see Figure F-24).
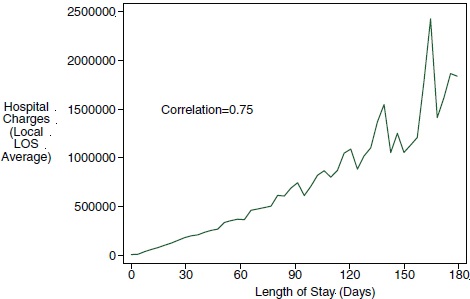
FIGURE F-21 Correlation of charges with length of stay (LOS) in children’s hospitals.
SOURCE: Based on PHIS and Premier data, 2007-2012.
Note, though, that only 6 percent of those patients with the largest charges died. Stated differently, large hospital charges overwhelmingly are for children who survive.
Hospital Charges Across the Range of Predicted Probability of Death
If pediatric palliative care were to focus just on those patients with the highest probability of dying during that hospitalization, and this threshold could be set at a 50 percent predicted probability of dying (which, as was seen earlier, would translate into a slightly lower observed probability of dying), then the case mix would have a higher average hospital charge (approximately $500,000). These patients, though, account for only 4.7 percent of all charges (see Figure F-25). Furthermore, given that these large charges are accumulated over very long lengths of stay and that the probability of dying may have risen dramatically during the course of the hospitalization, the ability of pediatric palliative care to curtail these aggregate costs to a degree that would matter to the overall pattern of pediatric hospital expenditures is likely quite limited.
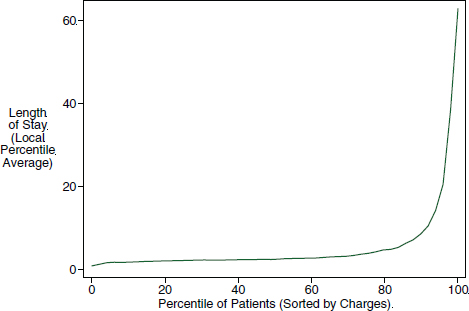
FIGURE F-22 Mean length of stay across the range of charges for patients in children’s hospitals.
SOURCE: Based on PHIS and Premier data, 2007-2012.
This is not to say, however, that hospital-based pediatric palliative care is not cost-effective. With most pediatric palliative care programs requiring operating budgets of approximately $2 million per year, curtailing the length of stay of even a few long-stay terminal hospitalizations per year (or preventing terminal hospitalizations in the first place) would offset operating expenses.
Concurrent Care and Studies of Cost Implications
Beyond the analysis just presented, we used the following keywords and their combinations to search for publications on health care cost savings of pediatric palliative or hospice care: “pediatric or child,” “palliative or hospice,” “costs or (cost effectiveness) or spending or expenditure or savings,” and “health care.” We also checked the citations of some publications to look for other potential papers. This search revealed only three publications that focus on children and compare the cost before and after the initiation of palliative care:
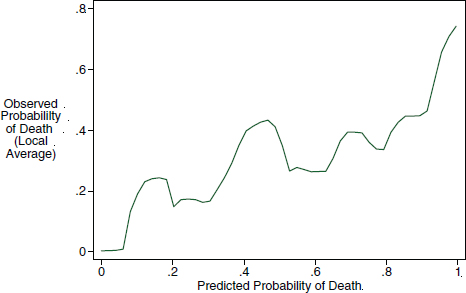
FIGURE F-23 Calibration of the predicted to the observed probability of death.
SOURCE: Based on PHIS and Premier data, 2007-2012.
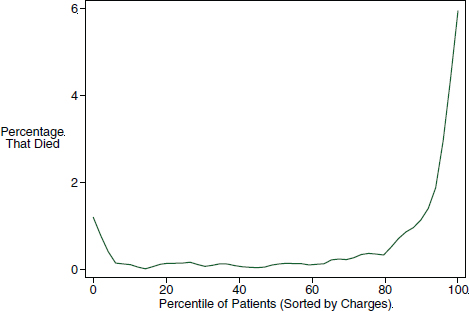
FIGURE F-24 Predicted probability of death across the range of hospital charges.
SOURCE: Based on PHIS and Premier data, 2007-2012.
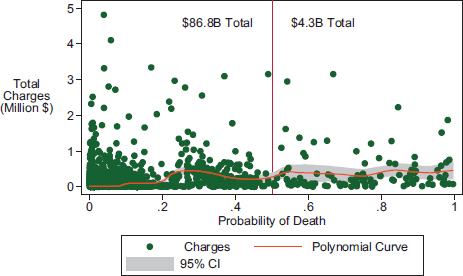
FIGURE F-25 Among patients in children’s hospitals, the typical individual total charge across the range of the predicted probability of death.
NOTE: Total dollar sums are for patients who could be fitted in the model.
SOURCE: Based on PHIS and Premier data, 2007-2012.
- A small study (N = 66) from a children’s hospital in Canada reports that providing respite care resulted in a mean decrease of $4,251.95 per month per patient (Pascuet et al., 2010).
- A California project shifted palliative care from hospital settings to in-home community-based care. The result was cost savings of $1,677 per child per month on average—an 11 percent decrease in spending on a traditionally high-cost population (Gans et al., 2012).
- Analyses involving data on Florida Medicaid children found that pediatric hospice users had higher inpatient (2.5 times), outpatient (1.1 times), ED (1.9 times), and pharmacy (2.3 times) expenditures than non-hospice users (a finding perhaps due to residual confounding by indication, whereby patients with greater ongoing need are referred to hospice more often than otherwise similar patients with less need). Black non-Hispanic and Hispanic children and children of other races incurred $730 to $880 less in hospice expenditures than whites (Knapp et al., 2009).
These mixed findings regarding the impact of pediatric palliative or hospice care on health care expenditures are consistent with the findings of a recent Cochrane Database Systematic Review focused on adult studies
regarding the impact of home-based services. While receipt of such services is warranted based on symptom management and preferred place of dying, the cost implications are mixed (Gomes et al., 2013).
To assess the cost impact of pediatric palliative or hospice services, studies will have to ensure that any change in expenditures before and after exposure is due to exposure to the service, and not to a temporally confounded choice to pursue palliative or hospice care at the same time as the choice is made to forego or avoid further hospital-based or highly invasive forms of care.
Other Key Considerations Regarding Charge/Cost-Focused Evaluations of Pediatric End-of-Life Care
First, as argued above, while there may be greater certainty as death draws near (within hours or days), the potential cost savings that could arise from such prognostic knowledge would affect expenditures only from that point forward. And because large hospital bills are built on long lengths of stay, the marginal impact on the overall health care cost for hospital care may be more limited than is commonly hoped.
Second, many of the pediatric patients who consume the most resources are disabled, and they are vulnerable because of both disability-associated stigma and the impoverishment of families that can result from having a medically complex patient in the family. These patients are also protected by law from discrimination.
Gaps in Knowledge
Critical gaps exist in the knowledge and evidence base regarding many aspects of pediatric palliative care, including the follow six priority areas:
- Comparative effectiveness studies of
- • Symptom management approaches
- – Pharmacologic
- - Effectiveness of different medications and use of medications
- - Potential problems of polypharmacy and drug-drug interactions
- – Nonpharmacologic
- – Pharmacologic
- • Different forms of providing decision support to patients and their surrogate decision makers
- – How to communicate clearly regarding the patient’s clinical situation
- • Symptom management approaches
-
- – How to communicate effectively regarding potential benefits and harms of medical interventions
- – How to solicit, examine, and potentially adapt goals of care over time
- – How to support emotional as well as cognitive processing of this information
- – Different bereavement support interventions for family members and community peers
- Descriptions of care
- • Received through hospice services and home nursing services, individually and in the concurrent care model
- • Received in different settings, including EDs, outpatient facilities, and long-term care facilities
- Cohort studies examining the effect of receipt of palliative or hospice care
- • On patient-reported outcomes
- • On proxy reports by parents or others regarding patient experience
- • On outcomes defined using large clinically detailed datasets
- Well-designed cost analyses regarding
- • The care received by pediatric patients with serious illness or complex chronic conditions
- • The impact of receipt of palliative care or hospice services
- Studies of the impact of having a child with serious illness, while alive and after death
- • On parents
- • On siblings
- • On other family members, such as grandparents
- • On the patient’s peer network of friends in school and elsewhere
- • Whether these impacts are modified if the patient or family is exposed to palliative or hospice care services
- Studies of hospital-based pediatric palliative and community-based pediatric hospice services
- • How to best staff these services
- • How to optimize interdisciplinary team function
- • Best management practices
- • Financing challenges and best practices
REFERENCES
Feudtner, C. 2007. Collaborative communication in pediatric palliative care: A foundation for problem-solving and decision-making. Pediatric Clinics of North America 54(5):583-607.
Feudtner, C., D. A. Christakis, and F. A. Connell. 2000. Pediatric deaths attributable to complex chronic conditions: A population-based study of Washington State, 1980-1997. Pediatrics 106(1, Pt. 2):205-209.
Feudtner, C., D. L. DiGiuseppe, and J. M. Neff. 2003. Hospital care for children and young adults in the last year of life: A population-based study. BMC Medicine 1(1):3.
Feudtner, C., J. A. Feinstein, M. Satchell, H. Zhao, and T. I. Kang. 2007. Shifting place of death among children with complex chronic conditions in the United States, 1989-2003. Journal of the American Medical Association 297(24):2725-2732.
Feudtner, C., T. I. Kang, K. R. Hexem, S. J. Friedrichsdorf, K. Osenga, H. Siden, S. E. Friebert, R. M. Hays, V. Dussel, and J. Wolfe. 2011. Pediatric palliative care patients: A prospective multicenter cohort study. Pediatrics 127(6):1094-1101.
Feudtner, C., J. W. Womer, R. Augustin, S. S. Remke, J. Wolfe, S. Friebert, and D. E. Weissman. 2013. Pediatric palliative care programs in children’s hospitals: A cross-sectional national survey. Pediatrics 132(6):1063-1070.
Fraser, L. K., M. Miller, R. Hain, P. Norman, J. Aldridge, P. A. McKinney, and R. C. Parslow. 2012. Rising national prevalence of life-limiting conditions in children in England. Pediatrics 129(4):e923-e929.
Gans, D., G. F. Kominski, D. H. Roby, A. L. Diamant, X. Chen, W. Lin, and N. Hohe. 2012. Better outcomes, lower costs: Palliative care program reduces stress, costs of care for children with life-threatening conditions. Policy Brief (UCLA Center for Health Policy Research (PB2012-3):1-8.
Gomes, B., N. Calanzani, V. Curiale, P. McCrone, and I. J. Higginson. 2013. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database of Systematic Reviews 6:CD007760.
Knapp, C. A., E. A. Shenkman, M. I. Marcu, V. L. Madden, and J. V. Terza. 2009. Pediatric palliative care: Describing hospice users and identifying factors that affect hospice expenditures. Journal of Palliative Medicine 12(3):223-229.
Lenton, S., P. Stallard, M. Lewis, and K. Mastroyannopoulou. 2001. Prevalence and morbidity associated with non-malignant, life-threatening conditions in childhood. Child: Care, Health and Development 27(5):389-398.
Pascuet, E., L. Cowin, R. Vaillancourt, W. Splinter, C. Vadeboncoeur, L. G. Dumond, A. Ni, and M. Rattray. 2010. A comparative cost-minimization analysis of providing paediatric palliative respite care before and after the opening of services at a paediatric hospice. Healthcare Management Forum 23(2):63-66.








































