Abstract: This chapter examines graduate medical education (GME) financing, focusing particularly on Medicare but including Medicaid and Veterans Health Administration GME funding as well as Health Resources and Services Administration programs that support residency training. Total federal GME funding exceeds $15 billion per year. The financial underpinnings of the GME enterprise are complex and largely undocumented. The committee found few informative data on GME financing and its outcomes. As a result, the financial impact of residency training programs on teaching hospitals and other sponsoring organizations is not well understood. Medicare GME payments are based on statutory formulas that were developed at a time when hospitals were the central—if not exclusive—site for physician training. The rules continue to reflect that era. GME monies are distributed primarily to teaching hospitals, which in turn have fiduciary control over the funds. This creates a disincentive to training in non-hospital settings where most residents will eventually practice and most people seek health care services. Because the Medicare formulas are linked to Medicare patient volume, the system disadvantages children’s hospitals, safety net hospitals, and other training sites that care for mostly non-elderly patients. Medicare-supported training slots are frozen where they existed almost two decades ago, perpetuating inequities in the geographic distribution of training slots and ignoring changes in the geography and demography of the U.S. population. Medicare GME funding is formula-driven, without accountability
for national health care needs or priorities. Complete and comparable data on the use or outcomes of GME funds are not available. The current GME financing system offers little, if any, incentives to improve the quality or efficiency of physician training.
Few taxpayers know that significant financial public support underlies the graduate-level training of the nation’s physicians. Perhaps even fewer people realize that two federal programs—Medicare and Medicaid—distribute an estimated $12 to 14 billion each year to support teaching hospitals and other training sites that provide graduate medical education (GME). Physicians who train in Medicare- or Medicaid-supported residencies are under no obligation to accept Medicare or Medicaid patients when they enter practice, nor are they required to provide any other types of services to these programs.
The objective of this chapter is to examine public spending on GME and what is known about private sources of GME support. The chapter begins with a brief overview of the principal sources of GME funding. It then describes the methods used by Medicare, Medicaid, the Health Resources and Services Administration (HRSA), and the Veterans Health Administration (VHA) to distribute these funds. The next section reviews what is known about the financial costs and benefits associated with residency training for teaching hospitals. The chapter concludes with a discussion of the implications and consequences of the current system for funding GME.
Tracking the flow of public GME funds is daunting, as Figure 3-1 illustrates. The financial underpinnings of the GME enterprise are complex and largely undocumented. Federal funding for GME includes both mandatory (i.e., Medicare and the federal Medicaid match) and discretionary appropriations (e.g., HRSA, VHA, Department of Defense [DoD]). Most states support GME through their Medicaid programs, and some states provide other GME support through state-based programs such as loan repayment incentives to address health workforce shortages (Henderson, 2013; Pathman et al., 2012; Spero et al., 2013).
GME is also supported by private sources. Private funding is difficult to quantify but may be significant. Private insurers support GME implicitly by paying higher rates to teaching institutions. Hospitals, universities, physicians’ organizations, and faculty practice plans also support residencies and fellowships. Private philanthropy and gifts or grants from industry (primarily pharmaceutical and medical device companies) are another source of financial support (Spero et al., 2013; Wynn, 2012). Many of these GME funding streams individually represent a minor fraction of GME funding
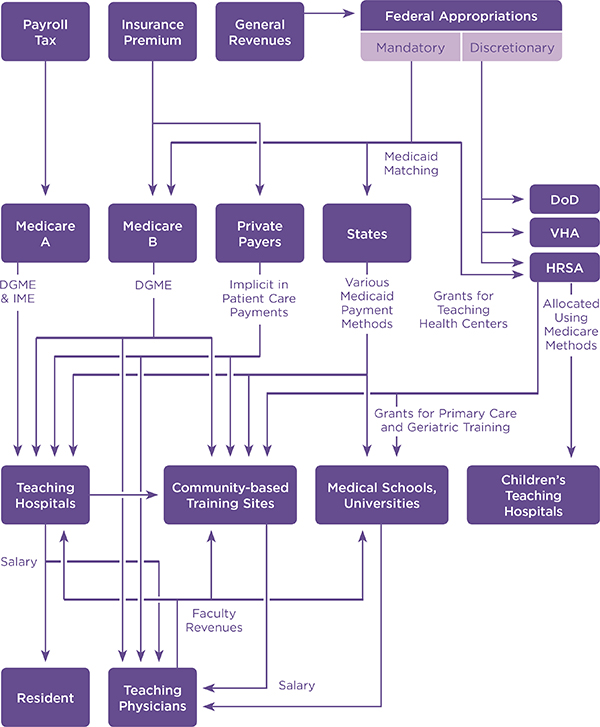
FIGURE 3-1 Current flow of GME funds.
NOTE: DGME = direct graduate medical education; DoD = Department of Defense; HRSA = Health Resources and Services Administration; IME = indirect medical education.
SOURCE: Adapted from Wynn, 2012 (Committee of Interns and Residents Policy and Education Initiative White Paper, “Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety”).
nationally, but for some teaching programs they may support most, if not all, of the operating budget.
Table 3-1 provides the most recent available estimates of GME funding by source. The single largest explicit contributor to GME is Medicare ($9.7 billion), followed by Medicaid ($3.9 billion) and the VHA ($1.4 billion). HRSA distributes approximately $0.5 billion through a variety of GME-related programs (HRSA, 2013c).
TABLE 3-1 Source and Estimated Amount of GME Funding, Selected Years
| Funding Source | Fiscal Year | Funding (in billions) |
| Medicare (total) | 2012 | $9.7 |
|
Acute care hospitals |
$9.6 | |
|
Indirect payments |
6.8 | |
|
Direct payments |
2.6 | |
|
Specialty hospitals |
0.1 | |
| Medicaid | 2012 | 3.9 |
| Veterans Health Administration (VHA) (total) | 2012 | 1.437 |
|
Indirect payments |
0.816 | |
|
Direct payments |
0.621 | |
| Department of Defense | NA | |
| HRSA (total ~$.464) | ||
|
Children’s Hospitals GME |
2013 | 0.251 |
|
NHSC Loan Repayments |
2011 | 0.096 |
|
Teaching Health Centers GME |
2011 | 0.046 |
|
Title VII Primary Care Programs |
2011 | 0.071 |
| Other state funding | NA | |
| Private insurers | NA | |
| Other private sources | NA | |
NOTES: VA indirect payments include training of all health professionals. Medicaid includes federal and state shares. CHGME estimate is from its operating budget while under sequestration in 2013. NA=not available.
SOURCES: Henderson, 2013; HRSA, 2013b. Medicare estimates provided by Marc Hartstein, Director, Hospital and Ambulatory Policy Group, Center for Medicare, CMS, September 4, 2013 (personal communication). VHA estimates provided by Barbara K. Chang, Director of Medical and Dental Education, VHA Office of Academic Affiliations, July 15, 2013 (personal communication).
The Medicare program has funded GME since its inception in 1965. Congress apparently intended Medicare GME funding to be temporary but wanted to ensure that Medicare beneficiaries had access to the highest quality hospitals (Iglehart, 1999). When the Medicare legislation was enacted, reports from the House and Senate said, “Educational activities enhance the quality of care in an institution, and it is intended, until the community undertakes to bear such education costs in some other way, that a part of the net cost of such activities (including stipends of trainees, as well as compensation of teachers and other costs) should be borne to an appropriate extent by the hospital insurance program.”1
At the outset, Medicare GME payments to teaching hospitals were calculated based solely on hospitals’ costs. With the advent of the Medicare prospective payment system (PPS) for acute care hospitals in 1983, two separate GME funding streams were established for teaching hospitals2: (1) Direct Graduate Medical Education (DGME) funding to cover the direct expenses associated with residency training (e.g., residents’ and faculty salaries and benefits and certain administrative and overhead costs); and (2) Indirect Medical Education (IME) funding, an adjustment to individual teaching hospitals’ PPS inpatient rates to help defray the additional costs of providing patient care thought to be associated with sponsoring residency programs. Of the $9.6 billion Medicare paid to acute care teaching hospitals for GME in 2010, about $6.8 billion (70.8 percent) were via the IME adjustment and $2.8 billion via DGME payments (29.2 percent).3 An additional $0.1 billion was paid to specialty hospitals for DGME and to psychiatric and rehabilitation inpatient facilities for IME.
Box 3-1 provides a timeline for the legislation that has shaped Medicare GME and other federal GME funding.
Medicare DGME and IME funds distribution to acute care hospitals is governed by strict, statutory formulas that are described below. It is important to note that Medicare GME funding was never intended to cover teaching costs for non-Medicare patients. Both the DGME and IME formulas include variables that tie payments to a teaching institution’s volume of Medicare patients. Regardless, most, if not all, residencies must train
________________
11965 Social Security Act (Senate Report No. 404, Pt. 1, 89th Congress, 1st Sess. 36 [1965]; H.R. No. 213, 89th Cong., 1st Sess. 32 [1965]).
2 Direct Graduate Medical Education and Indirect Medical Education payments to teaching hospitals for Medicare managed care enrollees are calculated to be equivalent to payments for fee-for-service Medicare beneficiaries (Wynn et al., 2013).
3 Personal communication, Marc Hartstein, Director, Hospital and Ambulatory Policy Group, Medicare Center, Centers for Medicare & Medicaid Services, September 4, 2013 (e-mail).
BOX 3–1
Legislative Milestones in Medicare Financing of Graduate Medical Education (GME)
| 1965 | The Medicare program is created and establishes retrospective cost-based reimbursement for hospital inpatient stays—certain Direct Graduate Medical Education (DGME) costs are included (e.g., trainees’ stipends, faculty compensation, and other costs). | |
| 1983 | Medicare cost-based reimbursement for acute care hospital operating costs ends with implementation of the Prospective Payment System (PPS). Medicare continues to pay for DGME on a cost basis but also makes an Indirect Medical Education (IME) adjustment to PPS rates: | |
|
||
| 1985 | Consolidated Omnibus Budget Reconciliation Act (COBRA) (Public Law 99-272) establishes a prospective payment for DGME and revises the IME formula. | |
|
||
| 1987 | Omnibus Budget Reconciliation Act (OBRA) (Public Law 100-203) reduces the IME adjustment factor from 8.1 to 7.7 percent effective in 1989. | |
| 1993 | OBRA of 1993 (Public Law 103-66) increases the PRA by about 6 percent for primary care and obstetrics trainees in 1994 and 1995. In addition: | |
|
||
| 1997 | Balanced Budget Act (BBA) (Public Law 105-33) includes provisions to stem increases in GME payments while extending GME to some non-hospital settings: | |
|
||
| 1999 | Balanced Budget Refinement Act of 1999 (Public Law 106-113) includes several changes to GME funding: | |
The Health Research and Quality Act (Public Law 106-129) creates the Children’s Hospital Graduate Medical Education (CHGME) Program to support residency training in freestanding children’s hospitals. The Act authorizes the Health Resources and Services Administration to make DGME and IME payments to eligible institutions. |
||
| 2000 | Medicare, Medicaid, and State Children’s Health Insurance Program (SCHIP) Benefits Improvement and Protection Act (Public Law 106-554) freezes the maximum PRA to 140 percent of the locally adjusted national average amount while also delaying or reversing previously enacted downward adjustments to DGME and IME: | |
|
||
| 2003 | Medicare Prescription Drug, Improvement, and Modernization Act (Public Law 108-173) includes several GME provisions: | |
|
||
| 2006 | The CHGME Support Reauthorization Act (Public Law 109-307) extends the program’s funding through 2011 and introduces a reporting requirement for participating children’s hospitals. | |
| 2010 | The Patient Protection and Affordable Care Act (ACA) (Public Law 111-148) contains several GME-related provisions focused on extending GME to underserved areas and populations: | |
|
||
aThe cut only applies to slots that were not filled in the previous 3 years.
bSome teaching hospitals are exempt, including new training sites in the midst of building their programs.
SOURCES: Baumann et al., 2004; COGME, 2013; Congressional Research Service, 2010; HRSA, 2011b; HRSA Bureau of Health Professions, 2012; Johns, 2010; MedPAC, 2001; National Health Policy Forum, 2001; Nguyen and Sheingold, 2011; Rich et al., 2002; Roth and Yolin, 2011; Wynn and Kawata, 2002.
physicians to treat a wide range of patients—many of whom are under age 65 and not eligible for Medicare coverage.
The mechanics and implications of the Medicare formulas are discussed below.
Direct GME Payment Method
The DGME payment for an individual institution is calculated by multiplying three factors (Wynn et al., 2006):
Weighted resident count * Per-resident amount * Medicare bed-day ratio
- (1) Weighted resident count: A 3-year rolling average of the hospital’s weighted number of full-time equivalent (FTE) residents in accredited programs in the most recent 3-year period (after taking into account the cap on allopathic and osteopathic residents).4 “Weighted” refers to the following: Only trainees in their initial residency period (i.e., the minimum time required for board eligibility or 5 years, whichever is shorter) are counted as 1.0 FTE. Other residents or fellows are counted as 0.5 FTE.
- (2) Per-resident amount (PRA): A dollar amount calculated by dividing the individual hospital’s base year (i.e., 1984 or 1985) DGME costs by the weighted residents count (adjusted for geographic differences and inflation).
- (3) Medicare day ratio: The ratio of the hospital’s Medicare inpatient days to total inpatient days (to approximate Medicare’s share of the training costs).
Per-Resident Amount
Because the PRA calculation is based on hospital costs in the mid-1980s, the DGME calculation is tied to a 30-year-old payment scale that has little relevance to today’s health care delivery system or current residency training programs. It also perpetuates significant inequities in GME payments among hospitals, localities, and geographic regions (Fryer et al., 2001).
As noted in Box 3-1, Congress has taken several steps to reduce hospital-to-hospital variation in the PRA. It established a floor and ceiling on
________________
4 Only residency programs accredited by the Accreditation Council for Graduate Medical Education, Council on Osteopathic Postdoctoral Training, Commission on Dental Accreditation of the American Dental Association, or Council on Podiatric Medical Education of the American Podiatric Medical Association are eligible for Medicare, Medicaid, and other federal funding. Chapter 4 describes the role of accreditation in the governance of GME funding.
hospitals’ PRAs in the Balanced Budget Refinement Act (BBRA) of 1999 by mandating that a hospital’s PRA could not be less than 70 percent of the level of the national average PRA. In 2000, the Benefits Improvement and Protection Act5 raised the minimum to 85 percent and it remains at that level today. The BBRA also eliminated the inflation adjustment for PRAs that were more than 140 percent of the locality-adjusted national average for 2 years; the Medicare Prescription Drug, Improvement, and Modernization Act extended that freeze through FY 2013. In 2008, the national average PRA was $98,846 (Wynn et al., 2013).
As the above formula indicates, the hospital’s PRA, weighted count of residents, and ratio of Medicare inpatient days to total inpatient days together determine the amount of DGME funds that each institution receives. Table 3-2 shows the average of each component of the DGME formula for different categories of teaching institutions based on geographic area, the number of residents on staff, and the low-income patient percentage (LIPP). On average, hospitals are paid 37 percent of their PRA for each (“adjusted”) resident FTE. However, there is considerable variation in the percentage of Medicare bed-days across hospitals and this factor significantly impacts an institution’s aggregate DGME funding. Safety net hospitals (i.e., those with a high LIPP), for example, tend to have relatively low Medicare ratios and, thus, low Medicare DGME PRAs. In 2008, the average Medicare PRA for safety net hospitals with the highest LIPP (65 percent or greater), was only $25,306, while for hospitals with a 15 to 25 percent LIPP the average was $46,857, more than 85 percent higher.
IME Payment Method
All acute care hospitals are paid a fixed diagnosis-related group (DRG) payment rate for each Medicare discharge based on each patient’s DRG assignment. In teaching hospitals, the DRG payment is increased by the IME adjustment factor.6 IME is one of several adjustments to Medicare DRG payments. Other adjustments address differences in local wages, disproportionate share of low-income patients, extraordinary high-cost cases, and other factors. The underlying assumptions in the IME payment adjustment are that residency training reduces a hospital’s productivity (efficiency)—thus increasing the costs of providing services—and that the Medicare program should pay for the higher spending. The IME amount was intended as a proxy for these costs.
When the IME operating adjustment was first established in law, it
________________
5 Public Law 106-554.
6 See Nguyen and Sheingold (2011) for a more detailed and comprehensive description of the Medicare IME adjustment.
TABLE 3-2 Per-Resident Amounts and Medicare Share by Hospital Characteristic, 2008
| Hospital Characteristic | Number of Hospitals | Number of Residents | Average PRA | Medicare Share of Days (%) | Medicare Share of the PRA ($) |
| All hospitals | 1,103 | 97,067 | $98,846 | 37.0% | $36,556 |
| Geographic area | |||||
| Large urban | 671 | 71,481 | 102,261 | 35.9 | 36,751 |
| Other urban | 379 | 24,414 | 89,820 | 39.8 | 35,737 |
| Rural | 53 | 1,171 | 86,218 | 48.6 | 41,903 |
| Number of FTE residents | |||||
| 0 < 10 | 294 | 1,241 | 95,644 | 42.5 | 40,612 |
| 10 < 25 | 222 | 3,808 | 96,243 | 47.3 | 45,506 |
| 25 < 100 | 309 | 15,607 | 95,791 | 44.2 | 42,343 |
| >= 100 | 278 | 76,412 | 99,696 | 34.9 | 34,762 |
| Low-income patient percentage | |||||
| 0 < 15 | 260 | 11,025 | 93,180 | 30.8 | 28,669 |
| 15 < 25 | 293 | 16,109 | 95,927 | 48.8 | 46,857 |
| 25 < 50 | 384 | 44,836 | 97,221 | 39.3 | 38,247 |
| 50 < 65 | 79 | 14,098 | 103,698 | 32.9 | 34,141 |
| >= 65 | 87 | 10,999 | 108,789 | 23.3 | 25,306 |
NOTE: FTE = full-time equivalent; PRA = per-resident amount. Excludes 38 hospitals that had reported GME costs but did not receive direct graduate medical education payments based on a current year resident.
SOURCE: Wynn et al., 2013. (c) RAND Corporation. Reprinted with permission.
was based on an analysis of spending differences between teaching and non-teaching hospitals (Nguyen and Sheingold, 2011). At that time, the evidence suggested “teaching intensity” (as measured by the resident-to-bed ratio) and a large proportion of low-income patients were both significantly associated with higher spending per Medicare discharge. There was concern that the new DRG payment system might underpay and, thus, harm teaching hospitals. More recently, two analyses have raised questions about these assumptions. The Medicare Payment Advisory Commission (MedPAC) has concluded that the current 5.5 percent is more than twice the level indicated through multivariate regression analysis of the teaching effect on hospital Medicare costs per discharge (MedPAC, 2010). In their later study, Nguyen and Sheingold (2011) came to similar conclusions.
Medicare makes a different IME adjustment to its payment for capital-related spending. This adjustment is set administratively based on a multivariate regression analysis of the teaching effect on total spending per discharge. The formula specifies teaching intensity differently, and because the capital IME adjustment is based on the measured effect of teaching, the adjustment is smaller. The capital-related IME payments are approximately 5.0 percent of total IME payments to acute care hospitals.
Specialty Hospitals
Specialty hospitals with GME programs—including children’s hospitals, psychiatric facilities, rehabilitation hospitals, long-term care hospitals, and critical access hospitals—are eligible for Medicare DGME payments under the same rules as acute care teaching hospitals. However, the IME adjustment for specialty hospitals differs by the type of facility. Among the hospitals paid under a prospective payment system, rehabilitation and psychiatric hospitals and units receive an explicit IME adjustment; long-term care hospitals do not. Medicare pays children’s and cancer hospitals on a reasonable cost basis so that any higher costs that these facilities occur for teaching activities are included in the costs that Medicare uses to determine its reimbursement rate for services provided to Medicare beneficiaries. Medicare pays critical access hospitals7 for most inpatient and outpatient care at 101 percent of reasonable costs, including any costs attributable to teaching activities.
Cap on Number of Medicare-Funded Training Slots
Until the enactment of the Balanced Budget Act (BBA) of 1997,8 Medicare support of GME was open-ended (Iglehart, 1999). Before the Act, hospitals had a potent financial incentive to add new residency slots because each new position generated additional Medicare PRA and IME revenues (MedPAC, 2003). In response to concerns about an oversupply of physicians9 and increasing Medicare costs, the BBA10 capped the number of Medicare-supported physician training slots (MedPAC, 2003; Salsberg et al., 2008). Hospitals are free to add residents beyond their cap, but these trainees do not generate additional Medicare revenues. The cap on Medicare
________________
7 Critical access hospitals are small rural hospitals that have an average annual length of stay of 96 hours or less.
8 Public Law 105-33.
9 As Chapter 2 describes, in the 1990’s there were widespread concerns that the nation faced a significant surplus of physicians.
10 The cap on GME funded training slots was just one of many provisions in the BBA of 1997 intended to curtail Medicare spending.
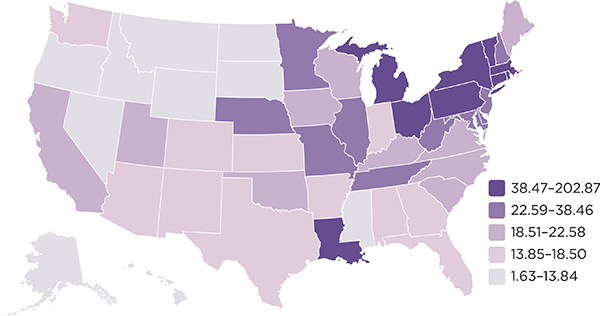
FIGURE 3-2 Number of Medicare-funded training positions per 100,000 population, 2010.
SOURCE: Mullan et al., 2013.
funding was set at each hospital’s resident count in the cost report period ending on or before December 31, 1996. With this step, the geographic distribution of Medicare-supported residencies was essentially frozen in place without regard for future changes in local or regional health workforce priorities or the geography or demography of the U.S. population. As Figure 3-2 illustrates, Medicare-supported slots are most highly concentrated in the Northeastern states, as is most of Medicare GME funding.
Hospitals without residency programs can obtain Medicare-funded training slots if they develop newly accredited teaching programs. After 5 years, Medicare then caps the hospital’s slots at the highest total number of residents for all specialty programs during that period. Only hospitals with programs created on or after January 1, 1995, are eligible to add slots in this way.11 After the cap is implemented, rural hospitals already receiving Medicare funding cannot increase funded slots for their existing program(s) but can receive additional Medicare-funded slots for any newly approved specialty programs.
The cap on training slots and its impact on the capacity of the GME system have stimulated vigorous debate (Goodman and Robertson, 2013; Green et al., 2013; Grover and Niecko-Najjum, 2013; Iglehart, 2013; Kirch
________________
11 See the following sources for further details on Medicare rules regarding the cap: CMS, 2013; Roth and Yolin, 2011.
et al., 2012). There are concerns, for example, that limiting Medicare GME subsidies in this way constrains the total number of available training positions and, thus, the production and national supply of physicians (as was the cap’s original intent). The evidence suggests otherwise, however. Many hospitals have expanded their teaching programs despite the cap. Teaching hospitals have added nearly 17,000 slots12 since the BBA limits were first implemented, an increase of about 17 percent (Brotherton and Etzel, 2013; Salsberg et al., 2008). There is no way to know whether the growth in GME positions would have been significantly greater, as some argue, without the caps. However, the available evidence shows that, for the last decade, the number of training positions has grown at the same pace as the period before the caps (Chandra et al., 2014).
Legislative attempts have been made to redistribute Medicare-funded training slots, but such efforts focused on reallocating vacant slots rather than changing the overall geographic distribution of Medicare GME support. In 2003, the Medicare Prescription Drug, Improvement, and Modernization Act13 sought to redistribute 3,000 unused Medicare-funded slots (CMS, 2004). Although the top priority for the redistribution was to expand training in rural areas, the impact on training in rural areas was minimal. Less than 3 percent of the redistributed positions were in rural areas and, of the 304 hospitals given additional slots, only 12 were rural institutions (Chen et al., 2013). More recently, the Patient Protection and Affordable Care Act (ACA)14 redistributed 65 percent of vacant, Medicare-funded slots and established rules for redistributing them to primary care and general surgery programs in states with low resident-to-population ratios (Roth and Yolin, 2011).
Medicare GME Payments to Non-Hospital Settings
As Figure 3-1 illustrates, most of the Medicare GME funding is distributed to teaching hospitals because that is where most clinical training takes place. Though GME programs may be sponsored by a teaching hospital, medical school, or educational consortium, Medicare funds are paid to the sites where training occurs and those organizations have direct fiduciary control over the use of the funds, whether they are the sponsor of the GME program or serve as an affiliate that “hosts” resident rotations.
Approximately 70 percent of Medicare GME funds are distributed
________________
12 The 17,000 slots are for Accreditation Council for Graduate Medical Education–accredited positions; data on the growth in osteopathic and non-accredited training slots are not available.
13 Public Law 108-173. Also referred to as the Medicare Modernization Act.
14 Public Law 111-148.
to acute care hospitals via the IME adjustment; the balance is distributed through the DGME payments (see Table 3-1). Non-hospital training sites may be eligible to receive DGME payments if they incur most of a residency program’s costs; in contrast, hospitals may be eligible to receive DGME payments for residents that rotate to non-hospital settings if the hospital pays for all or most of the resident’s training costs. Thus, community-based ambulatory care sites and other non-hospital sites are eligible for significantly less funding than teaching hospitals. Non-hospital teaching sites may well be faced with the types of additional training-related experiences that IME was created to address, but they are not eligible for these payments because they do not receive DRG payments.
In the context of this financial disincentive toward non-hospital training, it should be noted that the vast majority of clinical training occurs in teaching hospitals—even for primary care residencies. As Chapter 2 described, there is a striking mismatch between the sites where residents are trained compared with the sites where they are likely to spend most of their careers (Sisson and Dalal, 2011). As Table 3-3 shows, in academic year 2012-2013, teaching hospitals sponsored almost half (49.9 percent) of all residency programs and about half of all residents (52.1 percent) trained in programs sponsored by teaching hospitals. Institutions with multiple programs sponsored the vast majority of residency programs (96.1 percent). Community hospitals and ambulatory care settings sponsored less than 1.0 percent of residency programs and residents.
The ACGME views sponsoring organizations as the entities with the ultimate responsibility—both financial and academic—for residency programs.15 Medicare payments, however, are not aligned, in that funds are provided to the teaching site, rather than to the sponsoring organization. Often the sponsoring organization is a teaching hospital with residents learning on site and thus receiving Medicare funds directly. However, some sponsors of GME (i.e., those that are not teaching hospitals, or teaching hospitals that utilize affiliated training sites) do not have the fiscal control needed to select training sites based on curricular needs.
________________
15 The Accreditation Council for Graduate Medical Education (ACGME) defines a GME sponsoring institution as an “organization (or entity) that assumes the ultimate financial and academic responsibility for a program of GME. The sponsoring institution has the primary purpose of providing educational programs and/or health care services (e.g., a university, a medical school, a hospital, a school of public health, a health department, a public health agency, an organized health care delivery system, a medical examiner’s office, a consortium, an educational foundation)” (ACGME, 2013, p. 9). The American Osteopathic Association (AOA) defines sponsoring organizations as “base institutions which conduct AOA-approved training programs and issue trainee contracts”; these included hospitals, federally qualified health centers, community teaching health centers, freestanding ambulatory accredited surgery centers, and colleges of osteopathic medicine (AOA, 2012).
| Programs | Residents | Sponsors | ||||
| Number | Percent | Number | Percent | Number | Percent | |
| Multi-Program Sponsors | ||||||
| All multi-program sponsors | 9,276 | 100.0 | 112,780 | 100.0 | 437 | 100.0 |
| General/Teaching Hospital | 4,627 | 49.9 | 57,745 | 51.2 | 255 | 58.4 |
| Medical School - LCME UMC | 3,304 | 35.6 | 41,322 | 36.6 | 80 | 18.3 |
| Other | 526 | 5.7 | 5,475 | 4.9 | 21 | 4.8 |
| Consortium of Hospitals | 430 | 4.6 | 5,306 | 4.7 | 11 | 2.5 |
| Children’s Hospitals | 231 | 2.5 | 1,972 | 1.7 | 11 | 2.5 |
| Other Specialized Care | 64 | 0.7 | 432 | 0.4 | 6 | 1.4 |
| Ambulatory Care Clinic/Office | 40 | 0.4 | 156 | 0.1 | 3 | 0.7 |
| Other Specialized Hospital | 17 | 0.2 | 225 | 0.2 | 13 | 3.0 |
| Office | 14 | 0.2 | 13 | 0.0 | 13 | 3.0 |
| Community Hospital or Independent Medical Center | 7 | 0.1 | 85 | 0.1 | 9 | 2.1 |
| Federally Qualified Health Center | 1 | 0.0 | 29 | 0.0 | 1 | 0.2 |
| Unknown | 1 | 0.0 | 7 | 0.0 | 1 | 0.0 |
| Single-Program Sponsors | ||||||
| All single-program sponsors | 369 | 100.0 | 5,322 | 100.0 | 313 | 100.0 |
| General/Teaching Hospital | 183 | 49.6 | 3,573 | 67.1 | 154 | 49.2 |
| Other | 66 | 17.9 | 536 | 10.1 | 62 | 19.8 |
| Ambulatory Care Clinic/Office | 26 | 7.0 | 143 | 2.7 | 23 | 7.3 |
| Children’s Hospital | 19 | 5.1 | 295 | 5.5 | 7 | 2.2 |
| Other Specialized Hospital | 17 | 4.6 | 225 | 4.2 | 13 | 4.2 |
| Pathology Lab/Medical Examiner’s Office | 14 | 4.0 | 13 | 0.0 | 13 | 4.0 |
| Office | 14 | 3.8 | 13 | 0.2 | 13 | 4.2 |
| Medical School - LCME UMC | 14 | 3.8 | 241 | 4.5 | 11 | 3.5 |
| Federally Qualified Health Center | 1 | 0.3 | 29 | 0.5 | 1 | 0.3 |
| Unknown | 1 | 0.3 | 7 | 0.1 | 1 | 0.3 |
NOTE: LCME UMC=Liaison Committee on Medical Education University Medical Center.
SOURCE: Data drawn from ACGME, 2013.
Medicaid regulations do not recognize specifically—although the Centers for Medicare & Medicaid Services (CMS) does allow—GME as an approved component of inpatient and outpatient hospital services (CMS, 2007). If a state Medicaid program opts to cover GME costs, the federal government provides matching funds.16 The only mechanisms that states have for distributing Medicaid funds for GME are through add-ons to inpatient or outpatient payments or by incorporating GME support into Medicaid managed care capitation rates (CMS, 2007; Heffron, 2012). States have considerable flexibility in how they use Medicaid funds for GME purposes, including which professions and which settings and organizations are eligible to receive support for health professions education (CMS, 2007; COGME, 2004; GAO, 1997; Herz and Tilson, 2009). In 2007, CMS issued a Proposed Rule to end federal matching funds for all Medicaid GME payments, citing inconsistency with federal statute (Herz and Tilson, 2009). However, after a number of moratoriums imposed by Congress, as well as a Sense of the Senate resolution, the rule was not implemented (Henderson, 2010).
Because the federal government does not require separate reporting for Medicaid GME expenditures and most Medicaid funding is subsumed in payment for patient services, quantifying the overall level of Medicaid GME payments is problematic. Policy makers—including CMS Medicaid officials—look to privately sponsored surveys of state Medicaid programs for estimates of spending data.17 Unless otherwise indicated, the data in this section draw from a 2012 survey sponsored by the Association of American Medical Colleges (AAMC) (Henderson, 2013). Data from previous years are available from AAMC.18
Medicaid GME Spending
In 2012, 43 state Medicaid programs19,20 distributed approximately $3.87 billion to support local graduate medical education, primarily sponsored by teaching hospitals (Henderson, 2013). The number of participating states has declined in recent years. In 2005, for example, all but three
________________
16 The Medicaid program is jointly funded by the states and the federal government. The federal government’s share of Medicaid expenditures in each state depends on the state’s per capita income. In 2012, the federal matching percentage ranged from 50 to 74 percent (Kaiser Commission on Medicaid and the Uninsured, 2012).
17 Although CMS enhanced its reporting system to help identify Medicaid GME expenditures in October 2010, the states appear to have had mixed success in using it.
18 The surveys of state Medicaid programs are available at https://www.aamc.org.
19 Includes the District of Columbia.
20 Medicaid GME estimates include the federal and state shares.
state Medicaid programs provided GME support. Since then, several states have ceased—or reported that they are considering ending—Medicaid GME funding because of budgetary constraints (Henderson, 2006, 2010, 2013). Massachusetts, for example, discontinued its Medicaid GME program in 2010 as a cost-saving measure (Spero et al., 2013). Three years earlier the state tried to leverage Medicaid funds to expand primary care and psychiatry residencies with higher GME payments, but the incentive program was not successful in stimulating expansion in training slots in these specialties.
Despite the recent decline in participating states, aggregate Medicaid GME spending increased by about $1.5 billion (63 percent) from 1998 to 2012 (Henderson, 2013). Of those states participating in Medicaid GME, the amount of funding varies widely in total and on average per hospital or per resident. New York funding—$1.82 billion in 2012—dwarfs that of any other state. In 2012, New York accounted for nearly half (46.9 percent) of the nation’s total Medicaid GME spending and more than 10 times any other individual state. New York also directs more Medicaid dollars per teaching hospital ($20.9 million) and per resident ($115,500) than other states. In contrast, Michigan, the next highest state funder, paid $163.1 million ($3.1 million per teaching hospital; $33,500 per resident).
Medicaid GME funding exceeded $100 million in only seven other states in 2012—Virginia ($142.0 million), Pennsylvania ($124.2 million), North Carolina ($115.7 million), Arizona ($113.0 million), Washington ($111.0 million), South Carolina ($110.7 million), and Missouri ($110.1 million). In three of these states (North Carolina, South Carolina, and Washington), Medicaid GME funding exceeded Medicare GME funding.21 Spending in other states ranged from $375,000 in Alaska to $90 million in New Jersey.
Some of the non-participating states have GME programs sponsored by other state agencies. For example, California’s Song-Brown Program provides financial assistance to family practice residencies as well as family nurse practitioner, physician assistant, and registered nurse education programs throughout the state (California Office of Statewide Health Planning & Development, 2014).
Eligible Trainees
Although Medicare GME subsidies are limited to physicians, dentists, and podiatrists, states may use Medicaid funds for other clinicians. In 2012, 12 states used Medicaid funds to support training of other health care professionals, including advanced practice nurses, physician assistants,
________________
21 Committee comparison of Henderson and 2011 Medicare cost report data.
emergency medical technicians, chiropractors, dentists, pharmacists, and laboratory personnel (Henderson, 2013).22
Support of State Workforce Goals
Many states report that they invest Medicaid funds in GME in order to produce more physicians overall or in specific specialties, geographic areas, or clinical settings (Henderson 2013), presumably with the expectation that the trainees will remain in the state after graduation (COGME, 2004; Henderson, 2010, 2013; Spero et al., 2013). Many states also report shortages of physicians who are willing to serve Medicaid beneficiaries. However, there is little evidence that states have been able to effectively leverage Medicaid GME funds to achieve policy objectives. In a series of recent interviews with Medicaid officials in 14 states, Spero and colleagues (2013) found that teaching hospitals were free to choose how to use Medicaid GME funds, and few states coordinate GME decisions regarding the number, location, or specialty of new residency positions.
Several states have experimented with multi- or all-payer GME financing to promote state clinical workforce goals (COGME, 2004).
HEALTH RESOURCES AND SERVICES ADMINISTRATION
HRSA is the central federal agency responsible for promoting the production and training of the health care workforce, particularly for underserved populations. All but one of the HRSA GME-related funding programs—the Children’s Hospitals Graduate Medical Education (CHGME) program—focus on expanding residency training in primary care. These include the Teaching Health Centers (THCs) for training of primary care physicians in community settings, the National Health Service Corps (NHSC), and several Title VII grants programs.
Children’s Hospitals GME
Federal support of residency training in pediatrics varies substantially according to the setting in which the training occurs. If the pediatric residency is based primarily in a general teaching hospital, or in a children’s hospital within a larger health care system, the trainees are supported according to the Medicare GME payment rules described in this chapter. Freestanding children’s hospitals do not receive much Medicare support because, as noted below, Medicare GME funding is linked directly with an
________________
22 The 12 states are Colorado, Indiana, Iowa, Kansas, Louisiana, Minnesota, Mississippi, Ohio, Pennsylvania, South Carolina, Virginia, and Wisconsin.
institution’s Medicare patient volume. Children’s hospitals play a significant role in the training of the nation’s primary and subspecialty pediatricians—an estimated 29 percent of general pediatric residents and 44 percent of pediatric medical and surgical subspecialty trainees in academic year 2009-2010 (HRSA, 2013b). In addition, children’s hospitals are considered safety net hospitals as they serve a large number of Medicaid and uninsured patients and provide charity care (HRSA, 2013a).
The CHGME Payment Program was established by Congress in 1999 to help compensate for this discrepancy (Public Law 106-129). As noted in Box 3-1, the program has been reauthorized, most recently in 2011. It is administered by HRSA’s Bureau of Health Professions (HRSA, 2011a; HRSA Bureau of Health Professions, 2010).
CHGME Payment Methodology
Unlike Medicare GME, the total CHGME funding is determined by annual discretionary appropriations. In addition, the relative proportion of DGME and IME payments is set in statute. Regardless of the amount of the annual appropriation, DGME funding must be one-third, and IME, two-thirds of the total amount (HRSA, 2013b). Available funds are allocated to individual hospitals based on the Medicare GME payment formulae (HRSA Bureau of Health Professions, 2011). There are separate DGME and IME funding streams: DGME payments cover the direct cost of GME such as stipends and benefits for residents and faculty. IME payments are intended to cover the increase in clinical expenses associated with sponsoring a training program. Also like Medicare, the DGME per-resident amount is weighted by a factor of 1.0 for trainees in their initial residency and .5 for trainees beyond their initial residency period.
CHGME funding is considerably less stable than the GME funding provided by Medicare. For example, the FY 2013 CHGME sequestration budget of $251 million is more than 20 percent less than the appropriations for FY 2010, the program’s peak funding year. Table 3-4 shows the annual appropriations for CHGME since the program’s inception in 2000 through 2013. Eligible hospitals must apply for the funds each year and the amount of available funding varies with the annual discretionary appropriation. In recent years, the President’s budget has either called for a significant reduction or complete elimination of CHGME funding (AAMC, 2013; HRSA, 2011b). In 2013, HRSA’s proposed budget called for eliminating the IME portion of the CHGME payment, a potential $177.2 million cut in funding from the previous year (HRSA, 2013a). When this report was drafted, the future of the program was uncertain (Wong et al., 2013).
TABLE 3-4 CHGME Appropriations, 2000–2013
| Fiscal Year | Appropriation ($ in millions) |
| 2000 | $40.0 |
| 2001 | 235.0 |
| 2002 | 285.0 |
| 2003 | 290.1 |
| 2004 | 303.2 |
| 2005 | 300.7 |
| 2006 | 297.0 |
| 2007 | 297.0 |
| 2008 | 301.7 |
| 2009 | 310.0 |
| 2010 | 317.5 |
| 2011 | 268.4 |
| 2012 | 265.1 |
| 2013 | 251.2 |
SOURCES: HRSA, 2013b,c.
National Health Service Corps
Although the NHSC does not provide direct funding for residency training, it is an important source of financial support for the training of physicians and other health professionals and a potentially effective lever in directing physicians toward primary care practice in health professional shortage areas. Administered by HRSA’s Bureau of Clinician Recruitment and Service, NHSC provides scholarships to medical students and loan repayment to those who have finished their training if they commit to practicing primary care for a specified duration (HRSA Bureau of Clinician Recruitment and Service, 2013). The eligible physician specialties are family practice, general internal medicine, general pediatrics, general psychiatry, geriatrics, internal medicine/family practice, internal medicine/pediatrics; obstetrics and gynecology, and psychiatry. Physician assistants, dentists, dental hygienists, nurse practitioners, certified nurse-midwives, and behavioral health professionals are also eligible to participate.
The programs include
- The NHSC Scholarship Program pays up to 4 years of medical school tuition, fees, and other educational costs to primary care providers who agree to serve 2-4 years at an approved site in an underserved area.
- The NHSC Loan Repayment Program pays off qualifying educational loans for already trained primary care physicians who make a commitment to practice in a health professions shortage area. Participating physicians can receive up to $50,000 in tax-free loan repayment in exchange for 2 years of service and up to $140,000 for 5 years of service (HRSA Bureau of Clinician Recruitment and Service, 2013).
- The NHSC State Loan Repayment Program provides matching grants to states that administer their own loan repayment programs.
- The Students to Service Loan Repayment Program pays off loans up to $120,000 for fourth-year medical students (M.D. and D.O.) in exchange for providing primary care services for at least 3 years of full-time or 6 years of half-time service in health professional shortage areas (HRSA Bureau of Clinician Recruitment and Service, 2013).
In 2013, more than half of the NHSC scholars in the pipeline were minorities (18 percent Hispanic; 18 percent African American; 13 percent Asian or Pacific Islander; and 2 percent American Indian or Alaskan Native) (HRSA Bureau of Clinicial Recruitment and Service, 2013).
The ACA permanently reauthorized the NHSC and established a $1.5 billion trust fund to provide additional funding for the NHSC for a 5-year period (NACHC, 2010). The trust fund is a one-time supplement to NHSC’s existing discretionary funding. From 2009 through 2011, the NHSC received a one-time $300 million supplement to expand loan repayments (Pathman and Konrad, 2012).
Teaching Health Centers
One of the key workforce provisions of the ACA was the creation of the Teaching Health Center GME program. The program is a 5-year initiative intended to expand the number of residents in primary care medicine and dentistry training in community-based, ambulatory care settings. Eligible GME programs include family medicine, internal medicine, internal medicine-pediatrics, obstetrics and gynecology, psychiatry, geriatrics, and general and pediatric dentistry (HRSA Bureau of Health Professions, 2012).
TABLE 3-5 Selected Data on Teaching Health Center (THC) Funding, Fiscal Years 2011–2013
| Fiscal Year | Total Funding (millions) | Number of | |||
| Funded THC Organizations* | Funded Residency Programs | Participating Residents | States with One or More Center | ||
| 2011 | $2.4 | 11 | 11 | 63 | 11 |
| 2012 | $12.5 | 19 | 22 | 141 | 15 |
| 2013 | $28.3 | 32 | 45 | 333 | 21 |
*Refers to the THC sponsoring organizations, which may oversee residencies in multiple sites.
SOURCE: HRSA, 2013d; data on number of participating residents were compiled by Candice Chen, Assistant Research Professor in the Department of Health Policy, Milken Institute of Public Health at the George Washington University, and were provided by Katie Weider, Senior Research Assistant, August 2, 2013 (personal communication).
HRSA administers the THC grant awards and distributes the residency training funds directly to the participating sponsoring organizations. Eligible entities include federally qualified health centers, community mental health centers, rural health clinics, health centers operated by the Indian Health Service, and other ambulatory centers that receive funds under Title X of the Public Health Service Act. To date, most of the awardees have been residency programs in family medicine (HRSA, 2013d).
The number of THCs and THC physician trainees has grown steadily since 2011, when the first HRSA awards were granted (see Table 3-5). In fiscal year (FY) 2013, 45 residency programs training 333 residents in 21 states were supported by THC awards (HRSA, 2013d). Appropriations were authorized only from FY 2011 through FY 2015 and are reconsidered by Congress each year during that period. The long-term prospects of the program are uncertain. As a result, existing or prospective THCs may find it difficult to recruit future trainees without some assurance of future funding, because it takes 3 or more years to complete a residency program (Spero et al., 2013).
THC Payment Methodology
Like Medicare GME, THC funding is formula based and eventually will include separate fund flows for direct and indirect expenses (HRSA Bureau of Health Professions, 2012). In contrast to Medicare, which distributes GME funds directly to teaching hospitals, HRSA distributes the THC funds to the community-based training sites.
All eligible THC applicants are funded. Initially, HRSA is paying grantees an interim payment amount of $150,000 per full-time resident per year (covering both direct and indirect costs). The method for determining the IME and DGME payments was under review by the U.S. Department of Health and Human Services when this report was drafted. Once the methods are finalized, THCs will be paid according to the new formula.
Although the ACA authorized start-up grants to help eligible health centers develop new primary care training programs, Congress has not appropriated the funds to support such activities (MedPAC, 2011).
Title VII Health Professions Programs
HRSA also administers several Title VII grants programs that provide modest support for residency programs in primary care, pediatric medical and surgical subspecialties, preventive medicine and public health, geriatrics, and rural areas (HHS, 2011; Phillips and Turner, 2012; ReyesAkinbileje, 2013).
VETERANS HEALTH ADMINISTRATION
Education and training of health professionals is a statutory and core mission of the VHA (VHA Office of Academic Affiliations, 2012; VHA, 2008). As a whole, VHA health facilities comprise the nation’s largest single provider of clinical training in the United States. More than 100,000 health professionals—including physicians, nurses, and more than 40 other types of trainees—receive a portion of their training at a VHA facility each year (VHA Office of Academic Affiliations, 2012; VHA Office of Academic Affiliations, 2009). In 2012, an estimated 37,800 residents rotated through VA facilities (10,249 FTEs).23 Nationwide, nearly one in 10 funded GME residency positions are at a VHA facility (Chang, 2012). Nearly all of the residency programs utilizing VHA training sites are sponsored by an affiliated medical school or teaching hospital rather than by the VHA.
In FY 2012, the VHA paid its academic affiliates an estimated $621 million in direct GME payments and distributed $816 million in funding to VHA medical centers for the indirect costs of training physicians and other health professionals (see Table 3-1). (Estimates of the indirect costs attributable solely to physician training are not available.)
VHA GME funding comes solely from the agency’s annual appropriations. The VHA receives no Medicare funding by law, and VHA health care providers are not permitted to bill Medicare for patient services and thus
________________
23 Personal communication, Barbara K. Chang, Director of Medical and Dental Education, VHA Office of Academic Affiliations, July 15, 2013.
cannot receive any Medicare GME funding. However, the VHA is able to bill private insurers for services provided by residents if the patient’s condition is not connected to military service.
VA Affiliation Agreements
VHA affiliation agreements with medical schools and sponsoring organizations accredited by the Accreditation Council for Graduate Medical Education (ACGME) are central to the funding and operations of residency training in VHA facilities (VHA Office of Academic Affiliations, 2009). Because the VHA no longer sponsors residency programs, it looks to its affiliates to provide physician trainees who rotate through VHA facilities. In 2011, 124 VHA hospitals and 3 VHA independent outpatient clinics had affiliation agreements with 151 allopathic and osteopathic medical schools for medical student and physician education (VHA Office of Academic Affiliations, 2012). The affiliation agreements, although fundamentally local in nature, are circumscribed by VHA directives (VHA, 2008, 2012).24
VA Payment Methods
The VHA’s funding methodology differs markedly from Medicare’s approach (Chang, 2012). Direct GME payments are based on current costs and are paid either through a disbursement agreement with the sponsoring organization or directly to residents. Accredited residency and fellowship years are fully funded. Reimbursable direct costs include resident stipends, fringe benefits, and some individually approved items such as housing, parking, and lab coats or uniforms. There are statutory prohibitions against paying for salaries and benefits for GME staff based at an affiliate; affiliates’ administrative costs; and resident licensing fees, malpractice insurance, resident board exam fees, and other items.
The VHA tracks DGME spending to ensure that the funds are not used by its health care facilities for any purpose other than graduate medical education. Unused funds must be returned to the Office of Academic Affiliations (Chang, 2012).
The VHA uses the Veterans Equitable Resource Allocation (VERA) System to allocate most of its appropriations for health care services (GAO, 2011). VERA is a centrally driven, formula-based system that determines the appropriate allocation for each of the VHA health care networks, the Veterans Integrated Service Networks or VISNs. The VISNs in turn distribute the funding to their medical centers, including a centrally determined,
________________
24 The authority for the conduct of residency training programs in the Veterans Health Administration is contained in Title 38 United States Code (U.S.C.) 7302.
fixed IME amount based on the number of residents at each medical center in the current academic year.
The committee was not able to obtain data on the costs and financing of military GME programs. The DoD sponsors about 200 GME programs that train an estimated 3,200 residents annually (Schoomaker, 2012). Each branch of the military—the Air Force, Army, and Navy—operates its own residency programs. Residents are assigned to training slots via a military-specific match system (Durning et al., 2012). The composition and size of the training pool is directly related to the extent of military deployment and the end strength that is required.
THE BLACK BOX OF GME COSTS AND BENEFITS
Remarkably little is known about the individual, institutional, and societal costs of residency training. There are also considerable conceptual challenges in defining and identifying the costs and cost savings related to residents’ presence within an institution. The most significant information gaps relate to the impact of GME on the costs of care, particularly regarding the indirect costs and cost savings (and/or revenue) associated with GME. This dearth of information exists, in part, because CMS requires only minimal reporting from teaching hospitals as a condition of receiving funding, despite the nearly $10 billion annual Medicare investment in GME. Federal GME regulations are nearly silent regarding transparency and accountability for use of Medicare GME funds. Medicare statute requires teaching hospitals to report only aggregate DGME costs, the number of FTE trainees (with limited specificity regarding specialty and whether the residents are in their initial residency period),25 the amount of time residents spend on hospital and non-hospital rotations, and the intern and resident-to-bed ratio (CMS, 2012; Wynn et al., 2006). Sponsors of teaching programs have little incentive to maintain detailed documentation of GME-related expenses because Medicare and Medicaid payment regulations do not require it.
This section reviews the available information on the financial costs and benefits of sponsoring GME programs, focusing on non-VHA institutions. It also draws insights from a series of informal case studies at several major academic medical centers associated with members of the IOM committee (see Box 3-2).
________________
25 In some cases, counts of primary care, general surgery, and obstetrics/gynecology residents are reported (CMS, 2012).
BOX 3–2
Insights from the Institute of Medicine (IOM) Case Studies
The dearth of graduate medical education (GME) cost and revenue data is a barrier to any effort to understand the financial dynamics of residency training—including this IOM study. Early in its deliberations, the committee organized a small subcommittee to investigate what it could learn by interviewing and collecting de-identified GME cost and revenue data from each of four academic medical centers. It was apparent at the outset that any results from this informal inquiry with a small sample size could not be generalized to other GME programs. Thus, the objective of this inquiry was threefold:
- To learn whether teaching institutions could readily produce comprehensive cost and revenue data for their residency programs;
- To identify the principal elements of GME costs and revenues (or cost savings); and
- To examine differences across specialties and sponsoring organizations.
The IOM staff collected cost and revenue data from three training programs at a sample of four sponsoring organizations and reviewed the data with senior staff at each institution. The specialties included a primary care residency (family medicine, general internal medicine, or pediatrics), a urology residency, and another subspecialty (gastroenterology, orthopedic oncology, orthopedic surgery, or vascular surgery).
The following summarizes the insights from this effort.
- The bottom-line impact of sponsoring individual residency programs is not well understood.
- It is common for GME program staff to have little knowledge of or control over how GME funds flow within their own institutions. Because GME funds are not regarded as sufficient to cover costs, administrators see little value in tracking the GME dollars, which will be supplemented from other sources.
- GME financing arrangements vary across not only institutions but also programs within institutions. For example, faculty practice plans may play a central role in training and supervision of residents. However, the financial relationship between the sponsoring institution and faculty can be an employee–employer arrangement or an individual contract between the hospital and a faculty practice plan.
- Considerable developmental work would be needed to define and measure the data and outcome variables that should be included in an ongoing GME reporting system.
Direct Costs of GME
The DGME cost data that CMS collects from teaching institutions, aggregated across each hospital’s sponsored programs, have limited use in a national assessment becauase they are not sufficiently complete or detailed, and are not standardized or audited (Wynn et al., 2006, 2013).
GME cost analysis is further hampered by the fact that teaching hospitals often share the costs of training with one or more affiliated educational partners. The faculty practice plans that provide the faculty and clinical supervisors for residents and fellows may be an organizational component of the teaching hospital, a medical school, or an outside independent organization. In addition, there are various arrangements for compensating attending physicians. For example, the hospital may or may not compensate attending physicians for their time spent in supervising trainees. Attendings may bill third parties for their services, and their clinical income can be influenced up or down by participation in teaching and supervision. The reported data do not reflect these idiosyncratic and often unique arrangements. Moreover, published analyses of residency training costs must be interpreted with caution because they do not take into account financial benefits such as increased patient revenues or contributions to the productivity of faculty or attending physicians (MedPAC, 2010; Nguyen and Sheingold, 2011; Wynn et al., 2013). Thus, the Medicare reported costs do not reflect true net costs.
An assessment of residency training costs appears in a recent report commissioned by MedPAC (Wynn et al., 2013). The study, described by the researchers as “exploratory” because of the data limitations, provides important insights and a useful framework for examining how residency programs affect direct GME and patient care costs. The relevant findings are discussed below.
Components of DGME Costs
The direct, explicit costs of GME are straightforward, and they include expenses related to the compensation of residents, faculty, other program staff, and supervising physicians as well as a range of program-related administrative expenses, fees, materials costs, etc. (see Box 3-3). The nature and extent of these expenses are driven, in large part, by program size, attending physician compensation, malpractice costs, and the accreditation standards set by the ACGME and the Residency Review Committees (RRCs) for each specialty, and the AOA through its Program and Trainee Review Committee and the Specialty College Evaluating Committees (SPECs) for each specialty (ACGME, 2012; AOA, 2012; Wynn et al., 2013). Accreditation standards circumscribe residents’ hours and activities and require that certain technological resources be available (e.g., simulation labs, electronic access to medical information, etc.) to support education and clinical activities. Individual training programs must also conform to minimum time commitments, minimum thresholds for specific clinical experiences, and required administrative and clinical faculty-to-resident ratios required by the RRCs. Table 3-6 illustrates the variability in
BOX 3–3
Usual Components of the Direct Costs of Sponsoring GME Programs
The extent to which the program sponsor or affiliated institution(s) pays for the costs of training (described below) varies according to individual affiliation agreements.
Labor Costs
- Salaries, stipends, and fringe benefits for trainees, faculty, graduate medical education (GME) program staff, and attending physicians:
- – Residents’ salaries increase with the postgraduate year in which the training occurs and tend to be the same across specialties within an institution.
- – Faculty and other physician compensation varies considerably by specialty.
Fees and Subsidies for Residents Vary Substantially Across Programs and Institutions
- Malpractice insurance
- Conference travel and fees
- Parking, housing, and other subsidies
- License fees
- Outside tuition (e.g., for board review, courses, other degree programs)
- Education allowances (e.g., for texts, laptops)
Program Administration
- Overhead for clinical and non-clinical space
- Resident recruitment costs
- GME accreditation fees
- Retreats
- Orientation programs
- Credentialing
- Faculty development
- Graduation
Educational Materials
Simulation equipment, software, in-training examinations, anatomy lab, etc.
the standards among a group of selected specialties, which helps to explain some of the differences in educational costs.
Residents’ compensation The stipends that residents receive tend to be the same across specialties for a given postgraduate training year within
TABLE 3-6 Residency Review Committee Faculty Staffing Requirements for Selected Specialties
| Administrative Faculty | Clinical/Core Faculty | |||
| Specialty | Minimum Hours | Minimum Ratio of Faculty to Residents | Minimum Hours | Minimum Ratio of Faculty to Residents |
| Internal medicine (IM) | Residency program director: 20 hours per week Assistant directors: 20 hours per week |
Assistant directors:
• 1 for 24–40 residents • 2 for 41–79 residents • 3 for 80–119 residents • 4 for 120–159 residents • 5 for 160 or more residents |
15 hours per week | 4 for up to 60 residents |
| 1 more faculty person for every 1-15 additional residents | ||||
| Additional specialty education coordinators are required in 11 IM subspecialties | ||||
| Cardiology | Program director: 20 hours per week (average) | Not specified | 2 clinicians who devote at least 10 hours weekly | If more than 5 fellows: 1 clinician for 1.5 residents |
| Family medicine | Program director: Must be full-time excluding non-teaching clinical services | Not specified | Full-time | 1 full-time equivalent (FTE) for every 6 residents (minimum of 2) 1 supervising physician for 4 residents in continuity clinics |
| Dermatology | Full-time program director | Not specified | Not specified | 1 for 3 residents (is desirable) 2 FTEs (including the program director) |
| General surgery | Program director: 30 percent | Not specified | Full-time | 1 for each chief resident (i.e., PGY-5) |
| Urology | Not specified | Not specified | Not specified | 1 (including program director) for 2 residents |
| Radiation oncology | 1 program director; hours not specified | Not specified | At least 4 FTE faculty who devote their professional time to teaching | Not specified |
NOTE: Full-time equals 1,400 hours per academic year; PGY = postgraduate year.
SOURCE: Wynn et al., 2013. (c) RAND Corporation. Reprinted with permission.
an institution. Across institutions there is modest variation, with somewhat more significant regional differences (AAMC, 2012a). Data regarding trainee compensation are available from the Association of American Medical Colleges (AAMC) (which conducts annual surveys of teaching hospitals regarding trainee compensation and fringe benefits) and CMS (AAMC, 2012b; CMS, 2013; Wynn et al., 2013). The stipends increase as trainees advance from one postgraduate year to the next (see Table 3-7). In academic year 2012-2013, mean stipends ranged from $47,898 for first-year residents in Southern states to $65,839 for sixth-year residents in the Northeast (AAMC, 2012a). Most residents also receive health benefits and a variety of other fringe benefits such as annual vacation, paid holidays, subsidized parking and/or housing, and sometimes meals when working. Nevertheless, compared to other health professionals who might provide many of the same services, residents may be an inexpensive source of labor for teaching institutions, particularly for some specialties (Wynn et al., 2013). Some economists argue that if residents weren’t contributing more than they cost, then they wouldn’t be paid and would instead be charged a tuition (Chandra, 2014).
Faculty compensation Although residents’ salaries tend not to vary by specialty, faculty compensation does. In academic year 2010-2011, the median compensation level for full professors at private medical schools was more than $300,000. The range, by specialty, was wide: family medicine, $198,000; geriatrics, $212,000; cardiology, $338,000; anesthesia, $376,000; radiology, $401,000; and orthopedic surgery, $505,000 (Zhang and Wisniewski, 2012). Faculty rank, geographic location, and percentage of billable clinical activity are also important determinants of faculty salaries.
Other factors Wynn and colleagues (2013) examined an array of other factors that might contribute to differences in DGME costs among hospitals. Although data limitations precluded a quantitative analysis, their research suggests that a number of variables are important, including an affiliated academic health center or community-based affiliation, rural or urban location, and the economies of scale that accrue from sponsoring large and/or multiple residency programs (see Table 3-8). For example, training in rural areas and community-based settings appears to be more expensive per resident, particularly if the program is the only residency at the site—a situation typical of family medicine, for example.
The costs of malpractice insurance also drive training costs and vary considerably by specialty (Wynn et al., 2013). Primary care specialties (not including obstetrics) have the lowest premium rates; general surgery physicians, the highest.
TABLE 3-7 Mean Resident/Fellow Stipends by Region, Academic Year 2012-2013
| All Respondentsa | Northeast | South | Midwest | West | All Regionsb |
| 1st Post-M.D. Year | $53,636 | $47,898 | $49,309 | $49,546 | $50,274 |
| 2nd Post-M.D. Year | 55,705 | 49,478 | 50,938 | 51,917 | 52,222 |
| 3rd Post-M.D. Year | 58,394 | 51,210 | 52,617 | 54,492 | 54,373 |
| 4th Post-M.D. Year | 60,704 | 53,103 | 54,585 | 57,216 | 56,536 |
| 5th Post-M.D. Year | 63,305 | 55,041 | 56,712 | 59,834 | 58,767 |
| 6th Post-M.D. Year | 65,839 | 57,089 | 58,751 | 62,099 | 61,035 |
a Includes four for-profit hospitals.
b Includes one medical school in Puerto Rico.
SOURCE: AAMC, 2012a.
Indirect Costs of GME
The extent to which residents have an indirect financial impact on teaching hospitals—and the net direction of this impact—is an unresolved question. Unlike DGME, there are no requirements for teaching hospitals to document IME “costs” and, by definition, indirect costs are challenging to identify and measure. Nevertheless, IME accounts for most of the federal GME outlay (i.e., an estimated $6.8 billion in 2010).
Several factors may contribute to indirect costs of GME, including residents’ likelihood to do the following:
- Order more diagnostic tests and procedures than experienced clinicians and take more time to interpret the results;
- Require frequent reorientation to new settings and practices because they rotate among different services and experiences, which would logically impede efficiency; and
- Provide some services that have to be repeated by faculty or supervising physicians (e.g., portions of history taking and physical exams), and provide many services less efficiently than would more experienced clinicians.
Stakeholders also assert that teaching hospitals have broad missions, and that their roles in education, research, and providing care (including as safety net providers) are inextricably intertwined (AAMC, 2011). From this perspective, some argue that the calculation of the indirect costs of teaching should consider not only the inefficiencies related to the presence
TABLE 3-8 Direct GME Costs by Hospital Characteristics, 2008
| Hospital Characteristic | Number of Hospitals | Number of Residents | Total GME Costs Per Resident | Total GME Costs: Facility Percentiles | ||
| 25th | 50th | 75th | ||||
| All hospitals | 1,141 | 97,577 | $141,240 | $95,403 | $134,803 | $177,674 |
| Geographic location | ||||||
| Large urban | 690 | 71,787 | $142,391 | $95,382 | $133,369 | $171,239 |
| Other urban | 391 | 24,603 | $137,583 | $95,403 | $137,971 | $190,157 |
| Rural | 60 | 1,186 | $147,485 | $100,604 | $125,786 | $189,824 |
| Number of FTE residents | ||||||
| Less than 10 | 319 | 1,314 | $145,697 | $75,075 | $117,199 | $197,090 |
| 10 to 24 | 231 | 3,963 | $153,938 | $103,270 | $142,627 | $189,405 |
| 25 to 99 | 313 | 15,888 | $142,077 | $106,914 | $137,971 | $170,703 |
| 100 or more | 278 | 76,412 | $140,331 | $104,128 | $136,578 | $171,054 |
| Percentage of residents in primary care training | ||||||
| Less than 25% | 165 | 3,525 | $161,779 | $77,511 | $116,626 | $180,391 |
| 25 to 49 | 239 | 59,802 | $132,956 | $92,982 | $124,292 | $154,419 |
| 50 to 74 | 242 | 22,720 | $154,753 | $107,448 | $139,548 | $171,487 |
| 75 or more | 426 | 11,082 | $153,162 | $107,772 | $150,490 | $199,507 |
| GME affiliations | ||||||
| Academic health center | 828 | 88,342 | $141,269 | $98,976 | $137,323 | $180,336 |
| Community based | 292 | 8,779 | $140,073 | $88,935 | $126,457 | $169,777 |
NOTE: FTE = full-time equivalent.
SOURCE: Wynn et al., 2013. (c) RAND Corporation. Reprinted with permission.
of residents, but also the costs of providing an array of expensive, high-tech, and complex services not available elsewhere (e.g., specialized burn and transplant units) (Koenig et al., 2003). However, others question whether such costs should be subsidized by federal GME programs. From their perspective, the costs are not part of the education process and paying for them, in this way, may encourage inefficiencies. It also creates inequities because teaching hospitals vary in their level of engagement in these activities (Anderson et al., 2001; Koenig et al., 2003; Wynn et al., 2006) and some non-teaching hospitals provide comparable services.
Teaching hospital advocates also assert that they are also more financially vulnerable because they care for large numbers of low-income and sicker, high-cost patients. However, since the prospective payment system was implemented in 1983, refinements have been made to the payment system to address these concerns. Annual refinements to the patient classification system have improved how the system accounts for differences in patient severity and complexity. In particular, Medicare severity-adjusted DRGs, implemented in 2008, had the effect of increasing the average DRG relative weight for teaching hospitals relative to non-teaching hospitals (Wynn, 2008). Second, Medicare has made an additional payment to teaching and other hospitals if they serve a disproportionate share of low-income patients (referred to as the Disproportionate Share Hospital, or DSH, payment). Stakeholders assert that the adjustment is insufficient. Because it has been an adjustment to the DRG rate, the subsidies have been lower for hospitals with fewer Medicare inpatients. Further, the payment formula has not explicitly targeted charity care and other uncompensated care costs. However, the ACA made significant changes to the DSH program in anticipation of the expansion of health insurance. Starting in FY 2014, CMS began to reduce the link with Medicare payment volume by replacing 75 percent of DSH payments with allocations from an uncompensated care pool based on a hospital’s share of total uncompensated care costs (America’s Essential Hospitals, 2013). The effect of this change will be to increase the subsidies to safety net hospitals with high charity care caseloads relative to other hospitals. As uninsurance rates decline nationwide, the separate DSH payments will be reduced.
Indirect Benefits of GME for Teaching Hospitals
The financial benefits of GME are not tracked or reported, and they are rarely acknowledged when the costs of GME are examined. Institutions may experience lower personnel costs because residents, compared with other clinicians, perform a wide range of services at a low rate of pay and have relatively flexible job descriptions and schedules. For example, in some specialties, fellows can provide on-call services in lieu of fully
trained attending physicians—at significantly lower costs to the hospital. The presence of residency programs may be a signal of higher quality to private insurers and may also result in higher commercial rates. Also, in some circumstances, residents or fellows are likely to enhance the efficiency and productivity of the attending physicians with whom they work. These factors may contribute to significant cost savings for teaching institutions, but the magnitude of such savings is difficult to estimate—much less calculate. They may also lead to additional GME-related revenues. GME-related revenues include the explicit payments that hospitals and their educational partners receive for graduate medical education training, such as from Medicare and Medicaid and HRSA. It also includes patient care revenues that are indirectly related to resident services. For example, more senior residents sometimes generate incremental clinical revenues for hospitals or faculty practices. As residents assume more clinical responsibilities in their later training years, they may increase the number of patient services for which attending physicians can bill.
Net Financial Impact of GME
The committee finds a dearth of available evidence regarding indirect costs and indirect benefits of GME, and thus the net financial impact of GME on teaching institutions is unclear. The restrictiveness of the GME cap offers important insight into the underlying finances of GME. Despite this cap, there has been considerable expansion in training slots. As noted earlier, teaching hospitals added nearly 17,000 new positions to accredited residency and fellowship programs26 between 1997 and 2012, without any further subsidization by IME or DGME funding (Brotherton and Etzel, 2013; Salsberg et al., 2008). If it is assumed that hospitals would not add the direct and indirect expenses of trainees unless those expenses are offset by gains (which is debatable), such additions above the cap suggest that residents add value in excess of those costs—even with no subsidization (Chandra et al., 2014).
Several studies do suggest that teaching hospitals have higher spending per DRG than community hospitals. However, it is likely that the financial burden associated with GME is significantly less than the current IME adjustment amount, and some analysts question whether Medicare should continue to pay the full amount. MedPAC, for example, has estimated that the IME adjustment is twice its empirically justified level (MedPAC, 2009). Nguyen and Sheingold (2011) came to a similar conclusion. Moreover, these aggregate estimates of indirect expenditures obfuscate substantial differences across individual programs.
________________
26 Includes only residents in ACGME-accredited residencies.
Research by Wynn and colleagues (2013) suggests that the net financial impact of GME varies considerably, depending on the characteristics of the residency program. Using a variety of information sources, including data from Medicare cost reports, survey data from the AAMC and the Medical Group Management Association, and hospital and cost data from the California Office of Statewide Health Planning and Development, the researchers assessed the relative financial impact of various program characteristics. Table 3-9 provides some of their findings; see the full report for details on their methods and findings (Wynn et al., 2013). The analysis demonstrates substantial differences across specialties. For example, the financial impact (presumably benefit) of the on-call services provided by residents depends on how often the specialty needs on-call services and the alternative cost of compensating a fully trained physician to provide the service. This suggests that the financial benefit of having residents on call in dermatology and radiation oncology is minimal because on-call services are rarely needed. In contrast, surgical residents provide considerable savings to institutions because their services are required frequently and the cost of compensating a fully trained surgeon is significant.
Of the specialties studied by Wynn and colleagues (2013), residents appear to be particularly costly in outpatient settings for family medicine, dermatology, and radiation oncology compared to cardiology, general surgery, and urology.
It is not surprising that the Medicare GME payment system, fixed in statute, has concerned researchers, policy makers, and stakeholders for decades (ACP, 2011; COGME, 2004, 2007; Dower, 2012; Iglehart, 2011; IOM, 1989; Johns, 2010; Ludmerer and Johns, 2005; Macy Study Group on Graduate Medical Education, 1980; MedPAC, 2010; Morris, 1993; Rich et al., 2002; Weinstein, 2011). Their concerns—and the committee’s—stem largely from the rigidity of the formulas, the lack of accountability for how the funds are used, the inequities in the distribution of the funds, and the embedded disincentives to train physicians outside of the hospital setting.27
This discussion focuses on the committee’s conclusions regarding Medicare GME financing because Medicare has the greatest potential leverage for improving GME outcomes.
Table 3-10 describes the unintended consequences of the basic features of Medicare GME financing. Under the status quo, Medicare distributes
________________
27 See Chapter 2 for a review of the current makeup and characteristics of the residency pipeline and physician workforce. Chapter 4 describes current governance, including mechanisms to ensure accountability for GME funding.
| Relative Financial Impact by Specialty | |||||||
| Program Characteristic | Internal Medicine | Cardiology | Family Medicine | Dermatology | General Surgery | Urology | Radiation Oncology |
| Residents provide on-call services that benefit both the hospital and attending physicians | |||||||
| Residents teach more junior residents and medical students | |||||||
| Some specialty programs have a larger cost impact on inpatient costs than others after controlling | NA | NA | |||||
| Resident training increases the cost of ambulatory care | |||||||
NOTE: Program characteristics that are likely to increase costs per resident are shown with up arrows; those that are likely to reduce costs are shown with down arrows. The relative magnitude of the direction is reflected in the shading. If the impact across programs is in the same direction, the arrows, the specialty program is shown with black specialty program is shown with white arrows, and those that fall in between are shown with grey arrows. If the impact is a cost for one or more programs and a benefit for the remaining programs, the shading of the arrow depicts the magnitude of the direction so that the black arrows denote a greater impact than the unshaded arrows. NA = not applicable.
SOURCE: Wynn et al., 2013. (c) RAND Corporation. Reprinted with permission.
TABLE 3-10 Unintended Consequences of Current Medicare GME Payment Methods
| Features of Current Medicare GME Payment Methods | Unintended Consequences |
| Separate funding streams that flow directly to teaching hospitals |
|
| Payments directly linked with Medicare patient volume |
|
| IME adjustment to DRG rates |
|
| DGME PRA across all specialties |
|
| Cap on Medicare-funded slots based on training programs and local health care delivery organization in 1996 |
|
NOTE: DGME = direct graduate medical education; DRG = diagnosis-related group; IME = indirect medical education; PRA = per-resident amount.
GME monies directly to teaching hospitals in two independent funding streams (DGME and IME). Both funding streams are linked with hospitals’ volume of Medicare inpatients. The hospitals have fiduciary control over the use of the funds. By giving the funds directly to teaching hospitals, the payment system discourages physician training in the clinical settings outside the hospital where most people seek care. Primary care residency programs are at a distinct disadvantage because of their emphasis on training in ambulatory care settings. Hospitals’ control over the allocation of GME funds may also encourage the overproduction of specialists in disciplines that generate financial benefits for an individual institution rather than for the health care system overall.
The direct linkage of payments with Medicare patient volume also systematically disadvantages children’s hospitals, safety net hospitals, and other training sites that care for non-elderly patients. Non-clinical, population-based specialties, such as public health and preventive medicine, are similarly affected. The HRSA CHGME program directs some funding to children’s hospitals, but the funding is unpredictable because it is subject to the annual appropriations process. This undermines the capacity of the affected training programs to plan beyond the fiscal year. Teaching Health Centers also have time-limited federal support despite their potential for expanding the nation’s capacity to train physicians in ambulatory care. Funding for THCs is scheduled to expire at the end of FY 2015.
The cap on Medicare-supported training slots is also problematic—not because it limits Medicare GME funding in the aggregate but because the slots that receive financial support are frozen where they existed almost two decades ago. This perpetuates inequities in the geographic distribution of training slots and ignores changes in the geography and demography of the U.S. population.
Finally, as many observers have noted, the absence of accountability in Medicare GME funding is a serious concern. By guaranteeing an automatic add-on to Medicare inpatient rates through the IME adjustment, the system lacks any incentive for quality or efficiency. Complete and comparable data on the use or outcomes of GME funds are not available. The DGME cost data that CMS collects have limited use because they are not complete, sufficiently detailed, standardized, or audited. Importantly, the financial benefits of GME for hospitals are rarely acknowledged when the costs of GME are examined, and the direction and magnitude of net financial impact are not known.
AAMC (Association of American Medical Colleges). 2011. Proposed reductions in Medicare IME payments to AAMC teaching hospitals: National and state economic impacts. https://www.aamc.org/download/253360/data/trippumbach.pdf (accessed February 25, 2014).
AAMC. 2012a. AAMC survey of resident/fellow stipends and benefits. https://www.aamc.org/download/312786/data/2012stipendsurveyreportfinal.pdf (accessed June 27, 2013).
AAMC. 2012b. A snapshot of the new and developing medical schools in the U.S. and Canada. https://members.aamc.org/eweb/upload/A%20Snapshot%20of%20the%20New%20and%20Developing%20Medical%20Schools%20in%20the%20US%20and%20Canada.pdf (accessed June 27, 2013).
AAMC. 2013. Children’s Hospital Graduate Medical Education Payment Program (CHGME). https://www.aamc.org/advocacy/gme/275136/chgme.html (accessed July 12, 2013).
ACGME (Accreditation Council for Graduate Medical Education). 2012. Program director guide to the common program requirements. http://www.acgme.org/acgmeweb/Portals/0/PDFs/commonguide/CompleteGuide_v2%20.pdf (accessed August 22, 2013).
ACGME. 2013. Glossary of terms. http://acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/ab_ACGMEglossary.pdf (accessed March 4, 2014).
ACP (American College of Physicians). 2011. Aligning GME policy with the nation’s health care workforce needs: A position paper. Philadelphia, PA: ACP.
America’s Essential Hospitals. 2013. NAPH Summary of Proposed Medicare DSH Regulations. http://essentialhospitals.org/wp-content/uploads/2013/11/Medicare-DSHSummary-5-9-13.pdf (accessed March 4, 2014).
Anderson, G. F., G. Greenberg, and B. Wynn. 2001. Graduate medical education: The policy debate. Annual Review of Public Health 22:35-47.
AOA (American Osteopathic Association). 2012. The basic documents for postdoctoral training. http://www.osteopathic.org/inside-aoa/accreditation/postdoctoral-training-approval/postdoctoral-training-standards/Documents/aoa-basic-document-for-postdoctoraltraining.pdf (accessed June 5, 2013).
Baumann, M. R., T. F. Vadeboncoeur, and R. W. Schafermeyer. 2004. Financing of emergency medicine graduate medical education programs in an era of declining Medicare reimbursement and support. Academic Emergency Medicine 11(7):756-759.
Brotherton, S. E., and S. I. Etzel. 2013. Graduate medical education, 2012-2013. JAMA 310(21):2328-2346.
California Office of Statewide Health Planning & Development. 2014. Song-Brown Program. http://www.oshpd.ca.gov/HWDD/Song_Brown_Prog.html (accessed February 27, 2014).
Chandra, A., D. Khullar, and G. R. Wilensky. 2014. The economics of graduate medical education. New England Journal of Medicine 370:2357-2360.
Chang, B. K. 2012. VA funding of graduate medical education. Paper presented at Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI) GME Summit, Seattle, WA, March 23. http://uwmedicine.org/Education/WWAMI/Documents/Chang-VA-GME-%20Funding.pdf (accessed June 22, 2013).
Chen, C. P., I. Xierali, K. Piwnica-Worms, and R. Phillips. 2013. The redistribution of graduate medical education positions in 2005 failed to boost primary care or rural training. Health Affairs 32(1):102-10.
CMS (Centers for Medicare & Medicaid Services). 2004. CMS Manual System. Instructions Related to “Redistribution of Unused Resident Positions,” Section 422 of the Medicare Modernization Act of 2003 (MMA), P.L. 108-173, for Purposes of Graduate Medical Education (GME) Payments. http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R87otn.pdf (accessed May 18, 2014).
CMS. 2007. Proposed Rule. Medicaid program: Graduate medical education. http://www.gpo.gov/fdsys/pkg/FR-2007-05-23/html/07-2576.htm (accessed June 27, 2013).
CMS. 2012. 42 CFR 413.75—Direct GME Payments: General Requirements. http://www.gpo.gov/fdsys/pkg/CFR-2011-title42-vol2/xml/CFR-2011-title42-vol2-sec413-75.xml (accessed June 22, 2013).
CMS. 2013. Direct graduate medical education (DGME). http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/dgme.html# (accessed June 22, 2013).
COGME (Council on Graduate School Medical Education). 2004. Resource paper: State and managed care support for graduate medical education: Innovations and implications for federal policy. http://www.hrsa.gov/advisorycommittees/bhpradvisory/cogme/Publications/managedcarerpt.pdf (accessed June 27, 2013).
COGME. 2007. Nineteenth report: Enhancing flexibility in graduate medical education. Rockville, MD: HRSA.
COGME. 2013. Twenty-first report: Improving value in graduate medical education. http://www.hrsa.gov/advisorycommittees/bhpradvisory/cogme/Reports/twentyfirstreport.pdf (accessed February 25, 2014).
Congressional Research Service. 2010. Public health, workforce, quality, and related provisions in the Patient Protection and Affordable Care Act (P.L. 111-148). Washington, DC: Government Printing Office.
Dower, C. 2012. Health policy brief: Graduate medical education. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=73 (accessed September 1, 2012).
Durning, S. J., A. R. Artino, T. Dong, D. F. Cruess, W. R. Gilliland, K. J. DeZee, A. Saguil, D. M. Waechter, and J. E. McManigle. 2012. The Long-Term Career Outcome Study (LTCOS): What have we learned from 40 years of military medical education and where should we go? Military Medicine 177(9S):81-86.
Fryer, G. E. J., L. A. Green, S. Dovey, and R. L. J. Phillips. 2001. Direct graduate medical education payments to teaching hospitals by Medicare: Unexplained variation and public policy contradictions. Academic Medicine 76(5):439-445.
GAO (Government Accountability Office). 1997. Medicaid graduate medical education. GAO Report B-276272. http://www.gao.gov/assets/90/86259.pdf (accessed July 16, 2013).
GAO. 2011. VA health care: Need for more transparency in new resource allocation process and for written policies on monitoring resources. http://www.gao.gov/new.items/d11426.pdf (accessed August 7, 2013).
Goodman, D. C., and R. G. Robertson. 2013. Accelerating physician workforce transformation through competitive graduate medical education funding. Health Affairs 32(11): 1887-1892.
Green, L. V., S. Savin, and Y. Lu. 2013. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Affairs 32(1):11-19.
Grover, A., and L. M. Niecko-Najjum. 2013. Building a health care workforce for the future: More physicians, professional reforms, and technological advances. Health Affairs 32(11):1922-1927.
Heffron, D. E. 2012. GME payments in Medicaid. Paper presented at workshop of the IOM Committee on the Governance and Financing of Graduate Medical Education, Washington, DC, September 4.
Henderson, T. M. 2006. Medicaid direct and indirect graduate medical education payments: A 50-state survey. Washington, DC: AAMC.
Henderson, T. M. 2010. Medicaid direct and indirect graduate medical education payments: A 50-state survey. Washington, DC: AAMC.
Henderson, T. M. 2013. Medicaid graduate medical education payments: A 50-state survey. https://members.aamc.org/eweb/upload/Medicaid%20Graduate%20Medical%20Education%20Payments%20A%2050-State%20Survey.pdf (accessed June 22, 2013).
Herz, E., and S. Tilson. 2009. CRS report: Medicaid and graduate medical education. http://aging.senate.gov/crs/medicaid8.pdf (accessed September 29, 2012).
HHS (U.S. Department of Health and Human Services). 2011. Annual report on the preventive medicine and public health training grant program, fiscal year 2010. http://bhpr.hrsa.gov/grants/publichealth/pmr2010report.pdf (accessed February 26, 2014).
HRSA (Health Resources and Services Administration). 2011a. Children’s Hospitals Graduate Medical Education Payment Program. Funding Opportunity Announcement. Bureau of Health Professionals. HRSA-12-007. Rockville, MD: HRSA.
HRSA. 2011b. Children’s Hospitals Graduate Medical Education Payment Program. Funding Cycle View. HRSA-12-007. https://grants3.hrsa.gov/2010/Web2External/Interface/FundingCycle/ExternalView.aspx?&fCycleID=30B17241-92E6-45A5-B313-FBC02D7D65DD&txtAction=View+Details&submitAction=Go&ViewMode=EU (accessed August 13, 2013).
HRSA. 2013a. Justification of Estimates for Appropriations Committees. http://www.hrsa.gov/about/budget/budgetjustification2013.pdf (accessed August 6, 2013).
HRSA. 2013b. Report to Congress: Children’s Hospitals Graduate Medical Education (CHGME) Payment Program. http://bhpr.hrsa.gov/childrenshospitalgme/pdf/reporttocongress2013.pdf (accessed June 21, 2013).
HRSA. 2013c. Sequestration Operating Plan for FY 2013. http://www.hrsa.gov/about/budget/operatingplan2013.pdf (accessed June 21, 2013).
HRSA. 2013d. Teaching Health Center GME Payments. http://bhpr.hrsa.gov/grants/teachinghealthcenters/payments.html (accessed August 1, 2013).
HRSA Bureau of Clinician Recruitment and Service. 2013. National Health Service Corps. http://www.hrsa.gov/about/organization/bureaus/bcrs/nhscoverview.html (accessed February 24, 2014).
HRSA Bureau of Health Professions. 2010. Children’s Hospitals Graduate Medical Education Payment Program. Documentation Guidance. Rockville, MD: HRSA.
HRSA Bureau of Health Professions. 2011. The A, B, C’s of the CHGME Payment Program from policy to payments. http://bhpr.hrsa.gov/childrenshospitalgme/ppt/policytopayments.pptx (accessed August 3, 2013).
HRSA Bureau of Health Professions. 2012. Teaching Health Center Graduate Medical Education (THCGME). Funding opportunity announcement fiscal year 2013. Rockville, MD: HRSA.
Iglehart, J. K. 1999. Support for academic medical centers: Revisiting the 1997 Balanced Budget Act. New England Journal of Medicine 341(4):299-304.
Iglehart, J. K. 2011. The uncertain future of Medicare and graduate medical education. New England Journal of Medicine 365(14):1340-1345.
Iglehart, J. K. 2013. Expanding the role of advanced nurse practitioners—risks and rewards. New England Journal of Medicine 368(20):1935-1941.
IOM (Institute of Medicine). 1989. Primary care physicians: Financing their graduate medical education in ambulatory settings. Washington, DC: National Academy Press.
Johns, M. M. E. 2010. Ensuring an effective physician workforce for America. Proceedings of a conference sponsored by the Josiah Macy Jr. Foundation, Atlanta, GA, October 24-25.
Kaiser Commission on Medicaid and the Uninsured. 2012. Medicaid financing: An overview of the Federal Medicaid Matching Rate (FMAP). http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8352.pdf (accessed March 4, 2014).
Kirch, D. G., M. K. Henderson, and M. J. Dill. 2012. Physician workforce projections in an era of health care reform. Annual Review of Medicine 63:435-445.
Koenig, L., A. Dobson, S. Ho, J. M. Siegel, D. Blumenthal, and J. S. Weissman. 2003. Estimating the mission-related costs of teaching hospitals. Health Affairs 22(6):112-122.
Ludmerer, K. M., and M. M. E. Johns. 2005. Reforming graduate medical education. JAMA 294(9):1083-1087.
Macy Study Group on Graduate Medical Education. 1980. Graduate medical education present and prospective: A call for action. New York: Josiah Macy Jr. Foundation.
MedPAC (Medicare Payment Advisory Commission). 2001. Chapter 10—Treatment of the initial residency period in Medicare’s direct graduate medical education payments. Washington, DC: MedPAC.
MedPAC. 2003. Impact of the resident caps on the supply of geriatricians. Washington, DC: MedPAC.
MedPAC. 2009. Report to Congress: Improving incentives in the Medicare program. Washington, DC: MedPAC.
MedPAC. 2010. Graduate medical education financing: Focusing on educational priorities. In Report to the Congress: Aligning Incentives in Medicare. Washington, DC: MedPAC. Pp. 103-126.
MedPAC. 2011. Federally Qualified Health Centers. In Report to the Congress: Medicare and the Health Care Delivery System. Pp. 145-160. http://www.medpac.gov/documents/jun11_entirereport.pdf (accessed August 2, 2013).
Morris, T. Q., and C. M. Sirica. 1993. Taking charge of medical education: To meet the nation’s needs in the 21st century. New York: Josiah Macy Jr. Foundation.
Mullan, F., C. Chen, and E. Steinmetz. 2013. The geography of graduate medical education: Imbalances signal need for new distribution policies. Health Affairs 32(11):1914-1921.
NACHC (National Association of Community Health Centers). 2010. Health centers and health care reform: National health service corps. http://www.nachc.com/client/Health%20Reform%20Fact%20Sheet%20-%20NHSC%20Final2.pdf (accessed August 6, 2013).
National Health Policy Forum. 2001. Federal and state perspectives on GME reform. http://www.nhpf.org/library/issue-briefs/IB764_GMEReform_6-22-01.pdf (accessed August 6, 2012).
Nguyen, N. X., and S. H. Sheingold. 2011. Indirect medical education and disproportionate share adjustments to Medicare inpatient payment rates. Medicare & Medicaid Research Review 1(4):E1-E19.
Pathman, D. E., and T. R. Konrad. 2012. Growth and changes in the National Health Service Corps (NHSC) workforce with the American Recovery and Reinvestment Act. Journal of the American Board of Family Medicine 25(5):723-733.
Pathman, D. E., J. C. Morgan, T. R. Konrad, and L. Goldberg. 2012. States’ experiences with loan repayment programs for health care professionals in a time of state budget cuts and NHSC expansion. Journal of Rural Health 28(4):408-415.
Phillips, R. L., Jr., and B. J. Turner. 2012. The next phase of Title VII funding for training primary care physicians for America’s health care needs. Annals of Family Medicine 10(2):163-168.
Reyes-Akinbileje, B. 2013. CRS report. Health workforce programs in Title VII of the Public Health Service Act. http://www.cq.com/pdf/crsreports-4336312 (accessed September 3, 2013).
Rich, E. C., M. Liebow, M. Srinivasan, D. Parish, J. O. Wolliscroft, O. Fein, and R. Blaser. 2002. Medicare financing of graduate medical education. Journal of General Internal Medicine 17(4):283-292.
Roth, A. B., and N. S. Yolin. 2011. Graduate medical education reimbursement under the Patient Protection and Affordable Care Act. Bureau of National Affairs Medicare Report. Arlington, VA: BNA, Inc.
Salsberg, E., P. H. Rockey, K. L. Rivers, S. E. Brotherton, and G. R. Jackson. 2008. U.S. residency training before and after the 1997 Balanced Budget Act. JAMA 300(10): 1174-1180.
Schoomaker, E. 2012. Testimony presented at meeting of the IOM Committee on the Governance and Financing of Graduate Medical Education. Washington, DC. September 4.
Sisson, S. D., and D. Dalal. 2011. Internal medicine residency training on topics in ambulatory care: A status report. American Journal of Medicine 124(1):86-90.
Spero, J. C., E. P. Fraher, T. C. Ricketts, and P. H. Rockey. 2013. GME in the United States: A review of state initiatives. Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill.
VHA (Veterans Health Administration). 2008. VHA handbook 1400.05. Disbursement agreements procedures (corrected copy). http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=1769 (accessed January 8, 2013).
VHA. 2012. VHA handbook 1400.01. Resident supervision. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2847 (accessed January 7, 2013).
VHA Office of Academic Affiliations. 2009. The Report of the Blue Ribbon Panel on VA-medical school affiliations. http://www.va.gov/oaa/archive/BRP-final-report.pdf (accessed August 7, 2013).
VHA Office of Academic Affiliations. 2012. Mission of the Office of Academic Affiliations. http://va.gov/oaa/oaa_mission.asp (accessed August 7, 2013).
Weinstein, D. 2011. Ensuring an effective physician workforce for the United States; Recommendations for graduate medical education to meet the needs of the public. Paper read at The Second of Two Conferences—The Content and Format of Graduate Medical Education, Atlanta, GA, May 16-19.
Wong, C. A., J. C. Davis, D. A. Asch, and R. P. Shugerman. 2013. Political tug-of-war and pediatric residency funding. New England Journal of Medicine 369(25):2372-2374.
Wynn, B. O. 2008. Comparative Performance of the MS-DRGS and RDRGS in Explaining Variation in Cost for Medicare Hospital Discharges. Working paper prepared for Health Systems Consultants, Inc. Arlington, VA: RAND.
Wynn, B. O. 2012 (unpublished). GME financing models. Presentation to the IOM Committee on the Governance and Financing of Graduate Medical Education. Washington, DC. September 5, 2012.
Wynn, B. O. and J. H. Kawata. 2002. Analysis of Children’s Hospital Graduate Medical Education Program fund allocations for indirect medical education costs. Santa Monica, CA: RAND.
Wynn, B. O., C. Guarino, L. Morse, and M. Cho. 2006. Alternative ways of financing graduate medical education. http://aspe.dhhs.gov/health/reports/06/AltGradMedicalEdu/report.pdf (accessed August 6, 2013).
Wynn, B. O., R. Smalley, and K. Cordasco. 2013. Does it cost more to train residents or to replace them? A look at the costs and benefits of operating graduate medical education programs. Santa Monica, CA: RAND. http://www.rand.org/pubs/research_reports/RR324 (accessed October 14).
Zhang, F., and S. Wisniewski. 2012. Report on medical school faculty salaries. Washington, DC: AAMC.














































