Key Findings
- Young adults are at elevated risk of morbidity and mortality in a surprising variety of ways compared with adolescents and older adults.
- Policies and programs aimed at reducing the incidence and prevalence of disease and injury among young adults can be improved by taking a developmental perspective.
- The differential effects of public health interventions on subpopulations of young adults have not been adequately explored. Efforts to address health inequities will have to account for the transitional experiences of young adults, given that the effects of interventions during this period of life are likely to last for several decades.
- Mobile digital media and social networking have the potential to play a pivotal role as vehicles for public health interventions, and research on the effectiveness of these technologies is a high priority.
- The most successful public health interventions for young adults have been those that involve comprehensive, multilevel strategies using ecological approaches in multiple channels and venues to influence changes at the individual, organizational, and societal levels that can be sustained over time.
- The heightened vulnerability of young adults to a variety of health and safety risks supports an extension of some protective health policies beyond the legal definition of adulthood.
- An effective approach to public health policy and practice focused on young adults requires better integration and coordination of federal and state public health programs and effective use of the preventive services component of the Patient Protection and Affordable Care Act.
When their health, safety, and well-being are viewed from a developmental life-course perspective, young adults are at elevated risk of morbidity and mortality in a surprising variety of ways compared with adolescents and older adults. What makes this surprising is that conventional wisdom suggests young adults ought to be in peak physical condition, given that they are beyond the pitfalls of adolescence and not yet experiencing the declines of aging. The vulnerability is even greater among those of lower socioeconomic position and from racial and ethnic minorities, who are exposed to greater risks and dangers than their more advantaged peers and lack safety nets to protect them (NIHCM, 2007). Policy makers and practitioners have recognized that the health, safety, and well-being of adolescents can be enhanced—during adolescence and thereafter—by basing policy and practice on an integrated understanding of this distinct period of development. A key conclusion of this report is that the health, safety, and well-being of young adults can similarly benefit from bringing a life-course perspective to bear on public health policies and programs and on the delivery of health care.
As chronic health conditions become the key health challenge for the 21st century, community-based prevention efforts will increasingly become an important focus for both the public health and health care delivery systems. It is important to recognize the mutually reinforcing connection between effective population-level and individual-level interventions. At the same time needs for treatment are reduced through prevention, public health activities can help increase the effectiveness of health interventions. In fact, Milstein and colleagues (2011) estimate that if protective public health interventions were integrated with coverage and care approaches, in 10 years they could save 90 percent more lives in the United States and in 25 years 140 percent more lives than could be saved through coverage and care approaches without such interventions (Milstein et al., 2011).
This chapter addresses policies and programs undertaken by the public health system (public agencies and their partners at the national, state, and community levels) aimed at reducing the incidence and prevalence of disease and injury among young adults. The next chapter addresses the
delivery of health care services for young adults, including both preventive services and treatment delivered by primary care physicians and other health care providers. The chapter begins with a brief overview of public health perspectives and activities. After highlighting the public health issues associated with young adulthood, we then review the literature on the effectiveness of public health initiatives, particularly those targeting health and safety problems with elevated prevalence among young adults, and summarize features of public health interventions that have been successful in reducing the risk of morbidity and mortality among young adults. Next we give special attention to the potentially pivotal role of mobile digital media and social networking as vehicles for public health interventions. We then turn to the role of public health policies, such as those related to the purchase of alcohol and tobacco, in protecting the health, safety, and well-being of young adults. In the next section, we look at the extent to which state and federal public health programs focus on those issues most salient to young adults, and on how these programs can be improved and better coordinated to best address these issues. The final section presents conclusions and recommendations.
OVERVIEW OF PUBLIC HEALTH PERSPECTIVES AND ACTIVITIES
The mission of public health has been defined as “organized community efforts aimed at the prevention of disease and promotion of health. It links many disciplines and rests upon the scientific core of epidemiology” (IOM, 1988, p. 41). Figure 6-1 shows how the different sectors involved, while acting individually, also work together as a public health system in pursuing health goals. Moreover, contemporary public health activities are grounded in an ecological approach that takes account of cross-level influences on individual health behaviors and conditions, including the natural, social, and built environments and the contributions of other government agencies or sectors—such as transportation, environment, economic development, and education—that influence population health (IOM, 2011, 2012b; Sallis et al., 2008). Similarly, public health interventions encompass a wide array of policies and programs, ranging from tax policies to media campaigns.
Although broad action on multiple determinants involving diverse public and private actors is needed to achieve the greatest effects on population health, the governmental public health infrastructure serves an essential coordinating role and, in many contexts, service delivery and regulatory roles (IOM, 2011). In the context of ensuring the health, safety, and well-being of young adults, we focus here on the 10 essential activities of state and local public health agencies listed in Box 6-1, which have become widely accepted in the field (IOM, 2011).
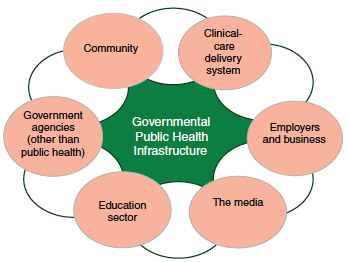
FIGURE 6-1 The intersectoral public health system.
SOURCE: IOM, 2011.
BOX 6-1
10 Essential Public Health Services
- Monitor health status to identify and solve community health problems.
- Diagnose and investigate health problems and health hazards in the community.
- Inform, educate, and empower people about health issues.
- Mobilize community partnerships and action to identify and solve health problems.
- Develop policies and plans that support individual and community health efforts.
- Enforce laws and regulations that protect health and ensure safety.
- Link people to needed personal health services and ensure the provision of health care when otherwise unavailable.
- Ensure a competent public and personal health care workforce.
- Evaluate the effectiveness, accessibility, and quality of personal and population-based health services.
- Conduct research to attain new insights and innovative solutions to health problems.
SOURCE: IOM, 2011.
The leadership role of public health agencies should not be regarded as synonymous with a directive role. When public health was focused primarily on infectious disease control, its activities often were based on coercive legal authority. However, as the scope of public health has broadened to include preventing chronic disease, promoting healthy communities, and reducing or even eliminating health disparities, collaborative and facilitative approaches have become predominant. Greater attention is being paid to mobilizing and engaging important stakeholders, including community-based organizations, in promoting public health. This multisectoral approach is based on the premise that local agencies and organizations have a better understanding of the local context in which public problems can be studied and solutions can be developed, executed, and sustained (Israel et al., 2008; Minkler and Wallerstein, 2008; Ramanadhan et al., 2012).
It must be noted that the list of essential public health services today would also include ensuring equity within and across different population groups. Despite tremendous investments in research, planning, and deployment of public health strategies and their success, it has become clear that the benefits of these programs are accruing unequally across socioeconomic and racial/ethnic groups (Spalter-Roth et al., 2005). The challenge of erasing persistent health disparities has been the subject of extensive attention in recent years (IOM, 2002, 2012c), and the contributing social and individual factors are now better understood. These factors—which include social class, race and ethnicity, social and economic policies, racism, geography, housing, and communication inequalities, among many others—appear to explain why certain groups experience greater adversity due to risk conditions and also are often unable to take advantage of programs and policies that should ameliorate such conditions (IOM, 2011). A great deal of this work has focused on either childhood poverty or the experience of adults, with much less attention to young adults. But it is clear that any efforts to address health disparities will have to account for the experience of this important age group, as the effects they experience are likely to last for several decades.
PRIORITY PUBLIC HEALTH ISSUES FOR YOUNG ADULTS
Some recent reviews of young adult health have pointed to encouraging trends, such as decreases in rates of suicide, gonorrhea, and cigarette use1 (Mulye et al., 2009; Park et al., 2006, 2014). However, the mortality rate for young adults aged 20-24 is 93.5 per 100,000, compared with
__________________
1 Although use of cigarettes is declining, the use of other tobacco products, such as electronic cigarettes, may be increasing (King et al., 2013).
60.8 among older adolescents (aged 15-19) and 17.4 among younger adolescents (aged 10-14), showing a substantial increase with age (CDC, 2014a). Young adults are at greater risk for short- and long-term impacts on health and have worse health outcomes than adolescents in many areas (Park et al., 2014). Overall, as compared with other age groups, young adults have the highest rate of death and injury from motor vehicles, homicides, mental health problems, sexually transmitted infections (STIs), and substance abuse (Neinstein, 2013). Yet in general, most of the leading causes of illness and death among young adults are largely preventable (Mulye et al., 2009).
Important developmental changes occurring during young adulthood can promote or compromise health and well-being (Harris et al., 2006; Mulye et al., 2009; Neinstein, 2013). Most young adults are transitioning from direct parental supervision to living on their own, which can create a period of vulnerability to unsafe and unhealthy behaviors. Many young adults need help coping with stressful circumstances in school or on the job, and a significant subset are at risk of experiencing acute emotional distress and the onset of major mental disorders (Garcia, 2010). These conditions can, in turn, impact education and workplace achievement in the short term as well as throughout life. There are also profound health and well-being consequences for young adults who have children (as discussed in Chapter 3). Moroever, risk-taking behaviors associated with morbidity and mortality across the life span tend to emerge or peak during young adulthood, with important immediate and long-term health consequences (Park et al., 2006, 2014). For example, use of tobacco and low levels of fitness and poor nutrition increase the probability of developing diseases such as cardiovascular and pulmonary disease and cancer later in life (Santelli et al., 2013). The collective impact of these problems is noticeable at the public health level, where little change in risky behavior has occurred over the past decade. And while in some ways, young adults appear relatively healthy, many public health concerns for young adults remain inadequately and ineffectively unaddressed (Park et al., 2006, 2014).
“Many people think, ‘you just have the blues, and you will get over it.’ Many people don’t recognize the long-term effects in terms of employment, general quality of life, et cetera.”*
For the past 30 years, Healthy People has set the national objectives for improving public health. Healthy People 2020 focuses more on adolescents and young adults as compared with previous decades (Koh et al.,
__________________
* Quotations are from members of the young adult advisory group during their discussions with the committee.
2011). Based on guidance from national experts, Healthy People 2020 identifies 41 “core indicators for adolescent and young adult health,” which concentrate on individual outcomes, as well as systems that influence health for these populations.2 The indicators span seven domains: health care (health insurance coverage, well care, immunizations), healthy development (adult connection, graduation, sleep, transition planning3), injury/violence prevention (motor vehicle crashes, riding with a drinking driver, graduated driver licensing laws, homicide, exposure to violence, physical fighting), mental health (suicide rate and attempts, depression, treatment), substance abuse (marijuana use, binge drinking, treatment), sexual and reproductive health (pregnancy prevention, STIs, HIV, reproductive health services), and prevention of chronic disease (oral health, hearing, obesity, physical activity, tobacco) (HHS, 2012a). Although all of the indicators are important for the health, safety, and well-being of young adults, this chapter focuses on an illustrative selection of public health challenges that are related most specifically to the health, safety, and long-term well-being of young adults and that pose substantial public health burdens—motor vehicle injuries; homicide and nonfatal assaultive injuries; sexual assault and intimate partner violence; mental health disorders and suicide; substance abuse; sexual and reproductive health; and chronic disease prevention, including decreasing obesity, reducing tobacco use, and increasing immunizations. Box 6-2 presents key findings on the public health challenges for young adults.
In addition, race, ethnicity, sex, sexual identity, age, disability, education, socioeconomic position, and geographic location all are associated with the health and safety of young adults (Mulye et al., 2009). Among both adolescents and young adults, certain populations have higher rates of risky behaviors, such as unhealthy eating, lack of physical activity, unprotected sexual activity, substance use, and unsafe driving (Park et al., 2014). Some examples are presented in Box 6-3. Major gender differences exist, as well as considerable ethnic and racial disparities, with non-Hispanic black and American Indian/Alaska Native young adults faring worse in many areas (Park et al., 2014). As Box 6-3 shows, many statistics are worse for certain populations than for others, but it is important to note that the differences go both ways. For instance, black males have a higher homicide rate than white males in this age group (100.3 versus 11.4 homicides per 100,000), but the reverse is true for the use of marijuana between early adolescence and young adulthood (Chen and Jacobson, 2012; Smith and Cooper, 2013).
__________________
2 See http://www.healthypeople.gov/2020/learn/Draft_Core_Indicators_Web.pdf (accessed October 22, 2014) for a full list of indicators.
3 Transition planning refers to individuals with special health care needs whose health care provider has discussed transition planning from pediatric to adult health care.
BOX 6-2
Illustrative Public Health Challenges for Young Adults
Below are some of the public health challenges that impose the greatest burdens on the health, safety, and well-being of young adults. They are presented using the Healthy People 2020 adolescent and young adult domains as a guide.
Injury and Violence Prevention
Reducing Motor Vehicle Injuries
- Motor vehicle crashes account for the largest percentage (approximately 20 per 100,000) of unintentional injury fatalities for 18- to 25-year-olds in the United States (Neinstein, 2013).
- Nonfatal injury rates also are higher among 18- to 25-year-olds than among 12- to 17-year-olds and 26- to 34-year-olds (Neinstein, 2013).
- In 2010, motor vehicle–related hospitalization and treatment of young adults in emergency departments cost the health care system $9 billion (Neinstein, 2013).
- In 2012, 32 percent of 21- to 24-year-olds involved in fatal motor vehicle crashes had blood alcohol levels of .08 or higher, followed by those aged 25-34 (29 percent) (versus 18 percent for those aged 16-20) (NHTSA, 2013).
- Drivers in their 20s accounted for 23 percent of drivers involved in fatal crashes and 27 percent of distracted driving fatalities, 34 percent of which involved use of cell phones (NHTSA, 2014).
Reducing Homicide
- Homicide is the second leading cause of mortality for 18- to 25-year-olds (Neinstein, 2013).
- Young adults aged 18-24 had the highest homicide rate of any age group but also experienced the greatest rate (22 percent) of decline from 2002 (15.2 per 100,000) to 2011 (11.9 per 100,000) (Smith and Cooper, 2013).
- Between 1981 and 2010, firearms accounted for nearly 80 percent of all homicides among 10- to 24-year-olds, and on average, firearms homicides occurred at 3.7 times the annual rate of nonfirearms homicides (CDC, 2013b).
Reducing Nonfatal Assault
- Males aged 18-25 are 70 percent more likely to be assaulted than 12- to 17-year-old males and 50 percent more likely than 26- to 34-year-old males (Neinstein, 2013).
- Young adults aged 18-25 are 220 percent more likely than 12- to 17-year-olds and 75 percent more likely than 26- to 34-year-olds to be injured by firearms (Neinstein, 2013).
- In 2011, more than 700,000 10- to 24-year-olds were treated in emergency departments for physical assault injuries (CDC, 2012).
- In 2011, the nonfatal assault-related injury rate was highest for those aged 20-24, with a rate of 1,867.5 per 100,000 for males and 1,215.1 per 100,000 for females (CDC, 2013d).
Reducing Sexual Assault and Intimate Partner Violencea
- Females aged 18-34 are more likely to experience sexual violence (about 4 victimizations per 1,000) than 35- to 64-year-olds (approximately 1.5 per 1,000) (Planty et al., 2013).
- Between 2004 and 2006, more than 100,000 females and 3,500 males aged 10-24 received emergency medical care for nonfatal sexual assault injuries (Gavin et al., 2009).
- The majority of female victims (79.6 percent) experienced their first completed rape before age 25—42.2 percent before age 18 (Black et al., 2011).
- In a study of undergraduate females, almost 20 percent reported experiencing completed sexual assault since entering college (Krebs et al., 2009).
- Almost one-third of female veterans were raped or sexually assaulted while serving in the military (Natelson, 2009), and in fiscal year 2013, among the 3,337 sexual assault investigations in the military, 65 percent of victims were under 25 (DoD, 2014).
- Intimate partner rape, physical violence, and/or stalking has been experienced by 35.6 percent of women and 28.5 percent of men (Black et al., 2011).
- Almost half of women (47.1 percent) and 38.6 percent of men who ever experienced intimate partner rape, physical violence, and/or stalking were aged 18-24 (Black et al., 2011).
- Intimate partner violence can lead to negative physical and mental health outcomes, ranging from gastrointestinal problems, migraines, and depression to posttraumatic stress disorder and suicidal thoughts and behavior (Randle and Graham, 2011; Stewart and Robinson, 1998).
Mental Health Conditions
Preventing Mental Health Disorders
- Approximately 75 percent of lifelong mental health disorders are manifest by age 24 (Kessler et al., 2005), and many conditions, such as depression, anxiety disorders, psychoses, and eating and personality disorders, start before age 24 and persist into adulthood (IOM and NRC, 2013; Patel et al., 2007; Paus et al., 2008).
- Data from the National Study of Drug Use and Health (NSDUH) from 2010 to 2012 indicate that 18.7 percent of 18- to 25-year-olds had had any mental illness in the past year, and 3.9 percent had had a serious mental illness (SAMHSA, 2014). In the past year, among those with any mental illness, 66.6 percent had not received mental health services, and 47 percent with a serious mental illness had not received treatment (SAMHSA, 2014).
Preventing Suicide
- Suicide is the third leading cause of mortality in young adults aged 18-25 (Neinstein, 2013).
- Current young adult suicide rates are almost twice as high as those for adolescents (CDC, 2014d).
Substance Abuse
Reducing Substance Use Disorders
- Compared with adolescents, young adults have a higher rate of drug-related causes of death: 16.7 percent of all deaths among 20- to 29-year-olds have drug-related causes versus 2.2 percent among 10- to 19-year-olds (Mack, 2013).
- NSDUH data from 2012 indicate that 18.9 percent of young adults had substance dependence or abuse disorders, a rate markedly higher than that among 12- to 17-year-olds (6.1 percent) and adults 26 and over (7.0 percent) (SAMHSA, 2013).
- From adolescence to young adulthood, alcohol use increases fourfold, binge drinking (five or more alcoholic drinks on a single occasion in the past 2 weeks) fivefold, and heavy alcohol use (five or more binge drinking episodes in the past month) 10fold (SAMHSA, 2013).
- Among 16- to 34-year-olds, 21- to 25-year-olds are most likely to drive under the influence of alcohol (Neinstein, 2013).
- In 2012, 39.5 percent of 18- to 25-year-olds participated in binge drinking and 12.7 percent in heavy drinking, rates similar to those in 2011 (39.8 percent and 12.1 percent, respectively) (SAMHSA, 2013).
- Among young adults aged 18-22, full-time college students have higher binge drinking rates than non-full-time students (Neinstein, 2013).
- Rates of past-month marijuana use double from adolescence (7.6 percent) to young adulthood (18.8 percent); after age 26, rates of use drop to approximately 5 percent (SAMHSA, 2012).
- About 1.1 percent of 18- to 25-year-olds reported using cocaine in the past month, which is similar to the rate for hallucinogens (SAMHSA, 2013).
- Young adults aged 18-25 have the highest rates of abuse of prescription opioid pain relievers, attention-deficit hyperactivity disorder stimulants, and antianxiety drugs (NIH, 2014).
- Approximately 3,000 young adults died from prescription drug (mainly opioid) overdoses in 2010, which is more than the number who died from heroin and cocaine overdoses; many more needed emergency treatment (NIH, 2014).
Sexual and Reproductive Health
Reducing Unintended Pregnancies and Promoting Healthy Birth Spacing
- In 2012, the mean age of mother at first birth was 25.8, an increase from 25.6 in 2011 and from 21.4 in 1970 (Martin et al., 2013).
- The highest rates of unintended pregnancy occur in 20- to 24-year-olds (50 percent, compared with 25 percent in 25- to 44-year-olds) (Mosher et al., 2012; Neinstein, 2013). This means that about 2.6 million births between 2002 and 2006 among 20- to 24-year-olds were unintended, and these percentages have remained relatively steady since 2002 (Mosher et al., 2012).
- The percentage of unintended pregnancies ending in abortion is 37 percent among 15- to 19-year-olds and 41 percent among 20- to 24-year-olds (Neinstein, 2013).
Sexually Transmitted Infections (STIs)/HIV Prevention
- The Centers for Disease Control and Prevention (CDC) estimates that almost 20 millionb new STIs occur yearly in the United States; 15- to 24-year-olds account for 50 percent of all new STIs, although they represent just 25 percent of the sexually experienced population (CDC, 2013c).
- Cervical and human papillomavirus (HPV) infections are the most common STIs, with 74 percent of new infections (6.2 million) each year occurring in 15- to 24-year-olds (Neinstein, 2013).
- Between 2008 and 2010, HIV rates increased (CDC, 2013e), with the highest rate of new cases occurring in 20- to 24-year-olds.
Preventing Chronic Diseases
Decreasing Obesity
- Overweight and obesity rates increase from adolescence to young adulthood. Rates are almost 50 percent in male and female 18- to 25-year-olds and are nearly 60 percent in female and more than 70 percent in male 26- to 34-year-olds (Neinstein, 2013).
- Even though young adults are doing better at meeting the recommended physical activity guidelines, about 40 percent still do not do so (Neinstein, 2013).
- In the National Health and Nutrition Examination Survey, males aged 18-24 reported about 5.4 hours a day of sedentary activity versus 7.4 hours for 12- to 17-year-old males; the corresponding figures for females were 5.7 and 8.0 hours (Neinstein, 2013).
Reducing Tobacco Use
- Approximately 90 percent of smokers start smoking by age 18, and 99 percent start by age 26 (HHS, 2012b).
- Of all age groups, young adults have the highest rate of current cigarette smoking, with approximately one of every three young adults under 26 being a smoker (HHS, 2012b).
- Among 18- to 22-year-olds, 21.3 percent of full-time college students reported smoking cigarettes in the NSDUH, compared with 37.2 percent among those not enrolled in college full time (SAMHSA, 2013).
- In 2012, among 18- to 25-year-olds, 10.7 percent had smoked cigars and 5.5 percent had used smokeless tobacco (the highest prevalence of any age group) in the past month (SAMHSA, 2013).
Increasing Immunizations
- Currently, 30 percent of 19- to 26-year-old females, 2.8 percent of 19- to 21-year-old males, and 1.7 percent of 22- to 26-year-old males are initiating HPV vaccination (Kester et al., 2014).
- In 2010, 25 percent of 18- to 25-year-olds received the influenza vaccine, versus 31 percent of 26- to 34-year-olds, and only 12-16 percent of 18- to 25-year-olds received the pertussis vaccinec (Neinstein, 2013).
________________
a Intimate partner violence, as defined by the National Crime Victimization Survey, includes rape or sexual assault, robbery, aggravated assault, and simple assault committed by the victim’s current or former spouse, boyfriend, or girlfriend (Catalano, 2013).
b This estimate is based on eight common STIs: chlamydia, gonorrhea, hepatitis B virus, herpes simplex virus type 2, HIV, human papillomavirus, syphilis, and trichomoniasis.
c The pertussis vaccine prevents against a respiratory disease, commonly known as “whooping cough,” that is highly contagious.
BOX 6-3
Illustrative Health Disparities
Below are some of the public health disparities (presented in alphabetical order) that impact the health, safety, and well-being of young adults.
Chronic Disease Prevention
- Among females over 18, the overall prevalence of obesity in 1999-2010 was 51 percent among non-Hispanic blacks, compared with 41 percent among Mexican Americans and 31 percent among non-Hispanic whites (May et al., 2013).
Homicide
- The peak rate of homicide victimization for black males occurs at the age of 23 (100.3 homicides per 100,000 population). This is almost 9 times higher than the peak rate for white males, which occurs at the age of 20 (11.4 homicides per 100,000 population) (Smith and Cooper, 2013).
- Homicide rates among black females peak at age 22 (11.8 homicides per 100,000), compared with white females, whose homicide rate is highest before the age of 2 (4.5 per 100,000) (Smith and Cooper, 2013).
Immunizations
- In females aged 18-26, there were significant increases in uptake of HPV vaccination (≥1 dose) from 2008 to 2012 (11.6 to 34.1 percent). However,
Hispanics and women with limited access to care continued to have lower rates of vaccination (Schmidt and Parsons, 2014).
Intimate Partner Violence
- The rate of intimate partner violence for females of all ages (5.9 per 1,000) is nearly six times that for men of all ages (1.1 per 1,000) (Catalano, 2013).
Mental Health Conditions
- Studies have found that 15- to 24-year-old males are more reluctant to try to find professional care for mental health problems than their female counterparts, and young indigenous and ethnic minorities may be even less likely to do so than whites (Rickwood et al., 2007). Black young adults aged 18-26 are less likely than other racial/ethnic groups to receive mental health services (Broman, 2012).
- A study of 21- to 25-year-olds found that rates of mental disorders and suicidal behavior among those with a predominantly homosexual orientation were 1.5 to 12 times higher than the rates among those with an exclusively heterosexual orientation (Fergusson et al., 2005).
Motor Vehicle Injuries
- Among 20- to 24-year-olds, rates of mortality due to motor vehicle crashes are significantly higher for males (25.8 per 100,000 population) than for females (4.2 per 100,000). The highest rates are among African American males (106.1), followed by non-Hispanic American Indian/Alaska Native males (20.6 per 100,000) (CDC, 2014a).a
Nonfatal Assault
- Males aged 18-25 are more than 8 times as likely as their female counterparts to be nonfatally shot (Neinstein, 2013).
- In 2012, among 20- to 24-year-olds, the unadjusted violent victimization rate was 100.6 per 1,000 for persons with disabilities and 36.6 for those without disabilities (Harrell, 2014).
- In 2012, 35.8 percent of overall hate violence survivors and victims were aged 19-29, a slight increase from 2011 (33 percent) (NCAVP, 2013).
Reproductive Health
- In 2012, among unmarried females aged 20-24, birth rates were highest among African Americans (103.5 per 1,000) and Hispanics (96.5 per 1,000), while the birth rate for non-Hispanic whites of the same age was 46.6 per 1,000 (Martin et al., 2013).
Sexual Assault
- Among 18- to 25-year-olds, females are 18 times more likely to be sexually assaulted than males (Neinstein, 2013).
- Among 12- to 34-year-olds, African Americans have the highest rates of sexual assault; among 18- to 25-year-olds, they are 63 percent more likely than whites and 216 percent more likely than Hispanics to be sexually assaulted (Neinstein, 2013).
Sexually Transmitted Infections (STIs)/HIV Prevention
- The rate of HIV diagnosis per 100,000 African American 20- to 24-year-olds (146.9) is more than 4 times the rate for Hispanics (33.3) and almost 12 times that for whites (12.3) in the same age group (CDC, 2013e).
- Among all gay and bisexual males aged 13-24, there was an increase of 22 percent in the incidence of HIV infection from 2008 to 2010 (7,200 to 8,800). The highest incidence within this age group was among African American males, accounting for 4,800 cases (CDC, 2012).
Substance Use
- Past-month alcohol use rates are similar among females (58 percent) and males (63 percent) aged 18-25, with the highest rates being among whites (67 percent) and Hispanics (54 percent) and the lowest among Native Hawaiians/Other Pacific Islanders (43 percent). Binge drinking is higher among males (46 percent) than females (33 percent) of the same age group, and lowest among African Americans (27 percent) and highest among whites (46 percent) and non-Hispanic Native Americans/Alaska Natives (41 percent) (SAMSHA, 2013).
- Past-month marijuana use is higher among males (23 percent) than females (14 percent) aged 18-25, with the highest rates being among African Americans (22 percent) and whites (20 percent), followed by Native Americans/Alaska Natives (16 percent) (SAMSHA, 2013).
- Between early/middle adolescence and young adulthood, whites generally exhibit the highest levels of alcohol use and heavy drinking, while African Americans exhibit the lowest levels, although levels of alcohol use and heavy drinking do not show significant variation across different racial and ethnic groups after age 30 (Chen and Jacobson, 2012).
PUBLIC HEALTH INTERVENTIONS FOR YOUNG ADULTS
Public health interventions include a broad array of activities, such as informing or educating the targeted population about risks, persuading them to reduce risk, creating incentives or disincentives to encourage them to adopt healthy or safe behaviors, and modifying the environment to reduce exposure to risks or to promote or facilitate safe or healthy behaviors. Exposures include not only environmental toxins and dangerous products but also adverse social experiences, such as racism, violence, and social threats or health risks resulting from poor living and working con-
- Even though their levels of marijuana use start to decline after age 29, African Americans have the highest rates of marijuana use after their late 20s compared with whites, Hispanics, and Asians (Chen and Jacobson, 2012).
Suicide
- In the 18-25 age group, non-Hispanic blacks are 1.3 times, Asians 1.7 times, Native Americans/Alaska Natives 1.6 times, and Native Hawaiians/Other Pacific Islanders 7.1 times more likely to have suicidal ideation than whites (Han et al., 2014).
- Among those aged 20-24, suicide is approximately three times higher in males (13.8 per 10,000) than in females (4.7 per 10,000) (CDC, 2014a).
- High school graduates aged 18-25 are 1.3 times more likely than college graduates to have suicidal ideation; unemployment also is associated with a higher risk of suicidal ideation in 18- to 25-year-olds (Han et al., 2014).
- The lifetime prevalence of suicide attempts in gay and bisexual male adolescents and adults was four times that in comparable heterosexual males, and the prevalence among lesbian and bisexual females was almost twice that among heterosexual females. This is the opposite of the gender pattern found in the general population (HHS, 2012c; King et al., 2008).
Tobacco Use
- Past-month cigarette use rates among 18- to 25-year-olds are highest among non-Hispanic Native Americans/Alaska Natives (62 percent), followed by whites (44 percent) and African Americans (32 percent); the rates are lowest among Asians (19 percent) (SAMSHA, 2013).
- Cigarette use is highest for whites through adolescence and young adulthood, while use among African Americans is higher after age 30 than for other racial and ethnic groups (Chen and Jacobson, 2012).
________________
a These rates do not include those classified as “undetermined intent.” If those are added, the rates rise to 42 per 100,000 for males and 13.7 for females, and the highest rate is 58.2 for American Indian/Alaska Native males.
ditions. To the extent that individual behaviors play a causal role, recent public health approaches go beyond changing those behaviors to focus on mobilizing and engaging different sectors to create an environment that facilitates and sustains behavior change, as well as on changing public health practice and policies. These interventions can target the whole population of a community or specific subpopulations thought to be at elevated risk. They can be deployed separately or used in combination, creating synergy. Tools may also include legal requirements or prohibitions. All of these approaches have been used, with varying degrees of success, to address the
significant problems identified above that threaten the health, safety, and well-being of young adults, although previously, the focus was primarily on changing individual behavior rather than altering the broader context and environment.
When a multilayer approach is implemented—for example, to reduce the incidence of unsafe driving due to either alcohol use or distracted driving—the likelihood of success is greater (Park et al., 2006). The ecological model or approach assumes that individual behaviors are products of influence at multiple levels, including intrapersonal, interpersonal, organizational, community/built environment, and public policy (Bronfenbrenner, 1979; Sallis et al., 2008). Moreover, a critical assumption is that behaviors are outcomes stemming from interactions across levels and that the context in which behaviors occur can exert significant influence on individuals (Bronfenbrenner, 1979; Sallis et al., 2008). With respect to risky behaviors, for instance, young adults working in the construction industry are likely to be socialized to a different set of norms and practices than those attending 4-year colleges. As an example, the greater use of tobacco among blue-collar workers may be attributable to a lack of knowledge and social supports at the individual level and perhaps to fewer restrictions on smoking in the workplace (Sorensen et al., 2004). Ecological approaches draw on a variety of theories and are robust when applied to specific behaviors. While these approaches have been used for some time, rigorous research has just begun to explore the mechanisms explaining the outcomes of multilevel interventions. In this section, we summarize the evidence base on public health interventions in selected priority areas to illustrate what is known.
Goals of Public Health Interventions
Promoting change in public health is a complex endeavor in terms of both the outcomes expected to result from a campaign and the context in which campaign messages are disseminated and received (Randolph and Viswanath, 2004). Health outcomes vary considerably, including changes in cognition, attitudes, beliefs, affect, salience, preferences, behavioral intentions, and behaviors at the individual level. A campaign may focus on the initiation of new behaviors, such as beginning to eat healthfully or engaging in physical activity (Snyder et al., 2004). In the case of risky behaviors, such as unsafe sex and use of tobacco, alcohol, or illicit drugs, one goal is to deter initiation, but a second stage can be directed at those who may not have been deterred or preventing relapse in the case of tobacco or drug use. Other campaigns may reinforce positive health messages, promoting maintenance, whether of healthy eating or physical activity (Atkin and Rice, 2012). The temporality of campaign effects is another critical consideration, ranging from short-term effects (e.g., influenza vaccination) to longer-term
effects, such as maintaining healthy lifestyles in youth, the effects of which may last well into adulthood (Marcus et al., 2006). The idea of deferring immediate rewards to reap future well-being, such as by stopping smoking in youth to protect oneself from cardiovascular diseases or cancer in adulthood, is a challenging message to communicate, particularly to adolescents and young adults (Hoek et al., 2013). Finally, aside from the effects of an intervention on individual behavior, public health campaigns may aim to shape social norms and to promote, advocate, and instill changes at the institutional and community levels (Holder and Treno, 1997; Hornik, 2002; Hornik and Yanovitzky, 2003; Viswanath and Finnegan, 2002).
In the following sections, we briefly review public health campaigns and other interventions in some of the priority areas discussed earlier.4 We then offer a distillation of lessons learned from these campaigns.
Tobacco Use
Using tobacco can cause cancer and heart and lung disease and can affect fetal well-being (Viswanath et al., 2010b). Tobacco use is estimated to cost 480,000 lives per year as a result of cancer in at least 18 different organ sites and other chronic diseases, such as cardiovascular and chronic obstructive pulmonary diseases (HHS, 2014c; Viswanath et al., 2010b), yet it is one of the most preventable causes of mortality and disease in the United States. Not surprisingly, public health interventions attempting to dissuade people from initiating tobacco use, as well as promoting cessation among users, have received considerable attention.
Tobacco control interventions are an outstanding example of multilevel approaches whereby interventions at one level have been aided by interventions at other levels (NCI, 2008). At the societal and community levels,
__________________
4 To review the interventions focused on young adults that are discussed, we conducted an extensive search of the literature using PubMed and a number of search terms derived from the priority areas specified in Chapter 5, including the combined terms “young adult,” and “intervention.” Additional search terms included “African American,” “Latino,” and “low income” to capture a more diverse sample. A secondary search was conducted using “young adult” and “intervention” in the Cochrane Review Database. Searches were restricted to articles published between 2009 and 2014, although reviews that included individual articles before this date were included. Other inclusion criteria were (1) reported findings of an intervention (those reporting only protocols or cost analyses were excluded); (2) inclusion of samples of healthy individuals that were not pregnant or diagnosed with cancer, diabetes, or another chronic condition; and (3) inclusion of samples of young adults aged 18-25 (articles including ages above or below this range were considered only if they were review articles or studies in which the mean age was within this range). The search was not exhaustive; reference lists were not searched for other relevant articles, and other search terms could have been used to identify additional articles. Priority was given to articles that were systematic reviews or emphasized population-level strategies.
evidence shows that comprehensive tobacco control programs, including tax increases, public smoking bans, media campaigns, youth access restrictions, and cessation programs, have reduced the prevalence and intensity of tobacco use (HHS, 2012b; IOM, 2007). At the individual level, media campaigns have focused on promoting knowledge of risks resulting from tobacco use and denormalizing tobacco use behaviors. The focus on individual behaviors is complemented by drawing attention to the deceptive practices of the tobacco industry; offering cessation supports in different institutional settings; promoting support for increased taxes on tobacco; and at the policy level, placing restrictions on marketing, advertising, and using tobacco in different localities, such as the workplace and restaurants (HHS, 2012b; IOM, 2007).
“I am not sure many people quit smoking because they see an ad from an anti-smoking campaign. I think it is more likely that smoking has negative health effects for them or someone they know and they decide at that point to make a change.”
While a large body of work addresses tobacco control interventions among teens and adults (NCI, 2008), interventions focused specifically on young adults have been somewhat limited. A Cochrane review examined the impact of mass media campaigns on smoking prevention among young people (under age 25) (Brinn et al., 2012). Media were defined broadly to include television, radio, newspapers, billboards, posters, leaflets, and booklets. The review examined 7 of 84 studies that met the inclusion criteria and found that they were conducted systematically, drew on sound theories and research-informed interventions, and used extended campaigns to ensure exposure. Brinn and colleagues (2012) report modest evidence that mass media interventions could be successful in the prevention of smoking among young people. In a review of 25 studies examining the effectiveness of multicomponent interventions in reducing smoking uptake among young people, Carson and colleagues (2011) report that one intervention generally was successful in reducing smoking in the short term, and nine showed significant long-term effects. Improvements also were seen in changes in intentions to smoke (six of eight interventions), improved attitudes (five of nine), risk perceptions (two of six), and knowledge of tobacco use (three of six).
In contrast, short-term and/or single-component interventions are less likely to be successful. Villanti and colleagues (2010) conducted a systematic review of 14 studies of interventions promoting smoking cessation among young adults in the United States. The interventions focused on
young adults aged 18-24 and were conducted in multiple settings, including universities, a community college, an airforce basic training unit, a quitline, and a rural community. Interventions were delivered either through interpersonal channels, such as peer coaches, counselors, and health educators, or a computer website. The authors report limited support for the efficacy of the interventions, although brief interventions with an extended dose via telephone or electronic media were somewhat effective. Villanti and colleagues (2010) recommend using standardized measures and interventions that take the smoking trajectories among young adults into account and are conducted among diverse population groups.
The use of electronic media, such as telephone quitlines and text messaging, to promote cessation of tobacco use has drawn the attention of several researchers. The Internet and social media hold considerable promise in promoting cessation. Sims and colleagues (2013) compared the effectiveness of cessation counseling through quitlines with a group receiving only mailed self-help material. They report only short-term effects among the group receiving counseling on the telephone. On the other hand, Brown (2013) reviewed eight studies assessing the impact of technology-based interventions that included tailored texts, emails, counseling, and a discussion board on tobacco use among participants aged 18-30 and found that in at least four studies, there was significant 7-day abstinence in the intervention group.
Similarly, Skov-Ettrup and colleagues (2014) report on a randomized controlled trial involving 2,030 daily smokers aged 15-25. The intervention arm received tailored text messages on self-efficacy, beliefs about smoking, and topics chosen by the user, whereas the control group received only generic messages. While there were no significant differences between the two groups in self-reported cessation, the researchers report higher rates of quitting among those in the tailored messaging group who used the text messages. That is, when the participants actually used the messages, the desired effects were much more likely to occur.
This review highlights four points when it comes to tobacco control interventions among young adults. First, comprehensive tobacco control strategies have had a demonstrable effect in reducing the prevalence and intensity of consumption at the population level (HHS, 2012b; IOM, 2007). Second, more focus is needed on developing and testing effective interventions targeting young adults, especially at a time when new tobacco products are being introduced at a rapid pace. Third, most of the interventions appear to have been carried out in colleges or white collar settings, and more effort needs to be made to include population groups of diverse racial, ethnic, and socioeconomic backgrounds. Last, the new information and communication technologies hold considerable promise in promoting tobacco control, but remain underexplored.
Alcohol Use
Alcohol consumption carries a risk of adverse health and social consequences and is the third leading cause of death in the United States (CDC, 2010). It can have a major impact on individuals, families, and communities that can have cumulative effects, contributing significantly to costly social, physical, mental, and public health problems. Alcohol use is associated with both short- and long-term health risks. Short-term risks, most often caused by binge drinking, include injuries, violence, risky sexual behaviors, miscarriages, and alcohol poisoning (CDC, 2014b). Long-term risks include neurological, cardiovascular, psychiatric, and social problems; cancer; liver diseases; and gastrointestinal problems (CDC, 2014b).
Most public health interventions targeting alcohol use by young adults have focused on college students. Paschall and colleagues (2011a,b) conducted a randomized controlled trial in 30 universities where freshmen were delivered an intervention designed to reduce alcohol use and binge drinking. The intervention was delivered over the Internet in two doses and covered such topics as alcohol laws, policies, and risks; setting personal goals; and dealing with friends with alcohol problems. A booster session was delivered 30-45 days later. Limited reductions in alcohol use and binge drinking occurred immediately following the intervention, but the effects did not persist until the second assessment, in the spring semester (Paschall et al., 2011a,b). In another Web-based screening and intervention program targeting college students aged 17-24, Kypri and colleagues (2014) found that intervention group students receiving personalized feedback and information correcting misperceptions of alcohol use among their peers reported only minimal effect. Both of these Internet-based studies show that use of the Internet alone may not be the most effective intervention strategy with respect to outcomes.
“When I was in college, we had a rule that if you saw somebody who was sick from too much alcohol or from using drugs, you wouldn’t get in trouble if you got them the help that they needed. People shouldn’t be punished for bad behavior; we should make sure they are getting access to health care.”
Similar modest effects were found by Moore and colleagues (2013) in a cluster randomized trial of students in residence halls in Wales, United Kingdom. The intervention focused on correcting misperceptions about the drinking behaviors of peers in order to reduce alcohol consumption. Messages were delivered through nonmedia channels such as posters, coasters,
meal planners, and stickers. There were no significant effects on perceived norms or alcohol consumption between the groups, although there were some other modest effects.
On the other hand, a more broad-based community organizing approach focused on changing the environment with respect to high-risk drinking behavior among college students in North Carolina showed positive outcomes (Wolfson et al., 2012). The intervention encompassed campus-community coalitions; action plans; community organizers in each school; and promotion of environmental strategies, including awareness, enforcement, and policy. It also involved correcting misperceptions about alcohol use and limiting exposure to pro-alcohol messages. The intervention had a significant impact on decreasing consequences due to students’ own drinking, such as requiring medical treatment, getting a driving under the influence/driving while intoxicated ticket, and being taken advantage of sexually, as well as on alcohol-related injuries caused to others. No differences, however, were seen in actual drinking behavior.
Many environmental policy interventions have been effective in decreasing drinking and driving and motor vehicle crashes that involve alcohol among young adults (Hingson, 2010). However, it has been found that for policies to be effective, they need to be put into action and enforced at the local level (Hingson, 2010). It also has been found that multicomponent college-community approaches among college students that incorporate a legal component can decrease alcohol use and drinking and driving (Hingson, 2010).
Three main lessons can be drawn from this review. First, most interventions addressing alcohol use problems among young adults appear to have been conducted among college students, with virtually little or no focus on noncollege youth. Second, single-component approaches (e.g., only promotion or policy) or those using a single channel (e.g., television) are not effective, while a multipronged approach focusing on both the environment and individual behaviors may be more effective. Schulenberg and Maggs (2002) point out that binge drinking at college campuses is multiply determined and held at high rates by a number of pillars ranging from community standards to students’ assumptions about their rights to party. Addressing just one of these pillars is insufficient because the others will pick up the slack and keep the rates high. Third, multimodal community-wide interventions, including legal enforcement, have been shown to reduce drunk driving and alcohol-involved crashes among young adults.
Chronic Disease Prevention
Many interventions for chronic disease prevention center on maintaining a healthy lifestyle and focus on prevention of weight gain, weight loss,
healthy eating, and physical activity. Obesity increases the risk of chronic illness and is associated with reduced quality of life and adult success, as well as substantial human and societal costs (IOM, 2012a). Individual effects include illness (e.g., cardiovascular disease, diabetes, hypertension), disability, social ostracism, discrimination, depression, and poor quality of life (IOM, 2012a). Moderate amounts of daily physical activity are recommended for people of all ages both to remain healthy and to improve health. A decline in physical activity is one of the lifestyle changes that can occur during young adulthood.
Many studies have targeted the transition to college, most often using the college setting to recruit participants and deliver intervention components. In one example, undergraduate health classes were used to administer a goal-setting intervention. Participants who wrote if-then statements about healthy eating goals significantly increased their fruit and vegetable consumption relative to participants assigned to a general goal-related task (Chapman et al., 2009). Likewise, over a 15-week period, a college class-based intervention involving 80 students that met three times per week, emphasizing healthy choices and in-class activities, also significantly increased the consumption of fruits and vegetables among participants (Ha and Caine-Bish, 2009). And a sample of college freshmen who were administered an alternative-reality game during a college health education course significantly increased their physical activity compared with controls, although both groups gained a significant amount of weight over the study period, suggesting that other factors in the college experience were impacting weight changes (Johnston et al., 2012).
Online sources also have been used to influence healthy behaviors and weight loss, again in a college setting. For example, Gow and colleagues (2010) administered an intervention using an Internet classroom tool, finding that participants who received the intensive 6-week intervention with feedback on their weight had significantly lower body mass index than controls. The authors note that the combination of monitoring, feedback, and education had a stronger effect on behavior than each component separately. In another study, an Internet-based curriculum that provided 10 online lessons focused on healthy eating and physical activity to students across eight universities significantly increased fruit and vegetable intake and physical activity, with positive, lasting effects being seen over the course of 15-month follow-up (Greene et al., 2012). In another study, however, although an intervention using texts, emails, and a smartphone application led to decreases in body weight and increases in physical activity and healthy eating among the intervention group, no significant differences were observed relative to the control group (Hebden et al., 2014).
Reviews of weight loss interventions among young adults have shown mixed results. Interventions combining diet, exercise, and motivation con-
sistently show weight loss among young adults, although because of the varied components of these interventions, determining what elements are the most effective is problematic (Poobalan et al., 2010). Another review of 37 studies found that university course-based interventions often resulted in weight loss, with many self-monitoring interventions showing positive results as well (Laska et al., 2012). However, both reviews highlight the need to develop and evaluate rigorous weight gain prevention interventions focused on young adults that fully reflect the rapidly shifting life circumstances of this age group and incorporate more diverse populations.
Studies in this area have shown varying degrees of success. Many of the researchers acknowledge that an environmental approach is necessary to fully address the range of issues faced by young adults as they transition into making their own health-related choices, including pressure to engage in certain harmful behaviors.
Prevention of Sexually Transmitted Infections/HIV
STIs are infections that are transmitted primarily through sexual contact. Although they are largely preventable, they remain a significant public health concern, and some have the potential to cause serious health problems, especially if not diagnosed and treated early. The consequences of untreated STIs often are worse for young women than for young men, even though the yearly number of new infections is roughly equal among them (51 percent and 49 percent, respectively) (CDC, 2013c). Although HIV transmission is generally preventable, there is no vaccine or cure. As a result, HIV continues to be a major public health concern.
Several strategies have addressed STI and HIV prevention among diverse samples of young adults across a number of settings, often focusing on increasing condom use and decreasing risky sexual practices. In their sample of U.S. university students aged 18 and older, Norton and colleagues (2012) found that participants exposed to a 60-minute DVD addressing motivation, information, and behavioral skills with respect to increasing condom use and decreasing risky sexual practices changed these behaviors more when the topic was prevention of STIs or unplanned pregnancy than when it was HIV prevention.
Community-based participatory research was used to create a culturally congruent HIV prevention intervention, AMIGAS (Amigas, Mujeres Latinas, Inform andonos, Gui andonos, y Apoy andonos contra el SIDA [friends, Latina women, informing each other, guiding each other, and supporting each other against AIDS]), for young Latina women living in Miami, Florida, modeled after the evidence-based SiSTA (Sistas Informing Sistas about Topics on AIDS) program for African American women (DiClemente and Wingood, 1995; Wingood et al., 2011a). Within the
AMIGAS intervention, Latina health educators delivered four interactive group sessions emphasizing cultural and gender pride, the importance of healthy relationships, HIV knowledge, and how experiences unique to Latina women may increase HIV risk (Wingood et al., 2011a). At the 6-month follow-up, program participants reported significantly more consistent condom use, greater self-efficacy for negotiating safe sex, greater HIV knowledge, and fewer perceived barriers to using condoms compared with controls.
Several studies have targeted African American young adults in various community- and technology-based settings for the reduction of HIV risk behaviors. Aronson and colleagues (2013) developed a pilot intervention with 57 participants that used community-based participatory research partnerships among students, university faculty, and community partners to create a retreat for young adult African American men in which to discuss safe sex, followed by reinforcement messages via electronic media over the course of 3 months. Average number of sex partners and condom errors decreased significantly among participants, with the authors attributing much of this success to the high level of engagement with community partners. In a pilot study by Kennedy and colleagues (2013), a theory-driven, single-session condom promotion program delivered to 18- to 24-year-old African American men recruited from neighborhoods bordering urban community centers significantly increased condom use, perceived condom availability, and positive reasons to use condoms compared with a comparison group that received a general health curriculum. Results suggest that this brief, culturally appropriate prevention program may reduce risky sexual behaviors among high-risk youth from urban communities.
An HIV intervention for young African American women at Planned Parenthood in Atlanta, Georgia, used two computer-based 60-minute interactive sessions also modeled after the SiSTA program (DiClemente and Wingood, 1995; Wingood et al., 2011b). The intervention significantly increased knowledge of HIV prevention, condom self-efficacy, and condom use in participants compared with a control group that received a small-group session on general health topics (Wingood et al., 2011b). Another intervention with low-income African American young women at high risk for HIV used smartphones to stream a soap opera highlighting HIV risk reduction (Jones et al., 2013). Although no statistically significant differences were seen between the intervention and control groups, participants who viewed the videos found them engaging and wished to continue receiving them, prompting further research on how to reach this population on a popular messaging platform.
International studies also have shown success. A Dutch Web-based study involved a tailored intervention for young adults that used a virtual clinic with motivational interviewing, participant-specific feedback, and educational models. Significantly higher condom use and maintenance re-
sulted from the intervention compared with general feedback or treatment as usual (Mevissen et al., 2011). A study in India found that a workplace-based PowerPoint, video, and training session significantly increased positive perceptions of condoms and knowledge of proper wearing techniques among males aged 18-30 (Ray et al., 2012). The authors emphasize that simply providing knowledge may not be sufficient, and that a range of education on behavior, perception, and skill may be needed with this group.
In sum, many interventions targeting STI or HIV prevention saw success when they focused on topics most relevant to young adults; included culturally competent, tailored materials; and introduced skill components along with this tailored feedback.
Human Papillomavirus (HPV) Vaccination
HPV vaccination, recommended for females under 26 and males under 21, entails a series of three shots that protect against HPV infection and HPV’s associated health problems, such as cancer and genital warts (CDC, 2014c). Brief intervention techniques highlighting the benefits of HPV vaccination have been shown to increase positive perceptions of the vaccine and increase vaccination intention and reception. For example, Kester and colleagues (2014) recruited a sample of 18- to 26-year-olds at a minority health fair. Intervention group participants received a 5- to 10-minute small-group presentation on HPV infection, detection, and treatment; additional information sources; and a list of locations where the vaccine could be received. Participants had higher HPV knowledge scores and vaccination intention compared with controls.
HPV education also has been delivered to university populations in school computer labs. Intentions to be vaccinated increased significantly among women viewing an HPV website that provided information tailored to their specific perceived barriers to vaccination compared with women who viewed standard information (Gerend et al., 2013). Short videos also were used by Hopfer (2012), with intervention groups watching videos narrated by peers, medical experts, or both, while another arm reviewed a generic video or HPV website or received no message. HPV vaccination nearly doubled among the participants who watched the combined peer-expert video compared with controls; however, these results were not found for the peer- or expert-only videos, highlighting the importance of the communication source and suggesting that peer messages that normalize medical expert messages may play a crucial role in vaccination.
Direct provision of information about HPV and HPV vaccination may be a simple and effective way to motivate young adults to initiate HPV vaccination (Kester et al., 2014). Tailoring this information to ameliorating or removing specific barriers may enhance the effectiveness of this approach (Gerend et al., 2013).
Sexual Assault and Intimate Partner Violence
Black and colleagues (2011) found that nearly 1 in 5 women and 1 in 17 men reported experiencing rape at some point in their lives (Black et al., 2011). Approximately 1 in 20 women and men (5.6 percent and 5.3 percent, respectively) had experienced sexual violence other than rape.
Several interventions have sought to address sexual assault by providing girls and women tools needed to prevent these acts from occurring. One study focused on the transition of young adult women to the college environment, enlisting their mothers to participate with them the summer prior to their freshmen year (Testa et al., 2010). Mothers in the intervention condition were advised to complete a workbook on alcohol safety with their daughter before the start of school, with participants in the enhanced intervention condition also receiving a workbook chapter on college dating. Both intervention conditions were correlated with decreased incapacitated rape levels during the first year and increased communication among mothers and daughters, which predicted fewer drinking episodes, leading to lower sexual victimization rates involving alcohol.
Another study delivered an intervention for women to promote group responsibility, environmental awareness, and safe personal conduct as groups of college-aged students crossed the border to patronize Tijuana bars. The program led to a significant decrease in reports of sexual victimization (Kelley-Baker et al., 2011). Other strategies have focused on both men and women. A Web-based intervention for college students who were in longer-term relationships advised them on problem solving, communication techniques, and ways to enhance positive relationships, with weekly reminders to employ these skills (Braithwaite and Fincham, 2009). Intervention participants experienced improved mental health and relationship outcomes that continued over time, although anxiety, physical assault, and aggression grew worse before they ultimately improved.
Despite these findings, a meta-analytic Cochrane review of education- and skill-based interventions designed to reduce violence in the context of relationships and dating among youth aged 12-25 found no evidence of a significant effect on relationship violence episodes or on attitudes toward violence (Fellmeth et al., 2013). The 38 interventions included in the review were predominantly educational, and components were delivered in such settings as college classrooms, dorms, and fraternity halls, with sample populations ranging from coed to all-male or all-female. Intervention strategies included group discussions, videos of dramatic vignettes, role playing, problem solving and communication skills, and discussion of rape myths. Despite a trend found in increased knowledge about relationship violence, there was no evidence that these strategies improved participants’ attitudes, actions, or proficiency with respect to violence in relationships. The authors
highlight that the existing evidence relates primarily to determining changes in attitudes and knowledge, and that interventions both across communities and within families may be needed to reduce relationship violence. Further studies with longer-term follow-up and validated, standardized measures also are required to maximize the comparability of results (Fellmeth et al., 2013).
Mental Health Conditions
Mental health and substance use disorders are public health concerns for numerous reasons. First, they can cause death through the act of suicide. Mental health and substance use disorders also affect families and harm individuals by reducing their ability to achieve social, educational, and vocational goals; increasing the potential for further impairment and compromised functioning throughout life; and imposing costs related to extra care requirements and social disruption (NRC and IOM, 2009; Patel et al., 2007), as well as lost productivity (Birmbaum et al., 2010; Kessler et al., 2006). Of all types of illnesses, moreover, mental health and substance use disorders cause the greatest burden of disability in young adults (IOM and NRC, 2013). Furthermore, given the age of onset of behavioral health conditions, preventing or addressing mental and behavioral health needs in this period of life has the potential to reduce lifelong impact, since many fewer new cases occur after age 24 (Kessler et al., 2005). Timely mental health intervention can reduce morbidity and increase long-term health and well-being.
“I have severe mental health issues that I haven’t addressed yet because I don’t want to go to a therapist. I don’t feel comfortable. Why am I going to go to this person and tell them my problems? After what I went through, I have a hard time trusting people to talk about my problems.”
In addition, although not a psychiatric disorder, the experience of stress is pervasive in young adults (APA, 2013). Compared with older adults, young adults experience greater levels of daily stressors (Stawski et al., 2008) and perceive their lives as more stressful (Scott et al., 2013). One of the benefits of maturity appears to be coping better with stressful situations (Luong and Charles, 2014; Price and Dunlap, 1988; Schilling and Diehl, 2014). Even among young adults, the youngest struggle more with stressful events than their slightly older counterparts (Jackson and Finney, 2002). Psychological stress can contribute to the onset of mental illness (Blazer et al., 1987;
Corcoran et al., 2003; Kendler et al., 1999; Muscatell et al., 2009), and its relationship to physical health is well established (McEwen, 2008; McEwen and Gianaros, 2010).
Although mental health treatment is available and effective (HHS, 1999; NIH, 2009; NIMH, 2000), young people, especially young men and young indigenous and ethnic minorities, are reluctant to obtain professional care for problems relating to mental health (Edlund et al., 2012; Gulliver et al., 2010; Rickwood et al., 2007; Wu et al., 2007). Other studies have found that only about 18-34 percent of young people with depression and anxiety disorders seek professional help (Guilliver et al., 2010). Friends and family members rather than health professionals are preferred sources of help (Rickwood et al., 2007). Likewise, Wu and colleagues (2007) found that approximately 4 percent of full-time college students, 7 percent of part-time college students, and 6 percent of nonstudents aged 18-22 with an alcohol use disorder had sought help within the past year. Gayman and colleagues (2011) found that only about one-third of young adults with a substance use disorder had ever sought help; those in whom the onset of the disorder occurred at 18 or older were less likely to have sought help than those whose onset occurred earlier.
Perceived barriers to young adults’ seeking help for behavioral health disorders include stigma and embarrassment, difficulty recognizing symptoms or the need for treatment (i.e., lack of behavioral health literacy), a preference for self-reliance, and lack of confidence that their insurance will pay for treatment (Cellucci et al., 2006; Eisenberg et al., 2007; Gulliver et al., 2010; van der Pol et al., 2013). Perceiving the need for help or being encouraged by family, friends, or others to seek help increases the likelihood of help seeking (Caldeira et al., 2009).
The mental health literacy of young adults is not high (Farrer et al., 2008). Studies in Australia found that fewer than 50 percent of 12- to 25-year-olds could identify depression, and only about 25 percent could identify psychosis (Wright et al., 2005). Rates of recognition are lower in young men than in young women (Cotton et al., 2006). Lack of mental health literacy is regularly given as one of the explanations for missed opportunities to intervene with individuals with serious mental illness (Gulliver et al., 2010; IOM, 2004; Jorm, 2012).
As noted, the stigma attached to having a behavioral health disorder is one important impediment to help seeking by young people, and reducing stigma also is one of the major policy approaches proposed for reducing levels of unmet need for mental health services (HHS, 1999). Public stigma is the reaction of the general population toward a condition; self-stigma is the internalized impact of public stigma, and thus the prejudice people with behavioral health conditions turn against themselves (Corrigan and Watson, 2002); and personal stigma is the reaction
of an individual. All three forms of stigma can reduce willingness to seek behavioral health services (Eisenberg et al., 2009; Held and Owens, 2013), with some evidence suggesting that personal stigma may be a stronger disincentive than public stigma for college students (Eisenberg et al., 2009; Lally et al., 2013). Personal stigma also may pose a barrier to help seeking by reducing recognition of the impact of symptoms and thus the need for help (Schomerus et al., 2012). Generally, however, the specific roles of the various forms of stigma in help seeking are not well understood, specifically in young adults with behavioral health conditions. Many of the studies of public and self-stigma and help seeking in young adults examined these issues in general populations, most of whom did not have a behavioral health disorder.
One study illustrates the potential for unexpected and counterproductive consequences of public service announcements designed to reduce stigma; the announcements actually increased self-stigma and reduced help seeking in individuals with depression (Lienemann et al., 2013). In addition, help-seeking intentions have been studied much more thoroughly than actual help seeking. Thus, any public health campaign to reduce the stigma of behavioral health conditions and encourage help seeking for these conditions should be informed by research aimed at understanding the impact of stigma and of various types of public service announcements on help-seeking behavior in a wide range of young adults with behavioral health disorders.
A further impediment to adequate treatment of behavioral health disorders in young adults is that they are more likely than older adults to drop out of treatment once they have started (Edlund et al., 2002; Hadley et al., 2001; Sinha et al., 2003).
The onset of many mental health conditions during the young adult years has prompted a range of strategies aimed at preventing or treating mental health conditions in this population. A review of community-based prevention and early intervention programs found that the majority of interventions for young adults focus on strategies employing cognitive-behavioral therapy (CBT), which has shown the most reliably positive outcomes for treatment of anxiety or depression (Christensen et al., 2010). A later review focused on technology use among 18- to 25-year-old college students found that of diverse strategies employing the Internet, video, and audio, Internet-based strategies using CBT may be particularly useful for targeting anxiety, and to a lesser extent depression (Farrer et al., 2013). The authors conclude that the use of technological interventions targeting certain mental health problems holds promise for students in university settings, although more research is needed to assess the use of technology for other specific mental disorders. A review of 15 interventions targeting prevention of suicide and self-harm among 12- to 25-year-olds found highly
limited evidence regarding effective interventions for young adults experiencing suicide attempts, deliberate self-harm, or suicidal ideation (Robinson et al., 2011). While the authors acknowledge that CBT may show some promise, more methodologically rigorous trials of this approach are needed (Robinson et al., 2011).
Motor Vehicle Safety
Motor vehicle safety is a major concern for young adults, particularly since, compared with adolescents and adults aged 26-34, young adults (aged 18-25) are more likely to be injured or die in motor vehicle crashes and have more motor vehicle crash-related hospitalizations and emergency room visits (Neinstein, 2013). Historically, actions to prevent motor vehicle crashes and resulting injuries and deaths have taken an ecological approach, including multiple levels of influence such as policy designed to increase seat belt use. Indeed, the most notable road safety campaigns have promoted and enforced seat belt use (Dinh-Zarr et al., 2001) and have used enforcement campaigns to increase their use (Wakefield et al., 2010). For example, the Click It or Ticket program in North Carolina was associated with an increase in seat belt use from 63 percent to 81 percent and lower rates of highway deaths and injuries (Williams et al., 1996). Increasingly, states also are passing laws banning texting while driving, and in some cases any use of cell phones by drivers under age 18, to address distracted driving, a significant factor in motor vehicle crashes (NHTSA, 2014).
“The ‘Distracted Driving’ campaign was interesting and impactful, but I still struggle with being on the phone when driving. Laws about using the phone while driving seem to be making more of an impact than the campaign by itself.”
Law enforcement and repeated short-term mass media exposure appear to be important components of effective motor vehicle safety campaigns (Elder et al., 2004; Morrison et al., 2003; Salzberg and Moffat, 2004; Williams and Wells, 2004). The power of mass media also has been harnessed for drinking and driving campaigns. A social norms–based campaign delivered through television, radio, print, and theater advertisements in Montana reduced normative misperceptions about the frequency of drunk driving, increased designated driver use, and decreased drinking and driving rates among 21- to 34-year-olds within the intervention region (Perkins et al., 2010). Another social marketing approach targeting drunk driving
in Seattle, Washington, also saw success. A campaign delivered through messaging at taxi stands, at points of alcohol purchase, and in mass media significantly increased the use of designated drivers and taxis among the heaviest drinkers aged 21-34 (Rivara et al., 2011).
Despite the promising results of these campaigns, they may have unintended effects if inappropriate message formats are used. A group of college students that viewed fear-based public service announcements on distracted driving (such as talking on a cell phone, texting, or eating) reported significantly higher intentions to engage in the distracting behaviors after viewing the videos, indicating a boomerang effect (Lennon et al., 2010). The authors caution that fear-based messages may encourage young adults to behave in the opposite way from what is advocated in the message.
Many states are using graduated driver licensing (GDL) systems. Yet the results of a recent study indicate that some of the lives saved by GDL among 15- to 17-year-old novice drivers are offset by associated increases in fatal crashes among 18- to 19-year-old drivers (Fell and Romano, 2013). The reasons for this finding are unclear. It could be due to (1) novice 18- to 19-year-olds beginning to drive without the protective framework of a GDL program as a result of delaying licensure in the “good” GDL states5; (2) increased risk taking behaviors by 18- and 19-year-old drivers (e.g., impaired driving, late night driving, driving with teen passengers, lack of seat belt use, distracted driving); and/or (3) lack of exposure to risky situations (e.g., late night driving, driving on high-speed roads) among 18- to 19-year-old drivers in the good GDL states because of the protection from these situations when they were 16 and 17 years old (Fell and Romano, 2013). Further research is required to clarify the finding that those who seek a license in their young adult years actually endanger themselves even more as they lack the checks and family oversight of younger drivers.
Most individual-level driving safety interventions currently focus on educating novice drivers during the high school years as they gain their permit for the first time, often involving parents (Ramirez et al., 2013; Zakrajsek et al., 2013) and working within driver education classes (Zakrajsek et al., 2013). Relatively fewer studies have focused on the driving behaviors of young adults, using various tactics to reduce risky and distracted driving behaviors. An in-car education program involving 23 young men with a history of challenging driving behavior provided coaching sessions and in-car
__________________
5 The Insurance Institute for Highway Safety rated a GDL law “good” if it had five or more of the following components: minimum learner’s permit age, mandatory waiting period before applying for an intermediate license, minimum hours of supervised driving, minimum age for an intermediate license, nighttime restriction, passenger limitation, and minimum age for full licensing (Fell and Romano, 2013).
feedback by a monitoring system. The program significantly improved driving skills in the intervention group, leading to positive changes in tailgating and unofficial races with other cars (Tapp et al., 2013). However, other studies with young adults have not shown the same success during actual time on the road. For example, teaching strategies using computer-based training modules to prevent distraction led to a decline in the intervention group’s willingness to engage in distracting activities and an increase in perceived risk, but no benefits were seen when the car was in motion (Horrey et al., 2009). Furthermore, a 20-hour prevention program for youth with multiple traffic citations showed no significant change in high-risk traffic behaviors and traffic citations compared with the control group, highlighting the need for further development of behavioral interventions to address high-risk driving behaviors (Nirenberg et al., 2013).
In summary, successful campaigns promoting motor vehicle safety have combined mass media messaging with legal enforcement, often engaging social networks to amplify the message and change norms. Single-component approaches and short-term campaigns have limited impact on intended outcomes.
Multiple Risk Behaviors
In addition to interventions addressing one or a set of related risk behaviors, there may be merit in multicomponent interventions that target various risk behaviors (Jackson et al., 2012). Such interventions may reflect the environmental approach needed to address the multiple transitions young adults experience, and may help focus on building resilience to adversity during these transitions by addressing multiple domains of risk and protective factors (Jackson et al., 2012). For example, a brief intervention among college students consisted of a one-on-one consultation featuring gain- and loss-framed messages tailored to students’ specific behaviors, followed by a goal-setting session. This intervention led to significant increases in health-related quality of life, fewer days of poor spiritual health, moderate exercise, and fewer days of driving after drinking compared with controls (Werch et al., 2010). Brody and colleagues (2010) focused on the period leading into the young adult years among African American students in rural counties who were in the past year and a half of secondary school, using a family-based intervention to increase the ability to cope with life stressors associated with the transition to adulthood. The intervention was found to buffer stress and increase resilience, leading to significant decreases in risk behaviors such as marijuana use, alcohol use, and risky sex among the intervention group compared with controls.
Lessons Learned
Although strategies and findings vary by priority area, some overall conclusions can be drawn from this brief review. First, the available evidence provides grounds for systematically investigating the potential utility of multifaceted health and safety campaigns targeting young adults. Single-component interventions focusing on one level, in general, have limited, short-term effects. Evidence of effectiveness as measured by health or safety outcomes at the population level (rather than solely by modification of individual-level beliefs, attitudes, or intentions) is weak for stand-alone interventions in many of the domains with particular application to young adults. By contrast, in the few health areas in which multilevel interventions have been used, the positive effects tend to be larger and long-lasting. Most community-based campaigns have used media but also sought to mobilize different sectors to create environmental and policy supports to facilitate healthy behaviors. Such intersectoral mobilization is exemplified by campaigns on tobacco use, HIV, and youth abuse of alcohol (Ramanadhan et al., 2012; Valente et al., 1993), among other areas. Law enforcement and repeated short-term mass media exposure also appear to be important components of motor vehicle safety campaigns.
Second, the most successful interventions have been those that involve comprehensive, multilevel community initiatives using ecological approaches to influence changes at the individual, organizational, and societal levels, sustained over time through a variety of channels and venues. Community and stakeholder engagement is critical to the sustained effectiveness of interventions. Many successful public health campaigns include such approaches as community-engaged social change and community-based participatory research (Koh et al., 2011; Minkler and Wallerstein, 2008).
Third, and related to the first two points, the most robust effects have been seen in those areas in which policy makers and researchers have collaborated to address the problem and evaluate interventions and, as a result, in which the most experience and evidence have been accumulated.
Fourth, a major limitation of current studies of young adults is that they have largely involved samples of university students. The focus on this population does not fully represent how young adults who do not attend college experience the transition after high school. Given the inequalities between youth and young adults from different socioeconomic and racial and ethnic groups, more information on how to develop and deploy robust interventions among noncollege youth are sorely needed. In particular, rigorous trials using standardized measures are needed so behavioral outcomes can be compared across groups.
This point is related to a broader concern—that public health campaigns that are media based or include a media component are less likely
to benefit people from disadvantaged socioeconomic and racial and ethnic groups, a phenomenon characterized as communication inequalities (IOM, 2006; Link and Phelan, 1995; Viswanath, 2006; Viswanath et al., 2013). The reasons for these health campaign inequalities are many, including a lack of access to media; a lack of attention; the complexity of the messages and practices recommended; and the economic, environmental, and social barriers to acting on messages. These inequalities in campaign effects offer a partial but robust explanation for the challenges encountered in attempting to eliminate or ameliorate health inequalities so well documented in the literature (Kawachi and Berkman, 2001; Link and Phelan, 1995; Marmot, 2013; WHO, 2001). It is worth noting, however, that these gaps are less likely to be seen when public health interventions and media campaigns focus explicitly on using strategies to reach different social groups, including minorities and those of lower socioeconomic position.
SOCIAL MEDIA AND THE HEALTH OF YOUNG ADULTS
Social media play an increasing role in curating information and driving audiences. Among those aged 18-29, for example, 97 percent use the Internet, 98 percent have a cell phone, and 83 percent have a smartphone, although income, urbanicity, and education are strongly associated with this phenomenon (Fox and Lee, 2014). More than 70 percent of Internet users use social media, with this number rising to 84 percent among those aged 18-29 (Duggan and Smith, 2013).
At the same time, a steady erosion in audiences for traditional media has occurred. In a Pew survey of online news consumption, for example, 39 percent of respondents reported getting news online—19 percent from social media, 16 percent from email, and 8 percent from podcasts (Pew Research Center, 2013). More germane, 60 percent of those in younger age groups rely on digital sources for their news. And more than one-third of youth aged 18-24 get their news from social media. Ownership of mobile devices, such as mobile phones and tablets, has actually increased news consumption, with people accessing information from multiple platforms (Pew Research Center, 2014). In line with this phenomenon, social media have emerged as key platforms for participation and engagement, particularly among youth.
In light of this dramatic transformation in information and communication technologies and their adoption among youth, it is important to explore the implications of these developments for public health. Social technologies afford new opportunities to reach out to and stay connected with young adults. Social and mobile media, in particular, provide a variety of contexts through which young adults can learn about, contribute to, and engage with developing narratives about public health. These media amplify
points of connection with young adults, and they enable broad, rapid, and convenient access to information and a variety of relational interfaces.
The empirical evidence for successful deployment of social media to promote health is nascent, and much of the literature is replete with commentaries and speculation. As these media become more ubiquitous, however, they increasingly are being incorporated into interventions. As the leading social networking site in the United States (Duggan and Smith, 2013), Facebook has been used to promote a number of healthy behaviors among young adults (Carrol and Kirkpatrick, 2011), but with mixed results. Exposure to a Facebook page delivering STI prevention messages to young adults in the community, for example, resulted in increased condom use at 2 months postintervention, although these results were not sustained at 6-month follow-up (Bull et al., 2012). In another study involving college students, using the private message function of Facebook to deliver social norms feedback successfully corrected misperceptions about drinking, reducing the amount and frequency of alcohol consumed postintervention and at 3-month follow-up (Ridout and Campbell, 2014). Enrollment in a Facebook group had no significant effect on increasing physical activity among a group of female undergraduate students (Cavallo et al., 2012). However, Napolitano and colleagues (2013) found significantly greater weight loss among college students exposed to a Facebook Plus intervention group (access to a weight loss–focused Facebook page plus goal setting, self-monitoring, and social support) compared with Facebook-only and control groups. This finding suggests that weight loss material delivered through a social networking platform alone may not be sufficient to effect changes in behavior.
“In college, lack of sleep is bragged about; if you get less sleep, you’re working harder. Until the culture changes, a health campaign isn’t going to make a difference.”
A systematic review of the use of online social networks for interventions focused on weight loss and physical activity among participants of all ages found that 9 of the 10 articles included in the review reported significant improvements in these behaviors, albeit with small effect sizes (Maher et al., 2014). However, a meta-analysis by Williams and colleagues (2014) found no effects of the use of social media on weight or physical activity levels, citing problems with recruitment, retention, and poorly reported methods among reviewed studies. A systematic review of sexual health interventions among young adults also revealed a lack of evidence for the impact of social media on behavior. While interventions using social media or
text messages were found to significantly increase knowledge of STIs among samples of young adults, the evidence for impact on reducing sexual risk behaviors and increasing STI testing was mixed (Jones et al., 2014). Studies emphasize that this field of research is in its infancy, and future studies need to use high-quality research methods and large samples and determine how behavior change can be sustained over time to fully understand the promise of this widely used resource for health behavior change.
Based on experiences from other fields and data from current use, it is possible to formulate some hypotheses about the use of social media for public health interventions. We emphasize that these are hypotheses only that warrant more systematic testing in further research.
First, unlike traditional mass media, social technologies afford two- and multiway communication among audiences, especially when the members know each other or share some common interests. The open-ended opportunity for engagement may facilitate personal contributions or the tailoring of campaign content, which is known to result in a stronger impact on outcomes.
“A lot of young adults and teens don’t want to trust adults; they want to experiment and experience things themselves. Think about a way to give them the experience without actually giving them the experience.”
Second, social media may allow public health campaign planners to take advantage of the memetic potential for virality embedded within socially oriented technology. Several contemporary health campaigns are premised on the engagement principle, with the Avatars Anonymous project being an example of how health avatars can be personalized to convey health messages more effectively (Wood, 2014). Unlike traditional media, which access people as passive interlocutors, social and mobile media provide opportunities to turn passive audiences into active content producers. By “flipping” traditional roles, social and mobile media suggest new ways of engaging the target audience with public health campaigns. Because of its potential for engagement, the flipping model has become popular in redesigning educational experiences. In the health care and public health sector, the Flip the Clinic model,6 supported by the Robert Wood Johnson Foundation, is an example of interactive learning and active engagement with routine health care processes. Whether “flipping,” in either classroom
__________________
6 See http://fliptheclinic.org/about (accessed October 22, 2014) for details on the Flip the Clinic project.
or clinical settings, is more effective than traditional approaches has yet to be empirically documented.
Third, the storytelling tradition is embedded in a range of cultures, and commercial advertisers often have resorted to this strategy to sell products and services. In social change programs, including those focused on health, narratives and exemplars are frequently used to promote change. Narratives offer both negative and positive examples of influence on health behaviors. Several studies have documented, for example, that exposure to depictions of tobacco use in movies is strongly related to both initiation and sometimes continued smoking among youth in the United States (Dalton et al., 2009; NCI, 2008) and young adults and adults in India (Viswanath et al., 2010a). On the other hand, narratives have also been used to help smokers quit smoking (Strecher et al., 2008). Using social and mobile media to support storytelling invites others to connect with the stories emotionally through the process of adding to, remixing, and reproducing them. This sustained loop of engagement could potentially create a sense of community supportive of health and well-being, a key element in new public health strategic directions.
“Messages aren’t successful when young adults are told what to do. We want to be autonomous, and we want to be treated in a respectful way. Presenting messages in a way that gives young adults the power to choose will be successful.”
Fourth, social and mobile media augment points of connection among people, networks, and information. They connect disparate and overlapping networks in ways that sustain existing and enable new connections. In this way, they offer networked “neighborhoods” more accessible to a variety of people than physical places where people traditionally have convened.
Overall, use of social and mobile media appears to hold promise for reaching young adults with public health campaigns. However, the effectiveness of these new technologies in fulfilling this promise has yet to be established. Studies indicate that going beyond the provision of information to include skill-based components may yield the greatest success (Jackson et al., 2012).
PROTECTIVE PUBLIC POLICIES FOR YOUNG ADULTS
Legislatures and public health agencies often adopt protective policies focused on young adults. They may do so for a variety of developmental
and behavioral reasons. For example, some risky behaviors that are permitted for adults pose a heightened risk to young people because of the shortsightedness, impulsivity, or other deficits in mature judgment and decision making that often characterize this age group. Legal restrictions are designed either to delay these behaviors until young people mature or to allow a transition period for training and experience. Legal permission to use alcohol and tobacco, to drive a motor vehicle, and to use firearms offers the most pertinent examples.
A key policy issue in all these contexts is where the line should be drawn in formulating these “wait” rules. As discussed in Chapter 2, some of the key policy-relevant features of adolescence, including sensation seeking, impulsivity, and shortsightedness, persist into the early 20s, and there are of course substantial individual variations above and below 18. Although 18 may be a sensible point at which to demarcate the generic “age of majority” for most legal purposes, drawing this line in each setting ultimately requires contextualized value judgments. In the present context, protecting young people from taking unreasonable risks must be balanced with respecting their right to direct their own lives. Cognitive and emotional factors that may affect the maturity of judgment exercised by adolescents and young adults will vary in different social contexts, as will the health and safety consequences of setting the “legal age” at one point or another. It may be sensible to draw the line lower in some health and safety contexts (e.g., obtaining a license to operate a motor vehicle) and higher in others (e.g., lawful access to alcohol) (Bonnie and Scott, 2013; NRC and IOM, 2004).
In recent years, the trend in the United States has been to take a more protective stance toward older adolescents and young adults, a trend that is reinforced by the prolonged transition to economic and social independence described in Chapter 2. In the public health context, this trend is most clearly evident in legislation setting the minimum age for purchasing alcohol, marijuana, and tobacco, and heightened by increasing concern about commercial targeting of young people by manufacturers of these products.
Age of Purchase for Alcohol, Marijuana, and Tobacco
After the repeal of Prohibition in 1933, the vast majority of states set the minimum drinking age at 21. However, when the national voting age was set at 18 by the 26th Amendment in 1971, 29 states changed the drinking age to 18, 19, or 20, which led to a dramatic increase in motor vehicle fatalities related to alcohol among 18- to 20-year-olds (Wagenaar and Toomey, 2002). Many states then raised the minimum age to 21, and a robust literature showed that alcohol-related fatalities declined. In 1984, Congress induced all states to restore the minimum age to 21 by threatening to withhold a percentage of highway funds from noncompliant states (NRC
and IOM, 2004). Subsequent studies showed significant decreases among young people in fatal and nonfatal motor vehicle crashes and alcohol-related crashes and arrests (NRC and IOM, 2004). In a comprehensive report published in 2004, the National Research Council (NRC) and the Institute of Medicine (IOM) proposed a strategy for reducing underage drinking and driving based on the idea that, in a world where alcohol is so widespread and aggressively promoted, reducing drinking by adolescents and young adults is a “collective responsibility.” Parents and other adults must take the law seriously instead of accepting the idea that teen drinking is a rite of passage to adulthood (NRC and IOM, 2004). Moreover, given the widespread availability of alcohol and easy access by underage drinkers, minimum drinking age laws must be enforced more effectively, along with social sanctions. The effectiveness of underage drinking laws could be enhanced through such approaches as compliance checks, server training, zero tolerance laws, and GDL laws (NRC and IOM, 2004).
Notwithstanding the NRC and IOM report’s reaffirmation of the wisdom of setting the minimum drinking age at 21, political efforts are occasionally launched to reduce the minimum drinking age to 18 or 19. Yet a recent literature review reinforces the point that establishing 21 as the minimum drinking age has decreased “alcohol-related traffic crashes and alcohol consumption among youth, while also protecting drinkers from long-term negative outcomes they might experience in adulthood, including alcohol and other drug dependence, adverse birth outcomes, and suicide and homicide” (Dejong and Blanchette, 2014, p. 113). The U.S. Task Force on Community Preventive Services recommends implementing and maintaining a minimum drinking age of 21 based on strong evidence for the effectiveness of doing so, which includes a median 16 percent decrease in underage motor vehicle crashes in states that increased the legal drinking age to 21 (Shults et al., 2001).
The alcohol experience appears to have guided policy makers in states that have chosen to legalize marijuana, where the age of purchase has uniformly been set at 21. Although marijuana policy has been highly controversial since the 1960s (Bonnie and Whitebread, 1974), recent developments have fundamentally changed the regulatory landscape and are likely to have profound effects on the epidemiology of marijuana use (IOM, 1999). The voters of California legalized medical use of marijuana in 1996, and analogous laws have been enacted by more than 20 other states (NCSL, 2014).
Colorado and Washington voters approved initiatives legalizing recreational marijuana use for people over 21 in 2012 and directing state legislatures to license the cultivation and distribution of marijuana and impose taxes on marijuana transactions (American Psychiatric Association, 2014). Although the cultivation, distribution, and possession of marijuana for either medical or recreational purposes remain illegal under federal law,
the U.S. Department of Justice has promulgated enforcement guidance to the U.S. Attorneys. That guidance allows for declining to enforce the Controlled Substances Act against persons who comply with the requirements of state law as long as the conduct allowed by the states does not endanger overriding federal interests, such as preventing “distribution of marijuana to minors” and “drugged driving and the exacerbation of other adverse public health consequences associated with marijuana use” (Cole, 2013).
Many questions remain unanswered about the effects of marijuana, especially when used in high-potency preparations. Public health concerns focus on the onset of dependence during adolescence and young adulthood, possible damaging neurodevelopmental effects, and increased risk of psychosis in psychologically vulnerable youth (Volkow et al., 2014). A key question raised by the legalization debate is how different approaches to legalization are likely to affect the prevalence and patterns of marijuana consumption and the extent to which marijuana will be used as a substitute for alcohol. However marijuana policy unfolds, the committee assumes that policy makers will take meaningful steps to discourage its use among youth below the age of purchase, which is nearly certain to be at least 21, and that state and federal public health agencies will establish the surveillance systems necessary to monitor patterns of consumption and the effects of policy changes on the public’s health.
The age of purchase for tobacco products also has come under scrutiny. Until the 1990s, the minimum purchase age (typically 16) varied substantially from state to state and was rarely enforced anywhere. In 1992, Congress enacted legislation (known as the Synar Amendment) tying state eligibility for substance abuse prevention and treatment block grant funds to enforcement of youth tobacco access laws, and reports published by the surgeon general (CDC, 1994) and by the IOM (1994) 2 years later highlighted the importance of reducing youth initiation of smoking as a priority component of state tobacco control. In 1996, the U.S. Food and Drug Administration (FDA) promulgated its Tobacco Rule, establishing a federal minimum purchase age of 18 and restricting tobacco advertising and promotion targeting adolescents (Redhead and Burrows, 2009). Although the Supreme Court invalidated the Tobacco Rule in 2000,7 Congress revived it in the Family Smoking Prevention and Tobacco Control Act of 2009,8 and the FDA reissued the rule in 2010. While codifying 18 as the federal minimum age of purchase, Congress authorized the states to adopt a higher minimum purchase age and directed the FDA to assemble an expert panel to assess the public health implications of increasing the minimum purchase
__________________
7Food and Drug Administration, et al. v. Brown & Williamson Tobacco Corp., et al. 529 U.S. 120, 2000.
8 Public Law 111-31, 111th Cong. (June 22, 2009).
age for tobacco products. At the FDA’s request, the IOM has convened a panel to assess the effects of raising the minimum age to 19, 21, or 25, and the panel’s report is expected in 2015.
Advertising and Promotion of Alcohol, Marijuana, and Tobacco
Recent consideration of marijuana legalization has drawn attention to the challenge of designing a regulatory structure that will adequately protect the public health (American Psychiatric Association, 2014). The shortcomings of current regulatory approaches to alcohol and tobacco are mentioned prominently in the policy debate (Bonnie, 2014), and attention has focused particularly on the effects of advertising and promotional activities targeting young adults. While a review of the effects of advertising and promotion on young adults is beyond the scope of this study, a substantial body of research has accumulated on the exposure of young adults to alcohol advertising, the increasing number of tobacco promotions targeting young adults, the intertwining of alcohol and tobacco advertising, and the rapid acceleration of marijuana advertising in Colorado (Pacula et al., 2014; Richardson et al., 2014; Sepe and Glantz, 2002; Smith and Foxcroft, 2009).
IMPROVING AND COORDINATING PUBLIC HEALTH PROGRAMS
This section examines state and federal public health programs to ascertain whether and to what extent they focus on key issues, such as those presented earlier in Box 6-2, that are relevant for young adults. Although relatively good epidemiological surveillance data are available for many of these issues, information is rarely adequate for evaluating the effectiveness of programs and policies specifically for young adults. This is the case because, while a variety of public health programs and policies have been implemented to improve overall population health, specific data have not been available on whether they have adequately reached young adults and with what effects, or subanalyses of this particular age group have not been conducted. As discussed in Chapter 2, young adults have developmentally distinct characteristics that may require strategies different from those used for children, adolescents, or older adults. Additionally, programs and policies often have been shaped by the needs of distinct groups, as well as resource limitations, resulting in the development of specific eligibility requirements—for example, those at greatest risk of HIV/AIDs. The consequence has been a siloed approach to population health that fails to reflect the fact that the same young adult may be engaged in multiple risk behaviors, such as substance abuse and unprotected sexual activity.
Coordination of State and Local Public Health Programs
The IOM’s influential report on the future of public health (IOM, 1988) identifies three core functions performed by state and local public health departments: (1) assess the health of the community (assessment), (2) lead and promote evidence-based policies that are in the public’s interest (policy development), and (3) ensure the availability of community and personal health services that are viewed by constituents as appropriate and necessary (assurance). Building on that foundation, recent IOM reports (e.g., IOM, 2011) have endorsed a list of the 10 essential public health services displayed earlier in Box 6-1, which provide the foundation for state and local public health systems that play a lead role in ensuring the delivery of public health services (IOM, 1988, 2003).
The U.S. public health system is made up of 51 state,9 2,794 local, and 565 American Indian and Alaska Native tribal public health agencies (Hyde and Shortell, 2012; NACCHO, 2009). The scope of these agencies’ duties and authorities and the agencies’ organizational structure vary among states (IOM, 2003). Virtually all state public health agencies provide immunizations, conduct infectious disease control and reporting, provide health education, and maintain health statistics (IOM, 2003). At the local level, local health departments are involved in various activities related to public health, such as population-based primary prevention services, immunization, and maternal and child health services. Research describing how these services are delivered is limited (Hyde and Shortell, 2012).
Funding for public health services at the state and local levels comes from a mix of federal, state, local, and private monies. In 2008, about 50 percent of state agency funding came from federal grants, contracts, and cooperative agreements; 24 percent from state general funds; and 26 percent from other sources (ASTHO, 2009). At the local level, in 2007, 25 percent of funds came from local contributions, 20 percent from state contributions, 17 percent from federal pass-through funding, 15 percent from Medicaid and Medicare reimbursements, and 11 percent from fees (NACCHO, 2009). Sources of funding vary widely at both the state and local levels, and agency activities are typically fragmented and siloed, depending on the funding stream. For example, many grantees of the federal Title X Family Planning Program administered by the Office of Family Planning face numerous challenges impacting their ability to provide family planning services because of management and administrative burdens, including funding limitations and increasing supply costs, as well as difficulty coordinating and managing multiple funding sources at the federal, state, and local levels (IOM, 2009). In addition, funding for public health infra-
__________________
9 Including the District of Columbia.
structure is chronically inadequate and tends to decrease during recessions, eroding the capacity of local health departments to provide essential community services (NACCHO, 2014a). Since 2008, local health departments have lost 48,300 jobs as a result of layoffs and attrition, and 36 percent of the population currently lives in a jurisdiction affected by budget cuts (NACCHO, 2014a).
Nonetheless, all state and local public health programs deal at some level with many of the public health priorities for young adults described in this chapter, including tobacco control, obesity prevention, injury prevention, and prevention of unprotected sexual activity. However, fragmentation of organizational structures contributes to inefficiencies and gaps in the performance of the core public health functions, weakening responses to the needs of young adults (among other groups). For instance, the administration of different funding streams, each with its own priorities, eligibility requirements, and scope of work, carried out with little coordination or integration, results in programs reaching some groups of young adults but not providing a comprehensive approach when they are reached, while other young adults may not receive any of the services they need. Thus, for example, young adults may have access to reproductive health services offered through health departments, but may not receive screening for obesity and diabetes. These lost opportunities to take a more comprehensive approach contribute to unevenness in service provision. Furthermore, given the resources available, many young people may not have had the opportunity to access health services—either because their local jurisdiction does not make services available; because eligibility requirements preclude their access to care; or because they lack information about available resources, such as screening for STIs through public health clinics.
States have recognized the importance of integration of services for adolescents, and many state public health agencies have created adolescent topic areas or designated state adolescent health coordinators to help coordinate health programs and policies bearing on the health, safety, and well-being of adolescents (SAHRC, 2012). For example, a number of states have developed comprehensive adolescent health plans to help bring together different funding streams. Most public health departments have had an adolescent health coordinator position over the past 20-30 years, and these coordinators were initially supported directly as part of the Title V Maternal and Child Health (MCH) Block Grants to States Program. Many coordinators continue to work within Title V programs; as state funding and public health structures have changed, however, many are now funded through other divisions within public health agencies, such as family planning and chronic disease divisions.10 As of June 1, 2014,
__________________
10 See http://nnsahc.org/images/uploads/1-_AHC_Overview.pdf (accessed October 22, 2014).
all states except Alaska, Montana, North Dakota, Tennessee, Utah, and Virginia and the District of Columbia had an adolescent health coordinator in place (SAHRC, 2014). The coordinators’ position and role vary greatly by state with respect to their responsibilities and areas of focus, but all are committed to improving the health, safety, and well-being of adolescents (NNSAHC, 2012). In 2012, 54 percent of state adolescent health coordinators had worked in adolescent health and 66 percent in public health for more than 11 years, and 20 percent for more than 20 years. Most take a broad approach to their work, with 64 percent focusing mainly on youth development, 52 percent on general adolescent health, and 38 percent on building health systems for adolescents; more than one-third have engaged adolescents in some way in their work (NNSAHC, 2012).
Very few states have implemented a similar approach for young adults, although some have extended the adolescent health coordinator’s role to include young adults. One example is Maine, whose program encompasses ages 10-24 and focuses on the issues of health service access and education and youth development, with the vision that all the state’s youth will be healthy, safe, and respected (King, 2014). In Texas, beginning in fiscal year 2015, contractors will be able to serve young adults up to age 24 in their programs. Contractors must select at least one of eight risk areas (motor vehicle safety, juvenile delinquency, substance abuse, dating violence, obesity, mental health issues, HIV/STIs, and access to care) on which to focus their activities. They are also required to facilitate a Youth-Adult Council (ages 12-24) to help guide their program development and incorporate a positive youth development framework.11
Two statewide innovations merit careful review and consideration by other states. In Colorado, the public health department convened Colorado 9to25, a partnership of more than 200 organizations, to promote the health, safety, and well-being of youth aged 9-25 (see Box 6-4). And in Maryland, the governor convened an interagency activity—the Transition Age Youth Initiative—to focus on the transition needs of young adults with intellectual disabilities or behavioral health problems (see Box 6-5).
Federal Public Health Programs
Compared with state and local government agencies, the federal government has a limited role in delivering public health services. “Nevertheless, it plays a crucial role in protecting and improving the health of the population by providing leadership in setting health goals, policies, and standards, especially through its regulatory powers” (IOM, 2003, p. 111),
__________________
11 Personal communication, Carol Harvey, Office of Title V & Family Health, Texas Department of State Health Services, July 17, 2014.
BOX 6-4
Convening by the Public Health Department: Colorado 9to25
Colorado 9to25 (CO9to25) is an innovative partnership of youth and adults in Colorado aimed at ensuring that youth aged 9-25 (1) are safe; (2) are physically and mentally healthy; (3) receive a quality education; (4) are connected to caring adults, schools, and their communities; and (5) are contributing to their community (e.g., volunteering, working). CO9to25 is convened by the state’s public health department but brings together more than 200 state, local, private, nonprofit, and for-profit organizations to work to improve programs, practices, and policies that impact the health, safety, and well-being of youth. The program recognizes that youth experience difficulties during various transition periods in their lives that can lead to dangerous and unhealthy risks and habits, so the goal of the program is to provide resources and connect youth to statewide initiatives that impact their health and well-being. CO9to25 identifies state problems and then convenes youth, adults, and participating organizations to address them.
Although CO9to25 targets a broad age range, one program focus is on addressing the health needs of young adults as they transition between adolescent and young adult health systems. This work is conducted through social media, webinars, events, and training and by connecting individuals who work with young adults with special health care needs, those with behavioral health needs, those aging out of foster care and at risk of being homeless, and those graduating from high school or completing a General Educational Development credential who need extra learning supports. The program also is working on changing its partner organizations’ policies to enable the hiring of young adults as expert advisors instead of their serving in a more limited capacity as interns.
SOURCES: www.co9to25.org; Wood, 2014.
as well as in supporting research. It also contributes operational and financial resources necessary to increase the effectiveness of the public health infrastructure at the federal, state, and local levels (IOM, 2003).
Although few federal programs specifically target young adults, many programs can be utilized to improve the health, safety, and well-being of this population. Table 6-1 illustrates the broad range of current federal public health programs that affect young adults, although, as discussed below, specific data on how many young adults are being served by these programs are not readily available. This table is not exhaustive, but is intended to provide examples within various categories of public health (e.g., substance abuse, reproductive health).
Many programs specifically target adolescents (e.g., the U.S. Department of Health and Human Services’ [HHS’s] Adolescent Pregnancy and Prevention Grant Programs) or mothers and children (e.g., HHS’s Services
BOX 6-5
Convening by the Governor’s Office: Maryland Interagency Transition Council for Youth with Disabilities
Maryland’s efforts toward providing mental health services to youth and young adults (aged 16-25) initially started under the leadership of the Governor’s Office of Disabilities with the goal of establishing a statewide transition plan, the result largely of advocates representing the disability community. While the initial effort was built primarily around the disability community, mental health was added later on. This effort led to a governor’s executive order that established an Interagency Transition Council for Youth with Disabilities, with the Mental Health Hygiene Administration and mental health advocates as mandatory partners on the committee. This enabled services for individuals with developmental and intellectual disabilities to be extended to individuals with mental health issues, particularly youth and young adults with emotional and behavioral disabilities.
In 2007, the council was tasked with recommending policies and identifying funding requirements to meet the transition needs of all youth with disabilities within Maryland. Maryland’s Transition Age Youth (TAY) initiative was an effort to create a service delivery system for youth and young adults. It started with 12 TAY-specific programs provided through local mental health agencies in 2000; currently there are 24 programs, all tailored to the developmental needs of this population. Funding has come from the state, as well as federal and other resources. While most states situate these programs in the child and youth services division, Maryland’s programs are situated in the Office of Adult Services within the Mental Hygiene Administration. This was done intentionally to focus on adult indicators, such as having a job, affordable housing, and relationships with others, that typically are not measured in child and adolescent systems. The programs were designed to provide youth and young adults with skills and supports during the transition phase to minimize further involvement in the adult service system.
Programs leveraged existing services and resources and varied in scope, focus, age range (14-25), type of intervention, and service modality. As knowledge and experience working with this population developed, interventions were refined. Currently, Maryland is in the process of aligning all the services within the
Grant Program for Residential Treatment for Pregnant and Postpartum Women). While young adults meet some of these programs’ age eligibility requirements, evidence of whether tailoring has been used in the delivery of care or services has not been formally documented. One notable exception is incorporated as part of the National State-Based Tobacco Control Program, which aims to prevent adolescents and young adults from initiating tobacco use. It is also likely that some other programs, such as the family
various programs with the intent of developing expertise in empirically supported approaches that can be brought to scale and replicated statewide.
Key policy changes that have emerged from this initiative include the following:
- Eligibility for TAY was expanded to provide continuous, uninterrupted access to developmentally appropriate services across systems serving youth with disabilities and those with mental health issues so they do not drop off the eligibility cliff upon aging out of child and adolescent services.
- Since employment among this population is a predictor of postschool success, TAY programs were granted access to evidence-based practices supporting employment programs at age 16, prior to graduation from high school.
Many lessons have been learned from the TAY programs that could be useful for other state and local agencies and organizations. These include the following:
- The average length of TAY services is 2 years.
- Among 16- to 25-year-olds in TAY programs, 70 percent are employed, versus 46 percent of those involved in other services in the mental health system.
- The increased number of people eligible for Medicaid under the Patient Protection and Affordable Care Act and children in foster care being able to maintain Medicaid up to age 26 will likely create an increased demand for TAY services.
- Initiatives need to include employment and education as a point of entry to other mental health services.
- Coordination requires pooling of funding and resources among multiple systems of care across government agencies.
- Core competency training is needed for all staff involved in the provision of services.
SOURCE: Reeder, 2014.
planning services provided under Title X funding, which target primarily younger adults (51 percent of Title X clients are in their 20s), may use approaches best suited to young adults (Fowler et al., 2012).
Recently, the National Prevention Council released its Annual Status Report, which describes how federal government departments are collaborating in cross-sector efforts addressing prevention and health.12 Many of these strategies may impact the young adult population, but the report
__________________
12 See http://www.surgeongeneral.gov/initiatives/prevention/2014-npc-status-report.pdf (accessed October 22, 2014).
TABLE 6-1 Selected Federal Public Health Programs Relevant to Young Adults
| Policy/Program | Department/Agency | Population Served | Funding (from the Catalog of Federal Domestic Assistance)a (in millions) |
| FAMILY PLANNING, MATERNITY, PARENTING | |||
| Maternal and Child Health Services Block Grants to States | HHS/HRSA | Mothers and children and their families, especially low-income | FY12 $541 FY13 est. $512 FY14 est. $550 |
| Maternal and Child Health Federal Consolidated Programs | HHS/HRSA | Mothers and children | FY12 $128 FY13 est. $126 FY14 est. $128 |
| Affordable Care Act Maternal, Infant, and Early Childhood Home Visiting Program | HHS/HRSA | Mothers and children; eligibility categories include pregnant women under 21 | FY12 $309 FY13 est. $345 FY14 est. $345 |
| Adolescent Pregnancy Prevention Grant Programs | HHS/ACF | Varies by program but primarily 10- to 19-year-old youth and young adults at risk and vulnerable to pregnancy; some programs also include young parents up to 21 | FY12 na FY13 na FY14 na |
| Pregnancy Assistance Fund Program | HHS/Office of the Secretary | Pregnant and parenting teens and women; also supports fathers and families | FY12 $24 FY13 est. $22 FY14 na |
| Services Grant Program for Residential Treatment for Pregnant and Postpartum Women (PPW) | HHS/SAMHSA | Low-income women aged 18 and over who are pregnant or postpartum and their minor children aged 17 and under | Total funding available: $8,384,000 |
| Family Planning Services (provided under Title X) | HHS/Office of Population Affairs | Universal; priority to people with low income of reproductive age | FY12 $274 FY13 est. $245 FY14 na |
| Policy/Program | Department/Agency | Population Served | Funding (from the Catalog of Federal Domestic Assistance)a (in millions) |
| SEXUALLY TRANSMITTED INFECTIONS (STIs)/HIV | |||
| Ryan White HIV/AIDS Program | HHS/HRSA | Universal, all ages | FY12 $2,392,178,000 FY13 $2,248,638,000b FY14 na |
| HIV Prevention Programs for Women | HHS/Office of the Secretary | Women | FY12 $5 FY13 est. $4 FY14 na |
| DoD HIV/AIDS Prevention Program | DoD | Universal (includes international) | FY12 $28 FY13 est. $30 FY14 na |
| SUBSTANCE USE/ABUSE | |||
| Drug-Free Communities | HHS/SAMHSA | Universal | FY12 $84 FY13 est. $59 FY14 est. $39 |
| National State-Based Tobacco Control Programs | HHS/CDC | Universal; focus on youth and young adults | FY12 $0 FY13 est. $0 FY14 est. $58 |
| Tobacco Regulation Awareness, Communication, and Education Program | HHS/FDA | Universal; focus on youth | FY12 $0 FY13 est. $0 FY14 est. $0 |
| Drug Court Training and Technical Assistance | Executive Office of the President | Universal | FY12 $1 FY13 est. $1 FY14 na |
| Model State Drug Laws Initiative | Executive Office of the President | Universal | FY12 $1 FY13 est. $1 FY14 na |
| Veterans Rehabilitation Alcohol and Drug Dependence | VA Health Administration Center/Department of Veterans Affairs | Veterans | FY12 na FY13 na FY14 na |
| Policy/Program | Department/Agency | Population Served | Funding (from the Catalog of Federal Domestic Assistance)a (in millions) |
| CHRONIC DISEASE PREVENTION AND HEALTH PROMOTION | |||
| Centers for Research and Demonstration for Health Promotion and Disease Prevention | HHS/CDC | Universal | FY12 $30 FY13 est. $21 FY14 est. $20 |
| INJURY PREVENTION AND CONTROL | |||
| Injury Prevention and Control—Research and State and Community Based Programs | HHS/CDC | Universal | Cooperative agreements: FY12 $70 FY13 est. $68 FY14 est. $71 Project grants: FY12 $12 FY13 est. $11 FY14 est. $11 |
| MOTOR VEHICLE SAFETY | |||
| State and Community Highway Safety | DOT/NHTSA | Universal | FY12 $235 FY13 est. $235 FY14 est. $235 |
| Alcohol Impaired Driving Countermeasures Incentive Grants I | DOT/NHTSA | Universal | FY12 $139 FY13 est. $0 FY14 est. $0 |
describes only one effort specifically targeting young adults—the launch of HHS’s partnership with the American College Health Association and the University of Michigan, which supports the Tobacco-Free College Campus initiative. This initiative resulted in increasing the number of designated smoke-free campuses from 774 to 1,342. The rest of the programs included in the report do not specifically mention young adults, although several federal public health programs (e.g., the Maternal and Child Health Services Block Grant Program, the Ryan White HIV/AIDS Program, Federally Qualified Health Centers) deal with many of the key issues impacting young adults listed earlier in Box 6-2 (see Box 6-6). A similar pattern can be seen at the state and local levels, where, as discussed earlier, numerous public health programs are relevant to young adults.
| Policy/Program | Department/Agency | Population Served | Funding (from the Catalog of Federal Domestic Assistance)a (in millions) |
| Occupant Protection Incentive Grants | DOT/NHTSA | Universal | FY12 $25 FY13 est. $0 FY14 est. $0 |
| Alcohol Open Container Requirements | DOT/NHTSA | Universal | FY12 $115 FY13 est. $0 FY14 est. $0 |
| Incentive Grant Program to Increase Motorcycle Safety | DOT/NHTSA | Universal | FY12 $7 FY13 est. $4 FY14 est. $0 |
| NHTSA Discretionary Safety Grants | DOT/NHTSA | Universal | FY12 $7 FY13 est. $0 FY14 est. $0 |
| National Priority Safety Programs | DOT/NHTSA | Universal | FY13 est. $265 FY14 est. $272 |
NOTES: ACF = Administration for Children and Families; CDC = Centers for Disease Control and Prevention; DoD = U.S. Department of Defense; DOT = U.S. Department of Transportation; FDA = U.S. Food and Drug Administration; HHS = U.S. Department of Health and Human Services; HRSA = Health Resources and Services Administration; na = not available; NHTSA = National Highway Traffic Safety Administration; SAMHSA = Substance Abuse and Mental Health Services Administration.
a For most programs, three fiscal years of funding is available in the Catalog of Federal Domestic Assistance.
b See http://hab.hrsa.gov/data/reports/funding.html (accessed October 22, 2014).
The committee found that in most cases, the number of young adults being served by each federal program is not reported as a separate category, reflecting the fact that young adults are not consistently identified as a group with their own set of health conditions, risk factors, and needs. Nor is evidence available on whether programs tailor their efforts to different developmental ages and whether these modifications result in improved outcomes. Moreover, age data are reported differently for each program. As noted throughout this report, young adults should not automatically be combined with adolescents and older adults in public health programs. Breaking down data collection and analyses by adolescents, young adults, and older adults, as well as by gender and race/ethnicity, wherever possible, would help in assessing whether strategies and interventions are
BOX 6-6
Young Adults in Federal Programs: Examples from the Health Resources and Services Administration
The examples below provide a summary of how young adults are currently included in several key public health programs within the Health Resources and Services Administration (HRSA).
Title V Maternal and Child Health Services Block Grant Program (HRSA Title V)
HRSA provides services to mothers, pregnant women, infants, children and youth (including children and youth with special health care needs), and their families by funding states through its Title V program (HRSA, 2014d). Programs range from those that have produced clinical guidelines for child health supervision from infancy through adolescence, standards for prenatal care, and health safety standards for out-of-home child care facilities, to those that are focused on nutrition care during pregnancy and lactation and the incorporation of childhood injury prevention strategies (HRSA, 2000).
Young adults can receive services and support through HRSA’s Title V program under the “child” or “mother” category. Title V defines individuals as children until they turn 22. Within that parameter, however, each state can specify how “children” are defined for the purposes of its own block grant program. In Maine, for example, children are defined as ages 1 to 19, but in Louisiana, they are defined as ages 1 to 14. Only Connecticut defines children as up to 22 years of age (HRSA, 2014e). These varying definitions represent states’ decisions regarding the population for which they are willing to provide benefits, with states and jurisdictions being required to match every $4 of federal Title V money received with at least $3 of state and/or local money. This matching results in more than $6 billion available annually for maternal and child health programs at the state and local levels (HRSA, 2014d). This state-level variability contrasts with the provision of the Patient Protection and Affordable Care Act that enables children to remain on their parents’ health insurance plan until age 26 (KFF, 2011).
Ryan White HIV/AIDS Program
The Ryan White HIV/AIDS Program works with cities, states, and local community-based organizations to provide HIV-related services to more than half
being modified for different developmental age groups, whether diverse eligible populations are actually being served, and what outcomes are being achieved by age group.
Finally, the federal Maternal and Child Health Bureau has established an Adolescent and Young Adult Health Program. This program is designed “to promote comprehensive healthy development, health, safety, and well-being of adolescents and young adults . . . by strengthening the abilities of
a million people each year. The program serves those who lack sufficient health care coverage or financial resources for coping with HIV disease (HRSA, 2013), thus filling gaps in care not covered by other sources. The program reaches an estimated 529,000 people, 7 percent of whom are aged 13-24 and 41 percent of whom are aged 25-44, and program components are designed to serve youth (HRSA, 2012, 2013).
In addition to the Ryan White Program, HRSA’s HIV/AIDS Bureau supports a range of activities addressing the needs of HIV-positive youth. These include research initiatives and evaluations of innovative models of care focused on HIV-impacted youth, including women of color and young men who have sex with men (HRSA, 2012). In addition, HRSA is working to reduce barriers to early HIV identification and ensure access to health care, as well as engaging in other efforts, including community collaborations with national organizations, such as the National Minority AIDS Council and HealthHIV, that are addressing HIV among youth (HRSA, 2012).
Federally Qualified Health Centers
Federally Qualified Health Centers (FQHCs) are community-based organizations that serve medically underserved areas and/or vulnerable populations to improve public health. In 2012, these HRSA-supported health centers served more than 1 million homeless individuals, more than 900,000 agricultural workers and their families, more than 200,000 individuals in public housing, and almost 7,000 Native Hawaiians (HHS, 2014a).
In 2012, FQHCs served more than 3,700,000 patients aged 18-29, representing 18 percent of their patient population. In addition, approximately 166,000 patients aged 18-29 were served by federal Look-Alikes, representing 17 percent of their patient population (HRSA, 2014b,c).
The U.S. Department of Health and Human Services recently announced the availability of an additional $100 million (under the auspices of the Affordable Care Act) that will support an estimated 150 new FQHC sites in 2015, an expansion intended to increase access to health care in communities with the greatest need for services (HHS, 2014b). The expansion does not specifically target young adults, but if the patterns described above persist, nearly one in five new patients served will be in this age group.
[Title V programs] as well as of public health and clinical health professionals, to better serve these population groups, which range in age from 10 to 25 years” (HRSA, 2014a). The program is an example of a formal effort to recognize young adults as a separate population with their own needs. However, it represents only a small component of public health systems’ response to the needs of this population. Where necessary, new data collection efforts, disaggregated by these age groupings and other identifiers, are warranted to support improvements in public health programs and
campaigns aimed at improving the health, safety, and well-being of young adults.
Preventive Care Opportunities Under the Affordable Care Act
The Patient Protection and Affordable Care Act (ACA) includes numerous provisions intended to increase access to preventive health care, focused at both the individual and population levels. The architects of the ACA recognized the need for population-level investments that can help modify the environments that are the contexts for public health, as well as reinforce the act’s individual preventive focus. The ACA increases incentives for adminstering preventive care and financially supports primary prevention initiatives of communities and public health agencies. The Prevention and Public Health Fund (PPHF), for example, while not specifically focused on young adults, is used to support community and clinical prevention programs, strengthen the public health infrastructure and workforce, and expand public health research and tracking efforts (APHA, 2013). Yet while the ACA includes commitments to prevention, through both an emphasis on the provision of clinical preventive services (see Chapter 7) and the PPHF, the federal government’s public health investment would need to be doubled to address current public health needs (IOM, 2012b).
In fiscal year 2012, under the auspices of the PPHF, $401.1 million was set aside to fund community prevention activities proven to reduce health care costs and improve health behaviors. These funds support such initiatives as the Community Transformation Grant (CTG) program, administered by the CDC (APHA, 2012). The CTG program is “designed to address the behavioral, physical, social, and environmental risk factors associated with chronic diseases, such as tobacco use and exposure to secondhand smoke, poor screening systems for disease risks, and lack of access to healthy food and safe environments for physical activity” (Hennrikus, 2013, p. 16).
Ultimately, the CTG program is anticipated to impact 40 percent of the U.S. population (Hennrikus, 2013). CTG grants fund evidence-based programs that address major causes of chronic disease, such as heart disease, diabetes, and cancer, in communities, and promote tobacco-free living, physical activity, healthy eating, services to prevent and control high blood pressure and high cholesterol, social and emotional wellness, and healthy and safe environments (Hennrikus, 2013). State and local government agencies, tribes and territories, and nonprofit organizations are eligible for CTG funds. Thus far, the CTG-funded programs have been implemented in an array of sectors, such as health care, education, and transportation. In 2011, $103 million was distributed among 36 states to 61 state and local government agencies, tribes and territories, and nonprofit organizations for
the implementation of evidence-based programs (CDC, 2013a; Hennrikus, 2013). Although many of these programs are likely to improve the contexts in which young people live, their impact on contributing to improved population-level outcomes among young adults cannot be known absent the improvements in data collection and analysis discussed above.
CONCLUSIONS AND RECOMMENDATIONS
Policy makers and practitioners have recognized that the health, safety, and well-being of adolescents can be enhanced, during adolescence and thereafter, by basing policy and practice on an integrated understanding of this distinct period of development. A key conclusion of this report is that the health, safety, and well-being of young adults can similarly benefit from bringing a developmental perspective to bear on public health policies and programs and on the delivery of health care (discussed in Chapter 7). The literature reviewed in this chapter also makes the following points clear:
- The effects of interventions—especially those that include only one component, focus on only one level, and are brief in duration—generally are small and not sustainable. On the other hand, multipronged and reinforcing approaches that target and are tailored to individual behaviors and their social, environmental, and legal contexts and are implemented over a period of at least several years generally are more successful and their effects more sustained.
- Approaches that promote collaboration and participation among multiple stakeholders create the right environment for individual change and foster health-related social change.
- The use of mobile digital media and social networking to implement interventions shows considerable promise, although evidence for the effectiveness of this approach remains to be developed.
- The notable success of some multilevel public health campaigns targeting older adolescents and young adults provides a solid foundation for developing and fielding innovative community initiatives that combine health messages with environmental interventions addressing cross-cutting health and safety challenges for young adults.
- Public health campaigns that are media based or include a media component are less likely to benefit people who are educationally or economically disadvantaged or are from racial and ethnic minorities, as well as young adults who are not in college.
- Formulating an integrated approach to public health policy and practice focused on young adults will require improvements in
-
the data assembled for surveillance and research, as well as better coordination of federal and state public health programs.
- A major aim of policies focused on improving population health should be to incorporate screening and prevention into primary health care and other health settings for young adults, as well as social settings where at-risk groups congregate (e.g., STI screening in bars or nightclubs).
- The importance of identifying and rectifying health disparities among young adults has received little attention in the design and administration of public health programs, as well as in intervention research.
- Few state or local programs have attempted to coordinate or integrate programs for young adults, although innovations to this end have been undertaken in a handful of states.
- Several recent federal initiatives reflect a nascent effort to promote and support policies and practices reflecting an integrated understanding of young adulthood.
State and Local Coordination Efforts
No states have addressed the needs of young adults aged 18-26 in a large-scale way. Under the new Adolescent and Young Adult Health Program funded by the Health Resources and Services Administration and administered by the MCH Bureau, states and localities will be encouraged to expand care beyond adolescents. To advance this transformation, the committee makes the following recommendation:
Recommendation 6-1: State and local public health departments should establish an office to coordinate programs and services bearing on the health, safety, and well-being of young adults. If a separate office is not established for young adults, these responsibilities should be assigned to the adolescent health coordinator.
The committee is mindful that many state and local public health agencies are underfunded and have limited capacity to take on new responsibilities. Elevating the visibility and importance of young adults may also require additional training and skill development for staff. The committee regards this recommendation as requiring a change in orientation to shape an array of activities that will respond to the documented pressing needs of this population. Aside from bringing together the necessary expertise on the development and needs of young adults, improved coordination of young adult programs and services can also be expected to identify gaps in
existing services and opportunities for new services and allow more efficient allocation of resources.
Once an office for coordinating programs and services for young adults is created or linked to an existing office, an evaluation program will be important. Evaluation will provide processes and tools that can be applied to obtain accurate, reliable, and credible data to address program performance questions. Data collection needs to be feasible for health departments and other organizations, which are unlikely to have the resources for elaborate measurements of populations, polices, and environments. Better data will lead to better comparisons across time and may lead to better benchmarks. There are a variety of ways to accomplish this (see the American Evaluation Association’s Guiding Principles for Evaluators13 for examples).
Colorado 9to25, described earlier in this chapter, highlights the potential synergies of a multisectoral model of community mobilization focused on young adults (or adolescents and young adults). The U.S. Department of Education’s Promise Neighborhoods and the U.S. Department of Housing and Urban Development’s Choice Neighborhoods are analogous initiatives. Building on these models, state public health agencies (or local agencies with adequate staff and authority) should convene multistakeholder initiatives potentially called “Healthy Transitions to Adulthood,” as stand-alone activities or a component of already-existing community initiatives. The coalition should reach out to all local organizations with a stake in the healthy, successful development of young adults, including large employers, residential and nonresidential colleges and universities, community colleges, other providers of vocational training, faith-based organizations, and health care systems. A broad scope of activities might be undertaken by such coalitions, encompassing the entire range of transitional tasks in young adulthood and the range of outcomes associated with health and well-being. Young adults should play a pivotal role in these efforts from the outset.
Recommendation 6-2: Each community should establish a multistakeholder private-public coalition on “Healthy Transitions to Adulthood,” with the goal of promoting the education, health, safety, and well-being of all young adults. State or local public health agencies should take the lead in convening these coalitions. The coalitions should include young adults; colleges and universities; providers of career and technical education; employers; youth organizations; nonprofit organizations; medical specialties providing primary care to young adults; and other community organizations serving, supporting, or investing in young adults. These initiatives should mobilize public and private engagement and support; set priorities; formulate strategies for reaching all groups
__________________
13 See http://www.eval.org/p/cm/ld/fid=51 (accessed October 22, 2014).
of young adults who need services and support; and design, implement, and evaluate prevention activities and programs. Initiatives should also incorporate the valuable input of young adults in shaping their scope and activities to ensure that there is traction among those initiatives aimed at improving their health, safety, and well-being.
The committee is aware of the difficulty of initiating multisector community mobilization efforts and understands that many such efforts do not succeed. However, the creative energy that can be brought to bear on such an initiative provides a solid basis for optimism. Some states may choose to build on the efforts they have devoted to adolescents, extending the purview of those efforts to recognize the importance of the transition into adulthood. The intent is not to dilute existing efforts to improve adolescent health, but to recognize the importance of the young adult years within the life course and the necessity of investing in this particular age group as well.
Finally, once a Healthy Transitions to Adulthood coalition has been formed, stakeholders should be identified and an evaluation process designed with their input so that the evaluations will meet the goals of all stakeholders.
Community Transformation Grants
The CTG program’s 5-year measurable performance goals are to decrease all of the following by 5 percent: death and disability due to tobacco use, the rate of obesity through nutrition and physical activity interventions, and death/disability due to heart disease and stroke (CDC, 2013a). While the first two of these areas clearly are congruent with the needs for prevention among young adults, it is not feasible to ascertain how many young adults have benefited directly from these investments to date. As illustrated by Box 6-2, moreover, many priority issues for young adults are not addressed by the CTG program. Since these national investments are currently being made, however, the CTG program presents an opportunity to deal with at least some of the issues that are important for young adults.
Reducing tobacco use is a key issue because smokers who quit before the age of 30 will reverse much of the damage to their health due to tobacco use (HHS, 2012b). Therefore, although much of the focus is appropriately on reducing the initiation rate for tobacco use among people under age 18, the young adult years also are critical for reducing lifelong rates of tobacco use. Similarly, weight gain during young adulthood may be one of the most important determinants of cardiovascular and cancer risk factors, so this time period is critical for reducing rates of obesity through both improved nutrition and physical activity.
Recommendation 6-3: Recipients of Community Transformation Grants—including state and local government agencies, tribes and territories, and nonprofit organizations—should incorporate specific targets for young adults in their plans to reach the 5-year measurable performance goals in the areas of reducing death and disability due to tobacco use and reducing the rate of obesity through nutrition and physical activity interventions.
As communities consider the types of public health interventions they could implement to support young adults, they might make use of two resources—CDC’s The Guide to Community Preventive Services14 and the New York Academy of Medicine’s Compendium of Proven Community-Based Prevention Programs.15 These resources identify particular programs that have succeeded in reducing obesity and related diseases, including heart disease, hypertension, diabetes, and some forms of cancer—all issues that pose a risk for young adults. Communities also might consider other examples of approaches for impacting young adults. In the area of obesity prevention, for example, HHS, the U.S. Department of Agriculture, the U.S. Department of Defense, and the U.S. Department of Veterans Affairs are engaged in ensuring that federal programs and facilities meet the Dietary Guidelines for Americans.16
Key Areas for Research
Given existing gaps in the current public health infrastructure for young adults, research is needed in several key areas to inform public health policies and programs:
- The effectiveness of multilevel interventions in achieving health outcomes, including how to connect with difficult-to-reach young adults. More research is needed to understand the impact of multilevel interventions, including public health campaigns and initiatives, on prevention and the amelioration of risk factors among young adults. Multidisciplinary researchers can review lessons learned as well as evidence in other relevant areas, such as the use of social marketing for other populations. Most of the young adult population is involved in some type of system (e.g., college, community college, military services), but active outreach to those not connected to these communities, or marginalized in other ways, is
__________________
14 See http://www.thecommunityguide.org/index.html (accessed October 22, 2014).
15 See http://healthyamericans.org/report/110 (accessed October 22, 2014).
16 See http://fasinfat.org/national-prevention-strategy (accessed October 22, 2014).
-
needed. There is limited evidence on these difficult-to-reach populations and on what strategies may be most effective in engaging them so they are better able to recognize and care about the potential risks they create or encounter.
- The influence of social media on health outcomes. The dramatic shift to reliance on information and communication technologies and the significant uptake of social media by young adults point to the promise of harnessing this form of communication to better connect this population with health-related content. The nature of social media may allow for a rich, interactive learning environment that can both engage youth and tailor content directly to their perceptions, barriers, and needs. The capability for two-way communication may further engage young adults and may turn passive audiences into active participants. But despite the promise of media for connecting young adults with both health information and resources in their communities, more research is needed to determine how best to integrate this platform into health interventions. Those conducting such research will need to use high-quality research methods and large samples, understand what other resources may be needed to supplement social media content, and determine how behavior change may be sustained over time.
- Better understanding of how social determinants, mechanisms, and trajectories contribute to health disparities among young adults, including within different groups. The preponderance of research involving young adults often focuses on college campuses, particularly for priority areas such as alcohol and tobacco consumption. However, the focus on this population fails to fully represent how young adults who do not attend college experience the transition after high school, and thus may obscure how those from different socioeconomic and racial and ethnic groups may be impacted by this transition. More research on how to develop and deploy robust interventions among noncollege youth in diverse community- and work-based settings is sorely needed, including rigorous trials using standardized measures so that behavioral outcomes can be compared across groups. Furthermore, studies with diverse groups may benefit greatly from partnerships with community organizations to increase reach, promote sustainability, account for cultural factors, and tailor the content of interventions more effectively to the needs of the target group.
- Better understanding of the impact of the advertising and promotion of alcohol, tobacco, and marijuana on the health, safety, and well-being of young adults. Research is needed to assess the impact, singly and in combination, of the promotion and advertising of al-
cohol, tobacco, and marijuana on the health, safety, and well-being of young adults. The importance of this research is highlighted by the proliferation of new tobacco products, including e-cigarettes, and the combined use of tobacco products and marijuana in jurisdictions that have legalized marijuana’s medical or recreational use.
American Psychiatric Association. 2014. Resource document on the need to monitor and assess the public health and safety consequences of legalizing marijuana. http://www.psychiatry.org/learn/library--archives/resource-documents (accessed August 29, 2014).
APA (American Psychological Association). 2013. Stress in America: Missing the health care connection. https://www.apa.org/news/press/releases/stress/2012/full-report.pdf (accessed July 15, 2014).
APHA (American Public Health Association). 2012. The prevention and public health fund: A critical investment in our nation’s physical and fiscal health. Center for Public Health Policy Issue Brief. Washington, DC: APHA.
APHA. 2013. Get the facts: Prevention and public health fund: Dedicated to improving our nation’s public health. Washington, DC: APHA.
Aronson, R. E., K. L. Rulison, L. F. Graham, R. M. Pulliam, W. L. McGee, J. D. Labban, D. Dingman, and S. D. Rhodes. 2013. Brothers leading healthy lives: Outcomes from the pilot testing of a culturally and contextually congruent HIV prevention intervention for black male college students. AIDS Education and Prevention 25(5):376-393.
ASTHO (Association of State and Territorial Health Officials). 2009. Profile of state public health: Volume one. Arlington, VA: ASTHO.
ASTHO. 2014. Profile of state public health: Volume three. Arlington, VA: ASTHO.
Atkin, C. K., and R. E. Rice. 2012. Theory and principles of public communication campaigns. In Public communication campaigns, 4th ed., edited by R. E. Rice and C. K. Atkin. Thousands Oak, CA: Sage Publications. Pp. 3-19.
Birnbaum, H. G., R. C. Kessler, D. Kelley, R. Ben-Hamadi, V. N. Joish, and P. E. Greenberg. 2010. Employer burden of mild, moderate, and severe major depressive disorder: Mental health services utilization and costs, and work performance. Depression and Anxiety 27(1):78-89.
Black, M. C., K. C. Basile, M. J. Breiding, S. G. Smith, M. L. Walters, M. T. Merrick, J. Chen, and M. R. Stevens. 2011. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, CDC.
Blazer, D., D. Hughes, and L. K. George. 1987. Stressful life events and the onset of a generalized anxiety syndrome. American Journal of Psychiatry 144(9):1178-1183.
Bonnie, R. J. 2014. The impending collision between first amendment protection for commercial speech and the public health: The case of tobacco control. Virginia Public Law and Legal Theory Research Paper No. 2014-34.
Bonnie, R. J., and E. S. Scott. 2013. The teenage brain: Adolescent brain research and the law. Current Directions in Psychological Science 22(2):158-161.
Bonnie, R. J., and C. H. Whitebread. 1974. The marijuana conviction: A history of marijuana prohibition in the United States. Charlottesville: University Press of Virginia.
Braithwaite, S. R., and F. D. Fincham. 2009. A randomized clinical trial of a computer based preventive intervention: Replication and extension of ePREP. Journal of Family Psychology 23(1):32-38.
Brinn, M. P., K. V. Carson, A. J. Esterman, A. B. Chang, and B. J. Smith. 2012. Mass media interventions for preventing smoking in young people. Evidence-Based Child Health: A Cochrane Review Journal 7(1):86-144.
Brody, G. H., Y. F. Chen and S. M. Kogan. 2010. A cascade model connecting life stress to risk behavior among rural African American emerging adults. Development and Psychopathoogy 22(3):667-678.
Broman, C. L. 2012. Race differences in the receipt of mental health services among young adults. Psychological Services 9(1):38-48.
Bronfenbrenner, U. 1979. Contexts of child rearing: Problems and prospects. American Psychologist 34(10):844-850.
Brown, J. 2013. A review of the evidence on technology-based interventions for the treatment of tobacco dependence in college health. Worldviews on Evidence Based Nursing 10(3):150-162.
Bull, S. S., D. K. Levine, S. R. Black, S. J. Schmiege, and J. Santelli. 2012. Social media-delivered sexual health intervention: A cluster randomized controlled trial. American Journal of Preventive Medicine 43(5):467-474.
Caldeira, K. M., S. J. Kasperski, E. Sharma, K. B. Vincent, K. E. O’Grady, E. D. Wish, and A. M. Arria. 2009. College students rarely seek help despite serious substance use problems. Journal of Substance Abuse Treatment 37(4):368-378.
Carrol, J. A., and R. L. Kirkpatrick. 2011. Impact of social media on adolescent behavioral health. Oakland: California Adolescent Health Collaborative.
Carson, K. V., M. P. Brinn, N. A. Labiszewski, A. J. Esterman, A. B. Chang, and B. J. Smith. 2011. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews (7):Cd001291.
Catalano, S. 2013. Intimate partner violence: Attributes of victimization, 1993-2010. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics.
Cavallo, D. N., D. F. Tate, A. V. Ries, J. D. Brown, R. F. DeVellis, and A. S. Ammerman. 2012. A social media-based physical activity intervention: A randomized controlled trial. American Journal of Preventive Medicine 43(5):527-532.
CDC (Centers for Disease Control and Prevention). 1994. Preventing tobacco use among young people: A report of the Surgeon General. Atlanta, GA: HHS, Public Health Service, CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
CDC. 2010. Alcohol and public health. http://www.cdc.gov/alcohol/ardi.htm (accessed July 14, 2014).
CDC. 2012. Estimated HIV incidence among adults and adolescents in the United States, 2007-2010. HIV Surveillance Supplemental Report 17(4)1-26.
CDC. 2013a. Community transformation grants (CTG). http://www.cdc.gov/nccdphp/dch/programs/communitytransformation/ (accessed March 24, 2014).
CDC. 2013b. Homicide rates among persons aged 10-24 years—United States, 1981-2010. Morbidity and Mortality Weekly Report 62(27):545-548.
CDC. 2013c. Incidence, prevalence, and cost of sexually transmitted infections in the United States. http://www.cdc.gov/std/stats/sti-estimates-fact-sheet-feb-2013.pdf (accessed August 11, 2014).
CDC. 2013d. Youth violence: National statistics. http://www.cdc.gov/violenceprevention/youthviolence/stats_at-a_glance/nfa_age-sex.html (accessed July 7, 2014).
CDC. 2013e. 2011 HIV surveillance report. Vol. 23. http://www.cdc.gov/hiv/topics/surveillance/resources/reports (accessed July 15, 2014).
CDC. 2014a. Compressed mortality, 1999-2011 data provided by CDC wonder online database. http://wonder.cdc.gov/cmf-icd10.html (accessed September 4, 2014).
CDC. 2014b. Fact sheets: Alcohol use and health. http://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm (accessed July 9, 2014).
CDC, 2014c. Fact sheets: Genital HPV infection. http://www.cdc.gov/std/hpv/stdfact-hpv.htm (accessed August 11, 2014).
CDC. 2014d. Leading causes of death reports, national and regional, 1999-2011. http://webappa.cdc.gov/sasweb/ncipc/leadcaus10_us.html (accessed July 10, 2014).
Cellucci, T., J. Krogh, and P. Vik. 2006. Help seeking for alcohol problems in a college population. Journal of General Psychology 133(4):421-433.
Chapman, J., C. J. Armitage, and P. Norman. 2009. Comparing implementation intention interventions in relation to young adults’ intake of fruit and vegetables. Psychology and Health 24(3):317-332.
Chen, P., and K. C. Jacobson. 2012. Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health 50(2):154-163.
Christensen, H., E. Pallister, S. Smale, I. B. Hickie, and A. L. Calear. 2010. Community-based prevention programs for anxiety and depression in youth: A systematic review. Journal of Primary Prevention 31(3):139-170.
Cole, J. M. 2013. Memorandum for all United States attorneys. Washington, DC: U.S. Department of Justice.
Corcoran, C., E. Walker, R. Huot, V. Mittal, K. Tessner, L. Kestler, and D. Malaspina. 2003. The stress cascade and schizophrenia: Etiology and onset. Schizophrenia Bulletin 29(4):671-692.
Corrigan, P. W., and A. C. Watson. 2002. Understanding the impact of stigma on people with mental illness. World Psychiatry 1(1):16-20.
Cotton, S. M., A. Wright, M. G. Harris, A. F. Jorm, and P. D. McGorry. 2006. Influence of gender on mental health literacy in young Australians. Australian and New Zealand Journal of Psychiatry 40(9):790-796.
Curtin, S. C., J. C. Abma, S. J. Ventura, and S. Henshaw. 2013. Pregnancy rates for U.S. women continue to drop. National Center for Health Statistics, Data Brief (123):1-7.
Dalton, M. A., M. L. Beach, A. M. Adachi-Mejia, M. R. Longacre, A. L. Matzkin, J. D. Sargent, T. F. Heatherton, and L. Titus-Ernstoff. 2009. Early exposure to movie smoking predicts established smoking by older teens and young adults. Pediatrics 123(4):e551-e558.
Dejong, W., and J. Blanchette. 2014. Case closed: Research evidence on the positive public health impact of the age 21 minimum legal drinking age in the United States. Journal of Studies on Alcohol and Drugs (17):108-115.
DiClemente, R. J., and G. M. Wingood. 1995. A randomized controlled trial of an HIV sexual risk-reduction intervention for young African-American women. Journal of the American Medical Association 274(16):1271-1276.
Dinh-Zarr, T. B., D. A. Sleet, R. A. Shults, S. Zaza, R. W. Elder, J. L. Nichols, R. S. Thompson, and D. M. Sosin. 2001. Reviews of evidence regarding interventions to increase the use of safety belts. American Journal of Preventive Medicine 21(4):48-65.
DoD (U.S. Department of Defense). 2014. Department of Defense annual report on sexual assault in the military: Fiscal year 2013. Washington, DC: DoD.
Duggan, M., and A. Smith. 2013. Social media update 2013. http://www.pewinternet.org/2013/12/30/social-media-update-2013 (accessed July 11, 2014).
Edlund, M. J., P. S. Wang, P. A. Berglund, S. J. Katz, E. Lin, and R. C. Kessler. 2002. Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. American Journal of Psychiatry 159(5):845-851.
Edlund, M. J., B. M. Booth, and X. Han. 2012. Who seeks care where?: Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. Journal of Studies on Alcohol and Drugs 73(4):635-646.
Eisenberg, D., E. Golberstein, and S. E. Gollust. 2007. Help-seeking and access to mental health care in a university student population. Medical Care 45(7):594-601.
Eisenberg, D., M. F. Downs, E. Golberstein, and K. Zivin. 2009. Stigma and help seeking for mental health among college students. Medical Care Research and Review 66(5):522-541.
Elder, R. W., R. A. Shults, D. A. Sleet, J. L. Nichols, R. S. Thompson, and W. Rajab. 2004. Effectiveness of mass media campaigns for reducing drinking and driving and alcohol-involved crashes: A systematic review. American Journal of Preventive Medicine 27(1):57-65.
Farrer, L., L. Leach, K. M. Griffiths, H. Christensen, and A. F. Jorm. 2008. Age differences in mental health literacy. BMC Public Health 8:125.
Farrer, L., A. Gulliver, J. K. Chan, P. J. Batterham, J. Reynolds, A. Calear, R. Tait, K. Bennett and K. M. Griffiths. 2013. Technology-based interventions for mental health in tertiary students: Systematic review. Journal of Medical Internet Research 15(5):e101.
Fell, J. C., and E. Romano. 2013. Are strong graduated driver licensing laws having unintended consequences? Annals of Advances in Automotive Medicine 57:351-352.
Fellmeth, G. L., C. Heffernan, J. Nurse, S. Habibula, and D. Sethi. 2013. Educational and skills-based interventions for preventing relationship and dating violence in adolescents and young adults. Cochrane Database of Systematic Reviews 6.
Fergusson, D. M., L. J. Horwood, E. M. Ridder, and A. L. Beautrais. 2005. Sexual orientation and mental health in a birth cohort of young adults. Psychological Medicine 35(7):971-981.
Fowler, C. I., S. Lloyd, J. Gale, J. Wang, and E. McClure. 2012. Family Planning Annual Report: 2011 National Summary. Research Triangle Park, NC: RTI International.
Fox, S., and R. Lee. 2014. The web at 25 in the U.S. http://www.pewinternet.org/2014/02/27/the-web-at-25-in-the-u-s (accessed May 3, 2014).
Garcia, C. 2010. Conceptualization and measurement of coping during adolescence: A review of the literature. Journal of Nursing Scholarship 42(2):166-185.
Gavin, L., A. P. MacKay, K. Brown, S. Harrier, S. J. Ventura, L. Kann, M. Rangel, S. Berman, P. Dittus, N. Liddon, L. Markowitz, M. Sternberg, H. Weinstock, C. David-Ferdon, and G. Ryan. 2009. Sexual and reproductive health of persons aged 10-24 years—United States, 2002-2007. Morbidity and Mortality Weekly Report Surveillance Summaries 58(6):1-58.
Gayman, M. D., G. S. Cuddeback, and J. P. Morrissey. 2011. Help-seeking behaviors in a community sample of young adults with substance use disorders. The Journal of Behavioral Health Services & Research 38(4):464-477.
Gerend, M. A., M. A. Shepherd, and M. L. Lustria. 2013. Increasing human papillomavirus vaccine acceptability by tailoring messages to young adult women’s perceived barriers. Sexually Transmitted Diseases 40(5):401-405.
Gow, R. W., S. E. Trace, and S. E. Mazzeo. 2010. Preventing weight gain in first year college students: An online intervention to prevent the “freshman fifteen.” Eating Behaviors 11(1):33-39.
Greene, G. W., A. A. White, S. L. Hoerr, B. Lohse, S. M. Schembre, D. Riebe, J. Patterson, K. K. Kattelmann, S. Shoff, T. Horacek, B. Blissmer, and B. W. Phillips. 2012. Impact of an online healthful eating and physical activity program for college students. American Journal of Health Promotion 27(2):e47-e58.
Gulliver, A., K. M. Griffiths, and H. Christensen. 2010. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 10:113.
Ha, E. J., and N. Caine-Bish. 2009. Effect of nutrition intervention using a general nutrition course for promoting fruit and vegetable consumption among college students. Journal of Nutrition Education and Behavior 41(2):103-109.
Hadley, D. C., J. R. Reddon, and R. D. Reddick. 2001. Age, gender, and treatment attendance among forensic psychiatric outpatients. Journal of Offender Rehabilitation 32(4):55-66.
Han, B., R. McKeon, and J. Gfroerer. 2014. Suicidal ideation among community-dwelling adults in the United States. American Journal of Public Health 104(3):488-497.
Harrell, E. 2014. Crime against persons with disabilities, 2009-2012 statistical tables. Washington, DC: Bureau of Justice Statistics.
Harris, K. M., P. Gordon-Larsen, K. Chantala, and J. R. Udry. 2006. Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Archives of Pediatrics & Adolescent Medicine 160(1):74-81.
Hebden, L., A. Cook, H. P. van der Ploeg, L. King, A. Bauman, and M. Allman-Farinelli. 2014. A mobile health intervention for weight management among young adults: A pilot randomised controlled trial. Journal of Human Nutrition and Dietetics 27(4):322-332.
Held, P., and G. P. Owens. 2013. Stigmas and attitudes toward seeking mental health treatment in a sample of veterans and active duty service members. Traumatology 19(2):136-143.
Hennrikus, D. 2013. The ACA invests in community health: The community transformation grant program. http://www.epi.umn.edu/mch/wp-content/uploads/2012/05/HG_Fall20132.pdf (accessed March 24, 2014).
HHS (U.S. Department of Health and Human Services). 1999. Mental health: A report of the Surgeon General. Rockville, MD: HHS.
HHS. 2012a. Healthy people 2020: Core indicators for adolescent and young adults health. http://www.healthypeople.gov/2020/learn/Draft_Core_Indicators_Web.pdf (accessed July 14, 2014).
HHS. 2012b. Preventing tobacco use among youth and young adults. Washington, DC: HHS, CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
HHS. 2012c. 2012 National Strategy for Suicide Prevention: Goals and objectives for action. Washington, DC: HHS.
HHS. 2014a. FY 2015 congressional justification for the Health Resources and Services Administration (HRSA). http://www.hrsa.gov/about/budget/budgetjustification2015.pdf (accessed September 4, 2014).
HHS. 2014b. HHS announces the availability of $100 million in Affordable Care Act funding to expand access to primary care through new community health centers. http://www.hhs.gov/news/press/2014pres/07/20140708a.html (accessed July 14, 2014).
HHS. 2014c. Reports of the Surgeon General. In The health consequences of smoking-50 years of progress: A report of the Surgeon General. Atlanta, GA: HHS, CDC, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
Hingson, R. W. 2010. Magnitude and prevention of college drinking and related problems. Alcohol Research & Health 33(1-2):45.
Hoek, J., A. Hoek-Sims, and P. Gendall. 2013. A qualitative exploration of young adult smokers’ responses to novel tobacco warnings. BMC Public Health 13(1):1-10.
Holder, H. D., and A. J. Treno. 1997. Media advocacy in community prevention: News as a means to advance policy change. Addiction 92(Suppl. 2):S189-S199.
Hopfer, S. 2012. Effects of a narrative HPV vaccination intervention aimed at reaching college women: A randomized controlled trial. Prevention Science 13(2):173-182.
Hornik, R. 2002. Public health communication: Evidence for behavior change. New York: Lawrence Erlbaum Associates.
Hornik, R., and I. Yanovitzky. 2003. Using theory to design evaluations of communication campaigns: The case of the national youth anti-drug media campaign. Communication Theory 13(2):204-224.
Horrey, W. J., M. F. Lesch, and A. Garabet. 2009. Dissociation between driving performance and drivers’ subjective estimates of performance and workload in dual-task conditions. Journal of Safety Research 40(1):7-12.
HRSA (Health Resources and Services Administration). 2000. Understanding Title V of the Social Security Act. Rockville, MD: HRSA.
HRSA. 2012. The Ryan White HIV/AIDS Program: Population fact sheet. http://hab.hrsa.gov/abouthab/populations/youthfacts2012.pdf (accessed July 14, 2014).
HRSA. 2013. The Ryan White HIV/AIDS Program overview. http://hab.hrsa.gov/abouthab/files/programoverviewfacts2012.pdf (accessed September 4, 2014).
HRSA. 2014a. Adolescent and Young Adult Health National Resource Center Program. http://www.acf.hhs.gov/hhsgrantsforecast/index.cfm?switch=grant.view&gff_grants_forecastInfoID=66854 (accessed October 3, 2014).
HRSA. 2014b. Table 3a—Patients by age and gender. http://bphc.hrsa.gov/uds/datacenter.aspx?q=t3a&year=2012&state= (accessed July 14, 2014).
HRSA. 2014c. Table 3a—Patients by age and gender. http://bphc.hrsa.gov/uds/lookalikes.aspx?q=t3a&year=2012&state=national (accessed September 18, 2014).
HRSA. 2014d. Title V Maternal and Child Health Services Block Grant Program. http://mchb.hrsa.gov/programs/titlevgrants/ (accessed September 16, 2014).
HRSA. 2014e. Title V information system. https://mchdata.hrsa.gov/tvisreports/MeasurementData/HSCI/HSCI06Search.aspx?measurenum=06B&from=pd (accessed July 14, 2014).
Hyde, J. K., and S. M. Shortell. 2012. The structure and organization of local and state public health agencies in the U.S.: A systematic review. American Journal of Preventive Medicine 42(5, Suppl. 1):S29-S41.
IOM (Institute of Medicine). 1988. The future of public health. Washington, DC: National Academy Press.
IOM. 1994. Growing up tobacco free: Preventing nicotine addiction in children and youths. Washington, DC: National Academy Press.
IOM. 1999. Marijuana and medicine: Assessing the science base. Washington, DC: National Academy Press.
IOM. 2002. Guidance for the national healthcare disparities report. Washington, DC: The National Academies Press.
IOM. 2003. The future of the public’s health in the 21st century. Washington, DC: The National Academies Press.
IOM. 2004. Health literacy: A prescription to end confusion. Washington, DC: The National Academies Press.
IOM. 2006. Examining the health disparities research plan of the National Institutes of Health: Unfinished business. Washington, DC: The National Academies Press.
IOM. 2007. Ending the tobacco problem: A blueprint for the nation. Washington, DC: The National Academies Press.
IOM. 2009. A review of the HHS Family Planning Program: Mission, management, and measurement of results. Washington, DC: The National Academies Press.
IOM. 2011. For the public’s health: The role of measurement in action and accountability. Washington, DC: The National Academies Press.
IOM. 2012a. Accelerating progress in obesity prevention: Solving the weight of the nation. Washington, DC: The National Academy Press.
IOM. 2012b. For the public’s health: Investing in a healthier future. Washington, DC: The National Academies Press.
IOM. 2012c. How far have we come in reducing health disparities?: Progress since 2000: Workshop summary. Washington, DC: The National Academies Press.
IOM and NRC (National Research Council). 2013. Improving the health, safety, and well-being of young adults: Workshop summary. Washington, DC: The National Academies Press.
Israel, B. A., A. J. Schulz, E. A. Parker, A. B. Becker, A. J. Allen III, and J. R. Guzman. 2008. Critical issues in developing and following CBPR principles. In Community-based participatory research for health: From process to outcomes, edited by M. Minkler and N. Wallerstein. San Francisco, CA: Jossey-Bass. Pp. 56-73.
Jackson, C. A., M. Henderson, J. W. Frank, and S. J. Haw. 2012. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. Journal of Public Health 34(Suppl. 1):i31-i40.
Jackson, P. B., and M. Finney. 2002. Negative life events and psychological distress among young adults. Social Psychology Quarterly 65(2):186-201.
Johnston, J. D., A. P. Massey, and R. L. Marker-Hoffman. 2012. Using an alternate reality game to increase physical activity and decrease obesity risk of college students. Journal of Diabetes Science and Technology 6(4):828-838.
Jones, K., P. Eathington, K. Baldwin, and H. Sipsma. 2014. The impact of health education transmitted via social media or text messaging on adolescent and young adult risky sexual behavior: A systematic review of the literature. Sexually Transmitted Diseases 41(7):413-419.
Jones, R., D. R. Hoover, and L. J. Lacroix. 2013. A randomized controlled trial of soap opera videos streamed to smartphones to reduce risk of sexually transmitted human immunodeficiency virus (HIV) in young urban African American women. Nursing Outlook 61(4):205-215.e203.
Jorm, A. F. 2012. Mental health literacy: Empowering the community to take action for better mental health. American Psychologist 67(3):231-243.
Kawachi, I., and L. F. Berkman. 2001. Social ties and mental health. Journal of Urban Health 78(3):458-467.
Kelley-Baker, T., M. B. Johnson, E. Romano, E. A. Mumford, and B. A. Miller. 2011. Preventing victimization among young women: The SafeNights intervention. American Journal of Health Studies 26(4):185-195.
Kendler, K. S., L. M. Karkowski, and C. A. Prescott. 1999. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry 156(6):837-841.
Kennedy, S. B., S. Nolen, Z. Pan, B. Smith, J. Applewhite, and K. J. Vanderhoff. 2013. Effectiveness of a brief condom promotion program in reducing risky sexual behaviours among African American men. Journal of Evaluation in Clinical Practice 19(2):408-413.
Kessler, R. C., P. Berglund, O. Demler, R. Jin, K. R. Merikangas, and E. E. Walters. 2005. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62(6):593-602.
Kessler, R. C., H. S. Akiskal, M. Ames, H. Birnbaum, P. Greenberg, R. M. Hirschfeld, R. Jin, K. R. Merikangas, G. E. Simon, and P. S. Wang. 2006. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. American Journal of Psychiatry 163(9):1561-1568.
Kester, L. M., R. B. Shedd-Steele, C. A. Dotson-Roberts, J. Smith, and G. D. Zimet. 2014. The effects of a brief educational intervention on human papillomavirus knowledge and intention to initiate HPV vaccination in 18-26 year old young adults. Gynecologic Oncology 132(Suppl. 1):S9-S12.
KFF (The Henry J. Kaiser Family Foundation). 2011. The uninsured: A primer—key facts about Americans without health insurance. http://obamacarefacts.com/obamacare-docs/kisair-people-without-health-insurance.pdf (accessed September 16, 2014).
King, B. A., S. Alam, G. Promoff, R. Arrazola, and S. R. Dube. 2013. Awareness and ever use of electronic cigarettes among U.S. adults, 2010-2011. Nicotine & Tobacco Research.
King, M., J. Semlyen, S. S. Tai, H. Killaspy, D. Osborn, D. Popelyuk, and I. Nazareth. 2008. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry 8:70.
King, S. 2014. Teen and young adult health program. http://www.maine.gov/dhhs/mecdc/population-health/tya/index.html (accessed July 14, 2014).
Koh, H. K., J. J. Piotrowski, S. Kumanyika, and J. E. Fielding. 2011. Healthy people: A 2020 vision for the social determinants approach. Health Education & Behavior 38(6):551-557.
Krebs, C. P., C. H. Lindquist, T. D. Warner, B. S. Fisher, and S. L. Martin. 2009. College women’s experiences with physically forced, alcohol- or other drug-enabled, and drug-facilitated sexual assault before and since entering college. Journal of American College Health 57(6):639-647.
Kypri, K., T. Vater, S. J. Bowe, J. B. Saunders, J. A. Cunningham, N. J. Horton, and J. McCambridge. 2014. Web-based alcohol screening and brief intervention for university students: A randomized trial. Journal of the American Medical Association 311(12): 1218-1224.
Lally, J., A. O’Conghaile, S. Quigley, E. Bainbridge, and C. McDonald. 2013. Stigma of mental illness and help-seeking intention in university students. The Psychiatrist 37(8):253-260.
Laska, M. N., J. E. Pelletier, N. I. Larson, and M. Story. 2012. Interventions for weight gain prevention during the transition to young adulthood: A review of the literature. Journal of Adolescent Health 50(4):324-333.
Lennon, R., R. Rentfro, and B. O’Leary. 2010. Social marketing and distracted driving behaviors among young adults: The effectiveness of fear appeals. Academy of Marketing Studies Journal 14(2):95-104.
Lienemann, B. A., J. T. Siegel, and W. D. Crano. 2013. Persuading people with depression to seek help: Respect the boomerang. Health Communication 28(7):718-728.
Link, B. G., and J. Phelan. 1995. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior Spec. No. 80-94.
Luong, G., and S. T. Charles. 2014. Age differences in affective and cardiovascular responses to a negative social interaction: The role of goals, appraisals, and emotion regulation. Developmental Psychology 50(7):1919-1930.
Mack, K. A. 2013. Drug-induced deaths—United States, 1999-2010. Morbidity and Mortality Weekly Report Surveillance Summaries 62(Suppl. 3):161-163.
Maher, C. A., L. K. Lewis, K. Ferrar, S. Marshall, I. De Bourdeaudhuij, and C. Vandelanotte 2014. Are health behavior change interventions that use online social networks effective? A systematic review. Journal of Medical Internet Research 16(2):e40.
Marcus, B. H., D. M. Williams, P. M. Dubbert, J. F. Sallis, A. C. King, A. K. Yancey, B. A. Franklin, D. Buchner, S. R. Daniels, and R. P. Claytor. 2006. Physical activity intervention studies: What we know and what we need to know: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation 114(24):2739-2752.
Marmot, M. 2013. Universal health coverage and social determinants of health. Lancet 382(9900):1227-1228.
Martin, J., B. Hamilton, M. Osterman, S. Curin, and T. J. Mathews. 2013. Births: Final data for 2012. Washington, DC: HHS.
May, A. L., D. Freedman, B. Sherry, and H. M. Blanck. 2013. Obesity—United States, 1999-2010. Morbidity and Mortality Weekly Report Surveillance Summaries 62(Suppl. 3):120-128.
McEwen, B. S. 2008. Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators. European Journal of Pharmacology 583(2-3):174-185.
McEwen, B. S., and P. J. Gianaros. 2010. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Annals of the New York Academy of Sciences 1186:190-222.
Mevissen, F. E., R. A. Ruiter, R. M. Meertens, F. Zimbile, and H. P. Schaalma. 2011. Justify your love: Testing an online STI-risk communication intervention designed to promote condom use and STI-testing. Psychology and Health 26(2):205-221.
Milstein, B., J. Homer, P. Briss, D. Burton, and T. Pechacek. 2011. Why behavioral and environmental interventions are needed to improve health at lower cost. Health Affairs 30(5):823-832.
Minkler, M., and N. Wallerstein. 2008. Community-based participatory research for health: From process to outcomes, 2nd ed. San Francisco, CA: Jossey-Bass.
Moore, G. F., A. Williams, L. Moore, and S. Murphy. 2013. An exploratory cluster randomised trial of a university halls of residence based social norms marketing campaign to reduce alcohol consumption among 1st year students. Substance Abuse Treatment, Prevention, and Policy 8:15.
Morrison, D. S., M. Petticrew, and H. Thomson. 2003. What are the most effective ways of improving population health through transport interventions? Evidence from systematic reviews. Journal of Epidemiology and Community Health 57(5):327-333.
Mosher, W., J. Jones, and J. C. Abma. 2012. Intended and unintended birth in the United States. Hyattsville, MD: National Center for Health Statistics.
Mulye, T. P., M. J. Park, C. D. Nelson, S. H. Adams, C. E. Irwin, Jr., and C. D. Brindis. 2009. Trends in adolescent and young adult health in the United States. Journal of Adolescent Health 45(1):8-24.
Muscatell, K. A., G. M. Slavich, S. M. Monroe, and I. H. Gotlib. 2009. Stressful life events, chronic difficulties, and the symptoms of clinical depression. The Journal of Nervous and Mental Disease 197(3):154-160.
NACCHO (National Association of County and City Health Offıcials). 2009. National profıle of local health departments. Washington, DC: NACCHO.
NACCHO. 2014a. Local health department budget cuts and job losses: Findings from the 2014 forces of change survey. http://www.naccho.org/topics/research/forcesofchange/upload/Budget-Cuts.pdf (accessed July 14, 2014).
NACCHO. 2014b. National profile of local health departments. http://nacchoprofilestudy.org/chapter-2 (accessed July 14, 2014).
Napolitano, M. A., S. Hayes, G. G. Bennett, A. K. Ives, and G. D. Foster. 2013. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity 21(1):25-31.
Natelson, R. 2009. A case for federal oversight of military sexual harassment. Clearinghouse Review: Journal of Poverty Law and Policy 43:277-573.
NCAVP (National Coalition of Anti-Violence Programs). 2013. Lesbian, gay, bisexual, transgender, queer and HIV-affected hate violence in 2012. New York: New York City Gay and Lesbian Anti-Violence Project, Inc.
NCI (National Cancer Institute). 2008. The role of the media in promoting and reducing tobacco use. Tobacco Control Monograph No. 19. Bethesda, MD: NCI.
NCSL (National Conference of State Legislatures). 2014. State medical marijuana laws. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx (accessed August 29, 2014).
Neinstein, L. S. 2013. The new adolescents: An analysis of health conditions, behaviors, risks, and access to services among emerging young adults. Executive Summary. http://www.usc.edu/student-affairs/Health_Center/thenewadolescents/doc/TheNewAdolescents_Final_Locked.pdf (accessed September 5, 2014).
NHTSA (National Highway Traffic Safety Administration). 2013. Alcohol-impaired driving. Washington, DC: NHTSA’s National Center for Statistics and Analysis.
NHTSA. 2014. Distracted driving 2012. Washington, DC: NHTSA’s National Center for Statistics and Analysis.
NIH (National Institutes of Health). 2009. DrugFacts: Treatment approaches for drug addiction. http://www.drugabuse.gov/publications/drugfacts/treatment-approaches-drug-addiction (accessed July 15, 2014).
NIH. 2014. Abuse of prescription (Rx) drugs affects young adults most. http://www.drugabuse.gov/related-topics/trends-statistics/infographics/abuse-prescription-rx-drugsaffects-young-adults-most (accessed July 10, 2014).
NIHCM (National Institute for Health Care Management). 2007. Reducing health disparities among children: Strategies and program for health plans. Washington, DC: NIHCM.
NIMH (National Institute of Mental Health). 2000. Treatment of children with mental disorders. Bethesda, MD: NIMH.
Nirenberg, T., J. Baird, R. Longabaugh, and M. J. Mello. 2013. Motivational counseling reduces future police charges in court referred youth. Accident Analysis & Prevention 53:89-99.
NNSAHC (National Network of State Adolescent Health Coordinators). 2012. State adolescent health coordinator survey. http://nnsahc.org/images/uploads/2012NNSAHC_SurveySummary.pdf (accessed July 14, 2014).
Norton, W. E., J. D. Fisher, K. R. Amico, J. F. Dovidio, and B. T. Johnson. 2012. Relative efficacy of a pregnancy, sexually transmitted infection, or human immunodeficiency virus prevention-focused intervention on changing sexual risk behavior among young adults. Journal of American College Health 60(8):574-582.
NRC and IOM. 2004. Reducing underage drinking: A collective responsibility. Washington, DC: The National Academies Press.
NRC and IOM. 2009. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, DC: The National Academies Press.
Pacula, R. L., B. Kilmer, A. C. Wagenaar, F. J. Chaloupka, and J. P. Caulkins. 2014. Developing public health regulations for marijuana: Lessons from alcohol and tobacco. American Journal of Public Health 104(6):1021-1028.
Park, M. J., T. Paul Mulye, S. H. Adams, C. D. Brindis, and C. E. Irwin, Jr. 2006. The health status of young adults in the United States. Journal of Adolescent Health 39(3):305-317.
Park, M. J., J. T. Scott, S. H. Adams, C. D. Brindis, and C. E. Irwin. 2014. Adolescent and young adult health in the United States in the past decade: Little improvement and young adults remain worse off than adolescents. Journal of Adolescent Health 55(1):3-16.
Paschall, M. J., T. Antin, C. L. Ringwalt, and R. F. Saltz. 2011a. Effects of AlcoholEdu for college on alcohol-related problems among freshmen: A randomized multicampus trial. Journal of Studies on Alcohol and Drugs 72(4):642-650.
Paschall, M. J., T. Antin, C. L. Ringwalt, and R. F. Saltz. 2011b. Evaluation of an Internet-based alcohol misuse prevention course for college freshmen: Findings of a randomized multi-campus trial. American Journal of Preventive Medicine 41(3):300-308.
Patel, V., A. J. Flisher, S. Hetrick, and P. McGorry. 2007. Mental health of young people: A global public-health challenge. Lancet 369:1302-1313.
Paus, T., M. Keshavan, and J. N. Giedd. 2008. Why do many psychiatric disorders emerge during adolescence? Nature Reviews Neuroscience 9(12):947-957.
Perkins, H., J. W. Linkenbach, M. A. Lewis, and C. Neighbors. 2010. Effectiveness of social norms media marketing in reducing drinking and driving: A statewide campaign. Addictive Behaviors 35(10):866-874.
Pew Research Center. 2013. State of the news media 2013. http://stateofthemedia.org/2013/overview-5/ (accessed September 15, 2014).
Pew Research Center. 2014. State of the news media 2014. http://www.journalism.org/packages/state-of-the-news-media-2014 (accessed April 3, 2014).
Planty, M., L. Langton, C. Krebs, M. Berzofksy, and H. Smiley-McDonald. 2013. Female victims of sexual violence, 1994-2010. Washington, DC: Bureau of Justice Statistics.
Poobalan, A., L. Aucott, E. Precious, I. Crombie, and W. Smith. 2010. Weight loss interventions in young people (18 to 25 year olds): A systematic review. Obesity Reviews 11(8):580-592.
Price, D., and L. Dunlap. 1988. Stress and coping of adults and young adults in economically uncertain rural areas. Lifestyles 9(2):123-144.
Ramanadhan, S., C. Salhi, E. Achille, N. Baril, K. D’Entremont, M. Grullon, C. Judge, S. Oppenheimer, C. Reeves, C. Savage, and K. Viswanath. 2012. Addressing cancer disparities via community network mobilization and intersectoral partnerships: A social network analysis. PLoS ONE 7(2):e32130.
Ramirez, M., J. Yang, T. Young, L. Roth, A. Garinger, L. Snetselaar, and C. Peek-Asa. 2013. Implementation evaluation of steering teens safe: Engaging parents to deliver a new parent-based teen driving intervention to their teens. Health Education & Behavior 40(4):426-434.
Randle, A. A., and C. A. Graham. 2011. A review of the evidence on the effects of intimate partner violence on men. Psychology of Men & Masculinity 12(2):97-111.
Randolph, W., and K. Viswanath. 2004. Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annual Review of Public Health 25:419-437.
Ray, S., V. Bhaskar, S. Bhandari, and C. Kodange. 2012. Impact of a behaviour change intervention model for promotion of condoms amongst young adult males in an occupational setting. Medical Journal Armed Forces India 68(4):316-321.
Redhead, C. S., and V. K. Burrows. 2009. FDA tobacco regulation: The Family Smoking Prevention and Tobacco Control Act of 2009. Washington, DC: Congressional Research Service.
Reeder, S. 2014. Innovative state and local approaches: The Maryland transition age youth system change experience. Presentation at IOM Workshop to Explore the Current and Potential Roles of State Policies and Programs and Media and Information Technology, Washington, DC. http://www.iom.edu/~/media/Files/Activity%20Files/Children/ImprovingYoungAdultsHealth/Reeder%20Presentation.pdf (accessed September 5, 2014).
Richardson, A., V. Williams, J. Rath, A. C. Villanti, and D. Vallone. 2014. The next generation of users: Prevalence and longitudinal patterns of tobacco use among U.S. young adults. American Journal of Public Health 104(8):1429-1436.
Rickwood, D. J., F. P. Deane, and C. J. Wilson. 2007. When and how do young people seek professional help for mental health problems? Medical Journal of Australia 187(Suppl. 7):S35-S39.
Ridout, B., and A. Campbell. 2014. Using Facebook to deliver a social norm intervention to reduce problem drinking at university. Drug and Alcohol Review (2014):1-7.
Rivara, F. P., D. Boisvert, A. Relyea-Chew, and T. Gomez. 2011. Last call: Decreasing drunk driving among 21-34-year-old bar patrons. International Journal of Injury Control and Safety Promotion 19(1):53-61.
Robinson, J., S. E. Hetrick, and C. Martin. 2011. Preventing suicide in young people: Systematic review. Australian and New Zealand Journal of Psychiatry 45(1):3-26.
SAHRC (State Adolescent Health Resource Center). 2012. What is a state adolescent health coordinator? http://nnsahc.org/images/uploads/1-_AHC_Overview.pdf (accessed September 4, 2014).
SAHRC. 2014. State adolescent health coordinators & contacts. http://nnsahc.org/images/uploads/StateAHCwebroster.pdf (accessed July 14, 2014).
Sallis, J. F., N. Owen, and E. B. Fisher. 2008. Ecological models of health behavior. In Health behavior and health education: Theory, research, and practice, Vol. 4. San Francisco, CA: John Wiley & Sons, Inc. Pp. 465-485.
Salzberg, P. M., and J. M. Moffat. 2004. Ninety five percent: An evaluation of law, policy, and programs to promote seat belt use in Washington state. Journal of Safety Research 35(2):215-222.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2012. 2010-2011 National Survey on Drug Use and Health: Model-based prevalence estimates (50 states and the District of Columbia). http://www.samhsa.gov/data/NSDUH/2k11State/NSDUHsae2011/ExcelTabs/NSDUHsaeTables2011.pdf (accessed September 2, 2014).
SAMHSA. 2013. Results from the 2012 National Survey on Drug Use and Health: Summary of national findings. NSDUH series H-46, HHS publication no. (SMA) 13-4795. Rockville, MD: SAMHSA.
SAMHSA. 2014. The CBHSQ report: Serious mental health challenges among older adolescents and young adults. Washington, DC: Center for Behavioral Health Statistics and Quality, SAMSHA.
Santelli, J. S., K. Sivaramakrishnan, Z. R. Edelstein, and L. P. Fried. 2013. Adolescent risk-taking, cancer risk, and life course approaches to prevention. Journal of Adolescent Health 52(5):S41-S44.
Schilling, O. K., and M. Diehl. 2014. Reactivity to stressor pile-up in adulthood: Effects on daily negative and positive affect. Psychology and Aging 29(1):72-83.
Schmidt, S., and H. M. Parsons. 2014. Vaccination interest and trends in human papillomavirus vaccine uptake in young adult women aged 18 to 26 years in the United States: An analysis using the 2008-2012 National Health Interview Survey. American Journal of Preventive Medicine 104(5):946-953.
Schomerus, G., C. Auer, D. Rhode, M. Luppa, H. J. Freyberger, and S. Schmidt. 2012. Personal stigma, problem appraisal and perceived need for professional help in currently untreated depressed persons. Journal of Affective Disorders 139(1):94-97.
Schulenberg, J. E., and J. L. Maggs. 2002. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol and Drugs (14):54.
Scott, S. B., M. J. Sliwinski, and F. Blanchard-Fields. 2013. Age differences in emotional responses to daily stress: The role of timing, severity, and global perceived stress. Psychology and Aging 28(4):1076-1087.
Sepe, E., and S. A. Glantz. 2002. Bar and club tobacco promotions in the alternative press: Targeting young adults. American Journal of Public Health 92(1):75-78.
Shults, R. A., R. W. Elder, D. A. Sleet, J. L. Nichols, M. O. Alao, V. G. Carande-Kulis, S. Zaza, D. M. Sosin, and R. S. Thompson. 2001. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. American Journal of Preventive Medicine 21(4):66-88.
Sims, T. H., T. McAfee, D. L. Fraser, T. B. Baker, M. C. Fiore, and S. S. Smith. 2013. Quitline cessation counseling for young adult smokers: A randomized clinical trial. Nicotine & Tobacco Research 15(5):932-941.
Sinha, R., C. Easton, and K. Kemp. 2003. Substance abuse treatment characteristics of probation-referred young adults in a community-based outpatient program. American Journal of Drug and Alcohol Abuse 29(3):585-597.
Skov-Ettrup, L., L. Ringgaard, P. Dalum, T. Flensborg-Madsen, L. C. Thygesen, and J. S. Tolstrup. 2014. Comparing tailored and untailored text messages for smoking cessation: A randomized controlled trial among adolescent and young adult smokers. Health Education Research 29(2):195-205.
Smith, E. L., and A. Cooper. 2013. Homicide in the U.S. known to law enforcement, 2011. Washington, DC: Bureau of Justice Statistics.
Smith, L., and D. Foxcroft. 2009. The effect of alcohol advertising, marketing and portrayal on drinking behaviour in young people: Systematic review of prospective cohort studies. BMC Public Health 9(1):51.
Snyder, L. B., M. A. Hamilton, E. W. Mitchell, J. Kiwanuka-Tondo, F. Fleming-Milici, and D. Proctor. 2004. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. Journal of Health Communication: International Perspectives 9(Suppl. 1):71-96.
Sorensen, G., E. Barbeau, M. K. Hunt, and K. Emmons. 2004. Reducing social disparities in tobacco use: A social-contextual model for reducing tobacco use among blue-collar workers. American Journal of Public Health 94(2):230-239.
Spalter-Roth, R., T. A. Lowenthal, and M. Rubio. 2005. Race, ethnicity, and the health of Americans. http://www2.asanet.org/centennial/race_ethnicity_health.pdf (accessed August 18, 2014).
Stawski, R. S., M. J. Sliwinski, D. M. Almeida, and J. M. Smyth. 2008. Reported exposure and emotional reactivity to daily stressors: The roles of adult age and global perceived stress. Psychology and Aging 23(1):52-61.
Stewart, D. E., and G. E. Robinson. 1998. A review of domestic violence and women’s mental health. Archives of Women’s Mental Health 1(2):83-89.
Strecher, V. J., J. B. McClure, G. L. Alexander, B. Chakraborty, V. N. Nair, J. M. Konkel, S. M. Greene, L. M. Collins, C. C. Carlier, C. J. Wiese, R. J. Little, C. S. Pomerleau, and O. F. Pomerleau. 2008. Web-based smoking-cessation programs: Results of a randomized trial. American Journal of Preventive Medicine 34(5):373-381.
Tapp, A., A. Pressley, M. Baugh, and P. White. 2013. Wheels, skills and thrills: A social marketing trial to reduce aggressive driving from young men in deprived areas. Accident Analysis & Prevention 58:148-157.
Testa, M., J. H. Hoffman, J. A. Livingston, and R. Turrisi. 2010. Preventing college women’s sexual victimization through parent based intervention: A randomized controlled trial. Prevention Science 11(3):308-318.
Valente, S. M., J. M. Saunders, and M. Z. Cohen. 1993. Evaluating depression among patients with cancer. Cancer Practice 2(1):65-71.
van der Pol, P., N. Liebregts, R. de Graaf, D. J. Korf, W. van den Brink, and M. van Laar. 2013. Facilitators and barriers in treatment seeking for cannabis dependence. Drug and Alcohol Dependence 133(2):776-780.
Villanti, A. C., H. S. McKay, D. B. Abrams, D. R. Holtgrave, and J. V. Bowie. 2010. Smoking-cessation interventions for U.S. young adults: A systematic review. American Journal of Preventive Medicine 39(6):564-574.
Viswanath, K. 2006. Public communications and its role in reducing and eliminating health disparities. In Examining the health disparities research plan of the National Institutes of Health: Unfinished business, edited by G. E. Thomson, F. Mitchell, and M. B. Williams. Washington, DC: The National Academies Press. Pp. 215-253.
Viswanath, K., and J. R. Finnegan. 2002. Reflections on community health campaigns: Secular trends and the capacity to effect change. In Public health communication: Evidence for behavior change, edited by R. C. Hornik. Mahwah, NJ: Lawrence Erlbaum Associates. Pp. 289-313.
Viswanath, K., L. K. Ackerson, G. Sorensen, and P. C. Gupta. 2010a. Movies and TV influence tobacco use in India: Findings from a national survey. PLoS ONE 5(6):e11365.
Viswanath, K., R. S. Herbst, S. R. Land, S. J. Leischow, and P. G. Shields. 2010b. Tobacco and cancer: An American association for cancer research policy statement. Cancer Research 70(9):3419-3430.
Viswanath, K., R. McCloud, S. Minsky, E. Puleo, E. Kontos, C. Bigman-Galimore, R. Rudd and K. M. Emmons. 2013. Internet use, browsing, and the urban poor: Implications for cancer control. Journal of the National Cancer Institute Monographs 2013(47):199-205.
Volkow, N. D., R. D. Baler, W. M. Compton, and S. R. Weiss. 2014. Adverse health effects of marijuana use. New England Journal of Medicine 370(23):2219-2227.
Wagenaar, A. C., and T. L. Toomey. 2002. Effects of minimum drinking age laws: Review and analyses of the literature from 1960 to 2000. Journal of Studies on Alcohol (Suppl. 14):206-225.
Wakefield, M. A., B. Loken, and R. C. Hornik. 2010. Use of mass media campaigns to change health behaviour. Lancet 376(9748):1261-1271.
Werch, C. E. C., M. J. Moore, H. Bian, C. C. DiClemente, I. Huang, S. C. Ames, D. Thombs, R. M. Weiler, and S. B. Pokorny. 2010. Are effects from a brief multiple behavior intervention for college students sustained over time? Preventive Medicine 50(1):30-34.
WHO (World Health Organization). 2001. The world health report 2001—Mental health: New understanding, new hope. Geneva, Switzerland: WHO.
Williams, A. F., and J. K. Wells. 2004. The role of enforcement programs in increasing seat belt use. Journal of Safety Research 35(2):175-180.
Williams, A. F., D. Reinfurt, and J. K. Wells. 1996. Increasing seat belt use in North Carolina. Journal of Safety Research 27(1):33-41.
Williams, G., M. P. Hamm, J. Shulhan, B. Vandermeer, and L. Hartling. 2014. Social media interventions for diet and exercise behaviours: A systematic review and meta-analysis of randomised controlled trials. BMJ Open 4(2)1-16.
Wingood, G. M., R. J. DiClemente, K. Villamizar, D. L. Er, M. DeVarona, J. Taveras, T. M. Painter, D. L. Lang, J. W. Hardin, E. Ullah, J. Stallworth, D. W. Purcell, and R. Jean. 2011a. Efficacy of a health educator-delivered HIV prevention intervention for Latina women: A randomized controlled trial. American Journal of Public Health 101(12):2245-2252.
Wingood, G. M., J. J. Card, D. Er, J. Solomon, N. Braxton, D. Lang, P. Seth, J. Cartreine, and R. J. Diclemente. 2011b. Preliminary efficacy of a computer-based HIV intervention for African-American women. Psychology & Health 26(2):223-234.
Wolfson, M., H. Champion, T. P. McCoy, S. D. Rhodes, E. H. Ip, J. N. Blocker, B. A. Martin, K. G. Wagoner, M. C. O’Brien, E. L. Sutfin, A. Mitra, and R. H. DuRant. 2012. Impact of a randomized campus/community trial to prevent high-risk drinking among college students. Alcoholism: Clinical and Experimental Research 36(10):1767-1778.
Wood, S. 2014. Colorado9to25. Presentation at IOM’s Improving the Health, Safety, and Well-Being of Young Adults: A Workshop on State Policies and Programs and Social Media and Information Technology, Washington, DC. http://www.iom.edu/~/media/Files/Activity%20Files/Children/ImprovingYoungAdultsHealth/Wood%20Presentation.pdf (accessed September 5, 2014).
Wright, A., M. G. Harris, J. H. Wiggers, A. F. Jorm, S. M. Cotton, S. M. Harrigan, R. E. Hurworth, and P. D. McGorry. 2005. Recognition of depression and psychosis by young Australians and their beliefs about treatment. Medical Journal of Australia 183(1):18-23.
Wu, L. T., D. J. Pilowsky, W. E. Schlenger, and D. Hasin. 2007. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatric Service 58(2):192-200.
Zakrajsek, J. S., J. T. Shope, A. I. Greenspan, J. Wang, C. R. Bingham, and B. G. Simons-Morton. 2013. Effectiveness of a brief parent-directed teen driver safety intervention (checkpoints) delivered by driver education instructors. Journal of Adolescent Health 53(1):27-33.












































































