Key Findings
- Young adults have significantly lower rates of health care system utilization compared with other groups, but significantly higher emergency room visit rates compared with those immediately younger and older than them. These lower utilization rates do not necessarily indicate better health; for example, the use of specialty psychiatric services by those with mental health conditions falls from approximately 20 percent of adolescents to about 10 percent of young adults.
- The transition from child to adult medical and behavioral health care often is associated with poor outcomes among young adults. Challenges include discontinuities in care, differences between the child/adolescent and adult health systems, a lack of available adult providers, difficulties in breaking the bond with pediatric providers, lack of payment for transition support, a lack of training in childhood-onset conditions among adult providers, the failure of pediatric providers to prepare adolescents for an adult model of care, and a lack of communication between pediatric and adult providers and systems of care.
- Young adulthood provides an important opportunity for prevention. Serious illnesses and disorders can be avoided or mana-
-
ged better if young adults are engaged in wellness practices and screened for early signs of or untreated illness, and the risk taking that is common during these years can impact lifelong functioning. Yet young adults rarely receive preventive counseling on important issues for this age group, such as smoking and mental health, and there is no consolidated package of preventive medical, behavioral, and oral health guidelines specifically focused on the young adult population.
- While there are effective behavioral health treatments and strategies for adults, the efficacy of these treatments specifically for young adults is largely undemonstrated because typical clinical trials and research studies (e.g., studies of adults aged 18-55) are insufficient to establish efficacy in young adults.
- Young adults without health insurance or with gaps in insurance coverage are less likely to access health services than young adults who are continuously insured. Health insurance coverage rates for young adults, however, have historically been the lowest of any age group. Certain groups of young adults—such as young adults exiting the foster care system, young adults involved in the justice system, and unauthorized immigrants—have particular difficulties in obtaining health care coverage. The Patient Protection and Affordable Care Act and state-level efforts are increasing coverage for many young adults, including young adults who age out of the foster care system, but others, such as unauthorized immigrants, remain outside the system.
Young adults often are perceived as healthy and as low users of health care, and recent attention has focused primarily on enrolling young adults in health care insurance to offset the higher costs associated with care for older adults. However, while young adults are clearly an important priority population for health insurance coverage, there also needs to be an expanded focus on improving the health care system’s ability and capacity to serve them. Important opportunities exist within the health care system to improve young adults’ health, safety, and well-being in both the short and long terms. Yet many young adults face serious challenges in accessing and navigating the health care system, with potentially serious repercussions.
Young adulthood provides an important opportunity for prevention. Serious illnesses or disorders can be avoided or managed better if young adults are engaged in wellness practices and screened for early signs of
or untreated illness. Furthermore, as described in earlier chapters, young adulthood is an age not only of opportunities, but also of risks that can impact lifelong functioning. Keeping young adults as healthy as possible during this critical stage of life may support more positive pathways into mature adulthood. Young adulthood also provides an opportunity to help young adults access and learn to navigate the adult health care system and develop the ability to work directly with health care providers to manage their health care more effectively.
Among the many young adults who are parents, moreover, there is an opportunity to minimize the potential impact of their behavioral and physical health problems on their children. For example, alcohol, tobacco, or drug use during pregnancy increases the likelihood of long-term cognitive and emotional development problems, such as attention-deficit hyperactivity disorder (ADHD), conduct problems, and lower school achievement, in the child (Knopik, 2009; Minnes et al., 2011). And children of depressed parents have three times the risk of anxiety disorders, major depression, and substance dependence compared with children of nondepressed parents (Weissman et al., 2006). Use of cognitive-behavioral therapies with parents with mental illness can help reduce mental health disorders in their children (Siegenthaler et al., 2012).
In addition to the challenges that almost all adults face in accessing and navigating a complicated health system, two challenges are particularly relevant for young adults: the transition from child to adult systems and the onset of certain health conditions, such as serious mental illness. Young adults are transitioning from pediatric to adult health care providers and from the child to the adult behavioral health system, and these new systems of care often differ significantly from those they used as children and adolescents. Some struggle as they assume primary responsibility for their health care for the first time. The health system may not be set up in ways that young adults find easy to use, and providers sometimes lack young adult–specific content knowledge and the skills needed to work effectively with this age group. This transition is widely recognized as challenging for those with
“Even with insurance, it is still hard to access health care. It is so complicated and you don’t really learn in school how to navigate it.”*
__________________
* Quotations are from members of the young adult advisory group during their discussions with the committee.
chronic illness, but it is also essential that all young adults make a successful transition to the adult health care system to ensure they receive preventive services that help them remain in good health, as well as the comprehensive array of physical and behavioral health services many of them need. Box 7-1 summarizes barriers discussed in the remainder of this chapter that impede young adults from accessing and continuing to use health care.
BOX 7-1
Barriers to Optimal Health Care for Young Adults
The following are barriers faced by young adults in accessing care and/or continuing to receive care in the health care system:
- Transitions
- − navigating the differences between pediatric and adult health care providers, including differences in treatment culture, family involvement, and care coordination;
- − discontinuity of care caused by age-based changes in eligibility criteria or target populations for behavioral health services and management of chronic medical conditions; and
- − changes in insurance coverage.
- Content
- − no unified set of young adult preventive care guidelines; and
- − significant gaps in interventions and treatments with strong evidence of efficacy for young adults, particularly in preventive and behavioral health.
- Cost and difficulty of obtaining health care coverage.
- Young adults’ lack of health literacy and knowledge of how to access and complete the enrollment process, identify providers in the community, and navigate the health system.
- The stigma of behavioral health and substance abuse problems.
- Systems issues
- − few incentives to provide transition care, preventive care, counseling, and health education, particularly about treatment for or early signs of mental health problems and risk behaviors such as substance use;
- − inconsistency among pediatric systems in offering adolescent patients and their families preparation and planning for the transition to adult systems and for an adult model of care;
- − adult systems’ being unfamiliar with how to engage and integrate young adults into their practice;
- − inadequate health care provider training and skills for caring for adult manifestations of childhood diseases; and
- − confidentiality concerns.
Health systems are currently undergoing significant changes that affect both young adults and the general population. A key provision of the Patient Protection and Affordable Care Act (ACA) is the requirement that health insurance plans extend dependent coverage so that young adults can be added to a parent’s plan until they turn 26; several states also had initiated expansion of insurance coverage before the ACA was enacted (Blum et al., in press). Driven by advocacy goals and the fiscal need to enroll healthy individuals to offset the cost of older and sicker individuals, the White House, states, health insurance companies, and advocacy organizations across the country have recently developed campaigns to increase young adult enrollment in insurance plans (e.g., Colorado Consumer Health Initiative and ProgressNow Colorado Education, 2014; HealthSource RI, 2014; Ostrom, 2014; Young Invincibles, 2014). Results of a 2013 survey indicate that of 15 million 19- to 25-year-olds who enrolled in a parent’s plan, 7.8 million would not have been able to do so prior to the ACA (Collins et al., 2013). In addition, federal surveys suggest that 1-3 million previously uninsured young adults have gained coverage since this provision took effect (Blumenthal and Collins, 2014). This change is likely to have a significant impact on young adults’ relationship with the structure and content of the health care system for years to come, and the evolving system offers opportunities for integrating further changes to benefit young adults.
In this chapter, we examine young adults in the health care system and provide recommendations for improving the system’s role in enhancing their health, safety, and well-being. As described in Chapter 1, the term health care is used broadly in this report to include both physical and behavioral health, and the term behavioral health encompasses the promotion of emotional health; the prevention of mental and substance use disorders; and treatments and services for substance abuse, addiction, and mental and substance use disorders (SAMHSA, 2011). Since the epidemiology of young adults is covered in greater depth in Chapters 2 and 6, this chapter focuses on health care delivery.
We first briefly describe where young adults currently receive health care services and what services they use. We then explore in turn transitions from pediatric to adult medical health care systems and from child to adult behavioral health care systems, preventive care for young adults, behavioral health interventions for young adults, health care coverage, and systems issues related to young adults. The chapter ends with conclusions and recommendations for improving health care for young adults. Note that the primary recommendations offered in this chapter are applicable to health systems in a variety of forms and are not restricted to specific implementations of the ACA. Some of our suggestions are not exclusive to young adults, but with the current large influx of young adults into the
system, there is an opportunity to think about how to get the system right for them and then extend it to others.
CURRENT USE OF HEALTH CARE BY YOUNG ADULTS
Comprehensive care with a medical home does not appear to characterize the health care delivery system for young adults as compared with children and adults (for a discussion of medical homes for 10- to 17-year-olds, see Adams et al., 2013).1 An analysis of health care utilization conducted before the passage of the ACA found that young adults had significantly lower health care system utilization rates than other groups (see Table 7-1). Specifically, this age group had significantly lower rates of office-based and dental visits. Of interest is that young adults had significantly higher emergency room visit rates compared with those immediately younger and older than them. In addition, the use of specialty psychiatric services by those with mental health conditions falls from approximately 20 percent of adolescents to about 10 percent of young adults (Copeland et al., in press). The use of services in general—including medical care, educational and job services, and services provided through organizations such as Big Brother—by individuals with mental health conditions drops from about half of adolescents to a quarter of young adults.
“I would like to receive my health information from my doctor. The problem here is that I only go to the doctor when things go wrong, as do many other young adults.”
The prevalence and trends of the major health-related problems affecting young adults are discussed extensively in Chapters 2 and 6. Table 7-2 highlights the percentages of young adults utilizing the various types of health care services. This table shows that small percentages of young adults received care for substance use and mental health disorders, even though more than 50 percent reported having a usual source of care and having received a routine general checkup within the past 12 months, and even though early young adulthood is often when the burden of illness emerges for substance abuse and mental health conditions. Emergency rooms represent a major component of care for young adults, utilized by an estimated 15 to 20 percent of this age group (Fortuna et al., 2010; Lau et al., 2014a), although evidence from three states suggests that the ACA
__________________
1 The patient-centered medical home is a model for primary care that promotes effective care coordination, accessibility, quality, and safety (AAFP et al., 2007; IOM, 2013a).
TABLE 7-1 Past-Year Health Care Utilization Rates by Age Group: 2009 Medical Expenditure Panel Survey (rates adjusted for pregnancy)
| Children (aged 0-11) | Adolescents (aged 12-17) | Young Adults (aged 18-25) | Adult (aged 26-44) | Adult (aged 45-64) | Adult (aged 65+) | |
| Utilization % had any health care utilization |
88%*** | 83%*** | 72% | 78%*** | 89%*** | 97%*** |
| Office-based visits % had visit(s) |
77%*** | 67%*** | 55% | 65%*** | 79%*** | 91%*** |
| Hospital outpatient visits % had visit(s) |
7% | 5%* | 7% | 12%*** | 20%*** | 30%*** |
| Emergency room visits % had visit(s) |
15% | 12%** | 15% | 12%** | 12%*** | 17% |
| Inpatient hospitalizations % had visit(s) |
2%*** | 4%*** | 5% | 6% | 7%* | 19%*** |
| Prescription medications % had prescription(s) |
50% | 49% | 48% | 57%*** | 75%*** | 92%*** |
| Dental visits % had visit(s) |
44%*** | 53%*** | 34% | 37%* | 47%*** | 44%*** |
NOTES: Hospital outpatient visits are to general clinics that are hospital-based. ***p<0.001, **p<0.01, *p<0.05.
SOURCES: Adapted from Lau et al., 2013a, 2014a.
TABLE 7-2 Health Service Utilization by Type of Service
| Variable | Year | % | Source |
| Preventive Care: Attended a preventive care visit within the past 12 months (ages 18-25) | 2011 | 48 | MEPS |
| Mental Health: Received any mental health treatment/counseling in the past year (does not include substance abuse treatment) (ages 18-25) | 2012 | 12 | NSDUH |
| Substance Abuse: Received treatment at any location for illegal drug or alcohol use in the past year (ages 18-25) | 2012 | 2.4 | NSDUH |
| Reproductive Health: Among all women (ages 20-24), used sexual and reproductive health services | 2006-2010 | 72 | NSFG |
| Reproductive Health: Among sexually experienced women (ages 20-24), used | 2006-2010 | NSFG | |
|
Any sexual and reproductive health services |
81 | ||
|
Contraceptive services |
64 | ||
|
Services for sexually transmitted infections (STIs) |
30 | ||
| Emergency Care: Proportion of young adults’ (ages 20-29) health care visits occurring in the emergency department | 2006 | 22 | NAMCS |
| Dental Care: Had a dental visit in the past 12 months (ages 19-25) | 2012 | 59 | NHIS |
NOTE: MEPS = Medical Expenditure Panel Survey; NAMCS = National Ambulatory Medical Care Survey; NHIS = National Health Information Survey; NSDUH = National Survey on Drug Use and Health; NSFG = National Survey of Family Growth.
SOURCES: MEPS: Lau et al., 2014b; NAMCS: Fortuna et al., 2010; NHIS: Vujicic et al., 2014; NSDUH: SAMHSA, 2013a,b; NSFG: Hall et al., 2012.
has reduced emergency department use (Hernandez-Boussard et al., 2014). There appear to be no population data documenting the use of services for management of chronic medical or mental health conditions for young adults.
Most young adults face the challenge of accessing a new health care system and new health care team independently of their parents or guardians. In addition to the differences between pediatric and adult health care systems and the possibility that the adult system is less well suited to their developmental stage, they may have changes in insurance coverage and face confidentiality concerns. These challenges are amplified when the young
adult has a chronic physical or mental health condition that requires ongoing coordinated care. Pediatric providers may not prepare adolescents for an adult model of care, and there is a lack of adult providers who are familiar with managing the adult progression of childhood chronic diseases (AAP et al., 2011). In this section, we first examine the transition from pediatric to adult medical health care for young adults with chronic health conditions, and we then we explore transitions in behavioral health care and substance abuse treatment. While much of the published literature focuses on the transition challenges for those with chronic illness, requiring close medical care, there appears to be no systematic coordination of the transition to adult care for those without chronic medical conditions. It is important to improve the transition process for all youth moving to the adult health care system, not just those who have identified chronic medical conditions.
“Even if you have private insurance and you are transitioning from pediatric care to adult care, you are just kind of on your own in terms of finding doctors, in terms of figuring out how the system works. I didn’t particularly have anybody to help me go through that process. I had to figure it out on my own. I am still figuring it out.”
Transitions for Young Adults with Chronic Health Conditions
As noted, most transition research has focused on young adults with chronic health conditions, including cystic fibrosis, rheumatological diseases, diabetes mellitus, sickle cell anemia, acute lymphocytic leukemia (ALL), organ transplant, inflammatory bowel disease, and congenital heart disease (CHD). In this context, transition has been defined as “the purposeful, planned movement of adolescents and young adults with chronic physical and medical conditions from child-centered to adult-oriented health care systems” (Blum et al., 1993, p. 570). Although it is recommended that transition planning begin during early adolescence, expert consensus suggests that the actual transfer should generally occur during the early young adult years, between ages 18 and 21 (AAP et al., 2011). Before young adults reach the age at which they can legally make their own decisions regarding their care, which could include discontinuing or not accepting available treatment, it is important that they understand their own health conditions and have the tools needed to make such decisions.
The transition from pediatric to adult care is a time of vulnerability
that can result in poor outcomes among individuals with chronic health conditions. Poor health outcomes can result from discontinuities of care during the transition process itself, including difficulties identifying a new care team. In a survey of more than 900 adults with CHD, 42 percent reported a lapse of care of more than 3 years, and 8 percent reported a lapse of greater than 10 years; the most frequent age at which lapses occurred was 20 (Gurvitz et al., 2013). Further, a study of 360 young adults (aged 19-21) in Canada with CHD showed that more than one-quarter had not seen a cardiologist since the age of 18 (Reid et al., 2004). These health care lapses among young adults with CHD result in poor health outcomes (Kovacs and McCrindle, 2014).
Concerns also arise regarding young adults’ health outcomes after they have transitioned into adult care. For example, a study of 185 participants found that young adults with diabetes had poor glycemic control after they transitioned from pediatric to adult care compared with those young adults who did not make this transition (Lotstein et al., 2013). A large retrospective study of sickle cell disease–related emergency department visits and hospitalizations found that young adults aged 18-30 had higher rates of acute care encounters and rehospitalizations compared with those immediately younger and older (Brousseau et al., 2010). A longitudinal study of individuals with sickle cell disease also found that deaths most frequently occurred after age 18 and after the transfer to adult care (Quinn et al., 2010), although stronger data are needed to fully support the conclusion that the transfer caused the poorer outcomes (DeBaun and Telfair, 2012). In addition, a recent study found increased intubation risk and longer lengths of stay for those young adults (aged 16-25) with sickle cell disease and acute chest syndrome who were cared for in adult hospitals versus those who were cared for in pediatric hospitals (Jan et al., 2013).
Barriers to implementing an effective system to improve transitions have been well documented (e.g., McManus et al., 2008). Some of the critical barriers include those mentioned above: a lack of trained adult providers able to accept young adults with adult manifestations of childhood chronic illnesses, apprehension among patients and families and pediatric providers that care will be compromised during transition, lack of reimbursement for recommended transition practices, a lack of tools with which to assess readiness for transition, and a lack of time for the provider (McManus et al., 2008). The uptake of better practices also has been hampered by the lack of widespread dissemination of research findings.
Despite these challenges, it is possible to plan for a smooth transition with good outcomes. In the case of cystic fibrosis, a chronic illness for which more programs have been implemented for transition care relative to most childhood conditions, a recent study contradicts many previous studies, finding that those who transitioned to adult care had a less rapid
decline in respiratory status than patients with similar characteristics who stayed in pediatric care (Tuchman and Schwartz, 2013). These inconsistent research results necessitate greater focus on what constitutes the content of the most effective health care for these and other populations of young adults.
Along with increases in life expectancy in recent decades, many more children with serious childhood-onset diseases are now living into the young adult years. For example, 25 years ago, approximately 30 percent of people with cystic fibrosis were age 18 or older, whereas today approximately half of people with cystic fibrosis are adults, and the median predicted survival age is over 40 (CFF, 2012). This change underscores the need for a successful transition to adult health care. Next we further explore reasons behind the poor outcomes associated with that transition.
Limitations of Adult Health Care Providers’ Familiarity with the Disease Process and Developmental Needs of Young Adults
Because many individuals with serious congenital and childhood-onset diseases are now living into the young adult years, many are now receiving care from adult-focused health professionals who previously did not see patients with these diseases and may not have received training in these areas (e.g., Tuchman et al., 2010). From a neurosurgery perspective, for example, caring for an individual with childhood-onset hydrocephalus is very different from caring for an adult in whom this condition emerged as a result of hemorrhage, infection, or tumor (Simon et al., 2009). In a survey, only 15 percent of general internists felt comfortable providing primary care to adults with cystic fibrosis, and 32 percent felt comfortable providing primary care to adults with sickle cell disease (Okumura et al., 2008). In another survey, a lack of training was cited by 24 percent of general internists as a significant or severe limitation on their ability to treat young adults with childhood-onset chronic diseases, although these reports were not statistically associated with physicians’ perceived quality of care (Okumura et al., 2010).
In addition, disease manifestation in young adults may differ from that in older adults. Health care providers who provide care for conditions that most commonly affect older adults, such as cancer, may be less familiar with the disease process in young adults. Studies on adolescent and young adult oncology training for health professionals have emphasized the importance of understanding tumor biology, pointing out that the epidemiology and biology are different for many cancers in adolescents and young
adults compared with children and older adults (Bleyer and Barr, 2009; Bleyer et al., 2008; Hayes-Lattin et al., 2010).2 Similarly, young adults may have different concerns and psychosocial needs than older adults. For example, fertility preservation is a great concern for young adults with cancer (Gupta et al., 2013). Young adults with cancer also have a high desire for information and services in the areas of cancer diagnosis, nutrition, physical activity, complementary and alternative services, and health insurance assistance (Gupta et al., 2013; Zebrack, 2008). However, research also indicates that these needs frequently go unmet; in a survey of 217 young adults with cancer, 40-50 percent of respondents indicated that these needs were unmet (Zebrack, 2008). These young adults also expressed needs for or interests in services and supports such as “camp programs and retreats, counseling or guidance related to sexuality, counseling for family members, infertility treatment and adoption services, transportation assistance, child care, and alcohol or drug abuse counseling” (Zebrack, 2008, p. 1). Again, more than 50 percent reported that these needs were unmet. A comparison by age showed that young adults aged 18-29 had greater unmet needs than those aged 30-40.
Differences Between the Child and Adult Medical Care Systems
In pediatric longitudinal studies over the last few decades, the 5-year survival rate for pediatric ALL has increased to 90 percent (Robison, 2011). Unfortunately, there has been no similar increase for adolescent and young adult ALL; currently, the overall survival rate for adults is 30-40 percent (Narayanan and Shami, 2012). Yet there is evidence that treatment in a pediatric cancer center increases survival for adolescents and young adults (De Bont et al., 2004; Peppercorn et al., 2004; Ramanujachar et al., 2006). Box 7-2 examines potential reasons for this difference. In the case of cancer treatment, it may be that the transition to adult care should be based not on age but on disease outcome, meaning that some people may need to have pediatric subspecialty care even though they have transitioned to adult primary care and taken on adult roles in other areas of life.
Like some adult providers, adult health systems are new to providing care to large numbers of young adults with serious childhood-onset diseases. Until the 1980s, for example, only childhood cystic fibrosis centers existed (Tuchman et al., 2010). Now that many more individuals with the disease are living well into adulthood, adult programs have been developing, but in many cases they are provided in the same location as pediatric programs, and adult patients often are hospitalized in pediatric settings
__________________
2 In this field, “adolescents and young adults with cancer” are typically defined as those aged 15-39 (NCI, 2014).
BOX 7-2
Caring for Young Adults with Chronic Diseases in Pediatric Versus Adult Settings
Adolescents and young adults with chronic diseases such as cancer and sickle cell disease generally have better outcomes if treated in pediatric rather than adult centers (De Bont et al., 2004; Jan et al., 2013; Peppercorn et al., 2004; Ramanujachar et al., 2006). This difference persists even when young adults are treated in the adult system using pediatric protocols. The factors that account for this difference are not yet clear, but the following may be factors: wraparound care, a developmental approach, and familiarity with the disease in pediatric care systems. The latter is especially the case with diseases such as acute lymphocytic leukemia (ALL) that can be considered pediatric diseases that either persist into adulthood or have their onset in late adolescence or young adulthood (Narayanan and Shami, 2012).
An important question is whether young adults should be kept longer in pediatric settings or changes can be made to the adult health care system. An argument for the former approach is that adult care systems are burdened with a growing elderly population and lack the resources to care for young adults. On the other hand, one could argue that keeping young adults in pediatric centers does not facilitate their being treated as adults with appropriate preventive care and confidentiality, and that adult systems are not being encouraged to develop appropriate systems of care based on a life span approach. Additional research on this question is needed.
Despite this open question, institutions are already reacting to the evidence of past poorer outcomes in adult systems by building systems within children’s hospitals to care for adolescents and young adults. Examples include the Adolescent and Young Adult Cancer Program at Seattle Children’s Hospital (Seattle Children’s Hospital, 2014) and the Adolescent and Young Adult Program at MD Anderson Children’s Cancer Hospital in Texas (MD Anderson Cancer Center, 2014).a In addition, some adult systems are creating follow-up clinics especially for those with pediatric-onset diseases. An example is the Thriving After Cancer clinic at the George Washington Cancer Institute/George Washington University Medical Faculty Associates, which provides care that addresses young adults’ needs in an appropriate adult setting (GW Cancer Institute, 2014; personal communication, September 17, 2014, April Barbour, M.D., The George Washington Medical Faculty Associates).
____________
a For additional examples of care programs for adolescents and young adults with cancer, see IOM (2013b).
(Tuchman et al., 2010). Thus the age-appropriateness of care offered for adult patients in a pediatric setting is a concern (AAP et al., 2011). In the survey by Okumura and colleagues, physicians responded that a lack of subspecialty access and having an office structure that did not facilitate coordination of care for young adults with special health care needs had
the greatest negative impact on their perceived quality of care (Okumura et al., 2010). In another study, internists saw a need to obtain the consent of young adults for family involvement in their care (Peter et al., 2009).
Studies on the perspectives of patients, providers, and families underscore the general discomfort with and lack of a structured process for the transition to adult health care (Peter et al., 2009; Reiss et al., 2005). Some pediatric providers who have developed successful relationships with patients and their families delay transitioning young adults to adult care because of “difficulty letting go,” previous experiences with difficult patient transitions, and the perception that the transfer will result in negative health outcomes (Reiss et al., 2005). An American Academy of Pediatrics (AAP) survey of pediatric providers’ activities related to transition found that few offered youth and their families preparation for transitioning to an adult model of care at age 18, communicated directly with the adult provider, offered medical summaries for the youth/family and the adult provider, and/or created a medical transition plan (McManus et al., 2008). Also of note is the internist perspective that there is a need for better training in congenital and childhood-onset conditions and an urgent need for more training for adult subspecialists (Peter et al., 2009). The perspectives of patients and physicians, coupled with concern for financial support to care for these complex patients, are important factors in successful planning for transition by all concerned (Peter et al., 2009).
Efforts to Improve the Transition Process
The transition from pediatric to adult care has been identified as a problem for decades. Yet there has been minimal systematic implementation and evaluation of institutional change to address concerns about the increasing numbers of pediatric patients with chronic conditions who are now living into adulthood.
“At my age—19—my friends and I don’t even know the first thing about looking into health care services. I think that it would be very beneficial to start educating us about these things now rather than later.”
Multiple consensus studies have been published on the transition from pediatric to adult care, starting with a Surgeon’s General Conference in 1989 (AAP, 1996; AAP et al., 2002, 2011; Blum et al., 1993; Magrab and Millar, 1989). The 2011 recommendations of the AAP, American Academy of Family Physicians (AAFP), and American College of Physicians (ACP) identify best practices in transitions (see Box 7-3)
BOX 7-3
Recommendations for Successful Transitions from the American Academy of Pediatrics (AAP), American Academy of Family Physicians (AAFP), and American College of Physicians (ACP)
AAP, AAFP, and ACP have together developed a health care transitions planning algorithm for all youth and young adults in medical home settings. The plan components are (a) assess for transition readiness, (b) plan a dynamic and longitudinal process for accomplishing realistic goals, (c) implement the plan through education of all involved parties and empowerment of the youth in areas of self-care, and (d) document progress to enable ongoing reassessment and movement of medical information to the receiving (adult care) provider. These apply to all youth and young adults, and the guidelines provide additional information for youth and young adults with special health care needs.
The document also identifies the following educational and policy recommendations for the transition from pediatric to adult health care systems:
- enhanced payment for transition services;
- case finding of those in need of transition services who are not receiving them;
- insurance coverage for patients in need of transition planning;
- standards of care and credentialing of providers;
- training for primary care physicians and medical subspecialists to promote transitions within the medical home; and
- promotion of training and clinical learning experience on transition and transfer of youth and young adults (both with and without special needs) for trainees in all medical fields.
SOURCE: AAP et al., 2011.
and state that additional elements of health care delivery and reimbursement systems are needed to achieve a successful transition (AAP et al., 2011). Recently, the Agency for Healthcare Research and Quality (AHRQ) published a technical brief on transition for children with special health care needs that reiterates many of the same findings published in 1989 (McPheeters et al., 2014). Efforts also have been made to apply the Institute for Healthcare Improvement’s Triple Aim3 framework to this transition (Benson et al., 2014; Berwick et al., 2008).
__________________
3 The Institute for Healthcare Improvement’s Triple Aim framework is aimed at achieving three goals: “Improving the patient experience of care (including quality and satisfaction); improving the health of populations; and reducing the per capita cost of health care” (IHI, 2014).
Various federal agencies support transition-related activities. For example, the Got Transition initiative/Center for Health Care Transition Improvement, a cooperative agreement between the Health Resources and Services Administration’s (HRSA’s) Maternal and Child Health Bureau and the National Alliance to Advance Adolescent Health, aims to improve health care transitions by developing and expanding the use of transition materials, training the workforce, enhancing youth and parent leadership, promoting health system changes, and serving as a resource clearinghouse (The National Alliance to Advance Adolescent Health, 2014a). This initiative has developed updated recommended core elements (Six Core Elements of Transition) for pediatric, internal medicine, family medicine, and med-peds4 practices (The National Alliance to Advance Adolescent Health, 2014b):
- establishing a transition policy,
- tracking and monitoring transition progress,
- conducting transition readiness assessments,
- planning for adult care,
- transferring into adult care (if applicable), and
- integrating the young adult into an adult practice.
Materials are organized and customized for three different situations, with corresponding types of health care providers:
- transitioning youth to adult health care providers (pediatric, family medicine, and med-peds providers);
- transitioning to an adult approach to health care without changing providers (family medicine and med-peds providers); and
- integrating young adults into adult health care (internal medicine, family medicine, and med-peds providers) (The National Alliance to Advance Adolescent Health, 2014b).
These recommended core elements and available customizable tools are based on the AAP/ACP/AAFP Clinical Report (2011) and were created using the quality improvement approach outlined by the Institute for Healthcare Improvement’s change framework. This approach may set the stage for less fragmentation of care in transition, with clear guidance for coordination and communication between pediatric and adult providers, improved preparation for the transfer to adult health care, improved integration of young adults as a special population into the adult health care setting, and ways to evaluate the transition process.
__________________
4 Combined internal medicine and pediatric practice.
Similarly, the Substance Abuse and Mental Health Services Administration (SAMHSA) sponsors the Emerging Adulthood Initiative. This initiative is focused on improving outcomes among adolescents and young adults with serious mental health conditions as they transition to adulthood, including transitions in health care (Georgetown University Center for Child and Human Development, 2014).
Beyond the transition issues for children with chronic medical conditions, health systems need to accommodate the needs of young adults who do not have a chronic condition but still have increased health care needs due to their stage of development and heath behaviors and the emergence of new mental and physical health conditions. The increased emergency room utilization noted above may speak to the difficulty experienced by young adults in transitioning to the adult health care system and their unmet health needs.
Behavioral Health Care Transitions
Behavioral health care systems typically are separate from medical health care systems, and include both mental health and substance abuse systems. The 1999 Surgeon General’s report on mental health describes the “de facto” mental health system as comprising four sectors (a description that applies equally well to substance abuse services): “the specialty mental health sector, the general medical/primary care sector, the human services sector, and the voluntary support network sector” (HHS, 1999, p. 73).
Funding of this de facto system generally is split between public/government sources (e.g., Medicaid, Medicare, state funding) and private sources (including services provided through private funding and services provided directly by private agencies, such as employer-provided insurance) (HHS, 1999). Behavioral health services may be office based (typically 1-6 hours/week), home based (usually more intensive than office-based treatment), intensive outpatient (in which clients sleep at home but receive treatment for several hours per day), residential/inpatient, and intensive inpatient (which includes more extensive medical care, typically for a relatively brief period of time). Until recently, private insurance often limited payment for treatment to a restrictive amount that was easily exceeded by more serious treatment needs. Individuals then either paid out of pocket or applied to the public sector for services (HHS, 1999).
The Mental Health Parity and Addiction Equity Act, enacted in 2008, targets reducing the large disparity in insurance coverage for behavioral and physical health treatment. The legislation requires insurance groups to provide the same level of benefits they provide for general medical treatment for mental health or substance use disorders. Under final rules for this act, effective July 1, 2014, deductibles for behavioral health must be on par with
those for similar services for other medical conditions, and treatment limits or co-pays more restrictive than those for medical/surgical services are prohibited. Standards for reimbursement for psychosocial treatments also are being discussed, and the Institute of Medicine (IOM) has been asked to conduct a study to develop a framework for establishing efficacy standards for psychosocial interventions used to treat mental disorders; the results of these discussions will have important implications for young adults (Insel, 2014; IOM, 2014). In addition, the ACA now prohibits lifetime or annual dollar limits for essential health benefits, which include mental health and substance abuse care (CMS, 2014a). Future research examining the impact of these new rules and requirements will help determine the extent to which needed behavioral health care is more affordable and accessible to young adults.
Aging Out of Child-Serving Systems
For young adults with mental health or substance use treatment needs, an additional factor that complicates service delivery is the many funding streams, state-funded services, and ways of organizing treatment that are age defined (Davis et al., 2009). Age-defined services and systems include special education (ending at age 21), foster care (typically ending at age 18 or 21), juvenile justice (typically ending at age 17 or 18), and adult criminal justice (starting at ages 16, 17, or 18). Public mental health systems also are typically divided organizationally and fiscally between child and adult services (Davis, 2003; Davis et al., 2006). Each of these systems may provide or coordinate behavioral health services. Thus, young adulthood marks an age when particularly vulnerable individuals’ behavioral health services are disrupted by “aging out” of children’s service systems. Continuity of care as individuals age out is dependent on access and strong connections to behavioral health services from adult systems. In addition, within public mental health services, policies that define eligibility criteria or target populations for services are distinctly different for child and adult mental health (Davis and Koroloff, 2006), with adult criteria typically being more narrow. This produces a barrier to access based on changing age, not changing need.
“It took me about 6 months to get an intake appointment. My psychologist left after 2 months.”
Another factor that contributes to discontinuities in care for any young adult with health care needs is the age-based eligibility criteria for Medicaid
and Supplemental Security Income (SSI).5 Medicaid has different eligibility criteria for children (dependent members of a household) and adults. Those who age out can fail to meet the adult criteria (Pullman et al., 2010). Qualifying for Medicaid by meeting the Social Security Administration’s (SSA’s) definition of disability also is impacted by age-based definitions of “disability” (e.g., ADHD is a qualifying mental disorder for children but not for adults). According to SSA, each year tens of thousands of child SSI recipients reach age 18, and their medical eligibility is redetermined according to adult disability standards (Hemmeter, 2012). Overall, about one-third of these children (37 percent) lose eligibility (Hemmeter, 2012). Among youth with mental health disorders that fall under the “other mental disorders” category (e.g., anxiety, affective, and disruptive behavior disorders)—who make up 28 percent of all children receiving SSI after reaching age 18—more than half (53 percent) lose eligibility upon redetermination (Hemmeter, 2012). Overall, these age-based criteria contribute to higher risk of Medicaid disenrollment during young adulthood, even among highly vulnerable clinical populations (Davis et al., 2014; Pullman et al., 2010), and may contribute to reduced access to needed behavioral health care (Slade et al., 2014). Although discussed here in the context of behavioral health transitions, many of these same discontinuities apply more generally to health care coverage issues for young adults.
Differences Between Child and Adult Mental Health Systems
Several typical treatment culture differences characterize child and adult mental health systems. The first is the manner in which parental figures are involved. In their seminal work defining system-of-care principles for children with emotional disturbance, Stroul and Friedman (1986) focus on the importance of partnering with parents to provide appropriate treatment and supports for their child. Since that work was published, child mental health systems have largely changed to work more closely with parental figures in developing and implementing treatment and service plans for their children (Stroul, 2002). Approaches such as the wraparound process (VanDenBerg and Grealish, 1996) and multisystemic therapy (Henggeler et al., 1998) are formalized means of partnering with family members to address the child’s mental health condition and resulting functional impairments. However, family involvement is less emphasized in adult mental health systems, and once they turn 18, youth can legally restrict providers from sharing any treatment information with family members. Yet client factors that facilitate shared decision making often are still immature in the
__________________
5 In most states, SSI beneficiaries are automatically eligible for Medicaid, while other states require a separate application and determination of eligibility (SSA, 2014).
youngest adults (Delman, 2012; Joseph-William et al., 2014). Given the unique role parents can play in the lives of young adults (as described in Chapter 3) and the help they could provide with decision making, excluding their potential supports may compromise the efficacy of treatment for a young adult needing behavioral health services. Indeed, family cognitive-behavioral treatment appears to be an important component of early intervention in psychosis (Gleeson et al., 2009).
Another substantial difference in practice between child and adult mental health systems is related to care coordination. Children with serious mental health conditions often are involved in multiple systems, including child welfare, juvenile justice, special education, and mental health. Providers in these systems typically are aware of the involvement of other systems, and often communicate and coordinate with them. Adult mental health, by contrast, is often insular, so that services such as vocational rehabilitation or drug treatment are provided within the mental health system rather than in partnership with those systems (Davis et al., 2012b). Disconnects in cross-system connections, especially between child and adult systems, can cause disruptions or redundancies in services, especially for 18- to 21-year-olds who are still involved in child systems.
Finally, adult mental health systems often fail to recognize the unique needs of young adults, and there are few interventions with strong evidence of efficacy for this age group (GAO, 2008). With the exception of interventions to treat early psychosis, few interventions have been devised specifically for this age group, and all are in early stages of development (Davis, 2012a). Evidence of the efficacy of evidence-based adult or child interventions with a young adult population is limited (Davis et al., 2012a). Clinical trials including this age group as part of a larger age group (e.g., studies of adults in general) cannot sufficiently establish efficacy in the young adult population. For an age effect to be detected, a large sample size of the young adult age group is needed, and few age group comparisons have been conducted thus far in published studies. However, some studies have reported significant differences in outcomes or relative effectiveness of psychosocial interventions between older and younger age groups (e.g., Burke-Miller et al., 2012; Haddock et al., 2006; Kaplan et al., 2012; Rice et al., 1993). Applying interventions that have been established in older or younger populations and adapting those interventions for young adults is a reasonable starting point for research and service provision. For example, the individual placement and support model for adults with severe mental illness (Bond, 1998) has been adapted and tested for use with young adults with first or early episodes of psychosis (Killackey et al., 2008; Major et al., 2010; Porteous and Waghorn, 2007), with results providing support for its use in this age group.
Substance Abuse Care Transitions
Many of the issues of transition faced by young adults with mental health conditions are also faced by those with substance use disorders: involvement in multiple child systems that end variably between ages 18 and 21, adolescent and adult treatment providers who are trained to work with one but not the other age group, stricter diagnostic criteria for adult than child Medicaid coverage for substance abuse-based eligibility, and few interventions with efficacy for reducing substance use specifically in young adults. Several of the unique aspects of the substance use system are worth noting, however. Foremost is the heightened stigma of substance abuse problems. Most substance use is illegal, and alcohol use is illegal for young adults under age 21. Recreational use of marijuana also is illegal except in Washington and Colorado for those over the age of 21. Moreover, use of substances often is seen as a moral issue, and problematic substance use is viewed as a volitional problem rather than a chronic illness. The legal issues and moral values have two major consequences—reducing funding for treatment and posing a barrier to treatment seeking (Cutcliffe and Saadeh, 2014; Drucker, 2012). The result is a scarcity of substance abuse services and long wait lists for those services.
Brief substance use treatments for which there is growing evidence of efficacy are increasingly available on college campuses, but for the many young adults with substance use problems that are not in college or the military, or for college students whose substance abuse problems require more than brief treatment, the challenge of finding a provider after the significant step of acknowledging the need for help is a formidable barrier to care. The scarcity of treatment resources, in combination with the need for young adults to advocate on their own behalf despite their inexperience in doing so, can lead to a large unmet need for treatment in this age group (Tighe and Saxe, 2006). Mental health and substance use disorders can further impede young adults’ abilities to advocate for themselves. Young adults’ inexperience with self-advocacy also means that simply providing them with information about how and where to obtain health insurance or care, while important, is not sufficient. Also necessary are active and effective preparation of adolescents and young adults and outreach by the health care system to help them access and complete needed treatment.
PREVENTIVE CARE FOR YOUNG ADULTS
The majority of health problems during young adulthood are preventable, and behaviors associated with negative health outcomes have high prevalence among young adults, as described in Chapter 6. These behaviors often are also responsible for the onset of many chronic health conditions
(e.g., obesity, diabetes, addiction to substances, mental health disorders) that lead not only to functional impairment throughout adulthood but also to a shortened life span. Many of these behaviors represent an opportunity for cessation of harmful behaviors, the development of healthy alternatives, or further entrenchment of the behaviors that threaten adult health.
Use of Preventive Care in Young Adults
Knowledge of the use and delivery of preventive services for young adults is limited by the lack of attention to this age group in clinical delivery systems and health services research noted throughout this report. A few recent studies, either population-based assessments or based within health care delivery systems, have documented the relatively low rates of preventive services in this population (Fortuna et al., 2009; Lau et al., 2013b; see Table 7-3). Considerable variation is related to gender, race/ethnicity, and having a usual source of care. With the exception of influenza vaccination, young females are more likely than males to receive preventive services (Lau et al., 2013b). Young adults who have a source of care they typically use also are more likely to receive preventive services. Black young adults are more likely than their white counterparts to receive the full range of sexually transmitted infection (STI), cholesterol, and diet counseling (Lau et al., 2013b). Compared with whites, Asians are less likely to receive STI
TABLE 7-3 Percentage of Visits During Which Preventive Counseling Was Provided to Young Adults (aged 20-29), 1996-2006
| All Specialties (%) | Primary Care (%) | Ob/Gyn (%) | |
| Any | 30.6 | 32.7 | 33.6 |
| Injurya | 2.4 | 3.1 | 0.8 |
| Smoking | 3.1 | 4.2 | 3.1 |
| Exercise | 8.2 | 9.4 | 8.2 |
| Weight reductionb | 3.0 | 3.8 | 3.4 |
| Mental health | 4.1 | 4.2 | 1.3 |
| STI/HIVc | 2.7 | 2.6 | 7.1 |
NOTES: “Mental health” does not include substance abuse or use; STI = sexually transmitted infection.
Primary care includes internal medicine, pediatrics, family practice, general practice, general preventive medicine, or public health or general preventive medicine.
a Data were available for 1996-2000 and 2005-2006.
b Data were available for 2001-2006.
c Data were available for 1996-2000.
SOURCE: Adapted from Fortuna et al., 2009.
TABLE 7-4 Past-Year Receipt of Screening or Preventive Services Among Young Adults Aged 18-25 Who Had a Past-Year Visit, National Health Interview Survey, 2011
| Blood Pressure Check | Fasting Blood Sugar Check | Talked About Diet | Talked About Smoking If a Smoker | Pap Screen for Women | Flu Shot | |
| % Who received screening or preventive service | 87.3 | 22.3 | 22.8 | 52.0 | 66.5 | 26.2 |
SOURCE: Analysis done by Sally H. Adams @ University of California, San Francisco, Division of Adolescent & Young Adult Medicine.
and emotional health screening, and Latinos/as are more likely to receive cholesterol and diet counseling (Lau et al., 2013b).
Analysis of National Health Interview Survey (NHIS) data from 2011 reveals that among young adults who had a clinical visit during the past year, access to a range of preventive services ranged in frequency from 87 percent receiving a blood pressure check to 22 percent receiving a fasting blood sugar check (see Table 7-4). It is important to note that such preventive screening can take place during any clinical encounter with a provider or in alternative delivery systems (e.g., pharmacies, work or school sites). Providers need to be encouraged to use any visit as an opportunity to address a component of preventive care.
Guidelines for Preventive Care for Young Adults
This section examines existing guidelines, their implementation, and monitoring of adherence.
Existing Guidelines
There continue to be no specific medical, behavioral, or oral health guidelines focused specifically on the young adult population. The clinical preventive services recommendations6 of the U.S. Preventive Services Task Force (USPSTF) consist of evidence-based recommendations across several specific health areas. For the past two decades, there has been a strong movement toward developing consensus-based guidelines for care for adolescents, starting with the American Medical Association’s Guidelines for
__________________
6 See http://www.uspreventiveservicestaskforce.org/recommendations.htm for details (accessed October 22, 2014).
Adolescent Preventive Services: Recommendations and Rationale (Elster and Kuznets, 1994) and Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents (Green, 1994). The most recent Bright Futures edition includes preventive care recommendations up to age 21 (Hagan et al., 2008). A revision of Bright Futures is expected to be released in 2015.
Several groups have called for the development of care guidelines for young adults (Callahan and Cooper, 2010; Fortuna et al., 2009; Irwin, 2010; Ozer et al., 2012). Recently, Ozer and colleagues (2012) conducted an analysis to identify evidence-based guidelines for young adults by reviewing professional consensus guidelines and the evidence-based guidelines from the USPSTF that include young adults (aged 18-26). They found that four groups—AAP, the American Congress of Gynecologists and Obstetricians (ACOG), AAFP, and ACP—had developed guidelines relevant to young adults.
“Most young adults don’t want to pay for anything if they can, so even though preventive care is for your benefit and you can access it at any time, some people don’t realize that that is the case. They think they may not be covered and may have to pay for services.”
Increasingly, health care plans have incorporated an annual preventive care visit with limited or no co-pays as part of the core benefits for subscribers. The ACA has expanded the opportunity for young adults to receive an annual preventive visit with no associated co-payments, and a recent study documents an increase in young adults’ receipt of a general checkup in the first year of implementation of the ACA—48 percent in 2011 as compared with 44 percent in 2009 (Lau et al., 2014b). Table 7-5, adapted from Ozer et al. (2012), lists the preventive services that most private plans must cover under the ACA, which include the evidence-based screening and counseling services rated highly in either Category A or B by the USPSTF,7 the Advisory Committee on Immunization Practices’ recommended immunizations, the Bright Futures recommendations, and the services specified in the Women’s Preventive Services Guidelines (HHS, 2012). The Women’s Preventive Services Guidelines (HRSA, 2014; IOM, 2011) specify that in addition to the services provided for all adults, the services
__________________
7 The USPSTF defines Category A as follows: “The USPSTF recommends the service. There is high certainty that the net benefit is substantial.” Category B is defined as follows: “The USPSTF recommends the service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial” (USPSTF, 2012).
TABLE 7-5 Preventive Health Care Services for Young Adults (aged 18-26) Covered Under the Affordable Care Act
| Services Covered for All Young Adults (ages 18-26) | Additional Services Covered for Young Adults Ages 18-21 | Additional Services Covered for Women (ages 18-26) |
|
Alcohol misuse screening and counseling Tobacco use screening Blood pressure screening Diabetes (Type 2) screening for those with high blood pressure* Diet counseling* Obesity screening and counseling Cholesterol screening* Depression screening HIV screening STI prevention counseling* Syphilis screening* Immunizations Hepatitis A Hepatitis B Human papillomavirus Influenza Measles, mumps, rubella Meningococcal Pneumococcal Tetanus, diphtheria, pertussis Varicella |
Annual wellness visit Screening and counseling for illicit drugs Suicide screening Safety/violence screening Family/partner violence (male and female) Fighting Use of helmets Use of seat belts Driving under the influence Use of firearms Bullying Polio immunization |
Well-woman visits Contraception Folic acid supplements Domestic and interpersonal violence screening and counseling (women of all ages) Cervical cancer screening (if sexually active) Chlamydia infection screening Gonorrhea screening* Breast cancer genetic test counseling (BRCA)* Breast cancer chemoprevention counseling* Hepatitis B screening for pregnant women Rh incompatibility screening for pregnant women Anemia screening for pregnant women Gestational diabetes screening Urinary tract or other infection screening for pregnant women Comprehensive support and counseling for breastfeeding |
* If at higher risk.
NOTE: STI = sexually transmitted infection.
SOURCES: Adapted from Ozer et al., 2012, 2013. Original sources are the evidence-based screening and counseling services rated highly either in Category A or B by the USPSTF, immunizations recommended by the Advisory Committee on Immunization Practices, the Bright Futures recommendations, and the services specified in the Women’s Preventive Services Guidelines.
listed in Table 7-5 must be provided to women by private plans without cost sharing (Armstrong, 2012a,b; HHS, 2012; HRSA, 2014). Note that Table 7-5 summarizes what evidence-based services are currently covered, and does not provide a comprehensive list of what this committee deems should be covered.
Comprehensive dental guidelines for young adults could not be identified, although the American Academy of Pediatric Dentistry recommends
that a dental home be established when the adolescent patient, family, and dentist agree that it is time to transition to adult dental care (AAPD, 2013).
Implementation of Guidelines
Multiple approaches can be used to incorporate preventive guidelines into clinical practice for young adults. At present, however, there is no consensus among health professional organizations, the USPSTF, health care plans, and state and federal agencies on guidelines that should be used as the starting point for implementation.
Barriers that impede the delivery of preventive services in clinical settings include both clinician factors (e.g., lack of knowledge of guidelines; attitudes toward the efficacy of preventive services; and lack of training, skills, and confidence to deliver the services) and external factors (e.g., time constraints, lack of screening tools, lack of reimbursement) (e.g., Ozer et al., 2005). Efforts comparable to those over the past two decades to increase the delivery of preventive services to adolescents are just beginning for young adults. Multiple models shown to increase preventive screening in adolescents could be adapted for use for young adults (Boekeloo and Griffin, 2007; Boekeloo et al., 2003; Klein et al., 2003; Olson et al., 2009; Ozer, 2007; Ozer et al., 2005; Sanci et al., 2012; Stevens et al., 2008; Tylee et al., 2007).
Monitoring of Adherence to Guidelines for Young Adult Preventive Care
No mechanisms for monitoring adherence to guidelines relevant to young adult preventive care currently exist. With the implementation of preventive care under the ACA, it will be necessary to identify national- and state-level datasets that can be used to monitor the implementation of these guidelines. Monitoring guideline adherence for young adult preventive care is important in both the public health and health care domains. Below are identified existing datasets that could be used for this purpose and describe associated challenges.
Four nationally representative ongoing surveys that include some measures of preventive screening and counseling for adults in general can be accessed to obtain estimates specifically for young adults: the NHIS, a survey of health status and health care access; the Medical Expenditures Panel Survey (MEPS), a household survey of health, health care, and health care expenditures; the National Ambulatory Medical Care Survey, which monitors the services patients receive from clinicians in ambulatory settings; and the Behavioral Risk Factor Surveillance System, a survey of behavioral risk factors associated with major morbidity and mortality (AHRQ, 2014; CDC, 2014a,b,c). In addition, the Centers for Medicare & Medicaid Ser-
vices (CMS) is developing and implementing a revised set of adult health care quality measures in conjunction with AHRQ (CMS, 2014e; GPO, 2012; Mann, 2012). Many of these measures are applicable to young adults (e.g., influenza vaccinations, body mass index assessment, screening for clinical depression) and will be of use in assessing the implementation of clinical preventive screening in Medicaid-enrolled young adults. The use of these measures is encouraged by CMS but is optional for the states. It is not clear how states will choose the measures on which they will report and what capability they will have to access data specific to young adults.
Despite the availability of these data, researchers, policy makers, funders, and other stakeholders need to have the expertise to break out the specific ages that make up young adulthood, examine state-level data, and differentiate specific subpopulations. Moreover, some of these datasets are more readily accessible than others. In many cases, online analysis can be carried out, but there usually are restrictions on the specificity of age groups and the breadth of subgroup analyses possible. In addition, most national survey data centers allow analysis of state-level data upon request, but the datasets are not always sufficiently large to study the states with smaller populations.
For both national- and state-level data analysis, data elements that help differentiate special populations may be insufficient. Gaps may exist for youth who have been in foster care or were recently homeless or incarcerated. For the CMS data, only young adults enrolled in Medicaid will be able to be assessed with the new adult core measures.
Some of the survey procedures also may introduce bias into the survey responses. For example, the MEPS data collection procedures identify the adult respondent for the entire household, including young adults, as the adult who is most knowledgeable about the health care utilization and expenditures of all household members (AHRQ, 2014). For many young adults, parents may be unaware of health care accessed confidentially; through college health services; or through other systems of care, such as public health clinics and pharmacies (Lau et al., 2014a).
In addition, current adult health care monitoring efforts do not cover many key topics relevant to young adult screening and counseling, such as obesity-related issues, substance use, and reproductive health issues. When these topics are assessed, a lack of specificity often limits the utility of the assessment. For example, the USPSTF recommends that young adults have their blood pressure screened every 2 years when it is is below 120/80 mm Hg (NAHIC, 2014). Yet surveys such as the NHIS asking about the recency of blood pressure monitoring do not always ask respondents to report their blood pressure, so adherence to this guideline cannot be determined.
Preventive Care for Behavioral Health Conditions
There are fewer rigorously tested approaches for preventing behavioral health disorders than exist for many physical disorders (e.g., encouraging diet or exercise in all patients to reduce the likelihood of their developing cardiovascular disease). One example of an accessible behavioral health prevention approach is encouraging aerobic physical activity to prevent the development of depression (Mammen and Faulkner, 2013).
Most prevention approaches for behavioral health target children and adolescents based on the young ages at which many behavioral health conditions develop and the ready access to these populations in schools (IOM, 1994; Stice et al., 2009). Studies of prevention interventions for conditions common to young adults—including Web-based technologies to reduce the risk of developing depression (Van Voorhees et al., 2011) and anxiety (Braithwaite and Fincham, 2007; Christensen et al., 2010; Cukrowicz and Joiner, 2007)—have targeted primarily college students. SAMHSA funds the Campus Suicide Prevention Grants8 to support efforts at postsecondary institutions to prevent suicide and to improve services for students with problems that put them at risk of suicide, such as depression, substance abuse, and other behavioral health issues; however, there are currently no rigorously tested interventions to implement. A growing body of research documents brief interventions for reducing college binge drinking with some evidence of efficacy (e.g., Kulesza et al., 2013). Preliminary evidence also suggests that parents who talk with their children about binge drinking before they depart for college can decrease excessive drinking and alter drinking perceptions (Turrisi et al., 2001).
Instead of going to college, some young adults enter the military after high school. As discussed in Chapter 5, military personnel who have been deployed are at heightened risk of developing posttraumatic stress disorder and other mood and anxiety disorders and for suicide. While several interventions have been developed for use both before and during deployment to prevent the development of posttraumatic stress disorder or suicide, none have as yet been rigorously tested (Hoge and Castro, 2012; Hourani et al., 2011). Predeployment mental health screening also has been used to either divert some individuals from deployment or provide additional mental health support (mainly medication) during deployment (Warner et al., 2011). There is evidence of reduced mental health needs in brigades with screening compared with those without (Warner et al., 2011).
For civilian young adults not enrolled in college or in colleges that offer some preventive interventions, most interventions are designed for
__________________
8 See http://www.samhsa.gov/grants/2013/sm-13-009.aspx for details (accessed October 22, 2014).
individuals at high risk of developing a mental health disorder or with conditions that increase this risk. For example, cognitive-behavioral interventions can reduce the risk of developing posttraumatic stress disorder if administered within days or weeks after a traumatic event (Agorastos et al., 2011). Given the high risk of violent victimization in young adulthood, including sexual violence and witnessing violence, prevention of trauma symptoms and posttraumatic stress disorder is particularly relevant in this age group.
The experience of psychological stress is pervasive in young adults and may contribute to the subsequent development of behavioral or physical health disorders, as described in Chapter 6. A variety of stress reduction techniques are available for which there is evidence of efficacy in adults, such as mindfulness-based approaches or cognitive therapy (Abbott et al., 2014; Querstret and Cropley, 2013), cognitive-behavioral techniques (Cruess et al., 1999), and relaxation techniques (Shah et al., 2014). Some of these techniques can reduce symptoms of behavioral health conditions (Chiesa and Serretti, 2014; Khoury et al., 2013; Shah et al., 2014), although findings on the benefits for physical conditions are more mixed (Abbott et al., 2014; Fordham et al., 2013; Hughes et al., 2013; Lauche et al., 2013; Reiner et al., 2013). As with other behavioral health interventions, direct evidence of the efficacy of these stress reduction approaches specifically in young adults is limited, and studies have focused primarily on college students (Bodenlos et al., 2013; Tanis, 2012).
There are also approaches for reducing the development of depression in high-risk groups, such as adolescent children of parents with depression or adolescents with elevated depression symptoms (Beardslee et al., 2013; Clarke et al., 1995, 2001). One such approach has been adapted for Web-based intervention and has shown moderate effects in young adults (Clarke et al., 2009). In addition, pharmacological treatment combined with psychotherapy reduces the likelihood of suicide in individuals who have unipolar or bipolar affective disorders (Rihmer and Gonda, 2013). And since young adulthood is a common age for becoming a parent, preventing postpartum depression is particularly relevant in this age group. While cognitive-behavioral therapies reduce postpartum depression, evidence is currently insufficient regarding approaches for identifying those at risk and providing preventive interventions (Nardi et al., 2012).
Finally, because young adulthood is the peak age of onset of psychosis (Copeland et al., 2011), prevention of these most serious mental illnesses is a high priority. There is growing evidence that cognitive-behavioral therapies and complex psychotherapies can delay the transition from symptoms indicating high risk of developing psychosis to the development of a psychotic disorder, while pharmacotherapy does not appear to be beneficial for this purpose (Stafford et al., 2013). Both psychotherapies and pharma-
cotherapies can, however, help reduce the likelihood of a second episode of psychotic illness in those who have recently experienced a first episode (Álvarez-Jiménez et al., 2011).
BEHAVIORAL HEALTH INTERVENTIONS FOR YOUNG ADULTS
Effective behavioral health treatments and strategies exist for adults. The efficacy of these treatments specifically for young adults, however, is largely undemonstrated because they typically group young and other adults together (Davis et al., 2012a).
Pharmacological interventions are expected to be as efficacious in young as in older adults, although noncompliance may be greater in young adults (Baillargeon et al., 2000; Kessing et al., 2007). Psychosocial interventions, however, cannot be assumed to be as efficacious in young as in older adults, as they can be influenced by many of the factors that are changing or less mature in young compared with older adults. Such factors include responsibility taking, response to authoritative figures, changing roles within the family, and responses to behavioral contingencies. Indeed, young and older adults even perceive various qualities of their interaction with physicians differently (Bradley et al., 2001). Consequently, psychosocial interventions need to be explicitly tested in young adults. To this end, the young adult sample size needs to be large enough to detect an age effect compared with older or younger age groups (Davis et al., 2012a). Few published studies have compared age groups, although some have yielded significant findings comparing young and older adults with respect to outcomes or the effiacy of psychosocial interventions (e.g., Burke-Miller et al., 2012; Haddock et al., 2006; Kaplan et al., 2012; Rice et al., 1993; Sinha et al., 2003). With the exception of interventions to treat early psychosis, few interventions have been developed specifically for young adults; all are in early stages of development, and there are few for which efficacy has been demonstrated in this age group.
HEALTH CARE COVERAGE FOR YOUNG ADULTS
Young adults without health insurance or with gaps in insurance coverage are less likely to access health services compared with young adults who are continuously insured (see Figure 7-1). Health insurance coverage rates for young adults, however, have historically been the lowest of any age group. In 2010 and 2011, for example, young adults aged 19-25 had an uninsured rate of 28 percent and were the age group most likely to be uninsured (Todd and Sommers, 2012). The rate of uninsurance among empoyed young adults also is one-third higher than that among older
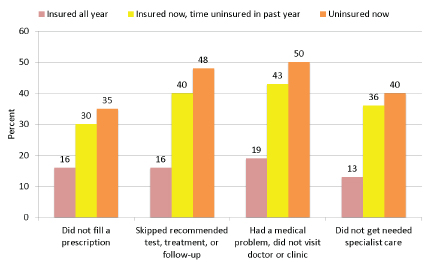
FIGURE 7-1 Percentage of young adults aged 19-29 who experienced different types of health care access problems in the past year because of cost (2010 data).
SOURCE: Collins et al., 2012.
employed adults because the part-time, entry-level, seasonal, and small-business jobs held more commonly by young versus older adults often do not include health benefits (CMS, 2014d).
In this section, we describe state-level efforts to enhance coverage for young adults and the impact of the ACA on this population. We also discuss several groups of young adults who have particular difficulty accessing care, including unauthorized immigrants, those exiting the foster care system, those involved in the justice system, and those with mental illness. The focus is primarily on financial barriers, but we identify additional barriers as well. It is important to keep in mind that access to adult care that fails to effectively engage and retain young adults or address their particular needs also is insufficient. A recent study showed that even though young adults’ coverage increased following en-
“My boss took the time to discuss general health care information with me, which helped me understand my choices better.”
actment of the ACA, the impact on their health status and the care they received was limited (Kotogal et al., 2014), although their use of emergency departments for care does appear to have decreased (Hernandez-Boussard et al., 2014).
State-Level Efforts to Improve Young Adults’ Health Care Coverage
Prior to passage of the ACA, laws extending dependent coverage for young adults were passed in 37 states (Collins and Nicholson, 2010). These laws vary considerably in scope. For example, the age of dependency ranges from 23 in Oregon and Wyoming to 31 in New Jersey (Collins and Nicholson, 2010). Dependency criteria also vary by student, financial, and marital status, with some laws covering only young adults who are full-time students, financially dependent, living in the same state as their parents, or unmarried (Collins and Nicholson, 2010). In addition, under an option included in a 1999 federal law, 33 states took action to extend Medicaid coverage from age 18 to age 21 for youth exiting foster care (English et al., 2006; Lehmann et al., 2012).
The Patient Protection and Affordable Care Act
The ACA includes four principal pathways for increasing health insurance coverage for young adults—one specific to this age group (coverage under their parents’ employer-sponsored health plans) and the others shared with other age groups (health insurance for college students, Medicaid expansion, and insurance exchanges).
Providing for continued coverage for young adults is the intent of the ACA requirement that employer plans providing coverage for dependent children extend that coverage to young adults up to the age of 26. This employer mandate has had a notable impact on retention of young adults already covered by parental plans as well as new enrollment. The Health Insurance Tracking Survey of Young Adults found in 2013 that 19- to 25-year-olds on parental employer plans increased from 13.7 million to 15 million between November 2011 and March 2013, and that 7.8 million of these young adults who joined a parent’s plan would not have been eligible for coverage in the absence of the employer mandate (Collins et al., 2013). The survey also found notable increases (from 17 percent to 26 percent in 2013) among lower-income young adults, although this demographic group also is less likely to have parents with employer-sponsored health insurance (Collins et al., 2013).
The ACA addresses the high degree of variation in coverage and oversight of student health insurance by making these plans subject to the same protections as health insurance exchange plans. The act does not, however,
require guaranteed availability and guaranteed renewal because of the unique transient status of students (CMS, 2014b). As many as 3 million students may be covered under student health insurance plans at institutions of higher learning (CMS, 2014f).
Medicaid expansion and health insurance exchanges under the ACA are the major pathways for increasing coverage among lower-income young adults. Adults with incomes up to 133 percent of the federal poverty level (FPL) ($15,521 for an individual, $31,721 for a family of four for 2014) are now eligible for Medicaid or for coverage in new health insurance exchanges, with graded subsidies for incomes between 100 percent of the FPL ($11,670 for an individual, $23,850 for a family of four) and 400 percent of the FPL ($46,680 for an individual, $95,400 for a family of four) (FamiliesUSA, 2014). In 2013, 15.7 million 19- to 29-year-olds were uninsured for at least part of the prior year, and of these individuals, 82 percent had household incomes qualifying either for Medicaid under the ACA expansion or subsidized coverage in insurance exchanges (Collins et al., 2013). By the end of the first full ACA enrollment period in April 2014, there were 2.2 million young adults (aged 18-34) among the 8 million total enrollees in state-based or federally facilitated insurance exchanges (ASPE, 2014). Medicaid expansion in 27 states and the District of Columbia will increase the number of eligible insured young adults (KFF, 2014a).
Despite increases in young adult coverage under the ACA, young adult enrollment has been modest compared with the total estimated number of uninsured young adults. Moreover, it remains uncertain how many of the young adults newly enrolled in the exchanges will actually pay premiums to acquire, use, and sustain their coverage. Lack of awareness and knowledge of eligibility for subsidized insurance and concerns about affordability among young adults have been cited as major reasons for the slow uptake in this age group (Collins et al., 2013).
In addition, as of this writing, 21 states are not moving forward with Medicaid expansion, and 2 are in open debate on the issue (KFF, 2014a). An estimated 4.8 million adults who are uninsured, poor, and nonelderly could fall into the coverage gap in the states not expanding Medicaid, but it is not known how many of these individuals are young adults (KFF, 2014b). This failure to participate in Medicaid expansion will adversely impact the ability of lower-income young adults, particularly those of color, to obtain health insurance. These states provide much less Medicaid coverage than states adopting Medicaid expansion; for example, parents in a family of three have median eligibility limits of 46 percent and 138 percent of the FPL, respectively (KFF, 2014b). Nearly half of all nonelderly adults with family incomes below 138 percent of the FPL live in these states (KFF, 2014b).
Insurance exchanges at the state and federal levels are required to offer
a range of health plans that provide specific levels of coverage defined by the proportion of eligible expenses the plan will pay (actuarial value). These proportions range from 60 percent to 90 percent of eligible expenses—bronze, silver, gold, or platinum—with premiums rising accordingly. Premiums also are higher if the individual is a smoker, enrolls a family, or is over age 24 (GPO, 2013). Coverage of prevention services is mandatory (GPO, 2013), as is coverage for mental health, maternity, and newborn care and prescription medications—all especially relevant to young adults. Coverage of dental care is not required for adults, but may be offered as part of a health plan or as an independent policy. It has been estimated that the ACA could reduce dental uninsurance in all adults by approximately 5 percent, compared with about 55 percent in children younger than 19, for whom dental care is an essential health benefit (ADA, 2013).
Concern about affordability as an enrollment barrier for young adults, who generally are more financially constrained, healthier, and less likely to utilize health care services compared with older adults, prompted the addition of a fifth health plan category under the ACA. This “catastrophic coverage” entails low premiums, but very high deductibles that translate to little coverage until considerable out-of-pocket expenses have been incurred (CMS, 2014c). In the state of Connecticut, for example, a single young adult aged 27 earning $32,000 per year could purchase a catastrophic plan at $115.10 per month net of an ACA premium tax credit of $60.20 per month, and receive free preventive services and three free primary care visits. However, this plan requires that $6,350 of out-of-pocket expenses be incurred before any additional coverage is provided.9 “Catastrophic plans” were not a major contributor to increased young adult enrollment during the first enrollment period, with only 5 percent of 18- to 34-year-old young adult enrollees in federally facilitated exchanges selecting such a plan (ASPE, 2014).
Approximately 67 percent of young adult workers (aged 19-29) are enrolled in health insurance as a result of employer health benefits (Collins et al., 2013). Enrollment rates are higher among those aged 26-29 (79 percent) than those aged 19-25 (52 percent) (Collins et al., 2013). This differential may reflect the finding that up to half of 19- to 25-year-olds not enrolling in their employer plan are receiving coverage under their parental (34 percent) or spousal (19 percent) plan, while others may not be working enough hours to be eligible for employer benefits. Of those not enrolled in employer, parental, or spousal plans, most report unaffordability (22 percent) rather than lack of need (5 percent) as the principal reason for nonenrollment (Collins et al., 2013).
__________________
9 Calculation performed on access health CT, the Connecticut health insurance exchange, using these parameters during the first ACA enrollment cycle for 2014 coverage.
Young Adults Who Have Difficulty Accessing or Maintaining Care
As noted above, certain groups of young adults—including those exiting the foster care system, those involved in the justice system, those with mental illness, and unauthorized immigrants—face particular difficulty accessing care. Chapter 8 provides a broader look at these groups and other marginalized young adults and examines programs and policies that can support their well-being.
Young Adults Exiting Foster Care
Young people in foster care have higher rates of serious health problems compared with the general population of adolescents and young adults (English et al., 2014). They are also disproportionately members of racial and ethnic minority groups (English et al., 2014). Higher rates of both physical and mental health issues are found among children and youth in foster care, including birth defects, developmental delays, emotional adjustment problems, chronic medical problems such as asthma, dental caries, and substance abuse (AAP, 2012; CMHS and CSAT, 2013; Halfon et al., 1995). And it is estimated that more than 30 percent of older adolescents in foster care have a disability or chronic illness (Rosenbach et al., 2001). A portion of their health concerns are directly related to the issues that led to their placement in foster care, such as physical or sexual abuse; other health concerns arise during placement (English et al., 2014).
In 2012, approximately 23,396 individuals left foster care by “emancipation,” or “aging out” (Children’s Bureau, 2013). Up until 2008, most individuals in foster care exited at 18, although the exit age was older in some states (English et al., 2014). Thus, many youth face an abrupt ending to social, educational, and health services, including Medicaid services, for which virtually all foster care children and adolescents are eligible (English et al., 2014). In 2008, the federal Fostering Connections to Success and Increasing Adoption Act (P.L. 110-351) was signed into law. This act offers federal payments for young adults aged 18 or older who meet certain requirements related to their placement and who are working toward independence through activities such as educational programs, certain programs related to obtaining employment, and employment (Children’s Bureau Training and Technical Assistance Network, 2008). Many foster youth transitioning into young adulthood face a variety of problems, including poor or absent family support; problems with employment and low income; problematic living arrangements; medical, dental, and mental health issues; and lack of health care coverage. Therefore, continuation of support has been noted as crucial to successful transitions (AAP, 2012).
The ACA is expected to lead to significant changes in access to health
care for these youth. Starting in 2014, the ACA requires states to provide Medicaid coverage up to the age of 26 for most individuals aging out of foster care. Still, health care coverage accessibility challenges will likely remain for the foster care population, given their need for help in the enrollment process and the need to identify appropriate providers in their community (English and Park, 2012). Barriers such as lack of transportation and low health literacy may pose challenges as well.
Young Adults Involved in the Justice System
In the United States, millions of young adults have some form of contact with the justice system, ranging from arrest without prosecution to detention or incarceration in an adult facility (as discussed in greater detail in Chapter 8). A variety of studies have documented increased health concerns, particularly mental health and substance abuse issues, for this population, as well as vast disparities in access to needed health care (English et al., 2014). Many of these young adults have long-standing preexisting physical and mental health problems. For example, approximately 65-70 percent of the adolescent juvenile justice system population has a mental health disorder, and more than 25 percent of these disorders are considered serious enough to require significant and immediate treatment (Shufelt and Cocozza, 2006). These and other health profile data do not apply only to young adults involved in the juvenile justice system; adults in the criminal justice system generally experience many of the same health problems.
Access to health care for young adults is determined by many different factors, both while they are in the justice system and afterward. These factors can include their socioeconomic circumstances, their geographic location, and the particular part of the justice system in which they are involved. Young adults involved in the justice system frequently are living in poverty or come from families with very low incomes. Prior to enactment of the ACA, many young adults were not eligible for Medicaid unless they were pregnant or disabled, and in most states the Medicaid eligibility income threshold for adults was extremely low (Heberlein et al., 2012). Moreover, Medicaid funds may not be used for services to “inmates of public institutions” (Zemel and Kaye, 2009). Health care for this population is provided at the state and local levels, and its quality varies significantly. Even among those who are living in nonsecure residential placements or on probation or parole, health insurance coverage under both Medicaid and private plans is uneven (English et al., 2014).
Future effects of the ACA on low-income young adults in the justice system will depend primarily on their state’s decision about whether to expand Medicaid. As discussed above, young adults who do not qualify for Medicaid because of higher incomes may have access to health insurance
through a parent’s employer-based policy until they turn 26 or through the health insurance exchanges. Agencies and facilities in the justice system can play a critical role in ensuring that young adults enroll in insurance coverage for which they are eligible, particularly as they exit the system (NACo, 2012; National Conference of State Legislatures, 2014). Some states have taken steps to facilitate this coordination. For example, legislation in Nevada allows the director of the Department of Corrections to apply for determination of Medicaid eligibility on a prisoner’s behalf.10 Having health insurance in place before exiting the system is key so that follow-up health care appointments can proceed immediately thereafter. Among other benefits, this can help prevent recidivism, particularly for those with mental health and substance abuse issues (English et al., 2014).
Young Adults with Behavioral Health Disorders
Utilization of behavioral health care is lower among young adults relative to children and older adults (Hower et al., 2013; Pottick et al., 2008, 2014; Ringeisen et al., 2009). Beginning in 2014, the implementation of Medicaid expansion and insurance exchanges under the ACA, in addition to the 2008 legislation mandating parity for behavioral health care discussed above, improvements in Medicaid disenrollment rates and more continuous and integrated behavioral and physical health care can be expected for young adults. Many states are establishing administrative processes intended to simplify health care plan enrollment (KFF, 2013; Koyanagi and Alfano, 2013). Examples of these processes include using a single application for both Medicaid and exchange plans and designing exchange plans specifically for youth under age 21. In addition, states can choose to make adults without children with incomes up to 133 percent of the FPL eligible for Medicaid, with a much higher match from the federal government than for other populations, and to make those who have been uninsured for more than 6 months potentially eligible for federally subsidized, high-risk state insurance plans that provide coverage for individuals with preexisting conditions (Koyanagi and Alfano, 2013).
The potential effectiveness of these reforms for young adults with substantial behavioral health issues is unknown. For example, the application process for health care coverage can be a barrier to treatment for young adults. Studies of Massachusetts’ health care reform have found that young adults enrolled in Medicaid and health care exchanges at higher rates
__________________
10 Nevada S.B. 519. An Act relating to Medicaid; authorizing the Director of the Department of Corrections to apply on behalf of a prisoner for a determination of Medicaid eligibility; and providing other matters properly relating thereto.
(Gettens et al., 2011; Long et al., 2010), but those with behavioral health issues had lower enrollment rates (Capoccia et al., 2013).
Young adults also are much more likely than more mature adults to drop out of outpatient psychotherapy (Davis, 2013; Edlund et al., 2002). It is unclear to what extent the reasons for treatment dropout are similar and simply more prevalent in young than in older adults (e.g., insurance loss due to more frequent job change/loss), or the reasons are qualitatively different (e.g., related to peer influence in young adults but to spousal influence in mature adults). It is intriguing, however, that at least one study of a large-scale effort to tailor mental health care to the needs and characteristics of young people found much higher treatment enrollment rates in those settings than in standard adult settings (Gilmer et al., 2012).
Unauthorized Immigrants
An estimated 11-12 million unauthorized immigrants reside in the United States, representing about 17 percent (one in six) of all uninsured Americans (Gusmano, 2012; Passel et al., 2013). The age distribution of this population differs from the legal immigrant or U.S.-born population, with 18- to 39-year-old males making up 35 percent of unauthorized immigrants, compared with 18 percent of legal immigrants and 14 percent of the U.S.-born (Passel and Cohn, 2009). Overall, in 2008 unauthorized immigrants represented 4 percent of the population in the United States and 5.4 percent of the workforce (Passel and Cohn, 2009). The children of unauthorized immigrants may be unauthorized immigrants or U.S. citizens, and together they account for 6.8 percent of elementary and secondary school students (Passel and Cohn, 2009).
On average, this population has used subsidized medical care and other forms of public assistance less than legal immigrants and U.S.-born citizens (Wallace et al., 2013). Unauthorized immigrants represent approximately 13 percent of the uninsured; they remain ineligible for Medicaid and may not participate in the health exchanges or receive tax credits (KFF, 2014c). While there are important questions about whether and how this population and the communities in which they live would benefit from health insurance coverage, research suggests a positive relationship between extending coverage to all uninsured residents (regardless of legal status) and the more general health and well-being of everyone living in those communities (IOM, 2009; Pauly and Pagán, 2007).
The Obama Administration established the Deferred Action for Childhood Arrivals (DACA) program in 2012 (HHS, 2014a). Under this program, children who came to the United States without authorization before age 16 and were under age 31 as of June 15, 2012, may request relief from deportation for a period of 2 years, during which they are eligible for work
authorization (HHS, 2014a). Consideration of deferred action is available for individuals who “are currently in school, have graduated or obtained a certificate of completion from high school, have obtained a general education development (GED) certificate, or are an honorably discharged veteran of the Coast Guard or Armed Forces of the United States” and have no significant criminal record (HHS, 2014a). Approximately 1.7 million individuals nationally, primarily Hispanic youth (85 percent), were eligible for the DACA program when it started (Passel and Lopez, 2012). However, DACA recipients are specifically excluded from the ACA’s Medicaid expansion and health insurance exchanges (Brindis et al., 2014).
SYSTEMS ISSUES RELATED TO YOUNG ADULTS
While young adults have lower health care utilization than other age groups, this is not necessarily because they have less need for health care. In this section, we examine how several issues raised earlier can be adddressed to improve the health care system for young adults and help ensure that they enter and remain in the system to receive the care they need. Specifically, we consider the health care workforce providing care to young adults, confidentiality concerns, the need for better integration of behavioral and medical health care, and innovative approaches to care delivery that may better address young adults’ needs and preferences. The section ends with proposed frameworks for young adult health care.
The Health Care Workforce
As noted earlier in the discussion of transitions, health care providers require both biomedical and psychosocial knowledge and training to provide high-quality care to young adults. Some adolescent-focused medical boards, professional associations, and researchers have started to include young adults within their population of interest, although their primary focus remains on adolescence. Yet little attention has been given to the skills and training needed by both pediatric health care professionals and systems that provide adult health care to provide high-quality care to young adults; most youth with special health care needs are still with their pediatrician at age 18 (the lower end of the age definition for young adults for this report). The limited research in this area is focused primarily on care for young adults with special health care needs.
Over the past 50 years, the need to train a health care workforce to work with adolescents has increasingly been recognized, although important gaps and inadequacies remain (see, for example, Emans et al., 2010; Fox et al., 2010; Hergenroeder et al., 2010; NRC and IOM, 2009). Postgraduate fellowship training in adolescent medicine is available for those
TABLE 7-6 Inclusion of Young Adults in Training Programs and Materials
| Training Program/Materials | Incorporation of Young Adults |
| Child- and Adolescent-Focused Training | |
| Accreditation Council for Graduate Medical Education (ACGME) program requirements for graduate medical education in pediatrics | Young adults are mentioned in the program description: “Pediatrics encompasses the study and practice of physical and mental health promotion, disease prevention, diagnosis, care, and treatment of infants, children, adolescents and young adults during health and all stages of illness” (ACGME, 2012, p. 2). However, there is no educational unit on young adults as there is for adolescents. |
| Within the content outline for the adolescent medicine examination, young adults are mentioned only in a highly specific context: candidates should be able to “develop a plan of transition from child-centered to adult-centered health care for young adults with cystic fibrosis” (ABP, 2010, p. 4). | |
| ACGME program requirements for child and adolescent psychiatry | Young adults are not mentioned (ACGME, 2007). |
| Board certification in clinical child and adolescent psychology | Young adults are not mentioned in the examination manual (American Board of Clinical Child and Adolescent Psychology, 2013). |
| National Association of Social Workers, Standards for the practice of social work with adolescents | Young adults are not mentioned (NASW, 1993). |
who have completed accredited residency training in pediatrics, family medicine, or internal medicine. After the fellowship, candidates take an exam to be certified with a subspecialty in adolescent medicine. Among formal training programs and materials in medicine, public health, social work, and behavioral health, there is no comparable recognition of the uniqueness of young adulthood. Similarly, for example, the National Association of Social Workers has published standards for the practice of social work with adolescents (NASW, 1993).
Some adolescent-focused professional associations and training programs have begun to incorporate a greater focus on young adults. For example, the Society for Adolescent Health and Medicine includes both
| Training Program/Materials | Incorporation of Young Adults |
| Adult-Focused or All-Ages Training | |
| ACGME program requirements for graduate medical education in family medicine, internal medicine, and obstetrics and gynecology | Young adults are not mentioned in the ACGME program requirements for these relevant adult specialties. In contrast, family medicine residents must experience caring for adolescents (ACGME, 2013). The internal medicine program uses an encompassing definition “from adolescence to old age” (ACGME, 2009, p. 1), while the obstetrics and gynecology program mentions no specific age groups (ACGME, 2008b). |
| As noted above, for those in family and internal medicine who seek board certification in adolescent medicine, preparing adolescents with cystic fibrosis for the transition to adult care is mentioned in the examination content guide (ABP, 2010). | |
| ACGME program requirements for graduate medical education in hospice and palliative medicine | Young adults are mentioned among the types of patients with whom residents should work (ACGME, 2008a). |
| Maternal and child health leadership competencies | Adolescents are highlighted as a specific group of focus, but young adults are not (MCH Leadership Competencies Workgroup, 2009). |
| Association of Social Work Boards licensing examination | “Young adult behavior and development” is a topic on the bachelor’s examination (ASWB, 2014). |
| National Certification Examination for Addiction Counselors | Unlike adolescents and geriatric adults, young adults are not included as a special population in the examination manual (NCCAP, 2011). |
adolescents and young adults within its vision statement (SAHM, 2014). And its Journal of Adolescent Health also has recently recognized the importance of young adults by changing its tagline to “Improving the Lives of Adolescents and Young Adults.” As noted throughout this report, however, it is important to keep in mind that young adults have needs distinct from those of both adolescents and older adults and often are cared for by different health care providers from those who care for adolescents; therefore, the workforce training needs also are distinct. Table 7-6 provides
BOX 7-4
Kaiser Permanente Northern California’s Young Adult Specialist Model
The Kaiser Permanente Group in Northern California has developed a targeted effort for young adults that includes four critical steps: (1) develop a personalized transition from pediatric to adult medicine, (2) enhance the health insurance plan’s relationship with young adults, (3) develop a cadre of primary care providers trained through the plans with targeted skills and knowledge who are enthusiastic about young adult members, and (4) enable access to care and information around the clock through both virtual and physical paths (personal communication, Calvin Gordon, M.D., Kaiser Permanente Northern California). This Young Adult Specialist Model represents a unique approach to increasing both the skills of practitioners and the navigation skill of young adults.
examples of training programs and materials in medicine, public health, social work, and addiction counseling, along with information about how young adults are explicitly mentioned, if at all. It is important to note that training specific to young adults also is lacking in other areas relevant to young adults’ health. For example, few adult correctional settings provide staff members with training in the mental health needs of this age group (Fagan and Zimring, 2000). Of interest as well is the Young Adult Specialist Model developed by the Kaiser Permanente Group in Northern California, described in Box 7-4.
Resources and training materials for young adult health care are limited. Various curriculums and training materials are available that address adolescents and young adults together (EuTEACH, 2014; Neinstein, 2014; Partnership for Male Youth, 2014). However, reflecting the availability of material, the majority of videos, case studies, and cited references focus more on adolescents than on young adults. The National Adolescent and Young Adult Health Information Center has collected clinical preventive screening guidelines for young adults aged 18-26, extracting recommendations from the USPSTF, Bright Futures, and ACOG (NAHIC, 2014).
Confidentiality Concerns
While much has been written about the need for confidential care among adolescents, less attention has been paid to that need among young adults, even though they similarly seek and use sensitive services, such as
those related to sexual health, substance use, and mental health. Research has documented that adolescents will forego medical care if confidentiality is not ensured (NRC and IOM, 2009); serious consequences, such as unprotected sex, unintended pregnancy, untreated STIs, and mental health issues, can result (Ford et al., 2004; Lehrer et al., 2007; Slive and Cramer, 2012). This is particularly true for those adolescents most at risk. As more young adults are insured through the ACA, many more are expected to seek and receive services that entail senstive issues (Tebb et al., 2014), such as discussion of sexual behavior and provision of contraception; screening and treatment for STIs; and screening, counseling, and treatment related to mental health or substance use disorders.
At the same time, a number of important changes are occurring in how patient health care data are collected, stored, accessed, and shared. While these changes hold promise for improving care and keeping consumers better informed, they may result in breaches of confidentiality for both adolescents and young adults covered through their parents’ plans (Tebb et al., 2014). The general rule of the Health Insurance Portability and Accountability Act (HIPAA) is that individually identifiable health information cannot be released by a health care provider or insurer without written authorization if the patient is 18 or older. Yet a number of exceptions allow or require a provider or insurer to release individually identifiable health information without written authorization, giving insurance companies the discretion to share otherwise protected information with an insurance holder if the disclosure is for billing and payment purposes. Thus even though a parent/insurance holder does not have a right to demand full access to protected information, the insurer can provide that individual with information related to billing and payment (termed Explanation of Benefits [EOB]). The objective is to reduce insurance fraud and abuse by informing policy holders of insurance claims made and actions taken on their account by anyone covered under their policy (including dependents) (Tebb et al., 2014). There is no legal mandate to send this information; however, claims reflecting services received in a doctor’s office that are denied because they may not be part of the insurance benefits package need to be reported to the policy holder (Tebb et al., 2014). Thus, there is inherent tension between the importance of confidentiality and the need for policy holders to be informed about the costs of health care services and benefits under their health plan. This issue is less of a problem for individuals enrolled in Medicaid, because most state Medicaid programs do not send EOB information at all or withhold it for sensitive services (although policy holders must be notified when claims are denied) (Tebb et al., 2014).
The HIPAA regulations do give individuals the right to request that their insurers send such communications by alternative means or to an alternative location rather than by mail to the home address. However,
insurers need accept such a request only if it “clearly states” that disclosing the information involved might “endanger the individual.” Confidential conversations with several insurance companies suggest they receive very few such requests each year (Gudeman, 2013).
Creative solutions to this issue are emerging. In Massachusetts, New York, and Wisconsin, for example, plans are not required to send an EOB when no additional payment is required for services (Tebb et al., 2014). This might happen if an adolescent or young adult receiving services paid the co-pay or if a service were one of the preventive services for which co-pays cannot be imposed under the ACA. Some health care systems also are designing systems to protect confidentiality in multiple areas, such as the making of appointments, lab and pharmacy procedures, and electronic medical records and billing. The state of California passed the Confidential Health Information Act (SB138), scheduled to take effect in January 2015, which will enable patients to request that EOB information be sent to the beneficiary (in this case, the young adult) rather than the policy holder (Gudeman, 2013; Tebb et al., 2014).
Confidentiality issues will be different for young adults with intellectual disabilities, for whom guardianship and decision-making support may be appropriate. The Got Transition initiative has developed an overview of options for guardianship and alternative options for decision-making support (Center for Health Care Transition Improvement, 2012). In addition, special concerns have been raised regarding situations in which parents or other family members are serving caregiving roles for young adults with mental illness, leading to efforts to allow providers to make disclosures when necessary to prevent clinical deteroriation or harm to the patient or others.11
Better Integration of Behavioral and Medical Health Care
Emphasis is increasing on integrating the medical and behavioral health care systems. The ACA endorses collocated, collaborative care.
There is no one model of integrated care. Rather, there are three basic dimensions that vary in different models: collocation, integration, and collaboration (Blount, 2003; Perrin and Sheldrick, 2012). Collocation refers to physicians and mental health clinicians sharing space and having at least somewhat overlapping hours. Integrated practice includes sharing medical records; going to the same meetings; sharing office staff for scheduling and billing; sharing medical charts, referrals, and scheduling; and the like. Collaborative practices incorporate more purposeful strategies for ensuring coordinated care, including shared decision making across practices, shared
__________________
11 For example, Rhode Island Code § 40.1-5-27.1.
care of the same patients, and a single plan of treatment that incorporates both physical and behavioral health. Collocation is not required for integration and collaboration to occur. Integrated care can emphasize physical health care while linking patients to behavioral health care, or emphasize behavioral health care while linking patients to physical health care.
Given the health profile of young adults as described in Chapter 2, integrated behavioral and physical health care would be particularly beneficial to this age group. Having easy access to behavioral health services through primary care settings could increase early use of such services (i.e., before symptoms worsen) among a population in which, as discussed above, utilization of these services is low relative to other age groups. Moreover, one study found that about half of individuals with common behavioral health conditions were seen exclusively in primary care settings (Regier et al., 1993). Thus, better integration of services also could improve general medical practitioners’ treatment of common behavioral health conditions. And because going to a primary care setting is less stigmatizing than going to a behavioral health clinic (Bower, 2002; Bower et al., 2001; Kramer and Garralda, 2000), a primary care clinic with integrated behavioral health services could decrease dropping out of behavioral health treatment among young adults. Thus, access to primary care that offers prevention or early intervention for behavioral health problems could help reduce early mortality in young adults and prevent future conditions.
However, no studies have examined access to care or care outcomes for integrated care in young adults. In general, evidence indicates that collaborative care models based in primary care targeting depressive and anxiety disorders are more effective than usual care in reducing symptoms in adults (Archer et al., 2012). These models have demonstrated improved employment rates, functioning, and quality of life, as well as cost-effectiveness (Schoenbaum et al., 2001, 2002, 2004; Simon et al., 2001, 2002). Far less research has been conducted on other mental health disorders. Evidence on the benefit of connecting individuals receiving behavioral health care to physical health care interventions also is less clearly established, although randomized controlled trials have found some benefit (van Hasselt et al., 2013). Thus, while integrated care holds promise for better behavioral health care delivery and early intervention with physical health conditions that contribute to early mortality, research is needed to test this promise.
Innovative Approaches to Care Delivery
There is burgeoning interest in how to get young adults to come “in the door” and then stay engaged in the system. Unfortunately, little research has examined how young adults prefer to access and interact with the health system, limiting health care systems’ ability to improve the system design
for young adults. As noted above, for example, young adults receive care in emergency departments at higher rates than those immediately younger and older than them. However, it is unclear whether this is related to payment issues, a lack of knowledge about how to access care in other settings, or certain features of the emergency department that make it a more attractive place for young adults to seek care. Further research could investigate which features of emergency departments and/or urgent care are appealing to young adults so that these features could be incorporated into other care settings.
“Having a representative for health care organizations who is also a young adult would be a good way to engage other young adults. This person could go where other young adults are, promote health care, and get them to take an interest in their own health.”
One potential idea is to provide care to young parents and their children together. This could be accomplished through programs that focus explicitly on two generations together (see Glied and Oellerich, 2014). Or, for example, when young adult parents take their children in for preventive/well-child visits, there could be an opportunity to provide them with information on adult preventive/wellness services that may apply to them. In the U.S. health care system, however, structural barriers impede the development of such two-generation approaches to health. Glied and Oellerich (2014) identify as the primary barrier that most physicians specialize in treating children or adults and are not used to providing care to a whole family. Other barriers include financing constraints related to health insurance, access to care, and benefits.
Below we briefly describe research on technology-based and peer-led approaches to health care for young adults.
Harnessing Technology for Young Adult Health Care
The emerging field of “mHealth” focuses on innovative approaches to using social media and mobile technology for public health and health care delivery (see, for example, the annual mHealth Summit [2014], the mHealth Alliance [2014], the U.S. Department of Health and Human Services’ [HHS’s] mHealth initiatives [HHS, 2014b], and Jones et al. [2014]). While there is little evidence on the question of whether these approaches are effective generally, let alone for young adults, they appear to hold promise for this population, who, as discussed earlier in this report, are heavy users of these media. Therefore, further research in this area is warranted.
The limited research on harnessing technology to enhance the care provided to young adults suggests that caution and careful design are needed. Although young adults are heavy users of social and mobile media and the Internet, including to search for and receive health-related information, research suggests that they generally prefer face-to-face interaction with health care providers over interaction via telephone, webcam, email, or text message (Garrett et al., 2011; Labacher and Mitchell, 2013; Lindstrom Johnson et al., 2012). To explain this preference, young adults cite confidentiality concerns, and in one study, many participants said they thought they would receive more individualized and credible information during face-to-face interaction (Lindstrom Johnson et al., 2012). Young adults’ preferences are not homogenous: Cunningham and colleagues (2014) examined young adults’ preferences for how to receive information about anxiety and depression and found that they fell into three groups, one of which preferred working independently on the Internet to obtain this information.
“Having social media apps for health would be appealing to young people, yet there is definitely a concern about privacy. If I lose my phone and someone sees that I ate five ice cream sandwiches today, I don’t really care. But if I lose my phone and someone can see that I am taking an antibiotic for an STI or something, that is really embarrassing.”
It is important to recognize that the research described in the preceding paragraph has limitations with respect to determining the preferences of young adults in the United States. First, most of this research focuses on young adults with chronic health conditions, and their preferences and needs may not be applicable to all young adults. Second, there is little research to enable the exploration of commonalities and differences across subgroups of young adults. Third, some of the research in this area comes from Canada, European countries, and Australia, and cross-cultural differences may be relevant. In addition, the care delivery system in these countries is very different from that in the United States.
Research is needed in this area to address several key questions. First, would enhancing confidentiality/security policies and assurances increase young adults’ preferences for using technology for health care purposes? Second, would technology be particularly helpful for young adults who would otherwise lack access to services, such as those who are geographically remote from providers or otherwise unable to access care? Third, would offering technology approaches as an option work well for
certain subgroups of young adults? Fourth, how can technology be integrated to supplement face-to-face interactions?
The Quantified Self
A growing body of research on preventive health care, self-diagnosis, self-monitoring of health-related behaviors, and health awareness examines how technology can be used to track, store, and analyze data on an individual’s daily behaviors (Fox and Duggan, 2013). This research and the technologies that support it can be loosely summarized by the term “the quantified self.” This form of self-tracking is enhanced by wearable devices and by networked platforms that facilitate the collection and sharing of data, and is also referred to as “lifestreaming,” “lifelogging,” “lifehacking,” “self-quantifying,” or “personal informatics” (Marwick, 2013). The idea is to monitor one’s behaviors so as to improve both behavioral and physical health.
The sociotechnical environments and devices that support the quantified self may be described as “human augmentics.” The term describes technologies that are designed to assist sensory, cognitive, and physical systems in evolving beyond their limits (Kenyon and Leigh, 2011). Human augmentics include devices that connect and sustain the human augmentics ecosystem, such as displays, robots, sensors (wearable and not), and a variety of cognitive amplifiers (Kenyon and Leigh, 2011). They also include compensatory devices for both healthy and disabled populations, such as a variety of prostheses and brain-machine interfaces. At this time, however, there are no studies indicating whether young adults as a group are relying on such technology and how and under what circumstances they are using such devices and with what outcomes.
Peer-Led Approaches
Given the vital role of peer influence in the lives of young adults, peer-led approaches to health care are intuitively appealing. Although such approaches are offered with increasing frequency, however, research is limited on their efficacy among adults in general, and even more so among young adults. In a systematic review, Lloyd-Evans and colleagues (2014) found that the existing body of research on peer-led approaches among adults with severe mental health conditions is weak, with inconsistencies in both methods and reporting. Peer-led approaches appear to be as effective as, but no better than, usual behavioral health services provided to adults (Lloyd-Evans et al., 2014).
Another evidence-based health care approach that utilizes peer support is the chronic disease self-management model for adults (Lorig et al., 2009).
This model has been extended to address the health status of adults with serious mental illness, with promising results (Druss et al., 2010).
In the past, a lack of funding has served as a barrier to offering peer-led health services. However, many states now reimburse peer specialists under Medicaid (Kaufman et al., 2012). Because of the importance of peer influence among young adults, developing and rigorously testing well-specified peer-led interventions is an important area for future research.
Characteristics of High-Quality Health Care for Young Adults
In Box 7-5, we draw on two frameworks developed by the World Health Organization (WHO, 2001, 2009) and the IOM (2001) to identify the characteristics of high-quality care for young adults. The WHO framework, originally developed for adolescent-friendly services, is adapted here to the needs of young adults. Of course, the health care system could be improved for all adults. Nevertheless, focusing on improving the system for young adults is important because their access to and utilization of the health care system will be carried forward throughout their lives.
CONCLUSIONS AND RECOMMENDATIONS
From among the many topics discussed in this chapter, the committee selected three areas in which action would make a particular difference for young adults: improving the transition process from pediatric to adult health care, improving preventive care, and developing evidence-based practices. Health insurance coverage for young adults also is very important but, as the discussion above makes clear, extensive action is already occurring in this area. Improving behavioral and medical health care for young adults would improve their health, safety, and well-being, as well as their educational and employment outcomes. Young adults with chronic health conditions, including mental health and substance use disorders, often have lower educational attainment and less successful employment experiences and outcomes, as described in Chapter 4.
Improving the Transition Process
The transition from pediatric to adult health care—including both medical and behavioral health care—is associated with poor outcomes for young adults. Structural barriers, such as funding streams and eligibility requirements, as well as age limits set by health systems, impose artificial boundaries between the two systems. These barriers negatively impact the transition process by creating discontinuities in care and associated poor outcomes. Other challenges arise because of adult health care providers’
BOX 7-5
Characteristics of Two Frameworks for Delivering Health Care Services
Two general frameworks for delivering health care services may be applied to young adults’ health care as follows:
Framework for Delivering Young Adult-Friendly Health Services(WHO, 2001, 2009)
- Accessible—Policies and procedures ensure that services are broadly accessible for young adults.
- Acceptable—Policies and procedures consider culture and relationships and the climate of engagement for young adults.
- Appropriate—Health services fulfill the needs of all young adults.
- Effective—Health services reflect evidence-based standards of care and professional guidelines.
- Equitable—Policies and procedures enable the provision of and eligibility for services for all young adults.
Institute of Medicine Framework for Delivering Quality Health Care Services(IOM, 2001)
- Safe—Protocols are in place to reduce medical errors and foster quality assurance.
- Effective—Services reflect accepted standards of clinical care.
- Patient-centered—Services are sensitive to the needs and preferences of the patient.
- Timely—Waiting times between assessment and treatment are reduced.
- Equitable—Services do not reflect disparities within the young adult population.
- Incorporating consumer perspectives—Services reflect young adults’ perspectives on their health care needs (stay healthy, get better, live with illness or disability, or cope with the end of life).
- Efficient—Services are designed to reduce unnecessary time and costs.
lack of familiarity with disease processes and developmental issues among young adults.
Transitions of care have long been identified as an important problem in health care, as described in the IOM report To Err Is Human: Building a Safer Health System (IOM, 2000). As reported more recently,
An expanding evidence base demonstrates that serious quality problems exist for patients undergoing transitions across sites of care. Qualitative
studies performed in the United States as well as Canada, Europe, and Australia, have produced remarkably consistent results. These studies have shown that patients are often unprepared for their self-management role in the next care setting, receive conflicting advice regarding chronic illness management, are often unable to reach an appropriate health care practitioner who has access to their care plan when questions arise, have minimal input into their care plan, and are annoyed by having to repeatedly provide the same information to each new set of practitioners. Family caregivers voice feelings of frustration that they are often excluded from care planning meetings, despite their central role in the execution of this care plan. They are also dissatisfied with having to perform tasks that their health care practitioners have left undone. (Coleman, 2006, p. 254)
The ACA includes several provisions that impose penalties for poorly managed care transitions and offer financial incentives for improving transition care (Burton, 2012). Examples of these provisions include reduced payments for readmission rates that exceed particular targets and payment for transition care services in medical homes. State Medicaid agencies also can provide reimbursement for transition care that occurs in “health home” practices, which provide physical, behavioral, and long-term care services.
This recent movement has an associated focus on developing measures for and improving care transitions/handoffs. The transition to adult care is included in the National Committee for Quality Assurance’s (NCQA’s) 2014 Standards and Guidelines for NCQA’s Patient-Centered Medical Home (NCQA, 2014). Transition of care for youth with special health care needs also is included as a Healthy People 2020 indicator (HHS, 2014c). With these exceptions, however, the focus on measuring transitions generally has not included the transition between pediatric and adult systems. For example, the following transitions are considered by the National Transitions of Care Coalition Measures Working Group:
- “Within settings; e.g., primary care to specialty care, or intensive care unit (ICU) to ward.
- Between settings; e.g., hospital to sub-acute care, or ambulatory clinic to senior center.
- Across health states; e.g., curative care to palliative care or hospice, or personal residence to assisted living.
- Between providers; e.g., generalist to a specialist practitioner, or acute care provider to a palliative care specialist.” (NTOCC, 2008, p. 1)
Rather than developing a separate approach for improving the transition to adult health care, we propose drawing attention to this transition
and incorporating it in the current movement to improve transitions generally. Thus we propose that health care delivery systems develop a process for the transition from pediatric to adult care. The recommendations developed by AAP, AAFP, and ACP (AAP et al., 2011; see also Box 7-3) and the six core elements developed by the Got Transition initiative provide an appropriate guide for the develoment of this process, although additional research and evaluation are needed to support these recommendations. We also propose that health care delivery systems include metrics on this transition among their quality performance metrics. Since metrics for this transition do not yet exist, we suggest that AHRQ develop them.
Recommendation 7-1: Health care delivery systems and provider organizations serving young adults (e.g., medical homes, accountable care organizations)—with input from the Agency for Healthcare Research and Quality (AHRQ) and the Centers for Medicare & Medicaid Services (CMS)—should improve the transition process for young adults moving from pediatric to adult medical and behavioral health care.
To implement this recommendation, the committee recommends the following specific actions:
- AHRQ should develop quality performance metrics on the transition-of-care process to ensure continuity of care for young adults making this transition.
- CMS should encourage greater attention to this transition within the innovation models that it solicits and funds, such as those from the Center for Medicare & Medicaid Innovation.
- Health care delivery systems and provider organizations serving young adults should develop a coordinated pediatric-to-adult transition-of-care process within their organizations.
- Pediatric-to-adult transition-of-care performance metrics should be incorporated into quality measurement and reporting frameworks by the National Committee for Quality Assurance, the National Quality Forum, and other quality measurement entities for all health care delivery models serving young adults, such as medical homes, accountable care organizations, and integrated delivery systems.
- The Office of the National Coordinator for Health Information Technology should ensure that meaningful use criteria enable the capture of relevant data elements for this reporting.
- CMS, health insurers, and purchasing entities such as employer coalitions should incorporate young adult transition-of-care met-
-
rics into pay-for-performance initiatives, contracting, and other provider assessments.
- The Maternal and Child Health Bureau in the HRSA should expand its work on transition-of-care metrics for youth with special health care needs to include all youth and young adults, incorporate such metrics in Title V program requirements, and support related capacity development and training in states.
Careful design of these metrics is important so as not to generate perverse incentives for health systems to exclude young adults with special health care needs. Comprehensive coordinated health care delivery systems should give substantial weight to performance metrics for such patients to help ensure that they meet performance requirements by applying better practices to populations similar to those they have served in the past rather than by excluding more unhealthy patients.
The transition from pediatric to adult health care is a lengthier process than some of the other health care transition processes, such as transfers from primary to intensive care. When done well, the transition to adult health care begins several years prior to the actual transfer time and includes patient education and engagement. However, many of the issues related to discontinuities for this transition are analogous to those entailed in other types of transitions. Placing greater emphasis on this transition by including it in transition metrics is likely to have benefits for other aspects of the transition process from pediatric to adult care as well.
Improving Preventive Care for Young Adults
As described in Chapters 2 and 6, young adults are less healthy than commonly perceived, the majority of the health problems they face are preventable, and the health habits developed during these years have lifelong implications. Knowledge about the use and delivery of preventive services for young adults is limited, but the available evidence suggests that young adults receive little preventive care. As discussed earlier, for example, during visits with physicians, including primary care and obstetrics-gynecology providers, most young adults receive no preventive counseling on such critical issues for this age group as injury, smoking, exercise, weight reduction, mental health, and STIs/HIV. Various sets of recommendations (e.g., from USPSTF, ACOG, and Bright Futures) can inform the care of young adults aged 18-26, but there is no consolidated set of guidelines for preventive medical, behavioral, and oral health care specifically focused on the young adult population. Furthermore, the efficacy of these guidelines for young adults is unclear because the age ranges are broad, and young adults are grouped with adults overall. Because young adults’ burden of
disease is different from that of older adults and because other issues, such as fertility, may be of greater concern for this age group, it is important to have evidence-based recommendations assessed specifically for efficacy with young adults.
In addition to recommendations for adults in general, USPSTF provides a special focus on children and adolescents and older adults (USPSTF, 2011, 2013), and convenes workgroups and makes evidence-based recommendations specifically for these populations. USPSTF is the preferred body to develop a consolidated package of evidence-based recommendations for young adults because its existing model could be extended to provide a special focus on the health problems that most affect young adults.
Recommendation 7-2: The U.S. Preventive Services Task Force should develop a consolidated set of standardized evidence-based recommendations for clinical preventive services such as screenings, counseling services, and preventive medications specifically for young adults aged 18-26. Behavioral and oral health should be included in these recommendations.
Once these recommendations have been developed, they will need to be implemented. Federal, state, and local governmental entities that fund or provide physical or behavioral health services—including the U.S. Department of Defense, HHS (through AHRQ, CMS, HRSA, the Indian Health Service, and SAMHSA), the U.S. Department of Veterans Affairs, and corresponding state and local agencies—in partnership with commercial insurers and employer-sponsored health plans, should be involved in improving preventive care for young adults, including increased access to care and content of care that emphasizes preventive visits as part of an array of integrated, comprehensive services.
Recommendation 7-3: Federal, state, and local governments, commercial insurers, employer-sponsored health plans, and medical and behavioral health systems should adopt the clinical preventive services recommended by the U.S. Preventive Services Task Force, include the delivery of those services in quality performance metrics used for pay-for-performance and other health care provider assessments, and require public reporting of compliance.
To improve preventive care for young adults, it will be critically important to drive provider interest in engaging young adults in receiving preventive care, as well as monitor the delivery of these services. Given the broad variety of entities—both governmental and private—involved in providing
preventive care to young adults, we do not recommend specific approaches to driving provider interest and ensuring appropriate monitoring. Rather, we focus on outcomes that should be measured and leave it to organizations to develop their own processes and implementation approaches.
Developing Evidence-Based Practices for Young Adults
Most prevention approaches are targeted at children and adolescents, and some are targeted at college students. With the exception of interventions for treating early psychosis, there are few behavioral health interventions developed specifically for young adults, all of which are in early stages of development, and few interventions with demonstrated efficacy specifically in this age group. Although pharmacological treatments should be as effective in young adults as in older adults, psychosocial treatments and interventions need to be explicitly tested in this age group. Because of the psychosocial nature of nonpharmacological interventions, including preventive interventions, psychotherapy, and other related approaches, such interventions can be influenced by many of the factors that are changing or less mature in young compared with older adults, such as responsibility taking, response to authoritative figures, changing roles within the family, and responses to behavioral contingencies.
Recommendation 7-4: The National Institutes of Health should support research aimed at developing a set of evidence-based practices for medical and behavioral health care, including prevention, for young adults. This research should build on the existing and established evidence-based practices (EBPs) for populations that are older (i.e., adults in general) or younger (i.e., adolescents) to
- identify those EBPs that hold promise for being effective in this age group and test them for efficacy;
- identify EBPs that are likely to be effective with modification for this age group and test the efficacy of the modified versions; and
- identify behavioral and medical health care needs that are unlikely to be addressed by existing or modified EBPs and conduct research to develop and establish new EBPs for young adults in these areas.
In developing methodologies for implementing this recommendation, it will be important to take into account socioeconomic position and racial, ethnic, and geographic disparities and differences, as well as differences according to immigrant and refugee status, across the full spectrum of the social, behavioral, and health indicators under discussion.
Research Priorities
As described throughout this chapter, further research is needed to help improve medical and behavioral health care for young adults. We identified four research needs of particular importance:
- Develop preventive care guidelines for young adults (see Recommendation 7-2).
- Develop a set of evidence-based practices for young adults for medical and behavioral health care encompassing prevention and effective processes for the transition from pediatric to adult care (see Recommendations 7-1, 7-2, 7-3, and 7-4).
- Examine the efficacy of integrating behavioral and physical health care for improving health outcomes for young adults.
- Develop a comprehensive behavioral health screen. (Note that other efforts also are needed to ensure that treatment can be offered if concerns are identified during screening.)
AAFP (American Academy of Family Physicians), AAP (American Academy of Pediatrics), ACP (American College of Physicians), and AOA (American Osteopathic Association). 2007. Joint principles of the patient-centered medical home. http://www.pcpcc.net/content/joint-principles-patient-centered-medical-home (accessed September 11, 2014).
AAP. 1996. Transition of care provided for adolescents with special health care needs. Pediatrics 98:1203-1206.
AAP. 2012. Health care of youth aging out of foster care. Pediatrics 130(6):1170-1173.
AAP, AAFP, and ACP. 2002. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics 110(Suppl. 3):1304-1306.
AAP, AAFP, and ACP. 2011. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 128(1):182-200.
AAPD (American Academy of Pediatric Dentistry). 2013. Guideline on periodicity of examination, preventive dental services, anticipatory guidance/counseling, and oral treatment for infants, children, and adolescents. Clinical Guidelines 35(6):114-122.
Abbott, R. A., R. Whear, L. R. Rodgers, A. Bethel, J. Thompson Coon, W. Kuyken, K. Stein, and C. Dickens. 2014. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of Psychosomatic Research 76(5):341-351.
ABP (American Board of Pediatrics). 2010. Content outline: Adolescent medicine subspecialty in-training, certification, and maintenance of certification examinations. https://www.abp.org/abpwebsite/takeexam/subspecialtycertifyingexam/contentpdfs/adol2010.pdf (accessed March 28, 2014).
ACGME (Accreditation Council for Graduate Medical Education). 2007. ACGME program requirements for graduate medical education in child and adolescent psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/405_child_and_adolescent_psych_07012014.pdf (accessed July 25, 2014).
ACGME. 2008a. ACGME program requirements for graduate medical education in hospice and palliative medicine. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/540_hospice_and_palliative_medicine_02122008.pdf (accessed March 28, 2014).
ACGME. 2008b. ACGME program requirements for graduate medical education in obstetrics and gynecology. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/220_obstetrics_and_gynecology_07012014.pdf (accessed July 25, 2014).
ACGME. 2009. ACGME program requirements for graduate medical education in internal medicine. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/140_internal_medicine_07012013.pdf (accessed July 25, 2014).
ACGME. 2012. ACGME program requirements for graduate medical education in pediatrics. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013-PR-FAQ-PIF/320_pediatrics_07012013.pdf (accessed March 28 2014).
ACGME. 2013. ACGME program requirements for graduate medical education in family medicine. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/120_family_medicine_07012014.pdf (accessed July 25, 2014).
ADA (American Dental Association). 2013. Affordable Care Act, dental benefits examined. http://www.ada.org/en/publications/ada-news/2013-archive/august/affordable-care-act-dental-benefits-examined (accessed July 24, 2014).
Adams, S. H., P. W. Newacheck, M. J. Park, C. D. Brindis, and C. E. Irwin, Jr. 2013. Medical home for adolescents: Low attainment rates for those with mental health problems and other vulnerable groups. Academic Pediatrics 13(2):113-121.
Agorastos, A., C. R. Marmar, and C. Otte. 2011. Immediate and early behavioral interventions for the prevention of acute and posttraumatic stress disorder. Current Opinion in Psychiatry 24(6):526-532.
AHRQ (Agency for Healthcare Research and Quality). 2014. Medical Expenditure Panel Survey. http://meps.ahrq.gov/mepsweb (accessed July 24, 2014).
Álvarez-Jiménez, M., A. G. Parker, S. E. Hetrick, P. D. McGorry, and J. F. Gleeson. 2011. Preventing the second episode: A systematic review and meta-analysis of psychosocial and pharmacological trials in first-episode psychosis. Schizophrenia Bulletin 37(3):619-630.
American Board of Clinical Child and Adolescent Psychology. 2013. Examination manual for board certification in clinical child and adolescent psychology. http://www.abpp.org/files/page-specific/3352%20Clinical%20Child/16_Examination_Manual.pdf (accessed March 28, 2014).
Archer, J., P. Bower, S. Gilbody, K. Lovell, D. Richards, L. Gask, C. Dickens, and P. Coventry. 2012. Collaborative care for people with depression and anxiety. http://summaries.cochrane.org/CD006525/DEPRESSN_collaborative-care-for-people-with-depression-and-anxiety (accessed July 24, 2014).
Armstrong, E. 2012a. NHeLP breaks down preventive health services standards & contraceptive coverage under the ACA. Washington, DC: National Health Law Program.
Armstrong, E. 2012b. Q&A on preventive services for women coverage requirements. Washington, DC: National Health Law Program.
ASPE (Assistant Secretary for Planning and Evaluation). 2014. Health insurance marketplace: Summary enrollment report for the initial annual open enrollment period. Washington, DC: HHS.
ASWB (Association of Social Work Boards). 2014. Content outlines and KSAs: Social work licensing examinations. http://www.aswb.org/wp-content/uploads/2014/02/BachelorsKSAs.pdf (accessed July 25, 2014).
Baillargeon, J., S. Contreras, J. J. Grady, S. A. Black, and O. Murray. 2000. Compliance with antidepressant medication among prison inmates with depressive disorders. Psychiatric Services 51(11):1444-1446.
Beardslee, W. R., D. A. Brent, V. R. Weersing, G. N. Clarke, G. Porta, S. D. Hollon, T. R. Gladstone, R. Gallop, F. L. Lynch, and S. Iyengar. 2013. Prevention of depression in at-risk adolescents: Longer-term effects. JAMA Psychiatry 70(11):1161-1170.
Benson, R., D. Steidtmann, and Y. Valks. 2014. A triple aim approach to transition from pediatric adult health care for youth with special health care needs. http://cshcn.wpengine.netdna-cdn.com/wp-content/uploads/2014/05/A-Triple-Aim-Approach-to-Transition.pdf (accessed September 26, 2014).
Berwick D. M., T. W. Nolan, and J. Whittington. 2008. The triple aim: Care, health, and cost. Health Affairs 27(3):759-769.
Bleyer, A., and R. Barr. 2009. Cancer in young adults 20 to 39 years of age: Overview. Seminars in Oncology 36(3):194-206.
Bleyer, A., R. Barr, B. Hayes-Lattin, D. Thomas, C. Ellis, and B. Anderson. 2008. The distinctive biology of cancer in adolescents and young adults. Nature Reviews Cancer 8(4):288-298.
Blount, A. 2003. Integrated primary care: Organizing the evidence. Families, Systems, & Health 21(2):121.
Blum, A., A. Giordano, M. J. Park, S. Rosenbaum, and C. D. Brindis. in press. Implementing health reform in an era of semi-cooperative federalism: Lessons from the age 26 expansion. Journal of Health and Biomedical Law.
Blum, R. W., D. Garell, C. H. Hodgman, T. W. Jorissen, N. A. Okinow, D. P. Orr, and G. B. Slap. 1993. Transition from child-centered to adult health-care systems for adolescents with chronic conditions: A position paper of the Society for Adolescent Medicine. Journal of Adolescent Health 14(7):570-576.
Blumenthal, D., and S. R. Collins. 2014. Health care coverage under the Affordable Care Act—a progress report. New England Journal of Medicine 371:275-281.
Bodenlos, J. S., M. Noonan, and S. Y. Wells. 2013. Mindfulness and alcohol problems in college students: The mediating effects of stress. Journal of American College Health 61(6):371-378.
Boekeloo, B. O., and M. A. Griffin. 2007. Review of clinical trials testing the effectiveness of physician approaches to improving alcohol education and counseling in adolescent outpatients. Current Pediatric Reviews 3(1):93-101.
Boekeloo, B. O., M. P. Bobbin, W. I. Lee, K. D. Worrell, E. K. Hamburger, and E. RussekCohen. 2003. Effect of patient priming and primary care provider prompting on adolescent-provider communication about alcohol. Archives of Pediatrics & Adolescent Medicine 157(5):433-439.
Bond, G. R. 1998. Principles of the individual placement and support model: Empirical support. Psychiatric Rehabilitation Journal 22(1):11.
Bower, P. 2002. Primary care mental health workers: Models of working and evidence of effectiveness. British Journal of General Practice 52(484):926-933.
Bower, P., E. Garralda, T. Kramer, R. Harrington, and B. Sibbald. 2001. The treatment of child and adolescent mental health problems in primary care: A systematic review. Family Practice 18(4):373-382.
Bradley, G., B. Sparks, and D. Nesdale. 2001. Doctor communication style and patient outcomes: Gender and age as moderators. Journal of Applied Social Psychology 31(8): 1749-1773.
Braithwaite, S. R., and F. D. Fincham. 2007. ePREP: Computer based prevention of relationship dysfunction, depression and anxiety. Journal of Social and Clinical Psychology 26(5):609-622.
Brindis, C. D., M. Hadler, K. Jacobs, N. Pourat, M. Raymond-Flesch, R. Siemons, and E. Talamantes. 2014. Realizing the dream for Californians eligible for deferred action for childhood arrivals (DACA): Health needs and access to health care. San Francisco, CA: Philip R. Lee Institute for Health Policy Studies, University of California, San Francisco.
Brousseau, D. C., P. L. Owens, A. L. Mosso, J. A. Panepito, and C. A. Steiner. 2010. Acute care utilization and rehospitalizations for sickle cell disease. Journal of the American Medical Association 303:1288-1294.
Burke-Miller, J., L. A. Razzano, D. D. Grey, C. R. Blyler, and J. A. Cook. 2012. Supported employment outcomes for transition age youth and young adults. Psychiatric Rehabilitation Journal 35(3):171.
Burton, L. 2012. Health policy brief: Improving care transitions. Health Affairs September 12.
Callahan, S. T., and W. O. Cooper. 2010. Changes in ambulatory health care use during the transition to young adulthood. Journal of Adolescent Health 46(5):407-413.
Capoccia, V., C. Croze, M. Cohen, and J. P. O’Brien. 2013. Sustaining enrollment in health insurance for vulnerable populations: Lessons from Massachusetts. Psychiatric Services 64(4):360-365.
CDC (Centers for Disease Control and Prevention). 2014a. Ambulatory health care data. http://www.cdc.gov/nchs/ahcd.htm (accessed July 24, 2014).
CDC. 2014b. Behavioral Risk Factor Surveillance System. http://www.cdc.gov/brfss (accessed July 24, 2014).
CDC. 2014c. National Health Interview Survey. http://www.cdc.gov/nchs/nhis.htm (accessed August 7, 2014).
Center for Health Care Transition Improvement. 2012. Guardianship and alternatives for decision-making support. http://www.gottransition.org/resourceGet.cfm?id=17 (accessed September 25, 2014).
CFF (Cystic Fibrosis Foundation). 2012. Patient registry annual data report 2012. Bethesda, MD: CFF.
Chiesa, A., and A. Serretti. 2014. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse 49(5):492-512.
Children’s Bureau. 2013. The AFCARS report. Rockville, MD: HHS.
Children’s Bureau Training and Technical Assistance Network. 2008. Implementing the Fostering Connections Act: How the Children’s Bureau national resource centers and implementation centers can help states and tribes. https://www.ttaccportal.org/sites/www.ttaccportal.org/files/Implementing%20Fostering%20Connections%20Act%20Fact%20Sheet%20-%20Youth%20Transition%20D3%20ab%2011AUG08.pdf (accessed July 24, 2014).
Christensen, H., E. Pallister, S. Smale, I. B. Hickie, and A. L. Calear. 2010. Community-based prevention programs for anxiety and depression in youth: A systematic review. Journal of Primary Prevention 31(3):139-170.
Clarke, G. N., W. Hawkins, M. Murphy, L. B. Sheeber, P. M. Lewinsohn, and J. R. Seeley. 1995. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of a group cognitive intervention. Journal of the American Academy of Child & Adolescent Psychiatry 34(3):312-321.
Clarke, G. N., M. Hornbrook, F. Lynch, M. Polen, J. Gale, W. Beardslee, E. O’Connor, and J. Seeley. 2001. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Archives of General Psychiatry 58(12):1127-1134.
Clarke, G., C. Kelleher, M. Hornbrook, L. DeBar, J. Dickerson, and C. Gullion. 2009. Randomized effectiveness trial of an Internet, pure self-help, cognitive behavioral intervention for depressive symptoms in young adults. Cognitive Behaviour Therapy 38(4):222-234.
CMHS (Center for Mental Health Services) and CSAT (Center for Substance Abuse Treatment). 2013. Diagnoses and health care utilization of children who are in foster care and covered by Medicaid. Rockville, MD: CMHS and CSAT, SAMHSA.
CMS (Center for Medicare & Medicaid Services). 2014a. The Center for Consumer Information & Insurance Oversight: Additional information on proposed state essential health benefits benchmark plans. http://www.cms.gov/CCIIO/Resources/Data-Resources/ehb.html (accessed August 4, 2014).
CMS. 2014b. Student health insurance final rule. http://www.regulations.gov/#!documentDetail;D=CMS-2011-0016-0108 (accessed July 24, 2014).
CMS. 2014c. Catastrophic health insurance plans. https://www.healthcare.gov/can-i-buy-a-catastrophic-plan (accessed September 27, 2014).
CMS. 2014d. Young adults and the Affordable Care Act: Protecting young adults and eliminating burdens on families and businesses. http://www.cms.gov/CCIIO/Resources/Files/adult_child_fact_sheet.html (accessed July 24, 2014).
CMS. 2014e. 2014 core set of health care quality measures for adults enrolled in Medicaid. http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-ofCare/Downloads/AdultCoreMeasures.pdf (accessed July 24, 2014).
CMS. 2014f. Student health plans. http://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/Student-Health-Plans.html (accessed September 26, 2014).
Coleman, E. 2006. Transitional care performance measurement. Paper commissioned by the Institute of Medicine. In Performance measurement: Accelerating improvement (Appendix I). Washington, DC: The National Academies Press. Pp. 250-286.
Collins, S. R., and J. Nicholson. 2010. Realizing health reform’s potential: Young adults and the Affordable Care Act of 2010. New York: The Commonwealth Fund.
Collins, S. R., R. Robertson, T. Garber, and M. M. Doty. 2012. Young, uninsured, and in debt: Why young adults lack health insurance and how the Affordable Care Act is helping findings from The Commonwealth Fund Health Insurance Tracking Survey of Young Adults, 2011. Washington, DC: The Commonwealth Fund.
Collins, S. R., P. Rasmussen, T. Garber, and M. M. Doty. 2013. Covering young adults under the Affordable Care Act: The importance of outreach and Medicaid expansion. New York: The Commonwealth Fund.
Colorado Consumer Health Initiative and ProgressNow Colorado Education. 2014. Got insurance? http://doyougotinsurance.com/index.php?id=2 (accessed July 24, 2014).
Copeland, W., L. Shanahan, E. J. Costello, and A. Angold. 2011. Cumulative prevalence of psychiatric disorders by young adulthood: A prospective cohort analysis from the Great Smoky Mountains Study. Journal of the American Academy of Child and Adolescent Psychiatry 50(3):252-261.
Copeland, W. E., L. S. Shanahan, M. Davis, B. J. Burns, A. Angold and E. J. Costello. in press. Untreated psychiatric cases increase during the transition to adulthood. Psychiatric Services.
Cruess, D. G., M. H. Antoni, M. Kumar, G. Ironson, P. McCabe, J. B. Fernandez, M. Fletcher, and N. Schneiderman. 1999. Cognitive-behavioral stress management buffers decreases in dehydroepiandrosterone sulfate (DHEA-S) and increases in the cortisol/DHEA-S ratio and reduces mood disturbance and perceived stress among HIV-seropositive men. Psychoneuroendocrinology 24(5):537-549.
Cukrowicz, K. C., and T. E. Joiner, Jr. 2007. Computer-based intervention for anxious and depressive symptoms in a non-clinical population. Cognitive Therapy and Research 31(5):677-693.
Cunningham, C. E., J. R. Walker, J. D. Eastwood, H. Westra, H. Rimas, Y. Chen, and M. Marcus. 2014. Modeling mental health information preferences during the early adult years: A discrete choice conjoint experiment. Journal of Health Communication: Internatonal Perspectives 19(4):413-440.
Cutcliffe, J. R., and B. Saadeh. 2014. Grounded in evidence or a puritanical legacy: A critique of twenty-first-century U.S. drug policy. Mental Health and Substance Use 7(3):195-206.
Davis, M. 2003. Addressing the needs of youth in transition to adulthood. Administration and Policy in Mental Health and Mental Health Services Research 30(6):495-509.
Davis, M. 2013. Young adult mental health. Presentation at IOM/NRC Workshop on Improving the Health, Safety, and Well-Being of Young Adults, Washington, DC. http://www.iom.edu/~/media/Files/Activity%20Files/Children/ImprovingYoungAdultsHealth/Davis%20Presentation.pdf (accessed September 27, 2014).
Davis, M., and N. Koroloff. 2006. The great divide: How public mental health policy fail young adults. Community Based Mental Health Services for Children and Adolescents 14:53-74.
Davis, M., J. Geller, and B. Hunt. 2006. Within-state availability of transition-to-adulthood services for youths with serious mental health conditions. Psychiatric Services 57(11):1594-1599.
Davis, M., M. Green, and C. Hoffman. 2009. The service system obstacle course for transition-age youth and young adults. In Transition of youth and young adults with emotional or behavioral difficulties: An evidence-based handbook, edited by H. B. Clark and D. Unruh. Baltimore, MD: Paul H. Brookes Publishing Company. Pp. 25-46.
Davis, M., N. Koroloff, and M. L. Ellison. 2012a. Between adolescence and adulthood: Rehabilitation research to improve services for youth and young adults. Psychiatric Rehabilitation Journal 35(3):167-170.
Davis, M., N. Koroloff, and M. Johnsen. 2012b. Social network analysis of child and adult interorganizational connections. Psychiatric Rehabilitation Journal 35(3):265-272.
Davis, M., M. Abrams, L. Wissow, and E. Slade. 2014. Imminent Medicaid enrollment lapses after inpatient mental health treatment in young adults. Psychiatric Services 65(4):461-468.
De Bont, J., B. Van Der Holt, and A. Dekker. 2004. Significant difference in outcome for adolescents with acute lymphoblastic leukemia treated on pediatric vs. adult protocols in the Netherlands. Leukemia 18(12):2032-2035.
DeBaun, M. R., and J. Telfair. 2012. Transition and sickle cell disease. Pediatrics 130(5): 926-935.
Delman, J. 2012. Young adults with mental illness: Their active participation in medication decisions and in research. Ph.D. dissertation, Boston University.
Drucker, E. 2012. Drugs: The third rail of U.S. politics. Lancet 380(9854):1626-1628.
Druss, B. G., L. Zhao, S. A. von Esenwein, J. R. Bona, L. Fricks, S. Jenkins-Tucker, E. Sterling, R. DiClemente, and K. Lorig. 2010. The Health and Recovery Peer (HARP) Program: A peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophrenia Research 118(1):264-270.
Edlund, M. J., P. S. Wang, P. A. Berglund, S. J. Katz, E. Lin, and R. C. Kessler. 2002. Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. American Journal of Psychiatry 159(5):845-851.
Elster, A., and N. Kuznets. 1994. Guidelines for Adolescent Preventive Services (GAPS): Recommendations and rationale. Baltimore, MD: American Medical Association.
Emans, S. J., S. B. Austin, E. Goodman, D. P. Orr, R. Freeman, D. Stoff, I. F. Litt, M. A. Schuster, R. Haggerty, and R. Granger. 2010. Improving adolescent and young adult health—training the next generation of physician scientists in transdisciplinary research. Journal of Adolescent Health 46(2):100-109.
English, A., and M. Park. 2012. The Supreme Court ACA decision: What happens now for adolescents and young adults. Chapel Hill, NC: Center for Adolescent Health and the Law National Adolescent and Young Adult Health Information Center.
English, A., A. Stinnett, and E. Dunn-Georgiou. 2006. Health care for adolescents and young adults leaving foster care: Policy options for improving access. Chapel Hill, NC: Center for Adolescent Health and the Law.
English, A., J. Scott, and M. Park. 2014. Implementing the Affordable Care Act: How much will it help vulnerable adolescents and young adults? Chapel Hill, NC: Center for Adolescent Health and the Law.
EuTEACH. 2014. About EuTEACH. http://www.unil.ch/euteach/home/menuinst/abouteuteach.html (accessed March 28, 2014).
Fagan, J., and F. E. Zimring. 2000. The changing borders of juvenile justice: Transfer of adolescents to the criminal court. Chicago, IL: University of Chicago Press.
FamiliesUSA. 2014. Federal poverty guidelines. http://familiesusa.org/product/federal-poverty-guidelines (accessed July 25, 2014).
Ford, C., A. English, and G. Sigman. 2004. Confidential health care for adolescents: Position paper of the society for adolescent medicine. Journal of Adolescent Health 35(2):160-167.
Fordham, B., C. E. Griffiths, and C. Bundy. 2013. Can stress reduction interventions improve psoriasis?: A review. Psychology, Health and Medicine 18(5):501-514.
Fortuna, R. J., B. W. Robbins, and J. S. Halterman. 2009. Ambulatory care among young adults in the United States. Annals of Internal Medicine 151(6):379-385.
Fortuna, R. J., B. W. Robbins, N. Mani, and J. S. Halterman. 2010. Dependence on emergency care among young adults in the United States. Journal of General Internal Medicine 25(7):663-669.
Fox, H. B., M. A. McManus, J. D. Klein, A. Diaz, A. B. Elster, M. E. Felice, D. W. Kaplan, C. J. Wibbelsman, and J. E. Wilson. 2010. Adolescent medicine training in pediatric residency programs. Pediatrics 125(1):165-172.
Fox, S., and M. Duggan. 2013. Tracking for health. Washington, DC: Pew Research Center’s Internet and American Life Project.
GAO (U.S. Government Accountability Office). 2008. Young adults with serious mental illness: Some states and federal agencies are taking steps to address their transition challenges. Washington, DC: GAO.
Garrett, C. C., J. Hocking, M. Y. Chen, C. K. Fairley, and M. Kirkman. 2011. Young people‘s views on the potential use of telemedicine consultations for sexual health: Results of a national survey. BMC Infectious Diseases 11:285.
Georgetown University Center for Child and Human Development. 2014. Emerging adults initiative. http://gucchdtacenter.georgetown.edu/transitions.html (accessed July 26, 2014).
Gettens, J., M. Mitra, A. D. Henry, and J. Himmelstein. 2011. Have working-age people with disabilities shared in the gains of Massachussetts health reform? INQUIRY: The Journal of Health Care Organization, Provision, and Financing 48(3):183-196.
Gilmer, T. P., V. D. Ojeda, K. Fawley-King, B. Larson, and P. Garcia. 2012. Change in mental health service use after offering youth-specific versus adult programs to transition-age youths. Psychiatric Services 63(6):592-596.
Gleeson, J., S. M. Cotton, M. Álvarez-Jiménez, D. Wade, D. Gee, K. Crisp, T. Pearce, B. Newman, D. Spiliotacopoulos, and D. Castle. 2009. A randomized controlled trial of relapse prevention therapy for first-episode psychosis patients. Journal of Clinical Psychiatry 70(4):477-486.
Glied, S., and D. Oellerich. 2014. Two-generation programs and health. The Future of Children 24(1):79-98.
GPO (U.S. Government Printing Office). 2012. Medicaid program: Initial core set of health care quality measures for Medicaid-eligible adults. Federal Register 77(2):286-291.
GPO. 2013. Patient Protection and Affordable Care Act; health insurance market rules; rate review. Federal Register 78(39):13406-13442.
Green, M. 1994. Bright Futures: Guidelines for health supervision of infants, children, and adolescents. Arlington, VA: National Center for Education in Maternal and Child Health.
Gudeman, R. 2013. The Affordable Care Act and adolescent health. http://www.youthlaw.org/publications/yln/2013/jul_sep_2013/affordable_care_act_adolescent_health (accessed July 26, 2014).
Gupta, A. A., K. Edelstein, A. Albert-Green, and N. D’Agostino. 2013. Assessing information and service needs of young adults with cancer at a single institution: The importance of information on cancer diagnosis, fertility preservation, diet, and exercise. Support Care Cancer 21(9):2477-2484.
Gurvitz, M., A. M. Valente, C. Broberg, S. Cook, K. Stout, J. Kay, J. Ting, K. Kuehl, M. Earing, and G. Webb. 2013. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial). Journal of the American College of Cardiology 61(21):2180-2184.
Gusmano, M. 2012. Undocumented immigrants in the United States: U.S. health policy and access to care. http://www.undocumentedpatients.org/issuebrief/health-policy-and-access-to-care (accessed July 24, 2014).
GW (George Washington) Cancer Institute). 2014. Thriving after cancer. http://smhs.gwu.edu/gwci/patient-care/survivors/tac (accessed September 24, 2014).
Haddock, G., S. Lewis, R. Bentall, G. Dunn, R. Drake, and N. Tarrier. 2006. Influence of age on outcome of psychological treatments in first-episode psychosis. The British Journal of Psychiatry 188(3):250-254.
Hagan, J. F., J. S. Shaw, and P. M. Duncan. 2008. Bright futures: Guidelines for health supervision of infants, children, and adolescents. Elk Grove Village, IL: AAP.
Halfon, N., A. Mendonca, and G. Berkowitz. 1995. Health status of children in foster care: The experience of the Center for the Vulnerable Child. Archives of Pediatrics & Adolescent Medicine 149(4):386-392.
Hall, K. S., C. Moreau, and J. Trussell. 2012. Continuing social disparities despite upward trends in sexual and reproductive health service use among young women in the United States. Contraception 86(6):681-686.
Hayes-Lattin, B., B. Mathews-Bradshaw, and S. Siegel. 2010. Adolescent and young adult oncology training for health professionals: A position statement. Journal of Clinical Oncology 28(32):4858-4861.
HealthSource RI. 2014. HealthSource RI launches “nag tool kit” Facebook campaign for young invincibles and their moms. http://www.healthsourceri.com/press-releases/health-source-ri-launches-nag-tool-kit-facebook-campaign-for-young-invincibles-and-theirmoms (accessed July 24, 2014).
Heberlein, M., T. Brooks, J. Guyer, S. Artiga, and J. Stephens. 2012. Performing under pressure: Annual findings of a 50-state survey of eligibility, enrollment, renewal, and cost-sharing policies in Medicaid and CHIP, 2011-2012. Washington, DC: KFF.
Hemmeter, J. 2012. Research and statistics note no. 2012-04. http://www.socialsecurity.gov/policy/docs/rsnotes/rsn2012-04.html (accessed July 28, 2014).
Henggeler, S. W., S. K. Schoenwald, C. M. Borduin, M. D. Rowland, and P. B. Cunningham. 1998. Multisystemic treatment of antisocial behavior in children and adolescents. New York: Guilford Press.
Hergenroeder, A. C., P. A. Benson, M. T. Britto, M. Catallozzi, L. J. D’Angelo, J. C. Edman, S. J. Emans, E. C. Kish, R. H. Pasternak, and G. B. Slap. 2010. Adolescent medicine: Workforce trends and recommendations. Archives of Pediatrics & Adolescent Medicine 164(12):1086-1090.
Hernandez-Boussard, T., C. S. Burns, N. Ewen Wang, L. C. Baker, and B. A. Goldstein. 2014. The Affordable Care Act reduces emergency department use by young adults: Evidence from three states. Health Affairs 33(9):1648-1654.
HHS (U.S. Department of Health and Human Services). 1999. Mental health: A report of the Surgeon General. Washington, DC: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health.
HHS. 2012. Preventive services covered under the Affordable Care Act. http://www.hhs.gov/healthcare/facts/factsheets/2010/07/preventive-services-list.html (accessed July 24, 2014).
HHS. 2014a. Deferred action for childhood arrivals. http://www.dhs.gov/deferred-action-childhood-arrivals (accessed August 12, 2014).
HHS. 2014b. mHealth initiative. http://www.hhs.gov/open/initiatives/mhealth (accessed July 26, 2014).
HHS. 2014c. Healthy People 2020 DH-5 data details. http://www.healthypeople.gov/2020/topicsobjectives2020/DataDetails.aspx?hp2020id=DH-5 (accessed September 26, 2014).
Hoge, C. W., and C. A. Castro. 2012. Preventing suicides in U.S. service members and veterans: Concerns after a decade of war. Journal of the American Medical Association 308(7):671-672.
Hourani, L. L., C. L. Council, R. C. Hubal, and L. B. Strange. 2011. Approaches to the primary prevention of posttraumatic stress disorder in the military: A review of the stress control literature. Military Medicine 176(7):721-730.
Hower, H., B. G. Case, B. Hoeppner, S. Yen, T. Goldstein, B. Goldstein, B. Birmaher, L. Weinstock, D. Topor, and J. Hunt. 2013. Use of mental health services in transition age youth with bipolar disorder. Journal of Psychiatric Practice 19(6):464-476.
HRSA (Health Resources and Services Administration). 2014. Women’s preventive services guidelines. http://hrsa.gov/womensguidelines (accessed July 24, 2014).
Hughes, J. W., D. M. Fresco, R. Myerscough, M. H. van Dulmen, L. E. Carlson, and R. Josephson. 2013. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosomatic Medicine 75(8):721-728.
IHI (Institute for Healthcare Improvement). 2014. The Triple Aim Initiative. http://www.ihi.org/Engage/Initiatives/TripleAim/pages/default.aspx (accessed September 29, 2014).
Insel, T. 2014. Director’s blog: The paradox of parity. http://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml (accessed July 28, 2014).
IOM (Institute of Medicine). 1994. Reducing risks for mental disorders: Frontiers for preventive intervention research. Washington, DC: National Academy Press.
IOM. 2000. To err is human: Building a safer health system. Washington, DC: National Academy Press.
IOM. 2001. Envisioning the National Health Care Quality Report. Washington, DC: National Academy Press.
IOM. 2009. America’s uninsured crisis: Consequences for health and health care. Washington, DC: The National Academies Press.
IOM. 2011. Clinical preventive services for women: Closing the gaps. Washington, DC: The National Academies Press.
IOM. 2013a. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
IOM. 2013b. Identifying and addressing the needs of adolescents and young adults with cancer: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2014. Developing evidence-based standards for psychosocial interventions for mental disorders. http://iom.edu/Activities/MentalHealth/PsychosocialInterventions.aspx (accessed July 28, 2014).
Irwin, Jr., C. E. 2010. Young adults are worse off than adolescents. Journal of Adolescent Health 46(5):405-406.
Jan, S., G. Slap, K. Smith-Whitley, D. Dai, R. Keren, and D. M. Rubin. 2013. Association of hospital and provider types on sickle cell disease outcomes. Pediatrics 132(5):854-861.
Jones, S. P., V. Patel, S. Saxena, N. Radcliffe, S. Ali Al-Marri, and A. Darzi. 2014. How Google’s “ten things we know to be true” could guide the development of mental health mobile apps. Health Affairs 33(9):1603-1611.
Joseph-William, N., G. Elwyn, and A. Edwards. 2014. Knowledge is not power for patients: A systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Education and Counseling 94(3):291-309.
Kaplan, K., M. S. Salzer, and E. Brusilovskiy. 2012. Community participation as a predictor of recovery-oriented outcomes among emerging and mature adults with mental illnesses. Psychiatric Rehabilitation Journal 35(3):219-229.
Kaufman, L., W. Brooks, M. Steinley-Bumgarner, and S. Stevens-Manser. 2012. Peer specialist training and certification programs: A national overview. Austin: University of Texas at Austin Center for Social Work Research.
Kenyon, R. V., and J. Leigh. 2011. Human augmentics: Augmenting human evolution. Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society 2011:6758-6761.
Kessing, L. V., L. Søndergård, K. Kvist, and P. K. Andersen. 2007. Adherence to lithium in naturalistic settings: Results from a nationwide pharmacoepidemiological study. Bipolar Disorders 9(7):730-736.
KFF (The Henry J. Kaiser Family Foundation). 2013. Establishing health insurance exchanges: An overview of state efforts. http://kff.org/health-reform/issue-brief/establishing-health-insurance-exchanges-an-overview-of (accessed July 25, 2014).
KFF. 2014a. Status of state action on the Medicaid expansion decision, 2014. http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-theaffordable-care-act (accessed July 28, 2014).
KFF. 2014b. The coverage gap: Uninsured poor adults in states that do not expand Medicaid. Washington, DC: KFF. http://kff.org/medicaid/issue-brief/analyzing-the-impact-of-state-medicaid-expansion-decisions (accessed October 13, 2014).
KFF. 2014c. How will the uninsured fare under the Affordable Care Act? http://kff.org/health-reform/fact-sheet/how-will-the-uninsured-fare-under-the-affordable-care-act (accessed September 28, 2014).
Khoury, B., T. Lecomte, B. A. Gaudiano, and K. Paquin. 2013. Mindfulness interventions for psychosis: A meta-analysis. Schizophrenia Research 150(1):176-184.
Killackey, E., H. J. Jackson, and P. D. McGorry. 2008. Vocational intervention in first-episode psychosis: Individual placement and support v. Treatment as usual. The British Journal of Psychiatry 193(2):114-120.
Klein, J. D., T. S. Sesselberg, B. Gawronski, L. Handwerker, F. Gesten, and A. Schettine. 2003. Improving adolescent preventive services through state, managed care, and community partnerships. Journal of Adolescent Health 32(6):91-97.
Knopik, V. S. 2009. Maternal smoking during pregnancy and child outcomes: Real or spurious effect? Developmental Neuropsychology 34(1):1-36.
Kotogal, M., A. C. Carle, L. G. Kessler, and D. R. Flum. 2014. Limited impact on health and access to care for 19- to 25-year olds following the Patient Protection and Affordable Care Act. JAMA Pediatrics [Epub ahead of print].
Kovacs, A. H., and B. W. McCrindle. 2014. So hard to say goodbye: Transition from paediatric to adult cardiology care. Nature Reviews Cardiology 11:51-62.
Koyanagi, K., and E. Alfano. 2013. Promise for the future: How federal programs can improve the career outcomes for youth and young adults with serious mental health conditions. Worcester, MA: University of Massachusetts Medical School and Washington, DC: Bazelon Center for Mental Health Law.
Kramer, T., and M. E. Garralda. 2000. Child and adolescent mental health problems in primary care. Advances in Psychiatric Treatment 6(4):287-294.
Kulesza, M., M. A. McVay, M. E. Larimer, and A. L. Copeland. 2013. A randomized clinical trial comparing the efficacy of two active conditions of a brief intervention for heavy college drinkers. Addictive Behavior 38(4):2094-2101.
Labacher, L., and C. Mitchell. 2013. Talk or text to tell? How young adults in Canada and South Africa prefer to receive STI results, counseling, and treatment updates in a wireless world. Journal of Health Communication 18(12):1465-1476.
Lau, J. S., S. H. Adams, W. J. Boscardin, C. E. Irwin, Jr. 2013a. Health care utilization and expenditures among young adults prior to the Affordable Care Act 2010. Journal of Adolescent Health 52(2 Suppl 1):S1-121.
Lau, J. S., S. H. Adams, C. E. Irwin, Jr., and E. M. Ozer. 2013b. Receipt of preventive health services in young adults. Journal of Adolescent Health 52(1):42-49.
Lau, J. S., S. H. Adams, W. J. Boscardin, and C. E. Irwin, Jr. 2014a. Young adults’ health care utilization and expenditures prior to the Affordable Care Act. Journal of Adolescent Health 54(6):663-671.
Lau, J., S. Adams, M. Park, J. Boscardin, and C. E. Irwin, Jr. 2014b. Improvement in preventive care of young adults after the Affordable Care Act: The Affordable Care Act is helping. JAMA Pediatrics. Published online October 27, 2014. doi:10.1001/jamapediatrics.2014.1691.
Lauche, R., H. Cramer, G. Dobos, J. Langhorst, and S. Schmidt. 2013. A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. Journal of Psychosomatic Research 75(6):500-510.
Lehmann, B., J. Guyer, and K. Lewandowski. 2012. Child welfare and the Affordable Care Act: Key provisions for foster care children and youth. Washington, DC: Georgetown University Health Policy Institute.
Lehrer, J. A., R. Pantell, K. Tebb, and M.-A. Shafer. 2007. Forgone health care among U.S. adolescents: Associations between risk characteristics and confidentiality concern. Journal of Adolescent Health 40(3):218-226.
Lindstrom Johnson, S., S. D. Tandon, M. Trent, V. Jones, and T. L. Cheng. 2012. Use of technology with health care providers: Perspectives from urban youth. Journal of Pediatrics 160(6):997-1002.
Lloyd-Evans, B., E. Mayo-Wilson, B. Harrison, H. Istead, E. Brown, S. Pilling, S. Johnson, and T. Kendall. 2014. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry 14(1):39.
Long, S. K., A. Yemane, and K. Stockley. 2010. Disentangling the effects of health reform in Massachusetts: How important are the special provisions for young adults? The American Economic Review 297-302.
Lorig, K., P. L. Ritter, F. J. Villa, and J. Armas. 2009. Community-based peer-led diabetes self-management a randomized trial. The Diabetes Educator 35(4):641-651.
Lotstein, D. S., M. Seid, G. Klingensmith, D. Case, J. M. Lawrence, C. Pihoker, D. Dabelea, E. J. Mayer-Davis, L. K. Gilliam, and S. Corathers. 2013. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 131(4):e1062-e1070.
Magrab, P., and H. Millar. 1989. Growing up and getting medical care: Youth with special health care needs. Surgeon General’s Conference. Washington, DC: Georgetown University Child Development Center.
Major, B. S., M. F. Hinton, A. Flint, A. Chalmers-Brown, K. McLoughlin, and S. Johnson. 2010. Evidence of the effectiveness of a specialist vocational intervention following first episode psychosis: A naturalistic prospective cohort study. Social Psychiatry and Psychiatric Epidemiology 45(1):1-8.
Mammen, G., and G. Faulkner. 2013. Physical activity and the prevention of depression: A systematic review of prospective studies. American Journal of Preventive Medicine 45(5):649-657.
Mann, C. 2012. CMCS informational bulletin. http://www.medicaid.gov/Federal-PolicyGuidance/downloads/CIB-1-4-2012.pdf (accessed July 24, 2014).
Marwick, A. E. 2013. Status update: Celebrity, publicity, and branding in the social media age. New Haven, CT: Yale University Press.
MCH (Maternal and Child Health) Leadership Competencies Workgroup. 2009. Maternal and Child Health leadership competencies. Version 3.0. Rockville, MD: MCH, HRSA, HHS.
McManus, M. A., H. Fox, K. O’Connor, T. Chapman, and J. MacKinnon. 2008. Pediatric perspectives and practices on transitioning adolescents with special needs to adult health care. Washington, DC: National Alliance to Advance Adolescent Health.
McPheeters M., A. M Davis, J. L. Taylor, R. F. Brown, S. A. Potter, and R. A. Epstein. 2014. Transition care for children with special health needs. Technical brief no. 15. Rockville, MD: AHRQ.
MD Anderson Cancer Center. 2014. Adolescent and Young Adult (AYA) Program. http://www.mdanderson.org/patient-and-cancer-information/care-centers-and-clinics/childrenscancer-hospital/support-programs/aya-program.html (accessed April 24, 2014).
mHealth Alliance. 2014. mHealth Alliance. http://mhealthalliance.org (accessed July 26, 2014).
mHealth Summit. 2014. mHealth Alliance summit. http://www.mhealthsummit.org (accessed July 26, 2014).
Minnes, S., A. Lang, and L. Singer. 2011. Prenatal tobacco, marijuana, stimulant, and opiate exposure: Outcomes and practice implications. Addiction Science & Clinical Practice 6(1):57-70.
NACo (National Association of Counties). 2012. County jails and the Affordable Care Act: Enrolling eligible individuals in health coverage. Washington, DC: NACo.
NAHIC (National Adolescent and Young Adult Health Information Center). 2014. Summary of recommended guidelines for clinical preventive services for young adults ages 18-26. San Francisco, CA: UCSF Division of Adolescent and Young Adult Medicine.
Narayanan, S., and P. J. Shami. 2012. Treatment of acute lymphoblastic leukemia in adults. Critical Reviews in Oncology/Hematology 81(1):94-102.
Nardi, B., S. Laurenzi, M. Di Nicolo, and C. Bellantuono. 2012. Is the cognitive-behavioral therapy an effective intervention to prevent the postnatal depression? A critical review. International Journal of Psychiatry in Medicine 43(3):211-225.
NASW (National Association of Social Workers). 1993. NASW standards for the practice of social work with adolescents. https://www.socialworkers.org/practice/standards/sw_adolescents.asp (accessed July 24, 2014).
The National Alliance to Advance Adolescent Health. 2014a. About Got Transition. http://www.gottransition.org/about/index.cfm (accessed August 4, 2014).
The National Alliance to Advance Adolescent Health. 2014b. Six core elements of health care transition 2.0. http://www.gottransition.org/resourceGet.cfm?id=206 (accessed September 24, 2014).
National Conference of State Legislatures. 2014. Medicaid for juvenile justice-involved children: Juvenile justice guidebook for legislators. Denver, CO: National Conference of State Legislatures.
NCCAP (National Certification Council for Activity Professionals). 2011. National certification examination for addiction counselors, level 1 and level 2: Candidate handbook. http://www.ptcny.com/pdf/NCC.pdf (accessed July 25, 2014).
NCI (National Cancer Institute). 2014. Adolescents and young adults with cancer. http://www.cancer.gov/cancertopics/aya (accessed July 28, 2014).
NCQA (National Committee for Quality Assurance). 2014. Standards and guidelines for NCQA’s Patient-Centered Medical Home (PCMH) 2014. Washington, DC: NCQA.
Neinstein, L. S. 2014. Adolescent health curriculum: Outline of curriculum. http://www.usc.edu/student-affairs/Health_Center/adolhealth (accessed March 28, 2014).
NRC (National Research Council) and IOM. 2009. Adolescent health services: Missing opportunities. Washington, DC: The National Academies Press.
NTOCC (National Transitions of Care Coalition). 2008. Transitions of care measures. Washington, DC: NTOCC.
Okumura, M. J., M. Heisler, M. M. Davis, M. D. Cabana, S. Demonner, and E. A. Kerr. 2008. Comfort of general internists and general pediatricians in providing care for young adults with chronic illnesses of childhood. Journal of General Internal Medicine 23(10):1621-1627.
Okumura, M. J., E. A. Kerr, M. D. Cabana, M. M. Davis, S. Demonner, and M. Heisler. 2010. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics 125(4):e748-e754.
Olson, A. L., C. A. Gaffney, V. A. Hedberg, and G. R. Gladstone. 2009. Use of inexpensive technology to enhance adolescent health screening and counseling. Archives of Pediatrics & Adolescent Medicine 163(2):172-177.
Ostrom, C. M. 2014. State using fake rappers, real patients in new health-insurance ad campaign. The Seattle Times, February 19.
Ozer, E. M. 2007. The adolescent primary care visit: Time to build on strengths. Journal of Adolescent Health 41(6):519-520.
Ozer, E. M., S. H. Adams, J. L. Lustig, S. Gee, A. K. Garber, L. R. Gardner, M. Rehbein, L. Addison, and C. E. Irwin. 2005. Increasing the screening and counseling of adolescents for risky health behaviors: A primary care intervention. Pediatrics 115(4):960-968.
Ozer, E. M., J. T. Urquhart, C. D. Brindis, M. J. Park, and C. E. Irwin. 2012. Young adult preventive health care guidelines: There but can’t be found. Archives of Pediatrics & Adolescent Medicine 166(3):240-247.
Ozer, E. M., J. T. Scott, and C. D. Brindis. 2013. Seizing the opportunity: Improving young adult preventive health care. Adolescent Medicine: State of the Art Reviews 24:507-525.
Partnership for Male Youth. 2014. Health provider toolkit for adolescent and young adult males. http://www.ayamalehealth.org/index.php#sthash.qD9oPHAu.OO4iihBd.dpbs (accessed March 28, 2014).
Passel, J. S., and D. Cohn. 2009. A portrait of unauthorized immigrants in the United States. Washington, DC: Pew Hispanic Center.
Passel, J. S., and M. H. Lopez. 2012. Up to 1.7 million unauthorized immigrant youth may benefit from new deportation rules. Washington, DC: Pew Hispanic Center.
Passel, J. S., D. Cohn, and A. Gonazalez-Barrera. 2013. Population decline of unauthorized immigrants stalls, may have reversed. Washington, DC: Pew Hispanic Center.
Pauly, M. V., and J. A. Pagán. 2007. Spillovers and vulnerability: The case of community uninsurance. Health Affairs 26(5):1304-1314.
Peppercorn, J. M., J. C. Weeks, E. F. Cook, and S. Joffe. 2004. Comparison of outcomes in cancer patients treated within and outside clinical trials: Conceptual framework and structured review. Lancet 363(9405):263-270.
Perrin, E. C., and R. C. Sheldrick. 2012. The challenge of mental health care in pediatrics. Archives of Pediatrics & Adolescent Medicine 166(3):287-288.
Peter, N. G., C. M. Forke, K. R. Ginsburg, and D. F. Schwarz. 2009. Transition from pediatric to adult care: Internists’ perspectives. Pediatrics 123(2):417-423.
Porteous, N., and G. Waghorn. 2007. Implementing evidence-based employment services in New Zealand for young adults with psychosis: Progress during the first five years. The British Journal of Occupational Therapy 70(12):521-526.
Pottick, K. J., S. Bilder, A. Vander Stoep, L. A. Warner, and M. F. Alvarez. 2008. U.S. patterns of mental health service utilization for transition-age youth and young adults. The Journal of Behavioral Health Services & Research 35(4):373-389.
Pottick, K. J., L. A. Warner, A. Vander Stoep, and N. M. Knight. 2014. Clinical characteristics and outpatient mental health service use of transition-age youth in the USA. The Journal of Behavioral Health Services & Research 41(2):230-243.
Pullmann, M. D., C. A. Heflinger, and L. S. Mayberry. 2010. Patterns of Medicaid disenrollment for youth with mental health problems. Medical Care Research and Review 67(6):657-675.
Querstret, D., and M. Cropley. 2013. Assessing treatments used to reduce rumination and/or worry: A systematic review. Clinical Psychology Review 33(8):996-1009.
Quinn, C. T., Z. R. Rogers, T. L. McCavit, and G. R. Buchanan. 2010. Improved survival of children and adolescents with sickle cell disease. Blood 115(17):3447-3452.
Ramanujachar, R., S. Richards, I. Hann, and D. Webb. 2006. Adolescents with acute lymphoblastic leukaemia: Emerging from the shadow of paediatric and adult treatment protocols. Pediatric Blood & Cancer 47(6):748-756.
Regier, D. A., W. E. Narrow, D. S. Rae, R. W. Manderscheid, B. Z. Locke, and F. K. Goodwin. 1993. The de facto U.S. mental and addictive disorders service system: Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry 50(2):85-94.
Reid, G. J., M. J. Irvine, B. W. McCrindle, R. Sananes, P. G. Ritvo, S. C. Siu, and G. D. Webb. 2004. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 113(3):e197-e205.
Reiner, K., L. Tibi, and J. D. Lipsitz. 2013. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Medicine 14(2):230-242.
Reiss, J. G., R. W. Gibson, and L. R. Walker. 2005. Health care transition: Youth, family, and provider perspectives. Pediatrics 115(1):112-120.
Rice, C., R. Longabaugh, M. Beattie, and N. Noel. 1993. Age group differences in response to treatment for problematic alcohol use. Addiction 88(10):1369-1375.
Rihmer, Z., and X. Gonda. 2013. Pharmacological prevention of suicide in patients with major mood disorders. Neuroscience and Biobehavioral Reviews 37(10):2398-2403.
Ringeisen, H., C. Casanueva, M. Urato, and L. Stambaugh. 2009. Mental health service use during the transition to adulthood for adolescents reported to the child welfare system. Psychiatric Services 60(8):1084-1091.
Robison, L. L. 2011. Late effects of acute lymphoblastic leukemia therapy in patients diagnosed at 0-20 years of age. ASH Education Program Book 2011(1):238-242.
Rosenbach, M., K. Lewis, and B. Quinn. 2001. Children in foster care: Challenges in meeting their health care needs through Medicaid. Princeton, NJ: Mathematica.
SAHM (Society for Adolescent Health and Medicine). 2014. Mission. http://www.adolescenthealth.org/About-SAHM/Mission.aspx (accessed March 28, 2014).
SAMHSA (Substance Abuse and Mental Health Services Administration). 2011. Leading change: A plan for SAMHSA’s roles and actions 2011-2014. Rockville, MD: HHS.
SAMHSA. 2013a. Results from the 2012 National Survey on Drug Use and Health: Mental health findings and detailed tables. http://www.samhsa.gov/data/NSDUH/2k12MH_FindingsandDetTables/MHDT/NSDUH-MHDetTabsTOC2012.htm (accessed September 26, 2014).
SAMHSA. 2013b. Results from the 2012 National Survey on Drug Use and Health: Detailed tables. http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/DetTabs/NSDUH-DetTabsTOC2012.htm (accessed September 26, 2014).
Sanci, L., B. Grabsch, P. Chondros, A. Shiell, J. Pirkis, S. Sawyer, K. Hegarty, E. Patterson, H. Cahill, and E. Ozer. 2012. The prevention access and risk taking in young people (PARTY) project protocol: A cluster randomised controlled trial of health risk screening and motivational interviewing for young people presenting to general practice. BMC Public Health 12(1):400.
Schoenbaum, M., J. Unützer, C. Sherbourne, N. Duan, L. V. Rubenstein, J. Miranda, L. S. Meredith, M. F. Carney, and K. Wells. 2001. Cost-effectiveness of practice-initiated quality improvement for depression: Results of a randomized controlled trial. Journal of the American Medical Association 286(11):1325-1330.
Schoenbaum, M., J. Unützer, D. McCaffrey, N. Duan, C. Sherbourne, and K. B. Wells. 2002. The effects of primary care depression treatment on patients’ clinical status and employment. Health Services Research 37(5):1145-1158.
Schoenbaum, M., J. Miranda, C. Sherbourne, N. Duan, and K. Wells. 2004. Cost-effectiveness of interventions for depressed Latinos. Journal of Mental Health Policy and Economics 69-76.
Seattle Children’s Hospital. 2014. Adolescent and Young Adult (AYA) Cancer Program. http://www.seattlechildrens.org/clinics-programs/cancer/services/adolescent-young-adult-program (accessed July 24, 2014).
Shah, L. B., P. Klainin-Yobas, S. Torres, and P. Kannusamy. 2014. Efficacy of psychoeducation and relaxation interventions on stress-related variables in people with mental disorders: A literature review. Archives of Psychiatric Nursing 28(2):94-101.
Shufelt, J. L., and J. J. Cocozza. 2006. Youth with mental health disorders in the juvenile justice system: Results from a multi-state prevalence study. Delmar, NY: National Center for Mental Health and Juvenile Justice.
Siegenthaler, E., T. Munder, and M. Egger. 2012. Effect of preventive interventions in mentally ill parents on the mental health of the offspring: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry 51(1):8-17, e18.
Simon, G. E., W. J. Katon, M. VonKorff, J. Unützer, E. H. Lin, E. A. Walker, T. Bush, C. Rutter, and E. Ludman. 2001. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. American Journal of Psychiatry 158(10):1638-1644.
Simon, G. E., M. Von Korff, E. J. Ludman, W. J. Katon, C. Rutter, J. Unützer, E. H. Lin, T. Bush, and E. Walker. 2002. Cost-effectiveness of a program to prevent depression relapse in primary care. Medical Care 40(10):941-950.
Simon, T. D., S. Lamb, N. A. Murphy, B. Hom, M. L. Walker, and E. B. Clark. 2009. Who will care for me next? Transitioning to adulthood with hydrocephalus. Pediatrics 124(5):1431-1437.
Sinha, R., C. Easton, and K. Kemp. 2003. Substance abuse treatment characteristics of probation-referred young adults in a community-based outpatient program. The American Journal of Drug and Alcohol Abuse 29(3):585-597.
Slade, E., L. Wissow, M. Davis, M. Abrams, and L. Dixon. 2014. Medicaid lapses and low-income young adults’ receipt of outpatient mental health care after an inpatient stay. Psychiatric Services 65(4):454-460.
Slive, L., and R. Cramer. 2012. Health reform and the preservation of confidential health care for young adults. The Journal of Law, Medicine & Ethics 40(2):383-390.
SSA (Social Security Administration). 2014. Understanding Supplemental Security Income SSI and other government programs—2014 edition. http://www.ssa.gov/ssi/text-other-ussi.htm (accessed September 12, 2014).
Stafford, M. R., H. Jackson, E. Mayo-Wilson, A. P. Morrison, and T. Kendall. 2013. Early interventions to prevent psychosis: Systematic review and meta-analysis. British Medical Journal 346.
Stevens, J., K. J. Kelleher, W. Gardner, D. Chisolm, J. McGeehan, K. Pajer, and L. Buchanan. 2008. Trial of computerized screening for adolescent behavioral concerns. Pediatrics 121(6):1099-1105.
Stice, E., H. Shaw, C. Bohon, C. N. Marti, and P. Rohde. 2009. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology 77(3):486.
Stroul, B. A. 2002. Issue brief—system of care: A framework for system reform in children’s mental health. Washington, DC: Georgetown University Child Development Center, National Technical Assistance Center for Children’s Mental Health.
Stroul, B. A., and R. M. Friedman. 1986. A system of care for children and youth with severe emotional disturbances. Washington, DC: CASSP Technical Assistance Center, Center for Child Health and Mental Health Policy, Georgetown University Child Development Center.
Tanis, C. 2012. Performance enhancement and stress reduction using biofeedback with women collegiate volleyball players. Athletic Insight: The Online Journal of Sport Psychology 4(2):127-140.
Tebb, K. P., E. Sedlander, G. Pica, A. Diaz, K. Peake, and C. D. Brindis. 2014. Protecting adolescent confidentiality under health care reform: The special case regarding explanations of benefits (EOBs). San Francisco: Philip R. Lee Institute of Health Policy and Division of Adolescent and Young Adult Medicine, Department of Pediatrics, University of California, San Francisco.
Tighe, E., and L. Saxe. 2006. Community-based substance abuse reduction and the gap between treatment need and treatment utilization: Analysis of data from the “fighting back” general population survey. Journal of Drug Issues 36(2):295-312.
Todd, S. R., and B. D. Sommers. 2012. Overview of the uninsured in the United States: A summary of the 2012 Current Population Survey report. Washington, DC: HHS Office of the Assistant Secretary for Planning and Evaluation.
Tuchman, L. K., and M. Schwartz. 2013. Health outcomes associated with transition from pediatric to adult cystic fibrosis care. Pediatrics 132(5):847-853.
Tuchman, L. K., L. A. Schwartz, G. S. Sawicki, and M. T. Britto. 2010. Cystic fibrosis and transition to adult medical care. Pediatrics 125(3):566-573.
Turrisi, R., J. Jaccard, R. Taki, H. Dunnam, and J. Grimes. 2001. Examination of the short-term efficacy of a parent intervention to reduce college student drinking tendencies. Psychology of Addictive Behaviors 15(4):366-372.
Tylee, A., D. M. Haller, T. Graham, R. Churchill, and L. A. Sanci. 2007. Youth-friendly primary-care services: How are we doing and what more needs to be done? Lancet 369(9572):1565-1573.
USPSTF (U.S. Preventive Services Task Force). 2011. Focus on children and adolescents. http://www.uspreventiveservicestaskforce.org/tfchfocus.htm (accessed July 26, 2014).
USPSTF. 2012. Grade definitions. http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm (accessed September 26, 2014).
USPSTF. 2013. Focus on older adults. http://www.uspreventiveservicestaskforce.org/tfolderfocus.htm (accessed July 26, 2014).
van Hasselt, F., P. Krabbe, D. Ittersum, M. Postma, and A. Loonen. 2013. Evaluating interventions to improve somatic health in severe mental illness: A systematic review. Acta Psychiatrica Scandinavica 128(4):251-260.
Van Voorhees, B. W., N. Mahoney, R. Mazo, A. Z. Barrera, C. P. Siemer, T. R. Gladstone, and R. F. Muñoz. 2011. Internet-based depression prevention over the life course: A call for behavioral vaccines. Psychiatric Clinics of North America 34(1):167-183.
VanDenBerg, J. E., and E. M. Grealish. 1996. Individualized services and supports through the wraparound process: Philosophy and procedures. Journal of Child and Family Studies 5(1):7-21.
Vujicic, M., C. Yarbrough, and K. Nasseh. 2014. The effect of the Affordable Care Act’s expanded coverage policy on access to dental care. Medical Care 52(8):715-719.
Wallace, S., J. Torres, T. Nobari, and N. Pourat. 2013. Undocumented and uninsured: Barriers to affordable care for immigrant populations. Washington, DC, and New York: The Commonwealth Fund and the UCLA Center for Health Policy Research.
Warner, C. H., G. N. Appenzeller, J. R. Parker, C. M. Warner, and C. W. Hoge. 2011. Effectiveness of mental health screening and coordination of in-theater care prior to deployment to Iraq: A cohort study. American Journal of Psychiatry 168(4):378-385.
Weissman, M. M., P. Wickramaratne, Y. Nomura, V. Warner, D. Pilowsky, and H. Verdeli. 2006. Offspring of depressive parents: 20 years later. American Journal of Psychiatry 163(6):1001-1008.
WHO (World Health Organization). 2001. Global consultation on adolescent friendly health services: A consensus statement. Geneva, Switzerland: WHO.
WHO. 2009. Quality assessment guidebook: A guide to assessing health services for adolescent clients. Geneva, Switzerland: WHO.
Young Invincibles. 2014. Health care. http://younginvincibles.org/issues/health-care (accessed July 22, 2014).
Zebrack, B. 2008. Information and service needs for young adult cancer patients. Support Care Cancer 16(12):1353-1360.
Zemel, S., and N. Kaye. 2009. Medicaid eligibility, enrollment, and retention policies: Findings from a survey of juvenile justice and Medicaid policies affecting children in the juvenile justice system. Portland, ME: National Academy for State Health Policy.








































































