Health Research Needs and Actions: Lessons from Recent Disasters
A succession of public health emergencies and disasters in the past decade has challenged capacities both in the United States and abroad (Lurie et al., 2013). Each one is unique, but there are generalizable elements and common barriers and facilitators to response that can be learned from them. Bob Ursano, chair of the Department of Psychiatry and Director of the Center for the Study of Traumatic Stress at the Uniformed Services University of the Health Sciences, reiterated Lurie’s comments regarding the need to produce actionable science—not just research, but science preparedness and response. What are the research questions of most importance, what are the targets for answering those questions, what are the tools for accomplishing the research, and what are the resources that can be brought to bear and impediments to be overcome? This chapter considers the lessons learned from recent disasters regarding health research needs and actions, including examples of strong cohort participation and elements to support rapid funding. Cases explored include the 9/11 terrorist attacks, Hurricane Katrina in 2005, the Deepwater Horizon oil spill in 2010, and Hurricane Sandy in 2012.
Because disasters are unexpected, disaster research is inherently different from nondisaster research. In nondisaster research, scientists plan, collect data, analyze that data, and develop an intervention. In a disaster, intervention (i.e., the response to the disaster) must be immediate. Data collection occurs under difficult circumstances and is
confounded by the ongoing interventions and other stressors. Analysis of data is also impacted. David Prezant, chief medical officer for the Fire Department of New York City (FDNY), shared his perspectives on research challenges and lessons learned based on his experiences during the World Trade Center (WTC) rescue and recovery efforts following the terrorist attacks of September 11, 2001.
Why Research During a Response
Because funding and staffing situations can be fragile, questions on the need for research or activities not directly related to an emergency response are perpetually raised. Prezant elucidated an important example showing the need for timely research specifically related to the disaster at hand. As a result of the 2001 attacks in New York, two 110-story towers and several surrounding buildings were reduced to about four stories of pulverized rubble. What was not in the rubble pile was suspended in the air in an enormous dust cloud. Shortly after the collapse of the towers, news outlets were interviewing experts on television, some of whom said there would be no respiratory effects of exposure to the debris dust cloud. They based these statements, Prezant explained, on research that has demonstrated that particles must be less than 3 microns in size to enter the lower airways. At the very most, they predicted mild upper airway consequences (chronic sinusitis, rhinitis). These experts were wrong, Prezant said, because they were thinking about low-density, low-concentration inhalation experiments as would occur with tuberculosis or other infection agents or with metered-dose inhalers. This exposure lasted for several days, and about 16,000 FDNY rescue workers continued to be exposed to different levels of dust in encapsulated subterranean areas over the next 10 months during the intense rescue and recovery effort.
Prezant said firefighters came out of the rubble and told him that the air had a different smell and taste than anything they had experienced before in fighting fires. The firefighters at the WTC site were exposed to high concentrations of very alkaline dust (approximate pH of 10) containing a mixture of pulverized cement, gypsum, pulverized glass, asbestos, silica, fibrous glass, heavy metals, volatile organic compounds, and the organic combustion/pyrolysis products of all the building components and jet fuel (e.g., polycyclic aromatic hydrocarbons, dioxins, polychlorinated biphenyls). About 3 weeks into the recovery effort, a therapeutic, diagnostic bronchoscopic evaluation of a firefighter who was
sent to a nearby hospital in respiratory distress and arrest revealed uncoated asbestos fibers, glass, and pulverized ash. In other cases, macrophages in sputum samples collected 10 months after 9/11 contained encapsulated dust similar to that at the WTC site (Fireman et al., 2004). Air and respiratory monitoring while the response and clean-up was going on might have allowed responders and clinicians to more quickly see the potential hazards involved and change actions accordingly.
The Importance of Early Baseline Data
In many disasters, baseline data may not exist or are hard to access for the same cohort looking to be studied. This lack of access can make it even more difficult to pinpoint causes or link health outcomes to disaster exposures. Prezant also stressed the importance of acting immediately to get monitoring and treatment systems in place, so that data are not lost and so that credibility as a partner is established. An FDNY WTC responder cohort was established after 9/11, and a well-organized medical monitoring program has minimized longitudinal dropout with consistently high retention rates (92–95 percent). Because FDNY has been capturing health data, including pulmonary function tests, systematically since 1996, this is the only cohort with pre-9/11 health data, Prezant noted. This cohort also has the highest exposure to respiratory irritants and combustion by-products of any WTC cohort. Monitoring and treatment protocols are in place for respiratory and mental health issues as well as for late emerging diseases (e.g., cancer). This can also foster trust with participants by allowing them to be cared for quickly, which will continue to encourage study involvement and high retention (see Figure 3-1).
Coordinating Logistics to Execute Rapid and Sustained Research in Disaster Response
Research is a slow, deliberative, thoughtful, and collaborative process. Disaster research, however, has to absorb the immediacy of the event, Prezant said. Without that information, any of the outcomes of interest will remain elusive, regardless of the techniques used. The immediate data are essential to determine what did or did not happen; who was exposed, to what, and to what extent; and what the immediate
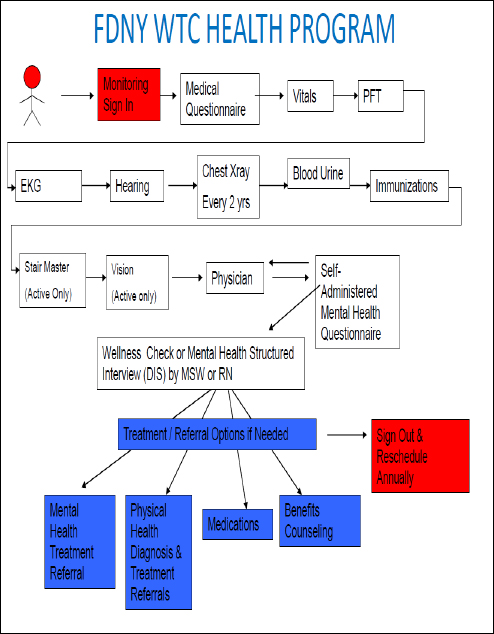
FIGURE 3-1 The World Trade Center Health Program for the Fire Department of New York.
NOTE: DIS = Diagnostic Interview Schedule; EKG = electrocardiogram; MSW = master of social work; PFT = Physical Fitness Test; RN = registered nurse.
SOURCE: Prezant presentation, June 12, 2014.
impact appears to be. The research questions are similar at every disaster, and preparedness requires prearranged studies that are ready to go, he added.
Partnering with Communities to Facilitate Pre-Event Assessment
Partnering with communities, Prezant said, including state and local government, is essential to facilitate access to pre-event data, collection of baseline data, and longitudinal assessment of the population (discussed further in Chapter 5). Participants need a reason to participate in research, Prezant continued; too often, participants view research as an experiment. They have already lived through one experiment (the disaster), and they are not inspired to volunteer for another. In addition, they are dealing with the aftermath of the disaster (e.g., the death of a loved one, loss of their home), and their energy and patience are limited. Therefore, participants need a reason to believe the research effort is worth their remaining energies and time. This involves developing trust, which requires credibility. IRB approval is not enough to garner trust and demonstrate credibility to people, Prezant said. They do not know what an IRB is. What is needed are partnerships and a history of service that preferably began before the disaster (as is seen with the FDNY responder cohort). There also needs to be a “stamp of excellence” from a major organization that the community trusts (e.g., the American Cancer Society, the American Heart Association, CDC) to help secure local buy-in and public labor and management support.
Participation is maximized if everyone agrees that disaster research is not an experiment. It’s a promise, with an end toward recovery.
—David Prezant
If we cannot monitor, assess, provide services, intervene, and reassess, we cannot provide what people need in a disaster, Prezant said. If we do not know what is going on in the communities, we cannot respond, or we respond with the wrong interventions, only making matters worse, he continued. The end point then is not the data, but the knowledge that can be used to guide recovery, including clinical services and systems improvements. Continued participation requires fulfillment of this promise, in the form of delivery on end points in the short term as well as in the longer term.
As an example of delivering on the promise of research, Prezant cited several published papers on declining pulmonary function in WTC
responders in the short term and persistence of reduced function in the long term (Aldrich et al., 2010; Banauch et al., 2006; Prezant et al., 2002). FDNY was also the first to publish an early assessment of cancer outcomes, showing a cancer signal only 7 years after 9/11. This affected federal health care policy, Prezant said, because cancer was then added to WTC covered conditions (Zeig-Owens et al., 2011).
FDNY is also involved in basic research. For example, blood banked during the first 6 months after 9/11 has been used for studies linking pulmonary function test outcomes to biomarkers that could potentially predict both susceptibility and resistance to disease (Cho et al., 2013; Nolan et al., 2012). Firefighters are saying yes to participating in basic science research, as long as they have a sense that it is going to help them or another firefighter who is exposed.
Obtaining Rapid and Sustained Research Funding
Research funding after a disaster has several phases, and they are generally based on public perception, Prezant said. Initially, small amounts of funding flow from governments and philanthropies because it is “the right thing to do.” This is often followed by disbelief about whether people were actually exposed to something dangerous, whether it was just an acute issue that will resolve spontaneously, or whether the exposure actually caused disease. The next phase is apathy, when funders question whether this research is still important and how much is enough, especially in the face of other national priorities.
The way to overcome these barriers to funding is data-driven advocacy, which requires research, Prezant said. Emotional advocacy secures the initial funding to look at uncertain exposures or health effects, but without data to show importance, there is a loss of credibility. No study is ever perfect, and this is especially true for disaster research where there are numerous, simultaneous, and often unknown confounders. However, multiple studies showing similar effects lead to a more perfect understanding and a more perfect response (i.e., improved services and systems). Research requires educating everyone involved (researchers, participants, funding agencies) as to what is achievable given the situation and adjustment of expectations across all of the funding agencies.
Improving Research Systems and Data Collection
Although everyone thinks their idea is worthy of immediate study, and there are novel issues that can occur, we need to remain focused on the main questions, Prezant said. Affected systems and populations have limited time for testing and questionnaires, and overburdening people can lead to longitudinal dropout. In addition, trying to capture too much data can reduce focus and lead to paralysis. The questions, data collection, and analyses need to be part of a predisaster, agreed-upon, focused agenda, he said.
Data collection should allow for immediate collection and real-time access, Prezant said. For example, a computerized, online questionnaire was developed predisaster as part of the regular annual monitoring exams for firefighters, and within 4 weeks after 9/11, FDNY was able to change the entire monitoring exam to focus on WTC. Questions were designed so that the introductory phrase could be changed with a single-stroke command. In 2000, the phrase was “during your career of firefighting have you ever.…” or “in the last 12 months have you ever.…” Between 9/11/01 and 10/01/01, the phrases were changed to “after the World Trade Center.…” When FDNY was deployed to assist with the Hurricane Katrina response, the phrase was changed to “after Hurricane Katrina.…”
The use of validated questionnaires is essential, but they are not as validated as we think, suggested Prezant. Many of them have not been studied in different populations, and almost none have been studied in a disaster population. Questionnaires may have been validated for one disease, but disasters cause multiple diseases. Using multiple, different validated disease-set questionnaires can lead to additional concerns. Concerns may be attention deficit after answering too many questions, confusion with different time spans for answers to questions (e.g., “in the last 4 weeks have you.…” or “in the last 3 months….”), or similar questions in each disease set that reduce specificity of the answers.
Prezant described the World Trade Center Health Program and how it monitors and assesses firefighters. The same day that data are collected and assessed, firefighters are informed of recommended treatment or referral options. Prezant noted that FDNY cannot force firefighters to do the follow-up, but they make it free (through their health benefits program) and as easy as possible to get mental health treatment, physical health treatment, medications, benefits counseling, and so on.
IRB Processes
FDNY leverages preexisting IRB relationships for rapid review in a disaster. In addition, as long as the questionnaires, tests, and interventions (if any) are standards of care that the local health care entity was going to do anyway, then the IRB is often willing to review only the analytic portion. Prezant expressed support for a national IRB. A concern highlighted by Prezant is that many IRBs still do not understand, or have little experience with, the Federal Confidentiality Certificate. Also, consent forms typically state that the researchers and their institutions are not responsible for any complications the subject may directly or indirectly suffer from the testing protocol. Unless this line is removed, he said, most workers will not sign this consent because they correctly or incorrectly presume they are giving up their rights to workers’ compensation and any litigation for damages.
Focusing on the Human Need to Help
Prezant stressed that the goal of research in response to a disaster is not just to record events, determine mechanisms and outcomes, and design interventions, although all of these are essential to response. The most important goal after a disaster, and the one required for all of the above to be possible, is to stimulate human decency, he said, by focusing on our natural impulse to reach out and help people and building a lasting relationship where at first there was only the desire and the urgency to help, and not the established scientific need to help.
Although Hurricane Katrina occurred nearly a decade ago in August 2005, it was such an enormous storm, affecting such a large geographic area and impacting so many lives, that remnants of the phenomenal amount of damage are still apparent today. Katrina had a huge effect on many different systems, including critical infrastructure, health, education, and community systems, said David Abramson, deputy director of the National Center for Disaster Preparedness at Columbia University. Abramson shared his perspectives on engaging in rapid research based on his experiences during and after Hurricane Katrina.
Gulf Coast Child and Family Health Study
Abramson elaborated on one of the larger community-based studies in which he participated, the Gulf Coast Child and Family Health Study, begun in 2006 and funded through the Children’s Health Fund and the Merck Foundation. The study focused on identifying health and social service needs among this displaced and heavily impacted population. Data were collected from 1,079 randomly sampled households over the span of 29 days for the start of a 5-year longitudinal study. The sample was intended to represent 60,000 to 100,000 displaced and/or heavily affected Katrina survivors.
The immediate challenges in operationalizing this study were enormous, Abramson said. Even though he and his colleagues started working on a protocol just a few weeks after the storm, the first barrier was access to sample frame data (or the set of information used to identify the population for research). Namely they were looking for information on where the displaced populations were, especially congregate settings to help frame their research protocol. FEMA was managing the congregate settings population and had meticulous data, he said, but they did not release any of it for his research. A second challenge, Abramson added, was that the sampling frame was a moving target after they got the initial access. For example, by the time the protocol was approved, FEMA had triggered its deadline for evacuees to leave the hotels, so identifying and locating participants had to be done all over again. Another challenge they anticipated was whether or not researchers would be able to gain access to these public and private sites once they found them. Time was the biggest issue, as it becomes more difficult to find people as time passes and recall bias can increase over time. Abramson said there was no reliable Internet access in many places they went, and to account for that anticipated challenge they developed field management databases for tablets that can batch data and upload later when an Internet connection is available. Researchers were also sure to have pens and hard copies of the survey they were administering.
To quicken the time line and mobilize the research infrastructure more rapidly, Abramson used the infrastructure and expertise he already had in place for an HIV longitudinal cohort study happening in the New York City metropolitan area. This existing infrastructure offered Abramson and his team rapid access to data systems, qualified interviewers, research staff, staff knowledge of working with vulnerable and elusive populations, and a common methodology for building and
maintaining a longitudinal cohort using multistage, stratified sampling strategies. Building these elements from scratch would have delayed the time line and kept them from getting into the field as quickly as possible to capture the ephemeral data. In addition, Abramson was connected with more than 25 graduate students who were interested in coming to the Gulf Coast to conduct the research. Although this worked as a great model in this case, it may be difficult to fund this type of “attaching” to an existing research infrastructure as a sustainable future model for disaster research. Standardizing that process across institutions nationwide that are interested in disaster research may be a challenge as well, but in cases where relationships are already built, it may also be very efficient.
By the time they were ready for the IRB submission, it was approximately 4 months after the storm hit. The IRB understood the need for speed in this case and provided a rapid expedited review. The process involved a back-and-forth dialogue and helped to establish a relationship that is now in place to facilitate rapid IRB approval in future disasters. Upon initial submission, the head of Columbia University Medical Center’s IRB informed Abramson that his protocol for the Gulf Coast Child and Family Health Study would need to consider additional elements: addressing the vulnerability of the subjects; systematic referral of subjects to care; ability to identify crises as they occur; endorsement from the community or government; the safety, training, and preparation of the field team; and compliance with local “Duty to Report” laws regarding abuse and neglect (which may differ by state). Agreeing that these items were important and needed to be examined, they were added to the protocol. The IRB director and chairs ultimately granted approval days before Abramson was to enter the field, and they now have an understanding of the time line importance for certain disaster-related projects. If an IRB is not as understanding and flexible as the one in this case, this could be another potentially vulnerable area for a researcher’s time line, especially in the case of multiple institutions working together and needing approval by separate IRBs. Education and sharing of disaster-related research projects at IRB forums and net-working events could be a way to shift perception of the IRBs from a barrier to a partner.
Engaging and Leveraging Existing Partners
Throughout the discussions, various participants noted the importance of building and sustaining relationships with organizations on the
ground and local to the affected community. The Gulf Coast Child and Family Health Study was fortunate to leverage partners of their home institution for resources, but also those local partners who were familiar with the community. Local partnerships can aid in efficiency as well as facilitate the “returning of data” back to the community to help them in making informed changes and future decisions. Abramson noted that a critical partner in achieving their rapid mobilization was the Children’s Health Fund, which already had clinical teams deployed in the field, having sent some of their mobile medical units to the Gulf for what they dubbed “Operation Assist,” and had existing connections with state and local officials. The Children’s Health Fund also had a stable funding mechanism, having raised $10 million to $15 million under the banner of Operation Assist, and was willing to share one of their mobile units as a public health field office. Trying to raise funds to support a mobile office and spend the time to make connections with government officials would have again delayed the research back even further. Abramson explained that the 35-foot-long mobile unit, branded with the Columbia University and Children’s Health Fund names and logos and set up inside with the necessary office equipment, was a centerpiece of the operation because of the branding of the mobile unit and the researchers (through the ID badges and distinctive tote bags and hats). This was a key element of success as the community became familiar with the project, and it offered an element of legitimacy.
Highlighting the need to connect with local institutions, Abramson said that the Louisiana Department of Health and Hospital was also a critical partner, endorsing the study, offering resources and assistance, and importantly, providing official Louisiana Department of Health and Hospital badges for researchers that helped to enable access to the trailer parks and other congregate settings. Abramson noted that for the Gulf study, this relationship with the Louisiana Department of Health and Hospital was more casual, and he would share research findings on occasion. Looking back, he realized it should have been more formalized, so for the more recent Hurricane Sandy Child and Family Health Study, he created the Public Partnership Group to make a more formal connection with the state agencies in New Jersey. This group is composed of the health department, children and families, and human services within the state, and has a more formal reporting structure so it will receive the data from the field within weeks to make sure it is actionable for policy and programmatic purposes. With mobile and electronic tools and resources they did not have during the Gulf Coast
Child and Family Health Study, they are actually now able to send data to their partners daily when available, making it possible for policy decisions to be made more quickly with more information. Having research teams connected as part of the formal response and recovery infrastructure could be a key method for connecting researchers and public health practice, sustain newly made relationships among partners, and elevate the significance of disaster research.
The results of the study first appeared on the front page of The New York Times and succeeded in calling attention to some of the unresolved issues in the Gulf following the storm that had not been appearing in national news. This galvanized the researchers, he said, because “we realized the impact we can have if we can get our research out and disseminate it widely.” While Abramson first encountered several difficulties in mobilizing a research team and identifying and sustaining a cohort for their work, this singular example illustrates the reach that disaster research could potentially have on future policy decisions, recovery funding, and informed research in the next disaster.
Shortly after the Deepwater Horizon oil spill in April 2010, NIH Director Francis Collins pledged $10 million in NIH funding to initiate the Gulf Long-term Follow-up (GuLF) Study, in which NIEHS is conducting research on the health impacts of the spill on workers and volunteers cleaning it up, said Birnbaum of NIEHS. Related NIEHS programs include Deepwater Horizon Research Consortia (an extramural consortium focusing on women and children, pregnancy issues, seafood safety, and resiliency of communities); toxicology research on the compounds involved (crude oil, dispersants, polyaromatic breakdown products); and worker training for people involved in the cleanup, provided through the NIEHS Worker Education and Training Program. Birnbaum noted that although many professionals were well trained in cleanup of oil spills, many volunteers were not (e.g., college students, housewives, un-employed). Within 2 weeks of the spill, NIEHS was distributing pocket-sized safety and health awareness booklets to the cleanup workers in English, Spanish, and Vietnamese.
A Transient Study Population
Key among the challenges to conducting oil spill research was working with the atypical study population of workers and volunteers. To identify potential study participants, NIOSH was able to provide a roster of 50,000 people who were involved, and the National Guard and the Coast Guard were able to provide lists of people involved in cleanup in some way. After many negotiations, British Petroleum (BP) also provided a list of more than 130,000 workers. NIH had hoped to recruit 50,000 people to assist in cleanup, but Birnbaum said it has been extremely challenging to recruit the 33,000 enrolled thus far. About 20 percent of the workers came from out of state and then dispersed, making it difficult to find them.
Timing Sensitivity
Although the intramural study development process was fairly rapid (the new study was developed, received the necessary approvals, and researchers were in field within 10 months after the event and 8 months from the time of funding), we need to be able to do research in a disaster situation from the start, Birnbaum said. Echoing Lurie’s concerns, she said waiting 8 months to 1 year later means missing baseline and peak exposure data collection and studying mid-term rather than acute effects. Awarding NIH extramural grants takes even longer: usually 12 to 14 months elapse from the time of request for funding opportunities until the actual grants are received and funded. NIH was able to fund the extramural consortium within 8 months, but in most cases individual IRB and other necessary approvals added significant time, making it 18 to 20 months from the time of the spill for most of the extramural grantees to begin to recruit for their studies. Following a more nimble NSF model Abramson mentioned, where smaller amounts of money can be disbursed more quickly, could help to address this, as well as streamlining the IRB process so researchers do not have to gather approvals with different requirements.
True baseline preexposure data were available for only a small fraction of the cohort (e.g., those from the Coast Guard), and Birnbaum suggested the need for baseline data and biospecimen collection from people who are rostered to work in a disaster cleanup. In addition, while there was a great deal of exposure data collected by BP and multiple federal and state agencies, the databases are not integrated, and Birnbaum
said it has taken significant time and resources to reconstruct exposures at different places and times during the cleanup.
Summarizing the lessons learned from the NIEHS experience with the Deepwater Horizon oil spill, Birnbaum said that in a disaster, in addition to the normal occupational cohort for the site, there may be National Guard and other servicemen and women, firefighters and police officers, volunteers, and other workers involved in the response, as well as local residents whose lives and livelihoods are impacted (e.g., Gulf fishermen). Birnbaum stressed the importance of rapid and ongoing communication with all of the stakeholders, including community groups, academic partners, and industrial partners. She also noted the need to develop better capabilities to rapidly evaluate the toxicity of the exposures.
Howard of NIOSH at CDC added that NIOSH has done extensive intramural research on the Deepwater Horizon disaster from the perspective of worker safety, and referred participants to recent articles for further details (Decker et al., 2013a,b; King and Gibbons, 2011; Kitt et al., 2012; Michaels and Howard, 2012; NIOSH, 2011).
Lewis Goldfrank, professor in the Department of Emergency Medicine at New York University (NYU) School of Medicine, described his research experience in New York City following Hurricane Sandy. Decisions made in each event must balance all of the stakeholders’ concerns (e.g., ethical, legal, practical, organizational, social, clinical), he stated. It is also important to understand whether the actions of the communities are based on societal need or scientific, political, or economic considerations. He added that providers and investigators in a hospital or university are also part of the impacted community, and in participatory action research, the study team members may find that they are both participants and investigators. This can be an asset, as the investigators already know the community they are studying, have existing relationships with other organizations, and can see past surface data, but it could also be a potential challenge if the investigators have been directly impacted by the disaster and may be more emotionally biased.
In the face of a disaster, decisions must be made regarding how best to spend fixed research resources (money, time, effort), both to salvage
existing research affected by the disaster (including cell lines, animals, specialty chemicals, antibodies, equipment, laboratories) and to initiate new research regarding the disaster. That said, if there is no IRB, no human capital, and no electronic infrastructure following the disaster, then even those stakeholders familiar with the research proposal process will find it difficult to initiate or operationalize a new proposal in the traditional sense, Goldfrank noted.
Goldfrank shared several examples of NYU research following Hurricane Sandy to illustrate his points about community. One study of outcomes among buprenorphine-naloxone1 primary care patients after Sandy found only minimal increases in self-reported substance abuse. Goldfrank attributed this, in part, to the fact that the providers/investigators were closely linked with the community and deeply involved in the continuity of care of their patients (Tofighi et al., 2014). He also cited two rapid response studies looking at gasoline and carbon monoxide exposures; he said the studies were possible only because the NYU School of Medicine faculty and fellows are embedded in the public health infrastructure with joint institutional appointments and commitments (Chen et al., 2013; Kim et al., 2013).
Dissemination
NYU researchers are also considering mechanisms for rapid dissemination of experiential learning in a disaster (Laskowski et al., 2013). Goldfrank noted that the traditional peer-review process impeded speedy publication of Sandy research results. He raised several questions for discussion: Should there be “disaster standards” for publication with regard to rigor, methodology, response rate, control groups, etc.? Does the public good of disaster research demand open access, and if so, who funds this? Who is the author, the investigator, or the participants? Do disciplines not traditionally associated with health care delivery achieve larger importance in the face of disaster (e.g., materials science, water and sanitary engineering) and can they be cosupported?
_______________
1Buprenorphine (Subutex) and buprenorphine and naloxone (Suboxone) are used to treat opioid dependence (addiction to opioid drugs, including heroin and narcotic painkillers). Buprenorphine alone and the combination of buprenorphine and naloxone prevent withdrawal symptoms when someone stops taking opioid drugs by producing similar effects to these drugs.
The Impact of Disasters on Hospitals and Health Care
There were many questions about the role of hospitals, emergency departments, and ambulatory care units in meeting the needs of the community during the crisis, and Goldfrank said most decisions on these questions were made in “an evidence-free zone” where guidance from other disasters would have been helpful. While these issues were debated, health care clinical deficits continued or were exacerbated. Goldfrank raised concerns about the ability of a city or state to respond to a disaster without total integration of the health care system. He explained that in evacuating the hospitals, all private staff were sent to other private hospitals, public hospital personnel were sent to other public hospitals, and U.S. Department of Veterans Affairs (VA) staff were sent to other VA facilities. Because there was no universal credentialing, and it can take 2 or 3 days for a provider to be credentialed in another hospital, many would go and wait, unable to deliver care. Goldfrank suggested that staffing with providers from closed hospitals benefits the other hospitals because then they do not have to pay overtime to their staff to have the necessary coverage.
With the above issues in mind, NYU is working on a project funded by an ASPR Recovery Grant to study the impact of a major adverse climate event on health system care and development of disaster response- and resilience-based metrics. The study will examine the comparative effectiveness of adaptive options (e.g., setting up an ambulatory care center or freestanding emergency department) and the decision making necessary for the entire health community to function.
Response Research Networks
Goldfrank supported the calls for the establishment of a broader medical and public health emergency response research network locally and nationally. This network would, for example, initiate continuous meaningful relationships at all levels; facilitate data sharing for immediate and long-term collaboration; define critical research needs, priorities, and obstacles; and consider the roles of embedded researchers in disaster response. A national network could provide priority funding to support laboratory, clinical, public health, and social science studies of public health emergencies that are not adequately addressed; establish the necessary infrastructure to support research; and develop rigorous
evidence-based research protocols and implementation plans for studies in anticipation of disaster.
Disasters consume health services in nontraditional ways. Where people can get care changes when the bridges or tunnels are closed, or when, for example, dialysis centers do not have power or generators. Interhospital collaborations are essential to support resiliency in a community and facilitate better research networks, Goldfrank continued. There have been numerous joint preparedness ventures among New York City public, private, and VA hospitals, and university and hospital affiliations move faculty and residents back and forth among hospitals, strengthening intellectual collaboration. The Poison Control Center and the Office of the Chief Medical Examiner are also key collaborators in research.
SHARED LESSONS ACROSS DISASTERS
Across the case presentations, some speakers highlighted the need to get into the field rapidly and immediately start collecting what Abramson referred to as “ephemeral data.” These baseline data can quickly disappear (e.g., toxin levels dissipate, people cannot be located for specimen collection, personal recall bias increases over time for a variety of intentional and unintentional reasons). In addition, structural and cultural barriers encountered during research attempts following disasters make it difficult to accomplish the goal of a robust science response. However, recent progress made in emergency planning and community resilience building lends possibilities for research to succeed.
Removing Structural Barriers
A few participants discussed further the need to address critical structural barriers and build better systems for everyday use that can be scaled up in a disaster, rather than focusing on building systems just for use in disasters. Goldfrank stressed the importance of being able to deliver everyday health care to everyone and opined that we “will not achieve excellence, as we would consider acceptable, unless we accomplish universal health care.” Prezant added that before the disaster, there need to be opportunities to develop relationships that can be translated into an improved health care infrastructure when needed (discussed further on page 39).
Abramson raised the issue of silos and proprietary data systems as barriers to disaster research. Many entities (e.g., FEMA, U.S. Department of Homeland Security, other emergency management) create their own data systems to facilitate their work and become very protective of their data, systems, and projects, making interoperability before and during an incident a challenge. Some even seem unwilling to acknowledge that data they are collecting could be very helpful to the community at large. Abramson noted that this goes beyond academic researchers seeking access, and he has heard from local and state health officials who could not access government datasets to help facilitate their work. At the local level the silos of information can also trickle down, making it difficult for local health departments, hospitals, and emergency ma-nagement agencies to easily talk and share data across sectors. A part-icipant noted the potential for a symbiotic relationship between local health departments and researchers. The resources and people that local health departments can pool can be beneficial to researchers, and the information that researchers generate can be beneficial to local health departments.
Prezant highlighted the need for funding streams for preparedness research and called for data-driven advocacy to establish and maintain credibility of the field after the initial emotional funding response subsides. Disaster response research cannot compete in the process as it exists now; for example, there is not time to write extensive proposals, the proper control groups are not always possible, and there are numerous simultaneous, and often unknown, confounders. We need to change the expectations of federal funding agencies with regard to disaster response research, he said.
Building Coalitions and Goodwill in Advance
A discussion point throughout the case studies was the benefit that could be realized in getting different groups to work together to prepare and develop “prepositioned goodwill” that can help them to be ready to work together in a disaster. Abramson highlighted the role of health care coalitions in getting hospitals to begin to work together and noted the need to broaden those coalitions so they begin to engage other health care providers within a larger health system and then the community stakeholder groups. Prezant commented that each area has its own challenges for developing networks. In a real disaster, many barriers tend to disappear for the first few days, but then they recur. In some cases
excellence can be a barrier, as expert entities do not want to make compromises. In other cases there may be little or no structure to begin with, making it difficult to develop any sort of network. What is needed is a solid public health infrastructure, because without a foundation for everyday medicine, there is no foundation for disaster medicine, he said.
Engaging the Community
The concept of developing prepositioned goodwill was discussed further with specific focus on engaging the community as both participants and partners in disaster research. It was noted that there are often misunderstandings about how research is used, in part because of the lack of dissemination of the findings to community members whose data were used. This can lead to a lack of trust of research and researchers. Abramson advocated for going back into the community with data in hand to talk about the findings in a direct and real way, so that the community can begin to have ownership over the findings. The community can also add perspective to the findings and will have a far better idea of potential causal mechanisms and relationships, he said. (This concept is further elaborated on in Chapter 5.) He acknowledged that it is very labor intensive, but if researchers plan to go into a community to begin research, they have to be committed to going back in after the study is done to share the data in a reasonable time frame.
Managing, defining, and redefining expectations is important, Prezant said, both our own expectations as well as the community’s. Repairing damage done in the past that has created this distrust may not be possible, but it is possible and essential to avoid causing further damage in the future. Abramson added that emergency preparedness gives public health the opportunity to partner with emergency management and community-based groups to bring marginalized populations to the table to talk about how disasters affect all of us and begin to empower different elements within the community. Later, when public health wants to engage them in other chronic issues—smoking, alcohol, nutrition, obesity—relationships are already built. This can operate in the reverse as well, as communities may identify needs they prioritize that affect them every day, and engaging them in those areas first could prove beneficial to later discussions about disaster research.
The next several chapters highlight the issues and ongoing progress by stakeholders within each of the identified key areas. Some discussions revolved around regulatory and standardization issues, such as facil-
itating a central IRB or creating funding mechanisms to be deployed. Others brought in important cultural conversations about communities—engaging the communities in this type of research and promoting citizen science. Concluding each section is a compilation of top items relative to the challenges and issues, opportunities for improvement, and critical partnerships and collaborations necessary to advance research response capabilities.




















