The History of Heart Valves:
An Industry Perspective
ERIN M. SPINNER
Edwards Lifesciences
The average heart beats 2.5 billion times in a human lifetime, during which its four valves must maintain unidirectional blood flow to maximize the heart’s efficiency and provide oxygenated blood to the entire body. Although heart valves were documented by Leonardo da Vinci in some of his early sketches over 500 years ago, they have been available for implantation only since the 1950s.
Valvular disease—usually associated with advanced age, but also caused by congenital defects—can interrupt, slow, or prevent the efficient function of the valves, which lose functionality if they cannot maintain a proper seal or open completely. When any one of the valves is not working properly it may affect a person’s ability to exercise or perform daily tasks and thus lead to a dramatic decrease in quality of life and even death. For these reasons, decades have been spent developing and perfecting devices to repair and replace the body’s valves when they no longer function properly.
Innovation and development of replacement heart valves have largely focused on the aortic valve, which directs oxygenated blood from the left ventricle to the rest of the body. The structure of the aortic and (similar) pulmonary valves is simpler than that of the other valves—they have greater symmetry and lack the subvalvular components characteristic of the mitral and tricuspid valves—making them an attractive target for early research. The aortic and pulmonary valves consist of three leaflets of similar size and shape that are attached to the tubular vessel; in contrast, the mitral and tricuspid valves have leaflets that vary in number and size. For the mitral and tricuspid valves, these leaflets attach both directly to the wall of the ventricle at the annulus and indirectly through numerous chords (Figure 1).
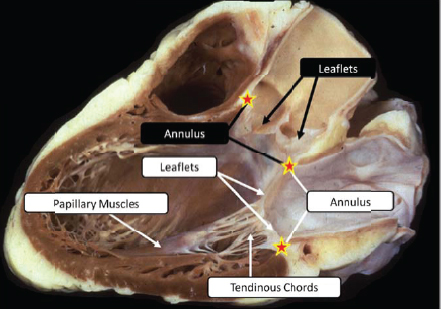
FIGURE 1 Anatomical comparison of the complexity of the aortic valve (black labels) and mitral valve (white labels). Note the subvalvular structure, including numerous chords and papillary muscles, in the mitral valve. Modified from Anderson and Kanani (2007).
Whereas past efforts focused on the aortic valve, current technologies are being developed to create devices for the more complex valves of the heart.
PAST TECHNOLOGIES
Valve replacement devices can be classified into two categories: whole valves and prosthetic valves. Whole valves consist of allografts and xenografts; prosthetic valves are composed of pericardial (tissue) and mechanical valves. The valve designs vary in numerous aspects and have evolved over time, but the goal has remained the same: an easily implantable and durable solution that increases blood flow while decreasing the risk of associated complications such as thrombosis. Each type of valve has advantages and disadvantages, which are taken into consideration when deciding which device is appropriate for an individual patient.
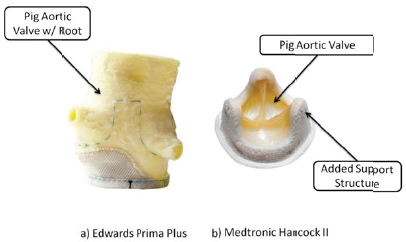
FIGURE 2 Examples of (a) stentless xenograft that uses the native support structure of the aorta and (b) supported xenograft with native aortic valve removed and added stent and sewing ring structure.
Whole Valves
Allografts are valves transplanted from another human, and xenografts are from another species. Cow and pig valves are usually selected for transplant as they best mimic the size and structure of human valves.
Attempts have been made to transplant mitral valves (Gulbins et al. 2000, 2002; Kumar et al. 2000), but the most successful and frequently used valves are pulmonary and aortic valves, which are often used interchangeably due to their similar geometry. Developments in transplanted valves have focused on improving structural support, which is necessary when the valve is removed from its native surroundings (Figure 2).
Vast strides have been made in tissue cryopreservation, which maintains high cell viability when thawed (O’Brien et al. 1987). But the appeal of allograft and xenograft valves suffers from their limited availability of size ranges and technically challenging procedure, in the case of stentless designs, which require the physician to remove the entire valve along with a portion of the aortic root to attach the replacement valve.
Prosthetic Valves
Transplanted whole valves remain a viable option, but prosthetic valves, including both mechanical and pericardial tissue valves, hold the largest share of
the market. Of valves implanted in the United States today, most (approximately 60,000) are made of pericardial tissue; in contrast, only 10,000 mechanical valves were implanted in 2013 (Millennium Research Group 2013), although design improvements are minimizing or often eliminating the disadvantages of mechanical valves (e.g., thrombogenicity requiring anticoagulation therapy).
Both pericardial and mechanical valves consist of a sewing ring (for securing them in place), a support structure, and leaflets. Mechanical valves are similar in structure to tissue valves, but differ in the leaflet design (Figure 3). Mechanical valves have seen the greatest variety in designs, optimized through geometry, hinge mechanisms, and materials.
These designs include ball and cage, floating/tilting disc, and bileaflet (Figure 3a); the latter is the leading design in today’s industry. These valves do not need to be replaced—indeed, they typically outlive the patient—but they require the constant use of anticoagulants, which is not appealing to most people and not an option for some. In contrast, tissue valves lack the longevity of mechanical valves but do not require anticoagulation, making them a preferred choice.
In contrast to mechanical valves, pericardial tissue, the sac that lines the heart, is highly durable and therefore used to construct the leaflets of a tissue prosthetic valve. The leaflets are then sewn to the stent support structure attached to the sewing ring. The attachment of the tissue to the structure is crucial to ensure durability and requires each valve to be hand assembled and sewn. The sewing ring may consist of a silicone band and cloth that support tissue ingrowth to the surrounding anatomy to provide future fixation support.
Although the overall design of the tissue valve has remained relatively unchanged throughout the years and mimics the design of the native aortic and pulmonary valves, the fixation process for the leaflets has been optimized. Vari-
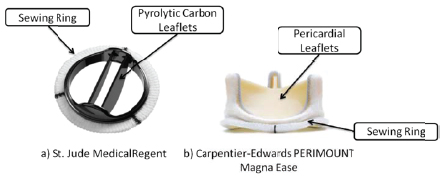
FIGURE 3 Examples of (a) bileaflet mechanical and (b) tissue prosthetic valves. Both valves shown can be used as replacements for all valves.
ous solutions are used to crosslink the collagen fibers and ensure durable leaflet structure. The method by which tissue is fixed and preserved is a proprietary process guarded by each company.
As with any design, tissue valves also have limitations, of which the most significant is durability. Typical tissue valves currently on the market can last up to 20 years before the leaflets lose functionality and experience structural deterioration, usually due to calcification (Schoen and Hobson 1985; Schoen and Levy 2005).
CURRENT TECHNOLOGIES
Over the past 10 years, noninvasive implantation of heart valves has revolutionized the field. Implants traditionally required the chest to be splayed open to allow access to the heart, but recent advances make it possible to access the valve through the femoral vein via an incision as small as an inch. This noninvasive approach, called transcatheter valve replacement, is suitable for patients who are not candidates for open-heart surgery and offers a faster recovery.
The first transcatheter delivery of a valve was attempted in the 1960s, but it has only recently become accepted as a viable procedure, aided by advances in stent design and noninvasive imaging techniques. The development of transcatheter heart valves showcases the power of a multidisciplinary approach: it merges technologies from numerous devices (e.g., coronary stents and balloon angioplasty) and disciplines (e.g., interventional cardiology and cardiac surgery) to create a paradigm-shifting advance.
There are many advantages to a transcatheter approach, but added complexity arises because the valve must work with the patient’s diseased anatomy. In the past the diseased valve was typically removed; now, the designs and their ability to succeed rely heavily on the patient’s anatomy. For example, a transcatheter aortic valve is secured in place by applying an outward force on the calcium deposits on the native leaflets.
An additional obstacle that transcatheter technologies have had to overcome is the loss of direct visualization afforded by open-heart surgery. This is especially important when deciding where to place the valve to ensure that it is secured while avoiding the coronary ostia, which is crucial to supplying blood to the heart (Figure 4). Advances in noninvasive imaging allow for real-time imaging using multiple modalities, such as echocardiography to visualize the native anatomy and fluoroscopy to visualize the device.
FUTURE TECHNOLOGIES
The valve replacement industry is beginning to focus on the other valves in the heart and developing devices that will work in concert with the native anatomy to repair instead of replace native valve function. The number of repair procedures is on the rise as compared to replacement procedures, which have remained steady
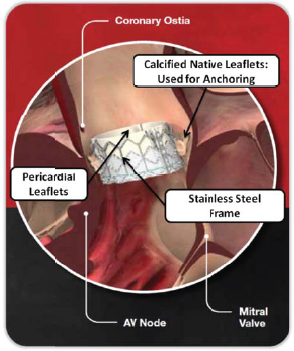
FIGURE 4 Transcatheter heart valve using the surrounding calcium in the native aortic valve to anchor. AV=atrioventricular. Source: Edwards Lifesciences.
from year to year. Recent trends favor repairing the native valve as opposed to replacing it, with approximately 32,000 mitral repairs as compared to 21,000 replacement procedures conducted in the United States in 2013 (Millennium Research Group 2013).
The introduction of transcatheter heart valves has brought new excitement to this area. Placed inside a defective tissue valve, transcatheter valves provide a way around the challenge of tissue valve durability: a tissue valve may be implanted in a younger patient with the idea that an additional valve can be placed if needed at a later date.
Valve manufacturers are expanding the number of diseases they can treat through transcatheter technologies; for example, companies are working to treat mitral valve regurgitation, a much larger market compared to aortic valve pathology. But, as mentioned, there are many hurdles in the transfer of technology and techniques to the mitral valve because it is more complex and patients tend to be in worse overall health with multiple comorbidities. That said, technology has
advanced such that it is possible to attack more subtle pathologies and not only a valve that is completely failing.
Mitral valve repair technologies today aim at correcting a specific pathology and do so by targeting any aspect of the valve, from replacing the chords, which attach the leaflets to the ventricle, to reducing the size of the annulus and bringing the leaflets closer together to allow for sealing. In attempts to replace the valve, designs require an anchoring location as they cannot be sewn in like a traditional surgical replacement. Engineers therefore retain the native leaflets or annulus when possible as an anchor site for the replacement part.
Because of the direct interaction with and reliance on the functionality of the native valve, engineers must expand their horizons and become experts in tissue mechanics as well. The frontier of heart valve engineering is less about engineering and more about applying engineering principles in a way that requires understanding of anatomy and physiology. Collaborations of engineers working side by side with clinicians, biomedical engineers, and biologists produce the best heart valve designs.
The future of heart valves is also reliant on new engineering materials. In addition to progress in the application of synthetic materials, especially with the mechanical valve, new biological and polymeric materials are being developed. With the advent of transcatheter valves, the limits of current materials are being challenged. Tissue, polymeric, and even cloth designs are being pushed beyond what was previously thought possible in the effort to increase strength and durability and reduce the device profile. The latter requires thinner leaflets, which in turn require ingenuity to develop a strong but thin material.
New tissue treatment processes are also being developed and tested. A recent advance allows valves to be shipped dry, no longer requiring the leaflets to be stored in solution. This development allows transcatheter valves to be shipped on the delivery catheter and eliminates the need for an engineer to be present at the procedure.
These examples are a testament to the benefits of new technologies: they both enable and force development beyond what was previously thought possible.
DESIGNING FOR THE FUTURE
Next generation heart valves have brought excitement to the field, but it is also important to understand how we as engineers go from a concept to a lifesaving device. We must first survey the patient population and identify a need, then develop a concept to address that need. Bench studies and animal studies are used in conjunction to test the functionality and durability of a design. Then the materials are tested in animal models to ensure that no adverse effects arise as a result of interactions with the body.
Complementing innovations in materials and design, new imaging protocols are being developed to ensure that a device is delivered to the correct location.
Using a combination of imaging techniques (e.g., echocardiography, angiography, MRI, and CT), the implantation team can visualize both the device and the anatomy without opening the chest. These techniques are also used to determine the success of the procedure both at the time of implantation and in follow-up examinations to ensure the device’s continued functionality.
When heart valves were first implanted, regulatory requirements to review the process for implantation were minimal or nonexistent. Now extensive testing is required to ensure short- and long-term success prior to implantation. The test data are submitted to a regulatory body and reviewed before implantation can be cleared. Pending full approval for general use, a first-in-human study may be conducted in compassionate cases, for patients who have no other options; these trials are usually limited to about 10 patients. If they show success a much larger clinical study is initiated, which can include hundreds of patients. From there the data are submitted to the regulatory body to get approval to commercialize the device and make it accessible to the approved patient population, ensuring that the patient’s safety is the priority. When the device is made available for the masses it fulfills its original goal of saving lives.
As with many engineering creations, the design process is never complete. Once the device is implanted in humans, improvements are constantly made based on evidence from the patients. Research and development efforts seek to recreate and simulate the human environment on the bench and in animals, but there are always lessons to be learned and from there improvements.
Additionally, as new technologies and innovations are introduced to the marketplace, even in different industries, these are applied to existing devices for optimization as necessary. A great example of this is the development of new biomaterials for orthopaedic and other cardiovascular applications, in which findings and testing history can be leveraged for the valve area.
CONCLUSIONS
Now is an exciting time for heart valve development as companies are pushing the limits, expanding into new areas, and helping more patients than ever before. Advances continue to move heart valve development forward. As designs are optimized engineers are turning their attention to other disease states with next generation designs and approaches. With increased confidence in current device durability for both mechanical and tissue valves, the focus is changing from surgical to transcatheter implants and from replacement to repair devices implanted with transcatheter methods.
Each advance requires greater understanding of the disease state of the valve. The greatest successes will involve technologies and techniques that work in concert with the human body.
REFERENCES
Anderson RH, Kanani M. 2007. Mitral valve repair: Critical analysis of the anatomy discussed. Multimedia Manual of Cardiothoracic Surgery (MMCTS)/European Association for Cardio-Thoracic Surgery 2007(0219):mmcts 2006 002147.
Gulbins H, Kreuzer E, Uhlig A, Reichart B. 2000. Mitral valve surgery utilizing homografts: Early results. Journal of Heart Valve Disease 9:222–229.
Gulbins H, Anderson I, Kilian E, Schrepfer S, Uhlig A, Kreuzer E, Reichart B. 2002. Five years of experience with mitral valve homografts. Thoracic and Cardiovascular Surgeon 50:223–229.
Kumar AS, Choudhary SK, Mathur A, Saxena A, Roy R, Chopra P. 2000. Homograft mitral valve replacement: Five years’ results. Journal of Thoracic and Cardiovascular Surgery 120:450–458.
Millennium Research Group. 2013. US markets for heart valve devices 2014. Available at www.mrg.net/Products-and-Services/Syndicated-Report.aspx?r=RPUS12HV13.
O’Brien MF, Stafford EG, Gardner MA, Pohlner PG, McGiffin DC. 1987. A comparison of aortic valve replacement with viable cryopreserved and fresh allograft valves, with a note on chromosomal studies. Journal of Thoracic and Cardiovascular Surgery 94:812–823.
Schoen FJ, Hobson CE. 1985. Anatomic analysis of removed prosthetic heart valves: Causes of failure of 33 mechanical valves and 58 bioprostheses, 1980 to 1983. Human Pathology 16:549–559.
Schoen FJ, Levy RJ. 2005. Calcification of tissue heart valve substitutes: Progress toward understanding and prevention. Annals of Thoracic Surgery 79:1072–1080.
This page intentionally left blank.










