3
A Framework for Integrating Health into Recovery Planning
“Long-term recovery planning is an opportunity to improve a community’s quality
of life and disaster resiliency. It has the potential to inspire communities to set goals
beyond restoration of the status quo.”
—Boyd, 2014, p. 3
Disaster recovery is a process of strategic community planning, similar to that which takes place in communities throughout the country every day, except that it entails the enormous challenges of time compression: a process that would normally occur over decades must be carried out within a relatively short period of time (Olshansky, 2014). Beginning the recovery planning process before a disaster and leveraging the products of other community planning efforts can make post-disaster recovery planning more efficient and also better ensure that opportunities for community betterment (including health improvement) are not missed. In this chapter, the committee uses the strategic planning process as a framework for describing the opportunities and mechanisms for incorporating health considerations into the recovery planning process, both before and after a disaster. It should be emphasized that the intent here is not to provide a comprehensive description of the recovery planning process; such a description is beyond the scope of this study and has been provided elsewhere.1
THE STRATEGIC PLANNING PROCESS AS A FRAMEWORK
In strategic planning, quantifiable data and a process of systematic analysis are used to develop goals, identify alternatives, and establish criteria for decision making. Although there are slight variations and differences in terminology, the general structure of such planning processes (whether developing a comprehensive plan, health improvement plan, or disaster recovery plan) is similar. After an initial period
________________
1 Of note, in 2014 the American Planning Association released Planning for Post-Disaster Recovery: Next Generation, an update of its 1998 report on recovery planning (APA, 2014). The committee suggests this report as a useful resource for those desiring a more detailed description of the disaster recovery planning process. The report is available online at: https://www.planning.org/research/postdisaster (accessed March 13, 2015).
of laying the groundwork, there is often a visioning process and an assessment of community status and needs, assets, and contextual factors (e.g., political environment). The results of these two processes are used to establish goals and set priorities by comparing the findings of the assessment against the community’s vision to identify gaps between the current status within the community and the desired state. Strategies are developed to close the gaps through input from stakeholders (including the public) and analysis of alternatives. These strategies are incorporated into a plan, and implementation partnerships (or operational structures) are developed. Finally, the plan is implemented. Resources are identified and applied, and progress is continuously measured using preestablished benchmarks. Even if it is not possible to tackle each priority area initially, a prioritized list makes it possible to evaluate future opportunities to determine how they can be leveraged to achieve the community’s shared vision. Thus, the process of implementation feeds into a continuous cycle of assessment, planning, and implementation.
The strategic planning process, if successful, creates new channels for communication and builds consensus on the community’s greatest needs going forward. This consensus building is critical to keep decision makers focused on long-term strategic objectives rather than on reactionary responses to the crisis of the day. Thus, obtaining buy-in from leadership is an essential step in ensuring that the plan is acted upon.
In the context of integrating health into the disaster recovery planning process, each of the steps in the strategic planning cycle presents opportunities. These are summarized below and then described in more detail throughout this chapter. It should be emphasized that, although the process is presented as sequential for purposes of exposition, in reality the order of steps may be varied, and some may be undertaken simultaneously. For example, visioning may occur before, simultaneously with, or after an assessment process, and because the process is a continuous cycle, the implementation step feeds into a new assessment used to evaluate the impact of the activities undertaken.
- Visioning: Recovery is viewed as an opportunity to advance a shared vision of a healthier and more resilient and sustainable community.
- Assessment: Community health assessments and hazard vulnerability assessments provide data that show the gaps between the community’s current status and desired state and inform the development of goals, priorities, and strategies.
- Planning: Health considerations are incorporated into recovery decision making across all sectors. This integration is facilitated by involving the health sector in integrated planning activities and by ensuring that decision makers are sensitized to the potential health impacts of all recovery decisions.
- Implementation: Recovery resources are used in creative and synergistic ways so that the actions of the health sector maximize health outcomes and the actions of other sectors yield co-benefits for health. A learning process is instituted so that the impacts of recovery activities on health and well-being are continuously evaluated and used to inform iterative decision making.
Building on Previous Strategic Planning Processes
Rationale for the Integration of Planning Processes
In the post-disaster period, there is intense pressure from the residents of the community to return to a state of normalcy. As a result, attempts to address deficiencies in pre-event conditions (including health deficiencies and disparities) through post-disaster planning alone will be challenging and may not be successful. Thus, pre-disaster recovery planning is critical to seizing opportunities for improving community conditions beyond the pre-disaster state. After a disaster, the resources that become available to support recovery can then be evaluated against the preestablished goals for improvement of health and social vulnerability, and relationships developed through the planning process can be leveraged in developing strategies for achieving the community’s preestablished vision of a healthy, resilient, and sustainable community.
In most cases, communities (cities, counties, towns) that have been struck by a disaster already have strategic plans in place that were created to guide decision making related to long-term development and
investment. It follows that these plans would be consulted in the process of developing a recovery strategy so that the recovery process can help the community advance toward a previously agreed-upon vision and set of goals. Figure 3-1 shows how products from previous planning processes—including a shared vision, assessments, and plans—are optimally leveraged and built upon to guide the disaster recovery planning process.
Relevant to the purposes of this report, a community’s comprehensive plan,2 health improvement plan, sustainability plan, and mitigation plan—and, in some cases, its regional development plan—can yield health-related goals and investment strategies to inform the recovery planning process. Ideally, the community health improvement plan (following from a community health assessment) will have informed the development of the comprehensive plan. The decisions and strategies that are the domain of the comprehensive planning process—land use, transportation, housing—determine the nature of the physical and social environments in which people live. Planning decisions over the past century have had enormous impacts on some of the nation’s most intractable public health challenges, such as obesity, chronic respiratory diseases, health disparities, and mental health (Dannenberg et al., 2003; Frumkin et al., 2004; Ricklin et al., 2012). Consequently, the comprehensive planning process is an important mechanism for enacting change in arenas beyond the direct influence of the health sector, such as the design of the built environment (APA, 2006a).
The integration of a health-focused community vision and health improvement goals into the community strategic planning process and the comprehensive plan itself helps ensure buy-in from leadership (since these plans must be formally adopted by the community’s governing body) and subsequently the incorporation of these elements into recovery strategic planning. According to the American Planning Association (Schwab et al., 1998, p. 238), “Post-disaster recovery plans should be a specific application of the relevant portions of the community comprehensive plan, designed to deal with the constraints and opportunities posed by disaster conditions.” Thus, a community that has undertaken this integration before a disaster is likely to be better equipped to address health considerations during recovery. Similar approaches are being promoted for the purposes of resilience. The Federal Emergency Management Agency (FEMA) now recommends the integration of hazard mitigation planning into the comprehensive plan as a means of ensuring that resilience is established as a community value and that hazard vulnerability is considered during all future development (FEMA, 2013a). According to the American Planning Association, “hazard mitigation works best as a policy objective of local planning when it is so completely integrated into the comprehensive plan that it becomes a normal assumption behind all daily planning activities” (Schwab et al., 1998, p. 61). The committee envisions the same outcome for health and social well-being.
The Current State of Integration of Planning Processes
Unfortunately, the committee found that the predominant model at present is one in which community comprehensive planning, health improvement planning, resiliency and sustainability planning, and disaster recovery planning occur largely in isolation. Barriers to integration noted by both public health and planning professionals include a lack of resources, tools, and guidelines, as well as an absence of qualified personnel able to bridge the two fields (APA, 2006a). In 2010, the American Planning Association surveyed planning departments across the United States to determine how comprehensive plans and sustainability plans are and can be used to protect and promote health. Just over a quarter of the nearly 900 respondents indicated that public health issues were addressed explicitly in their jurisdiction’s officially adopted comprehensive plan, either through stand-alone health planning elements or the incorporation of health concerns into other planning elements, such as land use (Hodgson, 2011). Common health topics in the examined plans included physical activity or active living, clean air and other environmental exposures, and public safety. However, there was a notable lack of focus on food and nutrition, health and human services, social
________________
2 The comprehensive plan, also known as the general plan, is the product of a community’s comprehensive planning process, which is used to determine community goals and aspirations for future community development.
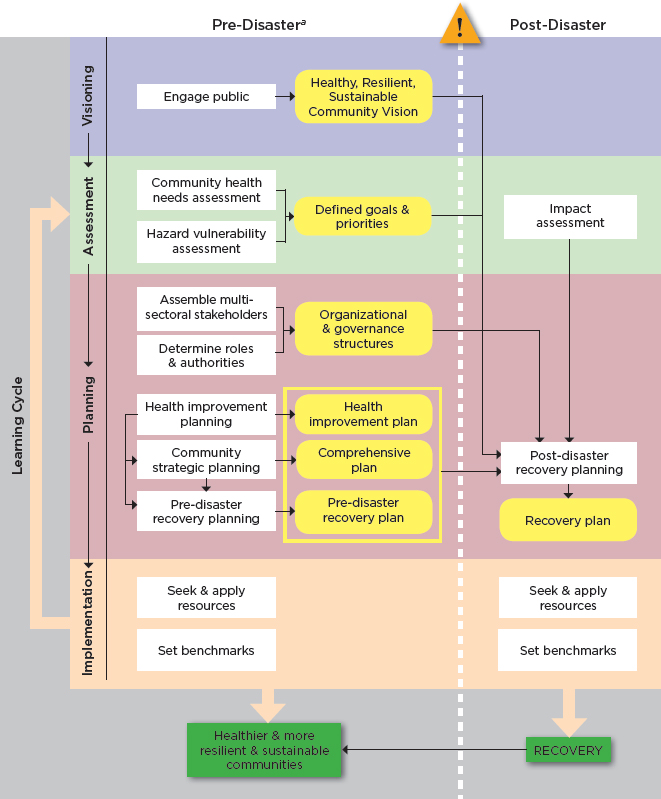
a Although the committee strongly encourages communities to undertake these activities in the pre-disaster period to maximize opportunities for leveraging the post-event recovery process to create healthier and more resilient and sustainable communities, there is still benefit to incorporating them into post-disaster recovery planning if they have not been undertaken beforehand.
cohesion, and mental health (Ricklin and Kushner, 2013). A 2010 International City/County Management Association survey found that although many communities have a range of sustainability activities that address social equity (e.g., affordable housing, preschool programs, workforce development initiatives), only about one-third of the approximately 2,100 responding local governments considered social justice a priority, and few were organizing and resourcing sustainability-related programs in a coordinated way or incorporating them into the comprehensive plan (ICMA, 2014). The two studies together indicate that the social aspects of health are not yet a focus for most local governments and that much greater effort is needed to integrate all determinants of health into comprehensive plans.
Similarly, the committee found little evidence of integration of a healthy community vision and long-term health improvement goals into pre-disaster recovery plans. Unfortunately, few communities have taken a proactive approach to the development of comprehensive pre-disaster recovery plans (Community Planning Workshop, 2010; Smith, 2011b). Two recent publications highlight cases in which pre-disaster planning for recovery was undertaken (City of Seattle, 2013; Community Planning Workshop, 2010), both concluding that few models were available to guide communities in the development of such plans. This paucity of pre-disaster recovery plans is due in part to the lack of incentives for communities to undergo what can be a complex, time-consuming, and controversial process (Community Planning Workshop, 2010). To better understand the degree to which community health improvement goals have been incorporated into pre-disaster recovery planning, the committee reviewed available pre-disaster recovery plans and sought testimony from public health, emergency management, and city management representatives. These information gathering processes yielded the following findings:
- Approximately three-quarters of the roughly two dozen pre-disaster recovery plans examined3 explicitly address health considerations to some degree but are focused almost exclusively on short- and intermediate-term recovery activities (e.g., reopening and restoring health facilities; retaining medical personnel; ensuring access to pharmaceuticals; meeting the needs of vulnerable populations; providing mental health assistance; handling mass casualties; controlling disease outbreaks; and preventing exposure to unsafe materials such as debris, mold, and chemicals).
- Pre-disaster recovery plans that are more operational in nature (lay out organizational structures, roles, and responsibilities) focus primarily on short- and intermediate-term recovery activities with discussion of long-term recovery being limited to a return to pre-incident conditions/normal operations. Although these plans address increasing resilience through recovery activities (e.g., through hazard mitigation processes), the committee found no references to using the recovery process as an opportunity to build healthier communities. Plans that are more visionary in nature4 are more likely to reference opportunities to use the recovery process to create healthier post-disaster communities, although none of the plans examined mentions leveraging the community’s health improvement process. However, several plans recommend incorporating the vision and goals of the comprehensive plan, reinforcing the importance of integrating health improvement and comprehensive planning prior to a disaster (Hillsborough County Government, 2010; Pinellas County, 2012).
- Testimony of public health officials from jurisdictions that have been through a disaster was focused largely on short- and intermediate-term needs (e.g., restoring health care operations, ensuring access to pharmaceuticals), although testimony from the former health commissioner of New Orleans did include considerable discussion of strategies undertaken in that city to rebuild both public health
________________
3 It should be noted that the vast majority of these plans were from Florida counties. Florida has led the development of pre-disaster redevelopment plans, spurred in part by a statute requiring all coastal communities to have them (Section 163.3177(6)(g), Florida Statutes; Section 163.3178(2), Florida Statutes). The state developed a planning guide, the Web link to which can be found in Appendix C.
4 The redevelopment plans of Hillsborough County (Hillsborough County Government, 2010) and Pinellas County (Pinellas County, 2012) in Florida were found to be good models for ensuring that health and social well-being considerations are incorporated into diverse aspects of recovery planning. Links to these plans are available in Appendix C.
-
and health care systems in a way that would improve the health of the community (DeSalvo, 2013). The testimony of urban and regional planners was more likely to include discussion of opportunities to build the community back in a way that promotes health—perhaps reflecting growing interest in health within the urban and regional planning and design fields since many of the opportunities to change the physical and social environments of a community fall under the purview of planning professionals.
- Health departments find leveraging the recovery process for long-term health improvement challenging because of their intense mission focus on response activities, the lack of funding to support long-term recovery projects, their lack of engagement in community long-term recovery planning, and the perception that a discussion of such topics as long-term health improvement strategies would not be well received by a community still dealing with significant acute post-disaster needs (Beardsley, 2014; Clements, 2014; Zucker, 2014).
- Although federal preparedness funds available from both the Centers for Disease Control and Prevention (CDC) and the Office of the Assistant Secretary for Preparedness and Response within the U.S. Department of Health and Human Services (HHS) are eligible for use to support recovery planning, there is currently little emphasis on using the recovery process for long-term community health improvement (Blumenstock, 2014; Shah, 2014).
- Nearly all communities in the nation are recipients of federal community development funding, and a large proportion of these local governments are using the targeted funds to revitalize troubled neighborhoods and address the needs of residents—efforts essentially similar to those of disaster recovery. Nonetheless, there is low awareness of pre-existing community development endeavors during the preparation of pre-disaster recovery and hazard mitigation plans.
In summary, based on the testimony of a diverse set of stakeholders, including the public health community, and a review of available recovery plans, the committee finds that a healthy community vision rarely guides the development of pre-disaster and post-disaster recovery plans. As a result, a health lens is not applied to the process of decision making regarding the allocation of recovery resources, and unique opportunities are being missed. The following four gaps impede the development of plans to “build back better,” and specifically in ways that contribute to an overall healthier community:
- inadequate pre-disaster community health improvement planning (not being done at all, or not using a process that engages the full range of community stakeholders in addressing the comprehensive physical and social determinants of health);
- inadequate integration of health improvement planning and the community comprehensive (strategic) planning process used to set priorities and allocate funds;
- lack of integration of health improvement planning and disaster recovery planning;
- insufficient awareness across all sectors of the health-related threats and opportunities posed by disasters and of the benefits to be gained from integrating community health improvement objectives and priorities into comprehensive and disaster recovery plans to achieve shared goals.
In some cases, these gaps reflect long-standing silos within and among institutional arrangements and staffing structures. Enhanced collaboration across sectors offers an opportunity to align planning processes around a shared vision and goals so as to optimize community health and social service outcomes during recovery. Table 3-1 illustrates potential roles for diverse community stakeholders in this integrative process. For the most vexing problems, however, especially where large-scale community revitalization is at stake, solutions may require significant leadership investment to achieve organizational readiness and the capacity for synergistic, multisector health-sensitive disaster recovery planning.
TABLE 3-1 Collaborative Roles of Sector and Community Stakeholders in the Integration of Strategic Planning Processesa to Achieve Healthier and More Resilient and Sustainable Post-Disaster Communities
| Visioning | Assessment | Planning | Implementation | ||||||
| Task | Educate community on elements of healthy, resilient, and sustainable communities | Conduct community health assessments, ensuring that Internal Revenue Service (IRS)required hospital Community Health Needs Assessments (CHNA) are integrated | Develop health improvement plan based on health assessment | Exercise pre-disaster recovery plan by practicing organizational arrangements suited to hypothetical disasters | |||||
| Lead(s) | Public health, emergency management, urban and regional planning | Public health, health care | Public health | Emergency management | |||||
| Partners | All sectors, all stakeholders, community members | Social services, behavioral health | All sectors | All sectors | |||||
| Whenb | |||||||||
| Task | Conduct community visioning process | Assess vulnerability of critical infrastructure | Develop comprehensive plan, ensuring inclusion of all relevant plans (e.g., hazard mitigation, health improvement, economic, redevelopment) | Adopt regulations, incentives, programs, budgets, and community outreach to achieve community vision and goals | |||||
| Lead(s) | Urban and regional planning, public health | Public health, public works, emergency management, facility management, planning | Urban and regional planning | Chief executive, community managers, elected governing body | |||||
| Partners | All other sectors | Management, finance, budget | Public health, emergency management, other local agencies | All implementing agencies and organizations | |||||
| Whenb | |||||||||
| Task | Incorporate community vision into comprehensive planning process | Identify areas with large socially vulnerable populations | Plan organizational structures for postdisaster coordination of activities | Seek methods for making optimum use of technology and information systems for both public outreach and pre-disaster policy analysis | |||||
| Lead(s) | Urban and regional planning, public health, environmental health, social services | Public health, urban and regional planning, emergency management, social services | Emergency management | Emergency management, public health, urban and regional planning | |||||
| Visioning | Assessment | Planning | Implementation | ||||||
| Partners | All sectors, plus management, finance, budget offices | Research organizations, community groups, neighborhood associations, health and medical system partners | All sectors | All sectors | |||||
| Whenb | |||||||||
| Task | Ensure that pre-disaster recovery plan incorporates community-developed vision of healthy, resilient, sustainable community | Periodically assess effectiveness of institutional arrangements that promote cross-sector collaborations and joint mitigation activities | Develop pre-disaster recovery plan | Establish joint communications center; facilitate information exchange on community recovery needs | |||||
| Lead(s) | Emergency management, urban and regional planning | Emergency management, urban and regional planning, public health | Urban and regional planning, economic development agency, emergency management | Emergency management, public officials | |||||
| Partners | Public health and other agencies | Education system, health and medical system partners, business representatives | All sectors | Public health, health care, behavioral health, social services | |||||
| Whenb | |||||||||
| Task | Periodically revisit community vision statements for relevance in light of changing conditions and altered vulnerabilities | Assess unmet social needs, pre- and postdisaster | Conduct health impact assessments to inform recovery planning | Develop recovery finance strategy, determine funding eligibility, apply for funds, administer grants | |||||
| Lead(s) | Urban and regional planning, public health, emergency management | Social services | Public health | Designated recovery manager | |||||
| Partners | All sectors, plus management, finance, budget offices | Public health, behavioral health, emergency management | All sectors | All sectors | |||||
| Whenb | |||||||||
| Task | Monitor economic development and community development initiatives that may strengthen the community, add resilience, create sustainability | Conduct postdisaster assessment of disaster impact on infrastructure and systems | Develop post-disaster recovery plan | Carry out recovery projects and programs; arrange project and program management | |||||
| Visioning | Assessment | Planning | Implementation | ||||||
| Lead(s) | Urban and regional planning, public health, emergency management | Emergency management | Emergency management, urban and regional planning | All sectors | |||||
| Partners | All sectors, plus management, finance, budget offices | Urban and regional planning, public works, public health, management | All sectors | Management departments such as budget, finance, legal services | |||||
| Whenb | |||||||||
a The processes to be integrated include community comprehensive planning, health improvement planning, mitigation/ resilience planning, and disaster recovery planning.
b 1 = pre-disaster; 2 = response and short-term recovery; 3 = long-term post-disaster recovery. Coloring of the symbols indicates urgency: red = priority; black = possibility.
A HEALTHY, RESILIENT, SUSTAINABLE COMMUNITY VISION FOR DISASTER RECOVERY
Disasters, although devastating, create an opportunity through the recovery process to advance a shared vision of a healthier and more resilient and sustainable community. In Chapter 2, the committee describes the elements of a healthy community and its linkages with the concepts of equity, resilience, and sustainability. How these elements are incorporated into the shared vision for an individual community needs to be defined as an integral part of community strategic planning processes conducted before an event, so that a clear vision is in place to drive post-disaster decision making as new resources become available and opportunities arise. Otherwise, pressure to rebuild quickly after a disaster may result in missed opportunities.
A common vision for recovery is highlighted by FEMA (2011c) as one of eight major components of a successful recovery in Lessons in Community Recovery, a 2011 report that presents lessons learned from 7 years of experience with the long-term community recovery emergency support function. A vision provides a “beacon for decision makers and some framework within which decisions will be taken” (Schwab et al., 1998, p. 47). Without an overall vision, goals and objectives often are disconnected from each other and from a larger purpose. A community’s vision becomes the foundation for subsequent policies and regulatory changes, and investments. A visioning process also can drive enthusiasm and provide a foundation for creative collaboration. It is not surprising, then, that many planning processes, including disaster recovery planning, begin with a visioning process that defines a desired future state.
The Importance of Having a Vision and Goals in Place Before a Disaster
Visioning is a common early step in the recovery planning process after a disaster. As the committee learned through testimony from disaster recovery experts and from a review of case studies, however, a community that has already gone through the process of envisioning its future and setting measurable goals and priorities before a disaster is in a better position to converge on a plan for recovery quickly after such an event (see Box 3-1). The urgency of the post-disaster period poses a significant challenge to the development of recovery plans that meet a community’s long-term needs. Governments facing the complex
BOX 3-1
The Value of Pre-Disaster Visioning and Planning: A Tale of Two Cities
The New Orleans Experience
The flooding of New Orleans that resulted from levee failure after Hurricane Katrina struck the Gulf Coast in 2005 is among the most catastrophic disasters in U.S. history. The recovery process in New Orleans continues today and was significantly impeded by disputes over processes and goals for reconstruction, with tensions arising from conflicting desires to quickly rebuild the familiar or to create a safer and more sustainable and equitable city (Kates et al., 2006). In many cases, ideas for reducing the size of the city and increasing green space were viewed as efforts to get rid of predominantly African American and low-income neighborhoods (Colten et al., 2008). Although the recovery planning process was initiated shortly after the flood, it took nearly 2 years and multiple rounds of planning initiated independently by the state and city to develop an officially accepted plan (the Unified New Orleans Plan). Despite these delays, the city of New Orleans has seized on the opportunities presented by disaster recovery to build back better. A 2010 update of the city’s comprehensive plan, Plan for the 21st Century: New Orleans 2030, includes as goals livability, opportunity, and sustainability (Collins, 2011).
The Cedar Rapids Experience
On June 13, 2008, the Cedar River, which flows through Cedar Rapids, Iowa, rose a record-setting 30+ feet, causing significant flooding in the city. Although no deaths resulted, the flood caused widespread destruction of the city’s physical infrastructure and resulted in the displacement of more than 10,000 residents. Fortuitously, the city council and city manager had initiated a broad community engagement effort just months before the flood to develop a shared vision for the community’s future (CARRI and CaRES, 2013). This existing engagement process, the resultant community vision, and a related effort to adopt a systems approach to government operations all enabled the community to come together quickly after the flood around a plan for what their new community would look like. The recovery plan, which incorporated input from thousands of residents, included such goals as encouraging active, healthy lifestyles; ensuring equitable redevelopment; building resource-efficient and resilient buildings; and protecting the city against future floods by rebuilding outside of flood-prone areas (ULI, 2014). Cedar Rapids has been recognized for its success by the U.S. Army Corps of Engineers, the American Planning Association, and the International Downtown Association, and it is touted as a model for other communities because of its ability to rapidly develop a publicly supported recovery plan that will create a better, safer future for all of its residents (CARRI and CaRES, 2013).
process of reconstruction after a disaster must balance two competing priorities—speed and deliberation (Johnson and Olshansky, 2013). Tensions inevitably arise between the need to restore infrastructure and a sense of normalcy as quickly as possible and the desire to leverage the recovery process as an opportunity for community betterment. Without a preexisting vision and associated goals, reactive decision making early in the recovery period may severely limit the range of options for betterment during later recovery phases. Accordingly, the phrase “window of opportunity” often is associated with the short period of time immediately after a disaster. As expressed by Jennifer Pratt, assistant director of planning services for the city of Cedar Rapids, Iowa, “One thing we heard from other communities that had suffered natural disasters was that it was important to have a plan rather quickly, because people naturally become nostalgic and just say, ‘Well, I want it the way it was before’” (ULI, 2014, p. 21).
Communities undertake a number of planning processes that yield a shared vision for the future that could be incorporated into pre- and post-disaster recovery planning efforts. A disaster should not change the long-term vision for a community, just the steps for achieving it. Plans that should be examined (if
available) include a community’s comprehensive plan, health improvement plan, and sustainability plan. If a holistic vision for a healthy, resilient, sustainable community is lacking, however, the pre-disaster recovery planning process can be used to build on previous visioning efforts. Using the shared vision as a guide, action plans can be developed after a disaster based on the new social, economic, and environmental conditions of the community (ASTHO, 2007).
Creating a Shared Vision as a First Step in Engaging the Public in Disaster Recovery
The involvement of informed and empowered individuals and communities through an authentic community engagement process is nearly universally recognized as a factor in the success of any community planning endeavor, including healthy community planning and disaster recovery (FEMA, 2011c; Love and Vallance, 2014). Community engagement has been defined as “the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people” (CDC, 1997, p. 9). “With and through” are the key words in this definition. Community engagement entails more than extracting information from residents about their needs and wants. True engagement integrates the affected community into every aspect of a project, from identifying needs to selecting priorities to implementing programs. Thus, there should be an “ongoing dialogue among residents to build relationships and a shared vision of what the community is, what it should be, and how to get there” (Norris and Pittman, 2000, p. 121).
The visioning process is an opportunity for communities to begin to rectify a legacy of exclusion that has contributed to the significant disparities apparent across U.S. communities today. Consequently, it is essential that groups representative of all members of the community—including the most vulnerable populations—be involved in the planning process, thus ensuring that the voices, perspectives, and needs of all segments of the community are addressed. Vulnerable populations often have special needs during and after a disaster, but they continue to be excluded from disaster planning processes (Sherry and Harkins, 2011). For example, low-income residents displaced by a disaster may not be able to return to the community as easily as their higher-income neighbors. Because of their absence, their voices are not heard at meetings and their perspective is not taken into account when rebuilding is being planned. In Galveston, Texas, this scenario led to a harsh outcome for low-income residents (Nolen, 2014). After 569 public housing units on the island were demolished following Hurricane Ike, many locals, including city council members, fought vigorously not to rebuild them. Community advisory committees that were providing input on recovery plans were limited to residents who were living in Galveston after the disaster, thus excluding anyone who had not yet returned. It took state and federal intervention to finally spur rebuilding of the units, a full 6 years after the hurricane struck (Rice, 2014). Had there been an attempt to include the displaced low-income residents in the crafting of the recovery plan, their voices would have been heard, and the public housing might have been rebuilt much more quickly.
Means of engaging the community in visioning often include town hall meetings, public workshops, surveys, and charrettes.5 Some activities undertaken while laying the groundwork for planning can help ensure the success of the visioning process. These activities may include but are not limited to
- identifying and engaging local health champions (from health and nonhealth sectors) to facilitate discussions;
- identifying other previous efforts and experiences that are relevant; and
- conducting health literacy efforts and educating the community on the elements of and benefits to healthy, resilient, and sustainable communities.
________________
5 A charrette is an iterative process that is often used to exchange ideas between urban and regional planners/designers and the community, resulting in an evolving series of designs (APA, 2006b).
ASSESSMENTS TO INFORM RECOVERY PLANNING
An assessment process is undertaken to inform the strategic approach to community planning. This process can be used to identify the needs, assets, and capacities of the community; prioritize interventions; and provide a baseline against which change can be measured. Three common assessments of relevance to disaster recovery planning are community health assessments, threat and hazard identification and risk assessments, and disaster impact assessments (see also the discussion of health impact assessments later in this chapter).
A community health assessment (sometimes referred to as a community health needs assessment) is “a systematic examination of the health status indicators for a given population that is used to identify key problems and assets in a community” (PHAB, 2011, p. 8). Community health assessments are part of a strategic planning process for health improvement, such as that described by the Mobilizing for Action through Planning and Partnerships (MAPP) framework (Lenihan, 2005). MAPP was developed to enable communities to “seek to achieve optimal health by identifying and using their resources wisely, taking into account their unique circumstances and needs, and forming effective partnerships for strategic action” (NACCHO, 2014c). Communities that use MAPP carry out a six-phase process: organizing, visioning, assessments, strategic issues, goals/strategies, and action cycle (NACCHO, 2014d). Although the collection of traditional health status indicators (e.g., obesity rates, numbers of uninsured) is an important part of the assessment process, it is necessary to adopt a more holistic approach. Other information relevant to a community health assessment may include community perceptions regarding health and quality of life, the performance of the local health system, and an evaluation of factors influencing health in the community (e.g., policies). Conducting a more comprehensive community health assessment to include these additional elements will provide a more complete understanding of the factors that influence community health (NACCHO, 2014b). Another valuable tool for community health assessment is the Community Health Needs Assessment Toolkit from Community Commons, an online tool that consolidates data from multiple sources and enables users to create maps and reports of health indicators (Community Commons, 2014).
Many local health departments, as well as nonprofit hospitals, are conducting community health assessments and leveraging them in the development of community health improvement plans. Health improvement planning is a requirement for public health agency accreditation, and under the Patient Protection and Affordable Care Act (ACA), the Internal Revenue Service (IRS) requires nonprofit hospitals to conduct a community health needs assessment (CHNA) at least once every 3 years as a condition for retaining tax-exempt status.6,7 Data from the 2013 National Profile of Local Health Departments indicate that within the past 5 years 70 percent of local health departments conducted a community health assessment, and more than half (56 percent) completed a community health improvement plan (NACCHO, 2014a). While the committee found these data encouraging, it is unclear how many of these plans have been successfully implemented. The suboptimal status of nationwide health statistics indicates that despite these increased planning initiatives, problems with implementation remain. Further, there is little evidence to suggest that these plans are aligned with broader community strategic planning processes such as those associated with the development of comprehensive or sustainability plans. As a result, the goals developed in those planning processes may not be sufficiently understood by the key community leaders and officials who are typically responsible for managing disaster recovery and, thus, may not be identified as priorities or leveraged during the recovery planning process.
________________
6 Under a final regulation effective as of December 29, 2014, a charitable hospital must (1) define the community it serves; (2) assess the health needs of that community; (3) take into account input from representatives of the community, including those with expertise in public health; (4) document the community health needs assessment in a written report; and (5) make that report available to the public (See 79 F.R. 78953, Dec. 31, 2014.)
7 79 F.R. 78953, Dec. 31, 2014.
Threat and Hazard Identification and Risk Assessments
Disaster recovery planning should be based on an assessment of locally specific risks. The threat and hazard identification and risk assessment process (described in Box 3-2) is a valuable tool for communities, helping them answer the following key questions as part of the pre-disaster planning process: “What do we need to prepare for, what sharable resources are required in order to be prepared, and what actions could be employed to avoid, divert, lessen or eliminate a threat or hazard?” (FEMA, 2014d). The assessment process is a community-wide initiative that emphasizes anticipation prior to assessment. As part of this process, community members themselves identify threats and hazards of concern and place them in the context of the greater community (FEMA, 2013b). The community then assesses each risk in context, developing capability targets and estimating the resources needed to achieve these targets for each of the core capabilities identified in the National Preparedness Goal. The use of community-level assessments, as opposed to traditional top-down assessments, reflects the fact that disasters and their impacts are unique to a given community and results in a more specific and informative assessment process overall. Internationally, the use of such community-level assessments has resulted in accelerated response and recovery (Reaves et al., 2014). Australia, for example, has expanded community-level input to its hazard anticipation and assessment as part of its Prepared Community model (Reaves et al., 2014).
Included among the capabilities under the National Preparedness Goal is Health and Social Services, as well as numerous other capabilities that impact a community’s health, such as Community Resilience, Long-Term Vulnerability Reduction, Risk and Disaster Resilience Assessment, Environmental Response/ Health and Safety, and Mass Care and Infrastructure Services. The Health and Social Services capability focuses on the ability to “restore and improve health and social services networks to promote the resilience, independence, health (including behavioral health), and well-being of the whole community” (FEMA, 2014a). Consequently, a community health assessment may inform the Threat and Hazard Identification and Risk Assessment process, particularly with regard to social vulnerability (discussed in Chapter 2), and there may be benefit to better integrating these two processes. Similarly, health care organizations are required to conduct a hazard vulnerability analysis as part of the accreditation process. These analyses help health care stakeholders prioritize risks so that appropriate planning, prevention, response, and recovery actions can be taken (The Joint Commission, 2005). The hazard vulnerability analysis provides an interface between the health care and emergency management sectors and should be complementary to the Threat and Hazard Identification and Risk Assessment process.
BOX 3-2
The Threat and Hazard Identification and Risk Assessment Process
- Identify Threats and Hazards of Concern: Based on a combination of experience, forecasting, subject matter expertise, and other available resources, identify a list of the threats and hazards of primary concern to the community.
- Give the Threats and Hazards Context: Describe the threats and hazards of concern, showing how they may affect the community.
- Establish Capability Targets: Assess each threat and hazard in context to develop a specific capability target for each core capability identified in the National Preparedness Goal. The capability target defines success for the capability.
- Apply the Results: For each core capability, estimate the resources required to achieve the capability targets through the use of community assets and mutual aid, while also considering preparedness activities, including mitigation opportunities.
SOURCE: Excerpted from FEMA, 2013b.
In the aftermath of a disaster, a disaster impact assessment can help determine what damage the disaster has caused, providing public officials and emergency management with information about the needs of an affected community. The assessment includes not just damage to infrastructure but all of the needs of the community. As part of this assessment, interview teams comprising staff and volunteers from state, local, and regional health departments conduct community-specific surveys. Officials can then use this information to identify what resources are needed and to target specific warnings to affected residents (IOM and NRC, 2005).
The disaster impact assessment helps identify unmet health needs. It is important that such assessments be conducted periodically throughout the response and recovery process following a disaster. Such reassessment provides real-time information about the status of various health-related factors such as housing, mental health, and utilities services. As response and recovery activities progress, the health needs of a community may change, especially if migration of families takes place into or out of an affected community (IOM and NRC, 2005). Conducting a disaster impact assessment immediately after a disaster and then reassessing throughout the recovery process enables continuous monitoring of how a disaster has impacted and continues to impact the health of a community.
Among the keys to successful community recovery identified by FEMA are preparing (establishing roles and responsibilities) and actively planning (FEMA, 2014b). As emphasized throughout this report, depending on the nature of the disaster, recovery initiatives present a multitude of opportunities to build the community back better (healthier and more resilient and sustainable). But arranging the planning process itself is complicated, and the inclusion of public health, medical, and social services requires that additional consideration and effort be devoted to crafting creative solutions that meet multiple needs. Resources must be harnessed in a coherent fashion matched to the situation in the community, incorporating both the current status and the prior developments that will be the foundation for future progress. Blending new features into community systems after a disaster, including consideration of socioeconomic and physical environments, is a significant design challenge: creative solutions and synergistic perspectives are required in deciding what can be rearranged, identifying institutional resources to accompany this redesign, building stronger, mitigating hazards, and incorporating an emphasis on health and social services for better outcomes. The goal is better recovery by all measures, a more vital community where resilience and stability add to overall well-being—a healthy community in the fullest sense.
In Chapter 2, the committee describes Health in All Policies as “an approach to public policies across sectors that systematically takes into account the health implications of decisions, seeks synergies, and avoids harmful health impacts, in order to improve population health and health equity” (WHO, 2013), and it presents a rationale for the relevance of this approach to the recovery context. Operationalizing Health in All Policies in the disaster recovery context entails (1) creating organizational structures that optimally enable the coordination of efforts and the creation of synergies whereby core missions of nonhealth sectors align with healthy community objectives, and (2) ensuring that information on the potential health impacts of recovery decisions is available to the decision makers within those structures. Each of these requirements is described in the sections below.
Organizing for an Integrated Approach
Communities are complex adaptive systems8 where decision making is distributed and myriad cross-sector interdependencies exist (Olshansky, 2014). Organizational structures influence the siloing of related
________________
8 Complex adaptive systems (1) are nonlinear and dynamic, (2) are composed of independent agents whose goals and behaviors may conflict, (3) are self-organizing, learning systems, and (4) have no single point of control (Rouse, 2000).
services and functions that can impede potential synergies and co-benefits. Despite the clear importance of an integrated approach (as discussed in Chapter 2), the committee consistently learned, through testimony (Nolen, 2014) and its review of the disaster literature (Johnson and Olshansky, 2013), about the inefficiencies and challenges during recovery related to a lack of coordination. As a result, resources are not used effectively and people suffer unnecessarily, especially those who were most vulnerable prior to the disaster. The resulting delays in individual and community recovery impact all facets of community life, including the health of the population, social cohesion, and economic viability. The committee concludes that disaster recovery and ultimately the health of the community would be improved by the development of organizational structures that support
- integrating horizontally across sectors and agencies;
- integrating vertically from the federal to the local level;
- integrating across phases of the disaster continuum, from pre-event planning to long-term recovery; and
- integrating health considerations into recovery planning and practices.
The new national framework describing a governance structure for disaster recovery—the National Disaster Recovery Framework (NDRF)—if implemented effectively, provides a structure for addressing all four of these dimensions of integration. As discussed below, however, some challenges remain.
The National Disaster Recovery Framework: A Structure for Integration
The NDRF, released in 2011, provides a guide for the federal government to facilitate effective recovery at the community level (FEMA, 2011d). The NDRF grew out of recognition of the failure to plan for recovery after Hurricane Katrina, the failure to link local needs with available resources, and the failure to plan for the actions of multiple parties to address disagreements about resource allocation (Smith, 2011a). In 2006, Congress passed the Post-Katrina Emergency Management Reform Act,9 which mandated the development of a national recovery strategy by the federal government. Spearheaded by FEMA and its federal partners, the NDRF is not an explicit plan; rather, it is a framework document that defines how federal agencies should organize and operate during recovery to support states, tribes, and localities. It defines “core recovery principles; roles and responsibilities of recovery coordinators and other stakeholders; a coordinating structure that facilitates communication and collaboration among all stakeholders; guidance for pre- and post-disaster recovery planning; [and] the overall process by which communities can capitalize on opportunities to rebuild” what the NDRF asserts are “stronger, smarter, and safer” communities (FEMA, 2011d, p. 1). As discussed below, the NDRF is intended for a wide audience of governmental, nongovernmental, and private organizations with expertise spanning all sectors.
Recovery roles and responsibilities under the NDRF The NDRF supports a whole-community approach to disaster recovery. Emergency management has historically been a strongly government-led enterprise. However, there has been increasing recognition that a solely government-driven approach cannot adequately meet the complex and unique needs of an individual community preparing for, responding to, and recovering from a disaster (FEMA, 2011a). Nongovernmental partners play critical roles in the restoration of the “social and daily routines and support networks” that promote health, well-being, and resilience after disasters (Chandra and Acosta, 2009, p. ix). However, these roles have been poorly represented in state and federal policy, and inadequate attention has been paid to the impacts of policy and guidance issued by federal agencies on nongovernmental entities. Within the past 5 years, FEMA has sought to foster a new philosophical approach based on the “whole community” (FEMA, 2011b). Through stakeholder engagement processes, the agency identified three core principles that drive its whole-community approach:
________________
9 Post-Katrina Emergency Management Reform Act of 2006, 109th Cong., S.3721 (October 4, 2006).
- Understand and meet the actual needs of the whole community.
- Engage and empower all parts of the community.
- Strengthen what works well in communities on a daily basis (FEMA, 2011a, pp. 4-5).
The objective is to perform emergency management functions in a manner that integrates needs, capabilities, and resources across the whole community and to empower the community—government, the nonprofit sector, and the private sector—to work together as partners (CDC and CDC Foundation, 2013). Roles for specific groups are outlined below.
- Individuals and households: The NDRF envisions that individuals and households need to be prepared to sustain themselves immediately after a disaster by carrying adequate insurance; holding essential supplies of medication, food, and water; and listening to public information announcements on the recovery process.
- Local government: Local government plays a central role in planning and managing all phases of a community’s recovery. When local governments are overwhelmed by their responsibilities, they seek the services of state and federal governments. Local governments also galvanize the preparation of hazard mitigation and recovery plans, raise hazard awareness, and educate the public prior to and during the recovery process.
- State government: The states are central players in coordinating recovery activities, including the provision of financial and technical assistance. One type of financial assistance entails issuing bonds for building critical infrastructure. States often manage federal resources and are conduits to local and tribal governments.
- Federal government: The central role of the federal government is to facilitate the efforts of state and local governments to leverage needed resources to rebuild communities. The federal government can use the NDRF to recruit and engage available department and agency capacities to promote local recovery. Federal support must be scalable and adaptable to meet community needs.
- The nonprofit sector: The nonprofit sector encompasses faith-based and other volunteer community organizations, charities, foundations and philanthropies, professional associations, and academic institutions. Major roles of the nonprofit sector include case management, volunteer coordination, behavioral health and psychological support, housing repair, and construction. Nonprofits tend to fill the gaps when governmental services and support do not meet a community’s comprehensive needs. Nonprofits often conduct advocacy for community members.
- The private sector: The private sector plays an essential role by retaining and providing employment and a stable tax base. It also owns and operates much of the country’s infrastructure, including electrical power, financial, and telecommunications systems. The private sector, including utilities, banks, and insurance companies, can foster mitigation and encourage community resilience. Public–private partnerships are critical resources during recovery and facilitate the coordinated leveraging of funding from multiple sources (FEMA, 2011d).
Recovery support functions Similar to the Emergency Support Functions (ESFs) defined by the National Response Framework,10 the NDRF defines six Recovery Support Functions (RSFs): Community Planning and Capacity Building; Economic; Health and Social Services; Housing; Infrastructure Systems; and Natural and Cultural Resources (described in more detail in Box 3-3). The RSFs help define an organizational
________________
10 The National Response Framework (NRF), also produced by FEMA, directs how the nation responds during the immediate period following all types of disasters and emergencies, ranging from “those that are adequately handled with local assets to those of catastrophic proportion that require marshaling the capabilities of the entire Nation” (FEMA, 2013c, p. 4). It “describes the principles, roles and responsibilities, and coordinating structures for delivering the core capabilities required to respond to an incident and further describes how response efforts integrate” with those of other related areas. Its objectives “define the capabilities necessary to save lives, protect property and the environment, meet basic human needs, stabilize the incident, restore basic services and community functionality, and establish a safe and secure environment moving toward the transition to recovery” (FEMA, 2013c, p. i).
structure for recovery operations that can promote vertical integration if aligned with structures created by state and local governments11 (see Figure 3-2). For each RSF, the NDRF specifies a federal coordinating agency, primary agencies, and supporting organizations. The coordinating agency furnishes leadership, coordination, and oversight. The primary agencies bring significant authorities, capabilities, roles, or resources to bear, but to a lesser extent than the coordinating agency. Supporting organizations, some of which are nongovernmental organizations, have specific capabilities or resources that complement those of the primary agencies. It should be noted that not all RSFs will be activated for all presidentially declared disasters; rather, decisions on RSF activation will be based on a post-disaster assessment of damage and needs. Existing pre-event recovery plans that delineate clear operational structures consistent with the NDRF, such as those of Fairfax County, Virginia, and Pinellas County, Florida, may be useful models (see Appendix C for links to these documents).
As the response period abates, emergency support functions will transition operations over to the RSFs, facilitating integration across disaster management phases. For example, responsibility for health and medical functions will transition from ESF #8 (Public Health and Medical Services) to the Health and Social Services RSF. Although there may be overlap in required expertise in the transition from response to early recovery, later recovery phases will necessitate the involvement of RSF representatives with different expertise, consistent with a transition from emergency functions to long-term reconstruction and community betterment activities. For example, transportation sector representatives supporting the Infrastructure Systems RSF should be those familiar with long-range transportation planning. For the health sector, the Health and Social Services RSF should include representatives working on an everyday basis to create healthier communities through community health improvement and social services activities. It is important to have clear plans in place for this transition and mechanisms for bringing in those trained in long-term community planning.
The NDRF also calls for three new leadership positions to monitor and coordinate disaster recovery through both the pre-disaster and the post-disaster period:
- A local disaster recovery manager who, among his/her many responsibilities, organizes the recovery planning process; ensures inclusiveness; develops and implements recovery progress measures; and communicates and coordinates with state, federal, and community stakeholders.
- A state disaster recovery coordinator leads statewide agencies by managing the recovery and by providing support for local initiatives. The state disaster recovery coordinator coordinates state, tribal, and federal funding streams; identifies gaps; and works collaboratively with recovery leadership at all levels to ensure a well-coordinated, timely, and well-executed recovery.
- A federal disaster recovery coordinator is responsible for facilitating recovery coordination and collaboration among all stakeholders. He/she monitors state and local decision making, evaluating the need for additional assistance. During the transition from response to recovery, coordination responsibilities will transition from the federal coordinating officer (who operates under the National Response Framework) to the federal disaster recovery coordinator.
The local disaster recovery manager, state disaster recovery coordinator, and federal disaster recovery coordinator facilitate vertical integration from the local to the federal level (FEMA, 2011c).
________________
11 Substate, regional organizations (e.g., Councils of Government, Metropolitan Planning Organizations, Regional Planning Commissions, Economic Development Districts) should also be considered in alignments with the federal NDRF structure since many states are organized into regional districts that are defined by a unified geography—established by state legislation—for diverse functions, both as regional entities with governing boards and as operating units of state agencies. These intergovernmental structures are key to organizing effective post-disaster community recovery. One example of a regional social service organization is an Area Agency on Aging. Such operations are often managed by Councils of Government or Regional Planning Commissions, offering a wide range of support services to senior citizens—who are often particularly vulnerable to the effects of disasters—including nutrition (Meals on Wheels, for example), transportation, and access to community programs.
BOX 3-3
Recovery Support Functions
Community Planning and Capacity Building
Coordinating Agency: DHS/FEMA
Primary Agencies: DHS/FEMA, HHS
The mission of this RSF is to promote and build recovery capacity and community planning resources for managing and implementing disaster recovery activities. This RSF assists States in developing pre- and post-disaster systems of support for local communities. This can be achieved in part by providing technical assistance and planning support to aid all levels of government to integrate sustainability principles—such as adaptive reuse of historic properties, mitigation considerations, smart growth principles, and sound land-use—into recovery decisions.
Economic
Coordinating Agency: DOC
Primary Agencies: DOC, DHS/FEMA, DOL, SBA, Treasury, USDA
Supporting Organizations include HHS
The mission of the Economic RSF is to help state, local, and community stakeholders to sustain and/or rebuild businesses and employment, as well as to develop economic opportunities that yield sustainable and economically resilient communities. This mission is achieved by leveraging federal resources, information, and leadership. The key is to encourage private investment and facilitate private sector lending and borrowing for restoring vital markets and economies.
Health and Social Services
Coordinating Agency: HHS
Primary Agencies: HHS, CNCS, DHS (FEMA, NPPD, CRCL), DOI, DOJ, DOL, ED, EPA, VA
Supporting Organizations: DOT, SBA, Treasury, USDA, VA, ARC, National VOAD
The mission of the Health and Social Services RSF is to help local-led recovery efforts in restoring public health, health care, and social services. The integration of these services promotes community resilience, health, independence, and well-being. (The term “health” subsumes public health, behavioral health, and medical services.) Among the many responsibilities of this RSF is to identify and coordinate with stakeholders an assessment of food, animal, water, and air conditions to ensure safety. Other responsibilities are to coordinate and leverage federal resources for health and social services, and to promote self-sufficiency and continuity of care of affected individuals, especially vulnerable populations. The NDRF envisions specific activities for the Health and Social Services RSF, including encouragement of behavioral health systems to meet the behavioral health needs of affected individuals, response and recovery workers, and the community; the reconnecting of displaced populations with essential health and social services; and the promotion of clear communications and public health messaging to provide accurate and accessible information that is available in multiple mediums, multi-lingual formats, alternative formats and is accessible to underserved populations.
Current limitations of the NDRF A comprehensive analysis of the challenges related to recovery and the utility of the NDRF for addressing them is beyond the scope of this report. Through its information gathering process, however, the committee noted several issues that will ultimately influence the effectiveness of the NDRF as a mechanism for integrating health into the recovery process and thus warrant discussion here.
First, although the NDRF promotes pre-event planning in principle, the framework is not accompanied by any funding to support such planning or capacity building for recovery. The reluctance of federal, state, and local governments to invest in these two critical functions in advance of a disaster has been described as one of the greatest barriers to achieving disaster resilience (Smith, 2011b). As discussed in Chapter 2,
Housing
Coordinating Agency: HUD
Primary Agencies: HUD, DHS/FEMA, DOJ, USDA
Supporting Organizations include HHS
The mission of the housing RSF is to facilitate delivery of federal resources to rehabilitate and reconstruct destroyed or damaged housing and to procure new, accessible permanent housing. This mission can be achieved in part by building accessibility, resilience, sustainability, and mitigation measures into housing recovery in as timely a manner as possible.
Infrastructure Systems
Coordinating Agency: DOD/USACE
Primary Agencies: DOD/USACE, DHS (FEMA and NPPD), DOE, DOT
Supporting Organizations include HHS
The mission of the Infrastructure RSF is to facilitate federal support to local, state, and tribal governments and other infrastructure owners and operators. The scope of this RSF includes energy, water, dams, communications, transportation systems, agriculture, government facilities, utilities, sanitation, engineering, and flood control. This RSF encourages rebuilding infrastructure in a manner that will reduce vulnerability to future disasters.
Natural and Cultural Resources
Coordinating Agency: DOI
Primary Agencies: DOI, DHS/FEMA, EPA
Supporting Organizations do not include HHS
The mission of this RSF is to channel federal assets and capabilities to assist state and local government and communities to address long-term environmental and cultural resource recovery. The key is to protect natural and cultural resources through recovery actions that preserve, conserve, rehabilitate, or restore them. This RSF works to leverage federal resources and available programs to meet local recovery needs.
___________________
NOTES: ARC = American Red Cross; CNCS = Corporation for National and Community Service; CRCL = Civil Rights and Civil Liberties; DHS = U.S. Department of Homeland Security; DOC = U.S. Department of Commerce; DOD = U.S. Department of Defense; DOE = U.S. Department of Energy; DOI = U.S. Department of the Interior; DOJ = U.S. Department of Justice; DOL = U.S. Department of Labor; DOT = U.S. Department of Transportation; ED = U.S. Department of Education; EPA = U.S. Environmental Protection Agency; FEMA = Federal Emergency Management Agency; HHS = U.S. Department of Health and Human Services; HUD = U.S. Department of Housing and Urban Development; NPPD = National Protection and Programs Directorate; SBA = U.S. Small Business Administration; USACE = U.S. Army Corps of Engineers; USDA = U.S. Department of Agriculture; VA = U.S. Department of Veterans Affairs; VOAD = Voluntary Organizations Active in Disaster.
SOURCE: FEMA, 2011d.
pre-disaster recovery planning is critical to seizing opportunities for health improvement during recovery. Further, lack of capacity can result in a protracted recovery process and associated negative health effects as community members languish under suboptimal living conditions and experience chronic, toxic stress.
Second, the committee noted incongruence of the NDRF with major federal funding sources that drive community planning at the state and local levels, both during steady-state times and after disasters. During steady state, grants and policies of the U.S. Department of Housing and Urban Development (HUD) and the U.S. Department of Transportation (DOT)—now collaborating along with the U.S. Environmental Protection Agency (EPA) under the banner of the Partnership for Sustainable Communities—are major drivers of urban and regional planning practices. As discussed in Chapter 2, the sustainability practices
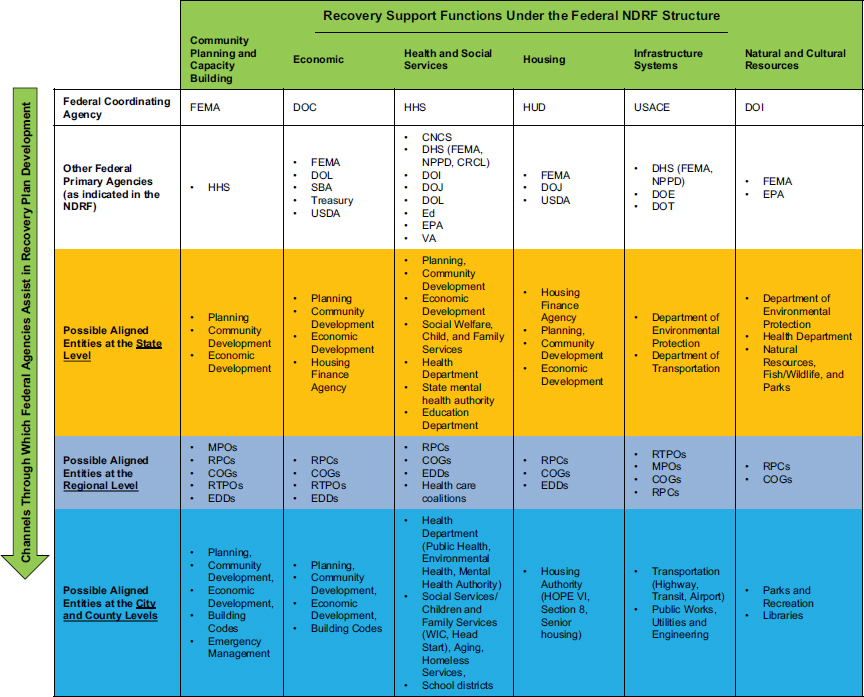
NOTES: Although the committee shows here an example in which state and local structures are identical to the federally defined recovery support functions, this need not be the case. Depicted here is a level between state and local—the regional planning level—which should also be considered in alignment with the federal NDRF structure.
CNCS = Corporation for National and Community Service; COG = Council of Governments; CRCL = Civil Rights and Civil Liberties; DHS = U.S. Department of Homeland Security; DOC = U.S. Department of Commerce; DOE = U.S. Department of Energy; DOI = U.S. Department of the Interior; DOJ = U.S. Department of Justice; DOL = U.S. Department of Labor; DOT = U.S. Department of Transportation; ED = U.S. Department of Education; EDD = economic development district; EPA = U.S. Environmental Protection Agency; FEMA = Federal Emergency Management Agency; HHS = U.S. Department of Health and Human Services; HUD = U.S. Department of Housing and Urban Development; MPO = metropolitan planning organization; NDRF = National Disaster Recovery Framework; NPPD = National Protection and Programs Directorate; RPC = regional planning commission; RTPO = regional transportation planning organization; SBA = U.S. Small Business Administration; USACE = U.S. Army Corps of Engineers; USDA = U.S. Department of Agriculture; VA = U.S. Department of Veterans Affairs; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children.
(e.g., affordable housing, transportation choices) promoted by the Partnership yield significant co-benefits in terms of health outcomes, and the committee sees great benefit to incorporating the Partnership’s livability principles (see Box 2-5 in Chapter 2) into recovery planning, as encouraged by HUD after Hurricane Sandy. Furthermore, HUD-funded community development (e.g., Community Development Block Grant) programs are a major element of community planning and have significant potential to impact the social determinants of health, but they appear to be unlinked to the NDRF structure. Neither HUD nor DOT is included even as a primary agency (both are listed as supporting organizations) for the Community Planning and Capacity Building RSF (FEMA is the coordinating agency).12 This appears inconsistent with the NDRF definition of primary agencies—those having “significant authorities, roles, resources or capabilities for a particular function within an RSF” (FEMA, 2011d, p. 39). Although HUD is the coordinating agency for the Housing RSF, that area of expertise is separate from the agency’s urban planning and community development role. Moreover, after a disaster HUD can have a significant influence on recovery planning at the state and local levels as a funding agency if Congress passes a supplemental appropriation through the HUD Community Development Block Grant for Disaster Recovery (CDBG-DR) vehicle (described in more detail in Chapter 4). After Hurricane Sandy, CDBG-DR funds to support recovery surpassed FEMA disaster relief funds (Donahue, 2014). It is not clear to the committee how CDBG-driven planning is integrated into the NDRF framework. Better incorporation of federal urban planning and community development expertise into the Community Planning and Capacity Building RSF could help address this apparent incongruence.
Finally, testimony provided to the committee revealed that the NDRF, released more than 3 years ago, has not yet been widely adopted and implemented at the state and local levels (Lockwood, 2014; Walsh and Schor, 2014). During a recent study on long-term recovery in which semi-structured interviews were used to collect data on training needs for community leaders in health-related functional roles, the National Center for Disaster Medicine and Public Health found that few respondents who had been actively involved in the recovery from Hurricane Sandy13 were familiar with the NDRF. Those who were familiar felt that its implementation had been problematic because of a lack of guidance, as well as conflicts with existing community recovery plans.14
Current limitations in integration of health into the NDRF The NDRF describes recovery as a continuum of coordinated processes, many concurrent, by which the community
- minimizes and overcomes the physical, emotional, and environmental impacts of a disaster;
- reestablishes an economic and social base that instills confidence in the community members and businesses regarding community viability;
- rebuilds by integrating the functional needs of all residents and reducing the community’s vulnerability to all hazards it faces; and
- demonstrates a capability to be prepared, responsive, and resilient in dealing with the consequences of disasters (FEMA, 2011d, p. 13).
This description clearly conveys the notion that community recovery is not just a “bricks and mortar” process of restoring physical infrastructure; rather, it entails the regeneration of all community systems, functions, and social structures in a way that addresses the full range of needs of the affected community members and ensures that the community has the capacity to meet its future needs. This represents a critical paradigm shift in the nation’s approach to disaster recovery, which has been criticized in the past
________________
13 The NDRF was released approximately 1 year before Hurricane Sandy.
14 Memorandum, K. Schor, Acting Director, National Center for Disaster Medicine and Public Health, to A. Downey, Institute of Medicine, May 28, 2014.
12 The committee did hear that a memorandum of agreement between FEMA and the U.S. Environmental Protection Agency is currently used as a mechanism to bring sustainability expertise into the recovery planning process when state and local partners express interest.
for its focus on physical infrastructure and lack of attention to meeting broader human recovery needs such as psychological and social well-being (Chandra and Acosta, 2010). Psychological and emotional recovery is among the core principles laid out in the NDRF, which acknowledges that community recovery is dependent on the recovery of individuals and families (FEMA, 2011d) and that health and social wellbeing are essential to recovery at all levels.
The committee was encouraged to see that Health and Social Services is one of the six RSFs in the NDRF, thus helping to institutionalize the role of health in recovery and to draw attention to the opportunities for improving population health and health systems beyond pre-disaster levels. As indicated in the description of responsibilities for this RSF given in Box 3-3, however, the Health and Social Services RSF is focused narrowly on restoration and delivery of public health, medical, behavioral health, and social services. Although these are unarguably functions critical to protecting and promoting short- and long-term health, they do not capture the full spectrum of factors that affect health within a community or the pathways to health discussed in this and the previous chapter (e.g., collaborations with nonhealth sectors such as urban planning and community development). Since the activities of all sectors will impact health during recovery, either positively or negatively, it is critical that health not be siloed but integrated with all other recovery functions, which should operate cohesively through a systems approach.
Table 3-2, although not comprehensive, illustrates how the activities of the other five RSFs have health implications. As shown in this table, HHS is associated with nearly all of these other RSFs, providing a mechanism for approaching health during recovery in a more holistic way, if RSFs are operationalized with this intent. Making HHS a supporting organization for the Natural and Cultural Resources RSF as well might better enable HHS and its component agencies to infuse health across the full spectrum of RSFs and promote a broader vision for the role of health in recovery. Although the Office of the Assistant Secretary for Preparedness and Response provides the coordinating function for the Health and Social Services RSF on behalf of the HHS Secretary, greater involvement of other HHS agencies and most notably the CDC, which is a major funder of both community health improvement and community resilience building efforts, might facilitate a healthy community approach to recovery. The CDC supports diverse community development planning initiatives with co-benefits for population health, such as transit-oriented development; programming of parks, open spaces, and trails; and nutrition strategies aimed at overcoming food deserts. The CDC is a policy leader in such initiatives nationally, taking a science-based approach to health disparities and low health status in many populations.
Building on a Foundation of Existing Organizational Structures and Initiatives
The path by which a community undertakes the long and complex process of recovery is dependent on the characteristics of the disaster—the type of event (e.g., tornado, flood) and the scale (amount) and pattern of damage (features of the community that were damaged)—as well as the prevailing organizational and governance structures utilized by elected and public officials. Consequently, decisions on how to structure recovery planning after a disaster must be locally driven, taking into consideration the different needs for local and regional events (see Box 3-4). The choices facing community leaders at the beginning of the recovery planning process are not about the content of the recovery plan; they are about assembling the resources (including human capital) and agendas for the work ahead. Because institutions often work in some degree of isolation, community leaders sometimes are unaware of the key stakeholders that should be integrated into the recovery planning process. The task after a disaster is to ensure that prior collaborations are added to the list of organizational assets and then to incorporate those personnel and groups into the recovery planning effort. As discussed earlier in this chapter, the committee observed that the dimensions of health and social services are not adequately integrated into disaster recovery planning, particularly in the long-term phase. More intentional efforts are needed to integrate health considerations into recovery planning and decision making.
All communities have in place structures and processes for strategic decision making regarding investments that will be made and projects that will be prioritized. As discussed in Chapter 2, strategies often
TABLE 3-2 Health Implications of Nonhealth Recovery Support Functions
| Recovery Support Function | HHS Association | Example Health Implications |
| Community Planning and Capacity Building | Primary agency | Community design influences physical activity, risk of injury, exposure to toxins, and access to goods (e.g., healthy food) and services (e.g., health care) essential to health. Community redevelopment investments can have significant impacts on social determinants of health. |
| Economic | Supporting organization | Social and economic factors (e.g., poverty) are among the greatest influences on health outcomes. Job training initiatives are complementary to other community development approaches that address social determinants of health. |
| Housing | Supporting organization | The quality of the indoor and outdoor housing environments affects health. Affordability of housing is a social determinant of health. |
| Infrastructure Systems | Supporting organization | Lifeline utilities such as water treatment and power systems are essential to health and hygiene. Transportation systems ensure access to goods (e.g., healthy food) and services (e.g., health care) essential to health. |
| Natural and Cultural Resources | None | Healthy environments and ecosystems are essential to healthy populations. Parks, trails, and other natural resources provide opportunities for recreation and physical activity. |
NOTE: HHS = U.S. Department of Health and Human Services.
are sought that use complementary investments to achieve synergies, reduce costs, and meet multiple objectives, thus maximizing benefits. Multisector approaches to strategic planning also reduce inefficiencies arising from duplication of effort. These mechanisms for everyday problem solving are well suited to envisioning recovery strategies, and collective priority setting for everyday problems equips a community with the systematic analysis and decision processes needed to address the complexities of a new set of physical, social, and economic problems in neighborhoods after a disaster. Although changes are made to decision-making structures within a community during the response phase of a disaster to enable decisive action that will save lives and protect property, the recovery phase sees a return to long-standing strategic planning processes used to prioritize investments. Most communities, for example, have ongoing community development initiatives designed to address the social and economic problems that degrade health and contribute to social vulnerability to disasters (although improved health may not always be an explicit goal of such efforts). Because of the complexity of these challenges, such initiatives are of necessity multisectoral in nature. Community development15 initiatives to meet the needs of low-income community members and address such issues as blight often utilize collaborative strategies involving charitable, nonprofit, and faith-based groups (the United Way, for example, often participates in local community development collaboratives). Leveraging local community development institutions during disaster recovery will have the effect of improving health outcomes. Given the magnitude of health disparities related to social equity issues, the potential health benefits of integrated approaches to place-based strategies for
________________
15 Community development is a category of planning and service delivery funded largely by HUD that supports the development of “stronger and more resilient communities through an ongoing process of identifying and addressing needs, assets, and priority investments” (HUD, 2014).
BOX 3-4
Recovery Planning on a Regional Scale
When people convene to conduct community disaster recovery planning, their perspective typically is drawn to the community in which they live or perhaps the community they serve. That makes sense, as most disasters are local. However, it is important to recognize that regional and national disasters also occur, some would say with increasing frequency. Experience shows that disaster recovery is different when entire regions are impacted, and the approach that communities take to community disaster recovery planning must differ accordingly.
Regional and local events differ in many ways. First, the expanded scale and scope of a regional disaster serve to magnify known deficiencies in the capacity and capabilities of public health, medical, and social service systems and may expose new challenges. Second, regional disasters encompass a multitude of jurisdictions, each with its own set of laws, regulations, policies, and norms. These differences complicate disaster recovery planning and recovery processes. Third, while disasters expose the disproportionate vulnerability of certain segments of a community, regional disasters demonstrate that these disproportionate vulnerabilities are not distributed proportionally: some communities are more vulnerable and are impacted more severely than others.
While regional disasters can be characterized by many more differences, those cited above are sufficient to support the need for a different approach to the management of regional recovery operations. First, the best-informed decisions come from decision makers who are best informed. That dictum, although obvious, points to the recurrent challenges of ensuring that federal, state, and local officials have access to the necessary channels of health-related information and are able to prioritize, implement, and adjust as needed. Second, the multitude of jurisdictions involved in a regional disaster brings a wider array of players, perspectives, and priorities, all of which need to be incorporated into the decision-making process and harmonized around an integrated strategy and inclusive set of objectives. And third, disasters that span an entire region also are likely to cross political boundaries that may well bring an intensity of interest and beneficial level of visibility.
Community leaders will want to be mindful of the possibility of a region-wide disaster as they develop their vision for improving health outcomes in a post-disaster environment, assess the comprehensiveness of their social networks, and conduct disaster recovery planning. The National Disaster Recovery Framework and its Recovery Support Functions (RSFs) (detailed in Box 3-3) were designed in part to assist communities in planning for just this type of scenario. The inclusion of every federal agency with a role in disaster recovery within the RSF structure provides a channel for their involvement in coordinating the grant processes and funding streams that will be needed to improve health outcomes after a disaster. The linkages among the Federal Emergency Management Agency, the U.S. Department of Health and Human Services, the U.S. Department of Housing and Urban Development, and other departments and agencies and their routine engagement with state and local public health officials can form the foundation for community awareness and set the stage for the collaboration and cooperation that are essential to full-scale recovery at a regional scale.
addressing employment, education, crime prevention, sustainability, and revitalization during post-disaster recovery could be substantial. Vulnerability to disasters also tends to coincide with the same socioeconomic indicators that relate to both populations and at-risk geographic areas.
Intersectoral collaboration to support Health in All Policies depends not only on a shared vision and goals but also on relationships built on trust (Rudolph et al., 2013). As highlighted in the Health in All Policies case study from Galveston, Texas, discussed in Chapter 2 (see Box 2-11), there are significant benefits to developing these relationships in advance of a disaster. According to Dr. Alexandra Nolen, former director of the Center to Eliminate Health Disparities—the organization championing the Health
in All Policies approach in Galveston—it took 5 years after the 2008 hurricane to reach the early stages of cross-sector collaboration because no such relationships were in place before the hurricane struck (Nolen, 2014). Thus, a community that is working across sectors to achieve improved population health during steady-state times is inherently better suited to recovering from a disaster. The organizational structures and participatory mechanisms used for health improvement during steady-state times can be leveraged after a disaster in developing a recovery strategy and determining priorities. Importantly, though, the benefits of improved organizational arrangements for community problem solving will accrue to the community during times other than disasters.
Organizational approaches such as those in Thurston County, Washington; Washtenaw County, Michigan; and King County, Washington (see Chapter 2) appear to hold promise for supporting Health in All Policies during both disaster recovery and steady-state times. Nonetheless, the committee believes additional research is needed to determine the comparative efficacy of alternative organizational structures for recovery operations. Pilot or demonstration projects could help elucidate best practices for organizational arrangements that could then be incentivized through federal grant funds. The committee is hopeful that such efforts would yield a road map that communities could use in developing disaster recovery arrangements among local institutions under the overarching structure of the NDRF to achieve improved post-disaster health outcomes. What is needed is not a one-dimensional hierarchy but a sophisticated set of participatory mechanisms customized to work in the context of the unique arrangements of a community’s pre-disaster agencies and work programs and its policy, technical, operational, and database assets.
Engaging the Whole Community in Recovery Planning
Successful recovery and the post-disaster rebuilding of healthier and more sustainable and resilient communities require the coordinated efforts of an extremely broad, multidisciplinary group of stakeholders (i.e., a whole-community approach). Yet many of these stakeholders are not accustomed to working in the emergency management context and are not familiar with the salient processes, terminology, or resources. Following an extensive review of the federal grey literature related to recovery and hearing testimony from experts at the federal, state, and local levels, the committee was concerned about how difficult it is for key stakeholders outside (and even within) the emergency management field to understand the relationships among the array of federal, state, and local resources that must be mobilized after a disaster; how they interrelate; and who is accountable at each level. The committee found no single federal-level document that provides a clear overarching review of the interconnections among the key legislation, directives, national-level strategies, and frameworks relevant to recovery—one designed to be understood by those outside the emergency management field and describing processes by which stakeholders can engage in the recovery planning process—both before and after a disaster—and leverage recovery resources.
Further, the committee noted inconsistencies among existing federal documents. For example, FEMA’s 2014 Overview of the National Planning Frameworks describes the eight core capabilities in the NDRF as Planning, Public Information and Warning, Operational Coordination, Economic Recovery, Health and Social Services, Housing, Infrastructure Systems, and Natural and Cultural Resources (FEMA, 2014c, p. 7). The NDRF itself makes no mention of core capabilities but describes the six RSFs discussed earlier: Community Planning and Capacity Building, Economic, Health and Social Services, Housing, Infrastructure Systems, and Natural and Cultural Resources (see Box 3-3). The overabundance of federal documents pertaining to the National Preparedness System (of which recovery is a core mission area) and the inconsistencies among them is confusing and intimidating to those not familiar with the emergency management field. Ambiguous terminology—for example, “planning,” which may refer generally to an operational process of coordinating efforts or alternatively to a process by which land use/community design decisions are made—adds further confusion.
To better support a whole-community approach to recovery, the committee has attempted to provide a cogent, high-level description of the processes and resources pertinent to disaster recovery (see Chapter
4 and Appendix A), drawing on a number of federal and nonfederal materials. These materials include but are not limited to
- National Preparedness Goal (FEMA, 2011e),
- National Preparedness System (FEMA, 2011f),
- Overview of the National Planning Frameworks (FEMA, 2014c),
- National Response Framework (FEMA, 2013c),
- National Disaster Recovery Framework (FEMA, 2011d),
- National Health Security Strategy (HHS, 2009, 2015),
- Robert T. Stafford Disaster Relief and Emergency Assistance Act,16
- Post-Katrina Emergency Reform Act of 2006,17
- Sandy Recovery Improvement Act of 2013,18 and
- Pandemic and All-Hazards Preparedness Act.19
In the face of such complexity, communities often need to hire outside professional consultants to navigate the disaster recovery process. The committee concludes that the federal government needs to make information on federal recovery policy and resources (and the process by which they are mobilized) available in a more accessible and coherent manner to facilitate maximum involvement by all stakeholders. Further, those leading recovery planning need to be sensitized to and trained on the importance of engaging all relevant stakeholder groups through robust outreach efforts. Key stakeholders themselves need to be educated on the importance of their participation and mechanisms by which they should engage proactively in the process.
The Role of Leadership
The effective governance of recovery from a disaster requires strong leadership that harnesses the actions of a broad array of agencies from multiple levels of government, along with the nonprofit and private sectors, to address highly complex and interrelated challenges using an integrated multidisciplinary approach. Several emerging approaches to leadership have particular relevance to the disaster recovery context:
- Meta-leadership is an approach to leadership focused specifically on breaking down organizational silos and fostering a spirit of cooperation that motivates people to work together (Marcus et al., 2006). Core to the concept of meta-leadership is the ability to lead by influence, since engaging organizations outside of one’s silo necessarily means reaching beyond lines of authority. This ability is particularly crucial during recovery, which has been characterized as “nearly the opposite of command and control” (City of Seattle, 2013, p. 5). A model meta-leadership program was developed by the National Preparedness Leadership Initiative, a joint venture of the Harvard School of Public Health’s Division of Policy Translation and Leadership Development and the Harvard Kennedy School’s Center for Public Leadership, to build heightened capacity for effective cross-agency coordination of effort through education and training (NPLI, 2013).
- Distributive leadership is based on the premise that diffusion of responsibility and authority is needed in situations where a centralized command and control approach cannot adequately meet complex decision-making needs. After a disaster, distributive leadership enables rapid response to changing conditions on the ground through locally informed decisions. “With distributive
________________
16 42 U.S.C. § 5121 et seq.
17 Post-Katrina Emergency Management Reform Act of 2006, 109th Cong., S.3721 (October 4, 2006).
18 Sandy Recovery Improvement Act of 2013, Public Law 113-2, 113th Cong., H.R.152 (January 29, 2014).
19 Pandemic and All-Hazards Preparedness Act, Public Law 109-417, 109th Cong., S.3678 (December 19, 2006).
leadership, there is a shift from reliance on systems and procedures to an increased capacity to adapt, to change, learn, and innovate” (Usdin, 2014, p.159).
Engaging the Public in a Participatory Planning Process
As discussed earlier in this chapter, community engagement does not end with visioning: the community should be an active participant in every aspect of the recovery process, including the development and implementation of plans. This participation is critical to ensuring that recovery decisions align with the community’s vision and that community values are respected in decisions about contested issues. Such conversations may center on short-term issues such as priority setting for access to scarce health resources (IOM, 2012) but also should encompass controversial long-term decisions such as buyouts through eminent domain.
Using an inclusive process that leverages existing community organizations and social networks builds trust, ensures that local needs will be met, and creates a sense of ownership, thereby increasing the likelihood of success (see Box 3-5 for how this was accomplished in Kobe, Japan, after a devastating earthquake). After a disaster, the active engagement of the community in the recovery planning process also promotes healing and strengthens resilience. When the community gathers together to plan and implement a recovery strategy, ties among residents are strengthened, thereby building social networks and empowering residents. Thus, organizational structures for recovery planning must enable bidirectional communication between the community and decision makers. Mechanisms to this end can include (1) partnerships between local government and community organizations and (2) official advisory bodies that act as a link between the community and decision makers and represent the voices and needs of the affected population.
Community partnerships A partnership between local government and community organizations can help foster the collaborative spirit and sense of community ownership that, while not always easily measured, can aid in building community resilience. Partnering with organizations that are already linked to the community can be an essential tool for local governments, helping them communicate with and assist difficult-to-reach populations. Community organizations often play a major role in recovery because of gaps in government-provided services. After Hurricane Sandy struck New York City, for example, many
BOX 3-5
Leveraging Social Networks After Disasters
Encouraging or even requiring the solicitation of input from neighborhood-level organizations (e.g., homeowners associations) in a community requiring significant redevelopment after a disaster can help ensure that the people most affected by recovery plans are included in their development. After the 1995 earthquake in Kobe, Japan, neighborhood associations organized into councils (called Machizukuri) that in many cases were recognized by city ordinance. These councils not only provided support to the community (e.g., finding temporary housing, coordinating food distribution, and providing updated information through newsletters) but also were actively engaged in the formulation of neighborhood redevelopment plans (Edgington, 2011). The councils served to balance what had initially begun as a top-down process. Social capital also was strengthened as participants in the council became more civically engaged. Residents in Kobe communities that engaged in this bottom-up planning process that sought to harness citizens’ visions for their neighborhoods reported higher satisfaction with the overall process than those with more top-down approaches (Aldrich, 2012; Nakagawa and Shaw, 2004).
residents found relief and assistance in community centers, tenant associations, or faith-based organizations. A survey of public housing residents in New York found that 59 percent accessed such assistance. These organizations have deep and long-standing ties with the community, and when government was slow to respond to residents’ needs, they stepped in. However, they did not have the expertise, resources, or capacity to fully meet the needs of the storm-struck residents and were not coordinated with government services. Since Hurricane Sandy, the New York City Housing Authority has proposed partnerships with these community organizations and has suggested using community centers as hubs for communication, counseling, and coordination of volunteers and supplies (The Alliance for a Just Rebuilding et al., 2014).
Advisory bodies Some jurisdictions have opted to create official bodies to engage with the community and obtain input on the recovery process. These bodies act as a link between the community and decision makers, and they should represent the full geographic, cultural, and economic diversity of the community to ensure that the voices and needs of all the affected population are heard. After severe weather caused major flooding in Iowa in 2008, for example, the governor established the Rebuild Iowa Advisory Commission (RIAC), a 15-member independent advisory body made up of a cross-section of Iowans. The RIAC traveled to affected areas of the state, holding town meetings and talking to residents to gain insight into their immediate- and long-term needs, and then developed recommendations for recovery and provided strategic direction to recovery decision makers. The RIAC proved to be an invaluable tool for focusing the recovery effort on the needs of residents and giving Iowans a channel for their feedback on the recovery process (Rebuild Iowa Office, 2011).
Using Health-Related Information to Inform Recovery Decision Making
Organizational structures such as those discussed earlier in this chapter provide essential scaffolding for decision-making processes but by themselves are not sufficient. The effectiveness of an integrated planning and recovery approach is greatly enhanced by shared information. One of the greatest challenges associated with disaster recovery is that decision makers often must take action before the information needed to support those decisions can arrive (Olshansky, 2014). Planning processes that may in normal times have been spaced out over a period of years must now be conducted in a timeframe of just months. Moreover, as discussed in the section on leadership above, decision making is distributed during disaster recovery, creating challenges related to coordination of actions. Recovery proceeds more effectively when the myriad actors involved are aware of each other’s actions. Thus, accelerating and broadening the flow of information is crucial to success (Johnson and Olshansky, 2013).
Several kinds of information can be used to support the incorporation of health considerations into the recovery decision-making process to improve health outcomes after a disaster. These include (1) knowledge of the potential health impacts of alternative decisions; (2) knowledge gained from past disaster experiences and in particular, effective (and ineffective) practices; (3) knowledge of available resources; and (4) up-to-date information on the recovery environment (i.e., status). Reliable sources of each of these kinds of information should be identified in advance of a disaster as part of pre-event planning. Sources of such information include
- health impact assessments;
- guidance, training, and technical assistance; and
- information systems, including health information systems.
Each is discussed further in the sections below.
Health Impact Assessments
Health impact assessment (HIA) is a process by which scientific data, professional expertise, and stakeholder input are used to determine the positive and negative public health impacts of a policy, project, plan, or program under consideration20 (NRC, 2011). HIAs can be used to generate recommendations on how to increase positive benefits and minimize negative impacts to health. According to Health Impact Project21 data, hundreds of HIAs either have been completed or are in progress in the United States spanning the federal, state, and local levels and covering diverse topics, including transportation, land use, agriculture, education, energy, and natural resources. HIAs are one of the key assets that public health professionals can contribute to community strategic planning by providing data and analytical skills to inform the prioritization of planning policies and to aid in the development of benchmarks for success (Ricklin et al., 2012).
HIAs can be performed on local, state, or federal policies or regulations, and they can be performed by governments, think tanks, academic institutions, nonprofits, or community organizations. The major steps in performing an HIA include screening (determining plans, projects, or policies for which an HIA would be useful); scoping (identifying which health effects to consider); assessing benefits and risks; developing recommendations; reporting; and monitoring and evaluating to determine the effect of the HIA on policy (CDC, 2015).
HIAs enable health professionals to raise awareness of the impact of recovery decisions on health outcomes. Box 3-6 describes how HIA is being used to inform recovery decision making in New Jersey as communities continue rebuilding after the effects of Hurricane Sandy. This tool can potentially be used in prioritizing different recovery initiatives for effective allocation of scarce resources so as to optimize long-term health outcomes. However, additional guidance on using HIA in the disaster recovery context is needed.
Although HIA has gained traction only recently as an important decision-making tool, a model for this kind of impact assessment has been in place in communities for decades. Under the National Environmental Policy Act22 (NEPA), all development projects funded with federal dollars must undergo a data-driven process of analysis with explicit consideration of alternatives and their respective degrees of environmental impact. As a result of NEPA compliance, this process of analysis of alternatives is well understood and accepted at the municipal level, paving the way for adoption of a similar technique for evaluating impacts on human health.
Guidance, Training, and Technical Assistance
Guidance As discussed earlier, the NDRF supports the idea that recovery goes beyond restoration of a community’s physical infrastructure and emphasizes the equal importance of providing adequate care to address the full range of needs of the affected community members and ensuring that the community has the capacity to meet its future needs. However, little guidance is available to support communities in the development of a strategy for restoring and ultimately improving their physical, mental, emotional, and social well-being. As guidance for each of the NDRF RSFs is developed, it will need to include health considerations for the recovery activities of that RSF. Guidance in Chapters 5-10 of this report may inform the development of such guidance initially but updates should reflect ongoing efforts to collect best practices.
For the health sector, it will be important to align current guidance for federal funding programs
________________
20 An HIA is distinct from a community health assessment (discussed earlier in this chapter). Whereas HIA is a process for determining health impacts of a policy, project, plan, or program, community health assessment is a process by which health status indicators for a given population are examined to identify key health problems and assets in a community.
21 The Health Impact Project, a collaborative effort of the Pew Charitable Trust and the Robert Wood Johnson Foundation, is promoting the use of HIAs as decision-making tools for policy makers. Information on completed and in-progress HIAs can be found at http://www.pewtrusts.org/en/multimedia/data-visualizations/2014/hia-in-the-united-states (accessed February 23, 2015).
22 National Environmental Policy Act of 1969, Public Law 91-190 (January 1, 1970).
BOX 3-6
Integrating Health Impact Assessment into Recovery
Decision Making and Planning
New Jersey’s Rutgers University is leading a project that will utilize health impact assessments (HIAs) to inform disaster decision making and recovery in the aftermath of Hurricane Sandy. Funding for this project, which began in September 2014 and will continue through February 2016, comes from the Health Impact Project, a collaboration of the Robert Wood Johnson Foundation and the Pew Charitable Trusts (Rutgers, 2014). HIA utilizes scientific data, health expertise, and public input to incorporate health considerations into decision making, providing a tool for predicting the frequently overlooked health impacts that may arise from decisions not typically considered related to health. As part of this project, Rutgers will conduct an HIA in two communities—Little Egg Harbor in Ocean County and Hoboken in Hudson County. Additionally, the project will generate a toolkit for use by other municipalities in New Jersey in integrating HIA into their decision making, as well as recommendations on integrating HIA into post-disaster decision making and planning more broadly in the United States (Rutgers, 2014).
In Little Egg Harbor, the HIA will provide officials with information on the potential health outcomes of a decision on whether to support a voluntary buyout strategy for properties in a flood-prone neighborhood. While many residents have responded favorably to the offer of a buyout, some officials remain concerned about the potential loss of tax revenue and the impact on the local economy. The HIA will aid in determining the physical and mental health outcomes associated with a variety of voluntary buyout scenarios (ranging from no buyout to full buyout of the area in question, as originally proposed). In particular, it will address how the program would affect vulnerable populations, household finances, social cohesion, and the municipal budget. It also will address how the buyout program would change the future risks of flooding damage and how the new open space created by buying out these homes would affect the health of the community (Lowrie, 2014).
The HIA in Hoboken is focused on a stormwater management plan for addressing chronic flooding. This HIA will provide information on health impact considerations currently absent from the consulting work and deliberations already under way regarding adoption of a stormwater management plan and ordinance. Persistent flooding and sewer system overflow are serious hazards in Hoboken, as are the resulting health risks. The HIA will focus on these problems to inform Hoboken’s City Council about the health risks of flooding and the resulting sewage overflow events, as well as the potential health benefits and risks of implementing green infrastructure solutions as part of the stormwater management plan (Carnegie, 2015).
that support the development of a health recovery capability—specifically, the Public Health Emergency Preparedness (PHEP) Cooperative Agreement and the Hospital Preparedness Program (HPP) (discussed in more detail in Chapters 5 and 6, respectively)—with the RSF-specific guidance so that cooperative agreement funds are used effectively. PHEP and HPP represent important opportunities to support incorporation of broad health considerations into an integrated recovery approach. Currently, however, there is a paucity of PHEP and HPP guidance specific to recovery. PHEP guidance, for example, addresses public health, medical, and behavioral health systems all together, with no specifics provided for any of these services. Additionally, although there is some emphasis on utilizing recovery actions to mitigate damage from future events, completely absent from current guidance is any messaging regarding the opportunities to use recovery as a vehicle for creating healthier communities or the need to create a healthy community vision to guide long-term recovery efforts—both of which need to be key messages of RSF-specific as well as PHEP/HPP guidance.
Training Outside of the disaster recovery context, there is increasing awareness of the importance of collaboration among public health, human services, and community planning stakeholders (including transportation and the community development enterprise) to support a coordinated approach for achieving healthy community goals, avoiding duplication of effort, and leveraging synergies among the missions of diverse community organizations. These kinds of connections function outside of the emergency management context and therefore may not be leveraged during recovery planning and implementation. All stakeholders with a role in recovery, and particularly elected and public officials who lead such efforts, need to be sensitized regarding the importance not only of short-term health protection concerns but also of long-term opportunities to create healthier and more resilient and sustainable communities. Training programs need to be developed for this purpose.
Given the need for intra- as well as intersectoral collaboration to support effective disaster recovery and a Health in All Policies approach, cross-training programs are needed to break down silos within sectors, including the health sector. As discussed earlier in this chapter, a healthy community approach to disaster recovery requires that public health professionals with an understanding of the key principles behind healthy communities be engaged in the recovery planning process. Although the public health sector increasingly is being engaged across the full continuum of the emergency management cycle, its representatives generally are those working in the field of public health emergency preparedness. Throughout its information gathering, the committee noted a divide between the public health professionals working in emergency preparedness and in the area of healthy communities (this separation of disciplines was not specific to public health but also was observed within the public management and planning fields). This siloing within public health is due in part to the structure of funding streams (PHII and NACCHO, 2008). In the past 50 years, conditions attached to the receipt of federal funds have institutionalized and reinforced siloing (Turnock and Atchison, 2002), and preparedness planning often is isolated from the expertise and input of other divisions within health departments (Duncan et al., 2007). Because of this siloing across the public health enterprise, public health emergency preparedness personnel may understand short-term health challenges relevant to the response and early recovery phases but not the opportunities for long-term population health improvement after a disaster. Cross-training is a means of bridging this divide so that both groups of professionals have a better understanding of each other’s roles in the recovery process and can leverage relationships within their agencies to bring the appropriate public health expertise to bear on strategic planning discussions.
Technical assistance Technical assistance can come from peer organizations that have previously undergone the process of disaster recovery or from state and federal partners (e.g., through ESF and RSF coordinating agencies). Even when there is no major disaster declaration, federal experts at regional- and national-level offices can provide targeted technical assistance to grantees through existing programmatic channels upon request. Technical assistance can be used to
- inform grantees about how to leverage existing programs, including repurposing of current grants;
- educate about waivers and flexibilities;
- disseminate information on best and promising practices;
- connect decision makers with leaders from other localities that have recovered from a disaster; and
- educate on how to meet the needs of specific populations.
Of interest to this committee is a recent (2010) memorandum of agreement (MOA) between FEMA and EPA. This MOA provides a pathway for EPA’s Office of Sustainable Communities to provide technical assistance to disaster-impacted communities on rebuilding in ways that protect the environment, reduce vulnerability, strengthen neighborhoods, support long-term economic vitality, and improve quality of life (DHS and EPA, 2010). After an F-5 tornado devastated the town of Joplin, Missouri, in 2012, for example, EPA provided technical assistance on the creation of a “multi-modal transportation corridor that would meet the need for more walkable, bikeable streets and also manage stormwater in a more environmentally
friendly manner” (EPA, 2014). Prior to initiating the project, FEMA helped local stakeholders identify long-term community recovery needs and then assisted EPA in matching its sustainable community assistance capabilities with those identified needs. This MOA serves as a model and a point of departure for a broader interagency effort to better coordinate federal assistance to local communities and help them use the post-disaster recovery process as an opportunity to rebuild healthier and more resilient and sustainable communities (DHS and EPA, 2010).
Information Systems, Including Health Information Systems
Recovery decision makers require frequently updated data to maintain situational awareness. This capability requires an investment in infrastructure (including mapping software and expertise) to support the acquisition, synthesis, and distribution of data at multiple scales (the city/county and neighborhood levels being most critical). However, this responsibility need not be carried out directly by government agencies. Those agencies, which often are hampered by the constraints of bureaucracy, also can leverage the assets and agility of nongovernmental organizations that often emerge to fill gaps related to coordination and information. After Hurricane Katrina, for example, the Greater New Orleans Community Data Center, now called The Data Center, a nongovernmental organization supported with philanthropic funds, provided critical and timely data to support recovery decision making across a number of fields and was valued for its independence and transparency (Plyer and Ortiz, 2011). Uses for recovery data such as those supplied by The Data Center include but are not limited to
- informing redevelopment decisions;
- justifying requests for funding;
- targeting services to areas of greatest need;
- providing updates to the public and institutional stakeholders; and
- supporting collaborations (e.g., coordination of services based on measured needs).
With regard to health-related data, in most cases, state, local, tribal, and territorial health departments will be primary resources for informing health sector and nonhealth sector decision makers. To this end, health departments can draw on vital statistics and health records, although nongovernmental organizations, including academic institutions, may help combine these data with other indicators to create a more comprehensive picture of community well-being (relevant data would include crime rates, median household income, and adequacy of affordable housing). Having preestablished systems in place for data aggregation and distribution (e.g., responding to data requests) increases the community’s ability to recover quickly and effectively, thus increasing its resilience (Plyer and Ortiz, 2011). Formal data-sharing agreements may be an important part of that infrastructure, with special attention to privacy protections as appropriate (DeSalvo et al., 2014). Ideally, such arrangements would be established before a disaster.
Seeking and Applying Recovery Resources
Developing a comprehensive financial strategy is an important component of the recovery planning process. This strategy should consider a community’s needs, known sources of recovery resources, and any potential gaps in funding (APA, 2014). It should be guided by the vision for a community’s recovery and, through the consideration of short- and long-term needs, serve as a road map by which recovery resources can be applied to restore—and, where possible, improve beyond pre-disaster levels—the community’s infrastructure, services, economy, and health. The process of distributing and applying recovery resources is complex, and it requires that a community best match the available resources to its needs. Furthermore, to obtain and implement these resources effectively requires a thorough understanding of
the varied sources of funding available, along with the requirements and restrictions associated with each (APA, 2014).
The committee identified a paucity of disaster recovery resources specifically targeted for health protection and promotion. In the case of a major disaster, funding may be available for short-term behavioral health support and for the repair of critical health care infrastructure. In addition, a supplemental appropriation can potentially generate funds for specific social services needs. Largely, though, recovery resources are allocated predominantly to other sectors and services. However, the activities of other sectors can be leveraged in ways that have a positive effect on health outcomes. It is here that health sector stakeholders need to have preestablished relationships with other agencies to ensure integration and coordination of resource allocation to support long-term health, resilience, and sustainability. The use of recovery resources by all sectors represents an opportunity to consider health impacts and to develop complementary strategies whereby these funds can be used to achieve multiple goals, one of which is improved health. Recovery assistance programs and their potential applications for health benefits are discussed in more detail in Chapter 4.
Disasters are relatively rare occurrences, and the success of recovery is based on community context. As a result, the evidence base for interventions is often imperfect, and scientific knowledge is only one of multiple factors that influence decision making during recovery. However, uncertainty cannot deter those responsible for making decisions that will drive the recovery process forward. Leaders must be prepared to act using the best information available and to change course as new information emerges. Consequently, decision-making frameworks need to be built on a learning system approach whereby new knowledge is captured as strategies are implemented and is fed back into the decision-making process to support continuous improvement.
Communities are complex adaptive systems, and an adaptive management approach to disaster recovery is therefore warranted. Adaptive management is an approach that allows community leaders and members to explore alternative ways of achieving disaster recovery objectives, identify potential outcomes, implement one or more methods, and monitor their impacts on the recovery process so that course corrections can be made in the process of iterative decision making. Continuous evaluation of progress toward recovery goals is thus an integral part of the process that needs to be incorporated into pre-event plans so that its results can be used to adjust future recovery management strategies. Evaluation can occur at multiple scales, including the individual organization, sector, and community levels (e.g., through a composite recovery indicator). This learning-based approach to decision making links learning with policy and implementation over time, providing a framework that enables policy planners to make good decisions in the face of uncertainty as outcomes from previous disaster recovery actions become better understood.
An important component of a learning system approach is metrics with which to evaluate progress toward identified goals (i.e., success as locally defined) and to inform strategy adjustments. Defined metrics also are needed to collect relevant baseline information, such as measures of health for a community, to enable comparison with pre-disaster states. The absence of core metrics with which to measure the progress of recovery is a major gap with which communities currently struggle (Chandra, 2014). The committee was not charged with the development of recovery metrics and thus did not undertake to propose a core set. However, the committee notes that several research institutions, including RAND Corporation and the University of North Carolina’s Natural Hazards Center, are evaluating recovery and community resilience metrics that, if validated, could be incorporated into future iterations of the NDRF. National-level rollout of a core data set would facilitate not only community-level evaluations but also comparison across disasters.
Evaluation of recovery efforts also requires a preestablished methodology. Although a methodology designed specifically to evaluate the impact of recovery efforts on community health status does not yet exist and further research in this area is needed, examples of existing measures and assessment tools that may help evaluators establish a methodology include
- community health rankings and associated measures such as those provided in America’s Health Rankings® annual report (United Health Foundation et al., 2014) and the Robert Wood Johnson Foundation’s County Health Rankings (2015);
- the Sustainable Communities Index, a set of methods for measuring environmental, economic, and social conditions of cities and neighborhoods (previously adapted to measure conditions during disaster recovery; see Appendix D);
- HUD’s Healthy Communities Index and Healthy Communities Assessment Tool (being developed to help local communities assess the physical, social, and economic roots of community health and use this assessment to inform evidence-based policies, planning, and development);
- AARP’s Livability Index (a Web-based tool in development that scores communities on measures of livability as identified by U.S. residents over age 50);
- the Social Vulnerability Index, used to identify and map risks for geographic clusters of socially vulnerable populations; and
- the National Health Security Preparedness Index™, a new, comprehensive annual measure of health security and preparedness at the federal and state levels.
These measures and tools are described in more detail in Appendix D.
The committee identified four key areas in which additional research could significantly improve the integration of health considerations into recovery planning processes:
- How does integration of health improvement plans with comprehensive plans and pre-disaster recovery plans prior to a disaster support a healthy community approach to disaster recovery?
- What are the optimal organizational arrangements at the state and local levels under the structure of the NDRF that facilitate coordination across sectors, including the often separate health and social services domains?
- What strategies can be used to better integrate the ongoing collaborative initiatives that occur in nearly all communities under the rubric of community development and human services transformation into NDRF-driven organizational and governance structures for recovery?
- What core set of metrics would best enable communities to evaluate the effects of recovery activities on health outcomes and adjust strategic approaches as needed in the context of a learning system?
SUMMARY OF FINDINGS AND RECOMMENDATIONS
The committee was charged with providing recommendations and guidance on actions that could be taken by all sectors to improve health outcomes after disasters. The committee took this charge to mean not just restoring systems to pre-disaster levels of functioning but building back better and in ways that contribute to an overall healthier community. This goal is best accomplished through pre-disaster planning informed by a community’s shared vision and a locally driven assessment of community health needs, assets, and risk. Those assessments are an essential component of a health improvement plan. Thus, incorporating health goals from a formal health improvement planning process into disaster recovery planning is a critical mechanism for ensuring improved individual and community health and resilience after a disaster. However, the committee recognizes that health improvement plans are underdeveloped or nonexistent in many communities, and when they do exist, they may be outdated and may not be familiar to or supported by current local leadership (Bennett, 2014). Further, health goals from a health improvement plan need to be integrated into the community’s strategic planning process, which is used to set priorities and allocate funds, so that decision making before and after a disaster is guided by a vision of a healthier community. A community that has already integrated health considerations into its strategic
planning process and comprehensive plan is better equipped to rebuild infrastructure and systems in ways that promote health, resilience, and sustainability because it is more likely to have leadership buy-in and collaborative structures that include health components. However, it is important to note that even if a healthy, resilient, sustainable community vision and associated goals have not been integrated into a community’s pre-disaster community strategic planning processes, this health perspective can still be included in post-disaster recovery planning.
Recommendation 1: Develop a Healthy Community Vision for Disaster Recovery.
The committee recommends that state and local elected and public officials incorporate a vision for a healthy community into community strategic planning and disaster recovery planning.
Implementation of this recommendation will require action at the state and local as well as federal levels. Specifically, at the state and local levels, the following actions should be taken:
- Public health leaders should enhance health improvement planning through engagement with a comprehensive group of community stakeholders (representing each of the audiences for this report; see Chapter 1) and ensure that plans are based on communities’ needs and assets.
- Elected and public officials, including emergency managers and local disaster recovery managers, should together lead relevant stakeholders in risk-based disaster recovery planning that develops the procedures, processes, and administrative arrangements to be used for integrated, coordinated recovery.
- Elected and public officials, including emergency managers and local disaster recovery managers, should integrate public health officials and health improvement plans into community strategic planning and disaster recovery planning before and after a disaster. To facilitate that integration, the community’s needs and plans for health improvement should be reflected in disaster recovery priorities.
At the federal level, a coordinated, interagency effort is needed to support state and local stakeholders in the development of recovery plans that ensure that communities build back stronger. To this end, the committee believes that aligned grant guidance and technical assistance are essential motivators. Alignment is key to promoting synergy and ensuring that opportunities are not missed. Federal agencies should use existing grant programs to enhance the capacity of state and local stakeholders to plan for and implement a healthy community perspective in disaster recovery. Specifically, federal agencies should take the following actions:
- HHS, HUD, DOT, EPA, and other federal agencies should use aligned grant guidance and technical assistance for existing and future grant programs to incentivize preparedness, community health, and community development grantees to collaborate on the integration of local health improvement goals into comprehensive plans and disaster recovery plans.
- The CDC and the Office of the Assistant Secretary for Preparedness and Response should revise preparedness grant guidance related to the recovery capability to include greater focus on long-term recovery and opportunities for using recovery to advance healthier and more resilient and sustainable communities.
- FEMA should incentivize emergency management preparedness program grantees to incorporate health considerations into recovery planning by providing grant guidance and technical assistance aligned with HHS guidance.
Every policy decision made regarding a community’s recovery should be seen as an opportunity to improve the health and well-being of the population. Although testimony to the committee from federal
agencies representing various RSFs demonstrated progress toward cooperation and even collaboration, the committee did not find evidence that this vision or level of health integration (i.e., Health in All Policies) has been achieved during operationalization of the NDRF at the federal level.
Disasters create and exacerbate unmet human needs that, if not addressed, have significant impacts on long-term health outcomes in a community. Because these unmet needs closely resemble those with which many communities struggle during normal times (i.e., the vulnerable populations before a disaster are also the vulnerable populations after the event), the municipal structures already established for dealing with these challenges represent an important resource that can be tapped to enable integrated, coordinated recovery planning and to facilitate Health in All Policies. In such cases, critical relationships have already been built and barriers to intersectoral collaboration overcome. In developing operational and governance structures under the framework of the NDRF, state and local decision makers should ensure that these collaborative arrangements operating prior to a disaster are added to the list of organizational assets and incorporated into the recovery planning effort.
Recommendation 2: Integrate Health Considerations into Recovery Decision Making Through the National Disaster Recovery Framework.
The committee recommends that the Federal Emergency Management Agency (FEMA) and the five other federal agencies that represent coordinating agencies for the Recovery Support Functions take steps to further develop and promote the National Disaster Recovery Framework (NDRF) as the basis for a locally defined organizing structure for disaster recovery at the state and local levels to promote information sharing and alignment of funding streams. Further, to ensure that health considerations are integrated into all recovery operations, FEMA, in consultation with the U.S. Department of Health and Human Services (HHS), should update the NDRF to explicitly include health implications for the activities of all Recovery Support Functions.
State and local elected and public officials should establish a steering committee to guide the development of an operational structure that incorporates the organizing principles of the NDRF—including a disaster recovery coordinator and the Recovery Support Functions—and builds on existing collaborative municipal and civic structures, authorities, and initiatives.
Successful recovery will require a systems approach with integration across the full range of community stakeholder groups, both horizontally and vertically, so that capabilities and resources, both public and private, are leveraged in a coordinated manner to achieve the best outcomes for the community as a whole. Many key stakeholders (including those from the public health, health care, behavioral health, and social services sectors) are not accustomed to working in the emergency management context and are not familiar with the relevant processes, terminology, or resources. Through this report, the committee hopes to facilitate the engagement and support of those stakeholders from both the health and the nonhealth sector whose involvement in recovery planning and implementation is essential to the building of healthier and more resilient and sustainable communities after disasters. This involvement will require (1) access to easy-to-use guidance materials describing the recovery process, including an overview of critical resources that are mobilized and accountable parties; and (2) a clear understanding of mechanisms for stakeholder engagement in the recovery planning process.
Recommendation 3: Facilitate the Engagement of the Whole Community in Disaster Recovery Through Simplified and Accessible Information and Training.
To facilitate the engagement of the whole community in building healthier communities after disasters, the Federal Emergency Management Agency should lead an interagency effort centered
on increasing the accessibility and coherence of information related to disaster recovery and the provision of relevant training.
Priorities should include
- the development of educational materials, including a single overarching federal document that serves as a primer on the recovery process and is easily accessible on the Web regardless of the pathway by which a stakeholder seeks to enter the recovery planning process;
- the development of companion guidance documents for state, local, and nongovernmental stakeholders for each of the Recovery Support Functions, providing more detailed descriptions that facilitate stakeholder understanding of available resources, best practices, and the pathways by which they can engage in the pre- and post-disaster recovery planning processes; and
- the development of coordinated training programs for stakeholders and their professional societies that raise awareness of threats and opportunities related to health and promote broad stakeholder participation in recovery planning under the NDRF.
Training programs should
- sensitize stakeholders to the importance of short-term health protection concerns and long-term opportunities to build healthier communities during recovery, highlighting the critical role of each sector in advancing community health, resilience, and sustainability;
- strengthen connections among emergency management, public health, community development, community planning, human services, and other stakeholder organizations to better prepare them to work together within the structure of the NDRF to increase the chances that recovery resources will be used for creating healthier communities; and
- raise awareness of steady-state community planning processes and administrative structures (partnerships and municipal and civic structures) and mechanisms for leveraging these existing processes and structures by identifying key partnerships and professional resources/sources of technical assistance.
When appropriate, existing federal and professional disaster preparedness training programs, such as those for public health emergency preparedness coordinators and the FEMA Emergency Management Institute’s classroom and independent study courses for emergency managers (including those for federal disaster recovery coordinators), should be leveraged. However, new training courses may be needed to meet the priorities listed above.
The participation of community members (including representatives from vulnerable populations) in all stages of the recovery process is essential to ensuring that recovery decisions align with the community’s shared vision. Achieving this participation will require robust community organizing and extensive outreach. After disasters, community planning initiatives that utilize equitable processes and increase interaction among residents can also build social capital—the social ties that are an integral feature of a community—promoting healing, restoring the social fabric of the community, and strengthening resilience. By partnering with schools, neighborhood associations, community groups, and private businesses, local governments can help foster the collaborative potential and sense of community ownership that are critical to optimal community health improvement and recovery planning. Ideally, these social networks should be developed in advance of a disaster as part of resilience-building efforts.
Recommendation 4: Enhance and Leverage Social Networks in Community Health Improvement and Recovery Planning.
Local elected and public officials should develop and support programs designed to strengthen social networks and deepen trust among community members before and after disasters, thereby increasing resilience. Strategies for enhancing and preserving social networks should be specifically included in community health improvement and disaster recovery plans. Before and after a disaster, existing social networks, such as neighborhood associations, should be leveraged to enhance mechanisms for integrating the community into recovery planning.
To support implementation of this recommendation, the committee offers the following suggestions for building social capital in advance of a disaster, preserving it during a disaster, and leveraging it thereafter:
- Building social capital prior to a disaster—Examples of successful programs that have enhanced social cohesion include community currency and time-banking programs (as discussed earlier in this chapter) (Richey, 2007); social marketing campaigns; and administrative and financial support for local initiatives and institutions such as faith-based organizations, sport and social clubs, and civil society organizations. An example of a social marketing campaign created as part of preparedness efforts is SF72, a program created by the San Francisco Department of Emergency Management in coordination with city residents that helps San Franciscans expand their social networks (SF72, 2014). The success of these programs can be measured through surveys of levels of social cohesion and civic and neighborhood participation.
- Preserving social networks during a crisis—During a disaster, local disaster managers, nongovernmental organizations such as the Red Cross, and federal agencies such as FEMA should ensure that disaster management policies support existing social networks. Following Hurricane Katrina, for example, the random placement of survivors in temporary housing across the country crippled social networks by separating kin and friends (Aldrich, 2012; Underhill, 2008). Despite time pressures, decision makers should do their best to ensure the continuation of social networks after a disaster, even during evacuation and temporary sheltering. Further, once survivors have been placed in shelters (ideally in groups that continue pre-disaster relationships), organizers should ensure that they have access to technologies that connect them with their networks.
- Leveraging social capital during recovery—Following a disaster, disaster managers should ensure that recovery plans and neighborhood rebuilding schemes develop through bottom-up and equitable neighborhood processes whereby local citizens, not outsiders, drive visions of the future. This can be achieved by encouraging or even requiring the solicitation of input from neighborhood-level organizations (e.g., homeowners associations) in a community requiring significant redevelopment, and outcomes can be measured through surveys that probe the depth of resident involvement in and satisfaction with planning activities.
The consideration of potential health impacts of recovery decisions in a systematic way necessitates a ready source of health information. Health impact assessments support a Health in All Policies approach and are increasingly being used to inform a wide range of policy decisions. While not yet widely applied to recovery decision making, this technique holds great potential. As operational structures for recovery are being developed and exercised, pathways for sharing information, including health information, should simultaneously be evaluated and delineated. To this end, a pre-disaster investment in infrastructure and, in some cases, data-sharing agreements are required. Continuous evaluation of health and recovery indicators through a learning system approach enables decision makers to evaluate progress toward a healthy, resilient, and sustainable community vision and adapt recovery management strategies as need. This learning process also supports efforts to identify best practices and expand the evidence base for guidance and training (Recommendation 3).
Recommendation 5: Establish Pathways by Which Health Information Can Inform Recovery Decision Making.
State and local elected and public officials should ensure that clear pathways for integration and dissemination of health information are established, including mechanisms that enable concerns and priorities of community members to be transmitted to disaster recovery decision makers. Additionally, a continual feedback process should be established to allow for updating to reflect changes in conditions and measured progress toward recovery. Thus, indicators for measuring progress and success should be (1) developed, (2) incorporated into pre-disaster recovery plans, and (3) updated after a disaster based on its health impact.
Aldrich, D. 2012. Building resilience: Social capital in post-disaster recovery. Chicago: University of Chicago Press.
The Alliance for a Just Rebuilding, ALIGN, Community Development Project, Community Voices Heard, Faith in New York, Families United for Racial and Economic Equality, Good Old Lower East Side, Red Hook Initiative, and New York Communities for Change. 2014. Weathering the storm: Rebuilding a more resilient New York City housing authority post-Sandy. http://www.rebuildajustny.org/wp-content/uploads/2014/03/Weathering_The_Storm.pdf (accessed October 20, 2014).
APA (American Planning Association). 2006a. Integrating planning and public health: Tools and strategies to create healthy places. Chicago, IL: APA.
APA. 2006b. Planning and urban design standards. Hoboken, NJ: John Wiley and Sons, Inc.
APA. 2014. Planning for post-disaster recovery: Next generation. Chicago, IL: APA.
ASTHO (Association of State and Territorial Health Officials). 2007. Disaster recovery for public health. http://www.astho.org/programs/preparedness/disaster-recovery-for-public-health (accessed November 18, 2014).
Beardsley, D. 2014. Session I: Public health, panel discussion. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Two, February 3, Washington, DC.
Bennett, G. 2014. Coordination among federal recovery support functions. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Three, April 28-29, Washington, DC.
Blumenstock, J. 2014. Coordination among state and local government agencies. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Three, April 28-29, Washington, DC.
Boyd, A. 2014. Long-term recovery planning: Goals and policies. In Planning for post-disaster recovery: Next generation: PAS report 576, edited by J. C. Schwab. Chicago, IL: APA. Pp. 72-91.
Carnegie, J. 2015. City of Hoboken, New Jersey proposed stormwater management plan health impact assessment (HIA). New Brunswick, NJ: Rutgers, The State University of New Jersey.
CARRI (Community and Regional Resilience Institute) and CaRES (Campus Resilience Enhancement System). 2013. Success stories: The importance of effective community engagement. http://www.resilientus.org/wp-content/uploads/2013/10/Oct-Success-Stories-Compilation-Community-Engagement.pdf (accessed December 1, 2014).
CDC (Centers for Disease Control and Prevention). 1997. Principles of community engagement. Washington, DC: CDC.
CDC. 2015. Health Impact Assessment. http://www.cdc.gov/healthyplaces/hia.htm (accessed March 26, 2015).
CDC and CDC Foundation. 2013. Building a learning community & body of knowledge: Implementing a whole community approach to emergency management. Atlanta, GA: CDC.
Chandra, A. 2014. Considerations for community health in disaster recovery. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Three, April 28-29, Washington, DC.
Chandra, A., and J. D. Acosta. 2009. The role of nongovernmental organizations in long-term human recovery after disaster: Reflections from Louisiana four years after Hurricane Katrina. Santa Monica, CA: RAND Corporation.
Chandra, A., and J. D. Acosta. 2010. Disaster recovery also involves human recovery. Journal of the American Medical Association 304(14):1608-1609.
City of Seattle. 2013. Toward a resilient Seattle: Post-disaster recovery plan framework. http://www.seattle.gov/Documents/Departments/Emergency/PlansOEM/Recovery/SeattleDisasterRecoveryPlanFrameworkJan2013final.pdf (accessed October 20, 2014).
Clements, B. 2014. Public health and community recovery: Texas’ experience. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Two, February 3, Washington, DC.
Collins, R. A. 2011. No more “planning by suprises”: Post-Katrina land use planning in New Orleans. In Resilience and opportunity: Lessons from the U.S. Gulf Coast after Katrina and Rita, edited by A. Liu, R. V. Anglin, R. M. Mizelle, and A. Plyer. Washington, DC: Brookings Institution Press. Pp. 161-172.
Colten, C. E., R. W. Kates, and S. B. Laska. 2008. Three years after Katrina: Lessons for community resilience. Environment: Science and Policy for Sustainable Development 50(5):36-47.
Community Commons. 2014. Community Health Needs Assessment (CHNA). http://assessment.communitycommons.org/chna/About.aspx (accessed November 18, 2014).
Community Planning Workshop. 2010. Pre-disaster planning for post-disaster recovery: Case studies. Eugene, OR: Community Planning Workshop.
County Health Rankings. 2015. Our approach. http://www.countyhealthrankings.org/our-approach (accessed April 1, 2015).
Dannenberg, A. L., R. J. Jackson, H. Frumkin, R. A. Schieber, M. Pratt, C. Kochtitzky, and H. H. Tilson. 2003. The impact of community design and land-use choices on public health: A scientific research agenda. American Journal of Public Health 93(9):1500-1508.
DeSalvo, K. B., N. Lurie, K. Finne, C. Worrall, A. Bogdanov, A. Dinkler, S. Babcock, and J. Kelman. 2014. Using Medicare data to identify individuals who are electricity dependent to improve disaster preparedness and response. American Journal of Public Health 104(7):1160-1164.
DeSalvo, K. B. 2013. The Katrina experience: Considerations for health system recovery. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting One, November 25, Washington, DC.
DHS (U.S. Department of Homeland Security) and EPA (U.S. Environmental Protection Agency). 2010. Memorandum of agreement between the Department of Homeland Security (DHS), Federal Emergency Management Agency (FEMA) and the Environmental Protection Agency (EPA). http://www.epa.gov/dced/pdf/2011_0114_fema-epamoa.pdf 10 (accessed November 18, 2014).
Donahue, K. 2014. Follow the money: Hurricane Sandy recovery, two years later. Harvard Political Review. http://harvardpolitics.com/united-states/follow-money-hurricane-sandy-recovery-two-years-later (accessed April 1, 2015).
Duncan, W. J., P. M. Ginter, A. C. Rucks, M. S. Wingate, and L. C. McCormick. 2007. Organizing emergency preparedness within United States public health departments. Public Health 121(4):241-250.
Edgington, D. W. 2011. Reconstructing Kobe: The geography of crisis and opportunity. Vancouver: University of British Columbia Press.
EPA (U.S. Environmental Protection Agency). 2014. EPA and FEMA partner to help communities prepare for and recover from natural disasters. http://www.epa.gov/smartgrowth/fema_moa.htm (accessed March 18, 2015).
FEMA (Federal Emergency Management Agency). 2011a. A whole community approach to emergency management: Principles, themes, and pathways for action. Washington, DC: FEMA.
FEMA. 2011b. FEMA strategic plan: Fiscal years 2011-2014. Washington, DC: FEMA.
FEMA. 2011c. Lessons in community recovery: Seven years of emergency support function #14 long-term community recovery from 2004 to 2011. Washington, DC: FEMA.
FEMA. 2011d. National disaster recovery framework. Washington, DC: FEMA.
FEMA. 2011e. National preparedness goal. Washington, DC: FEMA.
FEMA. 2011f. National preparedness system. Washington, DC: FEMA.
FEMA. 2013a. Building community resilience by integrating hazard mitigation: Integrating hazard mitigation into the local comprehensive plan. http://www.fema.gov/media-library-data/20130726-1908-25045-9918/factsheet1.pdf (accessed December 1, 2014).
FEMA. 2013b. Information sheet: Threat and hazard identification and risk assessment. http://www.fema.gov/media-library-data/1388146249060-7b2abfe6be10c67c4070ed42deaaadf1/THIRA%20Information%20Sheet_20131104.pdf (accessed March 18, 2015).
FEMA. 2013c. National response framework. Washington, DC: U.S. Department of Homeland Security.
FEMA. 2014a. Core capabilities. https://www.fema.gov/core-capabilities (accessed March 26, 2015).
FEMA. 2014b. Overview of the federal interagency operational plans. Washington, DC: U.S. Department of Homeland Security.
FEMA. 2014c. Overview of the national planning frameworks. Washington, DC: U.S. Department of Homeland Security.
FEMA. 2014d. Threat and hazard identification and risk assessment. https://www.fema.gov/threat-and-hazard-identification-and-risk-assessment (accessed December 2, 2014).
Frumkin, H., L. Frank, and R. Jackson. 2004. Urban sprawl and public health. Washington, DC: Island Press.
HHS (U.S. Department of Health and Human Services). 2009. National health security strategy of the United States of America. Washington, DC: HHS.
HHS. 2015. National health security strategy and implementation plan 2015-2018. Washington, DC: HHS.
Hillsborough County Government. 2010. Post-disaster redevelopment plan. http://www.hillsboroughcounty.org/index.aspx?nid=1795 (accessed November 18, 2014).
Hodgson, K. 2011. Comprehensive planning for public health: Results of the planning and community health research center survey. https://www.planning.org/research/publichealth/pdf/surveyreport.pdf (accessed December 1, 2014).
HUD (U.S. Department of Housing and Urban Development). 2014. Community development. http://portal.hud.gov/hudportal/HUD?src=/program_offices/comm_planning/communitydevelopment (accessed December 4, 2014).
ICMA (International City/County Management Association). 2014. Local governments, social equity, and sustainable communities: Advancing social equity goals to achieve sustainability. http://icma.org/en/results/sustainable_communities/projects/advancing_social_equity_goals_to_achieve_sustainability (accessed October 21, 2014).
IOM (Institute of Medicine). 2012. Crisis standards of care: A systems framework for catastrophic disaster response. Washington, DC: The National Academies Press.
IOM and NRC (National Research Council). 2005. Public health risks of disasters: Communication, infrastructure, and preparedness—workshop summary. Washington, DC: The National Academies Press.
Johnson, L. A., and R. B. Olshansky. 2013. The road to recovery: Governing post-disaster reconstruction. Land Lines:14-21. https://www.lincolninst.edu/pubs/2259_The-Road-to-Recovery--Governing-Post-Disaster-Reconstruction (accessed October 14, 2014).
The Joint Commission. 2005. Standing together: An emergency planning guide for America’s communities. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations.
Kates, R. W., C. E. Colten, S. Laska, and S. P. Leatherman. 2006. Reconstruction of New Orleans after Hurricane Katrina: A research perspective. Proceedings of the National Academy of Sciences of the United States of America 103(40):14653-14660.
Lenihan, P. 2005. MAPP and the evolution of planning in public health practice. Journal of Public Health Management and Practice 11(5):381-388.
Lockwood, B. 2014. Coordination among state and local government agencies. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Three, April 28-29, Washington, DC.
Love, R., and S. Vallance. 2014. The role of communities in post-disaster recovery planning: A Diamond Harbour case study. Lincoln Planning Review 5(1-2):3-9.
Lowrie, K. 2014. Mystic Island, New Jersey voluntary buyout scenarios: Health impact assessment. New Brunswick, NJ: Rutgers, The State University of New Jersey.
Marcus, L. J., B. C. Dorn, and J. M. Henderson. 2006. Meta-leadership and national emergency preparedness: A model to build government connectivity. Biosecurity and Bioterrorism 4(2):128-134.
NACCHO (National Association of County and City Health Officials). 2014a. 2013 national profile of local health departments. Washington, DC: NACCHO.
NACCHO. 2014b. The assessments. http://www.naccho.org/topics/infrastructure/mapp/framework/phase3.cfm (accessed March 18, 2015).
NACCHO. 2014c. MAPP basics: Introduction to the MAPP process. http://www.naccho.org/topics/infrastructure/mapp/framework/mappbasics.cfm (accessed December 1, 2014).
NACCHO. 2014d. Visioning. http://www.naccho.org/topics/infrastructure/mapp/framework/phase2.cfm (accessed August 25, 2014).
Nakagawa, Y., and R. Shaw. 2004. Social capital: A missing link to disaster recovery. International Journal of Mass Emergencies and Disasters 22(1):5-34.
Nolen, A. 2014. A health in all policies approach to disaster recovery: Lessons from Galveston. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Four, June 13, Washington, DC.
Norris, T., and M. Pittman. 2000. The healthy communities movement and the coalition for healthier cities and communities. Public Health Reports 115(2-3):118-124.
NPLI (National Preparedness Leadership Initiative). 2013. Who should apply? http://npli.sph.harvard.edu/executivedevelopment/who-should-apply (accessed March 26, 2015).
NRC (National Research Council). 2011. Improving health in the United States: The role of health impact assessment. Washington, DC: The National Academies Press.
Olshansky, R. 2014. Post-disaster recovery: How to rebuild cities in compressed time. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Two, February 3, Washington, DC.
PHAB (Public Health Accreditation Board). 2011. Acronyms and glossary of terms. http://www.phaboard.org/wpcontent/uploads/PHAB-Acronyms-and-Glossary-of-Terms-Version-1.0.pdf (accessed November 18, 2014).
PHII (Public Health Informatics Institute) and NACCHO. 2008. Taking care of business. https://phii.org/sites/default/files/resource/pdfs/Taking%20Care%20of%20Business%2006-08.pdf (accessed August 19, 2014).
Pinellas County. 2012. Pinellas County post-disaster redevelopment plan. Pinellas County, FL: Pinellas County.
Plyer, A., and E. Ortiz. 2011. Building data capacity to foster resilient communities. In Resilience and opportunity: Lessons from the U.S. Gulf Coast after Katrina and Rita, edited by A. Liu, R. V. Anglin, R. Mizelle, and A. Plyer. Washington, DC: Brookings Institution Press. Pp. 187-200.
Reaves, E. J., M. Termini, and F. M. J. Burkle. 2014. Reshaping US Navy Pacific response in mitigating disaster risk in South Pacific Island nations: Adopting community-based disaster cycle management. Prehospital and Disaster Medicine 29(1):60-68.
Rebuild Iowa Office. 2011. Disaster recovery lessons learned. http://publications.iowa.gov/11080/1/2011-06_Iowa_Disaster_Recovery_Lessons_Learned_final.pdf (accessed October 20, 2014).
Rice, H. 2014. Rebuilding begins for Galveston public housing 6 years after Ike. Houston Chronicle, 12. http://www.houstonchronicle.com/news/houston-texas/texas/article/Rebuilding-begins-for-Galveston-public-housing-6-5746823.php (accessed October 20, 2014).
Richey, S. 2007. Manufacturing trust: Community currencies and the creation of social capital. Political Behavior 29(1):69-88.
Ricklin, A., and N. Kushner. 2013. Integrating health into the comprehensive planning process: An analysis of seven case studies and recommendations for change. Chicago, IL: APA.
Ricklin, A., A. Klein, and E. Musiol. 2012. Healthy planning: An evaluation of comprehensive and sustainability plans addressing public health. Chicago, IL: APA.
Rouse, W. B. 2000. Managing complexity. Information, Knowledge, Systems Management 2(2):143-165.
Rudolph, L., J. Caplan, C. Mitchell, K. Ben-Moshe, and L. Dillon. 2013. Health in all policies: Improving health through intersectoral collaboration. Discussion Paper. September 18, 2013. http://iom.edu/~/media/Files/Perspectives-Files/2013/Discussion-Papers/BPH-HiAP.pdf (accessed December 1, 2014).
Rutgers. 2014. Health impact assessment in New Jersey: Assessing health outcomes of post-Sandy decision-making. http://njhic.rutgers.edu/wp-content/uploads/2014/10/PEW-Project-Overview-9-23.pdf (accessed March 12, 2015).
Schwab, J., K. C. Topping, C. C. Eadie, and R. E. Edyle. 1998. Planning for post-disaster recovery and reconstruction: PAS Report No. 483/484. Chicago, IL: APA.
SF72. 2014. SF72 is San Francisco’s hub for emergency preparedness. http://www.sf72.org/home (accessed December 4, 2014).
Shah, U. 2014. Coordination among state and local government agencies. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Three, April 28-29, Washington, DC.
Sherry, N., and A. Harkins. 2011. Leveling the emergency preparedness playing field. Journal of Emergency Management 9(6):11-16.
Smith, G. 2011a. The national disaster recovery framework: A new vision for recovery. In Planning for post-disaster recovery: A review of the United States disaster assistance framework. Fairfax, VA: Public Entity Risk Institute.
Smith, G. 2011b. Planning for post-disaster recovery: A review of the United States disaster assistance framework. Fairfax, VA: Public Entity Risk Institute.
Turnock, B. J., and C. Atchison. 2002. Governmental public health in the United States: The implications of federalism. Health Affairs 21(6):68-78.
ULI (Urban Land Institute). 2014. Housing in America: Integrating housing, health, and resilience in a changing environment. http://uli.org/wp-content/uploads/ULI-Documents/Housing-in-America-2014.pdf (accessed October 21, 2014).
Underhill, R. 2008. Katrina’s displacement: The untold consequences of disaster resettlement in Colorado. MA Thesis submitted by Megan Ruth Underhill to the Colorado State University Department of Anthropology.
United Health Foundation, APHA (American Public Health Association), and Partnership for Prevention. 2014. America’s health rankings®: A call to action for individuals and their communities. Minnetonka, MN: United Health Foundation.
Usdin, L. 2014. Building resiliency and supporting distributive leadership post-disaster. International Journal of Leadership in Public Services 10(3):157-171.
Walsh, L., and K. W. Schor. 2014. Education and training opportunities in long-term community recovery: Preliminary observations from the field. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Three, April 28-29, Washington, DC.
WHO (World Health Organization). 2013. Health in all policies. http://www.healthpromotion2013.org/healthpromotion/health-in-all-policies (accessed December 4, 2014).
Zucker, H. 2014. Post-disaster recovery: New York State Department of Health experience with Superstorm Sandy. Paper presented at IOM Committee on Post-Disaster Recovery of a Community’s Public Health, Medical, and Social Services: Meeting Two, February 3, Washington, DC.












































