Progress in any human endeavor is a product of an understanding of the circumstances in play, the tools available to address the controllable factors, and the resolve to take the actions required. Basic to each is the choice of measures—measures that give the best sense of challenges and opportunities, measures that guide actions, and measures that can be used to gauge impact. In times of rapid change and constrained resources, measures that are important, focused, and reliable are vital.
These are the circumstances in health and health care today. For Americans, health care costs and expenditures are the highest in the world, yet health outcomes and care quality are below average by many measures (OECD, 2013). If the effectiveness and efficiency of health expenditures are to be brought into alignment on behalf of better health and lower costs, keen attention and decisive actions will be required of all stakeholders—health professionals; payers; policy makers; and all individuals as patients, family members, and citizens—on what matters most. That is the focus of this report. What matters most for health and health care? What are the vital signs for the course of health and well-being in America?
As the number of available measures continues to grow without concomitant gains in health outcomes, responsibilities for assessing, measuring, and reporting can become a burden with marginal benefit (Meltzer and Chung, 2014). Identifying and prioritizing the most powerful among these myriad measures at each level of activity—establishing core measures—can enable the health system to work in a coordinated fashion with many stakeholders, most importantly with patients, citizens, and communities, toward a shared vision of America’s health future.
The development and adoption of core measures will depend on a culture of shared accountability for health. Responsibility for improving the nation’s health outcomes must be assumed by all members of the multisectoral health system, defined broadly to include the full array of sectors and entities—from clinicians and hospitals to schools and families—that influence the health of the population through their activities (IOM, 2012b). By garnering the attention of all stakeholders involved in the health system, measurement activities can be coordinated and redirected toward those outcomes that are most meaningful to all.
STUDY CHARGE
Prompted by growing awareness of the need both to reduce the burden of unnecessary and unproductive reporting and to better focus measurement on change that matters most, the Institute of Medicine (IOM) appointed the Committee on Core Metrics for Better Health at Lower Cost to conduct this study. The Committee’s work was made possible by the financial support of three sponsors: Blue Shield of California Foundation, the California HealthCare Foundation, and the Robert Wood Johnson Foundation. The charge to the Committee was to “conduct a study and prepare a report directed at exploring measurement of individual and population health outcomes and costs, identifying fragilities and gaps in available systems, and considering approaches and priorities for developing the measures necessary for a continuously learning and improving health system.” Specifically, the Committee was directed to
- “consider candidate measures suggested as reliable and representative reflections of health status, care quality, people’s engagement and experience, and care costs for individuals and populations;
- identify current reporting requirements related to progress in health status, health care access and quality, people’s engagement and experience, costs of health care, and public health;
- identify data systems currently used to monitor progress on these parameters at national, state, local, organizational, and individual levels;
- establish criteria to guide the development and selection of the measures most important to guide current and future-oriented action;
- propose a basic, minimum slate of core metrics for use as sentinel indices of performance at various levels with respect to the key elements of health and health care progress: people’s engagement and experience, quality, cost, and health;
- indicate how these core indices should relate to, inform, and enhance the development, use, and reporting on more detailed measures tailored to various specific conditions and circumstances;
- identify needs, opportunities, and priorities for developing and maintaining the measurement capacity necessary for optimal use of the proposed core metrics; and
- recommend an approach and governance options for continuously refining and improving the relevance and utility of the metrics over time and at all levels.”
The Committee carried out this study through four face-to-face meetings; multiple teleconferences; and solicitation of input broadly from the field, both by submitting written requests and by receiving testimony at public meetings. Three subCommittees were formed to address the analytic framework for the study, potential core measures, and implementation priorities. Two full surveys were developed and administered to the Committee members, soliciting their insights on the relative merits of and alternatives to candidate measures, their opinions on priorities, and any issues that may not have received adequate attention.
This summary describes the key context for this study, including the challenge of the burden of measurement, and then presents the Committee’s approach to selecting core measures. Next is a brief description of each of the selected measures, followed by a discussion of the anticipated implementation process. The final section presents the framing perspectives that underlie the Committee’s recommendations, followed by the recommendations themselves as an action agenda for the full range of stakeholders important to improving health and health care in America.
STUDY CONTEXT
Measurement in Health and Health Care
A dominant feature of the health system is its fragmentation, and that fragmentation is reflected in the measures currently in use. Health measurements are requested and required by many organizations for many purposes, including monitoring of population and community health status, monitoring of personal health, assessment of quality and patient experience, transparency, public reporting and benchmarking, performance requirements, and funder reporting. These requests and requirements for reporting rarely are synchronized among the various organizations involved. Because of the great number and variety of these organizations, the total number of health and health care measures in use today is unknown. Nonetheless, reference points such as the Centers for Medicare & Medicaid Services (CMS)
Measure Inventory, which catalogs nearly 1,700 measures in use by CMS programs, indicate that they number in the thousands (CMS, 2014). The National Quality Forum’s (NQF’s) measure database includes 630 measures with current NQF endorsement (NQF, 2014). The National Committee for Quality Assurance’s (NCQA’s) Healthcare Effectiveness Data and Information Set (HEDIS), used by more than 90 percent of health plans, comprises 81 different measures (NCQA, 2013). And in 2010, the Joint Commission required hospitals to provide data for measures selected from a set of 57 different inpatient measures, 31 of which were publicly reported at the time (Chassin et al., 2010).
Although many of these measures are of high quality and provide valid and useful information about health and health care, many examine only slight variations of the same target. Furthermore, numerous measures in use today are similar enough to serve the same purpose, but they also differ enough to prevent direct comparison among the various states, institutions, or individuals interested in the same target.
In addition to the sheer number of measures, another challenge lies in their focus. Many measurement programs limit their focus to narrow or technical components of health care processes instead of targeting outcomes or the multiple factors that lie outside the domain of the traditional health care system but represent the most important influences on health. Without understanding these factors, it will be difficult to make sustainable progress in improving the health of the nation. Figure S-1 presents a schematic of the current profile of measurement in health and health care today, highlighting various safety measures as an example. Even though the measures identified constitute just a partial listing, the graphic illustrates not only the substantial number of measure targets in various categories but also the much larger number of measures used to address these targets.
Despite the call by organizations such as NQF and the U.S. Department of Health and Human Services (HHS) for greater alignment and harmonization in health system measurement, the various efforts remain broadly uncoordinated both horizontally, or across various activities, and vertically, in terms of consistent and comparable measurements at the national, state, local, and institutional levels. The Committee believes that renewed attempts to align and harmonize measures to reduce redundancies and inefficiencies may now succeed because of the significant changes that have occurred in the environment for measurement. Notably, data capture capabilities have grown rapidly, with electronic health records and other digital tools seeing increasingly widespread use (IOM, 2011). The emerging health information technology infrastructure could support a real-time measurement system for the routine collection of information about care processes, patient needs, progress toward health goals, and individual and population health outcomes. The transformation of technology provides an
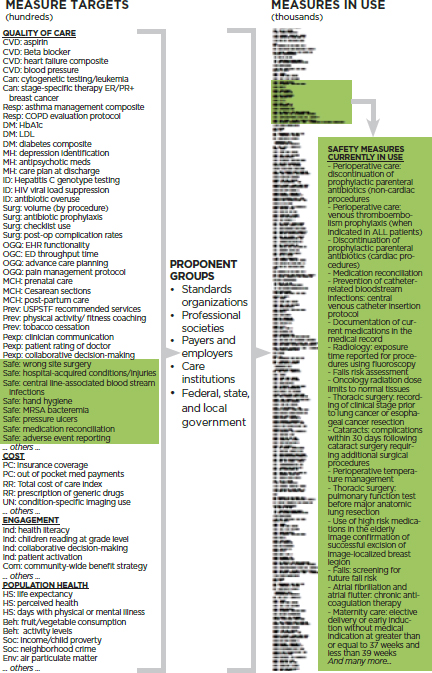
FIGURE S-1 Schematic illustration of the growth of measurement in health and health care. The column on the left (measure targets) gives examples of elements being assessed in various categories. The column on the right (measures in use) illustrates that many different measures are used to assess the same issue. Highlighted are examples of the target issues and measures used in the safety arena. See Figure 4-19 for figure legend.
opportunity to measure what matters most, enabling goals to drive measures rather than measures driving goals.
The Measurement Burden
Change is clearly needed. The rapid proliferation of interest in, support for, and capacity for new measurement activities has paradoxically blunted the effectiveness of those efforts. Absent a blueprint, strategy map, or common set of reference points, the variation inherent in thousands of disconnected measurement and accountability systems limits both insights on the comparability of different sections or levels of the health system and a focus on issues of highest priority. A case can be made that, while the health measurement landscape today consists of a great many high-quality measures, meaningful at some level for their intended purposes, the effectiveness of the health measurement enterprise as a whole is dependent on improved organizing focus, interrelationship, and parsimony in the service of truly meaningful accountability and assessment for the health system. Many process-oriented care measures have helped improve and standardize care as well as led to improved health outcomes; they are important. And many outcome measures are subject to the challenge of reliable risk adjusting. However, the fact that outcome measures are agnostic as to the mechanism or approach taken to achieve improvement ensures both that innovation is encouraged and that the measures used are likely to remain useful over a long period of time. Consequently, unless a process measure, or composite process measure set, offered the prospect of a broader impact on system performance, the Committee tended to give outcome measures priority over process measures.
Many of the individual measures in use today were developed and implemented for a particular purpose and circumstance, without attention to the broader context. The rapid growth in measures that health care organizations are required to report is due in part to redundancies and inefficiencies in data collection and measure specification, such that different organizations interested in assessing the same target or feature require different measures with different specifications. The result is a measurement system that lacks standardization for the assessment and reporting of data on commonly assessed health concepts. For example, the HHS Measure Policy Council initially found that across six HHS measurement programs, 61 different measures were in use for smoking cessation, 113 for HIV, 19 for obesity, and 68 for perinatal health (HHS, 2014a). The HHS Measure Policy Council continues to work across federal measurement programs to streamline and align federal measures, making considerable progress over the past few years.
As a result of this proliferation of measures, existing requirements impose a significant burden on providers, organizations, and the U.S. health care system as a whole. The development and validation of measures and the collection, analysis, and maintenance of data are ultimately coupled with an increasing volume of improvement initiatives. A 2006 study of a sample of hospitals found that each hospital reported to an average of five reporting programs; the authors identify 38 unique reporting programs (Pham et al., 2006). And a 2013 analysis found that a major academic medical center was required to report on more than 120 quality measures to regulators or payers, with the cost of measure collection and analysis consuming approximately 1 percent of net patient service revenue (Meyer et al., 2012). These activities often are viewed as a generally unquantified and undercompensated burden for the U.S. health care system and its various stakeholders. The return on investment for measurement with respect to improved quality and reduced cost of care falls short of expectations, in part because of inefficiency in the use of health measures. While preliminary in nature, an analysis developed in the context of the Committee’s work, based on the results of interviews with the leaders of 20 health systems, confirmed the rapid growth in reporting requirements, the high frequency of inconsistency in similar measures, the large time commitment required of staff and clinicians, and costs that typically number in the millions of dollars.
A core measure set cannot immediately eliminate this burden, but it can ensure stronger attention to the most important issues, as well as improvements in focus and accuracy for efforts in reporting, efficiency, innovation, and performance. A measure set that offers a reliable reflection of the status of health and health care at the national, state, local, and institutional levels will draw sustained attention to what is truly important, focus on results rather than processes, reduce the number of measurements required for reporting purposes, increase flexibility and capacity for innovation at the local and institutional levels, and enhance the effectiveness and efficiency of system performance. In short, a core measure set is a tool that can be used to accelerate progress toward better health at lower cost.
APPROACH TO THE SELECTION OF CORE MEASURES
Starting Point: Domains of Influence
The Committee’s starting point in identifying the foci for core measures was assessment of the key domains of influence—that is, those with the greatest potential to have a positive effect on the health and well-being of the population and each individual within it, now and in the years to come. The domains identified in the Committee’s charge include healthy people,
care quality, care costs, and people’s individual and collective engagement in health and health care. Implicit in the Committee’s charge is the notion that, while the nation’s foundational societal aspiration is healthy people, the health of the population is the product of the ability to make progress in each of these interrelated domains. Achieving the goal of healthy people depends on environments and cultures that are supportive of health. Gains in the quality of care and population health cannot be sustained without affordable care. Care quality and affordability cannot be optimized without engaged people. Each domain is itself a vital contributor to the nation’s health profiles while also being fundamentally intertwined with the others.
Healthy People
The foundational motivation of this report, and of the health system at large, is improving the health of individuals, communities, and the nation. From a population health perspective, the United States faces significant challenges, with chronic disease afflicting nearly half of all adults, violence and injury being the leading cause of death for people aged 1 to 44, and childhood obesity—a harbinger of poor health in adulthood—affecting 17 percent of America’s children (CDC, 2012a; Ogden et al., 2014; Ward and Schiller, 2013). From an international perspective, the United States is below average on a range of health measures, as illustrated in the National Research Council (NRC)/IOM report U.S. Health in International Perspective: Shorter Lives, Poorer Health (NRC and IOM, 2013). The United States spends nearly twice the OECD average on health care, yet Americans have a life expectancy of 78.7 years, below the OECD average of 80.1 years (OECD, 2013). To help improve population health, a core measure set must provide solid indicators of progress toward that goal.
Care Quality
While health care services are not the only or even the most important determinant of population health, their quality matters to individuals and families and influences both the outcomes and the costs of care. A major impetus for transforming the measurement enterprise is the health system’s uneven performance. Improving that performance creates an obvious need for better guideposts. Islands of excellence exist alongside areas in need of improvement. Clinical care has seen marked progress, as illustrated by such advances as antibiotic therapies for infectious diseases; multiple interventions for cardiovascular disease, from beta blockers to percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG); and pharmaceutical agents tailored to the specific genetic characteristics of HIV, a microbe identified just 30 years ago (Fauci, 2003; FDA, 2011;
Fischl et al., 1987; IOM, 2012a; Nabel and Braunwald, 2012; Simon et al., 2006). At the same time, the system has compelling needs for improvement. Medical errors remain common, occurring in almost one-third of hospitalized patients (Classen et al., 2011; Landrigan et al., 2010; Levinson, 2010, 2012). Health care also has become increasingly complex, resulting in shortcuts in decision making and clinical processes, fragmentation of care, preventable errors, and a lack of accountability.
Care Costs
The health care system is characterized by inefficiencies in spending and resource use, such that, according to the 2013 IOM report Best Care at Lower Cost (IOM, 2012a), an estimated 30 percent of health care spending is wasted. Health care costs now constitute almost a fifth of the nation’s economy (Hartman et al., 2013) and pose a challenge for the budgets of the federal and state governments, businesses, and families. Costs vary significantly and with no correlation with quality among different regions of the country, states, localities, and even clinicians operating in the same practice (IOM, 2013). High out-of-pocket costs place financial pressure on individuals and families, potentially leading people to avoid or delay care; to ration personal care resources by, for example, taking medications less frequently than prescribed; and to incur significant debt.
People’s Engagement in Health and Health Care
Patients, consumers, and the broader public are playing an increasing role in health and health care, facilitated by changes in technology and access to information, new models of care delivery, improved understanding of the link between progress in chronic disease and patient engagement, and legislative and payment reforms. Evidence suggests that people who are more actively involved with their health and health care may have improved outcomes. Research has found that people who use health-related social networking sites, such as PatientsLikeMe, TuDiabetes, and TheBody, show improved treatment adherence, have a better understanding of their medical conditions, and feel more in control of their disease management (Grajales et al., 2014; Wicks et al., 2010). Importantly, in the spirit of shared responsibility for maintaining the health of individuals and the population, the notion of engagement includes both the individual and the community. At the community level, such initiatives as those focused on preventing motor vehicle-related injuries, reducing sedentary behavior in workplaces, and reducing exposure to secondhand smoke that have led to significant improvements in health outcomes often depend on the active engagement of communities. While much remains to be learned on how to
facilitate greater individual and public engagement, the importance of doing so is clear and compelling.
Cross-Domain Priority: Disparities
In developing a core measure set, it is essential to focus on disparities to document progress toward and achievement of the goals of improved health status, care, quality, affordability, and public engagement. Substantial disparities exist among and within subpopulations in the United States with respect to the relative impact of each of the domains of influence on health and health care, including disparities by race, ethnicity, income, education, gender, geography, and urban or rural populations. In the aggregate, this issue represents one of the greatest health and health care challenges faced by the nation (HHS, 2011). While 70 percent of non-Hispanic white persons in the United States reported excellent or very good health in 2013, this was the case for only 60 percent of non-Hispanic African American persons and 57 percent of Hispanic persons (CDC, 2013). Individuals from minority racial and ethnic backgrounds experience a higher incidence and severity of certain diseases and health conditions relative to white individuals (APHA, n.d.). For example, the rate of hospitalization for uncontrolled diabetes without complications was almost five times higher in African Americans and four times higher in Hispanics than in whites (Russo et al., 2006). In 2012, difficulty in receiving care was experienced by about 7 percent of high-income individuals but 15 percent of people with family incomes below the federal poverty level (AHRQ, 2012). Children living in families with incomes below the federal poverty level also had lower vaccine coverage than children living in families at or above the poverty level (CDC, 2012b). And racial minorities experience more avoidable procedures, avoidable hospitalizations, and untreated disease than white individuals (Fiscella et al., 2000). Such disparities speak to the need for reliable core data at every level of the health system to help assess, target, and track efforts to close the gap.
Measures as Levers for Action
The Committee undertook its charge with full recognition that measurement in health care is a tool for improvement, not an end point or a solution in itself, as illustrated by the Committee’s definition of core measures (see Box S-1). The diversity of current health measures is a reflection of the wide variety of purposes and targets within health care that have the potential to be assessed empirically and monitored or compared systematically as a route to improvement. As defined in Box S-1, core measures, for present purposes, represent a parsimonious set of measures that provide a
BOX S-1
Definition of Core Measures
A parsimonious set of measures that provide a quantitative indication of current status on the most important elements in a given field, and that can be used as a standardized and accurate tool for informing, comparing, focusing, monitoring, and reporting change.
quantitative indication of current status on the most important elements in a given field, and that can be used as a standardized and accurate tool for informing, comparing, focusing, and monitoring change. A core measure set, therefore, is not intended to replace the full range of measures in use today, but is intended to help improve the focus of measures to reduce reporting burden while improving impacts. A core set can raise the profile of the most compelling health challenges facing the nation; draw attention to issues and actions that can trigger broader-scale system improvement; provide a platform for harmonizing efforts to monitor national, state, local, and institutional progress in health and health care; create opportunities for alignment and the resolution of redundancies in areas where measurement is burdensome; and guide the creation of a more robust multilevel data infrastructure.
The analytic framework used by the Committee begins with the identification of goals for health and health care, follows with an assessment of domains of influence that can promote those goals, and then identifies the key elements and measures that most represent those domains. Unlike many other measurement efforts, the Committee’s work on developing core measures did not start with the procedures, health care tasks, or conditions that are most commonly measured. Rather, the Committee’s approach helped identify ways in which a core measure set might help channel and transform the effectiveness of the many otherwise siloed efforts aimed at engaging the various potentially controllable determinants of health.
Identification of candidate core measures involved an assessment of the most important elements for each of the four domains identified above: for healthy people, these were length of life, quality of life, healthy behaviors, and healthy social circumstances; for care quality, they were prevention, access to care, safe care, appropriate treatment, and person-centered care; for care costs, they were affordability and sustainability; and for people’s engagement in health and health care, they were individual engagement and community engagement.
BOX S-2
Criteria for Core Measure Development
|
Criteria for core measures
|
Criteria for the set
|
As various candidate measures were considered, the Committee employed two sets of criteria: one for the selection of each core measure and the other for compilation of the set as a whole (see Box S-2). With respect to the individual measures, these criteria included importance for health, strength of linkage to progress, understandability of the measure, technical integrity, potential for broader system impact, and utility at multiple levels. While the attributes of individual measures are important, additional considerations are needed to construct a high-quality set of measures. The core set therefore resulted from application of the second set of criteria: systemic reach, outcomes-oriented, person meaningful, parsimonious, representative, and utility at multiple levels.
THE CORE MEASURE SET
Applying the above criteria, the Committee arrived at the core measure set presented in Table S-1. In this table, the domains represent the highest level of organization of the core measures, serving as a guiding framework for their selection and application; the key elements represent the broadest conceptually discrete components of the respective domains; the core measure foci express the most representative and specific focus for measurement for each key element, translating the conceptual key element into something measurable; and the best current measures are measures selected by the Committee from among those now in use in various settings as most representative of the foci of the specified core measures. While many of these best current measures are imperfect reflections of the core measures, they are intended to demonstrate how the core measure set could be applied today,
TABLE S-1 Core Measure Set
| Domain | Key Element | Core Measure Focus | Best Current Measure | Current National Performancea | |
| Healthy people | Length of life |  |
Life expectancy | Life expectancy at birth | 79-year life expectancy at birth |
| Quality of life |  |
Well-being | Self-reported health | 66% report being healthy | |
 |
Overweight and obesity | Body mass index (BMI) | 69% of adults with BMI 25 or greater | ||
| Healthy behaviors |  |
Addictive behavior | Addiction death rate | 200 addiction deaths per 100,000 people age 15+ | |
 |
Unintended pregnancy | Teen pregnancy rate | 27 births per 1,000 females aged 15 to 19 | ||
| Healthy social circumstances |  |
Healthy communities | High school graduation rate | 80% graduate in 4 years | |
| Care quality | Prevention |  |
Preventive services | Childhood immunization rate | 68% of children vaccinated by age 3 |
| Access to care |  |
Care access | Unmet care need | 5% report unmet medical needs | |
| Safe care |  |
Patient safety | Hospital-acquired infection (HAI) rate | 1,700 HAIs per 100,000 hospital admissions | |
| Appropriate treatment |  |
Evidence-based care | Preventable hospitalization rate | 10,000 avoidable per 100,000 hospital admissions | |
| Person-centered care |  |
Care match with patient goals | Patient–clinician communication satisfaction | 92% satisfied with provider communication | |
| Domain | Key Element | Core Measure Focus | Best Current Measure | Current National Performancea | |
| Care cost | Affordability |  |
Personal spending burden | High spending relative to income | 46% spent >10% income on care, or uninsured in 2012 |
| Sustainability |  |
Population spending burden | Per capita expenditures on health care | $9,000 health care expenditure per capita | |
| Engaged people | Individual engagement |  |
Individual engagement | Health literacy rate | 12% proficient health literacy |
| Community engagement |  |
Community engagement | Social support | 21% inadequate social support | |
a See Chapter 4 for current performance sources and definition of terms.
with the understanding that significant measure development is needed in many of these areas.
Each core measure focus identified by the Committee ranks among the most important foci for action at the national, state, local, and even institutional levels. The Committee has not specified all the core measures in detail because many will need further collaborative definition and refinement before being fully applicable. Standardized measurement approaches exist for life expectancy and overweight and obesity, but such widely accepted standardized measures are absent for most of the other foci, including well-being, addictive behavior, healthy communities, evidence-based care, spending burden, and individual and community engagement. Additionally, many of the core measures will need to be adapted when used at different levels of the health system. For example, while gross domestic product (GDP) is a useful tool for assessing cost at the national level, it clearly cannot be applied directly at the local or the institutional level. An alternative measure, such as total cost of care, is needed to assess spending for a population served by an institution. This adaptation for different levels will depend on active involvement and collaboration among relevant stakeholders and therefore lies beyond both the expertise of the Committee and the appropriateness of its efforts.
The lack of proven consensus measures is particularly notable for individual and community engagement. The Committee’s charge called for inclusion of measures for these key elements, and there was strong sentiment among the Committee members that these are essential influences on the national goals for health and health care. However, Committee members’ perspectives were divided on the question of whether the strength and precision of the definitions and measures available for engagement warranted their inclusion alongside the domains of health, care quality, and care cost. Individual and community engagement clearly work in service to, and as an element in the success of, activities directed at the Institute for Healthcare Improvement’s (IHI’s) Triple Aim of better health, better patient experience of care, and lower costs. Still, considerable definitional and analytic work is required to develop practical measures that can reliably capture the extent to which individuals are prepared for and engage in effective participation in health and health care planning, delivery, and improvement. Additionally, research is needed to explore how levers available for community-wide action are being employed effectively for improvement on matters of central importance to the health of the population. Given the identification of engagement as a domain in the Committee’s statement of task and the acknowledgment within the Committee that engagement represents an important—if underdeveloped—element of the changing landscape of health, the Committee’s deliberations were guided by the four domains of health, care, quality, care cost, and engagement.
Measure development and standardization were beyond the scope of the Committee’s charge. To accelerate the development and application of a fully specified core measure set, however, the Committee has specified what in its judgment is the best currently available measure for each core measure focus. This measure set, while imperfect, represents in the Committee’s view a powerful starting set of “vital signs” for tracking progress toward improved health and health care in the United States. The Committee believes further that the core measure set recommended herein comprises the vital signs on the status and progress of the nation’s health and health care, that a single measure can be chosen or developed for each of the core measure foci within each domain of influence, and that the development of a standardized measure is essential for each focus. The Committee also believes that, when applied, attention to these core measure foci will have the multiplier effect of improving performance broadly throughout the health and health care organizations engaged in their use.
Although they may be characterized in different ways and often are interrelated at some level, each of the key elements shown in Table S-1 is central to progress in health and health care. Quality of life is an aim basic to all individuals, and while length of life is not an immutable goal for every person at every stage of life, it is an accepted standard for the overall health
of populations. It also is now well established that the health of populations is substantially shaped by factors outside of health care, including patterns of health-related behaviors and social circumstances such as physical environments and socioeconomic status. High-quality care is a function of the interplay among access to care, prevention, and appropriate treatment. The interplay among and the reinforcing nature of these elements was a factor in the identification and consideration of core measures.
Brief descriptions follow for each of the core measure foci. As noted above, because most of these foci are not supported by widely accepted standardized measures accessible for application at every level of the health system, the Committee has recommended the best current measures shown in Table S-1 (see also Chapter 4). Examples include the use of childhood immunization status as a best current measure for the delivery of preventive services and self-reported health status as a measure of well-being. Many of these best current measures are currently imperfect because of limitations in scope, reliability, generalizability, or conceptual boundary and will require substantial work. For this reason, the Committee has recommended that, as stakeholders at various levels try out their own proxies for the core measure foci, the Secretary of HHS steward a broadly inclusive process to marshal the nation’s experience and expertise in the development of the standardized set of core measure foci (see Chapter 5).
Life expectancy: Life expectancy is a validated, readily available, and easily comprehensible measure for a critical health concept, length of life, based on the simple logic that healthier people tend to live longer. Because life expectancy depends on a full range of individual and community influences on health—from cancer to homicide—it provides an inclusive, high-level measure for health, broadly defined.
Well-being: Life expectancy and death rates from various diseases and injuries provide clear, “bright line” measures of health in a population group, but health and well-being in the population comprise many other components, including illness from chronic or acute diseases, injury, functional capacity, mental health, sense of security, and social networks. As the World Health Organization notes, health is “not merely the absence of disease” (WHO, 1946). The health of an individual has both objective and subjective dimensions. In fact, people’s perception of their own health is not just a reliable indication of well-being but often a predictor of utilization of and satisfaction with health care.
Overweight and obesity: Overweight and obesity represent a significant challenge to Americans’ health. Their prevalence is a feature of American life with causes and consequences that extend beyond the scope of the health system, including socioeconomic, cultural, political, and lifestyle factors—in particular diet and physical activity, which together constitute leading causes of early death. Therefore, reducing the prevalence of
overweight and obesity in the United States—and by extension, improving health and reducing the costs of care across the nation—will depend on the coordinated efforts of many stakeholder groups.
Addictive behavior: Addiction and addictive behavior represent a significant and complex challenge for the health system, as well as for communities and families. Approximately 18 percent of American adults smoke, 17 percent of adults binge drink, and an estimated 9 percent of people aged 12 years and older were found to have used an illicit drug within the past month (Agaku et al., 2014; CDC, 2012c; NCHS, 2014). The estimated economic cost of substance abuse and addiction in the United States is $559 billion per year (NIDA, 2008).
Unintended pregnancy: Unintended pregnancy presents a significant challenge for both individual and community health. According to a report from the Centers for Disease Control and Prevention’s (CDC’s) Division of Vital Statistics, it is the most direct available measure of women’s ability to choose the number and timing of their pregnancies. As such, it is a measure that aggregates a variety of social, behavioral, cultural, and health factors, particularly the availability and use of both knowledge and tools for family planning.
Healthy communities: Individual health is a function of a wide range of socioeconomic and community factors, ranging from environmental quality to infrastructure to education and social connections. Thus, the health of all individuals is closely tied to the health of the community in which they live, such that individual actions to improve health can benefit the community, and community actions to improve health can benefit each individual member. Community health includes critical elements of health that fall outside of the care system but have a major impact on care and health outcomes, such as housing, employment, and environment.
Preventive services: Preventive services—immunization, screening, counseling, and chemo prophylaxis—present a valuable opportunity for both improving health and adding value. Based on rigorous evidence standards, the U.S. Preventive Services Task Force recommends a range of services for different groups, from screening for hearing loss for infants to tobacco cessation counseling for current smokers (USPSTF, 2010).
Care access: The ability to receive care when needed is a critical precondition for a high-quality health system. Unmet need for health care may occur for a variety of reasons, including lack of or insufficient health insurance, clinician shortages, lack of transportation, cultural and linguistic barriers, and physical limitations. Regardless of the cause for unmet need, the avoidance or lack of needed care has a negative impact on health, which may result in the deferral of treatment until a condition becomes more serious and ultimately in higher costs for both the individual and the health system.
Patient safety: Avoiding harm is the primary obligation of the health care system, yet despite the steady decline in hospital mortality in the United States, one in every three hospitalized patients may be harmed during their stay, and one in five Medicare patients are rehospitalized within 30 days of admission (IOM, 2012a). These harms often are associated with certain risk factors, such as the use of indwelling medical devices, surgical procedures, injections, contaminations of the care setting, and misuse of antibiotics. Infections acquired in care settings are estimated to have an economic cost in the billions and to contribute to tens of thousands of lives lost each year (HHS, 2014b). Ensuring that patients are safe in all of their interactions with the health care system requires a systematic, coordinated approach to the provision of care services, as well as a culture of care in which safety is a priority.
Evidence-based care: One of the central challenges for the American health system is ensuring that care delivered is based on the best available scientific evidence of appropriateness and effectiveness. While advances in medicine and health care have led to substantial gains in life expectancy and quality of life over time, a variety of estimates suggest that many people still fail to receive recommended care or they receive care not based on scientific evidence. For example, one study found that in 2003, people received only a little more than half of recommended care (McGlynn et al., 2003). It is estimated that one-third of all health care expenditures do not contribute to improving health. Careful work is needed to identify the most reliable indices that an organization is structurally, culturally, and systematically devoted to ensuring that care delivered is care most important to patient health.
Care match with patient goals: Measuring person-centered care accurately and consistently can enable better understanding and new approaches for ensuring that the health care system responds to the needs and values of patients. Systematically determining patient aims and perspectives ensures that the health care system is focusing on those aspects of care that matter most for patients. In many ways, a focus on patient goals and experience represents a cultural shift in the nation’s understanding of health and health care, one necessary to the delivery of truly effective care.
Personal spending burden: As noted earlier, the United States spends more on health care than any other country, even after adjusting for the cost of living, yet the health outcomes of a majority of its citizens are far from the best in the world. This mismatch between cost and quality has adverse impacts not only on the American economy but also on the health and economic security of individuals. Care that is too expensive can limit people’s access to care, lead people to self-ration or altogether avoid care, or limit people’s ability to purchase other goods and services of value to them. Individual spending burden provides an indication of the financial
burden imposed by health care on households and, by extension, the limits that health care may place on other areas of consumer spending.
Population spending burden: In addition to the burden placed on individuals, health care spending consumes a large portion of the nation’s gross domestic product, dwarfing the relative investments of other countries in health care. While health care costs have grown more slowly than projected over the past few years, the magnitude of spending on care remains a significant challenge for the U.S. economy and has led to a growing number of initiatives aimed at curbing costs through performance-based pay, accountable care, and other models that challenge the standard approach of payment based on volume of services. The population spending measure recommended by the Committee will generate insights for decision makers not just at the national level but also at the state, local, and institutional levels.
Individual engagement: People play an active role in their own health, as choices about diet, exercise, lifestyle, and other behaviors have well-known implications for the development of chronic disease and other health consequences. Therefore, it is critical for people to be aware of their options and responsibilities in caring for their own health and that of their families and communities. Individual engagement means that people, patients, and families play an active role not only in their care but also in the range of factors that contribute to their health and the health of others, including environment, community, economy, social well-being, and generally health-oriented community culture. Individuals who are engaged are ready to manage their own health and health care, having the knowledge, skills, and tools needed to maximize their individual and family well-being.
Community engagement: In addition to engagement in health by individuals, a health-oriented community culture, as reflected in community priorities, investments, and initiatives, is important to improving individual and community health and health care. Across the United States, communities have different levels of resources available and utilized to support people’s efforts to maintain and improve their individual and family health. For example, some communities may have better access and availability for certain health facilities and services, such as addiction treatment programs or emergency medical facilities. Similarly, social engagement, such as involvement in elections or volunteering, varies both among and within communities.
The Committee also recognizes that, while ripple or multiplier effects are anticipated as a result of their use, the 15 core measure foci identified will not be sufficient to meet all of the interests of a given organization. To begin to accommodate this challenge, the Committee also identified 39 “related priority measures” for consideration, presented in Table S-2. These measures, together with the core measures, give a more detailed view of the
TABLE S-2 Core Measure Set with Related Priority Measures
| Core Measure Focus | Related Priority Measures | |
 |
Life expectancy | Infant mortality Maternal mortality Violence and injury mortality |
 |
Well-being | Multiple chronic conditions Depression |
 |
Overweight and obesity | Activity levels Healthy eating patterns |
 |
Addictive behavior | Tobacco use Drug dependence/illicit use Alcohol dependence/misuse |
 |
Unintended pregnancy | Contraceptive use |
 |
Healthy communities | Childhood poverty rate Childhood asthma Air quality index Drinking water quality index |
 |
Preventive services | Influenza immunizations Colorectal cancer screening Breast cancer screening |
 |
Care access | Usual source of care Delay of needed care |
 |
Patient safety | Wrong-site surgery Pressure ulcers Medication reconciliation |
 |
Evidence-based care | Cardiovascular risk reduction Hypertension control Diabetes control composite Heart attack therapy protocol Stroke therapy protocol Unnecessary care composite |
 |
Care match with patient goals | Patient experience Shared decision making End-of-life/advanced care planning |
 |
Personal spending burden | Health care–related bankruptcies |
 |
Population spending burden | Total cost of care Health care spending growth |
| Core Measure Focus | Related Priority Measures | |
 |
Individual engagement | Involvement in health initiatives |
 |
Community engagement | Availability of healthy food Walkability Community health benefit agenda |
state of the health system are sufficiently granular and specific to be actionable by stakeholders as needed for their particular circumstances, and serve as example components of composite measures to be developed.
IMPLEMENTATION: PUTTING THE CORE MEASURES TO USE
The successful implementation of the core measures will depend on their relevance, reliability, and utility to stakeholders. Key considerations in the introduction of any new initiative in a complex environment should include the multiple competing priorities of stakeholders, the degree of change proposed, and the overall pace of change in the system. Progress can be accelerated by ensuring that the core measure set is applied by, and adds value to, existing health programs, stakeholders, and activities with measure requirements.
Prominent examples of such existing programs, stakeholders, and activities include the Meaningful Use Program, the Medicare Shared Savings Program, payers and purchasers, state Medicaid waivers, categorical grants, community health planning, community benefit requirements, and related health care reform provisions. Table S-3 highlights some of the ways in which the core measure set can help streamline and improve the measurement and operational efficiencies of these entities.
Especially important to successful implementation will be the leadership brought to bear in the process. Leadership will be required from virtually every level of health and health care throughout the nation. CEOs of health care organizations, payers and employers, standards organizations, and public health agencies all are centrally important to the uptake, use, and maintenance of core measures as practical tools. But in an effort of this breadth and depth, stewardship and standardization of the core analytics are key, as are the levers for accelerating application. In the Committee’s view, the Secretary of HHS, with the support and leadership of the Executive Office of the President, is the appropriate person to assume the implementation, stewardship, and governance responsibilities required for the
TABLE S-3 Utility of the Core Measure Set
| Activity | Examples of Utility of Core Measures |
| Meaningful Use Program | Provide standardized measures for every electronic health record, contributing reliability and comparability to information on health and health system performance and advancing the goal of Meaningful Use. |
| Medicare Shared Savings Program | Facilitate comparability in the application of the 33 accountable care organization (ACO) measures, and provide an important tool for gauging the extent to which an ACO is delivering on the intended care and population health outcomes. |
| Payers and purchasers | Provide a stronger, more sustained focus on outcomes with standardized tools for assessing the performance of health care organizations and clinicians and results for covered populations. |
| State Medicaid waivers | Streamline and standardize the assessment and comparison of performance in improving core health outcomes under different circumstances and forms of waiver authority and across states, counties, facilities, and time. |
| Categorical grants | Enhance comparisons across sites and time; help identify best practices across programs, communities, and states; and facilitate look-back studies to identify postgrant results on certain important outcome dimensions. |
| Community health planning | Provide well-timed assessment of progress and changing needs for attention and resources, especially important to meeting growing responsibilities of health systems for population health improvement. |
| Community benefit requirements | Focus community benefit initiatives on issues most important to outcomes, and improve prospects for targeted coordination of efforts involving multiple organizations. |
| Related health reform provisions | Increase the quality and transparency of health, health care, and cost information to assist in people’s health and health care choices. |
core measures to reach the full potential of their successful application and contribution to progress in health and health care. It is the HHS Secretary who directs the agencies most involved in the collection and use of health data; who signs off on reporting requirements and responsibilities; who is centrally positioned to convene and work with the key stakeholders; and who, as the leader most responsible for the nation’s effectiveness and efficiency in delivering better health at lower cost, has the greatest potential to unlock the capabilities of the core measure set.
A first-order implementation leadership opportunity lies in the Secretary’s ability to embed the use of the core measure set in the programs
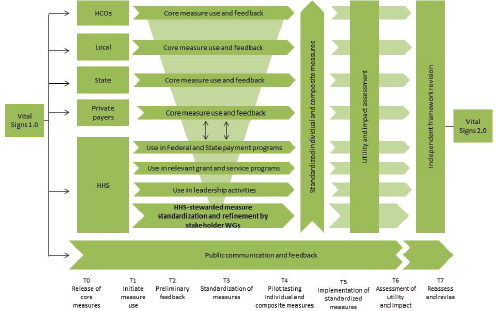
FIGURE S-2 Core measures implementation schematic.
NOTE: HCO = health care organization; HHS = U.S. Department of Health and Human Services; WG = work groups.
administered within HHS, as well as to help overcome the obstacles presented by the many entities with vested interests in maintaining the various measures and measure sets that favor their programs and priorities. As a member of the cabinet, the HHS Secretary also has the opportunity to facilitate cross-sectoral approaches to improving health by working with housing, transportation, environment, education, agriculture, and labor authorities.
Similarly, the HHS Secretary is the appropriate person to steward the eventual process of amending the core measure set. As times change, the content of the core set will need to change accordingly, and a process for periodic reassessment of its content will need to be developed. If the pragmatism of the principle of parsimony is a guide, and the Committee believes it should be, that reassessment process must be carefully designed and managed to guard against pressures to accommodate special causes. Specifically, all analyses, deliberations, and recommendations should be widely inclusive in process but completely independent of any particular stakeholder perspective in product. The often strongly expressed voices of various interests—economic, political, clinical, social, and otherwise—should be heard but should not overly influence outcomes. Measures reflect and affect
the interests and concerns of many stakeholders. Therefore, the creation of a measure set is more than a technical exercise, and its implementation requires leadership and compromise. To have the benefits of a more parsimonious and less costly measurement system, individuals and groups at different levels will need to be flexible and willing to give up certain autonomy and closely held perspectives in favor of shared benefits. Care in structuring the eventual approach to updating and amending the core set, at such time as that activity is deemed appropriate, will be vital. Presented in Figure S-2 is a schematic overview of the implementation process, illustrating the simultaneous use of the core set by multiple stakeholder groups, along with measure refinement and standardization by stakeholder groups through a development and testing process orchestrated by HHS.
FRAMING PERSPECTIVES AND RECOMMENDATIONS
Summarized in Box S-3 are framing perspectives developed in the course of the Committee’s work. These perspectives touch on the key conceptual and practical elements engaged by the core measures and their implementation, and they underpin the Committee’s recommendations. Because those recommendations are grounded in the basic notion that achieving the potential of core measures will require broad leadership from stakeholders throughout the nation, they are targeted to, and organized around, stakeholder opportunities and responsibilities. Given the health system’s complexity and the interdependence of health stakeholder communities,
BOX S-3
Committee Framing Perspectives
Measurement aims. Measurement aims to convey opportunity and priority, focus attention and activity, improve targeting and effectiveness, introduce accountability, identify what works, and help celebrate progress and motivate action to address shortfalls.
Contributions. Measurement has been at the heart of every major strategic health and health care improvement initiative, ranging from childhood immunization and high blood pressure control, to reducing tobacco use and heart attack deaths, improving the safety and effectiveness of medical and surgical services, and advancing air and water quality.
Challenges. As measurement has expanded with the growth of insights, tools, and programs, problems have emerged to limit its usefulness—lack of stan-
dardization, poor comparability, sporadic availability, and marginal institutional relevance. In addition, the large number of measures risks directing attention narrowly rather than to issues with broader-based overall impact.
Measurement burden. Meeting measurement and reporting requirements from different organizations, with sometimes parochial reference points and motives, has added administrative burdens that can be both expensive and clinically distracting, without concomitant return to the effectiveness, efficiency, or pace of health and health care improvement.
Core measure advantages. A parsimonious set of measures that is standardized, timely, available at multiple levels, and focused on issues most important to better health and health care, for individuals and the population—vital signs—will help drive attention to and action on those issues, reduce the need for many measures currently collected, and provide a stable anchor and reference point for improving the reliability and utility of measurement broadly.
Core measure content. The core measure set represents a blend of discrete and composite m¡easures of health status and health determinants (personal, behavioral, social, and environmental risks), health care quality, cost and affordability, and individual and community initiative for better health. The set includes both process and outcome measures whose commonality is their ability to reflect issues with broad impact.
Composite measures. Certain core measures are intended to be composites developed from individual elements collected discretely and reported in the aggregate to express how a family of condition-specific measures better reflects systemic performance than the individual measures. The whole is greater than the sum of the parts, and considering only the individual parts can obscure broader insights.
Relation to other measures. Application of core measures across the health and health care stakeholder communities can offer important advantages to other measurement activities by fostering more standardization, providing reliable reference points in the analysis of other data, improving reliability of trials and registries, and building patient and public familiarity and confidence in measurement. Over time, with increasing experience on the capacity of core measures to trigger broader change, some of the measures can be retired.
Committee limits. With the range and complexity of issues to be considered, no single group can, on its own, contain the necessary expertise to specify each measure’s details. The committee has identified the core set, but directly involved stakeholders are needed to specify the detailed features of the discrete standardized measures, the calculation of the composites, the field testing and refinement, and their implementation.
no single sector acting alone can bring about the transformative change needed to align and focus the measurement enterprise. Each sector faces different measurement challenges, has different roles and opportunities, and is accountable for different aspects of the system’s progress, but they all depend on the critical preconditions for success—leadership, strategy, alignment of incentives, infrastructure, culture, and continuous learning. Box S-4 presents the Committee’s recommendations.
BOX S-4
Committee’s Recommendations
The Nation
Recommendation 1: The parsimonious set of measures identified by the Committee should be widely adopted for assessing the state of America’s health and health care and the nation’s progress toward the goal of better health at lower cost.
All People—as Individuals, Family Members, Neighbors, Citizens, and Leaders
Recommendation 2: All people should work to understand and use the core measure set to assist in taking an active role in shaping their own health prospects and those of their families, their communities, and the nation.
The Federal Government
Recommendation 3: With the engagement and involvement of the Executive Office of the President, the Secretary of the U.S. Department of Health and Human Services (HHS) should use the core measure set to sharpen the focus and consistency and reduce the number and burden of measure reporting requirements in the programs administered throughout HHS, as well as throughout the nation. To this end, the Secretary should incorporate the standardized core measure set into federally administered programs, concomitantly eliminating measures for which the basic practical issues are engaged by the core set:
- HHS’s national agenda frameworks for health, including the National Quality Strategy and the National Prevention Agenda;
- the Meaningful Use Program, administered by the Centers for Medicare & Medicaid Services (CMS) and the Office of the National Coordinator (ONC), to ensure that the core measure set becomes a central element of every electronic health record;
- CMS’s accountable care organization measurement and reporting requirements;
- CMS’s strategies for promoting quality improvement and innovation in health care financing and delivery through the work of the Center for Medicare & Medicaid Innovation;
- federal health care reporting requirements;
- streamlined reporting requirements under state Medicaid waiver authority; and
- categorical health grant program management.
Recommendation 4: With the engagement and involvement of the Executive Office of the President, the Secretary of HHS should develop and implement a strategy for working with other federal and state agencies and national organizations to facilitate the use and application of the core measure set. This strategy should encompass working with
- the Secretary of the U.S. Department of the Treasury on use of the core measure set by tax-exempt hospitals and health systems in demonstrating their community benefit contributions;
- other Cabinet departments in administration of their health-related activities—for example, in social services, the environment, housing, education, transportation, nutrition, and parks and recreation;
- state and local governments and voluntary organizations in adapting use of the core measures to their needs and circumstances; and
- multiple stakeholders through the Center for Medicare & Medicaid Innovation in piloting implementation of the core measures through multilevel stakeholder initiatives.
Recommendation 5: The Secretary of HHS should establish and implement a mechanism for involving multiple expert stakeholder organizations in efforts to develop as necessary, maintain, and improve each of the core measures and the core measure set as a whole over time. The Secretary’s role should encompass stewardship of work on
- national standardization of the best current measures and related priority measures detailed in this report;
- development of the longer-term measures necessary to improve the utility and generalizability of the core measures;
- national standardization of reporting on health disparities for each of the core measures, including disparities based on race, ethnicity, gender, and socioeconomic status;
- periodic review and revision of the individual measures in response to changing circumstances; and
- periodic review and revision of the core measure set in response to changing circumstances.
Governors, Mayors, and Health Leaders
Recommendation 6: Governors, mayors, and state and local health leaders should use the core measure set to develop tailored dashboards and drive a focus on outcomes in the programs administered in their jurisdictions, and they should enlist leaders from other sectors in these efforts.
Clinicians and Health Care Delivery Organizations
Recommendation 7: Clinicians and the health care organizations in which they work should routinely assess their contributions to performance on the core measures and identify opportunities to work collaboratively with community and public health stakeholders to realize improvements in population health.
Employers and Other Community Leaders
Recommendation 8: Employers and other community leaders should use the core measures to shape, guide, and assess their incentive programs, their purchasing decisions, and their own health care interventions, including initiatives aimed at achieving transparency in health costs and outcomes and at fostering seamless interfaces between clinical care and supportive community resources.
Payers and Purchasers
Recommendation 9: Payers and purchasers of health care should use the core measures to capture data that can be used for accountability for results that matter most to personal and population health, to refine the analytics involved, and to make databases of the measures available for continuous improvement.
Standards Organizations
Recommendation 10: Measure developers, measure endorsers, and accreditors, such as the National Quality Forum (NQF), the National Committee for Quality Assurance (NCQA), and the Joint Commission, should consider how they can orient their work to reinforce the aims and purposes of the core measure set, and should work with the Secretary of HHS in refining the expression and application of the core measure set nationally.
Leadership is key at every level. In addition to the federal government, leadership on implementation of the core measure set will be required at other levels of the health system, including the community, county, and state levels, as well as within health stakeholder groups. While the core measures themselves represent a standard approach to measuring valued outcomes, achieving the required level of data reporting and use will present different challenges for different groups. A thoughtful planning process with broad input from relevant parties could support successful implementation by ensuring that responsibilities, challenges, and gaps are addressed early, and potential barriers are identified.
Incentives will need to be realigned. Many of the forces and incentives at play in the health system today are directed toward proxies or processes related to health care rather than toward the outcomes they are intended to influence. For example, fee-for-service models of care delivery incentivize the health care system to provide a high volume of services, although higher service volume does not necessarily equate to better outcomes or better quality.
Similarly, more measures do not necessarily equate to better outcomes or better quality. A strong effort is needed to reduce the number, sharpen the focus, and improve the comparability of measures. The widespread application of a limited set of standardized measures that reliably captured system outcomes would reduce the need for process measures in many instances. Moreover, core measures could be used to help better align the incentives and actions of multiple organizations at multiple levels: if they were striving for the same results, their activities would be more likely to align, or if they differed, would create natural experiments with which to assess the value of alternative routes to the same goals. But this opportunity for alignment must start with the existence of well-accepted, sound core measures of commonly sought outcomes.
Success also will require robust, interoperable infrastructure for routinely collecting and reporting key data elements. While in the short term, core measures at different levels of the health system can be assembled from unconnected data systems and with varying levels of detail and coverage, in the long term, core measures can drive advances in infrastructure development and interoperability around those measures that are of the highest priority for understanding and measuring progress in the health system. The motivation to take such steps will depend on how well the core measures—and the approaches taken to their implementation—accord with the culture and priorities of a stakeholder group or community. In particular, the core measures may meet with resistance if presented as a tool for assigning accountability or for assessing pay based on performance. Successful implementation of the core measures will depend on the ability of local leaders to
account for cultural factors that may present challenges and to ensure that the approach to implementation is tailored to cultural norms and priorities.
Finally, as noted earlier, the core measures are not intended to be static, but are expected to evolve over time, keeping pace with the needs and capabilities of the health system. Therefore, a continuous learning approach to implementation, emphasizing the dynamic nature of the measures and the implementation process, can ensure that the core measures will serve as a sustained and reliable guide to and prompt for improvement and progress through decades to come.
REFERENCES
Agaku, I. K., B. A. King, and S. R. Dube. 2014. Current cigarette smoking among adults—United States, 2005-2012. Morbidity and Mortality Weekly Report 63(2):29-34.
AHRQ (Agency for Healthcare Research and Quality). 2012. Medical Expenditure Panel Survey (MEPS): Table 4.1: Percent of persons unable or delayed in receiving needed medical care, dental care, or prescription medications, United States, 2012. Rockville, MD: AHRQ.
APHA (American Public Health Association). n.d. Health disparities: The basics. https://www.apha.org/~/media/files/pdf/factsheets/hlthdisparty_primer_final.ashx (accessed July 8, 2015).
CDC (Centers for Disease Control and Prevention). 2012a. Injury prevention and control: Data and statistics (WISQARS). Atlanta, GA: CDC.
CDC. 2012b. National, state, and local area vaccination coverage among children aged 19-35 months—United States, 2012. Morbidity and Mortality Weekly Report 62(36):733-740.
CDC. 2012c. Vital signs: Binge drinking prevelance, frequency, and intensity among adults—United States, 2010. Morbidity and Mortality Weekly Report 61(1):14-19.
CDC. 2013. Early release of selected estimates based on data from the January-June 2013 National Health Interview Survey. Atlanta, GA: CDC.
Chassin, M. R., J. M. Loeb, S. P. Schmaltz, and R. M. Wachter. 2010. Accountability measures—using measurement to promote quality improvement. New England Journal of Medicine 363(7):683-688.
Classen, D. C., R. Resar, F. Griffin, F. Federico, T. Frankel, N. Kimmel, J. C. Whittington, A. Frankel, A. Seger, and B. C. James. 2011. ‘Global trigger tool’ shows that adverse events in hospitals may be ten times greater than previously measured. Health Affairs 30(4):581-589.
CMS (Centers for Medicare & Medicaid Services). 2014. CMS measure inventory: Database with measure results already calculated. Baltimore, MD: CMS.
Fauci, A. S. 2003. HIV and AIDS: 20 years of science. Nature Medicine 9(7):839-843.
FDA (U.S. Food and Drug Adminsitration). 2011. Antiretroviral drugs used in the treatment of HIV infection. http://www.fda.gov/ForConsumers/ByAudience/ForPatientAdvocates/HIVandAIDSActivities/ucm118915.htm (accessed February 1, 2012).
Fiscella, K., P. Franks, M. R. Gold, and C. M. Clancy. 2000. Inequality in quality: Addressing socioeconomic, racial, and ethnic disparities in health care. Journal of the American Medical Association 283(19):2579-2584.
Fischl, M. A., D. D. Richman, M. H. Grieco, M. S. Gottlieb, P. A. Volberding, O. L. Laskin, J. M. Leedom, J. E. Groopman, D. Mildvan, and R. T. Schooley. 1987. The efficacy of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. New England Journal of Medicine 317(4):185-191.
Grajales, F., D. Clifford, P. Loupos, S. Okun, S. Quattrone, M. Simon, P. Wicks, and D. Henderson. 2014. Social networking sites and the continuously learning health system: A survey. https://www.iom.edu/~/media/Files/Perspectives-Files/2014/Discussion-Papers/VSRT-PatientDataSharing.pdf (accessed May 3, 2014).
Hartman, M., A. B. Martin, J. Benson, A. Catlin, and National Health Expenditure Accounts Team. 2013. National health spending in 2011: Overall growth remains low, but some payers and services show signs of acceleration. Health Affairs (Millwood) 32(1):87-99.
HHS (U.S. Department of Health and Human Services). 2011. HHS action plan to reduce racial and ethnic health disparities: A nation free of disparities in health and health care. Washington, DC: HHS.
HHS. 2014a (unpublished). Analysis by the HHS measure policy council, published with permission.
HHS. 2014b. National action plan to prevent health care-associated infections: Road map to elimination. Washington, DC: HHS.
IOM (Institute of Medicine). 2011. Digital infrastructure for the learning health system: The foundation for continuous improvement in health and health care: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2012a. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
IOM. 2012b. For the public’s health: Investing in a healthier future. Washington, DC: The National Academies Press.
IOM. 2013. Variation in health care spending: Target decision making, not geography. Washington, DC: The National Academies Press.
Landrigan, C. P., G. J. Parry, C. B. Bones, A. D. Hackbarth, D. A. Goldmann, and P. J. Sharek. 2010. Temporal trends in rates of patient harm resulting from medical care. New England Journal of Medicine 363(22):2124-2134.
Levinson, D. R. 2010. Adverse events in hospitals: National incidence among Medicare beneficiaries. Washington, DC: HHS, Office of Inspector General.
Levinson, D. R. 2012. Hospital incident reporting systems do not capture most patient harm. Washington, DC: HHS, Office of Inspector General.
McGlynn, E. A., S. M. Asch, J. Adams, J. Keesey, J. Hicks, A. DeCristofaro, and E. A. Kerr. 2003. The quality of health care delivered to adults in the United States. New England Journal of Medicine 348(26):2635-2645.
Meltzer, D. O., and J. W. Chung. 2014. The population value of quality indicator reporting: A framework for prioritizing health care performance measures. Health Affairs (Millwood) 33(1):132-139.
Meyer, G. S., E. C. Nelson, D. B. Pryor, B. James, S. J. Swensen, G. S. Kaplan, J. I. Weissberg, M. Bisognano, G. R. Yates, and G. C. Hunt. 2012. More quality measures versus measuring what matters: A call for balance and parsimony. BMJ Quality & Safety 21(11):964-968.
Nabel, E. G., and E. Braunwald. 2012. A tale of coronary artery disease and myocardial infarction. New England Journal of Medicine 366(1):54-63.
NCHS (National Center for Health Statistics). 2014. Health, United States, 2013: With special feature on prescription drugs. Atlanta, GA: CDC.
NCQA (National Committee for Quality Assurance). 2013. HEDIS 2013 measures. Washington, DC: NCQA.
NIDA (National Institute on Drug Abuse). 2008. Drug abuse costs the United States economy hundreds of billions of dollars in increased health care costs, crime, and lost productivity. Bethesda, MD: NIDA.
NQF (National Quality Forum). 2014. Quality positioning system. Washington, DC: NQF.
NRC (National Research Council) and IOM (Institute of Medicine). 2013. U.S. health in international perspective: Shorter lives, poorer health. Washington, DC: The National Academies Press.
OECD (Organisation for Economic Co-operation and Development). 2013. OECD health data 2014: How does the United States compare. http://www.oecd.org/unitedstates/Briefing-Note-UNITED-STATES-2014.pdf (accessed January 7, 2014).
Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal. 2014. Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association 311(8):806-814.
Pham, H. H., J. Coughlan, and A. S. O’Malley. 2006. The impact of quality-reporting programs on hospital operations. Health Affairs (Millwood) 25(5):1412-1422.
Russo, C. A., R. M. Andrews, and R. M. Coffey. 2006. Racial and ethnic disparities in potentially preventable hospitalizations, 2003. Healthcare Cost and Utilization Project (HCUP) Statistical Brief #10. Rockville, MD: AHRQ.
Simon, V., D. D. Ho, and Q. Abdool Karim. 2006. HIV/AIDS epidemiology, pathogenesis, prevention, and treatment. Lancet 368(9534):489-504.
USPSTF (U.S. Preventive Services Task Force). 2010. Recommendations. http://www.uspreventiveservicestaskforce.org/recommendations.htm (accessed June 11, 2014).
Ward, B. W., and J. S. Schiller. 2013. Prevalence of multiple chronic conditions among US adults: Estimates from the National Health Interview Survey, 2010. Preventing Chronic Disease 10:120203.
WHO (World Health Organization). 1946. Preamble to the constitution of the World Health Organization as adopted by the International Health Conference, New York, 19-22 June 1946; signed on 22 July 1946 by the representatives of 61 states (official records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948. Geneva: WHO.
Wicks, P., M. Massagli, J. Frost, C. Brownstein, S. Okun, T. Vaughan, R. Bradley, and J. Heywood. 2010. Sharing health data for better outcomes on patientslikeme. Journal of Medical Internet Research 12(2):e19.
































