In times of rapid change and constrained resources, progress depends on the ability to focus attention on the outcomes that matter most. Progress in any endeavor is a product of an understanding of the current state, the tools available for addressing challenges, and the resolve to take the actions required. Basic to each is the choice of measures—measures that give the best sense of progress, measures that guide actions, and measures that can be used to gauge impact.
For Americans today, health care costs and expenditures are the highest in the world, yet health outcomes and care quality are below average by many measures (OECD, 2013). If health expenditures are to be brought into alignment on behalf of better health and lower costs, keen attention and decisive actions will be required of all stakeholders—health professionals; payers; policy makers; and all individuals as patients, family members, and citizens—on what matters most. That is the focus of this report. What matters most for health and health care? What are the vital signs for the course of health and well-being in America?
Accurate information about health and health care enables success to be accurately defined, and it draws attention to gaps and shortfalls in need of attention. But the existence of too many measures can limit effectiveness. No single, objective measure set exists for the state or the priorities of the nation’s health and health care system. Rather, thousands of different measures are used to assess intermediate aspects or qualities of the four key domains of influence on health and well-being that helped frame this study—healthy people, care quality, care costs, and people’s engagement in health and health care—from emergency room wait times, to blood
pressure, to out-of-pocket costs, to life expectancy. Because standardized action-anchoring measures are relatively rare, the numerous measurements taken often are overlapping or redundant. One result is a diffusion of focus. Moreover, as the number of available measures continues to grow without concomitant gains in health outcomes, responsibilities for assessing, measuring, and reporting can become a burden in terms of cost, time, and efficiency, with marginal benefit (Meltzer and Chung, 2014). Identifying and prioritizing the most powerful of these myriad measures at each level of activity—establishing core measures—can enable the health system to work in a coordinated fashion toward a shared vision of America’s health future. Box 1-1 previews and summarizes some of the compelling issues that the Institute of Medicine (IOM) Committee responsible for this report identified and sought to address in the course of its work.
The implementation of core measures will depend on a culture of shared accountability for health. Responsibility for improving the nation’s health outcomes must be assumed by all members of the multisectoral health system, defined broadly to include the full array of sectors and entities—from clinicians and hospitals to schools and families—that influence the health of the population through their activities (IOM, 2012b). By garnering the attention of all stakeholders involved in the health system, measurement activities can be coordinated and redirected toward those outcomes that are most meaningful to all.
BOX 1-1
Committee Framing Perspectives
Measurement aims. Measurement aims to convey opportunity and priority, focus attention and activity, improve targeting and effectiveness, introduce accountability, identify what works, and help celebrate progress and motivate action to address shortfalls.
Contributions. Measurement has been at the heart of every major strategic health and health care improvement initiative, ranging from childhood immunization and high blood pressure control, to reducing tobacco use and heart attack deaths, improving the safety and effectiveness of medical and surgical services, and advancing air and water quality.
Challenges. As measurement has expanded with the growth of insights, tools, and programs, problems have emerged to limit its usefulness—lack of standardization, poor comparability, sporadic availability, and marginal institutional
relevance. In addition, the large number of measures risks directing attention narrowly rather than to issues with broader-based overall impact.
Measurement burden. Meeting measurement and reporting requirements from different organizations, with sometimes parochial reference points and motives, has added administrative burdens that can be both expensive and clinically distracting, without concomitant return to the effectiveness, efficiency, or pace of health and health care improvement.
Core measure advantages. A parsimonious set of measures that is standardized, timely, available at multiple levels, and focused on issues most important to better health and health care, for individuals and the population—vital signs—will help drive attention to and action on those issues, reduce the need for many measures currently collected, and provide a stable anchor and reference point for improving the reliability and utility of measurement broadly.
Core measure content. The core measure set represents a blend of discrete and composite m¡easures of health status and health determinants (personal, behavioral, social, and environmental risks), health care quality, cost and affordability, and individual and community initiative for better health. The set includes both process and outcome measures whose commonality is their ability to reflect issues with broad impact.
Composite measures. Certain core measures are intended to be composites developed from individual elements collected discretely and reported in the aggregate to express how a family of condition-specific measures better reflects systemic performance than the individual measures. The whole is greater than the sum of the parts, and considering only the individual parts can obscure broader insights.
Relation to other measures. Application of core measures across the health and health care stakeholder communities can offer important advantages to other measurement activities by fostering more standardization, providing reliable reference points in the analysis of other data, improving reliability of trials and registries, and building patient and public familiarity and confidence in measurement. Over time, with increasing experience on the capacity of core measures to trigger broader change, some of the measures can be retired.
Committee limits. With the range and complexity of issues to be considered, no single group can, on its own, contain the necessary expertise to specify each measure’s details. The committee has identified the core set, but directly involved stakeholders are needed to specify the detailed features of the discrete standardized measures, the calculation of the composites, the field testing and refinement, and their implementation.
MEASUREMENT IN HEALTH AND HEALTH CARE
The health and health care landscape in the United States is changing markedly for reasons that extend far beyond recent health care reform legislation, including an aging population, new science and technology, personalized medicine, shifts in the roles and perspectives of patients and clinicians, new payment models, and unsustainable costs. As a result, initiatives are under way throughout the country to promote the health of the population, improve health care quality, reduce health care costs, and engage people and communities in their health and health care. Finding the best ways to assess the results of these initiatives has become a major focus of tracking and improvement efforts, with payers collecting and analyzing claims data, hospitals tracking care quality, patients monitoring their own health through mobile apps, and public health agencies recording population-wide trends.
The need for change is further motivated by inconsistencies in overall health system performance. Multiple technological advances, including innovative imaging and diagnostic tools, new interventions for chronic disease, and new personalized treatment plans, have emerged in the health system. Yet the system is also characterized by shortfalls with respect to what is possible. Americans’ life expectancy and overall health tend to be poorer than in peer countries; the quality and safety of health care vary significantly across communities, regions, and states; health care is guided insufficiently by available evidence; and increases in health care costs generally have outpaced the nation’s economy (IOM, 2012a; McGlynn et al., 2003; NRC and IOM, 2013; OECD, 2013). The combination of these major challenges necessitates a new approach to monitoring progress and understanding whether reforms are leading to their expected results at the national, state, regional, community, and organizational levels.
A dominant feature of the health system is its fragmentation, and that fragmentation is reflected in the measures currently in use. Because of the great number and variety of organizations requiring information for claims, program performance, safety, and quality assurance purposes, the total number of health and health care measures in use today is unknown. Nonetheless, reference points such as the Centers for Medicare & Medicaid Services (CMS) Measure Inventory, which catalogs the nearly 1,700 measures in use by the U.S. Department of Health and Human Services (HHS), indicate that they number in the thousands (CMS, 2014). The National Quality Forum’s (NQF’s) measure database includes 620 measures with current NQF endorsement. The National Committee for Quality Assurance’s (NCQA’s) Healthcare Effectiveness Data and Information Set (HEDIS), used by more than 90 percent of health plans, comprises 81 different measures. And in 2010, the Joint Commission required hospitals
to provide data for measures selected from a set of 57 different inpatient measures, 31 of which were publicly reported at the time (Chassin et al., 2010). The measurement initiatives and reporting requirements included in Appendixes A and B, respectively, provide a sense of the range and diversity of measures in use today.
While many of these measures are of high quality and provide valid and useful information about health and health care, many examine only slight variations of the same focus. Furthermore, although many of the measures in use today are similar enough to serve the same purpose, they also differ enough to prevent direct comparison among the various states, institutions, or individuals interested in the same focus. The causes and consequences of this variability are explored in Chapter 2.
The current measurement enterprise is characterized by multiple initiatives across the many dimensions of the health system, with little alignment of measures or goals. Given the proliferation of measures in play, a key challenge is harmonizing and aligning measurement programs to minimize redundancies and unnecessary customization (Hussey et al., 2009; IOM, 2006; NQF, 2013; Wold, 2008). The collection and analysis of measures require significant effort, time, and resources; therefore, it is important to ensure that measurement produces the maximum amount of information for the least amount of investment in resources. Similarly, significant opportunity costs are entailed in devoting resources to inefficient, redundant, or poorly specified measurement activities, which can displace other valuable opportunities to improve health and health care. The appendixes of this report provide widely ranging examples of measurement activities, reporting requirements, and data sources that support measurement of different aspects of the health system. Yet while more than 27 organizations, 36 programs, and 1,235 individual measures are identified, they represent only a portion of the measurement activities under way.
In addition to the sheer number of measures, another challenge lies in their focus. Many measurement programs limit their focus to narrow or technical components of health care processes instead of targeting outcomes. Health care measures also often fail to capture the multiple factors that lie outside the domain of the traditional health care system but represent the most important influences on health (IOM, 2011b, 2013b; Kindig and Stoddart, 2003; McGinnis and Foege, 1993; McGinnis et al., 2002). Without understanding these factors, it will be difficult to make sustainable progress toward improving the health of the nation.
An increasing number of organizations require health care providers and others to report data on a variety of measures. These contractual requirements range from long-standing government programs, such as the reporting of vital statistics, to requirements related to specific programs, such as the Medicare Shared Savings Program for accountable care organizations (ACOs) or incentive payments for the Physician Quality Reporting System (PQRS). Reporting requirements often are aimed at assessing similar features and targets, such as readmission rates or costs of care, but with differently structured and implemented measures. As a result, hospitals and other health care organizations often are required to report redundant and overlapping measures, which imposes an additional time and resource burden. A detailed overview of major reporting requirements and their similarities and differences is provided in Appendix B.
Despite the call by organizations such as NQF and HHS for greater alignment and harmonization in health system measurement, the various measurement efforts remain broadly uncoordinated both horizontally, or across various activities, and vertically, in terms of consistent and comparable measurements at the national, state, local, and institutional levels. The Committee believes that renewed attempts to align and harmonize measures to reduce redundancies and inefficiencies may now succeed because of the significant changes that have occurred in the environment for measurement. Notably, data capture capabilities have grown rapidly, with electronic health records and other digital tools seeing increasingly widespread use (IOM, 2011a). The emerging health information technology infrastructure could support a real-time measurement system for the routine collection of information about care processes, patient needs, progress toward health goals, and individual and community health outcomes. The transformation of technology and capacity provides an opportunity to measure what matters most, enabling goals to drive measures rather than measures driving goals.
BETTER HEALTH AT LOWER COST: DOMAINS OF INFLUENCE
At the most basic level, the targets and outcomes of interest for measurement are those that reflect the greatest potential for the health and well-being of the population and each individual within it, now and in the years to come. This potential is shaped by the four key domains of influence noted above: healthy people, care quality, care costs, and people’s engagement in health and health care.
The foundational motivation of this report, and of the health system at large, is improving the health of individuals, communities, and the nation. From a population health perspective, the United States faces significant challenges, with chronic disease afflicting nearly half of all adults, violence and injury being the leading cause of death for people aged 1 to 44, and childhood obesity—a harbinger of poor health in adulthood—affecting 17 percent of America’s children (CDC, 2012; Ogden et al., 2014; Ward and Schiller, 2013). From an international perspective, the United States is below average on a range of health measures. The nation spends nearly twice the OECD average on health, yet Americans have a life expectancy of 78.7 years, below the OECD average of 80.2 years (OECD, 2013). The National Research Council (NRC)/IOM report U.S. Health in International Perspective: Shorter Lives, Poorer Health provides a broad look at the state of the nation’s health in comparison with other nations (NRC and IOM, 2013). A key finding in that report is that Americans fare worse than other developed nations in at least nine health areas: infant mortality and low birth weight, injuries and homicides, adolescent pregnancy and sexually transmitted infections, HIV and AIDS, drug-related deaths, obesity and diabetes, heart disease, chronic lung disease, and disability. Among the contributors to this American disadvantage are limitations in access to care, disparate quality of care delivered by the nation’s health systems, risky health behavior profiles, and socioeconomic disparities (NRC and IOM, 2013).
The U.S. health system is marked by significant challenges beyond the delivery of care in hospitals or provider offices. Such factors as socioeconomic status, behavior, environment, and health literacy have important implications for the health of individuals and communities. It is estimated that in the United States, 10 to 15 percent of preventable mortality is amenable to health care interventions, while approximately 40 percent of preventable deaths are attributable to behavior patterns that could potentially be modified (McGinnis et al., 2002). Paradoxically, it is estimated that 95 percent of U.S. spending on health goes to direct provision of health services, with the remaining 5 percent being spent on public health (McGinnis et al., 2002). While spending on health care is significantly higher in the United States than in other developed countries, the nation spends less, as a proportion of total spending, on public health and social programs that address those aspects of health outside of clinical care (Bradley et al., 2011). The IOM report For the Public’s Health: Investing in a Healthier Future explores in detail the state of America’s public health system and financing, and presents a case for reformulating the nation’s portfolio of health investments to focus more resources on public health and prevention as a
step toward improving health and reducing health care costs in the United States (IOM, 2012b).
A major impetus for transforming the measurement enterprise is the uneven performance of the health system, which is characterized by islands of excellence existing alongside areas in need of improvement. On the one hand, significant advances have been made in improving the public health. During the 20th century, life expectancy increased by nearly 60 percent (Guyer et al., 2000), while the mortality rate has declined by more than 60 percent over the past 75 years (Hoyert, 2012). Clinical care also has seen marked progress, including vaccines that have virtually eliminated many childhood infectious diseases; antibiotic therapies for infectious diseases; multiple interventions for cardiovascular disease, from beta blockers to percutaneous coronary intervention (PCI) and coronary artery bypass grafting; and cocktails of pharmaceutical agents tailored to the specific genetic characteristics of HIV, a microbe identified just 30 years ago (Fauci, 2003; FDA, 2011; Fischl et al., 1987; IOM, 2012a; Nabel and Braunwald, 2012; Simon et al., 2006).
At the same time, the system has compelling needs for improvement. A decade ago, in the report To Err Is Human: Building a Safer Health System, the IOM estimated that 44,000 to 98,000 people died in hospitals every year as a result of preventable medical errors (IOM, 1999). Medical errors remain common, occurring in almost one-third of hospitalized patients (Classen et al., 2011; Landrigan et al., 2010; Levinson, 2010, 2012). One recent analysis suggests that preventable harm may lead to more than 200,000 deaths per year (James, 2013). In addition, applicable research and evidence are not integrated routinely into direct patient care, with Americans receiving only about half of the care recommended by current evidence (McGlynn et al., 2003) and with a lag of years or even decades in the application of new evidence to current health practice (IOM, 2012a).
The care system also faces significant challenges in terms of access to care, with many Americans encountering limitations due to cost, transportation, wait times, and other factors that can impede their ability to receive the care they need at the right time and place. Relatedly, the care received often is limited in the extent to which it meets and accounts for the needs, priorities, and perspectives of patients.
Health care also has become increasingly complex, resulting in shortcuts in decision making and clinical processes, fragmentation of care, preventable errors, and a lack of accountability. Moreover, the health care system is characterized by inefficiencies in spending and resource use, such that an estimated 30 percent of health care spending is wasted. The 2012
IOM report Best Care at Lower Cost explores the causes and consequences of shortfalls in health care quality and outlines approaches for addressing them (IOM, 2012a).
The relative underperformance of the health system with respect to population health and health care quality has coincided with growth in health care costs that has vastly outpaced the rest of the economy, highlighting the lower levels of productivity being achieved by the health system (IOM, 2010, 2012a). Health care costs now constitute almost a fifth of the nation’s economy (Hartman et al., 2013) and pose a challenge for the budgets of the federal and state governments, businesses, and families. Costs vary significantly and with little correlation with quality among different regions of the country, states, localities, and even clinicians operating in the same practice (IOM, 2013c). Health care expenditures sometimes are only coincidentally related to care outcomes.
The costs of health care in the United States for individuals, states, and the nation pose significant challenges for the accessibility and affordability of care and raise questions as to whether the care being purchased is worth the investment. Growth in aggregate health care costs challenges the competiveness of U.S. companies and reduces take-home pay for working Americans. High out-of-pocket costs place financial pressure on individuals and families, potentially leading people to avoid or delay care or to ration personal care resources by, for example, taking medications less frequently than prescribed (Goldman et al., 2004). Health care also is a significant source of debt for many Americans (Doty et al., 2005), while health care costs are the major contributor to growth in the national debt. And demands placed on state and national budgets by health care costs may drive down investment in other critical areas impacting health, including education and the environment (McCullough et al., 2012). Although some recent trends in health care costs have been encouraging, with the pace of increases remaining lower than expected, the precise cause of this effect and whether it will continue over time are unclear (Blumenthal et al., 2013; Cutler and Sahni, 2013; Ryu et al., 2013).
Moving forward, how will the nation know whether its investments in the health care system are improving health and yielding a higher quality of life for its citizens? While the current measurement system evaluates many aspects of health care delivery, little attention is paid to measurement of the “value” of health care—better health outcomes per unit cost. No single measure of value exists, and improvements in quality or outcomes and in cost often are measured using different scales. In the absence of quality information, people tend to equate higher cost with higher quality. Moreover,
different people may assign different weight to various aspects of quality—for example, expected mobility versus length of recovery time or anticipated risk. Information should enable care choices and treatment that best match individual priorities. From a consumer perspective, therefore, price is a poor indicator of quality and, by extension, not a useful data point for choosing among services or providers. Unlocking the power of the demand side—people, patients, employers, families, and government programs—to drive progress in the health system will depend on the provision of meaningful, accurate, and comparable information about value.
People’s Engagement in Health and Health Care
In the context of legislative and payment reforms, changes in technology and access to information, new models of care delivery, and links between progress in chronic disease and patient initiative, patients, consumers, and the broader public are playing an increasing role in health and health care. Evidence suggests that people who are more actively involved with their health and health care may have improved outcomes. Research has found that people who use health-related social networking sites, such as PatientsLikeMe, TuDiabetes, and TheBody, have improved treatment adherence and a better understanding of their medical condition and feel more in control of their disease management (Grajales et al., 2014). One survey conducted in partnership with Consumer Reports found that American social media users have a high level of interest in sharing their personal data to improve the evidence base, assuming adequate privacy protections are in place. Fully 94 percent of people participating in the survey reported being willing to share their health data to help doctors improve care (Grajales et al., 2014).
Importantly, the concept of engagement pertains both to individuals and to the community. Individuals and communities share responsibility for maintaining and promoting the health of individuals and populations. Effective engagement is built on public understanding of the determinants of health. Similarly important is that determinants of health be reflected in public agendas for health improvement, which demonstrate the extent of a community’s commitment to addressing the population-wide factors in the community that shape people’s health, health care, and health prospects. While the evidence base is still evolving in this domain as it is in the domains of healthy people, care quality, and care costs, an effective strategy for marshaling greater individual and public engagement in health and health care is needed.
CHALLENGES TO MEANINGFUL MEASUREMENT
Ironically, the rapid proliferation of interest, support, and capacity for new measurement efforts for a variety of purposes—including performance assessment and improvement, public and funder reporting, and internal improvement initiatives—has blunted the effectiveness of those efforts. This situation reflects in part the fragmentation of the health care sector, as well as the range of legislatively mandated activities that involve measurement of health and health care. Absent a shared strategy, the variation inherent in thousands of disconnected measurement and accountability systems frustrates understanding of health system performance and the accomplishment of shared goals.
The Changing Measurement Landscape
Rapid change in the organizational and payment landscapes for health care has introduced new measurement responsibilities. Moreover, the introduction of multiple new models for delivering, paying for, and organizing health care has coincided with new initiatives to improve personal and population health. Developments range from ACOs, insurance marketplaces, and value-based payment programs to regional and community health improvement collaboratives. These new models and initiatives are not adequately supported by current assessment capabilities; better measurement tools are needed to support their operations and capture their successes (Schneider et al., 2011). Furthermore, the lack of alignment and comparability in the current measurement landscape limits the capacity to make meaningful comparisons among approaches or solutions and, by extension, may limit the spread of best practices and solutions for widely shared health system challenges.
Increasingly Burdensome Measurement Requirements
Tremendous growth in the development and use of measurement in the health system has led to a large number and variety of measures that, although in many cases of high quality, may create significant areas of overlap or redundancy. Health care organizations report rapidly growing requirements for the devotion of staff time and money—particularly clinician time—for measurement requirements of marginal utility in improving care and outcomes (Meyer et al., 2012). The burden of so many measurement activities and requirements can have negative consequences in terms of both the real cost of inefficiency in data collection and reporting and the opportunity costs associated with excessive spending on measurement. The growth of the measurement burden is discussed in greater detail in Chapter 2 as a key challenge for health and health care measurement.
A Blurred Focus on Priority Issues
New knowledge, alternative care delivery vehicles, the development of new incentive approaches for providers, expanded public input, and other factors are intersecting to drive rapid change in the health system. Most of these changes, however, occur in an independent and uncoordinated fashion, and the introduction of each new measure for assessing their results and outcomes tends to diffuse the ability to focus on what is most important. Fragmentation of the system leads to fragmentation of solutions, with different stakeholder groups and institutions working toward different goals with different tools and measures. For example, one study found that more than 30 percent of measures surveyed were either modifications of existing measures or homegrown, with 80 percent of programs modifying at least one measure and 40 percent of programs creating at least one new measure (Bazinsky and Bailit, 2013). This lack of coordination blurs focus, at every level, on the priority issues and outcomes with the greatest potential to improve health.
Lack of Standardization in Measuring Similar Concepts
The growth over the past decade in measures that health care organizations are required to report is due in part to redundancies and inefficiencies in data collection and measure specification, such that different organizations interested in assessing the same target or feature require different measures with different specifications. For example, one study found that across six HHS measurement programs, 61 different measures were in use for smoking cessation, 113 for HIV, 19 for obesity, and 68 for perinatal health (HHS, 2014). The result is a health measurement system that lacks standardization for the assessment and reporting of data on commonly assessed concepts.
A set of core measures is needed to promote improved health and health care. As defined in Box 1-2, core measures, for present purposes, consist of a parsimonious set of measures that provide a quantitative indication of current status on the most important elements in a given field, and that can be used as a standardized and accurate tool for informing, comparing, focusing, monitoring, and reporting change. A core measure set is not intended to replace the full range of measures in use today, rather, it is intended to enhance the focus of central health care actors on critical goals and routes toward those goals. A core measure set has the potential to accelerate improvement by concentrating attention, reducing inefficiency,
BOX 1-2
Definition of Core Measures
A parsimonious set of measures that provide a quantitative indication of current status on the most important elements in a given field, and that can be used as a standardized and accurate tool for informing, comparing, focusing, monitoring, and reporting change.
making reporting more powerful, and promoting innovation in measurement and care. In other words, a well-designed core measure set can lead to better health care at lower cost.
As detailed above, while the ability to measure discrete processes and features in health care has grown increasingly sophisticated, the availability of measures and data to enable direct comparisons of broader health outcomes and circumstances at the national, state, county, community, and institutional levels is a persistent challenge. Core measures present an opportunity to improve the nation’s ability to measure and improve performance on health, health care, affordability, and engagement by providing common points around which activities can be oriented and outcomes compared. By virtue of their central nature, core measures can drive improvements that will have a ripple effect on performance throughout the system; that is, if stakeholders align around a common set of well-designed measures, attention to improvement on those measures can lead to system-wide performance enhancement. The existence of a parsimonious core measure set also can free institutions to direct additional measurement focus and resources to issues tailored to their particular circumstances.
Relevance to Diverse Health Care Roles and Circumstances
To serve their purpose of focusing attention on overriding health care and health goals, core measures must be broad-based and high-level; they cannot, by definition, capture the particular concerns and perspectives of each actor in the health system, regardless of the validity and compelling nature of those interests. Nevertheless, the Committee believes that core measures are relevant to the work of virtually all stakeholders involved in advancing the health and health care of individuals and communities nationwide, even where the work of those actors is quite specialized and may call for legitimate, complementary measure sets. Specialists in allergy and immunology, for example, may not immediately see their primary service
activity directly reflected in the core measure set. However, their work is directly related to, and affected by, the profiles of their patients with respect to issues like well-being, healthy communities, preventive services, care access, evidence-based care, care math with patient goals, personal spending burden, and individual engagement.1 Furthermore, a core measure set that includes indicators of community health may focus the attention of these providers on the environmental and cultural factors that can so heavily influence the burden of allergic and immunologic illness among their patients. This awareness, in turn, can foster the sense of a professional opportunity to help address those community-wide influences. The process used to implement core measures must account for the requirement to make these translations into terms relevant to the many diverse health care actors.
In many cases, core measures may also need to be translated in ways that reveal their relevance and utility for actors at different levels of the health care system. For example, while the proportion of gross domestic product devoted to care provides a national view of health care spending, the concept of population spending burden is pertinent at the state, local, and institutional levels. At the state and local levels, the burden of health care spending could be compared against overall budgets or economic output, or spending levels could be assessed relative to peer states or to a performance benchmark. At the level of health care institutions, for example, the measure of total cost of care and resource use could provide actionable information on spending in the context of providing care services.
To address the increasingly urgent need for a framework, measures, and principles around which the nation might transform the efficiency, effectiveness, and utility of the health and health care measurement enterprise, the IOM, with the support of three sponsoring organizations—Blue Shield of California Foundation, the California HealthCare Foundation, and the Robert Wood Johnson Foundation—appointed the Committee on Core Metrics for Better Health at Lower Cost. The charge to the Committee, presented in Box 1-3, was essentially to articulate basic measurement needs focused on what matters most across all levels of the health system; identify a parsimonious set of core measures in those areas; describe how these core measures should relate to, shape, and enhance broader measurement efforts throughout the health system; and suggest strategic approaches
_______________
1 This sentence is an elaboration on that presented in the version originally released in prepublication format.
BOX 1-3
Charge to the IOM Committee on Core Metrics for Better Health at Lower Cost
An ad hoc committee will conduct a study and prepare a report directed at exploring measurement of individual and population health outcomes and costs, identifying fragilities and gaps in available systems, and considering approaches and priorities for developing the measures necessary for a continuously learning and improving health system. The Committee will:
- consider candidate measures suggested as reliable and representative reflections of health status, care quality, people’s engagement and experience, and care costs for individuals and populations;
- identify current reporting requirements related to progress in health status, health care access and quality, people’s engagement and experience, costs of health care, and public health;
- identify data systems currently used to monitor progress on these parameters at national, state, local, organizational, and individual levels;
- establish criteria to guide the development and selection of the measures most important to guide current and future-oriented action;
- propose a basic, minimum slate of core metrics for use as sentinel indices of performance at various levels with respect to the key elements of health and health care progress: people’s engagement and experience, quality, cost, and health;
- indicate how these core indices should relate to, inform, and enhance the development, use, and reporting on more detailed measures tailored to various specific conditions and circumstances;
- identify needs, opportunities, and priorities for developing and maintaining the measurement capacity necessary for optimal use of the proposed core metrics; and
- recommend an approach and governance options for continuously refining and improving the relevance and utility of the metrics over time and at all levels.
to implementation. The ultimate goal of the Committee’s work was to spur widespread improvement in health and health care through a more aligned and efficient measurement system. The breadth of the Committee’s charge reflected the extent of opportunities to achieve this goal.
The Committee convened to carry out this study comprised 21 individuals with a broad range of expertise, including health economics and policy, population health, health care delivery and safety net populations,
state and community health improvement, health measurement, and information technology and data infrastructure, as well as individuals who understand the perspectives of health care payers and purchasers, clinicians, researchers, and patients and consumers. Committee members’ biographies are presented in Appendix E.
Recognizing that success depends on concerted actions by all stakeholders in the system, the Committee sought input and feedback from a broad range of individuals and organizations. Staff contacted 126 leading health organizations to solicit their thoughts on the current state of measurement, challenges limiting its potential, and opportunities that could be transformative. The resources received from these organizations informed the Committee’s deliberations on the needs and opportunities in the field. The Committee also held open sessions at three of four of its meetings, during which stakeholders and practitioners from various organizations with ties to health and health care measurement—such as NQF, NCQA, CMS, the Agency for Healthcare Research and Quality (AHRQ), the Centers for Disease Control and Prevention (CDC), and the Office of the Secretary of HHS—provided additional perspective and background. Organizations representing patient and consumer perspectives also provided important input for these discussions.
The Committee deliberated during four in-person meetings and multiple conference calls over 2013 and 2014. The Committee’s overarching approach to identifying core measures is illustrated in Figure 1-1. Its initial deliberations focused on clarifying the scope of the study and gathering input, while later meetings focused on synthesizing conclusions and formulating recommendations that would move measurement forward. To accelerate its efforts, the Committee drew on related IOM work described below, particularly an earlier IOM workshop on the core measurement needs for better care, better health, and lower costs (IOM, 2013a). Furthermore, staff and Committee members reviewed the evidence related to measurement and
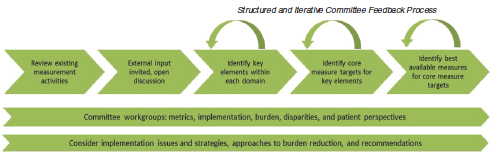
FIGURE 1-1 The Committee’s approach to identifying the core measure set.
case studies of measurement initiatives to inform the findings, conclusions, and recommendations presented in this report.
This report references and builds on the work of a wide range of other individuals and organizations devoted to addressing the nation’s changing health and health care measurement needs. These include activities stewarded through the HHS Secretary, the Secretary’s Prevention Agenda and Healthy People Leading Health Indicators, the National Quality Strategy, the Joint Commission, the Institute for Healthcare Improvement, and the organizations mentioned above (CMS, CDC, AHRQ, NQF, and NCQA). These and other measurement activities are discussed in Chapter 2.
RELATED WORK OF THE INSTITUTE OF MEDICINE
The IOM has produced several reports aimed at strengthening the focus of the national health agenda on matters of compelling urgency. These reports have explored approaches to measurement activities ranging from specific assessments of the needs for health care and public health to surveys that cut across the entire health system. In so doing, these reports have drawn attention to the gaps in the nation’s measurement capabilities and outlined opportunities for improvement.
At various levels, the present report draws on the broader foundation of the IOM work articulating a vision and strategy for improving health and the health care system. The 1999 report To Err Is Human: Building a Safer Health System and the 2001 report Crossing the Quality Chasm: A New Health System for the 21st Century together highlight some of the most significant challenges facing the health system and outline a potential path forward in terms of governance, health practice, and health culture (IOM, 1999, 2001). Those reports galvanized the nation’s attention to focus on the deficiencies in health care and the importance of engaging them directly.
Also related is the work of the IOM Roundtable on Value & Science-Driven Health Care in bringing together the nation’s health leaders with the common purpose of accelerating achievement of the health system’s full potential. The 12-volume Learning Health System series produced under the Roundtable includes discussion and ideas from a series of 15 workshops covering issues that range from research and technology infrastructure to leadership to patient engagement.
More recently, the 2012 IOM report Best Care at Lower Cost: The Path to Continuously Learning Health Care in America was issued. This report charts opportunities for marshaling advances in science and technology, as well as the market forces of increased public and patient involvement, to drive the health system toward the culture and practice of real-time and continuous improvement in the effectiveness and efficiency of care (IOM,
2012a). The present report outlines what steps are necessary and possible to track the nation’s progress toward the transformation envisioned in Best Care at Lower Cost.
Another recent effort related directly to the work of this Committee was the conduct of an IOM workshop and production of a workshop summary on the core measurement needs for better population health, improved quality of health care, and lower health care costs. This 2-day workshop garnered perspectives from patients and consumers, health care delivery organizations, clinicians, public health experts, researchers, purchasers and payers, health economists, measure developers, regulators, clinical researchers, experts in health information technology, state governments, community organizations, and regional collaboratives. The workshop discussions drew on existing measurement initiatives, identified the limitations of current measurement efforts, and began to identify a framework for core measures and the necessary infrastructure for implementation. The workshop summary, Core Measurement Needs for Better Care, Better Health, and Lower Costs: Measures That Matter, summarizes those discussions and served as a first step in the process of identifying a common core measure set suitable for assessing the health system (IOM, 2013a).
In 2006, the IOM released Performance Measurement: Accelerating Improvement. The purpose of that report was to build the measurement infrastructure needed to advance the goals of the earlier Quality Chasm report (IOM, 2001). To that end, the authoring Committee selected measures that would support quality improvement across the health care enterprise and identified the infrastructure necessary to support the implementation of those measures at the regional and national levels. The report endorses a starter set of performance measures with a strong evidence base, most of which were drawn from measure sets and individual measures acknowledged by major stakeholder groups. The report also analyzes the gaps in current measurement capabilities, identifying the need for measures in several areas, including efficiency, equity, and patient-centeredness; longitudinal care and care transitions; systems-level measures; and measures that can be used to assess care across multiple clinicians and organizations (IOM, 2006).
The 2002 IOM study Guidance for the National Healthcare Disparities Report was developed to provide guidance to AHRQ as it worked to improve the measurement and reporting of data on health disparities. The report highlights a variety of key issues relevant to core measures and presents potential approaches for measuring disparities consistently and accurately, as well as improving the availability of data on disparities for a range of valuable health measures (IOM, 2002).
Another prior effort to identify a set of core measures is documented in the 2009 IOM letter report State of the USA Health Indicators. This
report was intended to support the nonprofit State of the USA Inc., which was building an Internet site to assess the nation’s progress along several dimensions, including education, environment, and health. The Committee responsible for that report proposed 20 measures that could provide a broad picture of health and health care, encompassing overarching indicators of health, social and environmental factors influencing health, health behaviors and risks, and the quality and cost of health care. The report emphasizes that these health measures should not be considered in isolation; rather, the nonprofit should show the interconnections between health and the other areas it is tracking, such as education and environment (IOM, 2009).
The IOM explores the social and environmental factors that affect overall health in the 2010 report For the Public’s Health: The Role of Measurement in Action and Accountability. The authoring Committee found that the nation did not have the necessary tools to assess and respond to these factors, and that the lack of such information limited the nation’s ability to improve Americans’ health. To address these challenges, the Committee recommends that HHS provide greater leadership, coordination, and guidance on population health information and statistics; that HHS lead the creation of a core measure set focused on priority health outcomes to improve alignment and enable comparisons among different communities, regions, and states; and that the nation adopt a single summary measure of population health that yields an overall picture of health and well-being at multiple levels. These recommendations were intended to provide greater understanding of the factors that influence health and to galvanize action toward better health (IOM, 2011b).
In 2013, the IOM released an examination of HHS’s public health quality initiatives and the Leading Health Indicators for Healthy People 2020, with a particular focus on measures that can promote integration of clinical care and public health. The report Toward Quality Measures for Population Health and the Leading Health Indicators suggests that every community should use measures to assess progress on the Leading Health Indicators and recommends a systematic approach to developing and managing a portfolio of measures that span the entire health system. The authoring Committee also developed a logic model that shows the relationships among social, environmental, and behavioral factors; resources and community capabilities; interventions; and overall health outcomes. To show how this model translates to practice, the report includes four case studies illustrating how the model could be used to demonstrate the pathways from structure to process to outcomes and guide the development of quality measures (IOM, 2013b).
In a complementary project, a series of IOM consensus studies has focused on integrating population health factors into electronic health
records. The Phase 1 report, Capturing Social and Behavioral Domains in Electronic Health Records, identifies various domains and potential candidates for assessing such issues as socioeconomic status, race and ethnicity, sexuality, and health behaviors in the context of clinical records (IOM, 2014a). The Phase 2 report identifies with greater specificity 12 measures related to the selected domains and addresses issues related to incorporating these elements into electronic health records in a standardized way (IOM, 2014b). These recommended measures include four that are already in widespread use—race/ethnicity, tobacco use, alcohol use, and residential address—as well as an additional eight social and behavioral measures—education, financial resource strain, stress, depression, physical activity, social isolation, exposure to violence, and neighborhood median household income.
These many prior IOM activities provided a strong foundation for the assessment and recommendations presented in this report.
CORE MEASURES AND ISSUES: PREVIEW
A brief preview of the Committee’s recommended core measure set and approaches to certain issues is warranted. Presented in Table 1-1 is the analytic framework for the core measures. Because the scope of concepts, activities, and priorities is broad for each aspect of the four domains outlined above (healthy people, care quality, care costs, and people’s engagement in health and health care), the Committee’s working assumptions on the domains, their key elements, and associated core measure foci are presented below. Also summarized are the approaches taken to the issues of best current measures, related priority measures, disparities, and implementation, which are presented in detail in Chapter 4.
The Committee’s charge was to identify measures that best reflect healthy people, care quality, care costs, and people’s engagement in health and health care. Implicit in that charge is the notion that while the foundational societal aspiration is healthy people, population health is a product of the dynamics in each of these vital and interrelated domains of influence on health. The goal of healthy people cannot be achieved without quality care or engaged people. Gains in the quality of care and population health cannot be sustained without affordable care. And care quality and affordability cannot be optimized without engaged people.
Facilitating progress within and among these domains of influence depends on how their component elements are addressed. Although they may be characterized in different ways and often are interrelated at some level, each of the key elements presented in Table 1-1 is central to progress in health and health care. Quality of life is a goal basic to every individual, and although length of life is not an immutable goal for every person at every stage of life, it is an accepted standard for the overall health of populations. It also is now well established that the health of populations is substantially shaped by factors outside of health care, including patterns of health-related behaviors and social circumstances such as physical environments and socioeconomic status. High-quality care is a function of the interplay among access to care, prevention, and appropriate treatment.
The Committee proposes the core measure set presented in Table 1-1. Each core measure focus identified by the Committee represents an important focus for action at the national, state, local, and even institutional levels.
Measure development and standardization were beyond the scope of the Committee’s charge. However, to accelerate the development and
TABLE 1-1 Core Measure Framework
| Domain | Key Element | Core Measure Focus |
| Healthy people | Length of life | Life expectancy |
| Quality of life | Well-being | |
| Healthy behaviors | Overweight and obesity | |
| Addictive behavior | ||
| Unintended pregnancy | ||
| Healthy social circumstances | Healthy communities | |
| Care quality | Prevention | Preventive services |
| Access to care | Care access | |
| Safe care | Patient safety | |
| Appropriate treatment | Evidence-based care | |
| Person-centered care | Care match with patient goals | |
| Care cost | Affordability | Personal spending burden |
| Sustainability | Population spending burden | |
| Engaged people | Individual engagement | Individual engagement |
| Community engagement | Community engagement | |
application of a fully specified core measure set, the Committee has specified what in its judgment is the best currently available measure for each core measure focus. This measure set, while imperfect, represents in the Committee’s view a powerful starting set of “vital signs” for tracking progress toward improved health and health care in the United States. The Committee believes further that the core measure set recommended herein comprises the vital signs on the status and progress of the nation’s health and health care, that a single measure can be chosen or developed for each of the core measure foci within each domain of influence, and that the development of a standardized measure is essential for each focus. The Committee also believes that, when applied, attention to these core measure foci will have the multiplier effect of improving performance broadly throughout the health and health care organizations engaged in their use.
As noted above, the Committee has not specified each core measure in detail because, with few exceptions, the collaborative process of definition and refinement needed to develop widely accepted and fully specified measures was beyond the resources and scope of this study. Standardized measurement approaches exist for life expectancy and overweight and obesity, but such refinement has not yet been accomplished for measures in many other key areas, such as well-being, addictive behavior, healthy communities, evidence-based care, spending burden, and individual and community engagement. This is particularly true for individual and community engagement measures. The Committee focused considerable discussion on this focus, reflecting the relatively nascent state of conceptual and technical development of measures in this field. Committee members’ perspectives were divided on the question of whether the strength and precision of the definitions and measures available for engagement warranted their inclusion alongside the domains of health, care quality, and care cost. Still, there was strong sentiment within the Committee that individual and community engagement are significant determinants of health and health care, clearly working in service to and as elements in the success of activities directed at the Triple Aim of better health, better care, and lower costs. Nonetheless, considerable definitional and analytic work will be required to develop practical measures that can reliably capture the extent to which individuals are prepared for and engage in effective participation in health and health care planning, delivery, and improvement. Additionally, research is needed to explore how levers available for community-wide action are being employed effectively for improvement in matters of central importance to the health of the population. Given the identification of engagement as a domain in the Committee’s statement of task and the acknowledgment
within the Committee that engagement represents an important—if underdeveloped—element of the changing landscape of health, the Committee’s deliberations were guided by the four domains of health, care quality, care cost, and engagement.
Because most of the core measure foci shown in Table 1-1 are not supported by standardized measures accessible for application at every level of the health system, the Committee also specified, and presents for consideration in Chapter 4, best current measures for the core measure foci. Examples include the use of childhood immunization as a best current measure of the delivery of preventive services and self-reported health status as an indicator of well-being. Many of these best current measures are currently imperfect because of limitations in scope, reliability, generalizability, or conceptual boundary and will require substantial work. For this reason, the Committee recommends in this report that, as stakeholders at various levels try out their own proxies for the core measure foci in the short term, the Secretary of HHS steward a broadly inclusive process to marshal the nation’s experience and expertise in the development of the standardized set of core measure foci, see Chapter 5.
The Committee recognized that, while ripple or multiplier effects are anticipated as a result of the use of the 15 core measure foci identified, those foci will not be sufficient to serve all of the interests of given organizations. To begin to address this challenge, the Committee also identified 39 “related priority measures” for consideration, presented in Chapter 4. These measures, together with the core measures, give a more detailed view of the health system and are sufficiently granular and specific to be actionable by stakeholders as needed for their particular circumstances. The Committee believes that, as with the core measure foci, specification and stewardship of standardized approaches ought also to be undertaken for these related measures, although as a follow-on activity to that for the core measure foci.
The Committee presents in Chapter 4 and in discussion throughout this report data available for the core measure foci, and well beyond, that highlight the substantial disparities among subpopulations in the United States with respect to health status and health care. These include disparities based on race, ethnicity, income, education, gender, geography, and urban or rural
location. In the aggregate, this issue represents one of the greatest single health and health care challenges to the nation. Accordingly, the Committee considered recommending the development of a separate core measure aimed specifically at disparities. Instead, because the issue is so pervasive, the Committee discusses disparities in conjunction with each core measure.
The Committee emphasizes that the process of refining, applying, and implementing the core measures is fundamental to success. Although face validity was a central criterion in identifying each measure, these core measures will not implement themselves. A carefully designed effort under the stewardship of the HHS Secretary will be needed to focus the nation’s attention in a manner that will accelerate progress across the board. Therefore, the Committee’s recommendations place particular emphasis on the roles, responsibilities, and opportunities for implementation—the critical features and actions necessary to achieve adoption and application of the core measures. At the same time, the multilevel and broad-based features of the implementation activities identified by the Committee are also intended to reflect both content and processes that are as catalytic and open as possible.
This report summarizes the Committee’s deliberations on the issues, options, and successful strategies with respect to advancing measurement and enhancing collaborative efforts around measurement in the four domains of healthy people, quality of care, costs of care, and people’s engagement in health and health care. The evidence is distilled into detailed findings throughout the report that serve as the basis for the Committee’s conclusions and recommendations. Each recommendation describes a key goal for advancing measurement and is accompanied by specific strategies that stakeholders should undertake in implementing the recommendation. Additional actions will be needed from multiple stakeholders to sustain and advance the implementation process.
Following this introduction are five chapters. Chapter 2 describes the current use of measurement in health and health care in America. It includes discussion of existing measurement purposes and requirements, limitations in current measurement capacity, and the burden of measurement on the care system.
Chapter 3 provides an introduction and overview for the core measure set proposed by the Committee, including a description of the Committee’s deliberative process in approaching and completing the task of identifying these measures. Additionally, this chapter considers the potential benefits of
adopting core measures, how the focus of measurement can be expanded to encompass concepts meaningful to patients and the public, and desirable characteristics for a core measure set.
Chapter 4 presents the proposed core measure set, along with best current measures for use while the process of refining these measures is under way. This chapter serves essentially as a handbook for the core measures by providing details on each of the measures in turn, including the rationale for its selection, as well as the availability and quality of current data and measures and the path forward for improvement.
Chapter 5 outlines issues and approaches with respect to implementing the measure set and ensuring that it is updated and improved over time. Included is discussion of potential data production for dissemination of the core measures, as well as the uses envisioned for the measures by the Committee across stakeholder groups. Key challenges for stakeholders are identified, and approaches for integrating the core measures into existing programs, policies, and reporting activities and requirements are discussed.
The report concludes with an action agenda in Chapter 6 that summarizes the Committee’s findings, conclusions, and recommended actions for different stakeholder groups to achieve improved alignment and focus in measurement. This chapter also identifies the contextual features important for successful implementation of the core measures.
Finally, the report’s appendixes present prominent measurement initiatives, the landscape for reporting initiatives, and current data capabilities.
Bazinsky, K. R., and M. Bailit. 2013. The significant lack of alignment across state and regional health measure sets. http://www.bailit-health.com/articles/091113_bhp_measuresbrief.pdf (accessed December 6, 2013).
Blumenthal, D., K. Stremikis, and D. Cutler. 2013. Health care spending—a giant slain or sleeping? New England Journal of Medicine 369(26):2551-2557.
Bradley, E. H., B. R. Elkins, J. Herrin, and B. Elbel. 2011. Health and social services expenditures: Associations with health outcomes. BMJ Quality & Safety 20(10):826-831.
CDC (Centers for Disease Control and Prevention). 2012. Injury prevention and control: Data and statistics (WISQARS). Atlanta, GA: CDC.
Chassin, M. R., J. M. Loeb, S. P. Schmaltz, and R. M. Wachter. 2010. Accountability measures—using measurement to promote quality improvement. New England Journal of Medicine 363(7):683-688.
Classen, D. C., R. Resar, F. Griffin, F. Federico, T. Frankel, N. Kimmel, J. C. Whittington, A. Frankel, A. Seger, and B. C. James. 2011. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Affairs (Millwood) 30(4):581-589.
CMS (Centers for Medicare & Medicaid Services). 2014. CMS measure inventory: Database with measure results already calculated. Baltimore, MD: CMS.
Cutler, D. M., and N. R. Sahni. 2013. If slow rate of health care spending growth persists, projections may be off by $770 billion. Health Affairs (Millwood) 32(5):841-850.
Doty, M. M., J. N. Edwards, and A. L. Holmgren. 2005. Seeing red: Americans driven into debt by medical bills. Results from a national survey. Issue Brief (Commonwealth Fund) (837):1-12.
Fauci, A. S. 2003. HIV and AIDS: 20 years of science. Nature Medicine 9(7):839-843.
FDA (U.S. Food and Drug Administration). 2011. Antiretroviral drugs used in the treatment of HIV infection. http://www.fda.gov/ForConsumers/ByAudience/ForPatientAdvocates/HIVandAIDSActivities/ucm118915.htm (accessed February 1, 2012).
Fischl, M. A., D. D. Richman, M. H. Grieco, M. S. Gottlieb, P. A. Volberding, O. L. Laskin, J. M. Leedom, J. E. Groopman, D. Mildvan, and R. T. Schooley. 1987. The efficacy of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. New England Journal of Medicine 317(4):185-191.
Goldman, D. P., G. F. Joyce, J. J. Escarce, J. E. Pace, M. D. Solomon, M. Laouri, P. B. Landsman, and S. M. Teutsch. 2004. Pharmacy benefits and the use of drugs by the chronically ill. Journal of the American Medical Association 291(19):2344-2350.
Grajales, F., D. Clifford, P. Loupos, S. Okun, S. Quattrone, M. Simon, P. Wicks, and D. Henderson. 2014. Social networking sites and the continuously learning health system: A survey. http://www.iom.edu/Global/Perspectives/2014/~/media/Files/PerspectivesFiles/2014/Discussion-Papers/VSRT-PatientDataSharing.pdf (accessed January 5, 2015).
Guyer, B., M. A. Freedman, D. M. Strobino, and E. J. Sondik. 2000. Annual summary of vital statistics: Trends in the health of Americans during the 20th century. Pediatrics 106(6):1307-1317.
Hartman, M., A. B. Martin, J. Benson, A. Catlin, and National Health Expenditure Accounts Team. 2013. National health spending in 2011: Overall growth remains low, but some payers and services show signs of acceleration. Health Affairs (Millwood) 32(1):87-99.
HHS (U.S. Department of Health and Human Services). 2014 (unpublished). Analysis by the HHS Measure Policy Council, published with permission.
Hoyert, D. L. 2012. 75 years of mortality in the United States, 1935-2010. NCHS Data Brief (88):1-8.
Hussey, P. S., H. de Vries, J. Romley, M. C. Wang, S. S. Chen, P. G. Shekelle, and E. A. McGlynn. 2009. A systematic review of health care efficiency measures. Health Services Research 44(3):784-805.
IOM (Institute of Medicine). 1999. To err is human: Building a safer health system. Washington, DC: National Academy Press.
IOM. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2002. Guidance for the national healthcare disparities report. Washington, DC: The National Academies Press.
IOM. 2006. Performance measurement: Accelerating improvement. Washington, DC: The National Academies Press.
IOM. 2009. State of the USA health indicators: Letter report. Washington, DC: The National Academies Press.
IOM. 2010. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Washington, DC: The National Academies Press.
IOM. 2011a. Digital infrastructure for the learning health system: The foundation for continuous improvement in health and health care: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2011b. For the public’s health: The role of measurement in action and accountability. Washington, DC: The National Academies Press.
IOM. 2012a. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
IOM. 2012b. For the public’s health: Investing in a healthier future. Washington, DC: The National Academies Press.
IOM. 2013a. Core measurement needs for better care, better health, and lower costs: Counting what counts: Workshop summary. Washington, DC: The National Academies Press.
IOM. 2013b. Toward quality measures for population health and the leading health indicators. Washington, DC: The National Academies Press.
IOM. 2013c. Variation in health care spending: Target decision making, not geography. Washington, DC: The National Academies Press.
IOM. 2014a. Capturing social and behavioral domains and measures in electronic health records: Phase 1. Washington, DC: The National Academies Press.
IOM. 2014b. Capturing social and behavioral domains in electronic health records: Phase 2. Washington, DC: The National Academies Press.
James, J. T. 2013. A new, evidence-based estimate of patient harms associated with hospital care. Journal of Patient Safety 9(3):122-128.
Kindig, D., and G. Stoddart. 2003. What is population health? American Journal of Public Health 93(3):380-383.
Landrigan, C. P., G. J. Parry, C. B. Bones, A. D. Hackbarth, D. A. Goldmann, and P. J. Sharek. 2010. Temporal trends in rates of patient harm resulting from medical care. New England Journal of Medicine 363(22):2124-2134.
Levinson, D. R. 2010. Adverse events in hospitals: National incidence among Medicare beneficiaries. Washington, DC: HHS, Office of Inspector General.
Levinson, D. R. 2012. Hospital incident reporting systems do not capture most patient harm. Washington, DC: HHS, Office of Inspector General.
McCullough, J. C., F. J. Zimmerman, J. E. Fielding, and S. M. Teutsch. 2012. A health dividend for America: The opportunity cost of excess medical expenditures. American Journal of Preventive Medicine 43(6):650-654.
McGinnis, J. M., and W. H. Foege. 1993. Actual causes of death in the United States. Journal of the American Medical Association 270(18):2207-2212.
McGinnis, J. M., P. Williams-Russo, and J. R. Knickman. 2002. The case for more active policy attention to health promotion. Health Affairs (Millwood) 21(2):78-93.
McGlynn, E. A., S. M. Asch, J. Adams, J. Keesey, J. Hicks, A. DeCristofaro, and E. A. Kerr. 2003. The quality of health care delivered to adults in the United States. New England Journal of Medicine 348(26):2635-2645.
Meltzer, D. O., and J. W. Chung. 2014. The population value of quality indicator reporting: A framework for prioritizing health care performance measures. Health Affairs (Millwood) 33(1):132-139.
Meyer, G. S., E. C. Nelson, D. B. Pryor, B. James, S. J. Swensen, G. S. Kaplan, J. I. Weissberg, M. Bisognano, G. R. Yates, and G. C. Hunt. 2012. More quality measures versus measuring what matters: A call for balance and parsimony. BMJ Quality & Safety 21(11):964-968.
Nabel, E. G., and E. Braunwald. 2012. A tale of coronary artery disease and myocardial infarction. New England Journal of Medicine 366(1):54-63.
NQF (National Quality Forum). 2013. Report from the National Quality Forum: 2012 NQF measure gap analysis. Washington, DC: NQF.
NRC (National Research Council) and IOM (Institute of Medicine). 2013. U.S. health in international perspective: Shorter lives, poorer health. Washington, DC: The National Academies Press.
OECD (Organisation for Economic Co-operation and Development). 2013. OECD health data 2014: How does the United States compare. http://www.oecd.org/unitedstates/Briefing-Note-USA-2013.pdf (accessed December 9, 2013).
Ogden, C. L., M. D. Carroll, B. K. Kit, and K. M. Flegal. 2014. Prevalence of childhood and adult obesity in the United States, 2011-2012. Journal of the American Medical Association 311(8):806-814.
Ryu, A. J., T. B. Gibson, M. R. McKellar, and M. E. Chernew. 2013. The slowdown in health care spending in 2009-11 reflected factors other than the weak economy and thus may persist. Health Affairs (Millwood) 32(5):835-840.
Schneider, E. C., P. S. Hussey, and C. Schnyer. 2011. Payment reform: Analysis of models and performance measurement implications. Santa Monica, CA: RAND Corporation.
Simon, V., D. D. Ho, and Q. Abdool Karim. 2006. HIV/AIDS epidemiology, pathogenesis, prevention, and treatment. The Lancet 368(9534):489-504.
Ward, B. W., and J. S. Schiller. 2013. Prevalence of multiple chronic conditions among US adults: Estimates from the National Health Interview Survey, 2010. Preventing Chronic Disease 10:120203.
Wold, C. 2008. Health indicators: A review of reports currently in use. Washington, DC: The State of the USA.




























