A 2011 report by the National Research Council (NRC) declared, “Health care is coming home” (NRC, 2011, p. 9). The report further noted that although the costs of care are one driver of this change, the delivery of health care at home is valued by individuals and can promote healthy living and well-being when it is managed well. Living independently at home is a priority for many, especially individuals who are aging with or into disability. However, both the complexity and the intensity of the health care services provided in home settings are increasing.
Additionally, individuals with disabilities, chronic conditions, and functional impairments need a range of services and supports to keep living independently. However, there often is not a strong link between medical care provided in the home and the necessary social services and supports for independent living. Home health agencies and others are rising to the challenges of meeting the needs and demands of these populations to stay at home by exploring alternative models of care and payment approaches, the best use of their workforces, and technologies that can enhance independent living. All of these challenges and opportunities lead to the consideration of how home health care fits into the future health care system overall.
On September 30 and October 1, 2014, the Institute of Medicine
______________
1 The planning committee’s role was limited to planning the workshop, and the workshop summary has been prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of the individual presenters and participants and are not necessarily endorsed or verified by the IOM or the NRC, and they should not be construed as reflecting any group consensus.
(IOM) and the NRC convened a public workshop on the future of home health care. The workshop was supported by a group of sponsors (see p. ii of this workshop summary) and hosted by the IOM-NRC Forum on Aging, Disability, and Independence,2 an ongoing neutral venue in which stakeholders in government, academia, industry, philanthropic organizations, and consumer groups meet to discuss the intersection of aging and disability. The workshop itself was planned by an ad hoc committee. (See Box 1-1 for the committee’s statement of task.) Under the NRC guidelines, workshops are designed as convening activities and do not result in any formal findings, conclusions, or recommendations. Furthermore, the workshop summary reflects what transpired at the workshop and does not present any consensus views of either the planning committee or workshop participants. The purpose of this summary is to capture important points raised by the individual speakers and workshop participants. A webcast of the workshop is also available.3
The workshop brought together stakeholders from a spectrum of public and private organizations and thought leaders for discussions to improve their understanding of the current and potential future role of home health care in supporting aging in place and in helping high-risk adults (particularly older adults) with chronic illnesses and disabilities to receive health care and long-term services and supports (LTSS)4 in their homes and avoid potentially higher-cost, institution-based care. The workshop planners were especially interested in evaluating how home health care fits into evolving models of health care delivery and payment resulting from the Patient Protection and Affordable Care Act of 20105 and other policies, including those resulting from potential changes in the Medicare home health care benefit (which was designed nearly 50 years ago). In addition, the workshop sought to explore the key policy reforms and investments in workforces, technologies, and research that will be needed to maximize the value of home health care and to describe the ways in which research can help clarify the value of these services.
In this workshop, as in other settings, terms such as home health care, home health, home health services, home care, home-based care, and other
______________
2 See www.iom.edu/ADIForum (accessed December 5, 2014).
3 See http://www.iom.edu/activities/aging/futurehomehealthcare/2014-sep-30.aspx (accessed December 24, 2014).
4 “Long-term services and supports” are also referred to as “long-term care,” but the former term is now preferred as a more accurate and comprehensive description of the kinds of assistance needed by people with disabilities. This workshop summary generally uses the term LTSS, but it refers to long-term care in contexts in which the term has become standard, such as long-term care facilities or long-term care insurance.
5 Patient Protection and Affordable Care Act of 2010, Public Law 111-148, 111th Cong., 2nd sess. (March 23, 2010).
BOX 1-1
Statement of Task
An ad hoc committee will plan a 2-day public workshop, bringing together a spectrum of public and private stakeholders and thought leaders to improve understanding of (1) the current role of Medicare home health care in supporting aging in place and in helping high-risk, chronically ill, and disabled Americans receive health care in their communities; (2) the evolving role of Medicare home health care in caring for Americans in the future, including how to integrate Medicare home health care into new models for the delivery of care and the future health care marketplace; (3) the key policy reforms and investments in workforces, technologies, and research needed to leverage the value of home health care to support older Americans; and (4) research priorities that can help clarify the value of home health care.
The workshop will feature invited presentations and discussions that will
- Provide an overview of the current state of home health care, including the relevance of Medicare-certified home health agencies in supporting community-based care and healthy aging in place, and an understanding of current barriers to home health care (e.g., budgetary constraints, definitions, practice-level restrictions, and the absence of meaningful use incentives);
- Inform understanding of the evolving role of Medicare home health care and its role in the future by examining and exploring innovative models for the delivery of care that involve Medicare-certified home health agencies, home health care professionals, and other aspects of health care at home to achieve the triple aim of improving the patient experience of care (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of health care; and
- Inform understanding of how to facilitate the future role of home health care in achieving the triple aim by examining and exploring
- The infrastructure needs for home health care, the health care system as a whole, and the overall environment;
- The workforce needs, that is, the supply of professionals that are educated and trained to deliver home health care;
- The research and measurement needs for home health care to provide high-quality and efficient care and to allow healthy aging;
- The technology needs (including mobile, digital, monitoring, health information, therapeutic, and diagnostic needs) to enable and support the health care of patients at home; and
- The policy reforms (including funding and accountable care considerations) and communications strategies needed to recognize the value of home health care and the importance of home health care professionals as part of a comprehensive health care team.
similar terms were often used interchangeably, and with various intended meanings. In some instances, workshop speakers and participants implied a more strict interpretation of home health care (and other similar terms) as including only medical services or in reference to the Medicare home health care benefit only, whereas other speakers and participants spoke to home health care as more inclusive of a variety of services and supports provided in the home. This summary uses the term home health care for consistency (except in cases of direct quotes), recognizing that each speaker or participant may have intended a different spectrum of care. Where possible, the spectrum intended by the speaker is noted. In addition, although the statement of task (see Box 1-1) called for a focus on the Medicare home health care benefit, the workshop planners encouraged all speakers to also consider home health care broadly—that is, more than just medical services and more than just the Medicare benefit. As a result, some workshop speakers focused primarily on Medicare home health care, but many other topics included under a broader definition of home health care were also discussed, to varying degrees.
Workshop participants were welcomed by planning committee co-chairs Bruce Leff, Johns Hopkins University School of Medicine, and Elizabeth Madigan, Frances Payne Bolton School of Nursing, Case Western Reserve University, who began with an overview of home health care across the spectrum of services and supports (see Figure 1-1).
Moving from left to right, Figure 1-1 shows that this spectrum ranges from care for lower-acuity levels care to higher acuity, and from chronic care to more acute care. It also moves from models in which there is little or no medical doctor (MD) involvement in the home toward models in which MD involvement is substantial. The figure shows that this spectrum starts with informal care services provided at home, often by family members—typically, daughters, spouses, or daughters-in-law, Leff said. Estimates suggest that somewhere between 10 million and 15 million people currently receive such care in the home.
Next, moving right, is formal personal care services—that is, paid-for services—for people who need additional help or who do not have family at home to help them. An estimated 2 million Americans receive these formal personal care services, Leff said. Next is Medicare skilled home health care, which is used for post-acute care, as well as for people in the community who are homebound, according to the definitions of Medicare, and have skilled home health care needs (which was a focus of the discussion over the 2 days of the workshop). More than 3 million Medicare recipients use those services. Farther to the right is home-based primary care, which
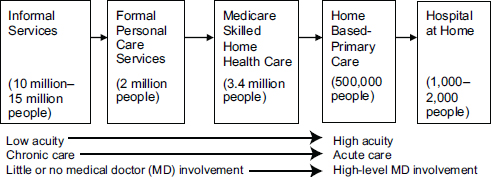
FIGURE 1-1 Home health care across the spectrum of services and supports, including numbers of individuals receiving care.
SOURCE: Reprinted with permission from Bruce Leff and Elizabeth Madigan,
2014.
involves physicians, nurse practitioners, or physician assistants providing longitudinal medical care, which is often team-based care and which is often provided in collaboration with social services providers to a population that is essentially homebound. Leff said that an estimated 500,000 people receive these services, acknowledging that this number “is the most back-of-the-envelope calculation” of the array. Finally, on the far right of Figure 1-1 are acute-care, hospital-level services provided in the home, including care provided through hospital-at-home-type models, such as the model developed by the Johns Hopkins Schools of Medicine and Public Health.6 To date, many fewer people receive these more intensive home-based services, although the workshop discussion suggested that the trend is for more and more people to receive such services.
Leff noted that the move from left to right in Figure 1-1 entails a move from the provision of health care services to individuals with lower-acuity levels of need to individuals with higher-acuity ones requiring a mix of acute and chronic care services and, finally, to the provision of acute care in the home. It also moves from models with little or no physician or medical involvement to those in which medical involvement is substantial, Leff said.
The four principal factors driving the development and use of these spectrum-of-care approaches are policy, payment, technology, and demographics, Madigan said. Much attention is paid to the last factor, “as we anticipate the aging of the American population, the projected increase in the number of people with multiple chronic conditions or functional impairments, and the impact that’s going to have on the health care system,”
______________
6 See http://www.hospitalathome.org (accessed December 24, 2014).
she said. Moreover, that growth is a constant, whereas the other factors—policy, payment, and technology—are amenable to change.
The current array of chronic care and home-based services is not well integrated, Madigan argued. Payments and some of the care providers are in separate silos. “From a patient’s perspective, you can have multiple agencies providing services, and they don’t know about each other or who is doing what piece [of the care],” Madigan said. In a true system of home health care, she said, services would be integrated and those providing these services would provide care along a continuum that would involve collaborations with partners in the community as well as those in facility-based long-term care, because patients often end up there at least for short periods, before going home again and receiving home health care services. In other words, across the spectrum of care, from informal services to the hospital in the home, what is needed is a focus “on what the patient needs and how we can help provide that in a seamless way,” said Madigan.
Personal testimony on caring for family members at home was presented by James Martinez from Oakland, California (see Box 1-2), and Karen Marshall, Kadamba Tree Foundation, Washington, DC (see Box 1-3).7 Although their experiences with home health care are different, their stories present two perspectives on some of the strengths and shortcomings of the current system of provision of health care in the home.
ORGANIZATION OF WORKSHOP SUMMARY
This workshop summary is limited to describing the presentations given and the general topics discussed during the workshop itself. Overall, each speaker’s presentation is captured in a section attributed to that individual. All of the workshop discussions with the audience have also been captured in a variety of ways. In some cases, the topics raised and the responses given during the discussion periods are incorporated into the section describing the speaker’s presentation. In other cases in which a new topic or line of discussion arose, a separate section describing the new topic is introduced at the end of the chapter. Comments made by workshop participants were attributed to the individuals by name when possible. (If identification of the speaker was not possible, the individual is referred to as a “workshop
______________
7 To watch these testimonies on video, see http://www.iom.edu/Activities/Aging/FutureHomeHealthCare/2014-SEP-30/Day-1/Session-1-Videos/2-Martinez-Video.aspx (accessed December 24, 2014) and http://www.iom.edu/Activities/Aging/FutureHomeHealthCare/2014SEP-30/Day-2/Overview/32-Marshall-Video.aspx (accessed December 24, 2014).
BOX 1-2
James Martinez’s Story
Home health was all new to me in 2011, when my mom was diagnosed with pancreatic cancer. She did not want to stay at home, because she didn’t have any health care there. I told her that if they would teach me what to do, I would take her home and I would take care of her until she passed. And it turned out, it was way better with home care than with the hospital. I was always at odds with the staff at the hospital.
So that’s what happened, with the support of the Sutter Home Care people up through hospice services, and they were there for me also, with the bereavement. They never left my side.
The following year, my dad got sick. I moved out of my house at that point and moved in with him, because he needed full-time care. I took care of him until May of this year. I couldn’t have done it without help, giving morphine and all these other drugs, knowing when to do it, and how to do it. I would call them, and I had just terrific telesupport. They’d call me back in 15 minutes, and if the drugs hadn’t worked, they would send out a nurse.
They showed me how to do everything. With my mom, I had to clean and change and administer the medicines through a PICC (peripherally inserted central catheter) line. With my dad, he had a nebulizer. He had air. They explained the equipment, so there were no questions, really.
Sutter took care of me, too. They came with a social worker and a nurse. The nurse would take care of my dad and do his vitals and all that and talk with him. The social worker would come into the kitchen with me, and we would sit and talk about me: how I can take care of myself, what I needed, because they said if I couldn’t be healthy, I couldn’t take care of him.
I didn’t have any help from any of my other family members. And I was trying to work and trying to do everything else that needed to be done around the house. Eventually, I had to quit my job. My dad’s retirement income was too much, so we weren’t eligible for me to be paid for his home care. If there was one thing that could change, it would be to give a little bit more financial help to the family.
I’m not the only one who’s done this. There are a lot of people. There’s a neighbor down the street. His dad passed away, and he took care of him. The two of us would talk and get a little bit of strength from each other.
SOURCE: Presentation by James Martinez, September 30, 2014.
participant.”) Presentations are also not necessarily organized in the same order in which they occurred at the actual workshop but have been rearranged to provide a better flow for the readers of this workshop summary.
Chapter 2 presents two keynote addresses (by Robert J. Rosati and Steven Landers, both of whom are with the Visiting Nurse Association Health Group) that address the current state of home health care overall
BOX 1-3
Karen Marshall’s Story
Karen Marshall began her presentation by quoting former First Lady Rosalynn Cartera:
There are only four types of people in this world:
Those who have been caregivers,
Those who are currently caregivers,
Those who will be caregivers, and
Those who will need a caregiver.
I must say, I wake up every morning and think about that quote. For the past 10 years, family caregiving has been a big part of my life. Like Mr. Martinez, I’m a repeat caregiver. I first cared for my mother, who had cancer. And a couple of months after she died, my father developed a heart problem. He was in his late 70s at the time and had never had any health problems. I suspect his heart broke, because along with me he was a caregiver for my mom.
That series of events really changed the trajectory of my life and how I think about caregiving, even though it has been a part of my life since I was a baby. My grandfather came to live with us when I was just a baby. His aging process took the same trajectory as many of the people in the rural neighborhood I grew up in, and when he was no longer able to stay home, he went to live with his daughter, my mother, who took care of him while she raised me. And when that was no longer feasible, he went into a nursing home.
Fast forward 20 years, and when I was in college, my grandmother had a stroke. My family helped her stay at home as long as possible, and eventually she moved in with us. While I was home for the summer, my mother and I split caregiving duties. A home health agency sent an aide to stay with her while we were at work. I only remember one agency at the time, which served a pretty broad multicounty area. That experience shaped how my family felt about home health care for a while, and it wasn’t necessarily a positive experience. It helped in that we could continue to work, but we were concerned about the skill and the quality of the care, and from others in the community, we heard stories about fraud and abuse.
Fast forward another 10 years, when my mother got sick in her early 60s. She was just 61 when she passed away, and her care at home was private pay. She did have private insurance. It helped that I could take a leave of absence from my job to help care for her in the last couple of months. At the time, I was an attorney here in DC, right on K Street, in a large firm. That’s when my perception of home health care began to shift, because the last time she was discharged from the hospital we knew she was going home to die. It was very comforting for my family to have the help of hospice. They set up the hospital bed in the bedroom. The nurse and caseworker really helped me understand what was going on and recognize the signs of her decline.
A couple of months after her death my father got sick. I did not see that coming. I was still winding down my mom’s estate. I was returning to work when
my father became ill, and it never really crossed our minds what would happen after he left the hospital. Part of the reason for that is that my big sister is a registered nurse, and she was able to take him home with her. He stayed with her several weeks until he went back to his own home, but he’d lost so much of his independence—a lot of his life. He was a logger, and up until his mid- to late 70s, he was going out into the woods chopping down trees every day. He’d lost his health, which he had always had, and his strength, which he had always prided himself on, and he had lost his spouse.
We did our best for several years to help him stay at home, which was his wish. In retrospect, it would’ve helped us tremendously to look at the home health care options. My dad was a little particular about how he wanted to be cared for, and we didn’t want to disrupt his expectations that much. But it became a burden to me. It was not uncommon for me to come out of a meeting to a voicemail that my dad was on his way to the emergency room, a 4-hour drive away. I went home every weekend for a long time and eventually cut back to several times a month.
It just became too difficult to juggle all these responsibilities, and eventually, in 2009, I left my job. The financial repercussions of that choice continue to this day. At the time I was married; I’m not anymore. I don’t regret my decision, but in retrospect I would have made different choices, especially given all that I now know—and have witnessed—about the options that home health care provides. Earlier this year my father was diagnosed with dementia.
This time we are relying on home health care. We have no choice. My sister has been on medical leave herself and can’t take additional time off. And I am just not in a position to stop working again. So we ended up relying on a home health agency to send in aides 24/7, which was not a long-term solution, as it cost us about $400 a day. We were applying for Medicaid benefits, and he primarily received his health care from the VA [the U.S. Department of Veterans Affairs], which was a great help. This financial assistance came through at just the right time, but still, the expenses were enormous.
I would go down there a few days every week. This was a difficult time for him, because he was coming to grips with his diagnosis and having me in and out was not necessarily the most comforting thing, which upset me because I was used to being of some comfort to him. The home health aides provided continuity. He got to know and like them. It helped to know I had eyes and ears to not only look after his medical situation but also his well-being in other ways.
Two social workers from our local Program of All-Inclusive Care for the Elderly (PACE) came in and did an evaluation, and they had an honest conversation with us about our options. They explained that it just wasn’t safe for him at home. We couldn’t guarantee that a health worker would always be around. This helped us feel better about a tough decision that we had to make. I still struggle a bit with that. I feel bad that after all of this effort: leaving my job, all the trips up and down I-95. Ultimately, his wish of being able to stay at home couldn’t come true. But every time I see him now he looks healthier. His medication is being managed properly. He’s gained his weight back. He smiles and he’s happy. And he’s not scared anymore. I really do credit home health care for helping us cross that bridge.
I would probably add a fifth person to First Lady Rosalynn Carter’s scenario of caregivers. I would add people who have to work with the caregiver. And that would include my former boss, who was very sad to see me go. That would include my coworkers, who had to pick up the slack on the days when I had to head down I-95 to an emergency room. That would include the health care professionals who had to tell us about my dad’s diagnosis while he was sitting there in the room. It would include the social workers who had to break the news to us about how difficult honoring my dad’s wish would be.
______________
a See the remarks of Rosalynn Carter at http://gos.sbc.edu/c/carter.html (accessed December 24, 2014).
SOURCE: Presented by Karen Marshall, October 1, 2014.
and changes occurring in the field, as well as an exploration of the future ideal state of home health care. Chapter 3 presents a keynote address by Eric Dishman of Intel on the role of home health care in achieving his vision of personal health. Chapter 4 examines the key issues and trends currently framing the discussion of home health care, such as trends in population health and public policy. The next several chapters explore the health care workforce (Chapter 5), the models of care and approaches to payment (Chapter 6), and the technology (Chapter 7) needed to reach the ideal state of home health care. Chapter 8 considers how home health care can be linked to the broader health care system, to communities, and to larger data systems. Finally, Chapter 9 provides reflections and reactions to the 2-day workshop from the perspectives of the moderators of the two panels on workforce and models of care and payment approaches on the first day of the workshop, from the perspectives of individuals who presented their reactions to the workshop presentations over both days of the workshop, and lastly, from the perspectives of the individual workshop participants, who described their own takeaways from the workshop.










