3
MODELING HEALTH RISKS OF CLIMATE CHANGE: STATUS, HURDLES, AND OPPORTUNITIES
“What is the information we need from modeling? We need to know where, and we need to know when [effects occur].”—Nick Ogden
“How do you take all the disparate data from different sources, scales, and times and space and come up with something that people can use to make decisions?”—Gregory Glass
Many organizations are modeling the effects of climate change on local, regional, and global scales. Most models focus on a particular sector, such as agriculture, energy, or the economy. Fewer models exist for the human health sector. What does it take to model the health risks posed by climate change? Workshop speakers outlined the basic mechanics of and key considerations for developing useful models. Discussions focused on recent model developments for evaluating the health effects of climate-induced spread of vectorborne disease and other health risks of changes in water and air quality and temperature. Discussions also explored overcoming hurdles to improve modeling capabilities.
DEFINITIONS, MECHANICS, AND KEY CONSIDERATIONS
The models needed to understand climate change and its effects on human health are complex. How can the climate-change community—scientists, model developers, policymakers, and other stakeholders—get a handle on the complexity? Ben Zaitchik, of Johns Hopkins University, outlined three factors that correspond to how the Intergovernmental Panel on Climate Change frames the issue: the physical environment, ecology (“natural processes”), and institutions. Those three factors mediate the relationships between changing climate conditions and human health outcomes. They also interact with one another. For example, climate change may result in increased rainfall (a component of the physical environment), and increased rainfall may support conditions for an increase in the population of a disease vector (ecology) in a country that lacks adequate institutionalized programs for vector control (institutions). Increased rainfall, increased number of disease vectors, and inadequate vector control all have effects on human health systems, such as medical practice and disaster response. Throughout the process of modeling, “we must think about humans,” Zaitchik emphasized. Humans “modify our physical environment and are deeply involved in ecologic processes and institutions,” he said. It takes many scientific disciplines and tools in addition to climate science to understand the interactions among the three factors and associated health outcomes, including hydrology, geography, ecology, agriculture, sociology,
economics, biomedical science, and clinical medicine. When it comes to developing models, data to feed the models, and potential model applications, “we need developments in all those fields . . . to help us to understand climate,” Zaitchik said.
What information is needed from models of climate-change effects? “We need to know where, and we need to know when” effects of climate change will occur, said Nick Ogden, a senior research scientist in the Public Health Agency of Canada. Ogden described four basic steps in developing and applying models of health risks due to climate change. First, we gather “our knowledge of current potential influences of climate and weather” on particular disease risks. Second, a model is used to “integrate the knowledge into abundance or presence and absence of diseases.” Third, we use model outputs to “obtain a quantitative relationship between the climate and the . . . disease risk.” Fourth, “we use this simple quantitative relationship or perhaps some more complex model to produce estimates of future risk.” Ogden noted that models can be made to predict where an effect may occur, forecast effects in the near term, or project effects in the long term (Box 3-1). Model predictions, forecasts, and projections are used to help to decide and design “what we’re going to do” about health risks posed by climate change and to “produce adaptation tools”, Ogden explained.
Zaitchik noted that “in the climate-science world there is now a lot of talk about climate services,” information that helps the health community to make decisions. The current framework for model development is top-down, beginning with climate and ending with health outcomes. Somehow, data on climate, physical environment, ecology, institutions, and human dynamics coalesce to “tell the health-system people what they’re supposed to be doing.” Zaitchik said that “a grand challenge” is to determine how decision-making needs of the health-system practitioners ought to drive model development from the bottom up. “We have this global framework for climate services that is fantastic,” Zaitchik said, and the US National Oceanic and Atmospheric Administration (NOAA), the US Environmental Protection Agency (EPA), and many others are working on this problem. And yet, he asked, “how do we actually transform communities to think in this way and rebuild our tools to make [climate services] work?”
How modeling is approached depends heavily on the needs of the user, noted Sari Kovats, of the London School of Hygiene and Tropical Medicine. The priorities of local, state, regional, national, and federal governments are different, she stressed. Hence, Kovats, George Luber, of the US Centers for Disease Control and Prevention (CDC), and other workshop speakers emphasized that a critical component of any model is its scale. The methods and assumptions used in modeling depend on the scale, Kovats said. The scale determines what data are available to users of model outputs.
The temporal scales range from hours to multiple decades, Luber explained. On the spatial scale, there can be a city or international range. The policy planning horizons range from annual budgets to infrastructure meant to be in place for multiple decades. Anthony Janetos, director of Boston University’s Frederick S. Pardee Center for the Study of the Longer-Range Future, said that there is generally a tradeoff between a model’s spatial resolution and the period of time that it simulates. High-resolution climate models cannot be used for long-term simulations. Long-term simulations inevitably have lower spatial resolution than many climate-change scientists desire, he said.
How model outputs are interpreted also depends on their scale, Mary Hayden, of the National Center for Atmospheric Research (NCAR), pointed out. National and regional
Box 3-1
Definitions: Predictions, Forecasts, and Projections
Nick Ogden provided definitions that his research group uses to frame different types of climate-change model outputs:
Predictions tell where an effect is occurring
Forecasts tell where and when an effect is likely to occur in the next week or month. As models move toward smaller temporal and spatial scales, they incorporate larger numbers of elements and involve a greater degree of complexity.
Projections estimate where and when an effect is likely to occur in the next decade, decades, or century.
assessments are great, but they can mask communities that are living in marginal conditions. If the goal is to mitigate hazards and develop adaptation strategies, models need to be adjusted for “local ecology” information. “Local-level assessment ensures a more targeted intervention, response, and adaptation,” Hayden explained.
In general, efforts to integrate climate-change models so that they can show the combined effects of different sectors are in their infancy. “We know that food and water interact, health interacts with many factors, and heat, urbanization, and air pollution all interact,” Kovats explained. Several types of modeling are used to study those interactions: one-way modeling, one-way modeling that includes adaptation and institutional responses, and two-way modeling (Box 3-2).
There are many challenges in model integration. For example, food security is important, but many facets of how the US food system works are not captured by the way that we have interconnected our agriculture, climate, and economic models, said Molly Brown, of the National Aeronautics and Space Administration. Brown came to that conclusion as a result of putting together a report on food security for the US Global Change Research Program’s recent National Climate Assessment.
Of the efforts toward intersectoral model integration, the furthest along are associated with combining modeling studies in different sectors, such as agriculture and hydrology, to explore interactions between sectors. The integrated-modeling community has been doing a lot of experiments with one-way modeling of effects, mostly physical and biologic effects, Janetos said. Studies on the effects of climate change rarely extend beyond physical and biologic effects to human health or economic consequences.
MODELING: THE STATE OF THE SCIENCE
Scientists studying health effects of climate change are endeavoring to generate data that link environmental changes to health outcomes and then to incorporate the data into models of health risks posed by climate change. Three subjects that many scientists are focusing on are 1) disease vectors, 2) water quality, and 3) heat and air quality. The World Health Organization recently completed a quantitative risk assessment of climate change with respect to selected causes of death, the first assessment of its kind (Box 3-3).
Box 3-2
Three Types of Integrated Models
Anthony Janetos defined three types of integrated modeling studies that endeavor to represent all world regions and sectors—such as agriculture, hydrology, and economics—to explore their interactions. Such studies do not always include health effects.
One-way models include climate variables as additional drivers of both disease and nondisease pathways of health outcomes. These are classical climate-impact/risk studies and include many of the models discussed in the workshop.
One-way models that include adaptation and institutional response assume that the health systems and institutions of 20, 30, or 50 years from now will not be the same as today’s. These models come closer to identifying actual health outcomes than simply assessing risk.
Two-way models include feedback from health outcomes and adaptation on the economy and on later consequences for both mitigation and future demographics. They offer the potential for “a complete integration of climate effects on health”. The value of two-way modeling is its ability to provide a better understanding of how the health effects themselves interact with future demographics.
Disease Vectors and Health
Ogden described models that are used to understand the effects of climate change on vectorborne diseases. “Historically, climate has had a relatively small role in the variation in the geographic occurrence of vectors” because such human activities as habitat alteration, vector-eradication programs, and adaptation (such as the use of bed nets) were considered more important drivers, Ogden explained. However, he hypothesized that climate change will be especially important in developing countries because of their relative inability to control the spread of vectorborne diseases. Most modeling efforts related to climate change and vectorborne disease focus on estimating future occurrence or abundance of disease vectors; this requires knowledge about various factors involved in vectorborne-disease cycles, including vector biology, reservoir host dynamics, host infection and transmission dynamics, and land-use dynamics, Ogden said. The advantage of models developed thus far is that they are built on “unequivocal” data—“true observed field or laboratory relationships between climate and some important attributes of the vectors or the pathogens”.
Simple mathematical models can be used for such science policy activities as country-level risk assessments or benefit–cost assessments. Simple models incorporate only one or two factors that have a known relationship between climate and a disease vector. Ogden and colleagues are using simple climatic indicators to project the distribution of the Asian tiger mosquito (Aedes albopictus) in Canada. The Asian tiger mosquito is a potential vector of chikungunya, an infectious disease typically found in the Caribbean. The number of infected travelers returning to Canada from the Caribbean is increasing because of the chikungunya epidemic in the Caribbean. Ogden compared two simple mathematical models that produced different outcomes. The model based on overwintering and annual mean temperature produced a map showing that the mosquito would not spread into Canada. The model based on temperatures in January and the summer and on annual rainfall produced a map showing that the mosquito could spread into Canada. “Much of the variation comes from the use of different indicators; this is one of the problems with simple models,” Ogden said.
Complex simulation models are used when a decision-maker needs to account for many variables and detailed information. The more complex models can be used to address such
Box 3-3
World Health Organization Quantitative Risk Assessment of Climate Change with Respect to Selected Causes of Death, 2030s and 2050s
In fall 2014, the World Health Organization (WHO) published a report on the first quantitative assessment of the health effects of climate change on a global scale. The report was prepared by a multidisciplinary, multinational team. Workshop speaker Sari Kovats was one of the report’s four editors. Kovats gave workshop participants a brief overview of the report objectives, approach, and model end points.
Objectives: The risk assessment was conducted in response to a WHO health-assembly mandate to update what is known about global health risks posed by climate change. No assessment of health effects of climate change had been conducted in over a decade.
Approach: The assessment looked at a “future world with and without climate change”. The integrated modeling was conducted with one carbon dioxide emission scenario (A1b emissions trajectory), one world population projection out to the year 2100, and three economic-growth scenarios: high growth, base-case (middle) growth, and low growth. Model assumptions included some adaptation in response to climate change. Kovats explained that for all health categories except mortality due to coastal flooding, the models assumed general improvement in population health due to improvements in economic development. For flooding, the models assumed increased population vulnerability due to rapid urban development in coastal areas.
Model End Points: The risk assessment included annual projections of mortality from all causes and from six specific causes: heat (in people over 65 years old), coastal flooding, diarrheal disease, malaria, dengue, and undernutrition. Of particular interest was the distribution of mortality in different regions. The models were “all fitted with the best available observational global data”,,” Kovats said, although in the cases of heat and diarrhea outputs from statistical models based on locational data were included.
Kovats shared conclusions drawn both from the risk assessment and from the process of conducting it. An important message of the 2014 WHO risk assessment is that “even if you assume a lot of adaptation and high economic growth, the effects are still adverse,” she said. In addition, “the effects are regionally focused”; for example, projected malaria-caused mortality is concentrated in eastern African countries. However, limitations need to be addressed. “We know that climate change will have more complex effects on health and on determinants of health” than the assessment includes, and “the uncertainties are large.” Identifying uncertainties is useful because it helps us to “point to where research is needed”, but Kovats cautioned that “we need to develop better methods to communicate and describe them.”
programmatic activities as risk mapping to determine targets for disease surveillance or intervention strategies, identifying populations at risk, and predicting evolution of new pathogenic variants, Ogden said. He emphasized that complex simulation models are the only option for making dynamic projections of a vector’s spread under different conditions. Ogden and his colleagues used a complex simulation model to assess Lyme disease emergence in Canada. The model was used to map projected distributions of blacklegged tick (Ixodes scapularis), the vector of Lyme disease, in 2020, 2050, and 2080. The risk map shows a “high risk” of spreading into most of eastern Canada. Ogden’s group validated its findings with a prospective study. “Unfortunately, it’s gone from a modeling exercise to a public-health issue,” he said. He added that “systematic surveillance . . . in time and space” is needed to develop useful simulation models for other disease vectors.
Ogden noted that a weakness in modeling efforts is in the translation of projections of vector presence into cases of disease. “The ultimate goal is to correlate human risk with vector population densities and climatic variables so that we can project how climate change will affect disease risk,” said Charles Benjamin Beard (Ben Beard), of CDC. To do that, “we need much more information on the distribution and abundance of vector populations, such as the
blacklegged tick,” he said. We also need local disease occurrence and information on the effects of temperature and precipitation on local vector populations. Beard emphasized the need “to continue to push the models to finer resolution” because public-health assessment and response are conducted at the local level.
Water Quality and Health
Juli Trtanj, of NOAA, discussed current efforts to develop models of climate-change effects on waterborne diseases and water-related illnesses. Waterborne diseases and water-related illnesses can arise through many pathways—exposures to bacteria or viruses in drinking water, to algal blooms in recreational water, to chemical contaminants in groundwater, and so on (Figure 3-1). The pathways are complex: the water cycle is combined with infrastructure, land use, and other biologic and physical factors. Trtanj explained that the reasons that the climate-change community is not farther along in developing coupled models is that neither the basic science underlying the water–health outcome pathways nor coupling of the factors involved is well understood. Trtanj indicated that although models of climate effects on sources of water contamination or on human exposure to water contamination are not yet advanced, such models are important stepping stones toward modeling health outcomes.
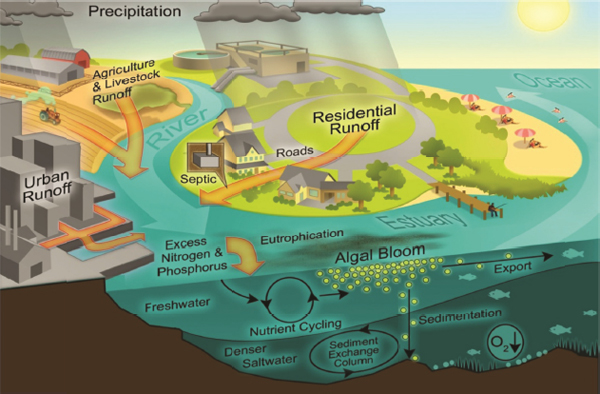
Figure 3-1 Waterborne-Disease Pathways, Freshwater–Marine Continuum
Julie Trtanj used this illustration to show the many factors in the pathway that links climate change to waterborne diseases and water-related illnesses. Such climate drivers as increasing ocean temperatures, ocean currents, and sea-level interact with exposure to contaminants from urban and rural environments or wildlife. Humans may be exposed to pathogens or other contaminants through drinking water and recreational or occupational water uses. Source: Juli Trtanj, workshop presentation, slide 3. Based on image originally created by Hans Paerl of the University of North Carolina, Chapel Hill for the US EPA.
Trtanj discussed a few case studies that used modeling on a regional scale to demonstrate “where we are” with modeling. One study looked at how projected increases in storms that result in sewage overflows may affect drinking water in the Great Lakes. “We already know that we are expecting an increased incidence of precipitation events because of climate change, and 67% of waterborne-disease outbreaks are preceded by precipitation events,” Trtanj said. In the Great Lakes, she explained, intense rainfall taxes the wastewater-treatment infrastructure. Researchers developed a model that projected future increases in rainfall. The result was that future rainfall would exceed the amounts planned for by wastewater managers. The rainfall output of the regional precipitation model was then used as an input for an “infrastructure model” of “how much water is going to be coming through the pipes.” The bottom line is that the model predicted that sewage overflows will increase by 20%, Trtanj said.
Trtanj and Jan Semenza, of the European Centre for Disease Prevention and Control, also described models for investigating climate-change effects on water temperature in relation to the potential for outbreaks of Vibrio species, bacteria that occur naturally in coastal waters. Vibrio can cause gastrointestinal-tract illnesses and wound infections and are responsible for 95% of seafood-related deaths in the United States. “If your doctor is not prepared for wound infection in the emergency room, you might well lose your limb,” Trtanj emphasized. Although there are not many cases of vibrio infection, there is a shift in the range of the bacteria in coastal waters, she said. Semenza was involved in an effort to predict the likelihood of vibrio infection in the Baltic Sea. V. vulnifucus starts to bloom when sea temperatures exceed 15°C and salinity is low. The research team used geospatial tools to monitor surface temperature and salinity to predict the likelihood of the occurrence of vibrio infection. They developed the Vibrio Risk Model. Semenza also investigated the relationship between West Nile fever (WNF), which is driven by the presence of infected birds, and climate’s influence on water temperatures in southeastern Europe. After analyzing the factors involved in a major outbreak in 2010, he and colleagues put together a multivariate model that included water temperature, the presence or absence of wetlands, and the presence of the virus in the previous year. The model successfully predicted the incidence of WNF in 2014.
Trtanj summarized the status of models of climate-change effects on waterborne diseases and water-related illnesses as mostly qualitative but quantitative when data are available; mostly regional, subregional, or local but not global; and mostly statistical although more dynamic, mechanistic models are needed. It will be important to incorporate “risk windows” for waterborne diseases into the models; it is necessary to factor in the habitat suitability and period that would be associated with changes in risk, said Erin Lipp, of the University of Georgia College of Public Health. Current models are able to link climate-induced changes to environmental exposures but have not linked them to health outcomes, and they do not include social variables, Trtanj said. She stressed that “gaps abound” and added that “we have to have the fortitude as agencies and scientists to figure out what we need to do, and do it,” even with the knowledge that advances will be neither inexpensive nor fast.
Heat, Air Quality, and Health
It is “critically important” to understand how environmental stressors, such as air quality, affect human health today if we are to understand what happens to the relationship in a changing climate, stressed Michelle Bell, of Yale University. Research has demonstrated that human exposure to tropospheric ozone causes “increased risk of hospital admissions,
premature mortality, increases in such respiratory symptoms as coughing and wheezing, reduced lung function, and other conditions.” More than 100 million people in the United States live in areas that exceed the US EPA’s health-based ozone standard, she said. Climate change may affect tropospheric ozone through multiple pathways, including changing precipitation patterns, changing wind speed and direction, and increased temperature. “Higher temperature means higher ozone,” Bell said. She explained that higher average temperatures increase the speed of chemical reactions for ozone formation and increase emissions of natural ozone precursors.
Bell described a study that her group published that used global climate, air quality, and meteorologic modeling to investigate how climate change could affect summer ozone concentrations in 50 eastern US cities. The goal was to “isolate the effect of climate on health”, so they modeled ozone emissions if we experienced the projected climate of 2050 today. For this study, estimates of what ozone emission magnitudes, technology, or population would be like in 2050 were not needed. “All the cities showed either a negligible difference or an increase in ozone,” she said. In particular, she said, the models showed increases of 12% or more in cities in the upper Midwest, including Ohio, Michigan, Indiana, and Illinois. Uncertainty of regional effects was somewhat high; the overall models projected that the number of days with unhealthy ozone concentrations would increase.
Bell told the audience about an exercise that used different models and climate scenarios to investigate how heat waves linked to climate change might affect mortality in Chicago in 2081–2100. The models accounted for changes in population. All the models and scenarios showed an increase in mortality. “The biggest uncertainty was associated with the choice of climate-change model,” Bell said.
Hayden pointed out that NCAR has developed a risk map of heat-related mortality at the census-block level for the city of Houston. The map is based on outputs of a hierarchic model in which spatially varied coefficients are based on death counts, numerical-model weather simulations, and census and parcel data, Hayden said. The risk maps produced from the model outputs help researchers to understand differential vulnerability. “We have learned that an increase in heat-stress nights will increase mortality and that extreme heat disproportionately affects the elderly, those who are socially isolated, those of low income, blacks, and people who use public transportation.”
The model also is able to look at each census block and determine what demographic factors contribute to risk at that level. A publicly available map enables users to find the nearest cooling centers, such as the closest community centers, pools, or Walmart store. The map shows how far away cooling centers are and the centers’ hours of operation. And it gives users access to CDC’s tips for cooling oneself immediately, Hayden said. “We think that these maps are an important step toward including drivers of vulnerability on multiple scales. They connect people with where they are, and they increase the ability of communities and stakeholders to develop a program to mitigate risk,” she said.
The climate-assessment literature tends to be extremely cautious about projecting health outcomes. Most studies are couched in terms of risk in part because whether adaptation is included is highly variable in the underlying literature, Janetos said.
It is difficult to link changes in climate with public-health outcomes because of the large variance in data and the low signal-to-noise ratio, Semenza said. Another challenge is dealing with multifactorial disease patterns that involve complex interactions with different drivers and teasing out the contributions of the different drivers. A third difficulty involves attributing individual climate events to health outcomes, he said. “Any climate-related effect on health is mediated by other physical and environmental factors. There is no such thing as a direct climate effect,” Zaitchik emphasized; for example, the built environment plays an important role. There is extreme heterogeneity in rural and urban environments with regard to exposure to heat and air quality, Luber said. “Even within an urban environment, there is great variability in a census block; even the side of the street can affect exposures,” he said.
Further complicating the challenge is the need to factor in what the Intergovernmental Panel on Climate Change calls “natural mediators”, such as the ecologic and biologic processes associated with the pathogens that cause infectious disease and with allergens, Luber said.
Brown, who was involved in the US Global Change Research Program’s recent National Climate Assessment, pointed out that many agricultural models do not include pests and disease and therefore could be optimistic in their projections of agricultural output in 2050 and 2100. “Such secondary effects may be enormous, especially in light of the acceleration of organism changes that we are trying to prevent with genetic engineering.”
No surveillance system attempts to link effects of climatic events to real outcomes, Semenza said. Many health effects are institutionally mediated, Luber added, pointing out as an example that climate change does not directly cause famine.
Public-health leaders often lack knowledge about climate change or shy away from the issue because it is not seen as a winnable battle, observed Richard Jackson, of the University of California, Los Angeles.
Systems modelers do not necessarily have the same objectives as stakeholders, said Gary Geernaert, of the US Department of Energy. Even among the world’s top modelers of the health risks posed by climate change, it is not always clear what questions the models are being produced to answer, said Kristie Ebi, an independent consultant with ClimAdapt, LLC.
That all adds up to a massively interdisciplinary problem, Zaitchik said. It is easier to model exposures and risks than health outcomes, he commented.
Furthermore, many data have been collected on the possible health effects of climate change, but not many have been collected in a desirable way, Ogden said.
An important issue related to collecting data is privacy concerns, said John Balbus, the senior adviser for public health in the National Institute of Environmental Health Sciences. “Are there ways to aggregate to ameliorate that issue?” he asked.
Georges Benjamin, of the American Public Health Association, raised the potential value of insurance claims data. Peter Berry, of Health Canada, pointed out that his agency has been trying to improve its links with the urban-planning community.
Models addressing climate change and health can leverage many existing data, said Anne Grambsch, of EPA. They include data on disasters, such as air pollution, and health data and research data focused on temperature sensitivity. Many models control for weather, she pointed out.
Databases contain many types of data, but it is important to understand the implications of how they were collected, Beard said. We need not only to put data into a model but work with people who understand the data. For example, in the United States, cases of disease are recorded by county of residence, not by where people might have been exposed to disease agents. Thus, if a case of a disease is related to travel, that is not captured, he said.
The availability of new satellite data and of expanded data services and low-cost sensors is improving our ability to model the physical environment, Zaitchik said. NASA’s Global Precipitation Measurement Mission, on a satellite launched in February 2014, is “game-changing”, he said. It provides more data on global precipitation than its predecessors gathered and at a much higher resolution, less than 10 km, with multiple passes each day. A satellite scheduled to launch in January 2015 will collect unprecedented information on soil moisture throughout the world with better resolution and the ability to “see through” vegetation to collect information that cannot be collected now. And NASA’s Giovanni data services are making satellite data more accessible than they were previously, he added.
Now that researchers have access to more than 35 years of satellite data, they can capture decadal-scale variability related to local environmental characteristics in a way that can reveal something about climate change, Zaitchik pointed out. The open-data policy that most institutions have adopted gives scientists better information to use in analyzing how the climate is changing.
The increased availability of sensors facilitates collection of local data, which in turn can add greater spatial resolution to models, Zaitchik continued Many of the sensors are small and inexpensive enough to be placed almost anywhere. The ability of cell phones both to act as sensors and to share data via crowd-sourcing allows interested citizens to get involved in data collection. Technologies for assimilating all the data collected by the satellites and sensors are also improving, he said.
Scientists’ increasing use of geographic information systems and information from remote sensing allows modelers to incorporate potentially useful data from such sources as weather stations, habitat maps, and digital elevation models, Ogden said.
New datasets on human mobility are also helping climate modelers. Those data, often captured by mobile phones, enable models to factor in “the human side of the ecology” in addition to the environmental ecology, Zaitchik said. An emerging field is coupled analysis that combines information about human population dynamics with such information as parasite population dynamics. Zaitchik said that he is working on a coupled analysis of how human and mosquito dynamics in the Amazon can affect malaria rates.
It is clear that diverse approaches are needed to model the health risks posed by climate change, Ebi summarized. Models can help to provide insight into exposure–response relationships, including how the relationships may change. They can also serve as early-warning systems, she said. And some can help to identify prices and benefit–cost relationships in association with climate variability and long-term change. “We do not know what the future will look like, so models have different sets of assumptions. As we move forward, we will need various models with various assumptions to address the questions that policy-makers will ask us,” she said.










