D
Selected Results from Commissioned Analyses
The following maps and tables include selected results from the Committee’s commissioned analysis of data from Cardiac Arrest Registry to Enhance Survival (CARES), Resuscitation Outcomes Consortium (ROC) Epistry, and Get With The Guidelines-Resuscitation (GWTG-R) registry. The commissioned reports are available on the Institute of Medicine website.
TABLE D-1 2013 Incidence and Outcomes of Out-of-Hospital Cardiac Arrest
| Cardiac Arrest Registry to Enhance Survival (CARES) | Resuscitation Outcomes Consortium (ROC) | |||
| Incidence (%) | Survival (%) | Incidence (%) | Survival* (%) | |
| Total, EMS-treated arrests of presumed cardiac etiology | 87.1 | 10.6 | 84.1 | 11.2 |
| Patient characteristics | ||||
| Mean patient age | 62.8 | 62.1 | ||
| Gender | ||||
| Male | 60.8 | 11.8 | 60.6 | 12.5 |
| Female | 39.2 | 9.6 | 39.4 | 9.2 |
| Cardiac Arrest Registry to Enhance Survival (CARES) | Resuscitation Outcomes Consortium (ROC) | |||
| Incidence (%) | Survival (%) | Incidence (%) | Survival* (%) | |
| Race | ||||
| White | 46.2 | 11.5 | 51.9 | 12.6 |
| American-Indian/ | 0.5 | 10.8 | ||
| Alaskan | ||||
| Asian | 1.6 | 10.4 | ||
| Black/African- | 18.8 | 9.3 | ||
| American | ||||
| Hispanic/Latino | 6.2 | 11.9 | ||
| Native Hawaiian/ | 0.7 | 7.1 | ||
| Pacific Islander | ||||
| Unknown | 26.1 | 10.9 | 19.3 | 9.3 |
| Other | 28.8 | |||
| Income | ||||
| <$20,000 | 3.6 | 8.4 | ||
| $20,000-$29,999 | 11.0 | 8.9 | ||
| $30,000-$39,999 | 17.9 | 8.7 | ||
| $40,000-$49,999 | 18.4 | 8.6 | ||
| $50,000-$59,999 | 15.9 | 8.8 | ||
| $60,000-$69,999 | 11.8 | 8.7 | ||
| $70,000-$79,999 | 8.2 | 9.2 | ||
| $80,000-$89,999 | 5.3 | 8.5 | ||
| $90,000-$99,999 | 3.0 | 8.4 | ||
| >$100,000 | 5.0 | 10.7 | ||
| Event characteristics Initial cardiac rhythm | ||||
| VF/VT/shockable rhythm | 21.1 | 29.4 | 20.5 | 30.0 |
| Unknown/ unshockable rhythm | 11.0 | 12.2 | 1.1 | 36.4 |
| Asystole | 46.4 | 2.8 | 49.4 | 2.2 |
| PEA | 21.5 | 9.7 | 24.1 | 9.8 |
| Etiology of arrest | ||||
| Presumed cardiac | 87.1 | 10.6 | 92.2 | |
| Other causes | 12.9 | 7.8 | ||
| Location of arrest | ||||
| Home/residence | 70.1 | 9.0 | 48.3 | |
| nursing home/ALF | 10.4 | 4.8 | 12.7 | |
| Cardiac Arrest Registry to Enhance Survival (CARES) | Resuscitation Outcomes Consortium (ROC) | |||
| Incidence (%) | Survival (%) | Incidence (%) | Survival* (%) | |
| Witness status | ||||
| Unwitnessed | 49.9 | 4.8 | 50.3 | 4.5 |
| Bystander witnessed | 37.7 | 16.4 | 35.9 | |
| 911/EMS-responder witnessed | 12.4 | 18.8 | 12.1 | |
| Bystander or EMS-responder witnessed | 17.5 | |||
| EMS characteristics | ||||
| Bystander CPR provided | 39.6 | 12.5 | 43.1 | |
| Bystander AED applied | 4.4 | 21.7 | 2.4 | |
| Yes | 15.2 | 20.0 | 4.1 | |
| No | 84.8 | 9.3 | 95.9 | |
| Hypothermia provided (in hospital) | ||||
| Yes | 50.1 | 36.6 | 41.6 | |
| No | 49.9 | 40.0 | ||
| Additional information | ||||
| Good neurologic status at discharge (CPC = 1; mRS ≤3) | ||||
| VT/VF | 70.5 | 89.9 | ||
| PEA | 45.8 | 81.8 | ||
| Asystole | 42.8 | 73.6 | ||
| Cardiac catheterization performed | 26.4 | |||
NOTES: ROC data on survival outcome was only available for the year 2011.
AED = automated external defibrillator; ALF = assisted living facility; CPC = cerebral performance category; CPR = cardiopulmonary resuscitation; mRS = Modified Rankin Score; PEA = pulseless electrical activity; VF = ventricular fibrillation; VT = ventricular tachycardia. The prepublication version of this report listed the PEA data point (under “additional information”) as 42.8 and the asystole data point as 45.8.
SOURCES: Based on data from the CARES and ROC registries. Daya et al., 2015; Vellano et al., 2015.
TABLE D-2 Incidence and Outcomes of In-Hospital Cardiac Arrest in 2013
| Get With The Guidelines - Resuscitation | ||
| Patient Characteristics | Incidence (%) | Survival (%) |
| Mean age | 65.1 | |
| Gender | ||
|
Male |
58.8 | 24.5 |
|
Female |
41.2 | 24.4 |
| Race | ||
|
White |
68.7 | 72.9 |
|
Black |
23.5 | 20.0 |
|
Other |
1.8 | 1.7 |
|
Unknown |
6.0 | 5.4 |
| Event Characteristics | ||
| Etiology of arrest | ||
|
Medical-cardiac |
37.2 | 40.2 |
|
Medical-noncardiac |
45.9 | 36.6 |
|
Surgical-cardiac |
6.6 | 11.3 |
|
Surgical-noncardiac |
10.4 | 11.9 |
| Location of arrest | ||
|
ICU |
48.8 | 39.7 |
|
Monitored unit |
15.0 | 18.0 |
|
Non-monitored unit |
14.4 | 12.9 |
|
ED |
12.4 | 13.8 |
| Initial cardiac rhythm | ||
|
Asystole |
28.0 | 23.1 |
|
PEA |
54.6 | 44.3 |
|
VF |
10.0 | 18.9 |
|
pVT |
7.4 | 13.7 |
| Other | ||
| Day and Time of Arrest | ||
|
Daytime |
49.3 | 27.5 |
|
Night time |
16.6 | 20.7 |
|
Weekend |
32.7 | 21.3 |
| AED use (among non-ICU patients only) | ||
|
Yes |
34.0 | 27.7 |
|
No |
66.0 | 29.5 |
| Get With The Guidelines - Resuscitation | ||
| Patient Characteristics | Incidence (%) | Survival (%) |
| U.S. Region | ||
|
North Mid-Atlantic |
13.8 | 24.1 |
|
South Atlantic |
20.7 | 23.4 |
|
North Central |
15.2 | 27.9 |
|
South Central |
17.8 | 22.9 |
|
Mountain Pacific |
8.9 | 26.0 |
| Is Hospital Rural or Urban? | ||
|
Rural |
2.6 | 24.4 |
|
Urban |
74.0 | 24.6 |
NOTE: AED = automated external defibrillator; ED = emergency department; ICU = intensive care unit; PEA = pulseless electrical activity; pVT = pulseless ventricular tachycardia; VF = ventricular fibrillation; VT = ventricular tachycardia.
SOURCE: Based on data from the GWTG-R registry.
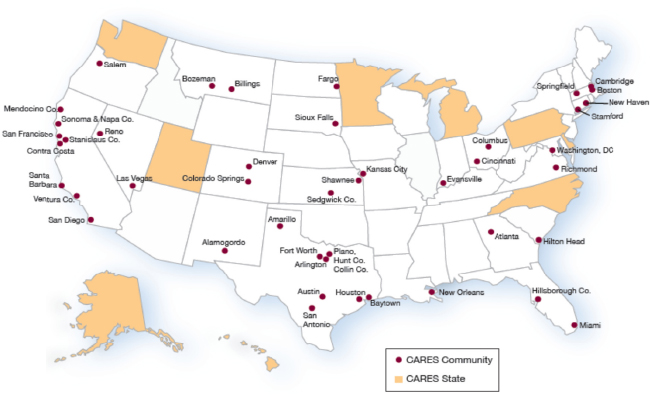
FIGURE D-1 Cardiac Arrest Registry to Enhance Survival (CARES) participatiing sites.
SOURCE: Vellano et al., 2015.
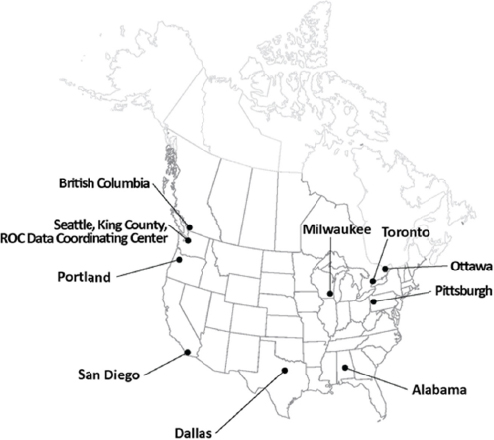
FIGURE D-2 Resuscitation Outcomes Consortium (ROC) participating sites.
SOURCE: Daya et al., 2015.
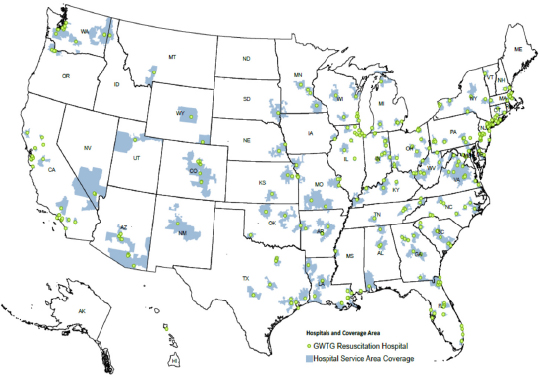
FIGURE D-3 Get With The Guidelines-Resuscitation registry.
NOTE: This map displays 317 hospitals. Data years: The American Heart Association hospital data from July 18, 2014; Dartmouth Atlas hospital service areas 2005; 2011 Environmental Systems Research Institute population estimates.
SOURCE: Reprinted with permission from Microsoft Dynamics.
REFERENCES
Chan, P. 2015. Public health burden of in hospital cardiac arrest. IOM Commissioned Report. http://www.iom.edu/~/media/Files/Report%20Files/2015/GWTG.pdf (accessed June 19, 2015).
Daya, M., R. Schmicker, S. May, and L. Morrison. 2015. Current burden of cardiac arrest in the United States: Report from the Resuscitation Outcomes Consortium. Paper commissioned by the Committee on the Treatment of Cardiac Arrest: Current Status and Future Directions. http://www.iom.edu/~/media/Files/Report%20Files/2015/ROC.pdf (accessed June 30, 2015).
Vellano, K., A. Crouch, M. Rajdev, and B. McNally. 2015. Cardiac Arrest Registry to Enhance Survival (CARES) report on the public health burden of out-of-hospital cardiac arrest. http://www.iom.edu/~/media/Files/Report%20Files/2015/CARES.pdf (accessed June 19, 2015).










