3
The Science and Technology of Non-Invasive Neuromodulation
Highlights
- Any part of the brain is a potential target for neurostimulation, and a better understanding of the neurobiological substrate of various symptoms could open the way to other therapeutic uses of noninvasive neuromodulation. (Hallett)
- Neurostimulation causes anatomical and functional changes of brain circuits; prolonged stimulation can affect metaplasticity. (Hallett)
- Because of the connectivity in brain circuits, the effects of brain stimulation extend beyond the stimulation site. (Fox)
- Neurostimulation affects children differently than adults, due both to anatomical differences and developmental changes in the brain. (Rotenberg)
- A range of transcranial electromagnetic devices and ultrasound have been shown to effectively modulate activity in the human brain. (Chen, Edwards, Elias, Krauthamer, Lisanby)
- Investigation of neurostimulation approaches in animal models helps scientists understand the molecular consequences and pharmacology of neurostimulation. (Rotenberg)
NOTE: The points in this list were made by the individual speakers identified above; they are not intended to reflect a consensus among workshop participants.
The history of neuromodulation goes as far back as ancient times, when electric fish were used to treat pain, explained Mark Hallett, chief of the Human Motor Control Section at the National Institute of Neurological Disorders and Stroke (NINDS). Today’s broad range of non-invasive neuromodulatory devices includes electroconvulsive
therapy (ECT), transcranial electrical stimulation (TES), transcranial magnetic stimulation (TMS), static magnet stimulation, transcranial direct current stimulation (tDCS), transcranial alternating current stimulation (tACS), random noise stimulation, ultrasound and focused ultrasound (FUS), and peripheral nerve stimulation, including stimulation of the cranial nerves. These tools not only provide insight into brain physiology, but can be used to modify the brain circuitry for a variety of therapeutic and non-therapeutic purposes, including neuroenhancement.
TARGETS AND MECHANISMS OF ACTION
Hallett suggested that any and every part of the brain could potentially be a target for neurostimulation. At this time, therapeutic applications of neurostimulation, such as repetitive pulse TMS (rTMS), have primarily been successful for the treatment of medication-resistant major depression. In these applications, stimulation is typically delivered to the dorsolateral prefrontal cortex (DLPFC), which has been identified as being hypometabolic in patients with depression (George et al., 1995; Martinot et al., 1990). However, Alvaro Pascual-Leone suggested that assuming the effects of neurostimulation come only from effects on the prefrontal cortex may miss the contribution of other brain areas. A better understanding of the neurobiological substrate of various symptoms may reveal other brain areas and neural circuits that may be modifiable through neurostimulatory approaches. For example, resting state functional connectivity maps may enable the identification of networks that may be modifiable using different stimulation approaches, possibly in combination with other interventions.
NEUROSTIMULATION EFFECTS ON THE BRAIN
Neurostimulation can alter brain function by creating a lesion or in some other way inducing an anatomical or functional change that will interrupt brain circuits or modulate oscillations within a circuit, said Hallett. In terms of non-invasive neuromodulation, most lesions are transient, although high-intensity focused ultrasound will create a more permanent lesion with longer lasting effects.
Neurostimulation interventions can produce either acute or persistent effects; however, the ability of a neurostimulatory device to produce a prolonged effect depends on its ability to use plasticity to change the brain. Neurostimulatory devices may produce a plastic change through multiple mechanisms, including strengthening or weakening synaptic strength and inducing anatomical changes such as increases in dendritic spines or axonal sprouting. According to Hallett, synaptic change and anatomical change are likely to occur sequentially. Moreover, it appears that treatments need to be repeated multiple times in order to get a long-lasting effect. This may reflect a transition from a physiologic to an anatomic change.
Michael Fox, assistant professor of neurology at Harvard University, noted that the physiologic effects of brain stimulation extend far beyond the site where stimulation is administered. For example, in order for TMS administered to the primary motor cortex to cause a muscle twitch, the polysynaptic neural response to the pulse must travel through the mid-brain and pons, cross the medulla, down the spinal cord, across a synapse to the alpha motor neuron, along that neuron down the limb and cross a neuromuscular junction, thus causing the muscle to contract. In other words, focal brain stimulation does not stay focal, but affects multiple areas of the brain (Fox et al., 2012b). Yet, for the goal of inducing long-term neuroplastic changes, a few particpants noted that there is importance in direct repetitive stimulation of the relevant brain structures (Pell et al., 2011).
Propagation of the neural response to the stimulation occurs outside of the motor cortex as well. For example, Fox and colleagues have shown, using several different imaging techniques, that when TMS is administered to the DLPFC for treatment of depression, there are also effects on the subgenual cingulate (Fox et al., 2012a). One implication of this is that connectivity in the brain can be used to identify locations on the surface of the brain that are accessible to non-invasive brain stimulation and that enable modulation of circuits and deep targets (Fox et al., 2012a). This work also demonstrates the usefulness of neuroimaging as a means of studying the different areas of the brain that may be affected by neurostimulation of a specific target.
The effects of non-invasive neuromodulation also depend on frequency and duration of stimulation. Administration of repeated pulses at low frequency or cathodal tDCS results in a reduction in the strength of the twitch, suggesting that excitability has been modulated, whereas administration of a high-frequency pulse of TMS or anodal tDCS results
in an excitatory effect and a stronger twitch. In addition, the behavioral and physiologic effects of stimulation last longer than the stimulation itself, although how long they last is unclear. For example, one study showed that effects on memory and changes in functional connectivity following multiple-day stimulation persisted for 2 weeks (Wang and Voss, 2015). Roi Cohen Kadosh, Wellcome Research Career Development Fellow and university research lecturer at the University of Oxford, showed data from another study where learning effects persisted for 6 months following transcranial random noise stimulation (tRNS) stimulation (Snowball et al., 2013).
NON-INVASIVE NEUROMODULATION IN CHILDREN
Several participants spoke about special medical and developmental considerations when using non-invasive neuromodulation in children. In addition, ethical issues arise with regard to children’s capacity to cooperate and to make informed decisions about the treatment; these are discussed in Chapter 7.
The brains of a child and adult have obvious anatomic differences, such as the density of the skull, the distance from the scalp to the brain, and the fact that the head and brain grow with time, said Alexander Rotenberg, associate professor of neurology at the Harvard Medical School and senior associate in neurology at Boston Children’s Hospital. In addition, throughout childhood there are changes in excitability, and with those changes come potential special vulnerability to injury. For example, the immature brain has an immature cortical inhibitory pattern, which makes it especially vulnerable to excitotoxic injury and seizures. Indeed, GABA, the inhibitory neurotransmitter in the mature brain, is actually excitatory in early life (Rakhade and Jensen, 2009). Rotenberg suggested that genetic mechanisms that switch GABA from excitatory to inhibitory may develop improperly in some disease states, such as autism and epilepsy.
The immature brain is also undergoing more neurogenesis, synaptogenesis, synaptic pruning, and myelination than the adult brain, yet little is known about how applied electric fields and other forces will affect these processes, or if prolonged exposure to current may have unexpected consequences. For example, Rotenberg mentioned a study in boys with autism that used TMS to assess synaptic plasticity. After delivering a train of repetitive TMS to the motor cortex, the investigators tested how long it took for corticospinal excitability to return to baseline.
The results indicated that there is a developmental trajectory to motor plasticity in this population, suggesting that frequency and duration of stimulation in children should take into account age and other developmental characteristics (Oberman et al., 2014). Rotenberg noted, however, that there have been few clinical trials that have segmented the pediatric population in order to examine mechanisms and neuroplasticity across the developmental trajectory.
One reason for the paucity of evidence regarding the effects of neurostimulation in children is that most human neuromodulation research excludes young people. In addition, studies in children are particularly challenging because of limits in patient availability, lack of homogeneity, interactions with other treatments, and limited access to tissue. Rotenberg said that more preclinical studies and animal models are needed to address these challenges. These models enable investigation of mechanisms at a resolution that is simply unavailable in humans, for example, looking at changes in regional gene expression or neurotransmitter receptor subtypes. The biggest advantage of animal models is found when large numbers of test animals are available, enabling systematic tweaking of protocols to identify the optimal dose, pattern and frequency of stimulation, etc. The molecular and electrophysiologic mechanisms are also accessible in isolated brain slices, which can be derived from experimental animals, and also (following brain surgery) from humans. Interestingly, said Rotenberg, because clinical applications of neurostimulation devices have been deployed well in advance of the basic science to support them, when data are acquired in the laboratory they can be rapidly translated to the clinic because the devices are already there.
MODELING ELECTRICAL DOSE AND EXPOSURE
Victor Krauthamer oversees a group of scientists at the FDA that aims to understand the fundamental mechanisms of neurostimulation as they are applied in devices seeking regulatory approval. Krauthamer directs the Division of Biomedical Physics in the Office of Science and Engineering Laboratories at the FDA’s Center for Devices and Radiological Health (CDRH). The studies undertaken in these labs are especially important to understand the safety of various modalities of electromagnetic stimulation on nerve cells. They have been able to predict, for example, the effects of high-frequency stimulation on
unmyelinated and myelinated cells (Krauthamer and Crosheck, 2002), illustrating the relative importance of the type of fiber that is being stimulated. Krauthamer’s group also has been working to understand the cellular mechanisms underlying emerging neurostimulation approaches such as those using near-infrared light (Katz et al., 2010), as well as the physiological and anatomical effects of low- and high-frequency ultrasound.
The FDA scientists use modeling and simulation at both the macroscopic, or anatomical, level, and the microscopic, or neuronal, level, to assess the effects of various neurostimulation devices on the brain, said Leonardo Angelone, research biomedical engineer at CDRH. For example, to study the electric fields generated by a given source applied transcranially, they are using an anatomical model of the human head that was developed through an international collaboration. This model will be made freely available to the scientific community, said Angelone (Iacono et al., 2015). It has been used, for example, to demonstrate how changing the location of electrodes on the head makes the field more focal.
Modeling also has been used to evaluate the differences among technologies—such as TMS compared with tDCS (Wagner et al., 2007)—to better understand the neuronal response and influence on behavior (Miniussi et al., 2013), and to examine the differenes in electric field distribution with different TMS coils (see Deng et al., 2013, for example).
A range of transcranial electromagnetic devices has been shown to effectively activate the human brain, although it is less clear how to leverage this for adaptive and durable neuromodulation, according to Dylan Edwards, director of the Non-Invasive Brain Stimulation and Human Motor Control Laboratory at Burke Medical Research Institute and Weill Cornell Medical College.
Electroconvulsive therapy is one of the earliest technologies developed for therapeutic purposes, used primarily for the treatment of depression and other psychiatric conditions. Though often not thought of as a “non-invasive” approach because it induces seizures, Sarah H. Lisanby, professor and chair of psychiatry and behavioral sciences at Duke University, said it remains a potent and rapidly acting treatment for
depression. The FDA has approved the use of ECT for six indications, although concerns about side effects and incomplete knowledge about the mechanisms of action limit its use primarily to those with severe, treatment-resistant depression (Kellner et al., 2012).
Transcranial electrical stimulation includes both tDCS and tACS, which are among the most readily available and cheap neurostimulatory devices in use. Indeed, a method used in 1804 by Giovanni Aldini to treat melancholia is not that different from the tDCS approaches that can be downloaded from the Internet today, said Krauthamer (Parent, 2004). Essentially, it involved delivery of a constant, low-intensity electric current over tens of minutes.
Transcranial magnetic stimulation was introduced in 1985 by Barker and colleagues as a non-invasive and painless method of electrically stimulating the human motor cortex (Barker et al., 1985). TMS devices deliver very brief, high-intensity magnetic pulses, with the neuromodulatory effect resulting from multiple pulses being delivered. Pascual-Leone and colleagues showed more than 20 years ago that a short burst of rapid rTMS increases excitability in the brain (Pascual-Leone et al., 1994). A few years later, Robert Chen and colleagues showed that low-frequency rTMS reduces excitability in the brain (Chen et al., 1997). In other words, just modulating the frequency will alter the effect on the brain, said Hallett. These differences can be converted into different therapeutic approaches for a variety of conditions, such as depression, stroke, movement disorders, epilepsy, and pain. In addition, said Rotenberg, because one can stimulate over a part of the brain and then quantify the response, TMS has robust diagnostic capacity, especially when coupled with other electrophysiological recording techniques.
The spatial distribution of the TMS field is controlled by coil design and placement on the head. Thus, the different coils differ in terms of coil focality and precision of stimulation (Deng et al., 2013). For example, the two coils approved for the treatment of depression—the figure 8 iron core by Neuronetics and the H-coil from Brainsway—have very different spatial distribution. The figure 8 coil is fairly superficial with minimal spreading, while the H coil has deeper penetration and greater spreading (see Figure 3-1). There are many other coil designs, each with a different corresponding electric field distribution (Deng et al., 2013). Lisanby noted how daunting it is to systematically evaluate these different devices, but added that this is where modeling and animal models are essential.
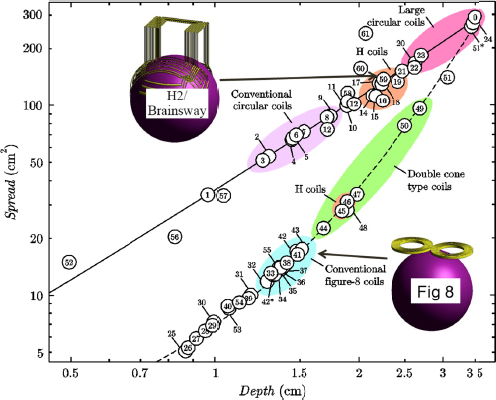
FIGURE 3-1 Focality/depth trade-off of 61 coils.
SOURCE: Presented by Sarah Lisanby at the IOM Workshop on Non-Invasive Neuromodulation of the Central Nervous System on March 2, 2015. Modified from Deng et al., 2013.
A few novel coil designs are also being tested in humans. One uses multiple magnetic coils to improve magnetic field focality (NCT01431001). Another uses low-frequency magnetic stimulation (LFMS, NCT01654796), a technology that grew from the serendipitous observation that one of the pulse sequences used in functional magnetic resonance imaging (fMRI) resulted in mood improvements in patients with bipolar disorder (Rohan et al., 2004). A third (NCT01370733) synchronizes the stimulation to a patient’s alpha frequency as measured by EEG (Leuchter et al., 2013).
Non-invasive neuromodulation with ultrasound is at a much earlier stage of development than TMS or tDCS. It has received CE Mark
clearance1 for therapeutic brain lesioning indications, indicating it is approved to be marketed in Canada and Europe; however, it has not yet been approved by the FDA.
Diagnostic ultrasound typically uses high-frequency waves that do not move through the skull very well. However, according to Jeffrey Elias, associate professor of neurological surgery and neurology and director of stereotactic and functional neurosurgery at the University of Virginia School of Medicine, there are some therapeutic frequencies that move through the skull better. Indeed, as far back as the 1950s, neuroscientists William and Frank Fry conceived the idea of focusing ultrasound beams deep inside the brain to treat movement disorders (Fry et al., 1958). Their technique could hardly be called non-invasive, however, because it required making a cranial window in the skull, which limited its development. Now that ultrasound can be delivered through the intact skull, non-invasive neuromodulation with lower intensities is receiving considerable attention.
For example, Elias’s lab is investigating the use of ultrasound’s mechanical effects to activate or inhibit brain circuits (Elias et al., 2013). Slice preparation studies have indicated that pulsing neurons with low-intensity ultrasound causes, through an unclear mechanism, an electrical stimulation of excitable or inhibitory response at the neurons (Tufail et al., 2010). Several labs are pursuing this line of research, mostly in small animals. They have shown that by pulsing the cortex, they can induce a behavioral response without causing any histological effect. Legon and colleagues have also tested this technology in humans. In this study, they were able to enhance performance on sensory discrimination tasks by targeting a specific area of the somatosensory cortex with transcranial focused ultrasound (tFUS) (Legon et al., 2014), and similar effects were later replicated by Yoo’s lab (Lee et al., 2015).
Elias said an advantage of low-intensity focused ultrasound is that it can be delivered deep in the brain without causing permanent damage or effects, thus lowering the bar for testing and brain mapping (Bystritsky et al., 2011). Potential indications include acute symptoms such as seizures as well as chronic conditions such as depression where plasticity might be affected. The main disadvantage is that much work remains to understand mechanism and refine the parameters to optimally activate or
__________________
1See http://www.jtultrasound.com/content/2/1/17 (accessed October 5, 2015).
inhibit neuronal circuits. The concepts and technology need to be further developed in the laboratory, he said, and then brought to the clinic.
PRECLINICAL STUDIES IN ANIMAL MODELS
Although TMS and other types of non-invasive brain stimulation have already been deployed in the clinic, Rotenberg noted that the basic science to support their use is lacking, and advocated increased use of preclinical studies in animal models to fill this gap. The large number of animals that can be employed in studies enable investigators to test and tweak systematically a range of stimulation protocols and doses to determine the optimal parameters to test in clinical studies. In addition, laboratory models enable studies of mechanisms of action at a resolution not available in humans, such as assessing regional gene expression, changes in neurotransmitter receptor subtypes, and other molecular consequences of neurostimulation. For example, in vitro slice cultures enable scientists to assess the effect of different levels of stimulation on different cellular populations within different brain regions, providing access to molecular mechanisms such as plasticity in a simplified structure (Vlachos et al., 2012). Animal studies also enable investigators to examine the effects of combining pharmacologic agents with neurostimulation, both in order to design combination trials where drugs facilitate the neurostimulation effects, and to identify drugs that may interfere with neurostimulation, said Rotenberg.
In summary, looking across non-invasive neuromodulation technologies, Lisanby compared the current state of knowledge to trying to develop a new drug without a complete understanding of the pharmacology, including the pharmacokinetics and pharmacodynamics, and many workshop participants identified gaps that need to be addressed in order to advance the field, ensure the safe application of devices, and develop devices with better efficacy. These research gaps, challenges, and opportunities were outlined in Chapter 2.










