E
Providing Sustainable Mental Health Care in
Kenya:
A Demonstration Project
Ana-Claire Meyera,b and David Ndeteic,d,e
A commissioned paper prepared for the January 13–14, 2015, workshop
on Providing Sustainable Mental Health Care in Kenya, hosted by the
National Academies of Sciences, Engineering, and Medicine’s Forum on
Neuroscience and Nervous System Disorders and Board on Global
Health. The authors are responsible for the content of this article, which
does not necessarily represent the views of the National Academies of
Sciences, Engineering, and Medicine.
_______________________
aVisiting Scientist, Kenya Medical Research Institute.
bAssistant Professor, Department of Neurology, School of Medicine, Yale University.
cUniversity of Nairobi.
dAfrica Mental Health Foundation.
eFaculty and Collaborator, The Chester M. Pierce, M.D. Division of Global Psychiatry, Massachusetts General Hospital, Harvard Medical School.
CONTENTS
Global Overview of the Burden of Mental, Neurological, and Substance Use Disorders
Prevalence of MNS Disorders in Kenya and Sub-Saharan Africa
Challenges for the Care and Treatment of MNS Disorders in Kenya and Sub-Saharan Africa
Collaboration with Traditional and Faith Healers
Target MNS Disorders for Kenya
Existing Community-Based Initiatives and Models for Target Disorders
Overview of the Existing Health Care System and Providers in Kenya
Overview of the Existing Health Information Systems in Kenya
Existing Resources for Selected MNS Disorders
Mental and Substance Use Disorders
Gaps in the Existing Resources for Selected MNS Disorders
GOAL
To develop sustainable access to health care for mental, neurological, and substance use disorders in Kenya, and ensure that the right patients get the right care and treatment, at the right time, and in the right setting.
EXECUTIVE SUMMARY
Mental, neurological, and substance use (MNS) disorders are a leading cause of burden of disease as measured using disability-adjusted life years (DALYs) in Kenya. There is a dramatic shortage of human and other resources to effectively care for these disorders. Furthermore, stigma greatly limits access to care and decreases quality of life for individuals affected by MNS disorders. Traditional and faith healers play an important role in provision of care for MNS disorders as many patients attribute disease causality and the development of pathology to a spiritual dimension.
We chose three priority conditions for the purposes of this demonstration project: depression, epilepsy, and alcohol abuse. We focused initially on these disorders because they (1) result in a high burden of disease in Kenya, (2) are not currently being addressed through other initiatives, (3) have existing evidence-based algorithms for diagnosis, treatment, and care, and (4) synergies exist in developing community-based interventions using laypersons or non-specialist health workers for these disorders.
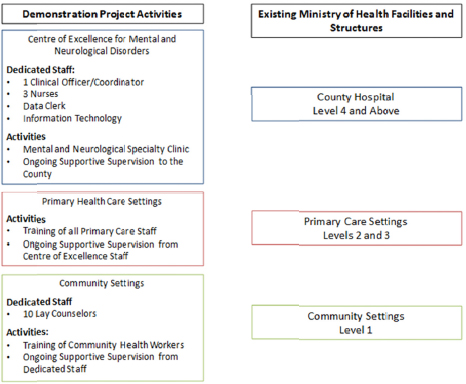
We propose several key components for this demonstration project (see Figure E-5) based on evidence-based principles:
- A decentralized, patient-centered, collaborative, stepped-care approach to care that is evidence based and locally relevant
- Strengthening of referral networks, including community-based referral and partnerships with traditional and faith-based healers
- A supportive supervisory framework and referral pathways, including increased numbers of lay and health care providers at various levels trained in the diagnosis, care, and appropriate referral of individual MNS disorders
- Promoting health literacy and community engagement through a model of social inclusion, self-help, and human rights for MNS
-
disorders
- Strengthening of existing infrastructure for distribution of essential drugs
- Strengthening and expansion of existing information systems infrastructure for MNS disorders
In collaboration with key stakeholders, such as the county governments, and in partnership with the Ministry of Health (MoH), Republic of Kenya, we propose a 4-year demonstration project that includes a planning phase and implementation phase and culminates with an evaluation phase in which ownership and management of the program is passed to the Ministry of Health or county government as appropriate.
In Year 1 we will focus on the planning phase. We will first work closely with key stakeholders to develop a learning curriculum and implementation plan. We will adapt existing training materials to a self-learning format that incorporates adult learning principles and ongoing supportive supervision. In Years 2 and 3, we will focus on the implementation phase and implement clinical services for mental, neurological, and substance use disorders in two counties. In Year 4, we will focus on evaluation of program objectives, dissemination of findings, and transfer of ownership to the county government, and copied to the MoH for information and support at the national level. Dissemination of the structure and results of this demonstration project to the remaining county governments will be a key activity of this final year, though we anticipate that the governor of the county supporting the demonstration project would provide ongoing reports to other county governors during the regular consultative meetings of governors and county Ministers of Health.
BACKGROUND
Global Overview of the Burden of Mental, Neurological, and
Substance Use Disorders
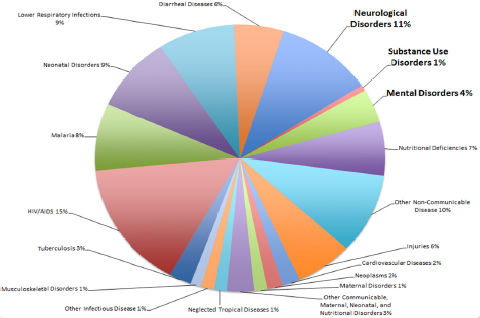
Worldwide, mental, neurological, and substance use disorders are a leading cause of burden of disease as measured using DALYs and account for 7.4 percent of DALYs worldwide.1 Neurological disorders result in 11.6 percent of DALYs lost worldwide.2
Using data from the Global Burden of Disease 2010 study, in Kenya,
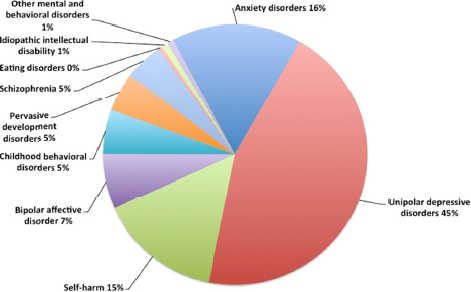
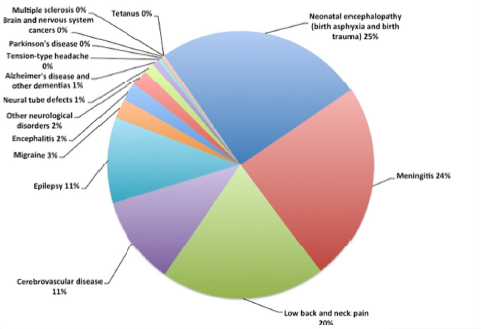
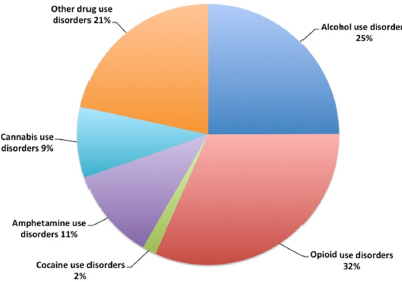
MNS disorders account for 16 percent of the burden of disease, more than HIV, which accounts for 15 percent (see Figure E-1).3 Neurological disorders alone account for 11 percent of the burden of disease in Kenya. Among mental disorders, unipolar depression accounts for the highest burden of disease (see Figure E-2). The disorders causing the greatest burden of neurologic disease are neonatal encephalopathy and meningitis, which together account for nearly 50 percent of the burden due to neurological disorders (see Figure E-3). Low back and neck pain, while relatively low morbidity, because of their high prevalence also contribute a large proportion of the burden of disease due to neurological disorders. Finally, epilepsy and cerebrovascular disease each contribute about 11 percent of the burden of disease due to neurological disorders. Among substance use disorders, alcohol use disorders are common and account for 25 percent of the burden, and opioid use, though relatively low prevalence in Kenya,4 accounts for a high burden of disease (see Figure E-4).
Despite the high burden of disease due to MNS disorders, there is a dramatic shortage of mental health specialists5 and neurologists.6,7 There are about 100 psychiatrists in Kenya. Most are based within Nairobi, the capital city.8 Outside of Nairobi, there is one psychiatrist per million population.9 There are 12 neurologists in Kenya and all practice primarily in the urban settings of Nairobi, Kisumu, and Mombasa and are primarily available in private settings.10
Furthermore, there is substantially lower usage of health services for mental health disorders11 and epilepsy12–15 in low- and middle- income countries as compared to high-income countries. For example, the treatment gap for mental health services ranged from 76–85 percent in less developed countries,16 and was 23–100 percent for epilepsy in low-income countries.12 Finally, people with MNS disorders experience stigma, discrimination, and human rights abuses worldwide.17–21
Prevalence of MNS Disorders in Kenya
and Sub-Saharan Africa
Mental Disorders
Mental disorders are highly prevalent and a leading cause of the global burden of disease.22 Mental disorders pose an increasing challenge to the global health care system.1 According to the World Health Organization (WHO), the prevalence of lifetime mental disorder globally
ranges from 18.1 to 36.1 percent.23 This means that more than one-third of the world’s population has at one time or another suffered from mental disorders of varying severity.
According to a study on the global prevalence of mental disorders commissioned by the WHO, slightly more than three-quarters of severe cases in the low- and middle-income world went untreated.16 Studies show that sub-Saharan Africa (SSA) has a huge burden of mental disorders. This picture takes a darker shade when one considers that increasingly more and more children and young people suffer from mental illness. A meta-analysis of studies on children’s mental health in Africa showed that 14.3 percent is the rate of psychopathology in all children.24 Furthermore, the study showed that 10 percent of children in the region have a specific psychiatric disorder. Add inadequate supply or limited access to effective treatment options25 and a powder keg of problems for an already overwhelmed health system is created.
Neurological Disorders
Neurological disorders are important and underrecognized causes of morbidity in SSA.26 As described previously, neonatal encephalopathies and meningitis/encephalitis have the highest burden in Kenya (see Figure E-3). Stroke is likewise an important contributor to the burden of disease. The prevalence and incidence of stroke are increasing across Africa yet still less than in high-income countries.27 This may be due to differences in risk factors for stroke, higher mortality rates in the acute setting leading to lower prevalence rates, and incomplete stroke registries. The overall prevalence of dementia among those over age 50 was about 2.4 percent, with Alzheimer’s disease the most prevalent (57.1 percent), followed by vascular dementia (26.9 percent).28 Nonetheless, dementia has a relatively low burden in resource-limited countries as the proportion of the population over 50 is much lower than in high-income countries. Low back and neck pain lead to a large burden of disease despite their relative low morbidity because these conditions are so common.
Epilepsy is also a significant contributor to the burden of neurological disease in Kenya (see Figure E-4).29 In a recent multisite study in Africa, the prevalence of epilepsy ranged from 0.7 to 1.5 percent;29 in one systematic review, the age-specific prevalence ranged from 0.3 to 1.1 percent with a bimodal distribution with peaks at ages 20 to 29 and 40 to 49.30 The treatment gap for epilepsy, the proportion of
individuals who require treatment, but do not receive it, approaches 100 percent in many low-income countries.12 Untreated epilepsy results in devastating social consequences and poor health outcomes. For example, children with epilepsy who have a seizure at school may be dismissed or ostracized, while adults may be barred from marriage or employment.18–21 In addition, persons with epilepsy have greater psychological distress, more physical injuries such as fractures and burns, and increased mortality.18,31–35
Substance Use
In recent years, there has been a marked increase in the prevalence of substance use disorders around the world. The 20 years between 1990 and 2010 saw an increase of nearly 40 percent in the global burden of substance use disorders.1 SSA is not left behind, and in some respects, the region is one of the leading contributors of the current upward trend seen in substance use.22 Considering the sky-rocketing rates of early-onset alcohol and substance use in the region, there is a serious cause for concern.36
Studies done in Kenya indicate high substance use rates.4 The most recent rapid assessment carried out by the National Authority for the Campaign against Alcohol and Drug Abuse (NACADA) shows that while tobacco use rates are on the decline, the age of onset for any substance use has fallen to 10 years of age and the prevalence of alcohol use is now at 13.3 percent. Increasingly, younger and younger individuals are using hard drugs at an increased rate.
Currently available treatments for substance use in Kenya have been unable to stem the problem. Whereas the government and private organizations have put in place rehabilitation centers and programs, these have not had great success in reducing the burden of substance use in the country, as shown by the increasing substance use rates. Most programs are generic, but substance use patterns vary by sex and age37 and may therefore suggest the need for cadre-specific interventions to combat this problem in Kenya.
Challenges for the Care and Treatment of MNS Disorders in Kenya
and Sub-Saharan Africa
Stigma
People suffering from MNS disorders are often victims of stigma.38 Stigma associated with mental illness has been shown to have devastating effects on the lives of people with psychiatric disorders, their families, and those who care for them.39 Three kinds of stigma may be associated with mentally ill people: public stigma, self-stigma, and label avoidance.40 Public stigma is the phenomenon of large social groups endorsing stereotypes about, and subsequently acting against, a stigmatized group: in this case, people with mental illness.41 In addition, supernatural, religious, and magical approaches play an important role in creating stigma against the mentally ill. This is prevailing in developing countries like Kenya, where people still believe mental illness is a doing of evil forces.42 Stigma experienced from family members is equally pervasive. Often the family members contribute to stigma because they feel blamed and responsible for having brought on the mental disorder either through negligence or inadequate care. Self-stigma is the loss of self-esteem and self-efficacy that occurs when people internalize public stigma. The vast majority of Kenyans believe that mental health disorders are caused by supernatural powers like evil spirits. Many believe that those who develop mental disorders do so to atone for sins committed against ancestors or as a result of being bewitched.43 Such stigma pervades society and hinders health-seeking behavior among mentally ill patients. Anecdotal evidence and data obtained from the Africa Mental Health Foundation (AMHF) indicates that stigma is widespread, increasing the barriers to seeking health care. This may contribute to the poorer outcomes in mentally ill patients. Between 12 and 18 percent of the population agree that mental illness is a form of punishment for bad deeds. Moreover, to avoid curses, which are more often than not heritable, society members, especially women, are taught to avoid individuals afflicted by mental illness.
Challenging stigma related to MNS disorders is essential in helping individuals accomplish recovery-related goals.44 Specific strategies to target certain types of stigma include protest, education, and contact. Stigma change for label avoidance, though scarcely tackled in literature, may also include the education and contact approaches used for public stigma. Moreover, increased penetrability of mental health care services
and public awareness in rural areas may be useful in reducing stigma. These actions can be achieved by identifying partners in the media to facilitate media campaigns to educate the public on the stigma against MNS. This has been successfully applied in the fight against stigma associated with HIV/AIDS. Furthermore, availability of a ready information channel for individuals suffering from MNS would provide an opportunity for these individuals to learn about their conditions and alleviate possible feelings of self-blame and guilt.
Collaboration with Traditional and Faith Healers
Traditional and faith healers (TFHs) play an important role in the provision of health care, especially mental health, in resource-depleted settings like Kenya. Many patients understand disease causality and the development of pathology in a spiritual dimension. Moreover in Kenya, as in many other sub-Saharan countries, TFHs are a cheaper alternative to conventional health care services.45 In contrast to health facilities, TFHs do not fail to treat a patient even without money and hence the poor are able to consult them and pay later. TFHs fear repudiation by the ancestors, spirits, or God, who bequeathed the skill on them.46 This is especially true for mental illness; traditional healers are the first to be contacted for mental illness in many parts of Africa.47,48 This is because they are not only available and accessible in the community, but they form part of the community’s cultural belief system, making them an integral part of the community.45 This makes them acceptable to the community.45 Indeed, though modern medicine may exist side by side with such traditional and/or spiritual practice, many patients in SSA still prefer traditional and spiritual therapies.49,50 Moreover, the deficiency of doctors, clinical officers, and nurses in Kenya, together with the urban clustering of these practitioners51 and the need to seek holistic treatment results in a significant proportion of patients consulting TFHs. However, the larger scientific community and modern medicine have remained critical and skeptical of the efficacy of such spiritual and traditional practices.52,53 Despite this, it is imperative to appreciate the critical role that TFHs can play in the health care system.
Increasing efforts have been made regionally and internationally, with success, to include TFHs in primary health care.53 Especially in SSA, positive returns have been demonstrated in inclusion of TFHs in provision of health care in the face of such challenges as HIV/AIDS, malaria, tuberculosis, and cancer.45 Among these challenges, cooperation
between TFHs and research scientists has been especially noteworthy in curbing the HIV/AIDs epidemic.54,55 This has also been demonstrated in several conditions like hearing impairment,56 tuberculosis, and malaria.57 The results of these studies suggest that TFHs are willing to collaborate with western medicine practitioners and report referring patients if they are not responding to treatment. An example of the use of TFHs in mental health has been seen with success in South Africa.58
However, challenges exist in incorporating TFHs into the health care system. These include lack of motivation to collaborate and communicate with modern health service workers49 as well as the absence of channels of referral and communication between them. In addition, although TFHs may be willing to cooperate with health care practitioners, this may not necessarily equate to referral of patients. For example, an intervention focused on HIV/AIDS and tuberculosis and collaboration reported that 99 percent of participants reported a “willingness” to collaborate, but only 43 percent were actually referring.54 Identifying factors associated with traditional healer referral practices of their mentally ill patients is central for developing and designing interventions to ensure that traditional healers refer more frequently and appropriately. Educating traditional healers on the fundamentals of mental disorders, including mood and anxiety disorders, is therefore important in this regard.58
Target MNS Disorders for Kenya
We chose three priority conditions for the purposes of this demonstration project: depression, epilepsy, and alcohol abuse. We based our decision on the following criteria:
- The disorder is prevalent or has a high burden of disease in Kenya
- The disorder is not currently being addressed through other initiatives
- Evidence-based algorithms for diagnosis, treatment, and care have been developed for resource-limited settings
- Synergies exist in developing community-based interventions using laypersons or non-specialist health workers for these disorders
Although it is impossible to completely separate these three conditions
from other MNS disorders, an initial focus on these disorders will enable us to build a foundation from which to expand treatment to other disorders such as anxiety, schizophrenia, primary and secondary stroke prevention, acute stroke care, Parkinson’s disease, and opiate and other drug abuse. While the three conditions discussed below are the priority conditions, all training and service provisions will use a psychosocial, patient-centered, collaborative care approach to enable gradual expansion to more comprehensive care programs for MNS disorders.
Depression
Depression is highly prevalent in Kenya and is the mental health disorder with the greatest burden. Evidence-based algorithms for treatment have been developed as part of the Mental Health Gap Action Program (mhGAP).59 Antidepressants, individual psychoeducation, and group interpersonal therapy have demonstrated efficacy in low-income countries.60 Community-based treatment approaches using laypersons and non-specialist health workers have demonstrated efficacy.
Epilepsy
Although the burden of disease due to neonatal encephalopathies and meningitis are higher than epilepsy, these disorders are already addressed as part of maternal–child health initiatives and communicable disorders. Stroke and epilepsy have a similar burden in Kenya, but we chose epilepsy because it is a stigmatized disease, much like mental and substance use disorders.18–21 Evidence-based algorithms for treatment have been developed as part of the mhGAP.59 Finally, epilepsy treatment is amenable to community-based approaches.61
Alcohol Abuse
Alcohol abuse is highly prevalent in Kenya although its overall burden is less than opiate abuse. Evidence-based algorithms for treatment have been developed as part of the mhGAP.59 Pharmacologic interventions with acamprosate and naltrexone are associated with longer abstinence times and improved completion rates for individuals participating in outpatient treatment programs.60 A brief physician-delivered intervention is associated with reduced intensity and amount of alcohol consumption, particularly in men.60
Existing Community-Based Initiatives and Models
for Target Disorders
There are various community-based approaches for preventing, screening, treating, and managing the three targeted disorders, depression, epilepsy and alcohol abuse. These strategies and initiatives have had different levels of success.
Depression
A recent U.S. study shows that community-based initiatives that incorporate social focal points, such as houses of worship, schools, and even salons, in low-income communities are more effective in combating some of the worst risk factors or effects of depression than clinic-based approaches.62 This model has been shown to increase an individual’s capacity to cope with the day-to-day challenges of life and significantly reduce the tendency toward homelessness and a person’s lack of employability.
A 2-year community-based intervention against depression carried out in Germany showed significantly decreased rates of suicide among patients with depression compared to the control site. The intervention consisted of “training of family doctors and support through different methods; a public relations campaign informing about depression; cooperation with community facilitators (teachers, priests, local media, etc.); and support for self-help activities as well as for high-risk groups.”63
Epilepsy
Community-based treatment of epilepsy is cost-effective, does not require specialized equipment, and is effective.61 The Global Campaign Against Epilepsy began in 1997 as a partnership among the International League Against Epilepsy, the International Bureau for Epilepsy (IBE), and the WHO.64 This effort included developing regional conferences and reports, an atlas for “Epilepsy Care in the World.”6,65 Importantly, this initiative included several community-based demonstration projects in Brazil,66 China,67 Georgia,68 Senegal,69 and Zimbabwe.70 Additional demonstration projects are being planned or initiated in Cameroon, Ghana, India, and Vietnam.64
Alcohol Use
Current trends in alcohol abuse research point to integration of preventive services and treatment interventions at the primary care level as the most cost-effective means of dealing with the problem.71 Over the years, there have been many community-based models for alcohol abuse, ranging from community-reinforced counseling72 to residence-based programs73 to enforcement of alcohol and drug-free zones in schools and campuses.74 A recent study comparing various community-based approaches for alcohol abuse showed that health care professionals believe that school-based programs and initiatives are the most effective alcohol interventions, followed closely by health promotion programs and other wider community initiatives.74
Overview of the Existing Health Care System
and Providers in Kenya
Health services in Kenya are provided through a network of just over 4,700 health facilities countrywide. The government oversees 41 percent of health facilities, nongovernmental organizations (NGOs) run 15 percent, and the private sector operates 43 percent. According to the new Constitution, the government-funded health system is broadly structured into the following levels:
- National referral hospital
- County referral hospital
- Subcounty hospital
- Health center
- Dispensary
- Community health worker75
Basic primary care is provided at dispensaries and health centers. Dispensaries, which provide outpatient services for simple ailments such as the common cold, flu, uncomplicated malaria, and skin conditions, are run and managed by enrolled and registered nurses who are supervised by a nursing officer at the respective health center. Those patients who cannot be managed by the nurse are referred to the health centers, which have a clinical officer in charge as well as one or more nursing officers. These, similar to dispensaries, provide preventive as well as curative services for the common ailments. County and subcounty hospitals
provide secondary care, which is integrated curative and rehabilitative care. Subcounty hospitals are similar to health centers with the addition of surgical units for C-sections and other procedures. County referral hospitals have the resources to provide comprehensive medical and surgical services and increasingly specialized care, including intensive care, life support, and specialist consultations. Further tertiary, specialized care is provided at the two public national referral hospitals, Kenyatta National Hospital in Nairobi and Moi Teaching and Referral Hospital in Eldoret.76 These two represent the apex of the health care system and provide diagnostic, therapeutic, and rehabilitative services. Gaps in the government-funded system are filled by private and church-run facilities. Most private clinics in the community are run by nurses. A smaller number of private clinics, mostly in the urban areas, are run by clinical officers and doctors. Tertiary care in the private sector is provided at equivalent private referral hospitals such as the Nairobi Hospital and the Aga Khan University Hospital, also in Nairobi.76
Kenya faces a significant shortage of physicians. According to the WHO, Kenya has just 1 doctor per 10,000 residents, a ratio that is below average for the Africa region. More than 50 percent of Kenyan physicians practice in Nairobi, which, with an estimated 3 million people, represents a small fraction of the approximately 44 million people that make up the country’s population.51,125
In 2011 there were 65,000 nurses on the Nursing Council of Kenya register. Further traditional midwives, pharmacists, and community health workers supplement the provision of health care. The migration of trained health workers from the public sector to higher paying positions in the private sector, or away from Kenya altogether, has made retaining qualified health personnel a persistent challenge. Kenya has one of the highest net emigration rates for doctors in the world, with 51 percent leaving the country to work elsewhere.77
Overview of the Existing Health Information Systems in Kenya
Kenya has several key sources for health and demographic information. The first is the Health Management and Information System (HMIS) of the MoH, which collects information on vital statistics and health indicators at MoH facilities nationwide. This information is complemented by occasional population-based surveys. Finally, there are five Health and Demographic Surveillance Systems (HDSSs) in Kenya, which follow populations longitudinally in Kilifi, Kisumu, Kombewa,
Nairobi, and Suba.
The Ministry of Health in Kenya first established systems for collecting information on health and health services in 1975, and these systems ultimately became the Health Information System Department. This department had three sections: Computing, Statistical and Medical Records, and the District HMIS.78 Data were collected at MoH facilities and then analyzed at a national level, but were not believed to be of high enough quality for planning and evaluation.78 Since then, there have been efforts to strengthen these data collection systems for various internationally funded initiatives on HIV/AIDS, malaria, child survival, and others. However, these were typically vertical initiatives with separate reporting tools, which increased the burden on health care workers.79 There have been several initiatives to streamline data collection and reporting and to improve the HMIS infrastructure via collaborative efforts with the MoH such as AIDS, Population, and Health Integrated Assistance; AfriAfya; the Community Based Health Information Management Project; and Afya Info.79–81 However, both the demographic and health information systems for much of the country are still based on handwritten, paper records.80 Continuing challenges include having too many indicators, with new indicators added by each international donor, a weak infrastructure for computing technologies, inadequate staffing and training, and little dissemination of existing information.80
Furthermore, over the past 15 years, several large population-based surveys have been conducted80:
- Kenya Population and Housing Census 1999
- Kenya Demographic and Health Survey (KDHS), 2003, 2008–200982
- Kenya National Health Accounts Survey, 2001–2002
- Kenya Household Health Expenditure and Utilization Survey Report, 2003
- Multiple Indicator Cluster Survey, 2000
- Kenya Integrated Household Budget Survey, 2005–2006
- Kenya Service Provision Assessment Survey, 2004
- Service Availability Mapping for Health, 2004
- Human Resource Mapping in Health, 2004
- Needs Assessment Report for Health Management Information System, 2004
- Kenya AIDS Indicator Survey (KAIS), 2007, 201283
Both KAIS and KDHS collect minimal information on alcohol and drug abuse, but do not collect data on other mental health disorders.
The HDSSs are complementary in that they observe populations with different environmental, epidemiological, and cultural back-grounds.84 However, there is little collaboration among HDSSs due to differing research concepts, objectives, and management systems84:
- The Kilifi HDSS was established in 2000 by the Kenya Medical Research Institute (KEMRI), the Wellcome Trust, and the University of Oxford, and surveys a population of about 260,000.85 Its original goal was to conduct research on infectious diseases of children, but it has also published extensively on epilepsy.29,86
- The Kisumu HDSS was established in 2001 by the U.S. Centers for Disease Control and Prevention and KEMRI and surveys a population of about 220,000.87 It was originally created as part of a large insecticide-treated bed net trial, but has served as the infrastructure for numerous clinical and effectiveness trials for malaria, tuberculosis, and HIV interventions.
- The Kombewa HDSS was established in 2007 by the U.S. Army Medical Research Unit-Kenya and KEMRI and surveys a population of about 142,000.88 This site was initially established to support malaria vaccine and treatment trials, but has participated in numerous studies, including polio/measles outbreaks, tuberculosis, pneumococcal vaccines, and arboviral infections.
- The Nairobi HDSS was established in 2002 by the African Population & Health Research Center and surveys a population of about 55,000.89 This site was initially established to evaluate the health of individuals residing in informal settlements or slums.
- The Mbita/Suba HDSS was established in 2006 as a collaboration between the Nagasaki University Institute of Tropical Medicine and KEMRI and surveys a population of about 54,000.84,90 Its original purpose was to support the study of tropical infectious diseases.
Existing Resources for Selected MNS Disorders
Mental and Substance Use Disorders
Health care provision in Kenya and especially psychiatric care and general mental health care remains limited in terms of infrastructure, staffing, and finances. Specialist psychiatric care is largely delivered at the district level by psychiatric nurses running outpatient clinics; by psychiatric nurses at provincial levels running inpatient units and outpatient clinics; and by national referral hospitals at Mathari, Kenyatta National Hospital/University of Nairobi, and recently, Moi University Teaching and Referral Hospital. The total number of mental health hospital beds for the whole population was 1,114 in 2009, a bed-to-population ratio of approximately 1:200,000.91 In total, there are just under 100 Kenyan psychiatrists. However, most of these are sequestered in urban centers, with up to a quarter of them (21) teaching at university. An estimated 20 live and work outside the country. Effectively, outside Nairobi, the psychiatrist population ratio is 1 per 3 to 5 million. Of the 500 trained psychiatric nurses, 250 are currently deployed in psychiatry. Seventy are deployed to Mathari National Mental Hospital, leaving 180 to the districts and provinces. As a result, each district does not even have one full-time equivalent psychiatric nurse. Many of the rest have either retired, died, left the country, or work in NGOs.
In the private sector, specialized psychiatric care is available in the major urban centers in the referral private hospitals. Kenya does not maintain a roll of clinical psychologists. It is therefore difficult to determine the exact number of these specialists who are involved in the provision of care for individuals with MNS.
However, the situation is not all gloomy. Several key stakeholders are involved in the provision of care for MNS disorders. The NACADA is the government agency that spearheads the campaign against alcohol and substance abuse. This authority, which receives funding from the national budget, provides an opportune partner in the campaign against MNS disorders. The NACADA also provides research grants to researchers in the area of MNS disorders, with the resultant availability of data that could further indicate areas of greatest need for resource allocation. Other stakeholders that are available for leverage include faith-based organizations and NGOs with special interests in MNS disorders.
Epilepsy
Overview of health care provider resources Most individuals with epilepsy who desired to seek care through the allopathic health care system would present for care at a Ministry of Health county government facility and would see a nurse or clinical officer. The system of care is as described in the previous section. Training in neurology is limited and nurses and clinical officers posted to rural districts report significantly more discomfort with diagnosis, care, and treatment of neurological disorders as compared to medical disorders.92 Kenya has eight adult neurologists and four child neurologists, and only two in public service at Kenyatta National Hospital. The remainder are only available in private settings.10
Availability of essential drugs The drugs listed on the essential medication list are
- Carbamazepine (tablet)
- Diazepam (injection)
- Magnesium sulfate (injection)
- Phenobarbital/phenobarbitone (injection, oral liquid, tablet)
- Phenytoin (injection, oral liquid, tablets)
- Sodium valproate (tablet)
The complementary list includes
- Carbamazepine (oral liquid)
- Ethosuximide (oral liquid or tablet)
- Sodium valproate (oral liquid)
Only two medications are recommended for the primary care level: magnesium sulfate (Level 3 and above: health center) and phenobarbitone (Level 2: dispensary). Nearly all the medications are listed as of vital importance and are on the core list.93 All of the above medications have at least one formulation registered with the Kenya Pharmacy and Poisons Board.94 However, only phenobarbitone tablets and injection, phenytoin tablets, carbamazepine tablets, diazepam injection, and magnesium sulfate injection are available for order by the Kenya Medical Supplies Authority (KEMSA), the primary supplier of MoH facilities.95
The recently released Kenya National Guidelines for the Management of
Epilepsy recommend that phenobarbitone, phenytoin, and sodium valproate (both tablet and syrup) be made available at the primary level. In addition, rectal diazepam and intravenous diazepam should be available for emergency care. The guidelines further call for the previously mentioned antiepileptic drugs plus clonazepam, clobazam, lorazepam, lamotrigine, gabapentin, ethosuximide, oxcarbazepine, topiramate, and levitiracetam to be available at the secondary and tertiary levels.96 All of these medications except clobazam are registered with the Kenya Pharmacy and Poisons Board.94 None are available through KEMSA.
Although these medications are listed, there are still significant challenges to making them available to patients. For example, stock-outs are common despite significant improvements in the KEMSA procedures. Furthermore, many institutions rely on user fees to finance the procurement of medications. Finally, rural settings continue to be significantly underserved.97
Financial resources allocated No specific funds are allocated for epilepsy.
Opportunities to leverage existing resources from ongoing projects There are several groups actively advocating for and improving services for people with epilepsy in Kenya. The organizations highlighted are not an exhaustive list:
- The Kenya Association for the Welfare of People with Epilepsy (KAWE) was established in 1982 and is a member of the IBE. KAWE has supported community-based education and stigma reduction through helping support the formation of 14 community-based organizations that support clinical activities by providing patient education and resource mobilization. KAWE also developed a feature film, “It’s Not My Choice,” which was awarded a gold medal at the International Audio-Visual Festival in New Delhi in 1989.98 KAWE promotes awareness of epilepsy by distribution of educational materials.99 In 2013, KAWE launched “FAFANUKA,” a mobile health awareness project that provides epilepsy education and directions to epilepsy clinics.99 Their primary focus has been on training health personnel. Since 1999 KAWE has trained over 1,428 medical personnel of various cadres and 2,894 community health workers.99 KAWE also developed a training manual for clinical officers and nurses that
-
was recognized by the WHO. Finally, KAWE runs three epilepsy clinics in Nairobi with nearly 8,000 visits recorded in 2013. KAWE established and now provides technical support to 16 clinics across the country.99
- The National Epilepsy Coordination Committee (NECC) was founded in 2010 to coordinate epilepsy activities in Kenya, including international organizations; research and academic institutions; pharmacy, medical, and professional societies; nongovernmental and community-based organizations; and people with epilepsy. In November 2013, it supported numerous outreach activities, including a roadshow through Kisumu, Mombasa, and Nairobi during National Epilepsy Awareness Month100 and supporting the Kenyan Purple Day for Epilepsy.101 Furthermore, the NECC coordinated the development and approval for Kenya National Guidelines for the Management of Epilepsy.96
- The Kenya Society for Epilepsy was established in 1997 and is a group composed of health professionals. It is a member of the International League Against Epilepsy. The group has approximately monthly meetings and continuing medical education events.
Gaps in the Existing Resources for Selected MNS Disorders
There are few resources for the diagnosis, care, and treatment of MNS disorders in Kenya and little data about the prevalence and severity of these disorders. We would like to highlight some key gaps that could be addressed by a demonstration project.
- Scarce human resources for MNS disorders at primary, secondary, or tertiary care levels
- Poor coordination of care among communities, traditional healers, faith-based healers, and primary, secondary, and tertiary care medical practitioners
- Stigma, misinformation, and discrimination against individuals living with MNS disorders
- Poor availability of essential drugs for MNS disorders
- Poor availability of epidemiological or health service data to enable planning for MNS disorders
DEMONSTRATION PROJECT
AND IMPLEMENTATION PLAN
As described previously, MNS disorders have a high burden in Kenya, but few resources are available for care. Nonetheless, there have been several key initiatives, including the presentation of a Mental Health Bill for the Kenya National Assembly this year,102 a mental health training initiative,91 development of national guidelines for epilepsy care,96 and the ongoing work of governmental and nongovernmental organizations such as the AMHF, the NECC, and NACADA.
We propose several key components for this demonstration project based on evidence-based principles as described in the prior sections of this document103–105:
- A decentralized, stepped-care approach to care that is evidence based and locally relevant
- Strengthen referral networks, including community-based referral and partnerships with traditional and faith-based healers, and links with higher levels of care
- A supportive supervisory framework and referral pathways, including adequate numbers of community health workers, primary care health workers, and specialists in MNS disorders
- Promote health literacy and community engagement through a model of social inclusion, self-help, and human rights for MNS disorders
- Strengthen existing infrastructure for distribution of essential drugs
- Strengthen and expand existing information systems infrastructure for MNS disorders
Study Site
We propose an intervention targeted at the county level, encompassing at least one county or subcounty hospital and its surrounding primary care sites and community. The selected county should demonstrate a commitment and ownership of the project by contributing matching funds for service provision as well as participating fully as a partner in the design and execution of the demonstration project. Building an effective partnership and involving the county
government from the early stages is a key factor in sustaining this effort after the demonstration period is complete. The primary goal of this demonstration project is to create a program that is replicable and scalable across the country and aligned to the WHO Mental Health Action Plan 2013–2020, to which the Government is a signatory. A secondary goal would be to establish the effectiveness of the demonstration project through a high-quality, community-based impact evaluation.
Project Components
- A decentralized, patient-centered, collaborative, stepped-care approach to care that is evidence based and locally relevant
- Strengthen referral networks, including community-based referral, partnerships with traditional and faith-based healers, and links with higher levels of care
We propose a community-centered approach that builds on the Ministry of Health infrastructure and begins at the level of the community health worker (CHW) (Level 1 Services).106 CHWs would provide some services such as counseling, social support, and referrals to primary care settings. We also propose engaging traditional and faith-based healers in the referral and treatment processes.
At primary care settings, services for MNS disorders would be integrated with primary care services, a model that has worked for other stigmatized disorders such as HIV.107 Furthermore, services would be provided using a collaborative care approach, which has demonstrated efficacy for depression as well as other chronic illnesses. Ultimately, service provision will align with priorities outlined in the WHO Mental Health Action Plan 2013–2020, to which the Government of Kenya is a signatory. Additional support for primary staffing is critical to handle the increased workload by adding more services.108. In primary care settings, first-line medical treatments would be provided using clinical algorithms.109 Complex patients would be referred to Centres of Excellence at the county and subcounty levels for second-line medical treatments or more complex services such as inpatient hospitalization.
- Adequate training and a supportive supervisory framework, including adequate numbers of community health workers, primary care health workers, and specialists in MNS disorders
We propose training all the CHWs in identification and referral of individuals with MNS disorders. We propose training several CHWs as lay counselors so they can provide community-based counseling and support to peer-led groups. We will additionally engage traditional and faith-based healers and provide training in MNS disorders. Finally, we also propose training nurses and clinical officers to provide primary care for mental disorders at MoH facilities.
Furthermore, we will provide advanced training for a cadre of individuals to develop mental health expertise, a team of one clinical officer and three nurses per district, to provide ongoing supportive supervision to primary health care workers as well as on-call mobile phone consultation and support for referrals to secondary or tertiary care facilities. These individuals would also staff the referral clinics at the county hospitals. Individuals providing support to primary care facilities will generally be nurses and clinical officers who have responsibility over a district and can provide higher level services at the district hospital level.
Innovative training models Prior efforts to train health care workers in Kenya to provide comprehensive mental health care have had modest success in improving health outcomes, but have not clearly improved diagnosis and treatment of mental health disorders.110,111 Diagnosis of mental and substance use disorders will have a foundation in a general psychosocial approach, and diagnosis of neurological disorders will be based on a comprehensive primary care approach. Approaches to care of MNS disorders will be grounded in a collaborative care approach.112,113
The training components on specific priority conditions will be delivered in a modular fashion, will be based on core competencies identified by the Institute of Medicine (IOM),109 and will build on the foundation of the WHO mhGAP modules.59,114 We will begin with the three priority conditions and hope to expand this training to include additional models for other key MNS disorders, such as anxiety, schizophrenia, primary and secondary prevention of stroke, acute stroke care, and opiate and other substance abuse. These modules will be locally adapted based on the prior experience and in partnership with bodies such as the Kenya Medical Training College and local NGOs.91,99 This training method has demonstrated effectiveness in training nonspecialist health care workers.115,116 Furthermore, we will draw from innovative strategies developed by the University of Nairobi Partnership for Advanced Clinical Education for HIV Education, which incorporates distance and adult learning principles. Educational activities will involve
self-learning and mentored face-to-face sessions, which are accompanied by a log book with activities, cases, and a core set of clinical encounters.117 These training activities are designed to occur primarily onsite, with support supervision, and are more cost-effective than traditional classroom training models.
Supportive supervision will be defined as a set of measures designed to ensure that personnel carry out their activities effectively through direct, personal contact on a regular basis in order to guide and assist staff and improve their competence.118 Supportive supervision has been shown to be an effective technique for ongoing training and evaluation in primary care settings in developing countries.118–122 Furthermore, it has been identified by health care workers as a critical component in providing ongoing mental health care in primary care settings.108 Mobile phone helplines have been effective in providing decentralized HIV care and could be adapted to help support primary care workers providing mental health care.123
- Promote health literacy and community engagement through a model of social inclusion, self-help, and human rights for MNS disorders
We will partner with local NGOs, many of whom have been conducting this work for some time, to develop locally relevant health literacy and community engagement campaigns to heighten awareness of and decrease stigma around MNS disorders using media campaigns, opinion leaders, and community mobilization strategies. In addition, we will build on existing organizations and facilitate the development of peer-led and health worker-supported community organizations for both social support and economic development.
- Strengthen existing infrastructure for distribution of essential drugs
Our goal was to address several key challenges identified by the IOM, including inappropriate selection, ineffective supply chains, high pricing, and poor financing.25 KEMSA, the national authority charged with procurement and distribution of medications to MoH facilities, provides medications to county governments when requested. We will work in partnership with county governments to continue to strengthen the supply chain from the requesting facility, to the county governments,
to KEMSA. We also propose an ongoing relationship with the Kenya Pharmacy and Poisons Board, the regulatory authority for Kenya, to improve the number of registered drugs and high-quality generics available for MNS disorders to decrease the costs of these medications. Finally, we will collaborate with government bodies and professional societies to improve the availability of medications and decrease medication-associated user fees for MNS disorders at the primary care level and to increase the number of medication options for providers.
- Strengthen and expand existing information systems infrastructure for MNS disorders
The county governments and Department of Health Information Systems of the MoH will be key partners and stakeholders in this project. Together with the county government and Mental Health Directorate of the MoH and other stakeholders, we will identify a core set of mental health measures to include in the county HMIS. In addition, we will work closely with the MoH to ensure that key variables relevant to MNS disorders are included in national health surveys such as KDHS and KAIS. We will also partner with HDSS groups in Kenya to include mental health variables as part of their routinely captured data.
Oversight
The lead grantee institution, in collaboration with the sponsor and the county government, will provide overall leadership and technical and financial oversight of the project. The lead grantee will have sufficient administrative and financial infrastructure to support the management and reporting required by the sponsor and coordinate a complex set of activities. It is envisioned that subawards would potentially be made as appropriate to organizations with expertise in developing educational content, community engagement, or providing clinical care around MNS disorders. The achievements of this project would be monitored annually by a board composed of key stakeholders, partners, and subawardees. A county or subcounty team will be developed to oversee day-to-day activities and meet on a quarterly basis. This team will be composed of the County Health Management Team and Health Management Board of the selected site, key community leaders, NGOs, and other local stakeholders.
Time Line and Workplan
We propose four stages to this project: (1) Situation analysis; (2) Planning; (3) Implementation; and (4) Evaluation.124 This document represents the first stages of the situation analysis and planning. We have gathered information about the needs for MNS disorders in Kenya, identified priority conditions, and identified available resources, including human resources, the strengths of the existing health system, potential funding streams, and relevant governmental, nongovernmental, and private-sector agencies. Furthermore, below we propose a method of service delivery that complements and builds upon the existing health system.
Thus, for this demonstration project we propose beginning at the end of the planning stage and moving rapidly into the implementation phase. Below we describe the general activities over an initial 4-year period:
- Year 1:
- Select implementation site in consultation with county governments and key stakeholders
- Develop training materials for health care providers aligned to the mhGAP-Intervention Guide (IG)
- Evaluate and strengthen distribution of essential medications
- Develop core set of variables for MNS disorders
- Integrate training on mental health, using the mhGAP-IG, into existing training programs and with emphasis on existing service providers at county and subcounty health facilities
- Year 2:
- Begin training existing primary health care providers and community health workers in the participating county, integrating training into existing training programs as much as possible
- Expand services across the county, with the goal of complete coverage by the end of the year
- Continue to develop additional training modules
- Year 3:
- Provide services across the county
- Year 4: Evaluation
- Transfer management to the county government
- Final evaluation
Resources
The concerned county government will be required to provide matching funds supported by a written commitment and provided for in the official budget by the county. These matching funds will support the county’s own involvement and own participation in the demonstration project as an equal partner at par with the implementing team. The demonstration project will not be involved in the expenditure of the matching funds, but will guide through the consultations on where the county government should spend on mental health. The demonstration projects will therefore not be involved in the accounting of those government expenditures. The details on give and take will be worked on with the willing county. The overriding condition is that they must make a commitment to put in some funds.
Key Stakeholders
The key stakeholders for this project are the county government partner and the MoH. The county governments are fiscally responsible for provision of health care services while the MoH provides technical guidance and coordination across the nation. These stakeholders should be engaged from the earliest phases of the project through to the monitoring and evaluation phase, and ultimately should extend beyond the life of the demonstration project and to scale up across the nation. The county government will also play a key role in national scale-up as a role model for other county governments.
At the community level, opinion leaders and community gatekeepers will be engaged through a series of meetings and discussions to secure their interest and buy-in, in support of the project. This will precede further community engagement activities not limited to public meetings (barazas), training seminars, and workshops to educate community members on mental health and reduce stigma.
Both formal and informal health service providers are vital to the success of the demonstration project. Formal health care providers such as nurses, doctors, clinical officers, and community health workers will be engaged both collectively, through their professional unions where applicable, and individually at the facility level. Traditional and faith healers will also play an important role in the success of this project. Training seminars and workshops will be held to educate them on the importance of integrating mental health into their routine services.
Informal health service providers, such as traditional and faith-based healers, shall also be included in individual and joint training sessions with actors from the formal sector to create the synergy that will be necessary to ensure that mental health services are truly integrated across the board of health service delivery in the country. The association of traditional and faith healers will be represented by the national and local leaders at the county level.
Nongovernmental and private partners will also be included in high-level discussions and in the monitoring of the project because their support will be crucial during the scale-up of the project. These partners include other organizations that provide health services routinely and have a huge stake in Kenya’s health care system.
Our approach will require early engagement with and involvement of county governments and governors from the conceptualization of the demonstration through its implementation. We believe this will lead to local ownership of the process and a smooth transfer of ownership at the conclusion of the demonstration project—and ultimately to the sustainability and scalability of these services across the country.
The key stakeholders necessary to provide sustainable mental health care in Kenya include the following:
- Government
- County government
- MoH
- Government agencies/departments
- Department of Health Information Services, Ministry of Medical Services, Kenya
- The National Authority for the Campaign against Alcohol and Drug Abuse
- Kenya Medical Supplies Authority
- Kenya Pharmacy and Poisons Board
- Kenya Medical Research Institute
- The Kenya Nursing Council
- The Kenya Clinical Officers Council
- Kenya Medical Practitioners and Dentists Board
- The Kenya Human Rights Commissions
- Other leading organization on mental and neurological disorders in Kenya
- The Society of Traditional and Herbalists in Kenya, which has authority over all traditional and herbalists in Kenya
-
- Africa Mental Health Foundation
- Kenya Society for Epilepsy
- Kenya Association for the Welfare of People with Epilepsy
- National Epilepsy Coordinating Committee
- BasicNeeds Kenya
- African Medical and Research Foundation
- Professional bodies
- Kenya Association of Psychologists
- East African College of Neurology
- Kenya Psychiatric Association
- Kenya Association of Physicians
- Other stakeholders
- Private and public universities
- Private health care organizations
- Local communities and community groups
- NGOs
- International partners
- Institute of Medicine
- World Health Organization
Outcome Measures/Metrics of Success
To evaluate the outcome of this proposed project, we propose two methods of ascertaining outcome data. The first would rely on routinely collected health information through the county health facilities. The second would rely on community-based assessments, which would extend to other MNS disorders to enable us to expand this work to encompass a greater range of disorders.
Outputs and Outcomes
Health facility assessment
Health facility
- Number of community health workers and health care workers trained to care for MNS disorders
- Availability of essential drugs for MNS disorders
- Stock-outs of essential drugs for MNS disorders
Health usage
- Number of individuals receiving MNS interventions by community health workers
- Number of individuals referred to primary care settings for treatment of MNS disorders
- Number of individuals receiving MNS interventions by primary care staff
- Number of individuals with MNS disorders receiving referrals to secondary or tertiary care
- Number of individuals with completed referrals to secondary or tertiary care
- Number of calls received by the hotline
Community-Based Assessment
Prevalence rates for MNS disorders
- Prevalence of mental disorders
- Depression
- Schizophrenia
- Prevalence of substance use disorders
- Alcohol
- Tobacco
- Other drugs
- Prevalence of neurological disorders
- Epilepsy
- Stroke
- Dementia
- Parkinson’s disease
Self-reported measures
- Stigma
- Perceived quality of care
- Quality of life
- Economic measures
Disease-specific outcome metrics
- Depression
- Change in depressive symptoms
- Epilepsy
- Number of individuals with active epilepsy
- Number of individuals with active epilepsy receiving adequate treatment
- Change in seizure frequency
- Alcohol use
- Change in quantity of alcohol use
- Change in severity of alcohol use
REFERENCES
1. Whitefort, H. A., L. Degenhardt, J. Rehm, A. J. Baxter, A. J. Ferrari, H. E. Erskine, F. J. Charlson, R. E. Norman, A. D. Flaxman, N. Johns, R. Burnstein, C. J. L. Murray, and T. Vos. 2013. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 382:1575-1586.
2. Stovner, L. J., J. M. Hoff, S. Svalheim, and N. E. Gilhus. 2014. Neurological disorders in the Global Burden of Disease 2010 Study. Facta Neurologica Scandinavica Supplementum 129(Suppl. 198): 1-6.
3. Institute for Health Metrics and Evaluation. 2010. Tree map (causes) Kenya (DALYs). http://vizhub.healthdata.org/gbd-compare (accessed November 25, 2014).
4. NACADA (National Authority for the Campaign Against Alcohol and Drug Abuse). 2012. Rapid situation assessment of the status of drug and substance abuse in Kenya, 2012. http://www.nacada.go.ke/documents-andresources/category/8-statistics-research-survey-findings (accessed November 24, 2014).
5. Kakuma, R., H. Minas, N. van Ginneken, M. R. Dal Paz, K. Desiraju, J. E. Morris, S. Saxena, and R. M. Scheffler. 2011. Human resources for mental health care: Current situation and strategies for action. Lancet 378:1654-1663.
6. WHO (World Health Organization). 2005. Atlas: Epilepsy care in the world. Programme for Neurological Disease and Neuroscience Department of Mental Health and Substance Abuse. Geneva, Switzerland: WHO.
7. WHO. 2004. Atlas: Country resources for neurologic disorders. World Federation of Neurology. Geneva, Switzerland: WHO.
8. Ndetei, D. M. 2014. Personal communication.
9. Kiima, D., and R. Jenkins. 2010. Mental health policy in Kenya—An integrated approach to scaling up equitable care for poor populations. International Journal of Mental Health Systems 4(19):1-8.
10. Meyer, A. 2014. East African College of Neurology: Needs assessment. Unpublished data.
11. Wang, P. S., S. Aguilar-Gaxiola, J. Alonso, M. C. Angermeyer, G. Borges, E. J. Bromet, R. Bruffaerts, G. de Girolamo, R. de Graaf, O. Gureje, J. M. Haro, E. G. Karam, R. C. Kessler, V. Kovess, M. C. Lane, S. Lee, D. Levinson, Y. Ono, M. Petukhova, J. Posada-Villa, S. Seedat, J. E. Wells. 2007. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 370 (9590):841-850.
12. Meyer, A., T. Dua, J. Ma, S. Saxena, and G. Birbeck. 2010. Global disparities in the epilepsy treatment gap: A systematic review. Bulletin of the World Health Organization 88:260-266.
13. Mbuba, C. K., A. K. Ngugi, C. R. Newton, and J. A. Carter. 2008. The epilepsy treatment gap in developing countries: A systematic review of the magnitude, causes, and intervention strategies. Epilepsia 49(9):1491-1503.
14. Meyer, A., T. Dua, W. J. Boscardin, J. J. Escarce, S. Saxena, and G. Birbeck. 2012. Critical determinants of the epilepsy treatment gap: A cross-national analysis in resource-limited settings. Epilepsia 53(12):2178-2185.
15. Mbuba, C. K., A. K. Ngugi, G. Fegan, F. Ibinda, S. N. Muchohi, O. Nyundo, R. Odhiambo, T. Edwards, P. Odermatt, J. A. Carter, and C. R. Newton. 2012. Risk factors associated with the epilepsy treatment gap in Kilifi, Kenya: A cross-sectional study. Lancet Neurology 11(8):688-696.
16. Demyttenaere, K., R. Bruffaerts, J. Posada-Villa, I. Gasquet, V. Kovess, J. P. Lepine, M. C. Angermeyer, S. Bernert, G. de Girolamo, P. Morosini, G. Polidori, T. Kikkawa, N. Kawakami, Y. Ono, T. Takeshima, H. Uda, E. G. Karam, J. A. Fayyad, A. N. Karam, Z. N. Mneimneh, M. E. Medina-Mora, G. Borges, C. Lara, R. de Graaf, J. Ormel, O. Gureje, Y. Shen, Y. Huang, M. Zhang, J. Alonso, J. M. Haro, G. Vilagut, E. J. Bromet, S. Gluzman, C. Webb, R. C. Kessler, K. R. Merikangas, J. C. Anthony, M. R. Von Korff, P. S. Wang, T. S. Brugha, S. Aguilar-Gaxiola, S. Lee, S. Heeringa, B. E. Pennell, A. M. Zaslavsky, T. B. Ustun, S. Chatterji, and WHO World Mental Health Survey Consortium. 2004. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Journal of the American Medical Association 291(21):2581-2590.
17. Drew, N., M. Funk, S. Tang, J. Lamichhane, E. Chávez, S. Katontoka, S. Pathare, O. Lewis, L. Gostin, and B. Saraceno. 2011. Human rights violations of people with mental and psychosocial disabilities: An unresolved global crisis. Lancet 378(9803):1664-1675.
18. Amoroso, C., A. Zwi, E. Somerville, and N. Grove. 2006. Epilepsy and stigma. Lancet 367(9517):1143-1144.
19. Baskind, R., and G. Birbeck. 2005. Epilepsy-associated stigma in sub-Saharan Africa: The social landscape of a disease. Epilepsy & Behavior 7(1):68-73.
20. de Boer, H., M. Mula, and J. W. Sander. 2008. The global burden and stigma of epilepsy. Epilepsy & Behavior 12(4):540-546.
21. Jacoby, A., D. Snape, and G. A. Baker. 2005. Epilepsy and social identity: The stigma of a chronic neurological disorder. Lancet Neurology 4(3):171-178.
22. Baingana, F., A. Alem, and R. Jenkins. 2006. Mental health and abuse of alcohol and controlled substances. International Bank for Reconstruction and Development. Washington, DC: The World Bank.
23. Kessler, R. C., S. Aguilar-Gaxiola, J. Alonso, S. Chatterji, S. Lee, J. Ormel, T. B. Ustün, and P. S. Wang. 2009. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiologia e Psichiatria Sociale 18(1):23-33.
24. Cortina, M. A., A. Sodha, M. Fazel, and P. G. Ramchandani. 2012. Prevalence of child mental health problems in sub-Saharan Africa: A systematic review. Archives of Pediatrics & Adolescent Medicine 166(3):276-281.
25. Institute of Medicine (IOM). 2014. Improving access to essential medicines for mental, neurological, and substance use disorders in sub-Saharan Africa: Workshop summary. Washington, DC: The National Academies Press.
26. Silberberg, D., and E. Katabira. 2006. Neurological Disorders. International Bank for Reconstruction and Development. Washington, DC: The World Bank.
27. Adeloye, D. 2014. An estimate of the incidence and prevalence of stroke in Africa: A systematic review and meta-analysis. PLoS ONE 9(6):e100724.
28. George-Carey, R., D. Adeloye, K. Y. Chan, A. Paul, I. Kolčić, H. Campbell, and I. Rudan. 2012. An estimate of the prevalence of dementia in Africa: A systematic analysis. Journal of Global Health 2(2):020401.
29. Ngugi, A. K., C. Bottomley, I. Kleinschmidt, R. G. Wagner, A. Kakooza-Mwesige, K. Ae-Ngibise, S. Owusu-Agyei, H. Masanja, G. Kamuyu, R. Odhiambo, E. Chengo, J. W. Sander, C. R. Newton, and Study of Epidemiology of Epilepsy in Demographic Sites (SEEDS) group. 2013. Prevalence of active convulsive epilepsy in sub-Saharan Africa and associated risk factors: Cross-sectional and case-control studies. Lancet Neurology 12(3):253-263.
30. Paul, A., D. Adeloye, R. George-Carey, I. Kolčić, L. Grant, and K. Y. Chan. 2012. An estimate of the prevalence of epilepsy in sub-Saharan Africa: A systematic analysis. Journal of Global Health 2(2):020405.
31. Birbeck, G. L. 2000. Seizures in rural Zambia. Epilepsia 41(3):277-281.
32. Birbeck, G., E. Chomba, M. Atadzhanov, E. Mbewe, and A. Haworth. 2007. The social and economic impact of epilepsy in Zambia: A cross-sectional study. Lancet Neurology 6(1):39-44.
33. Ding, D., W. Wang, J. Wu, G. Ma, X. Dai, B. Yang, T. Wang, C. Yuan, Z. Hong, H. M. de Boer, L. Prilipko, and J. W. Sander. 2006. Premature mortality in people with epilepsy in rural China: A prospective study. Lancet Neurology 5(10):823-827.
34. Jacoby, A., D. Snape, and G. A. Baker. 2005. Epilepsy and social identity: The stigma of a chronic neurological disorder. Lancet Neurology 4(3):171-178.
35. Jilek-Aall, L., and H. T. Rwiza. 1992. Prognosis of epilepsy in a rural African community: A 30-year follow-up of 164 patients in an outpatient clinic in rural Tanzania. Epilepsia 33(4):645-650.
36. Gore, F. M., P. J. Bloem, G. C. Patton, J. Ferguson, V. Joseph, C. Coffey, S. M. Sawyer, and C. D. Mathers. 2011. Global burden of disease in young people aged 10-24 years: A systematic analysis. Lancet 377(9783):2093-2102.
37. Mugisha, F., J. Arinaitwe-Mugisha, and B. Hagembe. 2003. Alcohol, substance and drug use among urban slum adolescents in Nairobi, Kenya. Cities 20:231-240.
38. Janz, N. K., and M. H. Becker. 1984. The health belief model: A decade later. Health Education Quarterly 11(1):1-47.
39. Phelan, J. C., B. G. Link, A. Stueve, and B. A. Pescosolido. 2000. Public conceptions of mental illness in 1950 and 1996: What is mental illness and is it to be feared? Journal of Health and Social Behavior 41(2):188-207.
40. Ben-Zeev, D., M. A. Young, and P. W. Corrigan. 2010. DSM-V and the stigma of mental illness. Journal of Mental Health 19(4):318-327.
41. Corrigan, P. W., F. E. Markowitz, and A. C. Watson. 2004. Structural levels of mental illness stigma and discrimination. Schizophrenia Bulletin 30(3):481-491.
42. Lauber, C., and W. Rössler. 2007. Stigma towards people with mental illness in developing countries in Asia. International Review of Psychiatry 19(2):157-178.
43. Kiima, D. M., F. G. Njenga, M. M. Okonji, and P. A. Kigamwa. 2004. Kenya mental health country profile. International Review of Psychiatry 16(1-2):48-53.
44. Scheffer, R. 2003. Addressing stigma: Increasing public understanding of mental illness. Presented to the Standing Committee on Social Affairs, Science, and Technology. Ontario, Canada: Centre for Addiction and Mental Health.
45. Mbwayo, A. W., D. M. Ndetei, V. Mutiso, L. I. Khasakhala. 2013. Traditional healers and provision of mental health services in cosmopolitan informal settlements in Nairobi, Kenya. African Journal of Psychiatry 16(2):134-140.
46. Chukwuemeka, N. K. 2009. Traditional psychiatric healing in Igbo land, southeastern Nigeria. African Journal of History and Culture 1(2):36-43.
47. Abiodun, O. A. 1995. Pathways to mental health care in Nigeria. Psychiatric Services 46(8):823-826.
48. Ngoma, M. C., M. Prince, and A. Mann. 2003. Common mental disorders among those attending primary health clinics and traditional healers in urban Tanzania. The British Journal of Psychiatry: The Journal of Mental Science 183:349-355.
49. Amzat, J., and A. A. Abdullahi. 2008. Roles of traditional healers in the fight against HIV/AIDS. EthnoMed 2(2):153-159.
50. Offiong, D. 1999. Traditional healers in the Nigerian health care delivery system and the debate over integrating traditional and scientific medicine. Anthropological Quarterly 72:118.
51. KNBS (Kenya National Bureau of Statistics). 2010. 2009 Kenya Population and Housing Census. Nairobi, Kenya: Ministry of Devolution and Planning.
52. Kothari, M. L., and L. A. Mehta. 1988. Violence in modern medicine. In Science, hegemony, and violence: A requiem for modernity, edited by A. Nandy. Oxford: Oxford University Press.
53. Richter, M. 2003. Traditional medicines and traditional healers in South Africa. In Discussion paper prepared for the Treatment Action Campaign and AIDS Law Project. http://www.tac.org.za/Documents/ResearchPapers/Traditional_Medicine_briefing.pdf (accessed August 17, 2015).
54. Peltzer, K., N. Mngqundaniso, and G. Petros. 2006. A controlled study of an HIV/AIDS/STI/TB intervention with traditional healers in KwaZulu-Natal, South Africa. AIDS and Behavior 10(6):683-690.
55. Okome-Nkoumou, M., F. Okome-Miame, E. Kendjo, G. P. Obiang, P. Kouna, O. Essola-Biba, J. Bruno Boguikouma, M. Mboussou, and P. Clevenbergh. 2005. Delay between first HIV-related symptoms and diagnosis of HIV infection in patients attending the internal medicine deparment of the Foundation Jeanne Ebori (FJE), Libreville, Gabon. HIV Clinical Trials 6(1):38-42.
56. de Andrade, V., and E. Ross. 2005. Beliefs and practices of black South African traditional healers regarding hearing impairment. International Journal of Audiology 44(9):489-499.
57. Okeke, T. A., H. U. Okafor, and B. S. Uzochukwu. 2006. Traditional healers in Nigeria: Perception of cause, treatment and referral practices for severe malaria. Journal of Biosocial Science 38(4):491-500.
58. Sorsdahl, K., D. J. Stein, and A. J. Flisher. 2013. Predicting referral practices of traditional healers of their patients with a mental illness: An application of the theory of planned behavior. African Journal of Psychiatry 16(1):35-40.
59. WHO. 2008. Mental Health Gap Action Programme (mhGAP): Scaling up care for mental, neurological, and substance use disorders. Geneva, Switzerland: World Health Organization.
60. Patel, V., R. Araya, S. Chatterjee, D. Chisholm, A. Cohen, M. De Silva, C. Hosman, H. McGuire, G. Rojas, and M. van Ommeren. 2007.
Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet 370(9591):991-1005.
61. Ding, D., Z. Hong, G. S. Chen, X. Y. Dai, J. Z. Wu, W. Z. Wang, H. M. de Boer, J. W. Sander, L. Prilipko, and D. Chisholm. 2008. Primary care treatment of epilepsy with phenobarbital in rural China: Cost-outcome analysis from the WHO/ILAE/IBE global campaign against epilepsy demonstration project. Epilepsia 49(3):535-539.
62. Wells, K. B., L. Jones, B. Chung, E. L. Dixon, L. Tang, J. Gilmore, C. Sherbourne, V. K. Ngo, M. K. Ong, S. Stockdale, E. Ramos, T. R. Belin, and J. Miranda. 2013. Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. Journal of General Internal Medicine 28(10):1268-1278.
63. Hegerl, U., D. Althaus, A. Schmidtke, and G. Niklewski. 2006. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychological Medicine 36(9):1225-1233.
64. de Boer, H. M., S. L. Moshé, S. R. Korey, and D. P. Purpura. 2013. ILAE/IBE/WHO global campaign against epilepsy: A partnership that works. Current Opinion in Neurology 26(2):219-225.
65. Dua, T., H. M. de Boer, L. L. Prilipko, and S. Saxena. 2006. Epilepsy care in the world: Results of an ILAE/IBE/WHO global campaign against epilepsy survey. Epilepsia 47(7):1225-1231.
66. Li, L. M., P. T. Fernandes, A. L. Noronha, L. H. Marques, M. A. Borgues, K. Borges, F. Cendes, C. A. Guerreiro, D. M. Zanetta, H. M. de Boer, J. Espíndola, C. T. Miranda, L. Prilipko, and J. W. Sander. 2007. Demonstration project on epilepsy in Brazil: outcome assessment. Arquivos de Neuro-psiquiatria 65(Suppl. 1):58-62.
67. Wang, W. Z., J. Z. Wu, G. Y. Ma, X. Y. Dai, B. Yang, T. P. Wang, C. L. Yuan, Z. Hong, G. S. Bell, L. Prilipko, H. M. de Boer, and J. W. Sander. 2006. Efficacy assessment of phenobarbital in epilepsy: A large community-based intervention trial in rural China. Lancet Neurology 5(1):46-52.
68. Lomidze, G., S. Kasradze, D. Kvernadze, N. Okujava, O. Toidze, H. M. de Boer, T. Dua, and J. W. Sander. 2012. The prevalence and treatment gap of epilepsy in Tbilisi, Georgia. Epilepsy Research 98(2-3):123-129.
69. Ndoye, N. F., A. D. Sow, A. G. Diop, B. Sessouma, F. Séne-Diouf, L. Boissy, I. Wone, K. Touré, M. Ndiaye, P. Ndiaye, H. de Boer, J. Engel, C. Mandlhate, H. Meinardi, L. Prilipko, and J. W. Sander. 2005. Prevalence of epilepsy, its treatment gap and knowledge, attitude and practice of its population in sub-urban Senegal: An ILAE/IBE/WHO study. Seizure 14(2):106-111.
70. Global Campaign Against Epilepsy. 2010. Demonstration project on epilepsy in Zimbabwe. http://www.globalcampaignagainstepilepsy.org/demonstration-project-on-epilepsy-in-zimbabwe (accessed No-ember 25, 2014).
71. McCrady, B. S., M. D. Owens, A. Z. Borders, and J. M. Brovko. 2014. Psychosocial approaches to alcohol use disorders since 1940: A review. Journal of Studies on Alcohol and Drugs 75(Suppl. 1):68-78.
72. Hung, G. M., and N. H. Azrin. 1973. A community-reinforcement approach to alcoholism. Behavior Research and Therapy 11:91-104.
73. Cheadle, A., D. Pearson, E. Wagner, B. M. Psaty, P. Diehr, and T. Koepsell. 1995. A community-based approach to preventing alcohol use among adolescents on an American Indian reservation. Public Health Reports 110(4):439-447.
74. Shakeshaft, A., D. Petrie, C. Doran, C. Breen, and R. Sanson-Fisher. 2012. An empirical approach to selecting community-based alcohol interventions: Combining research evidence, rural community views and professional opinion. BMC Public Health 12(25):1-11.
75. Ministry of Health, Republic of Kenya. 2005. Reversing the trends: The second national health sector strategic plan (NHSSP) of Kenya—NHSSP II. Nairobi, Kenya: Ministry of Health.
76. WHO. 2012. Kenya Country Profile. Geneva, Switzerland: WHO. http://www.who.int/countries/ken/en (accessed November 26, 2014).
77. Miller, M. J., and S. Castles. 1993. The Age of Migration, 4th ed. New York: The Guilford Press.
78. Odhiambo-Otieno, G. W., and W. W. O. Odero. 2005. Evaluation criteria for the district health management information systems: Lessons from the Ministry of Health, Kenya. International Journal of Medical Informatics 74(1):31-38.
79. Kombo, A. 2010. Strengthening the Kenya health management information system (HMIS) for monitoring and evaluation of the AIDS, Population, and Health Integrated Assistance (APHIA) II Nyanza Project, June 2006–December 2010. Nairobi, Kenya: EngenderHealth. https://www.engenderhealth.org/files/pubs/localized/kenya/aphia/strengthening-hmis.pdf (accessed August 17, 2015).
80. Kibet, S., P. Wanjala, F. Gikunda, M. Chiseka, S. Athman, H. Osoro, N. Amayo, A. Corea, and J. Onsongo. 2008. Republic of Kenya health sector report for the assessment of the health information system of Kenya. Nairobi, Kenya: Health Metrics Network. http://www.who.int/healthmetrics/library/countries/HMN_KEN_Assess_Final_2008_06_en.pdf (accessed August 17, 2015).
81. Public education in epilepsy. Bollettino—Lega Italiana contro l’Epilessia 2002:69-71.
82. KNBS and ICF International. 2010. Kenya demographic and health survey 2008-2009. Calverton, Maryland: KNBS and ICF Macro.
83. NASCOP (National AIDS and STI Control Programme). 2014. Kenya AIDS indicator survey 2012: Final report. Nairobi, Kenya: NASCOP. http://www.nacc.or.ke/images/documents/KAIS-2012.pdf (accessed August 17, 2015).
84. Kaneko, S., E. M. Mushinzimana, and M. Karama. 2007. Demographic surveillance system (DSS) in Suba district, Kenya. Tropical Medicine and Health 35(35):37-40.
85. Scott, J. A., E. Bauni, J. C. Moisi, J. Ojal, H. Gatakaa, C. Nyundo, C. S. Molyneux, F. Kombe, B. Tsofa, K. Marsh, N. Peshu, and T. N. Williams. 2012. Profile: The kilifi health and demographic surveillance system (KHDSS). International Journal of Epidemiology 41(3):650-657.
86. Kamuyu, G., C. Bottomley, J. Mageto, B. Lowe, P. P. Wilkins, J. C. Noh, T. B. Nutman, A. K. Ngugi, R. Odhiambo, R. G. Wagner, A. Kakooza-Mwesige, S. Owusu-Agyei, K. Ae-Ngibise, H. Masanja, F. H. Osier, P. Odermatt, C. R. Newton, and SEEDS group. 2014. Exposure to multiple parasites is associated with the prevalence of active convulsive epilepsy in sub-Saharan Africa. PLoS Neglected Tropical Diseases 8(5):e2908.
87. Odhiambo, F. O., K. F. Laserson, M. Sewe, M. J. Hamel, D. R. Feikin, K. Adazu, S. Ogwang, D. Obor, N. Amek, N. Bayoh, M. Ombok, K. Lindblade, M. Desai, F. ter Kuile, P. Phillips-Howard, A. M. van Eijk, D. Rosen, A. Hightower, P. Ofware, H. Muttai, B. Nahlen, K. DeCock, L. Slutsker, R. F. Breiman, and J. M. Vulule. 2012. Profile: The KEMRI/CDC health and demographic surveillance system—western Kenya. International Journal of Epidemiology 41(4):977-987.
88. Sifuna, P., M. Oyugi, B. Ogutu, B. Andagalu, A. Otieno, V. Owira, N. Otsyula, J. Oyieko, J. Cowden, L. Otieno, W. Otieno. 2014. Health and demographic surveillance system profile: The kombewa health and demographic surveillance system (Kombewa HDSS). International Journal of Epidemiology 43(4):1097-1104.
89. Kyobutungi, C., A. K. Ziraba, A. Ezeh, and Y. Yé. 2008. The burden of disease profile of residents of Nairobi’s slums: Results from a demographic surveillance system. Population Health Metrics 6:1-8.
90. Wanyua, S., M. Ndemwa, K. Goto, J. Tanaka, J. K’Opiyo, S. Okumu, P. Diela, S. Kaneko, M. Karama, Y. Ichinose, and M. Shimada. 2013. Profile: The Mbita health and demographic surveillance system. International Journal of Epidemiology 42(6):1678-1685.
91. Jenkins, R., D. Kiima, F. Njenga, M. Okonji, J. Kingora, D. Kathuku, and S. Lock. 2010. Integration of mental health into primary care in Kenya. World Psychiatry 9(2):118-120.
92. Cettomai, D., J. Kwasa, G. Birbeck, R. Price, E. Bukusi, and A. Meyer. 2011. Training needs and evaluation of a neuro-HIV training module for non-physician healthcare workers in western Kenya. Journal of the Neurological Sciences 307(1-2):92-96.
93. Ministry of Medical Services and Ministry of Public Health & Sanitation. 2010. Kenya Essential Medicines List 2010. Nairobi, Kenya: Ministry of Medical Services & Public Health and Sanitation. http://apps.who.int/medicinedocs/documents/s1869e-n/s18694en.pdf (accessed August 18, 2015).
94. Pharmacy and Poisons Board. 2015. Registered Human Drugs—Classical Gazette. Pharmacy and Poisons Board. http://pharmacyboardkenya.org/?p=516 (accessed November 24, 2014).
95. KEMSA (Kenya Medical Supplies Authority). 2013. KEMSA medicines and medical supplies price list. Nairobi, Kenya: KEMSA. http://kemsa.co.ke/pdfs/KEMSA%20New%20Business%20Model%20Price%20List.pdf (accessed August 18, 2015).
96. Division of Non-communicable Diseases. 2014. Kenya national guidelines for the management of epilepsy: A practical guide for healthcare workers. Nairobi, Kenya: Ministry of Health. http://www.epilepsykenya.org/downloads/epilepsy%20guidelines%20content%20lite.pdf (accessed August 18, 2015).
97. Luoma, M., J. Doherty, S. Muchiri, T. Barasa, K. Hofler, L. Maniscalco, R. Kirika, C. Ouma, and J. Maundu. 2010. Kenya Health Assessment 2010. Bethesda, MD: U.S. Agency for International Development. http://www.cmamforum.org/Pool/Resources/Kenya-HSA-ReportFinal-2010.pdf (accesed August 18, 2015).
98. Pharmaceutical Journal Online News. 2003. New anxiolytics from quinolones? The Pharmaceutical Journal 271(7279):806.
99. Miyanji, O. 2014. What is being done to target improved care for patients with epilepsy in east Africa. Presented at 2nd African Epilepsy Congress, May 21-24, 2014, Cape Town, South Africa.
100. Wafula, S. 2013. Epilepsy awareness month #kifafainatiba campaign launch. In My Mind, My Funk. http://sitawa.blogspot.com/2013/11/epilespy-awareness-month-kifafainatiba.html (accessed August 18, 2015).
101. Madegwa, D. 2013. Kenya: Purple day today to support epilepsy. AllAfrica Global Media. http://allafrica.com/stories/201303260853.html (accessed August 18, 2015).
102. Republic of Kenya National Assembly. Mental health bill 2014. 22. 2014.
103. Petersen, I., C. Lund, and D. J. Stein. 2011. Optimizing mental health services in low-income and middle-income countries. Current Opinion in Psychiatry 24(4):318-323.
104. WHO. 2013. Mental health action plan 2013-2020. Geneva, Switzerland: World Health Organization.
105. Patel, V., and G. Thornicroft. 2009. Packages of care for mental, neurological, and substance use disorders in low- and middle-income countries: PLoS medicine series. PLoS Medicine 6(10):e1000160.
106. Ministry of Health. 2006. Taking the Kenya essential package for health to the community: A strategy for the delivery of level one services. Nairobi,
Kenya: Ministry of Health. http://www.communityledtotalsanitation.org/sites/communityledtotalsanitation.org/files/commu nity_strategy.pdf (accessed August 18, 2015).
107. Odeny, T., J. Penner, J. Lewis-Kulzer, H. H. Leslie, S. B. Shade, W. Adero, J. Kioko, C. R. Cohen, and E. A. Bukusi. 2013. Integration of HIV care with primary health care services: Effect on patient satisfaction and stigma in rural Kenya. AIDS Research and Treatment 2013:1-10.
108. Petersen, I., J. Ssebunnya, A. Buhana, K. Baillie, and the Mental Health and Poverty Project Research Consortium. 2011. Lessons from case studies of integrating mental health into primary health care in South Africa and Uganda. International Journal of Mental Health Systems 5:1-12.
109. IOM. 2013. Strengthening human resources through development of candidate core competencies for mental, neurological and substance use disorders in sub-Saharan Africa: Workshop summary. Washington, DC: The National Academies Press.
110. Kauye, F., R. Jenkins, and A. Rahman. 2014. Training primary health care workers in mental health and its impact on diagnoses of common mental disorders in primary care of a developing country, malawi: A cluster-randomized controlled trial. Psychological Medicine 44(3):657-666.
111. Jenkins, R., D. Kiima, M. Okonji, F. Njenga, J. Kingora, and S. Lock. 2010. Integration of mental health into primary care and community health working in Kenya: Context, rationale, coverage and sustainability. Mental Health in Family Medicine 7(1):37-47.
112. Gilbody, S., P. Bower, J. Fletcher, D. Richards, and A. J. Sutton. 2006. Collaborative care for depression: A cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine 166(21):2314-2321.
113. Katon, W. J., E. Lin, M. Von Korff, P. Ciechanowski, E. J. Ludman, B. Young, D. Peterson, C. M. Rutter, M. McGregor, and D. McCulloch. 2010. Collaborative care for patients with depression and chronic illness. New England Journal of Medicine 363(27):2611-2620.
114. WHO. 2010. mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Mental Health Gap Action Programme. Geneva, Switzerland: WHO.
115. Kutcher, S., S. Chehil, C. Cash, and J. Millar. 2005. A competencies-based mental health training model for health professionals in low and middle income countries. World Psychiatry 4(3):177-180.
116. Glasgow, N. J., R. Wells, J. Butler, and A. Gear. 2008. The effectiveness of competency-based education in equipping primary health care workers to manage chronic disease in australian general practice settings. The Medical Journal of Australia 188(8 Suppl.):S92-S96.
117. Adachi, N., G. Alarcon, C. D. Binnie, R. D. Elwes, C. E. Polkey, and E. H. Reynolds. 1998. Predictive value of interictal epileptiform discharges during non-REM sleep on scalp EEG recordings for the lateralization of epileptogenesis. Epilepsia 39(6):628-632.
118. Djibuti, M., G. Gotsadze, A. Zoidze, G. Mataradze, L. C. Esmail, and J. C. Kohler. 2009. The role of supportive supervision on immunization program outcome—a randomized field trial from Georgia. BMC International Health and Human Rights 9(Suppl 1):S11.
119. Som, M., B. Panda, S. Pati, S. Nallala, A. Anasuya, A. S. Chauhan, A. K. Sen, and S. Zodpey. 2014. Effect of supportive supervision on routine immunization service delivery—a randomized post-test study in Odisha. Global Journal of Health Science 6(6):61-67.
120. Loevinsohn, B. P., E. T. Guerrero, and S. P. Gregorio. 1995. Improving primary health care through systematic supervision: A controlled field trial. Health Policy Plan 10(2):144-153.
121. Bosch-Capblanc, X., and P. Garner. 2008. Primary health care supervision in developing countries. Tropical Medicine & International Health 13(3):369-383.
122. Hill, Z., M. Dumbaugh, L. Benton, K. Källander, D. Strachan, A. ten Asbroek, J. Tibenderana, B. Kirkwood, and S. Meek. 2014. Supervising community health workers in low-income countries—a review of impact and implementation issues. Global Health Action 7:24085.
123. Karari, C., R. Tittle, J. Penner, J. Kulzer, E. A. Bukusi, R. Marima, and C. R. Cohen. 2011. Evaluating the uptake, acceptability, and effectiveness of Uliza! Clinicians’ HIV hotline: A telephone consultation service in kenya. Telemedicine Journal and e-health 17(6):420-426.
124. Eaton, J., L. McCay, M. Semrau, S. Chatterjee, F. Baingana, R. Araya, C. Ntulo, G. Thornicroft, and S. Saxena. 2011. Scale up services for mental health in low-income and middle-income countries. Lancet 378(9802):1592-1603.
125. UN Data. 2015. Kenya. Geneva, Switzerland: United Nations Statistics Division. http://data.un.org/CountryProfile.aspx?crName=kenya (accessed September 3, 2015).