F
Providing Sustainable Mental Health Care in
Ghana:
A Demonstration Project
Julian Eatona and Sammy Oheneb
A commissioned paper prepared for the April 28–29, 2015, workshop on
Providing Sustainable Mental Health Care in Ghana, hosted by the
National Academies of Sciences, Engineering, and Medicine’s Forum on
Neuroscience and Nervous System Disorders and Board on Global
Health. The authors are responsible for the content of this article, which
does not necessarily represent the views of the National Academies of
Sciences, Engineering, and Medicine.
“Knowing is not enough; we must apply.
Willing is not enough; we must do.”
Goethe
“No condition is permanent.”
Popular Ghanaian saying
aCBM International.
bUniversity of Ghana Medical School.
INTRODUCTION
Ghana has experienced a positive trend in its economic development over the past two decades, and seen a gradual strengthening of its democracy in recent years. This has led to its reclassification (by the World Bank) as a lower middle-income country, and it is on track to meet the Millennium Development Goal of halving extreme poverty by the year 2015. This positive overall picture hides persistent inequity. Infrastructure of basic services, including health, is far from meeting the needs of the population. This is particularly the case in mental health, where many years of neglect have left services even farther behind. This is now beginning to change. Ghana recently adopted a progressive Mental Health Act (2012), a reflection of the substantial efforts made by a growing civil society sector interested in mental health. These efforts, over the past decade, have also seen the emergence of one of the strongest service user movements in Africa, new cadres of trained personnel, and a greater awareness of mental health issues in the country.
This document sets out to propose a model for a project that will build on these considerable achievements, and bring together relevant aspects of evidence-based practice that would make a good fit for the needs of the situation in Ghana. The Institute of Medicine (IOM) has convened several activities related to strengthening the capacity for delivering quality mental health services in low- and middle-income countries (LMICs, a designation by the World Health Organization, or WHO) over many years. The landmark publication Neurological, Psychiatric and Developmental Disorder: Meeting the Needs in the Developing World1 was an early driver of the growth of global mental health as a discipline. In recent years, three key workshops have been held, bringing together international and local experts to explore sustainable solutions to service development challenges, including addressing the treatment gap and improving quality of care, human resource development, and access to appropriate medication.
The first section of the report provides a summary of the context in which the project will run, and the considerations made in development of the project. The second section contains the proposal for the demonstration project itself, made up of a project narrative and logical framework for its successful implementation.
SECTION 1: BACKGROUND AND SITUATION ANALYSIS
General Development Indexes
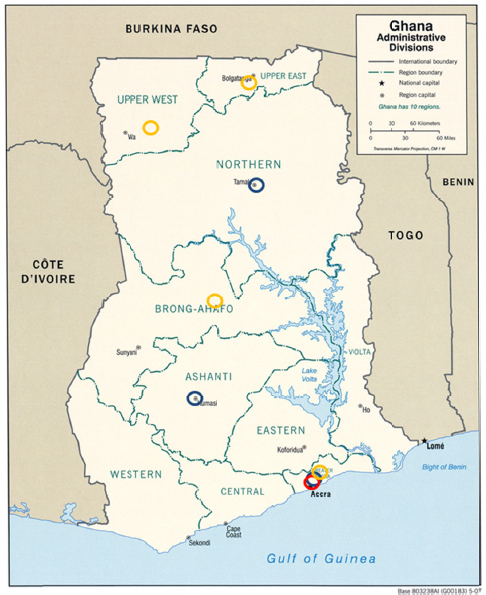
Ghana is a West African country with a population of approximately 25.3 million people (2012) (see Table F-1). About 45 percent of the population are below age 18 (2012), and there is an annual increase in population of 2.5 percent. The population is generally denser in the southern part of the country, and there is a rapid growth in urban populations (currently 52.8 percent of the total population), especially in Accra.
Although there is a strong growth in the economy (7.1 percent in 2013), 28 percent of the population still live on less than $1.23 USD per day, with greater levels of poverty and worse health and development indexes in the northern part of the country.
TABLE F-1 Main Development Indicators (Health, Education, Economy)
| Indicator | Value | Year | Source2, 28–30 |
|---|---|---|---|
| Total population | 25,366,500 | 2012 | Census |
| Population under 18 years | 11,423,500 (45% of total) | 2012 | Census |
| Population annual growth rate | 2.5% | 2012 | UNICEF |
| Life expectancy at birth | 61 years | 2012 | UNICEF |
| Under-5 mortality rate | 82 deaths/1,000 live births | 2011 | MICS |
| Maternal mortality rate | 378 deaths/100,000 live births | 2011 | UNICEF |
| Primary school net attendance rate | 73% | 2011 | MICS |
| Literacy rate (total) | 82% | 2012 | UNICEF |
| Population below international poverty line (USD 1.25 per day) | 28.6% | 2011 | World Bank |
| Gross national income per capita | USD 1,594 | 2011 | World Bank |
| GDP | $47.93 billion | 2013 | World Bank |
| GDP growth | 7.1% | 2013 | World Bank |
| Human development index and rank | 0.573 Rank 138th (out of 187) | 2014 | UNDP HDI/R |
NOTE: GDP = gross domestic product; HDI/R = human development index and rank; MICS = Multi-Indicator Cluster Survey (UNICEF); UNDP = United Nations Development Program; UNICEF = United Nations Children’s Fund; USD = United States dollar.
Health Services
Despite good progress since the 1990s, as shown by infant and under-5 mortality rates that have halved between 1980 and 2012 and an increasing life expectancy (see Figure F-1), provision of health services is generally weak and inconsistent in quality across the country.
The Ministry of Health (MoH) provides policy direction for all health-related issues in Ghana, and the Ghana Health Service (GHS) is responsible for provision of public health services. The system is functionally divided into the 216 administrative districts covering the 10 regions of the country. Each district has a District Health Management Team headed by a district director, who reports to the regional director. Every region has a regional hospital, and each district should have a district hospital, although the facilities available in some are limited. Subdistricts are served by health centers (see Table F-2).
The smallest unit of health care in the Ghanaian public health system is the Community-based Health Planning and Service Compounds (CHPS) compound, providing the most basic health care. Most communities have CHPS compounds, but the nearest health center or district hospital may be quite a distance away, especially in the northern parts of the country. Access is also further limited by the poor transportation network in many rural areas, and the high costs of transport.
A number of faith-based health facilities provide services in Ghana. Most are organized under the ambit of the Christian Health Association of Ghana (CHAG). Their facilities are controlled by the churches, while the Ghana government pays the salaries of the nurses and doctors who work there. CHAG runs 58 hospitals and 121 health centers. Their facilities are responsible for 20 percent of outpatient visits and 30 percent of hospital admissions.
Private clinics are available in parts of the country, and provide an important first point of contact with services for many people, especially in urban areas, but their services are generally more expensive.
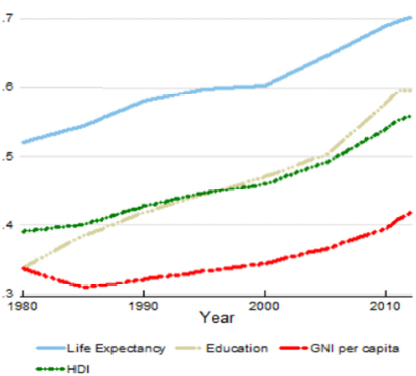
FIGURE F-1 Contribution of human development index (HDI) domains to gradual improvement in HDI and gross national income (GNI) in Ghana (1980–2012).c
TABLE F-2 Current Health Facilities and Human Resources
| Facilities | |
|---|---|
| Hospitals (total) | 244 |
| Regional hospitals | 10 |
| District hospitals | 130 |
| Health centers Community-based health planning and service compounds | 810 1,562 |
| Personnel | |
| Doctors (total) | 2,200 |
| Physician assistants | 2,280 |
| Registered nurses | 17,322 |
cAs defined by the Abuja Declaration of 2001.
The National Health Insurance Scheme (NHIS) introduced in 2007 provides coverage for most common disease conditions. It is available upon payment of an annual premium of GHS20.00 or $6.00, which is about 3 days of the minimum wage and considered affordable. Registration by an adult parent gives automatic coverage to all offspring below age 16. The poorest members of communities can register for free. About 10 million of the estimated 25 million population is currently covered. The low level of state funding has an impact on the quality of these services. For example, many service providers complain that they are not reimbursed for services provided in a reasonable time. Nevertheless, the plan is still widely used and serves to lessen considerably the strain on families. Perinatal care and delivery, including caesarean sections, in public facilities is free.
Mental Health Services
Mental health services are provided in three large psychiatric hospitals, all located in the coastal south, and in smaller psychiatric units in five regional hospitals (see Appendix 1). Three teaching hospitals, one each in the south (Accra), central (Kumasi), and northern (Tamale) parts of the country, provide services on a relatively small scale. Each has at least one psychiatrist, with services consisting of inpatient and busy outpatient departments.
Large parts of the country receive psychiatric services from community psychiatric nurses (CPNs), who can be found in 159 of the 216 districts. These CPNs work in the communities, but operate from district hospitals. There are four community-based mental health services, which are nongovernmental or faith based and mainly based in the middle and south of the country. In the Upper East and Upper West Regions, there are community-based rehabilitation (CBR) programs, again faith based, which link clients to GHS CPNs.
Since the Mental Health Act was enacted in 2012, a new Mental Health Authority has been charged with managing mental health issues, though it is still in its formative stages. The governing body of the Mental Health Authority is an 11-member board with a number of committees under it. There is an acting chief executive officer responsible for daily operations of the Authority. Legislative instrument and the law governing the source of mental health funding has yet to be passed, and funding streams for its activities have not been determined.
The psychiatric hospitals and CPNs provide the majority of psychiatric services in the country. The level of knowledge and standard of care offered to people with mental disorders by general practitioners and primary care services is generally poor. Most general practitioners avoid seeing people with psychiatric problems, preferring to refer them to the few mental health care providers. There are many reasons for the low level of interest in mental health. It is stigmatized and is not seen as an income-generating field or a positive career choice. Therefore, the area has been generally neglected by professionals and the health service sector, including international development agencies.
There are few non-health-oriented services, though a small number of CBRs interact with GHS-based nurses to provide a more comprehensive model of care in the north of the country. A few nongovernmental organizations (NGOs) provide community-based services, especially for substance abuse and in a few, for people with mental disorders.
Two special schools for children with intellectual disabilities, one private, and another funded by the government, exist in Accra. Every regional capital has a school for intellectual disabilities. A few small facilities for the care of children with autistic spectrum disorders have been set up by individuals. Professional psychiatric social work services are virtually non-existent and social services receive negligible funding from the state. There is no dedicated forensic psychiatric facility in Ghana, and the mentally ill who violate the law are often kept in the Accra Psychiatric Hospital, some indefinitely. Prisons have high rates of mental illness, with inadequate care provided.
Given this lack of services, particularly in more rural areas, it is not surprising that there is a large treatment gap. In nearby Nigeria, which has better resources, this gap was found to be 90 percent (as defined by those with DSM IV, or Diagnostic and Statistical Manual, version 4, disorders not receiving any treatment within the previous 12 months).3 The treatment gap for mental health disorders in Ghana is estimated at more than 98 percent.
The Informal Sector
Most people who start exhibiting signs of mental illness (especially in the rural communities) will first be taken to a traditional healer, herbalist, or religious leader, such as a Christian Pastor or Muslim Imam. This is because mental health problems are generally perceived as spiritual, and often seen as punishment for doing wrong. The treatment of-
fered, particularly for people with severe and enduring mental disorders like schizophrenia, can be very abusive and often makes the problem worse.4 Engaging faith leaders is important given their position of authority in communities in health care. Some efforts have been made to work constructively, but this remains a challenge due to the high levels of human rights abuse in some areas, and the fact that provision of modern mental health services can sometimes be unwelcome because it challenges authority and competes for their source of income.5
System Factors Impacting on Mental Health Services
Progressive change in mental health services cannot happen in a vacuum and is dependent on the existing health infrastructure, particularly if there is a commitment to investing in sustainable change through integration in mainstream structures. Comprehensive mental health services must provide access to biological, psychological, and social interventions (or facilitate access to such services for those who need them).
- Access to biological treatments: Having professionals in the right place with the right skills to prescribe appropriate medications is important, but cannot be done without a reliable supply of medications. This is particularly the case for severe mental disorders such as schizophrenia, bipolar affective disorder, moderate and severe depression, and epilepsy. Such evidence-based medical interventions are advised in the mhGAP Intervention Guide, a publication by the WHO Mental Health Gap Action Program (mhGAP).
The government policy on mental health care has always been and remains to provide psychiatric treatment, including admissions and all medications, for free. In the face of a very small budget, the range and quantities of medications provided is often grossly inadequate. There is a turnaround time of around 2 years in the public procurement cycle, and in practice most medications are only accessible in the specialist public psychiatric facilities, which often procure them from private pharmacies (or through private donations). In less urban areas, most pharmacies do not find it cost-effective to stock psychopharmacological agents beyond the most basic (and usually inappropriately used) benzodiazepines. The overall result is long periods of shortages
-
of medication, which can lead to relapse of illness, and in the case of epilepsy, dangerous recurrence of seizures.
Costs are generally affordable for the few drugs made available through the state system, but most patients are unable to afford medication, even if they can be obtained from private sources. The real challenge is making an appropriate range of medications easily available at all times to patients within the policy of free care. - Access to psychological treatments: In general, there has been a tendency for mental health services to mainly focus on biological treatments. There are a number of reasons for this: training is biologically focused, and there are few trained psychologists; patients expect and value medication; availability of appropriate, practical talking therapies has been limited even in international guidelines; and it is logistically more complex and expensive to provide talking treatments. Despite this, the evidence is growing for low-intensity, often group or peer, models of therapy, which is an important intervention in many disorders where the evidence implies talking therapies are equally or more effective than medications. Clinical psychologists are nearly absent from Ghana. There are only 16 clinical psychologists in public service in Ghana. This means any solution would require lay providers of simple psychological interventions.
- Access to social interventions: In general, there is inadequate intersectoral collaboration in providing the broad care that many people with mental health problems need. Apart from the few CBR programs, health, education, social welfare, and livelihood services do not engage well together. The emergence of organizations engaged in mental health advocacy made up of multiple stakeholders is a positive development that may help to break down some of the traditional vertical siloes in which different sectors work. The Mental Health Act has seen some collaborative work across agencies.
Health Management Information Systems
Recent years have seen a significant investment in improving the way that information is gathered and managed, both for recordkeeping and data collections for individual patients, and for service-level information. Unfortunately, as is often the case, mental health/psychiatry services
are often not sufficiently integrated into these mainstream systems, and must either develop their own or attempt to advocate for inclusion later.
With the stronger emphasis on mental health by international bodies such as the WHO, standard indicators are now being developed that can guide what data should be gathered for local and national planning, and for providing a means of comparison internationally. The indicators in the WHO Comprehensive Mental Health Action Plan6 are a good example.
Health Promotion, Prevention of Ill Health, and Surveillance
In general, health surveillance is strongest in child and maternal health services that have been a focus of government health efforts, largely driven by the Millennium Development Goals. Within mental health work, awareness-raising activities have been a part in some comprehensive programs. In general though, the capacity to identify people in need early to reduce unnecessary morbidity has been poor, and duration of untreated illness is usually very long, with patients presenting to services very late. Knowledge about mental ill health among first-line clinicians is poor, and referral routes unclear or non-existent outside of major cities.
Human Resources for Mental Health Services
A lack of human resources is often cited as a major barrier to scaling up services in LMICs, and this is a major challenge to delivery of adequate care in Ghana (see Table F-3). The number of psychiatric nurses was estimated at 2.47 per 100,000 in 2011,7 but this is probably an overestimate, particularly as only a proportion of this number work effectively in mental health settings, and the majority are not in the community or in rural areas. This reflects a general concentration of services in cities.
The country has 16 psychiatrists (around 1 per 1.5 million population), but they are mainly based in specialist hospitals in Accra. Many newly trained specialists leave the country to work abroad, where there is also often a shortage of psychiatric nurses and psychiatrists. In fact, there are more Ghanaian psychiatrists working abroad than in Ghana, mainly in the United States and the United Kingdom. Specialist psychiatrists from the diaspora occasionally come to provide teaching in Ghana.8 Within the country, many trained mental health nurses are posted to inappropriate placements in other branches of medicine, so they are inefficiently used.
TABLE F-3 Mental Health Facilities and Human Resources
| Mental health facilities | Number |
|---|---|
| Psychiatric hospitals | 3 |
| Regional hospital with psych unit | 5 |
| Teaching hospital with psych department | 3 |
| Substance Abuse Rehabilitation Centre | 1 |
| Day Centre | 1 |
| Mental health personnel9 | Number |
| Psychiatrists (total) | 16 |
| - of which work in public facilities | 9 |
| Community mental health officers | 493 |
| Psychiatric nurses | 967* |
| - of which are community psychiatric nurses | 160 |
| Clinical psychologists | 100 |
| - of which work in health facilities | 20 |
| Occupational therapists | 1 |
| Psychiatric social workers | 0 |
*Many of whom do not work in mental health.
It is generally accepted that if the challenge of closing the gap in human resources is to be met, this will be done through a task-sharing model, where greater clinical responsibility will be given to less senior personnel than has traditionally been the case. Most recent major, evidence-based global initiatives have followed this principle, but in order to result in safe and quality care, there need to be clearly establish roles and tasks, adequate training, ongoing supervision and support, and in some cases changes in policy and schemes of service. Some work has recently been carried out to establish candidate core competencies for different cadres, for example, by the IOM,10 and the West African Health Organization has recently finalized a process for harmonizing training for doctors, nurses, psychiatrists, and psychiatric nurses in the region. At present mental health/psychiatry training is not prioritized in medical and nursing schools, and many curricula are outdated.
The Kintampo College of Health, which specializes in training personnel for rural communities, has since 2011 been running a diploma program for community mental health officers, degrees for clinical psychiatric officers, and a diploma for medical assistants, specialized in psychiatry. This has started to fill an important gap in mid-level professionals at the community level. There is not a single psychiatric social worker active in the country.
Clinical psychologists number around 100, but fewer than 20 work in the public sector and are accessible mostly to people living in the two biggest cities. Several projects encourage development of self-help groups and peer support, an important source of care, not only in low-income contexts. The Mental Health Society of Ghana works to support these groups, not only for the potential therapeutic benefit, but for advocacy purposes.
Financing
At the individual and family levels, a chronic mental illness can have a catastrophic effect on financial security. The cyclical relationship between poverty and mental illness is well demonstrated, but there is increasing evidence to support intervention both in the “social drift” direction (mental ill health leads to poverty) and the “social causation” direction (social factors like poverty lead to mental ill health).11
Mental health services in the public sector of Ghana are, in principle at least, free as a matter of policy. This includes consultation, all medication, and admission, including food. Many people still spend large amounts on transportation and other opportunity costs to access services. The fact that services should be free can act as a barrier to internally generated revenue as an option for sustaining services.
NHIS is currently not designed for psychiatric services. Some psychotropic medications, however, are covered by NHIS when prescribed in general practice, and people with mental illness may access other NHIS services if they are registered.
In Ghana in the year 2012, total health expenditure as a percentage of gross domestic product was 5.2 percent—the agreed target is 15 percent.d In 2010, 1.3 percent of this figure was spent on mental health, very low when compared to the (global) estimate of 13 percent of total burden of disease attributable to mental, neurological, and substance use disorders (see Figure F-2).
With the recent increase in interest in mental health at the government level, and creation of the Mental Health Authority, it is hoped there will be a greater allocation of resources to mental health. Major donors such as the U.K. Department for International Development and the European Union have already invested in significant mental health program,
dAs defined by the Abuja Declaration of 2001.
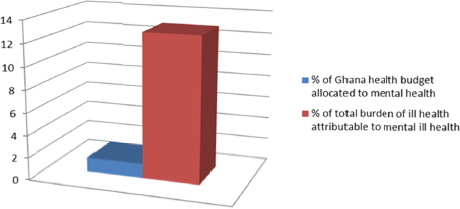
FIGURE F-2 Comparison between need (burden of disease, or disability-adjusted life years, for mental, neurological, and substance use disorders) and resource allocation (percentage of health budget for mental health) in Ghana.
in part because of the leadership shown by government and the positive framework for action that the Mental Health Act provides.
Lived Experience, Human Rights, and Social Inclusion
As well as the heavy cost to the individual and family from having a psychosocial disability, the stigma associated with these problems often leads to social exclusion, rejection from the community, and even to physical abuse. Holding people against their will is common when someone has destructive or aggressive behaviors, and traditional and religious treatments can involve beating, burning, and forced fasting, which can last for months at a time. Containment in a prison is common as a “solution” when families are unable to access the care they need for their relatives whose behavior they cannot manage, and women with severe mental illness are vulnerable to sexual abuse. Human Rights Watch published a comprehensive report on human rights in the formal and traditional sectors in 20124 that gained wide international attention. The new Mental Health Act provides some powers to the Mental Health Authority to enforce rights, and it will be interesting to see to what extent it will impact the experience of people being subject to human rights abuse in institutions and communities across the country.
Access to good health care is an important first step toward inclusion in community life, and acceptance into social structures. The human
rights messages in the awareness activities will reinforce this, with direct messages about social inclusion and reintegration after people have experienced discrimination while unwell.
Policy and Legislative Framework
The Mental Health Act 2012 (Act 846) is the current law that governs the practice of mental health in Ghana. It replaced the previous law, NRC Decree 30, of 1972, which focused largely on custodial care. It is the result of an 8-year collaboration among the WHO, civil society organizations including user groups, and Ghanaian mental health officials. Its eventual passage into law by the legislature was greatly facilitated by intense public advocacy and lobbying, which assumed an international dimension. The new law has been seen as a model for reform of mental health legislation in other parts of Africa. It is particularly strong in recognizing and upholding human rights of people with mental illness and emphasizes community care. Perhaps its greatest shortcoming is the absence of specific provisions recognizing suicide attempts as a sign of mental illness because Ghana still maintains suicide as an offense in its criminal code.
A novel feature of the Act is that it covers the operations of traditional and faith healers. The Mental Health Act also provides for setting up a mental health fund to provide a dedicated source of funds for mental health activities. This has yet to be made available for full roll-out of the provisions of the Act.
There are plans to build a forensic psychiatric facility, have a psychiatric hospital in each region, and have dedicated beds for psychiatric patients in every district and regional hospital. Day hospitals and rehabilitation centers in the community are all included in the vision of the new Mental Health Authority. None of these have actually taken off yet, however.
The latest mental health policy in Ghana dates from 1996 (revised in 2000), but was never implemented. In 2006 Ghana passed its Disability Rights Act (Act 715). Ghana is a signatory and has ratified the United Nations Convention on the Rights of People with Disabilities (in March 2007 and July 2012, respectively).12
Civil Society in Mental Health
Ghana can boast strong civil society organizations and established networks in mental health. This includes strong service user organizations, which is rare in Africa. It is generally recognized that they, alongside professionals, have played an important part in advocating for, drafting, and now implementing the new mental health legislation. International NGOs have played an important supportive role in this, with BasicNeeds standing out as having a particularly important long-term role in supporting civil society to promote change in Ghana. BasicNeeds mobilized the advocacy group that carried out a widespread and effective campaign that expedited the passing of a new mental health law in 2012. It has continued to support meetings to draft legislative instruments to actualize the law.
User associations of people with mental illness have been formed in many regions, which also helps with rehabilitation and even occasionally the supply of medications to affected individuals. Many have become economically independent through such activities. The Mental Health Society of Ghana has been formed, again through the support of BasicNeeds, to bring together various civil society organizations interested in mental health and thus bring sustainability to their activities. See Appendix 2 for a list of civil society organizations working in mental health. However, interest in mental health by general health and development organizations is less than ideal. For example, the Ghana Federation of the Disabled does not have strong mental health representation.
Research
Ghana has a strong history of research in mental health, going back many decades.13 Well-established local research institutions like the University of Ghana and the Kintampo Project have participated in important international collaborations such as the Mental Health and Poverty Project. International NGOs such as BasicNeeds and CBM International have a strong philosophy of evaluation and research within their projects, and have published examples of good practice.14,15 The WHO is collaborating on an important demonstration project related specifically to improving services in the field of epilepsy using the evidence base of mhGAP.
Summary
Quality community-based services improve access to care by the poorest, most rural populations, who are usually excluded from hospital services. Unfortunately, despite evidence of their efficacy, and government policy officially stating that they should be available, such services are rare beyond the existence of psychiatric nurses at decentralized locations. The development of accessible community-based services in Ghana will considerably increase the chances of people receiving the care they need. Experience shows that even if services are available, it is only with efforts to increase community awareness that the services are well used. Therefore it is important to deliver simple awareness messages, including basic human rights messages, positive messages about mental health issues (e.g., treatability), and advice on how to access care in the community.
SECTION 2: THE DEMONSTRATION PROJECT
Terms of Reference
This report is a concept for a demonstration project for improving access to mental health services in Ghana. It was commissioned to inform a workshop that will consider ways of taking forward mental health services in Ghana.
Overall Objective
“Persons with mental health needs and psychosocial disability are able to have access to good-quality mental health care through local mainstream health services, and to be included in community life.” A demonstration project will be carried out and evaluated to inform replication.
Principles Underlying Proposed Model
As a demonstration project, we have aimed to follow best practice principles, established evidence, and stakeholder consensus, to meet the specific needs using the available resources in Ghana.
The model is therefore designed to be:
- Comprehensive and holistic, addressing a wide range of issues that may be affected in the life of a person with a mental illness, and offering services encompassing biological (medical), psychological, and social interventions (often in combination)
- Accessible, made to be as easy to use as possible (taking into account proximity, cost, cultural acceptability)
- Integrated into the existing systems, mainstreaming mental health into general services, and reducing barriers across sectors
- Adapted for the local context and cultural norms of the people who would use the services
- Developed in a participatory way, from future users of the services to key decision makers whose buy-in at an early stage will facilitate future support
- Sustainable and economically viable in the economic context of Ghana, and able to show good value for investment by potential donors
- Replicable at scale; the project aims to inform possible scale up in Ghana and beyond
- Well evaluated; as a demonstration project, results that will be taken seriously by health leaders and planners need to be backed up by data collected in a methodologically sound way
Partnership
This technical proposal for a demonstration project in Ghana is an initiative of the IOM and developed with the collaboration of local partners. Subsequent refinement of the proposal will take place at a workshop in Accra, and implementation of the final proposal will depend on external funding. It is hoped that any such external funder will combine technical collaboration with funding of activities. Local implementation will depend on close collaboration with the MoH and GHS because the main thrust of the proposal is to integrate mental health into existing health structures, but the proposal is comprehensive and multisectoral. This means that other relevant government agencies (Ministry of Education, Ministry of Employment and Social Welfare) as well as Ghana’s strong civil society will also play an important role. Effective implementation of transformative initiatives usually relies on a strong
oversight committee and implementation team beyond the routine systems in place in the existing system.
Scope of the Project
This demonstration project is nested within the overall stated aim of the Government of Ghana to improve and scale up mental health services. It is therefore defined by the goals and priorities established in Ghana Law, Policy, and Strategy and will seek to support their implementation.
Timeframe
The project is ambitious in aiming to bring about change in established systems. While this has been shown to be feasible, particularly in defined structures, it takes time (see Appendix 4). We recommend a project should not be considered for less than 3 years (taking into account pre-project negotiations, contracts and legal authorization, inevitable bureaucratic delays, establishing a project team, and proper evaluation, etc.).
Catchment Area
The overall objective of the project is to inform a process of reform of mental health services in Ghana with the aim of increasing coverage of accessible mental health services in the country. This demonstration phase, then, will provide the information necessary to inform subsequent scale-up.
Districts have been chosen as the unit of implementation, as these are an important political entity, with responsibility for coordinating decentralized care under Ghanaian law and practice. The district contains management structures that can be used in this project, as well as general political forums to aid broader awareness about the work (District Assemblies). In general, integrated mental health services are not available in a typical district, so a successful implementation plan would have a huge impact by showing that it is possible to integrate into this level. We would aim to work in a comprehensive way in each district, such as within general hospitals and primary health care, depending on the resources a particular district has, and within the other sectors present in the district.
Two demonstration districts will be identified that represent a balance of urban and rural contexts. This is necessary due to the (increasing) disparity between urban and rural settings, requiring a different approach to making services accessible. Having sites that are specific to needs in this way allows not only generalizability to a greater number of districts for replication, but also the ability to analyze implementation outputs and processes to compare what works between two sites. Other factors that will be considered in choosing the two sites will be:
- Willingness of district authorities to support the project;
- Other local partners identified who can support the project;
- A track record of success in other projects;
- Adequate human resources (but not atypically well resourced); and
- Ease of access for monitoring and research.
The sites will be identified by the government and implementing partners based on transparent standard criteria, including these listed above.
Sustainability
This project aims to develop systems that are fully sustainable within the existing GHS structures. It has therefore been designed to be integrated, using an appropriate model that is in keeping with other components of the health service, and using existing resources without putting into place overly complex or resource-intensive interventions that cannot last beyond the timeframe of the project. This means that we would expect commitment from the health system to maintain any changes brought about: processes, staff deployment, good practice, supervision, etc. It will not be possible or appropriate to pay significant incentives for routine day-to-day work that we would expect to continue after the lifetime of the project. Some one-off or time-limited investment in activities is necessary to kick-start or develop an integration of mental health. This includes situation analysis, planning and model development, awareness raising, initial capacity building and training, and the necessary evaluation and dissemination, etc.
Assumptions and Risks
(see Appendix 3: Logical Framework Matrix)
The reasons mental health is not a priority and services are not widely available have been well documented.16 In addition to the risk analysis incorporated into the logical framework in relation to specific result areas (see Table F-4), we will briefly consider strategies to overcome these recognized barriers to change.
TABLE F-4 Barriers to Mental Health Care in Ghana
| Barrier15 | Situation in Ghana | Strategies to Address Barrier/Risk |
|---|---|---|
| 1. Insufficient funding for mental health services | Mental health is allocated 1.3% of health budget (which is 5% of GDP), which is very low, and mainly spent on specialist services. | Use temporary external funds to invest in a model of integrated mental health care that will show efficient and impactful outcomes with use of funds. Also acts as bridging funds for initial high investment. Advocate for increased resource allocation. |
| 2. Mental health resources centralized in and near big cities and in large institutions | Ghana has three large specialist hospitals, which are the main centers of care availability. Some examples of more accessible care exist, but are not fully integrated at a national level yet. | Use evaluation of demonstration project to show process and efficiency benefits of decentralization. |
| 3. Complexities of integrating mental health care effectively in primary-care services | The project is likely to encounter such challenges in creating change in established systems. | Specific focus on good consultation in project design (for buy-in), collaborative working, integrating into management structures, and using a deliberate systems approach. |
| Barrier15 | Situation in Ghana | Strategies to Address Barrier/Risk |
|---|---|---|
| 4. Low numbers and limited types of health workers trained and supervised in mental health care | Very low numbers of specialist personnel. Positive development of new mid-level professional grade in mental health. | Develop a task-sharing model using existing workers. Add training (in Mental Health Gap Action Program [mhGAP]) to capacitate to deliver tasks as defined. Advocate for appropriate posting to demonstration sites. Supervision. |
| 5. Mental health leaders often deficient in public health skills and experience | Relatively strong leadership in mental health compared to other countries in the region. | Use leaders with experience on Steering Committee, including those who have attended mhGAP. Clear policy briefs to update and inform health leaders in country on best practice for scale-up. |
NOTE: GDP = gross domestic product.
Project Activities
(see Appendix 3: Logical Framework Matrix)
Under the main result areas listed below, specific expected outcomes have been listed. As part of detailed project planning, the activities designed to achieve these outcomes will be established in detail. Similarly, the budget for the project will be detailed in line with these activities. In view of the desire to move toward implementation, a projected overall budget for each result area has been included in the logical framework.
1: Establish buy-in, management structure, and project oversight. Engage with relevant structures for integration of mental health.
Management Structure and Partnerships
(see organizational diagram in Appendix 5)
This project will integrate mental health services into state health infrastructure, using the resources within that system, but also key external expertise and support. It is therefore a public–private partnership, recognizing the different strengths of different actors, particularly in view of the need for rapid implementation of a novel service model and its comprehensive evaluation. Service delivery management will follow the lines of the GHS, but with a separate project management team to drive the implementation, administration, and evaluation of the project. As an externally funded project, there will be a need for high-quality financial and narrative reporting of activities by a dedicated team. It is hoped that an external funder will bring not only financial resources, but expertise. Similarly, project oversight will be provided by a Steering Committee under the Mental Health Authority, but this will be made up not only of health system leaders, but a variety of professionals, persons with project management experience, and service users.
Accountability will be ensured through inclusion of service users in the Steering Committee, with user satisfaction being a key indicator. Financial accountability to the donor and the government will be ensured by a finance/administration officer in the Project Management Team. To ensure independence and high standards in evaluation, the research component will be a collaboration of Ghanaian and international researchers. These partnerships would be laid out in a contract associated with a funded project.
2: Situation analysis and planning: Complete full situation analysis in identified demonstration sites, design implementation model, develop monitoring and evaluation (M&E) plan.
Project Development Process
Although the actions in this proposal are based on accepted best practice and the practical experience of the authors, it was not possible to follow an extensive participatory development process with all relevant stakeholders. Key leaders representing likely partners in any future implementation of the program were consulted, notably mental health leaders and members of the Ghana Mental Health Authority and the MoH, and asked to review the proposal outline. It will be essential, as first steps
in any implementation, to have a fuller engagement with stakeholders, particularly those who would be personally affected by the service. A structured process such as Theory of Change would enrich this proposed project outline with detail and provide a structured review of likely issues to manage any risks. Prior to implementation, there would also be need for a phase of more detailed situation analysis and baseline data collection.
3: Establish integrated Community Mental Health services in government health structures in two demonstration sites.
Evidence Base for Interventions
The project aims to be comprehensive and patient centered. This means health services are designed to be responsive to patient needs, with evidence-based interventions used to respond to those needs. This means biological, psychological, and social elements of care are available as near to the patient and as affordable as possible. Some elements will be delivered by the services, and some via referral to other services. Priority conditions will be determined based on identified needs, Ghana mental health policy, and canvassed opinion.
The evidence-based foundation for interventions will be provided by the WHO mhGAP program, particularly the Intervention Guide17 and other established sources, guidelines, and recommendations.18,19 Many of these have already been used in Ghana and other West African countries20,21 and an mhGAP adaptation has been carried out in Nigeria.22 Training would be based on the mhGAP materials for the identified priority conditions. There are Master Trainers available in the country. mhGAP also provides additional materials such as the M&E guide, Community Workers Training, that can be used as a resource. The evidence for implementation processes is also drawn from published sources,23,24 but significant efforts are made to ensure adaptation to local systems through significant input from local expertise, stakeholder validation of proposed activities, and regular review by experts and users throughout the processes. See notes above on the principles underlying the proposed model.
Task Sharing, Stepped Care, and Collaborative Care
These terms have come to be commonly used in service reform. They are defined in Box F-1.
These approaches will be used not only due to the limitation of available resources, but because much evidence supports their efficacy.25 The details of how this would be done in Ghana will depend on the situation analysis and planning process, but are likely to include tasks being done at certain levels, as summarized in Figure F-3. Among these different groups, there should be regular communication and supervision, and clear lines of referral.
4: Maintain a systemwide perspective to enable necessary resource availability and smooth running of the project. Ensure good intersectoral links to facilitate access to non-medical services.
BOX F-1
Definitions
Collaborative care: When mental health professionals and general practitioners work together to provide care for a patient, this is called collaborative care. For example, the psychiatric nurse might do initial assessments and an annual review, but general nurses in a primary health care (PHC) unit might carry out routine reviews. Collaborative care sometimes involves families collaborating as part of a care team as well.
Stepped care: While many cases can be managed at a decentralized location by staff trained to provide certain treatments, some people will require more complex care. Stepped care involves enabling community or PHC practitioners to provide first-line care, but then to have clear points at which referral is made to the next level of care.
Task sharing: Task sharing means distributing tasks to a wider range of people than in the traditional doctor-led approach. Usually staff with less training are assigned tasks that previously would have been done by someone with more professional training. For example, a nurse in a primary care unit would be allowed to treat a patient with medication or provide counseling. This is supported by good training and support to ensure that high standards are maintained.
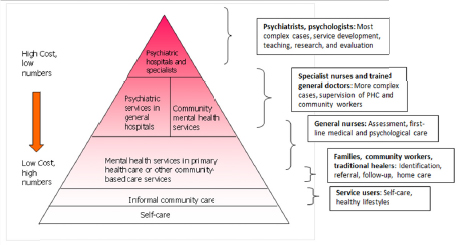
FIGURE F-3 The World Health Organization pyramid of mental health services. Self-care is pertinent at every level of the pyramid.
NOTE: PHC = primary health care.
Key Stakeholders
Although the main thrust of the service reform in this proposal occurs through integration into established (governmental) structures, there is an important role for others involved in mental health care in Ghana. They include service users and their families; NGOs providing health and social care services; advocacy and campaigning organizations and umbrella bodies; traditional and religious healers; international development organizations; and academic organizations interested in mental health. See stakeholder list in Appendix 2. A stakeholder analysis will be carried out as part of an activity in Result 2 to judge the best way for different actors to participate (Appendix 3).
Intersectoral Links
Mental health is uniquely crosscutting, with an impact on many related areas. By engaging with other sectors, it is possible not only to significantly impact the lives of persons with mental health problems encountering their services (in physical health, education, livelihoods, etc.), but also to improve the effectiveness of those other programs. A good example is how HIV/AIDS outcomes improve when mental health and medical issues are addressed together. Similar results have been
found with non-communicable diseases and maternal and child care services. In this project, we expect to include the Ministry of Education and the Ministry of Employment of Social Welfare because their work is central to an integrated approach that looks at patient needs as a focus for services.
In addition to intersectoral links, it will be necessary to engage with several discrete parts of the health system itself (MoH and GHS). For example, in advocacy efforts to improve access to medication and improve the health management information system, it will be necessary to engage with relevant departments to improve their focus on mental health. In each case, a thorough evaluation of the current system will be needed before a clear plan for addressing weaknesses and barriers to change can be implemented.
5: Increase community awareness of mental health issues, existence of new services. Challenge myths and stigma.
Changing Attitudes and Behavior
The negative experiences of discrimination and human rights abuse are frequently identified by service users and others as major priorities for action, given the detrimental impact on quality of life. In addition to the beneficial effect that a reduction in stigma and negative attitudes and behaviors would have, gaining awareness about services also increases use of those services.26 Unfortunately, the evidence for effective strategies for changing community attitudes and behavior is limited.27 One strategy that has been shown to be effective is direct exposure to people who have had mental health problems. This will be a central method used, harnessing Ghana’s strong service user community. Changing attitudes among young people is a key strategy not only to reducing population-level stigma and discrimination, but also to teaching mental health literacy and helping people to learn basic skills to maintain their own mental health. We propose to develop a basic module for inclusion in the school curriculum, which will be evaluated for a possible wider roll-out.
Engaging with Key Influencers of Opinion and Behavior
Key opinion influencers such as traditional leaders and healers will be engaged in forums that allow a frank exchange of ideas so as to gain a greater understanding of local explanatory models of disease. In this way
the demonstration model can more sensitively meet the needs of the population, and also allow a positive ongoing collaboration while addressing human rights concerns about conditions in traditional healer/prayer camps. Similarly, journalists will be made aware of more positive representations of people affected by mental illness, and the way that reporting can influence stigma and discrimination, as well as illness behavior, such as in the case of reporting on suicide. Addressing issues of human rights abuse and unhelpful negative myths will also be possible in the various multistakeholder forums that will be held to develop, oversee, and evaluate the program.
The Ministry of Education has a Schools Health Education Program division. We will engage them to include mental health in the curriculum. In each of these initiatives for specific target groups, expertise will be sought to carefully assess the evidence for “what works” to optimize impact at the design and implementation stages. This includes engaging experts in behavioral change.
6: Monitoring and evaluation, accountability, research, measuring impact.
Evaluation and Research
This project should be seen as an essential step toward providing evidence and guidance for supporting a long-term process of improving access to mental health services in Ghana and other sub-Saharan countries. As part of the project development, a monitoring and evaluation plan will be developed that will ensure that data are collected to answer key questions on how the project is running, what resources are being used, and what the impact is. This plan will include basic cost data in recognition of the fact that we aim to use this information for advocacy for scale-up. Research expertise for evaluation of the project and proper analysis to present evidence in an effective way will be provided by a collaborative group of experts from local and international institutions.
Maximizing Impact and Scaling Up
To ensure that any evidence generated and lessons learned are applied within the overall framework of scaling up services in Ghana:
- All stakeholders, including key decision makers, will be engaged from an early stage so that there is government ownership
- This will also ensure that the project is appropriately designed for the local context and is sustainable within existing health structures
- Attention will be paid to ensuring that proposed practical interventions are designed to be relevant to the local demonstration sites, but also with an eye to ensuring that national-level processes are influenced (e.g., medication supply chain or health information system reform)
- Results of the evaluation will be analyzed and presented in an accessible format for those involved in health service development in Ghana
- These results will include quantitative and qualitative evaluations, process indicators (how the processes for running the project worked), and data on cost-effectiveness
- As well as individual meetings, a workshop will be held to present the findings to local and national health authorities
- The findings will also be submitted for publication in peer-reviewed journals and presented at academic conferences
The evidence generated would be a great resource in a country that is recognized as having made great strides in development, and has proved to have a strong and effective advocacy movement.
Conclusion
As the evidence for individual interventions builds, this project offers a unique opportunity to combine many of the different components of an effective service, in a country that has made outstanding progress in the legal and policy environments. The results would not only be valuable in Ghana, but provide the guidance needed by many countries as they strive to meet the expectations to improve mental health services. There is growing international and local public pressure to bring mental health services into parity with physical health services, through local progressive legislation, and global agreements such as the Comprehensive Mental Health Action Plan. The results of this demonstration project would go a long way toward achieving these aspirations in Ghana.
Major Sources of Evidence for Demonstration Project
- Ghana Mental Health Act 2012
- Comprehensive Mental Health Action Plan 2013–2020, WHO 2013
- mhGAP Program suite of resources, WHO
- Lancet Global Mental Health Series (2007/2011)
- Reports and conclusions from previous IOM workshops on mental health in sub-Saharan Africa
Acknowledgment
This demonstration project proposal is an initiative of the IOM as part of a wider program supporting mental health in sub-Saharan Africa. It was prepared by Dr. Julian Eaton and Dr. Sammy Ohene, who gratefully acknowledge the support of many experts in Ghana, particularly the Mental Health Board members.
List of Acronyms
(NOTE: Acronyms used in the appendixes are listed here rather than at
the bottom of each appendix)
the bottom of each appendix)
| CBR | community-based rehabilitation | |
| CHAG | Christian Health Association of Ghana | |
| CHPS | Community-based Health Planning and Service Compounds | |
| CMD | common mental disorder (e.g., mild depression, anxiety) | |
| CMH | community mental health | |
| CPN | community psychiatric nurse | |
| DSM IV | Diagnostic and Statistical Manual, version 4 (of the American Psychiatric Association) | |
| GDP | gross domestic product | |
| GHS | Ghana Health Service | |
| (also the official acronym for Ghanaian New Cedi currency) | ||
| GNI | gross national income | |
| HDI | human development index | |
| HDI/R | human development index/rank | |
| HMIS | health management information system | |
| IOM | Institute of Medicine (U.S.) | |
| LMIC | low- and middle-income country (World Health Organization definition) | |
| LAMIC | low- and middle-income country (World Bank definition) | |
| MAKS | Mental heAlth Knowledge Scale | |
| M&E | monitoring and evaluation | |
| MGMH | Movement for Global Mental Health | |
| MH | mental health | |
| MH Authority | Mental Health Authority | |
| mhGAP | WHO Mental Health Gap Action Program | |
| MHIN | Mental Health Innovation Network |
| MICS | Multi-Indicator Cluster Survey (UNICEF) | |
| MoH | Ministry of Health (Ghana) | |
| NCD | noncommunicable disease | |
| NGO | nongovernmental organization | |
| NHIS | National Health Insurance Scheme | |
| PHC | primary health care | |
| PWPD | people with psychosocial disabilities | |
| SMD | severe mental disorder (e.g., schizophrenia, bipolar affective disorder, severe depression) | |
| ToT | Training of Trainers | |
| UNDP | United Nations Development Programme | |
| UNICEF | United Nations Children’s Fund | |
| USD | United States dollars | |
| WHO | World Health Organization |
Appendix 2
List of Civil Society Organizations Working in Mental Health
National Organizations
| Name | Field of Work | |
|---|---|---|
| National (multiple regions) | ||
| Mental Health Society of Ghana | User movement for persons with mental illness or epilepsy | |
| MindFreedom Ghana | Human rights–based organization involved in advocacy and public education | |
| Ghana Mental Health Association | Umbrella organization for all persons and organizations with interest in mental health | |
| Psycho-mental Health International | Public education | |
| Remar | Drug rehabilitation | |
| Chosen Rehab | Drug rehabilitation | |
| Presbyterian Church of Ghana | Community-based rehabilitation programs in Upper East Region | |
International Organizations
| Name | Field of Work | |
|---|---|---|
| BasicNeeds | Mental health and development | |
| CBM International | Disability and development | |
| Department for International Development | Bilateral donor | |
| European Union | Multilateral donor | |
| Name | Field of Work |
|---|---|
| Mental Health Educators in the Diaspora | Training local mental health personnel |
| World Health Organization | UN agency |
Research Groups Active in Mental Health Research
| Name | Area of Research | |
|---|---|---|
| National | ||
| Christian Health Association of Ghana-Project Fives Alive! | Maternal depression and epilepsy | |
| International collaborations | ||
| Kintampo Health Research Centre | Community mental health | |
| Fight Against Epilepsy Initiative | Epilepsy | |
Appendix 3: Logical Framework Matrix
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| Overall Objective | Persons with mental health needs and psychosocial disability in two demonstration sites are able to have access to quality mental health care through local mainstream health services, and to be included in community life. | Coverage: services established in two districts that will reach 20-40% of people with SMD and 5–10% of people with CMD regularly by 5 years. Quality of care provided by services. Service user satisfaction. | Project statistics on service activity. Patient outcome data collection and analysis. Additional qualitative work. | Assume government (national and local) cooperates and provides support. Assume other stakeholders will be motivated to form alliance. |
| Results 1: Establish buy-in, management structure, and project oversight. Engage with relevant structures for integration of mental health. | 1.1 Meet with, and gain approval from, figures of authority in health care in Ghana and identified districts. Identify focal person in established structures. 1.2 Build a Steering Committee within established health system structures: a diverse group of people with mental health and service development experience. Include representation of those providing the services and using services. 1.3 Build a strong project management team though transparent recruitment of qualified people, building their capacity to deliver the project and reporting requirements. | 1.1 Signed agreements for demonstration to go ahead, with commitments of support from MoH, GHS, and MH Authority. Support of other actors with a role in services for people with psychosocial disabilities. 1.2 Steering Committee meetings held quarterly, and project management team held to account through government structures and external donor system. 1.3 Full complement of appropriately qualified staff employed, in a suita- | Job descriptions for staff. Signed agreements to cooperate with work (Memorandum of Understanding) by government. Published document laying out plan for state MH development. | Government cooperation and support is needed. This is likely with good liaison. Also, there is little financial outlay on their part. Risk of change of government staff leading to need to repeat visits to engage new people. |
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| 1.4 Participate in forums relevant to mental health. Mainstream mental health into work of other sectors. | ble work environment within 4 months. Includes new project staff and 1.4 MH representation and engagement in other relevant forums. Evidence of MH inclusion in other sector plans (e.g., maternal/child health, NCDs, disability, livelihood, development). | |||
| Results 2: Situation analysis and planning: Complete full situation analysis in identified demonstration sites, design implementation model, and develop M&E plan. | 2.1 Carry out detailed situation analysis in identified demonstration sites to document needs and available resources. 2.2 Use detailed situation analyses to inform development of a project model. 2.3 Develop M&E plan in line with recognized indicators that will provide evidence and lessons for replicability (include costs and process indicators). Measure baseline for indicators. | 2.1.1 Situation analysis carried out and report written. Includes review of epidemiological data and policy framework. 2.1.2 Situation analysis reviewed and validated as part of a consultation to identify stakeholder priorities. 2.2.1 Detailed project model and implementation plan developed in participatory process. 2.2.2 Human resource availability mapped, and tasks defined at different levels of a stepped, collaborative care approach. Plan for training to meet task expectations and referral | Published reports on Ghana mental health situation (or extrapolation from other West African countries). Validation report. Baseline M&E report. | Assume information is available without need for major epidemiological work. Assume most major stakeholders will support plan for reform. Risk that even with task-sharing model, there are not enough personnel. |
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| system to support staff. 2.3.1 M&E plan developed and reviewed by experts and those who will use it. 2.3.2 M&E integrated into routine documentation and staff workplans. 2.3.3 Baseline indicators measured. | ||||
| Results 3: Establish integrated Community Mental Health services in government health structures in two demonstration sites. | 3.1 Proposal has support of authorities. 3.2 Build capacity of personnel at each level based on clearly defined tasks. 3.3 Ensure staff at each level are equipped with tools they need to work. 3.4 Provide ongoing training and clinical supervision. | 3.1 Relevant authorities at district level support implementation process. 3.2 Relevant personnel identified and trained according to required competencies (documented for each level of staff in Results 2 above). 3.3 Trained staff have requirements to fulfil tasks (leadership support, time, clinic space, furniture, stationery, medical equipment, medication). 3.4 Staff running services at district and PHC level receive quarterly training and supervisory visits. | Signed Memorandums of Understanding with districts. Documentation of personnel posted appropriately. Routine integrated MH statistics in health system. Quality of care provided by staff monitored in supervision process. Vehicle logs for supervision visits. | Assume resources will be available to implement. Risk that staff will not want to work in rural areas (reduced by recruiting from these areas for training). Assume that district authorities are willing to support reform, and that staff will be made available for program. Assume that access is possible throughout year. |
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| Results 4: Maintain a system-wide perspective to enable necessary resource availability and smooth running of the project. Ensure good intersectoral links to facilitate access to non-medical services. | 4.1 Systematically consider historical barriers to successful access of quality mental health care. Address: 4.2 Low availability of medication through detailed analysis of supply chain, and plan for finding solutions to barriers identified. 4.3 Lack of psychological care by ensuring best evidence-based, low-intensity approaches are incorporated. 4.4 Health management information system weaknesses, by engaging with relevant departments and proposing core set of indicators to be integrated into general system. 4.5 Ineffective referral and counter-referral/senior support. 4.6 Lack of intersectoral collaboration, including physical health education, social services, and traditional and religious healers. | 4.1 Review of possible barriers to success (part of situation analysis) used to plan proactive interventions. 4.2 Uninterrupted supply of essential psychotropic medication available at point of need through advocacy and necessary action taken. 4.3 Explore most appropriate model for making psychological support (mhGAP recommendations) for key disorders available in Ghana. 4.4 Health management information system integrated in the mainstream system, easy to use, and providing information that informs improved care. 4.5 Referral mechanisms in place that ensure appropriate pathways in stepped collaborative care model. 4.6 Local social services mapped, and pathways for accessing services for clients developed and used. | Systems indicators related to medication, psychological care availability. Pharmacy records. Client records. Health information system reports. Referral records. | Risk that long-standing barriers to reform will not be amenable to change. Risk of factors outside our control being a block to progress (importation of drugs, prescription laws, etc.). Risk that few social services in existence. Other sectors may not be willing to integrate MH into their work. |
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| Results 5: Increase community awareness of mental health issues, existence of new services. Challenge myths and stigma. | 5.1 Hold forums to engage with traditional custodians of care to understand explanatory models and better engage collaboratively. 5.2 Develop advocates and equip them to promote messages to communities. 5.3 Develop messages for target groups that might include: - Mental health promotion and illness prevention. - The treatability of mental disorders. - The existence of (new) services for people in communities who need them. - The right of PWPDs to be included in community life and not face discrimination. 5.4 Engage in local- and national-level campaigns to change attitudes. | 5.1 Key traditional leaders and healers in each district attend the forums. Report of findings and collaboration plan produced. 5.2 Advocates (including service users) who will engage in awareness-raising activities identified and trained. 5.3 Print materials for advocates to use in awareness-raising activities. 5.4.1 Expose target groups (schools, professionals, etc.) to people who can describe their experiences of living with mental health issues. 5.4.2 Brief module for school curriculum developed, used, and evaluated in demonstration districts. 5.4.3 Carry out event on World Mental Health Day. 5.4.4 Journalist training to reduce stigmatizing messages. | Pre- and post-knowledge and attitudes questionnaires (e.g., Mental heAlth Knowledge Scale, or MAKS). Copies of leaflets, posters, radio/TV programs. Awareness-raising plans. Qualitative research on stigma. | Assume advocates once trained will retain enthusiasm to do awareness-raising work. Should be the case as is funded, and those trained are stakeholders with a personal interest. Risk of attitude, behavior change, and experience of people with psychosocial disabilities not changing despite efforts (evidence is relatively weak). |
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| Results 6: Monitoring and evaluation, accountability, research, measuring impact. | 6.1 Internal recordkeeping, accounting, monitoring, and evaluation, so that reporting is of a high standard and audit occurs to maintain high standards. 6.2 Gather reliable data and analyze to have strong evaluation of model. Share evidence generated by research related to the program. 6.3 Document roll-out and make resources developed available. 6.4 Engagement with stakeholders in mental health (including government structures) so that findings can be disseminated and lessons learned to benefit Ghana and other LAMICs. | 6.1 Maintain records (evidence of activities completed and accounts) and produce timely reports. 6.2 Write a report for publication in a peer-reviewed scientific journal; present in conferences. Develop user-friendly versions of findings (policy briefs). 6.3 Develop program, materials (training, recordkeeping, HMIS, referral, etc.) in line with international and local standards that can be used as a resource in replication. Post online (e.g., MHIN, MGMH). 6.4 Dissemination meetings held for local community and health leadership in Ghana. | Quarterly and 6-monthly reports and audits. Program Annual Report. Published materials in journals. Presentations in conferences recorded in conference programs, minutes of management committee meetings. | Risk of personnel not completing reporting schedule (mitigated by intense training program and ongoing support). Risk of not being able to secure external funding for major research. |
ACTIVITIES TO ACHIEVE THE OBJECTIVE AND EXPECTED RESULTS
| Suggested Activities (to Be Planned in Detail) | Activity Means/Input | Projected Costs | Possible Barriers to Success and Means of Overcoming Barriers | |
|---|---|---|---|---|
| Results 1: Establish management structure and project oversight. Engage with relevant structures for integration of mental health. | Call meetings with MH leadership in Ghana. Clarify role of project in taking forward national MH strategy. Gain written commitment to support project (if possible financial commitment as matching funds). Transparent recruitment of team, and allocation of government staff. | |||
| Results 2: Situation analysis and planning: Complete full situation analysis in identified demonstration sites, design implementation model, develop M&E plan. | Allocate demonstration sites. Meet with local leadership to gain support. Hold mapping exercise for needs and resources (national and in detail in demonstration sites). Hold stakeholder meeting to identify priorities. Theory of Change workshop to pin down detailed plan. M&E workshop (include government HMIS department). | |||
| Suggested Activities (to Be Planned in Detail) | Activity Means/Input | Projected Costs | Possible Barriers to Success and Means of Overcoming Barriers | |
|---|---|---|---|---|
| Results 3: Establish integrated CMH services in government health structures in two demonstration sites. | Commission report on task-sharing options for Ghana. Validate with wide stakeholder group. Develop training for acquisition of defined tasks. Carry out TOT and trainings at each level. Ensure motivation of trained personnel to work in long term (remuneration). | |||
| Results 4: Maintain a systemwide perspective to enable necessary resource availability and smooth running of the project. Ensure good intersectoral links to facilitate access to non-medical services. | Establish small working groups of experts in barrier subject areas. Workshops to agree on action plans. Dedicate Steering Committee time and staff resources to advocating on these issues. If necessary implement parallel/support structures, e.g., drug revolving fund or HMIS, until integration is possible. Invite other sectors to MH meetings and awareness. Provide materials for others to understand how to incorporate MH, e.g., evidence on MH/NCDs, livelihoods disability. Hold forums to engage informal care sector in districts, and provide a space to share understandings of mental health and illness. | |||
| Project Description/Narrative | Indicators of Success | Source of Verification | Assumptions and Risks | |
|---|---|---|---|---|
| Results 5: Increase community awareness of mental health issues, existence of new services. Challenge myths and stigma. | Forums for engagement with traditional leaders and healers. Stakeholder workshop to understand main issues and desired messages. Planning group to design campaign based on these messages for specific identified target groups (e.g., police, prisons, teachers, Pastors/Imams, etc.), ideally using service users and family members as advocates. Design of curriculum module for schools, testing, and evaluation. Brief training for advocates. Campaign of visiting and delivering messages to groups. | |||
| Results 6: Monitoring and evaluation, accountability, research, measuring impact. | Regular (monthly) M&E meetings. Regular reports to director, Steering Committee, and international donors. Identify collaboration with Ghana and international research groups. Local dissemination meetings. Production of policy briefs. User-friendly report for government. Publication of papers in peer-reviewed journals. Sharing findings at conferences. | |||
Appendix 4: Timeframe
| Year 1 | Year 2 | Year 3 | Year 4 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Results 1: Establish buy-in, management structure, and project oversight. Engage with relevant structures for integration of mental health. | 1.1 Meet with figures of authority in health care in Ghana and districts. | ||||||||||||||||
| 1.2 Build a Steering Committee within established health system structures. | |||||||||||||||||
| 1.3 Build a strong project management team. | |||||||||||||||||
| 1.4 Participate in forums relevant to mental health; mainstreaming. | |||||||||||||||||
| Results 2: Situation analysis and planning: Complete full situation analysis in identified demonstration sites, design implementation model, develop M&E plan. | 2.1 Carry out detailed situation analysis in identified demonstration sites. | ||||||||||||||||
| 2.2 Use detailed situation analyses to inform development of a project model. | |||||||||||||||||
| 2.3 Develop M&E plan in line with recognized indicators. | |||||||||||||||||
| Year 1 | Year 2 | Year 3 | Year 4 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Results 3: Establish integrated CMH services in government health structures in two demonstration sites. | 3.1 Proposal has support of authorities. | ||||||||||||||||
| 3.2 Build capacity of personnel at each level based on clearly defined tasks. | |||||||||||||||||
| 3.3 Ensure staff at each level are equipped with tools they need to work. | |||||||||||||||||
| 3.4 Provide ongoing training and clinical supervision. | |||||||||||||||||
| Results 4: Maintain a systemwide perspective to facilitate necessary resource availability and smooth running of the project. Ensure good intersectoral links to facilitate access to non-medical services. | 4.1 Systematically consider historical barriers to success. | ||||||||||||||||
| 4.2 Address low availability of medication. | |||||||||||||||||
| 4.3 Lack of psychological care. | |||||||||||||||||
| 4.4 Health management information system weaknesses. | |||||||||||||||||
| 4.5 Ineffective referral and counter-referral/senior support. | |||||||||||||||||
| 4.6 Lack of intersectoral collaboration. | |||||||||||||||||
| Year 1 | Year 2 | Year 3 | Year 4 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Results 5: Increase community awareness of mental health issues. Challenge myths and stigma. | 5.1 Hold forums of traditional leaders and healers. | ||||||||||||||||
| 5.2 Develop advocates and equip them to promote messages to communities. | |||||||||||||||||
| 5.3 Develop messages for target groups. | |||||||||||||||||
| 5.4 Engage in local- and national-level campaigns to change attitudes. | |||||||||||||||||
| Results 6: Monitoring and evaluation, accountability, research, measuring impact. | 6.1 Internal recordkeeping, M&E, research, and dissemination. | ||||||||||||||||
| 6.2 Gather reliable data and analyze to have strong evaluation of model. | |||||||||||||||||
| 6.3 Document roll-out and make resources developed available. | |||||||||||||||||
| 6.4 Engagement so that findings can be disseminated and lessons learned. | |||||||||||||||||
REFERENCES
_______________________
1IOM (Institute of Medicine). 2001. Neurological, psychiatric, and developmental disorders: Meeting the challenge in the developing world. Washington, DC: National Academy Press.
2UNICEF (United Nations Children’s Fund). 2015. Ghana. UNICEF. http://www.unicef.org/ghana (accessed August 18, 2015).
3Gureje, O. 2002. Psychological disorders and symptoms in primary care. Association with disability and service use after 12 months. Social Psychiatry and Psychiatric Epidemiology 37(5):220-224.
4Ssengooba, M., S. Rau Barriga, C. Dufka, and R. Peligal. 2012. “Like a death sentence”: Abuses against persons with mental disabilities in Ghana. New York: Human Rights Watch.
5Ae-Ngibise, K., S. Cooper, E. Adiibokah, B. Akpalu, C. Lund, V. Doku, Mental Health and Poverty Project Research Programme Consortium. 2010. “Whether you like it or not people with mental problems are going to go to them”: A qualitative exploration into the widespread use of traditional and faith healers in the provision of mental health care in Ghana. International Review of Psychiatry 22(6):558-567.
6WHO. 2013. Mental health action plan 2013-2020. Geneva, Switzerland: World Health Organization.
7WHO. 2011. Mental Health Atlas 2011—Ghana. Department of Mental Health and Substance Abuse, World Health Organization. Geneva, Switzerland: WHO. http://www.who.int/mental_health/evidence/atlas/profiles/gha_mh_profile.pdf?ua=1 (accessed August 18, 2015).
8Mental Health Educators in the Diaspora (MHED). MHED. http://www.mentalhealtheducators.org (accessed August 18, 2015).
9Department of Psychiatry, University of Ibadan and CBM International. 2012. Mental health leadership and advocacy programme (mhLAP) Ghana. http://www.mhlap.org/country-of-activities/ghana (accessed August 18, 2015).
10IOM. 2013. Strengthening human resources through development of candidate core competencies for mental, neurological and substance use disorders in sub-Saharan Africa: Workshop summary. Washington, DC: The National Academies Press.
11Lund, C., M. De Silva, S. Plagerson, S. Cooper, D. Chisholm, J. Das, M. Knapp, and V. Patel. 2011. Poverty and mental disorders: Breaking the cycle in low-income and middle-income countries. Lancet 378(9801):1502-1514.
12WHO (World Health Organization). 2015. WHO MiNDbank: More inclusiveness needed in disability and development. http://www.mindbank.info (accessed August 18, 2015).
13Read, U. M., and V. Doku. 2012. Mental health research in Ghana: A literature review. Ghana Medical Journal 46(2 Suppl):29-38.
14Crabb, J., and E. Razi. 2007. Essential skills for mental health care. Accra, Ghana: BasicNeeds.
15Yaro, P., and V. de Menil. 2010. Lessons from the African user movement: The case of Ghana, edited by A. Barbato and M. Vallarino. Press Milan.
16Saraceno, B., M. van Ommeren, R. Batniji, A. Cohen, O. Gureje, J. Ma-honey, D. Sridhar, and C. Underhill. 2007. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet 370(9593):1164-1174.
17WHO. 2010. mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Mental Health Gap Action Programme. Geneva, Switzerland: WHO.
18Patel, V., and G. Thornicroft. 2009. Packages of care for mental, neurological, and substance use disorders in low- and middle-income countries: PLoS medicine series. PLoS Medicine 6(10):e1000160.
19WHO and World Organization of Family Doctors (Wonca). 2008. Integrating mental health into primary care: A global perspective. Geneva, Switzerland: WHO.
20Esan, O., J. Abdulmalik, J. Eaton, L. Kola, W. Fadahunsi, and O. Gureje. 2014. Mental health care in Anglophone west Africa. Psychiatric Services 65(9):1084-1087.
21Douma Maiga, D., and J. Eaton. 2014. A survey of the mental healthcare systems in five francophone countries in west Africa: Bénin, Burkina Faso, Côte d’Ivoire, Niger and Togo. International Psychiatry 11(3):69-72.
22Abdulmalik, J., L. Kola, W. Fadahunsi, K. Adebayo, M. T. Yasamy, E. Musa, and O. Gureje. 2013. Country contextualization of the mental health gap action programme intervention guide: A case study from Nigeria. PLoS Medicine 10(8):e1001501.
23Eaton, J., L. McCay, M. Semrau, S. Chatterjee, F. Baingana, R. Araya, C. Ntulo, G. Thornicroft, and S. Saxena. 2011. Scale up services for mental health in low-income and middle-income countries. Lancet 378(9802):1592-1603.
24WHO. 2007. Scaling up health service delivery: From pilot innovations to policies and programs, Edited by R. Simmons, P. Fajans, and L. Ghiron. Geneva, Switzerland: WHO.
25Thornicroft, G., and M. Tansella. 2002. Balancing community-based and hospital-based mental health care. World Psychiatry 1(2):84-90.
26Eaton, J., and A. O. Agomoh. 2008. Developing mental health services in Nigera: The impact of a community-based mental health awareness programme. Social Psychiatry & Psychiatric Epidemiology 43(7):552-558.
27Thornicroft, G. 2006. Shunned: Discrimination against people with mental illness. Oxford: Oxford University Press.
28The World Bank Group. 2015. Ghana. The World Bank Group. http://www.worldbank.org/en/country/ghana (accessed August 18, 2015).
29Ghana Statistical Service. 2015. Population Statistics. Accra, Ghana: Ghana Statistical Service. http://www.statsghana.gov.gh/pop_stats.html (accessed August 18, 2015).
30UNDP (United Nations Development Programme). 2014. Human development report 2014 sustaining human progress: Reducing vulnerabilities and building resilience. New York, NY: UNDP. http://hdr.undp.org/sites/default/files/hdr14-report-en-1.pdf (accessed August 18, 2015).