On April 14-15, 2015, the Institute of Medicine’s (IOM’s) Roundtable on Obesity Solutions held a 2-day workshop1 titled “Physical Activity: Moving Toward Obesity Solutions.” While the idea that physical activity impacts health can be traced as far back as Hippocrates, Russell Pate stated in his opening remarks that the scientific study of physical activity did not begin until the 20th century. By the 1990s, he said, researchers had collected enough evidence on the health implications of physical activity that the Centers for Disease Control and Prevention (CDC) and the American College of Sports Medicine were able to collaborate on the first of what would become many public health statements on the importance of exercise (Pate et al., 1995). In 2008, the U.S. federal government for the first time issued fully approved physical activity guidelines.
The science around the linkages between physical activity and health has continued to accumulate, Pate said. The April 14-15 workshop was held to provide an expert summary of the state of the science regarding the impact of physical activity in the prevention and treatment of overweight and obesity and to highlight innovative strategies for promoting physical activity across different segments of the population (Box 1-1 summarizes the workshop goals).
_______________
1 The planning committee’s role was limited to planning the workshop. This workshop summary was prepared by the rapporteur as a factual account of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants and are not necessarily endorsed or verified by the IOM. They should not be construed as reflecting any group consensus.
BOX 1-1
Workshop Goals
The workshop will explore the role of physical activity in the prevention and treatment of obesity and will feature expert speakers and discussion on the scientific basis for a focus on physical activity in obesity prevention and treatment. The workshop will include presenters and discussants on the subject of primary prevention of overweight and obesity in adults and children, as well as physical activity in overweight and obese populations. The workshop will also provide a space for speakers and attendees to share innovative strategies for promoting physical activity and preventing obesity in diverse settings and through various channels.
ORGANIZATION OF THE WORKSHOP AND THIS SUMMARY
The organization of this summary parallels that of the workshop itself (see Appendix A for the workshop agenda). This first chapter summarizes the welcoming remarks of Victor Dzau, president of the IOM at the time of the workshop and currently president of the newly formed National Academy of Medicine; Russell Pate’s introductory presentation, which provided historical context for understanding the current state of the science regarding the impact of physical activity on the prevention and treatment of obesity; keynote speaker James Hill’s presentation on the clarity of the evidence indicating that physical activity plays a significant role in reducing obesity; and Aviva Must’s overview of sociodemographic disparities in obesity and physical activity as one of its determinants.
Following these introductory overviews, the remainder of the first day of the workshop was dedicated to exploring in more detail what scientists have learned about the role of physical activity in preventing obesity in youth (summarized in Chapter 2); what is known about the role of physical activity in preventing obesity in adults (Chapter 3); and the health effects of physical activity in youth and adults who are overweight or obese (Chapter 4).
The second day of the workshop focused on ways to promote physical activity across different segments of the population. Speakers and participants considered policy strategies (summarized in Chapter 5), community strategies (Chapter 6), and institutional strategies (Chapter 7).
In the final session of the workshop, representatives from three community programs in different parts of the country, working with varying age,
socioeconomic, and racial/ethnic segments of the U.S. population, discussed how their programs promote physical activity (summarized in Chapter 8).
Each session ended with a panel discussion with the speakers. Summaries of those discussions are provided at the end of the respective chapters, organized by topic.
The Roundtable on Obesity Solutions was established in 2004 to engage leaders from multiple sectors and, through workshops such as this, to provide a venue for collaborations and policy initiatives designed to prevent and treat obesity and eliminate obesity-related disparities. In his welcoming remarks, Victor Dzau elaborated on the origins and goals of the roundtable and on the purpose of the workshop. While the roundtable began, he said, as a way to bring together thought leaders from multiple sectors, he expressed excitement that this workshop was engaging “people on the ground,” or, as he said, “people who actually do the work to make a difference.”3
At the time of this workshop, the IOM had produced more than a dozen consensus reports4 on different aspects of obesity, such as ways in which community resources can be used to reduce both child and adult obesity, ways in which government can make a difference, and evidence relating to prevention of obesity. With respect to the role of physical activity in preventing and treating obesity, Dzau highlighted two of the more recent consensus reports. The first, Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation (IOM, 2012), calls for physical activity to be an integral and routine part of life and for community planners, government officials, and others to work together to increase opportunities for and access to physical activities. The second, Educating the Student Body: Taking Physical Activity and Physical Education to School (IOM, 2013), emphasizes the need for a whole-school approach to foster and provide access to 60 minutes of physical activity per day in the school environment. Additionally, in 2015, just prior to this workshop, the roundtable issued a series of prospective papers on disparities in physical activity (Adeigbe and
_______________
2 This section summarizes information and opinions presented by Victor Dzau, M.D., president of the National Academy of Medicine.
3 In addition to the final session’s being dedicated to a discussion of three “on the ground” strategies currently being implemented, three active breaks were built into the workshop schedule—the first led by Shape Up Sisters of Vicksburg, Mississippi; the second by DC SCORES of Washington, DC; and the third by BOKS in Canton, Massachusetts.
4 In addition to these consensus reports, the IOM had produced a comparable number of workshop summaries on various aspects of obesity.
Ramirez, 2015; DiPietro, 2015; Rimmer, 2015; Taylor, 2015; Warne and Roanhorse, 2015; Whitaker and Gehris, 2015; see Appendix B).
In addition to its many publications on obesity, the IOM partnered with HBO to develop a series called The Weight of the Nation. Out of that partnership, Dzau said, came The Public Good Projects, which, together with the IOM, has been working on a campaign titled “A Healthy America” and addressing many of the same issues on which the roundtable focuses.
Dzau said he views the obesity challenge in the United States, as well as in other Western nations, as a problem of affluence and technology—with technologies today being less conducive to physical activity than in the past—but also as a problem of a lack of opportunities. For example, career circumstances and money challenges are reducing free time, and dangerous neighborhoods deter walking. From community planners to transportation and other government officials, Dzau said, “Everybody is thinking about how to create the right environment for physical activity.” He observed that the issue is a timely one, as reflected, among other efforts, in First Lady Michelle Obama’s Let’s Move! Campaign; the Partnership for a Healthier America; the National Physical Activity Plan; and work by the President’s Council on Fitness, Sports, and Nutrition.
AN INTRODUCTION TO PHYSICAL ACTIVITY AND ITS IMPACT ON HEALTH AND WELL-BEING5
Walking is man’s best medicine. —Hippocrates
A Brief History of Physical Activity and Health
The idea that physical activity is important to health is not new. Ancient scholars and physicians believed it, and Hippocrates wrote about it (460-357 B.C.). Probably intuitively, Russell Pate said, great leaders throughout history have understood the link between physical activity and health, but as noted earlier, it was not until the 20th century that what is known as science was applied to physical activity and exercise. European exercise physiologists—notably 1920 Nobel Prize winner August Krogh (1874-1949) and 1922 Nobel Prize winner A. V. Hill (1866-1977)—were among the first to work in the field. Pate noted that the field has not produced a Nobel Prize winner since then, and, he said, “We are overdue.” In the United States, the Harvard Fatigue Lab was active at around the same time, up until the end of World War II (1927-1947). It trained many of the scientists who
_______________
5 This section summarizes the information and opinions presented by Russell R. Pate, Ph.D., Arnold School of Public Health, University of South Carolina, Columbia.
populated the academic programs in exercise science across the country that continue to exist today, according to Pate.
In the first half of the 20th century, most of the science on physical activity and exercise was focused on understanding the basic physiological responses to exercise. By mid-century, some highly prestigious epidemiologists, including Jeremy Morris (1910-2009) and Ralph Paffenbarger (1922-2007), had become interested in the health implications of physical activity. Pate said, “I think you could probably argue that we are here this morning in no small way because of the work of Jeremy Morris in the U.K. and Ralph Paffenbarger in the U.S.” The field has benefited tremendously, in his opinion, from the credibility those early epidemiologists brought to their work. Morris is well known for his work in the early 1950s comparing health outcomes in active double-decker bus conductors versus sedentary drivers. Paffenbarger continued that work across a range of occupational groups, such as active longshoremen (i.e., cargo handlers) versus sedentary longshoremen, and conducted a well-known study of Harvard alumni with different physical activity levels (Paffenbarger et al., 1978). He also created what is known by many as the Paffenbarger curve, illustrating the relationship between physical activity and heart disease outcomes, with the low end of the activity continuum being associated with substantially elevated risks of fatal and nonfatal heart attacks (Paffenbarger et al., 1978) (see Figure 1-1). The Paffenbarger curve has been used to describe the relationship between physical activity and a wide range of other chronic disease outcomes as well, with fitness sometimes being used as a surrogate marker for physical activity (Blair et al., 1989) (see Figure 1-1). The basic message of the curve, said Pate, is that “you don’t want to be sedentary.”
By the early 1990s, evidence supporting the important health implications of physical activity had reached a critical point. In 1992, the American Heart Association issued what Pate believes, in retrospect, was a seminal statement on exercise, acknowledging that inactivity or low physical activity should be recognized as a risk factor for coronary heart disease (Fletcher et al., 1992). That statement, Pate said, “opened the floodgate.” Just a few years later, CDC and the American College of Sports Medicine collaborated to issue the first public health statement on physical activity, recommending that all adults accumulate 30 minutes or more of at least moderate-intensity physical activity on most, preferably all, days of the week (Pate et al., 1995). The 1995 statement was followed quickly by production of the first and still only surgeon general’s report on physical activity and health, which, according to Pate, essentially endorsed the same recommendations (HHS, 1999).
Concurrently with the release of some of these authoritative documents, “the science continued to accumulate,” Pate remarked, with publications on physical activity or exercise and health increasing curvilinearly.
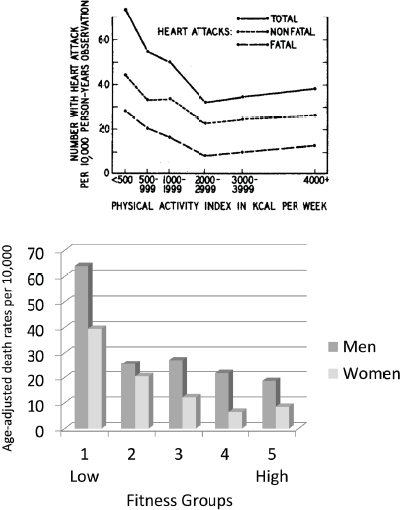
FIGURE 1-1 The so-called Paffenbarger curve, showing the relationship among physical activity or fitness, heart disease outcomes, and all-cause mortality.
NOTE: kcal = kilocalorie.
SOURCES: Presented by Russell Pate on April 14, 2015 (Blair et al., 1989; Paffenbarger, R. S., Jr., A. L. Wing, and R. T. Hyde. 1978. Physical activity as an index of heart attack risk in college alumni. American Journal of Epidemiology 108(3):161-175 by permission of Oxford University Press).
In the early 1990s, there were fewer than 5,000 publications on physical activity and health and fewer than 5,000 on exercise and health. Between 2011 and 2015, there were nearly 35,000 publications on physical activity and health and more than 30,000 on exercise and health.
As noted earlier, in 2008, the U.S. federal government for the first time issued fully approved physical activity guidelines (HHS, 2008). The advisory committee that informed the production of that report conducted an extensive review of the literature, according to Pate. That review revealed strong evidence for a broad constellation of important chronic disease and health benefits associated with higher levels of physical activity in both adults and older adults, including the prevention of weight gain. Additionally, there was moderate to strong evidence for reduced abdominal obesity, again in both adults and older adults. In children and adolescents, strong evidence supported an association between physical activity and favorable body composition. In sum, Pate said, the advisory committee concluded that physical activity was associated with important benefits with respect to the avoidance of overweight and obesity across the age range considered. The committee recommended 2.5 hours per week of moderate-intensity activity, which Pate noted was not really very different from the previously recommended 30 minutes most days of the week (i.e., Pate et al., 1995). For children and adolescents (6-17 years of age), the advisory committee recommended 1 hour per day.
Because most Americans are not meeting those guidelines, Pate said, the risk attributable to failure is tremendous. A number of published analyses have examined that risk, producing estimates ranging from 191,000 to 300,000 premature deaths per year in the United States attributable to physical inactivity (e.g., Danaei et al., 2009). Worldwide, Lee and colleagues (2012) estimate that 7-10 percent of several important chronic disease outcomes (e.g., coronary heart disease, colon cancer) can be explained on the basis of physical inactivity. “It is a remarkable conclusion,” Pate said. “Clearly the impact of physical inactivity constitutes a very substantial public health problem.”
Studying the Health Impact of Physical Activity
Pate provided an overview of the principles and premises applied by scientists in their study of physical activity. First, to study a construct, Pate said, scientists need to define it. Physical activity has been defined as “any bodily movement produced by skeletal muscles that results in energy expenditure.” Pate underscored the importance of the “energy expenditure” component of that definition and remarked that the energy throughput impact of physical activity is a fundamental component of physical activity research.
Pate emphasized the complex nature of physical activity. It is a behavior with many attributes, he explained, all of which are relevant to studying its health impact. They include the type of activity (e.g., aerobic, resistance), specific form (e.g., walking, swimming), frequency (e.g., bouts/day,
days/week), intensity, duration, and context (e.g., physical location, social setting).
To study a construct, Pate continued, scientists also need to be able to measure it. Physical activity has been measured in many different ways, including self-report; surrogate report (e.g., by parents or others around the target individual); direct observation; and, over the past 15 years or so, objective assessment (e.g., accelerometry, pedometry). In Pate’s opinion, the development of methods for objective assessment of physical activity represents an enormous advance in scientists’ ability to study physical activity and to produce findings well regarded by the scientific community.
Pate noted that physical activity is communicated in the literature in various ways. Sometimes it is expressed as a selected intensity of activity per unit time, such as moderate- to vigorous-intensity physical activity (MVPA) minutes per day. Sometimes it is expressed in terms of overall dose—for example, metabolic equivalent of task (MET)-minutes, a metric based on resting energy expenditure multiplied by the intensity and duration of an activity.6 Finally, physical activity sometimes is expressed in terms of compliance with a guideline (e.g., days/week).
Researchers have studied many different health outcomes associated with physical activity, including biomarkers (e.g., lipids, blood pressure, insulin, adiposity, fitness), disease morbidities and mortalities (e.g., cardiovascular disease, type 2 diabetes, obesity), and all-cause mortality. In Pate’s opinion, the field achieved a new status when the large epidemiologic databases matured such that it became feasible to examine all-cause mortality as an outcome.
As to why physical activity exerts its influence on health, Pate remarked that while scientists certainly have much to learn about underlying mechanisms, they know that acute exercise produces a profound physiologic response. The energy expended by skeletal muscle tissue during acute exercise requires such a response, and support for that response engages essentially all bodily systems, particularly the neuroendocrine control and cardiorespiratory function systems. The average person can increase his or her metabolic rate during physical activity by 5 to 10 times his or her resting level, and athletes can increase their rates by 15 to 20 times their resting levels. Regular participation in physical activity (i.e., chronic exercise) produces a broad range of adaptations, including multiple effects on the muscle metabolic apparatus (e.g., the muscles get better at performing the activity), changes in cardiorespiratory function, changes in neuroendocrine control mechanisms, tissue adaptations to the increased activity (e.g., in connective tissue, bone, adipose tissue), and improved fitness.
_______________
6 For example, a physical activity with a MET value of 5 is one that involves expending 5 times the energy expended at rest.
With respect to the mechanisms underlying the health effects of physical activity, insulin sensitivity is recognized as one such mechanism, especially with regular exercise, but also with acute bouts of exercise. Other known underlying mechanisms include lower visceral adiposity, improved immune function, increased blood volume and hemoglobin mass, and improved cardiac structure and function. Pate noted an ongoing effort to encourage the National Institutes of Health (NIH) to allocate more funding to research aimed at better understanding these and other yet to be confirmed or determined underlying mechanisms.
Looking at Physical Activity and Health Through Reductionist Versus Teleological Lenses
For Pate, there are two ways to look at the issue of physical activity and health. The first is to take a reductionist approach, that is, to examine in great detail specific changes that occur with increased physical activity. Another approach is to think teleologically about how human bodies evolved to be what they were when humans were physically active hunter-gatherers. If the human body evolved to support a lifestyle that humans are no longer living, Pate said, “it should not be that surprising things don’t always go well.” A teleological approach to examining the issue of physical activity and health would suggest that the adaptations produced by regular participation in physical activity reflect a “reversion to the norm, not some odd behavior pattern. . . . When we go back to living that way, good things happen.”
KEYNOTE: DOES PHYSICAL ACTIVITY HAVE A ROLE IN REDUCING OBESITY?7
Media headlines such as that for Time magazine’s August 17, 2009, cover story, “The Myth About Exercise,” have been sending the message that exercise really is not doing that much for you, remarked keynote speaker James Hill. While one might think, Hill said, “That’s the media . . . you can’t really pay that much attention to that,” the same message is being communicated in the peer-reviewed scientific literature. As an example, he pointed to a 2013 article published in the International Journal of Epidemiology titled “Physical Activity Does Not Influence Obesity Risk: Time to Clarify the Public Health Message” (Luke and Cooper, 2013). One of the arguments made to support that claim is that changes in physical activity happened long ago and that, as Hill said, “food is driving the
_______________
7 This section summarizes information and opinions presented by keynote speaker James O. Hill, Ph.D., University of Colorado Denver.
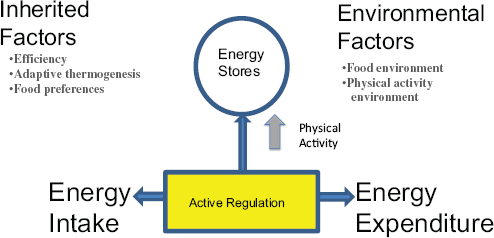
FIGURE 1-2 The energy balance system, with active regulation being a whole physiological system in and of itself.
SOURCE: Presented by James Hill on April 14, 2015.
bus right now.” Another argument often made is that one can consume a 560-calorie burger in 3 minutes, but it takes 45 to 60 minutes, depending on the activity, to burn it off, so physical activity cannot be that important. Hill asked, “Are we still lacking evidence that physical activity is important in obesity?”
To answer that question, Hill went back to his “roots,” that is, the science of energy balance. Anything that affects obesity must work through the energy balance system, he explained. That system is not as simple as calories in and calories out but is highly complex with interrelated parts, such that a change in any one factor changes the entire system. Moreover, an integral part of the system is active regulation, which is a whole physiological system in and of itself (see Figure 1-2). For the remainder of his presentation, Hill described what scientists do and do not know about how adding or subtracting physical activity impacts the energy balance system.
What Scientists Know About the Effects of Increasing Physical Activity
When physical activity is increased, whether an individual gains, maintains, or loses weight depends, Hill said, on compensation. Those who increase their level of physical activity may compensate in one of two ways: by being more sedentary at other times (i.e., when they are not exercising) than they were in the past or by consuming more calories. Most analyses of the effects of increased physical activity or exercise have failed to account for compensation, according to Hill.
Washburn and colleagues (2014) conducted a systematic review of the only approximately 30 studies in which researchers have considered whether participants were compensating for increased physical activity by being more sedentary at other times. They found strong evidence indicating that compensation did not occur in most cases. No reductions were seen in nonexercise physical activity or energy expenditure in response to prescribed physical activity or exercise training in 100 percent of cross-section studies (n = 4), 90 percent of short-term studies (n = 10), 50 percent of nonrandomized trials (n = 10), and 100 percent of randomized controlled trials (n = 7). “Certainly we need more data,” Hill said. But the data that do exist strongly suggest that people who exercise do not compensate, at least not completely. For most people, the net impact of adding exercise is a total increase in energy expenditure.
With regard to whether people who exercise eat more, which is what the Time magazine article argues, Hill stated that a fair amount of data indicate, again, that most people do not completely compensate in this way. In a meta-analysis of studies on acute exercise and subsequent energy intake, Schubert and colleagues (2013) conclude that, despite variability across studies, strong evidence suggests that exercise is effective for producing a short-term energy deficit and that individuals tend not to compensate for all of the energy expended during exercise by eating more. In a study of overweight sedentary people who underwent a 12-week supervised exercise program in which food intake was not controlled, John Blundell and colleagues found that while some participants gained or maintained weight, most lost weight (King et al., 2008). In a follow-up study conducted to determine how those who gained and lost weight in the King et al. (2008) study differed, Blundell’s group found that those who gained ate more, that is, increased their energy intake, while those who lost actually decreased their energy intake by a small amount.
In sum, the scientific literature indicates that when physical activity is added to a weight loss program, the majority of people do not compensate, at least not completely. The net result is that adding physical activity produces a negative energy balance. While results may vary among individuals, with some losing more weight and others less, Hill said, “There is no magic here. When you give people an exercise program, most people will lose weight.” Moreover, regardless of weight loss, other studies have shown that increased physical activity or fitness (e.g., as measured by VO2 max, which is the maximum rate of oxygen consumption as measured during incremental exercise) is associated with a lower percentage of stored body fat (e.g., Kriketos et al., 2000).
What Scientists Know About the Effects of Decreasing Physical Activity
Next, Hill considered what happens when people decrease their physical activity and whether doing so poses a risk for weight gain. He referred workshop participants to the energy balance science conducted in the mid-to late 1990s. In a calorimetry study on the effects of decreasing energy expenditure, for example, Stubbs and colleagues (2004) found that most people’s energy intake did not change—that is, they did not compensate by decreasing their energy intake, leaving them with a positive energy balance. In Hill’s opinion, a fair amount of evidence suggests that most people do not immediately decrease their energy intake when they decrease their physical activity, suggesting that decreased physical activity is likely an important risk factor for weight gain.
Active Regulation of Energy Balance
In Hill’s opinion, the greater question is not how physical activity affects energy expenditure or intake but how it affects the active regulation of energy balance (see Figure 1-2). Regarding what is involved in the active regulation of energy balance, scientists have learned a great deal in recent decades about how brain circuitry regulates food intake, how physical activity can impact that circuitry, and how the neural regulatory system differs between active and inactive people (e.g., Spiegelman and Flier, 2001). In addition to its impact on the brain, physical activity affects muscle, such that large changes are seen in both the structure and function of skeletal muscles when physical activity is increased (Egan and Zierath, 2013).
An important concept underlying the active regulation of energy balance, Hill continued, is metabolic flexibility versus inflexibility (Kelley, 2005). Metabolic flexibility is the ability to switch efficiently among fuels. During fasting, someone with a flexible metabolism is able to quickly suppress glucose oxidation and increase fat oxidation. A metabolically inflexible person, in contrast, has a blunted preference for fat oxidation and is not as able to suppress glucose oxidation. During insulin-stimulated conditions, again, a metabolically flexible person is able to quickly suppress, in this case, fat oxidation and increase glucose oxidation. A metabolically inflexible person, in contrast, is less able to suppress fat oxidation and stimulate glucose oxidation. Findings from Audrey Bergouignan in Hill’s lab have shown that metabolic flexibility is directly related to physical activity (Bergouignan et al., 2011).
Hill described metabolic flexibility as “the way your metabolism came out of the factory.” When people stop moving, their metabolism loses its flexibility. Losing weight does not necessarily increase metabolic flexibility, Hill said, which he suspects is one reason why weight loss without physical
activity is difficult to maintain. “You get the weight off,” he said, “but you don’t increase the metabolic flexibility.” Being metabolically inflexible does not necessarily mean that one is going to gain lost weight back, but it does increase the risk, depending on behavior and food intake patterns. People who are metabolically inflexible are more susceptible to storing rather than burning fat. “You have to be very vigilant with food intake,” Hill said.
To help explain active regulation of energy balance, Hill referred to Jean Mayer’s concept of a threshold of physical activity for optimal weight regulation (Mayer et al., 1956) (see Figure 1-3). Hill stressed that the threshold is a theoretical one, at least for now (Hill et al., 2012).
Above the threshold is what has been called the “regulated zone.” For people who occupy the regulated zone, Hill explained, as physical activity increases, energy intake increases, but body weight remains the same. The implications of this relationship are at least twofold. First, when conducting studies on physical activity, it is important to consider whether participants occupy the regulated or unregulated zone. If one were to conduct a study
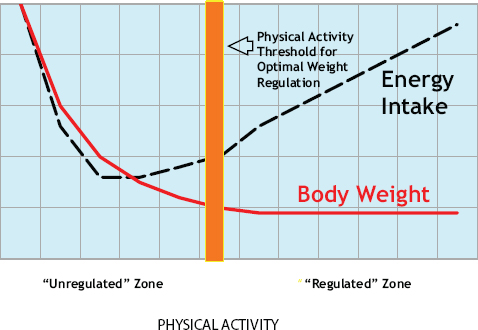
FIGURE 1-3 A theoretical graph illustrating the active regulation of energy balance.
NOTE: The dashed line represents energy intake as a function of physical activity level; the solid line represents body weight as a function of physical activity level.
SOURCE: Presented by James Hill on April 14, 2015 (modified and reprinted with permission from Mayer et al., American Journal of Clinical Nutrition [1956; 4:169-175]).
on people who occupy the regulated zone, one would observe a total compensation of energy intake with increased physical activity but no weight change. Second, the relationship suggests some feedback between physical activity and food intake, with people in the regulated zone being able to match intake with expenditure. Another way to think about this, Hill said, is that for people in the regulated zone, physical activity is driving the bus; food is just along for the ride. “I think this is the way our bodies work best,” he said.
On the other hand, for people who occupy the unregulated zone, as physical activity decreases, food intake actually increases. In contrast with the regulated zone, the coupling of physical activity and food intake is not very tight. Hill opined that most of the world is probably in this zone, where food intake, not physical activity, is in fact driving the bus.
There is no question, Hill said, that physical activity levels have decreased over the past decades. Church and colleagues (2011) report that daily occupational caloric expenditure decreased by 120 calories per day between 1960 and 2010. “That is enough,” Hill said, “to explain most of obesity.” While trends in housework energy increased for men (from 1,013 kcal/week in 1965 to 2,034 in 2010), they decreased for women over roughly that same time period (from 4,653 to 2,806). Physical activity levels are still declining, Hill said, and rapidly so in some parts of the world, such as China. “Everything we know about the science of energy balance suggests that this trend is a risk factor for weight gain,” he noted. According to Hill, every study conducted on highly palatable energy-dense diets combined with physical activity has shown less weight gain when physical activity was added to the diet compared with the diet alone. Even among people genetically susceptible to weight gain (with the fat mass- and obesity-associated FTO gene variants being among the strongest predictors of weight gain), adding physical activity can mitigate the effects of the genetic predisposition (Kilpeläinen et al., 2011).
Hill suspects that the decline in physical activity is the reason why most people today occupy the unregulated zone. In his opinion—which he admitted is based on theory, but supported by an increasing amount of data—the first step should be to get people into the regulated zone. It is not that physical activity alone is the answer; food intake, Hill agrees, is critically important. However, developing any single diet that will help people in the unregulated zone maintain their weight will be extremely difficult. And to enter the regulated zone, that is, to attain a healthy state in which they can regulate their energy balance, people need to exercise.
Regarding whether physical activity can help treat obesity, Hill remarked that John Jakicic would be exploring that question in detail during his presentation (see Chapter 4). Therefore, Hill mentioned only briefly some calorimetry work conducted in his lab showing that energy expendi-
ture decreases after weight loss because the body is smaller. If a 100 kilogram (220 pound) person were to lose 10 percent of his or her weight, or about 20 to 30 pounds, that person’s energy requirements would decrease by roughly 170 to 250 calories per day. A 20 percent weight loss (i.e., 40 to 60 pounds) would reduce the person’s energy requirements even further (i.e., by 325-480 calories/day). Work from Hill’s lab and elsewhere suggests an association between filling the “energy gap” with physical activity and the likelihood of maintaining weight loss. An increase in energy expenditure is more sustainable than a reduction in energy intake. Reducing energy intake by 200 calories per day is not trivial, Hill said, because it is very difficult to counter biological hunger mechanisms.
Should People Be Told to Exercise?
In summary, good evidence suggests that for most people, exercise will lower body fat mass. In terms of output, many studies have shown that physical activity increases energy output, as well as the capacity for protein, carbohydrate, and particularly fat oxidation. In terms of input, there may be some compensation for increased physical activity, but it is not complete, at least not among people who occupy the unregulated zone. (People who occupy the regulated zone and who are able to match energy intake with energy expenditure are “pretty good compensators,” Hill said, but they do not have a problem with excess body fat.) The bottom line, Hill concluded, is that everything known about the science of energy balance suggests that adding exercise has a positive effect on body fat mass.
Hill emphasized that physical activity and energy intake are two sides of the same coin. The best diet for an active, fit person is not the same as that for a sedentary, unfit person. Part of the problem in the obesity field, Hill said, is that dietary recommendations are aimed at sedentary, unfit people. During the Tour de France, for example, bicycle riders have been found to consume between 6,000 and 9,000 calories per day, 75 to 80 percent of which are carbohydrates, including 400 grams of simple sugars. Dietary recommendations for people burning calories the way those riders do are obviously different from those for most of the rest of the population. In Hill’s opinion, “we have one hand tied behind our back if we are just looking at the intake.” For the Tour de France riders, being as active as they are, what they eat does not matter. But that is true for only a small number of people, Hill said. Not many people are achieving energy balance at low fat mass through physical activity alone. Nor are very many people achieving energy balance at low fat mass through diet alone. Based on data from the National Weight Control Registry, only about 8 percent of the registry population is maintaining a reduced weight with diet alone. Most people, he said, are maintaining a reduced weight through a combination
of physical activity and diet, with greater levels of physical activity allowing for greater leniency with dietary intake.
What Is Missed by Focusing on Food Alone
Hill stressed that it is unlikely that obesity can be solved with food alone. The scientific evidence around energy balance strongly suggests that increasing physical activity prevents weight gain and that decreasing physical activity promotes it. More important, Hill reiterated the importance of physical activity in moving people from the unregulated to the regulated zone. Moreover, by focusing on food intake alone, many other benefits of physical activity are missed. Beyond helping to regulate weight, physical activity improves learning and cognitive function, cardiorespiratory fitness, and mental state (e.g., reduced depression), and it potentially leads as well to greater economic growth and stronger national security. In Hill’s opinion, however, the real challenge is getting people to increase their physical activity. People come to his clinic who do not really want to change their diet and do not want to exercise. They need a pretty powerful “why,” Hill said.
In conclusion, Hill highlighted four key points. First, studies of energy balance strongly suggest that changes in physical activity are directly related to changes in body weight in most people. Second, the greatest impact of physical activity may be in changing the active regulation of energy balance. Third, increasing physical activity should be an effective way to prevent and treat obesity. And fourth, the greatest challenge remains how to permanently increase people’s physical activity. Hill’s overarching conclusion was that the obesity epidemic cannot be reversed without increasing physical activity in the population.
DISPARITIES IN SOCIODEMOGRAPHIC DIMENSIONS OF PHYSICAL ACTIVITY8
Aviva Must began by suggesting that obesity in the United States was initially called an epidemic in the late 1990s because of its rapid and dramatic rise. Later, as it became apparent that obesity affected virtually all population subgroups, some called it a pandemic. Although the prevalence of obesity has increased in all groups, however, its distribution across subpopulations is not uniform. Like other health disparities, disparities in obesity and its determinants, notably physical activity, cut across social, demographic, environmental, and geographic groups, said Must. The bias,
_______________
8 This section summarizes information and opinions presented by Aviva Must, Ph.D., Tufts University, Boston, Massachusetts.
discrimination, and stigma experienced by socially disadvantaged and marginalized groups often are reflected in poor health and occupation of the “unregulated” zone described by Hill (see the previous section). Said Must, “We need to think about equitable access to physical activity opportunities, and with appropriate adaptations, and to appreciate how these can contribute to all groups achieving the highest level of health possible.”
Social disadvantage can limit physical activity in several ways, Must continued, the simplest being lack of access to the necessary material and time resources. The environment also matters; Must cited in particular the influence of stressful environments that induce depression on the uptake of physical activity. Additionally, racial discrimination and segregated neighborhoods create environments characterized by little investment in open space or facilities to promote physical activity. Finally, socially disadvantaged groups have reduced access to primary care and preventive services, so they may not receive information on physical activity’s preventive health benefits.
Must identified and went on to explore several key dimensions of both obesity and disparities in physical activity: race/ethnicity; disability; immigration status; socioeconomic status; geography (in terms of both where in the United States one lives and urban versus rural residence); and, cutting across all of these, age and gender. Regarding age and gender, she noted that, based on data from the National Health and Nutrition Examination Survey (NHANES), trends in obesity prevalence across the life course are striking, showing a steep increase with increasing age until about age 60, when a moderate decline is seen. There are no large disparities in gender across age, however (Ogden et al., 2014). Must included disability in her examination of disparities in physical activity because of an increasing awareness that disability, apart from any underlying physical manifestation, is also a social experience. People with disabilities often are subject to the same social marginalization experienced by racial and ethnic minorities, along with its consequences (i.e., lack of resources, lack of power, and lower social standing).
Race/Ethnicity
Probably the most striking disparity in obesity prevalence by race/ethnicity, in Must’s view, is the very high rate of obesity in African American women (Ogden et al., 2014). The prevalence of obesity is lower in children than in adults for all races/ethnicities, and for both children and adults, higher in blacks and Hispanics (compared with whites and Asians) and lowest in Asians (compared with whites, blacks, and Hispanics) (Ogden et al., 2014) (see Figure 1-4). Must noted that far less is known about other racial and ethnic groups and that although Hispanics encompass multiple
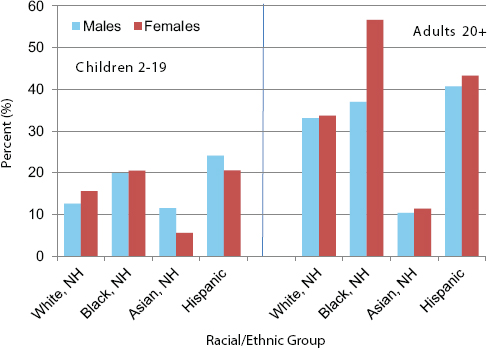
FIGURE 1-4 Prevalence of obesity by race/ethnicity and sex (National Health and Nutrition Examination Survey).
NOTE: NH = non-Hispanics.
SOURCE: Presented by Aviva Must on April 14, 2015 (Ogden et al., 2014).
groups, the most is known about Mexican Americans because they are the largest and most studied segment of the Hispanic population. Thus, data disparities exist as well.
With respect to physical activity, NHANES data, which include objective accelerometry measures of total activity minutes, indicate that MVPA in youth is similar for the three racial/ethnic groups considered (white, African American, Mexican American) (Belcher et al., 2010). Across all three groups, the data show a rapid and striking decline in activity in youth from 6-11 years to 12-15 years, and then again to 16-19 years (Belcher et al., 2010). Among youth, only males overall (all ages combined) and the youngest children (6-11 years) are meeting the recommendation of 60 minutes of MVPA per day.
Among adults, as with children, self-report data from the Behavioral Risk Factor Surveillance System (BRFSS) show very little racial/ethnic variation in physical activity, with low rates among all racial/ethnic groups. Based on 2013 BRFSS data, only about 20 to 25 percent of adults in most
racial/ethnic groups meet the U.S. national physical activity guidelines (i.e., those issued in the Physical Activity Guidelines for Americans [HHS, 2008]). In contrast, BRFSS data do show some variation in physical inactivity in adults across races/ethnicities, with blacks and Hispanics more likely to be physically inactive than whites and other subgroups. Must noted that estimates based on self-report data have more error than accelerometry-based data, but that no national survey accelerometry data exist with which to compare population subgroups of adults.
Epidemiologic data can be highly informative about physical activity levels by group, but they reveal very little about culturally determined attitudes toward physical activity and the extent to which those attitudes may be acting as either facilitators or barriers. According to Must, qualitative studies have shown that, while norms in some Asian cultures do not support strenuous activity for girls, in other Asian cultures physical activity is very much a part of daily life and is viewed as being important to maintaining one’s overall balance. Other qualitative work has shown that African American women often put the needs of others (particularly family members) before their own and are not encouraged to take care of themselves, creating a cultural barrier to physical activity.
Disability
Data show higher rates of obesity in people with disabilities (greater than 35 percent) than in any racial/ethnic group, even African Americans (CDC, 2010). Likewise, self-report data from the National Survey of Children’s Health show a higher prevalence of obesity among children who experience any of several different disabilities (hearing/vision disorder, learning disorder, developmental or physical disability, autism, attention-deficit/hyperactivity disorder [ADHD]) relative to children overall (Chen et al., 2010).
It is not surprising, Must offered, that given their unique needs, persons with mobility disabilities spend far fewer minutes in MVPA per day compared with people without disabilities, according to NHANES data (Loprinzi et al., 2014) (see Figure 1-5). Most remarkable for Must is the difference in the total amount of time spent engaged in MVPA: 28 minutes per day for people without disabilities and 12 minutes per day for people with mobility disabilities. “It is terrible for everybody,” she said, “but much worse for people with mobility limitations.”
In Must’s opinion, meeting the unique physical activity needs of individuals with disabilities is clearly a priority given the high rates of obesity in this population. She noted that meeting those needs requires special equipment and special training.
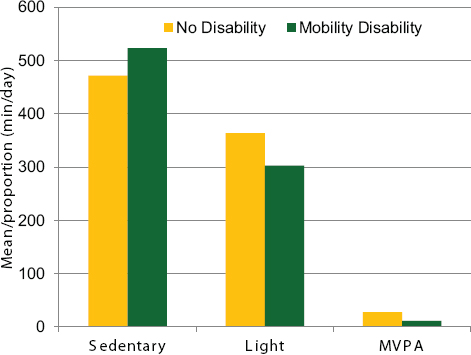
FIGURE 1-5 Time spent being sedentary, lightly active, and moderately to vigorously active for people with no disability compared with people with mobility disability.
NOTE: Mobility limitation status was self-reported; accelerometer-measured estimates of sedentary, light, and moderate- to vigorous-intensity physical activity (MVPA) were determined.
SOURCE: Presented by Aviva Must on April 14, 2015 (Loprinzi et al., 2014).
Immigration Status
National Health Interview Survey (NHIS) self-report data show rates of obesity increasing from 5-10 percent among people who have resided in the United States for less than 1 year to greater than 20 percent among those who have resided here for 15 years or more (Singh et al., 2011). This finding suggests to Must that immigrants arrive with better health behaviors than they acquire after they have arrived.
In contrast and somewhat surprising, in Must’s opinion, are self-report data from the National Survey of Children and Health (NSCH) showing that regular physical activity in children aged 6-17 years is greater among those who are U.S.-born with either one immigrant parent or two U.S. parents, compared with both foreign-born and U.S.-born children with
two immigrant parents (Singh et al., 2008). The same is true of sports participation; that is, U.S.-born children with one immigrant parent or two U.S. parents are more likely to participate in sports compared with both foreign-born and U.S.-born children with two immigrant parents. These patterns may be explained by socioeconomic status, as described in the following section.
Socioeconomic Status
Disparities in obesity and physical activity based on socioeconomic status are complicated, Must said, especially with respect to income and by sex. Based on NHANES data, obesity rates in white women decline as income increases (Chang and Lauderdale, 2005). For other racial/ethnic groups, in contrast, specifically non-Hispanic blacks and Mexican Americans, the trend is more variable (e.g., rates of obesity remain approximately the same for Mexican American women, while they vary for non-Hispanic blacks by income level but remain high in all income groups). Among non-Hispanic white men, although rates of obesity decrease as income increases, the differences are not as striking as is the case for white women. In contrast, for non-Hispanic black and Mexican American men, rates of obesity increase as income increases.
The relationship between income and physical activity is a little more straightforward, Must observed. According to 2013 BRFSS data, the likelihood of an adult’s meeting the national physical activity guidelines increases with income level. Must pointed out, however, that the percentage of adults meeting the guidelines is low across all income levels, with only 26 percent of people earning $75,000 or more meeting the nationally recommended levels of aerobic and muscle-strengthening physical activity.
Available income data do not reveal which aspect of financial resources drives income disparities in physical activity in adults. For example, are more affluent individuals more physically active because they are able to buy high-end bikes? Do they have more flexible work schedules that give them the time to engage in physical activity? Or are they privy to knowledge that makes health-related behaviors a priority?
Among children, recess policies have been shown to reflect some of the same income disparities; for example, access to school recess increases as income increases (Barros et al., 2009). School recess policies also vary by race/ethnicity, with white children having greater access than black and Hispanic children (Barros et al., 2009).
Geography
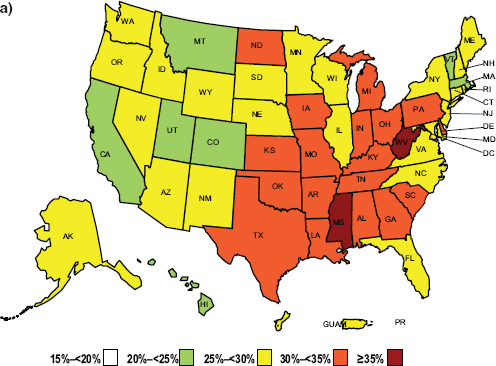
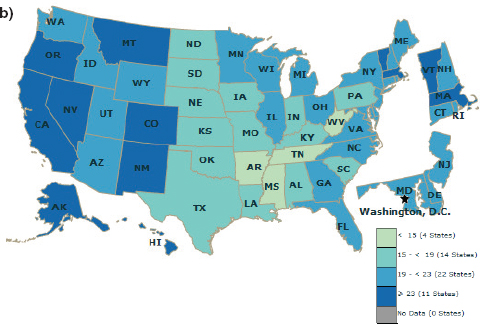
CDC’s map of adults meeting national guidelines for aerobic and muscle-strengthening physical activity corresponds quite well with CDC’s map of obesity prevalence, Must pointed out. Thus states that have the highest rates of obesity also have the lowest percentage of adults meeting the guidelines (see Figure 1-6).
In addition to being associated with geographic location, obesity rates have been associated with urbanization level, with NHIS data showing much higher prevalence in rural than in urban areas in the United States. Rural/urban differentials also are seen in physical inactivity levels: the prevalence of no leisure-time physical activity among adults is higher in rural than in urban areas, with the exception of a slight increase in physical inactivity among women in inner-city areas. Must suggested the need for better understanding of rural environments and the extent to which they may pose unique barriers to physical activity.
Although there has been little focus on rural versus urban living and its relationship to physical activity, Must observed that awareness of the impact of the built environment on physical activity is increasing. Many aspects of the built environment—such as sidewalks, accessibility of parks and recreation, bike lanes, and lighting at intersections—and their effects on physical activity have been studied. Must described one study of adults, by Gordon-Larsen and colleagues (2006), showing that the odds of engaging in five or more bouts of MVPA per week increased with the number of physical activity facilities per block (by 26 percent with seven facilities per block compared with one facility) and that the odds of being overweight decreased (by 32 percent with seven facilities compared with one facility). In Must’s opinion, public health practitioners can form strategic alliances with other public sectors to affect the built environment in ways that improve physical activity patterns for all inhabitants.
FIGURE 1-6 Behavioral Risk Factor Surveillance System (BRFSS) self-report data showing (a) the prevalence of obesity across the United States, and (b) the percentage of adults meeting national physical activity guidelines.*
NOTE: * = engaging in at least 150 minutes/week of moderate aerobic physical activity or 75 minutes/week of vigorous aerobic physical activity and in muscle-strengthening activities on 2+ days/week.
SOURCE: Presented by Aviva Must on April 14, 2015 (Centers for Disease Control and Prevention).
Achieving Physical Equity in Activity
“It is important that people become active,” Must asserted. But the barriers that socially disadvantaged groups face in becoming physically active are much greater than those faced by more advantaged groups. For the disadvantaged, said Must, “Getting from the unregulated zone to the regulated zone will be a longer journey.” She referred workshop participants to the series of commentaries on disparities in physical activity issued by the Roundtable on Obesity Solutions just prior to this workshop (Adeigbe and Ramirez, 2015; DiPietro, 2015; Rimmer, 2015; Taylor, 2015; Warne and Roanhorse, 2015; Whitaker and Gehris, 2015; see Appendix B).
To begin the panel discussion following Must’s presentation, moderator Pate asked whether the “cut-off” point for physical activity between the regulated and unregulated zones, as described by Hill, is possibly or likely different for different demographic subgroups given some of the trends described by Must. Hill responded, “I would be surprised if it is actually the same.” He reiterated that the threshold between the regulated and unregulated zones is theoretical. He suspects that, in actuality, it is different not only for different groups and subgroups but also among individuals within groups. Depending on genetics, some individuals may be able to occupy the regulated zone at lower levels of physical activity.
Pate asked Must whether anyone has combined or examined the interaction between the large datasets on overweight/obesity and physical activity. Must replied that some attempts have been made to examine the extent to which physical activity at the population level predicts some of the changes being observed in obesity prevalence, but no close associations have been reported. In her opinion, the lack of a close association is not surprising given the many other forces at play. Yet based on the physiology, she believes the association exists. The challenge is demonstrating that association given the crude measures and study designs available. “It’s always dangerous to draw firm conclusions from null studies,” Must cautioned. Hill agreed. If something makes sense physiologically, he said, null results mean “we still need to dive deeper.”
Pate added that, so often, the paradigm applied in studying the relationship between physical activity and weight status focuses on weight loss. If one were to buy into a prevention paradigm, in contrast, then the null, or no change, would in fact be the goal. But studies designed to understand no change in weight have been rare, Pate said. Hill agreed that such studies would be powerful but cautioned, “Those are tough studies to do.” They require a long period of time and large sample sizes. Plus, Hill said,
it is difficult to recruit participants to studies expecting no outcome. Must added that to some extent, those studies already exist in the natural experiments happening across the country as communities establish more physical activity–friendly policies and the prevalence of obesity decreases as a result.
To close the session, Pate asked the presenters whether they wished to communicate anything further to the workshop audience. Hill said that one of the things he thinks about a great deal with respect to physical activity is why? Why is anybody going to want to change his or her level of physical activity? People like their fast food, their big-screen televisions, and their automobiles. Yes, they would like to be fitter and leaner, but they are essentially choosing not to become fitter and leaner. He said, “We really need to know, what is the powerful ‘why?’”
Must called for a greater understanding of what she referred to as the physical activity version of making the healthy or natural choice. She wondered what could be learned from cultures in which physical activity is valued as something that keeps human beings “in balance.”


























