5
Collaborating and Leading in
Care Delivery and Redesign
According to The Future of Nursing, if nurses are to contribute fully to the transformation of the health care system, they must become leaders “from the bedside to the boardroom” (IOM, 2011). The report states that nurse leaders are needed to lead and participate in the ongoing reforms to the system, to direct research on evidence-based improvements in care, to translate research findings into the practice environment, to be full partners on the health care team, and to advocate for policy change. Rather than using a traditional top-down style of leadership, the report suggests that nurses should lead by engaging all members of the health care team in an environment of interprofessional collaboration and mutual respect. The report calls on health care organizations, nursing associations, nursing educators, and all nurses to create, support, and seek opportunities for collaboration and leadership at all levels and in every practice environment. The report offers two recommendations in this area:
- recommendation 2: Expand opportunities for nurses to lead and diffuse collaborative improvement efforts (see Box 5-1); and
- recommendation 7: Prepare and enable nurses to lead change to advance health (see Box 5-2).
These recommendations—and the Campaign’s work in this area—fall into three broad categories: interprofessional collaboration, preparing nurses to serve as leaders, and opening up opportunities for nurses to lead.
BOX 5-1
Recommendation 2 from The Future of Nursing:
Expand Opportunities for Nurses to Lead and
Diffuse Collaborative Improvement Efforts
Private and public funders, health care organizations, nursing education programs, and nursing associations should expand opportunities for nurses to lead and manage collaborative efforts with physicians and other members of the health care team to conduct research and to redesign and improve practice environments and health systems. These entities should also provide opportunities for nurses to diffuse successful practices.
To this end:
- The Center for Medicare and Medicaid Innovation should support the development and evaluation of models of payment and care delivery that use nurses in an expanded and leadership capacity to improve health outcomes and reduce costs. Performance measures should be developed and implemented expeditiously where best practices are evident to reflect the contributions of nurses and ensure better-quality care.
- Private and public funders should collaborate, and when possible pool funds, to advance research on models of care and innovative solutions, including technology, that will enable nurses to contribute to improved health and health care.
- Health care organizations should support and help nurses in taking the lead in developing and adopting innovative, patient-centered care models.
- Health care organizations should engage nurses and other front-line staff to work with developers and manufacturers in the design, development, purchase, implementation, and evaluation of medical and health devices and health information technology products.
- Nursing education programs and nursing associations should provide entrepreneurial professional development that will enable nurses to initiate programs and businesses that will contribute to improved health and health care.
SOURCE: IOM, 2011.
INTERPROFESSIONAL COLLABORATION
Despite being rated highly by the public for ethical standards and honesty and being considered “one of the most trusted sources of health information” (Gallup, 2010, 2015), nurses often are excluded from decision making and relegated to carrying out the instructions of others (IOM, 2011). The Future of Nursing notes that nurses often are the best source of knowledge and awareness of patients, families, and communities, but “do not speak up as often as they should”
BOX 5-2
Recommendation 7 from The Future of Nursing:
Prepare and Enable Nurses to Lead
Change to Advance Health
Nurses, nursing education programs, and nursing associations should prepare the nursing workforce to assume leadership positions across all levels, while public, private, and governmental health care decision makers should ensure that leadership positions are available to and filled by nurses.
- Nurses should take responsibility for their personal and professional growth by continuing their education and seeking opportunities to develop and exercise their leadership skills.
- Nursing associations should provide leadership development, mentoring programs, and opportunities to lead for all their members.
- Nursing education programs should integrate leadership theory and business practices across the curriculum, including clinical practice.
- Public, private, and governmental health care decision makers at every level should include representation from nursing on boards, on executive management teams, and in other key leadership positions.
SOURCE: IOM, 2011.
(IOM, 2011, p. 224). The report calls on health care organizations, nursing educators, and nursing associations to train, support, and encourage nurses to lead and manage interprofessional collaboration efforts. The report cites evidence that collaboration and mutual respect among health care professionals have been associated with improved patient outcomes, cost savings, and increased job satisfaction.
The Future of Nursing therefore recommends that there be expanded “opportunities for nurses to lead and manage collaborative efforts with physicians and other members of the health care team” and “opportunities for nurses to diffuse successful practices” (IOM, 2011, p. 279). Specifically, the report calls for organizations, including the Center for Medicare & Medicaid Innovation (CMMI), to support the development of models of care that use nurses in a leadership capacity, and for health care organizations to support nurses in “taking the lead in developing and adopting innovative, patient-centered care models” (IOM, 2011, p. 280).
Activity
Interprofessional Education
Interprofessional education has received a great deal of attention in recent years, bolstered in part by numerous activities and reports around this issue, including
- the World Health Organization’s Framework for Action on Interprofessional Education and Collaborative Practice (WHO, 2010);
- the report of the Lancet Commission on the Education of Health Professionals for the 21st Century titled Health Professionals for a New Century: Transforming Education to Strengthen Health Systems in an Interdependent World (Frenk et al., 2010);
- conferences and reports of the Josiah Macy Jr. Foundation, including the Conference on Interprofessional Education and Transforming Patient Care: Aligning Interprofessional Education with Clinical Practice Redesign (Josiah Macy Jr. Foundation, 2012, 2013b); and
- the Institute of Medicine (IOM) Global Forum on Innovation in Health Professional Education’s workshop summary Interprofessional Education for Collaboration: Learning How to Improve Health from Interprofessional Models Across the Continuum of Education to Practice (IOM, 2013).
Yet, as Thibault (2011) notes,
Interprofessional education is one strategy to improve nursing education and enhance the role of nurses as collaborative leaders in the health care system. . . . Although we have good evidence that health care provided in teams of professionals is more efficient and is associated with better patient outcomes, we have not structured education to prepare students for team care or team leadership. (p. 313)
The American Association of Colleges of Nursing (AACN) considers “interprofessional collaboration for improving patient and population health outcomes” to be an essential part of baccalaureate, master’s, and doctoral education, and has incorporated it into “Essentials” documents that outline necessary curriculum and expected competencies for each level of education (AACN, 2006, 2008, 2011). For a school to be accredited by the Commission on Collegiate Nursing Education (CCNE), it must comply with these Essentials documents (CCNE, 2013; Zorek and Raehl, 2012). For example, the Essentials document for baccalaureate programs in nursing states that the baccalaureate program prepares the graduate to, among other things, “use inter- and intraprofessional communication and collaborative skills to deliver evidence-based, patient-centered care”; “contribute
the unique nursing perspective to interprofessional teams to optimize patient outcomes”; and “demonstrate appropriate teambuilding and collaborative strategies when working with interprofessional teams” (AACN, 2008, p. 22). A study of the effectiveness of these types of accreditation standards found that nursing graduates may be among the “most prepared” for interprofessional collaborative practice (Zorek and Raehl, 2012, p. 6). Another study, however, found that the interprofessional opportunities offered in nursing programs were narrow in scope and most commonly focused on acute care simulation and seminars rather than on interprofessional work in community settings (Hudson et al., 2013).
In December 2014, CCNE entered into an agreement with five other health professions accreditors (the Accreditation Council for Pharmacy Education, Commission on Dental Accreditation, Commission on Osteopathic College Accreditation, Council on Education for Public Health, and Liaison Committee for Medical Education) to form the Health Professions Accreditors Collaborative (HPAC) (CCNE, 2014). These organizations meet regularly to determine how they can work together on interprofessional education, showing that in addition to efforts within the nursing profession to expand interprofessional education, health professionals from many disciplines are partnering to develop competencies and curricula for such education. As emphasized by Steven Weinberger, Executive Vice President and CEO, American College of Physicians, at the committee’s May 2015 workshop,
What we really need is a cultural change. This is a good example of culture eats strategy for lunch. Getting a cultural change with the older physician population is going to be very difficult, and this is going to have to be something that occurs over time. The critical area is in the training environment. We need to have more and more effective interprofessional education so that there is this sense of mutual respect and trust that is built from day zero.
The Association of American Medical Colleges (AAMC) developed the MedEdPORTAL® in 2005 to enhance knowledge about medical education resources (AAMC, 2015). In the 10 years since, it has expanded this portal to promote interprofessional collaboration by including resources and materials from across the health professions. In 2012, AAMC expanded the portal to be a “clearinghouse of competency-linked IPE [interprofessional education] learning resources and educational materials” (AAMC, 2012). The IPE Portal is an initiative of AAMC and the Interprofessional Education Collaboration (IPEC). Since its creation, AAMC also has partnered with the American Psychological Association and the American Board of Medical Specialties to expand the portal (AAMC, 2015). In 2014, AAMC and AACN partnered to provide awards for the best materials and curricula for improving interprofessional education in support of the Lifelong Learning in Interprofessional Education initiative (AAMC, 2014).
IPEC was formed in 2009 as a joint effort of AACN, the American Association of Colleges of Pharmacy, the American Association of Colleges of Osteo-
pathic Medicine, the American Dental Education Association, the Association of Schools of Public Health, and AAMC (IPEC, 2015). In 2011, IPEC published the report Core Competencies for Interprofessional Collaborative Practice (IPEC, 2011), which lays out a vision of interprofessional collaborative practice as “key to the safe, high quality, accessible, patient-centered care desired by all” (p. i) and specifies four core competencies that all health professionals need to develop. The report stresses that these competencies cannot be developed solely within the profession; rather, students of different professions must be engaged in interactive learning with each other. Within the competency domain relating to values and ethics for interprofessional practice are two specific competencies relating to cultural competency: “embrace the cultural diversity and individual differences that characterize patients, populations, and the health care team,” and “respect the unique cultures, values, roles/responsibilities, and expertise of other health professions” (p. 19). Addressing issues around cultural competence during education, training, and practice may ensure that members of health care teams understand and embrace diversity of backgrounds, approaches, and values as interprofessional collaboration becomes increasingly emphasized.
Interprofessional Practice
The Future of Nursing calls on private and public funders to advance research on models of care and innovative solutions that can enable nurses to contribute to the improvement of health. The report specifically calls on CMMI to support the development and evaluation of models of care delivery that use nurses as leaders. CMMI has since created the Health Care Innovation Awards program, which provides up to $1 billion to organizations that are implementing innovative projects to improve health and lower costs (CMS, 2013, 2015). Several of the funded projects include nurses as leaders or members of interprofessional teams (CMS, 2013). For example,
- Cooper University Hospital in Camden, New Jersey, received funding to use nurse-led interdisciplinary outreach teams, with the goal of improving primary care access and reducing hospital readmissions; and
- Developmental Disabilities Health Services received funding to test a model in which teams of nurse practitioners and physicians work together to provide primary care and case management to persons with developmental disabilities.
Another government-led initiative is the Health Resources and Services Administration’s (HRSA’s) Nurse Education, Practice, Quality, and Retention Program, which has provided more than $67 million between 2012 and 2015
to 66 different grantees for interprofessional collaborative practice.1 In its 2014 funding opportunity announcement, HRSA states that “the goals of the program and the purposes of the funding opportunity announcement are consistent with the statutory authority provided in Title VIII to provide coordinated care and for nurses to develop skills needed to practice in existing and emerging organized health care systems” (HRSA, 2014). One grantee, the Vanderbilt School of Nursing, has developed a model of interprofessional collaborative practice with an interprofessional team of providers comprising a family nurse practitioner, pharmacist, social worker, physician, community health advocate, part-time nurse, and medical assistant (Pilon et al., 2015a,b). The nurse practitioner is responsible for diagnosis, treatment, and referral and the overall care planning for the patient, and also has oversight of the care team and coordinates student clinical rotations. The team is based in a primary care clinic serving disadvantaged patients with complex health care needs. This clinic also serves as the clinical site for health professions students in the Vanderbilt Program in Interprofessional Learning (Pilon et al., 2015b).
In addition to government efforts, many organizations are working to expand interprofessional practice. The committee heard details about two such organizations:
- Community Health Center, Inc. (CHC) is a federally qualified health center that provides primary care and social services to primarily low-income persons in Connecticut (CHC, 2015). CHC uses innovative, team-based models of care and relies heavily on nurse practitioners as providers of primary care.
- The National Center for Interprofessional Practice and Education (NCIPE) was launched in 2012 through a cooperative agreement between HRSA and the University of Minnesota, and also is funded by the Robert Wood Johnson Foundation (RWJF), the Josiah Macy Jr. Foundation, and the Gordon and Betty Moore Foundation (NCIPE, 2013b,c). The center studies and advances collaborative, team-based care and health professions education (NCIPE, 2013a). Although NCIPE is a neutral convener that does not favor any one profession, many of the innovative models of care that are developed through the center are focused on nurses.
The Campaign addresses the recommendations of The Future of Nursing in the area of collaboration and leadership under the pillar of “fostering interprofessional collaboration” (CCNA, n.d.). As of December 2014, 25 state Action Coalitions were working to further interprofessional education and collaboration
___________________
1 Information derived from the HRSA Data Portal, filtered by Grant Activity Code UD7, August 18, 2015.
(CCNA, 2014b). For example, Colorado has received a grant from HRSA to support the implementation of Interprofessional Collaborative Practice Teams at community health centers; Hawaii is building an interprofessional workforce database; and Virginia, in a partnership with the Medical Society of Virginia Foundation, is implementing a pilot clinical leadership program that encourages pairings between nurses and other providers.
Two states—Rhode Island and Utah—have implemented an interprofessional collaboration practice and/or education model, while 10 other Action Coalitions are working toward this goal (CCNA, 2015d). Rhode Island’s collaborative practice is integrated into its residency model, while Utah’s includes an interprofessional education program at the University of Utah, where all health science students are required to take an interprofessional course.
Progress
Since The Future of Nursing was released, interprofessional education has expanded rapidly at schools of nursing. The Campaign tracks progress in this area by looking at the number of required clinical courses and/or activities at the top 10 nursing schools that include both registered nurse (RN) students and other graduate health professional students. In 2011, only 6 such courses or activities were offered at the top 10 nursing schools; by 2013, there were 22 (see Figure 5-1). Eight of the 10 schools have added these courses or activities since 2011.
Discussion
Interprofessional education and team-based, collaborative practice are not new concepts in the health professions (Bodenheimer et al., 2002; Grumbach and Bodenheimer, 2004; IOM, 2003; Leape et al., 2009; Needleman and Hassmiller, 2009; Wagner, 2000). The 2003 IOM report Health Professions Education: A Bridge to Quality notes the importance of interprofessional education, stating that “all health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team” (IOM, 2003, p. 3). This report further highlights work in interdisciplinary teams as one of five core competencies necessary for all clinicians to “cooperate, collaborate, communicate, and integrate care in teams to ensure that care is continuous and reliable” (p. 4). However, progress in advancing interprofessional education and collaboration has been particularly notable in recent years, both in the field of nursing and in other health care professions.
Since the release of The Future of Nursing, additional evidence has shown that when nurses collaborate with other health care professionals, outcomes are improved. For example, one study found that nurses’ collaboration with other disciplines was essential to safe and effective care in hospitals, including avoiding
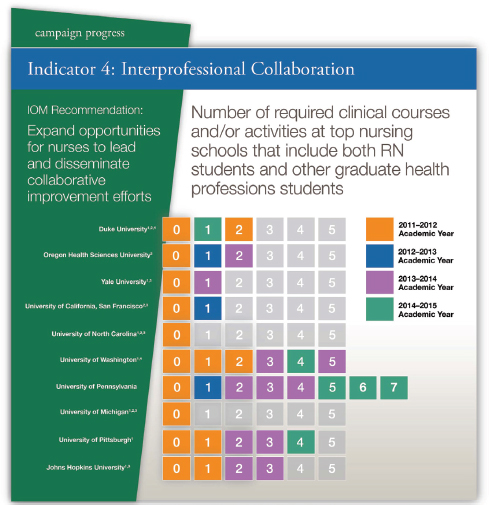
FIGURE 5-1 Number of required clinical courses and/or activities at the top 10 nursing schools that include both registered nurse (RN) students and other graduate health professional students.
NOTES:
1 No change between the 2011-2012 and 2012-2013 academic years.
2 No change between the 2012-2013 and 2013-2014 academic years.
3 No change between the 2013-2014 and 2014-2015 academic years.
4 This institution reduced the number of required courses and/or activities for the 2014-2015 academic year.
Data are from the top 10 nursing schools (as determined by U.S. News & World Report rankings) that also have graduate-level health professions schools at their academic institutions. Course offerings and requirements include clinical and/or simulation experiences.
SOURCE: CCNA, 2015e.
adverse drug events (Feldman et al., 2012). In another study, nurse leadership of teams was associated with improved safety and quality, including an 81 percent reduction in central line-associated bloodstream infections (Marstellar et al., 2012). The authors note that “this study was conceived as a nurse-led program and showed that nurses can effectively drive an interdisciplinary safety program in their units. Nurses did report during interviews, however, that greater physician engagement would have benefited them” (p. 2936). Thus, the study validated both the role of nurse leadership and the importance of interprofessional collaboration.
The trend toward interprofessional collaboration in all fields is consistent with recommendations 2 and 7 in The Future of Nursing, and progress has been made on many fronts, including some of the specific bullet points under these recommendations (see Boxes 5-1 and 5-2, respectively). Going forward, however, the scope of these recommendations will need to be broadened to acknowledge that nurses cannot expand interprofessional collaboration or education alone. Collaboration requires all members of a team working to their full potential on behalf of the patient and with respect for the contributions of other professions to the work. It will be important for health care teams to understand and navigate the professional and personal cultural backgrounds of individual team members. Nurses need to be prepared to serve as a part of the team and to lead or coordinate efforts as appropriate. To this end, it will be important to continue efforts to develop models of care that use nurses as team leaders. To achieve true interprofessional collaboration, however, all health care professionals will need to work together to plan how to attain this goal.
In 2013, the Campaign acknowledged that this shift was needed when it asked its Action Coalitions to “move beyond nursing and focus on improving health and healthcare for consumers and their families” and to “not ignore the diverse stakeholders critical to the [Action Coalitions’] success” (TCC Group, 2014, p. 1). In a survey conducted later that year, the vast majority of Action Coalitions (95 percent) stated that they did not ignore diverse stakeholders, but still only 27 percent of respondents agreed that their coalition “includes sufficient non-nursing-related organizations and representatives to make progress on [their] goals,” despite reaching out to new and diverse members (TCC Group, 2013, p. 14). Further, only one-quarter of Action Coalitions said they had moved beyond nursing. The TCC Group evaluators concluded that “this may have a lot to do with states that used the first couple of years to coalesce their nursing groups, clear natural allies, and are now trying to figure out legitimate ways to bring in other stakeholders” (TCC Group, 2013, p. 10).
Findings and Conclusions
Findings
This study yielded the following findings on interprofessional collaboration:
Finding 5-1. Significant efforts are directed toward strengthening interprofessional education and practice in nursing as well as in other health care professions.
Finding 5-2. Health care is shifting toward a team-based, interprofessional approach.
Finding 5-3. Three-quarters of the Campaign’s state Action Coalitions are not including non-nursing stakeholders in their coalitions.
Finding 5-4. The Campaign’s measure of success on recommendations 2 and 7 of The Future of Nursing is limited to counting interprofessional courses offered at the top 10 nursing schools.
Conclusions
The committee drew the following conclusions about progress toward nurses engaging in collaborative activities:
True interprofessional collaboration can be accomplished only in concert with other health professionals, not within the nursing profession alone.
State Action Coalitions need assistance in reaching out to non-nursing stakeholders.
In the new context of health care, the Campaign itself needs to be a broader coalition of stakeholders from all health care professions if it is to make progress.
The Future of Nursing notes that nurses at all levels need strong leadership skills, but it observes that, historically, nurses have not held leadership positions that have enabled them to contribute fully (IOM, 2011). In recommendation 7 (see Box 5-2), The Future of Nursing calls on nurses and the organizations that train, support, and employ them to work on developing necessary leadership competencies and to provide opportunities for nurses to lead at every level. Specifically, the report recommends that nurses take responsibility by seeking opportunities to develop leadership skills, that nursing education programs include entrepreneurship and leadership skills in their curriculum, and that nursing associations provide leadership development opportunities for their members.
Activity
Leadership development opportunities have been established and expanded by nursing education programs, nursing associations, and private organizations since The Future of Nursing was released.
Nursing Education Programs
A number of nursing programs offer opportunities for students to learn leadership and entrepreneurship either at the nursing school or in combination with another school. For example,
- Columbia University School of Nursing has a combined (MS/MBA) program that includes classes at both the school of nursing and the school of business2;
- Drexel University confers a master of science in nursing (MSN) degree in Innovation and Intra/Entrepreneurship in Advanced Nursing Practice3;
- New York University College of Nursing offers an undergraduate honors elective in social entrepreneurship that incorporates content from business, the humanities, and service learning (Gilmartin, 2013); and
- the University of Pennsylvania offers a dual degree program whereby enrollees complete a bachelor of science in nursing (BSN) degree through the School of Nursing and a bachelor of science in economics degree through the Wharton School, with the Wharton curriculum focusing on health care management and policy (University of Pennsylvania, 2015a).
Nursing Associations
Nursing associations are among the most active sponsors of programs designed to develop leadership and entrepreneurial skills for nurse leaders in a variety of positions. The American Organization of Nurse Executives (AONE) offers a variety of programs and opportunities that prepare nurses for leadership roles, including the Emerging Nurse Leader Institute, the Nurse Manager Fellowship, a Certificate in Health Care Finance, and a program that prepares nurses to be leaders on hospital governance boards. AONE also has partnered with academic institutions and organizations to provide interprofessional leadership development for its members. For example, AONE and Arizona State University offer an Interprofessional Fellowship in Innovative Health Leadership in partnership
___________________
2 See http://nursing.columbia.edu/academics/academic-programs/msmba-program-description-nursing-and-business-msmba (accessed September 11, 2015).
3 See http://drexel.edu/cnhp/academics/graduate/MSN-Innovation-and-Intra-Entrepreneurship-Nursing-Practice (accessed September 11, 2015).
with the Mayo Clinic’s Center for Innovation (Arizona State University, 2015). The fellowship is designed to help health professionals with executive leadership responsibilities develop the skills necessary to drive innovation at their organizations. AONE also has partnered with the Harvard Business School’s Managing Health Care Delivery program, a leadership development program that explores “designing your organization from the ground up, managing performance, and improving and innovating over time” (AONE, 2015; Harvard Business School, 2015). This partnership allows AONE to offer reserved seats in the program specifically to nurses (AONE, 2015).
The AACN-Wharton Executive Leadership Program was launched in 2012, with the support of the Jonas Center for Nursing Excellence, with the goal of enhancing leadership for change in health care (AACN, 2015a). The program is open to deans and directors and associate deans and directors of AACN nursing schools who serve as chief or associate chief nursing academic officers. The program is aimed at helping participants develop skills needed to “manage and lead change at an enterprise level, strategically influence and negotiate, and skillfully strategize and innovate value with internal and external stakeholders” (AACN, 2015b). Together with AACN, the Wharton School also offers the Wharton Nursing Leaders Program to upper-level nurse managers (University of Pennsylvania, 2015b). This program, however, focuses on nursing leadership and support for nurse managers and executives in clinical settings.
The American Academy of Nursing’s Jonas Policy Scholars Program was launched in 2014 to support 2-year fellowships for doctoral or postdoctoral nursing students to learn about health policy (AAN, 2014). According to Darlene Curley, executive director of the Jonas Center, “The Jonas Policy Scholars will serve at the highest levels of leadership in ensuring quality, cost-effective and accessible healthcare” (Jonas Center, 2015a).
Private Organizations
In addition to RWJF, other private, philanthropic organizations have been supporting the education and training of nurse leaders. For example, the Josiah Macy Jr. Foundation has a Faculty Scholars program, established in 2010, that provides support to faculty leaders at nursing and medical schools (Josiah Macy Jr. Foundation, 2013a). Five faculty leaders are chosen each year for the program, and they must commit to spending half of their time pursuing education reform projects at their institution; 40 percent of participants to date have been nursing faculty. Each scholar receives career advice from a committee of distinguished health care leaders.
The Jonas Center for Nursing and Veterans Healthcare has worked to improve nurse leadership by supporting the development of nursing doctoral students through its Jonas Nurse Leaders Scholar Program, which has grown dramatically since its launch in 2008 (Jonas Center, 2015b) (see Chapter 3). In addition to the
scholars program, which requires each of its scholars to complete a 40-hour leadership project focusing on one of the recommendations of The Future of Nursing (Curley, 2015), the Jonas Center provides support for convening and recognizing nurse leaders. Support recently has been provided for the AACN Student Policy Summit, the Sigma Theta Tau International Foundation Convention, and the AACN-Wharton Executive Leadership Program (Jonas Center, 2015c).
The Campaign has created a national nursing leadership strategy under the pillar “leveraging nursing leadership” (CCNA, n.d.). This pillar encompasses efforts around preparing nurses to lead and ensuring that nurses have leadership roles in health care. At the state level, 41 Action Coalitions were in the process of developing or implementing at least one leadership program as of December 2014, and some states had already established leadership institutes, programs to identify emerging leaders, or mentorship programs (CCNA, 2014b).
The Campaign also recently established the Breakthrough Leadership in Nursing Awards program to recognize and advance 10 nurse leaders (CCNA, 2015b). The awardees receive scholarships for a Leadership Development Program at the Center for Creative Leadership, which is designed to build skills, knowledge, and confidence.
Progress
The Campaign has no indicator with which to track how and whether nurses are being prepared to lead. While the committee identified a number of leadership programs and courses offered at nursing and other schools, there is no single source of information about nurse training in leadership, entrepreneurship, or innovation.
Discussion, Findings, and Conclusion
The Future of Nursing recognizes that for nurses to contribute fully in leadership positions, they must first develop the skills and competencies needed to do so. The report’s recommendations in this area are directed at the profession itself—a call for nurses to prepare themselves proactively for leadership roles. And as noted by Ann Kurth, Dean, Yale School of Nursing, at the committee’s July 2015 workshop, “In addition to the clinical aspects, nurses must also understand the financial, IT [information technology], and operational components to effectively design a sustainable future state model.”
Findings
This study yielded the following findings on nurse leadership:
Finding 5-5. A number of programs have been created or expanded to help nurses develop leadership, entrepreneurial, and managerial skills.
Finding 5-6. Data are lacking on how many nursing schools are offering courses in leadership, entrepreneurship, or management, or how many nursing students are taking these types of courses outside of their nursing school.
Conclusion
The committee drew the following conclusion about progress toward nurses becoming leaders:
To assess progress on leadership development, it is necessary to track programs and courses in leadership, entrepreneurship, and management in which nurses are participating.
NURSES IN LEADERSHIP POSITIONS
The Future of Nursing report’s recommendation 7 includes as one of its bullet points that “public, private, and governmental health care decision makers at every level should include representation from nursing on boards, on executive management teams, and in other key leadership positions” (IOM, 2011, p. 283; see Box 5-2). This recommendation followed from the report’s findings that nurses were greatly underrepresented in their own health care organizations’ governance structures, as well as on institution and hospital boards. A 2011 survey found that physicians made up 20 percent of board membership and nurses accounted for 6 percent; in 2014, the percentage of physician board members remained the same, while the percentage of nurse board members decreased to 5 percent (AHA, 2014). The IOM report suggests that nurses are needed in these leadership positions in order to contribute their unique perspective and expertise on such issues as health care delivery, quality, and safety.
Activity
Much of the Campaign’s focus has been on getting nurses appointed to health-related boards. The Nurses on Boards Coalition was launched in November 2014 as a “direct response” to the recommendation of The Future of Nursing, and in addition to RWJF and AARP, it includes as members 19 other nursing organizations (CCNA, 2015f). The goal of the effort is to place 10,000 nurses on corporate and nonprofit health-related boards of directors by 2020. The Nurses on Boards Coalition was born out of two national nursing leadership strategy meetings on April 21, 2014, and July 21, 2014, and a series of smaller meetings and webinars around nursing leadership (CCNA, 2014c,d, 2015d). The Campaign
also has worked to increase the representation of nurses on the boards of the organizations that make up its Champion Nursing Coalition, whose members include Aetna, Johnson & Johnson, and Target.4 At the state level, the Campaign assists Action Coalitions with collecting data on nursing leadership and increasing the numbers of nurse leaders on state and local boards. As of January 2015, 19 Action Coalitions were collecting data on nurses serving on boards, and 22 more planned to do so in the future (CCNA, 2015d).
Beyond the Campaign’s efforts, the committee heard about other efforts to increase nurse leadership, including the American Nurses Credentialing Center’s (ANCC’s) Magnet® recognition program. Hospitals and other health care organizations designated as Magnet are required to have nurses integrated into their governance structure (ANCC, 2015). Specifically, organizations must have an individual serving as the chief nursing officer (CNO), who is responsible for the standards of nursing practice across the organization. The CNO must be a member of the organization’s governing body, involved in decision making and strategic planning.
Progress
To assess progress on this recommendation, the Campaign tracks the percentage of hospital boards with RN members. In 2014, the Campaign reported a baseline of 5 percent, but it does not yet have updated numbers (CCNA, 2015e). The Campaign’s efforts to increase nurse representation on the boards of its Champion Nursing Coalition has seen some success, with 45 nurses serving on boards in May 2015, up from 10 in July 2013 (CCNA, 2014a, 2015a,d). State Action Coalitions have seen an increase in nurses serving on state and local boards, with the number rising from 268 in July 2014 to 310 in May 2015 (CCNA, 2014a, 2015d). In addition to this progress, the American Nurses Association, which continually tracks calls for nominations for agencies and organizations, reported that 11 nurses were appointed to 13 positions at the U.S. Office of the National Coordinator for Health Information Technology (ONC) within the past year (Cipriano, 2015).
Discussion, Findings, and Conclusions
In this recommendation, The Future of Nursing calls on those outside of the nursing profession to appoint nurses to leadership positions in all types of organizations.
___________________
4 See a full list of Champion Nursing Coalition members at http://campaignforaction.org/whosinvolved/champion-nursing-coalition (accessed November 20, 2015).
Findings
This study yielded the following findings on nurses in leadership positions:
Finding 5-7. The Campaign has had some success in getting more nurses appointed to private boards—one part of recommendation 7 of The Future of Nursing—but has been less active on the issue of nurses serving as leaders “on executive management teams, and in other key leadership positions” in “public, private, and governmental health care” organizations.
Finding 5-8. Data on nurses serving as leaders are scarce; the data that are available are fragmented and incomplete.
Conclusions
The committee drew the following conclusions about progress toward having more nurses serve in leadership positions.
It is necessary to gather more data on nurses serving as leaders.
More focus is needed on nurses serving in leadership positions other than on private boards.
THE CAMPAIGN FOR ACTION’S COMMUNICATION EFFORTS
TO SUPPORT COLLABORATION AND LEADERSHIP
As described in Chapter 1, the Campaign has made efforts to engage stakeholders in its activities. In addition to the nursing community, these stakeholders include business leaders, payers, philanthropic organizations, policy makers, consumers, and other health professionals. The ability to communicate effectively with these groups is critical to collaboration and leadership efforts. The Campaign has used a number of avenues for its communications through its state Action Coalitions, as well as at the national level (CCNA, 2015c; see also Chapter 1).
Activity and Progress
The Campaign acknowledges that the capacity and ability of the Action Coalitions to communicate about their efforts vary greatly, despite efforts by the Campaign’s leaders to develop branding guidance, templates, and other communication tools (CCNA, 2015c). Many Action Coalition leaders lack expertise in and experience with traditional and social media, and they have little time to learn because of competing priorities and commitments. The Action Coalitions that have staff dedicated to communications have had successes, according to
the Campaign (CCNA, 2015c). The Campaign thus believes that “decisions are needed about how important state-level communications are to the Campaign’s success, and how to put resources toward efforts deemed most appropriate” (CCNA, 2015c, p. 7). In making these decisions, it may be important to consider that Action Coalitions indicate that communication support from the Campaign is useful. In 2013, 67 percent of survey respondents said they had used Campaign communication support services, and 85 percent of those that had done so found the services useful (TCC Group, 2013).
In addition to supporting the communications of the Action Coalitions, the Campaign has engaged in several other communication initiatives:
- The Campaign has engaged targeted audiences, primarily the nursing and higher education communities, through strategic communication initiatives that have leveraged both traditional media and new media platforms (CCNA, 2015c; see also Chapter 1).
- The Speakers Bureau has sent Campaign representatives and leaders to various conferences across the country to raise awareness of and inform key audiences about the recommendations of The Future of Nursing, and to gather relevant data and information to advance Campaign goals.
- Online communication tools provide Campaign volunteers with materials to use in engaging media, policy makers, and interested stakeholders.
By the Campaign’s estimation, these communication efforts have “raised awareness [and] resulted in actions as well as policy and law changes. Consumers are more knowledgeable of efforts to advance nursing to create more affordable and accessible health care” (CCNA, 2015c, p. 5). However, a thorough evaluation of its many activities would be necessary to assess the actual impact of the Campaign’s communication efforts.
The stated goal of the Campaign is to engage a wide range of stakeholders; however, the Campaign acknowledges that its efforts have been focused largely on engaging nurses and that it needs to use its extensive “communications channels and platforms to reach broader, strategically important audiences” (CCNA, 2015c, p. 5). In 2013, the Campaign developed new imperatives that reflect this gap, including to “move beyond nursing and focus on improving health and healthcare for consumers and their families” and to “not ignore the diverse stakeholders critical to success” (TCC Group, 2014; see also Chapter 1 and the Interprofessional Collaboration section of this chapter). As noted earlier, the majority of Action Coalitions have worked to engage diverse stakeholders but do not believe that they have adequate non-nursing representation to further their goals. They also overwhelmingly indicated that they have had difficulty moving beyond nursing to focus on health care more broadly. The Campaign’s external evaluators concluded that the lack of progress in this area was due to the intense efforts of Action Coalitions in their formative years to gain the engagement of their allies
(TCC Group, 2013). The evaluators go on to suggest, “We would anticipate that groups will continue to benefit from communications support that helps them craft a message of broader health and healthcare, as well as new (and more visible existing) research demonstrating the health and healthcare benefits of each of the IOM recommendations” (p. 10). Indeed, a subsequent analysis by TCC Group (2014) showed that Action Coalitions that felt they were making progress in moving toward a more inclusive vision of health care had a clear understanding of the goals of the Campaign, were able to communicate effectively across their workgroups and stakeholders, and had used Campaign communication support.
Moving forward, the Campaign can, at both the national and the state level, expand the scope of its communication strategies to connect with a broader audience. For example, greater use of new media and other technology to inform health care consumers about The Future of Nursing could potentially help with the recruitment of volunteers from a cross-section of the community, including ethnic communities. The Campaign could engage physicians who support the recommendations of The Future of Nursing, particularly the recommendation on expanding nurses’ scope of practice (see Chapter 2), as spokespersons to further demonstrate a collaborative approach involving other health professionals. The Campaign’s social media engagement has been productive in disseminating messages in conjunction with National Nurses Week (CCNA, 2015c), but two-way engagement with key audiences has been limited by a lack of next steps for individuals to take to accomplish meaningful action. Development of an engagement ladder, including ways to work with the Action Coalitions on various tactics, would be a productive means of sustaining interest among a broader audience, including students, health care consumers, business leaders, philanthropic organizations, and payers. The Action Coalitions with little or no experience in working with traditional media and using social media tools could collaborate with those that have undertaken successful communication activities in order to learn best practices. In this way, Action Coalitions could learn from one another about which activities have had an impact on driving the recommendations of The Future of Nursing in specific states, and what resources are needed to increase public awareness of the recommendations that have been difficult to achieve.
Discussion
As the Campaign itself acknowledged, and the present report recommends, further progress on the implementation of the recommendations of The Future of Nursing will require diversifying the movement and going beyond nursing to engage other diverse stakeholders. It will be important for the Campaign to reassess its external messaging to determine whether the messages are broad enough or tailored to engage important allies outside of nursing, or outside of the health professional community entirely. The Jonas Center for Nursing and Veterans Healthcare has noted its own challenges with recruiting other stakehold-
ers, such as philanthropic organizations, using messages that some considered to be focused too exclusively on the nursing profession (Curley, 2015). And the Jonas Center has revised Campaign messages to emphasize the goal of improving patient care and health care delivery.5 As observed by Darlene Curley, executive director, Jonas Center for Nursing and Veterans Healthcare, at the committee’s July 2015 workshop, “It has been difficult to develop funding partnerships with many of our external funders because they see the report as nursing-centric and very nursing professional focused, sort of inside baseball.”
Strong relationships are needed with health policy and business reporters; editors and columnists at national, state, and local news outlets; and bloggers who cover issues related to the recommendations of The Future of Nursing. These relationships could enable members and stakeholders of the Campaign to promulgate stories, particularly patient and human interest stories, proactively and to become a credible resource on articles relevant to the nursing profession. Media outreach efforts and communication materials could be tailored for different target audiences. To increase engagement of frontline nurses, for example, communications could articulate how recent changes in the health care system, the recommendations of The Future of Nursing, and Campaign activities could affect their work, and encourage their involvement by describing specific ways they could be involved in the Campaign.
Spokesperson training courses, such as those conducted by the American Association of Nurse Anesthetists for its state association leaders (AANA, 2014), could confer a variety of skills that would be useful to nurses. For example, courses could teach nurses how to successfully handle media interviews, lead and manage collaborative efforts with physicians and other members of the health care team, lobby for legislative changes, negotiate contracts, and resolve workplace conflicts. The Campaign’s development of these training courses could help nurses in their efforts to implement the recommendations of The Future of Nursing, as well as in their everyday practice. In regions that have had less success in advancing the IOM report’s recommendations, multifaceted advertising and communication efforts could be beneficial (TCC Group, 2014). These advertising campaigns could include strategic use of traditional and new media and advertising methodologies to increase public awareness and to generate support among policy makers and those with influence.
For internal communications, the Campaign has sought to disseminate concise and timely information through the use of weekly email updates and quarterly newsletters. Continuing to disseminate this type of targeted communication, as well as identifying additional recipients within organizations and Action Coalitions, would help ensure that such information could be disseminated further and more effectively to a broader, more diverse audience of stakeholders.
___________________
5 Personal communication, D. Curley, Jonas Center for Nursing and Veterans Healthcare, September 4, 2015.
Findings and Conclusions
Findings
This study yielded the following findings on communication strategies in support of collaboration:
Finding 5-9. The resources and ability to communicate effectively about their work vary among the Action Coalitions.
Finding 5-10. The Campaign’s communication strategy has targeted, for the most part, the nursing community.
Conclusions
The committee drew the following conclusions about the Campaign’s use of communication strategy and activities:
For the Campaign to progress further, its communication strategy needs to expand beyond the nursing profession to other diverse stakeholders, including consumers.
State Action Coalitions need assistance from the Campaign and from other successful Action Coalitions to develop messaging, utilize traditional and new media, and engage audiences.
Education in communication to enhance the skills of nursing spokespersons would help further collaborative efforts.
Recommendation 7: Expand Efforts and Opportunities for Interprofessional Collaboration and Leadership Development for Nurses. As the Campaign broadens its coalition (see Recommendation 1), it should expand its focus on supporting and promoting (1) interprofessional collaboration and opportunities for nurses to design, implement, and diffuse collaborative programs in care and delivery; and (2) interdisciplinary development programs that focus on leadership. Health care professionals from all disciplines should work together in the planning and implementation of strategies for improving health care, particularly in an interprofessional and collaborative environment. Interdisciplinary development programs and activities should:
- Feature content in leadership, management, entrepreneurship, innovation, and other skills that will enable nurses to help ensure that the public receives accessible and quality health care. Courses could be offered through or in partnership with other professional schools. The Campaign should monitor nursing programs that offer these types of courses and programs and track nurses’ participation, if possible, in order to assess progress.
- Include interprofessional and collaborative development or continuing competence in leadership skills—for example, through the participation of nurses in spokesperson and communication programs designed to teach persuasive communication skills that will facilitate their leading and managing collaborative efforts.
Recommendation 8: Promote the Involvement of Nurses in the Redesign of Care Delivery and Payment Systems. The Campaign should work with payers, health care organizations, providers, employers, and regulators to involve nurses in the redesign of care delivery and payment systems. To this end, the Campaign should encourage nurses to serve in executive and leadership positions in government, for-profit and nonprofit organizations, health care delivery systems (e.g., as hospital chief executive officers or chief operations officers), and advisory committees. The Campaign should expand its metrics to measure the progress of nurses in these areas. Types of organizations targeted by this recommendation could include
- health care systems;
- insurance companies and for-profit health care delivery systems (e.g., Minute Clinic);
- not-for-profit organizations that work to improve health care (e.g., the National Quality Forum);
- the National Academy of Medicine and other professional membership groups; and
- federal, state, and local governmental bodies related to health (e.g., the Veterans Health Administration, U.S. Department of Defense, Centers for Medicare & Medicaid Services).
Recommendation 9: Communicate with a Wider and More Diverse Audience to Gain Broad Support for Campaign Objectives. The Campaign should expand the scope of its communication strategies to connect with a broader, more diverse, consumer-oriented audience and galvanize support at the grassroots level. The Campaign, including its state Action Coalitions, should bolster communication efforts geared toward the general public and consumers using messages that go beyond nursing and focus on improving health and health care for consumers and their
families. The Campaign should recruit more allies in the health care community (such as physicians, pharmacists, and other professionals, as well as those outside of health care, such as business leaders, employers, and policy makers) as health care stakeholders to further demonstrate a collaborative approach in advancing the recommendations of The Future of Nursing.
AACN (American Association of Colleges of Nursing). 2006. The essentials of doctoral education for advanced nursing practice. Washington, DC: AACN.
AACN. 2008. The essentials of master’s education in nursing. Washington, DC: AACN.
AACN. 2011. The essentials of baccalaureate education for professional nursing practice. Washington, DC: AACN.
AACN. 2015a. AACN-Wharton Executive Leadership Program. http://www.aacn.nche.edu/leadinginitiatives/aacn-wharton-executive-leadership-program (accessed September 11, 2015).
AACN. 2015b. AACN/Wharton Executive Leadership Program, August 10-13, 2015, Philadelphia, PA. http://www.aacn.nche.edu/leading-initiatives/2015-Wharton-Brochure.pdf (accessed September 11, 2015).
AAMC (Association of American Medical Colleges). 2012. Changing delivery system increases focus on interprofessional education. https://www.aamc.org/newsroom/reporter/sept2012/303656/ipe.html (accessed September 10, 2015).
AAMC. 2014. Lifelong learning initiative: Call for interprofessional in quality improvement and patient safety curriculum. https://www.staging.mededportal.org/icollaborative/about/initiatives/lifelonglearningcall (accessed September 11, 2015).
AAMC. 2015. MedEdPORTAL: Ten years strong. https://www.mededportal.org/about/10 (accessed September 10, 2015).
AAN (American Academy of Nursing). 2014. American Academy of Nursing Jonas Policy Scholars Program. http://www.aannet.org/academy-jonas-policy-scholars (accessed September 11, 2015).
AANA (American Association of Nurse Anesthetists). 2014. Spokesperson training for state association leaders. www.aana.com/meetings/aanaworkshops/Documents/SpokespersonTrainingforStateAssociationLeaders.pdf (accessed September 17, 2015).
AHA (American Hospital Association). 2014. 2014 National Health Care Governance Survey report. Chicago, IL: AHA Center for Healthcare Governance.
ANCC (American Nurses Credentialing Center). 2015. Magnet initial designation, organization eligibility requirements. http://www.nursecredentialing.org/OrgEligibilityRequirements (accessed August 4, 2015).
AONE (American Organization of Nurse Executives). 2015. Managing health care delivery. http://www.aone.org/education/hbs.shtml (accessed September 11, 2015).
Arizona State University. 2015. Interprofessional fellowship in innovative health leadership. https://nursingandhealth.asu.edu/non-degree/continuing-education/innovative-health-leadership (accessed September 11, 2015).
Bodenheimer, T., E. H. Wagner, and K. Grumbach. 2002. Improving primary care for patients with chronic illness: The chronic care model, part 2. Journal of the American Medical Association 288(15):1909-1914.
CCNA (Center to Champion Nursing in America). 2014a (unpublished). Future of Nursing: Campaign for Action biannual operations report, February 1, 2014-July 31, 2014. Washington, DC: CCNA.
CCNA. 2014b (unpublished). Future of Nursing: Campaign for Action presentation, December 19, 2014. Washington, DC: CCNA.
CCNA. 2014c (unpublished). National nursing leadership strategy meeting concept paper: A national strategy to increase the number of nurse leaders on boards, part II. Washington, DC: CCNA.
CCNA. 2014d (unpublished). National nursing leadership strategy meeting concept paper: One voice for nursing leadership: A national strategy meeting. Washington, DC: CCNA.
CCNA. 2015a (unpublished). CCNA 2014 workplan deliverables, November 2014-May 2015. Washington, DC: CCNA.
CCNA. 2015b. Culture of health: Breakthrough leaders in nursing. http://campaignforaction.org/breakthrough2015 (accessed September 11, 2015).
CCNA. 2015c (unpublished). Evaluation of the impact of the Institute of Medicine report “The Future of Nursing: Leading Change, Advancing Health” communications report, July 20, 2015. Washington, DC: CCNA.
CCNA. 2015d (unpublished). Future of Nursing: Campaign for Action biannual operations report, August 1, 2014-May 31, 2015. Washington, DC: CCNA.
CCNA. 2015e. Future of Nursing: Campaign for Action dashboard indicators. http://campaignforaction.org/dashboard (accessed October 29, 2015).
CCNA. 2015f. National coalition launches effort to place 10,000 nurses on governing boards by 2020. http://campaignforaction.org/news/national-coalition-launches-effort-place-10000-nurses-governing-boards-2020 (accessed September 12, 2015).
CCNA. n.d. Campaign progress. http://campaignforaction.org/campaign-progress (accessed September 23, 2015).
CCNE (Commission on Collegiate Nursing Education). 2013. Standards for accreditation of baccalaureate and graduate nursing programs. Washington, DC: CCNE.
CCNE. 2014. New health professions accreditors collaborative forms to stimulate interprofessional engagement. Washington, DC: CCNE. http://www.aacn.nche.edu/ccne-accreditation/HPACForms-Engagement.pdf (accessed November 20, 2015).
CHC (Community Health Center, Inc.). 2015. About us. http://chc1.com/About/AboutUS.html (accessed September 11, 2015).
Cipriano, P. 2015. Presentation to IOM Committee for Assessing Progress on Implementing the Recommendations of the Institute of Medicine Report The Future of Nursing: Leading Change, Advancing Health. Washington, DC, May 28, 2015.
CMS (Centers for Medicare & Medicaid Services). 2013. Health care innovation awards round one project profiles. http://innovation.cms.gov/files/x/hcia-project-profiles.pdf (accessed September 11, 2015).
CMS. 2015. Health care innovation awards. http://innovation.cms.gov/initiatives/Health-Care-Innovation-Awards (accessed September 11, 2015).
Curley, D. 2015. Presentation to IOM Committee for Assessing Progress on Implementing the Recommendations of the Institute of Medicine Report The Future of Nursing: Leading Change, Advancing Health. Washington, DC, July 27, 2015.
Feldman, L. S., L. L. Costa, E. R. Feroli, T. Nelson, S. S. Poe, K. D. Frick, L. E. Efird, and R. G. Miller. 2012. Nurse-pharmacist collaboration on medication reconciliation prevents potential harm. Journal of Hospital Medicine 7(5):396-401.
Frenk, J., L. Chen, Z. A. Bhutta, J. Cohen, N. Crisp, T. Evans, H. Fineberg, P. Garcia, Y. Ke, P. Kelley, B. Kistnasamy, A. Meleis, D. Naylor, A. Pablos-Mendez, S. Reddy, S. Scrimshaw, J. Sepulveda, D. Serwadda, and H. Zurayk. 2010. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 376(9756):1923-1958.
Gallup. 2010. Nursing leadership from bedside to boardroom: Opinion leaders’ perceptions. http://www.rwjf.org/content/dam/web-assets/2010/01/nursing-leadership-from-bedside-to-boardroom (accessed September 10, 2015).
Gallup. 2015. Honesty/ethics in professions. http://www.gallup.com/poll/1654/honesty-ethicsprofessions.aspx (accessed September 10, 2015).
Gilmartin, M. J. 2013. Principles and practices of social entrepreneurship for nursing. Journal of Nursing Education 52(11):641-644.
Grumbach, K., and T. Bodenheimer. 2004. Can health care teams improve primary care practice? Journal of the American Medical Association 291(10):1246-1251.
Harvard Business School. 2015. Managing health care delivery. http://www.exed.hbs.edu/programs/mhcd/pages/default.aspx (accessed September 11, 2015).
HRSA (Health Resources and Services Administration). 2014. HRSA-14-070 Nurse Education, Practice, Quality and Retention (NEPQR) program—interprofessional collaborative practice. http://www.grants.gov/view-opportunity.html?oppId=248734 (accessed September 11, 2015).
Hudson, C. E., M. K. Sanders, and C. Pepper. 2013. Interprofessional education and prelicensure baccalaureate nursing students. Nurse Educator 38(2):76-80.
IOM (Institute of Medicine). 2003. Health professions education: A bridge to quality. Washington, DC: The National Academies Press.
IOM. 2011. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press.
IOM. 2013. Interprofessional education for collaboration: Learning how to improve health from interprofessional models across the continuum of education to practice: Workshop summary. Washington, DC: The National Academies Press.
IPEC (Interprofessional Education Collaborative). 2011. Core competencies for interprofessional collaborative practice: Report of an expert panel. Washington, DC: IPEC.
IPEC. 2015. About IPEC. https://ipecollaborative.org/About_IPEC.html (accessed September 11, 2015).
Jonas Center (Jonas Center for Nursing and Veterans Healthcare). 2015a. American Academy of Nursing announces second cohort of students in program connecting nurse leaders with emerging scholars. http://www.jonascenter.org/news/post/american-academy-of-nursing-announces-second-cohort-of-students-in-program-connecting-nurse-leaders-with-emerging-scholars (accessed September 11, 2015).
Jonas Center. 2015b. Jonas Nurse Leaders Scholars. http://www.jonascenter.org/program-areas/jonas-nurse-leaders-scholars (accessed September 11, 2015).
Jonas Center. 2015c. Leadership grantees. http://www.jonascenter.org/program-areas/leadership/grantees (accessed September 11, 2015).
Josiah Macy Jr. Foundation. 2012. Conference on interprofessional education, April 1-3, 2012. New York: Josiah Macy Jr. Foundation.
Josiah Macy Jr. Foundation. 2013a. Macy Faculty Scholars. http://macyfoundation.org/macy-scholars (accessed September 11, 2015).
Josiah Macy Jr. Foundation. 2013b. Transforming patient care: Aligning interprofessional education with clinical practice redesign. New York: Josiah Macy Jr. Foundation.
Leape, L., D. Berwick, C. Clancy, J. Conway, P. Gluck, J. Guest, D. Lawrence, J. Morath, D. O’Leary, P. O’Neill, D. Pinakiewicz, and T. Isaac. 2009. Transforming healthcare: A safety imperative. Quality and Safety in Health Care 18(6):424-428.
Marsteller, J. A., J. B. Sexton, Y. J. Hsu, C. J. Hsiao, C. G. Holzmueller, P. J. Pronovost, and D. A. Thompson. 2012. A multicenter, phased, cluster-randomized controlled trial to reduce central line-associated bloodstream infections in intensive care units. Critical Care Medicine 40(11):2933-2939.
NCIPE (National Center for Interprofessional Practice and Education). 2013a. About us. https://nexusipe.org/about (accessed September 11, 2015).
NCIPE. 2013b. Funding. https://nexusipe.org/funding (accessed September 11, 2015).
NCIPE. 2013c. Vision and goals. https://nexusipe.org/vision (accessed September 11, 2015).
Needleman, J., and S. Hassmiller. 2009. The role of nurses in improving hospital quality and efficiency: Real-world results. Health Affairs 28(4):w625-w633.
Pilon, B. A., C. Ketel, and H. Davidson. 2015a. Evidence-based development in nurse-led interprofessional teams. Nursing Management 22(3):35-40.
Pilon, B. A., C. Ketel, H. A. Davidson, C. K. Gentry, T. D. Crutcher, A. W. Scott, R. M. Moore, and S. T. Rosenbloom. 2015b. Evidence-guided integration of interprofessional collaborative practice into nurse managed health centers. Journal of Professional Nursing 31(4):340-350.
TCC Group. 2013 (unpublished). Future of Nursing: Campaign for Action: Action Coalition Survey. Philadelphia, PA: TCC Group.
TCC Group. 2014 (unpublished). Robert Wood Johnson Foundation Future of Nursing Campaign imperative analysis. Philadelphia, PA: TCC Group.
Thibault, G. E. 2011. Interprofessional education: An essential strategy to accomplish The Future of Nursing goals. Journal of Nursing Education 50(6):313-317.
University of Pennsylvania. 2015a. Dual degree in nursing and Wharton. https://hcmg.wharton.upenn.edu/programs/undergraduate/program-information/dual-degree-nursing-wharton (accessed October 29, 2015).
University of Pennsylvania. 2015b. Wharton Nursing Leaders Program. http://executiveeducation.wharton.upenn.edu/for-individuals/all-programs/wharton-nursing-leaders-program (accessed October 29, 2015).
Wagner, E. H. 2000. The role of patient care teams in chronic disease management. British Medical Journal 320(7234):569-572.
WHO (World Health Organization). 2010. Framework for action on interprofessional education and collaborative practice. Geneva, Switzerland: WHO.
Zorek, J., and C. Raehl. 2012. Interprofessional education accreditation standards in the USA: A comparative analysis. Journal of Interprofessional Care 27(2):123-130.


























