3
Home and Community Settings: Services and Supports for Community Living and Participation
Living in the setting of one’s choosing and being a full participant in one’s community is a priority for many people. The workshop’s first panel, which addressed the issues involved in providing services and supports for community living and participation, featured presentations from four speakers. The speakers gave an overview of the population needing long-term services and supports, discussed the state of Minnesota’s efforts to reduce reliance on institutional care among older adults and those with disabilities, described current policies designed to support community living and participation, and provided the perspective of the Centers for Medicare & Medicaid Services (CMS) on community services and supports.
OVERVIEW OF THE POPULATION NEEDING LONG-TERM SERVICES AND SUPPORTS
H. Stephen Kaye
Professor, University of California, San Francisco
Approximately 11 million Americans who need long-term services and supports (LTSS) live in the community, said Stephen Kaye of the University of California, San Francisco. The needs of those living in the community vary widely. Approximately one-third of the LTSS population living in the community need help with one activity of daily living (ADL), which can affect their ability to get out of their home to engage in commu-
nity activities. Less than 10 percent of these individuals have paid help, but almost all of them have some type of unpaid help, Kaye said. At the other end of the spectrum, nearly 10 percent of the LTSS population living in the community requires assistance with all or nearly all of their ADLs and instrumental ADLs (IADLs). Only about 22 percent of these individuals have some form of paid help, although nearly all have unpaid help. This is despite the fact that many of them are relatively poor and might qualify to receive paid help through Medicaid home- and community-based services (HCBS).
Across the age spectrum, the vast majority of adults needing LTSS are limited in physical functioning. Back and spine problems are a leading cause of physical limitations among adults of all ages, and arthritis and heart conditions are also common among those 50 years of age or older, Kaye said. Aside from the high prevalence of physical limitations, many LTSS users have cognitive limitations, mental health disabilities, or both. Such mental health disabilities are most prevalent in younger LTSS users—affecting nearly half of adult LTSS users under age 50—but the percentage of LTSS users with mental health disabilities gradually declines with increasing age. Similarly, cognitive limitations are most prevalent among younger LTSS users—nearly half of LTSS users under 50 are affected, mostly by intellectual and developmental disabilities. LTSS users between the ages of 50 and 79 are less likely to have cognitive or mental health limitations, but the likelihood of having such limitations increases again among those 80 years of age or older, when dementia becomes more prevalent, Kaye said.
Because many people with LTSS needs have more than one type of limitation, pigeonholing people into particular programs according to the type of disability they have might not meet their service needs. Among working-age adults, there are more people who have some combination of physical, cognitive, and mental health limitations than who have only one type of limitation, Kaye said (see Figure 3-1). Among older adults, the most common limitation is physical alone, but few people with either a cognitive or a mental health limitation are completely free of physical limitations.
In contrast to the tremendous complexity in the spectrum of disabilities affecting those who need LTSS, the current system used to deliver services narrowly categorizes people by primary disability, which Kaye said is not an effective method for providing services. The Medicaid HCBS waivers for providing intensive services are broken down into hundreds of programs for specific high-need groups based on age, physical disability, mental health, cognitive limitations, and other classifications. Fortunately, Kaye noted, Medicaid is moving in the direction of delivering services through more integrated programs.
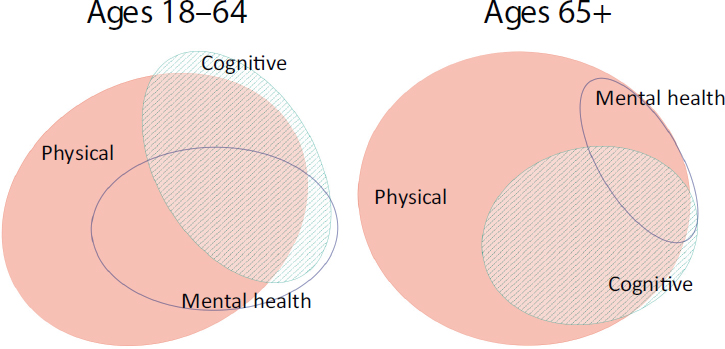
SOURCE: Kaye, 2015. Reprinted with permission from H. Stephen Kaye.
The majority of LTSS users report that their health is either fair or poor, though somewhat surprisingly, within this population health status is best among the oldest adults and worst among adults ages 50–64. One possible explanation for this may be the finding that the percentage of adults experiencing frequent pain or fatigue follows a similar pattern as overall health status in that the oldest adults report the least pain and fatigue while adults ages 50–64 report the most pain and fatigue.
Kaye said that social participation is “shockingly low” among the LTSS population, and not just among the oldest adults. Some 30 to 40 percent of LTSS users do not go out and socialize, and 50 percent or more do not participate in leisure or social activities. Furthermore, economic participation in terms of employment is even lower. Within this population, the vast majority of working-age adults are not working, and they are not looking for work. People with disabilities can lack opportunity, Kaye said, but most working-age adults report that their disability keeps them from working. “They think of themselves as being prevented from working,” Kaye said. Although many people would assert that everybody with a disability can work if given the appropriate accommodations, that may not be the case given the number of working age adults who report experiencing pain and fatigue. Kaye noted, too, that people who are not working tend to live in poverty. This is especially true for young adults; older adults who acquire a disability later in life may have had time to accumulate some financial resources first.
In conclusion, Kaye noted that there are false dichotomies and misunderstandings in the fields of disabilities and LTSS. One false dichotomy is between older adults with disabilities and those who are younger with disabilities: “Other than age, which is, as people say, just a number, there is no clear demarcation between older and younger LTSS users,” he said. “They are not really that different from each other.” One misunderstanding is to separate the social and medical models of care: High levels of reported pain, fatigue, and poor health—all medical conditions—among LTSS users are barriers to social and economic participation. Another misunderstanding, he said, is that because so many LTSS users are poor, especially younger adults, designing programs such that individuals must pay for services may not be an appropriate solution.
Kaye stressed that people who need LTSS do not fit into boxes, yet government programs often try to do just that. “Whatever stereotypes you have,” he said, “they are usually wrong. People are much more complicated and different from the vision we have of them.”
REDUCING RELIANCE ON INSTITUTIONAL CARE
Loren Colman
Assistant Commissioner of Continuing Care,
Minnesota Department of Human Services
The state of Minnesota has developed and implemented several programs and initiatives to achieve a balance between long-term community-based services and institutions, said Loren Colman of the Minnesota Department of Human Services. In fact, AARP and the Humphrey School of Public Affairs at the University of Minnesota have recognized Minnesota for its successful programs in LTSS.
Colman began by discussing Minnesota’s Return to Community initiative.1 The unique feature of this program, he explained, is that it targets private paying individuals living in nursing homes and assisted-living facilities. The program entails contacting these individuals, determining why they continued to live in nursing homes, and then providing them with the appropriate services, such as a community living specialist, and helping them move back into their homes if they would like to do so. Colman showed a video that explained this program in more detail.2 The
___________________
1 For more information, see www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVERSION&RevisionSelectionMethod=LatestReleased&dDocName=dhs16_148973 (accessed January 28, 2016).
2 Video can be found at: http://iom.nationalacademies.org/~/media/Files/Activity%20Files/Aging/AgingForum/2015%20OCT%2006/Presentations/Colman%20Presentation.pdf (accessed February 26, 2016).
program has resulted in not only better quality of life for these individuals but also savings for both the state government and the individuals by delaying moves into institutions, which can be very costly to both private and public resources. In any given year, the majority of the participants in the Return to Community program successfully remain at home if they so choose. This is somewhat ironic, Colman said, because at the same time that Minnesota is trying to expand Medicaid through the Patient Protection and Affordable Care Act (ACA) provisions, one goal of this and other programs in the state is to help individuals retain their resources and thus keep them from having to enroll in Medicaid.
Several other programs administered by the State of Minnesota reduce reliance on institutional care, Colman said. For example, the state has information and assistance systems, called linkage lines, for older adults,3 people with disabilities,4 and veterans.5 In addition, Minnesota requires a long-term care consultation for anyone considering moving into an assisted-living facility, regardless of whether the individual would be using a public or private source of payment. The state has found that for many individuals, this consultation has delayed movement into a facility. Furthermore, if and when individuals choose to move into assisted-living facilities, they are better and smarter purchasers, Colman said.
Housing Access Services6 is another program which, in partnership with The Arc,7 helps individuals with disabilities move out of their parents’ homes to create a life of their own. The state also has instituted a program called Essential Community Supports8 to help people with very low needs live in the community.
The MnCHOICES9 program employs a Web-based assessment process for participants in all of the state’s public LTSS programs. This tool identifies an individual’s needs and gathers information about that individual’s goals, desires, and informal supports. “It has not been an easy task to bring aging, disability, mental health—all of the various populations—
___________________
3 Senior LinkAge Line®: www.mnaging.org/advisor/SLL.htm (accessed January 22, 2016).
4 Disability Linkage Line®: www.mcil-mn.org/programs/disability-linkage-line (accessed January 22, 2016).
5 LinkVet: linkvet.custhelp.com (accessed January 22, 2016).
6 For more information, see http://www.thearcofminnesota.org/housing-access (accessed January 29, 2016).
7 The Arc is a community-based organization that advocates for and serves people with intellectual and developmental disabilities. For more information, see www.thearc.org (accessed January 22, 2016).
8 For more information, see http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVERSION&RevisionSelectionMethod=LatestReleased&dDocName=dhs16_148023 (accessed January 29, 2016).
9 For more information, see http://mn.gov/dhs/partners-and-providers/continuingcare/reform-initiatives/mnchoices (accessed January 29, 2016).
together to agree on one tool,” Colman said, “but we have done so and it has been implemented . . . [and] the lead agency assessors are using it.”
Working with the long-term care industry, Minnesota has been downsizing institutions and improving care. In the 1980s, Colman said, Minnesota had the highest number of nursing-home beds per capita in the United States. Since then, the state has paid facilities to downsize their numbers of beds and create private rooms. The process, which has been voluntary, has resulted in thousands of fewer beds in facilities.
Minnesota has also published a report card of quality in nursing facilities. This has proven to be effective at improving the quality of care at nursing facilities. The state is also preparing to introduce a report card for HCBS, which, Colman said, has been far more complicated. The goal is to provide a Web-based, Yelp-type review tool that gives people the opportunity to express their opinions about the services they receive. Minnesota has also strengthened its adult protective services by launching the Minnesota Adult Abuse Reporting Center,10 where the public can report suspected maltreatment of vulnerable adults using either a single state-wide toll free number or online reporting. This center replaces the more than 100 phone numbers that were formerly used to report abuse. Even before a public awareness campaign about this new system was launched, reports of abuse increased 160 percent, Colman said.
Another valuable program Minnesota has initiated to challenge providers to identify, develop, and implement new approaches to services is its state-funded Live Well at Home Grants program.11 This program integrates new technologies to improve home safety, create dementia-friendly communities, and take other actions to support people who remain in their homes and communities.
In summary, Minnesota has used a multi-pronged approach to reduce reliance on living in institutions, and this has contributed to the state’s increase in the numbers of people with disabilities and older adults living in the community.
___________________
10 For more information, see http://www.mn.gov/dhs/people-we-serve/adults/services/adult-protection/index.jsp (accessed January 29, 2016).
11 For more information, see http://mn.gov/dhs/partners-and-providers/continuingcare/grants-rfps/live-well (accessed January 29, 2016).
POLICIES TO SUPPORT COMMUNITY LIVING AND PARTICIPATION
Henry Claypool
Claypool Consulting
Henry Claypool of Claypool Consulting focused his remarks on how to address some of the significant issues that people are living with today. He discussed four suggestions that could be implemented in the near term: building on Medicaid LTSS provisions in the ACA; improving integrated care; increasing workforce participation; and bridging technology with social services and end users.
Medicaid Provisions for LTSS
Medicaid LTSS provisions in the ACA have triggered good work in the individual states, but some of the approaches need refining, Claypool said. There are multiple options and waivers that can be taken advantage of to make LTSS available in a given state, but this may not be possible in states with limited resources or staff. Some of these provisions could be streamlined and consolidated in order to bring them together under a single state plan authority, and then additional financing incentives could be created, he said. One such provision is Medicaid’s Balancing Incentive Program,12 which offers each state the opportunity to build a comprehensive plan for expanding access to HCBS and establish the tools to control how people get into nursing homes and institutional settings.
Integrated Care
Another aspect of the ACA that has gotten quite a bit of attention, and which Claypool said is consistent with delivery system reform, is the concept of integrated care. Although the medical community is interested in making care more integrated, Claypool cautioned that many clinicians have little understanding of how LTSS works in the community setting. Most health care professionals, he explained, are used to the static, controlled environment of the clinical setting, but the community environment is extraordinarily dynamic. There, environmental factors that are not in the control of clinicians drive people’s behaviors and affect their ability to do what is in their own medical best interest. What is needed, Claypool said, is to bridge the clinical- and community-based knowledge
___________________
12 For more information, see https://www.medicaid.gov/Medicaid-CHIP-ProgramInformation/By-Topics/Long-Term-Services-and-Supports/Balancing/Balancing-IncentiveProgram.html (accessed January 29, 2016).
and efforts to help medical professionals better understand what is in the community.
Integrated care, Claypool said, needs “a much more acute focus on getting payment systems right, making sure that reimbursement is there for the medical services that are provided to an individual that is classified as high needs [and] high cost. If we can do that, there will be reimbursement for community-based or follow-along services.” One impediment to getting payment systems right, Claypool added, is the lack of a robust dataset on the needs of this population. Policy making directed at changing payment systems will be driven by where there is an evidence base to support moving models to scale, Claypool predicted. He noted that Medicare reimburses physicians for time spent emailing with patients, and some private payers provide a similar benefit.
Workforce Participation
Work has become a focus for the intellectual and developmental disabilities community, particularly with regard to helping younger people with disabilities engage in work. Claypool referred to the data Kaye presented on the low level of workforce participation among young adults with disabilities and said there needs to be a concerted effort to remedy that situation through targeted supports that will enable those with disabilities who have work capacity to engage in that capacity. He said that this is critically important for improving both health outcomes and the quality of life for these individuals.
For older adults with disabilities, chronic conditions can make it difficult to stay engaged in the workforce. He suggested that, because of the stigma associated with disabilities, it may be preferable to talk about people working with “chronic conditions.” He said that policies need to be more strategic about how to support older individuals with disabling chronic conditions, and he proposed that paying for targeted training and retraining programs should be an option that policy makers consider. Not helping individuals maintain their earnings could not only present challenges to quality-of-life and health outcomes, but it could also have implications for the viability of the U.S. Social Security system.
Technology
The final point Claypool raised was the need to engage the technology community in order to ensure that the products and services it is developing truly meet the preferences of the aging adults and people with disabilities who will use them. He recounted his recent experience consulting with technology companies, during which he noticed that
they talk primarily among themselves and do not engage the potential end users. Technologies could revolutionize how people age in place or how people with disabilities get to work. Claypool wondered aloud what would happen if, for example, community-based meals programs were connected to companies like Uber to coordinate meal deliveries. Public–private partnerships could revolutionize the missions of community-based social services.
From a policy perspective, the use of technology in this context will raise questions about how to ensure data privacy and security. When people use smart phones, they generate tremendous amounts of data, which phone companies can collect. How that information is used can be a sensitive issue. Claypool suggested that individuals isolated in their homes might be much more willing to share information about their needs if there is a return on that investment, such as better coordinated services, more timely support, or higher-quality support. However, he added, it will be important to go “through a process of really engaging people and learning about what their preferences are for this data sharing.”
THE CENTERS FOR MEDICARE & MEDICAID SERVICES PERSPECTIVE
Shari Ling
Deputy Chief Medical Officer, Centers for Medicare & Medicaid Services
Delivery system reform is upon us, said Shari Ling of CMS, and although that can be daunting, it can also be a time ripe with opportunities that can lead to actionable next steps, including the opportunity to knit together the care delivery system in a way that is truly person-centered. She added that having a focus on quality will be key because quality has a tremendous impact on value across medical services, health care services, and HCBS.
To provide context for her remarks, Ling reminded the audience that CMS touches the lives of approximately one in three Americans. She added that the population of Americans that CMS serves is becoming increasingly complex, both in terms of their functional limitations and in terms of the number and types of conditions they have. One such group of people is those with cognitive impairments or behavioral health concerns. Ling said that a big part of care delivery reform will be to break down the barriers between the medical system and the community-based care that sits outside of the walls of traditional health care institutions so that people can live successfully and happily at home.
The silos dominating the current fee-for-service care delivery system are dissolving, she said, and there are goals to move toward a system that
is better coordinated, makes better use of home- and community-based systems and services, and is of better quality and higher value. She noted that there are many value-based purchasing programs on the horizon, in play, or rapidly evolving, and that these new programs will improve care, produce healthier populations, and result in smarter spending. This delivery system reform moves away from individually siloed service sessions and toward care delivery as part of a group, a community, and a system. The Secretary of Health and Human Services has stated goals of moving from fee-for-service to alternative payment models. Specifically, one goal for the Medicare program is for 30 percent of payments by the end of 2016, and 50 percent of payments by the end of 2018, to be delivered through alternative payment models. Ling said that although this goal focuses on clinical care, it is not specific to hospitals but instead applies to care provided across all settings, from institution to personal services at home. A second goal is for 85 percent of Medicare fee-for-service payments to be tied to quality or value by the end of 2016.
CMS’s Quality Strategy for quality fits with the priorities of the National Quality Strategy, Ling said. This focus on quality aligns all measurement efforts across every health care setting and also informs the direction of HCBS quality assessment. The priorities include providing person-centered care across all settings, providing care that is well coordinated, and including individuals in determining their own care and engaging them as full partners in developing their care plans. There are performance measure gaps in HCBS, but gaps in evidence can become research opportunities. “If we keep focus on what quality looks like and how to align those efforts across the span of health care, health services, community care, [and] home- and community-based services,” Ling said, “I think we can take some meaningful next steps.”
The Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014 provided CMS with the authority to standardize data elements across certain post-acute care settings in important areas where it had not had the authority previously, including the evaluation and assessment of function, self-care activities, mobility activities, and cognition. While developing such standardized data elements is challenging, Ling said, it offers the opportunity to be able to systematically inform, describe, and define in a standardized manner what people need at various points when transitioning from one care setting to another. The goal is to enable integrated service delivery across all settings and optimally align what those who receive these services actually need in a person-centered manner.
She also mentioned that in the innovation space, CMS has authority through the Center for Medicare & Medicaid Innovation to test new care and payment models. Examples include primary care transforma-
tion initiatives and bundled payment efforts. Although they are intended to transform clinical practice, these efforts can have effects beyond the services that are provided in clinical office settings as care coordination begins to link more closely to community-based services. There are also new billing codes that encourage clinicians to have conversations with their patients to develop individualized and person-centered goals of care. Other projects aim to develop chronic-care payment models and embrace the notion that the population CMS serves is becoming more complex and thus new solutions are needed to help address care needs in new ways.
Speaking about technical assistance, Ling highlighted the Transforming Clinical Practice Initiative, which will support clinicians in their practice to go beyond the traditional medical model to improve broader health outcomes for beneficiaries and reduce unneeded care and unnecessary hospitalizations. This transformation effort includes helping clinicians work with their patients to better coordinate care, and it facilitates links to community care to achieve outcomes that are important to each individual. This initiative is distinct from, but equally important to, payment model reform discussions that are supported by the Health Care Payment Learning and Action Network.
CMS has also issued additional rules for HCBS that address person-centered planning and home- and community-based settings. CMS has proposed a long-term care rule that modernizes and highlights the importance of quality care needed by the people in institutional facilities such as nursing homes. Ling noted that the area of employment and housing is also important to these discussions.
Ling concluded her talk by emphasizing the iterative cycle of engaging individuals and their families in their care at every opportunity, focusing on what the goals of care are, and articulating those goals and reassessing them in every engagement between the person receiving care and each provider. She noted that CMS has an “affinity group” dedicated to addressing individual and family engagement and integrating it into CMS policies. The iterative cycle, she said, represents an opportunity to extract meaning from every exchange between clinical and other providers and the individual who is receiving care.
DISCUSSION
An open discussion followed the panel’s presentations. Workshop participants were able to ask questions of and offer comments to the speakers. The following section summarizes the discussion.
Anne Montgomery of the Altarum Institute asked the panel speakers if they could envision an LTSS report card that evaluated different
service providers, such as nursing homes and Program of All-Inclusive Care for the Elderly13 plans, as a function of geographic region in order to better inform consumers about the choices available to them. Colman replied that developing Minnesota’s HCBS report card has been more challenging than anticipated and that his office has had to narrow the focus of its work to a limited number of services because there are so many different services that individuals can be using at any given time. He acknowledged that there would be value to taking a regional approach because families supporting the individuals making choices can be spread out across a broad geographical area rather than in one specific community, but so far his group has focused only within Minnesota.
Kaye said that he and Claypool were at a meeting to discuss a state-by-state LTSS scorecard that AARP, The SCAN Foundation, and The Commonwealth Fund are designing. The meeting participants found it challenging that information is often available only at the local or metropolitan area level and not at the state level. Claypool added that state-level scorecards could help address the fact that there are real disparities in how different states respond to similar needs, meaning that the same person could be served very differently by two state Medicaid programs simply because of where that person lives. “We need to be able to draw stronger comparisons between the states and make better arguments about why it is not okay that somebody living in one part of the country would receive [a different] quality of care or a lack of support . . . if they moved across the country,” Claypool said. Medicaid expansion may help with this. A scorecard that more accurately compares state Medicaid programs could create avenues for providing lower performing states with financial incentives to improve their programs, he added. Ling cautioned that there is an inherent assumption that the measures in reporting programs are comparing like with like. Ling said that the ideal scorecard would allow individuals to integrate their priorities, such as quality, geographic location, and care setting, into their searches for information so that they could make choices based on their goals. “That would be tremendous,” Ling said. “If we need to dream, dream big.”
___________________
13 For more information, see https://www.medicaid.gov/medicaid-chip-programinformation/by-topics/long-term-services-and-supports/integrating-care/program-of-allinclusive-care-for-the-elderly-pace/program-of-all-inclusive-care-for-the-elderly-pace.html (accessed January 29, 2016).
FACILITATED TABLE DISCUSSIONS
Three questions were posed to the workshop participants for short facilitated table discussions (answers were not limited to what was covered in panel presentations):
- What are the two or three biggest policy barriers to supporting community living and participation?
- What should be the top three research and policy priorities to support community living and participation?
- What best practices have been identified?
The reports from the table discussions were delivered by the following individuals, listed alphabetically: Margaret Campbell, National Institute on Disability, Independent Living, and Rehabilitation Research; Susan Chapman, University of California, San Francisco; Patricia D’Antonio, The Gerontological Society of America; Teresa Lee, Alliance for Home Health Quality and Innovation; Rasheda Parks, National Institute on Aging; Julianna Rava, National Institutes of Health Office of Autism Research; and Rebecca Sheffield, American Foundation for the Blind.
Policy Barriers
The facilitated table discussions produced the following list of policy barriers to supporting community living and participation, as noted by the table rapporteurs.
Disconnects, Fragmentation, and Lack of Integration Across Systems
- A disconnect between federal financing and delivery system programs, including confusion about which federal agencies have authority over integration (Campbell)
- A lack of integration of long-term care policies and settings, medical and clinical care policies and settings, and transportation and housing policies, all of which negatively affects person-centered care and the ability to live in the community (Chapman, D’Antonio, Lee, Sheffield)
- Poor communication and cultural barriers among aging services, disability services, and mental and behavioral health services, which create serious service gaps for those needing LTSS (Lee)
- Fragmentation of the financial systems supporting community-based services (D’Antonio, Parks)
- Electronic and personal health records that are not interoperable and lack the means to integrate LTSS data (Campbell)
Quality
- A lack of measures for assessing quality in HCBS and long-term care and for measuring outcomes that demonstrate value and efficacy (Campbell)
- Insufficient tools for giving guidance to providers on how to be successful at delivering quality care and LTSS under new payment models (Lee)
Financing
- Low reimbursement rates and a lack of data to justify reimbursement rates (Parks)
- A lack of understanding and clarity on the financial value of programs enabling community living, both in terms of saving taxpayer dollars for programs such as Medicare and Medicaid, and in terms of saving personal funds, a better understanding of which may provide the impetus for policy change (Lee)
- Competition for diminished funding for LTSS at a time when need is increasing and there is no sustainable plan for paying for LTSS (D’Antonio, Lee)
Additional Barriers
- A lack of data on outcomes needed to better understand workforce training needs (D’Antonio, Parks)
- Limited availability of accessible and affordable community living and LTSS options (Chapman, Rava)
- A lack of political will to address and tackle LTSS (Chapman)
- A lack of attention to the accessibility and usability of health information technology needed to enable person-centered delivery of services (Campbell)
Research and Policy Priorities
The facilitated table discussions produced the following list of research and policy priorities to support community living and participation, as noted by the table rapporteurs.
Areas for Additional Research
- Integrate data across the age span to understand life course outcomes (Parks, Rava)
- Collect data on workforce initiatives, HCBS quality, and technology applications (D’Antonio)
- Increase understanding of the technology needs of and the affordability and usability of new technologies for both consumers and medical professionals (D’Antonio, Sheffield)
- Study and promote the development of community- and state-level programs (D’Antonio)
- Conduct bottom-up research that identifies needs among people living in communities rather than developing solutions in search of a problem (Sheffield)
- Identify and develop measures and indicators of quality programs and services in order to identify those that maintain and improve quality of life (Sheffield)
- Establish practice-based research demonstrating both the gaps and the effectiveness or value added of LTSS from a person-centered goal perspective (Campbell)
- Develop measures of quality and functional status that can be integrated into all home- and community-based long-term care data systems (Campbell)
- Conduct research to understand the housing and HCBS needs and goals of an increasingly complex LTSS population, with a particular focus on low-income older adults and people with disabilities (Campbell)
Policy Priorities
- Increase federal funding for research on managed care and LTSS (Parks, Rava)
- Educate the U.S. population, including policy stakeholders, about the realities of aging and disability and the increasing demand for LTSS (Chapman)
- Address the stigma surrounding and the denial about LTSS (Chapman)
- Act on research findings that demonstrate the importance and impact of addressing the social determinants of health (Chapman)
Best Practices
The facilitated table discussions produced the following list of best practices, as noted by the table rapporteurs.
Programs at the Federal Level
- The U.S. Department of Veterans Affairs’ health care system, which integrates medical and community-based services and aligns responsibility for clinical and financial decisions and outcomes (Campbell, Parks)
- ACL’s Business Acumen Learning Collaborative initiative (Campbell)
- CMS paying for value (Chapman)
Programs at the State Level
- Minnesota’s framework for delivering community-based services and, in particular, the Return to Community program (Campbell, D’Antonio, Parks, Sheffield)
- California’s programs for delivering LTSS (D’Antonio)
Possible Approaches
- Self-directed service delivery, such as cash and counseling (Chapman)
- Individualized systems of care involving primary care plans and data collection (Sheffield)
In addition to reporting on the lists their tables developed, several of the rapporteurs repeated some insightful comments that were made during the discussions at their tables. Lee reported that her table discussed the inertia that inhibits policy change and suggested that investing in research that can quantify the value of community programs may help overcome that inertia. She also reported that her table thought that eliminating the silos between the different providers of services might help identify areas of overlap and streamline service delivery. Sheffield reported that the participants at her table noted that some urban and rural communities have housing systems and policies that limit access to affordable community living. Campbell recounted that the discussion at her table raised the point that federal waivers do not allow payment for housing and food even though these are needed to support community living. Chapman suggested looking at other countries around the world to identify additional best practices for increasing the awareness of LTSS.
















