Summary
The World Health Organization (WHO) defines social determinants of health as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life” (WHO, 2016a). These forces and systems include economic policies, development agendas, cultural and social norms, social policies, and political systems. Health inequities, “the unfair and avoidable differences in health between groups of people within countries and between countries” (WHO, 2016b), stem from the social determinants of health and result in stark differences in health and health outcomes. Other terms used to describe such differences reflect the countries in which they are used. In the United States, for example, the term “disparities” is often interpreted as racial or ethnic disparities (HHS, 2016) involving structural racism and other forms of unfair and unjust discrimination that create gaps in health among segments of the population. In the United Kingdom, the term “inequalities” is used to describe differences in health among groups based on socioeconomic conditions (Marmot and Allen, 2014). A consistent message embedded in each definition, regardless of its usage, is that if the underlying causes of disease and ill health are not addressed, the risk of perpetuating a cycle of inequity, disparity, and inequality will remain for generations to come.
PURPOSE OF THIS STUDY
Educating health professionals about the social determinants of health generates awareness of the potential root causes of ill health and the importance of addressing them in and with communities. The individual
sponsors1 of the Global Forum on Innovation in Health Professional Education of the Institute of Medicine (IOM) of the National Academies of Sciences, Engineering, and Medicine that called for a study of this topic expect greater awareness to lead to more effective strategies for improving health and health care for underserved populations now and in the future. Based on this premise, a diverse committee of experts was tasked with developing a high-level framework for educating health professionals to address the social determinants of health. Such a framework would draw on lessons learned by educators working in this sphere. It would also include elements of relevant frameworks and ideas advanced by international thought leaders with respect to their vision for health professional education. Additionally, the framework would consider health professional education in the social determinants of health across the learning continuum, from foundational education through continuing professional development.
DEFINING HEALTH PROFESSIONALS
Health professionals are classified and defined in the International Labour Organization’s International Standard Classification of Occupations, which is accepted and used by WHO as the reference for its policy resolutions and technical guidelines. While this list does not capture the full breadth of professions making up the health workforce, it does illustrate the point that health professionals are not a homogeneous group. Rather, they differ in the nature and scope of their roles, responsibilities, and functions in promoting, preventing, curing, rehabilitating, and palliating within a holistic health system. This system also employs health professionals as educators, administrators, public health advocates, researchers, and policy makers. Embedded within a holistic health system are caregivers and others, such as community health workers, who do not fit the classic definition of a health professional.2 In addition, a large segment of the health workforce is immersed in clinical practice environments. These clinical workers have an orientation to health systems that emphasizes disease-based, curative models of care for treating individual patients. Their role in addressing the social determinants of health is complementary to that of population health specialists, who focus on health promotion and disease prevention within communities and populations. In essence, everyone involved in the health arena has a role in addressing the social determinants of health.
___________________
1 For the full list of sponsors of the Global Forum on Innovation in Health Professional Education and also of this study, please see Appendix C. The sponsors represent 18 different professions and 9 countries.
2 Based on the statement of task for this study, the focus of this committee was on educating health professionals.
CREATING LIFELONG LEARNERS
Making the social determinants of health a core component of all health professionals’ lifelong learning pathways will engender in them the competence, skill, and passion to take action, independent of their role and position in the health system, on these crucial contributors to individual and community health, and enhance their ability to identify, engage, and partner with others to take this action. The social determinants of health can and should be integral to all health professional education and training. As they progress though their educational programs and their careers, health professionals can gain greater understanding of the social determinants of health and how to partner within and outside of the health sector and with communities through formal and informal continuing professional development.
While creating lifelong learners is frequently seen as starting with admission into a health professional program, in reality the process starts long before that and continues well beyond retirement (CEU, 2002; Perels et al., 2009). University–community partnerships that create quality primary and secondary education programs in vulnerable communities provide exposure of community organizations to health professional students while also potentially embedding a desire to learn in young minds. Additionally, investment in early childhood development and education will increase the pool of potential candidates for health workforce education and training, which could be further enhanced through bridging programs designed to help adults enter the health workforce later in life. With greater professional maturity and a deepening understanding of the economic, political, and social causes of health disparities, health professionals gain further appreciation of and skills for addressing the social determinants of health, both individually and collectively.
THE ROLE OF EDUCATORS
University faculty members who are motivated to offer experiential, cross-sectoral, and interprofessional educational opportunities often confront significant barriers to acquiring the training necessary to provide these opportunities. Faculty development is a key requirement for obtaining relevant educational competencies and skills, which must also be matched by career pathways and rewards from academic leadership. While many health professional schools embrace experiential, cross-sectoral, and interprofessional education in partnership with communities, many have limited ability and desire to adopt incentives that would encourage faculty to become trained in this area (Calleson et al., 2002; Frenk et al., 2010; Goldstein and Bearman, 2011; Meleis, 2016).
Educators in clinical settings also have a role to play in addressing the social determinants of health as they reinforce concepts learned by students and trainees during community and didactic educational experiences. In this way, students transitioning into practice see the impacts of the social determinants of health on the health and well-being of individual patients. All educators thus need to have a common understanding of how social, economic, and policy decisions affect populations and can negatively impact individual health outcomes.
Engaging educators (clinical and nonclinical) from different communities offers numerous benefits. Expanded diversity enhances creativity and performance gains while providing a wider array of culturally and linguistically distinct role models. Having educators from diverse backgrounds also increases the likelihood that a student will identify a mentor with personal and cultural characteristics similar to his or her own.
THE IMPORTANCE OF PARTNERSHIPS
Partnerships are key to effectively addressing the social determinants of health. These partnerships entail close working relationships among policy makers, educators, representatives of the health and nonhealth professions, community organizations, and community members. They also involve strong linkages between nonclinical faculty and clinical faculty or preceptors so that experiences in and with communities related to the social determinants of health are reinforced during clinical rotations. Through such partnerships, health professionals gain exposure to the broader social, political, and environmental context that influences the health and health outcomes of individuals, populations, and communities. Innovative forms of education consolidate the unique aspects and experiences of each partner. Learners are challenged to solve problems and make new connections through exposure to other professions, sectors, and populations. Bidirectional linkages between partners reinforce equality in the partnership, which can be strengthened through organizational support.
A UNIFYING FRAMEWORK
The committee’s review of the salient literature supports the need for a holistic, consistent, and coherent framework that can align the education, health, and other sectors, in partnership with communities, to educate health professionals in the social determinants of health. The outcome of such an education framework would differ based on the learner’s position within the education continuum, from foundational (where the emphasis would be on broad exposure of students to and understanding of the social determinants of health) to continuing professional develop-
ment (where health professionals would continue to learn from and with others to take action on the social determinants of health). Once trained, these individuals would become enlightened change agents competent to serve as faculty for students and peers to expand education on the social determinants of health. Ideally, they would be drawn from diverse communities.
One high-level assessment of health professional education posits that enlightened change agents are produced through transformative learning (Frenk et al., 2010). Instead of passive intake of facts, such learning emphasizes active participation in educational activities that build creative thinking and decision making, as well as competencies in collaboration. This notion heavily influenced the committee’s development of the framework presented in this report, informed as well by ideas formulated by the WHO Commission on Social Determinants of Health. The Commission, comprising international thought leaders, policy makers, and representatives of civil society, produced a report emphasizing that poor health of certain individuals and groups is due to inequities caused by unequal distribution of power, income, goods, and services (WHO, 2008a). The Commission produced a conceptual framework for action on the social determinants of health that captures these ideas (Solar and Irwin, 2010). Heads of government, ministers, and government representatives from 120 member states used the Commission’s framework and its other publications to draft their Rio Political Declaration on Social Determinants of Health (WHO, 2011a). In the Rio Declaration, the signatories affirm their “determination to achieve social and health equity through action on social determinants of health and well-being by a comprehensive intersectoral approach” (Marmot et al., 2013; WHO, 2011a, p. 1). They also emphasize that “health equity is a shared responsibility and requires the engagement of all sectors of government, of all segments of society, and of all members of the international community, in an ‘all for equity’ and ‘health for all’ global action” (WHO, 2011a, p. 1).
These global documents, along with ten relevant frameworks, programmatic examples of education in the social determinants of health described in the literature, presentations at a public meeting held by the committee, and the expert knowledge of the committee members formed the basis for the framework described below.
THE FRAMEWORK
The primary goal of creating partnerships and lifelong learners who desire more in-depth understanding of the social determinants of health is reflected in the committee’s framework, presented in Figure S-1. This framework captures education at all levels, from foundational to gradu-
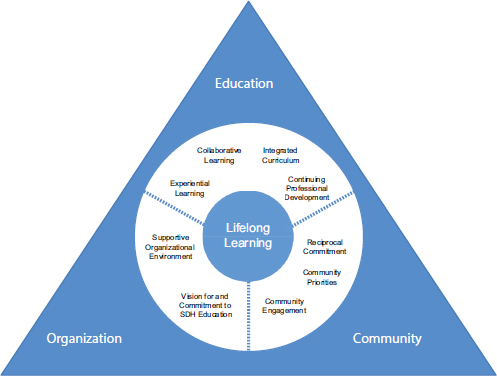
NOTE: SDH = social determinants of health.
ate to continuing professional development. This education, which applies transformative learning techniques, is built around three domains:
- education
- community
- organization
In Figure S-1, these three domains reside within a triangle signifying constant interaction among them. The white circle within the triangle contains nine domain components separated by dotted lines indicating that while these components apply predominantly to a particular domain, they can be applied to any of the domains. Lifelong learning is situated in the center of the framework, emphasizing its importance in the educational pathway of health professionals toward understanding and addressing the social determinants of health. Each of the three domains and its primary components are discussed in the sections below.
Education
The education domain is located at the top of the triangle in Figure S-1 to indicate that the framework is primarily about education. Listed within this domain are four components that education in the social determinants of health should include (see Figure S-1). Education should be experiential, integrated, and collaborative across the learning continuum, including continuing professional development. A desired outcome for health professional students in the early stages of professional education would be to demonstrate an understanding of how social, political, and economic factors determine the health and health outcomes of individuals, communities, and populations. For clinical faculty, the outcome would be to demonstrate an understanding of how the social determinants of health are incorporated into clinical care. And for nonclinical faculty, the outcome would be improved pedagogy for educating students in the social determinants of health; their impacts on individual, community, and population health; and the role of key partners in improving the conditions that lead to inequities. Clinical and nonclinical faculty who work together can reinforce important messages about the social determinants of health while validating the importance of partnering to take action.
In concurrence with member states’ call for action on the social determinants of health (as expressed in the Rio Declaration), numerous provider organizations and educational associations, as well as individual faculty members, programs, and universities, are moving forward with activities to demonstrate action on the social determinants of health. While these efforts may add value, the risk of eroding the trust of vulnerable communities is very real. Thus, it is essential to understand a community’s issues before acting on the social determinants of health through well-thought-out partnerships. Achieving consistency through a unified framework can help ensure that all health professionals understand the underlying social, economic, and political causes of poor mental and physical health among individuals and populations and are able to address these issues in a coordinated manner. Accordingly, the committee makes the following recommendation:
Recommendation 1: Health professional educators should use the framework presented in this report as a guide for creating lifelong learners who appreciate the value of relationships and collaborations for understanding and addressing community-identified needs and for strengthening community assets.
To demonstrate effective implementation of the framework, health professional educators should
- publish literature on analyses of and lessons learned from curricula that offer learning opportunities that are responsive to the evolving needs and assets of local communities; and
- document case studies of health professional advocacy using a health-in-all-policies approach.3
Community
Partnerships with communities are an essential part of educating health professionals in the social determinants of health. Three domain components would move education in this direction (see Box S-2). A reciprocal commitment ensures that the community is an equal partner in any initiative undertaken. The commitment is heavily based on community-identified priorities and real community engagement that are the second and third components of this domain. It is through shifts in power from health
___________________
3 “Health in all policies” denotes a policy or reform designed to achieve healthier communities by integrating public health actions with primary care and by pursuing healthy public policies across sectors (WHO, 2008b, 2011b).
professionals to community members and organizations that communities share in the responsibility for developing strategies for the creation of learning opportunities that can advance health equity based on community priorities and build upon community assets.
As suggested earlier, building pipelines to higher education in the health professions in underserved communities is a tested means of expanding the pool of viable candidates who have themselves been negatively affected by the social determinants of health. And while applications and admissions of such candidates may increase, equal emphasis on retaining them once they have been accepted into a program is essential, as is recruiting and retaining faculty from similarly underserved communities.
Recommendation 2: To prepare health professionals to take action on the social determinants of health in, with, and across communities, health professional and educational associations and organizations at the global, regional, and national levels should apply the concepts embodied in the framework in partnering with communities to increase the inclusivity and diversity of the health professional student body and faculty.
To enable action on this recommendation, health professional education and training institutions should support pipelines to higher education in the health professions in underserved communities, thus expanding the pool of viable candidates who have themselves been negatively affected by the social determinants of health.
Organization
The two components of this domain (shown in Box S-3) emphasize a commitment to addressing the social determinants of health and creating an environment that will support the sort of understanding and actions discussed under the education domain. How committed an organization is to addressing the social determinants of health is reflected in its founding and guiding policies, strategies, education programs, and leadership-promoted activities. And while the actual words “social determinants of health” may not always appear in its documents, other relevant terms, such as “social justice,” “disparities,” “equity,” “diversity,” and “inclusivity,” can reflect an organization’s commitment to education in the social determinants of health for students and employees.
Recommendation 3: Governments and individual ministries (e.g., signatories of the Rio Declaration), health professional and educational associations and organizations, and community groups should foster an enabling environment that supports and values the integration of the framework’s principles into their mission, culture, and work.
To implement this recommendation, national governments, individual ministries, and health professional and educational associations and organizations should review, map, and align their educational and professional vision, mission, and standards to include the social determinants of health as described in the framework. The following actions would demonstrate organizational support for enhancing competency for addressing the social determinants of health:
- Produce and effectively disseminate case studies and evaluations on the use of the framework, integrating lessons learned to build and strengthen work on health professional education in the social determinants of health.
- Work with relevant government bodies to support and promote health professional education in the social determinants of health by aligning policies, planning, and financing and investments.
- Introduce accreditation of health professional education where it does not exist and strengthen it where it does.
- Design and implement continuing professional development programs for faculty and teaching staff that promote health equity and are relevant to the evolving health and health care needs and priorities of local communities.
- Support experiential learning opportunities that are interprofessional and cross-sectoral and involve partnering with communities.
FITTING THE FRAMEWORK INTO A CONCEPTUAL MODEL
Applying concepts and ideas from multiple sources, the committee developed a conceptual model (see Figure S-2) for visualizing how the framework fits within a broader societal context (Frenk et al., 2010; HHS, 2010; Solar and Irwin, 2010; Sousa et al., 2013; WHO, 2006, 2008a, 2011a). The model depicts how social, political, and economic factors (i.e., the structures in which populations live) influence intermediary determinants (i.e., material and psychosocial circumstances, behavioral and/or biological factors, and the health system itself) that ultimately determine health equity and the well-being of populations. Communities and the future health workforce are influenced by the structural and intermediary determinants that form the environment for educating health professionals in the social determinants of health.
Positioned in the center of the model is the committee’s framework. To the left of the framework is the population/future health workforce,4 which forms the pipeline for the education and production of future health professionals. Through a transformative learning approach, health professionals, students, and trainees gain an understanding of how to establish equal partnerships with communities, other sectors, and other professions for action on the social determinants of health. Those who are educated
___________________
4 The population/future health workforce includes the pool of eligible students. The development of this workforce starts with primary and secondary education to encourage a new generation of health workers at the pre-entry stage. It also includes adults who might enter the health workforce from other sectors, as well as current health workers looking to expand their knowledge or change their employment position.
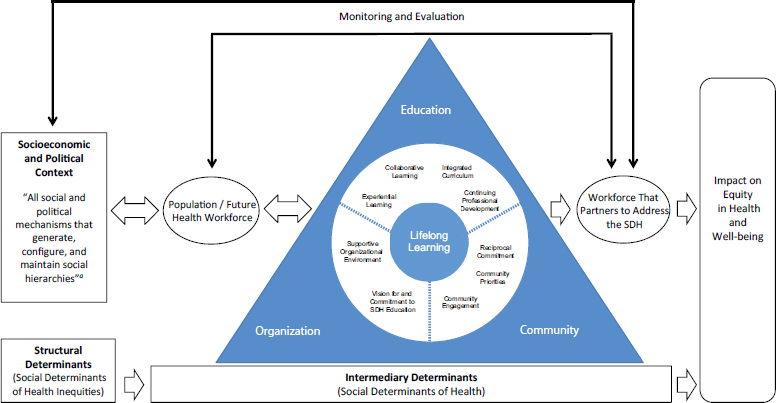
NOTE: SDH = social determinants of health.
a Solar and Irwin, 2010, p. 5.
in line with the framework also gain competency in addressing health system complexities within an increasingly global and interconnected world, thereby becoming part of a workforce that partners to address the social determinants of health toward the ultimate goal of achieving impact on equity in health and well-being.
Measuring the degree to which health professionals understand and partner to address the social determinants of health before and after undergoing transformative education in the social determinants of health is a way of determining the proximal impact of the framework. However, the desired impact of the framework is on the more distal outcomes of improving the health and well-being of individuals, communities, and populations. Using established methodology for analyzing cause-and-effect relationships between educational interventions and these distal outcomes will be critical to building an evidence base on the effects of the framework on both learning and health outcomes.
BUILDING THE EVIDENCE BASE
While numerous articles describe student activities within communities to address the social determinants of health, few publications offer evidence beyond student outcomes for analyzing the value to communities of such health professional education. The gap is due in part to a lack of well-established methods for conducting such an analysis. Reports outlining lessons learned from educational experiences designed to impact the social determinants of health are useful for understanding potential barriers to partnerships, but do not provide guidance for researchers or evaluators seeking to impact community outcomes. Further evidence that goes beyond self-examination is needed to inform the education of health professionals. Obtaining objective and subjective input from community partners would help build the evidence base for learning in and with communities while impacting the social determinants of health and inform best practices for lifelong learning.
Recommendation 4: Governments, health professional and educational associations and organizations, and community organizations should use the committee’s framework and model to guide and support evaluation research aimed at identifying and illustrating effective approaches for learning about the social determinants of health in and with communities while improving health outcomes, thereby building the evidence base.
To demonstrate full and equal partnerships, health professional and educational associations and organizations and community partners should pre-
pare their respective networks to engage with one another in a systematic, comprehensive inquiry aimed at building the evidence base.
MOVING FORWARD
Achieving lasting impacts on the social determinants of health will require action at multiple levels from multiple stakeholders. This report addresses one narrowly defined area—health professional education—while stressing the importance of strategic partnerships that extend beyond the walls of health professional schools. Extensive detail on the partners is beyond the scope of this report but warrants mentioning to encourage future studies, possibly with a broader mandate, focused in greater depth on these other critical stakeholders. One such key group is community health workers. These individuals usually come from the community served, are culturally and linguistically competent, and enjoy a high level of trust in the community. They are increasingly serving as members of health care teams and as facilitators of community engagement and training of health science students in community perspectives (Torres et al., 2014). Other critical groups include health workers educated and trained at community colleges and vocational training institutes, as well as representatives of nonhealth sectors such as education, labor, housing, transportation, urban planning, community development, and public policy.
Another crucial area for more thorough investigation is investment in health professional education. The committee recognizes that without adequate financial support and sustainable investment, the education envisioned in this report will remain predominantly a series of one-off, ad hoc efforts by motivated but often overburdened, undersupported individuals. And while a recommendation on funding is beyond the mandate and expertise of this committee, the following points are offered as considerations for future explorations of this topic.
First is the recognition that governments and ministries have the power to direct health professional education, and power brokers who control major resources within academic health centers and hospitals also have an important role in addressing the social determinants of health. By reallocating graduate education funding and examining the rules governing special tax status, for example, national governments can shift the focus of education and practice more toward community engagement. Similarly, ministries can direct the use of funds through educational requirements. Often such shifts require evidence demonstrating a return on investment relevant to a particular health system. For some this evidence will be financial savings, and for others it may involve tracking such indicators as the health and well-being of community residents and the social accountability of health
professional schools (Annis et al., 2004; Boelen et al., 2012; Danaher, 2011; Ryan-Nicholls, 2004).
A second point is that funders of and payers for health professional education and research need to be part of any discussion moving forward. This group includes students, employers, governments, and foundations with a stake in how health professionals are educated to address the social determinants of health. Foundations exert influence through the activities they support. If these activities build the evidence base for interventions that educate students while benefiting communities socially and financially, those data empower students, communities, and educators to advocate for a redirection of funding. In the context of this report, such redirection could focus funds toward expanding opportunities that promote incorporation of the social determinants of health into community programs that also train current and future generations of health professionals.
A third point is that many stakeholder groups will need to advocate for greater educational focus on the social determinants of health based on the potential financial, social, and health benefits to society, although these groups should be prepared for resistance. One way to overcome this resistance would be to build a business case. To this end, more data are needed to demonstrate efficient and equitable outcomes attributable to health professionals being educated in the social determinants of health because such information is currently sparse.
Resistance to change is just one likely challenge faced by advocates. Another is ensuring appropriate engagement of communities, especially marginalized communities with low-income populations who have previously been used by academic institutions for research that has not benefited them or their communities. At times, students and health professionals with extremely limited experience and exposure to community engagement and the social determinants of health may push for interventions in a way that is counterproductive to building community relations. And while requirements under accreditation standards may force programs to offer interprofessional, cross-sector, community-engaged learning, proper leadership support and adequate training also are necessary, or the quality of the programs offered may fulfill the requirements but fail to inspire a desire for lifelong learning in how to mitigate the root causes of ill health and disease.
In closing, it is the committee’s hope that leaders within health professional education who claim to already address elements of the framework will review their efforts in conjunction with staff, employees, students, and educators. These leaders could measure their success by evaluating the extent to which their educational interventions impact a desire for lifelong learning to better understand and act upon the social determinants of health in equal partnership with others.
REFERENCES
Annis, R., F. Racher, and M. Beattie. 2004. Rural community health and well-being: A guide to action. Brandon, Manitoba: Rural Development Institute. https://www.brandonu.ca/rdi/publication/rural-community-health-and-well-being-a-guide-to-action (accessed September 22, 2016).
Boelen, C., S. Dharamsi, and T. Gibbs. 2012. The social accountability of medical schools and its indicators. Education for Health (Abingdon, England) 25(3):180-194.
Calleson, D. C., S. D. Seifer, and C. Maurana. 2002. Forces affecting community involvement of AHCS: Perspectives of institutional and faculty leaders. Academic Medicine 77(1):72-81.
CEU (The Council of the European Union). 2002. Council resolution of 27 June 2002 on lifelong learning. Official Journal of the European Union. Brussels: C 163/1.
Danaher, A. 2011. Reducing disparities and improving population health: The role of a vibrant community sector. Toronto, ON: Wellesley Institute.
Frenk, J., L. Chen, Z. A. Bhutta, J. Cohen, N. Crisp, T. Evans, H. Fineberg, P. Garcia, Y. Ke, P. Kelley, B. Kistnasamy, A. Meleis, D. Naylor, A. Pablos-Mendez, S. Reddy, S. Scrimshaw, J. Sepulveda, D. Serwadda, and H. Zurayk. 2010. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 376(9756):1923-1958.
Goldstein, A. O., and R. S. Bearman. 2011. Community engagement in US and Canadian medical schools. Advances in Medical Education and Practice 2:43-49.
HHS (U.S. Department of Health and Human Services). 2010. Healthy People 2020. Washington, DC: HHS. http://www.healthypeople.gov/sites/default/files/HP2020_brochure_with_LHI_508_FNL.pdf (accessed January 11, 2016).
HHS. 2016. Healthypeople.gov: Disparities. http://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities (accessed January 28, 2016).
Marmot, M., and J. J. Allen. 2014. Social determinants of health equity. American Journal of Public Health 104(Suppl. 4):S517-S519.
Marmot, M., A. Pellegrini Filho, J. Vega, O. Solar, and K. Fortune. 2013. Action on social determinants of health in the Americas. Revista Panamericana de Salud Pública 34(6):379-384.
Meleis, A. I. 2016. Interprofessional education: A summary of reports and barriers to recommendations. Journal of Nursing Scholarship 48(1):106-112.
Perels, F., M. Merget-Kullmann, M. Wende, B. Schmitz, and C. Buchbinder. 2009. Improving self-regulated learning of preschool children: Evaluation of training for kindergarten teachers. British Journal of Educational Psychology 79(Pt 2):311-327.
Ryan-Nicholls, K. 2004. Rural Canadian community health and quality of life: Testing a workbook to determine priorities and move to action. Rural Remote Health 4(2):278.
Solar, O., and A. Irwin. 2010. A conceptual framework for action on the social determinants of health. Social determinants of health discussion paper 2 (policy and practice). Geneva, Switzerland: WHO. http://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf (accessed September 22, 2016).
Sousa, A., R. M. Scheffler, J. Nyoni, and T. Boerma. 2013. A comprehensive health labour market framework for universal health coverage. Bulletin of the World Health Organization 91(11):892-894. http://www.who.int/bulletin/volumes/91/11/13-118927.pdf (accessed September 22, 2016).
Torres, S., R. Labonté, D. L. Spitzer, C. Andrew, and C. Amaratunga. 2014. Improving health equity: The promising role of community health workers in Canada. Healthcare Policy 10(1):73-85.
WHO (World Health Organization). 2006. The world health report 2006: Working together for health. Geneva, Switzerland: WHO. http://www.who.int/whr/2006/en (accessed September 22, 2016).
WHO. 2008a. Closing the gap in a generation: Health equity through action on the social determinants of health, final report. Geneva, Switzerland: WHO Commission on Social Determinants of Health.
WHO. 2008b. The world health report 2008. Primary health care: Now more than ever. Geneva, Switzerland: WHO.
WHO. 2011a. Rio political declaration on social determinants of health. Adopted at the World Conference on the Social Determinants of Health, Rio de Janeiro, Brazil. Geneva, Switzerland: WHO. http://www.who.int/sdhconference/declaration/Rio_political_declaration.pdf?ua=1 (accessed September 22, 2016).
WHO. 2011b. Health systems strengthening glossary. http://www.who.int/healthsystems/hss_glossary/en (accessed September 22, 2016).
WHO. 2016a. Social determinants of health. http://www.who.int/social_determinants/en (accessed February 2, 2016).
WHO. 2016b. Social determinants of health. http://www.who.int/topics/social_determinants/ en (accessed February 2, 2016).
This page intentionally left blank.


















