7 Leveraging Leadership and Fostering a Culture of Learning
Trauma care, properly performed, involves an extremely complex system of interactions, handoffs, and teams. In military trauma care, for example, the doctrines of forward care, rapid transfer, and tiered levels of capability require highly reliable orchestration that spans multiple geographies, ranks, and roles. Similarly, high-quality civilian trauma care within the United States bridges numerous federal, state, and local agencies; prehospital and tiered inpatient systems; professional organizations; and academic societies. In such a cross-cutting and interconnected endeavor, knowledgeable and effective leadership at all levels is essential to success. The need for leadership is even greater in pursuit of a learning trauma care system, since the elements of a learning system promulgated by the Institute of Medicine (IOM, 2013) report Best Care at Lower Cost do not occur spontaneously; only leaders can plan, maintain, and support them. The challenges to the accomplishment of such a system include technical issues (such as ensuring the availability of proper real-time data systems); cultural concerns (such as avoiding fear in the workforce, which is inimical to curiosity, ambition, and transparency); and a paucity of leadership, policy, and resources to animate a national system. If the aims for the system include, as they should, continued bidirectional exchange between the military and civilian systems to continually improve and ensure the best trauma care possible in both sectors, national and regional leaders will have to commit to that communication and cooperation.
Leadership (inclusive of health leaders) is uniquely positioned to define and communicate the aims of a system, make continuous learning and improvement a priority, and provide the resources and environment neces-
sary to achieve the system’s aims. Accountability, culture, transparency, and incentives are powerful catalysts for change that can be leveraged to promote a learning trauma care system and drive all actors within the system to work cooperatively toward shared goals, ultimately saving lives. In contrast, a culture inhospitable to improvement and the absence of transparency and accountability can result in preventable deaths after injury (see Box 7-1). In this chapter, the committee examines the extent to which these catalysts are employed and aligned in the military and civilian sectors as a demonstration of leadership’s visible commitment to and rewarding of learning and improvement.
FOSTERING A CULTURE OF LEARNING
A culture of learning is driven by a belief in the value of continuous improvement. As discussed in Chapter 3, organizational culture can act as either a strong enabler or a deterrent for continuous learning and improvement. A learning trauma care system will function optimally in an environment that embraces teamwork and partnership, and in which actors are encouraged to improvise without fear (IOM, 2013). Within such a setting, leadership is responsible for defining and supporting an aim of continuous learning, translating that aim into practice at all levels, and removing cultural barriers that threaten to stall improvement.
The history of the 75th Ranger Regiment (also discussed in Chapter 1) attests to the positive outcomes that can be achieved in trauma care when leadership at the highest level makes improvement a priority and supports a culture of learning. In 1998, the commander of the 75th Ranger Regiment, then COL Stanley McChrystal, issued a directive that all rangers make four major areas of training a priority: marksmanship, physical training, small unit tactics, and medical training (Kotwal et al., 2011). This elevation of medical training to a tactical priority on par with a unit’s capability to shoot, move, and communicate drove the regiment to establish a casualty response system integrating tactical combat casualty care (TCCC) training at all levels (Pappas, 2001; Veliz et al., 2010). The result was zero medically preventable deaths in the prehospital setting (Kotwal et al., 2011). Unfortunately, this example of formal command leadership of trauma care learning and improvement appears to be more the exception than the rule. Across the military, service parochialisms and an inconsistent level of understanding by senior medical and line leadership of the value of a learning trauma care system impede continuous learning and improvement. The success of the 75th Ranger Regiment at the same time that nearly 25 percent of battlefield fatalities within the broader U.S. Department of Defense (DoD) resulted from potentially survivable injuries demonstrates the need for combatant commanders and line leaders along the chain of command
to assume responsibility for the performance of the trauma care system in theater (Butler et al., 2015; Eastridge et al., 2012).
A culture of teamwork and cooperation is a fundamental component of a learning trauma care system, in which an injured patient must be managed across a lengthy continuum of care entailing multiple transitions and handoffs between providers. The Joint Trauma System’s (JTS’s) use of weekly teleconferences in which all levels of medical personnel discuss casualties as they actively move across the evacuation chain exemplifies how such a culture fosters strong communication and coordination among providers (Bailey et al., 2013; Butler et al., 2015; Eastridge et al., 2009; Pruitt and Rasmussen, 2014). However, this level of partnership is far from universal. With regard to the civilian sector, the committee heard testimony that competition, particularly among emergency medical services (EMS) agencies (Osborn, 2015) and private health systems, remains a problem in civilian trauma care. The expansion of competing for-profit trauma centers in the civilian sector also threatens outcomes for injured patients (Johnson, 2015).
It is important to note that most, if not all, modern views of an effective learning organization emphasize the toxic effects of fear. When members of a workforce are afraid of what might happen to them should defects arise and become known, should they speak up with new ideas, or should a test of change fail, information is hidden, teamwork suffers, and self-defense displaces honesty (Garvin et al., 2008; IOM, 2013). These principles are well known in the military in, for example, the culture of after-action reviews, in which rank and hierarchy give way to open and honest exchange among all participants who may have information and ideas to offer (Garvin et al., 2008; Morrison and Meliza, 1999). As the military seeks to accelerate improvements in trauma care through learning, it is imperative that leaders—at all levels—understand and continually reduce those insidious forces—including fear, departmental politics, internal competition, egos and agendas, an unwillingness to accept responsibility, and a culture of blame—that threaten to undermine teamwork, progress, and the larger enterprise of continuous learning and improvement.
For a culture of learning to truly permeate a system, leadership must be willing to invest the time, resources, energy, and infrastructure necessary to facilitate learning. This support for learning rests on a belief in the value of continuous improvement. The efforts and accomplishments of the JTS, the Committee on Tactical Combat Casualty Care, and medical providers at all levels demonstrate the military’s commitment to these principles, driven by wartime’s immense burden of injury. The challenge at hand is whether an institutional commitment to continuous improvement in trauma care can be sustained throughout interwar periods. The military has been much lauded for reducing its case fatality rate to an unprecedented low over the course
of wars in Afghanistan and Iraq. What has not been emphasized, however, is the fact that in 2006, the case fatality rate in Afghanistan reached above 15 percent (Bailey et al., 2013). During the war in Vietnam, the case fatality rate was 15.8 percent (Holcomb et al., 2006). The startling consistency in these case fatality rates reveals the dangers of compliance and of the absence of a culture in which learning and constant improvement in trauma care are priorities. As the military transitions to an interwar period, it is essential that the wartime culture of learning and drive to improve persist so that the case fatality rate at the start of the next war is lower than or at least equal to that achieved at the end of the wars in Afghanistan and Iraq.
DEMONSTRATING A COMMITMENT TO TRANSPARENCY
Transparency incentivizes providers, hospitals, and systems to reassess their practices in order to improve (IOM, 2013) and thus plays an important role in a learning trauma care system. In addition, transparency of costs and outcomes enables patients and consumers to make well-informed decisions, encouraging continuous improvement and the delivery of high-quality care as providers and organizations respond to this external motivation. Transparency for the purposes of performance improvement is not possible, however, without a standard set of performance indicators. Equally important, as discussed above, is a culture in which fear—of disciplinary action, liability, or embarrassment—is not permitted to impede continuous learning (Garvin et al., 2008; IOM, 2007b).
As discussed in Chapter 3, four different but interrelated domains of transparency have been shown to improve outcomes, reduce errors, improve patient satisfaction, and lower costs:
- Clinician-to-patient—includes better communication, disclosure (cost and potential clinical outcomes), and patient engagement in decision making.
- Clinician-to-clinician—includes peer reviews such as regular and comprehensive morbidity and mortality conferences, sharing of best practices and lessons learned, open discussion of adverse events, and assurance that providers have access to their own performance data (e.g., expected versus actual mortality). Equally important are data comparing the performance of individual clinicians with that of their peers.
- Organization-to-organization—includes participation in national and regional collaboratives for data sharing and benchmarking across organizations.
- Public—includes public reporting on outcomes and costs (NPSF, 2015).
An assessment of communication with and engagement of patients in trauma care is presented in Chapter 6. The discussion here focuses on transparency and public reporting at the provider and organization levels.
The incorporation of performance improvement processes into health care systems and the delivery of care as a routine and ongoing process is an invaluable tool that can assist individual providers in understanding and improving their personal performance, as well as their contribution to the entire trauma care system (DHB, 2015; IOM, 2007b). To encourage this individual-level performance improvement, providers need access to their own data. Morbidity and mortality conferences are well-established processes that facilitate transparency at the provider level (Seigel et al., 2010). Open discussion among providers on medical errors and adverse events is a critical component of patient safety improvement efforts (ACS, 2014). However, this process does not provide clinicians with real-time data on their performance relative to that of their peers. The American College of Surgeons (ACS) and Vizient1 (formerly the University HealthSystem Consortium) both provide national-level quality improvement programs that facilitate transparency through external benchmarking.
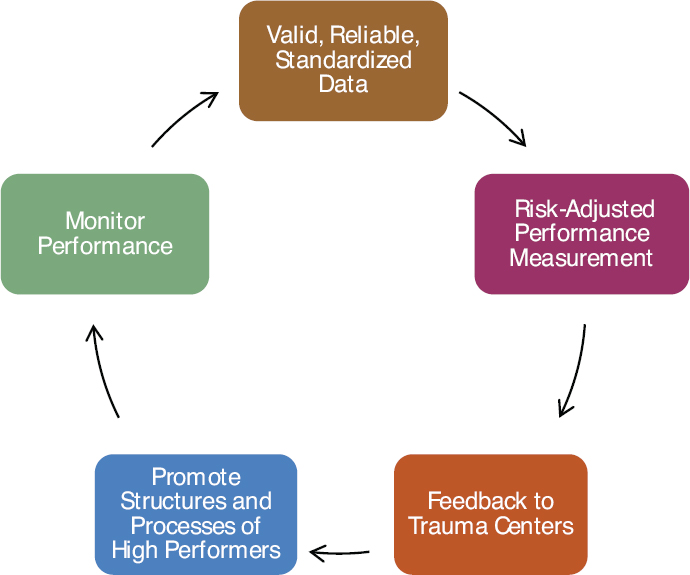
The ACS Trauma Quality Improvement Program (TQIP) provides participating trauma centers with risk-adjusted benchmark reports, online tools for drilling down into the data, and an opportunity to share successes and challenges at the annual TQIP meeting and training (ACS, 2015d) (see Figure 7-1). To take part in TQIP, centers must use the National Trauma Data Bank, be fully compliant with the National Trauma Data Standard (NTDS), pay an annual fee, and submit data quarterly (ACS, 2015a). Use of the NTDS ensures that data across centers are standardized and comparable. However, some issues with data may remain. For example, centers or providers may classify similar trauma outcomes differently, or preexisting classification fields may have to be “mapped” onto NTDS fields. ACS has attempted to address these issues through ongoing registrar training and data quality assessments (Nathens et al., 2012). In addition, ACS uses risk adjustment models to standardize data. These models help account for variation among trauma centers, such as differences in transport times to the centers, local patterns of injury or patient characteristics, and different policies regarding pronouncement of death. Risk adjustment also allows ACS to create models that can be used to compare expected and observed mortality and lengths of stay across centers (Nathens et al., 2012). This information allows centers to see how they compare with other centers and facilitates the identification of high-performing centers.
__________________
1 Vizient is the new member-owned health care services company formed following the 2015 merger of the VHA and University HealthSystem Consortium (UHC) hospital networks (Vizient, 2016b).
SOURCE: Reprinted from Nathens et al., 2012, with permission from Elsevier.
Similarly, participation in a Vizient learning network (e.g., academic medical center network) allows member organizations to benchmark their organizations, comparing outcomes and identifying areas for improvement (Vizient, 2016a).
Military Sector
In the military, the challenges associated with fragmented data repositories and the abstraction process—discussed in more detail in Chapter 4—limit the extent to which timely individual provider performance improvement is possible. A 2011 assessment of the military’s trauma system included the following observations about performance improvement processes in theater:
- The trauma performance improvement and patient safety process is fragmented. The awareness, implementation and integration of structured [performance improvement] processes vary by level of care,
-
branch of service and coalition partners. This less than desirable state results in a loss of transparency and creates difficulty in performing concurrent, multidisciplinary [performance improvement] and stifles the communication and learning between and amongst levels of care.
- Efforts to implement rudimentary trauma related [performance improvement] were present at each military trauma facility. Morbidity and mortality review varied widely from no review, to an exclusionary physician only review with little documented analysis or corrective actions, to a casual multidisciplinary verbal debriefing with no recorded corrective actions or loop closure documented in any of these observed systems. (Rotondo et al., 2011, pp. 11-12)
The JTS holds weekly teleconferences to review the treatment and outcomes for all casualties across the continuum of care. In the absence of easily accessible data on provider performance, this exercise fosters communication among the various providers for a single casualty, providing the opportunity to receive feedback (Bailey et al., 2013; Eastridge et al., 2009). System-wide, however, DoD lacks a codified and standardized approach to performance improvement, which results in a lack of transparency and hinders learning. To improve transparency and learning, it is important for deployed hospitals to conduct weekly morbidity and mortality conferences, with patient-specific information flowing between hospitals and across levels of care. These reports could be collated by the JTS and lessons learned rapidly distributed back to all providers in the system.
Military participation in national collaboratives such as TQIP is severely limited. At this time, only a single military hospital (Carl R. Darnall Army Medical Center) participates in the ACS TQIP Level III pilot benchmarking program.2 This lack of transparency at the organization level highlights an opportunity to improve the learning system for military trauma care through adoption of civilian best practices. Although only trauma centers are eligible to participate in TQIP, military treatment facilities (MTFs) that are not trauma centers may still be able to participate in Vizient’s quality improvement program.
Civilian Sector
In the civilian sector, the trauma performance improvement process—supported by a trauma registry—is a hallmark function of trauma centers, second only to trauma patient care. This process entails monitoring compliance with evidence-based practice, care delivered, and system performance
__________________
2 Personal communication, J. Dodd, American College of Surgeons, to E. Cornett, the National Academies of Sciences, Engineering, and Medicine, regarding the National Trauma Data Bank and Trauma Quality Improvement Program, March 18, 2016.
to ensure that opportunities for improvement are quickly identified and addressed, optimizing patient outcomes. The ACS Committee on Trauma requires that all verified trauma centers have a performance improvement and patient safety program that demonstrates a process of monitoring, assessment, and management to continuously improve care (ACS, 2014). This process helps identify unnecessary variation in care and adverse events that can subsequently be addressed through corrective actions, but it does not ensure that providers have access to timely and continuous information on their performance relative to that of their peers.
At the hospital level, ACS-verified and state-designated trauma centers are eligible to participate in TQIP. Currently more than 350 Level I and II centers are participating, and a program for Level III centers was launched in July 2016 (ACS, 2015e). Starting in January 2017, all centers seeking ACS verification or reverification must be TQIP participants.3 During a pilot study of 23 Level I and II trauma centers, 90 percent of survey respondents said they found the performance data report useful, and 63 percent indicated that they would take action based on the information it provided (Hemmila et al., 2010).
Although the ACS has been successful in establishing a system for performance improvement across trauma centers, an equivalent national program is notably lacking for prehospital care (challenges to benchmarking whole trauma systems are discussed in the next section). The problem has been largely cultural. While some success has been achieved at the state and regional levels in establishing programs to support the quality improvement of EMS care (see Box 7-2), a culture of continuous improvement has not yet been uniformly embraced by the EMS community.
An ongoing National Highway Traffic Safety Administration Office of EMS-funded initiative, EMS Compass, is developing measures for civilian prehospital care (see Box 7-3). The establishment of evidence-based measures through EMS Compass could enable benchmarking of EMS performance, serving as the first step toward the creation of a program similar to TQIP for comparing and assessing EMS systems. However, because EMS systems vary considerably in structure across the United States and their regulation is based at the state and local levels, enacting such a national program could be difficult. State EMS agencies could facilitate a national benchmarking program by requiring licensed agencies to use and report on the EMS Compass measures (Gainor, 2015).
__________________
3 Personal communication, M. Neal, American College of Surgeons, to E. Cornett, the National Academies of Sciences, Engineering, and Medicine, regarding the National Trauma Data Bank and Trauma Quality Improvement Program, April 12, 2016.
Benchmarking Across the Military and Civilian Systems
The ability to benchmark performance across trauma systems is comparatively undeveloped, if not altogether lacking. TQIP’s Collaborative Initiative enables a health system, region, or state to be evaluated as a single entity, comparing its outcomes with those at the national level as well as those of other similar collaboratives (Nathens et al., 2012). Trauma systems encompassing the entire continuum of care, however, cannot compare their outcomes against one another. Thus the military cannot compare its trauma system with those found in the civilian sector and vice versa. In addition, civilian trauma systems cannot compare their performance with that of other civilian systems. This lack of transparency at the regional and state levels inhibits the transfer of best practices from high-performing systems.
The absence of standard, national metrics for trauma care is a barrier to greater transparency and benchmarking at the system level. The National Quality Forum, which grew out of the President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry, has reviewed and endorsed numerous sets of measures, including those for hospital care, home health care, nursing home care, cardiac surgery, diabetes care, and emergency care (NQF, 2005, 2006, 2009, 2010, 2011). Currently, however, it has endorsed no measures of trauma care quality.
Metrics for Trauma
Throughout the development of regionalized trauma systems, rates of preventable death after injury and risk-adjusted mortality have served as the primary standards by which trauma center performance has been measured and compared (Gruen et al., 2012; Mann et al., 1999). Mortality is a simple metric to define and capture in a hospital setting. Using this measure, multiple studies have demonstrated a reduced risk of mortality when care is received at a trauma center (Haas et al., 2010; MacKenzie et al., 2006, 2010; Nathens et al., 2000). Evaluations of trauma system performance, however, tend to focus largely on hospital mortality data, often failing to capture and take into account outcomes across the trauma care continuum (particularly in the prehospital and out-of-hospital settings). At present, data on posttrauma health status and functional outcomes are sparse. In the context of a learning trauma care system, mortality is not a sufficient metric with which to measure care and encourage future improvements (Gruen et al., 2012; Mann et al., 1999). There is a need for validated measures that capture process and morbidity outcomes, including “functional and quality of life outcome measures as well as patient experience and indicators such as return to work, education, and social dependency” (Ardolino et
al., 2012, p. 1662). Measures need to be time based, linked to outcomes, system and provider oriented, and refined over time.
Public Reporting of Performance Data
Public dissemination of data on trauma system performance (both military and civilian) currently represents a notable gap in transparency. The reason is likely multifaceted, including a lack of data and quality measures for trauma care, competition among provider organizations, and tort concerns. Reports from national-level quality improvement programs, including those offered by ACS and Vizient, are not made publicly available. Although research has been conducted to demonstrate variability in trauma center performance, such information is publicized largely through journal articles, a channel unlikely to reach the public. The lack of public reporting may contribute to the documented misalignment of Americans’ perception that they will receive the best possible care after injury and the reality regarding variability in regional trauma care capabilities and patient outcomes across the nation (Champion et al., 2006). Given the nature of traumatic injury, increased public reporting likely would not guide individual choice of where to receive care, but it could raise awareness of the overall burden of injury and lead to greater public engagement in and advocacy for trauma system development, quality improvement, and research. Similarly, public reporting would inform community and policy leaders regarding geographic differences and potential gaps in the care and outcomes among trauma patients.
PROMOTING AND REWARDING HIGH-QUALITY TRAUMA CARE
Transparency is arguably one of the most powerful levers for effecting change in practices and improvement in trauma care outcomes, but as discussed in Chapter 3, high-performing learning systems apply an array of stimulants to encourage and reward continuous quality improvement. Although there has been increasing focus on the use of financial incentives to drive higher-quality medical care and lower costs in the United States, other levers include personal recognition (e.g., promotion, bonuses), regulatory requirements, tort, and competition. The best approach to improving trauma care in both the civilian and military sectors is to use multiple levers in a comprehensive effort.
Military Sector
Military trauma care providers are driven to improve first and foremost by the desire to help their fellow service members achieve the best
possible outcomes after injury. While financial incentives (e.g., variable reimbursement) are a powerful driver of change in the civilian sector, they have a much lesser role in the military. The military essentially functions as a single-payer system, which in theory should help align financial incentives across the continuum of care. However, a large budget for health care coupled with little financial accountability may encourage spending rather than pushing the system to reduce waste and reward high-quality care (Haut et al., 2016).
The backbone of the U.S. military is its system of rank and chain of command. Recognition in the form of promotions serves as one of the strongest incentives for military personnel who value the authority and prestige associated with a higher rank (Baker et al., 1988). Merit-based promotions in the military have received increasing attention in recent years. Defense Secretary Ash Carter has proposed a major overhaul of the way the military evaluates and promotes its service members, stressing merit over seniority (Tilghman, 2015). For line officers, promotions based on merit depend on evaluation of service members’ readiness for their combat mission. For medical personnel, however, promotions are not based on readiness for their combat medical mission. Therefore, while promotion serves as a strong incentive for line and infantry personnel to perform optimally and make readiness a priority, promotion incentives for medical personnel are misaligned. The absence of a clear measure by which line and medical leaders can be held accountable for the trauma system’s performance and casualty outcomes (Rotondo et al., 2011) is a barrier to leveraging this incentive mechanism to drive improvement.
In some cases, requirements for promotion can act as a disincentive. The committee heard, for example, that experienced nurses must shift from patient care to administrative positions in order to obtain the experience necessary for continued promotion4 (Wilmoth, 2016). Physicians face similar pressures (LaFraniere, 2014). Current promotion structures thus do not encourage or reward the growth of clinical trauma-focused expertise, reducing the pool of senior-level clinicians available at the point of care to shepherd continuous performance improvement efforts.
Civilian Sector
In the civilian sector, measures and financial incentives play a large role in current health care reform initiatives. For decades, the civilian sector operated under a largely fee-for-service payment system. Fee-for-service, however, leads to increased costs by rewarding providers for the complex-
__________________
4 Unlike the medical corps, nursing is not exempt from the promotion system of the Defense Officer Personnel Management Act.
ity and number of medical services provided (James, 2012). Unsurprisingly, more intense care does not necessarily equate to better outcomes, and can even prove harmful to patients (Chen et al., 2010; Fisher et al., 2003).
In the face of widespread recognition of serious deficiencies in the U.S. health care system, highlighted in the landmark IOM (2001) report Crossing the Quality Chasm: A New Health System for the 21st Century, policy makers and private and public payers have encouraged pay-for-performance initiatives as a way to realign the system’s incentive structure to encourage improvement in the quality, efficiency, and value of care (Miller, 2009). As a result, experimentation with a variety of financial incentives is under way. Payment-based strategies include incentive payments for processes (e.g., care coordination), penalties for unwanted outcomes (e.g., hospital-acquired infections), and shared accountability payment methods (e.g., bundled payment) (IOM, 2013). However, the evidence base is not yet robust enough to demonstrate the effectiveness of current strategies, and further investigation of different care delivery and financing approaches (e.g., through pilots) is needed and is under way to gauge impacts on health and cost measures and identify unintended consequences. Although pilots are being conducted on a small scale by private payers, the Center for Medicare & Medicaid Innovation at the Centers for Medicare & Medicaid Services (CMS) was established to identify, test, and diffuse new payment and service delivery models to reduce expenditures while maintaining or improving quality of care for CMS beneficiaries. If innovative care delivery models demonstrate evidence of cost reductions and/or improvements in outcomes, the U.S. Department of Health and Human Services (HHS) has the authority to expand those models without congressional action (CMS, 2015).
Trauma care is not encompassed within current health care reform efforts. CMS, as the nation’s largest payer organization for trauma care,5 has significant influence over how such care is delivered through the use of health care payment policies, and thus is well positioned to lead the development of innovative approaches to improving trauma care while lowering costs. However, the distribution of trauma care across the prehospital, hospital, and outpatient (post-acute care) settings raises some challenges to the use of financial incentives to drive changes in trauma care practice. As discussed above, there is currently no standard set of quality measures (e.g., National Quality Forum measures) that can be used to evaluate the performance of trauma systems. One can imagine a shared savings model applied to trauma care—for example, with a bundled payment to a region’s EMS organizations, emergency departments, and trauma center or centers—that
__________________
5 Combined, Medicare and Medicaid account for more than half of trauma care reimbursements (Velopulos et al., 2013).
would entail measuring the contribution of the system in the aggregate and each provider type to patient outcomes. However, given the current state of data capture and integration across the trauma care continuum (see Chapter 4), implementing regional measures, although optimal, is currently not feasible. In the face of these challenges, an alternative to pay-for-performance incentives that has been piloted as a means of improving trauma care is the pay-for-participation model, a minimal-risk method of encouraging engagement in regional quality initiatives (see Box 7-4).
Beyond bundled payment, another particularly powerful lever available to CMS for effecting change is its “conditions of participation” for designated provider types.6 To qualify for Medicare certification and reimbursement, health services providers must comply with these minimum health and safety standards, which are considered baseline requirements. Trauma system elements critical to continuous quality improvement (data collection systems, performance improvement programs) could be considered conditions of participation for all components of the care continuum. For the prehospital care component of the continuum, however, use of this approach would require including EMS as a provider type through legislative changes to the Social Security Act. EMS is currently considered a supplier of transportation under the Social Security Act and therefore is not subject to conditions of participation for providers.
The EMS reimbursement model used by CMS reimburses on the basis of transport to a medical facility (miles traveled to an emergency department and the level of service provided while en route). This “fee-for-transport” model, emulated by many other payers, ignores the increasingly complex care and lifesaving interventions performed by EMS providers at the point of injury and while en route (IOM, 2007a). This model thus represents an extreme misalignment of incentives. The fact that payers will deny reimbursement should transport not occur discourages EMS agencies from making determinations regarding the need for transport to a hospital, and as many as 11 to 61 percent of EMS transports to emergency departments are medically unnecessary (Gratton et al., 2003). These unnecessary transports add costs to the health care system, further burden hospital-based providers, limit the ability to respond to disasters, and hinder the implementation of processes that would allow EMS providers to transport patients to a more appropriate setting or treat and release (IOM, 2007a). Present EMS reimbursement practices thus act in direct opposition to the committee’s vision of a learning trauma care system. As national efforts to link health care to quality proceed, EMS is being left behind.
__________________
6 Provider types are specified in the Social Security Act.
ESTABLISHING OWNERSHIP
Defined leadership with comprehensive authority is necessary to shape and maintain a learning system’s culture, infrastructure, planning, oversight, and future development and to create and enforce policy and guidelines (DHB, 2015). Absent clear, consolidated leadership, limited progress will be made. With regard to leadership for trauma care, the committee observed the same fundamental challenge in the military and at the national level: no one owns trauma care. Fragmentation, silos, competing political interests, ambiguity of leadership, and conflicting aims are far too common in trauma care in both the military and civilian sectors and across the care continuum.
Military Sector
The gains in military trauma care made over the past two decades are significant. The refinement of a joint and successful tiered system of battlefield care and transport required learning, innovation, and attention to details of logistics and design. Similarly, advances in technical, clinical trauma care—such as new fluid resuscitation methods and tourniquet use—arose from agility, knowledge management, and the use of focused empiricism (described in Chapter 4) as an invaluable learning method. Many of these advances could not have occurred without assistance and encouragement (or at least tacit permission) from military leaders, but many appear to have come in fact from rather informal, entrepreneurial, emergent bottom-up ac-
tivities by people at various levels of seniority and without official guidance or direction. In effect, with respect to improvement in military trauma care, deep commitment from individuals has substituted in some ways for formal programs, systems, and command structures. This bottom-up change is an integral component of a learning system.
At the same time, a result of this process for change is that structures and offices that have emerged report to entities that may not have the ability to effect change, and they appear to have a somewhat ambiguous status and uncertain longevity within DoD’s Military Health System. The JTS, for example, has produced measureable success in advancing trauma care and saving lives on the battlefield over the past decade, yet despite this success, its influence, its scope, and even its very existence are threatened at present, given its lack of doctrinal authority,7 resources, and reporting structure (DHB, 2015; Rotondo et al., 2011). Although it was conceptually designed to serve as a consulting agency, the JTS’s impact is limited largely to Central Command (CENTCOM) because DoD has neither formalized its role nor developed any requirements for it to take part in or help develop a DoD-wide trauma system. With the exception of the Pacific Command, which is working proactively with the JTS to establish a Joint Theater Trauma System, the efforts of the JTS to engage other combatant commands have received limited response (Gross, 2015). Thus, the committee sees a paradox: creditable and necessary gains in trauma care during both wars in Afghanistan and Iraq, but weak or nonexistent formal joint structures to ensure that those gains are perpetuated (particularly during the interwar period), stable, and distributed uniformly across the combatant commands and services.
In the absence of standardization of a formal trauma system across all combatant commands, the many lessons learned over the course of the wars in Afghanistan and Iraq and the improvements made in combat casualty care may be lost. Maintaining these advances and a state of readiness will require continuous investment and commitment from the highest levels of DoD leadership. Otherwise, capabilities and outcomes will remain the same or deteriorate, instead of improving (Hoyt, 2015a; Winchell et al., 2015). This capability gap could be addressed if the Joint Requirements Oversight Council utilized the Joint Capabilities Integration and Development System process (see CJCSI, 2015) and made an all-of-DoD approach to trauma care a priority.
Ambiguity in trauma care ownership and instability of the nascent
__________________
7 Doctrine is the formal documentation of how military forces are to execute a specific military task. It establishes a framework for standardizing the conduct of operations and describes theory, history, practice, and lessons learned to ensure that operations across the military departments are consistent, repeatable, and reliable in their desired outcomes (DoD, 2016).
trauma system infrastructure are especially consequential with regard to an essential role of the Military Health System: readiness to deliver trauma care in support of the full range of military operations. Evidence of suboptimal trauma care and outcomes at the start of the wars in Afghanistan and Iraq—including a high rate of preventable battlefield deaths—testifies to gaps in trauma care readiness and a workforce inadequately trained to ensure that expert trauma care would be available for the very first (and last) casualty on the battlefield. As discussed in Chapter 5, it is not difficult to see why: the Military Health System lacks a sufficient volume of trauma cases to train and preserve expertise in a mission-ready trauma care workforce. Briefly put, line commanders assume Military Health System leaders will deliver providers expert in trauma care, while Military Health System leaders’ priority is beneficiary care, and they have limited financial resources and personnel to develop programs that would create a robust cadre of multidisciplinary trauma experts.
This conundrum is pervasive across the military, yet no single agent or agency appears to be responsible for addressing this gap. Despite several recent evaluations (summarized in Table 7-1) recommending the establishment of a unified medical command or the designation of a senior medical leader, directorate, or division solely responsible for combat casualty care, DoD continues to lack a unifying lead agency with the authority, oversight, and resources to lead all aspects of combat casualty care and readiness (DHB, 2015; Mabry, 2015; Maldon et al., 2015; Rotondo et al., 2011). Responsibility for the training and delivery of combat casualty care remains widely distributed across the Assistant Secretary of Defense for Health Affairs, the Defense Health Agency, the services, and the combatant
| Key Findings | Recommendations |
|---|---|
| Rotondo et al., 2011 The United States Military Joint Trauma System Assessment |
|
| “The Joint Trauma System (JTS) has no authority to develop or set policy or standards for trauma care.” | The JTS should be established as the statutory lead agency, authorized to set policy and enforce standards of care. It should be elevated within the U.S. Department of Defense (DoD) and given sustained support to be better aligned with its considerable responsibilities. |
| Key Findings | Recommendations |
|---|---|
| Kotwal et al., 2013 Saving Lives on the Battlefield |
|
| Best practices in prehospital military trauma care were implemented unevenly and sporadically, in part because of the lack of a “clearly responsible organization” and ownership of casualty care. | The JTS should be designated as the lead agency for trauma care. |
| Defense Health Board, 2015 Combat Trauma Lessons Learned from Military Operations of 2001–2013 |
|
| “Despite vast improvements in the military trauma care system achieved over the past decade, no unifying agency has oversight over all aspects of the combat casualty care system.” The Defense Health Board concurs with assessment of earlier reports regarding the need for a lead agency for the combat casualty care system. | A senior-level organization should be established as the lead agency. This agency should “continually assess the system’s structure, function, resources, and outcomes,” and be able to recommend policies that would standardize trauma care across DoD. |
| Maldon et al., 2015 Report of the Military Compensation and Retirement Modernization Commission |
|
| Advances in combat care have been unevenly implemented, and these advances are in danger of degrading during peacetime. | A Joint Readiness Command, led by a four-star general/flag officer, should be established and held responsible for the readiness of the military medical force and for the development of joint policies and requirements for medical care. |
| Butler et al., 2015 Implementing and Preserving the Advances in Combat Casualty Care from Iraq and Afghanistan Throughout the U.S. Military |
|
| “Divided and overlapping responsibilities and authorities create challenges to optimizing trauma care across an enterprise as large and complex as DoD.” | “The JTS should be a permanent entity within the Military Health System. Responsibility for managing and overseeing the JTS should rest at a senior and joint position within the DoD. The JTS should be empowered and resourced to act as the DoD’s lead organization for trauma care. The JTS should serve as a direct resource for the battlefield trauma care provider, senior military medical leaders, the military Services, and the Combatant Commands.” |
commands (see Box 7-5), with the consequence that no single organization or agency official “owns” or is accountable for DoD’s medical readiness mission (Butler et al., 2015). With respect to the assurance of continuous practice improvement, learning, and readiness in battlefield trauma care, no one is in charge—a reality at odds with a military system known and revered for the integrity and quality of its command and control methods.
This diffusion of responsibility is especially poignant on the battlefield. While the surgeons general have oversight over policy within their respective services, final authority and responsibility for the delivery of combat casualty care—including control over budget, personnel, training, and equipment—is assigned to combatant commanders (Mabry, 2015). These line leaders are highly focused on mission (national defense) and lack medical expertise, while medical leaders are focused on maximizing fitness and health and optimizing ways to reduce health risks. Although combatant commanders are structurally tasked with delivering optimal health and trauma care, they lack the numbers of trained personnel needed to deliver expert trauma care at all levels across the battlefield. While medical risks are considered, mission needs appropriately take precedence over medical concerns (e.g., diversion of helicopters from operations for casualty evacuation). Thus there is an ongoing tension between the medical and combat missions that, in some cases, can be resolved only with commitment and a clear message from the highest level, as exemplified by Secretary Gates’s Golden Hour Policy (see Box 7-6). The critical importance of direction originating from the Secretary of Defense has been recognized from within DoD itself—without it, “there is no assurance that advances in trauma care will be implemented consistently throughout the various components of the U.S. Military” (Butler et al., 2015, p. 323).
The consequences of the lack of ownership for combat casualty care include ineffective investment in trauma readiness and variation within and across combatant commands. Successful combat casualty care is a blend of both tactics and medicine, and it thus ideally would have the attention and support of combatant commanders (Kotwal et al., 2013). The successful history of the 75th Ranger Regiment, summarized previously, offers a compelling and informative counterexample of the unsurpassed outcomes that can emerge when the line commander takes full responsibility for the vitality and aims of a combat casualty care system: lives are saved. Equally compelling are the results when line leadership does not take this responsibility (see Box 7-7).
There have been efforts by some Military Health System leaders to change the current situation. However, structures and culture need to change if this deficit is to be addressed. Initially, greater clarity will be necessary to identify who in the military is responsible, in the final analysis, for the quality, learning processes, and readiness of military trauma care both in
peacetime and during conflicts. As always, with that responsibility must come the relevant authorities and resources—when those are unlinked, the responsibility lacks relevance. Further, as exemplified by the 75th Ranger Regiment, the culture of accountability will have to shift such that there is widespread understanding and acceptance among medical and nonmedical leadership that line commanders have a primary role in and must be engaged in the readiness of their forces to deliver optimal combat casualty care.
Civilian Sector
Since 1966, civilian trauma systems have developed in many areas of the country to varying degrees of maturity, resulting in varying levels of outcomes. This variation is due largely to a lack of national leadership, policy guidance, standardization, coordination, and metrics and incentives tied to outcomes. As discussed in Chapter 2, no single federal entity is accountable for trauma care or trauma system development in the United States. Most trauma systems are regional, coordinated at the state level through respective department of health or EMS offices. Consequently, the role of local, state, and federal government in U.S. civilian trauma care systems is variable and inconsistent, leaving authority and accountability for trauma capabilities fragmented and varying from location to location. Government leadership at the state and federal levels is highly variable with respect to knowledge of the need for and the value and function of a trauma system. Other critical constituents, including academic health systems, the
insurance industry, professional societies, and private industry, may have divergent values, contributing further to fragmentation. The result of this patchwork of systems for trauma care is mortality that varies twofold between the best and worst trauma centers in the nation (Hashmi et al., 2013). Mechanisms for examining variability across entire trauma systems do not even exist.
As in the military, the civilian trauma care sector appears to be ill equipped at present to set bold aims, as counseled by the IOM (2013) report Best Care at Lower Cost in its description of a learning health system. Advances do unquestionably occur, but it would be difficult under current circumstances to imagine anyone with the authority to declare, for example, that “zero preventable deaths after injury” ought to become a national goal. This represents a loss for the nation, since trauma deaths that could be averted with uniform best practices certainly number in the tens of thousands every year (Hashmi et al., 2016). Strong and capable civil society organizations8 do what they can to improve the quality of trauma care, but none has the authority to require the pursuit of this improvement.
In principle, the gaps in civilian trauma care practice and learning highlighted throughout this report suggest that clearer and more cogent leadership is needed, supported by a framework that defines national aims and system designs and includes trauma care in health care delivery reform efforts. As noted, this leadership appointment needs to be accompanied by responsibility, funding, and authority. This need for leadership is exemplified at present by the proliferation of trauma centers in some geographic areas, driven by business opportunities rather than true regional needs (Johnson, 2015). In some areas, the number of Level I and II trauma centers exceeds the number needed to concentrate the patient volumes shown to correlate with improved trauma care quality and outcomes (ACS, 2015b; Eastman et al., 2013). Absent leadership in planning at the national, state, and regional levels, this costly and disruptive trend may proceed unabated, with unfavorable implications for public health, costs, and safety. To determine the future course of trauma care in the United States, the following question must be answered: Is the American public willing to accept that, after a severe injury, where one lives may determine whether one lives? If the nation’s expectation is that variability in quality and outcomes based purely on geography is unacceptable, current systems for accountability need to be reexamined.
As in the military, the trauma care system in the civilian sector has witnessed a strong record of inaction or inadequate action in response to
__________________
8 While not comprehensive, a list of trauma-related associations is noted on the National Trauma Institute website: http://www.nationaltraumainstitute.org/home/trauma_related_organizations.html (accessed May 23, 2016).
widespread calls for more national-level leadership. The National Highway Traffic Safety Administration’s Trauma System Agenda for the Future, released in 2004, envisions a National Trauma System Leadership Council “to advocate for system development, serve as the locus for policy development and support, and coordinate the work of Federal agencies and professional organizations with injury-related programs” (NHTSA, 2004). However, no such council has been established. Likewise, the IOM’s Future of Emergency Care series recommends that Congress establish a lead federal agency for trauma and emergency care9 (inclusive of prehospital care) to be housed within HHS. The IOM Committee on the Future of Emergency Care in the United States deemed this lead federal agency necessary to
- serve as a federal advocate for trauma and emergency care, increasing its visibility within the government and among the public;
- move existing fragmented systems toward improved integration;
- provide unified and consistent federal leadership on policy development and funding;
- represent all providers and settings (to include the entire continuum of care); and
- create unified accountability for the performance of the trauma and emergency care system (IOM, 2007b).
Other individuals and organizations have called for the establishment of a federal home for emergency care within the federal government, but again, no such entity has emerged. While executive action did prompt the creation of the Emergency Care Coordination Center, this center is unfunded and thus extremely limited in its effect (Carr, 2015). Lacking authority and resources, by no means does this center approach the intent of the lead agency envisioned 10 years ago by the IOM Committee on the Future of Emergency Care in the United States. The present committee agrees with and supports previous assessments regarding the need for defined leadership for trauma and emergency care within HHS that serves to promote the integration of services across the continuum of care, from prehospital to rehabilitation and post-acute care.
__________________
9 Civilian trauma care differs from military trauma care in that it is more fully part of a larger emergency response system that provides care for many other time-critical health problems (e.g., stroke and myocardial infarction). Although needs related to the larger civilian emergency care system are beyond the scope of this report, the committee acknowledges that the leadership structures that can help improve civilian trauma care are highly likely to have overall emergency care improvement in mind.
Military–Civilian Leadership Partnerships
From the viewpoint of the committee, given its charge, the one inescapable conclusion about the need for stronger trauma system leadership and accountability at the national level relates to the core trauma care readiness mission of the military. As discussed in Chapter 5, the Military Health System lacks sufficient volumes of trauma patients within MTFs to train and maintain a mission-ready trauma care workforce. Consequently, the military needs to work with the civilian sector to advance best trauma care practices through collaborative research initiatives (see Chapter 4). Through its research and deliberations for this study, the committee determined that the only feasible solution is to forge a significant and ambitious partnership between the military and civilian sectors such that the civilian sector can serve as a reservoir and innovative engine for trauma care knowledge and a training platform for the military trauma care workforce during the interwar period. In addition, the integration of military and civilian trauma care is necessary to ensure the full transfer of lessons learned between the two sectors and thereby improve civilian trauma care outcomes. This latter point is important, since (as discussed in Chapter 1) the burden of trauma in the civilian sector (approximately 148,000 deaths per year) numerically dwarfs the burden among military personnel (approximately 6,850 deaths over a decade of war); thus ensuring that the best conceivable civilian trauma care can avert tremendous morbidity and mortality.
The committee discovered a number of formal and informal pathways through which the military and civilian trauma care systems currently exchange ideas and knowledge (as discussed in Chapter 2). Instances of formalized leadership-level collaboration have emerged, for example, in the prehospital setting with the Federal Interagency Committee on EMS (FICEMS, 2013; IOM, 2007a) and, for trauma surgery, the Military Health System/ACS Strategic Partnership (Hoyt, 2015b). However, where successful collaboration has occurred, it has depended largely on the drive, good will, and personal investment of key individuals in leadership positions. As a result, the sustainability of collaborative efforts is threatened when changes in personnel take place (IOM, 2007b).
As yet, a durable collaborative effort encompassing the entire continuum of trauma care with representation of all stakeholders, military and civilian, does not exist. Consequently, diffusion of knowledge across sectors is slow and incomplete, care is not optimal, and lives are placed in jeopardy. As discussed in Chapter 4, for example, tourniquet use in civilian trauma care is growing, but its penetration is far from complete (Haider et al., 2015). The absence of such all-encompassing collaboration does not signal that this task is impossible and not worth attempting. Successful examples of the emergence of defined leadership and national collaboration
on related aspects of trauma care (e.g., hemorrhage control) or on specific subsets of traumatic injury (e.g., traumatic brain injury) demonstrate that this type of collaboration is possible and impactful. The obstacle has not been the good will of individuals, but the institutional lack of will among leadership.
The enormous burden of trauma and the importance of an optimally functioning national trauma system to the nation’s health and national security make the need for national leadership that cuts across both military and civilian sectors all the more pressing and relevant. National leadership would help unify and ensure collaboration among existing efforts and points of authority spread not just across federal agencies but among state and local governments and professional organizations as well. The success of the hemorrhage control and traumatic brain injury movements suggests strategies and mechanisms for encouraging effective collaborative action as well as national leadership on trauma care in its entirety (see Box 7-8 for an overview of these positive examples).
SUMMARY OF FINDINGS AND CONCLUSIONS
CONCLUSION: The absence of a comprehensive, standardized process by which the military and civilian sectors engage in system-level trauma care quality improvement impedes learning, continuous improvement, and the bidirectional translation of best practices and lessons learned.
Related findings:
- In both the military and civilian sectors, performance transparency at the provider and system levels is lacking.
- Military participation in national trauma quality improvement collaboratives is minimal; only a single military hospital participates in an ACS TQIP benchmarking program.
CONCLUSION: A national system-based and patient-centered approach to prehospital trauma care is needed in the civilian sector to incentivize improved care delivery, the rapid broad translation of military best practices, reduced provider and system variability, uniform data collection and performance improvement, and integration with hospital trauma systems so that comprehensive trauma care can be evaluated for quality performance. However, designation of emergency medical services as a supplier of transportation under the Social Security Act impedes the seamless integration of prehospital care into the trauma care continuum and its alignment with health care reform efforts.
Related findings:
- No process exists for benchmarking trauma system performance across the entire continuum of care within, across, and between the military and civilian sectors.
- The absence of standard, national quality metrics for trauma care and present reimbursement practices for civilian EMS (i.e., pay-for-transport) are major impediments to the integration of prehospital care into the trauma care continuum.
CONCLUSION: Given current structures and diffusion of authority within DoD, the Military Health System and the line commands are not able to ensure and maintain trauma care readiness in peacetime, ensure
rapid transfer of best trauma care knowledge across DoD commands or between the military and civilian sectors, or ensure the availability of the infrastructure needed to support a learning trauma care system.
Related findings:
- Promotion incentives for military medical personnel are misaligned; current promotion structures do not encourage or reward the growth of clinical trauma-focused expertise.
- Within the military leadership structure, there is no overarching authority responsible for ensuring medical readiness to deliver combat casualty care.
CONCLUSION: The lack of formal, funded mechanisms for coordination, communication, and translation has led to inefficiency and variation across the civilian sector in clinical care practices, education and training, research efforts, and continuous performance improvement. Collectively, these deficiencies have contributed to suboptimal outcomes for injured patients in the United States and tens of thousands of preventable deaths after injury each year.
Related findings:
- Authority and accountability for civilian trauma care capabilities are fragmented and vary from location to location, resulting in a patchwork of systems for trauma care in which mortality varies twofold between the best and worst trauma centers in the nation.
- There is no single federal entity accountable for trauma care or trauma system development in the United States.
CONCLUSION: Despite the tremendous societal burden of trauma, the absence of a unified authority to encourage coordination, collaboration, and alignment across and within the military and civilian sectors has led to variation in practice, suboptimal outcomes for injured patients, and a lack of national attention and resources directed toward trauma care.
Related findings:
- The lack of integration of military and civilian trauma care has impeded a highly functioning military trauma care system and the full transfer of lessons learned between the two sectors.
- Previous White House-led national initiatives have helped unify and ensure collaboration among existing efforts and points of authority spread across military and civilian federal agencies, state and local governments, and professional organizations.
REFERENCES
ACS (American College of Surgeons). 2014. Resources for optimal care of the injured patient. Chicago, IL: ACS.
ACS. 2015a. Getting started. https://www.facs.org/quality-programs/trauma/tqip/getting-started (accessed December 22, 2015).
ACS. 2015b. Statement on trauma center designation based upon system need. http://bulletin.facs.org/2015/01/statement-on-trauma-center-designation-based-upon-system-need (accessed December 10, 2015).
ACS. 2015c. Strategies to enhance survival in active shooter and intentional mass casualty events: A compendium. ACS Bulletin Supplemental 100(Suppl. 1):1-90.
ACS. 2015d. TQIP services. https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/tqipservices.ashx (accessed December 22, 2015).
ACS. 2015e. Trauma Quality Improvement Program. https://www.facs.org/quality-programs/trauma/tqip (accessed December 22, 2015).
Al-Shaqsi, S. 2010. Response time as a sole performance indicator in EMS: Pitfalls and solutions. Open Access Emergency Medicine 2:1-6.
Ardolino, A., G. Sleat, and K. Willett. 2012. Outcome measurements in major trauma—results of a consensus meeting. Injury 43(10):1662-1666.
Bailey, J. A., J. J. Morrison, and T. E. Rasmussen. 2013. Military trauma system in Afghanistan: Lessons for civil systems? Current Opinion in Critical Care 19(6):569-577.
Baker, G. P., M. C. Jensen, and K. J. Murphy. 1988. Compensation and incentives: Practice vs. theory. Journal of Finance 43(3):593-616.
Butler, F. K., D. J. Smith, and R. H. Carmona. 2015. Implementing and preserving the advances in combat casualty care from Iraq and Afghanistan throughout the US military. Journal of Trauma and Acute Care Surgery 79(2):321-326.
Carr, B. G. 2015. Leadership and accountability: The Emergency Care Coordination Center. Paper presented to the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, Meeting Two, July 23-24, Washington, DC.
Champion, H. R., M. S. Mabee, and J. W. Meredith. 2006. The state of US trauma systems: Public perceptions versus reality—implications for US response to terrorism and mass casualty events. Journal of the American College of Surgeons 203(6):951-961.
Chen, L. M., A. K. Jha, S. Guterman, A. B. Ridgway, E. J. Orav, and A. M. Epstein. 2010. Hospital cost of care, quality of care, and readmission rates: Penny wise and pound foolish? Archives of Internal Medicine 170(4):340-346.
CJCSI (Chairman of the Joint Chiefs of Staff Instruction). 2015. Joint Capability Integration and Development System (JCIDS). CJCSI 3170.01I. https://dap.dau.mil/policy/Documents/2015/CJCSI_3170_01I.pdf (accessed February 1, 2016).
CMS (Centers for Medicare & Medicaid Services). 2015. About the CMS Innovation Center. https://innovation.cms.gov/About/index.html (accessed March 9, 2016).
DHA (Defense Health Agency). 2014. The Defense Health Agency: Reflections on our first year and future. Washington, DC: DHA.
DHB (Defense Health Board). 2015. Combat trauma lessons learned from military operations of 2001-2013. Falls Church, VA: DHB.
DHS (U.S. Department of Homeland Security). 2015. Stop the bleed. http://www.dhs.gov/stopthebleed (accessed February 17, 2016).
DHS. 2016. Partner efforts to support the bystander “Stop the Bleed” initiative. http://www.dhs.gov/efforts-support-stop-bleed (accessed February 17, 2016).
DoD (U.S. Department of Defense). 2014. Military Health System review: Final report to the Secretary of Defense. Washington, DC: DoD.
DoD. 2016. Department of Defense dictionary of military and associated terms: Joint publication 1-02. Washington, DC: DoD.
DoD, VA (U.S. Department of Veterans Affairs), HHS (U.S. Department of Health and Human Services), and ED (U.S. Department of Education). 2013. National Research Action Plan: Responding to the executive order improving access to mental health services for veterans, service members, and military families (August 31, 2012). Washington, DC: DoD, VA, HHS, and ED.
Eastman, A. B., E. J. MacKenzie, and A. B. Nathens. 2013. Sustaining a coordinated, regional approach to trauma and emergency care is critical to patient health care needs. Health Affairs 32(12):2091-2098.
Eastridge, B. J., G. Costanzo, D. Jenkins, M. A. Spott, C. Wade, D. Greydanus, S. Flaherty, J. Rappold, J. Dunne, J. B. Holcomb, and L. H. Blackbourne. 2009. Impact of joint theater trauma system initiatives on battlefield injury outcomes. American Journal of Surgery 198(6):852-857.
Eastridge, B. J., R. L. Mabry, P. Seguin, J. Cantrell, T. Tops, P. Uribe, O. Mallett, T. Zubko, L. Oetjen-Gerdes, T. E. Rasmussen, F. K. Butler, R. S. Kotwal, J. B. Holcomb, C. Wade, H. Champion, M. Lawnick, L. Moores, and L. H. Blackbourne. 2012. Death on the battlefield (2001-2011): Implications for the future of combat casualty care. Journal of Trauma and Acute Care Surgery 73(6 Suppl. 5):S431-S437.
EMS Compass. 2015a. About performance measures. http://emscompass.org/about-performancemeasures/#extensiveprocess (accessed February 17, 2016).
EMS Compass. 2015b. History. http://www.emscompass.org/about-performance-measures/history (accessed February 17, 2016).
EMSPIC (EMS Performance Improvement Center). 2016a. PreMIS. https://www.emspic.org/applications/premis (accessed February 16, 2016).
EMSPIC. 2016b. Who we are. https://www.emspic.org/about (accessed February 16, 2016).
FICEMS (Federal Interagency Committee on EMS). 2013. Five-year strategic plan. Washington, DC: FICEMS.
Fisher, E. S., D. E. Wennberg, T. A. Stukel, D. J. Gottlieb, F. L. Lucas, and É. L. Pinder. 2003. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Annals of Internal Medicine 138(4):273-287.
Gainor, D. 2015. EMS in the context of a learning health system. Paper presented to the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, October 26, Washington, DC.
Garvin, D. A., A. C. Edmondson, and F. Gino. 2008. Is yours a learning organization? Harvard Business Review 86(3):109.
Gates, R. M. 2014. Duty: Memoirs of a secretary at war. New York: Alfred A. Knopf.
Gratton, M. C., S. R. Ellison, J. Hunt, and O. J. Ma. 2003. Prospective determination of medical necessity for ambulance transport by paramedics. Prehospital Emergency Care 7(4):466-469.
Gross, K. 2015. Joint Trauma System. Paper presented to the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, Meeting One, May 18-19, Washington, DC.
Gruen, R. L., B. J. Gabbe, H. T. Stelfox, and P. A. Cameron. 2012. Indicators of the quality of trauma care and the performance of trauma systems. British Journal of Surgery 99(Suppl. 1):97-104.
Haas, B., D. Gomez, B. Zagorski, T. A. Stukel, G. D. Rubenfeld, and A. B. Nathens. 2010. Survival of the fittest: The hidden cost of undertriage of major trauma. Journal of the American College of Surgeons 211(6):804-811.
Haider, A. H., L. C. Piper, C. K. Zogg, E. B. Schneider, J. A. Orman, F. K. Butler, R. T. Gerhardt, E. R. Haut, J. P. Mather, and E. J. MacKenzie. 2015. Military-to-civilian translation of battlefield innovations in operative trauma care. Surgery 158(6):1686-1695.
Hashmi, Z. G., J. B. Dimick, D. T. Efron, E. R. Haut, E. B. Schneider, S. N. Zafar, D. Schwartz, E. E. Cornwell, 3rd, and A. H. Haider. 2013. Reliability adjustment: A necessity for trauma center ranking and benchmarking. Journal of Trauma and Acute Care Surgery 75(1):166-172.
Hashmi, Z. G., S. Zafar, T. Genuit, E. R. Haut, D. T. Efron, J. Havens, Z. Cooper, A. Salim, E. E. Cornwell III, and A. H. Haider. 2016. The potential for trauma quality improvement: One hundred thousand lives in five years. http://www.asc-abstracts.org/abs2016/15-12-the-potential-for-trauma-quality-improvement-one-hundred-thousandlives-in-five-years (accessed February 21, 2016).
Haut, E. R., N. C. Mann, and R. S. Kotwal. 2016. Military Trauma Care’s Learning Health System: The importance of data-driven decision making. Paper commissioned by the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector. nationalacademies.org/TraumaCare.
Hemmila, M. R., A. B. Nathens, S. Shafi, J. F. Calland, D. E. Clark, H. G. Cryer, S. Goble, C. J. Hoeft, J. W. Meredith, M. L. Neal, M. D. Pasquale, M. D. Pomphrey, and J. J. Fildes. 2010. The Trauma Quality Improvement Program: Pilot study and initial demonstration of feasibility. Journal of Trauma 68(2):253-262.
Holcomb, J. B., L. G. Stansbury, H. R. Champion, C. Wade, and R. F. Bellamy. 2006. Understanding combat casualty care statistics. Journal of Trauma 60(2):397-401.
Hoyt, D. B. 2015a. Leadership and accountability. Paper presented to the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, Meeting Two, July 23-24, Washington, DC.
Hoyt, D. B. 2015b. Looking forward—February 2015. Bulletin of the American College of Surgeons, February 1. http://bulletin.facs.org/2015/02/looking-forward-february-2015 (accessed October 28, 2015).
IOM (Institute of Medicine. 2001. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press.
IOM. 2007a. Emergency medical services: At the crossroads. Washington, DC: The National Academies Press.
IOM. 2007b. Hospital-based emergency care: At the breaking point. Washington, DC: The National Academies Press.
IOM. 2013. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: The National Academies Press.
James, J. 2012. Health policy brief: Pay-for-performance. Health Affairs, October 11. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=78 (accessed February 5, 2016).
Johnson, S. R. 2015. Better funding means trauma center shortage may become a glut. Modern Healthcare, November 28. http://www.modernhealthcare.com/article/20151128/MAGAZINE/311289988 (accessed February 16, 2016).
Kotwal, R. S., H. R. Montgomery, B. M. Kotwal, H. R. Champion, F. K. Butler, Jr., R. L. Mabry, J. S. Cain, L. H. Blackbourne, K. K. Mechler, and J. B. Holcomb. 2011. Eliminating preventable death on the battlefield. Archives of Surgery 146(12):1350-1358.
Kotwal, R. S., F. K. Butler, E. P. Edgar, S. A. Shackelford, D. R. Bennett, and J. A. Bailey. 2013. Saving lives on the battlefield: A Joint Trauma System review of pre-hospital trauma care in Combined Joint Operating Area-Afghanistan (CJOA-A). https://www.naemt.org/docs/default-source/education-documents/tccc/10-9-15-updates/centcom-prehospitalfinal-report-130130.pdf?sfvrsn=2 (accessed January 13, 2015).
Kotwal, R. S., J. T. Howard, J. A. Orman, B. W. Tarpey, J. A. Bailey, H. R. Champion, R. L. Mabry, J. B. Holcomb, and K. R. Gross. 2016. The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surgery 151(1):15-24.
Kragh, J. F., Jr., T. J. Walters, T. Westmoreland, R. M. Miller, R. L. Mabry, R. S. Kotwal, B. A. Ritter, D. C. Hodge, D. J. Greydanus, J. S. Cain, D. S. Parsons, E. P. Edgar, T. Harcke, D. G. Baer, M. A. Dubick, L. H. Blackbourne, H. R. Montgomery, J. B. Holcomb, and F. K. Butler. 2013. Tragedy into drama: An American history of tourniquet use in the current war. Fort Belvoir, VA: Defense Technical Information Center.
LaFraniere, S. 2014. Military hospital care is questioned; next, reprisals. New York Times, December 20. http://www.nytimes.com/2014/12/21/us/military-hospital-care-is-questionednext-reprisals.html?_r=0 (accessed March 9, 2016).
Mabry, R. L. 2015. Challenges to improving combat casualty survivability on the battlefield. Joint Force Quarterly 76(1):78-84.
MacKenzie, E. J., F. P. Rivara, G. J. Jurkovich, A. B. Nathens, K. P. Frey, B. L. Egleston, D. S. Salkever, and D. O. Scharfstein. 2006. A national evaluation of the effect of trauma-center care on mortality. New England Journal of Medicine 354(4):366-378.
MacKenzie, E. J., S. Weir, F. P. Rivara, G. J. Jurkovich, A. B. Nathens, W. Wang, D. O. Scharfstein, and D. S. Salkever. 2010. The value of trauma center care. Journal of Trauma 69(1):1-10.
Maldon, A., L. L. Pressler, S. E. Buyer, D. S. Zakheim, M. R. Higgins, P. W. Chiarelli, E. P. Giambastiani, J. R. Kerrey, and C. P. Carney. 2015. Report of the Military Compensation and Retirement Modernization Commission: Final report. Arlington, VA: Military Compensation and Retirement Modernization Commission.
Mann, N. C., R. J. Mullins, E. J. MacKenzie, G. J. Jurkovich, and C. N. Mock. 1999. Systematic review of published evidence regarding trauma system effectiveness. Journal of Trauma 47(Suppl. 3):S25-S33.
Mears, G. D., D. Pratt, S. W. Glickman, J. H. Brice, L. T. Glickman, J. G. Cabanas, and C. B. Cairns. 2010. The North Carolina EMS data system: A comprehensive integrated emergency medical services quality improvement program. Prehospital Emergency Care 14(1):85-94.
Miller, H. D. 2009. From volume to value: Better ways to pay for health care. Health Affairs (Millwood) 28(5):1418-1428.
Morrison, J. E., and L. L. Meliza. 1999. Foundations of the after action review process. Alexandria, VA: U.S. Army Research Institute for the Behavioral and Social Sciences.
Nathens, A. B., G. J. Jurkovich, P. Cummings, F. P. Rivara, and R. V. Maier. 2000. The effect of organized systems of trauma care on motor vehicle crash mortality. Journal of the American Medical Association 283(15):1990-1994.
Nathens, A. B., H. G. Cryer, and J. Fildes. 2012. The American College of Surgeons Trauma Quality Improvement Program. Surgical Clinics of North America 92(2):441-454.
NHTSA (National Highway Traffic Safety Administration). 2004. Trauma system agenda for the future. Washington, DC: NHTSA.
NPSF (National Patient Safety Foundation). 2015. Shining a light: Safer health care through transparency. Boston, MA: NPSF.
NQF (National Quality Forum). 2005. National voluntary consensus standards for cardiac surgery. http://www.qualityforum.org/Publications/2005/01/National_Voluntary_Consensus_Standards_for_Cardiac_Surgery.aspx (accessed February 17, 2016).
NQF. 2006. National voluntary consensus standards for adult diabetes care: 2005 update. http://www.qualityforum.org/Publications/2006/09/National_Voluntary_Consensus_Standards_for_Adult_Diabetes_Care__2005_Update.aspx (accessed February 17, 2016).
NQF. 2009. National voluntary consensus standards for emergency care. http://www.qualityforum.org/Publications/2009/09/National_Voluntary_Consensus_Standards_for_Emergency_Care.aspx (accessed February 17, 2016).
NQF. 2010. National voluntary consensus standards for home health care—additional performance measures 2008. http://www.qualityforum.org/Publications/2010/10/National_Voluntary_Consensus_Standards_for_Home_Health_Care_%E2%80%94_Additional_Performance_Measures_2008.aspx (accessed February 17, 2016).
NQF. 2011. National voluntary consensus standards for nursing homes. http://www.qualityforum.org/Publications/2011/07/National_Voluntary_Consensus_Standards_for_Nursing_Homes.aspx (accessed Febuary 17, 2016).
Osborn, J. 2015. Professional organization perspectives on charge to the committee. Paper presented to the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, Meeting One, May 18-19, Washington, DC.
Pappas, C. G. 2001. The ranger medic. Military Medicine 166(5):394-400.
Performance.gov. 2015. Cross-agency priority goal: Service members and veterans mental health. Progress update. https://www.performance.gov/node/3405/view?view=public#progress-update (accessed February 17, 2016).
Pruitt, B. A., Jr., and T. E. Rasmussen. 2014. Vietnam (1972) to Afghanistan (2014): The state of military trauma care and research, past to present. Journal of Trauma and Acute Care Surgery 77(3 Suppl. 2):S57-S65.
Rotondo, M., T. Scalea, A. Rizzo, K. Martin, and J. Bailey. 2011. The United States military Joint Trauma System assessment: A report commissioned by the U.S. Central Command Surgeon, sponsored by Air Force Central Command, a strategic document to provide a platform for tactical development. Washington, DC: DoD.
Seigel, T. A., D. C. McGillicuddy, A. Z. Barkin, and C. L. Rosen. 2010. Morbidity and mortality conference in emergency medicine. Journal of Emergency Medicine 38(4):507-511.
Tilghman, A. 2015. Carter: Change promotion and retention rules. Military Times, March 30. http://www.militarytimes.com/story/military/pentagon/2015/03/30/secdefpromotion/70667178 (accessed February 5, 2016).
Veliz, C., H. Montgomery, and R. Kotwal. 2010. Ranger first responder and the evolution of tactical combat casualty care. Journal of Special Operations Medicine 10(3):90-91.
Velopulos, C. G., N. Y. Enwerem, A. Obirieze, X. Hui, Z. G. Hashmi, V. K. Scott, E. E. Cornwall, E. B. Schneider, and A. H. Haider. 2013. National cost of trauma care by payer status. Journal of Surgical Research 184(1):444-449.
Vizient. 2016a. Our networks. https://www.vizientinc.com/our-networks.htm#Networks-and-member-groups (accessed March 8, 2016).
Vizient. 2016b. Who we are. https://www.vizientinc.com/who-we-are.htm (accessed March 8, 2016).
Walters, T. J., D. S. Kauvar, D. G. Baer, and J. B. Holcomb. 2005. Battlefield tourniquets: Modern combat lifesavers. Army Medical Department Journal 42-43.
White House. 2012. Executive order—improving access to mental health services for veterans, service members, and military families. https://www.whitehouse.gov/the-pressoffice/2012/08/31/executive-order-improving-access-mental-health-services-veterans-service (accessed February 17, 2016).
White House. 2015. Don’t be a bystander: Find out how you can “Stop the Bleed.” https://www.whitehouse.gov/blog/2015/10/06/stop-bleed (accessed February 17, 2016).
Wilmoth, M. 2016. Nursing in the context of a learning trauma care system. Paper presented to the Committee on Military Trauma Care’s Learning Health System and Its Translation to the Civilian Sector, January 15, Washington, DC.
Winchell, R. J., N. Sanddal, J. Ball, H. Michaels, C. R. Kaufmann, R. Gupta, T. J. Esposito, and H. Subacius. 2015. A reassessment of the impact of trauma systems consultation on regional trauma system development. Journal of Trauma and Acute Care Surgery 78(6):1102-1110.




































