A Case Studies
As an aid to understanding the military trauma care learning health system and its translation to the civilian sector, and in accordance with the committee’s statement of task, this appendix presents case studies that illustrate a broad spectrum of battlefield injuries relevant also to the civilian sector: extremity hemorrhage, blunt trauma with vascular injury, pediatric burn, dismounted complex blast injury, and severe traumatic brain injury. Collectively, the cases provide information on the following topics specified in the committee’s statement of task:
- Levels of evidence used to develop military and civilian (as applicable) clinical guidelines for the spectrum of trauma care in each case.
- Pertinent innovative changes (devices, medications, equipment, methods) that have been incorporated into the spectrum of trauma care for each case as a result of the U.S. Department of Defense’s (DoD’s) evidence-based improvement process.
- Processes by which patient and injury information was collected, stored, reviewed and analyzed by the Joint Trauma System (JTS), including how this information was used for the JTS’s evidence-based improvement process and made available for clinical and epidemiologic research.
- How collection, storage, review and analysis of patient injury and management information differed for those killed in action versus those wounded in action (i.e., different system for those who die prior to arrival at a medical center, thus eliminating ability to study ways to improve survival).
- Impact that evidence-supported changes in military trauma care and the JTS’s evidence-supported process improvement may have had on survivability.
- How the results of the military’s Defense Health Program (DHP) research investment and elements of focused empiricism have been integrated into the JTS, its clinical practice guidelines, and usual military practice.
- Evidence of how these changes may be effectively integrated into military training and doctrine (e.g., special units such as the Army Rangers) and how these lessons learned can be applied in the civilian sector.
- Time elapsed between the compilation/publication of evidence and development and implementation of clinical guidelines.
For each case, the DoD authors listed below provided information related to interventions, outcomes, levels of evidence for clinical guidelines, and relevant learning health system context:
- LTC (P) Andrew P. Cap, M.D., Ph.D., U.S. Army Institute of Surgical Research, FT Sam Houston, Texas
- LTC Matthew A. Borgman, M.D., San Antonio Military Medical Center, FT Sam Houston, Texas
- Dr. (COL ret) John F. Kragh, M.D., U.S. Army Institute of Surgical Research, FT Sam Houston, Texas
- COL Kirby R. Gross, M.D., Joint Trauma System, U.S. Army Institute of Surgical Research, FT Sam Houston, Texas
Dr. Leon Dent, a Robert Wood Johnson Fellow and Associate Professor and Chair of Surgery at Meharry Medical College, Nashville, Tennessee, provided additional assistance in crafting the case studies.
The committee is grateful for their efforts in support of this study.
The cases were reviewed for
- medical description of case (care provided, errors, factors that influenced outcome);
- military learning process (data management; description of military clinical performance improvement processes, including clinical guideline development and education and training initiatives; and impact of DoD trauma research investment); and
- knowledge transfer between the military and civilian sectors regarding best practices and lessons learned.
EXTREMITY HEMORRHAGE CASES
Case Description
Case 1
In 2006, a male American soldier suffered blast injuries isolated to both lower limbs. The right limb had soft tissue loss, including a length of a major artery, and the left limb injury was a mid-thigh traumatic amputation. In a “scoop-and-run strategy,” he was flown to the emergency room of a nearby combat support hospital (“Baghdad ER”), arriving 6 minutes after injury. Neither in the field nor in the aircraft was an attempt made to control bleeding from his extremity wounds. Upon arrival at the hospital, the first attempt to control bleeding was made when he was found to be pulseless, in hemorrhagic shock. Emergency providers placed a field tourniquet on each lower limb and resuscitation was attempted, but the patient was soon declared dead from the prior exsanguination.
Case 2
In a separate incident in 2006, a male American soldier was wounded when an explosion resulted in traumatic amputation of both lower limbs. One limb was amputated above the knee and the other below the knee; he had no other injuries. A fellow soldier, who was not a medic, placed tourniquets on both of the patient’s extremities. Bleeding was controlled promptly, and the casualty was flown to the “Baghdad ER.” Upon arrival at the hospital, he was in shock and received a massive transfusion of blood. He was taken to the operating room, where his leg wounds were debrided, and he survived.
Case Discussion
These two cases highlight how application of tourniquets in the prehospital setting has a significant impact on outcomes for this injury pattern. In Case 2, the tourniquet was applied at the point of injury by a nonmedic, indicating that the soldiers had been trained to use tourniquets and had tourniquets available. Prompt control of hemorrhage led to the patient’s survival despite traumatic amputation of both lower limbs. Case 1 had a similar injury pattern but did not survive because the tourniquets were not applied until the patient reached the hospital. The key point is that tourniquet application in Case 2 was prehospital, illustrating the importance of timely intervention focused on preventing blood loss and death.
Tourniquets were distributed to deployed service personnel in 2005, so it is possible that the device was available and could have been applied to Case 1 in the field, although this was not documented explicitly in the after-action review. Early in the war, poor outcomes resulted from a lack of knowledge regarding the proper use of tourniquets and their consequential application as a tool of last resort. The culture of the military as a whole and of this unit in particular had not yet incorporated practices of tactical combat casualty care (TCCC), which called for the use of tourniquets. Subsequent on-the-ground feedback to Case 1’s unit commanding officer resulted in immediate training in tourniquet use and equipping of the unit with tourniquets. In the years that followed this preventable fatality, TCCC guidelines for tourniquets were adopted widely. This case was used as an impetus for incremental improvements in the trauma care system, which in turn improved survival rates. From 2005 to 2011, an estimated 1,000 to 2,000 lives were saved by widespread tourniquet distribution to deploying U.S. military service members (Andersen et al., 2012). During this time period, the annual rate of deployed U.S. military service members dying from limb exsanguination decreased sixfold (Eastridge et al., 2012). Tourniquets are the most important lifesaving intervention during the war.
The Military Learning Process
Data Management
Important efforts in data collection regarding tourniquet use included debriefs of personnel from Special Operations Forces after they had redeployed, evaluations of data on preventable deaths through the office of the Armed Forces Medical Examiner (AFME), and several surveys of caregiver performance at the Baghdad combat support hospital. These data were used to refine best tourniquet practices. Intellectual aspects of decision making on whether to use a tourniquet were studied empirically to provide useful evidence. Under an institutional review board (IRB)-approved protocol and via the registry process, the in-theater research teams helped collect data, enabling rapid analysis and dissemination of information on the safety of tourniquets and the requirement for their prehospital application. Separate analyses conducted in 2005 and 2006 showed a transition to more frequent tourniquet use and improved outcomes (Beekley et al., 2008; Kragh et al., 2008). These findings were shared within the Joint Trauma System (JTS) communication network, leading to changes in care.
AFME data have been studied to determine whether fatally injured service members—such as the soldier described in Case 1—could potentially have survived in order to inform performance improvement efforts and identify medical capability gaps for further research and development. The
U.S. Army Institute for Surgical Research (USAISR) worked with AFME to conduct a preventable death analysis in 2004 (Kragh et al., 2013a). This analysis yielded reports (Holcomb et al., 2007; Kelly et al., 2008) noting that significant numbers of preventable deaths were due to extremity hemorrhage from tourniquet-amenable injuries. These findings spurred efforts to improve tourniquet distribution and use. Such studies have shown the importance of capturing data on dead (killed in action [KIA] and died of wounds [DOW]) and wounded casualties (including rehabilitation) and integrating these data into one registry to enable examination of the entire wounding continuum for new knowledge that can improve outcomes. However, these data are currently fragmented across multiple systems.
All patients admitted to Role 3 facilities (e.g., combat support hospitals) are captured in the Department of Defense Trauma Registry (DoDTR), and the Pre-Hospital Trauma Registry (PHTR) now captures data from the point of injury to support performance improvement initiatives. Kotwal and colleagues (2011) demonstrated the importance and effectiveness of a PHTR in the 75th Ranger Regiment. Although impeded initially by information assurance concerns, JTS efforts to develop a U.S. Department of Defense (DoD)-wide PHTR were eventually successful, and the PHTR was fielded in summer 2013. As of November 2015, the care records of approximately 770 patients had been entered in the PHTR. Prior to the creation of the PHTR, data on patients deemed KIA (i.e., died before reaching a treatment facility) and casualties who died at Role 2 military treatment facilities (MTFs) were not captured for inclusion in a DoD trauma registry other than the AFME system.1 Given the sensitive nature of KIA information, these data are housed separately from the medical records and the trauma registries.
All combat deaths undergo postmortem examination. However, case-specific results are not immediately available to individual providers, and preventable death analyses are not routinely performed. Currently, an effort is under way to provide definitions and a framework for preventable death analyses. Eastridge and colleagues (2012) report that nearly 1,000 servicemembers killed in action between 2001 and 2011 died of wounds that were potentially survivable). However, their objective was merely to review deaths from an anatomic perspective. A true preventable death analysis requires consideration of additional features, such as the tactical situation at the time of the casualty’s injury. The capability to conduct such analyses is difficult to develop, but is essential for a complete understanding of where resources need to be applied.
__________________
1 Trauma registries are designed to capture data relating to the quality of care provided by a trauma system. Patients who are KIA may or may not have received any care, depending on the mechanism and timing of their fatal injury.
Performance Improvement
The need for tourniquets was recognized in the very first papers on TCCC dating back to 1996 (Butler et al., 1996), and tourniquet use was taught at the military’s joint trauma training center at Ben Taub Trauma Center in 2001 (Kragh et al., 2013b). However, tourniquets were not widely issued to troops until a Baltimore Sun article in 2005 prompted multiple congressional inquiries (Kragh et al., 2013b). It was difficult to overcome inertia and conventional wisdom regarding tourniquets, and they were often used incorrectly as a last resort. After limb exsanguination deaths were recognized to be both common and preventable, the services changed their practice to the use of tourniquets as a means of first aid. Surveys of tourniquet use in Baghdad, including Case 2 above, were published to broadcast the findings to the widest possible audience. The importance of bleeding control was made clear, and by 2009, when the Combat Lifesaver Course book was revised, almost all soldiers had been trained in tourniquet use. This common experience soon helped change the culture of caregiving.
Widespread implementation of tourniquet use has been achieved through such efforts as improvement of clinical performance, refinement of logistic supply management, improvement of leadership in key organizations, improvement in training of all persons at risk, amendment of doctrinal practices, advancement of laboratory research, development of both medical devices and best practices, and use of intermittent surveys to measure progress in caregiving. Connections among medical, logistics, and training stakeholders were instrumental in ensuring the eventual inclusion of tourniquets in first-aid kits issued to all deploying soldiers and the eventual training of all soldiers in using tourniquets effectively. Implementation was initially uneven as Special Operations Forces implemented tourniquet use much earlier, more rapidly, and more thoroughly relative to the conventional military services. Knowledge was disseminated via consultant visits in theater, in-theater trauma conferences, JTS and TCCC guidelines, predeployment training sites, e-mail, presentations at military and civilian meetings, and journal publications.
Impact of DoD Trauma Research Investment
USAISR funded an early (2003) tourniquet distribution effort and, more important, a testing program for tourniquets. Laboratory studies showed that four out of seven tested tourniquets approved by the U.S. Food and Drug Administration (FDA) were not adequately effective at stopping bleeding (Walters et al., 2005). As a result of this effort, the combat application tourniquet (CAT) was selected as the TCCC tourniquet of choice, with subsequent widespread distribution. This capability to test approved
devices in military laboratories and identify a single recommended device is crucial, as no other independent laboratories have this capability. Initial experience with tourniquet testing prepared USAISR for later efforts in evaluating junctional tourniquets designed to control bleeding from vascular injuries in the groin and axilla. This work is discussed in the case study on dismounted complex brain injury later in this appendix.
Transfer of Knowledge Between Military and Civilian Sectors
The civilian sector’s implementation of best practices in tourniquet use has lagged behind that of the military. A majority of civilian trauma centers (55.1 percent) responding to a recent survey reported that fewer than 20 percent of patients who could have benefited from a tourniquet arrived with one in place (Haider et al., 2015). This lag in civilian use of tourniquets is due in part to the lack of reliable integrated prehospital, hospital, and medical examiner data that collectively describe the problem of preventable deaths from limb wound exsanguination. In addition, very few traumatic amputations or massive tissue disruption injuries resulting from high-velocity gunshots or artillery shell fragments occur in the civilian sector, making it difficult to promote tourniquet use among civilians. Only in the last few years have papers been published regarding civilian tourniquet use; an evidence-based clinical care guideline for external hemorrhage control was released by the American College of Surgeons in 2014 (Bulger et al., 2014).
Despite the lag, the success of tourniquet use on the battlefield has translated to successful use in civilian prehospital care, seen most clearly following the Boston Marathon bombings, where “without a doubt, tourniquets were a difference-maker and saved lives” (Elster et al., 2013). Recently, the Hartford Consensus Committee—a joint committee convened by the American College of Surgeons—developed recommendations for improving the outcomes from exsanguinating limb hemorrhage due to active shooter and other mass casualty events. The group recommends that a continuum of care be implemented that incorporates not only emergency medical services (EMS) response but also initiation of care by law enforcement officers and potentially lay bystanders as well. The foundation for this new paradigm is the body of guidelines issued by the U.S. Military’s Committee on Tactical Combat Casualty Care and its civilian counterpart, the Committee on Tactical Emergency Casualty Care. In October 2015, the White House launched a “Stop the Bleed” campaign to empower American civilians to stop life-threatening hemorrhage. Beyond raising awareness, the campaign is working to expand personal and public access to bleeding control kits that contain, among other items, tourniquets. The timeline for the development of greater tourniquet use in military and civilian sectors is summarized in Box A-1.
REFERENCES
Andersen, R. C., S. B. Shawen, J. F. Kragh, Jr., C. T. Lebrun, J. R. Ficke, M. J. Bosse, A. N. Pollak, V. D. Pellegrini, R. E. Blease, and E. L. Pagenkopf. 2012. Special topics. Journal of the American Academy of Orthopaedic Surgeons 20(Suppl. 1):S94-S98.
Beekley, A. C., J. A. Sebesta, L. H. Blackbourne, G. S. Herbert, D. S. Kauvar, D. G. Baer, T. J. Walters, P. S. Mullenix, and J. B. Holcomb. 2008. Prehospital tourniquet use in Operation Iraqi Freedom: Effect on hemorrhage control and outcomes. Journal of Trauma 64(Suppl. 2):S28-S37.
Bulger, E. M., D. Snyder, K. Schoelles, C. Gotschall, D. Dawson, E. Lang, N. D. Sanddal, F. K. Butler, M. Fallat, and P. Taillac. 2014. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehospital Emergency Care 18(2):163-173.
Butler, F. K., J. Hagmann, and E. G. Butler. 1996. Tactical combat casualty care in special operations. Military Medicine 161(Suppl.):3-16.
Eastridge, B. J., R. L. Mabry, P. Seguin, J. Cantrell, T. Tops, P. Uribe, O. Mallett, T. Zubko, L. Oetjen-Gerdes, T. E. Rasmussen, F. K. Butler, R. S. Kotwal, J. B. Holcomb, C. Wade, H. Champion, M. Lawnick, L. Moores, and L. H. Blackbourne. 2012. Death on the battlefield (2001-2011): Implications for the future of combat casualty care. Journal of Trauma and Acute Care Surgery 73(6 Suppl. 5):S431-S437.
Elster, E., E. Schoomaker, and C. Rice. 2013. The laboratory of war: How military trauma care advances are benefiting soldiers and civilians. Health Affairs Blog. http://healthaffairs.org/blog/2013/12/18/the-laboratory-of-war-how-military-trauma-care-advances-are-benefiting-soldiers-and-civilians (accessed May 21, 2015).
Haider, A. H., L. C. Piper, C. K. Zogg, E. B. Schneider, J. A. Orman, F. K. Butler, R. T. Gerhardt, E. R. Haut, J. P. Mather, and E. J. MacKenzie. 2015. Military-to-civilian translation of battlefield innovations in operative trauma care. Surgery 158(6):1686-1695.
Holcomb, J. B., N. R. McMullin, L. Pearse, J. Caruso, C. E. Wade, L. Oetjen-Gerdes, H. R. Champion, M. Lawnick, W. Farr, S. Rodriguez, and F. K. Butler. 2007. Causes of death in U.S. Special Operations Forces in the Global War on Terrorism: 2001-2004. Annals of Surgery 245(6):986-991.
Kelly, J. F., A. E. Ritenour, D. F. McLaughlin, K. A. Bagg, A. N. Apodaca, C. T. Mallak, L. Pearse, M. M. Lawnick, H. R. Champion, C. E. Wade, and J. B. Holcomb. 2008. Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003-2004 versus 2006. Journal of Trauma 64(Suppl. 2):S21-S26.
Kotwal, R. S., H. R. Montgomery, B. M. Kotwal, H. R. Champion, F. K. Butler, Jr., R. L. Mabry, J. S. Cain, L. H. Blackbourne, K. K. Mechler, and J. B. Holcomb. 2011. Eliminating preventable death on the battlefield. Archives of Surgery 146(12):1350-1358.
Kragh, J. F., Jr., T. J. Walters, D. G. Baer, C. J. Fox, C. E. Wade, J. Salinas, and J. B. Holcomb. 2008. Practical use of emergency tourniquets to stop bleeding in major limb trauma. Journal of Trauma 64(Suppl. 2):S38-S49.
Kragh, J. F., Jr., D. F. Beebe, M. L. O’Neill, A. C. Beekley, M. A. Dubick, D. G. Baer, and L. H. Blackbourne. 2013a. Performance improvement in emergency tourniquet use during the Baghdad surge. American Journal of Emergency Medicine 31(5):873-875.
Kragh, J. F., Jr., T. J. Walters, T. Westmoreland, R. M. Miller, R. L. Mabry, R. S. Kotwal, B. A. Ritter, D. C. Hodge, D. J. Greydanus, J. S. Cain, D. S. Parsons, E. P. Edgar, T. Harcke, D. G. Baer, M. A. Dubick, L. H. Blackbourne, H. R. Montgomery, J. B. Holcomb, and F. K. Butler. 2013b. Tragedy into drama: An American history of tourniquet use in the current war. Fort Belvoir, VA: Defense Technical Information Center.
Little, R. 2005. Modern combat lacking in old medical supply. Baltimore Sun. http://articles.baltimoresun.com/2005-03-06/news/0503060023_1_tourniquet-american-soldier-combat (accessed February 24, 2016).
Walters, T. J., J. C. Wenke, D. J. Greydanus, D. S. Kauvar and D. G. Baer. 2005. Laboratory Evaluation of Battlefield Tourniquets in Human Volunteers. USAISR Technical Report, Fort Sam Houston, TX.
BLUNT TRAUMA WITH VASCULAR INJURY CASE
Case Description
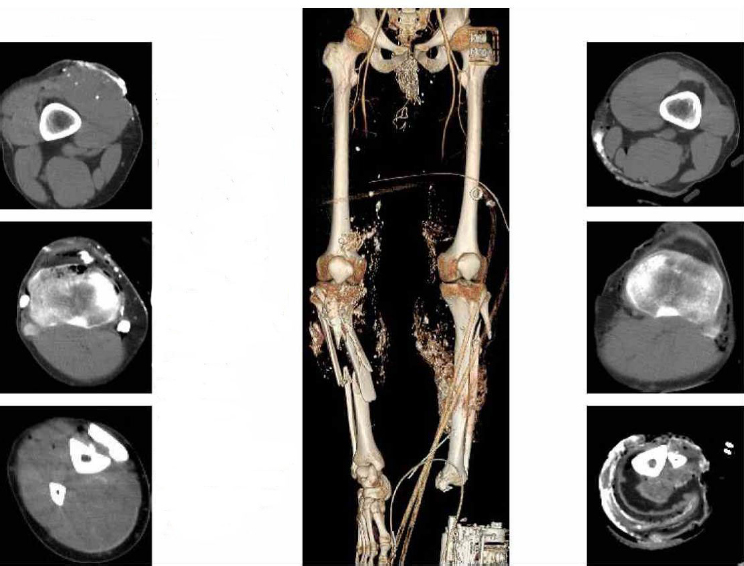
A 27-year-old male soldier was ejected from the turret at the top of his vehicle when it rolled over. He sustained multiple blunt injuries, including complex vascular, nerve, and soft tissue damage to the right upper extremity. He also sustained bilateral humeral fractures. The medic at the scene noted no loss of consciousness, but the patient was observed to have deformities of both upper extremities. Initial vital signs were systolic blood pressure (SBP) 90 mmHg (no diastolic blood pressure could be measured), heart rate (HR) 90 beats per minute (bpm), respiratory rate (RR) 20 breaths per minute (rpm), Glasgow coma score (GCS) 15. Upon the patient’s arrival at the receiving Role 3 MTF, the right upper extremity was pulseless, and no motor function or sensation was observed. The right upper extremity had suffered a laceration and soft tissue loss in the axilla and exhibited minimal bleeding. A computed tomography (CT) scan with contrast (see Figure A-1) revealed no flow in the right axillary artery, a left pneumothorax, a left
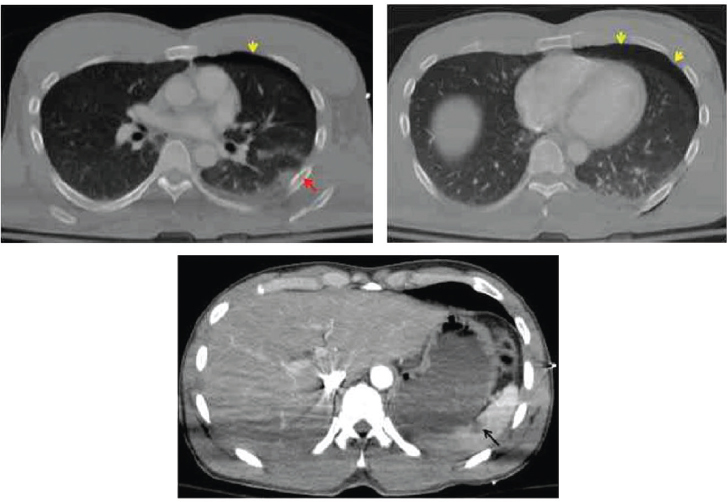
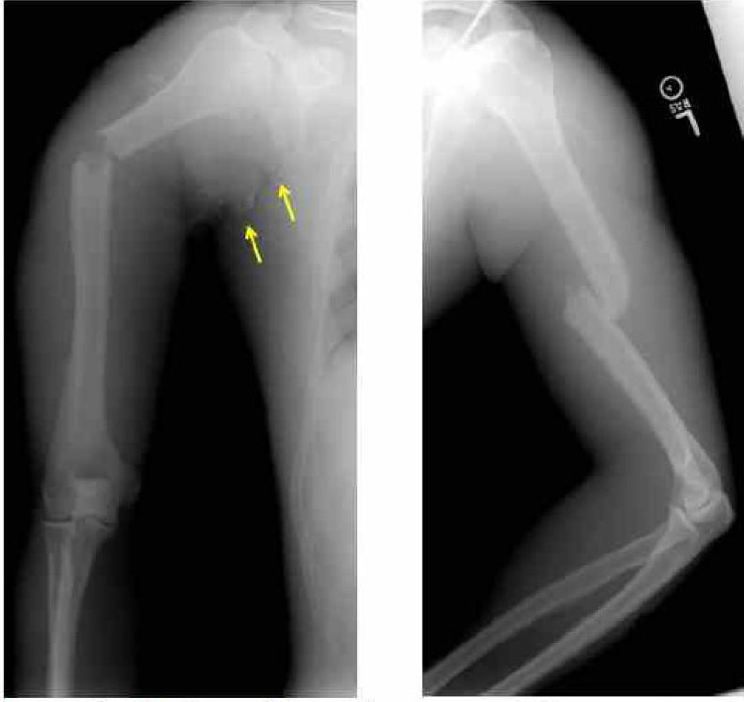
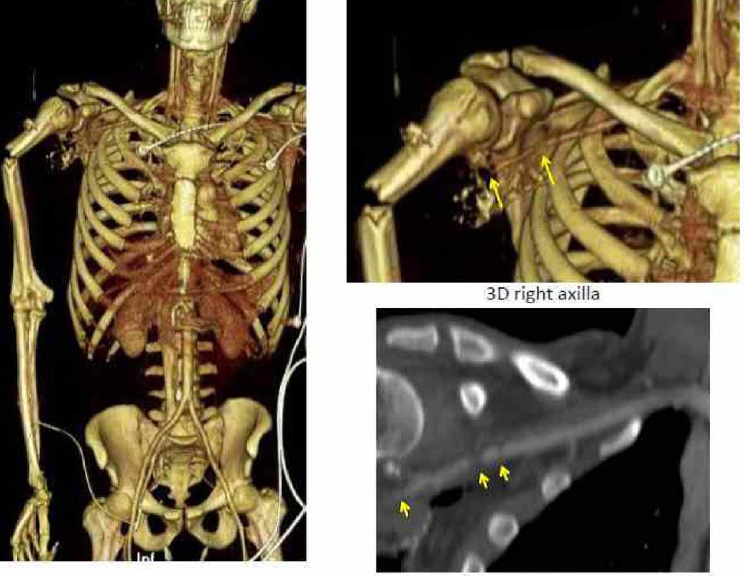
lung contusion, and a nondisplaced left sixth rib fracture. Abdominal CT images revealed a grade I hilar splenic injury and a nondisplaced L5 pars interarticularis fracture. There was no hemoperitoneum. Bilateral humeral fractures were present (see Figure A-2). A transected right axillary artery and vein were identified at the time of injury (see Figure A-3), in addition to anatomic disruption of the ulnar nerve.
Role of Care
In the field, bulky dressings were applied to a right upper extremity open fracture, and a cervical collar was placed. The patient was rapidly
evacuated in a 5-minute flight to a Role 3 MTF capable of providing subspecialty surgical care.
Role 3 Care
In the MTF operating room (OR), a left chest tube was placed, the left upper extremity was reduced and splinted, and a vascular shunt was placed from the axillary to the brachial artery. An external fixator was applied to the right humerus. Subsequently, the patient underwent arterial reconstruction, venous interposition, and fasciotomy (incomplete) of the right forearm. He was transfused 7 units of red blood cells, 6 units of fresh frozen plasma, and 1 apheresis unit of platelets. On post-injury day 1, he was transferred to the Role 3 strategic evacuation (STRATEVAC) hub. Repeat CT scanning at the STRATEVAC hub demonstrated a pneumothorax with the chest tube incorrectly placed in the extrapleural space. No bleeding from the spleen was noted. The patient was taken to the OR, where the right arm vascular repair was reassessed; the axillary artery had good flow, but the vein was thrombosed. The right forearm fasciotomy was completed,
and a latissimus dorsi muscle flap was mobilized to repair the axillary soft tissue defect and cover the vascular repair. Wounds were covered with negative-pressure dressings, and the patient was extubated prior to transfer to Germany on post-injury day 3.
Case Discussion
The overall good outcome of this patient was due to rapid evacuation (5 minutes) from the point of injury to the combat support hospital and prompt resuscitation from hemorrhagic shock. Prompt revascularization resulted in limb salvage. The use of a vascular shunt to delay definitive vascular repair was appropriate in this case given the nature of the polytrauma, the complex vascular injury, and the patient’s compromised hemodynamic status. A lengthy vascular repair performed in an austere environment by a surgeon who may perform vascular surgery infrequently is suboptimal. However, several errors in patient management were noted. The error in chest tube placement, resulting in a persistent pneumothorax, was potentially dangerous because of the possibility of the patient’s developing a life-threatening tension pneumothorax, particularly during air transport. The importance of obtaining a confirmatory chest x-ray following insertion of a chest tube is a long-held tenet of trauma surgery. The omission of a follow-up chest x-ray was most likely an oversight but may point to inadequate training. The incomplete fasciotomy probably contributed to the loss of the venous graft. Further opening of the forearm fascial compartments was performed on the patient in this case at the Role 3 air hub. This patient’s rehabilitation would have been aided by targeted nerve implantation of the axillary nerve roots into the pectoralis muscle. Targeted nerve implantation into muscle has been demonstrated to reduce the formation of painful neuromas, which occur in 13-32 percent of amputees (Pet et al., 2014), limiting or preventing the use of prosthetic devices. This procedure has been used in advanced civilian trauma centers since 2005, but has not been widely adopted.
The Military Learning Process
Data Management
The acquisition and storage of patient data have evolved within the military in recent years. To mitigate the problem of lost patient data and to assist with performance improvement efforts, patient information is now captured and stored in an electronic medical record (EMR), the Theater Medical Data Store. This system was built over the course of Operation Iraqi Freedom/Operation New Dawn and Operation Enduring Freedom as
the need for an EMR was recognized. In addition, JTS abstractors gathered data for inclusion in the DoDTR to support performance improvement.
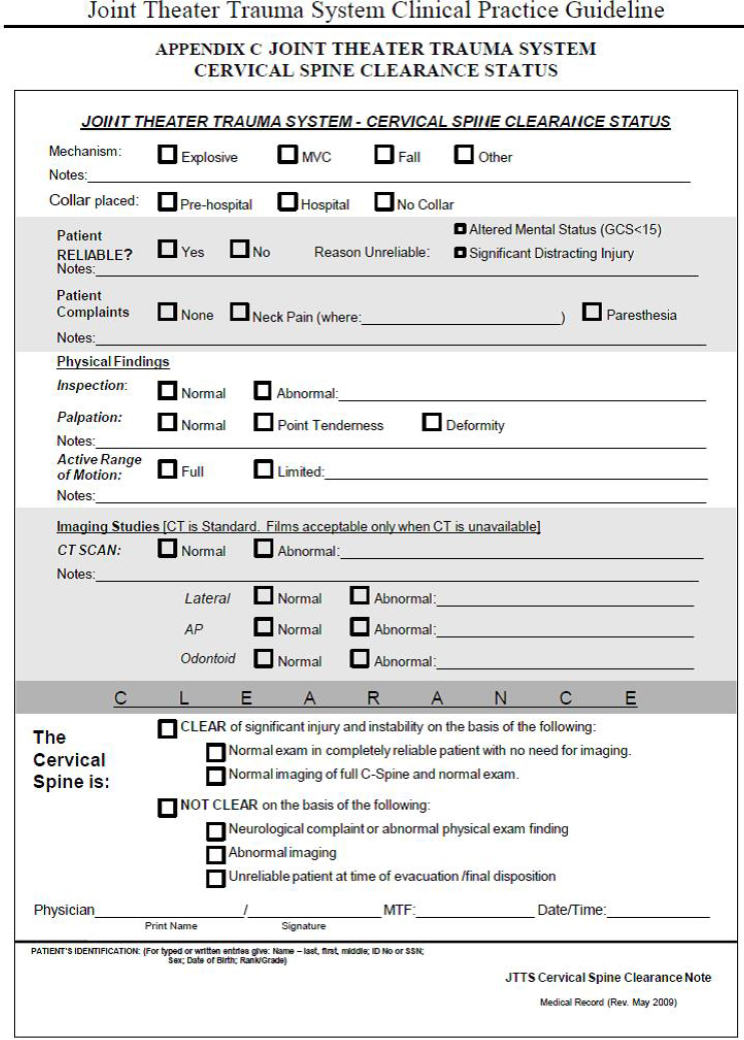
Patients such as the case presented herein undergo several transfers in care before returning to the United States. These transfers often entail loss of pertinent clinical information from one level of care to the next. Patient information from the point of injury to the initial MTF is transmitted primarily by verbal report from the flight medic to the receiving providers. For only 7 percent of casualties can a TCCC card be identified in the medical chart. Records from the Role 2 MTF are copied and transferred physically with the casualty to the Role 3 MTF. After the theater of operations became mature, nearly all Role 2 facilities had computers that could link to the Theater Medical Data Store to upload patient records. However, because of bandwidth limitations and periods during which the Internet was blocked as a result of operational security concerns, the most reliable means of ensuring that care provided at a Role 2 MTF was relayed to a Role 3 MTF was by hard copy. Entries made into the Theater Medical Data Store by the Role 2 MTF would eventually be available to the Role 3 MTF, where information technology support was much more robust. Before transfer out of theater, however, the entire medical record was copied and then moved physically with the patient. Hard-copy records could be useful to the critical care air transport teams during the 8- to 10-hour transport period out of theater. To further assist successive medical teams along the continuum of care by ensuring efficient transfer of patient data, clinical information sheets were created and transported with the patient. To indicate whether patients with a blunt mechanism of injury had met criteria for clearance of the cervical spine, for example, a spine clearance documentation sheet was included in accordance with the JTS Cervical Spine Evaluation Clinical Practice Guideline. This sheet (see Figure A-4) was completed for each casualty with a blunt injury mechanism and accompanied the patient during movement out of theater.
Performance Improvement
During the early experience of Operation Iraqi Freedom, colleagues at Landstuhl Regional Medical Center (Role 4) identified a higher-than-expected rate of incomplete fasciotomies. Many general surgeons lacked training in or experience with extremity injuries, as their orthopedic or vascular colleagues frequently manage these wounds. In the deployed environment, orthopedic surgeons may not be present at all MTFs. To provide feedback to downrange providers and correct deficiencies such as incomplete fasciotomy, a weekly Thursday Combat Casualty Care teleconference connecting in-theater MTFs with Landstuhl and U.S. MTFs was established in 2006. This teleconference provides near-real-time feedback to downrange
providers. Early in the conflicts, 15 to 20 cases per week were discussed in this forum, which afforded a chance to provide feedback regarding outcomes as well as opportunities for improvement.
The weekly Thursday Combat Casualty Care teleconference also serves to facilitate recognition of system-wide issues that may need to be addressed through the development of clinical practice guidelines (CPGs) and other performance improvement methods (e.g., educational campaigns). The process by which new CPGs are generated and existing CPGs are updated is described on the JTS CPG webpage (http:www.usaisr.amedd.army.mil/cpgs.html). Topics under consideration are presented to a theater trauma leader or the JTS director. An initial draft of the CPG is generated and reviewed by theater trauma leadership; theater trauma subject matter experts; and, subsequently, military trauma subject-matter experts (from each service) who are not currently deployed. Trauma directors at the stateside facilities that receive combat casualties also are asked to provide input. Input from these subject matter experts is collated by the chief of performance improvement at the JTS. Ideally, the JTS director, the chief performance improvement officer of the JTS, and theater trauma leadership reach consensus. The JTS director is the final clinical approval authority; however, the director may convene subject matter experts in an effort to achieve consensus. Current CPGs relevant to blunt trauma with vascular injury are listed in Box A-2.
The compartment syndrome and fasciotomy CPG, which prescribes
complete release of all compartments through full skin and fascial incisions when indicated in patients with ischemic extremities, was developed in June 2009, even though the problem of incomplete fasciotomies was identified as early as 2004. Measurement of the effectiveness of JTS performance improvement initiatives and compliance with CPGs is facilitated by core performance/adherence measures written into a performance improvement monitoring section of each CPG. For example, the core measures for compartment syndrome and fasciotomy CPG are that (1) when fasciotomy is performed, there is complete release of all compartments through full skin and fascial incisions, and (2) when indicated in patients with ischemic extremities, fasciotomy is performed at the time of revascularization. In an October 2012 audit filter review of core measure (1) only 2 of 144 patients undergoing revascularization were found to have required further fasciotomy. For core measure (2) fasciotomy was performed in 69 percent of cases of revascularization. Reviews of data on compliance with core measures during the weekly Thursday Combat Casualty Care teleconference proved to be an effective way of providing feedback on compliance with the CPGs.
The weekly Thursday Combat Casualty Care teleconference, now called the Combat Casualty Care Curriculum, has evolved from a strictly performance improvement focus to an educational forum. Each week a continuing medical education (CME) topic relevant to deployed care is selected, and one or two appropriate cases are presented.
General surgery residents completing their research year at San Antonio Military Medical Center have been directed by their general surgery program director to attend the weekly teleconferences so they can benefit from the lessons learned over the past decade of combat medicine. No other military physicians in training have been directed by leadership to participate in these teleconferences, even though they are an ideal way to meet military-specific education requirements for physicians in training and introduce them to the trauma system in which they will likely be participating. Topics chosen for CME presentations during the Thursday teleconferences are specific to combat casualty care. The topics are sequenced to coincide with the graduate medical education academic year, and all major topics of relevance to combat casualty care are discussed. Trauma system topics are covered early in the academic year. The curriculum also incorporates presentations by military medical historians and military medical research leaders.
The teleconferences will be continued indefinitely to ensure that the technical infrastructure for cross-theater communications is maintained, to reinforce the importance of the trauma system, and to provide combat casualty care education. Based on its demonstrated value in the U.S. Central Command (CENTCOM) area of operations, U.S. Pacific Command (PACOM) has established a similar teleconference, which reviews trauma cases, addresses trauma system issues, and serves as an educational forum.
Ideally, all U.S. combatant commands will establish a similar teleconference in their areas of responsibility.
Transfer of Knowledge Between Military and Civilian Sectors
Techniques to restore blood flow through injured vessels to prevent ischemic injury and limb loss have evolved through a continuous transfer of knowledge between military and civilian sectors. Despite evidence during World Wars I and II of the potential value of intravascular tubular devices for bridging arterial injuries and maintaining perfusion, interest in such devices waned during the Korean and Vietnam Wars as focus shifted to vascular repair approaches (Hancock et al., 2010). During this period, commercially available vascular shunts were developed in the civilian sector to permit flow during open, elective vascular procedures but there remained little investigation into the use of shunts for trauma applications until a significant burden of vascular injury during the wars in Afghanistan and Iraq generated the necessity. Vascular shunts were incorporated into damage control strategies at forward surgical sites (Role 2) early during the war in Iraq and were shown to be effective at restoring extremity perfusion until the patient could be evacuated to higher levels of care for definitive reconstructive vascular surgery (Hancock et al., 2010). Having shown that the use of vascular shunts extends the window of opportunity for limb salvage, efforts are under way to develop vascular shunts with specific application to military trauma management. The features useful in vascular shunts for trauma care would be a side port for blood pressure monitoring, anticoagulant administration, and contrast injection. Local anticoagulant administration would ensure that therapeutic dosage could be administered directly to a compromised extremity. Also, since combat trauma commonly involves multilevel injury, the distal vascular structures may benefit from radiographic imaging for identification of multilevel vascular injury prior to definitive vascular repair.
REFERENCES
Hancock, H., T. E. Rasmussen, A. J. Walker, and N. M. Rich. 2010. History of temporary intravascular shunts in the management of vascular injury. Journal of Vascular Surgery 52(5):1405-1409.
Kragh, J. F., Jr., J. San Antonio, J. W. Simmons, J. E. Mace, D. J. Stinner, C. E. White, R. Fang, J. K. Aden, J. R. Hsu, and B. J. Eastridge. 2013. Compartment syndrome performance improvement project is associated with increased combat casualty survival. Journal of Trauma and Acute Care Surgery 74(1):259-263.
Pet, M. A., J. H. Ko, J. L. Friedly, P. D. Mourad, and D. G. Smith. (2014). Does targeted nerve implantation reduce neuroma pain in amputees? Clinical Orthopaedics and Related Research 472(10):2991–3001. http://doi.org/10.1007/s11999-014-3602-1
White, J. M., A. Stannard, G. E. Burkhardt, B. J. Eastridge, L. H. Blackbourne, and T. E. Rasmussen. 2011. The epidemiology of vascular injury in the wars in Iraq and Afghanistan. Annals of Surgery 253(6):1184-1189.
Zonies, D., and Eastridge, B. J. 2012. Combat management of splenic injury: Trends during a decade of conflict. Journal of Trauma and Acute Care Surgery 73(2 Suppl. 1):S71-S74.
PEDIATRIC BURN CASE
Case Description
In fall 2004, a 2-year-old male presented to the 31st Combat Support Hospital emergency room (“Baghdad ER”) after a vehicle explosion. He had been seated in the back seat of a vehicle stopped at a checkpoint that exploded after being struck from behind by another vehicle. He suffered approximately 30 percent total body surface area flame burn (partial to full thickness) to the face, anterior torso, abdomen, bilateral hands, bilateral legs (left leg circumferentially), and lower back. His past medical history, surgical history, medications, and allergies were all unknown. His social history also was unknown, other than that his mother and brother had perished in the fire. The time of injury to presentation was not documented, but was presumed to be less than 2 hours. Upon arrival at the hospital, he was awake and crying, Glascow coma score (GCS) was 15. Initial vital signs were blood pressure 156/67, heart rate 124, respiratory rate 34, saturation 100 percent on supplemental oxygen delivered by nonrebreather mask. His estimated weight was 10 kg. He was breathing comfortably but had soot noted in the airway; his lungs were clear to auscultation. A venous blood gas measurement revealed acidosis and hypoxia: pH 7.12, pO2 62 mmHg, pCO2 31 mmHg, bicarbonate 20 mEq/L, base excess 9 mEq/L.
The patient was intubated and brought immediately to the operating room for debridement and dressing of burns. Lateral escharatomies were performed on the left leg and the dorsum of each foot. He received a total of 700 mL of crystalloid and had minimal blood loss. He was transferred to the intensive care unit (ICU) for continued care, with good pulmonary compliance noted. The child developed significant capillary leak and fluid overload in the initial 72 hours. Additional extremity escharatomies were performed on days 1 and 2 for compartment syndrome. A peritoneal drain was placed on day 3 for abdominal compartment syndrome. The child also developed severe acute respiratory distress syndrome. No advanced forms of invasive ventilation were available to treat his worsening pulmonary compliance, and he required peak inspiratory pressures of 90 mm Hg and positive-end expiratory pressure of 20 mmHg, as well as prone positioning, to maintain oxygen saturations greater than 85 percent and pH greater than 7.2. He required a total of approximately 25 days on the ventilator. Ultimately, he was successfully weaned to room air and was discharged to home on hospital day 40. He was able to receive limited physical therapy and rehabilitation while admitted.
Case Discussion
This case highlights several challenges in the care of burn patients, and pediatric patients in general. U.S. and Coalition military patients with severe burns are quickly evacuated out of theater by critical care air transport teams, and patients with the most severe burns are transported by a specialized burn team from the U.S. Army Institute of Surgical Research in San Antonio, Texas. In contrast, this patient, like other host nation citizens with significant burns, could not be evacuated to an alternative hospital with a specialized burn team and long-term rehabilitation capabilities (including nutritional and psychosocial resources).
This patient benefited from the care of a pediatric intensivist who happened to be deployed to Baghdad at the time. This kind of specialty care is not commonly available in a war zone. Although a good outcome was achieved, several deficiencies hampered the care of this child. No advanced forms of invasive ventilation, such as high-frequency oscillatory ventilation or inhaled nitric oxide support, were available to treat his worsening pulmonary compliance and edema. Devices for accurately measuring intra-abdominal pressure also were not available. Innovative use of bedside ultrasound in the hospital made it possible to determine that the patient was hypervolemic based on superior vena cava diameter and atrial size. This determination assisted in the diagnosis of abdominal compartment syndrome as the cause of the child’s anuria and renal failure. Overall, this patient was overresuscitated, as evidenced by his abdominal compartment syndrome. Where in the chain of care this occurred is unclear, but it was probably in the hospital stage. Documentation of prehospital care for this patient was not available.
Burn injury accounted for 14 percent of all pediatric patients seen at DoD Role 3 or 2b MTFs in Afghanistan and Iraq from 2003 through 2011. The average hospital length of stay was 10 days (range 0 to 171 days). Because of longer lengths of stay, children accounted for 11 percent of all bed days during this period, although representing only 5.8 percent of admissions. Their overall mortality was 13.3 percent (Borgman et al., 2015).
Despite the substantial numbers of pediatric patients cared for at expeditionary military hospitals, resources are inadequate for the acute and long-term care of critically ill children (and adult host nation burn patients). Early in the conflicts, clinicians had to improvise pediatric-sized medical equipment. In 2006, with input from pediatricians, the U.S. Army Medical Materiel Agency made available a set of pediatric supplies, which ultimately resulted in the assembly of the current pediatric humanitarian assistance augmentation medical equipment set. Even after 2006, however, when complete sets of pediatric equipment and medication had been developed,
lack of communication about the existence of these kits impaired the implementation of their use, as the kits had to be specially requested.
Although optimal supplies and personnel may not have been available to treat a pediatric casualty in a combat environment, the care the child in this case report received far exceeded that which was (and is) available in Baghdad. This was just one of many cases indicating the need to deploy a set of pediatric equipment and physicians trained in pediatric critical care to combat support hospitals in theater. Military doctrine still has not evolved to ensure the availability of critical care for pediatric combat casualties.
The Military’s Learning Process
Data Management
Although the DoDTR was initially envisaged as a means of tracking and informing the care of U.S. casualties, it is also a robust repository of data on severely injured children. Pediatric cases admitted to Role 3 MTFs are entered into the DoDTR; otherwise, data collection on these patients is extremely limited (case reports). DoDTR data enabled an in-depth epidemiological study of pediatric burn injuries in combat, which identified factors associated with mortality based on burn severity (Borgman et al., 2015). However, entry of pediatric data into the DoDTR has not been a priority, and as a result, there generally has been a considerable lag between the occurrence of pediatric cases and their entry into the system for analysis. Armed Forces Medical Examiner (AFME) data are not available to inform preventable death analyses for pediatric patients since the AFME performs autopsies on U.S. service members killed in action, not on host country nationals.
Performance Improvement
Resources for deployed physicians treating burn and pediatric patients were developed by the JTS primarily by expert consensus, but also informed by ongoing analysis of clinical data from the DoDTR. When this case occurred, no definitive guidance on the care of pediatric burns was available. The JTS Burn Care CPG (JTS, 2013) has evolved since this case occurred to include issues useful in the management of children with burns. However, there are no CPGs specific to pediatric burn care. The recommendations added to the burn care CPG with regard to children are more like rules of thumb and are not based on a rigorous analysis of CENTCOM outcomes in these patients (which would be hard to perform for long-term outcomes since host national patients are eventually discharged out of the military
system). Very few clinical trials have been conducted in these areas, so guidelines are frequently based on Level 3 evidence.
While capabilities to care for these complex pediatric patients generally have improved since the start of the wars, pediatric host national cases are not rigorously analyzed for performance improvement purposes, and there are no published studies on improvement in these patients over time nor is there any pediatric-specific monitoring of CPG compliance. Even when performance improvement processes such as mortality and morbidity reviews were carried out at combat support hospitals, transmission of the resultant lessons learned to the next group of physicians was a challenge. Lessons learned were often distributed by word of mouth and in a textbook that was published years later (Fuenfer and Creamer, 2010). To address potential knowledge and training deficits, the U.S. Army Medical Department Center and School developed a 5-day course—the Joint Forces Combat Trauma Management Course—that addresses burns, pediatric patients, and other topics relevant specifically to those providers deploying to Role 2 or 3 MTFs. Specialty-specific e-mail listservs (including separate teleconsultation groups for burn trauma and pediatrics) also were created so that deployed providers could rapidly contact specialists in the United States should complex clinical questions arise.
Impact of DoD Trauma Research Investment
The recent experience in Afghanistan and Iraq has led to significant improvements in the U.S. military’s ability to provide advanced care to adult burn patients in the deployed setting. For example, the recurrent problems encountered with fluid overload in burn management led to the development of the Burn Resuscitation Decision Support System (BRDSS) by the U.S. Combat Casualty Care Research Program. The BRDSS can enable providers to accurately resuscitate burn patients from the point of injury to definitive care using an algorithm that automatically generates patient-specific fluid rate recommendations for resuscitation. This medical device, available for use in hospitals and the field (mobile format deployed in 2014), started as a research project within the U.S. Army Medical Research and Materiel Command and was the first device to undergo advanced development and go from FDA approval to the field. Its success represents a development model that is also enabling progress in closing other combat casualty care capability gaps (DoD, 2015). However, the BRDSS is not currently indicated for pediatric patients (under 18 years of age), although future versions may include a pediatric module. Research on optimal clinician training and configuration of equipment sets and systems-level integration of host national pediatric and burn care into the overall DoD trauma system represent opportunities for further refinement of expeditionary medicine.
Transfer of Knowledge Between Military and Civilian Sectors
Care for pediatric burn patients provides a rich opportunity for military and civilian knowledge transfer and collaboration to fill gaps in both sectors. Several civilian pediatric burn centers have established protocols for care for pediatric burn patients that include timing of surgery, wound care management, sedation and analgesia, nutrition, pharmacology, and psychosocial care. These protocols could be adapted to resources available for pediatric burn care in an austere environment. As these protocols are not published, the process for knowledge transfer could involve subject matter experts teaming with military providers to create a best practices protocol.
Civilian pediatric trauma centers rarely encounter blast-related penetrating injuries, but this type of injury is commonplace in a war zone, enabling military researchers to conduct research that would be difficult or even infeasible in the civilian sector. For example, Borgman and colleagues (2011) used the DoDTR to develop the pediatric “BIG” trauma score for predicting mortality on admission in pediatric trauma patients. This method was later validated with data from German pediatric civilians as well as Canadian blunt trauma patients (Borgman et al., 2011; Davis et al., 2015), and may have use in a variety of civilian trauma and research centers.
Military experience with adult burn patients also has informed burn care in the civilian sector. For example, military data from burned soldiers were used to develop a revised fluid resuscitation formula (Modified Brooke) that has been widely applied to avoid fluid overload at civilian burn centers. In addition, the computerized decision support tool developed at the U.S. Army Institute of Surgical Research Burn Center to help guide fluid management has supported care for both civilian burned casualties and service members being evacuated out of theater.
REFERENCES
Borgman, M. A., M. Maegele, C. E. Wade, L. H. Blackbourne, and P. C. Spinella. 2011. Pediatric trauma BIG score: Predicting mortality in children after military and civilian trauma. Pediatrics 127(4):e892-e897.
Borgman, M. A., R. I. Matos, L. Blackbourne, and P. C. Spinella. 2012. Ten years of military pediatric care in Afghanistan and Iraq. Journal of Trauma and Acute Care Surgery 73(6 Suppl. 5):S509-S513.
Borgman, M. A., R. I. Matos, and P. C. Spinella. 2015. Isolated pediatric burn injury in Iraq and Afghanistan. Pediatric Critical Care Medicine 16(2):e23-e27.
Chung, K. K., S. E. Wolf, L. C. Cancio, R. Alvarado, J. A. Jones, J. McCorcle, B. T. King, D. J. Barillo, E. M. Renz, and L. H. Blackbourne. 2009. Resuscitation of severely burned military casualties: Fluid begets more fluid. Journal of Trauma and Acute Care Surgery 67(2):231-237.
Davis, A. L., P. W. Wales, T. Malik, D. Stephens, F. Razik, and S. Schuh. 2015. The BIG score and prediction of mortality in pediatric blunt trauma. Journal of Pediatrics 167(3):593-598.
DoD (U.S. Department of Defense). 2015. U.S. Combat Casualty Care Research Program (CCCRP): Capability gap closure analysis. Washington, DC: Defense Health Agency, DoD.
Fuenfer, M. M., and K. M. Creamer. 2010. Pediatric surgery and medicine for hostile environments. Washington, DC: Office of The Surgeon General, Borden Institute, Walter Reed Army Medical Center.
JTS (Joint Trauma System). 2013. Clinical practice guideline: Burn care. San Antonio, TX: JTS. http://www.usaisr.amedd.army.mil/cpgs/Burn_Care_13_Nov_13.pdf (accessed July 1, 2015).
DISMOUNTED COMPLEX BLAST INJURY CASE
Case Description
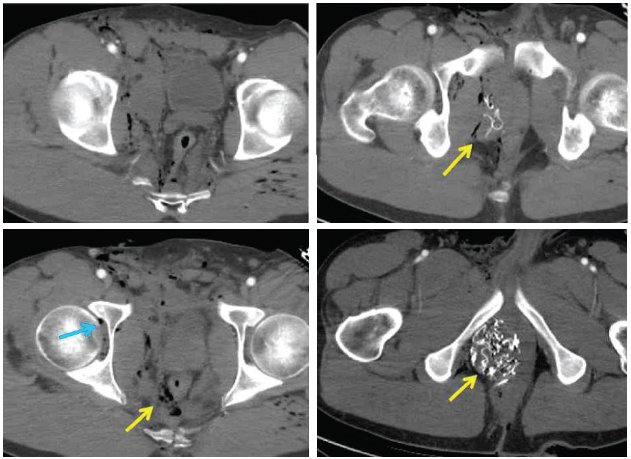
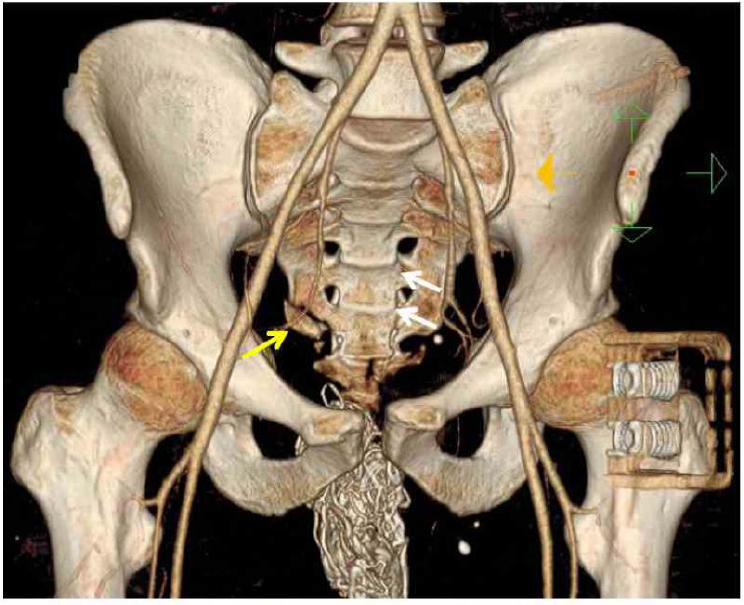
A 29-year-old male service member sustained injuries in 2009 from an improvised explosive device while on patrol. His injuries included traumatic amputation of his left lower extremity and a compound right lower extremity fracture (see Figure A-5). There was extensive soft tissue injury to both lower extremities. The field medic noted that the patient had a palpable radial pulse, heart rate 110, respiratory rate 15, Glasgow coma score 15, and severe pain. Further evaluation during tactical evacuation revealed a large perineal wound that later was shown to extend from the right groin through the perineum to the perirectal area (see Figure A-6). A computed tomography (CT) scan showed widening and misalignment of the patient’s symphysis pubis (see Figure A-7).
Role 1 Care
At the point of injury, the field medic applied the following interventions: two SOF-T tourniquets to the left lower extremity, makeshift splinting of the right lower extremity, pressure dressing application to the right lower extremity and right groin, a pelvic binder, saline lock placement, ketamine 50 mg intravenous for pain, and a hypothermia prevention and management kit. The patient exhibited signs of hemorrhagic shock (a thready pulse) and subsequently was given 300 ml saline.
Tactical Evacuation
During tactical evacuation, intraosseous vascular access was established, and further bleeding control measures were taken (packing and pressure on the perineal wound, and transfusion with 1 unit each of red blood cells and fresh frozen plasma). Additional ketamine was administered in an effort to manage pain.
Role 3 Care
At the receiving Role 3 MTF, pneumatic tourniquets were applied, and the patient received further resuscitation with whole blood and tranexamic acid (TXA). In the operating room, the colon was divided at the rectosigmoid junction and left in discontinuity. A temporary abdominal closure was applied. During the same operative intervention, a pelvic external fixator was placed, and both lower extremities were amputated through the knees. On the day following the injury, the patient was transported by a critical care air transport team to a Role 3 strategic evacuation (STRATEVAC) hub, where washouts of the lower extremity wounds were performed and negative pressure dressings applied, the pelvic external fixator was adjusted, and an end colostomy was fashioned. Nasoenteral feeding access was placed during an exploratory laparotomy by advancing a tube into the proximal jejunum. Subsequently, the fascia was closed.
Evacuation Out of Theater
The patient was transported out of theater on day 2 post-injury by a critical care air transport team. During the 8.5-hour flight, the patient received another transfusion with 4 units of red blood cells and 3 units of fresh frozen plasma to counter ongoing blood loss.
Role 4 Care
Upon arrival at Landstuhl Regional Medical Center in Germany, the patient’s wounds were washed out, and he was extubated. An oblique fracture of the third metacarpal bone and a ruptured tympanic membrane were identified. The patient remained in Germany for 3 days before being moved to the United States.
Role 5 Care
During the patient’s treatment at a U.S. MTF, both lower extremity amputations were revised to above the knee, and the sacroiliac joint was transfixed.
Case Discussion
This case typifies the dismounted complex blast injury (DCBI) pattern, caused by exposure of warfighters on foot patrol to blast and high-velocity fragments generated by the detonation of buried or concealed ground-level explosive devices. The injury pattern includes a traumatic amputation of at least one leg, a severe injury to another extremity, and pelvic, abdominal, or urogenital wounding. This pattern of injury was formally described as DCBI in 2010.
In this case, the medic’s actions to control blood loss (prompt application of tourniquets and packing of the groin wound) and prevent hypothermia in the field were consistent with TCCC guidelines and were key to this patient’s survival. According to TCCC guidelines, the patient might also have benefited from administration of TXA, antibiotics, and blood products for resuscitation (whole blood or red blood cells and plasma) in the field, as well as application of a junctional tourniquet. Currently, however, DoD has fielded junctional tourniquets on a very limited basis. Whole blood and freeze-dried plasma are available only in Special Operations units, and red blood cells and plasma are available only on a limited basis for medical evacuation (MEDEVAC), not for field care.
The Military Learning Process
Data Management
The patient described in this case received prehospital and hospital-based care. Data from his medical records for these two phases of care are currently entered into separate DoD databases. Point-of-injury care is abstracted into the Pre-Hospital Trauma Registry (PHTR), and data from Role 3, Role 4, and Role 5 MTFs are captured in the DoDTR. Patient data collected during tactical evacuation (intratheater) are abstracted into a separate TACEVAC (formerly called MEDEVAC) database developed by the JTS. Data capture for care provided at the point of injury and during transport between theater MTFs has been reliable since 2009. Because DoDTR inclusion criteria prior to 2013 required an admission to a Role 3 MTF, data on casualties who received care at a Role 2 facility were not abstracted into the DoDTR if (1) they did not require evacuation to a Role 3 facility or (2) they died at the Role 2 facility. Care provided to patients in these two categories was abstracted into a Role 2 database by Role 2 clinical staff. The separate databases for the different levels of care represent a suboptimal system design. Ideally, an integrated registry would be developed that is oriented less to the role of care and more to the casualty. Despite these limitations, however, the DoDTR was a critical resource in the identification of the DCBI injury pattern and subsequent efforts to improve care for service members sustaining these devastating injuries. In its absence, the ability to detect distinct and evolving wounding patterns may have been significantly delayed.
Performance Improvement
DoDTR data were analyzed in 2010 in response to concerns from deployed line and medical communities regarding an apparent increase in multiple limb amputations concomitant with severe genitourinary injury. This analysis revealed a clear increase in the frequency of the injury pattern described as DCBI. These data and the severe nature of the injuries prompted the Army Surgeon General to appoint a task force charged with studying the causation, prevention, protection, treatment, and long-term care options for this injury pattern. The task force’s report was released in June 2011.
Many of the best practices identified by the task force and applied to the care of DCBI patients represented advances made in the earlier years of conflicts in Afghanistan and Iraq. For example, the task force echoed TCCC recommendations to use tourniquets at the point of injury for hemorrhaging extremity injuries and to avoid large-volume crystalloid resuscitation.
CPGs—introduced initially in December 2004 as the deployed trauma system’s means of avoiding variation in care—had already been developed for the topics of resuscitation, management of war wounds, hypothermia prevention, and intratheater transport and were well accepted by the time of the dramatic increase in the DCBI wounding pattern. Recognition of DCBI prompted renewed attention to CPG implementation, education, and performance improvement measures. (CPGs relevant to DCBI are listed in Box A-3.)
A new CPG—the Invasive Fungal Infection CPG—was developed by the JTS in direct response to complications seen with this pattern of injury. The development of invasive fungal infections associated with DCBI was noted among marines injured during dismounted patrol in Helmand Province returning for treatment to the National Naval Medical Center (now the Walter Reed National Military Medical Center2). Trauma leadership at the National Naval Medical Center informed the JTS of these fungal infections, and infectious disease colleagues at Landstuhl Regional Medical Center and the Trauma Infectious Disease Outcomes Study Group at the Uniformed Services University of the Health Sciences undertook the development of the Invasive Fungal Infection in War Wounds CPG. The CPG, which was distributed in 2012, identified casualties at risk for invasive fungal infections and directed that these patients have Dakin’s solution applied to wounds as a countermeasure effective at low concentrations against fungus (Rodriguez et al., 2014). Evidence supporting this CPG is Level 3 and is based on retrospective review of a prospectively gathered database.
Other changes in the deployed trauma system were made in response to recommendations from the DCBI task force’s report. For example, the report prompted the deployment of urologists to Role 3 MTFs to improve care of genitourinary injuries in the DCBI context and the equipping of MEDEVAC helicopters with supplies to enable blood-product-based resuscitation (specifically plasma and red blood cell units delivered in a 1:1 ratio) for certain missions. To facilitate early blood-based resuscitation, the task force also called for a major effort to deliver a freeze-dried plasma product to the battlefield. Freeze-dried plasma lacks FDA approval, but freeze-dried plasma produced by the French Army was procured under an Expanded Access Investigational New Drug protocol for U.S. Special Operations Forces. No FDA-approved product is widely available to deployed troops.
Collectively, the changes in JTS guidance and care practices likely led to improvement in survivability. However, no data exist with which to determine impacts on outcomes associated with specific changes in practice, and quality-of-life metrics for survivors remain a significant gap in report-
__________________
2 Walter Reed Army Medical Center and the National Naval Medical Center came under one roof as a joint facility in Bethesda, Maryland, in August 2011.
ing as the focus has been on mortality. The JTS does not currently have the resources to obtain long-term functional recovery and quality-of-life data on combat casualties.
Impact of DoD Research Investment
The DCBI task force and related research efforts expanded on TCCC methods to incorporate use of junctional tourniquets to aid in the control of groin bleeding. Service members on foot patrol suffering improvised explosive device blasts may have very proximal traumatic amputations precluding effective application of extremity tourniquets. Dr. John Kragh at the U.S. Army Institute of Surgical Research demonstrated effective techniques for a junctional tourniquet (the combat-ready clamp) as early as 2012. To date, DoD’s Combat Casualty Care Research Program has yielded several junctional tourniquet models that have been approved by the FDA and fielded on a limited basis.
DCBI, which is associated with significant soft tissue injury and hemorrhage leading to the coagulopathy of trauma, also prompted a particular focus on evaluation of the use of TXA, an antifibrinolytic agent, to improve combat trauma mortality, based on the findings of the CRASH-2 (Clinical Randomization of an Antifibrinolytic in Significant Haemorrhage) trial, published in 2010 (Shakur et al., 2010). Initially, the JTS decided not
to add TXA to resuscitation guidelines because of questions about the applicability of the CRASH-2 study results to combat injuries. However, the Military Application of Tranexamic Acid for Trauma Emergency Resuscitation (MATTERs) study, a retrospective observational cohort study, demonstrated an association between TXA use and improved mortality outcomes in patients treated in deployed U.K.–U.S. MTFs (Morrison et al., 2012). Based on these research data, TXA was added to the Central Command (CENTCOM) formulary, and a recommendation for its use was added to the JTS Damage Control Resuscitation CPG in 2011, even though it has not been approved by the FDA for the treatment of hemorrhage.3 Because of continued concerns regarding potential adverse effects of TXA (e.g., thromboembolic events), its use and the associated risk of complications remain closely monitored through JTS performance improvement processes. DoD has funded several prospective randomized controlled trials of TXA that are currently under way at civilian trauma centers across the United States.
Overall, the recognition of DCBI, the work of the DCBI task force, and related research and development efforts have had a major impact on DoD medical doctrine, training, and materiel. Similar research, development, and education efforts were undertaken by the U.K. military, deepening already significant collaboration between the U.S. and U.K. military medical communities.
Transfer of Knowledge Between Military and Civilian Sectors
Although injury patterns like those associated with DCBI are rare in the civilian sector, valuable concepts from the battlefield warrant transfer to nonmilitary settings. For example, lessons learned related to massive hemorrhage control, including hemorrhage control and transfusion practices, have applicability to other types of injuries more commonly encountered in the United States.
As described above, bidirectional translation of knowledge between the military and civilian sectors and collaborative clinical investigations have been paramount in ongoing efforts to determine the safety and efficacy of TXA for treatment of hemorrhage. Damage control resuscitation more generally represents a notable example of successful translation of military experience to the civilian sector. Early in the wars, the military approach to resuscitation was based on civilian Advanced Trauma Life Support practices for care of acute trauma, but the opportunity to observe a high number of severe traumatic injuries requiring massive transfusion over a
__________________
3 TXA is FDA-approved for prevention or reduction of bleeding during dental procedures for patients with hemophilia and for control of heavy menstrual cyclic bleeding.
short period of time quickly led to the development and adoption of an alternative approach. In response to observations of worsening acidosis and coagulopathy attributed in part to dilution of hemostatic factors following administration of crystalloid and colloid, DoD resuscitative measures evolved to include early resuscitation with blood products (plasma and red blood cells) at a 1:1 or 1:2 ratio (Holcomb et al., 2007). A retrospective study using data from the Joint Theater Trauma Registry showed improved survival associated with use of a 1:1 plasma to red blood cell ratio during massive transfusion (Borgman et al., 2007). Subsequently, inclusion of platelets in massive transfusion was shown to be associated with improved survival, prompting adoption of the 1:1:1 red blood cells:plasma:platelets ratio (Perkins et al., 2009). Massive transfusion practices developed empirically in theater were later validated in large-scale clinical trials conducted in collaboration with the civilian sector. The 2013 PRospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) prospective cohort study (Holcomb et al., 2013) and the 2015 Pragmatic, Randomized Optimal Platelet and Plasma Ratios (PROPPR) randomized controlled trial (Holcomb et al., 2015) provided strong, high-quality evidence for early, balanced massive transfusion ratios.
Military damage control resuscitation practices have since been widely adopted in the civilian sector. In a national survey of trauma medical directors, 67 percent of respondents reported use of a 1:1:1 ratio of red blood cells:plasma:platelets in massive transfusions (Haider et al., 2015). Additional survey data led researchers to conclude that exposure to providers previously affiliated with the military and demonstrated benefits reported in the civilian literature contributed to civilian uptake of the military damage control resuscitation practices.
DCBI results in massive wounds and hemorrhage in the groin and perineum that are difficult to manage with pressure alone. Hemostatic gauze dressings impregnated with kaolin, chitosan, or zeolite have been used successfully on the battlefield to help control bleeding. These hemostatic adjuncts have proven effective and safe in civilian environments as well.
REFERENCES
Borgman, M. A., P. C. Spinella, J. G. Perkins, K. W. Grathwohl, T. Repine, A. C. Beekley, J. Sebesta, D. Jenkins, C. E. Wade, and J. B. Holcomb. 2007. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. Journal of Trauma 63(4):805-813.
Bridges, E., and K. Evers. 2009. Wartime critical care air transport. Military Medicine 174(4):370-375.
Cap, A. P., D. G. Baer, J. A. Orman, J. Aden, K. Ryan, and L. H. Blackbourne. 2011. Tranexamic acid for trauma patients: A critical review of the literature. Journal of Trauma 71(1 Suppl.):S9-S14.
Cap, A. P., P. C. Spinella, M. A. Borgman, L. H. Blackbourne, and J. G. Perkins. 2012. Timing and location of blood product transfusion and outcomes in massively transfused combat casualties. Journal of Trauma and Acute Care Surgery 73(2 Suppl. 1):S89-S94.
Haider, A. H., L. C. Piper, C. K. Zogg, E. B. Schneider, J. A. Orman, F. K. Butler, R. T. Gerhardt, E. R. Haut, J. P. Mather, and E. J. MacKenzie. 2015. Military-to-civilian translation of battlefield innovations in operative trauma care. Surgery 158(6):1686-1695.
Holcomb, J. B., D. Jenkins, P. Rhee, J. Johannigman, P. Mahoney, S. Mehta, E. D. Cox, M. J. Gehrke, G. J. Beilman, M. Schreiber, S. F. Flaherty, K. W. Grathwohl, P. C. Spinella, J. G. Perkins, A. C. Beekley, N. R. McMullin, M. S. Park, E. A. Gonzalez, C. E. Wade, M. A. Dubick, C. W. Schwab, F. A. Moore, H. R. Champion, D. B. Hoyt, and J. R. Hess. 2007. Damage control resuscitation: Directly addressing the early coagulopathy of trauma. Journal of Trauma 62(2):307-310.
Holcomb, J. B., D. J. del Junco, E. E. Fox, C. E. Wade, M. J. Cohen, M. A. Schreiber, L. H. Alarcon, Y. Bai, K. J. Brasel, and E. M. Bulger. 2013. The PRospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) study: Comparative effectiveness of a time-varying treatment with competing risks. JAMA Surgery 148(2):127-136.
Holcomb, J. B., D. P. Donathan, B. A. Cotton, D. J. Del Junco, G. Brown, T. V. Wenckstern, J. M. Podbielski, E. A. Camp, R. Hobbs, Y. Bai, M. Brito, E. Hartwell, J. R. Duke, and C. E. Wade. 2015. Prehospital transfusion of plasma and red blood cells in trauma patients. Prehospital Emergency Care 19(1):1-9.
Krueger, C. A., J. C. Wenke, and J. R. Ficke. 2012. Ten years at war: Comprehensive analysis of amputation trends. Journal of Trauma and Acute Care Surgery 73(6 Suppl. 5):S438-S444.
Langan, N. R., M. Eckert, and M. J. Martin. 2014. Changing patterns of in-hospital deaths following implementation of damage control resuscitation practices in US forward military treatment facilities. JAMA Surgery 149(9):904-912.
Morrison, J. J., J. J. DuBose, T. E. Rasmussen, and M. J. Midwinter. 2012. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) study. Archives of Surgery 147(2):113-119.
Morrison, J. J., J. D. Ross, J. J. DuBose, J. O. Jansen, M. J. Midwinter, and T. E. Rasmussen. 2013. Association of cryoprecipitate and tranexamic acid with improved survival following wartime injury: Findings from the MATTERs II study. JAMA Surgery 148(3):218-225.
O’Reilly, D. J., J. J. Morrison, J. O. Jansen, A. N. Apodaca, T. E. Rasmussen, and M. J. Midwinter. 2014. Prehospital blood transfusion in the en route management of severe combat trauma: A matched cohort study. Journal of Trauma and Acute Care Surgery 77(3 Suppl. 2):S114-S120.
Perkins, J. G., A. P. Cap, P. C. Spinella, L. H. Blackbourne, K. W. Grathwohl, T. B. Repine, L. Ketchum, P. Waterman, R. E. Lee, A. C. Beekley, J. A. Sebesta, A. F. Shorr, C. E. Wade, and J. B. Holcomb. 2009. An evaluation of the impact of apheresis platelets used in the setting of massively transfused trauma patients. Journal of Trauma 66(Suppl. 4):S77-S84.
Powell-Dunford, N., J. F. Quesada, R. F. Malsby, V. Chou, R. T. Gerhardt, K. R. Gross, and S. A. Shackelford. 2014. Risk management analysis of air ambulance blood product administration in combat operations. Aviation, Space, and Environmental Medicine 85(11):1130-1135.
Rodriguez, C. J., A. C. Weintrob, J. Shah, D. Malone, J. R. Dunne, A. B. Weisbrod, B. A. Lloyd, T. E. Warkentien, C. K. Murray, K. Wilkins, F. Shaikh, M. L. Carson, D. Aggarwal, and D. R. Tribble. 2014. Risk factors associated with invasive fungal infections in combat trauma. Surgical Infections (Larchmont) 15(5):521-526.
Shakur, H., I. Roberts, R. Bautista, J. Caballero, T. Coats, Y. Dewan, H. El-Sayed, T. Gogichaishvili, S. Gupta, J. Herrera, B. Hunt, P. Iribhogbe, M. Izurieta, H. Khamis, E. Komolafe, M. A. Marrero, J. Mejia-Mantilla, J. Miranda, C. Morales, O. Olaomi, F. Olldashi, P. Perel, R. Peto, P. V. Ramana, R. R. Ravi, and S. Yutthakasemsunt. 2010. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): A randomised, placebo-controlled trial. Lancet 376(9734):23-32.
SEVERE TRAUMATIC BRAIN INJURY CASE
Case Description
A 29-year-old male service member suffered a gunshot wound to the head while on patrol. In the field, he was noted to have strong carotid pulses, a heart rate (HR) of 130 beats per minute (bpm), and a respiratory rate (RR) of 75 breaths per minute. He was unresponsive and exhibited decorticate posturing.
Role 1 Care
In the field, a cricothyroidotomy was performed, and a surgical airway was placed. The patient was also wrapped in a hypothermia prevention blanket.
Tactical Evacuation
The patient was evacuated within 5 minutes of the request for evacuation. Transport to a Role 3 MTF required an hour, and on arrival the flight medics noted the following vital signs: blood pressure (BP) 80 mmHg (systolic only), HR 135 bpm, RR 30, Glasgow coma score (GCS) 3, oxygen saturation (SpO2) 95 percent. Both pupils were reactive; the right pupil measured 3 mm and the left pupil 4 mm. The patient had significant bleeding from his head wound, leading to concern about hypovolemia and shock. Hypertonic saline was administered, and he was transfused 2 units of red blood cells en route. He continued to exhibit decorticate posturing. Ventilation was maintained by bag-valve-mask, and SpO2 was sustained at 100 percent.
Role 3 Care
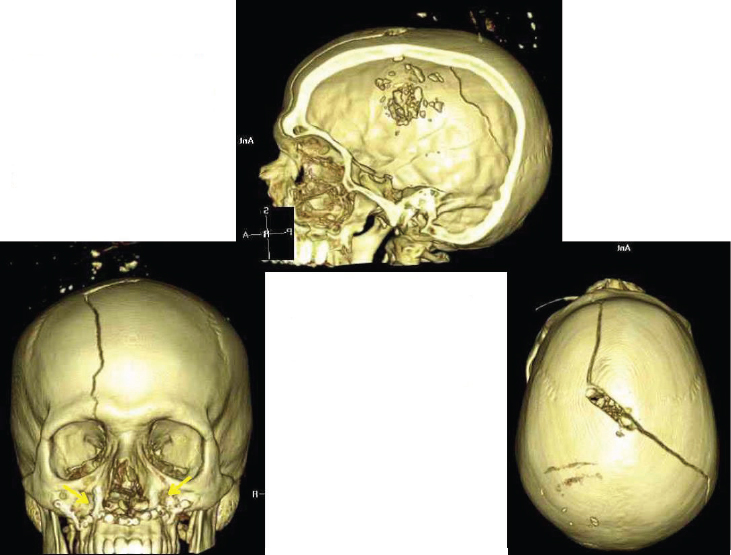
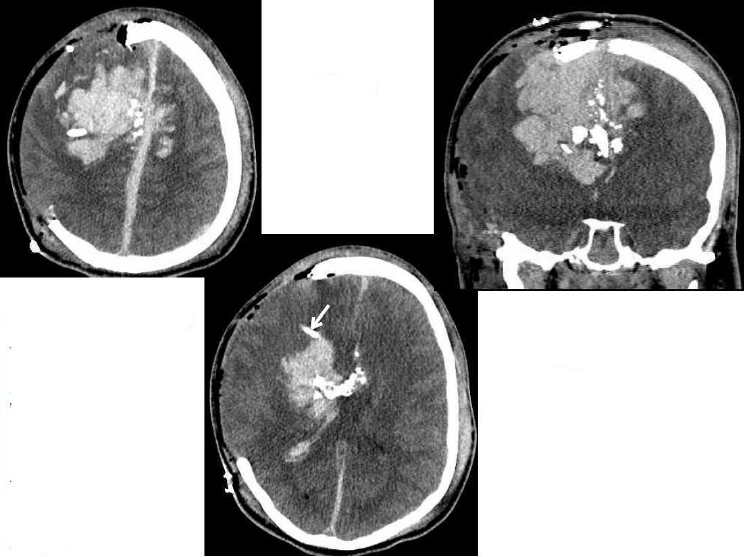
Upon the patient’s arrival at the Role 3 MTF, a CT scan revealed the gunshot wound to the vertex of the skull with displacement of multiple bone fragments (see Figures A-8 and A-9). The patient showed diffuse cerebral edema, intraparenchymal hematoma, subarachnoid hemorrhage, subdural hemorrhage, and epidural hemorrhage at the vertex in association with disruption of the middle third of the superior sagittal sinus. He was urgently taken to the operating room for decompressive hemicraniectomy, evacuation of subdural hematoma, and placement of a right-sided external ventricular drain (EVD). The 7.5F field cricothyroidotomy tube was replaced by an 8.0F tracheostomy. The patient was administered thyroxin on a standard T4 protocol, as well as 3 percent sodium chloride (NaCl).
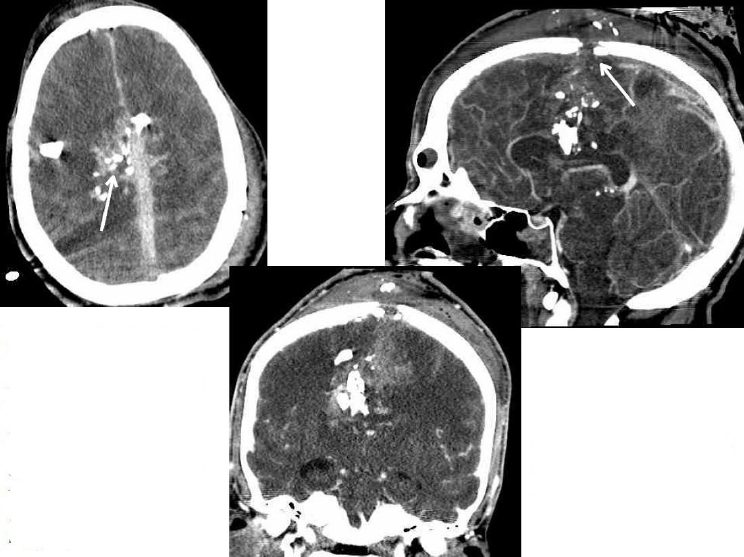
A second EVD was placed on the left side to control increased intracranial pressure measurement of 23 cm H2O resulting from bifrontal cerebral hemorrhaging. Following this intervention, intracranial pressure improved to 8-10 cm H2O, and the patient had a cerebral perfusion pressure of 60 mmHg. Tranexamic acid (TXA) was also infused in an effort to control bleeding. Ultimately, the patient’s GCS improved to 7T, with a motor score of 4. He underwent bronchoscopy to evaluate the effects of the surgical airway procedures and was found to have no evidence of tracheal injury.
Evacuation Out of Theater
The patient was transferred out of theater on post-injury day 1 via the critical care air transport team. Cerebral protective strategies were maintained throughout transport. Sedation was increased prior to transport,
resulting in a drop in GCS from 6T to 3T. In flight, cerebral perfusion pressure was maintained at greater than 60 mmHg with low-dose vasopressors, and intracranial pressure was maintained at less than 20 mmHg. The patient was transfused 2 units of red blood cells and a 300-mL bolus of normal saline. His hemoglobin increased from 8.2 to 9.2 g/dL. Upon arrival at Landstuhl Regional Medical Center in Germany, his GCS returned to 6T.
Role 4 Care
Upon arrival at Landstuhl, the patient was rapidly weaned off vasopressors and was evaluated by a neurosurgeon. His GCS was initially 5T, with intracranial pressure less than 20 cm H2O, and his brain stem reflexes were intact. A repeat CT scan revealed intraventricular and large intraparenchymal hemorrhages (see Figure A-10). His intracranial pressure gradually increased to greater than 20 mmHg, and he was taken back to the operating room for evacuation of hematomas and drain placement.
Following surgery, his intracranial pressure improved, and enteral feeding and prophylaxis for deep venous thrombosis were initiated. He was evacuated to the United States with a GCS of 4T.
Role 5 Care
On arrival in the United States, the patient was hemodynamically stable but febrile. The infectious diseases service was consulted and confirmed a diagnosis of right lower lobe pneumonia. The patient was administered antibiotics and antifungals, resulting in resolution of the pneumonia. His brain edema gradually resolved, and his GCS increased to 5T with a normal intracranial pressure. He was transitioned to Emerging Consciousness Rehabilitation after the ventriculostomies were removed on post-injury day 35. There, early rehabilitation was initiated with a multidisciplinary team specializing in this type of care. Long-term follow-up demonstrated
the patient’s dramatically improved mental status. He can communicate reliably and is fully oriented. However, he does exhibit several cognitive deficits, such as reduced attention span, reduced visual-spatial skills, and left-sided neglect, as well as some memory impairment. His physical status also has improved; he is able to use his right upper extremity and has modest antigravity strength in his right lower extremity. He has severe impairment of his left upper and lower extremities due to the site of his brain injury. He tolerates sitting for greater than 4 hours per day and can stand for 40 minutes at a time. His tracheostomy was removed, and he can eat a regular diet.
Case Discussion
Care for severe traumatic brain injury (TBI) fundamentally involves maintaining perfusion of the brain with oxygenated blood. This treatment applies whether the patient is injured on a highway in the United States or on a dismounted patrol in Afghanistan. In this case, the actions taken by the medic in the field to prevent hypoxia and secondary brain injury, prompt evacuation of the patient to a Role 3 MTF, rapid resuscitation to restore cerebral perfusion and ensure oxygenation, damage control resuscitation, aggressive neurosurgical interventions, and early multidisciplinary rehabilitation (Nakase-Richardson et al., 2013) all contributed to the successful outcome for this patient despite the challenges of caring for severe TBI cases in a remote, austere environment.
This case demonstrates how providing a more advanced resuscitative capability closer to the point of injury might improve outcomes in severe TBI. Hypoxia has been shown to be associated with poor outcomes for TBI in both the military and civilian literature (Badjatia et al., 2008). This patient immediately received measures to control his airway to ensure oxygenation. The cricothyroidotomy was an essential prehospital task performed by the field medic, especially in light of the anticipated transport, and indicates a high level of medic training. Administration of 3 percent saline by pre-MTF providers was introduced to the TCCC guidelines at the start of the recent conflicts; however, neuroprotective measures were not mentioned in the original TCCC article in 1996. Another example of increased capability for pre-MTF providers in the updated TCCC guidelines is the guidance to administer TXA.
This case also illustrates the military’s highly aggressive approach to managing service members with severe TBI. Cerebral resuscitation began during the tactical evacuation. The patient presented with hypotension, a neurologic emergency in the context of severe TBI (Badjatia et al., 2008). Administering blood products and hyperosmolar therapy and ensuring adequate oxygenation were essential in anticipation of the 1-hour trans-
port time to surgical intervention (Brain Trauma Foundation et al., 2007). In the Role 3 MTF, the patient underwent prompt surgery for hematoma evacuation, decompressive craniectomy, and EVD placement to control intracranial pressure. These interventions accord with the JTS Management of Severe Brain Trauma CPG (JTS, 2014) and Brain Trauma Foundation guidelines (Brain Trauma Foundation et al., 2007).
The Military Learning Process
Retrospective studies using DoDTR data have informed changes in military trauma care practices, codified through the JTS CPGs. DoD clinical investigators may submit queries to the JTS Data Analysis Branch if they wish to receive information from the DoDTR. A clinical investigator’s proposal is reviewed by his or her local regulatory group to determine whether the investigation is research or a performance improvement effort. If the clinical investigation is deemed research, a formal institutional review board review must be conducted.
While initially drawing heavily on civilian sector best practice guidelines for care of brain trauma (e.g., Brain Trauma Foundation guidelines), the JTS CPGs evolved as data showing the benefit of aggressive neurosurgical intervention and critical care management accumulated (DuBose et al., 2011). For example, a large retrospective analysis of Joint Theater Trauma Registry (JTTR)4 data for patients with severe TBI led to recommendations for early hemicraniectomy as part of damage control in anticipation of overseas transport (Bell et al., 2010). (The JTS CPGs relevant to severe TBI are listed in Box A-4.)
Another important intervention discussed in this case—the use of a hypothermia prevention blanket—represents an intervention implemented after review of JTTR data indicated worse outcomes in hypothermic TBI patients (Arthurs et al., 2006). Hypothermia is a major concern in the management of trauma patients, largely because of the impact of hypothermia on traumatic coagulopathy (Morrison et al., 2013). In 2006, the JTS released a CPG on hypothermia prevention, monitoring, and management, resulting in a significant reduction in hypothermia incidence (Nesbitt et al., 2010; Palm et al., 2012).
Transfer of Knowledge Between Military and Civilian Sectors
In contrast to previous conflicts, in which patients with severe TBI would have been treated as expectant, deployed medical providers in Afghanistan and Iraq adopted a highly aggressive posture in managing service
__________________
4 The JTTR was the precursor of the DoDTR.
members with these injuries (Bell et al., 2010). This approach has been supported by patient outcome data. With respect to short-term outcomes, 32 percent of casualties with an admission GCS of 3 to 5 progressed to functional independence (Weisbrod et al., 2012). Colleagues at Department of Veterans Affairs rehabilitation centers reported that most patients (64 percent) enrolled in a disorders-of-consciousness program emerged to regain consciousness during rehabilitation (Nakase-Richardson et al., 2013). Despite these encouraging outcome data, however, neurosurgical interventions for severe TBI are controversial in the civilian sector.
A study of severe TBI published in 2011 revealed that mortality outcomes in military patients compared favorably with those in the civilian population (DuBose et al., 2011). In this study, military TBI patients in the DoDTR meeting inclusion criteria were propensity matched to similar patients from the National Trauma Data Bank (DuBose et al., 2011). Military patients were much more likely to undergo any operative intervention (21.5 percent versus 7.2 percent in the civilian population) such as invasive intracranial pressure monitoring, craniectomy, or craniotomy. The overall mortality rate was approximately 3 times lower for military patients relative to their civilian counterparts (7.7 percent versus 21.0 percent). The difference in mortality outcomes was even more striking when the analysis was restricted to penetrating brain injury (5.6 percent and 47.9 percent for
military and civilian patients, respectively). This differential is surprising in light of the complex patient movements required for care of combat casualties with these severe injuries, and indicates that the civilian sector may benefit from evaluating and, as appropriate, adopting military approaches to the care of severe TBI. Currently, it is impossible to identify any one factor that may account for this differential, and there are significant differences in military and civilian settings (e.g., destructive force of weaponry, personal protective gear) that need to be considered. Prospective studies are needed to validate the application of aggressive TBI management practices in the civilian population and inform changes to civilian guidelines, such as those of the Brain Trauma Foundation and the Trauma Quality Improvement Program.
REFERENCES
Arthurs, Z., D. Cuadrado, A. Beekley, K. Grathwohl, J. Perkins, R. Rush, and J. Sebesta. 2006. The impact of hypothermia on trauma care at the 31st Combat Support Hospital. American Journal of Surgery 191(5):610-614.
Badjatia, N., N. Carney, T. J. Crocco, M. E. Fallat, H. M. Hennes, A. S. Jagoda, S. Jernigan, P. B. Letarte, E. B. Lerner, T. M. Moriarty, P. T. Pons, S. Sasser, T. Scalea, C. L. Schleien, D. W. Wright, Brain Trauma Foundation, and BTF Center for Guidelines Management. 2008. Guidelines for prehospital management of traumatic brain injury, 2nd edition. Prehospital Emergency Care 12(Suppl. 1):S1-S52.
Bell, R. S., C. M. Mossop, M. S. Dirks, F. L. Stephens, L. Mulligan, R. Ecker, C. J. Neal, A. Kumar, T. Tigno, and R. A. Armonda. 2010. Early decompressive craniectomy for severe penetrating and closed head injury during wartime. Neurosurgical Focus 28(5):E1.
Brain Trauma Foundation, American Association of Neurological Surgeons, and Congress of Neurological Surgeons. 2007. Guidelines for the management of severe traumatic brain injury. Journal of Neurotrauma 24(Suppl. 1):S1-S106.
Butler, F. K., J. Haymann, and E. G. Butler. 1996. Tactical combat casualty care in special operations. Military Medicine 161(Suppl. 3):3-16.
CoTCCC (Committee on Tactical Combat Casualty Care). 2014. Tactical combat casualty care guidelines. Available at http://www.usaisr.amedd.army.mil/pdfs/TCCC_Guidelines_140602.pdf.
DuBose, J. J., G. Barmparas, K. Inaba, D. M. Stein, T. Scalea, L. C. Cancio, J. Cole, B. Eastridge, and L. Blackbourne. 2011. Isolated severe traumatic brain injuries sustained during combat operations: Demographics, mortality outcomes, and lessons to be learned from contrasts to civilian counterparts. Journal of Trauma 70(1):11-16.
JTS (Joint Trauma System). 2014. Clinical practice guideline: Management of patients with severe head trauma. http://www.usaisr.amedd.army.mil/cpgs/Mgmt_of_Patients_with_Severe_Head_Injury_16Jun2014.pdf (accessed July 23, 2015).
Morrison, J. J., J. D. Ross, H. Poon, M. J. Midwinter, and J. O. Jansen. 2013. Intra-operative correction of acidosis, coagulopathy and hypothermia in combat casualties with severe haemorrhagic shock. Anaesthesia 68(8):846-850.
Nakase-Richardson, R., S. McNamee, L. L. Howe, J. Massengale, M. Peterson, S. D. Barnett, O. Harris, M. McCarthy, J. Tran, S. Scott, and D. X. Cifu. 2013. Descriptive characteristics and rehabilitation outcomes in active duty military personnel and veterans with disorders of consciousness with combat- and noncombat-related brain injury. Archives of Physical Medicine and Rehabilitation 94(10):1861-1869.
Nesbitt, M., P. Allen, A. Beekley, F. Butler, B. Eastridge, and L. Blackbourne. 2010. Current practice of thermoregulation during the transport of combat wounded. Journal of Trauma and Acute Care Surgery 69(1):S162-S167.
Palm, K., A. Apodaca, D. Spencer, G. Costanzo, J. Bailey, L. H. Blackbourne, M. A. Spott, and B. J. Eastridge. 2012. Evaluation of military trauma system practices related to damage-control resuscitation. Journal of Trauma and Acute Care Surgery 73(6 Suppl. 5):S459-S464.
Weisbrod, A. B., C. Rodriguez, R. Bell, C. Neal, R. Armonda, W. Dorlac, M. Schreiber, and J. R. Dunne. 2012. Long-term outcomes of combat casualties sustaining penetrating traumatic brain injury. Journal of Trauma and Acute Care Surgery 73(6):1525-1530.