Board on Children, Youth, and Families |
May 2016 |
Opportunities to Promote Children’s Behavioral Health: Health Care Reform and Beyond—Workshop in Brief
RESPONDING TO THE CHALLENGE
Neal Halfon, director, Center for Healthier Children, Families & Communities at the University of California, Los Angeles, began by noting that about one in five children and adolescents are seen with signs and symptoms of a disorder listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Those disorders include nervosa, major depressive disorder, bipolar disorder, schizophrenia, and bulimia nervosa, of which nearly three-quarters have their onset before age 25: see Figure 1. However, only an estimated 20 percent of the children receive mental health services (National Institutes of Health, 2007). He also noted that the child health system is one of fragmented service delivery, with significant inequities, difficulties in accessing services, and limited local responsibility. Overall, the system does not match the current needs of the population, and it faces substantial resource constraints.
Halfon argued for systemic change: “. . . from one focused on diagnosing and treating chronic diseases to one focused on optimizing population health.” He offered a four-point strategy: (1) fix what is broken in the current system, (2) increase the use of evidenced-based practices and resources, (3) adopt innovative approaches that drive improvements, and (4) undergo a transformative paradigm shift with changes to the operating system.
The ultimate goal, he said, is a national network for child health development that will fundamentally transform the entire children’s health care system. Halfon said that he and his colleagues have been working on such a transformation, which is designed to leverage the implementation of the ACA as a means to establish a systematic process of monitoring, analyzing, and responding to new challenges and prospects.
![]()
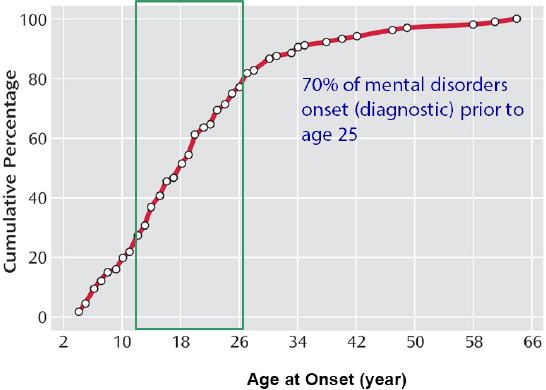
FIGURE1 Mental disorder diagnosis by age.
SOURCE: Presentation at workshop by Neal Halfon.
FUNDING: OPPORTUNITIES AND CHALLENGES
Currently, Medicaid and the Children’s Health Insurance Program (CHIP) cover one in three children in the United States. Since the ACA, it and other funding sources have created new modalities, such as managed care, to increase payment integration and promote coordination of care for children. The challenge is to integrate services and resources that take place at four levels, said Lindsey Browning, a policy analyst with the National Association of Medicaid Directors. Those four levels are service agencies, payment systems, health care providers, and practitioners of early intervention for children. Links across all the levels are needed to coordinate care, she said.
Mark Friedlander, chief medical officer for behavioral health for commercial plans at Aetna, explained that the challenge at the payment level is to transform the way behavioral services are delivered. Payment for delivery of behavioral services by primary care physicians is now in place. The focus should be on quality of the services that are being provided, he said, but private payers cannot evaluate the efficacy of care based on the reimbursement claims they receive. For example, two claims may appear similar when they come into the system, but the payer has no way of knowing if the patient was cured or not, or even if the care provided was of high quality.
Friedlander said that the ACA is beginning the needed transformation by increasing accountability through incentives to providers that produce high-quality care. He stressed that this change from fee-for-service to paying for accountability is a significant opportunity offered by the ACA. This focus on accountability allows for integrated care to be at the forefront of change.
Lindsey Browning, a policy analyst with the National Association of Medicaid Directors, stressed the importance of having high-quality measures in place in terms of reviewing integration across various populations. She noted that the National Quality Forum released a behavioral health clinical performance measure that focuses on depression screening and treatment.1
Mary Ann McCabe, associate clinical professor of pediatrics at George Washington University and affiliate faculty in psychology at George Mason University, noted that the focus on integration does not address the fact that at the state, community, and practice levels, physical and mental health conditions are viewed as two separate entities.
___________________
1Additional information on the National Quality Forum measures can be found at https://www.qualityforum.org [March 2016].
INNOVATIONS AT THE STATE AND LOCAL LEVELS
Several states have created programs and initiatives focused on children’s behavioral and integrated health care. Anthony Biglan, senior scientist at Oregon Research Institute (ORI), described several innovations in that state. The Oregon State Plan, which covers 26 percent of the state’s population, includes coordinated care organizations at the county or community level that act as health insurers. This model has succeeded in its goals. For example, in Lane County, Oregon, a coordinated care organization works with ORI on funding prevention activities in the community and on integrating behavioral health and primary care. Oregon has also created the Early Learning Council, which works on assessing the needs of young children for successful development. The key point of this council is that it focuses on working with the community to support children’s development. Currently, every child of a low-income family in Oregon has health insurance.
George Hagan, chief of pediatrics at the Cambridge Health Alliance and clinical instructor in pediatrics at Massachusetts General Hospital and Harvard Medical School, described some programs in that state. The Cambridge Health Alliance, the last free-standing public safety net entity in the state,2 works on the integration of mental health services within its primary care clinics, but all its efforts have been for adults, rather than children or families. The ACA has played a role in building a linkage between primary care and mental health providers with the state Medicaid program. Within the next 3 years, all Medicaid patients will be shifted to a fully owned risk model. There are several challenges associated with this push towards mental health integration, he said, including minimal data on expenses. However, planned change “is a work in progress.” Hagan said that in his own practice he is creating a working model of a collaborative practice in which a child psychiatrist and a child psychiatry fellow spend two afternoons a week at his practice and are fully integrated into his team.
Kelly Kelleher, a pediatrician at the Nationwide Children’s Hospital, described the pediatric accountable care organization, Partners for Kids, which consists of 800 providers, including primary care physicians, pediatricians, specialty care providers and the sponsoring hospital, Nationwide Children’s Hospital.3 He explained three lessons learned from taking on full capitation risk of a population across a large region. The first is that by creating a linkage for better communication among providers, there was a decrease in behavioral health readmission rates. The second is that data and metrics are becoming the driving force. The third is that prevention is a priority.
Lori Stark, division director of behavioral medicine and clinical psychology at Cincinnati Children’s Hospital Medical Center, noted that although the ACA created a stronger commitment by organizations to their communities, other challenges exist for those implementing innovative programs at the state and local levels. They include children in the juvenile justice and foster care systems who often lose certain supports as they transition to adulthood. Stark also indicated that despite the existence of innovative policies, some providers are unsure of how to implement them, especially when there is uncertainty as to whether or not they will be paid for their service. She said: “Not only do we need the policies, we also need the leadership and the vision within our own organizations to push for implementing those policies.”
INTERMEDIARY GROUPS FOR TWO-GENERATION APPROACHES
Parinda Khatri, chief clinical officer of the Cherokee Health System, said the next step in behavioral and mental health care is the two-generation approach: working with children and their parents or caregivers. The Cherokee Health System is an example of integrative health care, in which psychologists, social workers, care coordinators, community health workers, and psychiatrists are all working together with the entire family to address subclinical issues. Her organization collaborated with the Department of Children’s Services (DCS) and the foster care system in Tennessee to be able to provide care coordination to children in DCS custody or identified as at risk.
In prenatal clinics, providers have a particular focus on prevention of poor neonatal health outcomes for mothers who are at risk. Every woman is evaluated by a psychologist, has a case manager, and receives assistance in acquiring housing, transportation, food, and parenting skills. Khatri also discussed challenges associated with payers after the ACA.
___________________
2Additional information on the Cambridge Health Alliance can be found at http://www.challiance.org/ [March 2016].
3Additional information on Partners for Kids can be found at http://www.partnersforkids.org/ [March 2016].
One challenge is that payers generally focus on their most expensive cases (older adults with multiple chronic conditions). In addition, the system may overlook preventive care options when it requires certain illnesses to present themselves before services can be rendered. For instance, Khatri saw a young girl who weighed 240 pounds: when Khatri advocated that the patient needed to be enrolled in an obesity program, the child’s insurance company said that she needed to have diabetes prior to being eligible to join the program. “This is not the way we want to do it,” Khatri said.
School-based health centers are another way to implement integrated care and engage parents, noted John Schlitt, president of the School-Based Health Alliance. He said that school-based health centers are “the progenitors of health care transformation.” When providing care to children, the centers have an opportunity to work with parents (or guardians). Some school-based health centers are considered eligible to receive funding as a patient centered medical home, as defined by the Agency for Healthcare Research and Quality.4
The National Academy for State Health Policy (NASHP)—an independent academy of state health policy makers that includes representatives from Medicaid, children’s health insurance programs, state insurance exchanges, state mental health agencies, and public health agencies—is currently looking into mental health coverage in the small-group insurance marketplace. Karen VanLandeghem, senior program director at NASHP, explained that an important component of the ACA is the triple aims of improving patients’ care experience, improving the health of populations, and reducing the per capita cost of health care. The Maternal, Infant, and Early Childhood Home Visiting Program provides an opportunity to use the two-generation approach for pregnant women and children; however, it is currently used by a small percentage of women who need home visits. Another area of opportunity is for states to expand Medicaid coverage to individuals with incomes up to 138 percent of the federal poverty level. As several states still lack using this type of coverage option, VanLandeghem clarified that at this time mental health coverage is still ambiguous under the insurance exchanges.
The business sector is another area of opportunity to integrate mental health services. Sara Watson described the work of ReadyNation, a national business membership organization that encourages its members to meet with policy makers to promote the workforce of the future by investing in children.5 Watson stressed that when business leaders meet with a member of Congress, they have to have relevant data on how investments in children keep employers’ costs down in order to advocate for changes inside and outside the health care system.
INNOVATIONS IN PRIMARY CARE AND OTHER SETTINGS
Throughout, the workshop emphasized that primary care is a universal access point for health care. Rahil Briggs, associate professor of clinical pediatrics at Albert Einstein College of Medicine and director of pediatric behavioral health services at Montefiore Medical Group, described the integration of mental health programs in the primary care setting at Montefiore. They have implemented the Healthy Steps Program that uses an integrated early childhood two-generation mental health approach to recognize at-risk families during the prenatal period. It has now become a full lifespan integrated behavioral health system within a primary care network, serving about 300,000 patients. For instance, during every newborn visit, both parents and children receive trauma screening and then an annual screening thereafter. Caregivers also work with adolescent patients, using short-term modules on depression, anxiety, attention, conduct, and trauma. Briggs said that one challenge has been to develop the needed workforce in terms of finding qualified psychiatrists and psychologists. There is about one child psychiatrist for every 20,000 children in Montefiore’s location in the Bronx.
Many participants commented that prevention is key. Joseph F. Hagan, Jr., a clinical professor in pediatrics at the University of Vermont College of Medicine and Vermont Children’s Hospital, noted that the ACA recognized this in adopting the Bright Futures Guidelines, first published by the American Academy of Pediatrics in the early 1990s with a vision of health supervision in the context of family.6 The goal is enhancing the delivery of behavioral and developmental well-child care into approaches that can be applied to pediatric and family medicine practices across the nation. The ACA designated the Bright Future Guidelines as the standard of care for
___________________
4Additional information on patient centered medical home can be found at https://pcmh.ahrq.gov/ [March 2016].
5Additional information on ReadyNation can be found at http://www.readynation.org/ [March 2016].
6Additional information on Bright Futures can be found at https://brightfutures.aap.org/ [March 2016].
preventive services from birth to 21 years of age.
Barry Sarvet, chief of child and adolescent psychiatry at Baystate Medical Center and clinical professor at Tufts University School of Medicine, described the Massachusetts Child Psychiatry Access Project (MCPAP), of which he is the clinical director. MCPAP connects pediatricians to child psychologists and psychiatrists to improve mental health care and access. Although MCPAP focuses on secondary and tertiary prevention, it has created another program called MCPAP for moms in recognition that that care for maternal depression is crucial for primary prevention.
Child Health Improvement through Computer Automation (CHICA) is a clinical decision support system, developed at Indiana University School of Medicine by Dr. Steve Downs and colleagues that uses existing electronic medical records to augment clinic encounters (Anand et al., 2004). For instance, when a child comes to a clinic, CHICA downloads that patient’s record, runs several rules, and selects 20 yes-or-no questions to ask the patient’s family. It then gives no more than six reminders to the pediatrician to address during the encounter, with an alert to document how the pediatrician responded. The approach is based on guidelines from the American Academy of Pediatrics with recommendations from the U.S. Preventive Services Task Force, the Centers for Disease Control and Prevention, and other organizations.
Another program was described by Bernadette Melnyk, associate vice president for health promotion and dean of the College of Nursing at Ohio State University. As background, she noted that in 2013, more than 3 million children—most of them under the age of 1—required services from child welfare systems in the United States. The program she developed, with multiple randomized controlled trials, focused on interventions with parents of premature babies: this program decreased parental stress and improved child outcomes at 3 years, she reported. She also developed the Creating Opportunities for Personal Empowerment (COPE) Program, which is a life-style intervention to assist adolescents to engage in healthy behaviors and improve their mental health. Around 300 health care providers have been trained to use COPE and provide cognitive-behavioral therapy interventions to depressed or anxious children and teenagers. Providers are reimbursed for their time on COPE in primary care settings. Melnyk noted that the ACA is beginning to reimburse providers that follow evidence-based measures for screening and behavioral counseling.
Head Start and early childhood programs provide models for integration of services, stressed Kris Perry, executive director of the First Five Years Fund. For example, she said, health care professionals should think of early childhood educational programs as settings in which nutrition and other health-related education can be delivered. Responding to this point, Sheppard Kellam, professor emeritus at Johns Hopkins Bloomberg School of Public Health, contended that the educational system should be more engaged in health care and receive support from the community to do so. An example of the need, he said, is that schools collect data on students with attention deficit and hyperactivity disorders, but teachers are given minimal or no training on how to deal with these students in their classrooms.
THE RESEARCH LANDSCAPE FOR PRIMARY CARE AND CHILDREN’S BEHAVIORAL HEALTH
Joan Asarnow, professor of psychiatry and biobehavioral sciences at the David Geffen School of Medicine at the University of California at Los Angeles, turned to the subject of suicide, which is a leading cause of death for children (10- to 14-year olds), adolescents (15- to 19-year olds), and young adults (20- to 29-year olds). Those data point to the need for effective treatment for behavioral health problems. Interventions in childhood and adolescence are needed, she said, to prevent suffering, dysfunction, and premature death. Asarnow agreed with others that “integrated primary medical and behavioral health care provides at least part of the solution for addressing the behavioral health needs of children.”
Asarnow presented a recently published systematic meta-analysis that looked at behavioral health outcomes for children and adolescents with integrated medical-behavioral health care versus those with usual primary care (Asarnow et al., 2015). The meta-analysis showed a large variation in affects across studies and highlights the need for more promising models of integrated care. She described one such model, the Youth Partners in Care Program, in which children are screened for depression symptoms and are referred as appropriate to a care manager. The child is then given a book titled “Stress and Your Mood” that educates on stress, depression, and ways to decrease depressive symptoms. The care manager discusses the child’s needs with the child’s primary care provider and also helps the family and patient to explore treatment options.
They all then meet with the provider, who considers if further evaluation is needed by a specialist.
There are several challenges associated with treatment for behavioral health issues in primary care settings, Asarnow said: providers feel ill-prepared and in need of training, consultation, and additional resource materials; they report limited resources for collaborative care; and they express concern about inadequate follow-up. There is a need for a rigorous evaluation and continuous quality improvement process to improve care, she said. The next steps are to create effective integrated care models in primary care settings.
John Landsverk, research scientist at the Oregon Social Learning Center, commented further on the role of parents. “Involvement of parents is critical for children’s health, possibly even more so for behavioral health,” he said. Effective parenting skills, which are essential for positive outcomes, include reinforcement, emotion regulation, supervision, control, discipline, supportive behaviors to promote development, and discouraging child behaviors that prevent positive adaptation. The positive outcomes include improved social skills, increased language, sustained attention, less abuse, less involvement in juvenile justice system, safe home environments, reduced peer aggression, and fewer mental health symptoms.
LOOKING FORWARD: REFLECTIONS FOR PUBLIC POLICY AND RESEARCH
David Shern, National Association of State Mental Health Program Directors, turned to broader issues of public policy. He reported that the United States incarcerates more people, spends more money on health care, has the highest rates of mental illness, and has one of the lowest academic achievement levels of OECD nations. It is important to note, he said, that recent research shows that the antecedents for many of these problems involve unhealthy child behavioral-health development. These problems become a public health concern by establishing a life-course trajectory that evidences itself in behavioral health issues, academic challenges, decreased socioeconomic status, and a cycle of poverty, noted Shern.
Wilson Compton, deputy director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health (NIH), noted significant changes that have occurred because of the ACA and other health reforms. The key ones are primary care integration of mental health services and payment reforms and systems-level change, which is a shift to a population-based payment for services. There is also recognition of the need for workforce development, especially for developmental and behavioral pediatric, child psychology, and related expertise to provide the necessary services.
Involving the family is a pattern that was noted within the workshop. An approach that works under this model is the Family-to-Family Health Information Centers, which were described by Julianne Beckett, cochair of the FamilY Partnerships Network, an advisory group to the American Academy of Pediatrics Board of Directors. These centers, which now exist in every state and the District of Columbia, are managed by families, and they work with professionals to meet the needs of families including children with special needs. Shern stressed the importance of not blaming parents for behavioral problems in their children.
Jorielle Brown, director of the Division of Systems Development in the Center for Substance Abuse Prevention at the Substance Abuse and Mental Health Services Administration (SAMHSA), noted that prevention is at the intersection of primary care, mental health, and substance abuse but that there is still work to be done in translating research into practice. She described another program focused on prevention, “Talk. They Hear You.”7 The program focuses on the parents and guardians of children aged 9 to 15 and assists them in communicating about underage drinking. Through partnerships with primary care provider organizations, the campaign led to public service announcements in more than 30,000 doctor’s offices and has reached countless parents and guardians.
Participants discussed the need to consider the best modality to develop and disseminate messages that will influence public perceptions and receive political support. One participant noted that the Frameworks Institute does work on framing messages about the significance of early childhood development.8 Other suggestions included tracking the public interests and concerns, using television shows, strengthening the community of researchers and providers viewpoints, creating a federal office of children’s health, and integrating the vision of prevention and behavioral health into the foundation of Healthy People 2030.
___________________
7Additional information on “Talk. They Hear You.” can be found at http://www.samhsa.gov/underage-drinking/ [March 2016].
8Additional information on the FrameWorks Institute can be found at http://www.frameworksinstitute.org/ [March 2016].
David Hawkins, University of Washington School of Social Work, noted that some children do not have primary care providers and only come to clinics when they, or their parents, have a problem. One option might be “one-stop shopping” primary care clinics, but research is needed to see which approach is the best. McCabe noted the parallels that exist in integration of primary care. For instance, integrating behavioral health into health care, health care into communities, social services into the social and behavioral determinates of health have several similarities. Because of this, McCabe stressed the importance of integrating service and research agendas as well as facilitating connections across different professional groups and other stakeholders in order for all to work together.
Participants discussed several areas concerning behavioral health and the effects of health reform that need research. They include how to locate people who are currently not receiving services; analysis of benefits and costs of interventions; good models of providing care; assessment of the prevalence of families that are improving; how to increase use of the knowledge from behavioral economics; and how to increase minority researchers in the field. Compton, for example, said that this lack has been a major theme across NIH, and that NIDA has been particularly attentive to the issue, with a recent council review and a series of recommendations on the diversity of the scientific workforce. Attrition of minority researchers is particularly noticeable from graduate school to the postdoctoral level and from the postdoctoral level to the faculty level, he said, so NIDA is focusing its attention at these transitions, helping with such things as grant writing and career development. McCabe pointed out that professional associations also are working hard on this issue with federal agencies.
McCabe said that two key questions for everyone in the field are “how to make some things happen in a timely way,” and “where do we best put our energy and resources.”
REFERENCES
Anand, V., Biondich, P.G., Liu, G., Rosenman, M., and Downs, S.M. (2004). Child health improvement through computer automation: The CHICA System. MEDINFO, 107, 187-191.
Asarnow, J.R., Rozenman, M., Wiblin, J., and Zeltzer, L. (2015). Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta-analysis. JAMA Pediatrics, 169(10), 929-937.
Halfon, N. (2015). Optimizing the Behavioral Health of All Children: Implicationsfor Policy and Systems Change. Paper presented at Workshop on Opportunities to Promote Children’s Behavioral Health: Health Care Reform and Beyond, Washington, DC. Available: http://sites.nationalacademies.org/dbasse/bcyf/dbasse_170194 [May 2016].
Kessler, R.S., Amminger, G.P., Aguilar-Gaxiola, S. Alonso, J., Lee, S., and Ustun, T.B. (2007). Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry, 20(4), 359-364.
National Institutes of Health. (2007). Biological Sciences Curriculum Study. Information about mental illness and the brain NIH Curriculum Supplement Series [Internet]. Available: http://www.ncbi.nlm.nih.gov/books/NBK20369 [May 2016].
PLANNING COMMITTEE FOR THE WORKSHOP ON FUNDING OPPORTUNITIES FOR EVIDENCE-BASED PREVENTION AND INTERVENTIONS TO PROMOTE CHILDRENS COGNITIVE, AFFECTIVE, AND BEHAVIORAL HEALTH
MARY ANN McCABE (Chair), Society for Child and Family Policy and Practice; Society of Pediatric Psychology; School of Medicine, George Washington University; Department of Psychology, George Mason University; THOMAS F. BOAT, Cincinnati Children’s Hospital Medical Center; DAVID A. BRENT, Department of Psychiatry, University of Pittsburgh School of Medicine; WILMA P. CROSS, Feinberg School of Medicine, Northwestern University; Office of Disease Prevention, National Institutes of Health; COSTELLA GREEN, Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services Administration; J. DAVID HAWKINS, Social Development Research Group, School of Social Work, University of Washington; KIMBERLY E. HOAGWOOD, Society of Clinical Child and Adolescent Psychology; Department of Child and Adolescent Psychiatry, School of Medicine, New York University; LAUREL K. LESLIE, American Board of Pediatrics; Tufts University School of Medicine; JENNIFER NG’ANDU, Robert Wood Johnson Foundation; RUTH PEROU, Program Performance and Evaluation Office, Centers for Disease Control and Prevention; EVE E. REIDER, National Center for Complementary and Integrative Health, National Institutes of Health; GAIL F. RITCHIE, Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; PAT SHEA, Office of Technical Assistance, National Association of State Mental Health Program Directors; BELINDA E. SIMS, National Institute on Drug Abuse, National Institutes of Health; JOSÉ SZAPOCZNIK, Department of Public Health Sciences, Miami Clinical Translational Science Institute, and Center for Family Studies, University of Miami; VERA FRANCIS “FAN” TAIT, Department of Child Health and Wellness, American Academy of Pediatrics; WENDY KEENAN, Study Director.
DISCLAIMER: This Workshop in Brief has been prepared by Sara Saghir, rapporteur, as a factual summary of the presentations and discussion at the workshop. The statements made are those of the individual speakers and do not necessarily represent the views of all participants, the planning committee, the National Academies of Sciences, Engineering, and Medicine. The planning committee was responsible only for organizing the workshop, identifying the topics and choosing speakers.
REVIEWERS: To ensure that it meets institutional standards for quality and objectivity, this Workshop in Brief was reviewed by Kareemah Abdullah, National Community Anti-Drug Coalition Institute and Training Operations, Community Anti-Drug Coalitions of America, Alexandria, VA; Thomas F. Boat, Department of Pediatrics, Cincinnati Children’s Hospital Medical Center; and Jessica Jeffrey, Division of Population Behavioral Health, Semel Institute of Neuroscience and Human Behavior, University of California, Los Angeles. Patricia L. Morison, Division of Behavioral and Social Sciences and Education, served as review coordinator. The review comments and draft manuscript remain confidential to protect the integrity of the process.
SPONSORS: The Forum on Promoting Children’s Cognitive Affective and Behavioral Health is partially supported by the American Academy of Pediatrics; the American Board of Pediatrics; the American Orthopsychiatric Association; the American Psychological Association; Autism Speaks; the Centers for Disease Control and Prevention; Community Anti-Drug Coalitions of America; the Conrad N. Hilton Foundation; the Hogg Foundation for Mental Health; the National Institutes of Health; the Robert Wood Johnson Foundation; the Society for Child and Family Policy and Practice; the Society of Clinical Child and Adolescent Psychology; the Society of Pediatric Psychology; Substance Abuse and Mental Health Services Administration; U.S. Department of Health and Human Services, Assistant Secretary for Planning and Evaluation; U.S. Department of Justice.
Copyright © 2016 by the National Academy of Sciences. All rights reserved.
FORUM ON PROMOTING CHILDREN’S COGNITIVE, AFFECTIVE, AND BEHAVIORAL HEALTH
WILLIAM R. BEARDSLEE (Cochair)
Boston Children’s Hospital and Harvard Medical School
C. HENDRICKS BROWN (Cochair)
Feinberg School of Medicine, Northwestern University
KAREEMAH ABDULLAH
Community Anti-Drug Coalitions of America
DARA BLACHMAN-DEMNER
National Institute of Justice, U.S. Department of Justice
THOMAS F. BOAT
Cincinnati Children’s Hospital Medical Center
FELESIA R. BOWEN
School of Nursing, Rutgers University
DAVID A. BRENT
School of Medicine, University of Pittsburgh
LAUREN CALDWELL
American Psychological Association
WILMA P. CROSS
Office of Disease Prevention, National Institutes of Health
ALEXA EGGLESTON
Conrad N. Hilton Foundation
RICHARD G. FRANK
U.S. Department of Health and Human Services
AMY GOLDSTEIN
National Institute of Mental Health, National Institutes of Health
COSTELLA GREEN
Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services
RICK HARWOOD
National Association of State Alcohol and Drug Abuse Directors
J. DAVID HAWKINS
School of Social Work, University of Washington
KIMBERLY E. HOAGWOOD
Society of Clinical Child and Adolescent Psychology and New York University
COLLEEN HORTON
Hogg Foundation for Mental Health, University of Texas at Austin
JENNIFER W. KAMINSKI
U.S. Centers for Disease Control and Prevention
KELLY J. KELLEHER
Nationwide Children’s Hospital
UMA KOTAGAL
Cincinnati Children’s Hospital Medical Center
LAUREL K. LESLIE
American Board of Pediatrics and Tufts University School of Medicine
MARY ANN MCCABE
Society of Pediatric Psychology, Society for Child and Family Policy and Practice, George Washington University, and George Mason University
JENNIFER NG’ANDU
Robert Wood Johnson Foundation
JENNIFER OPPENHEIM
Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services
LAWRENCE A. PALINKAS
School of Social Work, University of Southern California
EVE E. REIDER
National Center for Complementary and Integrative Health, National Institutes of Health
MARY JANE ROTHERAM-BORUS
University of California, Los Angeles
PAT SHEA
National Association of State Mental Health Program Directors
ANDY SHIH
Autism Speaks
BELINDA SIMS
National Institute on Drug Abuse, National Institutes of Health
JOSÉ SZAPOCZNIK
University of Miami
VERA FRANCIS “FAN” TAIT
American Academy of Pediatrics
JENNIFER TYSON
Office of Juvenile Justice and Delinquency Prevention, U.S. Department of Justice
DONALD WERTLIEB
American Orthopsychiatric Association and Tufts University
For additional information about the Forum, visit http://nas.edu/ccab.








