4
Cross-Sector Collaboration to Provide Transportation Services in Rural/Small Urban/Suburban Settings
When transporting people and goods, there are often first-mile, last-mile issues to be addressed (i.e., how does the person get from home to transit, and then from transit to the final destination). In rural settings these become “first 50 mile, last 50 mile issues,” said moderator Rich Garrity, a senior associate at RLS and Associates. Speakers in this session continued the dialogue on cross-sector collaboration, but with a focus on suburban, small urban, and rural areas. Judy Kell, the hub operations manager for Pathways to Better Health of the Lakeshore, in Michigan, discussed efforts to link residents to the social determinants of health as well as the need for coordination across health, social services, and transportation. David Faldmo, the medical director and quality director at the Siouxland Community Health Center in Sioux City, Iowa, described the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) assessment tool that providers can use to screen for and address the social determinants of health, including transportation. Suzanne Alewine, the executive director of the Missouri Rural Health Association and co-founder of Community Asset Builders, described HealthTran, Missouri’s Rides to Wellness initiative. Dennis Johnson, the executive vice president for policy and advocacy and government affairs at the Children’s Health Fund, described using mobile health clinics to bring care to children in underserved communities.
The presentations were followed by comments from discussants Charles Carr, the director of the Office of Intermodal Planning for the Mississippi Department of Transportation; Amy Conrick, an assistant director for the Community Transportation Association of America (CTAA); Robin Phillips, the executive director of the National Rural Technical Systems
Program; and Marianne Stock, division the chief of Rural and Targeted Programs at the Federal Transit Administration (FTA) of the U.S. Department of Transportation. (Highlights are presented in Box 4-1.)
PATHWAYS TO BETTER HEALTH OF THE LAKESHORE
Muskegon County, Michigan, has a population of 172,000 and includes three very urban areas that are entitlement communities as well as suburban areas and rural areas that are large farming areas, Kell said. The county has 28 governmental units and 14 school districts. Twenty percent of the children in the county live in poverty, and only 58 percent of the adult popu-
lation has attended some college. The county ranks 81st of 83 Michigan counties in health risk behaviors and is below state and national standards for low-birth-weight babies.
People live in environments that do not support them, Kell said, and the Pathways to Better Health of the Lakeshore program links the people of Muskegon to the social determinants of care: housing, transportation, food, utility assistance, and anything else that might improve their health status. Community health needs assessments1 indicated that care coordination was desperately needed, not just among doctors, nurses, and specialty clinics, but across health and social service silos, including transportation, which Kell said was the main barrier for the population. Pathways to Better Health of the Lakeshore is administered by the Health Project, which is the community benefit ministry of the Mercy Health System. The program relies on community health workers who are indigenous to the community in which they work. The community health workers assist people in navigating the health care system, including linking them to transportation and assisting them en route as needed. The community hub coordinates all of the health care and social determinants of care for people in the program and provides clinical oversight to those community health workers who are deployed to assist. The budget for the hub includes funding for transportation, Kell noted. Any provider (e.g., hospital, emergency department [ED], clinic, physician office, etc.) can refer a patient into the hub. Patients are then referred out to the community health workers. The Pathways program uses an electronic record with checklists that assess eligibility and identify access to care, financial issues, and health improvement barriers. Pathways programs include, for example, medical home, medical referral, health coverage, social service, transportation, pregnancy, and smoking cessation. The program works through the barriers, provides documentation that the patient received the services needed, and creates accountability for the patient, agency, and health system. Community partnerships also play a role. Kell said that Muskegon was designated by the U.S. Environmental Protection Agency as a sustainable community and was provided with a transportation consultant who engaged all 28 governmental units and others in the community to develop a transportation plan. The plan included mobility coordinators and cross-sector collaboration among Muskegon County public transportation; private cabs; 10 care coordinating agencies that work with Mercy Health’s community health workers (including
___________________
1 Kell reminded participants that nonprofit hospitals must conduct a community needs assessment as part of their filings with the Internal Revenue Service in order to maintain their nonprofit tax status. Hospitals are then required to develop an implementation strategy with goals, objectives, and measurable outcomes for their efforts to improve health status in the communities.
federally qualified health centers, the Area Agency on Aging, the health departments, and a variety of social service agencies); churches, libraries, and public housing (which provide space for the community health workers to hold workshops on chronic disease management); and informal relationships with rural county transportation services. In addition, three buses were funded by the U.S. Department of Transportation (DOT) to extend routes out to three rural areas.
Initial evaluation results show that spending was lower than the comparison group prior to and after the Pathways program, and the data suggested that patients were receiving better care. Kell shared several examples of the impact of connecting patients to transportation. Patients in the Healthy Pregnancy Program, for example, reduced their number of ambulance rides to the ED by 25 percent. They now take cabs or the bus to a care provider. Patients in all Pathways programs are provided transportation to their Alcoholics Anonymous and Narcotics Anonymous meetings, along with treatment. There was also a $2.4 million cost reduction for the hospital system as a result of decreased use of the ED and increased use of nonemergency transportation and primary care visits. Participation in the workshops also decreased social isolation for patients.
Kell identified several barriers to implementing the Pathways program including, as was mentioned by other speakers, crossing county or state lines to access services. In addition, the definition of disability is confusing to some partners when determining eligibility for programs. In general, there is a lack of data to justify the investment in transportation for health care. There were also contract issues and stakeholder confusion or inertia.
In moving forward with cross-sector collaboration to provide transportation, Kell suggested the following steps:
- Find a champion and develop partnerships.
- Inform the community.
- Engage the patients as advocates for system change.
- Participate in local community needs assessments.
- Develop strategies and implement them via pilot projects.
- Develop data and return-on-investment studies.
- Seek change on the state and federal levels related to boundaries, funding, and definitions of disability.
- Institutionalize partnerships and funding.
In the case of the Pathways program, for example, the champion is the community. The program has been institutionalized through the use of community benefit dollars through the health system, and community members are encouraged to participate in their local community needs assessments.
PROTOCOL TO RESPOND TO AND ASSESS PATIENT ASSETS, RISKS, AND EXPERIENCES
Faldmo described the PRAPARE assessment tool as an example of a program that is addressing transportation needs. According to the National Association of Community Health Centers’ website, PRAPARE’s funding came from The Kresge Foundation, the Blue Shield of California Foundation, and the Kaiser Permanente National Community Benefit Fund at the Easy Bay Community Foundation.2 The protocol’s main objective is to create a tool that community health centers and other health care providers can use to screen for and address the social determinants of health, including transportation. PRAPARE also is intended to inform the development of community partnerships, to develop new programs to help overcome the social barriers to good health, and to decrease health care spending.
The Siouxland Community Health Center is part of a team of five states where community health centers are using the same electronic health record (EHR) system, Faldmo explained. Part of the project is to screen for social determinants of health and record them in the EHR. PRAPARE was designed specifically to aid health centers in gathering data that inform and address individual patient care and population health management, while capturing what makes health center populations unique. However, there are also local-, state-, and national-level goals, including informing advocacy efforts related to local policies concerning the social determinants of health (see Figure 4-1).
In using PRAPARE, patients are asked about transportation as well as whether lack of transportation has kept them from a medical appointment or from getting their medications. Faldmo shared data showing that 17 percent of patients being served by the six centers in Team 4 had transportation needs. That is nearly one out of every five patients who had a transportation need that kept them from getting the health care they needed, Faldmo emphasized.
Siouxland Community Health Center
Sioux City, Iowa, has a population of about 85,000 people, but becomes very rural, very quickly just outside of the city, Faldmo explained. Many of the Siouxland Community Health Center patients come from the outlying rural areas, and, as the city is in a tristate area, many of the patients come from South Dakota and Nebraska as well. The center has medical care (including urgent care, HIV care, and some behavioral health care), dental care, and a pharmacy all in house. There are about 95,000 patient visits per
___________________
2 See http://nachc.org/research-and-data/prapare (accessed September 22, 2016).
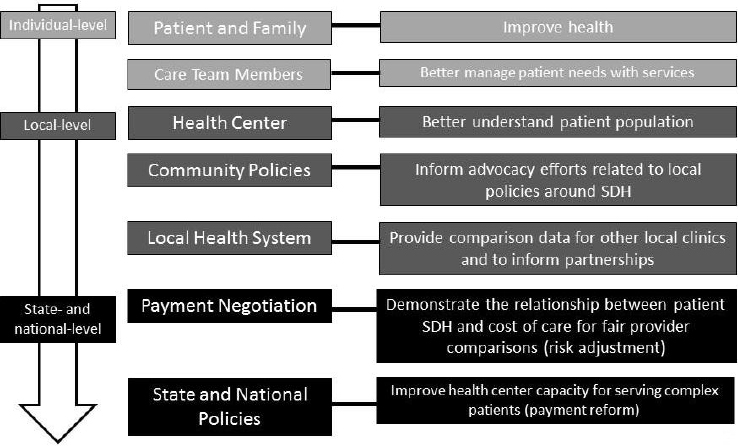
NOTE: SDH = social determinants of health.
SOURCE: Faldmo presentation, June 6, 2016.
year by about 25,000 unique patients. For the last decade, the center has provided taxi vouchers when a transportation need is identified. (This practice existed long before the social determinants of health project, Faldmo noted.) The vouchers are funded through a foundation associated with the center, and there is an annual fundraising dinner, with some of the funds collected being allotted for taxi vouchers. The center is also in discussions with the regional transit authority to form a more formal partnership and hopefully provide more than just taxi vouchers for patients. Faldmo noted that the Siouxland Regional Transit System crosses state lines and reaches out into the rural areas. Three managed Medicaid companies are also active in providing transportation vouchers to patients in need.
The no-show rate for the center is about 20 percent, Faldmo said. At this time, the reason for missing an appointment is not tracked, and it is up to the provider to decide if the patient needs to be contacted and rescheduled. He suggested that the center should be regularly assessing why patients are missing appointments and, if the reason involves transportation needs, what can be done to overcome that barrier. Faldmo also mentioned the need for appropriate metrics to assess the impact of addressing transportation for the patients.
Moving forward, the Siouxland Community Health Center will continue to systematically assess for social determinants of health, including
transportation, and document this in the EHR. The center is tracking interventions and the resources needed to address social the determinants of health and to navigate patients to community resources. The center is also working to strengthen relationships with community partners to overcome these determinants, including transportation, which has been identified as a need in the community. The center will identify how many missed appointments are due to lack of transportation and assess, during pre-visit preparation, which patients may have transportation needs for that visit as well as for laboratory testing or any overdue services. Faldmo said that the center wants to be more proactive in assessing the transportation needs before patients even come in, rather than waiting for them to not show up. Finally, the center will be working with the Siouxland Regional Transit System to identify additional ways to help patients.
The PRAPARE project to assess social determinants of health is just scratching the surface, Faldmo concluded, and transportation is a big part of the project, and community partnership is critical. Addressing the social determinants of health, Faldmo added, is also an essential part of moving from volume-based care to value-based care.
HEALTHTRAN
To help address the transportation component of health care access in rural areas, the Missouri Foundation for Health provided the Missouri Rural Health Association with a $500,000 grant over a 3-year period to examine ways to span the gap. This led to the launch of the HealthTran pilot program, which began as a cross-sector collaboration between the Missouri Rural Health Association and the Missouri Public Transit Association and now includes the state primary care association and local health care and transportation organizations. HeathTran serves 10 counties in rural southcentral Missouri that span nearly 8,000 square miles. The total population of the 10 counties is about 290,000 people, Alewine said, or less than 37 people per square mile. There is no major metropolitan area in that part of the state, she continued, and most people receive care at a rural tertiary hospital in the Ozarks community of West Plains, a small city of less than 15,000 people. There is a significant amount of poverty in the area and a lack of good economic opportunities and jobs. The public transit infrastructure in Missouri is woefully inadequate statewide, Alewine said, and most of the state funding goes to the two large metropolitan areas of the state. State funding for the rural areas is limited, she said, and thus FTA funding is important for rural areas.
The HealthTran pilot was designed to gather high-quality data to support the theory that transportation does, in fact, improve patient health; to use that data to advocate for increased transportation funding at the state
and federal levels to improve health care access and patient outcomes; and to create a sustainable and replicable program. The program is patient-centric, putting the needs of the patient/rider first. HealthTran coordinators serve as the interface between patients and the public transit providers in the region, scheduling transportation for the patients. Alewine said that at this time HealthTran uses public transit providers exclusively and advocates for increased public transit services (i.e., models involving private or volunteer transportation have not been used at this point).
Getting rides for patients is making a big difference, Alewine said, not only in the quality of life, but also in health care and health outcomes. She echoed the concerns of previous speakers, emphasizing the costs of missed appointments. An initial study at the start of HealthTran found that 20 percent of missed appointments were attributed to a lack of transportation. She pointed out that for a provider who schedules 20 patients per day at an average charge of $150 dollars each, the missed appointments will result in a loss of $3,000 per week, or an entire day’s worth of potential billable revenue. A round-trip ride ranges from $20 to $50, depending on the need of the patient (e.g., mobile patient, stretcher transport). If the average round trip ride is $30, the total cost of getting 20 patients to their appointments is $600 dollars. This is a 1:5 gross return on investment relative to the charge for the visit (compared to the ride cost). Assuming the provider nets 70 percent of the charges, the expected reimbursement would be $105. This type of data helps to make the case for transportation with health care partners, Alewine said.
In addition to the revenue for providers when patients get to their care appointments, which Alewine noted is a cost to the payers, there is also a significant benefit in terms of avoided ED visits and inpatient admissions. HealthTran is now engaging payers to gain access to patient-specific claims data in order to further understand and enhance the business case for including transportation as a component of benefits packages. Alewine said that it is a challenge to show the financial benefits to the health care system of getting patients to care and to present a mechanism for providers to invest in transportation for their patients without raising Anti-Kickback Statute and Stark Law (self-referral) concerns for Medicare and Medicaid patients. She added that the Missouri Rural Health Association is waiting on an advisory opinion on this issue from the Office of the Inspector General. Federally qualified health centers have a safe harbor under the Anti-Kickback Statute, she explained, which allows them to partner in transportation arrangements.
Of the HealthTran riders thus far in the pilot (380 people taking 3,735 scheduled trips), 55 percent are covered by Medicare, 34 percent are covered by Medicaid (Alewine clarified that HealthTran does not provide nonemergency medical transport), 18 percent are uninsured, 13 percent
have private insurance, 5 percent have veteran benefits, and 3 percent are veterans but without benefits. Most interesting, she said, are the numbers of trips by riders. Thirty-three percent of riders have taken one scheduled trip, 13 percent have ridden twice, 20 percent have ridden 3 to 9 times, and 25 percent have taken 10 or more rides to get to their care (e.g., patients with multiple, chronic issues).
The HealthTran model is designed around the patient, Alewine reiterated, and is designed to be sustainable. The cycle begins when the patient seeks care and says he or she has a transportation barrier. Alewine said that the clinic front office staff are being trained to ask whether patients have a ride to their next appointment. Patients in need of transportation are referred to HealthTran, then a coordinator facilitates the transportation through one of a variety of channels, and the patient is transported. The entire model is based on the ability to create a data-supported case demonstrating the value of transportation to the health care system. The next step, which HealthTran is still working on, is for the health care provider to realize a return on investment and share a percentage of that return with HealthTran so the cycle can continue. HealthTran is collecting data on the costs of patient rides and the billable cost for their care. The transportation and health care systems are valuable to each other, especially in rural areas, she concluded. Using data to demonstrate the financial value is the only way to achieve policy change. Alewine referred participants to the Missouri Rural Health Association website for additional data and reports on HealthTran.
CHILDREN’S HEALTH FUND
The Children’s Health Fund is dedicated to meeting the health care needs of children at risk. Founded in 1987, the Children’s Health Fund supports a network of pediatric care programs in 14 states and the District of Columbia, each in affiliation with a major teaching hospital or community health center. Johnson explained that more than 50 mobile clinics serving more than 300 sites totaling more than 275,000 visits per year, for a total of more than 3.6 million health encounters with children and families since inception. The Children’s Health Fund uses what it learns in its clinical programs to inform its policy and advocacy work to effect change, specifically, to get children into medical homes and help overcome barriers to health for medically underserved children and families.
Transportation as a Health Access Barrier
The lack of transportation is a critical health access barrier for children, Johnson said, although this fact was not obvious at first, even in a mobile
care model. The role of transportation first came to light in the homeless program in New York City. Children living in the shelters were seen in the mobile clinic and referred for specialty care in the Bronx. Although New York City has an extensive public transportation system, the adherence rate for children completing specialty care appointments was very low (around 10 percent), and it was determined that transportation was a significant barrier. Once transportation assistance was provided, adherence rose to nearly 70 percent.
Following the passage of the Children’s Health Insurance Program (CHIP) in the late 1990s, the Children’s Health Fund mounted a National Child Health Caravan, which delivered two Children’s Health Fund mobile medical units to the Mississippi Delta region and staged a series of town hall meetings along the route from New York to the Gulf Coast. At every one of those town hall meetings, Johnson said, a significant number of community residents said they were aware of CHIP and had enrolled their children but faced transportation barriers to getting to care. This prompted the Children’s Health Fund to develop a health transportation shortage index tool3 and to conduct a series of national and regional surveys to determine where there was transportation disadvantage across states and communities and who would require extra support to get to health appointments. Through the development of programs, partnerships, and advocacy efforts, the Children’s Health Fund is committed to working within its network to improve transportation access and to help ensure that medical appointments are being kept.
Johnson highlighted several of the implications of transportation as a health access barrier, particularly for medically underserved children, including missed opportunities for immunizations and routine well-child care; an increased incidence of untreated chronic illnesses (e.g., asthma); an increased use of EDs (and ambulances) for nonemergency care; and an increase in preventable hospitalizations.
Johnson described the results a study of EDs in the Mississippi Delta that found, again, that transportation is a barrier to keeping health care appointments (Grant et al., 2010). Even in communities where working families had a car, that car was often unavailable, generally because it was being used to transport a parent to work, and any routine child health care had to be postponed until that car was available. All (100 percent) of the interviewees in the study reported having missed a child’s health care appointment during the preceding 12 months because of transportation, and all of those respondents were after-hours ED users. The study concluded that non-urgent pediatric ED use could be reduced by extending
___________________
clinic hours, adding a walk-in service, and making transportation more available.
The bottom line, Johnson said, is that transportation is a key element of the “enhanced medical home” model of care and that transportation accessibility, promotion, and use will contribute to improved health outcomes for children and families. There is a tremendous potential value in a collaboration between the health and transportation sectors, he said. There is the potential for improved return on investment in terms of health costs, health outcomes, and the ability of infrastructure to provide the intended services. There are also opportunities to leverage technological innovation and for local economic development in underserved communities.
Transportation for Community Health Initiative
Transportation for Community Health is a strategic initiative to identify and reduce the impact of transportation barriers, to mobilize and engage key community leaders and stakeholders, and to focus on collaborative planning that incorporates community-based perspectives. The initiative is informed by integrated health and transportation sector data. It is focused on two very rural, very medically underserved counties in the interior of Mississippi, and it is partnering with the Mississippi Department of Transportation, the Community Transportation Association of America, the Sunflower-Humphreys Counties Progress, Inc., and others.
The proposed framework includes a needs analysis using the health transportation shortage index tool to geomap the state and identify areas of transportation disadvantage, Johnson said. Current data suggest that 65 percent of Mississippi counties (53 of 82) are at high risk for transportation shortages. A governance and oversight framework will be established, and the appropriate management coordination model to address the needs will be determined. The initiative will also identify potential resources, and strategize regarding ongoing sustainability. Finally, Johnson said, it will be important to determine the metrics for evaluation.
Johnson outlined some of the key elements of the Transportation for Community Health initiative. The initiative is a collaboration of national, state, and local partners; it cultivates local leadership; it builds on a shared understanding of how health access is shaped by a set of social determinants; it prioritizes establishing community trust as a key to progress in planning and decision-making processes; it recognizes that there are likely resource limitations; it encourages innovative approaches to mitigate; and it includes an early periodic screening, diagnosis, and treatment plan for evaluating success (based on a set of core screening benefits embedded within Medicaid for children).
Some of the lessons learned thus far from the Transportation for Community Health initiative, as outlined by Johnson, include
- The importance of establishing trust by aligning with anchor organizations that have a track record of success in convening community stakeholders.
- The irreplaceable value of momentum that is stakeholder generated and progress that is driven through local leadership.
- The critical need for strategic planning that recognizes that success will likely be incremental and nonlinear.
- Success in forging relationships and “moving the needle” in economically disadvantaged, underserved communities is hard won. There is often a degree of residual disaffection related to previous attempts to engage by non-local institutions.
- Investment in appropriate relationship building and outreach is necessary to encourage and support community stakeholders to engage, discuss, and take action on basic infrastructure issues that can improve access, opportunities, and outcomes for their community.
In closing, Johnson offered some questions for further discussion among participants. Do health sector (especially community-based) providers participate in the transportation planning process in your state and county? Should they be invited? How can this be incentivized? How can transportation be incorporated as a quality measure in the contractual process with managed care providers? How can we best make the case for the value of transportation services within the transforming health system? Innovation and new technologies are changing the face of health care delivery and transportation. Can this be a driver for collaboration?
DISCUSSION
Panelists, discussants, and participants discussed a variety of issues following the presentations. Topics included developing a relationship with the state DOT; cost sharing; making the case for the role of transportation in patient outcomes; and funding, regulatory, and other challenges.
Developing a Relationship with the State DOT
Carr prompted panelists to describe their relationship with the state DOT and how that relationship has helped to improve and sustain the examples discussed. Alewine said that HealthTran originally partnered with the two large rural public transit organizations in Missouri: OATS,
and Southeast Missouri Transportation Service. Through that partnership, the Missouri Department of Transportation (MoDOT) was brought to the table. As HealthTran has evolved, so has the relationship, she said, and the organizations are still learning the best ways to work together to support each other. She said that HealthTran just submitted an application for Rides to Wellness funding in partnership with MoDOT.
Faldmo said that the Siouxland Community Health Center is just starting its relationship with the Siouxland Regional Transit System and is working to partner with it and to formalize the relationship. Kell said that Pathways has done much of its work thus far within the counties, but is now at the point where cross-county assistance is needed, and it will be reaching out to develop a more formal relationship with the (state and local) DOT.
Carr emphasized the importance of cooperation, relationships, and establishing trust when working with a DOT to provide better outcomes for patients. He encouraged participants to work with their state DOT and said that, in most states, nonurban funding and specialized transportation funding goes through the DOT.
Cost Sharing
Carr recalled the discussion of bus passes and vouchers by panelists and asked about other cost-sharing efforts between the transportation and health care communities that have been successful. Kell responded that for Pathways to Better Health of the Lakeshore, the health system is funding the bus passes and vouchers along with covering the patients and has negotiated a fair contract with the transit authority at reduced cost. Costs are being shared among all three parties—the patient, the health care system, and the transit system.
For HealthTran, Alewine said, although there is no formal arrangement, rural public transit has stepped up with reduced-price options for patients who do not have rides. The health care partners are now in the process of developing a membership type model, and HealthTran will be able to pay for some transportation through a grant.
Faldmo reiterated that PRAPARE is in the preliminary stages, and health center leaders are looking to see if they can discount transportation costs for patients further through a formal contract with the DOT.
Conrick referred participants to the CTAA webpage where they can
learn more about the work of CTAA with regard to health care transportation, and to learn about the solutions health care grantees have submitted.4
The Role of Transportation and Patient Outcomes
Conrick raised the issue of encouraging the health care system to recognize the importance of transportation in patient outcomes. She observed that the International Classification of Diseases, ICD-10, now has several billable codes for transportation.
Kell pointed out that while Medicare is consistent nationwide, each state includes billable codes as part of its state Medicaid plan amendments, and every state is a little bit different. She noted that there are examples that indicate that the health care system is recognizing that transportation is significant. For instance, in addition to transportation being part of the Medicaid benefit in Michigan, community health workers teach beneficiaries how to use the benefit because many do not understand it. She highlighted the need to determine which efforts are most effective in helping patients use their transportation benefit and then start replicating best practices to achieve more systemic utilization on a national level.
Faldmo also reiterated the need for data and expressed optimism at the work of the National Association of Community Health Centers with PRAPARE to quantify the need for transportation to health care.
Johnson suggested that the uptake on the health side has been far less robust than it could be and that the transportation sector seems more aware of the need. As the health system is transformed, it is the demonstration of savings to the system that will help make the case for transportation.
Alewine highlighted the need to bring the payers into the discussions and suggested that value-based incentives could help to increase the attention to transportation for patients by health care providers.
Challenges
Participants discussed overcoming the funding, regulatory, and other challenges of bringing health care and transportation together. Stock provided a brief background on the FTA Section 5311 program (49 U.S.C. 5311), the Formula Grants for Rural Areas program through which the FTA funds public transit in rural areas. The funding is limited; Stock said that the total is about $600 million nationwide per year. She expressed hope
___________________
4 For information about CTAA programs on medical transportation, see http://web1.ctaa.org/webmodules/webarticles/anmviewer.asp?a=16&z=40 (accessed September 22, 2016). For information about grantee submissions of innovative transportation solutions, see http://nationalcenterformobilitymanagement.org/challenge (accessed August 4, 2016).
that the program would grow in the future, as the current level of funding does not come close to meeting the full need for public transit in rural areas.
Alewine said that one challenge has been waiting for delayed funds. For example, she said that Section 5310 dollars were expected to be awarded in January, but that due to issues on the FTA side of the process, the Missouri Rural Health Association was still waiting on contracts. The biggest barrier currently, she said, is the procurement process, which she described as “incredibly daunting” for smaller organizations to navigate. The association is working with the state DOT to address this barrier and to find a better and a faster way to do procurement that meets rules and requirements and does not have the hurdles.
Phillips briefly described the work of the National Rural Transit Assistance Program (RTAP). The program is a hub for knowledge management, gathering information from transit operators, and providing training that is specific to the transit operator’s needs. Every 2 years the National RTAP conducts a survey of rural transit operators and FTA program managers at the state level. She said that one of the issues for rural transit providers is funding, and she observed that health care organizations often do not understand the way that financing is done for rural transit (e.g., there is often a lack of state matching funds). Rural transit also often involves transporting one person at a time to a distant medical appointment, which is more costly than transporting several people at once. She stressed the need for communication and sharing quality information as well as the importance of partnerships and relationships between the provider of health care services and the provider of transportation services. It is also important to consider the environment being served and to use common sense. For example, people who are transit-dependent should be having dialysis on Monday, Wednesday, and Friday, when transit is running, instead of Tuesday, Thursday, Saturday, as many rural transit systems do not run on Saturday. Technology can help with communication and providing transit services when and where they are needed.
Sneha Peck of America’s Essential Hospitals asked about the role of the hospital or health system in initiating the transportation conversation and ensuring long-term sustainability for programs. Kell suggested that the process starts with the hospital’s community needs assessment and the community health improvement plan prepared with the health department. A challenge, however, is getting sufficient community participation in the community needs assessment plans and processes.
This page intentionally left blank.
















