3
Global Preparedness and Response Efforts
Chapter 3 presents several case examples of preparedness and response efforts at the global, regional, and national levels for the Ebola outbreak in West Africa.
FIRST RESPONSE: MÉDECINS SANS FRONTIÈRES’ EXPERIENCE AND PERSPECTIVE
Armand Sprecher of Médecins Sans Frontières (MSF) described his organization’s response to Ebola in West Africa, which was informed by their continuous involvement with filovirus diseases since the 1995 Kikwit outbreak. While noting that his remarks would be confined to MSF’s experience, he emphasized that many people, organizations, and countries responded to the recent epidemic, and he began his presentation to the workshop by acknowledging their contributions.
On March 18, 2014—before the outbreak had been declared—a team from MSF experienced in hemorrhagic fevers arrived in Guéckédou, Guinea, in response to an alert from that country’s ministry of health, Sprecher recounted. Within the next 2 weeks, they were joined by more than 60 additional MSF staff—a number that grew to more than 1,000 during the first year of the Ebola epidemic. Over the course of the epidemic, MSF has trained staff from several organizations and more than 4,000 West African nationals, he said. MSF opened 19 Ebola treatment units (ETUs) in 6 countries with a capacity of more than 700 beds, into which more than 8,000 patients had been admitted at the time of the workshop; they included more than 5,100 people with confirmed Ebola, of whom approximately 2,400 have survived the disease.
In addition to caring for patients, MSF distributed 70,000 home protection kits to areas of Monrovia, Liberia, that were hardest hit by Ebola, along with 650,000 antimalarial treatments there and 2.8 million in Freetown, according to Sprecher. The organization was also involved in clinical trials for several postexposure therapeutics.
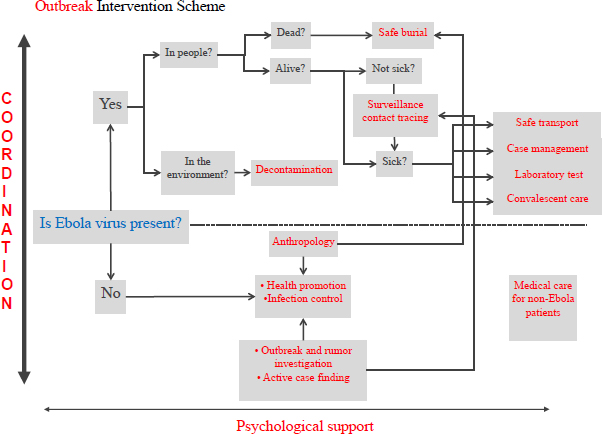
Sprecher identified and discussed several distinct challenges within the complex undertaking of an Ebola outbreak response. To present the problem of transmission control, he referred to the flow chart shown in Figure 3-1, which depicts MSF’s outbreak intervention scheme.
The first priority in Ebola outbreak intervention is to contain the virus, and MSF takes a multipronged approach to this objective. “In the community we carry out health promotion campaigns to try to change community infection behaviors and interrupt disease transmission, and in health care facilities we reinforce infection control to try and prevent transmission within the health structures,” Sprecher said. When cases are identified in the community, team members decontaminate households and the immediate environment and assist with safe burials.
SOURCE: Sprecher presentation, March 25, 2015.
To find Ebola cases in the community, MSF relies primarily on contact tracing, Sprecher reported. “When you get a list of contacts from a known case, you go and visit them and try and make it clear to them that it is in their best interest to be visited every day by the contact tracing team, so that as soon as they fall ill, if that is going to happen, they can be brought to care to protect their family and to allow them to receive the best care that we can offer at the time,” he explained. Unfortunately, Sprecher added,
What we have to offer isn’t great. It is better than not coming in, but it is not so evidently in their self-interest that they are terribly enthusiastic. In a setting where Ebola is stigmatized, people are not really thrilled to have the strange people come and knock on their door every day because it upsets the neighbors.
“I think this will change dramatically the day we have a therapeutic of some sort, because then people will have a significant self-interest in being identified . . . as soon as they become sick,” Sprecher said. Possible cases are transported to ETUs for care and for diagnostic testing performed by laboratory partners (such as the National Institutes of Health [NIH] or the U.S. Centers for Disease Control and Prevention [CDC]), as described later by Heinz Feldmann of the National Institute of Allergy and Infectious Diseases’ (NIAID’s) Rocky Mountain Laboratories in Hamilton, Montana. MSF also provides convalescent care for survivors and psychosocial support to patients, their families, and their communities.
Some communities enforced their own quarantines on people who were visited by contact tracers, Sprecher said. While he found this response draconian, and noted that it predisposed people to escape confinement and, potentially, spread disease, he also noted that it appeared to have effectively extinguished many chains of Ebola transmission.
MSF sent “an army of epidemiologists” into the field to find cases, investigate rumors of outbreaks, identify novel transmission behaviors, and assist with surveillance programs, Sprecher reported. Meanwhile, field anthropologists worked to improve community acceptance of interventions, such as burial practices, and to promote effective health communications. Among the particular challenges anthropologists faced was the need to enlist community support for cremation as the epidemic raged in Liberia and safe traditional burial became impossible. “We have gotten burials wrong so often, and have incurred the wrath of the community by burying people the wrong way, that I was horrified when I heard that this was necessary,” Sprecher recalled. “As it turns out the population realized also that it was necessary, and they lived with this for a while.”
Another technique MSF employed to enlist community support was to film activity within ETUs. “Then we take these films out into the community and we project them to show them what is actually going on so they can see that health care is in fact being delivered, because the rumors are impressive,” Sprecher said. “We have been accused of coming there to spread the disease, not to stop it, of drawing blood and sending it off to pharmaceutical companies to enrich Western
economies, and of stealing organs and selling them on the black market. So we have to be very transparent in what we do.”
Coordination and Other Challenges
The many and diverse aspects of Ebola outbreak response must be coordinated and integrated, Sprecher emphasized. For example, he noted, clinicians cannot make informed decisions about whom to admit and whom to turn away without understanding the epidemiology of the outbreak. The “interdependent, complex machine” required for effective outbreak response requires a lot of people, whether the outbreak is large or small, he noted. “I would much rather have an outbreak of 100 patients in one location than an outbreak of 40 patients in two locations, because you have to do all of these things twice,” he remarked.
As they attempted to keep up with the fast- and wide-spreading West African epidemic, MSF opened three ETUs in Guinea within the first 2 weeks of their response, in Guéckédou, Macenta, and Conakry; these were quickly followed by one in Monrovia, Liberia. “We had to expand and to move about and set up new operations on a regular basis over the course of this outbreak,” Sprecher stated. This has been a significant challenge for the organization, which he estimated had only 40 people on staff with experience of past Ebola outbreaks—and who were soon stretched thin.
Distrust for MSF’s operations ran high in Guinean communities, and at times manifested as physical violence, Sprecher reported. “People have been killed on outbreak control operations,” he said, referring to the September 2014 murder of eight members of an Ebola team by members of a Guinean village near the city of Nzérékoré, where the team was distributing information about the disease. More generally, he argued, Ebola became epidemic in West Africa not because outbreaks were not controlled in March, but because interventions were not accepted by communities. “If we had had a month’s earlier notice we would have been given the opportunity to fail to control the outbreak in February,” he observed. “Surveillance is important, but it is by itself insufficient . . . getting the communities onboard is a critical part of any Ebola intervention.”
Personal protective equipment (PPE) simultaneously secured and hindered those delivering Ebola care, Sprecher noted. PPE standards set by MSF may be excessive, he said, “but until we actually have better evidence we won’t be able to scale back.” Meanwhile, health workers can only wear PPE for 40 to 60 minutes without risking heat stress, he observed; thus, a worker in an ETU is only able to work under biosafe conditions for 2 to 3 hours per shift, drastically limiting contact time with the patients.
This problem has caused MSF to rethink and prioritize care delivery to make it more efficient—a daunting challenge given the scale of the West African
epidemic, Sprecher pointed out. In August and September 2014, for example, when the epidemic was at its peak, MSF was forced to suspend certain interventions, including intravenous rehydration, which did not lead to excessive fatality, he noted. However, this should not be interpreted as a lack of effect of intravenous rehydration, but the recognition that under similar conditions, the benefit might be modest.
Over nearly two decades of responding to Ebola outbreaks, no MSF staff member had ever become infected—until the West African epidemic, in which 28 staff members became ill and 14 died, Sprecher said. Other organizations bore a similarly heavy and unprecedented burden, he observed—and it must certainly have ripple effects on their entire staff. The epidemic was particularly hard on the West African resident staff, who worked without respite and were often rejected by their own communities and sometimes even by their families, he said. “Our mental health treatment capacity in the field is not only for our patients, it is also for our staff,” he stated. “We have to keep these people healthy and functional because we are not out of this yet.”
Management of the Response
In closing, Sprecher focused on the coordination and management of outbreak response—a role that physicians are rarely trained to play, he argued. “We give the management of our outbreak interventions to medical people on the assumption that the knowledge of the medical factors in play is important,” he observed, rather than for any skill they might have in coordinating large groups of people interacting through multiple activities. “Those various services that we have to deploy in the field to control the outbreak are complex human resources machines,” he said. “You have to take all of those resources and put them together into a well-functioning machine.”
“We need coordinators, and we need managers,” he urged. Sprecher continued:
There are wonderful WHO initiatives to develop new drugs, there are programs and organizations to improve our clinical care, there are people working on PPE—people have talked about governance changes. All of this is good. But [we must] realize this kind of intervention requires a skill set that maybe the medical people who’ve been empowered with this don’t have.
By acknowledging this gap, and providing the training or selective hiring to fill it, we might someday be able to look back on the West African epidemic as the “bad old days,” after which things got better, he concluded.
OTHER IN-COUNTRY RESPONSE EFFORTS
The Fondation Mérieux USA’s Efforts in Sierra Leone
Joseph Fair reflected on the Ebola epidemic in Sierra Leone, a country where he has worked for the past decade. He described factors that kindled the spread of disease, challenges in gaining and maintaining control of transmission chains, and lessons learned that should be applied immediately to end the epidemic, and in the future, to prevent another.
The Outbreak in Context
Building on Bausch’s description of the region in which the epidemic originated, where the borders of Guinea, Sierra Leone, and Liberia meet, Fair observed that these divisions were imposed by colonization on long-standing tribal territories that have far greater influence over routes of travel and trade. He also noted that the tri-state region is hyperendemic for Lassa fever, which has been the subject of ongoing disease surveillance in Sierra Leone funded by a consortium of U.S. government agencies.
Despite increasing awareness of Lassa fever in Sierra Leone, testing for other potentially confounding diseases, such as malaria, shigella, and typhoid fever, languished in the wake of recent civil war, Fair said. Indeed, many infectious pathogens are likely circulating undetected throughout the tri-state region, which has recently been ravaged by war and environmental upheaval, including the Ebola virus, based on enzyme-linked immunosorbent assay (ELISA) results from nearly a decade ago in suspected Lassa fever cases in Sierra Leone that turned out to be negative for that virus (Schoepp et al., 2014).
If Ebola was present in West Africa in 2006, why did it not spread as it did in 2014? Fair described several key developments in the region since then that encouraged Ebola transmission by enabling faster travel between rural areas and cities, along with major land use change associated with widespread slash-and-burn cultivation of cassava. By 2014, the tri-state region had become a local nexus of commerce and transport, he said.
In addition, over the past decade, civil conflict in Sierra Leone and Liberia produced mistrust of government authority, including public health messages about disease control—which, when they were issued to combat Ebola, were also unclear, according to Fair. Warnings about the lack of a treatment were widely interpreted as “There is absolutely nothing you can do for me,” thus, rather than report to a treatment center, many sick people hid. “They just came out of 10 years of civil war,” he explained. “Running and hiding was pretty much the only way to stay alive for a lot of their recent lives, and this is all part of their very recent memory. So in my own opinion I did think that influenced how the population behaved during this outbreak.”
Even worse, in Sierra Leone, the areas in which outbreaks occurred fell entirely in one territory of a deep national divide, Fair noted; the political party in power was opposed by the dominant party in the outbreak areas. Since the onset of the outbreak in Sierra Leone, there has been “a complete political breakdown and a very fragile political state, which greatly affected public health,” he observed—and it continues to do so. Meanwhile, rumors circulated in the outbreak area that the government was intentionally crippling its inhabitants to prevent them from voting in the next election.
While Sierra Leone’s public health infrastructure in 2014 was “nascent,” by Fair’s description, with only two physicians per 100,000 people, it was growing; it was also sensitized to Lassa fever, particularly in its three laboratories with virology capacity. These laboratories were quickly overwhelmed with samples to test when the Ebola epidemic ignited, he recalled. Similarly, the world—even the United States and other wealthy countries—proved inept at controlling Ebola, largely because there were no plans for addressing the disease on a regional or global scale, he concluded.
Now is the time to formulate policy and logistical contingencies for future Ebola outbreaks, Fair urged. “We need to make these plans while it is still really fresh in our minds what happened, what went wrong, and how can we fix this the next time—and actually do exercises to see if it works on a small scale,” he argued.
Fair observed that it took a multisectoral collaboration to gain control of Ebola in West Africa. Relationships that arose out of necessity between governments, academia, philanthropic and nongovernmental organizations (NGOs), and industry, should now be formalized and expanded, he advised. Combining these forces will not only improve global health security in the context of future pandemics, he predicted, but doing so will also specifically benefit each participating sector.
Getting to Zero
While the West African Ebola epidemic appeared to be on the wane at the time of the workshop, Fair (among others) reminded participants that much work remained before all transmission chains were extinguished. “In Liberia already there is complete complacency about Ebola,” he observed. “There are very few people, unless they survived it themselves or their family died, that are particularly worried about it right now,” he said. The outbreak has not been extinguished in Sierra Leone or Guinea, he warned; unless precautions are taken, it could reignite in Liberia just as easily as it began.
To prevent this from happening, Fair urged the reestablishment of baseline diagnostics for febrile diseases in Ebola-vulnerable countries, as well as testing for malaria, human immunodeficiency virus (HIV), and other major infectious diseases. He also encouraged ongoing, extensive community engagement. “When
these outbreaks are over we typically leave,” he said, but that would not be wise, given the magnitude of this public health disaster and its certain ongoing impact on the population. It will also be important to maintain active surveillance for Ebola—as well as other diseases with similar presentations, such as Lassa and yellow fever—after the epidemic is declared to be over, but it is uncertain who would fund such an effort, he noted.
Typically, one country’s engagement with another to protect global health security is viewed as a contract, Fair observed, but this goal would be better served in the context of friendship. For example, he noted, programs focused on pathogens from the standpoint of biodefense should also address significant public health threats in the countries where they are being conducted. While impoverished countries understandably benefit from the influx of money that such engagement brings, they also value the commitment of expertise and resources for disease prevention and treatment, he said.
To this end, Guinea and Sierra Leone will be included in a laboratory network established by the Fondation Mérieux USA in partnership with the French Development Agency, Fair announced. Called RESAOLAB (the French acronym of its title, the West African Bio-Laboratory Analysis Network), it links laboratories within several countries with the goal of establishing standardized diagnostics, improving staff training and management systems, and obtaining funding for and strengthening governance of laboratory systems.
RESAOLAB is part of the GABRIEL (Global Approach to Biological Research, Infectious Disease, and Epidemics in Low-Income Countries) Network, which encourages the sort of international health collaboration that will be necessary to address epidemic and pandemic diseases, Fair explained. By maintaining lines of communication and data sharing in real time, network participants should be better prepared to cooperate effectively in a global health emergency, he suggested.
The International Medical Corps’ Efforts in Liberia
Colin Bucks of Stanford University related his experiences as a clinician serving as a volunteer medical coordinator with the International Medical Corps between September and October 2014, in Bong County, Liberia. By way of introduction to this setting, he presented a video by The New York Times reporter Ben Solomon depicting daily life at the Suakoko ETU.1
“I am, for lack of a better term, boots on the ground,” Buck stated. What he took away from his experiences with approximately 130 suspected and confirmed
___________________
1 The video can be viewed at http://www.nytimes.com/2014/10/23/world/africa/ebola-liberiavideo-inside-the-ward.html (accessed November 16, 2016).
cases of Ebola, and what he shared with workshop participants, were lessons he hopes to use in preparing his home health care institution to treat Ebola patients.
Patient Care in Liberia
Patients arriving at the ETU were triaged according to a simple algorithm that determined “who stays, who gets admitted, and who goes home,” Bucks said. The treatment protocol they used—and which was typical of other ETUs across West Africa—was based on one for sepsis, a similar syndrome (Bray and Mahanty, 2003) and consisted largely of supportive measures focused on fluid replacement,2 along with anti-infectives for malaria, which frequently accompanied Ebola. The collected data from all such ETUs might someday suggest which interventions, at which stage of infection, were most effective, he noted; in the meantime, there are protocols to follow, which clinical staff tried their best to adapt. Most importantly, he emphasized, “everything hinges on infection control.”
The ETU staff applied a range of tools and approaches beyond PPE to meet this goal, Bucks explained. The unit was designed and constructed to simplify infection control in all activities, including moving patients, staff, and materials, providing water, and disposing of waste. Vigilance, checklists, and mutual responsibility reduced human error. “We stayed healthy,” he reported, but he warned that deadly mistakes are bound to occur, given enough time.
Bringing It Home
Bucks then turned to the challenge of translating successful elements of West African Ebola care to hospitals such as his home facility in the United States. Unlike the ETUs, U.S. hospitals provide treatment for a broad spectrum of health problems, into which Ebola care would need to be integrated, he noted. “There are tons of rules about how we will be trying to do this,” he observed, expressing his thankfulness for such guidelines. While recognizing the potential of Western health care to provide a higher level of care to Ebola patients than has been previously attained, he reminded the audience that the priorities of Ebola care are universal.
___________________
2 Sprecher had previously noted that, while Ebola has been characterized as a disease of hypovolemic shock, due to significant fluid loss, its effects could not simply be reversed by simple fluid repletion. Even so, he added, “I have faith . . . that a certain amount of our supportive care is deflecting the outcomes for a subset of the patients, but that’s just my clinical impression, that’s not based on evidence.” With the outbreak winding down in Liberia, it might now be possible for clinical staff to compare the effectiveness of various treatment modalities in the interest of improving the response to the next outbreak, he observed.
The prospect of treating Ebola patients caused staff and administration at Buck’s hospital to review their pandemic plan for the first time since 2009, and to operationalize it to address Ebola, he reported. To navigate the complex regulatory milieu that governs pandemic preparedness—which encompasses disaster planning, infection control, federal and state law, and union contracts—he found useful guidance in the CDC’s Detailed Hospital Checklist for Ebola Preparedness.3 Indeed, he noted, its opening message could be applied to hospital preparations for any emerging infection:
Every hospital should ensure that it can detect a patient with Ebola, and respond in a coordinated fashion. Many of the signs and symptoms of Ebola are nonspecific and similar to those of many common infectious diseases, as well as other infectious diseases with high mortality rates. Transmission can be prevented with appropriate infection control measures. . . . [E]nsure [that] your hospital is able to detect possible Ebola cases, protect your employees, and respond appropriately.
Acceptance of the CDC guidelines for Ebola treatment was strongly encouraged by Medicaid and Medicare, which provide significant funding for hospitals, Bucks pointed out. Similar guidelines were imposed on emergency physicians under the Emergency Medical Treatment and Labor Act (EMTALA). He said he welcomed this guidance, given the “lean, just-in-time, profit-driven environment” that is the U.S. health care system. This carrot-and-stick approach encourages hospitals to provide for the public good in a crisis without regard for profit, he concluded.
Specific preparations for Ebola care in hospitals—just as in an ETU—include protocols for patient isolation and planned movement of patients, staff, and materials. In addition, hospitals must be able to address Ebola in the context of labor and delivery, pediatrics, and other special populations. Staff must volunteer to work with Ebola patients, Bucks noted. “We need a PPE plan that meets all the guidelines and recommendations,” he continued, and a simulation facility where staff can be trained in these techniques. There must be protocols for safe waste disposal, as well as for both public and internal communications.
“Just like an ETU, you want as few people doing as much of the work [as possible], working like a team,” Bucks advised. They should be intensively trained in PPE and actively observing each other to ensure safety, and they should strive to minimize their exposure (in terms of both numbers and time) to patients in order to reduce the number of potential contacts, he said. In addition, the team should use dedicated equipment and follow guidance for its safe disinfection or disposal. “Whether it is housekeeping, nutrition, changing the beds, administering
___________________
3 As of June 2015, this document is no longer available. An updated version, Interim Guidance for U.S. Hospital Preparedness for Patients with Possible or Confirmed Ebola Virus Disease: A Framework for a Tiered Approach, is available at http://www.cdc.gov/vhf/ebola/hcp/us-hospitalpreparedness.html (accessed November 3, 2016).
medications, or doing clinical assessments, you are all working together,” he emphasized. “Working as a team is absolutely essential, as is having a defined set of protocols.”
While complex, the Ebola-appropriate PPE developed by Bucks and his Stanford colleagues is far cooler than the outfit he wore in Liberia, he said, but still uncomfortable—largely due to the necessity for full face coverage during doffing. The expense of PPE is a substantial component of the costs of Ebola preparation, which he estimated at $500,000 for his hospital. This will not be a hardship for a large institution, he noted, but on a nationwide scale, it represents a considerable expenditure, and one that is unlikely to be efficient.
Clinical care guidelines for Ebola treatment in the United States would do well to follow those set out by Canada (Canadian Critical Care Society et al., 2014), according to Bucks. They incorporate interventions unavailable in African ETUs, such as continual infusion, transfusions, mechanical ventilation, hemodialysis, and experimental antivirals—any of which (individually or in combination) could make a difference to patient outcomes, he said. He also noted the contrast between standard emergency medical protocol, driven by the adage that “time is tissue” for conditions such as heart attacks and gunshot wounds, and emergency care for Ebola and other emerging infections, in which infection control is the first priority, and the clinician’s first step is the time-consuming donning of PPE. Knowing this, and recognizing that there is no cure for Ebola, emergency physicians must reset their expectations of what they can accomplish for patients, he said, recognizing that those expectations could change if a cure became available.
Applying Lessons Learned
Evoking the memory of severe acute respiratory syndrome (SARS), Bucks remarked that the 2003 epidemic offered lessons that could have been applied to better address Ebola, and that should be applied to all emerging diseases. In particular, he—echoing other workshop participants—argued for the establishment of infection control standards for people and institutions that treat emerging infectious diseases. To illustrate this point, he compared the SARS experience in Toronto, where the first imported cases to enter a hospital were not immediately isolated and a major outbreak ensued, and, simultaneously, in Vancouver, where such a case was quickly isolated and infection control stepped up, extinguishing transmission.
Similarly, PPE developed to address Ebola should be adopted as a general standard for emerging infections, Bucks argued. “Let’s test it and make it good and fit it into our infection control procedures,” he said. Moreover, he added, “If every hospital in the country is required to have this, we should create the economies of scale so this is affordable in developing nations.”
In closing, Bucks offered an analogy between controlling Ebola outbreaks and wildfires, from the perspective of his experiences in both activities. In the
early, exciting days of fighting a wildfire, “Some of us are just hanging on by the seat of our pants,” he observed. “Firefighters are praying for rain at this time, but they are also gathering good stories and lots of lessons.” Then, as a fire comes under control, a process called mop-up begins:
Mop-up is tough; it takes a long time. At times, you take off your gloves and you crawl in the ashes and use your hands to find hot spots that still need to be dug out and then you put them out. If you don’t put them out, that fire can come raging back in a week. It is certainly not glamorous at all, and the newspapers don’t cover this. There are no video crews there. People lose attention. But if you don’t do this work diligently, then you lose everything that you started with. You cannot get to the big work of recovery and rebuilding unless you do the mop-up safely.
As the West African Ebola epidemic approached the mop-up stage, Bucks expressed hope that lessons learned then, as well as in the heat of raging outbreaks, could be applied to improve the preparedness of U.S. hospitals to face the next emerging disease.
THE U.S. PUBLIC HEALTH RESPONSE
Inger Damon of the CDC described her agency’s multifaceted response to the Ebola epidemic in West Africa, which involved activities within that region, as well as domestic training for outbreak responders, planning for the care of patients returned to the United States, and preparations for outbreak control in the event of an Ebola introduction.
The CDC’s Role in West Africa
At the time of the workshop, the CDC had deployed nearly 1,000 staff members to Guinea, Liberia, and Sierra Leone to pursue essential activities to reduce Ebola transmission, according to Damon. These included surveillance, contact tracing, data management, laboratory testing, incident management, emergency operation center development, safe isolation, and health education. Staff members were also deployed to nonaffected border countries to conduct assessments of Ebola preparedness. Many of the CDC’s activities in West Africa were conducted in concert with the Disaster Assistance Response Team (DART) from the U.S. Agency for International Development’s (USAID’s) Office of Foreign Disaster Assistance, which has overseen the U.S. response to the epidemic in West Africa.
In early fall 2014, as the epidemic reached a peak, the CDC developed novel strategies to relieve the shortage of treatment beds, including the development of community care centers, Damon noted. The agency has also conducted more than 230 facility assessments and assisted staffing laboratories within the three
affected countries, including a laboratory in Sierra Leone that has processed more than 12,000 samples using high-throughput technologies.
To prepare U.S. and African health care workers, support personnel, and volunteers to serve in Ebola treatment centers, the CDC held training sessions in both the United States and Africa. The introductory training course the agency created for U.S.-licensed clinicians intending to work in ETUs in Africa—which was based on materials developed by MSF—is available online as an “Ebola Training Toolkit” for NGOs and other organizations that offer training to health care workers preparing to work in African ETUs.4 Damon reported that more than 600 U.S.-based and international staff planning to deploy to West Africa had taken this course. The CDC has also instructed nearly 700 master trainers to conduct infection control training programs at West African health facilities, and they have assisted with the creation of technical materials used to train more than 23,000 frontline health care workers in Africa.
Fulfilling its more traditional role in international outbreak response, the CDC, together with the World Health Organization (WHO) and other partners, bolstered contact tracing and follow-up activities in all affected countries, including the short-lived outbreak in Nigeria, described by Tomori. There, rapid response efforts, the use of an emergency operation center originally established to address polio, and effective community outreach and communications produced a “shining example” of an effective outbreak response, Damon observed.
A global collaboration has provided laboratory support for the epidemic region, including real-time polymerase chain reaction (PCR) testing of suspected cases. As part of this effort, the CDC staffed and operated a field laboratory in Bo, Sierra Leone, where staff members developed methods to increase sample throughput, as well as transportation networks to move samples quickly from the field, Damon said. The Bo facility serves as a model field laboratory for producing reliable results and maintaining high-quality standards, she noted.
In addition to developing and disseminating infection control training programs, the CDC worked in concert with USAID, the International Federation of Red Cross, and other NGOs to provide technical assistance to burial teams in Guinea, Liberia, and Sierra Leone, Damon reported. “We also worked in the development of call centers to help identify case patients as well as deaths in the community that needed to be safely buried,” she stated. Meanwhile, communications specialists, working with anthropologists and other experts in Liberia and Sierra Leone, helped create safe burial protocols that were culturally accepted in Ebola-stricken communities. This work is not finished, however, because, as she noted, “One of the concerns as we are now approaching getting to zero, [is] that we are still seeing unsafe burials in these communities.” She pointed out the United Nations International Children’s Emergency Fund led many such
___________________
4 See http://www.cdc.gov/vhf/ebola/hcp/safety-training-course/training-toolkit.html (accessed November 3, 2016).
communications efforts, with the CDC playing a supporting role, along with ministries of health and local experts, on the practices of various tribes and communities.
Educational outreach has been a fundamental component of outbreak control in West Africa, Damon observed. This has been accomplished by engaging local groups and individuals such as community leaders, imams, and women’s committees to help spread key public health messages about Ebola. “We have been able to work with other partners to change standard operating procedures to allow for more transparency and more cultural sensitivity, to prepare scripts for teams in the field, and to adjust radio messaging and other mass media outreach,” she stated.
The CDC’s most recent efforts in West Africa have employed a strategy known as RITE (rapid isolation and treatment of Ebola), which proved effective in reducing Ebola transmission in Liberia, Damon noted. RITE is performed by teams of epidemiologists, clinicians, sanitation workers, data managers, and communications experts, who travel to areas experiencing clusters of cases, she explained. After this protocol was adopted in Liberia, the size and duration of local outbreaks decreased dramatically; thus, it is now being pursued in Guinea and Sierra Leone.
At the time of the meeting—before Liberia had been declared Ebola free—the news from that country was sufficiently promising that the CDC was beginning to focus on longer-term public health needs, Damon stated. In Sierra Leone and Guinea, where transmission chains continued to arise and resistance against health care workers threatened progress toward “zero,” the CDC continues its efforts, anticipating that an Ebola vaccine will improve its ability to control the disease.
The CDC’s Domestic Response
Anticipating the possibility of Ebola importation into the United States, and in response to the infection of two nurses who cared for an Ebola patient in a Dallas hospital, the CDC acted to educate U.S. health care workers about isolating Ebola patients and preventing infection, tightened previous infection control guidance for health care workers caring for such patients, and updated PPE guidance, Damon stated. Fifty-five hospitals, located within 200 miles of more than 80 percent of travelers arriving from West Africa, have been designated as Ebola treatment centers/assessment hospitals, she added. However, any hospital in the United States that receives an Ebola patient will be assisted by a CDC Ebola Response Team comprising 10 to 12 epidemiologists and clinicians who have experience with Ebola, along with sanitation workers and surveillance officers, she said.
The CDC has also provided more than $145 million to support state emergency preparedness programs through public health emergency preparedness
cooperative agreements, Damon stated. In addition, the agency and its partners have provided training in infection control to health care systems and public health systems, reaching more than 800,000 health care workers online and 6,500 in person.
Finally, Damon described the CDC’s enhanced entry screening and graduated follow-up procedures for travelers determined to be from low to high risk for the disease, established at the five U.S. airports where travelers from the three Ebola-affected West African countries enter the United States. All such travelers receive “check and report” Ebola kits with information on the disease, tools to help check their temperature and symptoms for 21 days, and information on who to call if they develop symptoms, she said. The CDC designates a person who has both consistent signs or symptoms of and risk factors for Ebola as a person under investigation, who is actively tracked in cooperation with state and local health departments.
Treating Ebola Patients in the United States
Building on the discussion by Bucks and Damon of the potential challenges facing those U.S. hospitals that would treat Ebola patients, Bruce Ribner of Emory University described the actual provision of such care, and the practical issues that arose in the course of his experience. The Emory Serious Communicable Diseases Unit team, which Ribner directs, has treated more patients with Ebola, and at high risk for Ebola infection, than any other facility in the resource-rich world, he stated. Thus, it was his institution that was selected to receive the first cases from the West African epidemic to enter the United States, in early August 2014.
The weeks following that event brought “a tsunami of media attention, first locally, then nationally and then internationally,” to Emory, Ribner recalled. More importantly, he continued, this experience revealed significant challenges in three areas, which he explored in his presentation: general preparedness for infectious disease outbreaks in the United States, the screening and follow-up of potential asymptomatic imported cases, and inpatient care for Ebola and other emerging infectious diseases.
Preparedness for Infectious Disease Care
Because of its proximity to both the CDC and the world’s busiest airport, Emory University Hospital began planning to accommodate patients with serious communicable diseases in 2001, giving it a considerable head start on other such institutions, Ribner noted. “We realized that if any of these individuals, either travelers or CDC employees, acquired a serious communicable disease, there was really no place in our city to treat them”—a conclusion shared by the CDC, he recalled.
The two institutions began a dialog that led to the creation of biocontainment units: treatment areas for the safe delivery of effective medical care for patients with a known or anticipated communicable disease (Fairley et al., 2016; Smith et al., 2006). Additional biocontainment units were subsequently established at the University of Nebraska in Omaha, and at the NIH in Bethesda.
“We had SARS in 2003; we had the H1N1 outbreak in 2009; we have MERS [Middle East respiratory syndrome], which started in 2012; we have the H7N9 influenza virus; and, of course, the virus which has brought us all here today, the Ebola virus,” Ribner recounted. “As each one of these outbreaks presented, we adjusted our policies and procedures to make sure they were, in fact, the best we could find available to treat patients with these infectious diseases.” Among the adjustments the Emory team made was to select a dedicated staff of 19 nurses and 5 physicians for the three-bed biocontainment unit, and to schedule them continuously, in order to limit response time to less than 1 hour, he said. They also chose to work with a single ambulance company, training a select group of emergency medical technicians (EMTs) who were always on call, and modifying an ambulance so it could be decontaminated. This model of specialized expertise has since been adopted (after some debate) by the CDC for Ebola care, he noted.
Emory’s biocontainment unit also features high-level PPE—which at first was criticized for evoking panic in the general public, but was eventually accepted as a standard for safe Ebola care, Ribner observed. Health care workers in the unit receive repeated training and testing in the performance of all Ebola-related practices and procedures, and specifically in the donning and doffing of proper PPE, he reported (Wu et al., 2015).
“Running a program like this is very expensive,” Ribner observed, noting that his budget had declined steadily since the biocontainment unit’s inception. Were it not for the West African Ebola epidemic, he said, the program would likely have been disbanded in 2015. Instead, federal funding has been granted to support one regional ETU for each U.S. Department of Health and Human Services region, and ancillary facilities will be designated to care for patients in the event of an overflow. All such treatment units will be equipped and staffed such that there is no disruption in overall hospital operations if a patient with a serious communicable pathogen such as Ebola is admitted, he added. “Regional centers will get $2.25 million for the first year, mainly for renovation, which I think is fine for most of us,” he said, but he also noted that funding for subsequent years has been cut to a level below which many such units will be able to sustain operations.
Screening and Follow-Up
Ribner then turned to the management of potential Ebola patients: travelers and medical personnel returning from West Africa, including possible asymptomatic cases. This issue is of particular importance at Emory, owing to its proximity
to both a major international airport and a medical nerve center. Because rules regarding the screening of travelers for disease are largely determined at the state level in the United States, there have been wide disparities in how asymptomatic travelers from Ebola-affected countries have been managed, Ribner stated. While one northern state confined a returning health care worker in a tent in the middle of winter, others have allowed travelers to simply go home, no matter how distant from a treatment center, he observed. However, as time has passed, states have become increasingly consistent in their approach to asymptomatic travelers from high-risk regions.
Recognizing that patients presenting with fevers of unknown origin that are under investigation for Ebola are also at risk for malaria, typhoid, or influenza—diseases that can kill quickly—hospital laboratories must be equipped to diagnose these conditions quickly, and not wait until Ebola has been ruled out, Ribner insisted. Emory’s unit “can tell whether a patient is viremic within an hour or two of identifying them as a person under investigation,” he noted—which, while it does not rule out Ebola, vastly simplifies safe testing for other confounding, life-threatening infections. Unfortunately, such rapid testing is not available in most U.S. hospitals, he added.
Emory’s outpatient management program is also expensive. Even in their relatively efficient, time-tested system, ruling out Ebola in a person under investigation costs as much as $2,500, Ribner estimated—yet, he remarked, third-party payers are unwilling to pay for more than a clinic visit in these cases. “I have been very fortunate in that our administration has underwritten this project for untold dollars,” he said, noting that few community hospitals are likely to possess such resources.
Inpatient Care
Ribner noted that Ebola care protocols in U.S. hospitals are much like those in Germany (see next section, “Preparedness for an Ebola-Like Disease”). While typical intensive care units at Emory have one nurse for two patients, within the ETU, there are three nurses per patient in order to avoid mistakes due to time pressure, he explained.
Many hospitals have elected not to become ETUs for two main reasons, according to Ribner: it could drive away patients who fear Ebola, and the significant expense of providing (and even offering to provide) Ebola care. “Third-party payers are not interested that we need extensive nursing care, that we need dedicated doctors,” he complained—and certainly they do not compensate for the considerable costs of ancillary services such as medical waste disposal. Again, while Emory’s administration has underwritten these expenses, other hospitals are unlikely to receive that level of support, he predicted.
Future Constraints
Ribner’s response to his rhetorical question as to whether support for infectious disease emergency preparedness will outlast the Ebola outbreak was pessimistic, as befits his experience. “I can only guess how long funding is going to persist if we have no major outbreaks over the next year or two, or if we are fortunate enough to control this Ebola outbreak over the next 6 to 12 months,” he remarked.
Likewise, Ribner observed that, although significant resources have been allocated for infectious disease preparedness, none have been earmarked for the very expensive treatment of people with dangerous infections. Our fee-for-service health care system is not designed to support outpatient evaluations of people with possible serious communicable disease, or to reimburse hospitals for the high cost of caring for such patients, he concluded.
PREPAREDNESS FOR AN EBOLA-LIKE DISEASE
Pan American Health Organization
The International Health Regulations (IHR) framed the Pan American Health Organization’s (PAHO’s) response to the West African Ebola epidemic, according to Sylvain Aldighieri, who coordinates the IHR, Alert and Response and Epidemic Diseases Unit, jointly with the WHO. In 2014, 13 of the 22 countries represented by PAHO had, by self-report, achieved compliance with IHR core public health capacities; thus, a significant component of regional preparedness involved identifying and filling gaps in public health functions necessary to prevent local transmission of Ebola, if it were introduced to the region.
This effort has been guided by temporary recommendations issued by the IHR emergency committee in early August 2014, which Aldighieri summarized as follows:
- There should be no general ban on international travel or trade; restrictions outlined in these recommendations regarding the travel of Ebola cases and contacts should be implemented.
- States should provide travelers to Ebola-affected and at-risk areas with relevant information on risks, measures to minimize those risks, and advice for managing a potential exposure.
- States should be prepared to detect, investigate, and manage Ebola cases; this should include assured access to a qualified diagnostic laboratory for Ebola and, where appropriate, the capacity to manage travelers originating from known Ebola-infected areas who arrive at international airports or major land crossing points with unexplained febrile illness.
- The general public should be provided with accurate and relevant information on the Ebola outbreak and measures to reduce the risk of exposure.
- States should be prepared to facilitate the evacuation and repatriation of nationals (e.g., health workers) who have been exposed to Ebola.
Translating this guidance into action, PAHO developed technical guidelines to address the potential introduction of Ebola into the region;5 conducted meetings and initiated collaborations across a range of sectors and disciplines, as well as with other organizations and partners within the region, such as the CDC and the Public Health Agency of Canada; established a regional PPE stockpile; and conducted trainings on risk communication, clinical management, and laboratory biosafety. After a period of consultation with member states to review capacities and identify gaps and needs, PAHO conducted technical missions to member states to individually prepare them to respond to Ebola, according to their specific needs and circumstances. These missions were conducted by teams of staff members, each of whom had years of experience dealing with Ebola in previous positions, according to Aldighieri. While these missions detected significant gaps in preparedness, he acknowledged, he also noted that they generated considerable momentum for change. At the time of the workshop, PAHO was engaged in follow-up activities to encourage implementation of recommendations from the mission teams, and to assess future disease control needs—recognizing that “no one size fits all” when it comes to such planning, Aldighieri reported. “Ownership, leadership, [and] knowledge of the local context by national authorities are essential for an effective response,” he stated, which can be undertaken even in resource-limited settings. One way of making this possible is through subregional organization of common needs (e.g., PPE, training, and harmonization of public health measures), he noted.
Germany
Reinhard Burger of the Robert Koch Institute (RKI) in Berlin offered another perspective on Ebola preparations in Western countries. (Dr. Burger’s contribution to this Proceedings of a Workshop can be found in Appendix C.) RKI spearheaded this effort in Germany and issued intervention guidelines for Ebola (RKI, 2014) similar to those published by the CDC (CDC, 2015) and the Public Health Agency of Canada (Canadian Critical Care Society et al., 2014). Germany’s preparations for Ebola closely followed the design that Bucks advocated in his workshop presentation: a flexible strategy focused on infection control that can be adapted to any emerging infectious disease.
At the time of the workshop, Germany’s association with the West African Ebola epidemic was primarily one of assistance in the affected countries, according to Burger; however, like other Western countries, Germany’s public health officials anticipated the possibility of imported cases, and had also accepted
___________________
5 Technical guidelines are available at www.paho.org/ebola (accessed November 3, 2016).
four patients evacuated from Africa for treatment. In developing its plans for managing and controlling Ebola in Germany, RKI assumed that the country was unlikely to receive cases unknowingly, and even less likely to experience disease transmission within its borders. Ebola was therefore addressed much like any other infectious disease of unknown origin: through a general protocol designed and coordinated by RKI and implemented at seven specialized “competence and treatment” centers, he explained. These centers are distributed across Germany in major cities, such that all are within a 3-hour drive of any location in the country.
Six of the seven centers are equipped not only to treat and isolate patients with dangerous infectious diseases but also to manage a spectrum of support services for disease control, including hospital hygiene and decontamination, transportation, and public information, Burger reported. The treatment centers, known by their German acronym, STAKOB,6 are prepared for any highly contagious agent, he said; currently they can accommodate 50 patients, and they are staffed by dedicated personnel who train regularly. Between infectious disease emergencies—that is, most of the time—these facilities are used to control more common infectious threats, such as multidrug-resistant tuberculosis. As a network, the centers compare therapeutic options and experiences, coordinate experimental therapies, set procedural standards, and support each other with personnel and equipment.
The competence centers provide an interface for public health officials, infectious disease clinicians, medical microbiologists and virologists, occupational medicine specialists, local government, and public services, such as ambulance, fire, and police. “They all attempt to achieve comparable standards so there are no quantitative differences in their performance,” Burger stated.
Upon discovery of a justified suspect Ebola case, the patient would be tested for the disease at the point of care, then transferred as quickly and safely as possible to one of the competence centers to receive appropriate care and further testing, Burger explained. “Blood samples would be taken only in exceptional cases, so this would be done in the specialized centers only,” he added. Local health authorities would pursue contact tracing and monitoring for confirmed cases, he said.
German health care workers returning from outbreak areas were determined not to be present risks for infection; so long as they had not reported a risky contact or showed symptoms of Ebola, they were not isolated, Burger stated. Usually such workers returned to their jobs gradually and were not initially assigned tasks that involved direct contact with patients, he added; any appearance of symptoms would result in isolation. Four patients arrived in Germany following medical evacuation in a special plane, the Robert Koch, equipped for patient isolation and general intensive care.
___________________
6 Acronym of Ständiger Arbeitskreis Kompetenz-und Behandlungszentren, Permanent Working Group Competence and Treatment Centers.
A major consideration for health crisis management in Germany is the coordination of state and national governments and their associated agencies, Burger observed. “It is definitely a challenge to coordinate properly for rapid reaction and to develop synergy,” he remarked, noting that this challenge spans a host of contingencies, from the handling of patients to public messaging. RKI generally communicates with professionals involved in infectious disease control to provide advice, analysis, and technical support, but in the case of a crisis, the institute also provides public information, he noted. “These efforts depend very much on political support,” he noted—and particularly that of Chancellor Angela Merkel, whom he characterized as both interested in and well informed about Ebola.
This page intentionally left blank.






















