1
Introduction1
Cardiac arrest often strikes seemingly healthy individuals without warning and without regard to age, gender, race, or health status. Representing the third leading cause of death in the United States, cardiac arrest is defined as “a severe malfunction or cessation of the electrical and mechanical activity of the heart . . . [which] results in almost instantaneous loss of consciousness and collapse” (IOM, 2015, p. 1). Although the exact number of cardiac arrests is unknown, conservative estimates suggest that approximately 600,000 individuals experience a cardiac arrest in the United States each year (Daya et al., 2015; IOM, 2015; Merchant et al., 2011).2 Of these, approximately 12,500 are children (Atkins et al., 2009; Morrison et al., 2013). Cardiac arrest survival rates are persistently low; for example, fewer than 6 percent of people who experience out-of-hospital cardiac arrests (OHCAs) survive (Daya et al., 2015; IOM, 2015).
Cardiac arrest survival rates vary widely among communities and
___________________
1 The planning committee’s role was limited to planning the workshop, and the workshop proceedings was prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and have not been endorsed or verified by the National Academies of Sciences, Engineering, and Medicine; they should not be construed as reflecting any group consensus.
2 This number includes approximately 395,000 people who have cardiac arrests outside the hospital (i.e., out-of-hospital cardiac arrests [OHCAs]) and 200,000 cardiac arrests occurring in hospitals (i.e., in-hospital cardiac arrests [IHCAs]).
hospitals and may be influenced by “individual demographics (e.g., race, age, gender, health status), location of arrest, initial cardiac arrest rhythm, rates of bystander cardiopulmonary resuscitation (CPR) and automated external defibrillator (AED) use, and characteristics of emergency medical services (EMS) and health care systems (e.g., response time, treatment availability, training, and care quality)” (IOM, 2015, p. 2). Moreover, negative outcomes from cardiac arrest disproportionately affect populations that are already at risk for poor health status (IOM, 2015). Yet some benchmark communities have demonstrated greater than 60 percent survival rates for specific types of witnessed OHCAs and have significantly increased rates of good neurologic and functional outcomes (see, e.g., Chatalas and Plorde, 2014), providing examples of what can be accomplished through organized and sustained actions of individuals and within systems of care.
On June 30, 2015, the Institute of Medicine (IOM)3 released its consensus report Strategies to Improve Cardiac Arrest Survival: A Time to Act, which evaluated the factors affecting resuscitation research and outcomes in the United States. Focusing on the public health dimensions of cardiac arrest treatment, the report included eight recommendations (see Appendix A) that emphasized the following:
- Establishing a national cardiac arrest registry
- Fostering a culture of action through public awareness and training
- Enhancing the capabilities and performance of EMS systems
- Setting national accreditation standards related to cardiac arrest for hospitals and health care systems
- Adopting continuous quality improvement programs
- Accelerating research on pathophysiology, new therapies, and translation of science for cardiac arrest
- Accelerating research on the evaluation and adoption of cardiac arrest therapies
- Creating a national cardiac arrest collaborative
Following the release of the consensus report, eight sponsors asked the Health and Medicine Division (HMD) to hold a 2-day workshop to assemble diverse stakeholders who would explore the barriers and opportunities for advancing the IOM recommendations (see Box 1-1). The
___________________
3 As of March 15, 2016, the Health and Medicine Division continues the consensus studies and convening activities previously undertaken by the IOM. Publications released prior to this change should be cited to the IOM in perpetuity, but all subsequent publications are branded under the National Academies of Sciences, Engineering, and Medicine.
workshop was held on July 11 and 12, 2016, with more than 120 in-person participants and 80 participants via webcast. The workshop agenda (see Appendix B) included five plenary sessions with panel presentations that focused on the IOM’s individual recommendations. Following each panel, members of the planning committee and the audience were able to make comments and pose questions to the speakers. Each plenary session was followed by one or more breakout groups, in which participants were asked to respond to a predetermined set of questions. Planning committee members moderated these breakout groups and presented summaries of the group discussions during the plenary session.
Generally, the format of this summary follows the structure of the workshop. However, some of the content has been rearranged to better highlight themes that emerged throughout the workshop and to enhance the flow of the material presented. The workshop rapporteurs have prepared this summary as a factual summation of the workshop discussions. The views included in this summary are solely the views of the workshop speakers and participants and do not represent the views of the National Academies of Sciences, Engineering, and Medicine; the planning committee; or other speakers and workshop participants, as a whole. Text that appears under individual presentations is wholly attributable to the presenter, unless stated otherwise.
This chapter provides background information on the origin of the dissemination workshop, offers perspectives from cardiac arrest survivors, and summarizes the overarching themes that emerged from workshop presentations and discussions. Chapter 2 discusses opportunities to advance cardiac arrest surveillance. Chapter 3 considers barriers and opportunities to advance research and the translation of research into care settings. Chapter 4 addresses issues related to public awareness and training. Chapters 5 and 6 focus on possible strategies to improve the quality of EMS and hospital system response to cardiac arrest, respectively. Finally, Chapter 7 examines the discussion regarding partnerships and the development of a cardiac arrest collaborative.
IMPROVING THE CHAIN OF SURVIVAL
Tom Aufderheide, Planning Committee Chair
Tom Aufderheide, planning committee chair, opened the meeting by thanking sponsors, participants, HMD staff, and the planning committee and providing a brief overview of highlights from the IOM report. He emphasized that the number of productive life years lost due to death and disability attributable to cardiac arrest signifies an enormous public health burden. Although there are effective and evidence-based actions and treatments that can significantly reduce death and disability from cardiac arrest, there are disparities in the access to, and application of, these treatments (IOM, 2015). As characterized by the chain of survival (see Figure 1-1), critical steps include early access to care through emergency 911 services, bystander-administered CPR, early defibrillation, high-performance EMS resuscitation practices, and optimized hospital-based care following a cardiac arrest. If these treatment options were more efficiently and comprehensively implemented, rates of death and disability could be reduced across the United States, said Aufderheide.
Although the chain of survival is useful for guiding actions at the
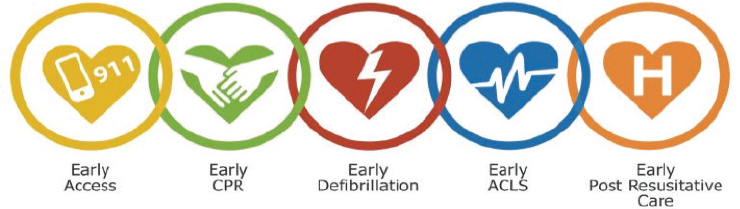
NOTE: ACLS = advanced cardiac life support; CPR = cardiopulmonary resuscitation.
SOURCE: Presented by Tom Aufderheide, July 11, 2016, A Dissemination Workshop on the Report Strategies to Improve Cardiac Arrest Survival: A Time to Act (citing Resuscitation Academy, n.d., p. 14).
operational level, the IOM report suggested that a more unifying, overarching framework for the resuscitation field was needed, explained Aufderheide. Taken as a whole, the new framework (see Figure 1-2) was meant to identify relationships and coordinate action. It includes the primary goal—improving survival and patient outcomes—as the roof of the structure, said Aufderheide. The foundation and steps represent a comprehensive, integral, and system-wide response that is required to rejuvenate the resuscitation field and improve public health (IOM, 2015). These steps provide a strong foundation for the five stakeholder groups, which are directly and indirectly responsible for the effective response to cardiac arrest and, ultimately, patient outcomes. Leadership, combined with accountability and transparency, are cornerstones for the entire framework.
Aufderheide emphasized the need to transform a culture of inaction into a culture of collaborative action. He remarked that this need for culture change spans the field and is applicable to all stakeholder groups—the public, EMS agencies, hospitals, health care providers, researchers, policy makers, and the full range of organizations and government agencies that are linked to resuscitation and cardiac arrest. Arthur Kellermann, one of the presenters, supported Aufderheide’s assertion, stating that the limited progress in cardiac arrest outcomes and of the resuscitation field, more broadly, are not a failure of knowledge, but rather a failure of action.
Aufderheide concluded by explaining that workshop presenters included a number of cardiac arrest experts, as well as speakers from outside the cardiac arrest community, whose experiences could serve as
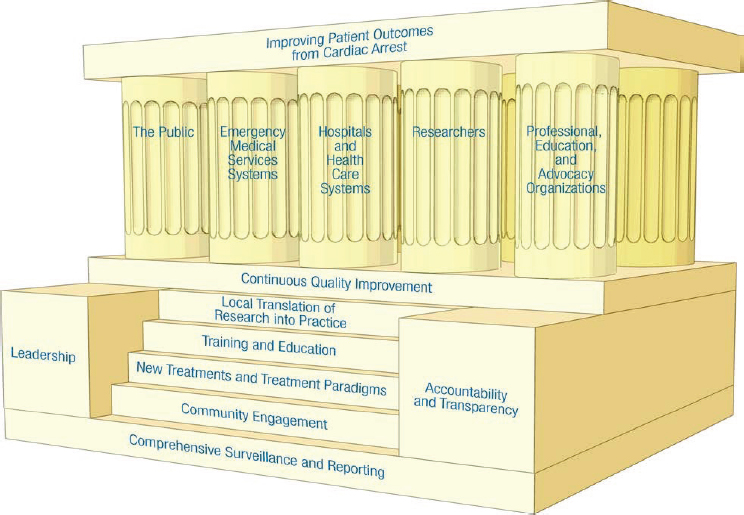
SOURCE: Presented by Tom Aufderheide, July 11, 2016, A Dissemination Workshop on the Report Strategies to Improve Cardiac Arrest Survival: A Time to Act (citing IOM, 2015, p. 7).
valuable examples to be interpreted and applied in the context of resuscitation. He urged participants to use the workshop to form new alliances and collaborations and to establish an action plan from which to advance the IOM report recommendations and improve cardiac arrest survival throughout the United States.
SURVIVING CARDIAC ARREST: THE REASON FOR ACTION
During the workshop, three speakers shared their personal cardiac arrest survival stories. The Sudden Cardiac Arrest Foundation also debuted a short video that featured survivors and their families, emphasizing the impact of immediate public reaction to cardiac arrest and urging members of the public to pursue CPR and AED training. These speakers offered perspectives on how the IOM report recommendations could be advanced and how survivors, the community, and the public could be involved in shaping the agenda moving forward. As Aufderheide noted, survivors represent a network of individuals whose lives have
been altered by cardiac arrest—spouses, children, parents, friends, and coworkers. Successful resuscitation and improved cardiac arrest outcomes affect not only the survivor but also the constellation of individuals who are closely connected to the survivor. Aufderheide said these stories of survival and the lives of the people touched by cardiac arrest are catalyzing action.
The Driving Force Behind Needed Change
James Niskanen, Sudden Cardiac Arrest Survivor
“It’s a great day to be alive! . . . I certainly have a renewed sense of what a great day of being alive means,” said James Niskanen, who had survived cardiac arrest 8 years prior to the workshop. Niskanen spoke to the audience not only as a survivor, but also as a thriver—someone who has moved beyond the initial survival of cardiac arrest and has gone on to experience a successful, fulfilling life.
Niskanen was teaching at a seminar in 2008 when he began to feel awkward, but initially dismissed the feelings as inconsequential. However, soon Niskanen began to sweat profusely and started feeling lightheaded, eventually passing out and hitting his head on the podium as he fell to the ground. As described by his best friend, Niskanen experienced “a perfect storm of good fortune” that day, because he was in a room full of CPR-trained individuals. Two women from the audience initiated CPR and others ran to retrieve a nearby defibrillator. A group of people formed a line to meet and direct the first responders. He was revived quickly with awareness of his surroundings, asking a colleague to finish his presentation for him as he was being taken to the ambulance. At the hospital, Niskanen was greeted with a capable response team. Following postarrest care, Niskanen was able to return home, where he continues to receive follow-up care in California.
Shortly after his cardiac arrest, Niskanen retired and became involved with the Citizen CPR Foundation and began speaking to interested stakeholders, including researchers, health care providers, and local communities. He was able to celebrate his 40th wedding anniversary and enjoys spending time with his grandchildren, some of whom had not yet been born prior to his cardiac arrest.
Unfortunately, not everyone survives and thrives following a cardiac arrest, said Niskanen. Just a week and a half before the HMD workshop, Niskanen lost a close friend to cardiac arrest. Despite best efforts, there were multiple breakdowns along the chain of survival; the preliminary CPR response was not optimal and the bystanders did not know where to find available AEDs. Although strengthening links in the chain of survival
may not have saved his friend, said Niskanen, it would have given him a better chance to survive.
Survivor Perspective
Kelly Sawyer, Sudden Cardiac Arrest Survivor
At the time of her cardiac arrest, Kelly Sawyer was completing a medical fellowship in emergency cardiac care and resuscitation at Virginia Commonwealth University. Near the end of her fellowship, she collapsed on campus. Two people witnessed her arrest and called 911 because the hospital code team did not respond promptly. Upon arrival the EMS personnel resuscitated Sawyer and transported her to the emergency department. Her colleagues were able to call on cardiologists, cardiac surgeons, and other specialists in a facility where access to advanced lifesaving techniques, such as extracorporeal membrane oxygenation (commonly known as ECMO) were available.
During the preliminary postarrest assessment, the emergency care physicians identified the underlying cause of Sawyer’s arrest—a massive pulmonary embolism. Sawyer was taken into emergency surgery, which was followed by the use of therapeutic hypothermia—her own area of research. Fortunately for Sawyer, everything was aligned in her favor—from the day of the week and the time of the day that the arrest occurred to the presence of a comprehensive postarrest care system. These factors and the available resources ensured not only her survival but also her quality of life. Sawyer emphasized the need for hospitals and medical systems to have effective response plans for cardiac arrests that occur on campus and beyond the reach of in-house response teams. From Sawyer’s perspective, postresuscitation care on how to ensure the functionality of patients who do survive was paramount.
From Expert to Survivor
Joseph Ornato, Virginia Commonwealth University
Joseph Ornato began by stating that, unlike other meetings on resuscitation, he had not been invited to speak as a lifelong researcher on the prevention and treatment of sudden cardiac arrest. Instead he had been asked to talk about being the beneficiary of his colleagues’ actions and knowledge, both in the EMS and hospital systems, when he suffered a massive pulmonary embolus a little more than 1 year ago. As a fairly well informed consumer in resuscitation, Ornato underscored the importance of translating the IOM report into action, including improving EMS and
hospital system performance to reflect existing knowledge. He emphasized the role of communities to implement what is already known to improve cardiac arrest survival. “It really does take a village to save a life from sudden cardiac arrest. The enemy of this particular problem is time . . . we can’t biologically control time, but we can stretch it [using techniques] such as citizen bystander CPR,” said Ornato. Improvements must occur at a local level, but it will require collaboration to bridge what have been siloed activities. Examples of success from other fields, such as the National Breast Cancer Coalition, can give us a vision and concrete guidance on how to advance our work together, concluded Ornato.
WORKSHOP THEMES
Throughout the workshop, panelists, planning committee members, and participants exchanged ideas, shared diverse perspectives, and considered the path forward for improving cardiac arrest response and outcomes. As the participants discussed opportunities and challenges connected to implement recommendations from the IOM report, a number of themes emerged from the presentations and discussions (see Box 1-2). These themes should not be viewed as conclusions or recommendations from the National Academies of Sciences, Engineering, and Medicine. Furthermore, these themes should not be interpreted as a consensus of the planning committee, speakers, or workshop participants cumulatively.
Investing in Survivors and Families
A number of workshop participants underscored the need to include more survivors and families in all resuscitation partnerships, priority-setting activities, advocacy and education efforts, and other initiatives from the local level through the national level. Aufderheide, Robert Davis, Joanne Howes, Edward Septimus, among others, emphasized the value and perspective that survivors can and should bring to partnerships across all aspects of cardiac arrest initiatives. Septimus stated that these patients and families can provide indispensable passion, advocacy, and powerful personal stories to motivate change across the resuscitation field.
A few workshop participants expressed support for establishing a national survivor network that actively involves survivors, patient advocates, families, and individuals who have lost a loved one to cardiac arrest. Although cardiac arrest survivor organizations do exist, some members of two breakout sessions called for uniting the survivor and family organizations to create a more visible and active national survivor network with stronger leadership. This network could participate in policy decisions
and be involved in efforts to educate the public about bystander CPR and AED use. To increase efficacy of the network and advocacy efforts, Howes remarked that participating survivors and family members should receive advocacy training and be centrally involved in outreach initiatives whenever possible.
Natasha Bonhomme and Gary Gibbons also emphasized the importance of patient, family, and public involvement throughout the research process. Bonhomme described the importance of building trust with patients and families to expand participation and involvement in the research process. She stated that participants should believe they are
playing an active role in research, not just a one-sided interaction in which they supply data to researchers. A number of workshop participants encouraged researchers and the resuscitation field to engage survivors and their families in a full range of activities, from setting research agendas and developing research questions to disseminating research findings and advocating for additional research funding. Niskanen commended community engagement at the neighborhood level, but noted that engagement can be difficult because it requires steadfast commitment, and some individuals or communities may be less receptive or do not share the same level of enthusiasm. Similarly, Davis emphasized the importance of enhanced public awareness to hold individuals accountable for a system’s performance level and to instill a culture of action.
Partnering to Expand Resources and Infrastructure
Current resource limitations and the health policy landscape present ongoing challenges for cardiac arrest surveillance and research activities that may require leveraging existing resources and infrastructure and expanding sustainable funding models, noted a number of participants. Michael Frankel, Gibbons, and Robert Merritt described current funding restrictions and competing priorities across government agencies and health care systems. These challenges limit new or expanded funding opportunities for cardiac arrest surveillance, research, and education initiatives as a sole programmatic focus. Aufderheide and some other workshop participants argued that financial sustainability and accountability should be considered for all surveillance, research, and quality improvement initiatives. Aufderheide, Laura Langmade, Merritt, and others suggested fostering public–private partnerships to build sustainable funding mechanisms and expand cardiac arrest surveillance and research infrastructure.
Demetris Yannopoulos and some members of a breakout session suggested exploring a bundled funding mechanism or a national funding initiative (which could pool resources from large corporate foundations and national entities, such as the American Heart Association, the Department of Defense [DoD], the National Institutes of Health [NIH], the National Science Foundation, and the Patient-Centered Outcomes Research Institute) to allocate sustainable research funds for agreed-upon research goals. Jeremy Brown and some members of his breakout group identified a number of existing federal government research programs where cardiac arrest could build on existing funding, resources, infrastructure, and partnerships.
A number of speakers emphasized the value and possible benefits of building on previous successes (e.g., Cardiac Arrest Registry to Enhance
Survival [CARES], National Emergency Medical Services Information System [NEMSIS]) and partnering with other fields that have existing, and possibly overlapping, infrastructure (e.g., stroke, trauma, other cardiovascular diseases). Noah Smith challenged the field to rethink data collection in light of new initiatives and focus on creative approaches to extract cardiac arrest data from existing data infrastructures. Langmade also emphasized the role that cognitive computing can have in aggregating data from disparate sources to improve the delivery of health care services through the promise of big data and evolving data analytics. Langmade encouraged the field to consider how relevant data are generated and collected, how those data will be mapped and moved across systems, and how the data will be monitored and validated.
A number of speakers described parameters for enhancing existing data collection and infrastructure to expand knowledge and create new research opportunities. For example, Nigel Hughes called for a large-scale data source that could be used to follow patients over decades in order to learn more about long-term outcomes. Yannopoulos and several participants in his breakout session identified a number of alternative research methods that could be used to respond to methodological limitations (e.g., adaptive trials, stratified patient groups, individualized protocols). Additionally, Frankel described the need for a system that could collect data across the continuum of care, from before and after hospitalization and beyond. Septimus commented on the importance of developing tools and resources that are scalable and manageable for all health care systems, regardless of size or budget.
Harmonizing Data and Research to Improve Performance
Improving cardiac arrest outcomes will require enhanced data and harmonization to better characterize the epidemiology of cardiac arrest and measure the impact of strategies on system performance and patient outcomes, suggested participants such as Christine Albert and Aufderheide. Several panelists and participants commented on the need for standardized performance and outcome measures. Bonhomme suggested starting with a shared infrastructure for collecting common data points across multiple conditions, and then tailoring and expanding the platform, as needed, to collect data points that are unique to cardiac arrest. Merritt, Smith, and several workshop participants articulated the significance of harmonized data sources and interoperable data exchange systems. Additionally, Raina Merchant challenged the resuscitation field to find meaningful ways to harness data that are available through social media and crowdsourcing for research. Aufderheide, Gibbons, and a few individuals during breakout sessions encouraged greater focus on imple-
mentation science to improve the translation of basic clinical science into effective interventions.
A number of participants emphasized the essential role of performance measurement and continuous quality improvement to ultimately improve patient outcomes. Aufderheide highlighted the need to understand the causes of variability in cardiac arrest care and survival rates across the United States. Kellermann urged all communities to benchmark performance around a few measures associated with the chain of survival, especially in the context of prehospital care. A number of workshop participants suggested that the implementation of continuous quality improvement programs in hospitals and EMS systems could help reduce this variability. Peter Taillac noted that a focus on quality and performance improvement would also instill a culture of excellence.
Combined with quality improvement initiatives, some workshop participants suggested that regionalization could also present opportunities to reduce variations in patient outcomes and improve the performances of local EMS and hospital systems. For example, Drew Dawson stated that a regionalized system for dispatcher-assisted CPR would maximize available resources, ensure high-quality CPR instruction for every 911 caller, and support high levels of performance. Similar to regional stroke and trauma centers, Mark Alberts described how a national network of cardiac arrest centers could lead to improved quality of cardiac arrest care and better outcomes.
Vinay Nadkarni called for hospital performance measures that could easily be adapted, measured, and compared across populations from adults through neonates. Mimi Peberdy suggested mandating hospital reporting and developing specific interim performance and outcome measures along the entire sequence of resuscitation events rather than solely focusing on the final outcome—neurologically intact survival to hospital discharge. A few individuals during breakout sessions warned against onerous data collection and reporting systems in the absence of demonstrable impacts on outcomes. Septimus reiterated that all process measures must be linked to better outcomes, and unintended consequences need to be considered when developing and implementing new process measures. Additionally, a number of workshop participants described limitations of current coding systems, stating that the lack of separate codes for in-hospital cardiac arrests, OHCAs, and pediatric cardiac arrests, as well as the lack of available coding for specific cardiac arrest therapies, create significant research challenges.
A number of workshop participants noted the potential to align efforts among related fields to improve surveillance and research. Smith suggested that the resuscitation field faces many challenges related to surveillance and research that are not unique to cardiac arrest, registries,
EMS, or hospital care, in general. Taillac suggested that improvements to EMS systems’ performance that combined cardiac arrest, trauma, stroke, and other fields could positively reshape patient safety and outcomes. Gibbons described the National Heart, Lung, and Blood Institute’s new Precision Medicine Initiative Cohort Program, which aims to improve knowledge about myriad diseases by enhancing data collection and sharing on genetic, social environment, economic status, geography, among other factors, from a cohort of more than 1 million participants.
Unifying Messaging and Broadening Engagement
Unified messaging and communication strategies can elevate the visibility of cardiac arrest as a serious public health concern, educate the public, strengthen advocacy efforts, and build momentum for future progress and policies. Niskanen and other participants noted common confusion about the differences between heart attacks and cardiac arrest. Generally the public is familiar with the term massive heart attack, Niskanen noted, because it implies that nothing could have been done to save a person. Bystanders need to understand that cardiac arrest is not a heart attack and know how to recognize the former because an individual’s actions can save a life, a number of workshop participants echoed.
A number of workshop participants observed that the lack of consistent messaging across the resuscitation field has hindered efforts to successfully engage communities and educate the public about cardiac arrest and the importance of bystander CPR. To overcome this barrier, Howes urged the field to come together and develop agreed-upon messaging and communication strategies to move the field forward with one voice. Davis, Howes, and Paul Pepe asserted that the messages need to be singular, simple, concise, easy to communicate, and compelling. To be effective, they said, the messages must be consistent yet applicable to different environments, ranging from broad public education and awareness efforts to technical discussions of research funding and findings. Pepe and several workshop participants called on the field to employ professional communications experts, as well as focus groups, to formulate the messages and gain consensus.
The resuscitation community must also focus on how to effectively communicate established messages to change behavior, said Merchant. Several workshop participants highlighted engaging experts in behavior change, marketing, and advertising when developing communication strategies that can reach diverse audiences. Howes suggested enlisting a spokesperson or an organization to lead communication efforts to represent the entire field. Davis, Merchant, and a few individuals during breakout sessions described how existing and emerging technologies,
such as mobile devices and social media, could be used to communicate messages, execute public education campaigns, and explore new research opportunities.
Effective messaging complements efforts to improve accountability for EMS and hospital system performance and establish higher standards of care—such efforts can clearly identify and explain examples of successes to emulate and failures from which to rebuild and improve, said Davis. In addition to their role in boosting public awareness, unified messaging and communication strategies are also essential components in advocacy efforts for research support and policy changes, stated one breakout group. For example, Howes highlighted the National Breast Cancer Coalition’s effort to train lay advocates, including survivors, about the science and how to talk about the more pressing issues with a wide range of stakeholder groups. Some members of another breakout group suggested that localities describe the magnitude of local challenges, progress being made, and measures of EMS and hospital performance in messaging to communities—all communities should know their numbers in terms of survival rates.
Cultivating Partnerships and Leadership
Many participants voiced support for the IOM report recommendation to establish a national cardiac arrest collaborative. Although the diverse range of organizations and stakeholders across the resuscitation field has provided a wealth of experience and knowledge, a national cardiac arrest collaborative with broad, inclusive membership could promote efficiencies and a common platform from which to advance resuscitation science and outcomes beyond the capacities of any single organization or entity, as described by Alberts, Vicky Whittemore, and several other workshop participants. Different speakers suggested that such partnerships and collaboration could help articulate shared vision, establish common goals and complementary agendas, generate consistent messaging, and promote joint initiatives. Furthermore, partnerships will be critical in defining and implementing standardized certification requirements and protocols, as well as quality improvement, performance, and outcome measures, remarked Frankel, Merritt, and others.
Workshop participants discussed the need for a flexible approach to collaborative structure and purpose in response to changes in the health policy landscape and membership composition. Whittemore discussed the evolution of collaboration in the epilepsy field, describing the transition from informal but regular communications among partners to the restructuring and rebranding of a formal collaborative that works to promote greater efficiency and impact. Albert talked about the critical sup-
port of the NIH and the National Institute of Neurological Disorders and Stroke, which provides support and infrastructure for the Brain Attack Coalition. Bonhomme described how Genetic Alliance evolved from a support group organization to a network of 10,000 organizations that advance policy, advocacy, education, and emerging scientific tools. Howes described the grassroots evolution of the National Breast Cancer Coalition, whose board includes expert volunteers from individual organizations, to advance breast cancer research and evidence-based health care in the fight to end breast cancer. Individual speakers discussed barriers to sustainable funding for not only infrastructure and day-to-day activities but also initiatives of the collaborative.
Active leadership is necessary to foster potential partnerships and collaborations and to leverage existing resources, said Lance Becker and Albert. Aufderheide said that the field will need to identify accountable, capable leaders at national, state, and local levels. Septimus and multiple breakout session participants called for champions and commitment from local hospitals and health care systems to promote cultures of improvement and excellence. Dawson, Pepe, and several workshop participants proposed more robust partnerships and active engagement across EMS agencies, EMS medical directors and personnel, public-safety answering points, health care systems, hospitals, a variety of health care providers, survivors, families, and the public to improve bystander, EMS, dispatcher, and hospital performance and to enhance cardiac arrest outcomes in communities across the United States.
REFERENCES
Atkins, D. L., S. Everson-Stewart, G. K. Sears, M. Daya, M. H. Osmond, C. R. Warden, and R. A. Berg, for the Resuscitation Outcomes Consortium Investigators. 2009. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation 119(11):1484–1491.
Aufderheide, T. C. 2016. Workshop on strategies to improve cardiac arrest survival. Presentation at the Dissemination Workshop on the Report Strategies to Improve Cardiac Arrest Survival: A Time to Act, Washington, DC. http://www.nationalacademies.org/hmd/~/media/Files/Activity%20Files/PublicHealth/TreatmentofCardiacArrest/JULY%202016%20Workshop/Aufderheide%20Day%201.pdf (accessed October 30, 2106).
Chatalas, H., and M. Plorde, eds. 2014. DivisionofEmergencyMedicalServices2014annualreport to the King County Council. Seattle, WA: Emergency Medical Services Division of Public Health Department—Seattle and King County. http://www.kingcounty.gov/healthservices/health/%7e/media/health/publichealth/documents/ems/2014AnnualReport.ashx (accessed October 30, 2016).
Daya, M., R. Schmicker, S. May, and L. Morrison. 2015. Current burden of cardiac arrest in the United States: Report from the Resuscitation Outcomes Consortium. Paper commissioned by the Committee on the Treatment of Cardiac Arrest: Current Status and Future Directions. http://www.iom.edu/~/media/Files/Report%20Files/2015/ROC.pdf (accessed October 30, 2016).
IOM (Institute of Medicine) 2015. Strategies to improve cardiac arrest survival: A time to act. Washington, DC: The National Academies Press.
Merchant, R. M., L. Yang, L. B. Becker, R. A. Berg, V. Nadkarni, G. Nichol, B. G. Carr, N. Mitra, S. M. Bradley, B. S. Abella, and P. W. Groeneveld, for the American Heart Association Get With the Guidelines–Resuscitation Investigators. 2011. Incidence of treated cardiac arrest in hospitalized patients in the United States. Critical Care Medicine 39(11):2401–2406.
Morrison, L. J., R. W. Neumar, J. L. Zimmerman, M. S. Link, L. K. Newby, P. W. McMullan, Jr., T. V. Hoek, C. C. Halverson, L. Doering, M. A. Peberdy, and D. P. Edelson, for the American Heart Association Emergency Cardiovascular Care Committee, the Council of Cardiopulmonary, Critical Care, Perioperative and Resuscitation; the Council on Cardiovascular and Stroke Nursing; the Council on Clinical Cardiology; and the Council on Peripheral Vascular Disease. 2013. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: A consensus statement from the American Heart Association. Circulation 127(14):1538–1563.
Resuscitation Academy. 2014. Strategies to improve survival from cardiac arrest: An evidence-based analysis. Seattle, WA: Resuscitation Academy. http://www.resuscitationacademy.org/downloads/RA-35-Strategies-to-Improve-CA-Survival.pdf (accessed October 30, 2016).
This page intentionally left blank.


















