7
Catalyzing Innovation
There must be a willingness to change the way global health business is conducted to better enable innovation and truly achieve sustainable and resilient health systems in every country, fostering prosperity and development. Given the multisectoral nature of health, simply addressing individual challenges in a singular, siloed manner will never solve the overall problem. Challenges in the drug development process for infectious and neglected diseases have plagued researchers and developers since before human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) captivated the world’s attention in the 1980s. But since then, the challenges have only expanded—many infectious diseases still plague the world without an effective cure or vaccine, and many chronic conditions or noncommunicable diseases (NCDs) in low- and middle-income countries (LMICs) face limited treatment options. The committee believes that, through innovations and the development of partnerships, critical medical product development can be accelerated and public health services can be provided in a more sustainable manner. Furthermore, the extraordinary advances in information technology have the potential to revolutionize global health and bypass the necessity of costly brick-and-mortar health services.
This chapter provides examples and strategies to catalyze these innovations to improve health outcomes, by first discussing the various ways to accelerate the development of medical products. This includes addressing multiple steps along the value chain, such as enabling innovative trial designs, streamlining regulation, ensuring both the supply and demand through manufacturing capacity and market incentives, and finally building research and development (R&D) capacity in LMICs. The chapter then
proceeds to review progress in digital health tools and uses worldwide, highlights remaining gaps, and charts a path forward for the United States to better support global health investments through technology.
ENABLING INNOVATION: ACCELERATING THE DEVELOPMENT OF MEDICAL PRODUCTS
The market for global health products suffers numerous failures—including lack of manufacturing capacity, a costly approval process, uncertain commercial potential, and poor workforce and laboratory capacities in LMICs. From 1975 to 1999, only 1.1 percent of new drugs were developed for neglected diseases. Given the international support and political attention resulting from the Millennium Development Goals1 in 2000 it would be expected that this percentage would climb. However, between 2000 and 2011, only 4 percent of new products were indicated for neglected diseases2 (Pedrique et al., 2013). This dearth of available medical products results in patients suffering from diseases, such as tuberculosis, malaria, and other potential pandemic diseases, without access to essential medicines. Though there are many promising process innovations, the entire value chain for global health products needs re-tooling. The committee considered a variety of means to streamline the R&D pipeline for global health products and offers strategies that government agencies, industry, and global health players can explore. These include enabling innovative trial design approaches; streamlining regulation; ensuring supply; creating market incentives; and building capacity for medical products manufacturing in partner countries to foster global health security and better support local needs.
Enabling Innovative Trial Design Approaches
Traditional clinical trials, though the mainstay of clinical research, often have shortcomings because of their rigidity or poor adaptability of results in real-life circumstances. For example, randomized clinical trials (RCTs) may require a large sample size and lengthy study duration (Bhatt and Mehta, 2016). In part because of these requirements, the costs of drug
___________________
1 The Millennium Development Goals are “The world’s time-bound and quantified targets for addressing extreme poverty in its many dimensions—income poverty, hunger, disease, lack of adequate shelter, and exclusion—while promoting gender equality, education, and environmental sustainability. They are also basic human rights—the rights of each person on the planet to health, education, shelter, and security” (Millennium Project, 2006).
2 For this analysis, the term neglected diseases includes 49 different diseases in five categories: malaria, tuberculosis, diarrheal diseases, the WHO list of 17 neglected tropical diseases, or other neglected diseases (19 of which did not fit into another category). See supplementary appendix of Pedrique et al. (2013) for a detailed listing.
development have increased nearly 100-fold between 1950 and 2010, when adjusting for inflation, despite fewer new drugs being approved by the U.S. Food and Drug Administration (FDA). The core problem of clinical trials seems to be that processes that support them have not been improved (Pammolli et al., 2011; Woodcock and Woosley, 2008). The committee believes that the costly drug development process could be improved to reduce costs and attract pharmaceutical companies to develop more products needed for neglected global health diseases. One way of accomplishing this goal is through the encouragement of manufacturers to use more innovative product development approaches that improve the effectiveness and efficiency of the clinical trial process. Three approaches emerged in recent years and include adaptive clinical trials, pragmatic clinical trials, and surrogate endpoints (or biomarkers).
Adaptive Trial Designs
Clinical trials are often hindered by the rigidity of the protocols. A traditional RCT may not offer the flexibility necessary to modify its study design based on interim data that emerges as a trial progresses (Mahajan and Gupta, 2010). The adaptive clinical trials method, an alternative approach to a traditional RCT, embraces more flexibility and efficiency. This provides manufacturers the opportunity to modify the study design and hypothesis based on the analysis of interim data (FDA, 2010), as well as possibility shortening the development time to speed up the process (Chow and Corey, 2011). Among other benefits, adaptive trials design allow a more rapid divestment from unsuccessful compounds without wasting as much time or resources. Importantly, though adaptive trials seek to make clinical research more efficient, they still involve randomization3 (Mahajan and Gupta, 2010). An additional adaptive method, the use of platform trials, are appealing because of their potential improved efficiency in creating superior evidence compared to single-sponsor, single-drug trials (Trusheim et al, 2016). A platform trial is a clinical trial with a single master protocol that can evaluate multiple treatments simultaneously, and can result in fewer patient failures and a shorter timeline—improving overall financial sustainability (Saville and Berry, 2016). While there are many benefits to be realized, conducting these types of trials effectively will require overcoming
___________________
3 Randomization in clinical trials means the random assignment of participants to treatment groups, which contributes to the efficacy and internal validity of a trial. Forms of randomization include simple randomization, in addition to block, stratified, and covariate adaptive randomization. Specific types of randomization used in adaptive trials are described by (Mahajan and Gupta, 2010). As each type has its advantages and disadvantages clinical trial teams will need to assess the context surrounding the trial before determining which type of randomization to use.
many operational and statistical challenges, such as coordinating multiple sponsoring companies in collaborative governance and ensuring standardized protocols are followed supported by adequate data sharing (Trusheim et al., 2016).
While FDA has issued draft guidance on the use of adaptive clinical trials (FDA, 2010), there is still lack of clarity on how they would be evaluated. However, with the passing of the 21st Century Cures Act in 2016,4 FDA has been directed to host a public meeting to discuss the incorporation of complex adaptive and other novel trial designs into clinical protocols and new drug applications as well as to issue additional guidance regarding their use (Brennan, 2016b). This could potentially set up a more efficient, yet safe environment conducive to accelerating development for certain diseases. Despite the promise of adaptive trials though, there can be several operational challenges such as pre-planning protocol deviations, complicated mathematical modeling, and the risk of false effectiveness conclusions (Chow and Corey, 2011; FDA, 2016a). These challenges will require continued evaluation when designing trials within this adaptive and accelerated environment.
Pragmatic Trials
In addition to the rigidity of their protocols, traditional RCTs, through strict control for biases, produce results that are statistically credible but not always applicable to real life circumstances such as demographics of the trial population, proximity to a study site, or patient adherence (Zwarenstein and Oxman, 2006). However, the use of “real-world evidence,” such as electronic health records, medical claims data, disease registries, and data gathered through personal devices, can complement the knowledge gained from clinical trials. As a result, researchers and medical product manufacturers have expressed interest in integrating such real world settings into clinical research (Sherman et al., 2016). As a result, pragmatic trials have emerged as a mechanism to incorporate such data into clinical trials so interventions are tested in the full range of clinical settings and the findings are more generalizable (Patsopoulos, 2011) to close the gap between research and care. Requirements for pragmatism are described by the PRECIS-2 tool,5 but overall pragmatic trials involve heterogeneity of participants and study settings in addition to numerous interacting com-
___________________
4 See https://www.congress.gov/bill/114th-congress/house-bill/34 (accessed April 6, 2017).
5 The PRECIS-2 tool includes dimensions of investigator and participant eligibility, recruitment, and setting; the organization of the intervention; the flexibility in delivery and adherence of the intervention; the nature of the follow-up; and the determination and analysis of the primary outcome (Ford and Norrie, 2016).
ponents, such as other medications or health conditions participants may have (Ford and Norrie, 2016; Patsopoulos, 2011). Though pragmatic trials seek to relax the control aspect of a clinical trial,6 they also still use randomization (Ford and Norrie, 2016) and often require a larger sample size as a result of the increased heterogeneity (Patsopoulos, 2011). Researchers should adopt features of pragmatic trials where feasible, but refrain if there are questions of trial quality compromise (Ford and Norrie, 2016).
Pragmatic trials and the use of real world data have been encouraged by the U.S. government, and future expanded use of this trial type looks promising. The American Recovery and Reinvestment Act included $1.1 billion for comparative effectiveness research (Patsopoulos, 2011). And with the passing of the 21st Century Cures Act, FDA is now required to develop a framework on evaluating real world evidence for drug regulation to guide its use in clinical trials (Hills and Zegarelli, 2017). However, pragmatic trials may present new challenges, such as participant recruitment and consent, practice variation, or risk determination (Anderson et al., 2015; Ford and Norrie, 2016; Sugarman and Califf, 2014), all of which will demand continued dialogue among multiple stakeholders to adequately address the scientific, ethical, and regulatory challenges.
Biomarkers as Surrogate Endpoints
The primary outcome of a clinical trial is known as a clinical endpoint, and it characterizes whether or not a participant develops a symptom, disease, laboratory anomaly, or even death in response to the disease course or treatment under study. While these are clear metrics for the success or failure of a treatment, some may occur years after the end of a trial. The use of biomarkers7 that can provide interim evidence about safety and effectiveness is an advancement in clinical research that addresses this issue, and therefore speeds up the drug development process. Establishing a biomarker as a surrogate endpoint,8 however, is difficult and requires strong evidence to validate its use.9 As a result, FDA approves the use of
___________________
6 A controlled trial is a type of clinical trial in which observations made during the trial are compared to a standard, called the control. The control may be observations of a group of participants in the same trial or observations from outside the trial—for example, from an earlier trial, which is called a historical control (NLM, 2017).
7 Biomarker: A substance, structure, or process that can be measured and influence or predict a clinical outcome or disease (WHO, 2001).
8 Surrogate endpoint: A well-characterized biomarker that can act as a substitute for a clinical endpoint (Strimbu and Tavel, 2010).
9 Strong scientific evidence must show that a biomarker be objectively measured, strongly correlates with the clinical endpoint, has predictive power in other related studies, and that it can be relied on to serve as a surrogate in other related clinical endpoints (Strimbu and Tavel, 2010).
biomarkers as surrogate endpoints on a provisional basis, requiring phase IV10 studies to prove correlation. It is important to note that even defined biomarkers may not always be an indicator of a clinical endpoint, and are likely to draw erroneous conclusions (Strimbu and Tavel, 2010). Thus, while biomarkers may improve the efficiency of clinical trials and their use has been encouraged by FDA (FDA, 2004), they must be further developed to improve their reliability. Encouraging researchers to identify biomarkers for use could be an integral step in this process, as this method will be difficult for FDA to review and assist without active participation through proposed biomarkers in relevant research. The committee hopes that, in compliance with the 21st Century Cures Act, FDA provides guidance on a review pathway (Brennan, 2016b) and collaborates with scientific partners to develop qualification plans. This would ensure a safe path forward for more rapid product development.
Communicating in Crisis
A trial design may use a combination of these approaches depending on the disease in question. As a result, early communication among researchers and regulators around the globe is vital to clarify the best approach and ensure study success. In fact, a 2017 National Academies of Sciences, Engineering, and Medicine report, Integrating Clinical Research into Epidemic Response: The Ebola Experience, noted that international researchers missed the opportunity to quickly and collaboratively come to an agreement on trial design, which stalled efforts (NASEM, 2017a). Furthermore, Peter Marx, director of the Center for Biologics Evaluation and Research at FDA, discussed early conversations of regulators with trial sponsors and suggested it could be beneficial to bring the scientific community and international regulators together during an international health emergency to review the results available from differing trial designs. Overall, all of these trial designs present alternative options to be explored, but continued investment and dedication from all parties, including regulators, industry, and academic researchers, will be needed to continue to shape the trials to produce safe and efficacious medical products and as efficiently as possible.
___________________
10 Phase IV studies are done after the drug or treatment has been marketed to gather information on the drug’s effect in various populations and any associated side-effects following long-term use. For more on clinical trial phases, see https://www.nlm.nih.gov/services/ctphases.html (accessed April 13, 2017).
Streamlining Regulation
As the oldest consumer protection agency in the United States, FDA requires drug manufacturers to prove the safety and efficacy of products before they enter the market, and continues these safety evaluations through post-market surveillance (Danzis, 2003; Merrill, 1996). Although the process of drug approval protects consumers, it is complex and costly, and it can take 12 to 15 years for a new drug to be developed and enter the market (see Figure 7-1). Furthermore, this process is a risky investment: The average cost of developing a drug is over $2.5 billion (DiMasi et al., 2016), and only 9.6 percent of all new drugs successfully progress from Phase 1 clinical trials to FDA approval (Thomas et al., 2015). Of all new drugs intended for infectious diseases, 19.1 percent are approved (Thomas et al., 2015). Private companies decide which products they will invest in based on a risk assessment to their business and potential for financial return. If a company believes the costs and risks for development are too high, or the market for the product is too uncertain and small, investment in this product is unlikely to occur.
To partially alleviate the gap in development for global health priorities, the Center for Drug Evaluation and Research (CDER), the division of FDA tasked with overseeing the approval process, offers a variety of alternative review mechanisms that can reduce costs and risks by speeding up the timeline. Typically, CDER is expected to review and act on 90 percent of new drug applications within 10 months. However, CDER employs four different regulatory mechanisms for expedited review: fast-track, breakthrough therapy, accelerated approval, and priority review, as described in Box 7-1. The expedited review mechanisms are an example of how the U.S. government can reduce or share the burden of development costs and risks with industry, effectively “pushing” a product through the pipeline.
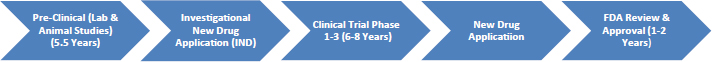
SOURCES: Adapted from Ciociola et al., 2014; Thaul, 2012.
In addition to expedited review, Congress has implemented mechanisms related to regulation to incentivize industry partners to develop needed global health products that may not have a clear commercial market. Examples include the Orphan Drug Act, the Priority Review Voucher (PRV), and the Generating Antibiotic Incentives Now (GAIN) Act, which are described in the section below. While each mechanism has elements designed to attract manufacturers, they have not been used as widely as needed to have a clear effect on the dearth of critical products. The committee believes that this is partially because these incentives do not compensate enough for the costs of regulatory approval, and sees an opportunity for reassessment and expansion of these mechanisms to further streamline the approval process for critical global health products.
Orphan Drug Act
The Orphan Drug Act of 1983 was introduced to incentivize drug development for rare diseases11 by providing pharmaceutical companies a 7-year market exclusivity, a tax credit that covers 50 percent of clinical trial costs, R&D grants, fast-track approval, and a waiver of the user fee associated with the application (Franco, 2013). As of November 2013, FDA has granted 2,923 diseases orphan status (relying on sponsors to request designation) (FDA, 2016b) but only granted market approval to 447 drugs (FDA, 2017).
The diseases receiving orphan designation have mostly been cancers with relatively few of them being neglected diseases. Those neglected diseases that have been given orphan status, such as malaria, tuberculosis, and leishmaniasis (Sachs-Barrable et al., 2014), are mostly prevalent among the U.S. military and travelers (Villa et al., 2009). Because the Orphan Drug Act was developed to address diseases in domestic markets (Villa et al., 2009) and neglected infectious diseases typically affect the world’s poorest, most pharmaceutical companies do not frequently pursue drug development for these diseases through this act (Warshaw, 2015). Leveraging the Orphan Drug Act to spur development for neglected diseases has been suggested, with one solution proposed in a past bill (HR 3156) submitted to the 111th Congress in 200912 met with little success. In 2014 multiple candidates to treat the Ebola virus were given orphan drug designation, but this does not guarantee the drug will be developed as some companies were hesitant to
___________________
11 Rare diseases are defined as those that affect 200,000 patients or less, or those that affect more but for which drug development costs are unlikely to be recovered in the United States.
12 To amend the Internal Revenue Code of 1986 to provide a credit against tax for expenses paid or incurred in non-clinical research for neglected diseases, H.R. 3156, 111th Congress. 2009–2010. See https://www.congress.gov/bill/111th-congress/house-bill/3156 (accessed April 9, 2017).
start the process until they had secured additional funding through a partnership or government (Lyon, 2015; Radke, 2014). This further highlights the need for sustainable, collaborative investment for neglected diseases.
Priority Review Voucher Program
The PRV program was established in 2007 and designed to reward innovators for developing novel treatments for diseases that would otherwise not attract development interest. While initially intended for neglected diseases, additional PRV programs have since been created to include rare pediatric diseases in 2012 (Gaffney et al., 2016) and medical countermeasures in 2016 (Brennan, 2016a). In exchange for producing drugs for such diseases, FDA grants manufacturers a voucher that allows them to designate another product in their pipeline for priority review (Aurora et al., 2016). If manufacturers have potential blockbuster drugs in their pipeline, the ability to enter market even 4 months in advance could translate into millions of dollars in profit. As of November 2016, 13 vouchers had been awarded—4 of which were for drugs treating neglected (or tropical) diseases (Gaffney et al., 2016). Furthermore, there are currently three products in the pipeline for this category—motivated by a PRV—targeting river blindness, tuberculosis, and dengue fever (Aurora et al., 2016).
While the PRV program has some novel aspects to incentivize drug development for neglected diseases, such as permitting FDA to add new pathogens to the list of eligible diseases “by order,”13 there are concerns about its effectiveness and whether the program is being exploited. The first PRVs granted for neglected disease were either already developed or in late-stage of development, leading some to question whether it is indeed incentivizing development or just acting as a giveaway to companies who were already doing that type of work. Furthermore, PRVs have been sold to other companies, often commanding high prices. The first ever sale was valued at $67 million, with subsequent vouchers being sold as high as $350 million (Gaffney et al., 2016). The most recent voucher was sold for $125 million (Brennan, 2017). Other concerns raised about the PRV program include the uncertainty that the drug will be approved, taken to market, or taken to market at an affordable price (Aurora et al., 2016). Finally, there are limitations in the application as only novel ingredients are eligible, so innovations in delivery such as follow-up formulations that can be applied to resource poor settings would not qualify (Kesselheim,
___________________
13 With the passing of Public Law 113-233 (December 16, 2014), FDA is now permitted to add new viruses to the list of voucher-eligible tropical diseases “by order” instead of “by regulation.” This allows FDA to make changes more quickly, without going through the typical notice-and-comment provisions of federal regulation (Gaffney et al., 2016).
2008). These concerns notwithstanding, the PRV program should be seen as one beneficial tool in the “incentives toolbox,” but would benefit from reevaluation, and assurance that FDA has the appropriate resources needed to optimally manage the program.
Generating Antibiotic Incentives Now Act
In contrast with the Orphan Drug Act and the PRV program, the GAIN Act does not address a rare or neglected disease, but still fills an unmet need. As discussed in Chapter 3, the dire health and economic challenges that antimicrobial resistance poses, in addition to the dwindling pipeline for new antimicrobials, makes it essential to spur development. This is compounded by the high cost of bringing a new medicine to market, especially when antimicrobials generate such small revenue compared to other drugs. The GAIN Act encourages the development of new products targeting “qualifying pathogens”14 by awarding an additional 5 years of market exclusivity, priority review, and eligibility for fast-track designation. In addition, the GAIN Act requires FDA to provide clarity on the development pathway of these therapeutics (Pew Charitable Trusts, 2013). As of September 2016, 40 new antimicrobials are in clinical development for U.S. market, many of which address indications eligible for GAIN Act benefits (Pew Charitable Trusts, 2016).
Ensuring Supply
Enabling the efficient development of medical products and streamlining regulatory processes to facilitate a faster timeline is only half the challenge of ensuring drugs, vaccines, and devices reach people in a timely manner. There is a need in the latter stages of development to ensure adequate manufacturing capacity for these products to meet global demand. This is especially important for diseases that might threaten the global population, such as pandemic influenza (reviewed in Chapter 3). The Biomedical Advanced Research and Development Authority (BARDA) within the Office of the Assistant Secretary for Preparedness and Response
___________________
14 Following a final rule July 7, 2014, the list of qualifying pathogens includes Acinetobacter species, Aspergillus species, Burkholderia cepacia complex, Campylobacter species, Candida species, Clostridium difficile, Coccidioides species, Cryptococcus species, Enterobacteriaceae (e.g., Klebsiella pneumoniae), Enterococcus species, Helicobacter pylori, Mycobacteriumtuberculosis complex, Neisseria gonorrhoeae, N. meningitidis, non-tuberculous mycobacteria species, Pseudomonas species, Staphylococcus aureus, Streptococcus agalactiae, S. pneumoniae, S. pyogenes, and Vibrio cholera. See https://www.federalregister.gov/documents/2014/06/05/2014-13023/establishing-a-list-of-qualifying-pathogens-under-thefood-and-drug-administration-safety-and (accessed April 7, 2017).
understands this need and has been working through global partnerships to increase manufacturing capacity for threats within their mission, such as pandemic influenza. In 2005, there were fewer than 1 million doses of influenza vaccine available worldwide, which prompted a move to advance clinical development by at least 9 developing country vaccine manufacturers and licensure by at least 7 developing country manufacturers (Bright, 2013).
In 2006, the Global Action Plan for Influenza Vaccines was implemented to increase capacity for manufacture and access to vaccines in LMICs. From 2006 to 2013, seasonal vaccines production increased from 500 million to 1.5 billion doses and pandemic vaccines rose from 1.5 billion to 6.2 billion doses (McLean et al., 2016). In 2015, pandemic vaccine capacity continued to increase from 6.2 billion to 6.4 billion doses, but seasonal vaccine capacity dropped to below 1.5 billion doses, largely due to a shift toward more quadrivalent vaccine15 production and increased use of adjuvants16 (McLean et al., 2016).
Since the pathogen that will cause the next pandemic is unknown, it would not be prudent to maintain ongoing capacity for every possible pathogen with pandemic potential. Yet, due to severe consequences of a pandemic, unique models are required to ensure supply of needed drugs, vaccines, and diagnostics. To help address this issue, in 2012 BARDA established three Centers for Innovation in Advanced Development and Manufacturing (CIADMs) that can transition quickly and cost effectively between products. CIADMs are public–private partnerships that bring together small biotechnology companies, academia, and large pharmaceutical companies with continued focus on improving current initiatives and medical countermeasures to reduce risk, increase yield, and reduce life cycle costs through flexible manufacturing. These CIADMs support workforce development through training current and future industry and government scientists, and can also augment manufacturing surge capacity in a public health emergency (HHS, 2017). Acknowledging the need for a long-term commitment and outlook when developing and manufacturing medical products, government contracts with CIADMs can be renewed for up to 25 years. While this is a step in the right direction, they will not solve the problem entirely, and have yet to be tested by the next pandemic. Sustained commitment and awareness in this area is needed.
___________________
15 A quadrivalent vaccine is one that works by stimulating an immune response against four different antigens, such as four different viruses or other microorganisms (NCI, n.d.).
16 An adjuvant is a substance that is formulated as part of a vaccine to enhance its ability to induce protection against infection. Adjuvants help activate the immune system, allowing the antigens—pathogen components that elicit an immune response—in vaccines to induce long-term protective immunity (NIAID, 2015).
Creating Market Incentives
When working with the private sector, the global health community and governments need to understand that companies are required to demonstrate a rational allocation of capital that provides the highest return on investment. There are areas of mutual interest and the private sector is a necessary partner in global health R&D, but it cannot be expected to make investments without any expectation of a return. As far back as the 1997 IOM report America’s Vital Interest in Global Health, experts have understood the need for public–private cooperation and development of incentives for the pharmaceutical, vaccine, and medical device industries to invest in R&D of products with risky or unfavorable markets. The 1997 report called for allowing multi-tiered pricing of drugs and vaccines, safeguarding intellectual property rights, and increasing incentives for product development (IOM, 1997). The world has seen a huge amount of progress in this area in the last 20 years, and with the creation of BARDA in 2006, many types of incentives have been explored for medical countermeasure development, though a mixture of push17 and pull mechanisms.18 However, because many incentives include payments from the government to pharmaceutical companies, there is often a challenge in securing trust and buy-in from the public because of the optics of this type of relationship.
There are general areas of consensus around pull incentives, such as the agreement on reducing market uncertainty by guaranteeing volumes and prices, and building in provisions for public health objectives. De-linkage models that separate price from R&D costs—either full or partial—are especially favored with regards to antibiotic development because it guarantees returns on investments and removes the motivation to oversell the product (Renwick et al., 2016). Challenges with pull mechanisms exist because the political commitment needs to be sustained for several years, which is difficult to guarantee when government leaders can change every few years. Additional barriers exist because pull mechanisms, administered through appropriation funds, guarantee that a product will be funded. Yet, if these products are funded and developed with U.S. taxpayer money and the disease that they address never manifests as a threat, Congress will be skeptical to fund future projects. Similarly, push mechanisms are difficult for the U.S. government to implement because of the extremely high costs of drug development; they would require a large infusion of money up front in order to incentivize involvement. In 2014 the President’s Council
___________________
17 Push mechanisms incentivize industry by reducing the cost of R&D. These can include product development partnerships and direct research grants (Dimitri, 2012).
18 Pull mechanisms incentivize industry by creating a market demand, which can include tiered pricing, advanced market commitments, and prize funds (i.e., a payment conditional on producing the product) (Dimitri, 2012).
of Advisors on Science and Technology (PCAST) report recommended a significant increase in economic incentives for developing urgently needed antibiotics (PCAST, 2014). The report proposed the establishment of an antibiotic incentive fund to provide advanced market commitments, or market guarantee, and milestone payments to reward developers. One new approved antibiotic per year was estimated to require an annual investment of $800 million.
Tiered pricing continues to be explored as a mechanism to expand access to affordable drugs and other health products. It has proven critical to the success of global immunization programs and expanded access to affordable vaccines. This mechanism is more effective when market risk is low, for example, when there is an assured source of financing like Gavi, the Vaccine Alliance (Gavi); and when there is a competitive market with adequate production capacity. The success of tiered pricing also depends on a tacit agreement of high- and middle-income markets that poorest countries will receive lower prices. Finally, mechanisms that help ensure that the low tier prices are available only in those approved low-income countries and do not leak into higher-income markets are important. When these conditions can be met, tiered pricing is a valuable mechanism to maintain a viable market for industry while ensuring the critical product is still available to the poorest people (Moon et al., 2011).
A Suite of Approaches
Overall, an important takeaway for incentives is that there is no magic bullet solution, as different approaches will be necessary for different shortcomings in the market. As a result, there is a need to articulate and test a suite of options and incentive models with multiple key stakeholders, as market shaping often requires partnership and coordination, since different options will appeal differently based on company characteristics (USAID, 2014). The U.S. Agency for International Development (USAID) has conducted market shaping for vital global health issues such as the latest Zika virus outbreak. To lower the risk and incentivize the private sector to accelerate the development of Zika diagnostics, USAID partnered with the United Nations International Children’s Emergency Fund (UNICEF) to create an advanced purchase commitment valued at $10 million (USAID, 2017). Considerations for incentive development will vary by stakeholder involved (i.e., large pharmaceutical companies vs. small biotechnology companies), and the product or process being targeted (i.e., emerging infectious diseases versus classic drug development). Regardless of the incentive used, it is important for stakeholders to act soon and adapt, as markets fluctuate constantly (USAID, 2014). Multiple other studies and reports have echoed the call for flexibility and diversity of incentives in order to be effective
when there is no clear market for the product—especially to address antimicrobial resistance (BCG et al., 2015; PCAST, 2014; Renwick et al., 2016; Review on Antimicrobial Resistance, 2015).
Research and Development Capacity
There are many opportunities to accelerate drug development through regulatory and market incentives, more innovative trial design approaches, streamlined regulations, and adequate supply. Yet, building local capacity to conduct clinical trials in countries where these diseases are endemic is paramount. As the world faces new health threats that can more easily cross national borders, investing in global R&D will require expansion of local capabilities to anticipate new threats and augment opportunities for the development of novel vaccines and therapeutics. As the economies of the world continue to grow, and many once-recipient countries begin to develop their own capacities for R&D, the role of the United States should also adapt.
Why Invest in Foreign Country Capacity?
True collaboration is vital to the success of R&D partnerships. They must be conceived through a clear understanding of the mutually understood benefits, resulting in a truly reciprocal approach for all parties (Lucas, 2005). This model provides the basis for strong collaborations that will help to dually develop capacity in LMICs and support the United States’ efforts to prevent global outbreaks. In their 2016 report on the U.S. government’s role in R&D for global health, the Duke University’s Global Health Institute also emphasized the need to build R&D capabilities in countries receiving development assistance for health (DAH). This 2016 report agreed with the Lancet Commission on Investing in Health that DAH funding should increasingly be spent on global functions for health (similar to the concept of global public goods discussed in Chapter 8). One way to achieve this, the Duke team reported, is to increase the amount of DAH that is directed to individual countries to develop their own R&D capabilities—and suggested using Fogarty International Center at the National Institutes of Health (NIH) as a mechanism (Yamey et al., 2017).
Continuing research capacity abroad will allow for the development of more drugs and therapeutics to address diseases that plague people in both the United States and LMICs. As an example, with the recent improvement in diplomatic relations with Cuba, the U.S. Department of Health and Human Services (HHS) and Cuba’s Ministry of Public Health “signed an umbrella accord that promises to make health a cornerstone of the new era of cooperation between the two countries” (Keck, 2016). This concept is
becoming tangible as Cuba has promising treatments that can prevent the need for amputation in patients with diabetes, which have been unavailable to Americans since 2006 due to a U.S. trade embargo. Cuba also has a promising lung cancer vaccine, CIMAvax, with early results suggesting improved survival and quality of life for many patients with non-small cell lung cancer (Keck, 2016). Only since last year, when the United States lifted a medical embargo, has this type of collaboration been allowed. There is much to be learned by each country, and extrapolating this example of partnership across the world, the United States has an opportunity to encourage information sharing and research collaboration among all health and medical researchers.
Developing the R&D Workforce
Often in response to an emergency, the international community deploys personnel from across the world to the emergency site. However, the labor pool that has experience working in the setting of the emergency can be sparse, which occurred during the Ebola response, making it difficult to integrate international responders without local and contextual understanding. As labor cannot be supplied from international sources indefinitely, developing the workforce capacity locally is a much-needed solution.19 U.S.-based institutions can play a role in fostering the development of a strong R&D workforce in LMICs and greater country independence through academic partnerships. The more developed institution provides the laboratory skills and expertise not available at the less developed institution, and the less developed institution contributes the clinical and contextual knowledge (Lucas, 2005). For example, the Academic Model Providing Access to Healthcare (AMPATH), an Indiana University–led initiative, has developed a partnership with Moi University in Kenya to provide 30 percent of medical students with financial aid to increase the number of Kenyan medical professionals (AMPATH, n.d.). This partnership supports the development of a local workforce that will provide health care to their own people, and also creates long-term mentorship opportunities for students and faculty with an interest in global health.20 Programs like this can strengthen the local workforce to operate more independently and become global partners in health with donor countries.
Although these types of partnerships can be costly to U.S.-based academic institutions, additional funding can be leveraged through the Fogarty International Center at NIH and USAID,21 which ensures sustainability of
___________________
19 Personal communication with Daniel Bausch, Tulane University, November 9, 2016.
20 Personal communication with Robert Einterz, AMPATH, December 5, 2016.
21 Personal communication with Troy Moon, Vanderbilt University, November 8, 2016.
current projects and encourages collaborations in future projects. For example, Troy Moon at Vanderbilt University has collaborated with the University of Zambia to train doctorate-level researchers with an NIH-sponsored grant (Snyder, 2015). The goal of the project is to improve partnerships and mentorships among scientists to encourage technical independence among researchers in partnering countries (Snyder, 2015). Through another NIH-sponsored grant, Vanderbilt University is working with Tulane University and the Kenema Government Hospital in Sierra Leone to build capacity and training programs for researchers in the recently Ebola-affected countries so that they can soon write grant proposals and conduct their own clinical trials. In addition to becoming primary researchers, these foreign trainees gain the technical expertise to become advisors to Ministers of Health for aid programs such as The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), and can have much greater success in influencing policy than “outsider” research scientists and diplomats.22 U.S. grants lower the barrier to entry for researchers who hope to collaborate with in-country universities in developing R&D workforce capacity sustainably. This type of capacity-building support through the Fogarty Center is widely used by many universities and provides learning and mentorship opportunities not otherwise available to U.S.-based institutions and depended on by international universities to help build the research component of their country’s health system.
USAID has created multiple programs to leverage investments by U.S. government science agencies to strengthen the research ecosystem in LMICs. For example, the Partnerships for Enhanced Engagement in Research (PEER) funds international scientists who work in partnership with institutions supported by U.S. federal science agency funding (USAID, 2016b). Additionally, USAID’s Higher Education Solutions Network (HESN) leverages the knowledge and assets of seven top U.S. universities to develop technological advancements and spur innovative local solutions by partnering with international academic institutions (USAID, 2016a). A 2017 National Academies report, The Role of Science, Technology, Innovation, and Partnerships in the Future of USAID, called for continued engagement with partner countries through innovative programs, such as PEER and HESN. Lessons should be gleaned and expanded on to sustain collaborations with in-country researchers and institutions (NASEM, 2017b).
With much success, PEPFAR has also explored methods for sustainable workforce training through the Medical Education Partnership Initiative and Nursing Education Partnership Initiative, also supported by the Fogarty International Center and Health Resources and Services Administration (explained in Chapter 4). These initiatives provide students with
___________________
22 Personal communication with Troy Moon, Vanderbilt University, November 8, 2016.
technical and diplomatic expertise and, in a similar way to Moon’s projects, build robust academic partnerships with in-country institutions, creating more formal networks for bidirectional information sharing.
Developing Laboratory Research Capacity
In addition to the workforce capacity needed for R&D in LMICs, building laboratory research capacity is another vital investment category. By increasing the ability to conduct research on endemic diseases, countries will be able to self-sufficiently implement appropriate solutions. Investments toward research capacity date back to 1974 when the World Health Organization (WHO) Special Programme for Research and Training in Tropical Diseases (TDR) was established. Its support has been instrumental for institution strengthening in LMICs. For example, TDR funding was able to create the Malaria Research and Training Center (MRTC) in Mali in 1998, which conducts extensive studies on vector biology, ecology, and genetics (Ogundahunsi et al., 2015). Owing to subsequent funding by USAID and NIH, the MRTC has since expanded and now is paired with multiple laboratories—one of which is a Biosafety Level 3 (BSL-3) lab (NIAID, 2014). To have ongoing benefits, both to the country and to the rest of the world, this laboratory capacity in LMICs must be sustained.
Building laboratory capacity is critical for outbreak response, as the health research system is a vital component of a country’s health system (NASEM, 2017a). As a recent example, when Ebola hit West Africa in late 2013, poor laboratory research capacity hindered efforts to quickly identify the source of the outbreak. The initial investigation conducted by the Ministry of Health in Guinea concluded that the cause was cholera, which impeded a swift and appropriate public health response because of the delay in accurate diagnosis (NASEM, 2017a). Even as CDC and other organizations sought to improve surveillance as the outbreak was declared, the weak laboratory capacity was a major barrier to continued case identification and implementation of proper public health measures. Conversely, the importance of adequate laboratory capacity is illustrated by the African Center of Excellence for Genomics of Infectious Diseases in Nigeria, which was able to accurately diagnose the index case of the Nigerian Ebola outbreak and enable the government to contain the spread before the outbreak became out of control (NASEM, 2017a).
Additionally, the U.S. Department of Defense’s Cooperative Biological Engagement Program (DoD–CBEP) deployed mobile laboratories in Sierra Leone and Guinea during the 2014 Ebola outbreak. In 2015 these laboratories analyzed more than 6,000 samples and quickly detected nearly 80 positive cases of Ebola in these 2 countries. As a step in capacity building, the laboratories increased diagnostic capabilities during the outbreak and
are now being transitioned to the countries’ government to support future outbreak detection and response efforts (GHSA, 2017). Considering these differing examples, there is a clear motivation for the U.S. government to continue its engagement in laboratory capacity-building for outbreak response.
Taken together—both workforce and laboratory capacity are essential to build a strong health system able to respond to infectious disease outbreaks before they lead to catastrophic consequences, and in a cost-effective manner. According to Costello and Zumla (2000), by helping to create an independent researching body in LMICs, researchers are trained in their home countries and are encouraged to stay there because of the existing infrastructure; in-country grants investigate the problems most of interest to the nation’s people; and results have a higher likelihood of leading to policy changes as compared to research conducted by individuals from other, high-income countries (Costello and Zumla, 2000). Similarly, local mental health research conducted in LMICs is found to be much more easily adaptable to solve local problems as compared to research conducted by high-income countries that is based on evidence from high-income countries (Sharan et al., 2007). Past estimates have shown that implementing recommendations for increased research and development capacity would cost $1 billion per year, which is much less than the potential cost of a pandemic (discussed more in Chapter 3) (GHRF Commission, 2016). The committee agrees with the statement made by the Committee on Clinical Trials During the 2014–2015 Ebola Outbreak, that “What seems certain to us is that the actual options are to pay now and prepare in advance, or to pay later when an outbreak occurs, with the likelihood that the cost will be multiple times greater in the latter case” (NASEM, 2017a, p. 185).
SUMMARY AND RECOMMENDATION
Underpinning health innovations is the necessary human and institutional capacity in the United States and globally. Yet the market for many global health products is often too uncertain or risky for private-sector partners to invest their know-how and capital in the development and manufacture of these products (Pedrique et al., 2013). Considering the extremely costly development process and the paucity of products in the pipeline to address neglected diseases, the current trial designs, regulatory approval options, and product supply motivations seem inadequate (Pedrique et al., 2013). Examining each of these areas and the methods and mechanisms currently available can provide an opportunity for the U.S. government to find ways to reduce the costs and timeline to ensure more products make their way into development all the way to approval. Push and pull incentivizing mechanisms can also ensure that appropriate vac-
cines, therapeutics, diagnostics, and devices are in the development pipeline for global health priorities with weak markets, including neglected diseases (Dimitri, 2012). In the absence of these mechanisms, the United States and other governments risk spending far more as they work to prevent, respond to, and treat diseases using suboptimal tools.
To complement the development of safe and efficacious products requires R&D capacity in countries where outbreaks begin and disease burdens are high (NASEM, 2017a). Although there are some notable exceptions, the necessary research capacity is weak in many such countries, making it difficult to conduct clinical and field trials, becoming even more of a costly and chaotic undertaking during a public health emergency (NASEM, 2017a). By examining the stages along the pharmaceutical development value chain, the U.S. government has an opportunity to identify specific actions that can be taken to streamline processes, reduce costs, and create more appropriate incentives to enable industry, academia, and others to contribute to developing the priority innovations for global health. This could be accomplished through an interagency working group, but would require dedicated commitment from all involved agencies, as well as coordination across the public and private sectors.
Conclusion: Despite substantial efforts from the U.S. government and other global health players, the pipeline of innovations for addressing persistent global health threats is inadequate. The U.S. government has the ability to design and expand push and pull mechanisms that can catalyze industry, academia, and others to develop, license, and introduce needed technologies and avoid the catastrophic loss of life and economic burdens that result from the lack of these innovations.
Conclusion: Creating the capacity for low- and middle-income countries to conduct clinical trials where the burden of disease is highest, using their own workforces and facilities, is both more efficient and more cost-effective than relying on donor nations for these efforts. Creating this capacity will require investing in laboratory capacity, and an appropriately trained research-competent workforce.
Recommendation 10: Accelerate the Development of Medical Products
U.S. government agencies should invest in a targeted effort to reduce the costs and risks of developing, licensing, and introducing vaccines, therapeutics, diagnostics, and devices needed to address global health priorities by enabling innovative trial design ap-
proaches, streamlining regulation, ensuring production capacity, creating market incentives, and building international capacity for research and development. This effort should include the following:
- Enabling innovative approaches for trial design: The U.S. Food and Drug Administration (FDA), the Biomedical Advanced Research and Development Authority (BARDA), the U.S. Department of Defense (DoD), and the National Institutes of Health (NIH) should actively encourage public- and private-sector product development efforts using innovative product development approaches, including platform studies, adaptive trial designs, pragmatic trials, and improved biomarker development. BARDA should assess expanding its list of priority products for codevelopment with industry, taking into account global health priorities.
- Streamlining regulation: FDA should receive adequate resources to improve the tropical disease priority review voucher program and should assess the application of the provisions outlined in the Generating Antibiotic Incentives Now Act to neglected tropical diseases beyond those on the qualified pathogen list.
- Ensuring production capacity: BARDA should increase its efforts to promote adequate global manufacturing capacity for priority technologies (e.g., Centers for Innovation in Advanced Development and Manufacturing).
- Creating market incentives: The U.S. government should invest in generating and disseminating accurate and transparent market estimates and should use the purchasing power of U.S. government agencies and global partnerships such as Gavi, the Vaccine Alliance, and the Global Fund to Fight AIDS, Tuberculosis and Malaria, as well as such creative financing mechanisms as volume guarantees, to reduce market uncertainty for priority health products.
- Building international capacity for research and development: The U.S. Centers for Disease Control and Prevention, NIH, and DoD should increase the number of people and institutions in partner countries capable of conducting clinical trials for global health priorities (e.g., through funding partnerships with academic institutions). This effort should encompass providing support for sustainable core capacities such as drug, vaccine, and diagnostic research capabilities and building the skills of principal investigators.
ENABLING INNOVATION: DIGITAL HEALTH
Telecommunications and wireless multimedia have contributed to significant advances in global health in recent years. By taking advantage of wireless network penetration in LMICs, digital health technology has bypassed deficiencies found in traditional “brick-and-mortar” health care systems and provides a myriad of solutions ranging from education for new and expectant mothers through the Mobile Alliance for Maternal Action (MAMA)23 (MAMA, 2013) to reminders for adherence to chronic disease management (Hamine et al., 2015). Although there have been many successful applications of digital health tools around the world, they have typically employed a shortsighted approach and a narrow perspective (Mehl and Labrique, 2014). While this was likely done to create a simpler process for faster and easier results, the current models fail to prevent unnecessary duplication and address broader health system needs. Finally, both U.S. global health programs and countries around the world have seen much progress in improved health outcomes stemming from technological advances and digital health tools. Although they will continue to face up-front costs of establishing the digital infrastructure and training a workforce to utilize the digital platforms, the long-term commitment to their use has the potential to reduce costs and improve efficiency of health care programs (MoH, n.d.; WHO, 2009). The committee believes that now is a time to pause, review all of the progress made and lessons learned, and chart a strategic path forward in digital global health, with an emphasis on systematic approaches, multidisciplinary public–private collaboration, and country ownership.
Applications of Digital Global Health
Many U.S. government agencies and their implementing partners, as well as private companies and other national governments, have employed digital health technology to facilitate elements of global health, whether for disease surveillance, patient tracking, inventory maintenance, or telemedicine. Though the applications of digital health technology are expansive, the committee has categorized them into three broad application areas for discussion: data systems creation, health care service optimization, and
___________________
23 The Mobile Alliance for Maternal Action (MAMA) was launched in 2011 as a public–private partnership between USAID, Johnson & Johnson, the UN Foundation, and BabyCenter with the goal of catalyzing a global community to deliver vital health information to new and expectant mothers and their families through mobile phones. BabyCenter created a core set of messages for MAMA that is timed and targeted to pregnant women and infants through 3 years old. Over just 5 years the program reached more than 7.5 million women and families (MAMA, 2013).
research efficiency, explored below, with examples of each highlighted in Box 7-2.
Data Systems
A hallmark of digital health utilization has been its support of data systems in developing countries. Health information in developing countries has long been captured on paper, which must then be physically transported, and the data manually aggregated and reentered, then extracted for review by high-level officials (Mehl and Labrique, 2014). This includes routine health facility data and acute event data, such as disease outbreaks. Understandably, delays and errors are commonplace—creating inefficiencies in a health system. Digital health tools have revolutionized this process, allowing for data collection, reporting, and action to occur much more rapidly, and with fewer opportunities to introduce error (RTI, n.d.). Box 7-2 illustrates an example of data systems improvement in LMICs through Coconut Surveillance.
Health Care Service Optimization
Access to quality health care in LMICs is often hindered by workforce shortages and poor infrastructure (MoH, n.d.). Though long-term, complete solutions to both of these issues requires the scale-up of human resources and creation of adequate amounts and types of clinics, digital health tools have been able to provide effective interim solutions. The most well-known form of digital health used to optimize service delivery is telemedicine, an effective means of providing access to more specialized care to remote regions (or those lacking high-skilled health care workers) in a cost-effective manner (Green, 2016; WHO, 2009). Other widely utilized modalities of digital health in this area include SMS reminders and mobile protocols (Hamine et al., 2015; MAMA, 2013).24 As a result, while the longer-term goal of increasing the number of high-level medical providers will still require lengthy timelines, patients can access high-level care now, through leveraging these technology tools. Box 7-2 illustrates an example of this type of innovation through Operation ASHA.
Research Efficiency
Biomedical research and clinical trials—especially for infectious diseases endemic to certain areas in LMICs, such as Lassa Fever, Ebola, or
___________________
24 Mobile Protocols: These tools enable health care providers to efficiently deliver health solutions, such as daily nutritional supplement reminders or dosage reminders.
Zika virus, depend on robust and capable sites in these same regions. Recruitment for trials is an arduous process as they require a large group of patients to comprise the study sample (Zimmer et al., 2010). Leaning on technology, databases of patients with particular diseases, or disease registries, have been positioned as a critical prelude to clinical trials and can help improve recruitment, identity patient cohorts, provide data for natural history studies, and stimulate new research (Groft, 2014). Furthermore, using digital health tools can also facilitate in-country trials. Typically, patients need to continuously return to a clinical trial site for periodic data collection, but this can be a barrier in remote or resource-poor areas where travel is lengthy and expensive. Having remote options for check-in and periodic follow-up can remove this barrier (Seguine, 2016). Additionally, having a disease registry in a city or country can allow for faster start-up for other studies on different diseases, making that area more attractive to researchers. See Box 7-2 for an example of a digital health solution for clinical trials.
A Need for a Paradigm Shift
The tremendous value and corresponding excitement that digital health provides has come at a cost, as the proliferation of interest and the variety of stakeholders involved has created a fragmented approach to the use of digital health tools in many countries. In fact, in 2012, Uganda issued a temporary moratorium on digital health pilots because its health system became overrun with them (Green, 2016). Aid programs, nongovernmental organizations, and private companies often create individual, disease-focused tools that fail to be interoperable with one another and are duplicative to in-country systems. Therefore, despite the large investment in digital health applications, these parallel structures often lead to inefficiencies because they cannot be used for other diseases or health priorities. Multiple donors and organizations may be funding and operating multiple surveillance systems for different diseases in the same country, instead of aligning themselves into one interoperable system, integrated with existing national health system infrastructure. The benefit of digital health applications notwithstanding, there is a clear need for a paradigm shift in digital health infrastructure investments. The global health community and U.S. global health programs need to move away from the current practice of single application solutions to a more strategic approach that acts holistically with both current country priorities and long-term goals (Mehl and Labrique, 2014). By better coordinating the development of digital health applications, stakeholders involved in digital health can reduce duplication and ensure that the platforms are more aligned with those priorities and goals.
The committee envisions not only digital tools for real-time collection of health and health-related data from anywhere in the world, but also connected systems that ensure the data can be aggregated and shared (when appropriate), instantly analyzed and intuitively visualized so that health professionals and policy decision makers at all levels—community, district, country, and global—can take action. The committee sees this occurring through the development of digital health platforms within countries. The hallmark of a digital health platform is that it must be adaptable to local health needs. However, it is neither efficient nor practical for each program or country to invest in developing a full suite of needed tools to support their health system. Therefore, a core characteristic of a common digital health platform would be that of an open innovation platform that holds and facilitates access to health care and health-related data for a multitude of applications. By building a digital health platform that is modular, countries can attract and engage third parties (including the private sector) to develop useful applications that can be customized to their unique context and then integrated sustainably. While such a platform would be useful for day-to-day health care delivery and operations, it would also revolutionize how surveillance and response for public health threats can be managed within and between countries. The committee sees a digital health platform revolutionizing the three broad areas of digital health: data systems, health care service optimization, and research efficiency, as described in the following sections.
Data Systems
Though some systems can collect data in remote areas and others offer near real-time data streams, they do not interact with each other and the data cannot be easily aggregated. This severely limits the potential of using such data to optimize health care service delivery or surveillance of potential emerging global health threats. The committee therefore advocates for a common digital health platform architecture that can create interoperability across existing or future data systems, but would not require each user to adopt a prescribed solution. Instead, data could be collected across disparate sites and systems and be aggregated for everyday health care needs, including delivery of services, payments for services, and global health threats. The digital financial sector has already made key advances in this area in LMICs, as evidenced by the success of m-Pesa25 or other
___________________
25 m-Pesa is a mobile money transferring system in Kenya that operates through users’ cell phones. Safaricom, the cellular telecommunications company that started m-Pesa, generates $250,000,000 per year in revenues from m-Pesa alone (CBS News, 2015). For more information, see https://www.safaricom.co.ke/personal/m-pesa (accessed April 7, 2017).
electronic payment systems. The digital health sector can learn from these innovations as related to their interoperability and privacy and to avoid developing them from scratch.
Health Care Service Optimization
Though digital health tools have provided numerous solutions in terms of augmenting health care workforces, a digital health platform can maximize this capacity. Enhanced access to data and information through a common digital platform will improve communication between patients and health care workers across the care continuum, as well as increase the productivity and quality of the workforce. While this does not replace the longer-term need to educate and train a larger workforce, these technology capabilities can address the short-term needs and expand the scope of a health workforce to match the demand for more integrated health services.
Research Efficiency
The digitalization of clinical trials and general global health research can reduce the waste of duplicative technology in global health and allow for streamlined and remote collection of data, thereby resulting in potential cost savings. A digital health platform can improve on the efficiencies already gained through facilitation of data-sharing among investigators, potentially allowing for novel research inquiry. For example, if two similar clinical trials are occurring simultaneously, a digital health platform could enable controlled sharing of data (within the scope of research ethics) to investigate another separate study question. Additionally, a common platform would likely allow for more targeted studies and faster recruitment, as country disease trends and relevant health information would be aggregated from multiple data streams to highlight burdens and gaps in existing care and tools.
Looking Forward: A Role for the U.S. Government in the World of Digital Global Health
As many partners around the globe, both public and private, have been supportive and involved with the creation of digital health tools, a need emerged for standardization and coordination as well as assistance to move from policy to implementation. To help bring clarity and coherence to governments on digital technology investment for health, WHO and partner organizations are developing a Global Digital Health Index, a tool designed to track, monitor, and evaluate the applicability of any digital technology
solution for a community’s or country’s health (Mechael and Kay, 2016). The Global Digital Health Index is further described in Box 7-3.
In addition to a global index, there is also increasing recognition of the importance of frameworks to help prioritize investments in digital health technology and identify opportunities for collaboration and integration with local health systems (Mehl and Labrique, 2014). Many national governments have started to adopt national e-health strategies, including Ghana (MoH, n.d.), Nigeria (MoH, 2015), and Tanzania (MoHSW, 2013). The common aspects of these frameworks include an efficient use of resources, improved data and information flow, and reduced fragmentation (HealthEnabled, n.d.-a). Donors often lack methods for the coordination and alignment of funding of digital health investments, which has resulted in fragmentation and an inability to scale. The national e-health strategies that are emerging signal a shift in thinking and open the door for better aid coordination driven by country priorities.
As the global community moves toward a more harmonized approach to digital technology application, the United States has an opportunity to re-assess its current strategy and direct resources and expertise toward the growing momentum for global alignment in this space. The United States can likely see greater returns on investment through coordinating U.S. digital health investments with the needs of the country, and where possible assisting countries to develop their e-health strategies. Furthermore, this alignment in partnership could incentivize local government toward
co-investment, thus facilitating better transition to country ownership and sustainability.
In 2015, 25 percent of Africa and 58 percent of Asia had an internet connection (Poushter, 2016), with this number expected to continue increasing. Additionally, many innovations and services have been created even without internet access, such as through the massive proliferation of cellular networks using simple mobile phones (e.g., m-Pesa, described previously). To facilitate further growth in connectivity, the United States recently passed, with bipartisan support, H.R. 600, the Digital Global Access Policy Act. This bill encourages efforts in developing countries to improve internet access to spur economic growth and improve health, in addition to ensuring effective use of U.S. foreign assistance.26 The act specifically calls for USAID to integrate efforts to expand internet access into education, development, and economic growth programs, as well as use of information and communications technologies for disaster relief. To do so, the Act calls for the use of the build-once principle, which hopes to lower the cost of infrastructure development by minimizing the number and scale of excavation activities when installing telecommunications infrastructure. The committee sees a strong opportunity for the United States to build on this goal and rethink its global health strategies to join the global momentum toward harmonization of digital health approaches.
SUMMARY AND RECOMMENDATION
Decreases in the costs and increased demand of mobile technology have allowed for the integration of successful digital health efforts in the United States and around the globe (Mehl and Labrique, 2014; Steinhubl et al., 2013). However, many of these investments in global health have been siloed and shortsighted in their approach, often focusing on single diseases or sectors and missing opportunities to develop a sustainable, integrated platform (Mehl and Labrique, 2014). Prioritizing health systems innovation through technical assistance and public–private partnerships in digital health can lead to better care and service delivery at lower cost, especially in situations in which already established technology is utilized (Mehl and Labrique, 2014; WHO, 2009). With growing mobile and internet connectivity worldwide and rapid advances in information and communication technology, the United States has an opportunity to better integrate digital health efforts in countries to reduce fragmentation and improve coordination and efficiency (Mehl and Labrique, 2014; Poushter, 2016).
___________________
26 Digital Global Access Policy Act of 2017, H.R. 600, 115th Congress.
Conclusion: Countries need cross-cutting digital health platforms that are adaptable to local requirements and sovereignty, and can provide real-time data and analytic insights to inform health-related decisions. Such platforms need to address each country’s health care priorities during steady-state times, thereby incentivizing country co-investment and ownership, while also serving as a resilient system for facilitating controlled sharing of data across countries to enhance surveillance, coordinate responses, and deliver services during an emergency.
Conclusion: Achieving the global health goals outlined in this report will require that U.S. global health programs leverage the expertise and resources of the U.S. government in digital health and the strong U.S. information and communication technology industry through public–private partnerships and smart financing strategies (see Chapter 8).
Recommendation 11: Improve Digital Health Infrastructure
Relevant agencies of the U.S. government should convene an international group of public and private stakeholders to create a common digital health framework that addresses country-level needs ranging from integrated care to research and development.
- The U.S. Agency for International Development (USAID) and the U.S. Department of State should incentivize and support countries in building interoperable digital health platforms that can efficiently collect and use health data and analytic insights to enable the delivery of integrated services within a country.
- USAID’s Global Development Laboratory should provide technical assistance to countries in the development and implementation of interoperable digital health platforms co-funded by the country and adaptable to local requirements.
- U.S. agencies should expand on the “build-once” principle of the Digital Global Access Policy Act and align U.S. funding in digital health by multiple agencies to reduce fragmentation and duplication, as well as maximize the effectiveness of investments. The provision of this funding should employ methods that reflect smart financing strategies to leverage private industry and country cofinancing (see Recommendation 13).
REFERENCES
AMPATH (Academic Model for the Prevention and Treatment of HIV). n.d. Mwangaza scholarships. http://ampathkenya.org/our-programs/education-partnerships/mwangaza-scholarships (accessed February 13, 2017).
Anderson, M. L., J. Griffin, S. F. Goldkind, E. P. Zeitler, L. Wing, S. M. Al-Khatib, and R. E. Sherman. 2015. The Food and Drug Administration and pragmatic clinical trials of marketed medical products. Clinical Trials 12(5):511-519.
Aronson, J. K. 2005. Biomarkers and surrogate endpoints. British Journal of Clinical Pharmacology 59(5):491-494.
Aurora, P., M. Romine, and G. Daniel. 2016. Are Priority Review Vouchers the answer to incentivize drug development? Not so fast. http://healthaffairs.org/blog/2016/06/15/are-priority-review-vouchers-the-answer-to-incentivize-drug-development-not-so-fast (accessed March 18, 2017).
BCG (Boston Consulting Group), Öpp Deutschland AG, and Technische Universität Berlin. 2015. Breaking through the wall: Enhancing research and development of antibiotics in science and industry. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/G/G7/Qualitaetswettbewerb_Gesundheitssystem_Whitepaper_2015-10-02.pdf (accessed January 10, 2017).
Bhatt, D. L., and C. Mehta. 2016. Adaptive designs for clinical trials. The New England Journal of Medicine 375(1):65-74.
Brennan, Z. 2016a. House E&C Committee clears new Priority Review Voucher program. http://www.raps.org/Regulatory-Focus/News/2016/07/14/25336/House-EC-Committee-Clears-New-Priority-Review-Voucher-Program (accessed February 15, 2017).
Brennan, Z. 2016b. Regulatory explainer: 21st Century Cures redux and what it will mean for FDA. http://raps.org/Regulatory-Focus/News/2016/11/28/26242/Regulatory-Explainer-21st-Century-Cures-Redux-and-What-it-Will-Mean-for-FDA (accessed March 18, 2017).
Brennan, Z. 2017. Sarepta sells Priority Review Voucher for $125m to Gilead. http://www.raps.org/Regulatory-Focus/News/2017/02/21/26898/Sarepta-Sells-Priority-Review-Voucher-for-125M-to-Gilead (accessed March 8, 2017).
Bright, R. 2013. “BARDA International Influenza Vaccine Manufacturing Capacity Building Program.” Presentation at 6th Meeting with International Partners on Prospects for Influenza Vaccine Technology Transfer to Developing Country Vaccine Manufacturers. Dubai. March 18-19, 2013. http://www.who.int/phi/Day1_3_Bright_BARDA_PM_Dubai2013.pdf (accessed May 4, 2017).
CBS (Columbia Broadcasting System) News. 2015. Want to text money? Kenya’s been doing it for years. http://www.cbsnews.com/news/want-to-text-money-kenya-has-been-doing-it-for-years (accessed March 15, 2017).
Chow, S.-C., and R. Corey. 2011. Benefits, challenges and obstacles of adaptive clinical trial designs. Orphanet Journal of Rare Diseases 6(1):79-88.
Ciociola, A. A., L. B. Cohen, and P. Kulkarni. 2014. How drugs are developed and approved by the FDA: Current process and future directions. American Journal of Gastroenterology 109(5):620-623.
Clinical Ink. 2015. Introduction to SureSource. http://www.clinicalink.com/wp-content/uploads/2015/04/Clinical-Ink_SureSource-Overview-Final_042815.pdf (accessed January 16, 2017).
Costello, A., and A. Zumla. 2000. Moving to research partnerships in developing countries. BMJ: British Medical Journal 321(7264):827-829.
Danzis, S. D. 2003. The Hatch-Waxman act: History, structure, and legacy. Antitrust Law Journal 71(2):585-608.
DiMasi, J. A., H. G. Grabowski, and R. W. Hansen. 2016. Innovation in the pharmaceutical industry: New estimates of R&D costs. Journal of Health Economics 47:20-33.
Dimitri, N. 2012. R&D incentives for neglected diseases. PLOS ONE 7(12):e50835.
FDA (U.S. Food and Drug Administration). 2004. Innovation and stagnation: Challenges and opportuinty on the critical path to new medical products. Silver Spring, MD: U.S. Food and Drug Administration, U.S. Health and Human Resources.
FDA. 2010. Guidance for industry: Adaptive design clinical trials for drugs and biologics. Silver Spring, MD: U.S. Food and Drug Administration, U.S. Health and Human Resources.
FDA. 2014a. Breakthrough therapy. http://www.fda.gov/ForPatients/Approvals/Fast/ucm405397.htm (accessed February 13, 2017).
FDA. 2014b. Fast track. http://www.fda.gov/ForPatients/Approvals/Fast/ucm405399.htm (accessed February 13, 2017).
FDA. 2014c. Priority review. http://www.fda.gov/ForPatients/Approvals/Fast/ucm405405.htm (accessed February 13, 2017).
FDA. 2016a. Adaptive designs for medical device clinical studies: Guidance for industry and Food and Drug Administration staff. https://www.fda.gov/downloads/medicaldevices/deviceregulationandguidance/guidancedocuments/ucm446729.pdf (accessed April 25, 2017).
FDA. 2016b. Designating an orphan product: Drugs and biological products. http://www.fda.gov/ForIndustry/DevelopingProductsforRareDiseasesConditions/HowtoapplyforOrphanProductDesignation/default.htm (accessed February 13, 2017).
FDA. 2017. Search orphan drug designations and approvals. Silver Spring, MD: U.S. Food and Drug Administration, U.S. Health and Human Resources.
Ford, I., and J. Norrie. 2016. Pragmatic trials. New England Journal of Medicine 375(5): 454-463.
Franco, P. 2013. Orphan drugs: The regulatory environment. Drug Discovery Today 18(3-4): 163-172.
Gaffney, A., M. Mezher, and Z. Brennan. 2016. Regulatory explainer: Everything you need to know about FDA’s Priority Review Vouchers. http://www.raps.org/Regulatory-Focus/News/2015/07/02/21722/Regulatory-Explainer-Everything-You-Need-to-Know-About-FDA%E2%80%99s-Priority-Review-Vouchers/ (accessed February 13, 2017).
GHRF Commission (Commission on a Global Health Risk Framework for the Future). 2016. The neglected dimension of global security: A framework to counter infectious disease crises. doi: https://doi.org/10.17226/21891.
GHSA (Global Health Security Agenda). 2017. Advancing the Global Health Security Agenda: Progress and early impact from U.S. investment. Washington, DC: Global Health Security Agenda.
Green, A. 2016. A new era in digital health. https://www.devex.com/news/a-new-era-in-digital-health-88327 (accessed December 15, 2016).
Groft, S. 2014. Patient registries as a prelude to clinical trials and post-approval studies. http://www.fda.gov/downloads/MedicalDevices/NewsEvents/WorkshopsConferences/UCM381523.pdf (accessed February 13, 2017).
Hamine, S., E. Gerth-Guyette, D. Faulx, B. B. Green, and A. S. Ginsburg. 2015. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: A systematic review. Journal of Medical Internet Research 17(2):e52.
HealthEnabled. n.d.-a. Country dashboards. http://healthenabled.org/index.php/healthe-africa/country-dashboards/ (accessed December 15, 2016).
HealthEnabled. n.d.-b. Global Digital Health Index. http://www.healthenabled.org/index.php/our-work/digitalhealthindex (accessed December 15, 2016).
HHS (U.S. Department of Health and Human Services). 2017. Department of Health and Human Services Centers for Innovation in Advanced Development and Manufacturing (HHS-CIDAM). https://www.medicalcountermeasures.gov/barda/core-services/ciadm.aspx (accessed February 13, 2017).
Hills, B., and B. Zegarelli. 2017. 21st Century Cures Act requires FDA to expand the role of real world evidence. https://www.martindale.com/health-care-law/article_Mintz-Levin-Cohn-Ferris-Glovsky-Popeo-PC_2239128.htm (accessed April 10, 2017).
IOM (Institute of Medicine). 1997. America’s vital interest in global health: Protecting our people, enhancing our economy, and advancing our international interests. Washington, DC: National Academy Press.
Keck, C. W. 2016. The United States and Cuba—turning enemies into partners for health. New England Journal of Medicine 375(16):1507-1509.
Kesselheim, A. S. 2008. Drug development for neglected diseases—the trouble with FDA review vouchers. New England Journal of Medicine 359(19):1981-1983.
Lucas, A. O. 2005. International collaboration in health research. Bulletin of the World Health Organization 82(7).
Lyon, K. 2015. ZMapp is granted orphan medicinal product designation by the EMA. In Status May Enable Faster Approval of ZMapp. San Diego, CA: LeafBio.
Mahajan, R., and K. Gupta. 2010. Adaptive design clinical trials: Methodology, challenges and prospect. Indian Journal of Pharmacology 42(4):201-207.
MAMA (Mobile Alliance for Maternal Action). 2013. Mobile Alliance for Maternal Action (MAMA). http://www.mobilemamaalliance.org (accessed February 13, 2017).
McLean, K. A., S. Goldin, C. Nannei, E. Sparrow, and G. Torelli. 2016. The 2015 global production capacity of seasonal and pandemic influenza vaccine. Vaccine 34(45):5410-5413.
Mechael, P., and M. Kay. 2016. Unlocking the potential of digital health. https://www.devex.com/news/unlocking-the-potential-of-digital-health-88274 (accessed December 15, 2016).
Mehl, G., and A. Labrique. 2014. Prioritizing integrated mHealth strategies for universal health coverage. Science 345(6202):1284.
Merrill, R. A. 1996. The architecture of government regulation of medical products. Virginia Law Review 82(8):1753-1866.
Millennium Project. 2006. What they are. Washington, DC: The United Nations Millennium Project. http://www.unmillenniumproject.org/goals (accessed March 10, 2017).
MoH (Nigerian Ministry of Health). 2015. National health ICT stratgic framework. Abuja, Nigeria: Federal Ministry of Health. http://www.uspf.gov.ng/images/files-temp/National_Health_ICT_Strategic_Framework2015-2020-DRAFT.pdf (accessed January 5, 2017).
MoH (Ghana Ministry of Health). n.d. Ghana e-Health strategy. Accra, Ghana: Ministry of Health. https://www.isfteh.org/files/media/ghana_national_ehealth_strategy.pdf (accessed January 5, 2017)
MoHSW (Ministry of Health and Social Welfare). 2013. Tanzania national eHealth strategy 2012-2018. Dar es Salaam, Tanzania: Ministry of Health and Social Welfare. http://www.who.int/goe/policies/countries/tza_ehealth.pdf (accessed January 5, 2017).
Moon, S., E. Jambert, M. Childs, and T. von Schoen-Angerer. 2011. A win-win solution?: A critical analysis of tiered pricing to improve access to medicines in developing countries. Globalization and Health 7(1):39.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2017a. Integrating clinical research into epidemic response: The Ebola experience. Washington, DC: The National Academies Press.
NASEM. 2017b. The role of science, technology, innovation, and partnerships in the future of USAID. Washington, DC: The National Academies Press.
NCI (National Cancer Institute). n.d. NCI Dictionary of Cancer Terms. https://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=752982 (accessed April 24, 2017).
NIAID (National Institute of Allergy and Infectious Diseases). 2014. Mali ICER program. https://www.niaid.nih.gov/about/mali-icer-program (accessed April 10, 2017).
NIAID. 2015. What is a vaccine adjuvant? https://www.niaid.nih.gov/research/what-vaccine-adjuvant (accessed April 24, 2017).
NLM (National Library of Medicine). 2017. Glossary of common site terms: Clinicaltrials.gov https://clinicaltrials.gov/ct2/about-studies/glossary#C (accessed April 24, 2017).
Ogundahunsi, O. A. T., M. Vahedi, E. M. Kamau, G. Aslanyan, R. F. Terry, F. Zicker, and P. Launois. 2015. Strengthening research capacity—TDR’s evolving experience in low- and middle-income countries. PLOS Neglected Tropical Diseases 9(1):e3380.
Operation ASHA. 2016. Ecompliance biometric tracking system. http://www.opasha.org/2016/09/20/ecompliance-biometric-tracking-system (accessed April 10, 2017).
Pammolli, F., L. Magazzini, and M. Riccaboni. 2011. The productivity crisis in pharmaceutical R&D. Nature Reviews Drug Discovery 10(6):428-438.
Patsopoulos, N. A. 2011. A pragmatic view on pragmatic trials. Dialogues in Clinical Neuroscience 13(2):217-224.
PCAST (President’s Council of Advisors on Science and Technology). 2014. Report to the president on combating antibiotic resistance. Washington, DC: Executive Office of the President.
Pedrique, B., N. Strub-Wourgaft, C. Some, P. Olliaro, P. Trouiller, N. Ford, B. Pécoul, and J.-H. Bradol. 2013. The drug and vaccine landscape for neglected diseases (2000-11): A systematic assessment. The Lancet Global Health 1(6):e371-e379.
Pew Charitable Trusts. 2013. Gain: How a new law is stimulating the development of antibiotics. http://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2013/11/07/gain-how-a-new-law-is-stimulating-the-development-of-antibiotics (accessed February 13, 2017).
Pew Charitable Trusts. 2016. Antibiotics currently in clinical development. http://www.pewtrusts.org/~/media/assets/2016/12/antibiotics_datatable_201612.pdf?la=en (accessed February 13, 2017).
Poushter, J. 2016. Smarthphone ownership and internet usage continues to climb in emerging economies—but advanced economies still have higher rates of use. Washington, DC: Pew Research Center.
Radke, J. 2014. Ebola drug given orphan designation—company seeking partners to develop. RareDiseaseReport. http://www.raredr.com/news/Another-Ebola-Drug-Orphan-Designation (accessed March 8, 2017).
Renwick, M. J., D. M. Brogan, and E. Mossialos. 2016. A systematic review and critical assessment of incentive strategies for discovery and development of novel antibiotics. Journal of Antibiotics 69(2):73-88.
Review on Antimicrobial Resistance. 2015. Securing new drugs for future generations: The pipeline of antibiotics. https://amr-review.org/sites/default/files/SECURING%20NEW%20DRUGS%20FOR%20FUTURE%20GENERATIONS%20FINAL%20WEB_0.pdf (accessed December 20, 2017).
RTI (RTI International). n.d. Coconut surveillance: Open source mobile tool designed to take on malaria, other infectious diseases. https://www.rti.org/impact/coconut-surveillance (accessed February 13, 2017).
Sachs-Barrable, K., J. Conway, P. Gershkovich, F. Ibrahim, and K. M. Wasan. 2014. The use of the United States FDA programs as a strategy to advance the development of drug products for neglected tropical diseases. Drug Development and Industrial Pharmacy 40(11):1429-1434.
Saville, B. R., and S. M. Berry. 2016. Efficiencies of platform clinical trials: A vision of the future. Clinical Trials 13(3):358-366.
Seguine, E. 2016. Innovation to build capacity and improve health. Paper read at Global Health and the Future of the United States: A Changing Landscape of Global Health, Washington, DC. http://www.nationalacademies.org/hmd/~/media/Files/Activity%20Files/Global/USandGlobalHealth/Global-Health-and-The-Future-of-the-US/Meeting-2-Files/Ed-Seguine-Presentation.pdf (accessed December 12, 2016).
Sharan, P., I. Levav, S. Olifson, A. de Francisco, and S. Saxena. 2007. Research capacity for mental health in low- and middle-income countries: Results of a mapping project. Geneva, Switzerland: World Health Organization & Global Forum for Health Research.
Sherman, R. E., S. A. Anderson, G. J. Dal Pan, G. W. Gray, T. Gross, N. L. Hunter, L. LaVange, D. Marinac-Dabic, P. W. Marks, M. A. Robb, J. Shuren, R. Temple, J. Woodcock, L. Q. Yue, and R. M. Califf. 2016. Real-world evidence—what is it and what can it tell us? New England Journal of Medicine 375(23):2293-2297.
Snyder, B. 2015. Grants bolster HIV-focused research capacity. https://news.vanderbilt.edu/2015/08/20/grants-bolster-hiv-focused-research-capacity (accessed February 13, 2017).
Steinhubl, S., E. Muse, and E. Topol. 2013. Can mobile health technologies transform health care? JAMA 310(22):2395-2396. doi:10.1001/jama.2013.281078.
Strimbu, K., and J. A. Tavel. 2010. What are biomarkers? Current opinion in HIV and AIDS 5(6):463-466.
Sugarman, J., and R. M. Califf. 2014. Ethics and regulatory complexities for pragmatic clinical trials. JAMA 311(23):2381-2382.
Thaul, S. 2012. How the FDA approves drugs and regulates their safety and effectiveness. Washington, DC: Congressional Research Service.
Thomas, D. W., J. Burns, J. Audette, A. Carroll, C. Dow-Hygelund, and M. Hay. 2015. Clinical development success rates 2006-2015. Washington, DC: BIO, Biomedtracker, Amplion.
Trusheim, M., A. Shrier, Z. Antonijevic,, Beckman, R. Campbell, C. Chen, K. Flaherty, J. Loewy, D. Lacombe, S, Madhavan, H. Selker, and L. Esserman. 2016. PIPELINEs: Creating comparable clinical knowledge efficiently by linking trial platforms. Clinical. Pharmacology and Therapeutics, 100:713-729.
USAID (U.S. Agency for International Development). 2013. Development innovation ventures: Investment portfolio. Washington, DC: United States Agency for International Development.
USAID. 2014. Healthy markets for global health: A market shaping primer. Washington, DC: Center for Accelerating Innovation and Impact, United States Agency for International Development.
USAID. 2016a. About the Higher Education Solutions Network. https://www.usaid.gov/hesn/about (accessed February 13, 2017).
USAID. 2016b. Partnerships for Enhanced Engagement in Research (PEER). https://www.usaid.gov/what-we-do/GlobalDevLab/international-research-science-programs/peer (accessed April 10, 2017).
USAID. 2017. CII 2017 impact brief. Washington, DC: Center for Accelerating Innovation and Impact, United States Agency for International Development.
Villa, S., A. Compagni, and M. R. Reich. 2009. Orphan drug legislation: Lessons for neglected tropical diseases. International Journal of Health Planning and Management 24(1):27-42.
Warshaw, R. 2015. The economics of orphan drugs: The effectiveness of Priority Review Vouchers on the development of drugs to combat neglected tropical diseases. Philadelphia: University of Pennsylvania.
WHO (World Health Organization). 2001. Biomarkers in risk assessment: Validity and validation. http://www.inchem.org/documents/ehc/ehc/ehc222.htm (accessed March 10, 2017).
WHO. 2009. Telemedicine: Opportunities and developments in member states: Report on the second global survey on eHealth. Geneva, Switzerland: World Health Organization.
Williams, C. T. 2016. Food and Drug Administration drug approval process: A history and overview. Nursing Clinics of North America 51(1):1-11.
Woodcock, J., and R. Woosley. 2008. The FDA Critical Path Initiative and its influence on new drug development. Annual Review of Medicine 59:1-12.
Yamey, G., A. Thoumi, J. Gonzalez-Smith, C. Binanay, I. Bharali, Z. Johar, D. Ridley, and N. Chapman. 2017. Strengthening the United States government’s role in research and development for global health. Durham, NC: Duke Global Health Institute, Duke Margolis Center for Health Policy.
Zimmer, L. O., T. L. Nolen, S. Pramanpol, D. Wallace, M. E. Walker, P. Pappas, and P. Chetchotisakd. 2010. International collaboration between US and Thailand on a clinical trial of treatment for HIV-associated cryptococcal meningitis. Contemporary Clinical Trials 31(1):34-43.
Zwarenstein, M., and A. Oxman. 2006. Why are so few randomized trials useful, and what can we do about it? Journal of Clinical Epidemiology 59(11):1125-1126.




































