3
Infectious Diseases, Pandemic Influenza, and Antimicrobial Resistance: Global Health Security Is National Security
National security is not just about protection from state and nonstate actors, but also encompasses protection from emerging infectious diseases and other health outcomes that can threaten the nation’s economic vitality and its very way of life. This point is demonstrated by the Director of National Intelligence’s inclusion of the threat of pandemics and other health hazards in the U.S. intelligence community’s worldwide threat assessment every year since 2009,1 including 2016, the most recent year in which that report was available (Clapper, 2016). The U.S. Army recently estimated that if a severe infectious disease pandemic were to occur today, the number of U.S. fatalities could be nearly double the total number of battlefield fatalities sustained in all U.S. wars since the American Revolution (GAO, 2017). In the last 13 years alone, the world has seen many infectious disease outbreaks—such as sudden acute respiratory syndrome (SARS), influenza A virus subtype H1N1, Middle East respiratory syndrome coronavirus (MERS-CoV), Ebola, and Zika virus—all of which presented serious risks to the health security of countries around the world. Yet when such public health emergencies occur, funds to combat them are released in a sporadic and disjointed manner, in amounts far greater than would have been needed for prevention and preparedness. In response to the Ebola outbreak in 2014, for example, Congress appropriated $5.4 billion (Kates et al., 2015), $1.1 billion of which was spent domestically (Epstein et al.,
___________________
1 Intelligence reports for each year can be found in the archives, located here: https://www.dni.gov/index.php/newsroom/testimonies/179-congressional-testimonies-2009 (accessed March 15, 2017).
2015), representing 120 percent of the approximately $900 million in total annual appropriations for building public health and health care preparedness capacity.2
As of the release of this report, both MERS-CoV and Zika continue to smolder beneath the surface with small-scale outbreaks, but there is no vaccine or treatment available should either erupt into a full-fledged epidemic in a populated area. The potential for the use of man-made biological weapons in acts of terrorism is an ongoing threat as well. While global crises have largely been avoided to date, the lack of a strategic approach to these threats could have grave consequences. If the system for responding to such threats remains reactionary, the world will not always be so lucky. Instead, strong public health infrastructure and preparedness systems are needed, along with a clear commitment from the U.S. government to drug and vaccine development. Yet in the face of competing priorities, funding for these purposes is often the first to be cut because of a failure to appreciate these threats and their potential consequences. Swift and proactive strategic action is needed now, before one or more of these threats rise to the surface and outpace the world’s ability to respond.
This chapter begins by describing in detail the various dimensions of the threats to and vulnerabilities of global health security. It then outlines the human and economic costs of failing to take action to address these security challenges. The third section describes current global health programs and commitments, and why they are inadequate to meet these challenges. The chapter then presents the committee’s vision of a new approach to global health security, focused on building preparedness capacity in the United States and abroad, ensuring sustainable funding for these efforts, and creating an environment for proactive research and development aimed at enhancing the nation’s preparedness and response capacity. The final section presents a summary and recommendations.
THE GLOBAL HEALTH SECURITY IMPERATIVE
The World Health Organization (WHO) defines global health security as the “activities required . . . to reduce the vulnerability of people around the world to new, acute, or rapidly spreading risks to health, particularly those that threaten to cross international borders” (CDC, 2016d). To adequately address the risks to global health security, however, it is necessary to understand the inherent vulnerabilities encompassed by this definition. Today’s domestic and regional health crises are increasingly influenced by
___________________
2 This percentage was calculated by using fiscal year 2016 amounts of Public Health Emergency Preparedness program funding ($660 million) and Hospital Preparedness Program funding ($255 million) as the preparedness amounts.
widely interrelated global changes and forces defined by climate change; loss of biodiversity; rapid unsustainable urbanization; and scarcities of water, food, and energy (Burkle, 2017). More precise threats include zoonotic spillover or the emergence of new infectious diseases, pandemic influenza, and growing antimicrobial resistance. Exacerbating the risks resulting from these threats are vulnerabilities such as degraded public health infrastructure, vulnerable supply chains for health and medical products, and fragile nation states. This section reviews these various threats and vulnerabilities, which are summarized in Table 3-1.
Rapid Urbanization and Loss of Biodiversity: Zoonotic Spillover
The trend toward urbanization is accelerating as individuals leave less prosperous agrarian jobs in rural regions to pursue better opportunities in cities. While this rural-to-urban migration is not a new phenomenon, it has been accelerated by globalization: In 1950, only 30 percent of people worldwide lived in urban areas, but this proportion had risen to 54 percent by 2014, and it is expected to grow to 66 percent by 2050 (UN, 2014). The number of megacities (cities with populations of 10 million or more), most of which are in low- and middle-income countries (LMICs), is also projected to grow, from 28 to 41 in the next 15 years (UN, 2014). And as highlighted in the U.S. intelligence community’s worldwide threat assessment, Asia and Africa are urbanizing more rapidly than any other regions (Clapper, 2016).
While urbanization is an indication of economic growth and opportunity, it also reduces biodiversity through habitat loss, fragmentation, and biological homogenization (McKinney, 2002; Pauchard et al., 2006). Since 2000, the global community has witnessed numerous outbreaks of diseases such as SARS, Ebola, Marburg, hantavirus, and avian influenza, as a result of human impacts on biodiversity (COHAB Initiative, 2010). Almost of all of these outbreaks were due to infectious disease spillover, which occurs when an immunologically naïve population comes in contact with a reservoir population that has a high pathogen prevalence. In addition to loss of biodiversity, urbanization and high population density can create an environment in which infections such as tuberculosis (TB) can thrive; more virulent strains of pathogens can evolve (Pongsiri et al., 2009); antimicrobial resistance occurs (Allen et al., 2010); and the rapid spread of disease becomes possible.
While the majority of the disease burden in past outbreaks has fallen on developing countries, increases in human mobility have increased the distances and accelerated the speed over which microbes can travel (Labonte et al., 2011). Thus, despite the global community’s efforts to conquer communicable diseases in the poorest regions of the world, it has witnessed the
TABLE 3-1 Health Threats and Vulnerabilities Associated with Globalization
| Threat | Global Impact | U.S. Impact |
| Zoonotic diseases and spillover | From 2000 to 2010, zoonotic diseases caused $200 billion in indirect economic losses (World Bank, 2010). Additionally, more than 2.5 billion cases and 2.7 million deaths can be attributed to the top 56 zoonoses (Gebreyes et al., 2014). | Since 1999, West Nile virus (WNV) has infected an estimated 3 million people (Petersen et al., 2013), resulting in approximately 43,000 illnesses due to its asymptomatic nature (Cahill et al., 2017). Costs of WNV in the United States are estimated to be $56 million per year (Barrett, 2014). |
| Antimicrobial resistance (AMR) | At the current rate of development of drug resistance, losses of 10 million lives per year and a cumulative loss of $100 trillion in global economic output by 2050 are projected (Review on Antimicrobial Resistance, 2016). | In the United States, AMR results in 23,000 deaths and $55–$70 billion in economic losses annually (PCAST, 2014) |
| Pandemic influenza | A moderately severe influenza pandemica would result annually in 700,000 deaths and a cost of $570 billion (due to income loss and mortality) globally (Fan et al., 2016). | An influenza pandemic in the United States would result in 89,000–207,000 deaths and an economic loss of $71.3–$166.5 billion (Meltzer et al., 1999). |
| Weak public health infrastructure and protectionsb | The Zika virus, spread by Aedes mosquitoes,c emerged in Brazil in 2014 and spread rapidly to 26 neighboring countries, infecting up to 1 million people (Petersen et al., 2016). Zika’s estimated cost to Latin America and the Caribbean was $3.5 billion in 2016 (World Bank, 2016c). Once eradicated from 18 countries in 1962, Aedes aegeypti saw a resurgence due to public health complacency and failed vector control (Whitman, 2016). | Aedes aegeypti is found in the southern region of the United States, meaning these states are also at risk for Zika. Mosquito surveillance and control efforts in the United States are implemented in a patchwork manner at the state and county levels (Schmidt, 2016). The urgency of combating Zika led to a $1.89 billion request by President Obama, yet appropriations were delayed by 7 months (Wexler et al., 2016). Unfortunately, the delay led to more Zika cases, and as of March 1, 2017, 5,074 cases of Zika had been confirmed in the continental United States (CDC, 2017a). |
| Threat | Global Impact | U.S. Impact |
| Supply chain vulnerabilities | During the 2014 Ebola outbreak, high demand for personal protective equipment (PPE) was met with low inventory and capacity, and manufacturers struggled to meet the need. As a result, many countries in West Africa had to consider splitting deliveries over time (UNICEF, 2014). | A shortage of saline solution, an essential product for U.S. hospitals, occurred in 2014 as a result of recalls from the few U.S. manufacturers and weather issues. The U.S. Food and Drug Administration (FDA) had to begin importing the solution from Germany, Norway, and Spain to alleviate the need (FDA, 2016), as the lack of access to saline can be a death sentence for dialysis patients (Dembosky, 2014). |
| Fragile states/conflict zones | Although Nigeria had been declared polio free in 2015, conflict with Boko Haram in its northern region prevented the establishment of proper surveillance programs, and four types of wild polio viruses were found in 2016. Because polio is highly contagious, public health officials had to initiate a massive campaign to vaccinate millions of children across West and Central Africa (Beaubien, 2016). Costs of this campaign have yet to be estimated. | The U.S. government is currently the largest donor to the Global Polio Eradication Initiative (GPEI), with a commitment of $228 million in fiscal year 2016. This funding has contributed to significant gains in reducing polio endemicity (KFF, 2016). However, state fragility is a barrier to polio eradication, and results in a need for continuous U.S. investment due to the ongoing threat. |
a Defined as having a mortality rate of less than 10 standardized mortality units (SMUs), where 1 SMU corresponds to 735,000 deaths (Fan et al., 2016). For perspective, seasonal influenza causes 250–500,000 deaths per year (WHO, 2016c).
b Public health infrastructure is considered to include safe water and sanitation, as well as community preventive programs (e.g., vector control, vaccines).
c Aedes mosquitos are widespread throughout the tropics and transmit other arboviruses, such as chikungunya, dengue, and yellow fever. The principal vector for Zika, Aedes aegypti, is widely distributed throughout the Americas (Petersen et al., 2016). Zika has also been found to be spread by mother-to-child transmission, sexual activity, and blood transfusions (Schmidt, 2016).
reemergence of known and the emergence of new diseases. SARS is the most notable recent example of the amplification of the spread of disease enabled by today’s increased interconnectedness. The first case of SARS was identified in the Guandong province, China, in November 2002 (CDC, 2013b), and by May 2003, the disease had spread to 30 countries on 6 continents (WHO, 2017b).
Pandemic Influenza
A persistent theme of the health security conversation is the threat of an influenza pandemic. Unlike seasonal influenza, a pandemic influenza virus results from a dramatic mutation in the virus. In the 20th century, three major influenza pandemics occurred—in 1918, 1957, and 1968—causing millions of deaths and wide-scale economic disruption. The 1918 pandemic alone resulted in approximately 50–100 million deaths (3–5 percent of the global population at the time) (Jeffery and David, 2006), and is cited as the most devastating epidemic in recorded history (see Annex 3-1 at the end of this chapter). However, even less severe pandemics could pose a threat to the global community, as evidenced by the two multicountry influenza pandemics that have occurred since 2000 (the 2005 H5N1 pandemic and the 2009 H1N1 pandemic). The 2009 H1N1 pandemic resulted in approximately 284,000 deaths worldwide (Viboud and Simonsen, 2012). The frequency with which influenza pandemics have occurred in the past suggests that an influenza pandemic is likely to occur again (see Box 3-1 for a description of China’s current H7N9 outbreak).
Regardless of severity, the scale of morbidity and mortality for any influenza outbreak is unpredictable. Thus, any potential outbreak poses a continued national security threat and necessitates a strong public health approach (including immunization infrastructure and surveillance) in addition to continued research into vaccines and other medical tools that can mitigate their impacts from the outset. Yet progress on a universal influenza vaccine has been a hope for years (The Energy and Commerce Committee: Subcommittee on Oversight and Investigations, 2013; Vergano and Szabo, 2011), and it is increasingly difficult to maintain private-sector interest in the development of annual seasonal influenza vaccines (Ridley et al., 2016), as well as to foster high vaccination rates. For example, only 10 states vaccinated at least half of their population against the seasonal flu during the 2015–2016 flu season (Segal et al., 2016). Yet even as robust seasonal flu vaccination remains out of reach, direct medical costs of seasonal flu for the U.S. population are estimated at $10.4 billion annually, with projected annual lost earnings estimated even higher at $16.3 billion (Molinari et al., 2007).
Antimicrobial Resistance
Antimicrobial resistance (AMR) refers to the phenomenon whereby pathogens stop responding to the drugs customarily used to combat them, making the drugs ineffective. AMR is usually attributed to overuse and inappropriate use of antimicrobial drugs, in addition to the growing issue of substandard or counterfeit drugs (Kelesidis et al., 2007). Regardless of its cause, resistance inevitably arises when pathogens become exposed to the drugs used against them. This means that use of antibiotics in livestock feed and agriculture can also contribute to the development of resistance (Littmann and Viens, 2015). As resistant microbes are found in people, animals, food, and water, they can spread from animal to person and from person to person. Globalization and increased migration, travel, and trade have substantially increased the risk of AMR around the world, as signified by the fact that resistance is found in every country (WHO, 2016a). Multidrug-resistant tuberculosis, for example, a particularly vexing public health issue, has been seen in South America, Eastern Europe, and across the African and Asian continents (WHO, 2016b). Likewise, at the Médecins sans Frontières hospital in Amman, Jordan, half of all wound infections among patients arriving from the war in Iraq and Syria are resistant to antibiotics (MSF, 2014). Each year in the United States, 2 million people
experience infections that are resistant to the antimicrobials commonly used to treat them, and 23,000 people die as a result of such infections (CDC, 2013a) (see a recent example in Box 3-2). Globally, 700,000 annual deaths are attributed to drug-resistant infections (Review on Antimicrobial Resistance, 2014).
In addition to its human costs, the occurrence of resistance has major economic implications at the community, country, regional, and global levels (World Bank, 2016b). For example, AMR not only directly affects health care systems by draining workforce capacity and increasing the costs of hospital stays and second-line drugs (Long et al., 2010), but also compromises the progress achieved in reducing the burden of critical infectious diseases, such as human immunodeficiency virus (HIV), TB, and malaria (as
explored more in Chapter 4). Furthermore, according to the World Bank, failing to contain AMR would jeopardize achievement of the Sustainable Development Goals by 2030, as well as reverse the poverty reduction and economic growth attained through the effective use of antimicrobials (World Bank, 2016b).
The global health challenge of AMR, like many others emphasized throughout this report, cannot be solved by governments alone; private-sector involvement will be critical to achieving success. In January 2016, the pharmaceutical, biotechnology, and diagnostics industries signed a declaration on combating AMR, committing to investing in research and development aimed at meeting public health needs and to improving access to high-quality and new antibiotics for all (IFPMA, 2016). Support from all country governments in creating a sustainable market for the products of these efforts and in implementing measures to prevent further development of resistance will also be crucial. Yet unless the United States can mobilize resources and action to address this problem internationally as well as domestically, success will not be realized. Having reviewed some of the priority emerging global health threats, the section will now continue by articulating underlying vulnerabilities that can exacerbate the threats for the United States.
Public Health Infrastructure
To prevent threats such as those described in the previous sections, the United States and the global community need to support appropriate public health measures, including access to clean water and sanitation, food safety, and robust immunizations campaigns. Given that not all health security events can be prevented, however, there is also a need for preparedness and response capacity in the event of an outbreak.
Well-built and -maintained public health infrastructure geared toward both prevention and preparedness is the first line of defense against health threats. Furthermore, activities related to prevention, epidemic investigation, and control require a sophisticated level of decision making and resource coordination (Burkle, 2006). Yet, nations across the world, including the United States, have failed to invest in the necessary infrastructure and capacities. By sacrificing prevention and preparedness, nations have inevitably compromised the ability of public health systems to respond rapidly to health threats. These globally shared deficiencies became evident during the 2002–2003 SARS outbreak and the 2003–2004 H5N1 outbreak, and again during the 2014 Ebola outbreak (GHRF Commission, 2016).
Over the past decade, public health funding in the United States has remained flat at the federal level, but has been cut at drastic rates at the state and local levels (Levi et al., 2015a). During 2012, 48 percent of all lo-
cal health departments reduced or eliminated services, with immunization, maternal and child health, and emergency preparedness being the program areas most affected (Levi et al., 2015a). Similarly, dedicated public health and health care emergency funding has been steadily decreasing during the last decade (see Figure 3-1).
Recent memoranda on health security from the Johns Hopkins Center for Health Security to the new administration and Congress stress the importance of building sufficient surge capacity in the U.S. health care system to provide clinical care during epidemics and catastrophes. The memoranda also emphasize building public health infrastructure with the expertise and technology to provide earlier warning of outbreaks and disasters (Inglesby and Cicero, 2017). While the implementation of such a system can be resource-intensive, it also can reap crucial rewards. Uganda, for example, was able to respond effectively to three outbreaks of Ebola (between 2007 and 2013) and one outbreak of Marburg (in 2014) because of the public health infrastructure it built after experiencing an Ebola outbreak in 2000, the largest in global history until 2014 (CDC, 2014, 2016f; GHRF Commission, 2016). Likewise, Nigeria was able to respond rapidly to its 2014 Ebola outbreak because of a preexisting polio surveillance structure and
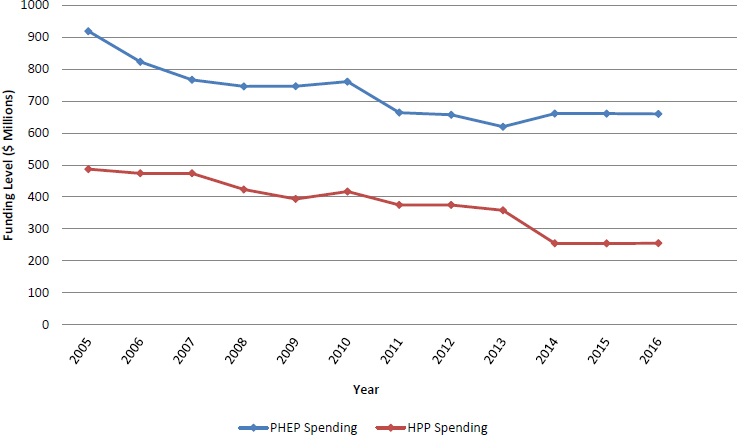
NOTE: HPP = Hospital Preparedness Program; PHEP = Public Health Emergency Preparedness.
SOURCES: Boddie et al., 2015; Levi et al., 2015b; Segal et al., 2016.
emergency operations center, as well as trained field epidemiologists. The country was able to rapidly shift the target of these capabilities from polio to contain the Ebola outbreak in Lagos, a city of 21 million people, to just 19 cases and 7 deaths (WHO, 2014b).
To ensure a strong health system, it is essential to continually support key public health programs. Public health suffers from the “out of sight, out of mind” phenomenon; consequently, success often goes unnoticed and results in complacency. When this happens, funding is cut and programs are scaled back, which often results in the resurgence of an infectious disease that was previously under control. Until resurgence occurs, however, gaps in prevention draw little attention. To illustrate this cycle, Box 3-3 describes the examples of dengue and yellow fever resurgence in Brazil, malaria resurgence in Venezuela, and polio resurgence in conflict zones.
The Supply Chain System
The current supply chain system that supports the deployment of medical products is not well matched to the demands that a health security threat would create—a gap that represents a significant vulnerability. For everyday needs, the medical and public health sectors have come to rely on a just-in-time delivery system. Less a delivery system than an inventory strategy, such a system aims to supply a small amount of products as needed. The resulting limited stockpiles of medical products are the most notable aspect of this vulnerability, and the supply chains for these stockpiles only contribute to the problem. The United States, for example, currently imports 75–80 percent of the raw materials for drugs meant for the U.S. domestic market (GAO, 2007), which increases susceptibility to the effects of a public health emergency should an outbreak occur in an exporting country. Supply chain issues are not limited to raw materials, but also apply to widely used medications themselves. A 2009 study, for example, found that 100 percent of 30 identified essential generic life-saving medicines3 were manufactured overseas—mainly in India or China—with long supply chains and no significant stockpiles. In the event of a pandemic in these countries or a disruption at any point along these supply chains, U.S. hospitals would lose the ability to provide these drugs to patients (Osterholm and Olshaker, 2017). Similarly, according to a 2016 report by the Trust for America’s Health (TFAH), 40 percent of states lack backup medical supplies to cope with a pandemic influenza or other major outbreak should their supplies be low (Segal et al., 2016). Because of the just-in-
___________________
3 The list of 30 drugs was based on responses from hospital pharmacists about what drugs were absolutely needed in their specialty. These included albuterol, heparin, insulin, nitroglycerine, and various other drugs and antibiotics (Osterholm and Olshaker, 2017).
time delivery system, many health care systems can be one local supply breakdown away from an emergency for their patients. Box 3-4 provides examples of the effects of these limitations in supply chains during previous public health emergencies.
As evidenced by the examples in Box 3-4, the supply chain systems currently in place are not always capable of meeting a surge in demand. Because ensuring surge capacity and adequate stockpiles will likely result in financial losses for manufacturers, governments must incentivize them to do so. For example, Canada purchases flu vaccines from manufacturers annually—10.4 million in 2013 (The Canadian Press, 2014)—to ensure the production of a reserve supply (Public Health Agency of Canada, 2017). The U.S. Office of the Assistant Secretary for Preparedness and Response (ASPR) has begun to take similar action through its partnership with the Centers for Innovation in Advanced Development and Manufacturing, focused on assisting in addressing the shift in vaccine production capabilities overseas by the biopharmaceutical industry (see Chapter 7). However, this vaccine initiative addresses just one part of the problem; and additional solutions are needed even for such items as saline, gloves, masks, and other routine health supplies.
Fragile States Threatening Global Successes
Despite the political and public health progress achieved in many countries, the governments of some LMICs have become so ineffective that these countries are considered failed states. Violence and war threaten the stability of their region and the world, including the progress of global health successes such as immunization and infectious disease control. The 2017 World Economic Forum Annual Risks Report identifies involuntary large-scale migration as the second most likely global risk of concern. The nature of this risk has been demonstrated in Syria, where conflict has driven migration to neighboring countries, transferring pressures to already weakened economies, fueling radicalization and violence, and demonstrating the consequences of ignoring such challenges (WEF, 2017).
Of particular relevance in the present context, the occurrence of conflict and war often results in the destruction of a health system and its public health interventions, creating an ideal environment for diseases to spread unchecked (Michelle et al., 2007).4 Prior to the current civil war in Syria, for example, its vaccination rates were among the highest in the Mediterranean region—at above 90 percent (Alwan, 2015). In 2014, however, polio, measles, and pertussis resurged in Syria and spread to Iraq, threatening public health in both countries. When such resurgence occurs, it can require drastic responses, since as long as cases exist anywhere in the world, such diseases will constantly be a threat to everyone. Even those who have been vaccinated are at risk given the need for herd immunity for vaccinations to be fully effective (Fine et al., 2011). As another example, as a result of recent conflict and war in Yemen, that country launched a major polio vaccination campaign in February 2017 because of fears that the disease would reappear, even though the country was declared polio-free in 2009.
Given the real dangers posed by state fragility and conflicts, the global community has an imperative to take action. However, a response all too often is launched after an emergency has occurred—a pattern that needs to end. According to Frederick Burkle of the Harvard Humanitarian Initiative,
If one accepts that disasters keep us honest by defining the public health and exposing its vulnerabilities, the global community must emphasize prevention and preparedness and re-legitimize it under international law to ensure protective strategies that intercede in fragile states before they deteriorate to the point of no return. (Burkle, 2017, p. 2)
___________________
4 Regions of the world that have been particularly affected by conflict in recent years are the Lake Chad region in Africa and the WHO Mediterranean Region. Conflict caused by Boko Haram near Lake Chad has raised concerns by officials about polio resurgence. Countries in the WHO Mediterranean Region, which consists of the Middle East and North Africa, have been struck by conflict and wars, but most of those affected are inaccessible to aid and medical supplies, leading to disease resurgence and a state of emergency (Alwan, 2015).
U.S. leadership plays an important role in supporting healthy societies abroad. However, the effects of state fragility on security and progress in global health warrant early and swift intervention. The costs of failing to support global health, especially in terms of basic public health protections, can be high.
Finding: Wide-ranging threats to global health security influenced by resource scarcity, rapid urbanization, and inadequacies in stewardship of medications are poised to exploit the vulnerability of all countries, including the United States. These threats range from infectious disease spillover to pandemic influenza, to antimicrobial resistance, and are exacerbated by such vulnerabilities as degrading public health infrastructure, weak medical supply chains, and fragile states.
THE COSTS OF INACTION
Failure to act to address the threats and vulnerabilities detailed above has severe human and economic costs, many of which have been demonstrated throughout previous outbreaks and emergencies.
Human Costs
Since 2009, the world has witnessed multiple regional and global outbreaks of diseases whose effects could have been mitigated had better prevention and preparedness measures been in place. Following the H1N1 outbreak in 2009, the U.S. Centers for Disease Control and Prevention (CDC) led an international research team that examined the global death toll from the pandemic; the team’s estimate was 284,000 deaths worldwide due to H1N1 directly. In addition, the virus indirectly caused 201,200 respiratory deaths and another 83,300 deaths due to cardiovascular disease (Roos, 2012). In another example, as of April 2016, 11,325 people had died in the 2014 Ebola outbreak in West Africa (CDC, 2016a), and if the outbreak had unfolded in any nearby megacity, the death toll would have been far higher. Moreover, an additional 10,623 people were estimated to have died from other causes in the three Ebola-affected countries during the outbreak, simply as a result of the chaos and reduced availability of services (Parpia et al., 2016). This latter figure represents an almost 100 percent increase in deaths that occurred simply because the health system had to halt or reduce all other services to focus its attention on Ebola, reversing progress on many diseases and health issues because of the lack of surge capacity. Looking to future threats, according to the National Bureau
of Economic Research, even a moderately severe influenza pandemic could lead to 2 million or more excess deaths worldwide (Fan et al., 2016).
Economic Costs
Past outbreaks have illustrated that the economic losses they cause can far exceed the costs of preventing them. For example, the eradication of smallpox worldwide led to benefits outweighing costs at a ratio of 159:1 globally (Barrett, 2013). The costs of infectious disease outbreaks are likely to rise, moreover, as such outbreaks become more frequent as a result of expanding travel and trade, as well as environmental changes (Pike et al., 2014). The costs are only partially attributable to treating and controlling the disease itself; additional costs result from panic and the “worried well” flooding hospitals and stripping pharmacies of medical supplies. Indeed, panic can have more of a negative effect on an economy than an outbreak itself, as evidenced by the discourse in the United States during the Ebola outbreak. Once an Ebola patient had been diagnosed in the United States and $5.4 billion in response funds had been allocated, $1.1 billion was spent on domestic response, including public health studies, state and local laboratory capacity, state and local preparedness, and domestic migration activities (Epstein et al., 2015). Of this amount, $119 million was spent just on domestic quarantine activities, including screening at five major U.S. airports, medical consultations, investigations of potentially sick travelers, and follow-up (CDC, 2015a). And while commendable efforts were made by thousands of federal, state, and local government workers (White House, 2015), it is important to keep in mind that this domestically focused $1.1 billion was disbursed in response to only four cases nationwide.5 The amount spent likely would have increased greatly if the number of cases had risen even to 10 or 20.
Following the SARS outbreak in 2003, which lasted less than 1 year, global costs of the pandemic were assessed to be $40–$54 billion (Jonas, 2014a; McKibbin, 2004). According to a World Bank policy research paper, the four most affected economies in East Asia (China, Hong Kong, Taiwan, and Singapore) experienced estimated gross domestic product (GDP) losses of $13 billion (Brahmbhatt and Dutta, 2008). Similarly, Guinea, Liberia, and Sierra Leone together were projected to suffer a crippling loss in foregone economic growth in 2015 as a result of the Ebola epidemic. After positive GDP growth in 2013 in all three countries, 2014 saw Guinea’s GDP growth drop from 4 percent to 0.1 percent and Liberia’s from 8.7 percent to 0.7 percent, while Sierra Leone’s GDP growth declined from
___________________
5 This number does not include cases of patients who became sick while working in West Africa and returned to the United States for treatment.
4.6 percent in 2014 to –21.5 percent in 2015 (World Bank, 2016a). Many of these economic losses could have been prevented had a more resilient health system capable of preventing and detecting outbreaks been in place (World Bank, 2015).
In addition to determining the cost of past outbreaks, it is important to examine models of future outbreaks to better inform policy and planning. The projected economic impact of an influenza pandemic ranges from $570 billion per year, including the intrinsic value of lives lost prematurely and illness suffered (Fan et al., 2016),6 to $2 trillion7 in direct costs, worker absenteeism, and disruptions in business (Burns et al., 2008).
The Bottom Line
Infectious disease outbreaks clearly impose terrible costs in terms of human suffering and mortality, as well as economic costs that threaten progress and stability in countries around the world, and that greatly exceed the costs of prevention and preparedness measures (GHRF Commission, 2016; Jonas, 2014b). Given the human and economic toll repeated time and again, the question then arises of how many more such outbreaks must occur before the global community acknowledges this as a threat that warrants taking sustainable action and musters the collective will to do so.
Finding: The committee believes that these threats will only become more prevalent, due to global changes such as urbanization, resource scarcity, population growth, and environmental changes, resulting in high human and economic costs.
THE CURRENT GLOBAL COMMITMENT
Even as increasing globalization is making the world ever more vulnerable to infectious disease outbreaks—whether due to natural, accidental, or intentional causes—thereby threatening national and global security, methods of distributing global aid are changing. While U.S. development policy has remained focused on U.S. aid as a way to build prosperous nations, it has become increasingly clear that, to achieve better health for their people, recipient countries no longer want to be considered beneficiaries of
___________________
6 This study, conducted by the National Bureau of Economic Research, estimated the effect of a moderately severe pandemic (one with a mortality rate of less than 10 SMUs, where 1 SMU corresponds to 735,000 deaths). The costs include expected income losses and the intrinsic value of lives lost and illness suffered (Fan et al., 2016).
7 This study, conducted by the World Bank, estimated the cost of a moderate influenza pandemic (one that would reduce global output by more than 2 percent). The costs included are direct costs, worker absenteeism, and disruptions in business (Burns et al., 2008).
bilateral aid, but rather partners in multilateral groups (Birdsall and Leo, 2016). Given that no single nation can be protected if other nations remain unprepared to counter biological threats,8 the United States has a unique opportunity to capitalize on this shift in the nature of desired relations. It should move to encourage partnerships and cross-sector coordination focused on achieving the shared goal of security from infectious disease threats for all people. To fully understand the importance of this commitment, one must first know the history that contributed to the need for such investment of U.S. resources abroad.
The International Health Regulations
The International Health Regulations (IHR), which replaced the International Sanitary Regulations in 1969, were updated in 2005 following the global SARS outbreak to reflect the rapid expansion of international trade and tourism. While WHO had developed the vision for this update in the late 1990s, the 2003 SARS pandemic brought increased attention to the need to shift from halting diseases at national borders to finding and halting them at their source. This revision helped strengthen capacity and cooperation in many countries. However, the 2009 H1N1 pandemic, which served as the first true test of the revised IHR, revealed continued vulnerabilities in public health capacities at all levels, limitations in scientific knowledge concerning response, difficulties in decision making under uncertain conditions, complexities in international cooperation, challenges in communication among experts and with the public, and shortcomings of WHO decision making (WHO, 2011a).
Unfortunately, as of 2014, only about 33 percent of the 196 WHO member countries were in compliance with IHR core capacities (Katz, 2016). Thus, there exists an imperative for robust information sharing, monitoring, and response capacities both in the United States and abroad—where most infectious disease outbreaks originate—to enable proper preparation for the next and perhaps more dangerous outbreak. Many experts have recommended working toward an international consensus framework to fulfill the obligation of Article 44 of the IHR. Such a framework would guide best practices in collecting and sharing research and surveillance data in a timely and accurate manner across countries and with the public and private sectors to inform the management of any type of infectious disease event (Nuzzo and Shearer, 2017).
___________________
8 Executive Order 13747, Advancing the Global Health Security Agenda to Achieve a World Safe and Secure from Infectious Disease Threats, 3 C.F.R. 13747.
The Global Health Security Agenda
To ensure that countries around the world would meet IHR core capacity requirements for public health emergencies, the U.S. government, along with international partners, launched the Global Health Security Agenda (GHSA) in February 2014. Originally a 2-year, $85 million commitment (Morrison, 2014), support for the GHSA increased as a result of the Ebola outbreak. Now supported by one-time supplemental funding9 (Frieden, 2016) of $1 billion (GHSA, 2017), the GHSA seeks to improve national-level capacity to prevent, detect, and respond to infectious disease threats, and it has established 11 action packages10 to achieve these goals (CDC, 2016c). Rather than creating a new strategy aimed at health security, the GHSA builds on existing U.S. strategies that provide for capacity building, technical assistance, and commodity support. Where the GHSA is novel, however, is in its coordination of these strategies and its elevation of global health security to senior-level attention (Holgate, 2014).
Building Epidemiological Capacity
In line with the GHSA’s mandate of building workforce capacity, fostering the development of a cohort of public health experts with knowledge of the salient science and policy can help with early detection of and response to outbreaks. If this capacity building is done in a sustainable manner, a full transfer of U.S., Canadian, and European public health responders will not be necessary whenever an outbreak occurs. During the 2014 Ebola outbreak, the strong public health capacity in Nigeria—encompassing trained field epidemiologists and an active and functioning emergency operations center (previously supporting polio surveillance)—managed to successfully monitor 900 people through deployment of the country’s established team of field epidemiologists while also engaging community leaders and members (Courage, 2014; Frieden, 2014). The Field Epidemiology and Training Program (FETP) within CDC develops expertise in detecting diseases locally and preventing them from spread-
___________________
9 The GHSA is partially funded by leftover Ebola emergency funds in the fiscal year (FY) 2015 Omnibus Package (Consolidated and Further Continuing Appropriations Act, 2015, Public Law 113-235, Title VI, 113th Congress), which became redirected but expire in FY2019 (Segal et al., 2016).
10 The GHSA’s Action Packages are categorized into three domains: Prevent, Detect, and Respond. Under the Prevent Domain are the Action Packages for Antimicrobial Resistance, Zoonotic Disease, Biosafety and Biosecurity, and Immunization. Under the Detect Domain are the Action Packages for National Laboratory Systems, Real Time Surveillance, International Reporting, and Workforce Development. Under the Response Domain are the Action Packages for Emergency Operation Centers, Multisector Rapid Response, and Medical Countermeasures/Personnel Deployment (CDC, 2016c).
ing globally. The program has trained more than 3,100 epidemiologists in more than 70 countries since 1980 (CDC, 2016e), and has been based in Nigeria since 2008. In 2013–2014 alone, African FETP graduates responded to more than 100 outbreaks, including Lassa fever in Nigeria, polio in Cameroon and Nigeria, and monkeypox in The Democratic Republic of the Congo (CDC, 2015b). This program is also supported by the GHSA, which, through its action package on workforce development, saw the establishment, expansion, or participation of 17 countries in FETP programs to increase the number of disease detectives (GHSA, 2017) (see Box 3-5). Continued support of epidemiology training improves surveillance and detection capabilities abroad, and provides another opportunity for more robust institutional pathways for bidirectional information sharing, allowing for faster detection of new diseases and outbreaks and changes in protocols that may be necessary.
Concerns for the Future of the GHSA
The GHSA is financed by one-time supplemental funding, which will run out by 2017 (Frieden, 2016), and there is concern about what will happen thereafter. In information-gathering requests administered to CDC country directors and comments made by high-ranking government officials (GU GHSS and HGI, 2017), strong support for the continuation of the GHSA has been expressed. Although an executive order signed by President Obama in November 2016 called for GHSA’s advancement and established long-term policy objectives for the United States to build on its achievements (Rice, 2016), there is no guarantee as to its future direction.
Global health security requires stable support systems for preparedness and response capacity in LMICs. Sustained funding by the global community is imperative to support this capacity and prevent the reversal of the progress that has been achieved. Following the West Africa Ebola outbreak, multiple high-level panels and commissions were charged with identifying needed WHO reforms (described further in Chapter 9). These groups also highlighted the need for countries to partner with WHO to ensure that they can implement the core capacities necessary to comply with the IHR, with the goal of having every government develop and publish concrete plans by 2020 (Gostin et al., 2016). Meeting this need will require continued participation by the United States. The GHSA is a valuable initiative that has been able not only to coordinate the vast array of U.S. programs in global health security but also to create transparent and mutually accountable means for countries around the world to assess their own capacities. While it is hoped that capacity-building efforts will eventually be assumed by national governments, until then, the umbrella of programs supported by the GHSA and the focus of global health security itself requires continuous funding. Absent this concerted effort to ensure the development of resilient health systems in LMICs, capable of preventing and responding to emergencies, the risk of another Ebola-like epidemic remains a very real threat to all countries around the world.
Efforts to Combat Antimicrobial Resistance
In 2014, recognizing the growing threat of AMR and its national and global implications, President Obama signed an executive order on combating antibiotic-resistance bacteria.11 This executive order formed the basis of the National Strategy for Combating Antibiotic-Resistant Bacteria (White House, 2014b) and established a federal interagency task force for Combat-
___________________
11 Executive Order 13676. Combating Antibiotic-Resistant Bacteria. 3 C.F.R. 13676.
ing Antibiotic-Resistant Bacteria.12 Among its functions, the task force was asked to submit a 5-year National Action Plan incorporating the recommendations of the report on combating antibiotic resistance of the President’s Council of Advisors on Science and Technology (PCAST) (PCAST, 2014). In addition, the task force co-chairs were charged with establishing the Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria (PACCARB) to provide advice and guidance for their work.
While the PACCARB acknowledged that important steps have been taken to achieve the milestones outlined in the National Action Plan, its initial assessment identified overarching issues and generated recommendations for further improvement. Goal 5 of the plan—“Improve international collaboration and capacities for antibiotic-resistance prevention, surveillance, control, and antibiotic research and development”—has particular relevance to global partnerships (PACCARB, 2016), and PACCARB therefore made recommendations for improving international collaboration and capacity that include
- improving measures of effectiveness by identifying outcome indicators,
- ensuring resources commensurate with supporting the goals,
- expanding the number of countries involved,
- leveraging the expertise of nongovernmental organization (NGO) assets,
- broadening the scope of One Health, and
- expanding engagement around research and development.
Up to 30 percent of drugs sold in LMICs have been found to be counterfeit, an issue that represents a significant risk for the development of AMR (Cockburn et al., 2005). The U.S. government has made efforts to stem the flow of substandard and counterfeit pharmaceuticals by engaging with NGOs and nonprofits, efforts that could help combat AMR. The U.S. Agency for International Development (USAID) has entered into a number of partnerships in hopes of reducing the number and availability of counterfeit drugs. Perhaps the most important of these is with the U.S. Pharmacopeial Convention—the Promoting the Quality of Medicines Program. This program operates in 28 countries and has been able to assist 17 countries
___________________
12 The task force is co-chaired by the secretaries of defense, agriculture, and health and human services and made up of representatives from the U.S. Departments of State, Justice, Veterans Affairs, and Homeland Security, as well as the U.S. Environmental Protection Agency, the U.S. Agency for International Development, the Office of Management and Budget, the Domestic Policy Council, the National Security Council, the Office of Science and Technology Policy, and the National Science Foundation. Executive Order 13676, Combating Antibiotic-Resistant Bacteria, 3 C.F.R. 13676.
with quality monitoring and surveillance (USP, 2017a,b). Building on such partnerships could help combat the significant threat to the supply chain of pharmaceuticals posed by counterfeit drugs.
Additionally, embracing the One Health approach across sectors can help not only in optimizing the use of resources but also in improving the effectiveness of interventions aimed at promoting health in humans, animals, and the environment. The One Health approach recognizes that human health is closely related to the health of the environment and of animals. Given that 6 of every 10 infectious diseases in humans are spread from animals, the One Health approach aims to encourage collaborative efforts of multiple disciplines working locally, nationally, and globally to achieve the best health for people, animals, and the environment (CDC, 2017b). This approach is implemented in global activities such as the GHSA and the use of animal–human interface officers at CDC’s Global Disease Detection sites (CDC, 2016b).
While there has been progress toward Goal 5 of the National Action Plan, there remain challenges that hinder its full realization, including difficulties in providing incentives for the development of diagnostics and therapeutics. However, a particularly critical barrier is the lack of sufficient funds to advance the AMR agenda. Although Congress appropriated $1 billion in FY2016 for combating AMR, the overwhelming majority of that funding was earmarked for domestic spending, with approximately $835 million being allocated to the U.S. Department of Health and Human Services (HHS) (Cabezas, 2016). U.S. hospitals certainly deserve and demand high levels of proper stewardship and infection control, but unless preparedness and surveillance capacities are built and sustained internationally, AMR will continue to threaten U.S. citizens regardless of how prepared U.S. hospitals may be. The example presented previously in Box 3-2 highlights how rapidly bacterial pathogens can spread and how important it is to invest in these capacities globally.
World leaders committed to uniting in the fight against AMR at a high-level meeting on AMR held at the United Nations (UN) in September 2016, only the fourth time that the UN General Assembly has met to discuss a health issue. This high level of political commitment provides a unique opportunity to develop and implement a coordinated global strategy for addressing the problem (UN, 2016). The committee concurs with the initial assessment of PACCARB and underscores the critical need to accelerate this work to ensure that milestones and deliverables of the National Action Plan are realized. Annex 3-2 provides additional detail on efforts to combat AMR and the National Action Plan.
Finding: The growing threat of antimicrobial resistance resulting from poor stewardship, weak surveillance systems, and a lack of
potential new therapeutics will be a major threat to the entire global community—in terms of both lives lost and impacts on the global economy—in the next 10 years.
A NEW APPROACH TO MEETING THE CHALLENGES OF GLOBAL HEALTH SECURITY
Despite many efforts at the global, regional, national, and community levels, the world is no safer now from infectious diseases than it was 20 years ago when the Institute of Medicine report America’s Vital Interest in Global Health was written. By virtue of their unpredictability and global effect, infectious diseases remain a perpetual challenge for the global community (Fauci and Morens, 2012). Since 1997, each U.S. presidential administration has been faced with an emerging or reemerging infectious disease that assumed high political priority, including HIV/AIDS, H5N1 influenza, SARS, MERS-CoV, Ebola, and Zika (Fauci, 2017). More recently, AMR received high-level attention from the UN as a global crisis (UN, 2016), and, as described earlier in Box 3-1, the largest outbreak of influenza A (H7N9) to date is currently occurring in China (Iuliano, 2017). Whether the challenge is attributable to limitations of the design and methods employed or the vision and funding for programs being too short-sighted and ad hoc, the United States needs to reorient programs and platforms to truly protect U.S. citizens, at home and abroad, from threats to their health and safety and the corresponding economic consequences. This reorientation needs to focus on preparing to prevent and preparing to respond, both of which require strong coordination and innovation while building resilience across all sectors.
Preparedness and Disaster Risk Reduction
The first need is for intentional stewardship of a true preparedness agenda. Building strong public health systems becomes more difficult each year with declining funding. The United States needs to take a more proactive approach to being prepared and reducing the risk of public health emergencies.
Mitigation Through Building Capacity
Parallel to this shift of focus on adequate and forward-looking funding, capacity building and outbreak prevention need to be prioritized. Since the Ebola outbreak, numerous reports have been written that advocate for building country capacity and creating resilient health systems in developing countries to enable better responses in the future. Domestically, the
Federal Emergency Management Agency (FEMA) began shifting its priorities from disaster response to mitigation and prevention, finding that for every $1 it invests in mitigation, it saves $4 in response (MMC, 2005). The agency now has begun incorporating incentives into its frameworks and funding for localities that can demonstrate investment in mitigation. This same concept can be applied to investments in global health security through a lens of disaster risk reduction (see Box 3-6). Effective strategies for comprehensively building resilient health systems in low-resource settings remain elusive. However, disaster risk reduction (DRR) can make it possible to address the challenge incrementally through such goals as increasing health workforce capacity and building resilience.
The 2015 Sendai Framework for Disaster Risk Reduction calls for investing in DRR for resilience through cost-effective measures that can save lives, reduce losses, and enhance economic and social well-being (UNISDR, 2015). Such measures include strengthening the design and implementation of inclusive policies through engagement with the community, such as by improving access to basic health care, food security, housing, and education, with the goal of eradicating poverty (UNISDR, 2015). Also necessary is coherence across systems and cooperation among the academic, scientific, governmental, and private sectors to promote capacity building. Viewing these efforts through a lens of DRR can synergize existing programs, create opportunities for partnership, and lead to greater systems capacity in a country. Through such partnerships as the GHSA, it is more cost-effective
to invest in building resilience and preventing outbreaks than to respond once an epidemic is out of control (World Bank, 2012). Supporting this concept, an international commission released a report in 2016 calling for building health system core capacities in developing countries and aligning them with the SDGs to better respond to health emergencies (GHRF Commission, 2016).
At Home and Abroad
In addition to building capacity at the source of an outbreak, achieving global health security for the United States will require a robust U.S. infrastructure to detect and respond to biological threats, whether naturally occurring, accidental, or intentional. Yet, a 2016 report issued by TFAH states that over the past 15 years, one-third of funds for health security and one-half of funds for health care system preparedness have been cut. In 2002, for example, health emergency preparedness funding was $940 million, and by FY2016 it had decreased to $660 million (Segal et al., 2016)—this despite the constant emergence of threats that the U.S. health infrastructure has often just barely avoided. Similarly, annual funding for health care system preparedness has been reduced to just $255 million nationally, an amount intended to support every hospital in the country in being prepared for disasters. As noted earlier, these preparedness amounts are moderate, yet whenever public health emergency or outbreak occurs, large amounts of funding are directed toward response. Indeed, the money the United States has spent on just five outbreak responses since 2005 exceeds the combined spending on public health and health care preparedness capacity building efforts in that same time period (see Figure 3-2).
A report from the Blue Ribbon Study Panel on Biodefense recommends that Public Health Emergency Preparedness cooperative agreements for state and local infrastructure be funded to authorized levels or the president’s request, whichever is higher (Blue Ribbon Study Panel on Biodefense, 2015). Although this recommendation was implemented through the Consolidated Appropriations Act of 2016, neither President Obama nor Congress returned funding to levels that existed following the 2001 anthrax attacks (Blue Ribbon Study Panel on Biodefense, 2016). The committee believes that now more than ever, sustainable and adequate funding is needed to build readiness into public health and health care infrastructure, and that appropriate funding levels for this purpose are those that were in place in the initial years of the Public Health Security and Bioterrorism Response Act of 2002. This assessment is supported by those of other experts who call for funding levels to return to FY2006 levels, or roughly $1 billion (Watson et al., 2017).
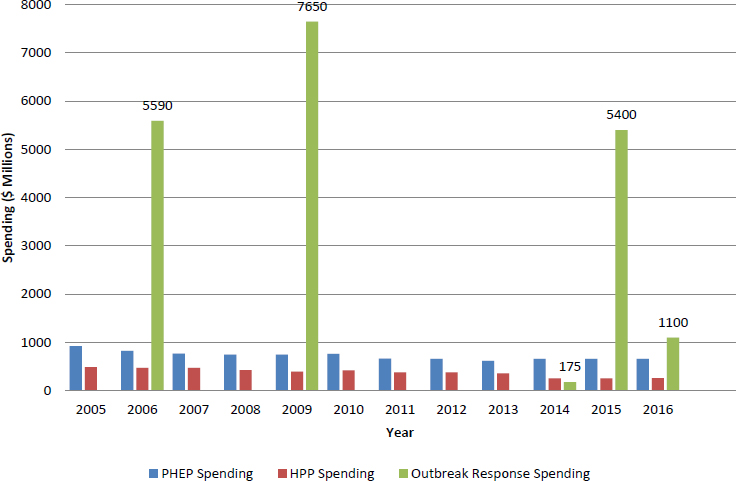
NOTE: HPP = Hospital Preparedness Program; PHEP = Public Health Emergency Preparedness.
SOURCES: Appropriations Committee, 2016; BARDA, 2007; Kates et al., 2015; Levi et al., 2015b; Segal et al., 2016; White House, 2009, 2014a.
Finding: Funding for preparedness has decreased dramatically since the Public Health Security and Bioterrorism Response Act was enacted in 2002. In fiscal year 2016, funding for the Public Health Emergency Preparedness program decreased from its initial level of $1.03 billion to $660 million, and funding for the Hospital Preparedness Program decreased from an initial level of $515 million to $255 million.
A Well-Coordinated Response
Although strong and prepared health systems, both in the United States and abroad, are of paramount importance for identifying and containing the next outbreak, some level of response capability will always be necessary. As discussed above, however, the funding needed for response can be reduced by investments in prevention and preparedness. The direct costs of treating just two Ebola patients in the United States at the specialty
center in Nebraska, for example, were estimated at more than $1 million (Gold, 2014). If mitigation and prevention efforts can halt an outbreak at the source, before it extends beyond a region, these costs are less likely to be incurred. For the United States, the current approach to organizing response is inadequate, and a better system for disbursing response funds is long overdue.
U.S. Interagency Coordination
During the Ebola outbreak, the United States contributed key resources and critical global leadership in a time of crisis. However, many suggestions have been made since then for how to better execute such a massive response. First, no response framework currently exists to guide agencies during this type of international event (similar to FEMA’s domestic National Response Framework); thus, there is no clear leader for the United States in an international health emergency. Creation of an international response framework would provide a command structure and an awareness of roles and responsibilities for the agencies involved, including the blending of international and domestic responses. The success of a U.S. response is dependent on the strengths of each agency working in parallel—the logistics of the U.S. Department of Defense (DoD); the policy of HHS; the coordination and international authorities of the U.S. Department of State; the country-level knowledge of USAID and CDC; and the wealth of expertise from the private sector, NGOs, and academia. The Ebola response initially was chaotic and lacking in coordination until the White House appointed a czar to direct it. Although this was a step in the right direction, there were pitfalls that could have been avoided from the beginning. Moreover, simply selecting a czar every time a new outbreak occurs prevents the development of a longitudinal knowledge base that can be drawn on in future public health emergencies.
The 2016 report of the Blue Ribbon Study Panel on Biodefense also identifies this problem with the overall U.S. strategy, and calls for a Biodefense Coordination Council in the office of the vice president (Blue Ribbon Study Panel on Biodefense, 2016). As of the release of this report, that recommendation has yet to be implemented. Echoing this need for high-level coordination, other experts have recommended a dedicated leadership position and office to lead health security efforts (Watson and Watson, 2017). Options to this end include creating a department or office in one of the agencies involved in a response or creating an interagency working group. However, challenges arise with respect to the politics of such a coordinating role and the authority needed to drive a massive, multifaceted response. USAID’s Office of Foreign Disaster Assistance (OFDA) assumes this coordinating role for the U.S. response during nonhealth emergencies,
such as earthquakes and famines in other countries, but typically is not activated for health emergencies (although a disaster assistance response team [DART] was deployed during the 2014 West Africa Ebola outbreak) (Gavi, 2014). Expanding the mandate of OFDA and the DART capability could be a mechanism for the necessary coordination. Yet given the breadth of expertise needed during a complex health emergency and the difficulties of coordinating so many agencies, the committee believes a strong coordinating body is needed for health emergencies that has appropriate authority, logistics, and subject matter expertise, as well as a dedicated budget.
Finding: Although multiple agencies bring unique expertise to a U.S. government–led response, it is difficult to coordinate an urgent plan during a crisis without strong leadership, a well-defined chain of command, and an adequate budget.
Sustainable Funding
Though preparedness has proven a difficult agenda for which to compel resources, once an emergency does occur, funding, often in large amounts, is directed retroactively to that issue. By this point, most of the damage has already been done, and clinicians, epidemiologists, researchers, and other stakeholders are scrambling to catch up with the emergency. The nation simply cannot afford to stand by while critical funds to fight these outbreaks are held back. After 7 months of disagreement and delay in approving President Obama’s request for $1.9 billion in Zika funding, for example, Congress finally approved $1.1 billion with the passage of the Zika Response Appropriations Act of 201613 (Wexler et al., 2016). Until then, agencies were forced to shift funds from other accounts for Zika-related activities, including borrowing from the Ebola supplemental funding and from CDC’s state-level emergency public health care preparedness account (Epstein and Lister, 2016; Kodjak, 2016).
Many experts have called for a standing public health emergency fund. The committee agrees with this recommendation; however, it is important to understand that this funding would be reserved for response activities only. Multiple respondents from the information gathering conducted by the committee (explained in Chapter 1) reported that global budgets for fighting diseases such as TB and malaria can lapse when large-scale outbreaks occur because money is redirected. A lack of secure funding for outbreak response prevents—and, the committee believes, sometimes reverses—progress in other global health arenas. Money to address an outbreak once the United States is in response mode is important and nec-
___________________
13 Zika Response Appropriations Act, H.R. 5243. 2016.
essary, but carving it out of existing pools of funds dedicated to important ongoing health issues would be imprudent, and could even seed the risk for a separate future outbreak. In a 2016 letter, PCAST recommended that Congress establish a public health emergency response fund14 of at least $2 billion, modeled after the U.S. Disaster Relief Fund for FEMA (PCAST, 2016). FEMA’s Disaster Relief Fund is funded annually, and unused funds from the previous fiscal year are carried over to the next. The recommended public health emergency response fund would likewise consist of funds that would carry over across years and could be replenished by routine and emergency appropriations. Access to the funds would be contingent on the express authorization of the President or the joint agreement of the secretaries of HHS and the U.S. Department of Homeland Security (DHS) (PCAST, 2016). The committee, along with other stakeholders (Watson et al., 2017), concurs with this recommendation, supporting the rapid mobilization of federal responses across the interagency community that plays a leading role in these events.
Finding: When an emergency does occur, funding for response is mired in bureaucratic processes, so that the funds are not available in a timely manner, but are often eventually released in amounts that far outweigh what is requested to prevent the emergency.
Innovation Agenda: Getting Ahead of the Pathogens
Budget caps and annual appropriations have challenged global health research and development funding, which in turn can compromise agencies’ ongoing efforts when they are forced to plan the development of critical medical products just 1 year at a time. Additionally, for such diseases as Ebola and Zika and other emerging threats, funding for research and development of critical medical products, including vaccines and therapeutics, is highly reactionary. Unless money is invested up front, researchers and agencies will constantly be scrambling to get ahead of an outbreak, and industry will always consider the risks of becoming involved. Like the challenge of antimicrobial resistance, these problems cannot be solved after a threat has emerged.
___________________
14 According to the PCAST letter, “There is a Public Health Emergency Fund that was authorized in 1983 and placed at the disposal of HHS, but it has not been replenished since 1993, despite repeated national level infectious disease emergencies. In addition to being moribund, it is specific to HHS and therefore more narrow than what we propose here. There is also a Public Health and Social Services Emergency Fund. This fund is used by the Assistant Secretary for Preparedness and Response to fund some preparedness activities, but it has not been used as a contingency or reserve fund” (PCAST, 2016).
The Public Health Emergency Medical Countermeasure Enterprise
Successfully developing and procuring vaccines and drugs that are needed during an outbreak will require forward thinking and exploration of unique solutions that may not be risk-free. To help coordinate the efforts of the federal government, in 2006 HHS established the Public Health Emergency Medical Countermeasure Enterprise (PHEMCE). Its mission is to coordinate efforts related to medical countermeasures with all interagency partners. Led by the Office of the Assistant Secretary for Preparedness and Response, core members include CDC, the National Institutes of Health (NIH), the U.S. Food and Drug Administration (FDA), the U.S. Department of Veterans Affairs (VA), DoD, DHS, and the U.S. Department of Agriculture (USDA). The PHEMCE has made much progress since its inception, but because of its focus on preparedness, its scope does not encompass all global health research and development. Thus, questions remain around information sharing related to rare or noncommunicable diseases (global health research and development is explored further in Chapter 7). Additionally, opportunities remain for improved communication and coordination even within the focus on medical countermeasures. The 2016 letter from PCAST calls in the near term for a new interagency entity charged with planning, coordination, and oversight of national biodefense activities, including development of a national biodefense strategy (PCAST, 2016). Creation of this entity would further encourage information sharing related to research priorities and areas of synergy for agencies involved in the development of medical countermeasures.
Leveraging Assets from the U.S. Department of Defense
A 2016 analysis led by Duke Global Health Institute found opportunities for using what works well more effectively and identified DoD’s medical research capabilities as having greatly underutilized potential for global health research and development (Yamey et al., 2016). In particular, DoD has both Army and Navy overseas laboratories in key strategic locations that facilitate international research collaboration, laboratory diagnostics, and surveillance. Because of their focus on locally relevant diseases and their reliance on locally hired research personnel, these laboratories have become integrated into public health efforts of the host nations, and can be assets in capacity building in those countries (Peake et al., 2011). To realize this potential, some have called for longer tours of duty at these laboratories and better communication with the academic and private sectors (Peake et al., 2011). The increase in defense spending pledged by the current administration—perhaps as much as $500 billion (Tiefer, 2016)—presents an opportunity to leverage DoD’s research capacity to improve
global health research and development. This idea was echoed at a 2015 workshop held by the National Academies of Sciences, Engineering, and Medicine on rapid medical countermeasures response (NASEM. 2016b), and further highlighted by DoD’s involvement in the development of an Ebola diagnostic test that became the first to receive emergency use authorization for use with U.S. citizens (BioFire Defense, 2014). While DoD’s mission is to protect military personnel, many of its research and development efforts can be leveraged to protect the civilian population, both domestic and international.
The Importance of Proactive Partnerships
The U.S. government plays a key role in promoting research and development for global health. While funding from the National Institutes of Health (NIH) and DoD is critical for research on the basic science of emerging infectious diseases, Biomedical Advanced Research and Development Authority (BARDA) funding is filling a vital gap. In addition, FDA ensures safety and efficacy throughout the research and development process. However, governments alone cannot be responsible for driving the global health research and development agenda forward, as the vast amounts of money required for the development of vaccine and therapeutics far outstrip the available government resources (see Table 3-2 for funding levels).
Partnerships are vital; the private sector is and will continue to be a key player, but it needs to be included from the initial design stage of projects and be viewed as a partner, not just a source of funds. The newly launched Coalition for Epidemic Preparedness Innovations (CEPI), for example, supported by the governments of Germany, Japan, and Norway plus the Bill & Melinda Gates Foundation and the Wellcome Trust, is investing $540 million to finance and coordinate the development of new vaccines to protect against infectious diseases, and views industry partnerships as a cornerstone operating principle (CEPI, 2017). Chapter 7 explores market incentives for accelerating research and development for medical product development in more detail, but these types of public–private partnerships and alternative business models are critical to making progress in many of these complex global health areas that lack a clear market.
Finding: Sufficient progress has not been made on the development of vaccines and diagnostics to successfully prevent, detect, and respond to these threats. No system exists to support this development beyond the interagency Public Health Emergency Medical Countermeasures Enterprise and the goodwill of industry partners, which is not a sustainable model.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
|---|---|---|---|---|---|---|---|
| NIH | |||||||
| NIAID | $4,818.28 | $4,775.97 | $4,490.71 | $4,256.33 | $4,401.20 | $4,417.56 | $4,715.70 |
| FIC | $69.98 | $69.32 | $69.49 | $65.55 | $67.58 | $67.58 | $70.12 |
| General Influenza Funding | $308.00 | $272.00 | $251.00 | $304.00 | $262.00 | $263.00 | $284.00 |
| BARDA | $32.00 | $378.00 | $415.00 | $415.00 | $413.05 | $473.00 | $522.00 |
| FDA | |||||||
| Pandemic Influenza | $46.70 | $43.60 | $30.00 | $32.10 | $38.30 | $38.30 | $40.00 |
| Antimicrobial Resistance | $30.20 | $27.70 | $44.10 | $25.90 | $26.80 | $32.50 | $47.30 |
| Advancing Medical Countermeasures Initiative | $0 | $170.00 | $20.00 | $21.80 | $24.60 | $24.50 | $24.50 |
| Life Sciences Biodefense Lab | $0 | $0 | $0 | $0 | $17.70 | $17.70 | $17.70 |
| TOTAL | $5,305.16 | $5,736.59 | $5,320.30 | $5,120.68 | $5,251.22 | $5,334.13 | $5,721.31 |
NOTE: BARDA = Biomedical Advanced Research and Development Authority; FDA = U.S. Food and Drug Administration; FIC = John E. Fogarty International Center for Advanced Study in the Health Sciences; NIAID = National Institute of Allergy and Infectious Diseases; NIH = National Institutes of Health.
SOURCES: Boddie et al., 2015; NIAID, 2015.
Reducing Impacts of Disaster Through Emergency Response Capacity in Low- and Middle-Income Countries
For LMICs, simple and cost-effective intervention strategies can reduce the effects of acute disasters. Emergency response capacity may appear to be a secondary priority in LMICs, but there are simple interventions that can build their resilience as well as their capabilities for emergency response. The implementation of the previously explained DRR principles, aimed at enhancing capabilities to minimize the impacts of mass casualty events and natural disasters, is a crucial need in all of these countries. In fact, more than 5 million people die each year as a result of injuries worldwide—1.7 times the number of fatalities that result from malaria, TB, and HIV/AIDS combined (WHO, 2014a). More than one-quarter of these deaths are road fatalities (WHO, 2017c), which occur predominantly in LMICs (Ning et al., 2016; WHO, 2009). Thus, these countries have a great unmet need for building trauma response capacity. Meeting this need will require the combined efforts and capabilities of research funding organizations, professional societies, NGOs, ministries of health, and governments. Regardless of whether injuries are caused by traffic crashes, earthquakes, or terrorist attacks, there are low-cost opportunities for increasing emergency response capacity to all hazards. While equipping these countries with functional modern trauma hospitals may not be feasible, providing basic training in essential surgical skills, expanding the workforce with the capacity to respond to trauma, and enabling more robust and rapid information sharing are cost-effective options that can help reduce the burden of injury and reduce mortality during a disaster (Acerra et al., 2009; King et al., 2015; Mock et al., 2012).
Increasing Trauma Capacity Through Training
Close to 2 million lost lives—one-third of all deaths due to injury—in LMICs could have been saved in 2008 by training a workforce to implement inexpensive, basic trauma care (Mock et al., 2012). Training nonphysicians in prehospital triage, for example, allows for the appropriate allocation of health care resources to respond to injuries as well as emergent diseases. Improving and standardizing care at the prehospital level has the potential to significantly decrease mortality at the earliest stages of disaster response.
These basic needs can be met by educating the workforce and disseminating guidelines and standardized protocols of care to create elementary but cost-effective systems of emergency and trauma care. The WHO Essential Trauma Care Project could be used to provide first responders with minimal training in simple life-saving care (Acerra et al., 2009; Mock et al., 2006). LMICs, in collaboration with such institutions and agencies as
DoD, NIH, and USAID, are poised to design and implement programmatic interventions and capacity-building programs tailored to the local and regional needs of poor communities and thereby develop more resilient health systems.
A Role for the U.S. Department of Defense
DoD recognizes the logistical impossibility of maintaining force readiness entailing continuously deployed medical facilities in all vulnerable regions of the world. Understanding this limitation, DoD has achieved tremendous gains in trauma care on the battlefield over the last decade that have had a dramatic impact on survival rates among warfighters (Mabry, 2015). Deployed medics and physicians often are depended upon to operate outside of their areas of expertise (NASEM, 2016a), a task-shifting approach that can be applied in low- and middle-income settings. Thus, with the ultimate goal of saving every injured warfighter on the battlefield, DoD has developed a rapid and nimble learning health system. Through an approach termed “focused empiricism,”15 it has identified interventions that work, and then adapts its clinical protocols to rapidly implement this new evidence.
This knowledge, however, does not always translate back to civilian health systems. Accordingly, a 2016 National Academies report was commissioned to advise the United States on how better to integrate the expertise and evidence from DoD into HHS and civilian hospitals. The authoring committee of that report found that prehospital military trauma care is often more advanced than what U.S. civilian emergency medical services protocols allow (Elster et al., 2013; NASEM, 2016a). Just as that committee identified an opportunity for disseminating DoD knowledge to the U.S. civilian health system, there is also an opportunity for knowledge gained from operating in austere conditions to be shared and implemented around the world.
Some key lessons from military health operations include using pain medications, such as ketamine, in the prehospital stage to minimize pain and postinjury mental health sequelae (NASEM, 2016a). Ketamine has
___________________
15 As defined by a recent National Academies report (NASEM, 2016a, p. 6), “Focused empiricism is a concept embraced by U.S. military medical leadership to capture its approach to process improvement under circumstances in which (1) high-quality data are not available to inform clinical practice changes, (2) there is extreme urgency to improve outcomes because of high morbidity and mortality rates, and (3) data collection is possible (Elster et al., 2013). A key principle of focused empiricism is using the best data available in combination with experience to develop clinical practice guidelines that, through an iterative process, continue to be refined until high-quality data can be generated to further inform clinical practice and standards of care.”
been found to be an extremely useful anesthetic in the global south because of its applicability in low-resource settings without access to electricity for ventilators or oxygen and its ease of administration by nonanesthetists. As shown by the military, it is also often used off-label as an analgesic and makes surgeries such as cesarean sections possible in many austere environments, leading WHO to designate it as an essential medicine. Combat gauze, a clotting agent used to stop blood loss more quickly, is another important life-saving advance used in the military, which has been found to be associated with a 93 percent survival rate (Ran et al., 2010). An easy and cost-effective intervention, combat gauze could be adopted by responders in LMICs. Inspiring the Stop the Bleed campaign in the United States, military first responders also carry proper tourniquets for hemorrhage control when assessing for evacuation to a higher-level facility. A study following the 2013 Boston Marathon bombing found that prehospital response to extremity exsanguination was inadequate, and that better transfer of information on techniques and tools from the battlefield is needed (King et al., 2015), which could be accomplished through proper use and administration of tourniquets. This same observation applies to global health programs and platforms.
The lessons learned from the battlefield about injury assessment, triage, and emergency care can be used to dramatically improve trauma care in LMICs. Building this capacity in U.S. partner countries would be beneficial not only for citizens of those countries but also for U.S. citizens traveling abroad. It also would support DoD interests abroad, as maintaining a civilian trauma system—especially during conflict—is an obligation of the military that helps it achieve its own strategic objectives. The better such a system functions, the fewer injured civilians will require treatment in military field hospitals. These efforts already occur, as the military understands the benefits of engaging with partner nations and building and supporting their health system capabilities (DHA, n.d.). In a recent example, U.S. Navy sailors provided Kenyan soldiers tactical combat medical training, including basic cardiopulmonary resuscitation; first aid; techniques for stopping massive bleeding; and the use of tourniquets, splints, and compression (DeNault, 2016). Similar training was provided to Ugandan soldiers as well (McDonald, 2015). Conducting workshops for local communities that provide such training can improve their ability to mitigate their burden of injury and trauma, as well as increase their readiness for disaster and build resilience. These types of training opportunities and information exchanges could become more prevalent through increased communication between DoD, the U.S. Department of State, and countries’ militaries or ministries of health, or through USAID in health systems–building activities.
Finding: An emergency response workforce can be developed through traditional public health training programs; rapid and nimble implementation of emerging evidence and best practices for providing effective and efficient health care; and leveraging the knowledge base developed in other networks, such as the U.S. military.
SUMMARY AND RECOMMENDATIONS
Wide-ranging threats to global health security influenced by resource scarcity, rapid urbanization, and inadequacies in stewardship of medications are poised to exploit the vulnerability of all countries, including the United States (Clapper, 2016; GAO, 2017; WHO, 2016a). These threats range from infectious disease spillover to pandemic influenza, to antimicrobial resistance, and are exacerbated by such vulnerabilities as degrading public health infrastructure, weak medical supply chains, and fragile states. It is critical for the United States to realize the severity of these threats and to take proactive measures to combat them by building capabilities and protections in a sustainable and cost-effective manner.
However, health preparedness systems and infrastructure (in the United States and abroad) are drastically underresourced (Boddie et al., 2015; Levi et al., 2015b). As a result, levels of preparedness are decades behind where they should be, making it difficult to meet the massive needs that arise when an emergency occurs. Funding for preparedness has decreased dramatically since the Public Health Security and Bioterrorism Response Act was enacted in 2002. In fiscal year 2016, funding for the Public Health Emergency Preparedness program decreased from an initial level of $1.03 billion in 2003 to $660 million (Levi et al., 2015b; Segal et al., 2016) and funding for the Hospital Preparedness Program decreased from an initial level of $515 million in 2004 to $255 million (Segal et al., 2016). Yet, once an emergency does occur, large amounts of funding are released, but typically not in a timely or systematic manner. For example, during the Ebola outbreak in 2014, which involved just four U.S. cases, the United States spent $1.1 billion on domestic response (Epstein et al., 2015), more than 120 percent of the nation’s entire annual budget for capacity building for health preparedness systems. Airport screening and follow-up of potentially sick passengers alone incurred costs totaling $119 million (CDC, 2015a). However, in response to the Zika virus the following year, the funding response was much different. After 7 months of disagreement and delay in approving President Obama’s request for $1.9 billion in Zika funding, Congress finally approved $1.1 billion with the passage of H.R. 524316
___________________
16 Zika Response Appropriations Act, H.R. 5243. 2016.
(Wexler et al., 2016). Until then, agencies were forced to shift funds from other accounts for Zika-related activities, including borrowing from the Ebola supplemental funding and from CDC’s state-level emergency public health care preparedness account (Epstein and Lister, 2016; Kodjak, 2016). Moreover, although multiple agencies bring unique expertise to a U.S. government–led response, it is difficult to coordinate an urgent plan during a crisis without strong leadership, a well-defined chain of command, and an adequate budget.
Finally, sufficient progress has not been made on the development of vaccines and diagnostics to successfully prevent, detect, and respond to these threats. No system exists to support this development beyond the interagency Public Health Emergency Medical Countermeasures Enterprise and the goodwill of industry partners, which is not a sustainable model. Adequately protecting U.S. citizens requires strong capabilities to detect the potential for a pandemic, ensure the availability of needed medical products, and provide the necessary capacity in the nation’s hospitals and health departments.
Conclusion: The current system for addressing health security threats described in this report is inadequate. A proactive, comprehensive approach would be more cost-effective and generate higher returns than ad hoc reactionary responses to individual events as they occur. The former approach can be enabled through the development of cross-cutting platforms, and a targeted systematic investment strategy (discussed in Recommendations 12 and 13 in Chapter 8) can enable this needed approach. Simultaneously, there is a need for improved coordination during an international public health emergency that combines the knowledge, networks, and assets of domestic and international health emergency response within the relevant U.S. government agencies and empowers action and decision-making through dedicated leadership and funding.
Conclusion: Health preparedness systems and infrastructure (in the United States and abroad) are drastically underresourced. As a result, levels of preparedness for health departments and hospitals are decades behind where they should be, making it difficult to meet the massive needs that arise when an emergency occurs. Addressing these inadequate funding levels is a critical priority.
Conclusion: An important positive step to improve rapid response capacity would be to implement the recommendation of the President’s Council of Advisors on Science and Technology to establish a public health emergency response fund, with adequate funding
in place, to be used only for response activities in declared public health emergencies.
Conclusion: To ensure that the drugs, vaccines, diagnostics, and devices critically needed to address health security threats are developed and available, a critical medical product development fund is required. This fund would support long-term, stable research and development to engage industry, academia, and other partners in the development of medical products for high-priority threats (based on the listing of the Public Health Emergency Medical Countermeasures Enterprise).
Recommendation 1: Improve International Emergency Response Coordination
The administration should create a coordinating body for international public health emergency response that is accountable for international and domestic actions and oversee preparedness for and responses to global health security threats. This body should have its own budget, experience with handling logistics, and the authority necessary to coordinate players across the government at the deputy secretary level. This coordinating body should do the following:
- Oversee the creation of an International Response Framework to guide the U.S. response to an international health emergency. Through this framework, this body would coordinate and direct activities involved in international response and preparedness, but would not duplicate functions already established in the Office of the Assistant Secretary for Preparedness and Response, the U.S. Centers for Disease Control and Prevention, the U.S. Agency for International Development, or the U.S. Department of Defense.
- Oversee three separate funding streams, dedicated to investments in preparedness, emergency response, and critical medical product development. The Office of Management and Budget should conduct an analysis to determine the appropriate levels for these three funding streams, commensurate with the associated risk, understanding that predictable and timely funds for these three purposes are critical.
- Align and coordinate efforts with effective multilateral organizations to reduce duplication and promote efficiency in building capacity and resilience in other countries.
The growing threat of antimicrobial resistance resulting from poor stewardship, weak surveillance systems, and a lack of potential new therapeutics will be a major threat to the entire global community—in terms of both lives lost and impacts on the global economy—in the next 10 years. While there has been progress toward Goal 5 of the National Action Plan, there remain challenges that hinder its full realization, including difficulties in providing incentives for the development of diagnostics and therapeutics. However, a particularly critical barrier is the lack of sufficient funds to advance the AMR agenda. While funds have been appropriated in recent years toward domestic efforts, there is very little money for international activities focused on AMR. Yet, with up to 30 percent of drugs being sold in LMICs found to be counterfeit (Cockburn et al., 2005; WHO, 2011b), there is a need for focused attention on safeguarding legitimate pharmaceutical supply chains that can complement a “One Health” approach to ensure proper stewardship of antibiotics and robust communication across the human and animal health sectors (CDC, 2017b), thereby reducing the spread of AMR.
Conclusion: A coordinated and dedicated global effort to address the threat of antimicrobial resistance is needed, with a focus on countries experiencing a high incidence.
Conclusion: It is essential to remain engaged and coordinated with domestic and international stakeholders, including the World Health Organization, the United Nations Secretary-General’s Committee on Antimicrobial Resistance, and the Global Health Security Agenda.
Recommendation 2: Combat Antimicrobial Resistance
The U.S. Department of Health and Human Services, the U.S. Department of Defense, the U.S. Department of Agriculture, and the U.S. Agency for International Development (USAID) should continue to invest in national capabilities and accelerate the development of international capabilities to detect, monitor, report, and combat antibiotic resistance. Efforts to this end should include the following:
- Enhance surveillance systems to ensure that new resistant microbial strains are identified as soon as they emerge.
- Assist low-income countries in improving infection control and antimicrobial stewardship.
- USAID should leverage current supply chain partnerships with other countries to strengthen antibiotic supply chains, thus reducing the use of illegitimate antimicrobials and improving drug quality.
- Incentivize the development of therapeutics (including alternatives to antibiotics), vaccines, and diagnostics for use in humans and animals.
While many low- and middle-income countries function in low-resource settings during steady-state times, disasters can plunge these countries into even more challenging and austere circumstances. While modern infrastructure often is not feasible in these countries because of high costs, smaller-scale steps entailing process innovation can be taken in communities to improve their ability to respond to disasters. Whether responding to more slowly evolving public health emergencies such as disease outbreaks or more immediate injury events such as road traffic accidents, earthquakes, or terror attacks, having a properly trained workforce in accordance with the principles of disaster risk reduction can lead to safer and more resilient communities. Such a workforce can be developed through traditional public health training programs; rapid and more nimble implementation of emerging evidence and best practices for providing effective and efficient health care; and leveraging of the knowledge base developed in other networks, such as the U.S. military. Enabling the right systems capacity to reduce risk, respond, and then iterate and innovate can allow for greater progress in a shorter period of time. After many years of insufficient siloed and ad hoc investments, this type of systems approach, information exchange, and country coinvestment and partnership would be a welcome change.
Conclusion: Simple yet effective strategies exist for reducing the risk of disaster for communities around the world. Employing the principles of disaster risk reduction when developing capacity for health care preparedness and response provides a framework for continuous learning and its iterative application to health care delivery systems.
Recommendation 3: Build Public Health Capacity in Low- and Middle-Income Countries
The U.S. Centers for Disease Control and Prevention, the National Institutes of Health, the U.S. Department of Defense, and the U.S. Agency for International Development should expand training and information exchange efforts to increase the capacity of
low- and middle-income countries to respond to both public health emergencies and acute mass casualty disasters. This training and information exchange should encompass core capacities such as surveillance, epidemiology, and disaster and injury care response, as well as enhanced capabilities to improve communication and information pathways for the dissemination of innovative findings.
ANNEX 3-1
THE 1918–1919 INFLUENZA PANDEMIC
The 1918–1919 influenza pandemic occurred toward the final years of World War I and infected up to 500 million people (one-third of the global population at the time), resulting in 50–100 million deaths (3–5 percent of the global population) (Jeffery and David, 2006). The war and the influenza pandemic were closely intertwined, and as a result, the disease spread globally and affected almost every country involved in the war. In addition to its global reach, the pandemic had a number of unique characteristics. Rather than appearing in the familiar annual pattern of influenza, the 1918–1919 pandemic took place in three waves that occurred in quick succession, the first of which was in the spring of 1918.
While identifying a point of origin for the pandemic is difficult given that it appeared to spread simultaneously throughout Europe, Asia, and North America, evidence suggests that it emerged in the United States (Barry, 2004) and spread to Europe when the United States entered the war (Byerly, 2010). During the first wave, illness rates were high, but death rates were close to normal. The second wave, occurring in the fall of 1918, spread the disease globally and was highly fatal, likely a result of the crowded conditions in training camps and trench warfare that enabled the virus to evolve. The third phase occurred in early 1919, and although less deadly, continued to spread the disease.
The occurrence of three pandemic waves in such quick succession was unprecedented, as was the age group the pandemic uniquely affected: young adults. Typically, the highest influenza mortality rates occur among the very young and the very old. However, the 1918–1919 pandemic also heavily affected those aged 20–40, an age group in which half of the deaths during the pandemic occurred.
Although 675,000 Americans were among the dead, the legacy of the 1918–1919 influenza pandemic has receded from memory in the United States, such that historians call it “America’s forgotten pandemic” (Garrett, 2007). This fading from memory is dangerous considering that learning from the past is instrumental in adequately preparing for the future. That the pandemic likely originated in the United States, moreover, serves as a reminder that such threats can emerge anywhere.
ANNEX 3-2
COMBATING ANTIMICROBIAL RESISTANCE
Global Community Efforts
The global community has given increased attention to the threat of antimicrobial resistance (AMR) in recent years as a result of multigovernment and multistakeholder declarations calling for immediate concerted global action to address this issue. The 2009 US-EU Summit Declaration established a Transatlantic Taskforce on AMR to strengthen collaboration between the United States and the EU in promoting the adequate use of antimicrobials for animal and human health, implementing prevention strategies in hospital and community settings, and developing new antimicrobials (TATFAR, 2014).
In 2014, the 67th World Health Assembly (WHA) requested that the World Health Organization (WHO) director general develop a global action plan to address the growing threat of AMR. In a tripartite collaboration with the World Organisation for Animal Health (OIE) and the Food and Agriculture Organization (FAO) of the United Nations (UN), and embracing the One Health approach, the World Health Organization (WHO) developed the Global Action Plan on AMR with the technical support of its Strategic and Technical Advisory Group on AMR (STAG-AMR) (WHO, 2015). This global action plan outlines five strategic objectives with corresponding actions for Member States, the Secretariat (composed of WHO, OIE, and FAO), and international organizations and other partners. The five objectives are
- to improve awareness and understanding of AMR through effective communication, education, and training;
- to strengthen the knowledge and evidence base through surveillance and research;
- to reduce the incidence of infection through effective sanitation, hygiene, and infection prevention measures;
- to optimize the use of antimicrobial medicines in human and animal health; and
- to develop the economic case for sustainable investment that takes account of the needs of all countries and to increase investment in new medicines, diagnostic tools, vaccines, and other interventions.
WHO called on Member States to develop national action plans aligned with these global plan objectives within 2 years of the plan’s endorsement by the WHA in May 2015. WHO, in collaboration with FAO and OIE,
prepared a manual to guide the development or refinement of these national plans and a monitoring and evaluation framework to help countries track the progress of the implementation of their national plans. As of the release of this report, only 31 countries had shared their national action plans for AMR with the WHO library, with only a few months remaining until the deadline in May 2017 (WHO, 2017a).
The U.S. National Action Plan
The U.S. National Action Plan for Combating Antibiotic-Resistant Bacteria was released in March 2015 (CDC, 2015c). The plan outlines in detail objectives; subobjectives; Year 1, Year 3, and Year 5 milestones; performance metrics; and implementation timelines for each goal in the National Strategy. These goals include the following:
- Slow the Emergence of Resistant Bacteria and Prevent the Spread of Resistant Infections.
- Strengthen National One-Health Surveillance Efforts to Combat Resistance.
- Advance Development and Use of Rapid and Innovative Diagnostic Tests for Identification and Characterization of Resistant Bacteria.
- Accelerate Basic and Applied Research and Development for New Antibiotics, Other Therapeutics, and Vaccines.
- Improve International Collaboration and Capacities for Antibiotic-Resistance Prevention, Surveillance, Control, and Antibiotic Research and Development.
As required by executive order, the Task Force for Combating Antibiotic-Resistant Bacteria submitted a report (PACCARB, 2016) assessing the progress made toward the proposed milestones for each of the National Action Plan goals after the first 180 days of the plan’s release. That report identified key actions taken to advance each of the five goals.
For goal 1, the report noted that both human and animal health stewardship efforts were under way: the Centers for Medicaid & Medicare Services revised the participation requirements for inpatient and long-term care facilities to include antibiotic stewardship programs, and the U.S. Food and Drug Administration (FDA) amended the veterinary feed directive (VFD) regulations to allow the use of a VFD drug only under the supervision of a licensed veterinarian. For goal 2, the U.S. Centers for Disease Control and Prevention (CDC), in collaboration with FDA, launched the AR Isolate Bank, a repository of samples of well-characterized resistance bacteria profiles. This repository will serve as a data source for industry and academia for the development of new diagnostics and treatment. For goal 3,
the National Institutes of Health (NIH) invested more than $11 million to support the first year of research for nine projects aimed at developing rapid diagnostic tools for resistant bacteria. Goal 4 proved to be one of the most challenging, as the pipeline for antibiotic development is quite small, with very limited incentives for industry. Nevertheless, the U.S. government continues to support discovery and early-stage development of new drugs. Finally, for goal 5, the U.S. government worked closely with international partners to support implementation of WHO’s Global Action Plan on AMR through its work with the Global Health Security Agenda (GHSA) AMR Action Package. Specifically, the GHSA AMR Action Package supports the development of national action plans; the development and strengthening of surveillance and laboratory capacity; and the development of new treatments, diagnostics, preventive measures, and systems to prolong the effective use of current therapies.
REFERENCES
Acerra, J. R., K. Iskyan, Z. A. Qureshi, and R. K. Sharma. 2009. Rebuilding the health care system in Afghanistan: An overview of primary care and emergency services. International Journal of Emergency Medicine 2(2):77-82.
Akil, L., and H. A. Ahmad. 2016. The recent outbreaks and reemergence of poliovirus in war and conflict-affected areas. International Journal of Infectious Diseases 49:40-46.
Allen, H. K., J. Donato, H. H. Wang, K. A. Cloud-Hansen, J. Davies, and J. Handelsman. 2010. Call of the wild: Antibiotic resistance genes in natural environments. Nature Reviews Microbiology 8(4):251-259.
Alwan, A. 2015. The cost of war. http://www.who.int/mediacentre/commentaries/war-cost/en (accessed December 15, 2016).
Appropriations Committee. 2016. Division B: Zika response and preparedness. https://www.appropriations.senate.gov/imo/media/doc/092216-CR-Zika%20Supplemental%20Summary.pdf (accessed February 19, 2017).
Atchon, K. 2016. Resurgence of poliomyelitis in Nigeria: A big blow to the world eradication efforts? MOJ Public Health 4(6).
BARDA (Biomedical Advanced Research and Development Authority). 2007. Report to Congress: Pandemic preparedness spending. Prepared in Response to Request in Conference Report 109-359.
Barrett, A. D. T. 2014. Economic burden of West Nile virus in the United States. The American Journal of Tropical Medicine and Hygiene 90(3):389-390.
Barrett, S. 2013. Economic considerations for the eradication endgame. Philosophical Transactions of the Royal Society B: Biological Sciences 368(1623):20120149.
Barry, J. M. 2004. The site of origin of the 1918 influenza pandemic and its public health implications. Journal of Translational Medicine 2(1):3.
Beaubien, J. 2016. How Boko Haram is keeping polio alive in Nigeria. http://www.npr.org/sections/goatsandsoda/2016/09/14/493755014/nigeria-has-to-wipe-out-polio-again (accessed February 14, 2017).
Beaubien, J. 2017. Brazil’s expanding yellow fever outbreak started with monkeys. http://www.npr.org/sections/goatsandsoda/2017/02/17/515444290/brazils-expanding-yellow-feveroutbreak-started-with-monkeys?utm_content=buffer23e6e&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer (accessed February 23, 2017).
BioFire Defense. 2014. Biofire defense receives emergency use authorization of FilmArray Ebola tests. Salt Lake City, UT.
Birdsall, N., and B. Leo. 2016. The White House and the world—practical proposals on gloabl development for the next U.S. President. Washington, DC: The Center for Global Development.
Blue Ribbon Study Panel on Biodefense. 2015. A national blueprint for biodefense: Leadership and major reform needed to optimize efforts. Washington, DC: Hudson Institute and Inter-University Center for Terrorism Studies.
Blue Ribbon Study Panel on Biodefense. 2016. Biodefense indicators: One year later, events outpacing federal efforts to defend the nation. Washington, DC: Hudson Institute, Potomac Institute for Policy Studies, and Inter-University Center for Terrorism Studies.
Boddie, C., T. K. Sell, and M. Watson. 2015. Federal funding for health security in FY2016. Health Security 13(3):186-206.
Brahmbhatt, M., and A. Dutta. 2008. On SARS type economic effects during infectious disease outbreaks. Washington, DC: World Bank.
Burkle, F. M. 2006. Globalization and disasters: Issues of public health, state capacity and political action. Journal of International Affairs 59(2):231-265.
Burkle, F. M. 2017. The politics of global public health in fragile states and ungoverned territories. PLOS Currents: Disasters 1.
Burns, A., D. van der Mensbrugge, and H. Timmer. 2008. Evaluating the economic consequences of avian influenza. Washington, DC: World Bank.
Byerly, C. R. 2010. The U.S. military and the influenza pandemic of 1918–1919. Public Health Reports 125(Suppl 3):82-91.
Cabezas, M. 2016. U.S. government budgets dedicated to combating antibiotic-resistant bacteria activities. Washington, DC: U.S. Department of Health and Human Services Office of Budget.
Cahill, M., Y. Yao, D. Nock, P. Armstrong, T. Andreadis, M. Diuk-Wasser, and R. Montgomery. 2017. West Nile virus seroprevalence, Connecticut, USA, 2000–2014. Emerging Infectious Disease Journal 23(4).
Casey, N. 2016. Hard times in Venezuela breed malaria as desperate flock to mines. New York Times. August 15.
CDC (U.S. Centers for Disease Control and Prevention). 2013a. Antibiotic resistance threats. Washington, DC: Centers for Disease Control and Prevention, HHS.
CDC. 2013b. CDC SARS response timeline. https://www.cdc.gov/about/history/sars/timeline.htm (accessed February 22, 2017).
CDC. 2014. Marburg hemorrhagic fever outbreak in Uganda. https://www.cdc.gov/vhf/marburg/outbreaks/uganda/2014-oct.html (accessed February 27, 2017).
CDC. 2015a. CDC’s Ebola response in the United States and abroad. https://www.cdc.gov/budget/documents/ebola/2015-ebola-and-gh-security-activities-factsheet.pdf (accessed December 15, 2016).
CDC. 2015b. Infographic: Field Epidemeology Training Programs in Africa. https://www.cdc.gov/globalhealth/infographics/fetp_africa.htm (accessed February 14, 2017).
CDC. 2015c. National Action Plan for Combating Antibiotic-Resistant Bacteria. Atlanta, GA: U.S. Centers for Disease Control and Prevention.
CDC. 2016a. 2014-2016 Ebola outbreak in West Africa. https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa (accessed December 15, 2016).
CDC. 2016b. Global activities. https://www.cdc.gov/onehealth/global-activities/index.html (accessed March 15, 2017).
CDC. 2016c. Global Health Security Agenda: Action packages. https://www.cdc.gov/globalhealth/security/actionpackages (accessed December 10, 2016).
CDC. 2016d. Global Health Security Agenda: Frequently asked questions. https://www.cdc.gov/globalhealth/healthprotection/ghs/faqs.htm#one (accessed December 15, 2016).
CDC. 2016e. How CDC invests in people: Developing disease detectives. Updates from the field Spring 2016(21).
CDC. 2016f. Outbreaks chronology: Ebola virus disease. https://www.cdc.gov/vhf/ebola/outbreaks/history/chronology.html (accessed February 22, 2017).
CDC. 2017a. Case counts in the US. https://www.cdc.gov/zika/geo/united-states.html (accessed March 6, 2017).
CDC. 2017b. One Health. https://www.cdc.gov/onehealth (accessed March 15, 2017).
Cegielski, J. P. 2010. Extensively drug-resistant tuberculosis: “There must be some kind of way out of here.” Clinical Infectious Diseases 50(Supplement 3):S195-S200.
CEPI (Coalition for Epidemic Preparedness Innovations). 2017. New vaccines for a safer world. http://cepi.net/sites/default/files/CEPI_2pager_03_Feb_17.pdf (accessed February 14, 2017).
Chen, L., R. Todd, J. Kiehlbauch, M. Walters, and A. Kallen. 2017. Notes from the field: Pan-resistant New Delhi metallo-beta-lactamase-producing Klebsiella pneumoniae—Washoe County, Nevada, 2016. Morbitity and Mortality Weekly Report 66:33.
CIDRAP (Center for Infectious Disease Research and Policy). 2017. Pan-resistant CRE reported in Nevada. http://www.cidrap.umn.edu/news-perspective/2017/01/pan-resistant-cre-reported-nevada (accessed February 14, 2017).
Clapper, J. 2016. Statement of James R. Clapper, Director of National Intelligence before the House Permanent Select Committee on Intelligence. Hearing on Worldwide Threat Assessment of the U.S. Intelligence Community. February 25, 2016.
Cockburn, R., P. N. Newton, E. K. Agyarko, D. Akunyili, and N. J. White. 2005. The global threat of counterfeit drugs: Why industry and governments must communicate the dangers. PLOS Medicine 2(4):e100.
COHAB (Co-operation on Health and Biodiversity Initiative). 2010. The importance of biodiversity on human health. https://www.cbd.int/doc/health/cohab-policy-brief1-en.pdf (accessed December 15, 2016).
Courage, K. 2014. How did Nigeria quash its Ebola outbreak so quickly? Scientific American, October 18.
Dembosky, A. 2014. Shortage of saline solution has hospitals on edge. http://www.npr.org/sections/health-shots/2014/06/22/323679204/shortage-of-saline-solution-has-hospitalson-edge (accessed March 3, 2017).
DeNault, T. 2016. U.S. sailors hold medical training with Kenyan defense forces. http://www.health.mil/News/Articles/2016/10/12/US-Sailors-hold-medical-training-with-Kenyan-Defense-Forces (accessed February 14, 2017).
DHA (Defense Health Agency). n.d. Building partner capacity and interoperability. http://www.health.mil/Military-Health-Topics/Health-Readiness/Global-Health-Engagement/Building-Partner-Capacity-and-Interoperability (accessed February 14, 2017).
Elster, E. A., F. K. Butler, and T. E. Rasmussen. 2013. Implications of combat casualty care for mass casualty events. Journal of the American Medical Association 310(5):475-476.
Epstein, S. B., and S. A. Lister. 2016. Zika response funding: Request and congressional action. Washington, DC: Congressional Research Service.
Epstein, S. B., S. A. Lister, A. Belasco, and D. J. Jansen. 2015. FY2015 funding to counter Ebola and the Islamic State (IS). Washington, DC: Congressional Research Service.
Fan, V. Y., D. T. Jamison, and L. H. Summers. 2016. The inclusive cost of pandemic influenza risk. Cambridge, MA: National Bureau of Economic Research.
Fauci, A. S. 2017. Keynote address. In Pandemic Preparedness in the Next Administration: Georgetown University Center for Global Health Science and Security and Harvard Global Health Institute.
Fauci, A. S., and D. M. Morens. 2012. The perpetual challenge of infectious diseases. New England Journal of Medicine 366(5):454-461.
FDA (U.S. Food and Drug Administration). 2016. FDA updates on saline drug shortage. http://www.fda.gov/Drugs/DrugSafety/ucm382255.htm (accessed February 14, 2017).
Fine, P., K. Eames, and D. L. Heymann. 2011. “Herd immunity”: A rough guide. Clinical Infectious Diseases 52(7).
Frieden, T. R. 2014. CDC telebriefing: CDC update on first Ebola case diagnosed in the United States, October 5, Atlanta, Georgia.
Frieden, T. R. 2016. Presentation by Dr. Thomas Frieden (CDC director). In Global Security Forum 2016: The Global Health Security Agenda–Its First Years and the Way Forward. Center for Strategic and International Studies.
GAO (U.S. Government Accountability Office). 2007. Drug safety: Preliminary findings suggest weakness in FDA’s program for inspecting foreign drug manufacturers. Washington, DC: Government Accountability Office.
GAO. 2017. Defense civil support: DOD, HHS, and DHS should use existing coordination mechanisms to improve their pandemic preparedness. Washington, DC: Government Accountability Office.
Garrett, T. A. 2007. Economic effects of the 1918 influenza pandemic: Implications for a modern-day pandemic. St. Louis, MO: Federal Reserve of St. Louis.
Gavi (Gavi, the Vaccine Alliance). 2014. Co-financing policy evaluation. http://www.gavi.org/results/evaluations/co-financing-policy-evaluation (accessed February 13, 2017).
Gebreyes, W. A., J. Dupouy-Camet, M. J. Newport, C. J. B. Oliveira, L. S. Schlesinger, Y. M. Saif, S. Kariuki, L. J. Saif, W. Saville, T. Wittum, A. Hoet, S. Quessy, R. Kazwala, B. Tekola, T. Shryock, M. Bisesi, P. Patchanee, S. Boonmar, and L. J. King. 2014. The global One Health paradigm: Challenges and opportunities for tackling infectious diseases at the human, animal, and environment interface in low-resource settings. PLOS Neglected Tropical Diseases 8(11):e3257.
Ghafoor, S., and N. Sheikh. 2016. Eradication and current status of poliomyelitis in Pakistan: Ground realities. Journal of Immunology Research V.2016, article no. 6837824.
GHRF Commission (Commission on a Global Health Risk Framework for the Future). 2016. The neglected dimension of global security: A framework to counter infectious disease crises. doi: https://doi.org/10.17226/21891.
GHSA (Global Health Security Agenda). 2017. Advancing the global health security agenda: Progress and early impact from U.S. investment. Washington, DC: Global Health Security Agenda.
Gold, J. 2014. Statement of Chancellor Jeff Gold, M.D. University of Nebraska Medical Center, Omaha, Nebraska before the Committee on Energy and Commerce Subcommittee on Oversight & Investigations (Date: 11/18/2014). Hearing on Update on the U.S. Public Health Response to the Ebola Outbreak. https://energycommerce.house.gov/hearings-and-votes/hearings/update-us-public-health-response-ebola-outbreak (accessed January 15, 2017).
Gostin, L. O., O. Tomori, S. Wibulpolprasert, A. K. Jha, J. Frenk, S. Moon, J. Phumaphi, P. Piot, B. Stocking, V. J. Dzau, and G. M. Leung. 2016. Toward a common secure future: Four global commissions in the wake of Ebola. PLOS Medicine 13(5):e1002042.
GPEI (Global Poliomyelitis Eradication Initaitive). n.d. Endemic countries. http://polioeradication.org/where-we-work/polio-endemic-countries (accessed March 3, 2017).
GU GHSS and HGHI (Georgetown University Center for Global Health Science and Security and Harvard Global Health Institute). 2017. Pandemic preparedness in the next administration. Georgetown University Center for Global Health Science and Security and Harvard Global Health Institute.
Hinshaw, D., and J. Bunge. 2014. U.S. buys up Ebola gear, leaving little for Africa. The Wall Street Journal, November 24.
Holgate, L. 2014. Presentation by NSC. In The Launch of the Global Health Security Agenda. Center for Strategic and International Studies.
IFPMA (International Federation of Pharmaceutical Manufacturers & Associations). 2016. Declaration by the pharmaceutical, biotechnology and diagnostics industries on combating antimicrobial resistance. Davos, Switzerland: International Federation of Pharmaceutical Manufacturers & Associations.
Inglesby, T., and A. Cicero. 2017. Protecting the nation from health security threats. Health Security 15(1):1-5.
Iuliano, A. D. 2017. Increase in human infections with avian influenza A (H7N9) virus during the fifth epidemic—China, October 2016–February 2017. Morbidity and Mortality Weekly Report 66.
Jeffery, K. T., and M. M. David. 2006. 1918 influenza: The mother of all pandemics. Emerging Infectious Diseases 12(1):15-22.
Jonas, O. 2014a. Global health threats of the 21st century. Finance and Development 51(4).
Jonas, O. 2014b. Pandemic Risk. Washington, DC: World Bank.
Kates, J., J. Michaud, A. Wexler, and A. Valentine. 2015. The U.S. response to Ebola: Status of the FY2015 emergency Ebola appropriation. Washington, DC: The Henry J. Kaiser Family Foundation.
Katz, R. 2016. Presentation for the National Academies of Sciences, Engineering, and Medicine. Paper read at Global Health and the Future of the United States: A Changing Landscape of Global Health, September 29, Washington, DC.
Kelesidis, T., I. Kelesidis, P. I. Rafailidis, and M. E. Falagas. 2007. Counterfeit or substandard antimicrobial drugs: A review of the scientific evidence. Journal of Antimicrobial Chemotherapy 60(2):214-236.
KFF (Kaiser Family Foundation). 2016. The U.S. government and global polio efforts. http://www.kff.org/global-health-policy/fact-sheet/the-u-s-government-and-global-polio-efforts (accessed March 10, 2017).
King, D. R., A. Larentzakis, and E. P. Ramly. 2015. Tourniquet use at the Boston marathon bombing: Lost in translation. Journal of Trauma and Acute Care Surgery 78(3):594-599.
Kodjak, A. 2016. Congress ends spat, agrees to fund $1.1 billion to combat Zika. http://www.npr.org/sections/health-shots/2016/09/28/495806979/congress-ends-spat-over-zika-funding-approves-1-1-billion (accessed December 15, 2016).
Labonte, R., K. Mohindra, and T. Schrecker. 2011. The growing impact of globalization for health and public health practice. Annual Review of Public Health 32:263-283.
Levi, J., L. M. Segal, R. Gougelet, and R. St. Laurant. 2015a. Investing in America’s health: A state-by-state look at public health funding and key health facts. Washington, DC: Trust For America’s Health.
Levi, J., L. M. Segal, D. A. Lieberman, K. May, and R. St. Laurant. 2015b. Outbreaks: Protecting Americans from infectious diseases. Washington, DC: Trust For America’s Health.
Littmann, J., and A. M. Viens. 2015. The ethical significance of antimicrobial resistance. Public Health Ethics 8(3):209-224.
Long, L., M. Fox, I. Sanne, and S. Rosen. 2010. The high cost of second-line antiretroviral therapy for HIV/AIDS in South Africa. AIDS 24(6):915-919.
Lowy, I. 2017. Leaking containers: Success and failure in controlling the mosquito Aedes aegypti in Brazil. American Journal of Public Health 107(4):517-524.
Mabry, R. 2015. Challenges to improving combat casualty survival on the battlefield. Military Medicine 179(5):477.
McDonald, O. 2015. Navy corpsmen, Ugandans work together to save lives. http://www.health.mil/News/Articles/2015/12/17/Navy-corpsmen-Ugandans-work-together-to-save-lives (accessed February 14, 2017).
McKibbin, W. J. 2004. Economic modeling of SARS: The G-Cubed approach. Sydney, Australia: The Lowy Institute for International Policy.
McKinney, M. L. 2002. Urbanization, biodiversity, and conservation: The impacts of urbanization on native species are poorly studied, but educating a highly urbanized human population about these impacts can greatly improve species conservation in all ecosystems. BioScience 52(10):883-890.
Meltzer, M. I., N. J. Cox, and K. Fukuda. 1999. The economic impact of pandemic influenza in the United States: Priorities for intervention. Emerging Infectious Diseases 5(5):659-671.
Michelle, G., L. Dominique, F. Pierre, and A. C. Maire. 2007. Conflict and emerging infectious diseases. Emerging Infectious Diseases 13(11):1625.
MMC (Multihazard Mitigation Council). 2005. Natural hazard mitigation saves: An independent study to assess the future savings from mitigation activities. Washington, DC: National Institute of Building Sciences, The Multihazard Mitigation Council.
Mock, C., M. Joshipura, J. Goosen, and R. Maier. 2006. Overview of the essential trauma care project. World Journal of Surgery 30(6):919-929.
Mock, C., M. Joshipura, C. Arreola-Risa, and R. Quansah. 2012. An estimate of the number of lives that could be saved through improvements in trauma care globally. World Journal of Surgery 36(5):959-963.
Molinari, N. A., I. R. Ortega-Sanchez, M. L. Messonnier, W. W. Thompson, P. M. Wortley, E. Weintraub, and C. B. Bridges. 2007. The annual impact of seasonal influenza in the US: Measuring disease burden and costs. Vaccine 25(27):5086-5096.
Morrison, J. S. 2014. Introduction. In The Launch of the Global Health Security Agenda. Washington, DC: Center for Strategic and International Studies.
MSF (Médecins Sans Frontières). 2014. The fight against antibiotic resistance. http://www.doctorswithoutborders.org/article/fight-against-antibiotic-resistance (accessed February 14, 2017).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016a. A national trauma care system: Integrating military and civilian trauma systems to acheive zero preventable deaths after injury. Washington, DC: The National Academies Press.
NASEM. 2016b. Rapid medical countermeasure response to infectious diseases: Enabling sustainable capabilities through ongoing public and private-sector partnerships: Workshop summary. Washington, DC: The National Academies Press.
NIAID (National Institute of Allergy and Infectious Diseases). 2015. Fiscal year 2015 fact book. Bethesda, USA: National Institute of Allergy and Infectious Diseases.
Ning, P., D. C. Schwebel, H. Huang, L. Li, J. Li, and G. Hu. 2016. Global progress in road injury mortality since 2010. PLOS ONE 11(10):e0164560.
Northam, J. 2014. Ebola protective suits are in short supply. http://www.npr.org/2014/10/07/354230895/ebola-protective-suits-are-in-short-supply (accessed December 15, 2016).
Nuzzo, J. B., and M. P. Shearer. 2017. International engagement is critical to fighting epidemics. Health Security 15(1):33-35.
Osterholm, M. T., and M. Olshaker. 2017. Deadliest enemy: Our war against killer germs. New York: Little Brown and Company.
PACCARB (President’s Advisory Council on Combating Antibiotic-Resistant Bacteria). 2016. Initial assessments of the national action plan for combating antibiotic-resistant bacteria. Washington, DC: U.S. Department of Health and Human Services.
Parpia, A. S., L. Ndeffo-Mbah Martial, N. S. Wenzel, and A. P. Galvani. 2016. Effects of response to 2014–2015 Ebola outbreak on deaths from malaria, HIV/AIDS, and tuberculosis, West Africa. Emerging Infectious Diseases 22(3):433-441.
Pauchard, A., M. Aguayo, E. Pena, and R. Urritia. 2006. Multiple effects of urbanization on the biodeversity of developing countries: The case of a fast-growing metropolitan city (Concepción, Chile). Biological Conservation 127:272-281.
PCAST (President’s Council of Advisors on Science and Technology). 2014. Report to the president on combating antibiotic resistance. Executive Office of the President, President’s Council of Advisors on Science and Technology.
PCAST. 2016. Biodefense letter to President Obama. Executive Office of the President, President’s Council of Advisors on Science and Technology.
Peake, J. B., J. S. Morrison, M. M. Ledgerwood, and S. E. Gannon. 2011. The Defense Department’s enduring contributions to global health. Washington, DC: Center for Strategic & International Studies.
Petersen, E., M. E. Wilson, S. Touch, B. McCloskey, P. Mwaba, M. Bates, O. Dar, F. Mattes, M. Kidd, G. Ippolito, E. I. Azhar, and A. Zumla. 2016. Rapid spread of Zika virus in the Americas—implications for public health preparedness for mass gatherings at the 2016 Brazil Olympic Games. International Journal of Infectious Diseases 44:11-15.
Petersen, L. R., P. J. Carson, B. J. Biggerstaff, B. Custer, S. M. Borchardt, and M. P. Busch. 2013. Estimated cumulative incidence of West Nile virus infection in US adults, 1999-2010. Epidemiology & Infection 141(3):591-595.
Pike, J., T. Bogich, S. Elwood, D. C. Finnoff, and P. Daszak. 2014. Economic optimization of a global strategy to address the pandemic threat. Proceedings of the National Academy of Sciences of the United States of America 111(52):18519-18523.
Pongsiri, M. J., J. Roman, V. O. Ezenwa, T. L. Goldberg, H. S. Koren, S. C. Newbold, R. S. Ostfeld, S. K. Pattanayak, and D. J. Salkeld. 2009. Biodiversity loss affects global disease ecology. BioScience 59(11):945-954.
Public Health Agency of Canada. 2017. Supply and distribution of flu vaccine in Canada. http://www.phac-aspc.gc.ca/im/supply-approvisionment-eng.php (accessed February 27, 2017).
Ran, Y., E. Hadad, S. Daher, O. Ganor, J. Kohn, Y. Yegorov, C. Bartal, N. Ash, and G. Hirschhorn. 2010. QuikClot Combat Gauze use for hemorrhage control in military trauma: January 2009 Israel defense force experience in the Gaza strip—a preliminary report of 14 cases. Prehospital and Disaster Medicine 25(06):584-588.
Review on Antimicrobial Resistance. 2014. Antimicrobial resistance: Tackling a crisis for the health and wealth of nations. London, UK: Review on Antimicrobial Resistance.
Review on Antimicrobial Resistance. 2016. Tackling drug-resistant infections globally: Final report and recommendations. London, UK: Wellcome Trust and UK Government.
Rey, M., and M. P. Girard. 2008. The global eradication of poliomyelitis: Progress and problems. Comparative Immunology, Microbiology, & Infectious Diseases 31(2-3):317-325.
Rice, S. E. 2016. Statement by National Security Advisor Susan E. Rice on the executive order on advancing the global health security agenda. The White House.
Ridley, D. B., X. Bei, and E. B. Liebman. 2016. No shot: US vaccine prices and shortages. Health Affairs (Millwood) 35(2):235-241.
Roos, R. 2012. CDC estimate of global H1N1 pandemic deaths: 284,000. http://www.cidrap.umn.edu/news-perspective/2012/06/cdc-estimate-global-h1n1-pandemic-deaths-284000 (accessed December 15, 2016).
Schmidt, C. W. 2016. Zika in the United States: How are we preparing? Environmental Health Perspectives 124(9):A157-A165.
Schnirring, L. 2017a. China confirms high-path H7N9 in market poultry. http://www.cidrap.umn.edu/news-perspective/2017/02/china-confirms-high-path-h7n9-market-poultry (accessed March 5, 2017).
Schnirring, L. 2017b. H7N9 analyses hint at genetic mutations, drug resistance. Center for Infectious Disease Research and Policy, February 20.
Segal, L. M., D. A. Lieberman, and K. May. 2016. Ready or not: Protecting the public’s health from diseases, disasters, and bioterorrism. Washington, DC: Trust For America’s Health.
Simpson, D. M., N. Sadr-Azodi, T. Mashal, W. Sabawoon, A. Pardis, A. Quddus, C. Garrigos, S. Guirguis, S. S. Zahoor Zaidi, S. Shaukat, S. Sharif, H. Asghar, and S. C. Hadler. 2014. Polio eradication initiative in Afghanistan, 1997-2013. Journal of Infectious Diseases 210 (Suppl 1):S162-S172.
TATFAR (Transatlantic Task Force on Antimicrobial Resistance). 2014. Progress report. Atlanta, GA: Transatlantic Taskforce on Antimicrobial Resistance (U.S. Department of Health and Human Services and European Commission).
The Canadian Press. 2014. Flu vaccine supply could be boosted by half-million doses. http://www.cbc.ca/news/health/flu-vaccine-supply-could-be-boosted-by-half-milliondoses-1.2491983 (accessed February 27, 2017).
The Energy and Commerce Committee: Subcommittee on Oversight and Investigations (113th Congress). Influenza: Perspective on current season and update on preparedness. February 6, 2013.
Tiefer, C. 2016. President Trump is likely to boost U.S. military spending by $500 billion to $1 trillion. Forbes, November 9.
UN (United Nations). 2014. World urbanization prospects. New York: United Nations Department of Economic and Social Affairs, Population Division.
UN. 2016. Draft political declaration of the high-level meeting of the General Assembly on antimicrobial resistance. New York: United Nations.
UNICEF (United Nations International Children’s Emergency Fund). 2014. Ebola virus disease: Personal protective equipment and other Ebola-related supplies. Washington, DC: United Nations International Children’s Emergency Fund.
UNISDR (United Nations International Strategy for Disaster Reduction). 2015. Sendai Framework for Disaster Risk Reduction. Geneva, Switzerland: United Nations Office for Disaster Risk Reduction.
UNISDR. 2016. What is disaster risk reduction? https://www.unisdr.org/who-we-are/what-is-drr (accessed March 17, 2017).
USP (U.S. Pharmacoepial Convention). 2017a. 2017. http://www.usp-pqm.org/results/pqm-in-numbers (accessed March 15, 2017).
USP. 2017b. Where we work. http://www.usp-pqm.org/where-we-work (accessed March 15, 2017).
Vergano, D., and L. Szabo. 2011. Long-term, universal flu shot on horizon. USA Today, July 26.
Viboud, C., and L. Simonsen. 2012. Global mortality of 2009 pandemic influenza A H1N1. The Lancet Infectious Diseases 12(9):651-653.
Watson, C. R., and M. Watson. 2017. Funding and organization of US federal biosecurity programs. Health Security 15(1):6-7.
Watson, M., J. B. Nuzzo, M. P. Shearer, and D. Meyer. 2017. Strengthening U.S. public health prepardness and response operations. Health Security 15(1):20-21.
WEF (World Economic Forum). 2017. The global risks report 2017. Geneva, Switzerland: World Economic Forum.
Wexler, A., S. Oum, and J. Kates. 2016. The status of funding for Zika: The President’s request, congressional proposals, and final funding. http://kff.org/global-health-policy/issue-brief/the-status-of-funding-for-zika-the-presidents-request-congressional-proposals-final-funding (accessed March 6, 2017).
White House. 2009. Letter from the President regarding H1N1. Washington, DC: The White House. https://obamawhitehouse.archives.gov/the-press-office/letter-president-regarding-h1n1 (accessed March 10, 2017).
White House. 2014a. Fact sheet: U.S. response to the Ebola epidemic in West Africa. Washington, DC. https://obamawhitehouse.archives.gov/the-press-office/2014/09/16/fact-sheet-us-response-ebola-epidemic-west-africa (accessed March 6, 2017).
White House. 2014b. National Strategy for Combating Antibiotic Resistant Bacteria. The White House.
White House. 2015. Fact sheet: Progress in our Ebola response at home and abroad. Washington, DC: Office of the Press Secretary.
Whitman, E. 2016. How Zika virus–carrying Aedes aegypti mosquitos were eradicated, and then returned. http://www.ibtimes.com/how-zika-virus-carrying-aedes-aegypti-mosquitoes-were-eradicated-then-returned-2309666 (accessed March 6, 2017).
WHO (World Health Organization). 2009. Global status report on road safety: Time for action. Geneva, Switzerland: World Health Organization.
WHO. 2011a. Strengthening response to pandemics and other public-health emergencies: Report of the review committee on the functioning of the International Health Regulations (2005) and on pandemic influenza (H1N1) 2009. Geneva, Switzerland: World Health Organization.
WHO. 2011b. Survey of the quality of selected antimalarial medicines circulating in six countries of sub-Saharan Africa. Geneva, Switzerland: World Health Organization.
WHO. 2014a. Injuries and violence: The facts. Geneva, Switzerland: World Health Organization.
WHO. 2014b. WHO declares end of Ebola outbreak in Nigeria. http://www.who.int/mediacentre/news/statements/2014/nigeria-ends-ebola/en (accessed December 15, 2016).
WHO. 2015. Global Action Plan on Antimicrobial Resistance. Geneva, Switzerland: World Health Organization.
WHO. 2016a. Antimicrobial resistance. http://www.who.int/mediacentre/factsheets/fs194/en (accessed February 14, 2017).
WHO. 2016b. Global tuberculosis report. Geneva, Switzerland: World Health Organization.
WHO. 2016c. Influenza (seasonal) fact sheet. http://www.who.int/mediacentre/factsheets/fs211/en (accessed February 15, 2017).
WHO. 2016d. WHO vaccine-preventable diseases: Monitoring system. 2016 global summary. http://apps.who.int/immunization_monitoring/globalsummary/estimates?c=BRA (accessed February 23, 2017).
WHO. 2017a. Antimicrobial resistance: Library of national action plans. Geneva, Switzerland: World Health Organization.
WHO. 2017b. Cumulative number of reported probable cases of severe acute resiratory syndrome (SARS). http://www.who.int/csr/sars/country/en (accessed February 27, 2017).
WHO. 2017c. Top 10 causes of death. http://www.who.int/mediacentre/factsheets/fs310/en/index1.html (accessed March 18, 2017).
World Bank. 2010. People, pathogens and our planet: Volume 1—towards a One Health approach for controlling zoonotic diseases. Washington, DC: World Bank.
World Bank. 2012. People, pathogens and our planet: Volume 2—the economics of One Health. Washington, DC: World Bank.
World Bank. 2015. Ebola: Most African countries avoid major economic loss but impact on Guinea, Liberia, Sierra Leone remains crippling. http://www.worldbank.org/en/news/press-release/2015/01/20/ebola-most-african-countries-avoid-major-economic-loss-butimpact-on-guinea-liberia-sierra-leone-remains-crippling (accessed February 27, 2017).
World Bank. 2016a. 2014–2015 West Africa Ebola crisis: Impact update. Washington, DC: World Bank Group.
World Bank. 2016b. Drug-resistant infection: A threat to our economic future (discussion draft). Washington, DC: World Bank.
World Bank. 2016c. The short-term economic costs of Zika in Latin America and the Caribbean. http://pubdocs.worldbank.org/en/410321455758564708/The-short-termeconomic-costs-of-Zika-in-LCR-final-doc-autores-feb-18.pdf (accessed March 6, 2017).
Wysocki, B. J., and S. Lueck. 2006. Just-in-time inventories make U.S. vulnerable in a pandemic: Low stockpiles at hospitals boost efficiency but leave no extras for flu outbreak. The Wall Street Journal, January 12.
Yamey, G., A. Thoumi, J. Gonzalez-Smith, C. Binanay, I. Bharali, Z. Johar, D. Ridley, and N. Chapman. 2016. Strengthening the United States government’s role in product development for global health. Durham, NC: Duke Global Health Institute and Duke Margolis Center for Health Policy.
This page intentionally left blank.
























































