5
Selected Hearing Technologies1
This chapter provides an overview of assistive products and technologies that mitigate the effects of hearing loss. After briefly reviewing the prevalence and severity of hearing loss and the extent of use of hearing aids, the chapter presents a taxonomy of assistive devices for hearing loss. It then turns to clinical considerations in addressing hearing loss. Issues of evaluation and monitoring, training and adaptation, and access to and availability of hearing products and technologies and related services are then examined in turn. The chapter ends with findings and conclusions.
Hearing loss can manifest at any time throughout life or be present from birth. It has two categories of causes: congenital and acquired. Congenital causes lead to hearing loss or deafness at birth or soon after. They include genetic syndromes; maternal rubella, syphilis, or certain other infections during pregnancy; low birth weight; lack of oxygen at birth; and severe jaundice in the neonatal period (birth to 1 month). Almost 50 to 60 percent of childhood hearing loss in developed countries is genetic (Morton and Nance, 2006). Acquired hearing loss can be caused by meningitis, measles and mumps, otosclerosis, chronic ear infections, fluid or infection in the ear (otitis media), tympanic membrane (ear drum) thickening or perforation, some head injuries and other traumas, excessive long-term exposure to noise, cerumen (wax) or foreign bodies blocking the ear canal, or aging (WHO, 2015).
Conditions such as otitis media, ear canal blockage, and some forms
___________________
1 Sections of this chapter draw heavily on a recent report titled Hearing Health Care for Adults (NASEM, 2016).
of otosclerosis can result in conductive hearing loss, which affects the outer or middle ear and is often treated medically or surgically (HLAA, 2017). Other conditions result in sensorineural hearing loss, which affects the inner ear, the auditory nerve, and more central auditory pathways; it is permanent and progressive and typically is not medically or surgically treatable. Therefore, common interventions for sensorineural hearing loss amplify sound and, if possible, improve the audibility of speech and other sounds. These interventions include hearing aids, assistive listening devices, aural rehabilitation services, and training to improve communication and coping strategies.
Age-related hearing loss, or presbycusis, is characterized by increased hearing thresholds (i.e., poorer ability to detect low-level sounds); impaired suprathreshold processing of higher-level sounds (including reduced frequency and temporal resolution); and impaired ability to understand speech, especially in noisy or complex listening environments (Yamasoba et al., 2013). Although the primary pathology of the process is unknown, it involves both intrinsic and extrinsic factors such as genetic mutations, degeneration of cellular structures in the cochlear lateral wall, age-related loss of auditory nerve fibers, and a lifetime of environmental exposures (especially to noise and ototoxic drugs) (Yamasoba et al., 2013). These factors affect the “ability of the inner ear and higher neural centers to process acoustic signals and effectively separate the primary speech signal from interfering speech and noise” (NASEM, 2016, p. 22). The functional consequences, regardless of which auditory pathways are affected, can include inability to hear low-level sounds, particularly high-frequency sounds; inability to understand subtle differences in spoken words (e.g., “I’ll see you Sunday” versus “I’ll see you someday”), especially in noisy environments; poorer ability to process acoustic information quickly relative to younger individuals; and difficulty identifying sources of sound (Roth, 2015; Yamasoba et al., 2013). There is no single etiologic pathway for age-related hearing loss since various factors influence its age of onset and severity. Individuals usually have symmetrical loss that is more apparent with high-frequency sounds and commonly more severe in men than in women (van Eyken et al., 2007).
OVERVIEW OF PREVALENCE AND SEVERITY OF HEARING LOSS AND USE OF HEARING AIDS
Prevalence
According to data from the National Health and Nutrition Examination Survey (NHANES), hearing loss is highly prevalent with aging. As shown in Figure 5-1, the prevalence of hearing loss rises with age from 0.3 percent
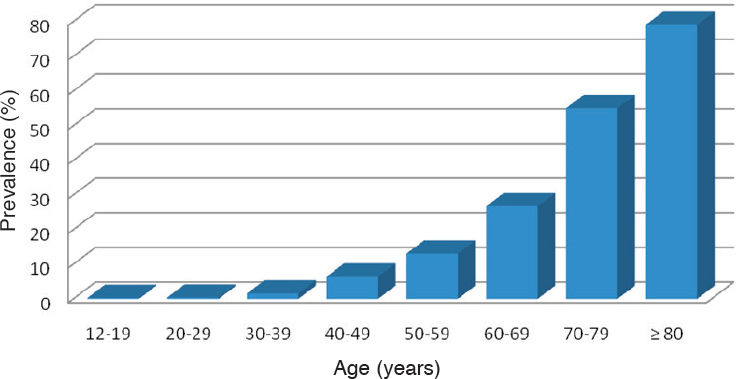
NOTE: Hearing loss is defined by a pure tone average (PTA) of 0.5-4 kHz thresholds in the better-hearing ear of greater than 25 dB.
SOURCE: Data from Lin et al., 2011d.
among those aged 12 to 19 to 79 percent among those aged 80 and older (Lin et al., 2011d). True population prevalence is likely underestimated because NHANES does not include data on individuals in assisted care facilities, group homes, or nursing homes or on individuals who were unable to come to the mobile examination center. NHANES data also show that 30 million individuals who are 12 and older have bilateral hearing loss, while 48 million have poor hearing in at least one ear (Lin et al., 2011d).
In the Epidemiology of Hearing Loss Study cohort, conductive hearing loss was present in 8 percent of participants; 0.2 percent had a history of otosclerosis (an uncommon but disabling form of hereditary hearing loss that can be aggravated by pregnancy, becomes disabling in midlife, and in older age is functionally complicated by presbycusis); and 1.9 percent reported the onset of the impairment before age 20 (Cruickshanks et al., 1998). Most participants with hearing loss had bilateral symmetrical loss, which is consistent with sensorineural hearing loss acquired in adulthood being the predominant type among adults.
Severity
Studies generally use a clinically significant cut point for defining hearing loss, which includes any hearing loss that is mild or greater (i.e., above
25 dB). However, the severity of the loss is a critical factor affecting the extent of its impact on communicative functioning and potential working capacity. Adults with a mild hearing loss, for example, may note only occasional communication problems in settings with background noise, while those with a severe to profound hearing loss may have trouble even in face-to-face conversation in a quiet room. The standardized prevalence of hearing loss by severity in individuals aged 12 and older is reported by Goman and Lin (2016) based on NHANES data from 2001 to 2010. Table 5-1 shows that most individuals with hearing loss had a mild loss, with moderate or greater losses becoming more prevalent with increasing age. The Blue Mountains Hearing Study also found that the severity of hearing loss increased with age (Mitchell et al., 2011), but again, the most common level of loss was mild, in this case until the oldest age group of 85 and above (Mitchell et al., 2011).
Extent of Hearing Aid Use
Compared with the prevalence of hearing loss in the United States, the prevalence of hearing aid use is low (see Table 5-2). In NHANES, 1999-2006, audiological testing was conducted in a sample of participants aged 50 to 69 from 1999 to 2004 and was conducted in all participants aged 70 and older in 2005. Using these data, Chien and Lin (2012) found that approximately 3.8 million, or 14.2 percent, of individuals in the United States who had hearing loss wore hearing aids (see Table 5-2). An earlier study (Lin et al., 2011c) found a strong relationship between hearing aid use and severity of hearing loss: 3 percent of those with mild loss, 40 percent of those with moderate loss, and 77 percent of those with severe loss wore a hearing aid regularly (Lin et al., 2011c). Other variables, such as college education and exposure to leisure noise, but not race/ethnicity, age, sex, or income, were significantly associated with hearing aid use (Lin et al., 2011c).
In the Epidemiology of Hearing Loss Study, current hearing aid use was 14.6 percent among individuals with hearing loss, while former use was 6 percent (Popelka et al., 1998). Current use was 33 percent among participants reporting significant communication problems and handicaps2 and 32 percent among those with moderate to severe loss (Popelka et al., 1998). Hearing aid use was associated with factors that included severity of hearing loss, older age, college education, poor performance on word recognition tests, and self-reported hearing loss and handicap. Similar low use of hearing aids was seen in the adult children of participants in the
___________________
2 Significant communication problems and handicaps refer to a Hearing Handicap Inventory for the Elderly (screening version) score greater than 8 (Popelka et al., 1998).
Epidemiology of Hearing Loss Study: 4 percent for those with mild loss and 23 percent for those with moderate to severe loss (Nash et al., 2013).
Although NHANES data demonstrate no differences in hearing aid use by race/ethnicity, this may be due to the low number of Hispanics/Latinos enrolled in the study (Nieman et al., 2016). Among those Hispanics/Latinos that were enrolled, hearing aid use was less than 10 percent (Lee et al., 1991). Even among individuals in the study with hearing loss more severe than mild (pure tone average greater than 40 dB), hearing aid use was low, at 5 percent among men and 11 percent among women.
TAXONOMY
Treatment for hearing loss includes hearing products and technologies (described below)3 and auditory rehabilitation and counseling. The products and technologies differ based on various factors, including type of hearing loss, unique needs in daily life, personal preferences, and financial means.
Hearing Aids
Hearing aids are defined by the U.S. Food and Drug Administration (FDA) as “any wearable instrument or device designed for, offered for the purpose of, or represented as aiding persons with or compensating for, impaired hearing.”4 Components of hearing aids include the microphone, analog-to-digital converter, digital sound processor, output transducer, and battery. Unlike glasses that can correct vision loss, current hearing aids cannot correct or restore normal hearing. Instead, they improve the audibility of soft sounds such as speech or music and ensure that other audible sounds do not interfere by becoming too loud. Customizing hearing aids to suit users’ needs is important. Greater satisfaction has routinely been documented in users whose hearing aids are fitted with real-ear probe microphone measurements and speech mapping as part of the fitting process (Cox and Alexander, 1999; Kochkin, 2009; Valente et al., 2006). Additionally, fewer postfitting adjustments are needed for patients whose fitting includes loudness scaling and speech-in-noise testing (Shi et al., 2007). Multiple studies have assessed the benefit of one versus two hearing aids and have found a preference for using two (Cox et al., 2011; Most et al., 2012; Noble and Gatehouse, 2006).
___________________
3 Medical and surgical treatments (such as cochlear implants), as well as auditory rehabilitation and counseling, were not included in the statement of task for this study (see Box 1-1 in Chapter 1).
4 21 CFR § 801.420.
| Hearing Loss Category and Age, y | Prevalence, % (95% CI) | Number With Hearing Loss (Millions) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Profound | Overall | Mild | Moderate | Severe | Profound | Overall | |
| Bilaterala | ||||||||||
| 12-19 y | 0.14 (0.04, 0.24) | 0.03b (0.00, 0.06) | …c | 0.00b (0.00, 0.01) | 0.18 (0.07, 0.28) | 0.05 | 0.01 | …c | <0.01 | 0.06 |
| 20-29 y | 0.34b (0.00, 0.88) | 0.07b (0.00, 0.20) | …c | …c | 0.42b (0.00, 0.97) | 0.15 | 0.03 | …c | …c | 0.18 |
| 30-39 y | 1.01b (0.18, 1.84) | 0.55b (0.00, 1.21) | 0.08b (0.00, 0.25) | …c | 1.64 (0.23, 3.06) | 0.41 | 0.23 | 0.03 | …c | 0.68 |
| 40-49 y | 6.05 (3.71, 8.40) | 0.48b (0.00, 1.01) | …c | …c | 6.53 (4.19, 8.88) | 2.46 | 0.20 | …c | …c | 2.65 |
| 50-59 y | 10.48 (7.34, 13.62) | 2.13 (0.79, 3.46) | 0.35b (0.00, 0.78) | 0.34b (0.00, 0.99) | 13.29 (9.76, 16.81) | 4.57 | 0.93 | 0.15 | 0.15 | 5.80 |
| 60-69 y | 19.94 (15.03, 24.84) | 5.85 (3.53, 8.17) | 0.76b (0.00, 1.70) | 0.25b (0.00, 0.75) | 26.80 (22.25, 31.35) | 6.92 | 2.03 | 0.27 | 0.09 | 9.31 |
| 70-79 y | 35.62 (31.03, 40.22) | 15.83 (13.63, 18.04) | 2.86 (1.60, 4.12) | 0.30b (0.02, 0.59) | 54.62 (49.27, 59.97) | 6.84 | 3.04 | 0.55 | 0.06 | 10.49 |
| ≥80 y | 36.02 (32.03, 40.01) | 37.92 (33.40, 42.44) | 6.97 (4.94, 9.01) | 0.56b (0.01, 1.10) | 81.47 (78.12, 84.82) | 3.98 | 4.19 | 0.77 | 0.06 | 9.01 |
| Total | 25.39 | 10.66 | 1.77 | 0.35 | 38.17 | |||||
| Loss in at least 1 ear (unilateral and bilateral) | ||||||||||
| 12-19 y | 1.18 (0.77, 1.59) | 0.46 (0.18, 0.74) | 0.31 (0.11, 0.51) | 0.01b (0.00, 0.03) | 1.96 (1.39, 2.54) | 0.39 | 0.15 | 0.10 | <0.01 | 0.65 |
| 20-29 y | 2.32 (0.92, 3.72) | 0.62b (0.00, 1.75) | 0.02b (0.00, 0.05) | 0.26b (0.00, 0.65) | 3.22 (1.38, 5.07) | 1.02 | 0.28 | 0.01 | 0.11 | 1.42 |
| 30-39 y | 3.50 (1.91, 5.09) | 1.38 (0.15, 2.62) | 0.30b (0.00, 0.76) | 0.25b (0.00, 0.63) | 5.43 (3.28, 7.58) | 1.44 | 0.57 | 0.12 | 0.10 | 2.23 |
| 40-49 y | 10.02 (7.41, 12.64) | 2.00 (1.01, 3.00) | 0.86b (0.00, 1.88) | 0.06b (0.00, 0.19) | 12.95 (9.85, 16.04) | 4.07 | 0.81 | 0.35 | 0.03 | 5.25 |
| 50-59 y | 21.30 (16.57, 26.02) | 5.49 (3.35, 7.63) | 0.82b (0.06, 1.57) | 1.08b (0.06, 2.10) | 28.69 (23.63, 33.74) | 9.30 | 2.40 | 0.36 | 0.47 | 12.52 |
| 60-69 y | 29.38 (24.46, 34.29) | 12.12b (8.62, 15.62) | 2.06 (0.61, 3.51) | 1.30b (0.29, 2.31) | 44.86 (40.79, 48.92) | 10.20 | 4.21 | 0.72 | 0.45 | 15.58 |
| 70-79 y | 37.51 (33.10, 41.92) | 21.14 (17.88, 24.40) | 7.47 (5.75, 9.19) | 2.04 (1.06, 3.01) | 68.15 (62.78, 73.53) | 7.21 | 4.06 | 1.43 | 0.39 | 13.09 |
| ≥80 y | 31.42 (26.75, 36.08) | 40.83 (36.42, 45.24) | 13.80 (11.13, 16.47) | 4.24 (2.49, 5.99) | 90.29 (87.20, 93.39) | 3.47 | 4.51 | 1.53 | 0.47 | 9.98 |
| Total | 37.10 | 16.99 | 4.61 | 2.03 | 60.73 | |||||
Note. Cl = confidence interval. Hearing loss was defined as a pure-tone average (at 0.5, 1, 2, and 4kHz) of above 25 dB hearing level. The sample size was n = 9648.
a Severity of bilateral loss is based on the better ear.
b The unweighted number of individuals in the categoryis < 10.
c No individuals with this hearing loss severity level were observed in the sample.
SOURCE: Goman, A. M., and F. R. Lin. 2016. Prevalence of hearing loss by severity in the United States. American Journal of Public Health 106(10):1820-1822. American Public Health Association.
TABLE 5-2
Prevalence of Hearing Aid Use Among Adults with Hearing Lossa >25 dB (95% CI)b
| Sex | Hearing Loss Severityc | Total | |||||
|---|---|---|---|---|---|---|---|
| Age, years | Male | Female | Mild (>25–40 dB) | Moderate or Greater >40 dB | Overall Prevalence of Hearing Aid Use | Number with Hearing Aids, millions | Number with Hearing Lossa >25 dB, millions |
| 50–59 | 4.3 (0–9.5) | 4.5 (0–13.5) | 2.7 (0–6.6) | 11.8 (0–27.5) | 4.3 (0–8.8) | 0.20 | 4.5 |
| 60–69 | 7.3 (2.5–12.1) | 7.2 (1.4–13.0) | 2.6 (0–5.2) | 23.9 (10.6–37.2) | 7.3 (3.6–10.9) | 0.44 | 6.1 |
| 70–79 | 21.1 (14.5–27.6) | 12.7 (6.0–19.5) | 3.4 (0.3–6.5) | 47.8 (37.0–58.6) | 17.0 (12.4–21.6) | 1.5 | 8.8 |
| 80+ | 28.1 (20.3–35.9) | 17.9 (11.2–24.7) | 3.4 (0–7.7) | 35.7 (28.7–42.7) | 22.1 (18.5–25.8) | 1.6 | 7.3 |
| Estimated total number of individuals with hearing aids and with hearing loss, respectively, in millions | 3.8c | 26.7 | |||||
NOTE: CI = confidence interval.
a Hearing loss defined as a speech-frequency pure tone average (PTA) of hearing thresholds at 0.5, 1, 2, and 4 kHz tones presented by air conduction in the better hearing ear of >25 dB.
b All values represent percent prevalence unless otherwise noted.
c Numbers do not sum to group total because of rounding.
SOURCE: Data from Chien and Lin, 2012.
Air-conduction hearing aids (discussed further below) capture sound vibrations through one or more microphones. The signal is treated, amplified, and played back through an earphone that is placed in the ear canal (Lorenzi and Chaix, 2016). These conventional hearing aids can be fitted behind the ear, in the ear, or in the ear canal. These various placements provide different levels of visibility and ease of control as well as different features (Consumer Reports, 2015; NIDCD, 2013).
Adults with mild to moderate sensorineural hearing loss typically have difficulty understanding speech, especially in noisy environments. When hearing loss is measured using a speech-in-noise task, the results may show that a more beneficial signal-to-noise ratio5 is required to understand speech for individuals with loss relative to those with normal hearing. The signal-to-noise ratio may be improved when a hearing aid fits well (i.e., is properly programmed) and is capable of improving speech audibility at higher frequencies. In some cases, however, well-fit hearing aids may not improve the signal-to-noise ratio and therefore do not improve speech recognition in noisy environments. In addition to hearing aids, hearing assistive technologies (discussed below) and auditory rehabilitation may be useful for individuals with mild to moderate hearing loss.
Hearing Aid Telecoil and Induction Loop Technologies
Telecoils are small copper coils that are available for a majority of hearing aids but not for all types and models. However, most consumers are unaware of this feature or the fact that it can be added6 (HLAA, 2016). Telecoils also can help in enhancing the performance of wired and wireless telephones.
Hearing induction loop technology7 consists of a telecoil in a hearing aid or neck loop receiver and earphones connecting wirelessly to a room’s sound system, which eliminates background noise and improves clarity of sound. The hearing loop, which is connected to the room’s sound system, is wired around the perimeter of the room. The telecoil in the hearing aid or the receiver transmits electromagnetic signals from the sound system.
___________________
5 Signal-to-noise ratio measures the signal strength relative to background noise (Rouse, 2016).
6 According to the Consumer’s Guide to Hearing Aids (HLAA, 2016), telecoils are available as a standard or an additional feature for a majority of hearing aids.
7 Further discussion of hearing induction loop technology is not provided since this technology is beyond the scope of the committee’s statement of task.
Hearing Assistive Technologies Beyond Hearing Aids
A variety of hearing assistive technologies beyond hearing aids can help individuals with hearing loss—particularly those whose loss is moderate to severe—connect to or receive information from communication channels such as a telephone or television or from sound systems in offices, classrooms, theaters, auditoriums, or other public spaces. These technologies range from products for personal and home use to systems made available in public spaces and for larger audiences to meet consumer needs, as well as to comply with requirements of antidiscrimination laws such as the Americans with Disabilities Act (ADA), which was revised in 2010 to include a number of requirements focused on individuals with hearing loss.
Personal Sound Amplification Products
Personal sound amplification products (PSAPs) include a wide range of devices currently classified by the FDA as designed to “amplify environmental sound for non-hearing impaired consumers” (FDA, 2013). Some PSAPs look very similar to hearing aids and may be a suitable amplification tool for those who cannot afford a hearing aid or are seeking a low-cost introduction to amplification. However, PSAPs are not meant to compensate for hearing impairment.
Wireless Connectivity in Hearing Aids
Wireless connectivity in hearing aids mitigates many communication issues through use of a remote microphone. When a speaker wears a remote microphone, background noise levels typically remain well below the signal of interest, the sources of reverberation are reduced, and the integrity of high-frequency speech sounds is maintained to a greater extent. Listening can thereby be enhanced in both quiet environments and those with background noise, in distance listening, and in listening to media (e.g., television, videos, music). Wireless connectivity systems are designed to work in conjunction with hearing aids. The systems are proprietary and require programming by an audiologist to ensure that they are recognized by hearing aids. They utilize a microphone and an auxiliary piece, often worn around the neck, to stream the sound from the external source to the user’s hearing aid(s). Although not available from all hearing aid manufacturers at present, direct to hearing aid couplings are becoming more readily available.
Frequency-Modulated and Infrared Technologies
Radio signals are used to transmit sound from a speaker’s microphone or other sound system in frequency modulated (FM) systems. FM may also be referred to as digital modulation (DM). Wireless FM transmissions can be processed by some hearing aids. In other cases, the user wears a receiver that is connected to earphones or a neck loop that converts the transmission to an electromagnetic signal that can be picked up by the telecoil in the user’s hearing aid (ASHA, 2017b; Chisolm et al., 2007; Kim and Kim, 2014). FM/DM systems are beneficial in one-to-one communication in noisy environments. They are also used in large gathering places such as theaters, museums, and auditoriums and can be used to transmit sound from radio, television, and other sources (ASHA, 2017b). When radio signals penetrate the walls of a room, mixed signals can result unless different frequencies are used. Although performance varies among users, FM/DM systems can help with better hearing in an environment with background noise (Thibodeau, 2014).
Infrared technologies entail using infrared light waves that must be transmitted via line of sight. Like FM systems, they may transmit to either a receiver and headphones or a neck loop and hearing aid telecoil. While infrared systems can contain the signal in a room and are subject to less interference from other signals relative to FM systems, they have a drawback in that the light waves they transmit can compete with natural light (Holmes et al., 2000; Kim and Kim, 2014).
Hard-Wired Microphone Systems
Some very basic microphone systems whose components are tethered together limit the user to a range of about 4 to 6 feet from the speaker and provide limited amplification of a speaker’s voice. These generic systems are not coupled to the user’s hearing aid(s). Despite their limitations, they are low-cost and easy-to-use systems that can be purchased from a hearing health care provider or at a consumer electronic venue and can be a suitable solution for some listening situations.
Captioning
Captioning, which can be done either on-site or remotely, involves converting discussions or programming into text that is displayed on a screen. It is usually provided for live events, such as sports events in real time, and can be projected through television and other media, through a website, or directly onto a screen visible in the location of the event. In 1993, the ADA required closed captioning for the auditory portion of programs
for all televisions 13 inches or larger (Holmes et al., 2000). Captioning also may be provided for telephones and may be used along with the Telecommunications Relay Service (TRS), discussed below.
Telecommunications Relay Service
The telecommunications relay service (TRS) is “a telephone service that allows persons with hearing or speech disabilities to place and receive telephone calls”8 (FCC, 2016). The Federal Communications Commission manages the program. The service uses operators, called communication assistants, who facilitate calls for individuals with hearing and speech impairments. To initiate a TRS call, an individual with such an impairment dials 711 using a teletypewriter or other text input device and then gives the communication assistant the number of the individual being called. The communication assistant acts as a link between the two parties by converting text to voice and voice to text. This service also allows individuals with hearing loss to speak directly to the people being called and hear their voice. Captioning in conjunction with TRS may be preferred by users who have some hearing capacity and can use their own voices, whereas people who employ sign language to communicate may prefer video relay technology used along with sign language interpreters.
___________________
8 There is no cost to the user for TRS.
Box 5-1 provides definitions of selected hearing technologies. More detailed information on the features and functionality of these devices is provided in Annex Tables 5-1 and 5-2, respectively, at the end of this chapter.
CLINICAL CONSIDERATIONS
Clinical considerations in addressing hearing loss include the functioning of affected individuals, particularly, in the present context, their functioning at work; the effectiveness of hearing aids and other assistive devices; and factors affecting the success of treatment.
Functioning
The World Health Organization has identified participation in work as one of the major areas of life (WHO, 2001). As the U.S. government increases the age at which an individual becomes eligible for Medicare, a larger number of adults will continue to work at later ages, which in turn will lead to a higher prevalence of hearing impairment in the workplace in the near future. Occupations today rely increasingly on communication skills, which places a greater burden on those suffering from hearing loss. Such issues as unemployment, underemployment, sick leave (due to stress), lower earning potential, and early retirement often are more pervasive among workers with hearing loss relative to their normal-hearing peers.
The U.S. Census Bureau reported an employment rate of 41.1 percent among adults of working age (21-64) with disabilities, compared with 79.1 percent of this age group without disabilities (Brault, 2012). Employment is also low among those who suffer from hearing difficulties (1,837) (Brault, 2012). One study found that hard-of-hearing professionals reported a sense of having lost their competitive edge and having been passed over for promotion or having missed job advancement opportunities as a result of their hearing loss (Tye-Murray et al., 2009). Nachtegaal and colleagues (2012) found a significant association between hearing loss and experiencing limitations in the kind or amount of work that can be performed, with the odds of experiencing such limitations increasing significantly with increases in the decibels of hearing loss. Another study found that sick leave was significantly higher (77 percent) among those with hearing loss relative to those with normal hearing (55 percent) because of “fatigue, strain and burnout” (Kramer et al., 2006). And according to Kochkin (2005), people with severe hearing loss earn $12,000 less per year than those with mild hearing loss.
Jennings and Shaw (2008) argue that the specific implications of hearing loss in the workplace are not fully understood because of the lack of research in this area. They note that the most pertinent experiences of workers with hearing loss on the job are mental distress, fatigue, need for
recovery after work, and lack of knowledge and job control. The authors suggest further that, aside from equipment and environmental management (appropriate hearing assistive technology), hard-of-hearing workers would benefit from a more favorable signal-to-noise ratio. Additionally, they assert, it is important for hard-of-hearing workers to gain knowledge of how to disclose their hearing loss, how to educate their coworkers to be supportive, how to become better advocates for themselves, and how to better understand their rights to accommodation under the law.
The workplace is a complex environment. Thus, for a hard-of-hearing employee’s abilities and limitations to be assessed and addressed adequately, a multilevel, multidisciplinary, and integrated approach is necessary. With such an approach, functioning and disability are seen as outcomes of interactions between a person’s health condition (hearing loss) and contextual factors. As described in Chapter 2, contextual factors are both environmental (room acoustics, noise levels, colleagues, tasks, schedules) and personal (age, cognitive capacity, coping styles, education). In using the International Classification of Functioning, Disability and Health (ICF) to determine the goals of a rehabilitation program for someone with hearing loss, it is essential to involve that person, who is the one most qualified to identify the activity limitations and/or participation restrictions to be addressed. In addition, the rehabilitation program, its goals, and the technology to be used to achieve those goals need to be formulated in functional terms specific to the client (Southall et al., 2010).
Studies have examined the links between hearing loss and falls or declines in physical functioning and hospitalization, although more research, particularly longitudinal studies, is needed in this area. Severe hearing loss was found to be associated with increased risk of falls in a study of retired workers (Girard et al., 2014); in cross-sectional data from NHANES (Lin and Ferrucci, 2012); and in observational data from the Health ABC study, which also showed increased risk of frailty (Kamil et al., 2016). Further, in a study examining hospitalization of participants in the Health ABC study, a higher incidence of hospitalization and annual rate of hospitalization were found among those older adults with hearing loss (Genther et al., 2015). Higher rates of decline in physical functioning also were seen in the Health ABC study among participants with hearing loss (Chen et al., 2015).
The longitudinal Blue Mountains Health Study evaluated the effect of hearing impairment on independence and use of support services. At the baseline hearing test visit, a total of 1,457 participants reported no use of community support services, no use of nonspouse family or friend support, or an inability to go out alone. The 5-year incidence analysis showed that all three of these factors increased with age. Nonetheless, the results showed that baseline hearing loss was not significantly associated with the 5-year incidence of these factors. Results also showed, however, that, relative to
people with normal hearing, those with moderate to severe hearing loss had a 2.7-fold increased risk of needing help from family and friends, indicating that individuals with these levels of hearing loss may have a greater need for support services relative to those without hearing loss.
Both the Wisconsin Longitudinal Study and the Medical Expenditure Panel Survey examined the impact of hearing on health care using self-reported hearing loss. In the Wisconsin Longitudinal Study, reports of difficulties and delays in accessing health care in the previous year were 1.85 times higher among individuals reporting than among those not reporting hearing loss (Pandhi et al., 2011). Results of the Medical Expenditure Panel Survey showed that individuals with hearing loss had better access to health care relative to those with other disabilities who experienced higher unmet needs due to environmental barriers (Horner-Johnson et al., 2014). Although several studies have reported longitudinal associations between hearing and mortality risk (Contrera et al., 2015; Fischer et al., 2014; Genther et al., 2015; Gopinath et al., 2013; Wahl et al., 2013), most have shown no association after controlling for confounding factors (Contrera et al., 2015; Genther et al., 2015; Wahl et al., 2013).
Effectiveness of Hearing Aids and Other Assistive Devices
More peer-reviewed studies have focused on the impact of hearing aid use among children relative to adults with hearing loss. As noted by Mäki-Torkko and colleagues (2001, p. 8), “only a few studies on hearing aid outcomes meet strict scientific criteria and even fewer studies correlate rehabilitation outcome with the degree of hearing impairment disability or handicap.” Although studies have examined the use of hearing aids and owners’ satisfaction with and barriers to their use, outcome measures used to assess the efficacy and effectiveness of hearing aids vary widely.
Studies of the effectiveness of hearing aids are primarily experimental studies examining the impact of specific technical aspects or components of the device using small numbers of study subjects; many have been focused on the technical rather than on the clinical or functional outcomes associated with hearing loss (Humes and Krull, 2012). There has been only one true randomized controlled trial of hearing loss treatment examining outcomes beyond measures of speech perception (Mulrow et al., 1990). This trial, which was conducted more than two decades ago, randomized 192 veterans into two groups: one with treatment (provision of a single monaural analog hearing aid) and one without. The results showed improved social and emotional function, communicative abilities, and cognitive function among the treatment group (Mulrow et al., 1990). These results, however, were not confirmed in a trial with a larger representative cohort that used more current hearing rehabilitative strategies (e.g., digital hearing aids)
and evaluated cognitive and other functional outcomes comprehensively with longer follow-up periods.
Some observational epidemiological studies have examined the association of hearing aid use with functional outcomes, but the results of these studies are difficult to interpret. For example, most studies have demonstrated a trend toward a positive association between self-reported hearing aid use and cognitive functioning, yet these studies have not yielded data on other key variables (e.g., years of hearing aid use, adequacy of hearing aid fitting and rehabilitation) that would affect the success of hearing loss treatment, as well as any observed associations (Amieva et al., 2015; Dawes et al., 2015; Lin, 2011; Lin et al., 2011a,b, 2013). It is important, moreover, to interpret results of observational studies with caution because individuals who use a hearing aid differ significantly from those who do not with respect to both measured and unmeasured factors. Therefore, a randomized controlled trial would help determine whether hearing rehabilitative strategies can affect functional outcomes.
Most prior studies of the efficacy/effectiveness of hearing aids have focused on speech or other audiologic outcomes and have compared the results for different hearing aids rather than hearing aids versus placebo or no treatment. These studies often have compared different versions of a technology, such as directional and omnidirectional microphones (e.g., Gnewikow et al., 2009; Hawkins and Yacullo, 1984; Keidser et al., 2013; Wu et al., 2013), multimemory and volume controls (e.g., Banerjee, 2011), noise reduction technologies (e.g., Oeding and Valente, 2013), and various types of circuits and compression options (e.g., Hawkins and Naidoo, 1993; Kokx-Ryan et al., 2015; Moore et al., 2001; Shanks et al., 2002).
Only a few studies of hearing aids have used control groups or randomized methods. As noted by van Vliet (2005, p. 416), “Peer-reviewed publications describing performance of various techniques and hearing aid circuits are available, but high-quality evidence about what works for patients in the form of randomized, blinded studies designed to answer critical questions about candidacy for hearing aids, hearing aid selection, fitting, and rehabilitation are rare.” A clinical trial conducted by the U.S. Department of Veterans Affairs (VA) and the National Institute on Deafness and Other Communication Disorders examined the benefits of hearing aids among 360 participants with sensorineural hearing loss. The participants were randomized to examine three hearing aid circuits that made up 70 percent of the U.S. hearing aid market at the time of the study (Larson et al., 2000; Noffsinger et al., 2002; Shanks et al., 2002). Each circuit was used for 3 months, and in this double-blinded study using six sequences of circuits, the major outcomes examined were loudness, noise interference, and overall quality. Some outcome measures included speech recognition tests, perceived sound quality, and self-reported assessment of benefit.
Participants using all three circuits reported considerable benefits and only “small differences” in loudness and distortion of sounds.
In a study by Yueh and colleagues (2001), 30 veterans with service-related hearing loss who were eligible to receive a hearing aid were randomly assigned to receive either a programmable hearing aid with a directional microphone or a nonprogrammable aid. Hearing-related quality of life was measured among these veterans as well as among 30 veterans with non-service-connected hearing loss who either did not have a hearing aid or received an assistive listening device. Results showed highest scores on measures of hearing-related quality of life among individuals using the programmable hearing aid, followed by the nonprogrammable aid, the assistive listening device, and finally no hearing device.
In a randomized crossover trial, Cox and colleagues (2014) examined speech understanding among 25 participants (with bilateral mild to moderate sensorineural hearing loss) who used four types of hearing aids (two basic and two premium level). Participants, who included both new and experienced hearing aid users, used each type of hearing aid for 1 month and then completed laboratory speech understanding tests, responded to standardized questionnaires, and recorded journal entries on their experiences with the hearing aids during the month. The study results showed benefits associated with all four types of hearing aids, with experienced users reporting greater benefits (Cox et al., 2014). No statistically significant differences in speech understanding were found between the premium and the basic hearing aids.
Some studies have examined hearing aid use longitudinally (Humes and Wilson, 2003; Humes et al., 2002; Turner et al., 1996). Contrary to what might be expected, these studies have produced no consistent evidence that users of hearing aids grow used to them over time and come to better understand amplified speech.
Factors Affecting the Success of Treatment
Myriad factors affect the success of hearing rehabilitative treatment in enhancing the functional capabilities of individuals with hearing loss. Among these factors are the extent of hearing loss; the type of hearing loss (sensorineural, conductive, or mixed); and the individual’s word recognition abilities, processing speed, and ability to process speech in more complex listening environments (such as those that are noisy) (Gatehouse et al., 2003). These factors likely are best understood within the context of the ICF model. For example, the severity and duration of an individual’s hearing loss (characterized by the structure/function of the cochlea and peripheral auditory system) and his or her intrinsic cognitive resources and auditory processing abilities will affect that person’s hearing and communicative
abilities (Gatehouse et al., 2003; Humes et al., 2006). Similarly, a person’s functional abilities will be affected by environmental factors such as the listening environment at work/home, the communicative behaviors of other people, and the type of hearing aid or other assistive listening devices the individual is using. Finally, personal factors, such as an individual’s willingness to utilize hearing rehabilitative strategies, also will greatly affect the benefit of any type of treatment and the person’s resulting functional abilities. Therefore, assessment of an individual’s lifestyle/job functions in conjunction with objective and subjective testing can help in determining which devices(s) will yield the greatest benefit for that person.
There are many reasons why people may not wear their hearing aids successfully after being fitted with them. First, users may have issues with the devices related to wearing or handling them and to their effectiveness. Moreover, a significant reason people do not use their hearing aids relates to their value for understanding speech (McCormack and Fortnum, 2013). The success of assistive listening technology varies with the listening situation. In almost all instances, users will benefit from some type of assistive technology in one-on-one communication in a quiet environment. Hearing aids, remote microphone technology, and PSAPs generally are used most successfully when the listener is in close proximity to the speaker, has no other auditory distractions, and can utilize speech reading (Mueller et al., 2006; Nilsson et al., 1992). Thus, small-group discussions in quiet environments utilizing properly programmed hearing aids will likely be beneficial for most users, and the more distance and background noise that are introduced, the less likely the user will have a favorable listening experience.
EVALUATION AND MONITORING
Given that hearing loss can make communication difficult, effective communication is especially important in health care settings to ensure patient safety and enable a person-centered approach (Middleton et al., 2010). Since performing hearing tests usually is not routine during primary care visits, the individual or family is responsible for recognizing symptoms of hearing loss and seeking treatment. Efforts to improve hearing health literacy are ongoing.
Individuals may seek audiological services and a hearing evaluation for several reasons: because of their own concerns, referral resulting from a medical evaluation that has revealed indicators of poor hearing, the advice of a family member or friend, or in the context of routine health care. An individual also may have congenital hearing loss that is stable or has progressed or may have incurred hearing loss due to injury or illness. Evaluations may vary based on the risk for ear disease. Regardless, any
evaluation for hearing loss is focused on determining any impacts on overall functioning and the potential for treatment.
Patient History and Otoscopic Exam
The first step in an evaluation for hearing loss is to gather the person’s medical and hearing history, including the duration and extent of the loss; salient past events and circumstances, such as ear infections or pain, a family history of hearing loss, and use of relevant prescription and over-the-counter medications; and any use of treatments for hearing loss. Further information may be gathered to assess the impact of hearing loss on the individual’s daily life (see below). The second step is to perform an otoscopic examination “to evaluate the pinna (outer ear), external auditory canal, and tympanic membrane for any conditions that could be contributing to hearing loss or that may require further evaluation and treatment (e.g., cerumen impaction, an abnormality of the tympanic membrane, etc.)” (NASEM, 2016, p. 81). A patient may be referred to a physician for additional evaluation based on the results of these two steps.
Diagnostic Testing
Diagnostic testing for hearing loss includes pure tone, speech, and immittance audiometry.
Pure Tone Audiometry
Pure tone audiometry is a test that “measures the lowest intensity level at which an individual can detect calibrated pure tones at specific frequencies between 250–8,000 Hertz” (NASEM, 2016, p. 82). The “threshold” is defined as the intensity level at which the person can detect a calibrated pure tone 50 percent of the time. “Intensity levels are calibrated in decibels (dB) relative to average normal hearing (dB hearing level or dB HL) and can range from −10 dB HL to 120 dB HL” (NASEM, 2016, p. 82). Normal limits for pure tone thresholds are between −10 dB HL and 20 dB HL.
Pure tones can be delivered through headphones or delivered to the skull using a bone oscillator. When headphones are used, pure tones are delivered to each of the ears individually; the sound travels through each ear canal and middle ear to the cochlea within the inner ear (termed “air-conduction” hearing). When pure tones are delivered to the skull using a bone oscillator, the sound passes through the skull directly, stimulating the cochlea and bypassing the ear canal and middle ear (“bone-conduction” hearing). The practitioner conducting the test can draw conclusions about the nature of the hearing loss by looking at the patterns of air-conduction or
bone-conduction thresholds, with the former thresholds being higher than the latter. A conductive hearing loss is the result of damage to or disease of the ear canal, eardrum, or middle ear, while a sensorineural hearing loss is identified when air-conduction and bone-conduction thresholds are similar but fall outside the limits of normal hearing.
Speech Audiometry
In a speech audiometry test, two-syllable words are transmitted to each ear individually through headphones to determine the speech recognition threshold—the lowest intensity level at which the person can repeat 50 percent of the words correctly. Some tests simulate quiet and/or noisy environments to help determine the individual’s function needs and assess the potential benefits of amplification devices. If an individual shows disproportionately poor speech recognition relative to his or her thresholds for pure tones, changes to the function of the cochlea, auditory vestibular nerve, brainstem, or central processing may be suspected. While speech testing can guide a clinician in the development of a rehabilitation plan, there can be many variables that prevent speech testing from being an objective way of demonstrating the overall benefit that one can achieve from wearing hearing aids. These include variations in the measurement conditions (speech level, background noise level) as well as patient variability (hearing thresholds) and the available gain of the hearing aid at each frequency. Establishing objective measures of real-world communicative functioning is vital to promoting a better understanding of the effects of audiometric hearing function and hearing devices on real-world communicative function.
Immittance Audiometry
Immittance audiometry, also known as “acoustic impedance” or “admittance” testing, includes tympanometry and assessments of the acoustic reflex threshold. These tests are used to establish middle ear pressure and to estimate the transfer of acoustic energy through the middle ear system, which can help differentiate among different disorders.
Assessment of Communicative Function
During a functional communication assessment, an individual’s hearing- and communication-related audiologic and nonaudiologic needs are defined, the impact of hearing loss on the individual and his or her communication partners (e.g., family) is established, and the services and technologies that can benefit the individual are determined (ASHA, 2017d; Valente et al., 2006). The use of technologies and/or rehabilitation to manage
hearing difficulties may be beneficial and sufficient when a strong relationship exists between measured hearing impairment and reported hearing and communication difficulties. When such a relationship does not exist, on the other hand, other considerations come into play, such as the individual’s environment, the people with whom the person interacts and how those people behave, as well as such personal factors as intellectual capacity and psychological state. These factors accord with the biopsychosocial model of the ICF as well as the framework of environmental facilitators described in Chapter 2.
In relation to the ICF framework, audiological testing identifies the impairment aspect of auditory function. Accordingly, it is important for audiologists to be aware of hearing difficulties that occur in situations that do not involve communication—for example, when attempting to locate sounds or recognizing the sound of a nearby event, such as a coin falling on the floor. It is also important to note that, because of variations in people’s auditory environments, it can be difficult to evaluate an individual’s ability to understand conversation in various settings and at various levels of intensity.
Finally, individuals with functional consequences from hearing loss usually have a chronic problem that is unlikely to improve spontaneously or through medical or surgical treatments. Thus, the goal of treatment is to maximize the capacity that remains to an individual.
Use of Results
The results of an audiological evaluation should be used to address the following:
- whether the individual’s hearing loss is due to a medical condition that requires care
- whether the hearing loss is great enough to interfere with the individual’s functioning and, if so, whether the person’s complaints are traceable to the deficit
- whether psychosocial factors can explain any mismatch between the individual’s complaints and his or her measured hearing loss and, if so, whether further evaluation or referral is necessary
- if there is no such mismatch, what treatment approach (e.g., technologies, rehabilitation) will best maximize the person’s functioning
- if the person’s hearing impairment is not of sufficient magnitude to indicate disease or compromise full functioning, whether there is a risk of that occurring in the future and, if so, whether there are ways to mitigate that risk
Such information can help drive the individualized audiological treatment plan. Some of these questions can be deferred to a referring physician after the audiological evaluation is performed. Although most of the traditional tests for auditory function focus on the diagnosis of disease, the same set of tests can be used to evaluate both the possibility of disease and the effects of hearing loss on function. Additional tests, such as otoacoustic emissions tests and tests for characterization of tinnitus, can be administered to distinguish among more complex forms of otologic disease or auditory dysfunction.
TRAINING AND ADAPTATION
As emphasized throughout this report with respect to all of the disabilities considered and as reflected in the ICF model, the impact of hearing loss depends on multiple factors, such as the individual’s lifestyle, interactions with others, and environments. Therefore, two individuals with the same degree of hearing loss can report different difficulties. In addition, an individual’s personality, coping style, resiliency, and duration of hearing loss may all play a role in how that person perceives his or her hearing abilities. Adaptation to hearing aid use also depends on many factors, such as degree of hearing loss, age and personality of the user, duration of the loss, and performance of the hearing aid (Brooks, 1996). These complex factors and interactions highlight the need for a personalized approach to treatment for hearing loss.
Selection, Fitting, Maintenance, and Use of Hearing Products and Technologies
Users of hearing products and technologies receive services that most commonly include the provision of and assistance with the use of hearing aids, consisting of device selection, fitting, verification, and validation, within the context of the functional communication assessment.9,10 According to U.S. best practices in audiology, selection of a hearing aid is based on “an individual’s needs and requirements for hearing aid gain, ear canal geometry, occlusion, special features (e.g., directional microphone, noise reduction circuit, feedback suppression, telecoil), ease of insertion and manipulating volume controls, and cosmetics” (NASEM, 2016, p. 85). Gain processing is initially determined by means of validated prescriptive
___________________
9 Refer to ASHA (2017d) and Valente et al. (2006) for best practice guidelines for audiologic management of hearing loss in adults.
10 Refer to Oh and Lee (2016) for a review of hearing aid fitting management across worldwide guidelines.
procedures, such as those developed by the National Acoustics Laboratories (Byrne and Dillon, 1986; Byrne et al., 2001; Johnson and Dillon, 2011; Mueller, 2005). Hearing aid evaluations also “include selection of output limiting and compression features, and consideration of the need for special technologies (e.g., bone-anchored hearing aids, contralateral routing of signal fittings, and middle-ear implants)” (NASEM, 2016, p. 85). The most reliable method for validating that prescriptive gain targets have been achieved is gain verification using a probe microphone (“real-ear” measures) (Abrams et al., 2012; Mueller, 2001).
Next, the provider discusses with the patient how best to operate, maintain, and use the selected device. With respect to the device, the focus is on insertion and removal, the schedule for use, features of the device, how to reduce feedback and change batteries, and maintenance. With respect to the patient, the focus is on establishing goals and expectations, adjusting to amplification, understanding communication strategies, and the possible need for supplementary treatment (e.g., training in speech reading or speech perception). The final step is to formulate a plan for assessing the benefits of the selected device, based on both subjective and objective measures (for examples, see Cox and Alexander, 1995; Cox et al., 2003; Dillon et al., 1997; Ventry and Weinstein, 1982). Follow-up visits also may be necessary to perform more adjustments; to provide further education on the correct operation, maintenance, and usage of the device (Desjardins and Doherty, 2009); and to ensure that the device provides optimal performance and that hearing is stable.
Although health care professionals who treat patients with hearing loss most commonly provide services and support for hearing aids, they may offer similar services for other hearing assistive technologies that they do not dispense. It is important for these professionals to be trained in the full range of such technologies so they can help patients determine which technology is most useful for meeting their needs.
A personalized approach to treatment for hearing loss is important to the user’s experience. In a study by Abrams and Kihm (2015), 81 percent of hearing aid users reported satisfaction with their devices. The survey also showed the devices’ positive impacts on relationships, work performance, ability to communicate, ability to participate in group activities, and overall quality of life (Abrams and Kihm, 2015). Factors that were barriers to hearing aid adoption included financial constraints, lack of perceived need, and being unaware of where to go to receive an evaluation (Abrams and Kihm, 2015).
User Training/Adaptation to Hearing Rehabilitation
Hearing aids cannot address all of the challenges of living with hearing loss, which include the loss itself, communication difficulties, changes in quality of life, and possible comorbidities. Rather, “hearing loss requires a holistic, individual-centered approach to care that blends both medical and non-medical solutions, such as auditory rehabilitation (also referred to as aural rehabilitation or audiological rehabilitation)” (NASEM, 2016, p. 86). Auditory rehabilitation is intended to help individuals with hearing loss learn how to live with that loss, to provide information on the use of hearing aids and other hearing assistive technologies, to teach strategies for better listening and communication, and in some cases to offer psychosocial support (ASHA, 2017a; Boothroyd, 2010; Sweetow and Palmer, 2005). Auditory rehabilitation programs can take many forms. They can be offered with a group in a community setting or on an individual basis in an audiology clinic; sessions may be led by an audiologist, a speech-language pathologist, or a trained volunteer; and individuals may take part in self-paced, multimedia rehabilitation programs from their homes (Bally and Bakke, 2007). Studies have consistently shown the benefits of group auditory rehabilitation (Hawkins, 2005; Laplante-Levesque et al., 2011; Northern and Beyer, 1999; Preminger, 2011).
ACCESS AND AVAILABILITY
The costs of hearing aids and other nonsurgical approaches to managing hearing loss, as well as related services, generally are not covered by health insurance, although coverage can vary from state to state depending on the insurer. Therefore, these costs most commonly are paid for out of pocket by consumers. The cost of a hearing aid or other assistive device is usually set according to a “bundled” pricing model that includes the cost of professional services in addition to that of the device itself. The price may also include fees for comprehensive assessment of hearing loss and hearing aid candidacy; assessment of communication needs; hearing aid fitting and programming; and other associated services, such as routine maintenance for a defined period of time and accessories. These services assist the user in achieving optimal fit and maximal benefit from the device and in learning strategies for maximizing the quality of communication. Alternatively, in an unbundled or itemized billing model, the prices of each test, device, and service are listed individually. In 2003, the average retail price for a pair of hearing aids was $4,700 (a bundled price including services) (range $3,300 to $6,000) (Strom, 2014). As a result, many adults with hearing loss and without sufficient financial resources or coverage of hearing devices and services do not receive care. While some emerging, less expensive hearing
technologies (e.g., PSAPs) are available to consumers, these options vary substantially in quality and the ability to mitigate impairment effectively, and individuals may require additional assistance to utilize them optimally. Coverage of devices and services for individuals with hearing loss under various programs is reviewed below. Also described are the various types of hearing health care personnel.
Social Security Administration
Currently, U.S. Social Security Administration (SSA) disability benefits are available only for profound hearing loss or deafness, not for mild or moderate hearing loss. The loss must be diagnosed by an audiologist, an otolaryngologist, or a licensed physician. The criteria for qualifying for benefits include air-conduction results of 90 dB HL or worse in the better ear, with bone-conduction results of 60 dB HL or poorer in the better ear. Alternatively, one must receive a score poorer than 40 percent correct on word recognition testing. Such hearing loss is generally at a level at which conventional hearing aids cannot fully mitigate communication impairments. Therefore, the current criteria for hearing disability in SSA’s Listing of Impairments generally reflect a level of hearing loss severity at which amplification with a hearing aid is insufficient to substantially mitigate impairments and restrictions on participation due to hearing loss. Currently, SSA’s residual functional capacity assessment for hearing loss may include specific restrictions on the type of work an individual can do because of poor hearing, such as working near or operating hazardous machinery.
Medicare
Original Medicare (also referred to as Medicare Parts A and B) covers costs related to hospital stays and outpatient services and supplies considered medically necessary in diagnosing and treating a disease or condition. A hearing test is covered only if a physician or other health care provider orders the test to diagnose a hearing or balance disorder (CMS, 2016c). Audiologists who conduct this test also can be reimbursed. However, Medicare does not pay for other services they provide to beneficiaries, such as rehabilitation, despite its being within their scope of practice. The Social Security Amendments of 196511 specify that Medicare does not provide coverage of hearing aids. Section 1862(a)(7) of the act states, “Notwithstanding any other provision of this title, no payment may be made under part A or part B for any expenses incurred for items or services . . . where such expenses are for . . . hearing aids or examinations
___________________
11 Social Security Amendments of 1965, Public Law 89-97 (July 30, 1965).
therefor.” This policy is codified in the regulation at 42 CFR 411.15 (d), which states that hearing aids and examinations for the purpose of prescribing, fitting, or changing hearing aids are excluded from Medicare coverage.
Medicare Advantage
Under Medicare Advantage (also referred to as Medicare Part C), a person who is eligible for original Medicare (Parts A and B) can withdraw from that program and choose a private insurance plan instead. The federal government will then redirect money from what is paid into Medicare to the individual’s Medicare Advantage program. Medicare Advantage allows beneficiaries to choose plans that meet their specific needs, such as coverage for hearing health care services and devices or the ability to purchase extra coverage for hearing health care. The number of beneficiaries enrolled in a Medicare Advantage plan has increased since 2004, with approximately 31 percent of Medicare beneficiaries joining such plans in 2015 (Kaiser Family Foundation, 2015).
Medicaid
As of early 2015, only 28 states covered purchases of hearing aids for adult Medicaid beneficiaries (HLAA, 2015). Medicaid coverage varies widely among states, in some cases being very limited. For individuals to be eligible for Medicaid coverage for hearing aids, they are required by states to have an established minimum hearing loss, and many states also require a medical exam in addition to an audiological evaluation to determine whether a hearing aid is medically necessary. However, some states have limitations on the types of hearing aids covered and on the number of aids and accessories that may be received in a given time period, and some impose annual caps on payment and even require prior approval from a physician. Another hurdle can be finding a provider who will accept Medicaid.
The Early and Periodic Screening, Diagnostic, and Treatment Program
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program provides health care services for children enrolled in Medicaid until they turn age 21 (CMS, 2016a). This program requires that each state provide minimum hearing health care services to its beneficiaries that include diagnosis, treatment, and hearing aids. When these beneficiaries turn 21, they transition to the Medicaid program for adults and receive hearing health care benefits provided by the state in which they reside, as described above. In states that do not provide hearing health care benefits to adults, the transition for children aging out of the EPSDT program is very
challenging. Another challenge is that children covered under the Children’s Health Insurance Program (CHIP)—a benefit program for uninsured individuals under age 19 whose family income is too high for them to enroll in Medicaid—may not be able to enroll in EPSDT since states are not required to extend this program to those covered by CHIP.
Patient Protection and Affordable Care Act
The Patient Protection and Affordable Care Act (ACA) requires individual state marketplace health insurance plans and expanded Medicaid programs to cover 10 “essential health benefits,” including “rehabilitative and habilitative services and devices (services and devices to help people with injuries, disabilities, or chronic conditions gain or recover mental and physical skills)” (CMS, 2016b, p. 1). States vary in their interpretations of what constitutes the benefit. The benchmark insurance plans selected by states may not include hearing health care services or hearing aids for adults, and if this is the case, their expanded Medicaid program (if they have one) and the plans offered in their marketplace are not required to do so either. Only 7 of 50 states (Arizona, Hawaii, Nevada, New York, Rhode Island, Texas, and Wisconsin) and the District of Columbia chose benchmark plans that offer this coverage for adults, which varies by state.
Employer-Sponsored and Private Health Insurance
Few private insurance companies cover hearing health care for adults (Andrews, 2012; Consumer Reports, 2015). Employer-sponsored plans provide some coverage of hearing health care. Some cover diagnostic and evaluation services; others cover some or all costs of hearing aids; and some offer their employees the option of purchasing hearing health care insurance, similar to optional dental or vision insurance (ASHA, 2017c). By 2014, only three states—Arkansas, New Hampshire, and Rhode Island—mandated that health insurance plans include coverage for hearing aids for adults (ASHA, 2017e). However, self-insured plans are exempt from this mandate. This means that even in the states with mandated coverage, large self-insured companies with thousands of employees need not provide hearing health care coverage. Coverage for hearing aids and other services for adults with hearing loss is provided by some Federal Employee Health Benefits plans, fee-for-service plans, and health maintenance organizations (HMOs) (HLAA, 2008), but the comprehensiveness of the coverage varies among plans.
Benefits for Veterans
TRICARE is a health care program serving members of the military, military retirees, and their families that covers hearing aids and hearing aid services for beneficiaries with hearing loss that meets specific parameters (TRICARE, 2015). VA services and the Retiree At-Cost Hearing Aid Program also offer hearing services that military retirees may be able to access (MAA, 2016; TRICARE, 2015).
For U.S. military veterans, the most prevalent causes of service-related disability are hearing loss and tinnitus, which affect veterans of all ages; this makes audiology one of the most highly utilized services in the VA (Chandler, 2015; VA Office of the Inspector General, 2014). Veterans who are enrolled in the VA health care system receive diagnostic audiology services and hearing aids. Hearing aids provided through the VA cost qualified recipients very little or nothing; in most cases, however, veterans can qualify only if they have a predefined minimum hearing loss that resulted from active military service (Beck, 2015).12 Veterans also may be eligible for service-connected disability compensation for hearing impairment based on results from unaided pure tone audiometry and unaided speech recognition scores. The amount of disability compensation varies according to the joint results on both of these tests according to the established VA Schedule for Rating Disabilities.13
Vocational Rehabilitation Programs
State vocational rehabilitation programs funded under the Rehabilitation Act of 197314 are focused on individuals who have a physical or an intellectual disability that prevents them from engaging in part- or full-time employment or postsecondary education. To qualify for the program requires a determination that vocational rehabilitation will help an individual with a disability gain employment or postsecondary education. Once this has been determined, eligible individuals work with a counselor to establish an Individualized Plan for Employment. The Workforce Innovation and Opportunity Act of 201415 amended the Rehabilitation Act of 1973 to require that all state agencies operating these programs allocate at least 15 percent of their federal funds to services for those transitioning from secondary education to postsecondary education or employment. An example
___________________
12 38 CFR § 3.385.
13 38 CFR § 4.87.
14 Rehabilitation Act of 1973, Public Law 93-112, 93rd Cong. (September 26, 1973).
15 Workforce Innovation and Opportunity Act, Public Law 113-128, 113th Cong. (July 22, 2014).
of such services is summer programs for students with hearing loss who are transitioning to college.
Vocational rehabilitation services for individuals with hearing loss or deafness include provision of hearing aids and other hearing health care services. These services are administered by the state and funded through the U.S. Department of Education’s Rehabilitation Services Administration (U.S. Department of Education, 2016). State vocational rehabilitation agencies use a process termed “order of selection” for services in which the highest priority for benefits is given to clients with the most significant functional limitations, while those with less severe limitations may be placed on a waiting list to receive services. The state decides which functional limitations have the highest priority. People with hearing loss may not be accorded priority since their functional limitation may be seen as less significant than those of other consumers (University of Arkansas Rehabilitation Research and Training Center, 2008).
Hearing Health Care Personnel
There are a variety of providers with whom one can work to treat hearing loss. Insurance coverage for visits to these providers varies. Some insurance providers, for example, will cover an audiologist visit, but others require referral by a primary care physician before they will cover all or part of the cost of a hearing test. There are also some providers who may not be eligible to bill insurance. An overview of the various types of hearing health care personnel is presented below.
Hearing Instrument Specialists
Hearing instrument specialists, also known as hearing aid specialists, “identify individuals with hearing loss, assess their need for hearing aids, dispense hearing aids, and educate patients and their family members about their hearing loss” (NASEM, 2016, p. 76). By law, minimum qualifications for hearing instrument specialists in most states are a high school diploma, a 2-year apprenticeship, and a license to practice. Although licensure requirements vary from state to state, most states require completion of an annual application form and payment of a fee, and some states require certification by the business owner (offered through the National Board for Certification in Hearing Instrument Sciences). According to the U.S. Bureau of Labor Statistics, there are approximately 5,920 hearing instrument specialists in the United States; most are located in large cities (BLS, 2015b).
Audiologists
Audiologists offer services to identify patients with hearing difficulties, assess and diagnose their hearing needs, treat their needs through hearing aid dispensing and/or habilitation, and educate patients and caregivers about hearing loss prevention. Audiologists must obtain a doctor of audiology degree, which usually requires completion of a 4-year program in addition to a bachelor’s degree from an accredited institution. Although state licensing requirements for audiologists vary, many states require an advanced degree, a qualifying examination, and supervised experience in a clinical fellowship, as well as ongoing continuing education. The United States currently has approximately 12,070 practicing audiologists; again, most are located in urban areas (BLS, 2015a).
Otolaryngologists
Otolaryngologists (i.e., ear, nose, and throat [ENT] physicians) are “physicians trained in the medical and surgical management and treatment of patients with diseases and disorders of the ear, nose, throat, and related structures of the head and neck” (NASEM, 2016, p. 76). They treat, medically and surgically, conditions of the ear that include hearing loss, ear infections, balance disorders, and tinnitus (American Academy of Otolaryngology-Head and Neck Surgery, 2015). Although there were approximately 10,000 otolaryngologists in the United States in 2009, the number of residents seeking board certification in this field has declined since 2006 (Neuwahl et al., 2012). There are various subspecialties in ENT medicine, not all of these physicians see patients with hearing loss.
Primary Care Providers
Primary care providers may often be the first to assess and diagnose patients with hearing loss, and they may even provide treatment to these patients without referring them to a hearing health care specialist. A primary care provider can treat outer or middle ear infections, identify and discontinue ototoxic medications, and conduct simple hearing screening tests and primary otologic examinations.
Availability of Hearing Health Care Personnel
These multiple entry points to accessing hearing health care and even the decline in otolaryngologists seeking board certification can create many challenges for adults with hearing loss. More qualified providers and clinics with the knowledge, skill, and expertise to properly evaluate, prescribe,
and train people in the use of hearing devices are needed. Proper fitting and training are complex but necessary elements to maximize performance among hearing device users. Consumers who work with providers trained in the use of properly prescribed and fitted hearing devices can expect better results than those who use off-the-shelf products.
FINDINGS AND CONCLUSIONS
Findings
5-1. The distribution of providers and clinics with the knowledge, skill, and expertise to properly evaluate, prescribe, and train people in the use of hearing devices varies greatly throughout the United States.
5-2. Current SSA Listing of Impairments criteria for hearing disability generally reflect a level of hearing loss at which amplification with a hearing aid is insufficient to substantially mitigate impairments and restrictions on participation due to hearing loss.
5-3. There are no established objective measures of real-world communicative functioning.
5-4. Research investigating the impact of audiometric hearing function and/or hearing devices on real-world communicative functioning is extremely limited.
5-5. Audiologists cannot bill Medicare or insurance for audiological rehabilitation services.
5-6. Reimbursement for hearing aids is statutorily excluded by Medicare.
5-7. Compared with the prevalence of hearing loss, the prevalence of hearing aid use is low in the United States.
5-8. Access to hearing devices varies significantly across reimbursement and funding sources in the United States.
5-9. The vast majority of individuals do not have insurance that covers hearing aids or related services.
5-10. The cost for hearing aids is usually covered under a bundled model that includes the costs of the devices and of the professional services required to fit them properly and follow up for rehabilitation.
Conclusions
5-1. Qualified providers and clinics with the knowledge, skill, and expertise to properly evaluate, prescribe, and train people in the use of hearing devices are needed. [Finding 5-1]
5-2. Proper fitting and training are complex but necessary elements of maximizing performance among users of hearing devices. Consumers who work with providers trained in the use of properly prescribed
and fitted hearing devices can expect better results than those who use off-the-shelf products. [Finding 5-1]
5-3. Even with advances in technology, hearing aids and other hearing assistive devices may help but do not fully mitigate impairments or restrictions on participation caused by hearing loss. Environmental and personal factors are as important in determining the overall communicative functioning of individuals with hearing loss. [Finding 5-2]
5-4. The establishment of objective measures of real-world communicative functioning is vital to promoting a better understanding of the effects on this functioning of audiometric hearing function and hearing devices. [Findings 5-3, 5-4]
5-5. The widespread lack of insurance coverage for hearing devices and related services is an impediment to optimizing communicative functioning and maintaining gainful employment among adults with hearing loss. [Findings 5-5, 5-6, 5-7, 5-8, 5-9]
REFERENCES
Abrams, H. B., and J. Kihm. 2015. An introduction to MarkeTrak IX: A new baseline for the hearing aid market. http://www.hearingreview.com/2015/05/introduction-marketrak-ix-new-baseline-hearing-aid-market (accessed February 6, 2017).
Abrams, H. B., T. H. Chisolm, M. McManus, and R. McArdle. 2012. Initial-fit approach versus verified prescription: Comparing self-perceived hearing aid benefit. Journal of the American Academy of Audiology 23(10):768-778.
American Academy of Otolaryngology-Head and Neck Surgery. 2015. What is an otolaryngologist? http://www.entnet.org/content/what-otolaryngologist (accessed January 13, 2017).
Amieva, H., C. Ouvrard, C. Giulioli, C. Meillon, L. Rullier, and J. F. Dartigues. 2015. Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. Journal of the American Geriatrics Society 63(10):2099-2104.
Andrews, M. 2012. Unlike most insurers, United Healthcare is offering big discounts on hearing aids. The Washington Post, April 9. https://www.washingtonpost.com/national/health-science/unlike-most-insurers-unitedhealthcare-is-offering-big-discounts-on-hearing-aids/2012/04/09/gIQA8I0Z6S_story.html?utm_term=.41e62d96906d (accessed January 13, 2017).
ASHA (American Speech-Language-Hearing Association). 2017a. Adult aural/audiologic rehabilitation. http://www.asha.org/public/hearing/Adult-Aural-Rehabilitation (accessed January 13, 2017).
ASHA. 2017b. FM systems. http://www.asha.org/public/hearing/FM-Systems (accessed January 9, 2017).
ASHA. 2017c. Health insurance coverage for hearing aids. http://www.asha.org/public/hearing/Health-Insurance-Coverage-for-Hearing-Aids (accessed January 13, 2017).
ASHA. 2017d. Hearing aids for adults. http://www.asha.org/Practice-Portal/Professional-Issues/Hearing-Aids-for-Adults (accessed January 13, 2017).
ASHA. 2017e. State insurance mandates for hearing aids. http://www.asha.org/advocacy/state/issues/ha_reimbursement (accessed February 9, 2017).
Bally, S. J., and M. H. Bakke. 2007. A peer mentor training program for aural rehabilitation. Trends in Amplification 11(2):125-131.
Banerjee, S. 2011. Hearing aids in the real world: Use of multimemory and volume controls. Journal of the American Academy of Audiology 22(6):359-374.
Beck, L. 2015. Perspective from Department of Veterans Affairs. Presented at the Committee on Accessible and Affordable Hearing Health Care Meeting, Washington, DC, June 30.
Blackwell, D. L., J. W. Lucas, and T. C. Clarke. 2014. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital and health statistics 10(260):1-161.
BLS (U.S. Bureau of Labor Statistics). 2015a. Occupational emloyment and wages, May 2015: 29-1181 Audiologists. http://www.bls.gov/oes/current/oes291181.htm (accessed January 13, 2017).
BLS. 2015b. Occupational employment and wages, May 2015: 29-2092 Hearing aid specialists. https://www.bls.gov/oes/current/oes292092.htm (accessed January 13, 2017).
Boothroyd, A. 2010. Adapting to changed hearing: The potential role of formal training. Journal of the American Academy of Audiology 21(9):601-611.
Brault, M. W. 2012. Americans with disabilities: 2010. Current Population Reports 7:1-131.
Breitbart, D., J. Xu, J. Johnson, and R. Cox. 2014. Is there a preference between hearing aids and personal sound amplification products (PSAPs)? http://www.harlmemphis.org/files/2513/9628/6861/Breitbart2014.pdf (accessed February 6, 2017).
Brooks, D. N. 1996. The time course of adaptation to hearing aid use. British Journal of Audiology 30(1):55-62.
Byrne, D., and H. Dillon. 1986. The National Acoustic Laboratories’ (NAL) new procedure for selecting the gain and frequency response of a hearing aid. Ear and Hearing 7(4):257-265.
Byrne, D., H. Dillon, T. Ching, R. Katsch, and G. Keidser. 2001. NAL-NL1 procedure for fitting nonlinear hearing aids: Characteristics and comparisons with other procedures. Journal of the American Academy of Audiology 12(1):37-51.
CDC (U.S. Centers for Disease Control and Prevention). 2011. NHANES 2011-2012 questionnaire data. https://wwwn.cdc.gov/Nchs/Nhanes/Search/DataPage.aspx?Component=Questionnaire&CycleBeginYear=2011 (accessed February 6, 2017).
Chandler, D. 2015. Perspective from Department of Veterans Affairs. Presented at the Committee on Accessible and Affordable Hearing Health Care Meeting, Washington DC, April 27.
Chen, D. S., J. Betz, K. Yaffe, H. N. Ayonayon, S. Kritchevsky, K. R. Martin, T. B. Harris, K. R. Martin, T. B. Harris, E. Purchase-Helzner, S. Satterfield, Q. L. Xue, S. Pratt, E. M. Simonsick, and F. R. Lin for the Health ABC Study. 2015. Association of hearing impairment with declines in physical functioning and the risk of disability in older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 70(5):654-661.
Chien, W., and F. R. Lin. 2012. Prevalence of hearing aid use among older adults in the United States. Archives of Internal Medicine 172(3):292-293.
Chisolm, T. H., C. M. Noe, R. McArdle, and H. Abrams. 2007. Evidence for the use of hearing assistive technology by adults: The role of the FM system. Trends in Amplification 11(2):73-89.
Ciorba, A., C. Bianchini, S. Pelucchi, and A. Pastore. 2012. The impact of hearing loss on the quality of life of elderly adults. Clinical Interventions in Aging 7(6):159-163.
CMS (Centers for Medicare & Medicaid Services). 2016a. Early and periodic screening, diagnostic, and treatment. https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Early-and-Periodic-Screening-Diagnostic-and-Treatment.html (accessed February 27, 2016).
CMS. 2016b. Health benefits and coverage: What marketplace health insurance plans cover. www.healthcare.gov/coverage/what-marketplace-plans-cover (accessed February 27, 2016).
CMS. 2016c. Your Medicare coverage: Hearing and balance exams and hearing aids. https://www.medicare.gov/coverage/hearing-and-balance-exam-and-hearing-aids.html (accessed February 28, 2016).
Consumer Reports. 2015. Hearing aid buying guide. http://www.consumerreports.org/cro/hearing-aids/buying-guide.htm (accessed December 28, 2016).
Contrera, K. J., J. Betz, D. J. Genther, and F. R. Lin. 2015. Association of hearing impairment and mortality in the National Health and Nutrition Examination Survey. JAMA Otolaryngology—Head & Neck Surgery 141(10):944-946.
Cox, R. M., and G. C. Alexander. 1995. The abbreviated profile of hearing aid benefit. Ear and Hearing 16(2):176-186.
Cox, R. M., and G. C. Alexander. 1999. Measuring satisfaction with amplification in daily life: The SADL scale. Ear and Hearing 20(4):306-320.
Cox, R. M., G. C. Alexander, I. M. Taylor, and G. A. Gray. 1996. Benefit acclimatization in elderly hearing aid users. Journal of the American Academy of Audiology 7(6):428-441.
Cox, R. M., G. C. Alexander, and C. M. Beyer. 2003. Norms for the international outcome inventory for hearing aids. Journal of the American Academy of Audiology 14(8):403-413.
Cox, R. M., K. S. Schwartz, C. M. Noe, and G. C. Alexander. 2011. Preference for one or two hearing aids among adult patients. Ear and Hearing 32(2):181-197.
Cox, R. M., J. A. Johnson, and J. Xu. 2014. Impact of advanced hearing aid technology on speech understanding for older listeners with mild to moderate, adult-onset, sensorineural hearing loss. Gerontology 60(6):557-568.
Cruickshanks, K. J., T. L. Wiley, T. S. Tweed, B. E. Klein, R. Klein, J. A. Mares-Perlman, and D. M. Nondahl. 1998. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin. The Epidemiology of Hearing Loss Study. American Journal of Epidemiology 148(9):879-886.
Dawes, P., K. J. Cruickshanks, M. E. Fischer, B. E. Klein, R. Klein, and D. M. Nondahl. 2015. Hearing-aid use and long-term health outcomes: Hearing handicap, mental health, social engagement, cognitive function, physical health, and mortality. International Journal of Audiology 54(11):838-844.
Desjardins, J. L., and K. A. Doherty. 2009. Do experienced hearing aid users know how to use their hearing aids correctly? American Journal of Audiology 18(1):69-76.
Dillon, H., A. James, and J. Ginis. 1997. Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology 8(1):27-43.
FCC (Federal Communications Commission). 2016. Telecommunications relay service. https://www.fcc.gov/consumers/guides/telecommunications-relay-service-trs (accessed January 9, 2017).
FDA (U.S. Food and Drug Administration). 2013. Regulatory requirements for hearing aid devices and personal sound amplification products—Draft guidance for industry and Food and Drug Administration staff. https://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm373461.htm (accessed February 22, 2017).
Fischer, M. E., K. J. Cruickshanks, A. Pinto, B. E. Klein, R. Klein, and D. S. Dalton. 2014. Hearing impairment and retirement. Journal of the American Academy of Audiology 25(2):164-170.
Gatehouse, S., G. Naylor, and C. Elberling. 2003. Benefits from hearing aids in relation to the interaction between the user and the environment. International Journal of Audiology 42(Suppl.1):S77-S85.
Genther, D. J., J. Betz, S. Pratt, S. B. Kritchevsky, K. R. Martin, T. B. Harris, E. Helzner, S. Satterfield, Q. L. Xue, K. Yaffe, E. M. Simonsick, and F. R. Lin. 2015. Association of hearing impairment and mortality in older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 70(1):85-90.
Girard, S. A., T. Leroux, R. Verreault, M. Courteau, M. Picard, F. Turcotte, and J. Baril. 2014. Falls risk and hospitalization among retired workers with occupational noise-induced hearing loss. Canadian Journal on Aging (La Revue canadienne du vieillissement) 33(1):84-91.
Gnewikow, D., T. Ricketts, G. W. Bratt, and L. C. Mutchler. 2009. Real-world benefit from directional microphone hearing aids. Journal of Rehabilitation Research & Development 46(5):603-618.
Goman, A. M., and F. R. Lin. 2016. Prevalence of hearing loss by severity in the United States. American Journal of Public Health 106(10):1820-1822.
Gopinath, B., J. Schneider, C. M. McMahon, G. Burlutsky, S. R. Leeder, P. Mitchell, and L. Chao. 2013. Dual sensory impairment in older adults increases the risk of mortality: A population-based study. PLOS ONE 8(3):e55054.
Hawkins, D. B. 2005. Effectiveness of counseling-based adult group aural rehabilitation programs: A systematic review of the evidence. Journal of the American Academy of Audiology 16(7):485-493.
Hawkins, D. B., and S. V. Naidoo. 1993. Comparison of sound quality and clarity with asymmetrical peak clipping and output limiting compression. Journal of the American Academy of Audiology 4(4):221-228.
Hawkins, D. B., and W. S. Yacullo. 1984. Signal-to-noise ratio advantage of binaural hearing aids and directional microphones under different levels of reverberation. Journal of Speech and Hearing Disorders 49(3):278-286.
HLAA (Hearing Loss Association of America). 2008. Great news on federal employee insurance coverage for hearing aids. http://www.hearingloss.org/content/great-news-federal-employee-insurance-coverage-hearing-aids (accessed January 13, 2017).
HLAA. 2015. Medicaid regulations. http://www.hearingloss.org/content/medicaid-regulations (accessed February 9, 2017).
HLAA. 2016. Consumer’s guide to hearing aids. www.hearingloss.org/content/consumers-guide-hearing-aids (accessed December 28, 2016).
HLAA. 2017. Types, causes, and treatment. http://www.hearingloss.org/content/types-causes-and-treatment (accessed February 7, 2017).
Holmes, A. E., H. S. Kaplan, and J. P. Saxon. 2000. Assistive listening devices and systems: Amplification technology for consumers with hearing loss. Journal of Rehabilitation 66(3):56-59.
Horner-Johnson, W., K. Dobbertin, J. C. Lee, and E. M. Andresen. 2014. Disparities in health care access and receipt of preventive services by disability type: Analysis of the Medical Expenditure Panel Survey. Health Services Research 49(6):1980-1999.
Humes, L. E., and V. Krull. 2012. Hearing aids for adults. In Evidence-based practice in audiology: Evaluating interventions for children and adults with hearing impairment, edited by L. Wong and L. Hickson. San Diego, CA: Plural Publishing. Pp. 61-91.
Humes, L. E., and D. L. Wilson. 2003. An examination of changes in hearing-aid performance and benefit in the elderly over a 3-year period of hearing-aid use. Journal of Speech, Language, and Hearing Research 46(1):137-145.
Humes, L. E., D. L. Wilson, N. N. Barlow, and C. Garner. 2002. Changes in hearing-aid benefit following 1 or 2 years of hearing-aid use by older adults. Journal of Speech, Language, and Hearing Research 45(4):772-782.
Humes, L., J. H. Lee, and M. P. Coughlin. 2006. Auditory measures of selective and divided attention in young and older adults using single-talker competition. The Journal of the Acoustical Society of America 120(5):2926-2937.
Jennings, M. B., and L. Shaw. 2008. Impact of hearing loss in the workplace: Raising questions about partnerships with professionals. Work (Reading, Massachusetts) 30(3):289-295.
Johnson, E. E., and H. Dillon. 2011. A comparison of gain for adults from generic hearing aid prescriptive methods: Impacts on predicted loudness, frequency bandwidth, and speech intelligibility. Journal of the American Academy of Audiology 22(7):441-459.
Kaiser Family Foundation. 2015. Medicare advantage. http://kff.org/medicare/fact-sheet/medicare-advantage (accessed February 27, 2016).
Kamil, R. J., J. Betz, B. B. Powers, S. Pratt, S. Kritchevsky, H. N. Ayonayon, T. B. Harris, E. Helzner, J. A. Deal, K. Martin, M. Peterson, S. Satterfield, E. M. Simonsick, and F. R. Lin. 2016. Association of hearing impairment with incident frailty and falls in older adults. Journal of Aging and Health 28(4):644-660.
Keidser, G., H. Dillon, E. Convery, and J. Mejia. 2013. Factors influencing individual variation in perceptual directional microphone benefit. Journal of the American Academy of Audiology 24(10):955-968.
Kim, J. S., and C. H. Kim. 2014. A review of assistive listening device and digital wireless technology for hearing instruments. Korean Journal of Audiology 18(3):105-111.
Kochkin, S. 2005. The impact of untreated hearing loss on household income. Alexandria, VA: Better Hearing Institute. http://www.betterhearing.org/sites/default/files/hearingpediaresources/M7_Hearing_aids_and_income_2006.pdf (accessed January 22, 2017).
Kochkin, S. 2009. Marketrak VIII: 25-year trends in the hearing health market. Hearing Review 16(11):12-31.
Kokx-Ryan, M., J. Cohen, M. T. Cord, T. C. Walden, M. J. Makashay, B. M. Sheffield, and D. S. Brungart. 2015. Benefits of nonlinear frequency compression in adult hearing aid users. Journal of the American Academy of Audiology 26(10):838-855.
Kramer, S., T. Kapteyn, and T. Houtgast. 2006. Occupational performance: Comparing normally-hearing and hearing-impaired employees using the Amsterdam checklist for hearing and work. International Journal of Audiology 45(9):503-512.
Laplante-Levesque, A., L. Hickson, and L. Worrall. 2011. Predictors of rehabilitation intervention decisions in adults with acquired hearing impairment. Journal of Speech, Language, and Hearing Research 54(5):1385-1399.
Larson, V. D., D. W. Williams, W. G. Henderson, L. E. Luethke, L. B. Beck, D. Noffsinger, R. H. Wilson, R. A. Dobie, G. B. Haskell, G. W. Bratt, J. E. Shanks, P. Stelmachowicz, G. A. Studebaker, A. E. Boysen, A. Donahue, R. Canalis, S. A. Fausti, and B. Z. Rappaport. 2000. Efficacy of 3 commonly used hearing aid circuits: A crossover trial. NIDCD/VA Hearing Aid Clinical Trial Group. Journal of the American Medical Association 284(14):1806-1813.
Lee, D. J., D. L. Carlson, H. M. Lee, L. A. Ray, and K. S. Markides. 1991. Hearing loss and hearing aid use in Hispanic adults: Results from the Hispanic Health and Nutrition Examination Survey. American Journal of Public Health 81(11):1471-1474.
Lin, F. R. 2011. Hearing loss and cognition among older adults in the United States. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 66(10):1131-1136.
Lin, F. R., and L. Ferrucci. 2012. Hearing loss and falls among older adults in the United States. Archives of Internal Medicine 172(4):369-371.
Lin, F. R., L. Ferrucci, E. J. Metter, Y. An, A. B. Zonderman, and S. M. Resnick. 2011a. Hearing loss and cognition in the Baltimore Longitudinal Study of Aging. Neuropsychology 25(6):763-770.
Lin, F. R., E. J. Metter, R. J. O’Brien, S. M. Resnick, A. B. Zonderman, and L. Ferrucci. 2011b. Hearing loss and incident dementia. JAMA Neurology 68(2):214-220.
Lin, F. R., R. Thorpe, S. Gordon-Salant, and L. Ferrucci. 2011c. Hearing loss prevalence and risk factors among older adults in the United States. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 66(5):582-590.
Lin, F. R., J. K. Niparko, and L. Ferrucci. 2011d. Hearing loss prevalence in the United States. Archives of Internal Medicine 171(20):1851-1852.
Lin, F. R., K. Yaffe, J. Xia, Q. L. Xue, T. B. Harris, E. Purchase-Helzner, S. Satterfield, H. N. Ayonayon, L. Ferrucci, and E. M. Simonsick. 2013. Hearing loss and cognitive decline in older adults. JAMA Internal Medicine 173(4):293-299.
Lorenzi, A., and B. Chaix. 2016. Hearing aids. http://www.cochlea.org/en/treatments/hearing-aids (accessed February 8, 2017).
MAA (Military Audiology Association). 2016. Hearing aids. http://militaryaudiology.org/aids (accessed February 28, 2016).
Mäki-Torkko, E. M., B. Brorsson, A. Davis, I. W. S. Mair, K. I. Myhre, A. Parving, R. P. Roine, U. Rosenhall, M. J. Sorri, and S. Stilvén. 2001. Hearing impairment among adults—Extent of the problem and scientific evidence on the outcome of hearing aid rehabilitation. Scandinavian Audiology 30(3):8-15.
McArdle, R., T. H. Chisolm, H. B. Abrams, R. H. Wilson, and P. J. Doyle. 2005. The WHO-DAS II: Measuring outcomes of hearing aid intervention for adults. Trends in Amplification 9(3):127-143.
McCormack, A., and H. Fortnum. 2013. Why do people fitted with hearing aids not wear them? International Journal of Audiology 52(5):360-368.
Middleton, A., A. Niruban, G. Girling, and P. K. Myint. 2010. Communicating in a healthcare setting with people who have hearing loss. British Medical Journal 341:726-729.
Mitchell, P., B. Gopinath, J. J. Wang, C. M. McMahon, J. Schneider, E. Rochtchina, and S. R. Leeder. 2011. Five-year incidence and progression of hearing impairment in an older population. Ear and Hearing 32(2):251-257.
Moore, B. C., M. A. Stone, and J. I. Alcántara. 2001. Comparison of the electroacoustic characteristics of five hearing aids. British Journal of Audiology 35(5):307-325.
Morton, C. C., and W. E. Nance. 2006. Newborn hearing screening—A silent revolution. New England Journal of Medicine 354(20):2151-2164.
Most, T., L. Adi-Bensaid, T. Shpak, S. Sharkiya, and M. Luntz. 2012. Everyday hearing functioning in unilateral versus bilateral hearing aid users. American Journal of Otolaryngology 33(2):205-211.
Mueller, H. G. 2001. Probe microphone measurements: 20 years of progress. Trends in Amplification 5(2):35-68.
Mueller, H. G. 2005. Fitting hearing aids to adults using prescriptive methods: An evidence-based review of effectiveness. Journal of the American Academy of Audiology 16(7):448-460.
Mueller, H. G., J. Weber, and B. W. Hornsby. 2006. The effects of digital noise reduction on the acceptance of background noise. Trends in Amplification 10(2):83-93.
Mulrow, C. D., C. Aguilar, J. E. Endicott, M. R. Tuley, R. Velez, W. S. Charlip, M. C. Rhodes, J. A. Hill, and L. A. DeNino. 1990. Quality-of-life changes and hearing impairment. A randomized trial. Annals of Internal Medicine 113(3):188-194.
Nachtegaal, J., J. M. Festen, and S. E. Kramer. 2012. Hearing ability in working life and its relationship with sick leave and self-reported work productivity. Ear and Hearing 33(1):94-103.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Hearing health care for adults: Priorities for improving access and affordability. Washington, DC: The National Academies Press.
Nash, S. D., K. J. Cruickshanks, G. H. Huang, B. E. Klein, R. Klein, F. J. Nieto, and T. S. Tweed. 2013. Unmet hearing health care needs: The Beaver Dam Offspring Study. American Journal of Public Health 103(6):1134-1139.
Neuwahl, S., E. P. Fraher, H. C. Pillsbury, M. C. Weissler, T. C. Ricketts, and K. Gaul. 2012. Trends in the otolaryngology workforce in the U.S. Bulletin of the American College of Surgeons 97(3):30-34.
NIDCD (National Institute on Deafness and Other Communication Disorders). 2013. Hearing aids. http://www.nidcd.nih.gov/health/hearing/pages/hearingaid.aspx (accessed December 28, 2016).
Nieman, C. L., N. Marrone, S. L. Szanton, R. J. Thorpe, Jr., and F. R. Lin. 2016. Racial/ethnic and socioeconomic disparities in hearing health care among older Americans. Journal of Aging and Health 28(1):68-94.
Nilsson, M., D. Gelnett, J. Sullivan, S. D. Soli, and R. L. Goldberg. 1992. Norms for the hearing in noise test: The influence of spatial separation, hearing loss, and English language experience on speech reception thresholds. The Journal of the Acoustical Society of America 92(4):2385.
Noble, W., and S. Gatehouse. 2006. Effects of bilateral versus unilateral hearing aid fitting on abilities measured by the Speech, Spatial, and Qualities of Hearing Scale (SSQ). International Journal of Audiology 45(3):172-181.
Noffsinger, D., G. B. Haskell, V. D. Larson, D. W. Williams, E. Wilson, S. Plunkett, and D. Kenworthy. 2002. Quality rating test of hearing aid benefit in the NIDCD/VA clinical trial. Ear and Hearing 23(4):291-300.
Northern, J., and C. Beyer. 1999. Reducing hearing aid returns through patient education. Audiology Today 11(2):10-11.
Oeding, K., and M. Valente. 2013. Sentence recognition in noise and perceived benefit of noise reduction on the receiver and transmitter sides of a BICROS hearing aid. Journal of the American Academy of Audiology 24(10):980-991.
Oh, S. H., and J. Lee. 2016. General framework of hearing aid fitting management. Journal of Audiology & Otology 20(1):1-7.
Pandhi, N., J. R. Schumacher, S. Barnett, and M. A. Smith. 2011. Hearing loss and older adults perceptions of access to care. Journal of Community Health 36(5):748-755.
Preminger, J. E. 2011. Group audiologic rehabilitation for adults and their communication partners. The ASHA Leader 16(8):14-17.
Popelka, M. M., K. J. Cruickshanks, T. L. Wiley, T. S. Tweed, B. E. Klein, and R. Klein. 1998. Low prevalence of hearing aid use among older adults with hearing loss: The Epidemiology of Hearing Loss Study. Journal of the American Geriatrics Society 46(9):1075-1078.
Roth, T. 2015. Chapter 20: Aging of the auditory system. In Handbook of clinical neurology, Vol. 29, edited by G. G. Celesia and G. Hickok. Edinburgh, U.K.: Elsevier. Pp. 357-373.
Rouse, M. 2016. Signal-to-noise ratio. http://searchnetworking.techtarget.com/definition/signal-to-noise-ratio (accessed February 8, 2017).
Shanks, J. E., R. H. Wilson, V. Larson, and D. Williams. 2002. Speech recognition performance of patients with sensorineural hearing loss under unaided and aided conditions using linear and compression hearing aids. Ear and Hearing 23(4):280-290.
Shi, L. F., K. A. Doherty, T. M. Kordas, and J. T. Pellegrino. 2007. Short-term and long-term hearing aid benefit and user satisfaction: A comparison between two fitting protocols. Journal of the American Academy of Audiology 18(6):482-495.
Southall, K., J.-P. Gagné, and M. B. Jennings. 2010. Stigma: A negative and a positive influence on help-seeking for adults with acquired hearing loss. International Journal of Audiology 49(11):804-814.
Strom, K. E. 2014. HR 2013 hearing aid dispenser survey: Dispensing in the age of Internet and big box retailers. http://www.hearingreview.com/2014/04/hr-2013-hearing-aid-dispenser-survey-dispensing-age-internet-big-box-retailers-comparison-present-past-key-business-indicators-dispensing-offices (accessed February 9, 2017).
Sweetow, R., and C. V. Palmer. 2005. Efficacy of individual auditory training in adults: A systematic review of the evidence. Journal of the American Academy of Audiology 16(7):494-504.
Thibodeau, L. 2014. Comparison of speech recognition with adaptive digital and FM remote microphone hearing assistance technology by listeners who use hearing aids. American Journal of Audiology 23(2):201-210.
TRICARE. 2015. Hearing aids. http://www.tricare.mil/CoveredServices/IsItCovered/HearingAids.aspx (accessed February 28, 2016).
Turner, C. W., L. E. Humes, R. A. Bentler, and R. M. Cox. 1996. A review of past research on changes in hearing aid benefit over time. Ear and Hearing 17(Suppl. 3):14S-25S.
Tye-Murray, N., J. L. Spry, and E. Mauzé. 2009. Professionals with hearing loss: Maintaining that competitive edge. Ear and Hearing 30(4):475-484.
University of Arkansas Rehabilitation Research and Training Center. 2008. Model state plan for vocational rehabilitation services to persons who are deaf, deaf-blind, heard of hearing, or late deafened. Little Rock, AR: University of Arkansas.
U.S. Department of Education. 2016. Welcome to RSA. http://www2.ed.gov/about/offices/list/osers/rsa/index.html (accessed February 28, 2016).
VA (U.S. Department of Veterans Affairs) Office of the Inspector General. 2014. Audit of VA’s hearing aid services. Washington, DC: VA.
Valente, M., H. Abrams, D. Benson, T. Chisolm, D. Citron, D. Hampton, and R. Sweetow. 2006. Guidelines for the audiologic management of adult hearing impairment. Audiology Today 18(5):32-37.
van Eyken, E., G. Van Camp, and L. Van Laer. 2007. The complexity of age-related hearing impairment: Contributing environmental and genetic factors. Audiology and Neurotology 12(6):345-358.
van Vliet, D. 2005. The current status of hearing care: Can we change the status quo? Journal of the American Academy of Audiology 16(7):410-418.
Ventry, I. M., and B. E. Weinstein. 1982. The Hearing Handicap Inventory for the Elderly: A new tool. Ear and Hearing 3(3):128-134.
Wahl, H. W., V. Heyl, P. M. Drapaniotis, K. Hörmann, J. B. Jonas, P. K. Plinkert, and K. Rohrschneider. 2013. Severe vision and hearing impairment and successful aging: A multidimensional view. The Gerontologist 53(6):950-962.
WHO (World Health Organization). 2001. International Classification of Functioning, Disability and Health. Geneva, Switzerland: WHO.
WHO. 2015. Deafness and hearing loss fact sheet. http://www.who.int/mediacentre/factsheets/fs300/en (accessed December 20, 2016).
Wu, Y. H., E. Stangl, R. A. Bentler, and R. W. Stanziola. 2013. The effect of hearing aid technologies on listening in an automobile. Journal of the American Academy of Audiology 24(6):474-485.
Yamasoba, T., F. R. Lin, S. Someya, A. Kashio, T. Sakamoto, and K. Kondo. 2013. Current concepts in age-related hearing loss: Epidemiology and mechanistic pathways. Hearing Research 303(Suppl.):30-38.
Yueh, B., P. E. Souza, J. A. McDowell, M. P. Collins, C. F. Loovis, S. C. Hedrick, S. D. Ramsey, and R. A. Deyo. 2001. Randomized trial of amplification strategies. Archives of Otolaryngology—Head & Neck Surgery 127(10):1197-1204.
ANNEX TABLE 5-1
Selected Hearing Technologies Taxonomy
| Device | Cost Range | Prevalence of Use (%)a (age range) | Intended Use | Requirements for Use |
|---|---|---|---|---|
| Hearing Aid(s) | $1,000–$4,000 / ear (Kochkin, 2009) | 15–30%d of adults with hearing loss (Blackwell et al., 2014) | Situational to all waking hours (Chien and Lin, 2012) |
|
| Remote Microphone Systems (Hearing Assistive Technology) | $1,000– $3,000e |
2–3% of adults with hearing loss (CDC, 2011) | High in noise (Thibodeau, 2014) |
|
| PSAPs Personal Sound Amplification Products | $25–$400 (Breitbart et al., 2014) | 10% of adults with hearing loss (Abrams and Kihm, 2015) | Low (Breitbart et al., 2014) |
|
NOTE: FDA = U.S. Food and Drug Administration.
a Prevalence of use data based on number of adults with hearing loss who report using devices.
b Most devices require limited training or adaptation to use.
c Limitations of device vary based on degree of hearing loss, age, and other factors.
d Based on calculations by NIDCD Epidemiology and Statistics Program staff using data collected by (1) the National Health Interview Survey (NHIS) annually for number of persons who have ever used a hearing aid [numerator], and (2) periodic NHANES hearing exams for representative samples of the U.S. adult and older adult population [denominator].
e Range of retail prices on June 1, 2016.
| Training and Adaptionb | Benefits of Device | Limitations of Devicec | Life Span of Device (years) | Maintenance | Other Considerations |
|---|---|---|---|---|---|
| Immediate to short term (Cox et al., 1996) |
|
High in noise; Low in quiet (Ciorba et al., 2012; McArdle et al., 2005) | 4–6 years | 2–4 check-ups annually to maintain small parts |
|
| Immediate to short term |
|
Low in noise (Thibodeau, 2014) | 4–6 years | 1–2 check-ups annually to maintain small parts |
|
| Immediate to short term |
|
|
1–3 years | Annual check to verify function |
|
ANNEX TABLE 5-2
Selected Hearing Technologies Function
| Device | One-on-One Communication in Quiet |
Small Group Discussions in Quiet | Large Group Discussions in Quiet | Distance Listening in Quiet | Communication via Telephone with One Person in Quiet |
|---|---|---|---|---|---|
| Hearing Aid(s)a Varying levels of technology | 1 | 2 | 3 | 2–3 | 3–4 |
| Remote Microphone Hearing Assistive Technology | |||||
| Connectivity system with hearing aid | 1 | 1 | 2–3 | 1 | Varies |
| FM/DM system with hearing aid | 1 | 1 | 1–2 | 1–2 | Varies |
| Independent microphone system (aka PocketTalker) | 1 | 3–5 | 5 | NA | NA |
| Select Personal Sound Amplification Products (non-customized ear-level devices)b |
1 | 1–2 | 3 | 3–4 | 3–4 |
NOTES: Ranking scale 1–5, 1, most if not all, will benefit to 5, less likely to receive benefit. NA = not accessible.
a Assumes hearing devices are programmed and fitting is completed using real ear probe microphone measurements and prescriptive targets to verify maximum audibility of the speech spectrum has been achieved. Maximum benefit also includes proper counseling regarding the care and use of the technology after the fitting. An audiologist is the most qualified professional to provide rehabilitation for the nonmedical/nonsurgical treatment of hearing loss.
b Not specifically approved for treatment of hearing loss. PSAP products are highly heterogeneous. While some select products that are properly designed could offer benefit, most others will not.
| Communication via Telephone (conference call) in Quiet | One-on-One Communication in Noise |
Small Group Discussions in Noise | Large Group Discussions in Noise | Distance Listening in Noise | Listening Without Visual Cues (videos, phone) | Sound Localization (as required for safety at work/home) |
|---|---|---|---|---|---|---|
| 4–5 | 3–4 | 4–5 | 5 | 5 | 3–5 | 3–4 |
| Varies | 3–5 | 3–5 | 4–5 | 4–5 | Varies | Varies |
| Varies | 2–5 | 2–5 | 3–5 | 3–5 | Varies | Varies |
| NA | 4–5 | 4–5 | NA | NA | NA | NA |
| 4–5 | 3–4 | 4–5 | 5 | 5 | 3–5 | 3–4 |
This page intentionally left blank.












































