3
Wheeled and Seated Mobility Devices
Wheeled and seated mobility devices (WSMDs) are medical devices that are intended to provide mobility and function for persons with restricted or no ability to ambulate without assistance from technology. This chapter begins with an overview of the use of WSMDs and a detailed taxonomy of the various types of these devices. The chapter next reviews the use of WSMDs and clinical considerations in the choice of a WSMD for a particular individual. Evaluation and monitoring, training and adaptation, and access and availability are then addressed in turn. The chapter ends with findings and conclusions.
OVERVIEW OF THE USE OF WHEELED AND SEATED MOBILITY DEVICES
The Survey of Income and Program Participation (SIPP), conducted by the U.S. Census Bureau, is a population-based source of information for overall use of WSMDs in the United States (U.S. Census Bureau, 2016). In 2010, the SIPP found that 1.5 percent of the population aged 15 and older (3.6 million people) used a WSMD (wheelchair or scooter) (U.S. Census Bureau, 2016). A study using the Canadian Survey on Disability, conducted in 2012, found the prevalence of wheelchair and scooter use among community-living Canadians aged 15 and older to be approximately 1.0 percent of the total population (Smith et al., 2016). The difference between these prevalence rates for the U.S. and Canadian populations is not discussed by the authors.
Figure 3-1 projects the number of wheelchair users over a 25-year
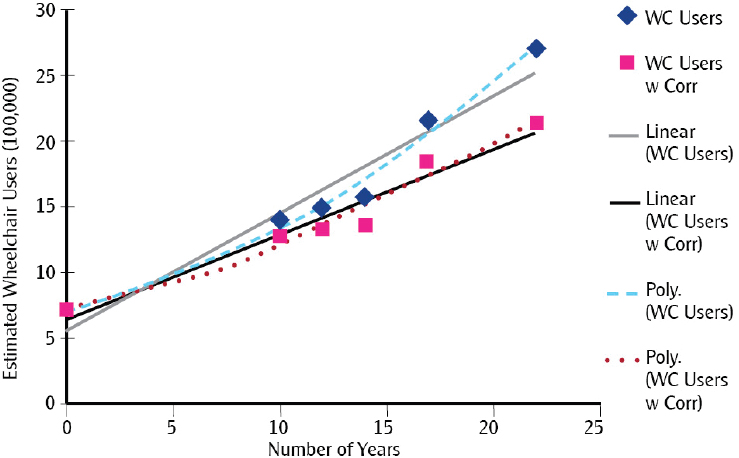
SOURCE: Flagg, J. 2009. Wheeled mobility demographics. In The industry profile on wheeled mobility, edited by S. M. Bauer and M. E. Bunning. Buffalo, NY: Rehabilitation Engineering Research Center on Technology Transfer. Pp. 7-29.
period beginning in 2005 based on data from both the National Health Interview Survey-Disability (NHIS-D) and the SIPP (CDC, 2016; Flagg, 2009; U.S. Census Bureau, 2016). These estimates include both correction for population growth (“WC Users w Corr”) and no correction for population growth (“WC Users”) (Flagg, 2009). The figure suggests a quadrupling of the estimated number of wheelchair users into the next decade.
Obtaining population-based prevalence information related to access, user characteristics, cost, and evaluation of outcomes for working-age users of WSMDs is challenging. The challenge is related to the fact that in the United States, multiple agencies and service providers are responsible for determining the need for assistive devices, providing the devices, delivering the training in their use, monitoring their use, and assessing outcomes (Crane and Minkel, 2009). This fragmented approach to the delivery of assistive device–related health care services is discussed in detail elsewhere in this report. As a result of this fragmentation, no single public-use data source includes prevalence information related to use of WSMDs specifically among individuals of working age (20-67).
TAXONOMY1
WSMDs can improve function, independence, home and community integration, activity, participation, comfort, and quality of life (Chaves et al., 2004; Davies et al., 2003; Edwards and McCluskey, 2010; Laferrier et al., 2010; Salminen et al., 2009; Scherer, 2002; Trefler et al., 2004). Many different types of such devices exist. In 2005, through the National Coverage Determination (NCD) process, the Centers for Medicare & Medicaid Services (CMS) issued function-based criteria for mobility assistive equipment (MAE), which entail an algorithmic process called the “Clinical Criteria for MAE Coverage.”
Because, as reviewed in subsequent sections of this chapter, so many such devices exist and individual needs are complex, the process for choosing and customizing the appropriate devices for a person encompasses many steps (Arledge et al., 2011). Several types of devices may serve various needs for an individual throughout the day in different contexts, especially in and around work (Iezzoni et al., 2009). A common example is the scooters used by grocery store customers. Likewise, standing wheelchairs or scooters are commonly used as workplace accommodations. Moreover, given the need for regular maintenance and repair, it is important to have a back-up WSMD to reduce or avoid maintenance- or repair-related “sick days.”
The most appropriate primary manual wheelchairs for individuals with such conditions as paraplegia due to spinal cord injury are customizable and of the lightest weight possible. The most appropriate primary powered wheelchairs are customizable and have programmable controls (Paralyzed Veterans of America Constorium for Spinal Cord Medicine, 2005). Customizable manual wheelchairs have been shown to be more durable, cost-effective, and comfortable than noncustomizable manual wheelchairs (Cooper et al., 1999; DiGiovine et al., 2000; Fitzgerald et al., 2001). Likewise, customizable powered wheelchairs have been shown to improve function, to prevent wheelchair-associated injuries, and to have significantly better durability compared with standard powered wheelchairs (Cooper, 2001; Fass et al., 2004; Worobey et al., 2012). In general, less customizable wheelchairs are more likely to fail on standardized fatigability and durability testing (DiGiovine et al., 2000).
Employment is most likely among people with good upper-body strength, coordination, and endurance who use customized or well-fitted ultra-light manual wheelchairs, sometimes with power assist devices. For individuals with impaired upper-body strength, coordination, or endurance,
___________________
1 The images in this section serve as examples of device categories only and should not be considered an endorsement of specific products or manufacturers.
a powered wheelchair with powered seating functions is most helpful for supporting employability. Powered seat elevation and powered standing are among the most important features used to increase function related to employment. Unfortunately, neither is covered by CMS.
The following subsections describe the various types of WSMDs. A summary of these descriptions is provided in Box 3-1. More detailed information on the features and functionality of these devices is provided in Annex Tables 3-1 and 3-2, respectively, at the end of this chapter.

SOURCE: Rollator Walker with Fold Up and Removable Back Support and Padded Seat. Material used with permission from Drive DeVilbiss Healthcare.
Rollators
Rollators (see Figure 3-2) are WSMDs used by individuals who have the ability to ambulate but require assistance with balance and may need to have a seat readily available to address fatigue. Rollators are most commonly used by individuals with severe cardiopulmonary limitations, those with cerebral palsy, and those who have had a cerebral vascular incident. Rollators may be covered by insurance or purchased from any number of retail outlets. They commonly cost from $100 to $150 but may cost more depending on their features. They provide very limited support for seating balance and positioning, and they require gross motor function of both the upper and lower extremities. Minimally, they extend range of reaching, lifting, and carrying. For individuals with the ability to ambulate, rollators may improve mobility, which in turn improves participation in activities of daily living (ADLs), community integration, and employment.
Manual Wheelchairs
The wide variety of manual wheelchairs can be divided into two general categories: (1) those intended to be propelled by an assistant, and (2) those intended to be propelled by the user. Within these broad categories are multiple subcategories and many options and combinations. Describing all the different varieties, styles, and options of manual wheelchairs is not feasible; therefore, only broad groupings based on Medicare coding are included here. It is worth noting that outside of the United States, most countries use a coding scheme based on International Organization for Standardization (ISO) 9999. Relative to the ultra-lightweight manual wheelchair (K0005), other manual wheelchairs tend to be larger and heavier, which makes them difficult to self-propel (especially over such surfaces as carpet or on ramps) and heavy (making them difficult to load in a vehicle), and they require
large turning radii, which, for example, makes it difficult to turn from a hallway into a bathroom within the home. Clinical practice guidelines and many research studies have shown that ultra-lightweight manual wheelchairs last longer, require less maintenance, and induce fewer injuries to the upper extremities compared with other types of manual wheelchairs (Paralyzed Veterans of America Constorium for Spinal Cord Medicine, 2005).
Standard Manual Wheelchairs (K0001, K0003, K0006, K0007)
The K0001standard manual wheelchair (see Figure 3-3) has few adjustable features and is intended primarily for short-term or temporary use, commonly defined as less than 3 months. The weight of such wheelchairs is typically in the range of 60-80 pounds. These devices are not suitable for individuals whose primary means of mobility will be a wheelchair. They tend to be difficult to propel by the user and to function well only on smooth, firm, flat indoor surfaces. These wheelchairs also provide limited support for seating balance and positioning and require gross motor function of the upper extremities. Their fixed seating does not extend range of reaching, lifting, and carrying. Prices range from a low of $150 to a high of $1,000, depending on the configuration and accessories. A K0003 is nearly the same as a K0001 but lighter in weight. It is intended for individuals who cannot adequately propel a K0001. Either a K0001 or a K0003 may be equipped with a reclining backrest (E1226) if required. Wheelchairs coded K0006 are for individuals who weigh more than 250 pounds, while those coded K0007 are intended for individuals who weigh more than 300 pounds. Large individuals tend to be better served by powered wheelchairs because of the strain on their upper extremities that results from their propelling a manual wheelchair. All of these wheelchairs provide minimal

SOURCE: iStock.com/prill.

SOURCE: Start M3 Hemi. Courtesy of Ottobock.
mobility, which severely limits participation in ADLs, community integration, and employment.
Standard Hemi-Wheelchair (K0002)
Like the standard manual wheelchairs described above, the standard hemi-wheelchair (K0002), depicted in Figure 3-4, typically has few adjustable features and is intended primarily for short-term or temporary use, commonly defined as less than 3 months. These wheelchairs are intended primarily for individuals who are of short stature or who need to place their feet on the ground for propulsion. Otherwise, many of their features are similar to those of a standard manual wheelchair (K0001). They provide limited support for seating balance and positioning; they require gross motor function of the upper extremities; and their fixed seating does not extend range of reaching, lifting, and carrying. These chairs also provide minimal mobility, which severely limits participation in ADLs, community integration, and employment.
High-Strength Lightweight Model Wheelchair (K0004)
The high-strength lightweight model wheelchair (K0004), depicted in Figure 3-5, has minimal adjustable features, which commonly include a small range of rear axle adjustment, arm rest positioning, and leg rest length. K0004 wheelchairs are used longer term relative to the standard manual wheelchairs and standard hemi-wheelchairs described above, primarily by people who travel very short distances in indoor environments. Individuals who use K0004 wheelchairs typically use them at least 2 hours per day; self-propel; and according to Medicare guidelines, which are followed by

SOURCES: A. Poly Fly Light Weight Transport Chair Wheelchair with Swing away Footrest. Material used with permission from Drive DeVilbiss Healthcare; B. PANTHERA X. Courtesy of Panthera.
most insurers, require such a wheelchair for at least one mobility-related ADL. K0004 wheelchairs are acceptable for short-distance mobility over flat, firm, and stable surfaces. However, they provide limited support for seating balance and positioning; they require gross motor function of the upper extremities; and their fixed seating does not extend range of reaching, lifting, and carrying. These chairs also provide minimal mobility, which severely limits participation in ADLs, community integration, and employment. Costs for K0004 wheelchairs range between $250 and $5,000. There are some challenges related to the K0004 coding, as there are large disparities in the quality of these wheelchairs and their suitability for meeting various users’ needs. They range, for example, from low-cost steel wheelchairs that are similar to K0003 wheelchairs in nearly every respect to very high-performance carbon fiber wheelchairs designed with minimal adjustments for experienced and skilled users.
Ultra-Lightweight Model Wheelchair (K0005)
The ultra-lightweight model wheelchair (K0005) (see Figure 3-6) includes all of the essential adjustable features or custom fittings required to meet the needs of long-term (greater than 3 months) wheelchair use as the primary means of mobility (defined as at least 2 hours per day). Relative to the wheelchairs described above, K0005 wheelchairs have been shown to be more durable, to require less maintenance, and to be safer for
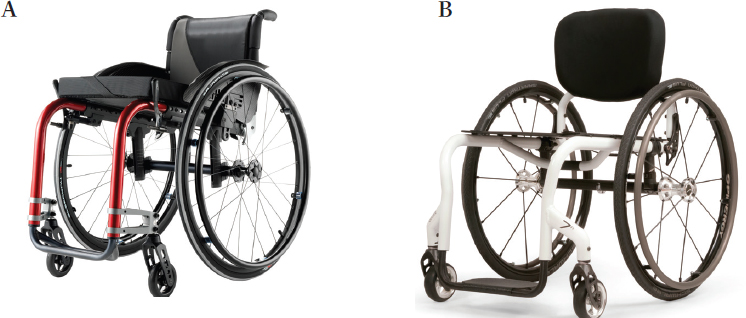
SOURCES: A. Küschall® Advance™. © Invacare Corporation. Used with permission; B. QUICKIE 7R. Photo courtesy of Sunrise Medical® and the QUICKIE® brand.
most long-term manual wheelchair users. Clinical practice guidelines for individuals with spinal cord injury, which are relevant to other diagnoses, recommend K0005 wheelchairs. These wheelchairs are fitted to suit individual user needs and the environment in which the user lives. They are easier to propel than the other classes of wheelchairs and are suitable for all indoor environments and for common Americans with Disabilities Act (ADA)-compliant outdoor environments. The cost for a K0005 wheelchair ranges from $1,000 to $8,000. These wheelchairs vary widely in style, form, weight, and function. They provide preferred support for seating balance and positioning; they require gross motor function of the upper extremities; and their custom or adjustable seating extends range of reaching, lifting, and carrying. These wheelchairs provide functional mobility with minimal limitations for participation in ADLs, community integration, and employment.
Powered Wheeled and Seated Mobility Devices
Although there are many different types of powered WSMDs, they fall into three broad categories: (1) those that are manually steered with speed/braking control; (2) those that are manually propelled with power assist; and (3) those that have power steering and speed/braking. According to Medicare guidelines, a person who qualifies for coverage of a powered WSMD must meet the following conditions:
(A) the person must have a mobility limitation that significantly impairs his or her ability to participate in one or more Mobility-Related Activities of Daily Living (MRADLs) in customary locations in the home; (B) the person’s mobility limitation cannot be sufficiently and safely resolved by using an appropriately fitted cane or walker; and (C) the patient does not have sufficient upper extremity function to self-propel an optimally configured manual wheelchair in the home to perform MRADLs during a typical day. (CMS, 2009)
The U.S. Department of Veterans Affairs (VA) applies broader criteria that include the veteran’s participating in his or her health care and the prevention or treatment of further injury. There are numerous types of powered WSMDs, including a number of devices in use that are not regulated by the U.S. Food and Drug Administration or covered by Medicare and other insurance companies. Examples include the Segway and similar products that are used as mobility devices without modification of their original equipment manufacturer design, as well as versions that have been radically modified (see Figure 3-7) either by the person using the device or in some cases by an after-market manufacturer. There are also devices that use tracks or clusters of wheels for specialized purposes, such as outdoor mobility over unfinished terrain (see Figure 3-8) or climbing stairs. These devices have their place in the market and meet the needs of their users, in some cases including vocational needs. For someone who works on

NOTE: The seat is identified as the Sui Generis Seat.
SOURCE: Sui Generis Seat, 2015.

SOURCE: Action Trackchair. Courtesy of Action Manufacturing.
construction sites or outdoors as a park employee, for example, an outdoor wheelchair may be entirely appropriate. Several classes of powered WSMDs are described below. Group 5 devices are primarily for pediatric use and are intended for individuals who weigh less than 125 pounds and are expected to grow.
Power Operated Vehicles
Power operated vehicles (POVs) (see Figure 3-9), also known as scooters, are three- or four-wheeled mobility devices that are manually steered and provide control for speed/braking. According to Medicare guidelines, to be eligible for coverage of a POV, a person must meet the general criteria described previously and also meet the following criteria:
- The person must be able to transfer safely to and from a POV.
- The person must be able to operate the manual tiller steering system.
- The person must be able to maintain postural stability and position while operating the POV in the home.
- The person’s mental and physical capabilities must be sufficient for safe mobility using a POV in the home.
- The person’s weight must be less than or equal to the weight capacity of the POV and greater than or equal to 95 percent of the weight capacity of the next-lower-weight class of POV.
- The person’s home must provide adequate access between rooms, maneuvering space, and surfaces for the operation of the POV.
- Using a POV will significantly improve the person’s ability to participate in MRADLs, and the person will use the POV in the home.
- The person has not expressed unwillingness to use a POV in the home. (CMS, 2015b)
POVs generally provide limited seating options, typically only height and minimal seat-to-backrest angle adjustment. Specialized seating and pressure-relieving cushions usually are not options. Because of their length and manual tiller steering, POVs tend to have larger turning radii relative to wheelchairs. They are intuitive to operate and frequently are used by individuals with cardiorespiratory or standing balance issues. Ranging in cost from about $500 to $5,000, these devices are intended primarily for outdoor use in ADA-compliant environments, although some small models provide indoor mobility within the home; however, caution must be exercised when using a high-seat-height and narrow-footprint POV outdoors. These wheelchairs provide limited support for seating balance and positioning; they require gross motor function of the upper extremities; and their fixed seating does not extend range of reaching, lifting, and carrying. These chairs also provide minimal mobility, which severely limits participation in ADLs, community integration, and employment.

SOURCES: A. Spitfire Scout 3 Wheel Travel Power Scooter. Material used with permission from Drive DeVilbiss Healthcare; B. Invacare® Colibri Scooter. © Invacare Corporation. Used with permission.

SOURCE: Cobalt X16 Transportable Power Wheelchair Rear-Wheel Drive. Material used with permission from Drive DeVilbiss Healthcare.
Group 1 Powered Wheelchairs
Powered wheelchairs in Group 1 (see Figure 3-10) are basic units without specialized or custom seating and with standard programmable joystick controls. Powered wheelchairs use differential steering, which basically means that the powered wheels turn at different speeds depending on the signals from the joystick (or other user control interface) used to turn the wheelchair. Group 1 powered wheelchairs are used by individuals whose needs are not adequately met by a manual wheelchair or a POV but who do not require a powered wheelchair from Group 3 or 4. Group 1 powered wheelchairs are designed primarily for flat, smooth, firm, and stable indoor surfaces, although minimal slopes can be negotiated. The cost of Group 1 powered wheelchairs varies from about $1,200 to $5,000. These devices are used primarily in institutional settings. They provide limited support for seating balance and positioning; they require fine motor function of the upper extremities; and their fixed seating does not extend range of reaching, lifting, and carrying. These chairs provide minimal mobility, which severely limits participation in ADLs, community integration, and employment.
Group 2 Powered Wheelchairs
There are many different types of Group 2 powered wheelchairs (see Figure 3-11), which fall into four basic categories: (1) power base with captain seat, (2) power base or integrated powered wheelchair with rehabilitation seating, (3) power base with single power seating option, and

SOURCE: Jazzy® 600 ES. Photo courtesy of Pride Mobility Inc.
(4) power base with multiple power seating option. Rehabilitation seating is used to help prevent pressure ulcers and/or to accommodate postural asymmetries and for individuals with impaired sensation. Group 2 powered wheelchairs are intended primarily for indoor use within home environments, but they are suitable for use over short distances outside of the home in ADA-compliant environments. Their durability is modest, as they last about 3 years before replacement or significant repair becomes necessary. Power seat functions may be included in Group 2 powered wheelchairs, including seat tilt, seat recline, and leg rest elevation. Medicare does not currently cover seat elevation; however, the VA and some other providers do. Seat elevation has been shown to improve the user’s ability to transfer safely, to improve functional reach, and to increase the usable workspace (Arva et al., 2009). Group 2 powered wheelchairs range in price from about $2,000 to $12,000. They provide limited to moderate support for seating balance and positioning; they require fine motor function of the upper extremities; and their seating may to a limited degree extend range of reaching, lifting, and carrying. These chairs also provide minimal mobility, which limits participation in ADLs, community integration, and employment.
Group 3 Powered Wheelchairs
Powered wheelchairs in Group 3 (see Figure 3-12) are similar to those in Group 2 in many respects. They include rehabilitation seating and, in many cases, at least one powered seat function. Three primary factors differentiate a Group 3 wheelchair: (1) the person requires alternative

SOURCE: F3 Corpus. Copyright © 2017 Permobil.
controls, (2) a qualified clinical professional deems a specialized seating system necessary, and (3) the person requires a more durable or active user-powered wheelchair because of his or her home environment. Group 3 powered wheelchairs are suitable for indoor use and for outdoor use in ADA-compliant environments. Their durability is about 5 years with regular maintenance, with the frequency of maintenance increasing with the usage of power seat functions and alternative controls. Group 3 powered wheelchairs have a range of about 10 to 12 miles on a single charge under optimal conditions. Their cost ranges from $5,000 to $30,000, depending on the features required. These wheelchairs provide support for seating balance and positioning; alternative controls are available for individuals without fine motor function of the upper extremities; and their seating may extend range of reaching, lifting, and carrying. These chairs also provide mobility that permits participation in ADLs, community integration, and employment.
Group 4 Powered Wheelchairs
Medicare does not cover Group 4 powered wheelchairs (see Figure 3-13) because it considers them to have additional capabilities that are not necessary for use within the home (e.g., speed of 6 mph, curb climb of 75 mm,
range of 16 miles/charge). The VA and other providers do cover Group 4 devices. The difference is due primarily to Medicare’s focus on in-home usage, whereas the VA and state vocational rehabilitation programs have a broader mandate that includes participation in health management and return to work or school.
Some Group 4 devices would probably be better classified as Group 3 or otherwise covered because they offer the same features as Group 3 devices but have higher performance, durability, or safety; are appropriate for use in the home; and would better meet users’ health and mobility needs. In other cases, the Group 4 classification provides little guidance because Medicare, as well as insurers that take their lead from Medicare coding experts, has tended to use this category to encompass “all other wheeled mobility devices.” Some Group 4 devices are the most appropriate mobility device for particular users given their level of activity, their functional performance needs, and their environment. For example, college students need to be able to travel across campus to participate in their education.

SOURCES: A. Prototype Next Generation iBOT Base. Photo is copyright DEKA Research & Development Corp. Used with permission; B. F5 Corpus. Copyright © 2017 Permobil.
Thus, they require year-round indoor and outdoor mobility, including the ability to travel more than several miles per day. As another example, a person may wish to return to work as a construction site manager or civil engineer and be able to negotiate uneven terrain over unfinished surfaces. In some cases, a Group 4 device may simply be needed to attend appointments with health care professionals within a large medical complex that requires negotiating hills or longer distances. Given the broad range of devices encompassed by Group 4, prices range from about $6,000 to $50,000, depending on the features and capabilities. These wheelchairs provide significant support for seating balance and positioning; alternative controls are available for individuals without fine motor function of the upper extremities; and their seating may extend range of reaching, lifting, and carrying. These chairs also provide mobility that permits participation in ADLs, community integration, and employment.
Power Assist Wheelchairs
Power assist wheelchairs (see Figure 3-14) are hybrid devices that have some of the attributes of manual wheelchairs and some of the benefits of powered wheelchairs. The power to propel the wheelchair comes from a combination of the user’s arms and a power source (typically a battery) and motors (either integrated into the wheels or using a separate wheel or set of wheels). Power assist wheelchairs do not have all of the features of powered wheelchairs and cannot accommodate some impairments; however, they offer an alternative to a powered wheelchair for individuals who could otherwise use a manual wheelchair but lack the ability to propel a manual wheelchair effectively because of strength or endurance limitations

SOURCE: Quickie Xtender on a Quickie 2 wheelchair. Photo courtesy of Sunrise Medical® and the QUICKIE® brand.
or pain. Power assist wheelchairs are intended primarily for indoor use and for outdoor use in ADA-compliant environments. Their cost ranges from $4,000 to $10,000. These wheelchairs generally provide support for seating balance and positioning; they require some degree of gross motor function of the upper extremities; and their custom or adjustable seating extends range of reaching, lifting, and carrying. These chairs also provide functional mobility with minimal limitations that permits participation in ADLs, community integration, and employment.
Standing Wheelchairs
Standing wheelchairs may be manual, powered, or some combination thereof. They either promote passive standing in a stationary position (normally the case with manual devices) or provide some mobility on level surfaces. There are many physiological benefits to standing, but one of the most important is extended reach and range of motion that support employment-related activities. Standing wheelchairs may be used, for example, by health care professionals to perform medical procedures, by technicians to operate machines, and by teachers to access laboratory equipment and whiteboards. Powered wheelchairs with powered standing features are most commonly used for employment as they provide a stable and mobile platform. These wheelchairs extend range of reaching, and they may improve participation in ADLs, community integration, and employment.
THE USE OF WHEELED AND SEATED MOBILITY DEVICES
The committee used three data sources to examine WSMD use, including the association among diagnosis, impairment, and type of device used by working-age adults: (1) the SIPP (U.S. Census Bureau, 2016); (2) the National Center for Health Statistics’ National Health Interview Survey (NHIS) and NHIS-D (CDC, 2016); and (3) CMS’s Durable Medical Equipment (DME) files (CMS, 2013). The SIPP, NHIS, and NHIS-D include data on the civilian noninstitutionalized population and use similar methodologies for data collection and reporting. Differences include variations in years of study, sampling, scope, and level of detail gathered. The CMS DME files used in the analyses presented below are based on a random sample of the Medicare beneficiary population. Of particular interest to the committee are individuals aged 20-67 who receive Social Security Disability Insurance (SSDI). Table 3-1 highlights characteristics of the SIPP; the NHIS, including the NHIS-D; and the CMS DME.
Other sources of national-level data on WSMDs include the VA health care system, databases of state departments or offices of vocational rehabilitation, and data files of large health care systems (e.g., Kaiser Permanente).
TABLE 3-1
Characteristics of the SIPP, NHIS/NHIS-D, and CMS DME Data Sources
| Characteristic | SIPP | NHIS/NHIS-Da | CMS-DME |
|---|---|---|---|
| Population | Noninstitutionalized U.S. population (does not include nursing homes) | Noninstitutionalized U.S. population (does not include nursing homes) | Medicare beneficiaries |
| Level of Device Detail | Single category for manual or electric wheelchair or electric scooter | Separate categories for manual wheelchair, electric wheelchair, and scooter | Healthcare Common Procedure Coding System for Durable Medical Equipment—wheelchairs (manual and powered) and scooters |
| Definition of Wheelchair Users | Participants stated that they used a wheelchair at the time of the survey | Must have been, or must be expected to be, using the device for 12 months or longer | Diagnosis and approved provider prescription for medical necessity using CMS codes |
| Date (years) | Panels 1984–2008 | 1957–2013 NHIS 1994–1997 NHIS-Da |
2010–2014 |
NOTE: CMS = Centers for Medicare & Medicaid Services; DME = Durable Medical Equipment; NHIS = National Health Interview Survey; NHIS-D = National Health Interview Survey-Disability; SIPP = Survey of Income and Program Participation.
aRepresents a separate more detailed survey with additional questions and information on persons with a disability.
SOURCES: CDC, 2016; CMS, 2013; U.S. Census Bureau, 2016.
A study by Hubbard and colleagues (2007), for example, is the first to investigate Veterans Health Administration costs for providing wheelchairs and scooters and to compare regional prescription patterns. However, the committee did not attempt to review data from these sources to determine the association between disability diagnoses and WSMD use for two reasons: first, the extent to which these data sources are representative of the working population is not known; and second, the data are restricted, proprietary, or not available as public-use files for analyses.
The analyses and figures presented below are based on information included in the CMS DME files (see Appendix C for a detailed description of the analysis methods). The DME files include a level of detail and number of variables not available in government-funded population-based surveys. For example, information on health conditions and medical diagnoses
can be compared with the prescription and purchase of specific types of WSMDs. Likewise, the geographic location, distribution, and cost of WSMDs can be related to individual characteristics (age, gender, race/ethnicity), medical diagnosis (International Classification of Diseases, Ninth Revision [ICD-9] codes), and facility factors (urban versus rural, nonprofit versus profit).
Moreover, national surveys that collect WSMD information employ inconsistent methodologies, which makes it difficult to combine the data and identify trends and growth (Flagg, 2009). For example, the surveys use different criteria for determining a WSMD user, as well as for determining device use. As shown earlier in Table 3-1, the NHIS-D has separate categories for manual wheelchairs, electric wheelchairs, and scooters; the CMS DME files contain categories for manual wheelchairs, powered wheelchairs, and scooters. However, the SIPP contains a single category that includes manual wheelchairs, electric wheelchairs, and electric scooters. In addition, few surveys contain data on the magnitude and growth of wheelchair sales and use (Flagg, 2009). In particular, data are limited on who buys, rents, and uses powered wheelchairs (Edwards and McCluskey, 2010). There is also limited research on mobility scooters (Mortenson and Kim, 2016). According to Flagg (2009), few studies analyze the relationship between wheelchair use and gender. Furthermore, there are limited data showing the relationship between individual users’ medical conditions and health (e.g., comorbidities) and/or sociodemographic characteristics and the specific types of WSMDs they use.
The DME files contain fee-for-service claims submitted by DME suppliers. DME includes a wide range of devices and services for persons with illness, injury, or chronic health conditions. Examples include crutches, hospital beds, and oxygen equipment, as well as WSMDs. The files include medical diagnoses (ICD-9 codes), comorbidities, services/devices provided as defined by the CMS Healthcare Common Procedure Coding System (HCPCS), dates of service, reimbursement amounts, and beneficiary demographic information.
It is important to identify and understand the limitations2 of the DME files to interpret the information presented below. Since the committee’s focus was on the working-age population, only persons aged 20-67 were included in the analyses. Participants under age 65 were receiving benefits from SSDI or the Medicare End-Stage Renal Disease program. Individuals who qualify for SSDI are automatically enrolled in Medicare after receiving disability benefits for 2 years. In 2015, more than 5 million Medicare beneficiaries were under age 65 and qualified for SSDI (CMS, 2015a). In 2013, more than 380,000 beneficiaries qualified for the fee-for-service Medicare
___________________
2 Further information on data limitations is given in Appendix C.
TABLE 3-2
Demographic Characteristics of Users of Wheeled and Seated Mobility Devices by Gender
| Variable | Female | Male | Total |
|---|---|---|---|
| DME Sample (5%): number (percent) | 10,691 (56.3%) | 8,303 (43.7%) | 18,994 |
| Age: mean (standard deviation) | 57.31 (9.56) | 56.20 (10.04) | 56.83 (9.79) |
| Age: number (percent) | |||
|
20–45 |
1,346 (51.6%) | 1,261 (48.4%) | 2,607 |
|
46–55 |
2,246 (54%) | 1,917 (46%) | 4,163 |
|
56–64 |
3,900 (56.7%) | 2,974 (43.3%) | 6,874 |
|
65–67 |
3,199 (59.8%) | 2,151 (40.2%) | 5,350 |
| Race: number (percent) | |||
|
White |
7,206 (56.4%) | 5,571 (43.6%) | 12,777 |
|
Black |
2,228 (58.7%) | 1,565 (41.3%) | 3,793 |
|
Hispanic |
894 (52.7%) | 803 (47.3%) | 1,697 |
|
Other |
363 (49.9%) | 364 (50.1%) | 727 |
NOTE: Information from 5 percent random sample of 2013-2014 Durable Medical Equipment (DME) Medicare beneficiaries aged 20–67.
SOURCE: DME Research Identifiable File, Centers for Medicare & Medicaid Services.
End-Stage Renal Disease program; approximately 19 percent of them were under age 65 (CMS, 2013).
Table 3-2 includes demographic information for a 5 percent random sample of beneficiaries from the Medicare DME files. This sample was used to estimate WSMD use and address issues identified for this study by the U.S. Social Security Administration (see Chapter 1), including the number of selected devices by the characteristics of users; the availability of the devices; and variation in their use across settings, age groups, and different diagnostic conditions and impairments. The data presented in all of the following tables are unadjusted for beneficiaries’ sociodemographic and clinical characteristics.
Table 3-3 shows the numbers of various types of WSMDs among the DME sample displayed in Table 3-2. Medicare classifies WSMDs using the HCPCS codes.
The standard and lightweight wheelchairs accounted for about 49 percent of the WSMDs used by Medicare beneficiaries in the DME files for 2013 and 2014. (See the descriptions of these devices in the previous
| HCPCS Descriptiona | Number | Percent | Cumulative Number | Cumulative Percentb |
|---|---|---|---|---|
| Standard wheelchair | 6,579 | 34.6 | 6,579 | 34.6 |
| Lightweight wheelchair | 2,798 | 14.7 | 9,377 | 49.4 |
| Powered wheelchair, Group 2 standard, captains chair, patient weight capacity up to and including 300 pounds | 2,229 | 11.7 | 11,606 | 61.1 |
| High-strength, lightweight wheelchair | 1,720 | 9.1 | 13,326 | 70.2 |
| Heavy-duty wheelchair | 858 | 4.5 | 14,184 | 74.7 |
| Extra-heavy-duty wheelchair | 769 | 4.0 | 14,953 | 78.7 |
| Powered wheelchair, Group 2 heavy-duty, captains chair, patient weight capacity 301 to 450 pounds | 590 | 3.1 | 15,543 | 81.8 |
| Powered wheelchair, Group 3 standard, multiple power option, sling/solid seat/back, patient weight capacity up to and including 300 pounds | 555 | 2.9 | 16,098 | 84.8 |
| Ultra-lightweight wheelchair | 504 | 2.7 | 16,602 | 87.4 |
| Manual adult-size wheelchair, includes tilt-in-space | 428 | 2.3 | 17,030 | 89.7 |
| Powered wheelchair, Group 2 standard, sling/solid seat/back, patient weight capacity up to and including 300 pounds | 340 | 1.8 | 17,370 | 91.4 |
| Powered wheelchair, Group 3 standard, single power option, sling/solid seat/back, patient weight capacity up to and including 300 pounds | 334 | 1.8 | 17,704 | 93.2 |
| Transport chair, adult size, patient weight capacity up to and including 300 pounds | 323 | 1.7 | 18,027 | 94.9 |
| Standard hemi (low-seat)-wheelchair | 206 | 1.1 | 18,233 | 96.0 |
| Power operated vehicle, Group 1 standard, patient weight capacity up to and including 300 pounds | 150 | 0.8 | 18,383 | 96.8 |
| HCPCS Descriptiona | Number | Percent | Cumulative Number | Cumulative Percentb |
|---|---|---|---|---|
| Powered wheelchair, Group 3 standard, sling/solid seat/back, patient weight capacity up to and including 300 pounds | 78 | 0.4 | 18,461 | 97.2 |
| Powered wheelchair, Group 2 heavy duty, sling/solid seat/back, patient weight capacity 301 to 450 pounds | 62 | 0.3 | 18,523 | 97.5 |
| Powered wheelchair, Group 1 standard, captains chair, patient weight capacity up to and including 300 pounds | 57 | 0.3 | 18,580 | 97.8 |
| Powered wheelchair, Group 2 very heavy duty, captains chair, patient weight capacity 451 to 600 pounds | 54 | 0.3 | 18,634 | 98.1 |
| Powered wheelchair, Group 3 standard, captains chair, patient weight capacity up to and including 300 pounds | 46 | 0.2 | 18,680 | 98.3 |
| Powered wheelchair, Group 3 heavy-duty, multiple power option, sling/solid seat/back, patient weight capacity 301 to 450 pounds | 41 | 0.2 | 18,721 | 98.6 |
| Powered wheelchair, Group 2 standard, single power option, sling/solid seat/back, patient weight capacity up to and including 300 pounds | 37 | 0.2 | 18,758 | 98.8 |
| Powered wheelchair, Group 2 standard, portable, captains chair, patient weight capacity up to and including 300 pounds | 35 | 0.2 | 18,793 | 98.9 |
| Powered operated vehicle, Group 1 heavy-duty, patient weight capacity 301 to 450 pounds | 34 | 0.2 | 18,827 | 99.1 |
| Manual wheelchair accessory, push-activated power assist | 24 | 0.1 | 18,851 | 99.2 |
NOTE: Information from 5 percent random sample (n = 18,994) of 2013–2014 Durable Medical Equipment (DME) Medicare beneficiaries aged 20–67.
a Data not shown for HCPCS wheelchairs with cell sizes <20.
b Percentages may not total because of rounding.
SOURCE: DME Research Identifiable File, Centers for Medicare & Medicaid Services.
TABLE 3-4
Use of Manual Versus Powered Wheelchairs by Age and Race/Ethnicity
| Age Category | Wheelchair Type: Number (Percent) | ||
|---|---|---|---|
| Manual Wheelchair | Powered Wheelchair | Totala | |
| 20–45 | 1,991 10.48% |
616 3.24% |
2,607 13.73% |
| 46–55 | 2,998 15.78% |
1,165 6.13% |
4,163 21.92% |
| 56–64 | 4,970 26.17% |
1,904 10.02% |
6,874 36.19% |
| 65–67 | 4,280 22.53% |
1,070 5.63% |
5,350 28.17% |
| Total | 14,239 74.97% |
4,755 25.03% |
18,994 100.00% |
| Race/Ethnicity | Wheelchair Type: Number (Percent) | ||
| Manual Wheelchair | Power Wheelchair | Totala | |
| White | 9,456 49.78% |
3,321 17.48% |
12,777 67.27% |
| Black | 2,798 14.73% |
995 5.24% |
3,793 19.97% |
| Hispanic | 1,406 7.40% |
291 1.53% |
1,697 8.93% |
| Other | 579 3.05% |
148 0.78% |
727 3.83% |
| Total | 14,239 74.97% |
4,755 25.03% |
18,994 100.00% |
NOTE: Information from 5 percent random sample (n = 18,994) of 2013–2014 Durable Medical Equipment (DME) Medicare beneficiaries aged 20–67.
a Percentages may not total because of rounding.
SOURCE: DME Research Identifiable File, Centers for Medicare & Medicaid Services.
section.) Seventy-five percent (14,239) of the wheelchairs in the DME sample were classified as manual and 25 percent (4,755) as powered.
Table 3-4 shows a breakdown of the use of manual versus powered wheelchairs among the 5 percent DME sample by age and race/ethnicity. In this sample of 18,994, approximately 36 percent of all WSMDs were used by persons aged 56-64. Powered wheelchairs were used by only 3.2 percent of the persons in the sample aged 20-45. Consistent with the demography of race and ethnicity in the United States, approximately 67 percent of WSMDs were used by non-Hispanic whites, 20 percent by blacks, and 9 percent by Hispanics. Powered wheelchairs were used substantially less
across all racial and ethnic groups. Only 1.5 percent of powered wheelchairs were used by Hispanics.
The number of WSMDs was higher for females (56.3 percent, n = 10,691) than for males (43.7 percent, n = 8,303). The use of powered wheelchairs also was higher for females (13.5 percent) than for males (11.5 percent) in the sample (data not shown).
The number of WSMDs varies by primary medical diagnoses (see Table 3-5). The primary diagnoses are classified based on the system CMS uses to aggregate primary diagnoses for the Basic Stand Alone DME Public Use Files. The Data Dictionary and Codebook for this system is available from CMS (2013). The committee used the diagnostic categories available in the DME public-use files because they allow comparison with information that is publicly available without the need for a data use agreement or completion of other Medicare privacy-related requirements.
Table 3-5 indicates that approximately 33 percent of all users of WSMDs included in the Medicare DME sample were in the diagnostic categories of diseases of the nervous system and diseases of the musculoskeletal system and connective tissue. The category diseases of the nervous system (ICD-9 codes 320-359) includes the following subcategories: inflammatory diseases of the central nervous system, hereditary and degenerative diseases of the central nervous system, pain, headache syndromes, disorders of the central nervous system, and disorders of the peripheral nervous system. The category diseases of the musculoskeletal system and connective tissue (ICD-9 codes 710-739) includes the following subcategories: arthropathies and related disorders, dorsopathies, rheumatism (excluding the back), osteopathies, chondropathies, and acquired musculoskeletal deformities. The first six primary diagnostic categories in Table 3-5 account for almost 79 percent of all users of WSMDs included in the Medicare DME sample.
CLINICAL CONSIDERATIONS
Factors Affecting Wheeled and Seated Mobility Device Selection
The types of WSMDs that are most appropriate for particular individuals and the extent of their use depend on a number of factors, including body function and activity and environmental and personal factors (Cooper et al., 2015; Dicianno et al., 2011; Paralyzed Veterans of American Consortium for Spinal Cord Medicine, 2005). Body function and activity factors include physical and cognitive abilities and secondary health conditions/comorbidities, and the types of devices used by individuals need to be adjusted to changes in these factors resulting from maturation (transitioning from adolescence to adulthood, as well as aging) and disease progression, which may be accompanied by deterioration of physical and cognitive
TABLE 3-5
Estimated Number of Wheeled and Seated Mobility Devices by CMS Diagnostic Categories
| Primary Diagnosisa | ICD-9 Codes | Number | Percent | Cumulative Number | Cumulative Percentb |
|---|---|---|---|---|---|
| Diseases of the nervous system | 320–359 | 3,181 | 16.7 | 3,181 | 16.7 |
| Diseases of the musculoskeletal system and connective tissue | 710–739 | 3,054 | 16.1 | 6,235 | 32.8 |
| Endocrine, nutritional and metabolic, and immunity disorders | 240–279 | 2,471 | 13.0 | 8,706 | 45.8 |
| Injury and poisoning | 800–999 | 2,145 | 11.3 | 10,851 | 57.1 |
| Diseases of the circulatory system | 390–459 | 2,130 | 11.2 | 12,981 | 68.3 |
| Diseases of the respiratory system | 460–519 | 1,962 | 10.3 | 14,943 | 78.7 |
| Symptoms, signs, and ill-defined conditions | 780–799 | 1,453 | 7.6 | 16,396 | 86.3 |
| External causes of injury and supplemental classification | E and V codes | 686 | 3.6 | 17,082 | 89.9 |
| Neoplasms | 140–239 | 446 | 2.3 | 17,528 | 92.3 |
| Diseases of the skin and subcutaneous tissue | 680–709 | 384 | 2.0 | 17,912 | 94.3 |
| Diseases of the genitourinary system | 580–629 | 364 | 1.9 | 18,276 | 96.2 |
| Congenital anomalies | 740–759 | 227 | 1.2 | 18,503 | 97.4 |
| Mental disorders | 290–319 | 220 | 1.2 | 18,723 | 98.6 |
| Infectious and parasitic diseases | 001–139 | 119 | 0.6 | 18,842 | 99.2 |
| Diseases of the digestive system | 520–579 | 93 | 0.5 | 18,935 | 99.7 |
| Diseases of the blood and blood-forming organs | 280–289 | 26 | 0.1 | 18,961 | 99.8 |
NOTES: Information from 5 percent random sample (n = 18,994) of 2013–2014 Durable Medical Equipment (DME) Medicare beneficiaries aged 20–67. ICD-9 = International Classification of Diseases, Ninth Revision.
a Data not shown for primary diagnostic categories with cell sizes ≤20.
b Percentages may not total because of rounding.
SOURCE: DME Research Identifiable File, Centers for Medicare & Medicaid Services.
function. Other body function and activity factors include specific work or personal activities. A wide range of environmental factors also impact the types and extent of use of WSMDs, including weather, topography (terrain), geography (rural or urban), political/economic factors (funding sources, availability, and costs/accessibility), social factors (attitudinal barriers), and home/school/work environments (accessibility, maneuverability). Personal factors that impact the choice and use of WSMDs may include personal preferences, cultural and spiritual issues, and cosmetic concerns. Lastly, because of the need for physical and/or occupational therapists to evaluate the fit and seating systems of WSMDs and train individuals in their proper use, users need to have the time and money to make use of these services.
Physical Environment
The physical environment encompasses topography, geography, and weather, all of which impact the types of WSMDs that are most appropriate for individuals and the potential need for multiple types of WSMDs for a particular person. Environments that are flat, have paved surfaces, and are free from snow are suitable for all WSMDs. In contrast, if the environment is hilly and/or snow-covered, the use of a manual device may be limited, such that a powered WSMD is needed; however, those who use primarily a manual wheelchair may be able to navigate these more challenging environments using a power assist device or tire adaptions without having to have more than one WSMD.
Functional Capacity
A WSMD needs to be suited to an individual’s physical and cognitive abilities (Cooper, et al., 2015; Dicianno et al., 2011; Paralyzed Veterans of American Consortium for Spinal Cord Medicine, 2000, 2005). The use of a manual wheelchair requires both adequate strength and endurance of the upper extremities and the absence of significant pain, spasticity, or contractures in the upper or lower extremities. Individuals who are at risk of pressure ulcers (such as those with spinal cord injury, spina bifida, or vascular compromise) must be capable of independently performing pressure relieves. Propelling a manual wheelchair requires at a minimum antigravity strength in the shoulders, elbow flexors, and wrist extensors. Individuals with full strength in all upper-extremity muscle groups relative to those with less upper-extremity muscle function are more likely to have relatively unlimited community mobility, including such higher-level wheelchair skills as negotiating curbs, inclines, and declines and independently performing even and uneven transfers. Individuals with full strength in all upper-extremity muscle groups relative to those with less upper-extremity
muscle function also are less likely to have overuse syndrome with premature aging and upper-extremity pain. In addition, these individuals are more capable of carrying items on their lap and accessing items in backpacks or other storage devices attached to their wheelchair. Those with less than full strength in their upper extremities, especially those with weak elbow extensors, may have limited ability to transfer independently without a sliding board and/or some assistance.
For individuals who are unable to use a manual wheelchair and who have no or limited ability to ambulate, a powered wheelchair or a manual wheelchair with power assist may be appropriate. Wheelchairs with power assist, either integrated into the wheel itself or as an add-on, are appropriate for individuals with upper-extremity function that allows them to hand propel the wheelchair to some extent. For those with less upper-extremity function, a powered wheelchair may be more appropriate. The appropriate control mechanism depends on the individual’s upper-extremity function and ranges from a joystick for those with adequate arm function (minimum of biceps function) to chin control, head array, or sip and puff for those with lesser arm function. For individuals with sensory loss or vascular compromise, a powered wheelchair should be equipped with power tilt-in-space and/or power recline to enable the performance of pressure relieves. Powered wheelchairs with power standing or elevating seat functions allow the user to access items, tabletops, and cabinets above the normal sitting height and to be at eye level with other individuals. A major limitation of powered wheelchairs is their size and weight, which requires the use of a van with a wheelchair lift when the user is traveling in a motor vehicle. In addition, because of the size, weight, and maneuverability of powered wheelchairs, the home and work environments must allow accessibility throughout, as well as have accessible entries/exits. When powered wheelchairs are malfunctioning, moreover, they are generally unusable, so that a back-up manual or powered wheelchair is needed.
A scooter may be appropriate for individuals who have some ambulatory ability but require a WSMD in their home, school, or work environment or in the community and are unable to use a manual wheelchair because of endurance limitations. To use a scooter, an individual must be able to sit independently and not be susceptible to pressure ulcers because of the limited seating options. Scooters may be equipped with a power elevating seat function that allows the user to access items, tabletops, and cabinets above the normal sitting height and to be at eye level with other individuals. Major limitations of scooters include their limited maneuverability and their weight, which requires that a motor vehicle used by an individual have a dedicated carrier.
There are several reasons why an individual may need more than one wheelchair and/or progress from one type of wheelchair to another. For
those who use a manual or powered wheelchair, a back-up wheelchair is needed in the event that their primary wheelchair is not usable. For those who use primarily a manual wheelchair, a power assist option (integrated into the wheels or as an add-on) may be required for longer-distance mobility. For example, an adolescent with a C6 spinal cord injury who uses a manual wheelchair may require power assist when he or she attends college or becomes employed and must negotiate greater distances on campus or to and from the workplace. Because of aging and overuse of their upper extremities, individuals who utilize primarily a manual wheelchair may need to add a power assist option to that wheelchair or progress to a powered wheelchair. Individuals with disorders characterized by progressive deterioration in their motor control, muscle strength, or endurance may need to progress sequentially from manual to power assist to powered wheelchairs, and those whose course is rapidly progressive may benefit from using a power assist or powered wheelchair earlier on.
All individuals who are at risk of pressure ulcers—for example, because of spinal cord injury, spina bifida, or vascular compromise—need to have pressure-reducing seating systems guided by pressure mapping and prescribed by a knowledgeable and experienced clinician (Paralyzed Veterans of America Consortium for Spinal Cord Medicine, 2014). These seating systems need to include a pressure-reducing cushion and, as appropriate, a pressure-reducing back. For individuals who are at risk of pressure ulcers and who are not capable of independently performing pressure relieves, a powered wheelchair equipped with power tilt-in-space and/or power recline is needed to accomplish pressure relieves. For individuals with inadequate trunk and/or neck support, seating systems need to provide adequate support for sitting, which may include side bolsters, head rests, contoured seat backs, or customized seating systems. Individuals who are at risk of pressure ulcers and who transfer to a standard chair need to utilize an appropriate pressure-reducing seating device whenever they are sitting in a standard chair. Individuals with pressure ulcers that are in contact with the surface of their WSMD, such as ischial or sacral ulcers, ideally should remain off of their pressure ulcers and hence should not be sitting.
A manual or powered wheelchair needs to be appropriate for the individual’s weight and body dimensions (Dicianno et al., 2011). Bariatric chairs are available for those weighing more than 300 pounds. The key dimensions of a wheelchair are the width, length, and dump of the seat and the position of the foot plate so that in the absence of significant contractures, the person is sitting with the hips, knees, and ankles in a neutral position. The dump of the seat needs to allow the individual to sit comfortably with adequate trunk support. Evaluations of the WSMD and seating system need to be conducted at least annually because of changing needs, as well as fluctuations in weight and dimensions due to pregnancy, weight gain, or
weight loss as a result of illness. In the event of a decline in cognition, the type of WSMD may need to be changed or additional safeguards instituted.
For individuals who utilize augmentative communication devices, these devices need to be mounted appropriately on the WSMD and readily accessible to the individual. A removable lap tray for the WSMD may be needed by those in powered wheelchairs that cannot fit easily under standard desks and tables.
Another clinical consideration is the existence of comorbid impairments. Major comorbid impairments (secondary health conditions) that affect and impact the functioning, including sustained work activity, of many individuals who require a WSMD are musculoskeletal issues, including pain, contractures, spasticity, osteoporosis, and fractures. These musculoskeletal issues may affect an individual’s ability to propel a manual or power assist wheelchair, control a powered wheelchair, and perform transfers, and they limit the amount of time that the person can remain in a seated position. In addition, spasticity may make sitting in a WSMD or standard chair unsafe if the person experiences severe muscle spasms.
Autonomic dysfunction, such as orthostatic hypotension or autonomic dysreflexia (e.g., spinal cord injury), may impact functioning, including sustained work activity. Individuals who are susceptible to orthostatic hypotension may benefit from a WSMD that reclines.
Individuals with pulmonary compromise, such as high tetraplegic spinal cord injuries, amyotrophic lateral sclerosis (ALS), or muscular dystrophy, may require ventilator support from a portable ventilator, which requires that the person’s WSMD, which generally is a powered wheelchair, can accommodate the ventilator. The presence of a neurogenic bladder and bowel, such as in individuals with spinal cord injuries, spina bifida, or multiple sclerosis, may impact functioning, including sustained work activity. Wheelchair-accessible restrooms must be available and conveniently located. For those who are not independent in performing their bladder and bowel program, an assistant is required. Individuals who use a WSMD and have concomitant cognitive or visual impairments or movement/coordination disorders need to have individualized evaluation of their ability to use their WSMD with respect to their own safety and that of others. These evaluations need to be performed periodically depending on the severity and specifics of the cognitive deficits and the potential for cognitive deterioration.
Factors Associated with Use of Wheeled and Seated Mobility Devices
Even when an individual is appropriately matched to a WSMD, there are multiple factors that affect activity and participation. In the physical environment, all residential settings need to be accessible for entry and
exit, including emergency contingencies. In addition, the interior rooms of residential settings—whether they are permanent or temporary, private homes/apartments or hotels/motels or nursing homes—must be accessible to WSMDs for both entry/exit and maneuverability; this requirement must be met for all sleeping, dining, and living rooms as well as for work areas, bathrooms, and kitchens. The surfaces of all pathways into and within the residential setting must be suitable for WSMDs and ideally should be flat and hard without thresholds. Interior features of the residential or work setting need to be compatible with WSMD use both for progression throughout the setting and for maneuvering. This requirement encompasses furniture as well as more permanent structures such as hallways, landings, bathrooms, and kitchens. For powered WSMDs, proper and accessible power outlets/charging stations are needed in appropriate locations.
In addition, transportation is necessary for individuals to participate fully in their community, including leisure/recreation activities, employment, social activities, health care services, and shopping. Full access to one’s community may range from the neighborhood level, to an entire community, to the world beyond. Forms of transportation that facilitate participation range from personal motor vehicles (such as cars, trucks, and vans) to mass transportation (such as buses, trains, boats, and airplanes). To utilize all of these modes of community transportation, users of a WSMD require accessible ingress/egress for the WSMD; sufficient space to navigate within the vehicle; and adequate safety restraints for the individual, which may include appropriate wheelchair tie-downs (van Roosmalen et al., 2002). Transportation of wheelchairs and/or wheelchair users to workplaces may require such additional assistive equipment as ramps, lifts, adapted vehicles, and other WSMDs. For individuals who transfer from their WSMD to a seat, appropriate seating must be available to avoid skin breakdown for those who are susceptible to this condition as a consequence of sensory loss or vascular compromise. The transportation also needs to be readily accessible in a timely and reliable fashion and to provide expedient passage comparable to that provided for those who do not require a WSMD.
As described elsewhere in this report, the ADA makes it unlawful to discriminate against a qualified individual with a disability in such employment practices as recruitment, pay, hiring, firing, promotion, job assignments, training, leave, and benefits. To be protected under the ADA, an individual must have a substantial impairment—one that significantly limits or restricts a major life activity, such as hearing, seeing, speaking, breathing, performing manual tasks, walking, caring for oneself, learning, or working.3 To be protected by the ADA, an individual with a disability also must be qualified to perform the “essential functions” of the job with
___________________
3 42 U.S. 12102 (1990).
or without reasonable accommodation.4 (See Chapter 7 for additional information regarding the ADA.)
Individuals using WSMDs may face additional challenges even when they are able to perform the formal essential functions associated with a position and have been provided an accommodation by the employer. For instance, they may need to be provided an appropriate and usable (e.g., snow being removed during the winter) ramp for entering the workplace building. In addition, employees must get from their home to the workplace, which may involve complex issues related to driving and/or other transportation. After arriving at the workplace parking lot or garage, employees using WSMDs must be able to use the parking garage elevator and/or navigate from the parking lot to the office building and negotiate the ramp. To do so, they may have to travel over uneven terrain, slopes, curbs, gravel, or unpaved areas. Once in the building, they may face additional barriers related to such tasks as reaching heights and managing doors and filing cabinets that require a level of coordination, balance, and dexterity that can be challenging and may not have been included among the essential functions associated with the actual job. Ensuring that these employees have easy access to the restroom facility is also a major workplace concern. These factors and job requirements must be considered both by individuals with a disability and by the members of their rehabilitation team (Boles et al., 2004; Goetzel et al., 2004).
EVALUATION AND MONITORING
Individuals who require a WSMD need to be evaluated periodically: in general, not less frequently than annually. A thorough evaluation focuses on the individual’s physical condition; the functioning and fitting of the WSMD and associated seating system; the individual’s current ability to utilize the WSMD (ergonomics and safety); the individual’s satisfaction with the WSMD; the individual’s underlying disorder and associated secondary health conditions/impairments; and assessment of past, current, and future functional needs at home, in the community, and in the workplace. With respect to the individual’s work environment, it is important to take a thorough inventory of the person’s functional needs; workspace layout, including accessibility of restrooms, break room, and meeting rooms; and access into and out of the workplace, including emergency exits and/or contingency plans suitable for an individual in a WSMD. Also important is assessment of the individual’s current and future transportation to and from the workplace, workplace-related activities, the home, and community venues, such as the need to travel to multiple work sites.
___________________
4 42 U.S. 12111 (1990).
During periodic evaluations, it may also be advisable to consider changing to a technology that might improve an individual’s functioning, reduce secondary health conditions, and increase satisfaction in the workplace. Such technology changes include not only those related to the WSMD but also other technologies that would enhance the person’s ability to perform his or her work duties or would reduce secondary heath conditions, such as overuse (e.g., carpal tunnel syndrome).
TRAINING AND ADAPTATION
If the user is to benefit from a WSMD, the device must be properly fitted to the body and accommodate the person’s environment, and the user must be properly trained in its use and maintenance. Providing inappropriate WSMDs can have unintended consequences, such as elevated risk for trips, falls, and collisions; pain due to excessive vibration exposure; injuries due to component failures; soft-tissue injuries, including pressure ulcers; and repetitive strain injuries, such carpal tunnel syndrome, elbow tendinitis, and rotator cuff injuries. A WSMD needs to serve as an extension of the user, becoming integrated into the person’s life and facilitating independence and community participation. To this end, it is essential that WSMDs be tuned for their users and that users receive training in using the features of their devices in the specific environments to be encountered. A personalized approach to this training and adaptation is important to the user’s experience and can prevent dissatisfaction with and abandonment of the device. According to Galvin and Scherer (1996), failure to consider the user’s opinions and preferences in device selection is the most significant factor associated with abandonment (see also the section on clinical considerations above). Poor feature matching, which can include wheelchair design, size, weight, and maneuverability, is a major factor contributing to the failure of wheelchairs to meet users’ functional needs and allow them to participate in community roles (Kittel et al., 2002). Although there is a dearth of literature on the adaptation time for WSMD use, it is important to note that the process can take place over a period of years (Barker et al., 2004; Bates et al., 1993). To be able to use a WSMD safely and effectively, each person needs training in a variety of skills.
Transfer Training
The user’s ability to safely enter and exit his or her WSMD is essential for health and community participation. Transfers can be independent, assisted by technology, assisted by a human, or assisted by a person using technology. The most appropriate means of transfer depends on the person being transferred, the environment (e.g., space available in which to align
the WSMD with the transfer surface), the type and features of the WSMD (e.g., size, presence of a seat elevator, leg rest type), and the surface to be transferred to/from (e.g., toilet, tub, shower bench, vehicle). Studies have shown that even people who are trained and can transfer independently typically are constrained to very limited ranges of horizontal and vertical separation between the two surfaces (Crytzer et al., 2017).
Transfers, along with wheelchair propulsion, weight relief, and overhead reaching, have been identified as key activities leading to the development of shoulder pain and injury. In a survey of individuals with spinal cord injury, 65 percent reported that pain interfered with their ability to transfer (Kankipati et al., 2015). Transfer skills also are important to a wheelchair user’s safety; of the falls reported to the Consumer Product Safety Commission between 1973 and 1987, 8.1 percent were related to transfers (Koontz et al., 2012). Performing sideways transfers without a sliding board is one factor associated with increased risk of accidents and falls (Toro et al., 2013).
When they first require a WSMD, many people participate in some form of rehabilitation that includes training in how to perform a safe and efficient transfer. Gaining independence with transfers often is a goal of both WSMD users and therapists because transfers are required to perform many essential functional activities. Even with the emphasis placed on transfers, however, the amount and type of training provided vary greatly, and there is no uniform way to evaluate transfer quality.
Clinicians can use the Transfer Assessment Instrument (TAI) to evaluate transfer quality and a patient’s adherence to transfer training (McClure et al., 2011). The TAI assesses conservation of upper-limb function, safety, and the ability of WSMD users to direct an assistant to help them with a transfer as necessary. Items on the TAI are based on clinical practice guidelines, available transfer literature, and techniques applied in clinical training (Paralyzed Veterans of America Constorium for Spinal Cord Medicine, 2005). The TAI can be used to evaluate independent transfers, modified independent transfers (with the use of assistive devices), human-assisted transfers, and dependent transfers (using only human assistance or human assistance and technology).
Wheelchair Skills Training
To use a wheelchair safely and effectively requires mobility training. Operating a wheelchair requires the integration of multiple senses and coordinated control of multiple actions. For manual wheelchairs, strength, flexibility, and motor coordination are necessary to perform common mobility and functional ADLs. Users of powered wheelchairs must be able to operate the controls safely and judge the device’s capabilities given their
environment and skill set. While nearly all wheelchair users receive some training, this training usually is insufficient.
Kirby and colleagues (2004) have developed and extensively studied the Wheelchair Skills Training Program, which involves teaching a wide variety of skills in a clinical (inpatient or outpatient) or community-based setting. Demonstrated to be safe, practical, and effective, this program incorporates common motor-learning principles into a rehabilitation setting and can improve wheelchair skills in about 2 hours.
Some instruments have been developed for use in assessing wheelchair skills. The Functional Mobility Assessment is a self-report outcomes tool designed to measure the effectiveness of WSMD interventions for people with disabilities. Test-retest reliability scores for all items and participants were found to be above the acceptable value for a clinical assessment tool (Kumar et al., 2013). The Functioning Everyday with a Wheelchair questionnaire is designed to measure perceived user function related to wheelchair and scooter use (Mills et al., 2007).
A few clinical tools are available to aid clinicians in evaluating people for power mobility. However, these tools simply record whether drivers can complete certain tasks; they cannot detect the specific motor, sensory, or cognitive impairments that are related to safe and effective driving—information needed to determine not only whether individuals are capable of ultimately learning to drive but also the type and amount of training they may need. Routhier and colleagues (2003) assert the need for a controlled-environment outcome measure using a standardized obstacle course for measuring driving skills, a need not met by existing instruments for evaluating powered wheelchair driving. The Power Mobility Indoor Driving Assessment (PIDA) and the Power-Mobility Community Driving Assessment were developed not as screening tools but as a means of identifying general areas in which more training is needed (e.g., parking under a table) or in which modifications to the powered wheelchair or environment are necessary (Letts et al., 2007). Scoring is subjective such that the evaluator rates how independently a driver can perform a given task, such as approaching a closet. However, only the PIDA evaluates indoor driving. Kirby and colleagues published a Wheelchair Skills Test (MacPhee et al., 2004). And Massengale and colleagues (2005) developed the Power Mobility Road Test, which incorporates portions of the PIDA and other wheelchair driving courses used in research settings. A driver is rated on 12 structured tasks entailing basic driving and 5 unstructured tasks involving moving obstacles. These tests are useful clinically to test proficiency at performing common wheelchair skills; they do not help identify specific motor, sensory, or cognitive impairments that may be contributing to unsafe driving. The latter information is crucial in planning the type and amount of training needed for an individual to become a skilled driver. To address these gaps,
Dicianno and colleagues developed the Power Mobility Screening Tool and the Power Mobility Clinical Driving Assessment Tool, which build on the foundation of the assessment and training used for adaptive motor vehicle assessments (Kamaraj et al., 2016).
Wheelchair Maintenance Training
Wheelchair breakdowns are one cause of users being injured or stranded, and the incidence of these breakdowns is increasing. Evidence suggests that wheelchair users who routinely maintain their devices are less likely to be injured. In one study, 62 percent (n = 616) of U.S. wheelchair users with spinal cord injury reported needing ≥1 repairs within a 6-month period; 27.4 percent experienced an adverse consequence as a result of the needed repair; 7.1 percent did not complete the repair; and most repairs were completed by a vendor for powered wheelchairs and by users themselves for manual wheelchairs (Worobey, 2016). The importance of routine maintenance is increased by poor wheelchair reliability. Many wheelchairs in the United States fail to meet minimum performance and durability standards (Fitzgerald et al., 1999). While higher-cost wheelchairs tend to do better in standards testing, they still fail early. A recent meta-analysis confirms these findings and provides further evidence that manufacturers are not producing wheelchairs that comply with standards, making attention to maintenance that much more important (Wang et al., 2010).
Several resources provide information on how to maintain wheelchairs. First, as required by American National Standards Institute (ANSI)/ Rehabilitation Engineering and Assistive Technology Society of North America (RESNA) Wheelchair Standards Section 15 (ANSI/RESNA, 2009), wheelchair manufacturers are required to include maintenance instructions in the user manual provided with the device. Second, maintenance checklists are available online (Cooper, 2013; Denison, 2006), including some at Spinlife,5 a popular online wheelchair retailer (Koontz, n.d.). Rehabilitation engineering books also dedicate sections to wheelchair maintenance (Cooper, 1998; Cooper et al., 2006). In fact, the book Wheelchair Selection and Configuration was translated into Turkish, Romanian, and Bulgarian and used to train wheelchair users in group settings in wheelchair maintenance (Cooper, 1998; Soydan et al., 2012). The course, however, was not openly available online. Third, professional organizations’ wheelchair provision and prescription guides recommend discussing maintenance as a vital component of wheelchair provision and include brief maintenance checklists for clinician (Arledge et al., 2011; Lukersmith et al., 2013).
___________________
5 See http://www.spinlife.com/en/caringformanualwheelchairs2.cfm (accessed July 18, 2017).
In addition, the World Health Organization (WHO) has launched the Wheelchair Service Training Package, which includes a section on wheelchair maintenance training (Khasnabis and Mines, 2012). This package is designed to train wheelchair service providers, such as clinicians, in six basic wheelchair maintenance and repair skills, although it covers only manual wheelchairs. The training curriculum includes PowerPoint slides, a video of a live demonstration, and an in-person demonstration. It explains why each maintenance task should be done, how often, and how. Finally, the Wheelchair Maintenance Training Program was created as a project of the Spinal Cord Injury Model System to help address the need for wheelchair maintenance training (Worobey et al., 2016).
In addition, the WHO has released Guidelines on the Provision of Manual Wheelchairs in Less Resourced Settings, which are aimed at enhancing the quality of life of wheelchair users. The guidelines in the service delivery section focus on “good practice at all stages of the service delivery process, from referral to assessment and prescription, funding, ordering, product preparation, fitting, user training and maintenance” (WHO, 2008, p. 10). According to a study by Toro and colleagues (2016), following the WHO’s guidelines has a range of positive outcomes, including increased satisfaction with the device and better quality of life.
Although these resources are available, routine wheelchair maintenance is not commonly performed by either wheelchair users or caregivers. In a study assessing wheelchair durability and its effect on user satisfaction, 26 percent of wheelchair users reported completing wheelchair repairs and 16 percent general maintenance in the past 6 months (Fitzgerald et al., 2005). And a study that assessed hospital wheelchairs showed that only 23 percent were safe and in good working condition (Young et al., 1985). Preventive maintenance services are uncommon, and users have reported seeking professional intervention only when the needed repairs have reached crisis levels (Nosek and Krouskop, 1995).
Seating and Positioning
The WSMD seating surface, including cushions and back support, is critical for comfort, safety, and prevention of such complications as pressure ulcers. Yet, while devices are available for clinical assessment of pressure distribution, as are cushions effective in distributing pressure, there remains a tremendous problem with wheelchair users incurring pressure ulcers. People who are active sitters (change their seated posture frequently) and/or perform regular pressure relief (lifting the buttocks off of the seat or dramatically changing posture by, for example, lying on the thighs) tend to be at lower risk of developing pressure ulcers. Educational tools (e.g., user guides, oral instruction, websites, apps) have proven
effective in increasing knowledge of the risk of pressure ulcers among wheelchair users, but they do little to improve compliance (Schofield et al., 2013). Reminders based on timers or simple pressure or contact switches have proven only modestly effective (Griffin et al., 2007). Research has shown promise for the Virtual Seating Coach from Permobil, Inc. in increasing compliance among users of powered wheelchairs who use power seat functions (Liu et al., 2010, 2012).
Training in performing pressure relief or dynamic repositioning is usually provided in a clinic with oral instructions, perhaps with feedback from a pressure mapping system, with minimal practice because of time limitations (Griffin et al., 2007). Given the need for new users to learn how to operate and maintain their device and to propel it safely, the challenges of learning to manage seated pressure can be overwhelming, and training often requires frequent reinforcement. And, given the numerous activities and tasks in which users must engage every day, it is easy to lose track of time and forget to perform pressure reliefs even for those who are aware of the importance of preventing pressure ulcers.
ACCESS AND AVAILABILITY
Availability of Wheeled and Seated Mobility Devices
WSMDs are made available through a complex network that involves a chain of professional providers, funding sources, and manufacturers. The Manual of Wheelchair Market Shares, Strategies, and Forecasts, Worldwide, 2012 to 2018, published in 2012, provides a comprehensive review of the multiple factors driving the demand for and availability of WSMDs (WinterGreen Research, 2012).
Two key factors influencing the availability of these devices are the level of the person’s functional limitations and his or her access to reimbursement. Discrepancies among various reimbursement and funding sources for WSMDs in the United States impact the availability of various types of these devices, as well as accessories and opportunities for training and education offered to both providers and users (Crane and Minkel, 2009). As discussed previously, for example, CMS classifies WSMDs as DME, defined under CMS rules as equipment that (1) can withstand repeated use, (2) is used to serve a medical purpose, (3) is not useful to a person in the absence of an illness or injury, and (4) is appropriate for use in the home. All of these requirements must be met to qualify for Medicare reimbursement. Thus, current Medicare policy determines the need for a manual or powered wheelchair based on the individual’s need for the device inside the home. This policy is an impediment to achieving gainful employment. It also shows that a mismatch exists between the types of WSMDs covered
by Medicare and those required to maximize individuals’ functioning based on their diagnosis and treatment.
In addition to affecting the availability of WSMDs at the level of the individual user, current Medicare policy impacts the production and distribution of these devices by manufacturers. Medicare is the largest funding source for WSMDs in the United States. Therefore, a significant portion of sales of these devices depends on Medicare beneficiaries (Crane and Minkel, 2009), and the production of WSMDs in the United States and the types produced are directly influenced by the Medicare reimbursement system (WinterGreen Research, 2012). The net effect is to make it less likely that the devices produced will facilitate productive work outside of the home.
In contrast to the CMS DME program, the VA has a consumer-friendly program, particularly for veterans who are of working age. A veteran who meets the enrollment criteria for VA benefits is assigned to one of eight numbered, priority groups. Qualified veterans are eligible to receive WSMDs to allow them to participate in tasks of daily living in the home, community, and work environments. Qualified individuals who use a manual wheelchair for primary mobility are eligible for a custom-configured ultra-lightweight model with options and accessories when appropriately justified, and individuals who use powered wheelchairs are provided with a back-up manual device. The differences in payment policies for WSMDs between the CMS DME program and the VA program (Hubbard et al., 2007) also have a significant impact on the availability of these devices in the United States. (Models of reimbursement for assistive technology [AT], including WSMDs, are described in detail in Chapter 7.)
Issues associated with access, availability, and service delivery are important modifiers of consumer outcomes. Factors within the service delivery process, such as wait times for appointments and assessments and the range of devices and accessories available, vary across providers and programs. Groah and colleagues (2014) found that standards of care for the provision of high-quality powered wheelchairs for individuals with spinal cord injury were not being met across payer sources, except at the VA. However, no payer source, including the VA, fully met standards of care for manual wheelchairs. The VA did outperform other payers on a variety of metrics. One study of 471 veterans with traumatic amputations found that use of two or more types of WSMD together improved rehabilitation outcomes and function (Laferrier et al., 2010). Another study of 723 individuals with spinal cord injury showed that those who received their wheelchair through the VA, compared with other payers, had fewer breakdown and repair issues (Worobey et al., 2012). However, this study also showed that the incidence and adverse consequences of repairs appeared to be increasing in the United States.
Clinician Expertise in Provision of Wheeled Mobility Devices
Whether an individual receives an appropriate or effective WSMD and experiences subsequent beneficial outcomes depends on a variety of other proximal variables, including factors related to the client, provider, payer, supplier, and health care system (Eggers et al., 2009). Since the development of the assistive technology professional (ATP) certification (described below), attention has been focused on such provider factors as training and credentialing, but little research has examined the relationship between credentialing and WSMD service delivery outcomes, despite evidence suggesting that expertise and training may be important modifiers of these outcomes (Hausmann et al., 2015).
The level of clinical experience related to seating assessment, training, and follow-up evaluation depends on the severity of the user’s functional limitations (physical and cognitive), the complexity of the technology, and the user’s physical and social environments. When the complexity of these factors is low, rehabilitation professionals, including occupational and physical therapists, with the appropriate clinical experience are qualified to conduct assessments and provide basic WSMD training and follow-up evaluation. As the severity of the users’ functional limitations becomes more profound and the complexity of the technology and the environment increases, the need for specialized training and coordinated team-based skills increases as well.
An example of the complexity associated with WSMDs is seen in standard ISO 7176-26, Wheelchairs—Part 26 (ISO, 2007). The standard classifies wheelchairs by their method of propulsion (manual or powered) and further by tilt and recline and the ability of the user (or assistant) to adjust the tilt or recline (ISO, 2007). Separate classification systems exist for seating. The Edinburgh classification of wheelchair seating equipment, for example, includes three levels of complexity (low, medium, and high) in which are nested eight levels of seating systems (Dolan and Henderson, 2013). The seating systems range in complexity from sling seat and sling back with or without a seating cushion (low), to foam carved, interlocking components or molded solid seat and/or solid back support shaped to match the user with or without additional postural support devices (high). The more complex WSMDs and seating systems require a level of specialized knowledge and skill beyond that of the typical rehabilitation professional. This level of expertise is available only in specialty rehabilitation hospitals and centers, particularly those with expertise in treating spinal cord injuries and cerebral palsy. Ensuring that complex WSMDs are properly configured and their users are adequately trained requires a coordinated interprofessional team approach to service delivery. The availability of experienced and knowledgeable clinicians is discussed below. It
involves the availability of academic training programs and the collaboration of rehabilitation centers and facilities with a clinical training mission to help ensure that customized WSMDs are properly configured and users are adequately trained in their use.
Access to Trained Clinicians
Most of the credentialing bodies for the professionals referred to above include education in WSMDs in their professional requirements. While the number of hours varies, the depth of training specifically related to these devices provides only fundamental knowledge, and postprofessional continuing education combined with professional experience is required to achieve a high level of proficiency. Among health care professionals who practice primarily within the field of AT, it is generally agreed that a team approach involving a therapist, an engineer, a physician, an AT supplier, and the client is optimal. The participation of other health care professionals and family members can further enhance the team.
The U.S. Bureau of Labor Statistics reports that there are more than 200,000 physical therapists and 110,000 occupational therapists in the United States (BLS, 2016a,b), while there are fewer than 10,000 certified orthotists and/or prosthetists and approximately 8,874 physicians board-certified in physical medicine and rehabilitation (PM&R).6 Physical therapy and physiatry require a doctoral degree before an individual qualifies for their board examination; occupational therapy currently requires a master’s degree but is transitioning toward a doctoral degree; and programs in orthotics and prosthetics require a master’s degree.
Degree-granting educational programs, however, represent only the beginning of the learning process necessary to maintain occupational and professional excellence in a rapidly expanding field such as rehabilitation AT. RESNA, an international, interdisciplinary organization with a commitment to technology for persons with a disability (RESNA, 2016b), provides professional development and training with approved continuing education credits, leading to certification as an ATP or seating and mobility specialist (SMS). Educational courses include Fundamentals in Assistive Technology and Advanced Seating Workshop, offered in conjunction with regular webinars related to AT. RESNA also is the home for Assistive Technology, the society’s official journal and a major source of scientific innovation for researchers, developers, clinicians, educators, and consumers involved in advancing AT.
___________________
6 As of January 4, 2017, this was the number of board-certified PM&R diplomates in the United States aged 65 or younger.
The ATP certification recognizes competence in analyzing the needs of WSMD users, helping with the selection of appropriate AT, and providing training in the use of the selected devices (RESNA, 2016c). The SMS certification is a specialty certification for professionals working in seating and mobility (RESNA, 2016c). Both certifications require an exam. The ATP exam is broad based, covering all major areas of AT while the SMS exam is focused specifically on seating, positioning, and mobility (RESNA, 2016c). To take the exam for ATP certification, candidates must meet both educational and work experience requirements (RESNA, 2016a). The education and training levels for individuals with ATP and SMS certifications differ greatly, resulting in a high degree of variability in the quality of services provided. Certified prothetists and orthotists have a scope of practice similar to that of those with ATP/SMS certification, but with formal education and training that includes obtaining a degree from an accredited program. The ATP/SMS certification could benefit from a similar model, perhaps achieving a higher standard of practice. Of course, higher standards could reduce access temporarily; in the long run, however, they could improve quality of service and access through recognition of the profession.
Another important resource for expanding professional knowledge and skill development in AT and WSMDs is the National Coalition for Assistive and Rehab Technology (NCART), a national association of suppliers and manufacturers of complex rehabilitation technology products and services that are used by individuals with significant disabilities and medical conditions (NCART, 2016). NCART’s mission is to ensure that federal, state, and private coverage and reimbursement policies allow individuals with significant disabilities to have appropriate access to specialized and individually configured products and services (NCART, 2016). WSMDs account for many of the complex rehabilitation technology products and services supported by NCART advocacy.
An important professional development and educational resource directly relevant to WSMDs is the International Seating Symposium, held biannually in the United States. This symposium is one of the premier meetings in the world dedicated to clinicians, researchers, manufacturers, and others who work to improve seating and mobility among people with disabilities (ISS, 2016). The symposium includes scientific and clinical papers, in-depth workshops, special topic sessions, poster sessions, and an extensive exhibit hall. Program objectives are to identify seating and mobility interventions for people with physical disabilities, discuss service delivery practices, explore current research, and understand the features and clinical impact of seating mobility technologies (ISS, 2016). Instructional courses are provided, with associated continuing education credits.
A major source for prompting and supporting research, continuing education, professional development, and the advancement of AT science
and evidence-based wheeled and mobility practice is the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR). NIDILRR is a federal agency in the Administration on Community Living in the U.S. Department of Health and Human Services that provides leadership and grant support for a comprehensive program of scholarly activity related to the rehabilitation of individuals with disabilities. NIDILRR’s extramural research is conducted through a network of research projects and centers located throughout the country. Among its largest funding programs are Rehabilitation Engineering Research Centers (RERCs), Disability Rehabilitation Research Program grants, and the Model Systems Centers of Excellence program. The Model Systems Centers of Excellence are focused on various diagnostic groups. The Model Systems Centers of Excellence in Spinal Cord Injury are particularly important resources for advanced training in state-of-the-art technology development, clinical practice, and research related to WSMDs.
Most insurance providers, including Medicare, require a physician’s prescription for a WSMD, for a therapist’s assessment for the specification of a device for long-term use due to a permanent disability, and for training in its safe and effective use. Medicare and other insurers may also require that the wheelchair be provided by a supplier or a manufacturer representative who is credentialed by RESNA as an ATP. The results of a cohort study examining patterns of ownership and use of mobility aids among working-age individuals with multiple sclerosis showed variation in access to reimbursement for WSMDs as well as in training in use of the devices (Iezzoni et al., 2010). Among users of powered wheelchairs, only 37 percent were reimbursed by insurance for any part of the cost, and only 41 percent received training in the device’s use (Iezzoni et al., 2010); almost 69 percent of this training was provided by the vendor and not a rehabilitation professional. Among manual wheelchair users, only 23 percent were reimbursed by insurance for any part of the cost (Iezzoni et al., 2010); 18 percent of users received training, 44 percent of them from the vendor and 44 percent from the rehabilitation provider (Iezzoni et al., 2010). Among scooter users, only 17 percent were reimbursed by insurance for any part of the cost (Iezzoni et al., 2010); only 24 percent received training in use of the device, primarily from the vendor (82 percent) and not a rehabilitation provider (Iezzoni et al., 2010). These variations have a significant impact on the types of WSMDs individuals receive, as do geographic variations in the availability of experienced and knowledgeable clinicians.
The distribution of ATP and SMS certified practitioners across the United States is depicted in Figure 3-15. As this figure illustrates, a disparity exists in the availability of practitioners holding both ATP and SMS certifications, with most being clustered around major urban areas and large medical
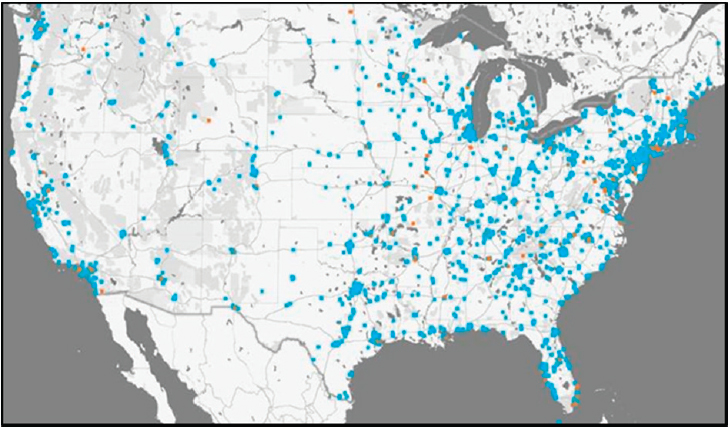
NOTES:
 = ATP certified
= ATP certified  = SMS certified.
= SMS certified.*Data provided by the Rehabilitation Engineering and Assistive Technology Society of North America. Data mapped by the University of Pittsburgh, School of Health and Rehabilitation Sciences, Department of Rehabilitation Science and Technology. This figure was created with the assistance of Mark Schmeler and Vince Schiappa at the University of Pittsburgh. Dr. Schmeler was one of the committee’s guest speakers.
centers. RESNA maintains a directory of certified practitioners (RESNA, 2016a), showing that currently 3,871 practitioners hold an ATP certification and 167 hold an SMS certification; a practitioner can hold both certifications. The majority of practitioners who are ATP certified identify seating, positioning, and mobility as a practice area. The number of ATP and SMS certified practitioners is small considering the need for their services.
Access to Clinics That Provide Wheelchairs
As noted above, the provision of a wheelchair generally involves a physician who writes a prescription, a therapist who conducts an assessment and generates a recommendation, and a supplier or a manufacturer representative. Some clinics employ a team approach to wheelchair provision and are capable of meeting the complex needs of individuals with severe disabilities. Unfortunately, there is no registry of such clinics, but there are ways to identify at least some of them. There are currently 24 VA Spinal
Cord Injuries and Disorders Centers located throughout the United States that provide comprehensive care to qualified veterans with spinal cord injuries, multiple sclerosis, and ALS. To decrease disparities and improve standards of care for WSMD service delivery, the VA established the Polytrauma Rehabilitation Assistive Technology (PRAT) Lab. The PRAT Lab currently provides consultation and resources to 27 VA facilities in 18 states.7 This network began with the five Polytrauma Rehabilitation Centers and has expanded to Polytrauma Network Sites, Polytrauma Support Clinical Teams, and other VA Centers interested in or currently implementing AT interventions and services. The PRAT Lab standardized the WSMD service delivery process across sites by using published, evidence-based guidelines for conducting assessments, and they developed a checklist to assist therapists in implementing these guidelines (Ambrosio et al., 2007). The VA has created clinical rehabilitation engineering positions requiring a relevant degree and the ATP credential. This model helps meet the need for formalized education and credentialing of rehabilitation engineers and AT providers.
For individuals who are not veterans, access to clinics that provide WSMDs generally is very limited. The 14 NIDILRR Model Systems Centers of Excellence in Spinal Cord Injury provide comprehensive care to individuals with spinal cord injuries, including the provision of complex wheelchairs and seating systems. This program also has contributed to several survey components on wheelchair mobility, including wheelchair service delivery models, what causes disparities, and whether providers’ prescriptions are appropriate. In addition, the Commission on Accreditation of Rehabilitation Facilities (CARF), an independent, nonprofit organization focused on advancing the quality of rehabilitation services, states on its website that there are 51 accredited AT clinics located throughout the United States. This list on the CARF website is not comprehensive as there are clinics that provide wheelchairs to a high standard but are not within the family of CARF-accredited facilities.
FINDINGS AND CONCLUSIONS
Findings
Access to Wheeled and Seated Mobility Devices
3-1. Persons in the neurological diagnostic group (e.g., spinal cord injury, multiple sclerosis) tend to use lightweight high-strength wheelchairs,
___________________
7 California, Colorado, Florida, Illinois, Iowa, Massachusetts, Michigan, Minnesota, Nebraska, New Mexico, New York, North Carolina, Ohio, Pennsylvania, Texas, Utah, Virginia, and Washington.
whereas those in the obesity diagnostic group use primarily heavy- and extra-heavy-duty wheelchairs.
3-2. Well-fitted, good-quality seating helps prevent secondary health conditions such as pressure sores and overuse injuries in people using wheelchairs.
3-3. Customizable powered wheelchairs have been shown to improve functioning.
3-4. The type of wheeled and seated mobility device (WSMD) that is most appropriate for an individual depends on a number of factors, including body functions and activity, as well as environmental and personal factors.
3-5. The variable dependability and availability of WSMDs impact individuals’ functioning and activity and their ability to be employed.
3-6. Access to WSMDs varies significantly across reimbursement and funding sources in the United States.
3-7. A mismatch exists between the types of WSMDs covered by Medicare and those required to maximize individuals’ functioning based on their diagnosis and treatment.
Access to Highly Qualified Providers
3-8. Even though wheelchairs are ubiquitous, they do not replace all of the complex functions of the lower extremities; in addition, proper fitting and training are complex but necessary elements of maximizing users’ performance, work potential, and health maintenance.
3-9. In the United States, multiple agencies and service providers are responsible for determining the need for WSMDs, providing the products and technologies, delivering the training, monitoring use of the products and technologies, and assessing outcomes.
3-10. The distribution of providers and clinics with the knowledge, skills, and expertise to properly evaluate, prescribe, and train people in the use of WSMDs varies greatly throughout the United States.
3-11. Providers of WSMDs vary in their level of knowledge, skills, and expertise.
Availability of Data
3-12. Data on the prevalence of use of WSMDs are fragmented and limited.
3-13. Factors affecting the ability to work for individuals using WSMDs include the ability to get ready for work, transportation to work, and access to the workplace.
3-14. There are limited data showing the relationship between individual users’ medical conditions and health (e.g., comorbidities) and/or
sociodemographic characteristics and the specific types of WSMDs they use.
3-15. The current fragmented approach to the delivery of WSMDs means that no single public-use data source includes information on the prevalence of these devices with a focus on persons of working age (ages 20-67).
Conclusions
Access to Wheeled and Seated Mobility Devices
3-1. The variation in reimbursement and funding sources and access to qualified professionals in the United States has a significant impact on the types of WSMDs individuals receive. [Findings 3-6, 3-7]
3-2. Medicare’s policy limiting coverage of WSMDs to those needed for home use is an impediment to achieving gainful employment. [Findings 3-5, 3-7]
3-3. Medicare policy affects manufacturers’ production and distribution of WSMDs. [Finding 3-7]
Access to Highly Qualified Providers
3-4. More qualified providers and clinics with the knowledge, skills, and expertise to properly evaluate, prescribe, and train people in the use of WSMDs are needed. [Findings 3-8, 3-10, 3-11]
3-5. A higher level of certification/training than the current assistive technology professional credential could improve the qualifications of providers in terms of the knowledge, skill, and expertise necessary to properly evaluate, prescribe, and train people in the use of WSMDs. The degree requirement from an accredited program and certification process for prosthetists and orthotists could serve as a good model for WSMD suppliers and technicians. [Finding 3-8]
Availability of Data
3-6. Information showing the relationship between individual users’ medical conditions and health and/or sociodemographic characteristics and the specific types of WSMDs they use would be useful for payers, providers, and consumers to support future planning for treatment programs, the production of technologies, the training of providers, and the allocation of resources for these assistive devices. [Finding 3-14]
3-7. Although wheelchairs are ubiquitous, advances in these devices have been stifled by reimbursement policies and a lack of professional training and research investment. These barriers have limited realization of the full potential of wheelchairs, such as the introduction of new materials and the integration of robotics technology for navigation, safety, and obstacle negotiation. These types of features could further expand the population of people with independent wheeled mobility, increase safety, and prolong independent mobility as people age. [Finding 3-7]
3-8. The U.S. Census Bureau’s Survey of Income and Program Participation is the best population-based source of information on the overall use of WSMDs in the United States. [Finding 3-12]
REFERENCES
Ambrosio, F., M. L. Boninger, S. G. Fitzgerald, S. L. Hubbard, S. R. Schwid, and R. A. Cooper. 2007. Comparison of mobility device delivery within Department of Veterans Affairs for individuals with multiple sclerosis versus spinal cord injury. Journal of Rehabilitation Research & Development 44(5):693-701.
ANSI/RESNA (American National Standards Institute/Rehabilitation Engineering and Assistive Technology Society of North America). 2009. RESNA American National Standard for Wheelchairs—Volume 1: Requirements and test methods for wheelchairs (including scooters). In Section 15: Requirements for information disclosure, documentation and labeling. Arlington, VA: RESNA.
Arledge, S., W. Armstrong, M. Babinec, B. E. Dicianno, C. Digiovine, T. Dyson-Hudson, J. Pederson, J. Piriano, T. Plummer, L. Rosen, M. Schmeler, M. Shea, and J. Stogner. 2011. RESNA wheelchair service provision guide. Arlington, VA: RESNA. http://www.resna.org/sites/default/files/legacy/resources/position-papers/RESNAWheelchairServiceProvisionGuide.pdf (accessed January 21, 2017).
Arva, J., M. R. Schmeler, M. L. Lange, D. D. Lipka, and L. E. Rosen. 2009. RESNA position on the application of seat-elevating devices for wheelchair users. Assistive Technology 21(2):69-72.
Barker, D. J., D. Reid, and C. Cott. 2004. Acceptance and meanings of wheelchair use in senior stroke survivors. American Journal of Occupational Therapy 58(2):221-230.
Bates, P. S., J. C. Spencer, M. E. Young, and D. H. Rintala. 1993. Assistive technology and the newly disabled adult: Adaptation to wheelchair use. American Journal of Occupational Therapy 47(11):1014-1021.
BLS (U.S. Bureau of Labor Statistics). 2016a. Occupational outlook handbook 2016-17 edition: Occupational therapists. https://www.bls.gov/ooh/healthcare/occupational-therapists.htm (accessed December 22, 2016).
BLS. 2016b. Occupational outlook handbook 2016-17 edition: Physical therapists. https://www.bls.gov/ooh/healthcare/physical-therapists.htm (accessed December 22, 2016).
Boles, M., B. Pelletier, and W. Lynch. 2004. The relationships between health risks and work productivity. Journal of Occupational and Environmental Medicine 46(7):737-745.
CDC (U.S. Centers for Disease Control and Prevention). 2016. National Health Interview Survey 2015 data release. https://www.cdc.gov/nchs/nhis/nhis_2015_data_release.htm (accessed July 30, 2016).
Chaves, E. S., M. L. Boninger, R. Cooper, S. G. Fitzgerald, D. B. Gray, and R. A. Cooper. 2004. Assessing the influence of wheelchair technology on perception of participation in spinal cord injury. Archives of Physical Medicine and Rehabilitation 85(11):1854-1858.
CMS (Centers for Medicare & Medicaid Services). 2009. Medicare coverage of power mobility devices (PMDs): Power wheelchairs and power operated vehicles (POVs). https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/PMDFactSheet07_Quark19.pdf (accessed January 25, 2017).
CMS. 2013. Basic stand alone DME public use files. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/BSAPUFS/BSA_DME_Line_Items_PUF.html (accessed August 1, 2016).
CMS. 2015a. CMS research statistics data and systems/statistics trends and reports. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMS-Statistics-Reference-Booklet/2015.html (accessed November 8, 2016).
CMS. 2015b. Power mobility devices: Complying with documentation and coverage requirements. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/pmd_DocCvg_FactSheet_ICN905063.pdf (accessed September 7, 2016).
Cooper, R. A. 1998. Wheelchair selection and configuration. New York: Demos.
Cooper, R. A. 2001. Advances in wheelchair and related technologies. Medical Engineering & Physics 23(4):iii-iv.
Cooper, R. A. 2013. The basics of manual wheelchair maintenance. PN Online, September 12.
Cooper, R. A., M. L. Boninger, and A. Rentschler. 1999. Evaluation of selected ultralight manual wheelchairs using ANSI/RESNA standards. Archives of Physical Medicine and Rehabilitation 80(4):462-467.
Cooper, R. A., H. Ohnabe, and D. A. Hobson. 2006. An introduction to rehabilitation engineering. Boca Raton, FL: CRC Press.
Cooper, R., R. A. Cooper, M. L. T. Hernandez, T. M. Crytzer, T. Bobish, R. Mankowski, J. Mankowski, J. Coltellaro, B. McCormick, E. C. Ferretti, M. A. F. de Mello, and N. Upadhyay. 2015. Assistive technology: An international approach to the comprehensive management (Chapter 38). In ISCoS textbook on comprehensive management of spinal cord injuries, edited by H. S. Chhabra. New Delhi, India: Wolters Kluwer. Pp. 594-612.
Crane, B., and J. Minkel. 2009. Legislation and funding. In Industry profile on wheeled mobility, edited by S. Bauer and M. E. Buning. Buffalo, NY: University at Buffalo. Pp. 50-78.
Crytzer, T. M., R. Cooper, G. Jerome, and A. Koontz. 2017. Identifying research needs for wheelchair transfers in the built environment. Disability and Rehabilitation: Assistive Technology 12(2):121-127.
Davies, A., L. H. De Souza, and A. O. Frank. 2003. Changes in the quality of life in severely disabled people following provision of powered indoor/outdoor chairs. Disability and Rehabilitation 25(6):286-290.
Denison, I. 2006. Wheelchair maintenance series. http://www.assistive-technology.ca/studies/wm_full.pdf (accessed August 29, 2013).
Dicianno, B. E., M. Schmeler, and B. Y. Liu. 2011. Wheelchairs/adaptive mobility equipment and seating. In Spinal cord medicine, edited by S. Kirshblum and D. I. Campagnolo. Philadelphia, PA: Lippincott Williams & Wilkins. Pp. 341-358.
DiGiovine, M. M., R. A. Cooper, M. L. Boninger, B. M. Lawrence, D. P. VanSickle, and A. J. Rentschler. 2000. User assessment of manual wheelchair ride comfort and ergonomics. Archives of Physical Medicine and Rehabilitation 81(4):490-494.
Dolan, M. J., and G. I. Henderson. 2013. Patient and equipment profile for wheelchair seating clinic provision. Disability and Rehabilitation: Assistive Technology 9(2):136-143.
Edwards, K., and A. McCluskey. 2010. A survey of adult power wheelchair and scooter users. Disability and Rehabilitation: Assistive Technology 5(6):411-419.
Eggers, S. L., L. Myaskovsky, K. H. Burkitt, M. Tolerico, G. E. Switzer, M. J. Fine, and M. L. Boninger. 2009. A preliminary model of wheelchair service delivery. Archives of Physical Medicine and Rehabilitation 90(6):1030-1038.
Fass, M. V., R. A. Cooper, S. G. Fitzgerald, M. Schmeler, M. L. Boninger, S. D. Algood, W. A. Ammer, A. J. Rentschler, and J. Duncan. 2004. Durability, value, and reliability of selected electric powered wheelchairs. Archives of Physical Medicine and Rehabilitation 85(5):805-814.
Fitzgerald, S., R. A. Cooper, A. Rentschler, and M. Boninger. 1999. Comparison of fatigue life for three types of manual wheelchairs. Proceedings of the First Joint BMES/EMBS Conference 601(1):606.
Fitzgerald, S. G., R. A. Cooper, M. L. Boninger, and A. J. Rentschler. 2001. Comparison of fatigue life for 3 types of manual wheelchairs. Archives of Physical Medicine and Rehabilitation 82(10):1484-1488.
Fitzgerald, S., D. Collins, R. Cooper, M. Tolerico, A. Kelleher, P. Hunt, S. Martin, B. Impink, and R. Cooper. 2005. Issues in the maintenance and repairs of wheelchairs: A pilot study. Journal of Rehabilitation Research & Development 42(6):853-862.
Flagg, J. L. 2009. Wheeled mobility demographics. In Industry profile on wheeled mobility, edited by S. Bauer and M. E. Buning. Buffalo, NY: University at Buffalo. Pp. 7-29.
Galvin, J. C., and M. J. Scherer. 1996. Evaluating, selecting, and using appropriate assistive technology. Gaithersburg, MD: Aspen Publishers Inc.
Goetzel, R. Z., S. R. Long, R. J. Ozminkowski, K. Hawkins, S. Wang, and W. Lynch. 2004. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. Journal of Occupational and Environmental Medicine 46(4):398-412.
Griffin, B., H. Cooper, C. Horack, M. Klyber, and D. Schimmelpfenning. 2007. Best-practice protocols: Reducing harm from pressure ulcers. Nursing Management 38(9):29-32.
Groah, S. L., I. Ljungberg, A. Lichy, M. Oyster, and M. L. Boninger. 2014. Disparities in wheelchair procurement by payer among people with spinal cord injury. PM&R 6(5):412-417.
Hausmann, L. R., L. Myaskovsky, C. Niyonkuru, M. L. Oyster, G. E. Switzer, K. H. Burkitt, M. J. Fine, S. Gao, and M. L. Boninger. 2015. Examining implicit bias of physicians who care for individuals with spinal cord injury: A pilot study and future directions. The Journal of Spinal Cord Medicine 38(1):102-110.
Hubbard, S. L., S. G. Fitzgerald, B. Vogel, D. M. Reker, R. A. Cooper, and M. L. Boninger. 2007. Distribution and cost of wheelchairs and scooters provided by Veterans Health Administration. Journal of Rehabilitation Research & Development 44(4):581-592.
Iezzoni, L., S. R. Rao, and R. P. Kinkel. 2009. Patterns of mobility aid use among working-age persons with multiple sclerosis living in the community in the United States. Disability and Health Journal 2(2):67-76.
Iezzoni, L. I., S. R. Rao, and R. P. Kinkel. 2010. Experiences acquiring and using mobility aids among working-age persons with multiple sclerosis living in communities in the United States. American Journal of Physical Medicine and Rehabilitation 89(12):1010-1023.
ISO (International Organization for Standardization). 2007. ISO 7176-26:2007 Wheelchairs—part 26: Vocabulary. http://www.iso.org/iso/home/store/catalogue_tc/catalogue_detail.htm?csnumber=44224 (accessed August 31, 2016).
ISS (International Seating Symposium). 2016. About the 2017 ISS. http://www.iss.pitt.edu/ISS2017/ISS2017about.html (accessed July 29, 2016).
Kamaraj, D. C., B. E. Dicianno, H. P. Mahajan, A. M. Buhari, and R. A. Cooper. 2016. Interrater reliability of the power mobility road test in the virtual reality-based simulator-2. Archives of Physical Medicine and Rehabilitation 97(7):1078-1084.
Kankipati, P., M. L. Boninger, D. Gagnon, R. A. Cooper, and A. M. Koontz. 2015. Upper limb joint kinetics of three sitting pivot wheelchair transfer techniques in individuals with spinal cord injury. The Journal of Spinal Cord Medicine 38(4):485-497.
Khasnabis, C., and K. Mines. 2012. Wheelchair service training package basic level. Geneva, Switzerland: WHO.
Kirby, R. L., N. J. Mifflen, D. L. Thibault, C. Smith, K. L. Best, K. J. Thompson, and D. A. MacLeod. 2004. The manual wheelchair-handling skills of caregivers and the effect of training. Archives of Physical Medicine and Rehabilitation 85(12):2011-2019.
Kittel, A., A. D. Marco, and H. Stewart. 2002. Factors influencing the decision to abandon manual wheelchairs for three individuals with a spinal cord injury. Disability and Rehabilitation 24(1-3):106-114.
Koontz, A. M. n.d. Manual wheelchair maintenance. http://www.spinlife.com/spintips/details/k/Manual%20Wheelchair%20Maintenance/a/116/c/2 (accessed August 28, 2013).
Koontz, A. M., M. Toro, P. Kankipati, M. Naber, and R. Cooper. 2012. An expert review of the scientific literature on independent wheelchair transfers. Disability and Rehabilitation: Assistive Technology 7(1):20-29.
Kumar, A., M. R. Schmeler, A. M. Karmarkar, D. M. Collins, R. Cooper, R. A. Cooper, H. Shin, and M. B. Holm. 2013. Test-retest reliability of the functional mobility assessment (FMA): A pilot study. Disability and Rehabilitation: Assistive Technology 8(3):213-219.
Laferrier, J. Z., L. V. McFarland, M. L. Boninger, R. A. Cooper, and G. E. Reiber. 2010. Wheeled mobility: Factors influencing mobility and assistive technology in veterans and servicemembers with major traumatic limb loss from Vietnam War and OIF/OEF conflicts. Journal of Rehabilitation Research & Development 47(4):349-360.
Letts, L., D. Dawson, I. Bretholz, E. Kaiserman-Goldenstein, J. Gleason, E. McLellan, L. Norton, and C. Roth. 2007. Reliability and validity of the power-mobility community driving assessment. Assistive Technology 19(3):154-163.
Liu, H.-Y., R. Cooper, R. Cooper, A. Smailagic, D. Siewiorek, D. Ding, and F.-C. Chuang. 2010. Seating virtual coach: A smart reminder for power seat function usage. Technology and Disability 22(1, 2):53-60.
Liu, H.-Y., G. Grindle, A. Kelleher, R. Cooper, R. Cooper, F. C. Chuang, D. Siewiorek, and A. Smailagic. 2012. A survey of feedback modalities for wheelchair power seat functions. IEEE Pervasive Computing 11(3):54-62.
Lukersmith, S., L. Radbron, and K. Hopman. 2013. Development of clinical guidelines for the prescription of a seated wheelchair or mobility scooter for people with traumatic brain injury or spinal cord injury. Australian Occupational Therapy Journal 60(6):378-386.
MacPhee, A. H., R. L. Kirby, A. L. Coolen, C. Smith, D. A. MacLeod, and D. J. Dupuis. 2004. Wheelchair skills training program: A randomized clinical trial of wheelchair users undergoing initial rehabilitation. Archives of Physical Medicine and Rehabilitation 85(1):41-50.
Massengale, S., D. Folden, P. McConnell, L. Stratton, and V. Whitehead. 2005. Effect of visual perception, visual function, cognition, and personality on power wheelchair use in adults. Assistive Technology 17(2):108-121.
McClure, L. A., M. L. Boninger, H. Ozawa, and A. Koontz. 2011. Reliability and validity analysis of the transfer assessment instrument. Archives of Physical Medicine and Rehabilitation 92(3):499-508.
Mills, T. L., M. B. Holm, and M. Schmeler. 2007. Test-retest reliability and cross validation of the functioning everyday with a wheelchair instrument. Assistive Technology 19(2):61-77.
Mortenson, W. B., and J. Kim. 2016. Scoping review of mobility scooter-related research studies. Journal of Rehabilitation Research & Development 53(5):531-540.
NCART (National Coalition for Assistive and Rehabilitation Technology). 2016. National Coalition for Assistive and Rehab Technology: Protecting and promoting access to complex rehab technology. http://www.ncart.us (accessed July 30, 2016).
Nosek, M. A., and T. A. Krouskop. 1995. Demonstrating a model approach to independent living center-based assistive technology services. Assistive Technology 7(1):48-54.
Paralyzed Veterans of America Consortium for Spinal Cord Medicine. 2000. Outcomes following traumatic spinal cord injury: Clinical practice guidelines for health-care professionals. The Journal of Spinal Cord Medicine 23(4):289-316.
Paralyzed Veterans of America Consortium for Spinal Cord Medicine. 2005. Preservation of upper limb function following spinal cord injury: A clinical practice guideline for healthcare professionals. Washington, DC: Consortium for Spinal Cord Medicine.
Paralyzed Veterans of America Consortium for Spinal Cord Medicine. 2014. Pressure ulcer prevention and treatment following spinal cord injury: A clinical practice guideline for health-care providers. Washington, DC: Consortium for Spinal Cord Medicine.
RESNA (Rehabilitation Engineering and Assistive Technology Society of North America). 2016a. ATP statistics. http://www.resna.org/get-certified/atp-statistics (accessed September 1, 2016).
RESNA. 2016b. About. http://www.resna.org/about (accessed August 1, 2016).
RESNA. 2016c. Certification. http://www.resna.org/certification (accessed February 3, 2017).
Routhier, F., C. Vincent, J. Desrosiers, and S. Nadeau. 2003. Mobility of wheelchair users: A proposed performance assessment framework. Disability and Rehabilitation 25(1):19-34.
Salminen, A. L., A. Brandt, K. Samuelsson, O. Töytäri, and A. Malmivaara. 2009. Mobility devices to promote activity and participation: A systematic review. Journal of Rehabilitation Medicine 41(9):697-706.
Scherer, M. J. 2002. Assistive technology: Matching device and consumer for successful rehabilitation. Washington, DC: American Psychological Association.
Schofield, R., A. Porter-Armstrong, and M. Stinson. 2013. Reviewing the literature on the effectiveness of pressure relieving movements. Nursing Research and Practice 2013.
Smith, E. M., E. M. Giesbrecht, W. B. Mortenson, and W. C. Miller. 2016. Prevalence of wheelchair and scooter use among community-dwelling Canadians. Physical Therapy 96(8):1135-1142.
Soydan, Y., S. Koksal, and O. Ciobanu. 2012. Training of wheelchair users for maintenance. Paper presented at 4th International Congress of Educational Research, Istanbul, May 4-7.
Sui Generis Seat. 2015. Sui Generis Seat. http://suigenerisseat.com (accessed April 6, 2017).
Toro, M. L., A. M. Koontz, and R. A. Cooper. 2013. The impact of transfer setup on the performance of independent wheelchair transfers. Human Factors 55(3):567-580.
Toro, M. L., C. Eke, and J. Pearlman. 2016. The impact of the World Health Organization 8-steps in wheelchair service provision in wheelchair users in a less resourced setting: A cohort study in Indonesia. BMC Health Services Research 16(1):26.
Trefler, E. M., S. G. P. Fitzgerald, D. A. P. Hobson, T. M. S. Bursick, and R. M. S. Joseph. 2004. Outcomes of wheelchair systems intervention with residents of long-term care facilities. Assistive Technology 16(1):18-27.
U.S. Census Bureau. 2016. Survey of income and program participation: 2008 panel wave 06. https://www.census.gov/programs-surveys/sipp/data/2008-panel/wave-6.html (accessed August 12, 2016).
van Roosmalen, L., G. E. Bertocci, D. A. Hobson, and P. Karg. 2002. Preliminary evaluation of wheelchair occupant restraint system usage in motor vehicles. Journal of Rehabilitation Research & Development 39(1):83-93.
Wang, H., H.-Y. Liu, J. Pearlman, R. Cooper, A. Jefferds, S. Connor, and R. A. Cooper. 2010. Relationship between wheelchair durability and wheelchair type and years of test. Disability and Rehabilitation: Assistive Technology 5(5):318-322.
WinterGreen Research. 2012. Manual wheelchair market shares, strategies, and forecasts, worldwide, 2012 to 2018. http://www.marketresearchstore.com/report/manual-wheel-chair-market-shares-strategies-and-forecasts-worldwide-2394 (accessed August 11, 2016).
WHO (World Health Organization). 2008. Guidelines on the provision of manual wheelchairs in less resourced settings. http://apps.who.int/iris/bitstream/10665/43960/1/9789241547482_eng.pdf (accessed February 24, 2017).
Worobey, L. 2016. Wheelchair breakdown: What is failing and what to do about it—Implications for users and clinicians and a potential intervention. http://asia-mmg.societyhq.com/2016annual/guide/protected/syllabus/lectures/2016-PA-1461334033-3953.pdf (accessed February 1, 2017).
Worobey, L., M. Oyster, G. Nemunaitis, R. Cooper, and M. L. Boninger. 2012. Increases in wheelchair breakdowns, repairs, and adverse consequences for people with traumatic spinal cord injury. American Journal of Physical Medicine & Rehabilitation/Association of Academic Physiatrists 91(6):463.
Worobey, L., J. Pearlman, T. Dyson-Hudson, and M. Boninger. 2016. Clinician competency with wheelchair maintenance and the efficacy of a wheelchair maintenance training program. Archives of Physical Medicine and Rehabilitation 97(10):e55.
Young, J. B., P. W. Belfield, B. H. Mascie-Taylor, and G. P. Mulley. 1985. The neglected hospital wheelchair. British Medical Journal 291(6506):1388-1389.
CHAPTER 3 ANNEX TABLES
ANNEX TABLE 3-1
Taxonomy of Wheeled and Seated Mobility Devicesa
| Device | Cost Range | Population | Intended Use | Requirements for Use | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Manual Wheelchairs | |||||||||||
| Standard (K0001), Hemi (K0002), and Lightweight (K0003) | $300– $600 |
Primarily elderly | Limited use for short time periods; may be used by individuals who can stand and walk to some degree | Upper- extremity function intact; good endurance in chair | |||||||
| High-Strength Lightweight (K0004) | $900– $2,000 |
Primarily for transport of individuals who have physical impairment and obesity | May be used by individuals who can stand and walk to some degree; users spend at least 2 hours/day in the wheelchair | Upper-extremity function intact; able to self-propel the wheelchair | |||||||
| Ultra- lightweight (K0005), Custom Manual (K0008), and Other (K0009) | $1,800– $4,000 |
Almost all ages (e.g., 18 months to 100 years) | Used as primary or sole mode of mobility | Able to self-propel the wheelchair; motivation | |||||||
| Heavy-Duty (K0006) and Extra-Heavy Duty (K0007) | $500– $2,000 |
Primarily for transport of individuals who have physical impairment and obesity | For individuals who weigh more than 250 pounds (K0006) or more than 350 pounds (K0007) | Weight more than 250 or 350 pounds | |||||||
| Need for Training and Adaption | Benefits of Device | Limitations of Device | Life Span of Device (Years) | Maintenance | Other Considerations |
|---|---|---|---|---|---|
| Minimal | Inexpensive and readily available | Heavy; difficult to propel; limited customiz-ability | 1–3 years | Minimal | For temporary use or transport of people within a health care facility |
| Minimal | Heavy; difficult to propel; difficult to transport | 1–3 years | Minimal | Limited seating options, do not accommodate specialized seating needs | |
| Moderate training for advanced wheelchair skills | Offers customized fit and configurability; easier to lift; easier to propel, essential for those with limited endurance or strength, such as patients with tetraplegia | Expense and difficulty of getting approval for funding | 3–5 years | Moderate; requires experienced technicians | Must be prescribed by a licensed/certified medical professional |
| Minimal | Can be used by people with weight above 250 or 350 pounds | Heavy; difficult to propel | 3–5 years | Moderate because of weight of user | Often better served with a powered wheelchair |
| Device | Cost Range | Population | Intended Use | Requirements for Use | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Powered Wheelchairs | |||||||||||
| Scooter/Power Operated Vehicle | $1,000– $6,000 |
Primarily elderly or people with early onset of progressive conditions (e.g., multiple sclerosis) | Supplemental form of mobility for those who can stand and ambulate to some degree | Cognitive ability to operate; arm and hand function intact | |||||||
| Group 1 Powered Wheelchair | $3,000– $8,000 |
Primarily elderly, temporary use, or back-up | Primarily indoor use | Cognitive ability to operate; arm and some hand function intact; ability to perform independent weight shift and transfers | |||||||
| Group 2 Powered Wheelchair | $3,000–$20,000 | Long-term use for individuals who can still independently weight shift or transfer | Cognitive ability to operate; arm and some hand function intact | ||||||||
| Group 3 Powered Wheelchair | $8,000– $35,000 |
Long-term wheelchair users without effective ability to propel a manual wheelchair, perform an independent weight shift, or propel in the community | Long-term use for individuals who cannot independently weight shift or transfer | Cognitive ability to operate; arm and some hand function intact or ability to use hands-free interface | |||||||
| Group 4 Powered Wheelchair | $10,000– $40,000 |
Active indoor/outdoor long-term wheelchair users without effective ability to propel a manual wheelchair, perform an independent weight shift, or propel in the community | Long-term use for individuals who cannot independently weight shift or transfer; better designed for use outside of the home; ideal for active users | Cognitive ability to operate; arm and some hand function intact or ability to use hands-free interface | |||||||
a Wheeled and seated mobility devices are medical devices with wheels that are intended to provide mobility to persons with restricted or no ability to ambulate without assistance from technology.
| Need for Training and Adaption | Benefits of Device | Limitations of Device | Life Span of Device (Years) | Maintenance | Other Considerations |
|---|---|---|---|---|---|
| Minimal | Intuitive to use | Poor seating for support and pressure reduction; instability and tipping; large turning radius | 1–5 years | Moderate; requires regular tire and battery maintenance | Requires additional equipment to transfer; difficult to use in-home, or when made for in-home presents safety risk in community |
| Minimal | Relative ease of use; lightweight compared with other powered wheelchairs; can be portable | Short range of only 3–5 miles; few advanced features, such as tilt or recline | 1–3 years | Frequent tire, battery, and hardware maintenance | Not durable for regular users of a powered wheelchair |
| Moderate; need for an experienced licensed/certified medical professional | Limited seat functions and customi-zability | Not as durable as Group 3; limited seat functions and customizability | 3–5 years | Minimal to moderate | |
| Moderate; need for an experienced licensed/certified medical professional | Intermediate range and speed | Designed for use in the home | 3–5 years | Requires skilled technicians | |
| Moderate; need for an experienced licensed/certified medical professional | Longest range and highest speed; most customizable and greatest number of options; greatest durability | Expense | 3–5 years | Requires skilled technicians | Limited funding available |
ANNEX TABLE 3-2
Functionality of Wheeled and Seated Mobility Devices
| Device |
Standing:
|
Balancing - Seated or Standing:
|
Climbing:
|
Balancing - Seating and Positioning:
|
Mobility Indoors:
|
|---|---|---|---|---|---|
| Manual wheelchairs | |||||
| Standard (K0001), Hemi (K0002), and Lightweight (K0003) | 1 | 1 | 1, 2, 3 | 1 | 1 |
| High- Strength Lightweight (K0004) |
1 | 1 | 1, 2, 3 | 1 | 1 |
| Ultra- lightweight (K0005), Custom Manual (K0008), and Other (K0009) |
1 | 2 | 1, 2, 3, 4 | 1, 2 | 1, 2, 3, 4, 5 |
Mobility Outdoors:
|
Reaching:
|
Carrying:
|
Dexterous Movements:
|
Lifting:
|
Communication:
|
|---|---|---|---|---|---|
| 1 | 2 | 1 | 1 | 1 | 1 |
| 1 | 2 | 2 | 1 | 1 | 1 |
| 1, 2 | 2 | 2 | 1 | 1 | 1 |
| Device |
Standing:
|
Balancing - Seated or Standing:
|
Climbing:
|
Balancing - Seating and Positioning:
|
Mobility Indoors:
|
|---|---|---|---|---|---|
| Heavy-Duty (K0006) and Extra- Heavy-Duty (K0007) |
1 | 1 | 1, 2, 3 | 1 | 1 |
| Powered Wheelchairs | |||||
| Scooter/Power Operated Vehicle | 1, 3 | 1 | 1, 2, 3 | 1 | 1, 2, 3 |
| Group 1 Powered Wheelchair | 1 | 1 | 1, 2, 3 | 1 | 1, 2, 3, 4, 5 |
| Group 2 Powered Wheelchair | 1, 3 | 2 | 1, 2, 3 | 3 | 1, 2, 3, 4, 5 |
| Group 3 Powered Wheelchair | 1, 3 | 2, 3 | 1, 2, 3 | 3 | 1, 2, 3, 4, 5 |
| Group 4 Powered Wheelchair | 1, 3, 5 | 2, 3, 4 | 1, 2, 3, 4, 5, 6 | 3 | 1, 2, 3, 4, 5 |
Mobility Outdoors:
|
Reaching:
|
Carrying:
|
Dexterous Movements:
|
Lifting:
|
Communication:
|
|---|---|---|---|---|---|
| 1 | 2 | 1 | 1 | 1 | 1 |
| 1, 2 | 2 | 2 | 1 | 1 | 2 |
| 1 | 2 | 3 | 2 | 1 | 2 |
| 1, 2 | 2, 3 | 3 | 2 | 2 | 2 |
| 1, 2 | 2, 3 | 3 | 2 | 2 | 3 |
| 1, 2, 3 | 1, 2, 3, 4 | 3 | 2 | 3 | 3 |
This page intentionally left blank.
































































