Proceedings of a Workshop
INTRODUCTION1
Though cancer was once considered to be a problem primarily in wealthy nations, low- and middle-income countries now bear a majority share of the global cancer burden, and cancer often surpasses the burden of infectious diseases in these countries. Effective low-cost cancer control options are available for some malignancies, with the World Health Organization (WHO) estimating that these interventions could facilitate the prevention of approximately one-third of cancer deaths worldwide (WHO, 2015a). Effective cancer treatment approaches are also available and can reduce the morbidity and mortality due to cancer in low-resource areas. But these interventions remain inaccessible for many people in the world, especially those residing in low-resource communities that are characterized by a lack of funds—on an individual or a societal basis—to cover health infrastructure and care costs. As a result, worse outcomes for patients with cancer are more common in
___________________
1 The planning committee’s role was limited to planning the workshop. The Proceedings of a Workshop was prepared by the rapporteurs as a factual account of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine. They should not be construed as reflecting any group consensus.
low- and middle-income countries compared with high-income countries. Disparities in cancer outcomes can also be found in high-income countries—communities within wealthier nations can experience worse cancer outcomes, especially if they have challenges in accessing cancer prevention and cancer care services.
Few guidelines and strategies for cancer control consider the appropriateness and feasibility of interventions in low-resource settings, which may undermine the effectiveness of care. For example, interventions that are designed for high-resource settings may not account for important considerations in low-resource settings, such as infrastructure and workforce requirements or a community’s capacity to deliver cancer care after a diagnosis. Patients in resource-constrained communities face delayed diagnoses of cancer, potentially resulting in progression to later stage cancers and worsened patient outcomes. In addition, social stigma, geopolitical issues, and cultural norms may limit access to adequate cancer care, including cancer prevention, early detection, and diagnosis; surgery, radiation, and drug-based cancer treatments; palliative care;2 and survivorship care. There are wide disparities in the availability and quality of all types of cancer care around the world and within countries.
Recognizing the challenges of providing cancer care in resource constrained settings, the National Cancer Policy Forum of the National Academies of Sciences, Engineering, and Medicine developed a two-workshop series examining cancer care in low-resource communities, building on prior work of the Institute of Medicine (IOM, 2007, 2013). Both workshops were held at the National Academies in Washington, DC. The first workshop, held on October 26 and 27, 2015, focused on cancer prevention and early detection.3
The second workshop was held on November 14 and 15, 2016, and focused on cancer treatment, palliative care, and survivorship care in low-resource areas. The following is a summary of this workshop, which featured invited presentations and panel discussions on topics that included
___________________
2 Palliative care is defined as “specialized medical care for people living with serious illness. It focuses on providing relief from the symptoms and stress of a serious illness. The goal is to improve quality of life for both the patient and the family. Palliative care is provided by a team of [health care professionals] . . . to provide an extra layer of support. It is appropriate at any age and at any stage in a serious illness and can be provided along with curative treatment” (CAPC, 2017).
3 See https://www.nap.edu/catalog/21892 (accessed February 1, 2017).
- Global cancer trends, including disparities in access to cancer care in low-resource settings, as well as the unequal global burden of cancer;
- Challenges in providing cancer care in low-resource areas, including infrastructure and workforce capacity constraints, limited financial resources, cultural differences, and education and training needs;
- Strategies to overcome cancer disparities, including resource prioritization, partnerships to deliver cancer care in low-resource areas, new technologies designed for use in low-resource settings, stratified cancer care guidelines, innovative cancer care delivery models, and improved access to clinical trials;
- Lessons learned from current efforts to improve cancer care in low-resource areas; and
- Funding for cancer care and policy opportunities to drive progress in improving cancer care in low- and middle-income countries as well as in low-resource areas in the United States.
A broad range of views and ideas were presented, and a summary of suggestions from individual participants about potential actions to improve cancer care in low-resource areas is provided in Box 1. The workshop Statement of Task is located in Appendix A and the workshop agenda is in Appendix B. The webcast and speakers’ presentations are archived online.4
CANCER INCIDENCE AND MORTALITY TRENDS
In the first workshop on cancer care in low-resource areas, a number of speakers discussed trends in cancer incidence and mortality in low-resource areas, both in the United States and internationally (see NASEM, 2016, for a more detailed discussion). For example, Greta Massetti, associate director for science in the Division of Cancer Prevention and Control at the Centers for Disease Control and Prevention (CDC), noted that 80 percent of cancers in low-income countries are found at a stage where cures are impossible (International Prevention Research Institute, 2013). Felicia Knaul, director of the Miami Institute for the Americas at the University of Miami, added that variation in cancer mortality is linked to national wealth, and that people with can-
___________________
4 See http://www.nationalacademies.org/hmd/Activities/Disease/NCPF/2016-NOV-14.aspx (accessed January 27, 2017).
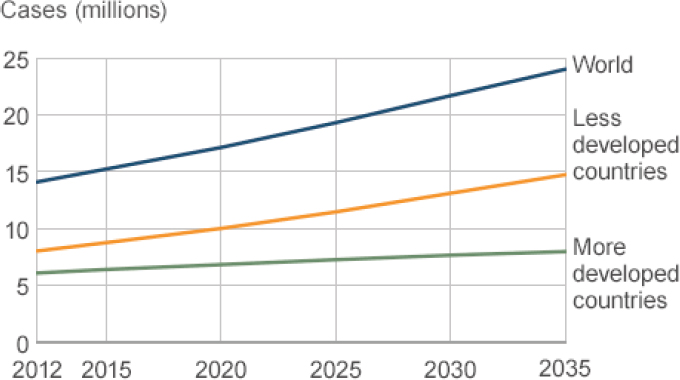
NOTE: Population forecasts were extracted from the United Nations’ World Population Prospects, the 2012 Revision. Numbers were computed using age-specific rates and corresponding populations for 10 age groups.
SOURCES: Jaffray presentation, November 14, 2016; Produced with permission from Ferlay J., Soerjomataram I., Ervik M., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray, F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr (accessed on April 12, 2017).
cer who live in higher-income countries are often less likely to die from their cancer, compared to people who live in lower-income countries (Enserink, 2011).
A number of speakers at this workshop also discussed trends in cancer in low-resource areas. Michael Barton, professor of radiation oncology at the University of New South Wales in Australia, noted that global data demonstrate that the burden of cancer is increasing worldwide and that there are major geographic disparities in cancer incidence and survival (Ferlay et al., 2013). In 2012, there were an estimated 14 million new diagnoses of cancer worldwide, but in 2035, there will be 24 million new diagnoses of cancer (Ferlay et al., 2013). The increase in cancer incidence will be steepest among low- and middle-income
countries, he said (see Figure 1).5 In addition, by 2030, the number of deaths due to cancer in sub-Saharan Africa is predicted to increase at a substantially greater rate than in the United States or in Europe (WHO, 2013), said Olufunmilayo Olopade, professor of medicine and human genetics at The University of Chicago Medicine.
More than 175,000 children worldwide are diagnosed with cancer annually, resulting in about 90,000 deaths each year (Magrath, 2013; UICC, 2011), said Sara Day, assistant dean of the College of Nursing at the University of Tennessee Health Science Center. Day added that advances in cancer treatment, health care infrastructure, professional training, and up-to-date resources in high-income countries have contributed to large improvements in pediatric cancer overall survival rates (e.g., children with cancer in the United States have overall survival rates of greater than 80 percent) (Siegel et al., 2013). However, the majority of childhood cancer diagnoses occur in low- and middle-income countries, where late diagnosis and limited access to appropriate cancer care has resulted in pediatric cancer overall survival rates of 20 percent or less (Barr et al., 2006; Howard et al., 2007), Day reported.
Olopade noted the significant state-to-state variability in breast cancer mortality among African Americans (State Cancer Profiles, 2017) (see Figure 2). “So when we talk about low resource, we are not just talking about out there [internationally], we are talking about in many parts of this country,” Olopade said. Augusto Ochoa, director of the Stanley S. Scott Cancer Center at Louisiana State University (LSU), added: “I am an immigrant to this country who came here from the third world, but the third world of the United States is right here, if you are talking about cancer.” Robert Carlson, chief executive officer of the National Comprehensive Cancer Network (NCCN), agreed, noting that “within a high-resource setting, such as the United States, you can have low-resource or mid-resource environments or systems, and that is a really important message.”
Lucile Adams-Campbell, associate director for Minority Health and Health Disparities Research at Georgetown University Lombardi Cancer Center, said cancer incidence among U.S. minorities is estimated to increase by 99 percent between 2010 and 2030, compared with only 33
___________________
5 At the first workshop, a number of speakers discussed factors contributing to the increases and disparities in cancer incidence and mortality (see NASEM, 2016).
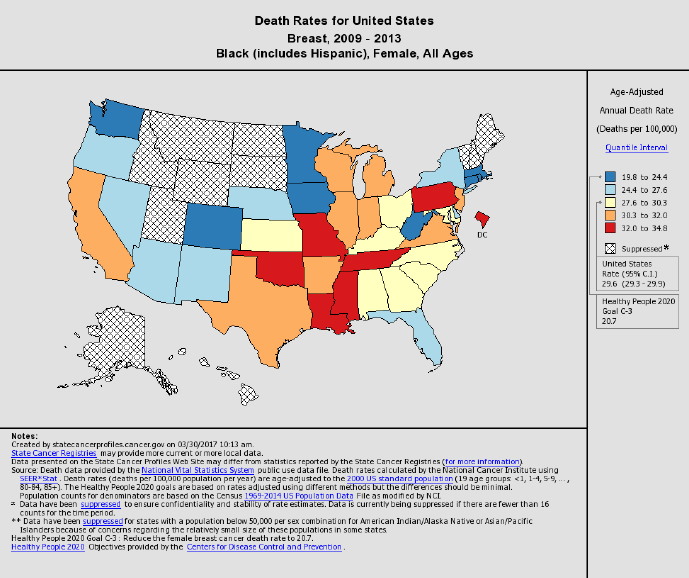
SOURCES: Olopade presentation, November 14, 2016; State Cancer Profiles, 2017.
percent for nonminorities; this difference is due to demographic changes in the population, including the increase in numbers of older adults and minorities in the United States (Smith et al., 2009). There are also disparities in cancer outcomes by race and ethnicity in the United States (ACS, 2017). Stephen Grubbs, vice president of clinical affairs at the American Society of Clinical Oncology (ASCO), noted that disparities in colorectal cancer mortality rates among African Americans and whites have persisted for all stages of the disease (local, regional, and advanced) (Robbins et al., 2012) (see Figure 3).
There are also differences in the prevalence of certain cancers in low-resource and high-resource settings, reported Benjamin Anderson, chair and director of the Breast Health Global Initiative at the Seattle Cancer Care Alliance, and Kathleen Schmeler, associate professor in the Department of Gynecologic Oncology and Reproductive Medicine at
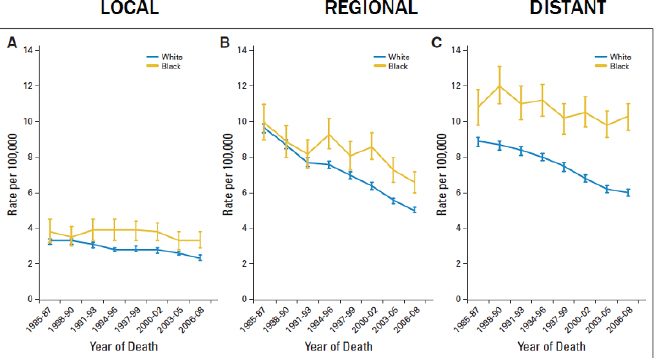
SOURCES: Grubbs presentation, November 14, 2016; Robbins, A. S., R. L. Siegel, and A. Jemal. 2012. Racial disparities in stage-specific colorectal cancer mortality rates from 1985 to 2008. Journal of Clinical Oncology 30(4):401-405. Reprinted with permission. © (2012) American Society of Clinical Oncology. All rights reserved.
The University of Texas MD Anderson Cancer Center. In high-income countries, breast, lung, colorectal, and prostate cancers comprise more than 50 percent of diagnosed cancers (Bray et al., 2012). Middle-income countries—such as those in Latin America—have high rates of esophageal, stomach, and liver cancers (Bray et al., 2012). In addition, 85 percent of cervical cancer diagnoses occur in low- and middle-income countries that often lack the resources for routine cervical cancer screening (WHO, 2015b). However, Schmeler said that certain regions in the United States, including the Rio Grande Valley along the Texas–Mexico border, also have low rates of cervical cancer screening and high rates of cervical cancer. In the Valley, Schmeler said that cervical cancer rates are approximately 30 percent higher than in regions in Texas that do not border Mexico, and less than 10 percent of eligible women receive recommended cervical cancer screening.
But Anderson added that the incidence of infection-related cancers (such as cervical, stomach, and liver cancers) is decreasing worldwide, while the incidence of cancers linked to reproductive, dietary, and hormonal factors are increasing (Bray et al., 2012). “This is important
because the way we address each of these cancers differs. If you have an infection-associated cancer such as cervical cancer, vaccinations are a very logical, appropriate strategy,” he said.
CHALLENGES OF DELIVERING CANCER CARE IN LOW-RESOURCE AREAS
Several speakers discussed challenges in delivering cancer care in low-resource areas. These challenges included issues such as an inadequate health care infrastructure across the continuum of cancer care; limitations in workforce education, training, and capacity; a lack of affordable cancer care for patients and their families; transportation barriers; difficulties in maintaining a healthy diet and having adequate physical activity; and misalignment of cancer care with the cultural needs of patients and their communities.
Health Care Infrastructure and Workforce Challenges
Workshop speakers described the challenges of inadequate infrastructure and workforce capacity and training to support high-quality cancer care in low-resource areas, both in the United States and internationally. For example, Olopade noted that political turmoil in a number of African countries has led to significant deficits in health systems and workforce availability that has impeded cancer care delivery and outcomes. However, she also said that some African countries have emerging economies that could support the financial costs of treating cancer patients, “but there are no resources or pharmaceutical companies even marketing drugs that they can buy. There are a lot of middle-class Africans who could afford to be treated for cancer, and we have not even approached the infrastructure they need.” Anderson added that a lack of infrastructure is a major challenge to providing cancer care globally. “Cancer is not cured in banks. When [there is funding available for cancer care], we need to have somewhere to send people [for cancer treatment]. If you do not have the [health care] infrastructure, the money will sit in the bank and people will [not see] results,” he said.
Workshop speakers described infrastructure and workforce challenges across the spectrum of cancer care, including surgery, pathology, radiotherapy, medical oncology, and palliative care. For example, Anderson said that there needs to be a focus on how to deliver cancer
drugs more effectively, noting that in many low-resource areas, clinicians lack basic equipment needed for chemotherapy administration, such as infusion pumps. “If we just focused on how to get what we already know works, we could make big shifts in mortality. We should not forget about the systems part, which may seem less exciting to us,” he stressed. David Jaffray, senior scientist at the Princess Margaret Cancer Centre in Canada, added, “This is a great opportunity to think about the common safety and communication systems that we need, and no one is taking a systems view on that right now. Instead everybody is trying to get their service supported, trying to figure out how to use separate infrastructure to do this, and it is the same exact conversation. We all need the same infrastructure.”
Many low-resource areas lack a workforce to provide cancer care, Schmeler said, including the counties along the Texas–Mexico border. Although cervical cancer screening programs exist there, many women with abnormal results do not receive follow-up and needed treatment because there is a lack of clinicians in the region, she said. Speakers also described a lack of patient navigation and psychosocial care services needed to support cancer care in low-resource areas. Ochoa added that in some rural areas in the Mississippi Delta region, there is no community oncologist. Melanie Royce, professor of medicine at the University of New Mexico Cancer Center, noted that in some states like New Mexico, there is only one National Cancer Institute (NCI)-Designated Cancer Center. She added that some patients have to travel more than 200 miles in the state to access cancer care. Judith Salmon Kaur, medical director of Native American Programs at the Mayo Comprehensive Cancer Center, noted that Alaska is the only state in which the Indian Health System has an oncology department within its medical center. Native Americans who live on reservations elsewhere in the country have to be referred to care outside of their medical system.
Surgery
Anderson said surgery is an indispensable part of health care, especially for cancer care. However, The Lancet Commission on Global Surgery found that two-thirds of the world’s population does not have access to safe surgery, and the poorest third of the world’s population receives only 6 percent of surgical procedures provided globally (Meara et al., 2015), Anderson reported. He added that 33 million people each
year face catastrophic expenses in order to pay for surgical care. The Lancet Oncology Commission on Global Cancer Surgery estimated that approximately 80 percent of 15.2 million people diagnosed with cancer worldwide in 2015 would need a surgical procedure at some point during their treatment (Sullivan et al., 2015), Anderson reported. However, for three-quarters of these patients, surgery is not available, is unsafe, or is unaffordable (Sullivan et al., 2015). The Commission estimated that at least 32 million cancer operations would be needed in 2015; by 2030, the need for cancer operations is estimated to reach 45 million (Sullivan et al., 2015) (see Figure 4).
Because investing in surgery saves lives and thus promotes economic growth, the Commission estimated that all countries are projected to lose between 0.5 and 1.5 percent of their gross domestic product annually between now and 2030 if surgical systems for cancer are not strengthened (Sullivan et al., 2015).
Anderson noted that the deficit in the world’s surgical capacity will not be resolved by surgeons in high-resource countries volunteering more of their time providing surgery in low-resource countries: “We
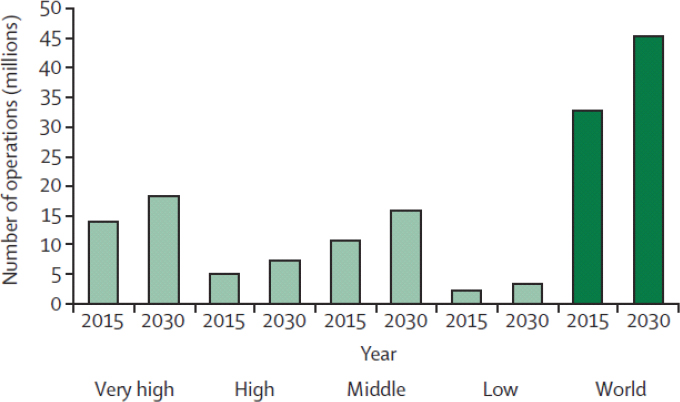
SOURCES: Anderson presentation, November 14, 2016; Reprinted from The Lancet Oncology, 16(11), Sullivan, R., et al. Global cancer surgery: Delivering safe, affordable, and timely cancer surgery, 1193-1224, Copyright (2017), with permission from Elsevier.
need to build in-country capacity with training and education, and build up a workforce because any surgeon knows that it is not just your magic hands; it is everybody around you that makes your hands do something effective,” he said. To achieve in-country capacity, Anderson said that The Lancet Oncology Commission on Global Cancer Surgery found that national cancer control plans need to include an emphasis on strengthening surgical systems by investing in public sector infrastructure, education, and training. However, he said that surgery is often given low priority within national cancer plans.
Anderson added that less than 5 percent of global cancer research is focused on surgery, and very limited research is conducted in low- and middle-income countries. He described several ongoing initiatives to improve the quality of surgical care and to increase surgical capacity and research in low-resource areas, such as the African Research Group for Oncology Consortium,6 and SURCARE.7
Pathology
Danny Milner, chief medical officer of the American Society for Clinical Pathology, described the critical importance of pathology in cancer treatment. Millner noted that without pathologists, clinicians may not be able to inform patients of their pathologic results, predict recurrence, or plan for additional therapy. However, in many low-resource areas, Milner said that there is a dearth of pathologists. In many African medical facilities, there may be only one pathologist and an enormous number of clinicians who rely on this pathologist to analyze their biopsies. He added that in some African countries, such as Benin and Somalia, there are no active pathologists, and in several others, pathologists are vastly underrepresented (Adesina et al., 2013). This can lead to months-long delays that can impede timely diagnosis and treatment. He stressed that no matter how accurate a diagnosis is, it is meaningless if it is not provided fast enough to be of value to the patient. Milner added that even when pathology results are timely, clinicians may not be available to act on these results and provide treatment
___________________
6 See https://www.mskcc.org/videos/african-research-group-oncology-seeks-improve-cancer-outcomes-low-and-middle-income-countries (accessed April 14, 2017).
7 See http://www.eortc.org/news/surcare-raising-quality-standards-in-cancer-surgery-research (accessed April 14, 2017).
for those patients. “We are all in a system and [if it is not] intact, health care is inferior and nonfunctional,” he said.
Milner highlighted four components of effective pathology services: a trained pathologist, a functional lab, adequate staffing, and quality assurance. Milner said that in low-resource areas, an essential component is often missing or inadequate. There may be a trained pathologist, but no functioning laboratory (e.g., if it was destroyed by an earthquake, has outdated equipment, or has inadequate supplies). Anderson added that there may also be a lack of workers who can maintain surgical and pathology equipment and supplies. “You may have a great immunohistochemistry lab, but nobody has bought the formalin,” he said. Without effective pathology infrastructure, Grubbs said that downstream cancer care decisions are at risk: “If you have the wrong pathology, you are going to have the wrong treatment and we are up the creek before we start.”
Radiation Therapy
According to The Lancet Oncology Commission on Expanding Global Access to Radiotherapy, radiation therapy is used in more of half of all people with cancer in high-income countries to cure localized disease, palliate symptoms, and control disease, said Jaffray. Thus, of the 24 million new diagnoses of cancer anticipated in the world in 2035, it is estimated that 12 million will require radiation therapy at least once (UICC, 2017), Barton reported. This treatment could save approximately 1 million lives each year by 2035, and 2.5 million people could have local cancer control where they would not otherwise (Atun et al., 2015). However, Barton noted that there are disparities in access to radiation therapy—access is the greatest in high-income countries and falls in proportion to the income level of the country, with low-income countries having the least access to radiation therapy (Yap et al., 2016). Jaffray added that the Commission found that worldwide access to radiation therapy is unacceptably low and that radiotherapy is often overlooked when building capacity for cancer therapy in low- and middle-income countries (Atun et al., 2015).
“The whole world has a distribution problem, not just the U.S.,” Barton said, noting that approximately 30 countries in Africa have no access to radiotherapy (see also Figure 5 for global radiotherapy coverage information). Jaffray added that less than 10 percent of the population
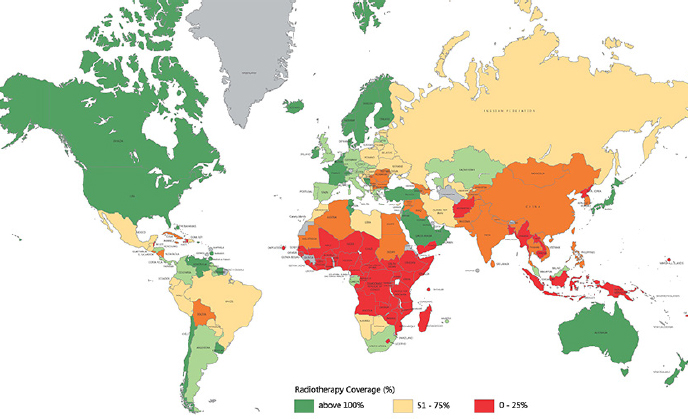
NOTE: This estimate is based on the assumption that 60 percent of cancer patients would require radiotherapy as a component of their optimal treatment plan and that one radiotherapy machine can treat 500 new patients with cancer every year.
SOURCES: Jaffray presentation, November 14, 2016; IAEA, 2014a.
in Africa has access to radiotherapy (Zubizarreta et al., 2015). With the exception of the United States, Barton said that every high-income country has a gap between demand and the number of machines available to provide radiotherapy. But the United States has approximately 1,000 more linear accelerators than needed for the current population.8 “So if you are finding a shortage of radiotherapy in the U.S., it is because it is in the wrong place, not because you do not have enough,” Barton said.
If everyone with lung cancer received appropriate access to radiotherapy treatment, a modeling study found that there would be an 8.3 percent increase in 5-year local-regional control of lung cancer, 11.4 percent increase in 2-year overall survival, and a 4 percent increase in 5-year overall survival (Shafiq et al., 2016), Barton said. He added that another modeling study is being conducted to estimate the local-regional control
___________________
8 A linear accelerator is the most commonly used device for radiation therapy. See https://www.radiologyinfo.org/en/info.cfm?pg=linac (accessed March 27, 2017).
and survival benefit of radiation therapy on all cancers. This modeling work suggests that evidence-based use of radiation therapy would result in a 10.4 percent increase in 5-year local-regional control, and a 4.1 percent increase in 5-year overall survival. Barton noted that low-income countries would have the largest benefit in terms of improved local-regional control and overall survival. “So the people who are more likely to benefit are the people who are least likely to get treated,” Barton said.
Barton and Jaffray also reported on inadequate radiation therapy workforce capacity. Barton said that estimating the radiation therapy workforce is difficult, in part because the workforce roles and titles can vary substantially by country. The Global Task Force on Radiotherapy for Cancer Control charged with estimating the worldwide radiology workforce needed to adequately treat cancer concluded that an additional 42,000 radiation oncologists, 130,000 radiation technologists, and 40,000 medical physicists need to be trained by 2035 (Atun et al., 2015). “That is a big task and if we do not get started now, it will not happen,” he said.
Cancer Drug Therapy
A number of speakers discussed the lack of cancer drug availability in low-resource areas, both in the United States and internationally.9 Lawrence Shulman, director of the Center for Global Cancer Medicine at the University of Pennsylvania Abramson Cancer Center, said the high cost of some cancer medicines is one of the reasons for their poor availability in low- and middle-income countries. For example, he calculated that in most countries in Africa, it would cost approximately $273 to treat a woman with hormone-receptor positive, human epidermal growth factor receptor 2 (HER2)-positive disease if trastuzumab (Herceptin) is not part of the drug regimen (four cycles each of doxorubicin, cyclophosphamide, and paclitaxel, and 5 years of tamoxifen treatment). Trastuzumab reduces mortality by approximately 50 percent for women who have early stage, HER2-positive breast cancer. But adding 1 year of trastuzumab to the treatment regimen could increase costs more than 100-fold. Countries “cannot afford it so they do not use it,” he said, “so we are again losing lives because of a lack of access.” He added
___________________
9 The affordability of cancer drugs in the United States is also discussed in Ensuring Patient Access to Affordable Cancer Drugs: Workshop Summary (IOM, 2014).
that a budget forecast for Botswana, a country that sees approximately 1,200 new cancer patients a year, estimated that $2.3 million per year is needed to cover cancer drugs for the entire country, but trastuzumab and rituximab alone accounted for about two-thirds of the entire budget. Shulman added that efforts to improve cancer drug availability in a number of countries are ongoing, such as the Clinton Health Access Initiative, The Max Foundation, and Partners In Health (PIH). He noted that in low-resource countries, even relatively inexpensive generic drugs may be unaffordable to patients. In Rwanda and Haiti, cancer drugs are provided free of charge to patients through PIH. But he stressed, “That is not a good long-term sustainable plan. It has to be put into the context of an infrastructure that is capable of safely and effectively administering them. It is all tied together with infrastructural capabilities and a good cancer plan. That is part of the challenge.”
Shulman added that another challenge to providing cancer medicines in low-resource countries is stock-outs (or shortages) of essential cancer medicines. In Botswana, he said that at least 40 percent of its essential cancer medicines were out of stock for a mean and median duration of 48 and 30 days, respectively during 2015. He stressed that such stock-outs can be lethal, such as when one medicine of a potentially curative combination therapy is out of stock.
Some clinicians in low-resource areas may also lack familiarity and training in cancer diagnosis and treatment options. For example, Anderson noted that in countries that lack early detection and screening programs, some clinicians in low-resource settings may not recognize early-stage cancer presentation.
Clinicians in low-resource areas also might not provide standard of care therapies; Olopade noted that when she worked in Nigeria 10 years ago, a common practice was to give women presenting with a breast lump tamoxifen, and women would be sent back to their village without surgical removal or biopsies to analyze whether it was cancer or whether the cancer would respond to the drug. Olopade added that adjuvant hormonal therapy among women with estrogen receptor–positive breast cancer can reduce mortality by 30 percent, but even in the United States, clinician prescribing rates varied (Daly et al., 2017) (see Figure 6). Factors such as geographic location, race, and whether women received surgery and radiation therapy were significantly associated with the variation in adjuvant hormonal therapy administration.
Shulman agreed, noting that if clinicians do not use appropriate
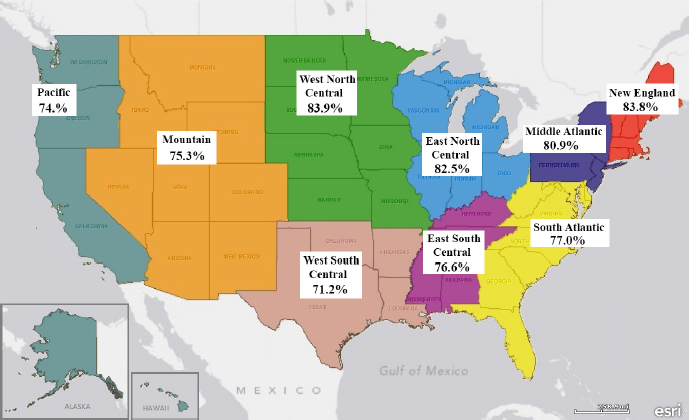
SOURCES: Olopade presentation, November 14, 2016; Reproduced with permission from JAMA Oncology. 2017. doi: 10.1001/jamaoncol.2016.6380. Copyright © (2017) American Medical Association. All rights reserved.
dosing and schedules, “you are exposing the patient to the toxicity [of the drugs] with a much-diminished chance of a positive outcome. . . . That happens unfortunately quite regularly in many places, sometimes even in the United States.” He suggested ensuring recordkeeping of dosing and schedules, as well as clinical outcomes to assess the effectiveness of treatment administered. Providing personal protective equipment for the nurses and pharmacists who are mixing and administering the drugs is critical for their safety, he added.
Palliative Care
Marie Bakitas, associate director of the Center for Palliative and Supportive Care at the University of Alabama at Birmingham School of Nursing, and James Cleary, professor of medicine at the University of Wisconsin Carbone Cancer Center, reported that palliative care is inadequately addressed in low-resource areas, both globally and in the United States (see Figures 7 and 8). Mark Lazenby, associate professor of nursing
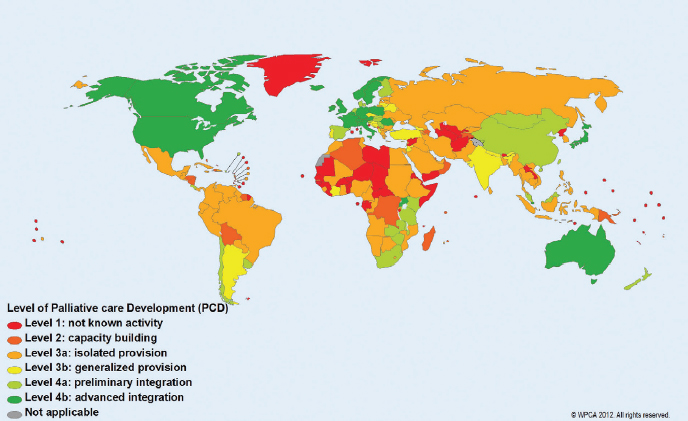
NOTE: WPCA = Worldwide Palliative Care Alliance.
SOURCES: Bakitas and Cleary presentations, November 14, 2016; Connor and Bermedo, 2014.
at the Yale School of Nursing, agreed and said that palliative care should begin at the time of cancer diagnosis and continue throughout care. The main purpose of palliative care is to prevent and treat the symptoms and side effects of cancer and its treatment, particularly the physical, social, and spiritual side effects, he said. Bakitas added that ASCO, noting that palliative care can extend life (Temel et al., 2010), has recommended that patients with advanced cancer receive dedicated palliative care services concurrent with active treatment (Ferrell et al., 2016). The WHO also released a global resolution in order to improve access to palliative care services as a component of health systems (WHO, 2014). But she pointed out that “the workforce is not prepared to address this issue, so we need more clinicians [to provide palliative care], including all members of interdisciplinary teams.”
A main component of palliative care is pain relief, but Cleary reported that there are disparities in access to opioid pain medications in the United States and globally. One study found that 42 percent of U.S. patients with metastatic cancers who were seen in outpatient cancer centers did not receive sufficient pain medicines (Cleeland et al., 1994).
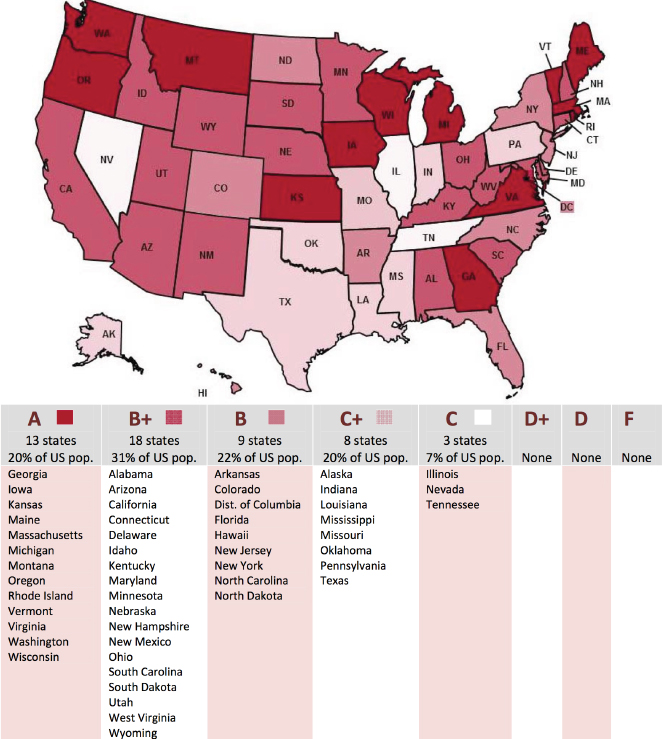
NOTES: A state’s grade represents the quality of its policies affecting pain treatment. It is calculated from the total number of provisions in a state fulfilling the evaluation criteria; higher grades mean more balanced state policies influencing pain management, including the medical use of opioid analgesics.
SOURCES: Cleary presentation, November 14, 2016; Pain & Policy Studies Group, 2014.
Cleary added that minority patients are also much more likely to receive inadequate treatment for pain compared to nonminorities, a situation that he said persists today (Cleeland et al., 1994; Fisch et al., 2012). Compared to white patients, African Americans are less likely to receive pain medicines in the emergency room (Singhal et al., 2016), and Afri-
can Americans with cancer are more likely to receive toxic pain medication for cancer-related pain, despite having insufficient kidney function (Meghani et al., 2014), Cleary reported. Bakitas added that minorities are known to use hospice care at much lower rates than whites.
Global disparities also exist in the use of opioid medicines to relieve pain, Cleary said. A study showing trends in consumption of opioids between 2001 and 2013 found that most regions of the world have inadequate access (Berterame et al., 2016). Cleary noted that only 16 percent of the world’s population resides in high-income countries, but they consume 90 percent of the world’s opioids. Cleary added that the numerous restrictions on opioid pain medicines to prevent drug abuse present a major challenge to providing palliative care globally. Additional barriers in opioid use for pain relief in low-resource countries include a lack of training for appropriate use of opioid medicines, fear of addiction, limited financial resources or sources for opioids, cultural and social attitudes, fear of diversion, control measures for international trade, and onerous regulatory frameworks for opioids (International Narcotics Control Board, 2016).
Blood transfusions can provide essential support for patients at any phase of cancer treatment (see Box 2). Jeffrey McCullough, emeritus professor at the University of Minnesota Department of Laboratory Medicine and Pathology, said blood transfusions may be needed for cancer care for multiple reasons, including treating anemia (caused by cancer treatment or advanced disease), thrombocytopenia, hemostasis
if hemorrhage is an acute problem, prophylactic transfusions to prepare for procedures, or surgical blood loss.
Rural areas of the United States have a shortage of palliative care experts and facilities, said Bakitas. “Size matters when we look at the likelihood of palliative care being available in the community for most of our cancer patients,” Bakitas said. Palliative care is less likely to be provided in the hospitals that are the sole community provider or in hospitals with fewer than 50 beds—only 22 percent of hospitals with 50 beds or less in the United States provide palliative care (Morrison et al., 2015).
The lack of palliative care services and facilities is especially pronounced in some rural areas of the United States, Bakitis said. In Alabama, 40 percent of residents reside in rural areas, and 14 counties have no hospice services. But the lack of hospice care in states like Alabama and Mississippi is not only due to the predominantly rural setting because there are other rural states, such as New Hampshire and Vermont, where hospice is more widely available and far fewer cancer patients are hospitalized during the last month of their lives, Bakitas noted.
There are also policy and clinical practice issues that may prevent patients with advanced disease from receiving palliative and hospice care (Bakitas et al., 2015a; CAPC, 2011; Ceronsky et al., 2013; Elliott et al., 2016; Fink et al., 2013; IOM, 2015). For example, critical access hospitals are required to discharge patients within 96 hours, “however, it is very difficult to get to know your patient, to understand what the issues are going to be, and to develop a relationship” to help them understand that with their advanced cancer, we can do just as much for them by transferring them home with hospice care. “There are disincentives because patients just need to be rushed out the door to someplace else,” Bakitas said.
Patient Navigation and Psychosocial Support Services
Several speakers noted that patients with cancer may need a broad range of support services, including help navigating their cancer treatment, locating financial and psychological counseling, and maintaining a healthy lifestyle, including smoking cessation, weight management, and physical activity. Olopade said that patients from low-resource areas are often blamed for not adhering to their cancer treatment and
survivorship plans, but this lack of adherence is often due to structural barriers in the health care system. “I do not care how rich you are, to actually get cancer care, you have to go through hoops,” she said, and going through those hoops is much more difficult for patients with limited resources.
Gina Villani, chief executive officer and medical director of the Ralph Lauren Center for Cancer Care (see Box 3), stressed that patient navigation is critically important in low-resource communities. She said patient navigators are trained, culturally competent health care workers who work with patients, families, clinicians, and others in the health care system to ensure that patient needs are appropriately and effectively addressed. She said patient navigators at the Ralph Lauren Center for Cancer Care “provide emotional support, help patients make appointments and understand their diagnosis, as well as help them with transportation, language services, [and] other support services . . . to make sure that patients get the services they need.” Patient navigators can help access available financial support, assist with related paperwork, and coordinate follow-up care and outreach to community support services.
Villani discussed findings from the NCI-funded Patient Navigation Research Program, which found that patients who underwent patient navigation during their cancer care were more likely to resolve abnormal findings with diagnosis and were more likely to initiate cancer treatment (NCI, 2015). Patients with navigation support also reported improved quality of life and increased satisfaction with the health care system and cancer care compared with those who did not receive navigation support, Villani said. She added that Paskett and colleagues (2011) conducted a systematic review of patient navigation that found the majority of studies focused on cancer screening and found a favorable impact. Of the seven treatment outcome studies included, five were inconclusive and two studies showed improvements in quality of life and lowered emotional distress among low-income patients (Paskett et al., 2011).
Marjorie Kagawa-Singer, research professor at the University of California, Los Angeles, Fielding School of Public Health, stressed that patient navigation can break down many of the structural barriers preventing patients from receiving the care they need. She said that in a screening outreach program among the Hmong community in California, the women were highly receptive to undergoing breast cancer screening, but did not know where to go for a mammogram. The program was able to identify screening sites and arranged for translators at
these sites, leading to 80 percent of the women receiving screening. “So it is not that they did not want to be screened, they just did not know how to navigate it, which becomes a critical piece,” Kagawa-Singer said.
Olopade noted that sometimes navigation services are needed following cancer treatment in order to locate appropriate survivorship care. She said a number of breast cancer survivors in low-resource communities stop their hormonal treatment because they had difficulties getting appointments with their clinicians to manage the side effects of these medications. She suggested nurse navigators could help patients with managing these symptoms and improve medication adherence.
Villani also said that financial advisors can help patients find insurance, obtain short- and long-term disability, or identify other
mechanisms of financial support. “The uninsured, the underinsured, and patients who are on Medicaid and Medicare need to [work with] a financial navigator,” she said.
Villani added that social workers and psychologists can help with patients’ psychological and emotional needs, and nutritionists can help advise patients on appropriate diets during their cancer treatment and survivorship care. Villani noted that the Ralph Lauren Center for Cancer Care has a restaurant voucher system that enables its patients to receive a meal at participating local restaurants free of charge.
Kaur added that family caregivers need support when taking care of loved ones with cancer: “How do we help those families who want to do
their best but do not feel they have the support and skills to take care of their loved ones . . . who cares for the caregivers?”
Villani noted that the Ralph Lauren Center for Cancer Care uses approximately 30 to 40 percent of its budget on patient outreach, including dispelling myths that patients may have about receiving cancer treatment, such as “if I walk in there, they are going to treat me poorly and I am going to sit around and wait for hours to be seen by somebody who does not care about me.” Kagawa-Singer said one patient attending a town hall meeting voiced similar concerns, saying, “I know I do not have money, but they make me feel poor when I go in, so I do not go.”
Affordability of Cancer Care for Patients and Their Families
Several speakers highlighted that cancer care can be extremely expensive for patients with cancer and their families. Olopade added that although the Patient Protection and Affordable Care Act has increased insurance coverage in the United States, some individuals still may not receive the cancer care they need due to a lack of insurance coverage, high insurance deductibles, or other cost sharing policies.10 She added that the affordability of cancer care “is not a problem just in this country—it is a global problem.”
The financial burden of cancer care, especially among minority patients, has been documented in a number of studies, said Villani. One U.S. study found that 68 percent of African Americans, 58 percent of Hispanics, and 45 percent of whites reported experiencing economic hardship one year after a cancer diagnosis (Pisu et al., 2015). Another study found that 4 years after being diagnosed with non-metastatic breast cancer, 15 percent of African American women reported having medical debt compared with 9 percent of white women (Jagsi et al., 2014). Villani added that a disproportionate number of minorities experience bankruptcy following cancer treatment (Ramsey et al., 2013). Cancer patients who experience bankruptcy are at a much higher risk of dying than cancer patients who do not experience bankruptcy (adjusted hazard ratio = 1.79; 95% confidence interval, 1.64 to 1.96) (Ramsey et
___________________
10 Cost-sharing refers to the share of costs that an individual covered by insurance has to pay out of his/her own pocket; this generally includes deductibles, coinsurance, and co-payments, or similar charges. See https://www.healthcare.gov/glossary/cost-sharing (accessed March 9, 2017).
al., 2016). Karen Meneses, professor and associate dean at the University of Alabama at Birmingham, added that she has found that in rural areas in the United States, many older breast cancer survivors face significant financial burdens that impede them from acquiring the follow-up care they needed.
Gwen Darien, executive vice president for patient advocacy at the National Patient Advocate Foundation, added that “it is not just about paying for treatment, it is also about how it affects you as a consumer and about the long-term debt you acquire.” She listed the top five financial issues for which patients ask for help from Patient Advocate Foundation case managers: co-pays associated with hospital and clinician visits (10.5 percent), transportation (9 percent), co-pays for pharmaceutical drugs (7.5 percent), rent or mortgage payments (6 percent), and utilities (5 percent) (Patient Advocate Foundation, 2015).11 “It does not matter whether your co-pay is $10 or $100. If you cannot afford $10, that is an incredible financial burden,” Darien said.
In 2015, the Patient Advocate Foundation collected data showing that 27 percent of patients had to stop or postpone treatment because they could not afford it. Twenty-six percent also reported they could not follow medical advice as prescribed because they could not afford it (Patient Advocate Foundation, 2015). “We talk a lot about financial toxicity, but we should talk about economic toxicity because it is the whole social system,” Darien said.
Olopade added that the expense of cancer care has implications on an entire family, and not just the individual undergoing treatment. She said that a patient of hers said that she would rather forego cancer treatment than lose her home to bankruptcy, because the patient felt it was the honorable thing to do for her family. Kagawa-Singer added that some patients with cancer have to travel away from their community to receive cancer treatment, which can be expensive for both the patient and for the caregiver accompanying them. Thus, some patients do not receive cancer treatment because they believe it is a drain on family resources and “it is not worth my life to make everybody else suffer,” Kagawa-Singer said.
___________________
11 Note: The issues that patients report to case managers are so diverse that the top five only reflect about 39 percent of all case management issues.
Transportation Barriers
Several presenters stressed how the lack of affordable, easy-to-use transportation options can be a major impediment to cancer care in low-resource communities, both in rural and urban areas. Shulman highlighted a literature review that found travel burdens can negatively influence a patient’s stage of diagnosis, appropriate treatment, health outcomes, and quality of life (Ambroggi et al., 2015).
Darien stressed that “transportation issues are really becoming an emerging obstacle to health care access and a critical health equity and health disparities issue.” She added that transportation can be a large expense for patients, and that inadequate transportation can result in missed appointments, delayed treatment or treatment abandonment, poor management of health conditions, and worsened health outcomes. Even when patients are able to travel to their appointments, they may not have the transportation available to pick up their prescriptions or obtain other follow-up care. “Patients struggle with this, whether they have to go 10 miles or just a few miles in an urban area. It can take people 2 hours to get to an appointment in the greater DC area if they have to take public transportation, and many people are not healthy enough to do so,” Darien said. Kagawa-Singer added that “if you have to take three buses to get to the treatment facility and you have your kids with you because you have no child care, how likely is it that you are going to follow through with your treatment?” In rural areas, Darien said some individuals may travel hundreds of miles to receive care, and described the experience of one couple who drove 100 miles per day, 5 days per week in order for the husband to receive radiation therapy.
Transportation can also be a significant barrier for delivery of the blood and other supplies that cancer patients need in low-resource countries, McCullough said. Shulman agreed, noting that a cancer center in Rwanda is a 2- to 3-hour drive on poorly passable dirt roads from the nearby city where blood is collected. He said there have been times when children with leukemia died because they lacked the timely administration of platelets.
Stephanie Petrone, executive director of medical operations at Novartis Oncology, agreed that “transportation is a key barrier for patients,” especially for those in rural areas who wish to participate in clinical trials, which are usually conducted at major urban medical institutions or large community settings. Many of these clinical trials
require research-trained clinicians and those proficient in oncology, but there may be a dearth of this expertise in rural communities. Darien added, “All the research and personalized medicine in the world are not going to solve health care crises if we cannot get them to people, and transportation is clearly a huge barrier to that.”
Poor Access to Healthy Nutrition and Exercise Facilities During Cancer Treatment and Survivorship
Sheila Davis, chief nursing officer at PIH, noted that in many low-resource countries, people earn less than a dollar per day, and that having enough money for food can be a competing priority with the cost of cancer care. Villani reported that the Ralph Lauren Center for Cancer Care has a food pantry that provides low-income patients with groceries to help ensure they have adequate nutrition during their cancer treatment.
Another challenge in some low-resource areas is food deserts, or places that lack stores providing healthy food options, including fruits and vegetables. Adams-Campbell noted that food deserts may have fast-food restaurants or convenience stores with inexpensive but unhealthy food options that can contribute to obesity. This makes it challenging for people to adhere to the healthy diets linked to a lower risk of cancer and better health outcomes following cancer treatment.
Adams-Campbell added that many African American cancer survivors in the United States live in unsafe neighborhoods and lack access to parks and other facilities in which they can exercise safely (Jones and Paxton, 2015; Meadows et al., 2017; Oyekanmi and Paxton, 2014). This can make it challenging to adhere to physical activity programs aimed at improving energy balance and lowering risk of cancer recurrence, she said.
Challenges in Meeting the Needs of Patients from Diverse Cultures
A number of speakers said that cultural differences among those providing cancer care and those receiving it can be a major challenge in the delivery of cancer care in low-resource communities. Kagawa-Singer defined culture as a tool that each member of the community uses to ensure survival and well-being, and to make life meaningful. She added that culture is a shared framework that is socially, morally, and legally integrated into the structures of a society’s institutions. Kaur noted that
“culture develops because it has a way of dealing with those important aspects of life—birth, marriage, death, healing, spirituality, emotions. And it definitely influences what a diagnosis and treatment plan might include, because people have certain cultural ideas. But we need to remember that culture is a living thing.” Kagawa-Singer agreed that culture is dynamic and can change with time, and added that historical circumstances play an important role in some cultures. For example, Bakitas said the Tuskegee study of syphilis in African Americans generated mistrust of the medical and scientific communities.12
Kagawa-Singer stressed that a person’s culture is central to how he or she operates in the world, including within the medical realm. She said that when working with other cultures, it is important to reach out and understand their goals prior to delivering medical care. Barton noted that although some programs bring in professional expertise from academic centers to low-resource countries, he suggested it is far more important to develop local expertise: “Local people know their culture. The biggest problem we have when specialists arrive is that they think they are going to be able to run a department like the one they were trained in, which was in a completely different setting, so we need to develop local expertise to make it work.”
Kaur stressed the importance of being respectful of other cultures, including communication styles, and how people relate to time, personal space, and spirituality. Other considerations include being mindful of a culture’s social organization and structure and their health beliefs and practices, especially regarding sexuality and reproduction when addressing gynecologic or breast cancers. Kaur said clinicians should also not fault people for being noncompliant with their treatment, but instead recognize and address the barriers that may be causing noncompliance.
Anderson said more understanding is needed about the social beliefs in a low-resource area, some of which may need to be addressed in order to provide cancer care. For example, a study found that Gazan women thought it was reasonable to receive a mammogram if they had signs and symptoms of breast disease, but that it was unnecessary without these signs and symptoms (Shaheen et al., 2011). Several workshop speakers said that some patients in low-resource communities have limited health literacy. Anderson stressed that “Awareness education might be the most important intervention we have in breast cancer. Women need
___________________
12 See https://www.cdc.gov/tuskegee/timeline.htm (accessed March 9, 2017).
to [recognize that], ‘I have this lump, it is not going away, and I am not debilitated, but I need to have it evaluated.’ This is really important.”
Anderson added that many cultures believe cancer is fatal and that can be a barrier to treatment. Kaur responded that for some people, cancer can be a death sentence because of inadequate care or delays in diagnosis and treatment. “So we have to take those health beliefs seriously. . . . In order [for us] to be believed, we have to provide [information about] how best care can occur, either in terms of showing survivorship or proving that we can take care of pain at the end of life,” she said. Kagawa-Singer responded that she has worked with many groups who think cancer is a death sentence based on personal experience, but people tend to be receptive to respectful outreach that helps improve understanding about treatment options, or that explains how early detection of cancer can improve outcomes.
Several speakers said that certain cultural beliefs can make it difficult to deliver palliative care across the care continuum. Cleary said that cultural beliefs can be a barrier to the use of opioid medications for cancer pain relief. Bakitas also noted that some people are mistrustful of hospice care and may incorrectly believe that the intent of palliative care is to deny people curative therapies. In addition to trying to dispel these beliefs, Bakitas suggested that “maybe we need to first find out what are the things that would meet their needs when they have serious illness and end-of-life issues.”
Kagawa-Singer said that an important component of culturally appropriate cancer care is the alignment with a population’s language and health literacy. “Make sure your population understands what you are trying to ask,” she said. “If we do not understand the lens that we, as researchers, have, it is going to be difficult to get at the culture of those we work with,” she added. Adams-Campbell also said it is important to understand the language preferences of a population, and noted that a focus group of African American cancer survivors preferred the term “positive energy balance” rather than “obesity.” “Sometimes we have to let the community decide what we present to them to get people to buy into the concept,” she said.
Kagawa-Singer also cautioned against clinicians using technical terminology or jargon when communicating with patients. She suggested speaking plainly, which takes time and expertise that clinicians may not have. To facilitate communication, she suggested that lay navigators, nurses, social workers, and other support staff could help
convey complex medical terms and concepts. Kaur added that “Personal culture and the culture of medicine often clash. We know we speak a foreign language and we need to learn how to speak the language of the community.”
Bakitas said clinicians should describe palliative care accurately, as an extra layer of support throughout the continuum of care, rather than describe it as an option of last resort. She noted that there is limited availability of culturally appropriate education materials describing palliative care. “Although many of our programs talk about palliative care, having that cultural perspective, which is so critical to becoming integrated into the community, is often lacking.”
Meneses said that a standard Spanish translation of educational outreach materials for Hispanic cancer survivors may not be sufficient, and noted that she has further tailored materials to address high-priority issues within a specific community, using culturally relevant terminology (Meneses et al., 2015). She added that her educational intervention for Latina breast cancer survivors was delivered by phone by bilingual Latinas, based on surveyed preferences. Kagawa-Singer added that when she conducted a breast and cervical cancer screening program for Hmong women in California, she included husbands in the outreach strategy because they are integral to family decision making in this community (Kagawa-Singer et al., 2009).
POTENTIAL STRATEGIES FOR IMPROVING CANCER CARE IN LOW-RESOURCE AREAS
A number of workshop participants suggested a variety of potential strategies for improving cancer care in low-resource areas, including
- Improving workforce education and training;
- Establishing partnerships;
- Using innovative and resource-appropriate technologies;
- Establishing and promoting resource-appropriate clinical practice guidelines and priorities for cancer care; and
- Exploring opportunities to eliminate disparities in cancer care.
“The standard model of cancer care is not always going to be viable in low-resource settings, so we need to think differently about solutions,” Barton stressed. Other speakers noted that there is no one-size-fits-all program
that can be applied to every low-resource community. Shulman found in his work in Botswana, Haiti, and Rwanda “that the challenges these countries face in the attempt to deliver cancer care are quite different from one another, and therefore our approaches in these countries are quite different.” Davis agreed that “it is important to remember that every country is different” and that the needs of a country can change over time. She suggested developing programs that have flexibility and can change as needed.
Workforce Education and Training
Several participants suggested opportunities to improve education and training of the workforce providing cancer care in low-resource areas, both in the United States and globally. These suggestions included mentoring and training collaborations, task shifting to enable a broader range of providers to deliver cancer care, preparing the workforce to deliver culturally appropriate care in resource-limited settings, and recognizing this expertise.
International Training and Mentoring
Jaffray suggested using innovative approaches to train and mentor clinicians in low-resource areas. He noted that the International Cancer Expert Corps is a mentoring network of cancer professionals who work with local and regional in-country groups to develop and sustain expertise for better cancer care.13 Medical Physics for World Benefit also provides support to improve the safe and effective use of radiation and related technologies in medicine, especially in low- and middle-income countries.14 Barton said the International Atomic Energy Agency has established an eLearning platform called the Virtual University for Cancer Control (VUCCnet), which has trained more than 500 African clinicians in cancer-related courses (IAEA, 2014b). “Our old face-to-face model is not going to work globally” to address the extensive needs Barton said. He also suggested providing training opportunities that are appropriate to the culture, resources available, and the cancer burdens of an area. Barton also suggested that clinicians receive training in the
___________________
13 See http://www.iceccancer.org (accessed March 12, 2017).
14 See http://www.mpwb.org (accessed March 12, 2017).
countries in which they reside because clinicians who are trained in other countries may not opt to return.
Schmeler said The University of Texas MD Anderson Cancer Center is working to build international workforce capacity for cancer care through telementoring (see Box 4); clinician trainee exchanges with
Brazil and Mozambique; hands-on training courses in surgical and medical oncology; and technical courses, including courses on loop electrosurgical excision procedures and fine-needle aspiration breast biopsies. The MD Anderson Cancer Center also holds classes in Brazil, and invites clinicians from other countries—such as Mozambique—to
attend. The MD Anderson Cancer Center raised funds to pay for the flights of clinicians attending from outside Brazil, and sister institutions in Brazil pay for the clinicians’ local expenses. In addition, the Mozambique Ministry of Health paid for the clinicians’ salaries while they were in Brazil for 3 months attending classes, Schmeler reported.
She has also worked with the International Gynecologic Cancer Society to create a global 2-year curriculum to train clinicians in gynecologic oncology in countries that do not have formal training in this specialty. This program will start in 2017 at pilot sites in the Caribbean, Ethiopia, Kenya, Mozambique, and Vietnam.
Royce suggested that remote technologies enabling web conferencing for meetings and interactions are also important in low-resource rural areas. She added that in New Mexico they use information technology (IT) solutions rather than face-to-face meetings when possible to avoid the time it takes to travel across the state. “The sooner you implement automation and IT solutions, the sooner your staff gets efficient. It may be costly in the beginning, but you will reap your rewards,” she said.
Kaur said she secured institutional funding to bring a physician from Ethiopia to learn about how the Mayo Clinic delivers palliative care, in order to help him develop a palliative care clinic in Ethiopia. This physician met with Mayo palliative care teams, made hospice visits, and observed chemotherapy administration and cancer surgeries. He also collaborated with a Mayo Clinic pharmacist and the Ministry of Health in Ethiopia to determine how he could access and administer morphine to Ethiopian patients. Cleary added that efforts of the Pain and Policy Study Group at the University of Wisconsin–Madison15 have also helped to improve opioid access throughout Ethiopia.
Kaur noted that the Mayo Clinic has also led a virtual international palliative care symposium that was well attended, and has also partnered with clinicians in the Indian Health Service to provide palliative care among Native American populations.
Task Shifting
Olopade suggested that improved use of task shifting could increase the number of clinicians providing cancer care in low-resource areas. For example, she suggested increased training for more nurses to administer
___________________
15 See http://www.painpolicy.wisc.edu (accessed April 20, 2017).
chemotherapy. Day agreed, noting that nurses conduct a wide range of tasks when there is a lack of specialty care in low-resource countries or communities. However, if nurses are to deliver more complex care tasks, Day said they need additional training. For example, St. Jude Children’s Research Hospital has developed regional training centers for nurses; she added that this approach can be done at low cost.16
Olopade suggested that primary care clinicians should be trained to prescribe and monitor hormonal therapies or to administer other drug therapies for cancer patients because primary care clinicians may have more contact with cancer patients in low-resource areas. She said that it was clear when working with primary care physicians on the south side of Chicago that the average primary care physician lacks knowledge that is essential for the care of their cancer patients. Cleary added that due to the low number of physicians in Uganda, appropriately trained nurses are allowed to prescribe and dispense opioids.
Preparing the Workforce to Deliver Culturally Appropriate Care in Low-Resource Areas
Several speakers said that additional work is needed to ensure that low-resource areas have enough clinicians with expertise in delivering culturally appropriate care to diverse individuals. Davis said we have a “moral imperative that we do work in these places.” Olopade agreed and said, “If you are a physician taking care of a patient, and you cannot even imagine where they are coming from, you are not going to be able to take care of them. We have to train health care professionals to think about whom we are taking care of.” She added that at her institution, all medical students take a course on health disparities, which requires them to work with low-resource communities to understand the types of challenges these patients can face (such as within a community health center; see Box 5). She said these training experiences can influence their career trajectories, including a commitment to practice in underserved settings.
Villani suggested creating a specialty in working with diverse, vulnerable, and underserved populations. This could motivate individuals to undertake these careers, provide clinicians with specialized expertise, and validate the importance of this career path.
Olopade agreed, adding, “We need to put more funding into that
___________________
16 See https://www.ncbi.nlm.nih.gov/pubmed/22102623 (accessed March 27, 2017).
type of career development and career path.” Meneses said that validating this career path could inspire future generations of clinicians and researchers: “We need to mentor and train the next generation of health disparities [and] health equity research scientists,” she said.
Examples of Partnerships to Improve Cancer Care in Low-Resource Areas
Speakers discussed a variety of partnerships and collaborations that aim to build capacity and improve cancer care in low-resource areas. These partnerships can involve a number of individuals and organizations, such as clinicians, cancer centers, government agencies, nonprofit organizations, and industry. When creating partnerships to serve low-resource areas, Meneses suggested using the framework of community-based participatory research, as was used in the Deep South Network
for Cancer Control (see Box 6). This framework involves evaluating community readiness, identifying community champions, using effective interventions, and customizing programs to better fit the needs identified by the community, including incorporation of sociocultural values and preferences. Meneses said asking a community for feedback on the program was essential. “Collaborate, partner, collaborate, partner, and then repeat,” she said.
Kaur said that initially, some people in a low-resource community may be unaware of a specific cancer intervention and may be unwilling to implement it in their community. “You have to find a way to do deliberative experimentation and localize the normalization of good health care, and eventually you reach a tipping point where you have the [community] leadership to go forward,” Kaur said. Important steps to take in that regard are to plan, engage community input, revise plans
according to community needs and readiness, and always be open to new ideas, she said.
Davis also said that interprofessional and interdisciplinary partnerships are needed to expand capacity in low-resource areas. “Building and strengthening capacity really requires an interdisciplinary team, including both nurses and physicians. It is not good enough just to have one health cadre go and try to teach the entire interdisciplinary team,” Davis said.
Edward Trimble, director of the Center for Global Health at the NCI, noted that U.S. government agencies provide funding and services for international partnerships abroad, including the Department of State (health and science diplomacy, U.S. Agency for International Development, and the President’s Emergency Plan for AIDS Relief), CDC, the Health Resources and Services Administration (HRSA), the Food and Drug Administration, and the Department of Defense (DoD). He
TABLE 1 Examples of Partnering Organizations for Cancer Care in Low-Resource Areas
| Advocacy Community | American Cancer Society |
| Institute of Hospice and Palliative Care in Africa | |
| International Union for Cancer Control | |
| The Max Foundation | |
| Professional Societies | American Society for Clinical Pathology |
| American Society of Clinical Oncology | |
| American Society of Hematology | |
| International Gynecologic Cancer Society | |
| Oncology Nursing Society | |
| Sociedad Latinoamericana y del Caribe de Oncología Médica | |
| Academic Community | Consortium of Universities for Global Health |
| National Cancer Institute–designated cancer centers | |
| National Comprehensive Cancer Network |
SOURCE: Trimble presentation, November 15, 2017.
added that DoD has “some of the best expertise in the world in terms of logistics and tackling surgical issues. They have a great tradition of working with other countries on their military as well as civilian medical systems.” Trimble highlighted partnership organizations involving the advocacy community, professional societies, and the academic community (see Table 1). He added that the International Cancer Control Partnership,17 Pink Ribbon Red Ribbon,18 and Global Cancer and Non-Communicable Diseases Research Centers of Excellence, which are consortia of universities in high-, middle-, and low-income countries, are also actively involved in partnerships to improve cancer care in low-resource areas.
Pathology-Focused Partnerships
Milner discussed ongoing partnerships involving the provision of pathology and surgical expertise in low-resource settings. For example, through PIH (see Box 7), pathologists at academic centers in the United
___________________
17 See http://www.iccp-portal.org (accessed April 14, 2017).
18 See http://pinkribbonredribbon.org (accessed April 14, 2017).
States or Europe were paired with clinicians at facilities in Rwanda and Haiti in order to review biopsies and generate pathology reports. These pathologists volunteered their time and their institutions covered the costs of processing. The clinicians who provided surgery, if needed, were paid field workers from PIH. If other cancer treatment was needed, clinical oncologists donated their time to provide the care. Milner said that the pros of such partnerships are that they provide access to high-quality care, including access to cutting edge diagnostics, serial follow-up, and continuity of information. But Milner added that the disadvantages of such partnerships are that they can be difficult to sustain because they are expensive and require volunteer time that may wane over time. Milner added that demand for pathology expertise in Haiti and Rwanda was so great that they built in country laboratories, and Milner and his colleagues worked to establish a pathology residency program and other educational programs so that these pathology services could be sustained.
Milner said that pathologists have also donated their time for 2- to 6-week intervals to provide their expertise onsite at facilities in low-resource areas. Volunteer pathologists are especially valuable at laboratories in which there is only one pathologist and a large backlog of slides that need to be reviewed, Milner added. The costs for such volunteer efforts include vacation time or departmental leave and travel expenses for pathologists. The site that receives these volunteers usually provides the workspace, caseload, and administrative support. But this type of partnership requires a working lab with the technicians and supplies, Milner added.
Partnerships to Increase Access to Palliative Care
Several speakers discussed partnerships focused on palliative care in low-resource areas, including Patient Care Connect, Project ENABLE, and International Pain Policy Fellowship program (see Box 8).
Partnerships to Increase Access to Cancer Drugs
Petrone reported on the partnership between Novartis and The Max Foundation that strives to increase patient access to the cancer drug imatinib (Glivec) in low- and middle-income countries, called the Glivec International Patient Assistance Program. Pat Garcia-Gonzalez, chief executive officer of The Max Foundation, said that the mission
of the Foundation is to increase global access to care and support for people living with cancer. The Foundation was founded in memory of Garcia-Gonzalez’s stepson, who died from leukemia before imatinib was available. “We started The Max Foundation to make sure that people in our situation had the help we could not get for Max,” she said.
The Foundation’s role in the partnership is to confirm that patients who apply to the patient assistance program are diagnosed with BCR--
ABL–positive19 chronic myeloid leukemia (CML), gastrointestinal stromal tumors, or other approved orphan indications and that these patients are not able to access imatinib through other means. Shulman added that The Max Foundation ensures that appropriate molecular testing for BCR-ABL is completed, and the foundation has the appropriate infrastructure to treat and follow patients over time. After the foundation confirms medical and socio-economic eligibility, Novartis provides the drug to these patients’ physicians free of charge. The Max Foundation works with 1,500 physicians in 80 countries; during the past 15 years, Novartis has provided approximately 3 million monthly doses of imatinib through the program. Compared to the inception of the program in 2002, Garcia-Gonzalez said that patients with CML participating in the program today are more likely to be in the chronic phase of the disease when the medication is requested, as opposed to the accelerated phase or in blast crisis. “We are really bringing treatment to the patients early on in their disease,” Garcia-Gonzalez said. Shulman added that partnership with The Max Foundation has resulted in 43 leukemia patients in Rwanda receiving imatinib, and these patients had an overall survival rate of 94.7 percent at median follow-up of 22.6 months (Tapela et al., 2016).
The Max Foundation has recently reached out to additional pharmaceutical companies to improve access to cancer drugs in low-resource areas, and is currently partnering with five companies to receive medication donations, Garcia-Gonzalez said. The Foundation has developed the licensing and network distribution capacities to deliver these medicines, and also plans to use this strategy to increase access to diagnostics in low-resource areas, Garcia-Gonzalez said.
Petrone also reported on the Novartis Access Program, which provides 15 of its drugs, both on and off patent, for cardiovascular disease, diabetes, respiratory disease, and breast cancer to governments, nongovernmental organizations, and other public-sector customers in low- and lower-middle-income countries at the cost of one U.S. dollar per treatment per month. The initial roll out of this program included Ethiopia, Kenya, and Vietnam, but the company plans to extend the program to up to 30 countries, and hopes to reach 20 million patients by 2020 (Novartis, 2017).
___________________
19 BCR-ABL is a fusion gene formed when pieces of chromosomes 9 and 22 break off and trade places, and is found in most patients with chronic myelogenous leukemia (NCI, 2017a).
Transportation Partnerships
Several workshop speakers discussed partnership opportunities to improve transportation to cancer care in low-resource areas. Milner suggested that partnerships with ridesharing services, such as Uber or Lyft, could help facilitate patient access to medical facilities. Shulman noted that one hospital in a low-resource area of Philadelphia developed a contract with a ridesharing service to assist with patient transportation. “It is a very facile way to move patients back and forth and have the billing directed to a central spot,” he said. Darien noted that there can be liability issues involved with transporting people with life-threatening illnesses, and said that ridesharing services would need to address these issues in order for these partnerships to work well. She added that the National Patient Advocate Foundation recently developed a coalition to explore potential opportunities for transportation partnerships. She encouraged “looking outside of our own community for where we could find likely partners to solve this issue.” She added that telemedicine initiatives may also help overcome transportation challenges for some types of cancer care. Steinberg suggested that new payment models for health care, such as bundled payments, allow for innovative delivery of services, and could include transportation expenses in their design.
Villani said that transportation should be considered an essential element of a clinical trial, similar to the completion of imaging or the provision of a drug. Petrone noted that some pharmaceutical companies that are conducting clinical trials are trying to improve transportation access through innovative partnerships with ridesharing companies and by developing easy ways to reimburse patients’ transportation expenses. Trimble added that a University of Alabama at Birmingham clinical trial gave participants a voucher to fill their gas tanks at the university gas station when they visited for medical appointments. “This worked well and aided retention of the patient volunteers,” he said.
Increasing Access to Clinical Trials in Low-Resource Areas
Several speakers said that although clinical trials are used to establish guidelines for cancer treatment, clinical trial participants often are not representative of the populations who receive cancer therapies. Shulman said that few patients with cancer participate in clinical trials, and trial participants tend to be healthier and less diverse. Clinical
trial results may also not be representative of countries with different population subgroups because cancers can have different genomic features, and people may have differences in genetic makeup that affects drug metabolism and response to therapy. “I do not think you could make assumptions that what worked in a general population in Harlem might work in Rwanda or somewhere else, because there may be real biologic reasons for things to turn out differently. . . . We cannot assume there is homogeneity in any of these areas, either biologically or culturally,” Shulman said (see Box 9).
Consequently, a number of groups have been working to increase access to clinical trials so that the trial results are more representative of the diverse populations found throughout the world, several speakers said. Petrone noted that traditionally a clinical trial is conducted at a fixed number of sites at major academic medical centers or large community practices. Ochoa agreed, and added that clinicians in these sites have access to innovative diagnostics and therapies, and that community oncologists typically do not have the expertise or the resources to offer these options in their own practices. Instead, community oncologists can refer their patients to an academic center or to an NCI-designated cancer center to participate in clinical research.
However, patients from rural areas or small community practices may not opt to participate in clinical trials, because they may need to travel long distances numerous times over the course of the trial. Royce agreed, and noted that some patients would have to travel hundreds of miles to be part of a clinical trial in New Mexico. “If patients have to leave their families, that is not just a financial burden, but an emotional burden to access a clinical trial,” she said.
However, Ochoa noted that community oncologists are very interested in providing their patients with access to clinical trials in the community setting. He reported on the impact of a grant from the NCI Community Oncology Research Program (NCORP). The program has increased the number of cancer patients participating in clinical trials in mostly low-resource settings in the Gulf region of the United States, which has one of the highest cancer mortality rates (see Box 10). Royce added that the New Mexico Cancer Care Alliance was established to increase access to clinical trials throughout the state (see Box 11).
Petrone added that Novartis has made efforts to improve access to their clinical trials by partnering with community physicians who have eligible patients. To encourage participation from a broader array
of community cancer practices, Novartis has established a hotline for research-qualified clinicians in order to rapidly enroll their patients in several Novartis-sponsored clinical trials within their practice. “We have been testing this model for a while and it has been very successful. We have absolutely broadened our reach,” Petrone said. She added that Novartis is trying to develop a program in which they can partner research-qualified clinicians with those who are not in order to enroll eligible patients and continue to expand access to clinical trials in the community.
Examples of Benefits and Lessons Learned from Partnerships
A number of speakers involved in partnerships to improve access and quality of cancer care in low-resource areas shared lessons they had learned from these experiences, such as the need to
- Assess community readiness and identify champions (Cleary, Milner, Ochoa, Schmeler, Vikram);
- Ensure commitment and sustainability (Grubbs, Milner, Schmeler);
- Collect data on outcomes (Milner);
- Respect and address cultural differences (Adams-Campbell, Meneses, Olopade, Royce);
- Build workforce capacity and training (Milner); and
- Encourage mutually beneficial partnerships (Anderson, Darien, Davis, Larson, Milner, Ochoa).
Barton noted that one overarching lesson learned is the need for improved understanding of how partnerships align with other efforts,
and suggested that efforts to improve cancer care in low-resource areas be better coordinated. “We have an enormous number of people doing very different things all around the world, and we really need to coordinate that effort and use it strategically,” Barton said.
Community Readiness, Ownership, and Champions
Several participants stressed the importance of assessing the readiness of communities to partner and engaging with community champions in these efforts. Milner said that he has used a detailed questionnaire to help assess readiness for a pathology laboratory partnership with facilities in other countries. This questionnaire is filled out by the Min-
istry of Health as well as the local site, and provides critical information that helps the partners collaborate and decide where resources could be best allocated, Milner said.
Ochoa stressed that a sense of ownership of the partnerships by everyone involved is critical, including ownership of the positive results by community partners in low-resource areas. “We have to let [care providers] shine in their communities and medical groups and nationally, so they have incentives to do this work,” he said. Ownership by the patients in the community is also key, Ochoa added. “The community needs to make decisions on how they can support and participate in research,” he said.
Part of engaging the community is determining who might be an
effective advocate or champion of the program, Schmeler said, and noted that the First Lady of Mozambique and other first ladies “have done a great job in bringing cervical cancer and breast cancer to the attention of various ministries in Africa.” Without such champions, there would have been less motivation to participate in cancer programs in their countries, Schmeler said. Kaur added, “We have to have the motivation and people who believe in what we are doing—champions who say ‘I think I can do that or I think I can learn how to do that.’”
Bhadrasain Vikram, chief of the NCI Clinical Radiation Oncology Branch, noted that progress in cancer care sometimes follows a high-profile individual’s personal experiences with cancer. He suggested that these individuals could serve as champions and help to push for further progress in improving cancer care. For example, he noted that the Cancer Moonshot was proposed after Vice President Joseph Biden’s son died from cancer.
Sustainable Support and Commitment
Grubbs stressed that a key to successful partnerships is a focused commitment by all parties, including government, health care providers, insurers, and advocacy groups. He added that strong support from the governor of Delaware was essential in the state’s efforts to address high colorectal cancer rates in the state and disparities in outcomes (see Box 12). “It really requires a commitment by all the parties to eliminate this disparity [in colorectal cancer mortality]. When everybody was going in the same direction, we were able to accomplish this,” he said.
Milner suggested that collaboration with Ministries of Health is needed to ensure there is a national cancer plan in place and that this plan, and the program one is trying to institute, will be feasible. Schmeler agreed and added “if cancer is not on the agenda of the Ministries of Health wherever we are working, then that is a problem.” She said that she and her colleagues participate actively in cancer control planning by working with Ministries of Health and the NCI Center for Global Health to assist countries in the development of cancer control plans. Milner said that in order to have successful pathology partnerships, countries receiving services need to be committed to the collaboration, and they also need a functioning, self-sustaining laboratory that has permanent, highly skilled pathologists. “If you do not have all those things, the partnership will be doomed to fail as soon as the partner
leaves,” he said. Only when those essential elements are in place should the network of partners be expanded, he said.
Grubbs said he had to lobby the state legislature to continue funding the Delaware colorectal cancer screening and treatment program, but because he was able to show that in the long term the program saves the state money, the state continues to fund it. He calculated that detection of colorectal cancer at earlier stages of the disease can avoid the need for chemotherapy and save program costs. “If we use our resources and develop our systems properly, we can afford to do this,” Grubbs said. However, “once you have achieved what you want to achieve, continuing to sustain it requires a lot of effort.” In recent years, Grubbs noted that colorectal cancer screening rates among African Americans have begun
to decrease in Delaware again. He attributed this decrease to budget cuts that eliminated marketing and outreach for this program.
Milner agreed that funding is critical for sustainability, but added that “what is really crucial is that you know where and when you are going to spend those dollars. Even if someone said tomorrow, ‘here is a check for $35 million,’ that would not help me because I need to have partnerships, collaborations, and agreements in place to take these things forward.”
Data on Outcomes
Milner and others stressed the importance of collecting data to evaluate the impact of partnership programs (see also section on Col-
lecting and Using Evidence to Support Policy Changes). Data such as morbidity and mortality statistics are key to persuading governments and agencies to support the continuation of effective programs, Milner said. He added that partnerships need built-in mechanisms for quality assurance and quality improvement efforts. “The lab has to run just [as effectively as] a lab in the United States and if you do not have these metrics, then you do not know if you are [providing] the highest-quality care,” Milner said. Shulman also stressed the importance of data collection and measuring outcomes of care. “You have to know exactly how many patients are living and dying . . . and whether there are things you can do to improve the outcomes,” he said.
Respecting Culture
Several speakers discussed the importance of respecting cultural differences and beliefs. Meneses said that her experiences in low-income areas in the southern United States have highlighted the need to address social stigmas and beliefs about cancer, including fear, denial, and fatalism. For example, she has worked with a community to establish a cancer support group that purposely did not include the word cancer in the title. “There was a lot of silence in regard to talking about one’s cancer and cancer treatment,” she said.
Adams-Campbell stressed the importance of using peers in cancer interventions. She said participants appreciate the involvement of fellow breast cancer survivors as coaches in a survivorship program; these peers can encourage each other to increase their physical activity and eat more healthy foods, for example. She also said programs should be tailored to community needs, including functional assessment forms. For example, a form that asked patients how many blocks they walk, how often they play tennis or racquetball, or how many stairs they climb a day was inappropriate for rural communities in Nigeria, in which there were no city blocks, most houses were one story, and no one plays tennis or racquetball.
“Understanding the places that you are going to work is very important, and [so is] recognizing that the population” may be different than your own, Adams-Campbell said. Similarly, Olopade noted mismatches that occur when programs are delivered to low-resource areas, pointing out one program in which mammogram vans were delivered to rural
parts of Uganda that lacked reliable roads and other infrastructure that were needed to use them.
Adams-Campbell also stressed that researchers studying survivorship care should understand the dynamics of the population they wish to study and design clinical trials that suit the population’s needs. For example, she noted some populations prefer to exercise in group settings, while others prefer to do their exercise at home. When designing clinical trials on exercise, she suggested soliciting community preferences in order to offer interventions that people in a given community are more likely to choose. She also noted the importance of offering a menu of lifestyle interventions and clinical trials so if they are not eligible or interested in one, they can find another one in which they can participate. “That is really important [to] get people motivated and interested to do things,” Adams-Campbell said.
She added that when developing survivorship programs for low-income African Americans, she conducted many focus groups to decide what types of physical activities they were most likely to undertake. “You have to pick things that are appropriate and important to the community, otherwise you do not get the buy-in to the program. We do not want to design studies that no one is going to participate in,” she stressed. The materials offered in programs also have to be sensitive to the communities they target, Adams-Campbell added, noting that for an exercise program brochure, she originally included photographs of fit individuals running in workout gear, but her community advisors pointed out that the people in the photos did not resemble the people in the communities where she wanted to recruit. “It is important to have your pulse on the community and make certain the community keeps the reins on you so that you will be in the right direction at all times,” she said. For another exercise program for breast cancer patients receiving radiation treatment, Adams-Campbell provided an exercise apparatus that enabled women to peddle while sitting in a chair for 15 minutes at the hospital either before or after their radiation treatment (Dash et al., 2016).
Royce also suggested being flexible, emphasizing that “when you have statewide clinical trials, one size does not fit all.” Meneses added that she found it important to adapt survivorship programs so they are more tailored to meet community needs. She noted that a program sponsored by the NCI called Research-tested Intervention Programs has a searchable database of evidence-based cancer control programs designed to provide
health care professionals easy access to research-tested materials and also provide guidelines for selecting and adapting the programs for use in different care settings (NCI, 2017b). “The focus should really be on what is going to work best for your community and how it needs to be customized,” Meneses said.
For a breast cancer survivorship program in Florida, for example, she tailored an intervention originally designed for an urban cancer center to better meet the needs of a rural, Spanish-speaking community. For another program offered to a predominantly Latina community of breast cancer survivors, Meneses added educational resources on how to address the needs of their children and spouses after having conversations with this population about what their needs were.
Royce stressed the importance of communication in partnerships, including relationship management and the establishment of shared expectations to provide clarity when the complexity of a partnership increases and problems occur. “It is very important to communicate what the tasks and expectations are so that there are no problems,” she said.
Building Capacity and Training
Successful partnerships also require training, Milner stressed. Visiting pathologists can help relieve the backlog of slides that need to be reviewed in low-resource facilities, as well as help train clinicians, but Milner stressed that these are temporary efforts, and a plan is needed for the laboratory’s sustainability. “You have to have a bridge so they can get to the other side,” he said. “If you are not training people or building resources and capacity, then the volunteers are really wasting their time,” Milner said. Building that capacity requires funding, so “fundraising is really important to make this successful,” Milner said. He added that the international pathology collaboration projects in which he has been involved have been enhanced when oncologists and surgeons also have participated.
Mutually Beneficial Partnerships
Milner noted that it is important for partnerships to be mutually beneficial to all parties involved. For example, partners who are on the receiving side benefit by having accurate, timely diagnoses that can
enable staging and appropriate treatment. But he added that participating pathologists providing their services also benefit because they have access to a wider range of challenging diagnostic situations that they may normally not encounter. “It is really great for residents and we improve our own diagnostic processes,” he said. Darien added that “one of the deepest relationships I formed was with a breast cancer survivor from Uganda. We helped her develop patient advocacy in Uganda and she helped us to understand what the issues were across the world.”
Ochoa noted partnerships have to be win–win collaborations to be sustained. “It cannot be ‘you send me your patient, I will treat them.’ Or ‘I am going to teach you how to treat your patient’ because then it is not a win–win, but paternalistic. It has to be a win–win situation to work, not only with our doctors but within our communities, too,” he said.
Anderson echoed Ochoa by adding, “We should be able to take what we learn in other places and bring it home. We typically go in paternalistically and say ‘good news, we are here to help you’ and we forget to find out what countries are actually doing to make things work. Navigation is a great example of something that crosses over to all countries. We should maybe be paying for this in the U.S., because it would have measurable outcomes. We have to learn from our partners.”
Davis agreed, noting “there are many things that need to be figured out that can translate to other places. We are using a lot of the lessons learned globally and applying them to our work with the Navajo and in South Dakota. Bidirectionality is key. We have learned how to deliver care well with very few resources that we can apply to sites here. Viewing everything as a global problem seems the best way we could all win in trying to figure out the best way that we can provide care, including simplifying the care we provide.”
Steinberg added that HRSA has established an Office of Global Health in recognition that U.S. and international partners each have something to gain from collaborating in cross-cultural partnerships targeting low-resource areas. In addition, HRSA is sending personnel from its Bureau of Primary Health Care and other offices to community health centers in South Africa, and has held meetings to determine how the agency can bring international lessons learned back to the United States.
Technology-Based Approaches to Cancer Care Delivery
Several participants suggested several technology-based solutions for providing cancer care in low-resource areas, including telemedicine approaches such as telepathology and telementoring, as well as the use of resource-appropriate technologies.
Telemedicine
Shulman noted that the current demand for cancer care in the world greatly outstrips the supply of medical oncologists, and said that estimates suggest that it will likely be three to four decades until there will be enough medical oncologists to treat all the cancer patients in the world. To help meet the demand for cancer care, he suggested having medical oncologists available to work part-time on the ground in low-resource areas who are supported remotely by oncologists at academic centers. This is similar to the PIH program in Rwanda in which he is involved. As mentioned previously, Schmeler discussed the use of telementoring to improve access to cancer care, as well as to build workforce capacity and expertise in a low-resource settings. Barton added that “a lot can be gained by shifting out much of the quality components of cancer care, particularly of radiotherapy, so that they are done remotely. This will increase safety, reduce costs, and generate more expertise.”
Milner reported on the White House Office of Science and Technology Policy’s call to action to improve access to pathology services in low- and middle-income countries.20 In response, the American Society for Clinical Pathology (ASCP) partnered with a number of organizations to establish a cancer diagnostics and treatment program in Africa that relies on telepathology (ASCP, 2017). For this project, pathologists from the United States are connected virtually to sites in different parts of Africa to provide diagnostic consultations and second opinions in real-time to local clinicians in Africa. Various companies in Africa provide the telecommunications technology, histology equipment, and immunochemistry technology.
___________________
20 See https://obamawhitehouse.archives.gov/blog/2015/10/26/cancer-diagnostics-developing-world (accessed April 4, 2017).
Resource-Appropriate Technologies
There was discussion among workshop speakers about adapting cancer treatment strategies to make them easier to implement and use in low-resource areas. For radiation therapy, Barton suggested using innovative particle accelerators that are less expensive and easier to maintain. Jaffray agreed, adding that at a recent meeting of the European Council for Nuclear Research, experts discussed making a linear accelerator that was more adaptable and accessible for low- and middle-income countries. He noted that solar technology could also be used to power radiation therapy accelerators. Schmeler reported that a bioengineer at Rice University, Rebecca Richards-Kortum, has a team of faculty and students focused on developing affordable technologies for solving problems in the delivery of medical care in low- and middle-income countries. For example, there has been a large turnover of nurses providing chemotherapy in Mozambique because they were being exposed to the drugs and lacked personal protective equipment. The Rice University bioengineering team is developing a device that can decrease the aerosolization of chemotherapy drugs and other substances that present health hazards, she noted. Some countries also lack devices that can prevent blood clots known as deep vein thrombosis, which are common and life threatening in many patients being treated for cancer. For example, Malawi is unable to afford the automated compression devices used in hospitals in high-resource areas to prevent these blood clots. The Rice bioengineering team, consequently, is now developing a low-cost compression device for this purpose.
Milner said researchers are trying to develop easier-to-use rapid diagnostic tests using the polymerase chain reaction to analyze fresh tissue biopsies for hormone receptor and oncogene status, in hopes that this technology could eventually replace the more traditional immunohistochemistry testing. Milner also reported on research conducted in a PIH facility in collaboration with Brigham and Women’s Hospital to determine how many immunohistochemical markers are needed to adequately analyze and classify hematopathology samples, in order to conserve resources. The researchers found that although pathologists in high-resource areas tend to use 15 to 20 stains, hematopathology
samples for specific histological patterns could be adequately classified using just 6 of the stains.21
McCullough also noted that for most transfusions in sub-Saharan Africa, whole blood can be used instead of packed red cells derived from whole blood. “Folks often feel guilty that they are not making more packed cells like they do in Western Europe and the United States. But it is expensive and many of their transfusions could be done [safely using] whole blood,” he said.
Schmeler reported on innovative and affordable technologies for cervical cancer diagnosis and treatment planning that can be used in low-resource areas. She noted that a mobile colposcope has the ability to capture photographs and patient data and then upload this data to a secure website. The colposcope could be used by health care workers in the field, and clinicians in another location can review the data and make recommendations regarding the diagnosis and treatment strategy.
Anderson added that better technologies are needed to replace the expensive intravenous (IV) technologies currently used for chemotherapy administration. “What about IV systems that do not depend on electricity? We would benefit a lot if we could come up with some inexpensive ways of doing what we currently do,” he said.
Several speakers suggested that simple solutions can often be found by thinking outside the box and using resources at hand. For example, McCullough reported that one clinician substituted vodka for rubbing alcohol as a fixative for blood smears when supplies of rubbing alcohol ran out at his facility in Uganda. He suggested that companies continue to develop and refine methods for assessing blood type and safety, to improve simplicity, quality, and cost. McCullough noted, however, that there is little commercial incentive to develop these tests, even though they are critical to improving the availability and safety of blood transfusions in low-resource areas. Shulman suggested that drones may be one way to overcome transportation barriers in remote areas to improve access to blood products. Olopade suggested clinicians could also use drones to deliver medicines to remote areas. “Technology can help us solve these problems,” she stressed.
Jaffray suggested using software systems that automate radiotherapy treatment planning. Such systems have been shown to improve the quality of radiation therapy treatment planning for breast cancer, while
___________________
21 Personal communication, Elizabeth Morgan, Brigham and Women’s Hospital.
also cutting the time required for treatment planning from 4 hours to 7 minutes (Purdie et al., 2011). In Canada, he noted that clinicians are increasingly given more work to do with no increase in budget. Thus, “digital technologies, efficiencies, workflow, and simplicity are the only ways we are going to afford [our health care],” he said, noting this is true of people practicing medicine in both high- and low-resource areas.
Guidelines and Standards for Cancer Care
Several speakers discussed the importance of adopting resource-stratified guidelines for cancer care, identifying essential medicines for cancer treatment, and defining standards for nursing care. “If we want to have the biggest effect on worldwide cancer mortality, we need to figure out how to safely and effectively bring the tools that we have today to the millions of people who do not have access to those tools,” Shulman said.
Resource-Stratified Guidelines for Cancer Care
Anderson said that many guidelines for cancer care were developed in high-income countries and are often inappropriate for many countries because they assume availability of resources that low- and middle-income countries may lack. Recognizing this, the Breast Health Global Initiative developed resource-stratified guidelines for breast cancer care by ranking interventions according to the impact they have, and prioritizing interventions based on that impact (Anderson et al., 2008).22 Some interventions, such as breast cancer surgery, were ranked as basic or fundamental services that are needed for any breast health care system to function effectively. Limited-level, or second tier resources, were those that would make significant improvements in mortality, and many cancer drug therapies would be considered limited-level resources, Anderson said. Enhanced-level (or third tier) resources include services that are optional but important because they increase the number and quality of therapeutic options available and enable patient-centered decision making, such as lumpectomy followed by radiation instead of mastectomy. Anderson said that maximal-level resources are the highest level of resources or services available and have lower priority in
___________________
22 The Breast Global Health Initiative has also developed resource-stratified guidelines for palliative and survivorship care for patients with breast cancer (Distelhorst et al., 2015).
low-resource areas due to extreme costs and/or lack of feasibility. For example, Anderson said that magnetic resonance imaging and positron emission tomography may fall in this category, because they can be used to provide a better imaging for treatment monitoring or surveillance, but these technologies do not treat the disease.
Anderson said that resource-stratified guidelines should not be viewed as a way to certify substandard care. “It is more about how do you build the system, particularly when you do not have one—where is the foundation, where is the first floor, where is the second floor? Because without that type of prioritization, you are not going to make systems function well,” he said. Building on this work, other groups have also begun to stratify and prioritize guidelines for cancer treatment for a variety of diseases, including NCCN, ASCO, and the WHO, Anderson reported. For example, NCCN’s 2015 guidelines for treatment of cervical cancer are stratified into maximal, enhanced, limited, and basic levels (NCCN, 2017).
Anderson added that referral systems and centralization of high-end diagnostics and treatments are especially important in low-resource areas. “We have to think out of the box to develop nationalized strategies that are functional. It is not just the cancer center, it is how the patients get to the cancer center that is equally important,” he said. Anderson pointed out that clinicians may have to rely on different diagnostic strategies and technologies in low-resource areas, especially when it is difficult for people to return for treatment or when diagnostics are limited. He reported on a triage protocol in Peru in which women do not undergo screening with mammography, but instead receive clinical breast examinations. If clinicians detect a mass on the breast exam, the tumor is biopsied using fine-needle aspiration. If a biopsy is positive or suspicious, then women will be sent to a regional hospital for more extensive evaluation and potential treatment.
Essential Medicines and Priority Medical Devices
Shulman said that the WHO has developed an Essential Medicines List for cancer treatment in order to provide public sector officials with information on medicines that are essential to cancer control planning. “The list helps governments and ministries decide what to purchase for their countries,” Shulman noted. The WHO Essential Medicines List specifies which cancers the medicines are used to treat, dosing and
scheduling information, and toxicity and efficacy information. Opioid pain medicines are also included on the Essential Medicines List (see Box 13). Shulman stressed that a drug’s inclusion on the WHO Essential Medicines List does not necessarily meant that a drug will be available to a patient. He noted that in 2013, the WHO listed 30 drugs as essential cancer medicines. However, a 2015 survey of 135 countries with a percapita gross national income of less than $25,000 found that no country provided access to all 30 drugs, and many countries provided less than half of the drugs listed (Robertson et al., 2016) (see Table 2).23
In 2014, the Union for International Cancer Control (UICC) responded to the WHO invitation to convene a team charged with creating a new framework for evaluation of cancer drugs included on the Essential Medicines List. More than 90 international volunteers participated, including Core Task Team members from UICC, the NCI, the European Society for Medical Oncology, ASCO, Societe Internationale d’Oncologie Pediatrique, Dana-Farber Cancer Institute, and NCCN International. The group proposed that the Essential Medicines List for cancer be expanded from 30 drugs to 52 drugs, Shulman reported. Based on this input, in 2015 the WHO approved the inclusion of 16 new cancer drugs on the Essential Medicines List and denied inclusion of 6 drugs.24 Review of the Essential Medicines List for cancer is currently being updated for 2016-2017, and Shulman said additional drugs have been recommended for inclusion, such as targeted therapies for non-small cell lung cancer (with associated diagnostic testing), tyrosine kinase inhibitors for CML after disease progression on imatinib, and bisphosphonates for malignant bone disease. The WHO has yet to determine if these recommendations will lead to the addition of these medications to the Essential Medicines List.
In addition to increasing access to cancer therapies in low-resource settings, Shulman said that another goal of the Essential Medicines List is to apply pressure to lower the cost of the drugs included on the list, but this effect has not yet been seen. Royce asked if biosimilars might create enough competition to reduce the cost of cancer drugs. Shulman
___________________
23 Shulman noted that the WHO is in the process of developing a list of priority medical devices to diagnose, treat, and manage cancer (WHO, 2017). The list of devices will focus on leukemia, cervical, breast, prostate, lung, and colorectal cancers across the continuum of cancer care.
24 See http://www.who.int/bulletin/volumes/94/10/BLT-15-163998-table-T1.html (accessed March 27, 2017).
responded that there is a biosimilar to trastuzumab that demonstrated equivalent efficacy and safety to trastuzumab (Rugo et al., 2016). This drug may be sold at one-third the price of the U.S. cost for trastuzumab, but he noted that even at that price it will be unaffordable for countries like Haiti or Rwanda. Shulman said that even if the cost of trastuzumab were reduced by 90 percent, it would still cost around $4,000 and be a very expensive medicine for very low-income countries, though it would become much more affordable in middle-income countries. “I have not seen examples that show me biosimilars are going to be widely affordable in a lot of the world,” Shulman said. Shulman added that
some drugs, such as luteinizing hormone-releasing hormone agonists, have been around for more than 30 years and although they are made by multiple companies, they are still extraordinarily expensive given the costs of producing them, and therefore unavailable to many in the developing world.
Barton asked how countries can be assured that generic drugs and biosimilars “are actually what they say they are, and are going to do what they say they will do?” He noted that Australia’s Therapeutic Goods Administration rejects about two-thirds of generic drugs that they test. Shulman responded that this is a valid worry worldwide and suggested
TABLE 2 Availability of Essential Cancer Medicines Listed by the WHO, by Regions
| WHO Region (number of countries) | Median # of Listed Medicines Available (minimum, maximum) | ||
|---|---|---|---|
| Medicines in the WHO EML 2013 (30 medicines) | Medicines Added in 2015 (16 medicines) | Medicines Not Added in 2015 (6 medicines) | |
| Overall (n = 135) | 17 (0, 25) | 3 (0, 15) | 0 (0, 4) |
| Africa (n = 37) | 13 (1, 23) | 1 (0, 14) | 0 (0, 1) |
| Americas* (n = 29) | 19 (3, 25) | 6 (0, 15) | 0 (0, 4) |
| Eastern Mediterranean (n = 14) | 23.5 (0, 25) | 6.5 (0, 15) | 0 (0, 4) |
| Europe (n = 26) | 18.5 (1, 25) | 10 (0, 15) | 0 (0, 4) |
| Southeast Asia (n = 11) | 21 (2, 24) | 1 (0, 13) | 0 (0, 0) |
| Western Pacific (n = 18) | 7 (0, 25) | 0.5 (0, 15) | 0 (0, 2) |
| Western Pacific** (n = 9) | 19 (9, 25) | 2 (1, 15) | 0 (0, 2) |
NOTE: EML = Essential Medicines List; WHO = World Health Organization.
* Does not include the United States.
** Excluding nine Pacific Island countries: Cook Islands, Kiribati, Marshall Islands, Nauru, Niue, Palau, Tonga, Tuvalu, and Vanuatu.
SOURCES: Shulman presentation, November 16, 2016; Robertson, J., R. Barr, L. N. Shulman, G. B. Forted, and N. Magrinid. Essential medicines for cancer: WHO recommendations and national priorities. BullWorld Health Organization 2016; 94 (10). 10.2471/BLT.15.163998. License: Creative Commons BY 3.0 IGO.
“it would be great if there was a worldwide clearinghouse for generic drugs.”
Turkan Gardenier, director of research at Pragmatica Corporation, asked if there were any planned efforts to provide access to immunotherapies in low-resource countries. Shulman said that these cancer treatments were introduced only recently in the United States and other high-resource countries, and that clinicians are still experiencing a learning curve on how best to use them, monitor response, and manage toxicities, and did not think that immunotherapies will likely be used extensively in low- and middle-income countries unless there was some way of addressing their extremely high cost. However, he noted that
some pharmaceutical companies have expressed an interest in testing immunotherapies in resource-limited settings.
Julia Rowland, director of the NCI Office of Cancer Survivorship, noted that in the past, the United States tended to aggressively pursue cancer treatments that extend life without adequate consideration of quality-of-life issues for patients with cancer. “We have this unique opportunity in time not to make that same mistake globally. . . . That is going to mean incorporating quality of life concerns right from the start. If we are going to increase the kinds of treatment we deliver, they have to be tied with good quality-of-life outcomes,” Rowland said. Bakitas agreed that “globally the focus on improving quality-of-life outcomes needs to be the primary goal and at the forefront of concern, not just for the patient, but for their family caregiver as well.”
Nursing Standards
Day stressed that a lack of high-quality nursing care is a major impediment to successful pediatric cancer treatment in low-income countries and contributes to low childhood cancer survival rates. There are numerous challenges to providing pediatric oncology nursing care in low-resource areas, including inadequate staffing, a lack of training, and limited equipment. She noted that the staffing ratios seen in hospitals in low-income countries may be as high as 15-30 pediatric patients per nurse. “If nurses have too many patients, they do not have the time to assess patients thoroughly and pick up when a patient’s condition is starting to deteriorate. If you do not get at that window of opportunity, you [can] have bad outcomes,” Day said.
She added that nurses might not receive specialized training in pediatric oncology, despite the high level of skills needed to provide care for these patients. This can be especially problematic if there is no physician available on nights or weekends, and nurses have to make high-level decisions without adequate consultation with physicians, Day reported. “Overall you have nurses who are without resources and lack preparation, yet they have more responsibility than nurses in high-income countries,” Day said.
Day reported that a study in Guatemala showed that there was a significant decrease in treatment abandonment when a national pediatric oncology unit adopted quality standards for nursing care, adequate staffing rates, and improved education for nurses (Day et al., 2013). In
addition, adequate nurse staffing contributes to shorter hospital stays, fewer complications, and lower mortality rates, while improved nursing education contributes to improved patient outcomes, including reductions in mortality (Estabrooks et al., 2005). In light of this research, Day said that the International Society of Pediatric Oncology developed baseline standards for pediatric oncology nursing (Day et al., 2014) (see Box 14).
These standards focus on staffing, communication, education and training, and safety equipment and supplies. She noted that officials from low-resource areas may believe they cannot afford to maintain these standards, but she countered “that with these patients, as sick as they are, not having some sort of basic standards in providing their care is unethical.” She added that adoption of some of the nursing standards could be done inexpensively.
Several international groups have endorsed these standards, including Childhood Cancer International, the Pakistan Society of Pediatric Oncology, World Child Cancer, and the Irish Cancer Society, Day reported. She and her colleagues are currently developing an instrument to assess how well the standards are being followed at various facilities. Day said that assessment can facilitate the development of national or institutional cancer plans. “It will be a very organized and specific way to show that if you invest this much money, make these changes, and increase your score, your quality of nursing will impact outcomes by this much,” she said, adding, “We want these standards to influence health policy decisions and help improve and support nursing. Nursing is a very important component and it is one of the least expensive things to fix.”
John Gardenier, a workshop participant, asked whether magnet hospital certification in the United States25 could be used in other countries. Day responded that some low- and middle-income countries have used a certification process similar to magnet status, called Joint Commission International Certification, for which they have to reach many of the baseline standards specified in the magnet certification process.
Prioritizing Funding for Cancer Care in Low-Resource Areas
A number of workshop participants noted that the burden of noncommunicable diseases (NCDs)—including cancer—in low- and middle-income countries exceeds the burden from communicable diseases (Lozano et al., 2012). At the same time, NCDs receive a disproportionately low investment of health spending globally (Gostin, 2014). Rifat Atun, professor of global health systems at the Harvard University
___________________
25 Magnet status is an award given by the American Nurses’ Credentialing Center, an affiliate of the American Nurses Association, to hospitals that satisfy a set of criteria designed to measure the strength and quality of their nursing (American Nurses Credentialing Center, 2017).
T.H. Chan School of Public Health, described what he called the 5/80 cancer disequilibrium: estimates suggest that only 5 percent of global resources for cancer are spent in low- and middle-income countries, even though these countries account for approximately 80 percent of the disability-adjusted life-years lost to cancer worldwide (Farmer et al., 2010). “There is a huge gap in terms of what is needed and what has been provided,” Atun said, adding that part of the funding gap is due to a lack of awareness, because NCDs, such as cancer, “are not on the radar screens of policy makers. People still think cancer is a problem of the developed world.” Stigma, poverty, and health system infrastructures that are ill-equipped to manage chronic conditions also contribute to the cancer burden in low- and middle-income countries, he said. Due to the lack of awareness of the burden of cancer in low-resource areas, in addition to the severity of the problem, Atun emphasized that the cancer community needs to call attention to the urgency of addressing the global cancer burden (see Box 15).
Atun noted that there is limited information on how much international financing is devoted to cancer, as well as what countries allocate domestically for cancer care. However, estimates suggest that over a 25-year period, approximately $6 billion was spent for all NCDs, including cancer, Atun said.26 “This is unacceptably low and something needs to be done,” he stressed. “There is a compelling case for developing a global funding mechanism for cancer. Unless we respond today, there is going to be a tsunami of [cancer] cases going forward with [health] systems that are not able to respond,” Atun said.
Eduardo Cazap, president of the Latinamerican & Caribbean Society of Medical Oncology, stressed that improving investments for cancer care in low-resource areas is not solely a question of money, but how that money is allocated. He noted that some low- and middle-income countries—including Costa Rica, Morocco, Singapore, and Uruguay—have developed good cancer control plans based on properly allocating existing resources. He added that some high-income countries have implemented the latest innovations in cancer care, but because of inadequate workforce capacity and training, these countries have not achieved better cancer outcomes with these investments. Olopade suggested that more international and domestic efforts focus on improved health care resource allocation and capacity building, as well as more transnational and international collaborative research activities.
Potential Funding Opportunities for Cancer Care
Atun discussed five opportunities for increasing funding for cancer care:
- Economic growth that creates a broader tax base and greater revenue for governments to allocate to cancer care;
- Reprioritization of health, especially cancer care, in government budgets;
- International borrowing of funds (or international development assistance);
- Innovative domestic or international financing; and
- Effective budget allocation and improving health systems efficiencies.
___________________
26 See http://vizhub.healthdata.org/fgh (accessed March 27, 2017).
Countries could enhance their sources of tax revenues by introducing tobacco, alcohol, or other taxes, but Atun noted these taxes may be challenging to achieve because of political opposition or difficulties in collecting these taxes once implemented. Atun added that countries have limited opportunities for raising tax revenues, particularly after the most recent economic crisis. He pointed out that the proportion of low-income developing countries with a negative primary balance gap (or rising debt) has increased since 2008; in 2014, the International Monetary Fund staff estimated that 21 of 39 low-income developing countries had rising debt. Atun added that a number of countries are already in debt because they borrowed funds to combat HIV/AIDS (human immunodeficiency virus/acquired immunodeficiency syndrome). “The economies in these countries are growing, but they are not strong and their ability to borrow is low, [since] they have future obligations,” Atun said.
Another challenge is that funding from international sources—donor assistance for health—has not increased since the economic crisis in 2008, Atun said. “There is limited funding for scaling up existing programs such as HIV, tuberculosis (TB), malaria, and child health that need to be sustained, let alone investing in new programs,” he said.
“To channel funding into new areas, one has to look for new innovative sources of financing,” Atun said, and suggested that innovative financing tools that mobilize, pool, channel, and allocate resources will be the primary mechanisms to address the global cancer burden. The Global Fund to Fight AIDS, Tuberculosis and Malaria, the Global Alliance for Vaccines and Immunization, and UNITAID are examples of innovative funding mechanisms, Atun said. He provided a number of examples27 of nontraditional fundraising strategies for health-related endeavors, including
- Solidarity levies on airline tickets used to finance funds for infectious diseases have raised approximately $2 billion between 2006 and 2015.
- The Children’s Investment Fund Foundation, which uses revenues generated from the income of a hedge fund to invest in health,
___________________
27 See http://www.undp.org/content/dam/undp/library/Poverty%20Reduction/Development%20Cooperation%20and%20Finance/InnovativeFinancing_Web%20ver.pdf (accessed April 3, 2017).
- nutrition, and climate change interventions. The Foundation raised approximately $2 billion from 2003 to 2013.
- Product (RED), in which a proportion of the profits from designated consumer products are contributed to the Global Fund.
- Debt2Health, a program in which creditor countries forgo the debt of countries that achieve targets related to health.
Atun noted that none of the funds raised by these mechanisms are allocated for cancer care. “There is a lot of work to be done on innovative financing mechanisms and tools for cancer,” he said. Innovative financial instruments include options such as social impact and development impact bonds, remittances and diaspora bonds, solidarity levies, and guarantees.28 He noted that many funding initiatives are not scaled up to global proportions. “From the beginning, one has to conceive this as an institutional entity that is going to reach global scale and be sustained,” Atun stressed.
Anderson asked what would be expected from countries receiving donations from a potential global fund for cancer (i.e., would they be expected to have or build the infrastructure needed to implement the funds properly?). He noted that New Guinea received $60 million in funding for AIDS, but they were not able to spend more than $20 million because they did not have the health services or infrastructure to use the money. Anderson added that corruption can also be a problem in low- and middle-income countries, with the risk that “the money donated goes somewhere else. So you have to have an effective system that can adequately deliver services if they are given resources,” Anderson said.
Atun responded that some funding sources, such as the Global Fund, require receiving governments to make contributions as a prerequisite of the funding, with the contribution increasing according to income level. The funding is then put toward financing a national program of HIV, TB, or malaria or for broader health system investments. He noted that when he was at the Global Fund, one-third of its investments went to funding health systems beyond those needed to scale up a response to HIV, TB, and malaria. “That is critically important,” he said.
___________________
28 See http://www.undp.org/content/dam/undp/library/Poverty%20Reduction/Development%20Cooperation%20and%20Finance/InnovativeFinancing_Web%20ver.pdf (accessed April 3, 2017).
Atun added that it is also important for countries to demonstrate how the funds will be used and what the expected results are, with funding based on performance. “It is not just sending money to countries,” he stressed. He noted that “to develop a global financing facility or a global fund for cancer, countries need to develop meaningful national cancer plans with clear targets and how they can be achieved. We need real plans that are going to show how much it is going to cost to establish a network of provider units to train people and to scale up. They need to be very realistic plans, which take time to develop, even when technical assistance is provided.”
Cazap added, “You need continuous monitoring of funds and reporting of outcomes, but that is something very unusual in many countries.” He noted that Argentina just passed a law that government agencies be transparent and provide information on how money they receive is allocated. He suggested that funders insist on implementation research methods for the planning of how funds will be allocated, as well as for assessing effectiveness of the funding on achieving outcomes. “If the money is not properly targeted, then there is the risk of it not being a good use of resources,” he said.
Allocating Resources for Cancer Prevention, Screening, and Treatment
A number of speakers, including Anderson, Atun, and Shulman, discussed the importance of funding a combination of cancer prevention, screening, and cancer treatment efforts in low-resource settings. However, speakers noted that this strategy has not been without controversy, as some have asserted thatcancer prevention and screening efforts may have a greater impact on reducing the burden of cancer and are more cost effective than cancer treatment in low-resource areas (Shastri and Shastri, 2014). However, Anderson said this is a false dichotomy, and suggested that low-resource areas need to address the whole continuum of cancer control. “Trying to look at therapy alone without thinking about early detection is like talking about one hand without talking about the other. This is a system and the two fit together inextricably. You have to look at both,” Anderson said.
Shulman added, “It is a false paradigm to talk about [cancer] prevention versus treatment. How many people here, if they had cancer, would go to their oncologist and say, ‘Well, I realize it is probably not a good way to spend our national resources, so do not give me that che-
motherapy and radiation that might actually have a chance of curing me.’? What we are really talking about is withholding treatment from the world’s poor. . . . We are talking about a lack of equity.” Cazap added that there is urgency to provide cancer treatment and pain relief now, because cancer prevention efforts take time.
“Just investing in prevention is not enough,” Atun said, adding, “Treatment has to be part of the picture, as well as palliative care. We cannot let people die in pain. This is not acceptable in the 21st century.” He added that there needs to be more discussion about the priorities of global cancer financing: “Do we invest on the basis of cost-effectiveness as a singular measure or do we focus on dignity as the primary factor, or maybe take into account equity considerations? There is no magic answer but this needs to be decided at both the country and global level.”
Potential Policy Strategies to Improve Prioritization of Cancer Care in Low-Resource Areas
In addition to discussions of funding efforts to address the global cancer burden, several speakers also suggested potential policy strategies that could be employed, including educating and advocating to policy makers to improve cancer care, using evidence to inform policy decisions, and highlighting successes to advance progress.
National and International Cancer Care Policy and Advocacy
Cazap said that international and national policies could be helpful in reducing the global burden of cancer. For example, international organizations, such as the WHO, the United Nations (UN), and the World Health Assembly, have recommended action plans for controlling cancer, Cazap said. However, he noted that these actions can be difficult to implement, because they are not binding legal requirements. As Atun mentioned previously, none of the Millennium Development Goals are tied to reducing the global cancer burden. Cazap also noted that the only globally agreed upon treaty aimed at cancer control is the Framework Convention on Tobacco Control. He asked how can we implement global actions if there is no global consensus. He noted that one alternative is to establish bilateral agreements aimed at controlling cancer within individual countries. But these efforts can be fragmented and poorly aligned Cazap said, noting one African country in which
more than 20 organizations created bilateral agreements for cancer, but the plans were all isolated from one another.
Cazap reiterated that there is a the need for improved structures and efficiencies in health care systems in low- and middle-income countries in order to effectively address the global burden of cancer. Cazap added that low- and middle-income countries can use national policy strategies, such as universal health care coverage and the development of cancer control plans to help address this need. Trimble reported on the International Cancer Control Partnership,29 which he described as a one-stop virtual shop for professionals in countries that are working to develop national cancer control plans. The website provides a searchable database of published national cancer control plans, a library of tools and materials for cancer planners, and information on worldwide case studies and best practices. “It can help professionals in countries that are both developing and implementing cancer control plans to actually talk to one another,” he said. Anderson agreed, and said that education materials—such as a guide to planning comprehensive breast cancer programs—can convey important knowledge about cancer to health care policy makers (Fred Hutchinson Cancer Research Center, 2017). “The people who make decisions about how health care resources are going to be administered generally are not people who are knowledgeable about cancer, and many are not medically trained,” Anderson said.
Cazap noted that relying on national plans and policies may be insufficient in many countries, because some governments may have poor accountability, inadequate monitoring, corruption challenges, and a lack of critical institutions.
To facilitate change, Cazap highlighted a suggestion from the World Oncology Forum—to apply public pressure to encourage government actions, including the creation of and adherence to national cancer control plans and international cooperation to address the global cancer burden (World Oncology Forum, 2013). Cazap suggested leveraging public awareness “that cancer is a problem that affects all of us.” He noted that public pressure from a civilian coalition prompted the Peruvian government to allocate revenue from its tobacco taxes to its budget for a national cancer institute and for cancer care. Cazap noted that “Cancer is not only a problem of doc-
___________________
29 See http://www.iccp-portal.org (accessed March 28, 2017).
tors and patients. We need to open our discussions to the civil society, politicians, lawyers, economists, media, and government.”
Milner added, “Strategy plus advocacy times publicity equals policy. After you know what you want to do and you are talking to the right people, you have to tout it as much as possible because that is what governments listen to and that is why they change policies.” Cazap agreed, suggesting that “political will and leadership [are] key component[s], and without [them], nothing will happen.”
Anderson suggested making global cancer surgery a higher priority in national cancer control plans. He added that The Lancet Oncology Commission on Global Cancer Surgery found a lack of investment in public surgical systems, low investment in research, and widespread gaps in training and education (Sullivan et al., 2015). “We need to be talking about it with the key opinion leaders, political leaders, and policy makers who have impact on these decisions because if we do not talk about it, it clearly is not going to happen,” he said. The Commission recommended that national cancer control plans include strengthening of surgical systems through investment in public-sector infrastructure, education, and training, Anderson reported (Sullivan et al., 2015).
Collecting and Using Evidence to Support Policy Changes
To convey the importance of prioritizing cancer control in global or national health care planning, Anderson suggested using compelling data that demonstrate the seriousness of the cancer burden as well as illustrating the effect of interventions on health outcomes and economic benefits. Anderson described the new Global Breast Health Analytics Map (GloBAM),30 which is an online tool that provides breast cancer statistics from individual countries and enables cross-country comparisons. In addition, he and his colleagues have developed situation analysis tools that use statistical modeling to estimate expected outcomes from different policy changes. With this tool “you could talk to policy makers and tell them that if they make this change, these are the sorts of outcomes they might anticipate,” Anderson said. He noted that this tool could illustrate the differences in health outcomes of various cancer screening and treatments strategies. For example, the modeling tool estimated the potential health impact of improving breast cancer
___________________
30 See http://globam.fredhutch.org (accessed March 28, 2017).
screening and the use of different treatment options for women with breast cancer (endocrine therapy alone versus endocrine therapy with chemotherapy) in Tanzania. Anderson also pointed out that in order for policy makers to improve cancer outcomes in their countries, data on outcomes need to be collected routinely, but this often is not done in low-resource countries.
Atun, Jaffray, and their colleagues have used data to make a business case for investing in radiotherapy for cancer treatment. Their analysis for the Commission found that the benefits of the therapy eventually outweigh the costs for middle-income countries in terms of full-income and human capital benefits, Atun reported (Atun et al., 2015). “Investing in radiotherapy for the top 10 cancer[s] is a good investment because not only does it produce good health, but economic benefits,” Atun said. He suggested conducting similar analyses for other cancers or other interventions. Jaffray agreed, adding, “We would love to [conduct this] analysis not just for radiotherapy, but for surgery and chemotherapy, including new emerging therapies, so we can understand the impact.” Jaffray added that data and modeling are also available to show how training clinicians to deliver radiotherapy results in an economic benefit to countries that invest in such training, which “opens up a conversation with the Minister of Finance as well as the Minister of Health.” Jaffray suggested that such investment modeling be used to compare competing health priorities and to guide future spending. “The investments that we make in the future should be very much driven by data,” he said.
Anderson also urged improved data collection in order to track outcomes once new policy initiatives are implemented. Trimble suggested that as countries develop their national cancer control plans, they should have access to technical assistance to make sure the plan is feasible and to build in monitoring and evaluation. “Just because something has worked in India does not mean it is necessarily going to work in Myanmar, and we think it is critical that as countries ramp up what they are doing, they evaluate it with the appropriate metrics,” Trimble said. Shulman suggested creating short-term goals and accountability for achieving them as part of national cancer control plans. “The most successful plan I saw had 12- and 24-month deliverables and accountability for trying to do what you promised you would do. You need to report back what the outcomes are,” he stressed. Trimble also said that a country can modify a program if the data show that it is not achieving the desired results.
Grubbs suggested that the evidence base for palliative care, which
demonstrates improved patient outcomes, be used to incentivize improved delivery of palliative care in low-resource areas. He noted that the United States is currently in a transformative time in health care in which alternative payment models tied to metrics are being examined, and palliative care could be an important measurement outcome. “What is going to make this [change] happen is that your payment will be dependent on providing this care and having measurements to show it worked properly,” Grubbs said.
Anderson said it is also worthwhile to conduct research on implementation strategies in real world settings. For example, a study on breast cancer screening practices in Colombia found that clinician education increased the number of women screened and lowered the stage of breast cancer diagnosis (Murillo et al., 2016). “This information is really relevant to health ministers trying to assess why they should put their funding in breast cancer screening as opposed to another program,” Anderson said.
Highlighting Success Stories
Cazap provided several examples of progress in countries that have made commitments to improving cancer care, and suggested that calling attention to these efforts is important for advancing further progress. For example, a pediatric oncology program in Nicaragua that involved improvements in clinician training and health system infrastructure increased childhood cancer survival rate from less than 20 percent to more than 60 percent (Masera et al., 1998). In Uruguay, where the president is a radiation oncologist, Cazap said the country has provided universal health coverage, including coverage of cancer prevention, and it is also the seventh country in the world to be designated smoke free.
Cazap also reported that advocacy by Princess Lalla Salma, the queen of Morocco, has been instrumental to a number of achievements in cancer control, including establishment of cervical and breast cancer screening, pediatric oncology, and tobacco control programs. Morocco has also created and equipped comprehensive cancer centers, trained practitioners, and developed a cancer registry. Cazap said this has been made possible through allocating 10 percent of its health care budget for cancer control. He added that the government is currently starting a program for universal health coverage.
Cazap noted that Princess Dina Mired of Jordan, who recently
became president-elect of UICC, was critical in improving Jordan’s cancer care infrastructure and served as the former director general of the King Hussein Cancer Center.
Cazap suggested duplicating these successful examples via collaborations and partnerships in which low-income countries exchange resources, technology, and knowledge. He also suggested more public–private partnerships. When countries do not have universal health care coverage, Trimble said there should be a partnership between private and public systems to provide and reimburse health care expenses. Trimble suggested using unique personal identifier numbers for patients so that records from public and private systems can be linked. “If India can give biometric identifiers to a billion people, then I think it should easily be done elsewhere, and we need to help countries figure out how to do that,” he said.
WRAP-UP
Richard Larson, director of the Hematologic Malignancies Clinical Research Program at The University of Chicago, re-emphasized the growing global burden of cancer. He said individuals have unmet cancer care needs not only in international low-resource areas, but also in areas of the United States. He added that there are unmet cancer care needs across all treatment modalities (surgery, radiation therapy, and drug therapy), as well as with palliative and survivorship care. In addition to resource constraints, other contributing factors include competing priorities and inadequate infrastructure and workforce capacity to deliver high-quality cancer care in low-resource settings.
Larson reiterated the need for resources across the entire cancer care continuum, from prevention to end-of-life care. He also pointed out that the United States has a real opportunity to learn from international cancer care experiences, just as international programs can apply lessons learned from low-resource settings in the United States.
Another theme Larson highlighted was the heterogeneity of low-resource areas, including the cultural heterogeneity of patients, biological diversity of cancers, as well as variability in health care infrastructure and resource availability. “The challenges are different within different settings and solutions are likely to be heterogeneous,” Larson said.
Larson also stressed the inadequate funding and prioritization of cancer care compared with the global burden of the disease, as well as the
inadequate consideration of quality of life and pain relief among patients with cancer. He said that improving cancer care will require cancer treatment resources and infrastructures—from pathology labs to the tools and facilities needed to provide surgery, radiation therapy, and chemotherapy—as well as strengthening and expanding the capacity of the cancer care workforce in low-resource areas. “Team-based cancer care is needed to improve patient outcomes, and will include the involvement of many different types of clinicians, including those in primary care, pathology, oncology, nursing, and others,” he said. He also stressed the importance of “improving the recognition and respect for professionals taking care of vulnerable patients in low-resource settings.”
Larson noted that a number of models and strategies to improve cancer care delivery were presented, including patient navigation, bundled payments to improve delivery of nutrition and psychosocial care, improved integration with primary care, as well as telementoring and telepathology services that could provide better access to specialized expertise and clinician training and education in remote areas.
Larson emphasized the need to better integrate palliative care throughout the cancer care continuum and improve access to it, especially in rural areas. “We need to address policy and legal factors that limit appropriate access to opioid medications to relieve cancer-related pain,” he said. He also noted the need to prepare for the growing number and diversity of cancer survivors by providing psychosocial care and interventions to support weight management, nutrition, and physical activity. These interventions should be tailored to community preferences and needs, Larson said.
Partnerships that are mutually beneficial, including those between community and academic practices and public–private partnerships, can also help improve cancer care in low-resource areas, Larson said. He added that both political and social will is needed to improve investment in cancer care in low-resource areas, and that this will require cancer care champions and an economic case for investing in cancer care. He suggested that prioritization and incremental improvements are an important step forward, and can be facilitated with the use of existing tools that include resource-stratified clinical practice guidelines, the WHO lists of essential medicines and priority devices, and baseline standards for nursing care. “Moving forward, sustainability—particularly of the successful pilot programs—is a key challenge that will need ongoing
attention and will require maintenance of progress, motivation, and financial support,” Larson said.
REFERENCES
ACS (American Cancer Society). 2017. Cancer Facts & Figures 2017. Atlanta, GA: American Cancer Society.
Adeniji, K. A., D. Huo, A. Khramtsov, C. Zhang, and O. I. Olopade. 2010. Molecular profiles of breast cancer in Ilorin, Nigeria. Journal of Clinical Oncology (Meeting Abstracts) 28(15 Suppl):1602.
Adesina, A., D. Chumba, A. M. Nelson, J. Orem, D. J. Roberts, H. Wabinga, M. Wilson, and T. R. Rebbeck. 2013. Improvement of pathology in sub-Saharan Africa. The Lancet Oncology 14(4):e152-e157.
Ambroggi, M., C. Biasini, C. Del Giovane, F. Fornari, and L. Cavanna. 2015. Distance as a barrier to cancer diagnosis and treatment: Review of the literature. The Oncologist 20(12):1378-1385.
American Nurses Credentialing Center. 2017. Homepage. http://www.nursecredentialing.org (accessed January 31, 2017).
Anderson, B. O., C.-H. Yip, R. A. Smith, R. Shyyan, S. F. Sener, A. Eniu, R. W. Carlson, E. Azavedo, and J. Harford. 2008. Guideline implementation for breast healthcare in low-income and middle-income countries. Cancer 113(S8):2221-2243.
Arora, S., K. Thornton, G. Murata, P. Deming, S. Kalishman, D. Dion, B. Parish, T. Burke, W. Pak, J. Dunkelberg, M. Kistin, J. Brown, S. Jenkusky, M. Komaromy, and C. Qualls. 2011. Outcomes of treatment for hepatitis C virus infection by primary care providers. New England Journal of Medicine 364(23):2199-2207.
ASCP (American Society for Clinical Pathology). 2017. The solution. https://www.ascp.org/content/functional-nav/global-impact/solution (accessed April 19, 2017).
Atun, R., D. A. Jaffray, M. B. Barton, F. Bray, M. Baumann, B. Vikram, T. P. Hanna, F. M. Knaul, Y. Lievens, T. Y. M. Lui, M. Milosevic, B. O’Sullivan, D. L. Rodin, E. Rosenblatt, J. Van Dyk, M. L. Yap, E. Zubizarreta, and M. Gospodarowicz. 2015. Expanding global access to radiotherapy. The Lancet Oncology 16(10):1153-1186.
Bakitas, M. A., K. Lyons, M. T. Hegel, S. Balan, F. C. Brokaw, J. Seville, J. G. Hull, Z. Li, T. D. Tosteson, I. R. Byock, and T. A. Ahles. 2009. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project Enable II randomized controlled trial. JAMA 302(7):741-749.
Bakitas, M. A., R. Elk, M. Astin, L. Ceronsky, K. N. Clifford, J. Nicholas Dionne-Odom, L. L. Emanuel, R. M. Fink, E. Kvale, S. Levkoff, C. Ritchie, and T. Smith. 2015a. Systematic review of palliative care in the rural setting. Cancer Control 22(4):450-464.
Bakitas, M. A., T. D. Tosteson, Z. Li, K. D. Lyons, J. G. Hull, Z. Li, J. N. Dionne-Odom, J. Frost, K. H. Dragnev, M. T. Hegel, A. Azuero, and T. A. Ahles. 2015b. Early versus delayed initiation of concurrent palliative oncology care: Patient outcomes in the ENABLE III randomized controlled trial. Journal of Clinical Oncology 33(13):1438-1445.
Barr, R., F. Antillon, B. Agarwal, P. Mehta, and R. Ribeiro. 2006. Pediatric oncology in countries with limited resources. In Principles and Practice of Pediatric Oncology, edited by P. A. Pizzo and D. G. Poplack. Philadelphia, PA: Lippincott, Williams & Wilkins. Pp. 1604-1616.
Berterame, S., J. Erthal, J. Thomas, S. Fellner, B. Vosse, P. Clare, W. Hao, D. T. Johnson, A. Mohar, J. Pavadia, A. K. E. Samak, W. Sipp, V. Sumyai, S. Suryawati, J. Toufiq, R. Yans, and R. P. Mattick. 2016. Use of and barriers to access to opioid analgesics: A worldwide, regional, and national study. The Lancet 387(10028):1644-1656.
Bray, F., A. Jemal, N. Grey, J. Ferlay, and D. Forman. 2012. Global cancer transitions according to the human development index (2008–2030): A population-based study. The Lancet Oncology 13(8):790-801.
CAPC (Center to Advance Palliative Care). 2011. The state-by-state report card on access to palliative care in our nation’s hospitals. https://reportcard.capc.org (accessed January 30, 2017).
CAPC. 2017. About palliative care. https://www.capc.org/about/palliative-care (accessed January 30, 2017).
Ceronsky, L., J. Shearer, K. Weng, M. Hopkins, and D. McKinley. 2013. Minnesota rural palliative care initiative: Building palliative care capacity in rural Minnesota. Journal of Palliative Medicine 16(3):310-313.
Cleeland, C. S., R. Gonin, A. K. Hatfield, J. H. Edmonson, R. H. Blum, J. A. Stewart, and K. J. Pandya. 1994. Pain and its treatment in outpatients with metastatic cancer. New England Journal of Medicine 330(9):592-596.
Connor, S. R., and M. C. S. Bermedo. 2014. Global atlas of palliative care at the end of life. http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf (accessed January 30, 2017).
Daly, B., O. I. Olopade, N. Hou, K. Yao, D. J. Winchester, and D. Huo. 2017. Evaluation of the quality of adjuvant endocrine therapy delivery for breast cancer care in the United States. JAMA Oncology. Epub ahead of print. doi: 10.1001/jamaoncol.2016.6380.
Dash, C., P. D. Randolph-Jackson, C. Isaacs, M. Mills, K. Makambi, V. V. Watkins, and L. L. Adams-Campbell. 2016. An exercise trial to reduce cancer related fatigue in African American breast cancer patients undergoing radiation therapy: Design, rationale, and methods. Contemporary Clinical Trials 47:153-157.
Day, S. W., R. M. Carty, and L. McKeon. 2013. Impact of the Guatemalan nursing program on treatment abandonment in children with cancer. Presented at the 24th International Nursing Research Congress.
Day, S. W., R. Hollis, J. Challinor, G. Bevilacqua, and E. Bosomprah. 2014. Baseline standards for paediatric oncology nursing care in low to middle income countries: Position statement of the SIOP PODC nursing working group. The Lancet Oncology 15(7):681-682.
Distelhorst, S. R., J. F. Cleary, P. A. Ganz, N. Bese, R. Camacho-Rodriguez, F. Cardoso, H. Ddungu, J. R. Gralow, C. H. Yip, and B. O. Anderson. 2014. Optimisation of the continuum of supportive and palliative care for patients with breast cancer in low-income and middle-income countries: Executive summary of the Breast Health Global Initiative. The Lancet Oncology 16(3):e137-e147.
Elliott, A. M., S. C. Alexander, C. A. Mescher, D. Mohan, and A. E. Barnato. 2016. Differences in physicians’ verbal and nonverbal communication with black and white patients at the end of life. Journal of Pain and Symptom Management 51(1):1-8.
Enserink, M. 2011. A push to fight cancer in the developing world. Science 331(6024): 1548-1550.
Estabrooks, C. A., W. K. Midodzi, G. G. Cummings, K. L. Ricker, and P. Giovannetti. 2005. The impact of hospital nursing characteristics on 30-day mortality. Nursing Research 54(2):74-84.
Fackenthal, J. D., J. Zhang, B. Zhang, Y. Zheng, F. Hagos, D. R. Burrill, Q. Niu, D. Huo, W. E. Sveen, T. Ogundiran, C. Adebamowo, A. Odetunde, A. G. Falusi, and O. I. Olopade. 2012. High prevalence of BRCA1 and BRCA2 mutations in unselected Nigerian breast cancer patients. International Journal of Cancer 131(5):1114-1123.
Farmer, P., J. Frenk, F. M. Knaul, L. N. Shulman, G. Alleyne, L. Armstrong, R. Atun, D. Blayney, L. Chen, R. Feachem, M. Gospodarowicz, J. Gralow, S. Gupta, A. Langer, J. Lob-Levyt, C. Neal, A. Mbewu, D. Mired, P. Piot, K. S. Reddy, J. D. Sachs, M. Sarhan, and J. R. Seffrin. 2010. Expansion of cancer care and control in countries of low and middle income: A call to action. The Lancet 376(9747):1186-1193.
Ferlay, J., I. Soerjomataram, M. Ervik, R. Dikshit, S. Eser, C. Mathers, M. Rebelo, D. M. Parkin, D. Forman, and F. Bray. 2013. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. http://globocan.iarc.fr (accessed April 4, 2017).
Ferrell, B. R., J. S. Temel, S. Temin, E. R. Alesi, T. A. Balboni, E. M. Basch, J. I. Firn, J. A. Paice, J. M. Peppercorn, T. Phillips, E. L. Stovall, C. Zimmermann, and T. J. Smith. 2016. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. Journal of Clinical Oncology 35(1):96-112.
Fink, R. M., K. S. Oman, J. Youngwerth, and L. L. Bryant. 2013. A palliative care needs assessment of rural hospitals. Journal of Palliative Medicine 16(6):638-644.
Fisch, M. J., J.-W. Lee, M. Weiss, L. I. Wagner, V. T. Chang, D. Cella, J. B. Manola, L. M. Minasian, W. McCaskill-Stevens, T. R. Mendoza, and C. S. Cleeland. 2012. Prospective, observational study of pain and analgesic prescribing in medical oncology outpatients with breast, colorectal, lung, or prostate cancer. Journal of Clinical Oncology 30(16):1980-1988.
Fred Hutchinson Cancer Research Center. 2017. Knowledge summaries. http://www.fredhutch.org/en/labs/phs/projects/breast-cancer-initiative_2-5/knowledge-summaries.html (accessed February 9, 2017).
Gostin, L. O. 2014. Healthy living needs global governance. Nature 511:147-149.
Grubbs, S. S., B. N. Polite, J. Carney, W. Bowser, J. Rogers, N. Katurakes, P. Hess, and E. D. Paskett. 2013. Eliminating racial disparities in colorectal cancer in the real world: It took a village. Journal of Clinical Oncology 31(16):1928-1930.
Howard, S. C., M. Marinoni, L. Castillo, M. Bonilla, G. Tognoni, S. Luna-Fineman, F. Antillon, M. G. Valsecchi, C.-H. Pui, R. C. Ribeiro, A. Sala, R. D. Barr, and G. Masera. 2007. Improving outcomes for children with cancer in low-income countries in Latin America: A report on the recent meetings of the Monza International School of Pediatric Hematology/Oncology (MISPHO)-Part I. Pediatric Blood Cancer 48:364-369.
Huo, D., F. Ikpatt, A. Khramtsov, J.-M. Dangou, R. Nanda, J. Dignam, B. Zhang, T. Grushko, C. Zhang, O. Oluwasola, D. Malaka, S. Malami, A. Odetunde, A. O. Adeoye, F. Iyare, A. Falusi, C. M. Perou, and O. I. Olopade. 2009. Population differences in breast cancer: Survey in indigenous African women reveals over-representation of triple-negative breast cancer. Journal of Clinical Oncology 27(27):4515-4521.
Hurst, C., and B. P. Dennis. 2013. Developing a clinical research associate training program at Dillard University: The impact of collaboration. Association of Black Nursing Faculty Journal 24(4):104-110.
IAEA (International Atomic Energy Agency). 2014a. Advisory group on increasing access to radiotherapy technology in low and middle income countries. http://cancer.iaea.org/agart.asp (accessed January 30, 2017).
IAEA. 2014b. VUCCnet. http://cancer.iaea.org/vuccnet.asp (accessed February 8, 2017).
International Narcotics Control Board. 2016. Availability of internationally controlled drugs: Ensuring adequate access for medical and scientific purposes. http://www.incb.org/documents/Publications/AnnualReports/AR2015/English/Supplement-AR15_availability_English.pdf (accessed February 6, 2017).
International Prevention Research Institute. 2013. The state of oncology 2013. http://www.i-pri.org/oncology2013 (accessed April 13, 2017).
IOM (Institute of Medicine). 2007. Cancer control opportunities in low- and middle-income countries. Washington, DC: The National Academies Press.
IOM. 2013. Delivering high-quality cancer care: Charting a new course for a system in crisis. Washington, DC: The National Academies Press.
IOM. 2014. Ensuring patient access to affordable cancer drugs:Workshop summary. Washington, DC: The National Academies Press.
IOM. 2015. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: The National Academies Press.
Jagsi, R., J. A. E. Pottow, K. A. Griffith, C. Bradley, A. S. Hamilton, J. Graff, S. J. Katz, and S. T. Hawley. 2014. Long-term financial burden of breast cancer: Experiences of a diverse cohort of survivors identified through population-based registries. Journal of Clinical Oncology 32(12):1269-1276.
Jones, A., and R. J. Paxton. 2015. Neighborhood disadvantage, physical activity barriers, and physical activity among African American breast cancer survivors. Preventive Medicine Reports 2:622-627.
Kagawa-Singer, M., S. P. Tanjasiri, A. Valdez, H. Yu, and M. A. Foo. 2009. Outcomes of a breast health project for Hmong women and men in california. American Journal of Public Health 99(Suppl 2):S467-S473.
Kurebayashi, J., T. Moriya, T. Ishida, H. Hirakawa, M. Kurosumi, F. Akiyama, T. Kinoshita, H. Takei, K. Takahashi, M. Ikeda, and K. Nakashima. 2007. The prevalence of intrinsic subtypes and prognosis in breast cancer patients of different races. The Breast 16(Suppl 2):72-77.
Lozano, R., M. Naghavi, K. Foreman, S. Lim, K. Shibuya, V. Aboyans, J. Abraham, T. Adair, R. Aggarwal, S. Y. Ahn, M. A. AlMazroa, M. Alvarado, H. R. Anderson, L. M. Anderson, K. G. Andrews, C. Atkinson, L. M. Baddour, S. Barker-Collo, D. H. Bartels, M. L. Bell, E. J. Benjamin, D. Bennett, K. Bhalla, B. Bikbov, A. B. Abdulhak, G. Birbeck, F. Blyth, I. Bolliger, S. Boufous, C. Bucello, M. Burch, P. Burney, J. Carapetis, H. Chen, D. Chou, S. S. Chugh, L. E. Coffeng, S. D. Colan, S. Colquhoun, K. E.
Colson, J. Condon, M. D. Connor, L. T. Cooper, M. Corriere, M. Cortinovis, K. C. de Vaccaro, W. Couser, B. C. Cowie, M. H. Criqui, M. Cross, K. C. Dabhadkar, N. Dahodwala, D. De Leo, L. Degenhardt, A. Delossantos, J. Denenberg, D. C. Des Jarlais, S. D. Dharmaratne, E. R. Dorsey, T. Driscoll, H. Duber, B. Ebel, P. J. Erwin, P. Espindola, M. Ezzati, V. Feigin, A. D. Flaxman, M. H. Forouzanfar, F. G. R. Fowkes, R. Franklin, M. Fransen, M. K. Freeman, S. E. Gabriel, E. Gakidou, F. Gaspari, R. F. Gillum, D. Gonzalez-Medina, Y. A. Halasa, D. Haring, J. E. Harrison, R. Havmoeller, R. J. Hay, B. Hoen, P. J. Hotez, D. Hoy, K. H. Jacobsen, S. L. James, R. Jasrasaria, S. Jayaraman, N. Johns, G. Karthikeyan, N. Kassebaum, A. Keren, J.-P. Khoo, L. M. Knowlton, O. Kobusingye, A. Koranteng, R. Krishnamurthi, M. Lipnick, S. E. Lipshultz, S. L. Ohno, J. Mabweijano, M. F. MacIntyre, L. Mallinger, L. March, G. B. Marks, R. Marks, A. Matsumori, R. Matzopoulos, B. M. Mayosi, J. H. McAnulty, M. M. McDermott, J. McGrath, Z. A. Memish, G. A. Mensah, T. R. Merriman, C. Michaud, M. Miller, T. R. Miller, C. Mock, A. O. Mocumbi, A. A. Mokdad, A. Moran, K. Mulholland, M. N. Nair, L. Naldi, K. M. V. Narayan, K. Nasseri, P. Norman, M. O’Donnell, S. B. Omer, K. Ortblad, R. Osborne, D. Ozgediz, B. Pahari, J. D. Pandian, A. P. Rivero, R. P. Padilla, F. Perez-Ruiz, N. Perico, D. Phillips, K. Pierce, C. A. Pope, III, E. Porrini, F. Pourmalek, M. Raju, D. Ranganathan, J. T. Rehm, D. B. Rein, G. Remuzzi, F. P. Rivara, T. Roberts, F. R. De León, L. C. Rosenfeld, L. Rushton, R. L. Sacco, J. A. Salomon, U. Sampson, E. Sanman, D. C. Schwebel, M. Segui-Gomez, D. S. Shepard, D. Singh, J. Singleton, K. Sliwa, E. Smith, A. Steer, J. A. Taylor, B. Thomas, I. M. Tleyjeh, J. A. Towbin, T. Truelsen, E. A. Undurraga, N. Venketasubramanian, L. Vijayakumar, T. Vos, G. R. Wagner, M. Wang, W. Wang, K. Watt, M. A. Weinstock, R. Weintraub, J. D. Wilkinson, A. D. Woolf, S. Wulf, P.-H. Yeh, P. Yip, A. Zabetian, Z.-J. Zheng, A. D. Lopez, and C. J. L. Murray. 2012. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. The Lancet 380(9859):2095-2128.
Magrath, I., E. Steliarova-Foucher, S. Epelman, R. C. Ribeiro, M. Harif, C-K. Li, R. Kebudi, S. D. Macfarlane, and S. C. Howard. 2013. Paediatric cancer in low-income and middle-income countries. The Lancet Oncology 14(3):e104-e116.
Masera, G., F. Baez, A. Biondi, F. Cavalli, V. Conter, A. Flores, G. Fontana, F. F. Bellani, P. Lanfranco, A. Malta, G. Mendez, E. Ocampo, C. Pacheco, L. Riva, A. Sala, F. Silva, C. Sessa, and G. Tognoni. 1998. North–south twinning in paediatric haemato-oncology: The La Mascota Programme, Nicaragua. The Lancet 352(9144):1923-1926.
May, P., M. M. Garrido, J. B. Cassel, A. S. Kelley, D. E. Meier, C. Normand, T. J. Smith, L. Stefanis, and R. S. Morrison. 2015. Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: Earlier consultation is associated with larger cost-saving effect. Journal of Clinical Oncology 33(25):2745-2752.
Meadows, R., T. Bonner, M. Dobhal, S. Borra, J. A. Killion, and R. Paxton. 2017. Pathways between physical activity and quality of life in African-American breast cancer survivors. Supportive Care in Cancer 25(2):489-495.
Meara, J. G., A. J. M. Leather, L. Hagander, B. C. Alkire, N. Alonso, E. A. Ameh, S. W. Bickler, L. Conteh, A. J. Dare, J. Davies, E. D. Mérisier, S. El-Halabi, P. E. Farmer, A. Gawande, R. Gillies, S. L. M. Greenberg, C. E. Grimes, R. L. Gruen, E. A. Ismail, T. B. Kamara, C. Lavy, G. Lundeg, N. C. Mkandawire, N. P. Raykar, J. N. Riesel, E. Rodas, J. Rose, N. Roy, M. G. Shrime, R. Sullivan, S. Verguet, D. Watters, T. G. Weiser, I. H. Wilson, G. Yamey, and W. Yip. 2015. Global surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. The Lancet 386(9993):569-624.
Meghani, S. H., Y. Kang, J. Chittams, E. McMenamin, J. J. Mao, and J. Fudin. 2014. African americans with cancer pain are more likely to receive an analgesic with toxic metabolite despite clinical risks: A mediation analysis study. Journal of Clinical Oncology 32(25):2773-2779.
Meneses, K., S. Gisiger-Camata, Y.-M. Schoenberger, R. Weech-Maldonado, and P. McNees. 2015. Adapting an evidence-based survivorship intervention for latina breast cancer survivors. Women’s Health (London, England) 11(2):109-119.
Morrison, R. S., D. E. Meier, T. Dumanovsky, and M. Rogers. 2015. America’s care of serious illness. https://reportcard.capc.org/wp-content/uploads/2015/08/CAPC-Report-Card-2015.pdf (accessed February 6, 2017).
Murillo, R., S. Díaz, F. Perry, C. Poveda, M. Piñeros, O. Sánchez, L. Buitrago, O. Gamboa, T. Lozano, H. Yu, C. Y. Wang, C. Duggan, D. B. Thomas, and B. O. Anderson. 2016. Increased breast cancer screening and downstaging in Colombian women: A randomized trial of opportunistic breast screening. International Journal of Cancer 138(3):705-713.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Cancer care in low-resource areas: Cancer prevention and early detection:Workshop summary. Washington, DC: The National Academies Press.
NCCN (National Comprehensive Cancer Network). 2017. NCCN framework for resource stratification of NCCN guidelines. https://www.nccn.org/framework (accessed February 8, 2017).
NCI (National Cancer Institute). 2015. Patient navigation research program. https://www.cancer.gov/about-nci/organization/crchd/disparities-research/pnrp (accessed February 7, 2017).
NCI. 2017a. NCI Dictionary of Cancer Terms. https://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=561237 (accessed April 4, 2017).
NCI. 2017b. Research-tested intervention programs (RTIPS) frequently asked questions. https://rtips.cancer.gov/rtips/faq.do (accessed February 1, 2017).
New Mexico Cancer Care Alliance. 2012. New Mexico Cancer Care Alliance. http://nmcca.org/about-us/nmcca-goals (accessed February 9, 2017).
Novartis. 2017. Novartis access. https://www.novartis.com/about-us/corporate-responsibility/expanding-access-healthcare/novartis-access (accessed February 1, 2017).
Oyekanmi, G., and R. J. Paxton. 2014. Barriers to physical activity among African American breast cancer survivors. Psycho-Oncology 23(11):1314-1317.
Pain & Policy Studies Group. 2014. Achieving balance in state pain policy: A progress report card (CY 2013). http://www.painpolicy.wisc.edu/sites/www.painpolicy.wisc.edu/files/prc2013.pdf (accessed March 31, 2017).
Paskett, E. D., J. P. Harrop, and K. J. Wells. 2011. Patient navigation: An update on the state of the science. CA: A Cancer Journal for Clinicians 61(4):237-249.
Patient Advocate Foundation. 2015. 2015 patient data analysis report. http://www.patientadvocate.org/pdar/2015_PDAR.pdf (accessed February 6, 2017).
PIH (Partners In Health). 2017. Our mission. http://www.pih.org/pages/our-mission (accessed February 1, 2017).
Pisu, M., K. Kenzik, R. A. Oster, P. Drentea, K. T. Ashing, M. Fouad, and M. Y. Martin. 2015. Economic hardship of minority and non-minority cancer survivors one year after diagnosis: Another long term effect of cancer? Cancer 121(8):1257-1264.
Purdie, T. G., R. E. Dinniwell, D. Letourneau, C. Hill, and M. B. Sharpe. 2011. Automated planning of tangential breast intensity-modulated radiotherapy using heuristic optimization. International Journal of Radiation Oncology*Biology*Physics 81(2):575-583.
Ramsey, S. D., D. Blough, A. Kirchhoff, K. Kreizenbeck, C. Fedorenko, K. Snell, P. Newcomb, W. Hollingworth, and K. Overstreet. 2013. Washington state cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Affairs 32(6):1-10.
Ramsey, S. D., A. Bansal, C. R. Fedorenko, D. K. Blough, K. A. Overstreet, V. Shankaran, and P. Newcomb. 2016. Financial insolvency as a risk factor for early mortality among patients with cancer. Journal of Clinical Oncology 34(9):980-986.
Robbins, A. S., R. L. Siegel, and A. Jemal. 2012. Racial disparities in stage-specific colorectal cancer mortality rates from 1985 to 2008. Journal of Clinical Oncology 30(4):401-405.
Robertson, J., R. Barr, L. N. Shulman, G. B. Forted, and N. Magrinid. 2016. Essential medicines for cancer: WHO recommendations and national priorities. Bulletin of the World Health Organization 94(10):735-742. http://www.who.int/bulletin/volumes/94/10/15-163998.pdf (accessed January 31, 2017).
Rugo, H., A. Barve, C. F. Waller, M. Bronchud, J. Herson, J. Yuan, A. Manikhas, I. Bondarenko, G. Mukhametshina, G. Nemsadze, J. D. Parra, M. L. T. Abesamis-Tiambeng, K. Baramidze, C. Akewanlop, I. Vynnychenko, V. Sriuranpong, G. Mamillapalli, S. Ray, E. P. Y. Ruiz, and E. Pennella. 2016. Heritage, a Phase III safety and efficacy trial of the proposed trastuzumab biosimilar, MYL-1401O vs trastuzumab. Annals of Oncology 27(Suppl 6):LBA16.
Shafiq, J., T. P. Hanna, S. K. Vinod, G. P. Delaney, and M. B. Barton. 2016. A population-based model of local control and survival benefit of radiotherapy for lung cancer. Clinical Oncology 28(10):627-638.
Shaheen, R., P. J. Slanetz, S. Raza, and M. P. Rosen. 2011. Barriers and opportunities for early detection of breast cancer in Gaza women. The Breast 20(Suppl 2):S30-S34.
Shastri, A., and S. Shastri. 2014. Cancer screening and prevention in low-resource settings. Nature Reviews Cancer 14:822-829.
Siegel, R., D. Naishadham, and A. Jemal. 2013. Cancer statistics. CA: A Cancer Journal for Clinicans 63(1):11-30.
Singhal, A., Y.-Y. Tien, and R. Y. Hsia. 2016. Racial-ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PLoS ONE 11(8):1-14.
Smith, B. D., G. L. Smith, A. Hurria, G. N. Hortobagyi, and T. A. Buchholz. 2009. Future of cancer incidence in the United States: Burdens upon an aging, changing nation. Journal of Clinical Oncology 27(17):2758-2765.
State Cancer Profiles. 2017. Interactive maps. https://statecancerprofiles.cancer.gov/map/map.withimage.php?00&001&055&02&2&02&0&1&5&0%20-%20results (accessed February 6, 2017).
Sullivan, R., O. I. Alatise, B. O. Anderson, R. Audisio, P. Autier, A. Aggarwal, C. Balch, M. F. Brennan, A. Dare, A. D’Cruz, A. M. M. Eggermont, K. Fleming, S. M. Gueye, L. Hagander, C. A. Herrera, H. Holmer, A. M. Ilbawi, A. Jarnheimer, J.-F. Ji, T. P. Kingham, J. Liberman, A. J. M. Leather, J. G. Meara, S. Mukhopadhyay, S. S. Murthy, S. Omar, G. P. Parham, C. S. Pramesh, R. Riviello, D. Rodin, L. Santini, S. V. Shrikhande, M. Shrime, R. Thomas, A. T. Tsunoda, C. van de Velde, U. Veronesi, D. K. Vijaykumar, D. Watters, S. Wang, Y.-L. Wu, M. Zeiton, and A. Purushotham. 2015. Global cancer surgery: Delivering safe, affordable, and timely cancer surgery. The Lancet Oncology 16(11):1193-1224.
Tapela, N., I. Nzayisenga, R. Sethi, J. B. Bigirimana, H. Habineza, V. Hategekimana, N. Mantini, T. Mpunga, L. N. Shulman, and L. L. 2016. Treatment of chronic myeloid leukemia in rural Rwanda: Promising early outcomes. Journal of Global Oncology 2(3):129-137.
Tayou Tagny, C., A. Diarra, R. Yahaya, M. Hakizimana, A. Nguessan, G. Mbensa, Y. Nébié, H. Dahourou, J. B. Tapko, C. Shiboski, E. Murphy, and J. J. Lefrère. 2009. Le centre de transfusion, le donneur de sang et le sang donné dans les pays d’afrique francophone. Transfusion Clinique et Biologique 16(5-6):431-438.
Temel, J. S., J. A. Greer, A. Muzikunsky, E. R. Gallagher, S. Admane, V. A. Jackson, C. M. Dahlin, C. D. Blinderman, J. Jacobsen, W. F. Pirl, J. A. Billings, and T. J. Lynch. 2010. Early Palliative Care with Metastatic Non-Small Cell Lung Cancer. New England Journal of Medicine 363(8):733-742.
Thannickal, B. 2015. Preliminary UAB study shows dramatic trend of cost savings in lay navigation program for cancer patients. https://www.uab.edu/news/focus-on-patient-care/item/6122-preliminary-uab-study-shows-dramatic-trend-of-cost-savings-in-lay-navigation-program-for-cancer-patients (accessed February 9, 2017).
UICC (Union for International Cancer Control). 2011. International Childhood Cancer Day. http://www.uicc.org/press-lounge/international-childhood-cancer-day (accessed April 7, 2017).
UICC. 2017. Access to essential radiotherapy. http://www.uicc.org/sites/main/files/atoms/files/UICC_Radiotherapy_4pager.pdf (accessed March 27, 2017).
University of Alabama at Birmingham. 2016. Deep south network for cancer control. http://www3.ccc.uab.edu/community-outreach/deep-south-network-for-cancer-control (accessed February 1, 2017).
The University of Texas MD Anderson Cancer Center. 2017. Project ECHO. https://www.mdanderson.org/education-training/global-outreach/project-echo.html (accessed February 8, 2017).
WHO (World Health Organization). 2009. Global database on blood safety summary report 2009. http://apps.who.int/bloodsafety/global_database/GDBS_Summary_Report_2009.pdf (accessed February 6, 2017).
WHO. 2013. Handbook for cancer research in Africa, edited by T. R. Rebbeck. Republic of Congo: WHO. http://apps.who.int/iris/bitstream/10665/100065/1/9789290232216.pdf (accessed January 30, 2017).
WHO. 2014. Strengthening of palliative care as a component of comprehensive care throughout the life course. http://apps.who.int/gb/ebwha/pdf_files/WHA67/A67_R19-en.pdf?ua=1 (accessed April 17, 2017).
WHO. 2015a. Cancer. http://www.who.int/mediacentre/factsheets/fs297/en (accessed January 27, 2017).
WHO. 2015b. Cervical cancer. http://globocan.iarc.fr/old/FactSheets/cancers/cervix-new.asp (accessed January 30, 2017).
WHO. 2017. WHO priority medical devices for cancer management. http://cedglobal.org/wp-content/uploads/2016/05/WHO-cancer-care-global-initiative-2016.pdf (accessed February 26, 2017).
World Oncology Forum. 2013. Stop cancer now! The Lancet 381(9865):426-427.
Yang, X. R., M. E. Sherman, D. L. Rimm, J. Lissowska, L. A. Brinton, B. Peplonska, S. M. Hewitt, W. F. Anderson, N. Szeszenia-Dąbrowska, A. Bardin-Mikolajczak, W. Zatonski, R. Cartun, D. Mandich, G. Rymkiewicz, M. Ligaj, S. Lukaszek, R. Kordek, and M. García-Closas. 2007. Differences in risk factors for breast cancer molecular subtypes in a population-based study. Cancer Epidemiology Biomarkers and Prevention 16(3):439-443.
Yap, M. L., E. Zubizarreta, F. Bray, J. Ferlay, and M. Barton. 2016. Global access to radiotherapy services: Have we made progress during the past decade? Journal of Global Oncology 2(4):207-215.
Zubizarreta, E. H., E. Fidarova, B. Healy, and E. Rosenblatt. 2015. Need for radiotherapy in low and middle income countries—the silent crisis continues. Clinical Oncology 27(2):107-114.
This page intentionally left blank.


































































































