4
Current Status of Federal and State Programs and Cross-cutting Issues
INTRODUCTION
A wide range of health outcomes—from fatal falls and amputations to chronic lung disease, musculoskeletal disorders, and cancer—are either caused or exacerbated by hazardous exposures in the work environment. Currently, there is no single, comprehensive occupational safety and health (OSH) surveillance system in the United States but rather an evolving set of systems using a variety of data sources that meet different surveillance objectives, each with strengths and weaknesses. As discussed, many federal and state agencies carry out this work. Figure 4-1 shows a Venn diagram representing major data sources for occupational injuries and illnesses (under the major categories of employers, medical records, and individuals) and the overlap among the systems that collect these data for occupational injury and illness surveillance. The degree of overlap is a best guess estimate of how much overlap there is between systems and illustrates that in the potential smart surveillance system of the future, there will be some overlap between the sources and that there will be a need to collect data from multiple sources to obtain a comprehensive picture of OSH problems. In Figure 4-1, the sources of data from employers are the Bureau of Labor Statistics’ Survey of Occupational Injuries and Illnesses (BLS SOII), workers’ compensation, and direct reports by employers to regulatory agencies. The sources of data from medical records are ambulance companies, audiometry providers, birth certificates, cancer registries, death certificates/medical examiners, hospitals; emergency departments, clinics, clinicians, laboratories, Medicare databases, and poison control centers. The sources
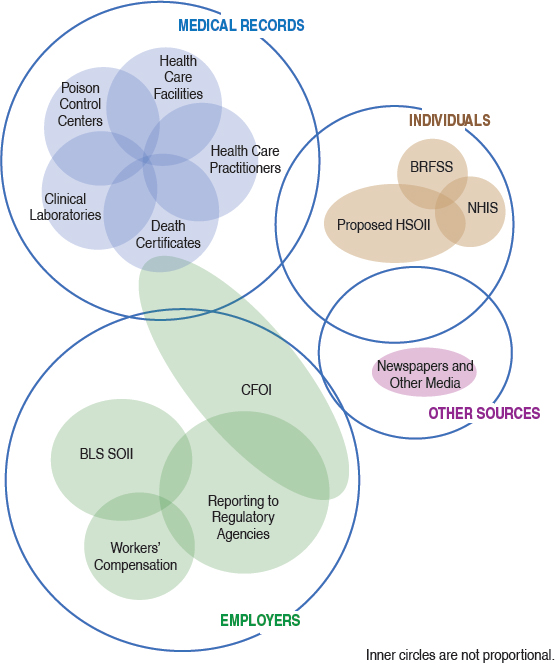
of data from individuals (current workers, retirees, disabled) are health surveys (BRFSS, National Health Interview Survey [NHIS], National Health and Nutrition Examination Survey [NHANES]), and proposed Household Survey of Nonfatal Occupational Injuries and Illnesses (HSOII). The other sources of data are newspaper reports/electronic media. There are limited data to show overlap between different sources, and examples of studies showing the degree of overlap are: BLS SOII and workers’ compensation (Rosenman et al., 2006; Boden and Ozonoff, 2008); or individual conditions such as acute traumatic fatalities (BLS, 2016a), amputations (Largo and Rosenman, 2015), burns (Kica and Rosenman, 2012) or skull fractures (Kica and Rosenman, 2014). The successful model for a multisource oc-
cupational surveillance system is the Census for Fatal Occupational Injuries (CFOI).
The major systems in place are largely focused on injury and disease outcomes. Hazard and exposure surveillance is important but currently very limited. In this chapter, we provide an overview of the major systems, organized by the health outcome under surveillance: fatal injuries, nonfatal injuries, and diseases. The current status of hazard surveillance is also discussed. The chapter concludes with a discussion of several crosscutting issues in OSH surveillance. A number of promising new developments in the field are described in Chapter 6.
SURVEILLANCE OF FATAL OCCUPATIONAL INJURIES
Substantial advances in the surveillance of fatal occupational injuries have been made over the past several decades with the development and implementation of several surveillance systems and programs (see Table 4-1).
In 1992, BLS (in the U.S. Department of Labor [DOL])—in response to recommendations in the 1987 National Research Council (NRC) report—established the Census of Fatal Occupational Injuries (CFOI), a nationwide surveillance system designed to produce a timely census of all fatal work injuries in the United States.1 A federal-state cooperative program implemented in all 50 states, CFOI uses multiple data sources, such as death certificates, police reports, federal agency administrative data, workers’ compensation claim records, and news media, to identify, verify, and describe fatal work injuries. For each death, information is collected about the deceased worker, including occupation and demographic characteristics, the establishment, the equipment involved, and the circumstances of the event. Two or more independent source documents are used to confirm that fatal injury cases are work related. National and state-level findings including both counts and rates2 by industry and occupation and other worker and establishment characteristics are issued annually, in the following calendar year. Surveillance findings are published through the media and made available on an interactive BLS website (BLS, 2017a). BLS has also published more extensive analyses of fatalities among workers in specific industries (e.g., road construction and landscaping), among specific worker groups (e.g., Hispanics, Asians), and due to specific events (e.g., machine-related deaths and suicides), as well as studies comparing analytic methods
___________________
1 BLS notes that “to be included in CFOI: a death must have resulted from a traumatic injury; the incident that led to the death must have occurred in the United States, its territories, or its territorial waters or airspace; and it must be related to work. Defining work-relatedness is complex and BLS CFOI applies a standard definition” (BLS, 2016a).
2 Rates exclude persons younger than 16 years of age, volunteers, and resident military personnel.
| Surveillance System | Scopea | Typeb | Responsible Agency(ies) | Condition(s) under Surveillancec |
|---|---|---|---|---|
| Census of Fatal Occupational Injuries (CFOI) | National 50 states | P | BLS* States* | O: Fatal occupational injuries |
| Fatality Assessment and Control Evaluation (FACE) Program | 7 states | C | NIOSH* States | O: Fatal occupational injuries—targeted incidents |
| Firefighter Fatality Investigation and Prevention Program | National State | C | NIOSH* | O: Fatal occupational injuries and heart attacks in line of duty |
| Commercial Fishing Incident Database | National Regional State | P | NIOSH* | O: Fatal occupational injuries and incident survivors |
| Fatalities in Oil and Gas Extraction | National | C | NIOSH* | O: Fatal occupational injuries and illnesses |
NOTES: BLS, Bureau of Labor Statistics; NIOSH, National Institute for Occupational Safety and Health; OSHA, Occupational Safety and Health Administration; asterisk denotes funding agency.
a Geographic levels at which findings are publicly available.
b P, population based: data are collected on a census or representative sample of a defined population and allow for assessing extent of a health related event and monitoring trends with
(Windau, 1998; Sincavage, 2005; Wiatrowski, 2005; Byler, 2013; Pegula, 2013; Harris, 2016). The National Institute for Occupational Safety and Health (NIOSH) also has access to the CFOI microlevel files to conduct more in-depth analysis and respond to public information requests, but limited resources to do this work. Given that BLS collects CFOI under the Confidential Information Protection and Statistical Efficiency Act (CIPSEA), CFOI data can only be used for statistical purposes (OMB, 2007).
BLS continues to make enhancements to CFOI and has, for example,
| Data Source(s) | Population Coveredd | Approach | Time Frame for Report Release |
|---|---|---|---|
| Multiple: OSHA, Coast Guard records, death certificates, police reports, media, etc. | All workers | Census | Annual |
| Field investigations and other data sources | All workers | Case series (¾2% all worker deaths in U.S.) | Ongoing |
| Field investigations and other data sources | All firefighters | Case series (¾40% all firefighter deaths in U.S.) | Ongoing |
| Multiple: Coast Guard records, death certificates, local media, etc. | All workers in commercial fishing industry | Census | Intermittent |
| Multiple: OSHA records, motor vehicle crash reports, police reports, media and professional contacts | All oil and gas extraction workers | Census | Intermittent |
this population over time/locale; C, case based: focus of data collection is on individual cases that require follow-up or immediate public health action. These approaches are not mutually exclusive.
c O, outcome; H, hazard; E, exposure.
d The population covered may include active and former workers, retirees, and others depending on the system.
expanded the number of variables collected to include birthplace, contracted worker status, and, in the case of a contracted decedent, ownership of the contracting firm. Distinguishing fatal work-related motor vehicle incidents from non-work-related incidents is particularly difficult, and BLS is currently working with NIOSH, the National Highway Traffic Safety Administration (NHTSA) and state agency partners to pilot new approaches to provide more comprehensive information about fatal occupational crashes.
BLS has also improved the timeliness of releasing CFOI findings to the public.
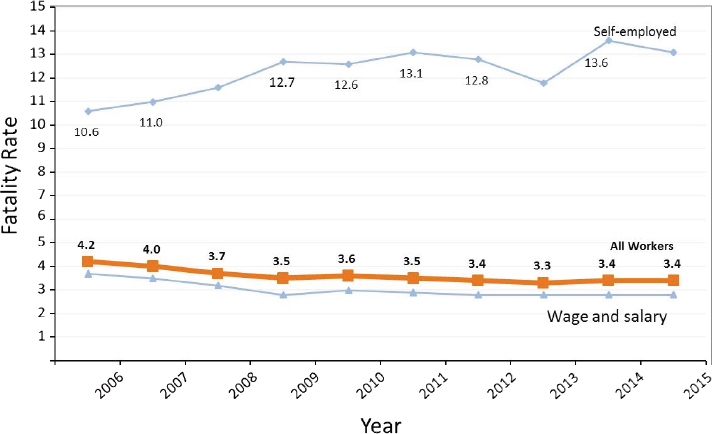
CFOI is well respected as an authoritative count of fatal work injuries at the national and state levels and a model for multisource surveillance of a health outcome. It provides robust information about the burden and distribution of fatal occupational injuries over time and serves as an important example of how surveillance findings can be used to monitor progress in meeting prevention goals, target intervention activities, and set research priorities. Findings have identified a decline in the fatal occupational injury rate over time as well as continuing high risk among workers in certain industries, such as fishing, construction, transportation, and the self-employed (BLS, 2016b) (Figure 4-2). The data have also brought to
light high-risk populations, including older workers and Hispanic workers (Byler, 2013; BLS, 2016b). Findings have also led to new federal outreach initiatives including, for example, a nationwide campaign to prevent falls in construction (OSHA, 2017a) and increased Spanish-language assistance for Hispanic employers and workers (OSHA, 2007).
While CFOI provides essential statistical data on the approximately 5,000 fatal occupational injuries that occur each year (BLS, 2017a), the CFOI data lack sufficient detail about underlying causes of fatal incidents needed to develop specific prevention recommendations, and, as described above, BLS confidentiality practices restrict the use of the data for case-level public health intervention. For instance, the system does not allow for case-based follow-up to intervene in specific workplaces to protect others at risk or to learn more about specific factors (e.g., names of specific chemicals) contributing to workplace injuries.
Since 1991, NIOSH has supported a collaborative endeavor with the states, the Fatality Assessment and Control Evaluation (FACE) program, to conduct in-depth investigations of targeted fatal occupational incidents with the objective of identifying factors contributing to these deaths. Currently seven states are funded by NIOSH to conduct approximately 100 investigations each year.3
NIOSH identifies national targets for investigation, which currently include falls from elevations and machine-related deaths, and the participating states have the option of identifying their own targets. FACE investigators use an approach developed by Haddon to identify underlying causes of the incidents (Haddon, 1970). This information is used to develop comprehensive recommendations for prevention. Each investigation results in a report with an incident description and prevention recommendations which is disseminated widely to industry, labor, equipment manufacturers, and other stakeholders. State FACE programs also work with local agency and private-sector partners to promote implementation of recommendations (NIOSH, 2017a). FACE provides valuable in-depth information about the circumstances leading to deaths that is either not collected or because of confidentiality not available in the CFOI statistics and exemplifies how data can be used to inform prevention. The investigation of sentinel fatalities through the FACE program has helped identify and increase public awareness of previously unrecognized hazards, and led to improvements in OSH practices at worksites, changes in public policy, and development of new, safer technologies. For example, FACE investigations in Michigan led to a nationwide alert on hazards of methylene chloride exposures associated
___________________
3 Some additional state health agencies, such as in Wyoming, that do not participate in the FACE program also track work-related deaths for public health intervention purposes (WY DWS, 2016).
with bathtub refinishing (MI FACE, 2013; OSHA, 2013); FACE investigations of deaths among floor finishers in Massachusetts contributed to state law banning the use of highly flammable floor sealing products (MA COSH 2005; Azaroff et al., 2011); and a Kentucky FACE investigation of the death of an auto technician led to the redesign of a handicapped-accessible accelerator pedal (CSTE, 2015a).
In 1998, Congress funded NIOSH to establish a Firefighter Fatality and Investigation Program modeled on FACE in which NIOSH staff conducts in-depth investigations of select firefighter deaths throughout the country (NIOSH, 2017b). Targets for this program go beyond fatal injuries to include outcomes such as heart attacks in the line of duty. NIOSH also supports more in-depth data collection on fatal incidents in several high-risk industries, including fishing and oil and gas extraction, and works with partners in these targeted industries to disseminate findings and promote use of the data for prevention (NIOSH, 2012, 2014a, 2017c).
In recent years, there has been increased interest by state health agencies, unions, community organizations, and others for more timely and detailed information on specific workplace fatalities. In response, the Occupational Safety and Health Administration (OSHA) made additional timely information (including the victim’s name) on workplace fatalities investigated by the agency4 available on its website until changing this practice mid-2017 (OSHA, 2017b). Inability to access CFOI data for purposes of public health intervention has been a challenge. BLS has taken some steps to address this and make available to the public and state public health agencies timely data on fatal occupational injuries that are available through public sources including the web (Pegula and Measure, 2016). Several nonprofit organizations have made data on work-related fatalities available through interactive mapping applications (CPWR, 2017; National COSH, 2017).
SURVEILLANCE OF NONFATAL OCCUPATIONAL INJURIES
Nonfatal occupational injuries as discussed in this chapter encompass traumatic injuries due to sudden events such as falls, motor vehicle crashes, violence, and being struck by machinery. Also included within this discussion are musculoskeletal disorders (MSDs), which are defined by NIOSH as “soft-tissue injuries that may be caused by either sudden or sustained
___________________
4 Only about a third of all fatal occupational injuries are investigated by OSHA (AFL-CIO, 2017; MA DPH, 2017); the remaining deaths are either outside of OSHA’s jurisdiction (e.g., self-employed, public sector in federal OSHA states), are due to causes such as on-the-road motor vehicle deaths or homicides at work not routinely investigated by the agency, or came to OSHA’s attention more than 6 months after the incident.
exposure to repetitive motion, force, vibration, or awkward positions”5 (NIOSH, 2016g).
Over the past several decades, federal agencies, in collaboration with states, have made improvements in surveillance of nonfatal occupational injuries. Major activities include the following:
- BLS enhancements to the SOII to collect additional data on more severe injuries, add data on public employees, and expand data analysis;
- OSHA’s severe injury reporting system;
- NIOSH’s leveraging of other national public health surveillance systems and surveys; and
- State-based projects, funded largely by NIOSH, using state data sources to conduct surveillance of nonfatal occupational injuries at the state level.
Survey of Occupational Injuries and Illnesses
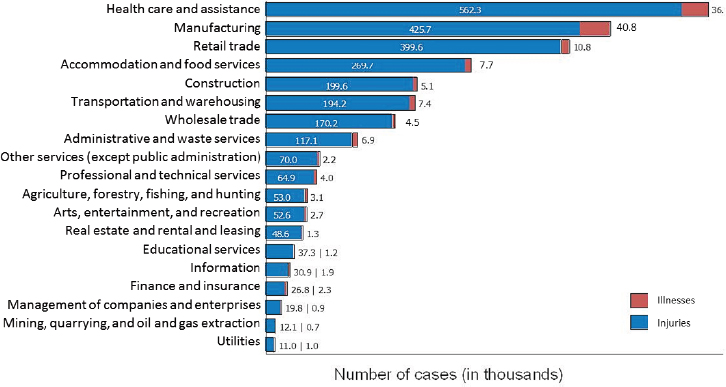
The SOII is the only source of uniform nationwide statistics on nonfatal work-related injuries in the United States, providing annual estimates of the number and rates of work-related injuries and illnesses for the nation and for the states that collaborate with BLS. This is available by industry, establishment employment size, and case severity as measured by work restriction or days of work lost (BLS, 2016c) (Figure 4-3). The SOII is conducted by BLS in collaboration with state agencies in 41 states, territories (Guam, Puerto Rico, and the U.S. Virgin Islands), and the District of Columbia, and data is collected directly by BLS in the other 9 nonparticipating states. The SOII is an annual nationwide survey with a sample of approximately 250,000 private industry and state and local government establishments, selected to represent all industries and all sizes of establishments. Data
___________________
5 The classification of MSDs in different surveillance systems is complicated. While in both the International Classification of Disease and the Occupational Injury and Illness Classification system used by BLS most MSDs are classified as injuries, there is a small set of conditions generally included in a broad definition of MSDs, such as carpal tunnel syndrome and Raynaud’s syndrome, that are classified as diseases. Since 2011, BLS and OSHA have applied a surveillance case definition for MSDs in employer-reported data aimed at identifying cases due to sustained exposure that takes into account information about both the nature of injury or illness and the event or exposure. Included are cases “where the nature of the injury or illness is pinched nerve; herniated disc; meniscus tear; sprains, strains, tears; hernia (traumatic and nontraumatic); pain, swelling, and numbness; carpal or tarsal tunnel syndrome; Raynaud’s syndrome or phenomenon; musculoskeletal system and connective tissue diseases and disorders, when the event or exposure leading to the injury or illness is overexertion and bodily reaction, unspecified; overexertion involving outside sources; repetitive motion involving micro tasks; other and multiple exertions or bodily reactions; and rubbed, abraded, or jarred by vibration” (NIOSH, 2016a).
from the railroad and mining industries included in the SOII published findings are obtained by BLS from the Federal Railroad Administration and the Mine Safety and Health Administration, which require reporting of all fatal and nonfatal work-related injuries and illnesses by railroad and mine employers.
The data collected by BLS for the SOII are based upon OSHA required records for occupational injuries and illnesses—the OSHA Log of Work-Related Injuries and Illnesses (Form 300), the Injury and Illness Incident Report (Form 301), and the Summary of Work-Related Injuries and Illnesses (Form 300A). Establishments selected for the SOII are required by law to maintain records of all work-related injuries and illness that meet the OSHA requirements for recordkeeping for 1 year (even if otherwise excluded from OSHA injury recordkeeping requirements) and report that information to BLS. Injuries and illnesses that are recordable for OSHA include those resulting in loss of consciousness, medical treatment beyond first aid, one or more missed days from work, restricted work activities, or transfer to another job (MI DCH, 2013). Since 1992, in addition to information from the OSHA Log, as recommended in the 1987 NRC report, the SOII has collected data on the nature and circumstances of the injury or illness (OSHA Form 301), as well as the characteristics of the affected workers for injuries resulting in one or more days away from work, which
currently account for 32 percent of all reported cases (BLS, 2016e). Given the changes in case management that can shift injured workers from lost-workday cases to restricted-work and job transfer cases, it is challenging to use these statistics as measures of injury severity.
This more detailed information is referred to as the case and demographic data. BLS collects data elements that employers are required by OSHA to record, along with several optional case and demographic variables including the race and ethnicity of the injured worker and the category that best describes the regular type of job or work. These variables, however, are generally not analyzed due to the limited reporting of these optional data (Wiatrowski, 2014). As with CFOI, national and state-level estimates are issued annually, and are published and made available on the web (BLS, 2016c).
BLS has continued to make improvements in the SOII. For example, in 2006, BLS began generating and publishing experimental rates by occupation, age, and gender, in addition to routinely published rates by industry, establishment, and case severity.6 In addition, starting in 2008, BLS expanded the scope of the SOII by collecting and reporting data about work-related injuries and illnesses among state and local government workers, who were previously not included in the nationwide survey.7 BLS has also piloted the collection of more detailed case and demographic data on a sample of injuries and illnesses that did not result in lost time but led to job transfer or restriction—which account for an increasing proportion of all cases reported over time—21 percent in 2015 (Wiatrowski, 2014; BLS, 2016f). Attention to enhanced information on all types of injuries is planned to be sought through a proposed household survey (see Chapter 6). BLS has also updated its injury and illness classification system to reflect current workplace hazards and has substantially reduced processing time to make the data more rapidly publicly available (Wiatrowski, 2014).
The information derived from the analysis of SOII data is used by federal and state government agencies to set standards, target enforcement compliance assistance activities, develop and update educational programs, and set research priorities. Industry and unions use the data for
___________________
6 Information on the number of employee hours provided by participating employers is used as the denominator in calculating rates by industry, establishment employment size, and case type. Since 2006, BLS has used external sources of denominator data (the BLS Current Population Survey and the Occupational Employment Statistics Program) to generate and publish experimental rates by occupation, age, and gender—as the employment data provided by participating employers are not broken down by these data elements.
7 Reporting by states and local agencies is voluntary for the 22 states without federally approved OSHA state plans covering state and local government workers. While the overall survey response rate for private-sector establishments is about 95 percent, it is around 80 percent for state and local governments (Wiatrowski, 2014).
benchmarking their own injury and illness experience. In some industries, most notably construction, industry-specific rates are used as criteria in assessing qualifications of contractors and subcontractors.
The SOII, however, has a number of significant limitations. Excluded from the SOII are the self-employed (e.g., independent contractors, including gig economy workers [on-demand contractors and freelance workers]), household workers, federal workers, U.S. Postal Service workers, and workers on farms with fewer than 11 employees. Altogether, these excluded populations represent about 9 percent of the workforce, the majority of whom are self-employed (Simpson, 2016). Also, the SOII does not collect case and demographic information for 70 percent of all reported injuries and illnesses (BLS, 2016e).
While it has long been recognized that the SOII does not adequately capture chronic occupational illnesses for reasons discussed under disease surveillance below, there is increasing evidence that undercounting of injuries and acute illnesses is also a significant limitation, and there may be differential rates of reporting by establishment, injury, and incident characteristics, as well as by state. In studies to quantify undercounting on OSHA Logs, estimates of the undercount range from 20 to 70 percent (Rosenman et al., 2006; Boden and Ozonoff, 2008; Wuellner et al., 2017). There is a consensus that the SOII substantially underestimates the true burden of work-related injuries among workers employed in establishments covered by OSHA and that multiple factors contribute to underreporting (Azaroff et al., 2002; Ruser, 2008; Spieler and Wagner, 2014; Wiatrowski, 2014; Wuellner and Bonauto, 2014; Rappin et al., 2016; Wuellner and Phipps, 2016; Wuellner et al., 2016, 2017; Fagan and Hodgson, 2017) (see Box 4-1).
Given concerns about the completeness of the injury and illness counts in the SOII, in recent years BLS has supported a program of research to better understand both the extent of the undercount and the contributing factors. Individual states have also compared findings from state systems combining data from multiple data sources (i.e., multisource surveillance systems) with SOII estimates (Kica and Rosenman, 2014; Largo and Rosenman, 2015). Recently reported findings based on interviewers with a sample of recordkeepers at establishments participating in the SOII indicated that many recordkeepers possess a limited understanding of the recordkeeping requirements and identified many common recording errors. Record-keeper characteristics (SOII experience, OSHA recordkeeping experience, and OSHA recordkeeping training) were found to be associated with better practices and knowledge (Wuellner and Phipps, 2016).
Additionally, there is concern that some of the most vulnerable workers, which often include racial and ethnic minority and immigrant workers, may be those whose injuries are least likely to be captured in the SOII
(Sabbath et al., 2017). Notably, because race and ethnicity are optional variables, these data elements are often incomplete. From 2011-2016, race and ethnicity information was not reported in the SOII for 36-39 percent of the cases involving days away from work (BLS, 2018). A related challenge is the inability to characterize the injury experience of temporary agency workers, as under OSHA recordkeeping rules, most injuries to temporary agency workers are recorded under the supervisory employer, which is more commonly the host employer rather than the “staffing agency,” which is the employer of record (OSHA, 2014). OSHA records and in turn the SOII are also unable to provide information across multiple employers who may be working at a single site with shared work environment responsibilities. This is an increasing concern as multiemployer workplaces, already common in the construction industry, are becoming more common in other industries (Weil, 2014, 2017).
In the last major revision to OSHA’s injury and illness recordkeeping regulations in 2001, the agency had proposed that construction employers
be required to maintain a site log for larger construction projects of the injuries and illnesses of all subcontractors with 11 or more employees working at the site. The proposal was widely supported by unions, but opposed by employers, and thus was not included as a provision, citing complexities for construction employers and questioning the utility of the data (OSHA, 2001).
Similarly, neither OSHA injury and illness recordkeeping and reporting requirements nor the SOII capture the enterprise-wide injury and illness experience for employers who operate multiple establishments. Thus, there is no ability to track injuries and illnesses at the enterprise or corporate level. OSHA had considered requiring enterprise level reporting by some larger employers as part of the new electronic injury reporting requirements issued in 2016 (discussed in Chapters 3 and 6), but the agency decided not to include such a provision in the final rule, again citing complexities involved with such reporting (OSHA, 2016a).
Another significant limitation of the SOII is the relatively small sample size at the state level. In all but the largest states, the sample is too small to provide sufficiently detailed data on different injury types in specific industries or occupations needed to target tailored intervention and prevention efforts (Davis et al., 2012). The SOII data are not routinely aggregated over years, although BLS is currently exploring methods for doing so. (On the other hand, in doing so trends in time would be less evident.) Finally, SOII, like CFOI, is a population-based surveillance system. BLS is required by CIPSEA to protect the confidentiality of SOII data and to ensure they are used only for statistical purposes. Establishment-level data are not made available to OSHA or other agencies for purposes of follow-up in specific workplaces to protect others at risk or for further information gathering. The SOII data are available to researchers for BLS-approved projects. In the past, this research had to be carried out at BLS headquarters but the Census Bureau and the Bureau of Labor Statistics are in the process of making certain BLS restricted data sets, including SOII and CFOI data, available to qualified researchers for statistical research exclusively through the Federal Statistical Research Data Centers managed by the U.S. Census Bureau.8
Potential Improvements in the SOII
BLS’s pilot collection of case and demographic data on the approximately 21 percent of recordable cases resulting in job transfer or restriction has demonstrated this is feasible (BLS, 2015, 2017b). Routine collection of these data in the SOII would provide important information about how
___________________
8 The SOII data set is now available at the Federal Statistical Research Data Centers and the CFOI data are planned to be made available at these centers in fall 2017.
occupational injuries and illnesses are managed and a much more complete accounting of the full range of injuries and illnesses and the circumstances in which they occur (NRC, 2001). Because, this would involve utilization of data already recorded by employers under the OHSA record-keeping rules and the large majority of employers report their data to SOII electronically, it would add little to the employer reporting burden. New natural language processing tools are being developed by BLS for auto-coding narrative information collected in the SOII (see Chapter 7), which can be anticipated to continue to improve over time and to help minimize the additional costs of processing these data at BLS.
Eliminating health disparities is a major goal of public health (CDC, 2016). Collection of information about race and ethnicity in public health surveillance systems is of high importance as it provides information to identify disparities in health across population groups. While there are robust data on the differential risk of fatal occupational injury across racial and ethnic groups available through CFOI, there is a paucity of such information on nonfatal injuries and illnesses. Collection of race and ethnicity data as an optional variable in the SOII for approximately 40 percent of cases suggests it is feasible for employers to report this information. However, incomplete reporting of these data underscore the importance of OSHA’s making this a mandatory data element in OSHA record-keeping. As described elsewhere, the changing nature of employment arrangements is a 21st century reality and occupational health surveillance systems will need to address this change. The current inability of the SOII to characterize the OSH risks faced by workers employed in nontraditional employment arrangements is a significant gap that can be addressed in part by collecting this information on OSHA logs and the SOII. It may benefit employers as well as provide information needed for accurate calculation of their establishment-specific illness and injury rates. Engagement of employers and workers in developing guidance on how to collect these data elements will be important.
An unheralded advantage of the SOII is its potential to foster use of data by employers and workers at the establishment level. Providing feedback to those who report data for surveillance purposes is a core component of an effective public health surveillance system (Thacker et al., 2012). Advances in information technology provide new opportunities for BLS to provide employers with feedback on their data and data analysis tools that they can use to target efforts to prevent work-related injuries and illness among their employees and reduce associated economic costs. As described, private sector employer participation in the SOII is legally mandatory. According to a 2011 analysis, the response rates of private sector employers were over 90 percent between 2003-2010 (Huband and Bobbit, 2013). While response rates for the SOII leave room for improvement, they are certainly
of a lesser concern than underreporting of injuries and illnesses. Making the data meaningful for employers so that it is seen as useful rather than as simply a reporting exercise has potential to improve not only response rate but data quality. Periodic assessment of undercount will continue to be an important activity of BLS to improve the accuracy and representativeness of the SOII estimates. OSHA enforcement of injury and illness recordkeeping requirements, including enforcement to protect workers who are retaliated against for reporting injuries, will remain critical to help ensure more complete and accurate recording and reporting.
Conclusion: Although limited, the SOII remains the most extensive system for standardized information on nonfatal occupational injuries and acute illnesses across the nation and the SOII continues to be an important source of information today. Better and more efficient use of the SOII to meet surveillance objectives, including characterization of disparities in risk among vulnerable groups of workers, is possible.
Recommendation A: BLS and OSHA should collaborate to enhance injury and illness recording and the SOII to achieve more complete, accurate, and robust information on the extent, distribution, and characteristics of work-related injuries and illnesses and affected workers for use at the worksite and at national and state levels. As part of this effort, BLS should routinely collect detailed case and demographic data for injuries and illnesses resulting in job transfer or restricted-duty work. Furthermore, OSHA should amend its injury and illness recording requirements to collect information on race and ethnicity as well as on employment arrangement to identify vulnerable worker populations and risks that may be associated with the changing nature of work.
In the near term:
- OSHA should make type of employment arrangement (e.g., traditional, independent contractor, temporary agency worker, and on-call worker) and race and ethnicity mandatory data elements on the OSHA Form 301, and BLS should incorporate this information into the SOII case and demographic data. OSHA should collaborate with BLS in determining the best approach to collecting this information (e.g., what questions should be included on Form 301).
- BLS should routinely collect detailed case and demographic data for injuries and illnesses resulting in job transfer or restricted duty as well as those resulting in days away from work.
- BLS should implement methods to aggregate SOII data over time to generate more robust and detailed state-level estimates.
- OSHA and BLS should collaborate to enhance recordkeeping train-
- ing for employers and BLS should evaluate approaches for providing initial information and ongoing feedback to data recorders in establishments enlisted to participate in the SOII both to improve the data quality and to promote employer use of data for prevention.
In the longer term:
- BLS and OSHA should collaborate to determine the best way to collect injury and illness data across multiple employers working at single sites, and across enterprises with multiple establishments.
- BLS should assess the feasibility and usefulness of extending collection of case and demographic data to all reported cases as automated approaches to coding SOII narratives are improved. Options for collecting such data should be evaluated in light of information that will be made available through the OSHA electronic reporting initiative.
OSHA Severe Injury Reporting
OSHA has undertaken many initiatives over the years to address the lack of access to establishment-specific injury and illness data in the SOII. Since OSHA was established in 1971, employers under OSHA jurisdiction have been required to promptly report workplace fatalities and incidents resulting in hospitalizations of three or more employees to the agency for evaluation and investigation. In 2014, OSHA expanded its reporting rules to require employers to report fatalities within 8 hours and all incidents resulting in in-patient hospitalization, amputation, or loss of an eye within 24 hours (referred to by OSHA as severe injuries). These expanded reporting requirements have enabled OSHA to better target limited enforcement and compliance assistance resources to the most dangerous workplaces and engage more high-hazard employers in eliminating serious hazards (Michaels, 2016). The data also have allowed the agency to gather information on the causes of incidents to identify serious hazards, prevent future incidents, and form the basis for revised standards.
The severe injury reporting rule went into effect January 1, 2015. During its first year of operation, OSHA reported that employers notified the agency of 10,388 nonfatal incidents, including 7,636 hospitalizations and 2,644 amputations. These data represent only reports made to federal OSHA, not the OSHA state plans.9 In addition, OSHA estimates that these
___________________
9 The 26 OSHA state plan states are required to adopt reporting requirements that are as effective as federal OSHA’s requirements. A number of states, including California and Washington, have required the reporting of all in-patient hospitalizations for many years. Other state plan states are in the process of adopting requirements similar to federal OSHA.
reports may represent fewer than half of the severe injuries that were required to have been reported to federal OSHA (Michaels, 2016). Recent findings from Massachusetts, a federal OSHA state, indicate that fewer than half of work-related amputations were reported by employers covered by OSHA (Grattan et al, 2017).
Since OSHA does not have the resources to conduct an onsite investigation or inspection for every severe injury report, the agency has developed a triage system for evaluating and responding to reports (OSHA, 2016b). Under its current procedures, all fatalities and reports of two or more hospitalizations are subject to an inspection as are reports involving a worker under 18 years of age, reports from employers with a history of similar incidents or multiple violations, or reports of incidents involving hazards covered by emphasis programs or any imminent danger. For other reports, OSHA gathers additional information from the employer about the incident, the injured employee, hazards involved, and history of the employer to determine whether to conduct an onsite inspection or an offsite rapid response investigation. Under a rapid response investigation, an employer is required to conduct its own investigation, abate any hazards found, report findings and abatement verification to OSHA in writing, and post the information in the workplace. To assist employers, OSHA is providing tools on conducting incident investigations, developed jointly with the National Safety Council.
OSHA is also collecting and compiling data from the severe injury reports. During the severe injury report intake process, the agency collects data on the employer, the employee (including employee’s age and employment arrangement [e.g., contract or temporary worker]), the injury, and the incident, and then enters it into the OSHA Information System (the agency’s primary program and regulatory database). Employer reports of fatalities and severe nonfatal injuries stripped of personal identifiers are made available by OSHA in a publicly accessible database (OSHA, 2017c). OSHA’s summary analysis of severe injury reports is conducted on an ad hoc basis.
From these reports, OSHA has identified industries with a higher number of severe injuries (e.g., construction, support activities for mining, and drilling and servicing for oil and gas). The reports have also helped OSHA identify patterns of severe injuries and take preventive action. For example, in 2015, OSHA’s Atlanta regional office noticed numerous reports of fingertip amputations among supermarket and restaurant workers using food slicers (Michaels, 2016). The agency took action to contact food service employers across the region and provide information about the hazards of food slicers and control measures to keep workers safe (OSHA, 2015).
NIOSH Use of Existing Surveillance Systems and Surveys
NIOSH conducts a number of surveillance activities aimed at filling gaps in information on nonfatal injuries. These include efforts using existing data sources in partnership with other federal agencies as well as support for injury surveillance in states, which will be discussed in the following section.
Since the early 1990s, NIOSH has had an interagency agreement with the Consumer Product Safety Commission to collect data on nonfatal occupational injuries through an occupational supplement to the National Electronic Injury Surveillance System (NEISS). NEISS collects data on injuries associated with consumer products or work that are treated in emergency departments from a sample of U.S. hospitals. From this sample, the total number of occupational injuries treated in hospital emergency rooms nationwide can be estimated. NIOSH publishes periodic reports based on these data and makes findings from 1998 forward publicly available through an interactive web-based application (CDC, 2017a) (Box 4-2). The data are also available to researchers for approved research projects. A significant advantage of this system, referred to as “NEISS-Work,” is that it captures information on all injured civilian workers who seek treatment in emergency departments, regardless of size of employer and nature of work or employment arrangement, and therefore includes workers who are excluded from the SOII, such as the self-employed or volunteers. Another advantage is that it does not require an employer to report or even be aware of the injury or for an employee to file a workers’ compensation claim. Also, information is abstracted from medical records and thus can be assumed to be more clinically accurate than employer-reported data. It has been estimated that approximately one-third of work-related injuries are treated in emergency departments (Jackson, 2001). While not all work-related injuries are captured in NEISS-Work, this system provides useful national estimates of the trends in nonfatal occupational injuries overall and by nature of injury and event, and demographic characteristics (see, for example, Table 4-2). Notably, findings from NEISS-Work provide a different picture of the trend in occupational injuries than that provided by the SOII. Whereas the SOII data indicate a downward trend in occupational injury rates since the early 1990s, NEISS rates have only more recently declined (Jackson, 2001; A. Reichard, NIOSH, personal communication, 2017). SOII and NEISS-Work injury rates by age also differ markedly. The findings from these two systems differ due to differences in the scope of the population covered and reporting by employers (Marsh et al., 2016; Rosenman, 2016; Tonozzi et al., 2016). A disadvantage of NEISS-Work is that information on occupation and industry has to be collected from the often incomplete medical record, making it less useful for targeting
prevention measures. Other disadvantages of NEISS-Work include a small sample size, lack of information about lost work time (other than limited information if the individual is hospitalized), and limited information about race and ethnicity. NEISS-Work does provide an important mechanism to conduct follow-back surveys of workers to obtain additional information, and NIOSH has conducted such surveys when additional resources have been available (Marsh et al., 2016). Recent follow-back studies by NIOSH found that the employers were aware of the injuries among their employees who were treated in the emergency departments and identified in the
NEISS system. Accordingly, any difference between the increased number of injuries identified in NEISS, as compared to the SOII, was not secondary to employers being unaware of the injury (Bhandari et al., 2016; Marsh et al., 2016; Tonozzi et al., 2016). NHTSA previously funded NIOSH to conduct targeted surveillance, including a follow-back survey of emergency medical service workers using NEISS-Work.
NIOSH supports additional focused activities to track nonfatal injuries in several industries. For example, as described, NIOSH funds the Center for Construction Research and Training, whose in-house data center uses a
| Characteristic | NEISS-Work (nonfatal injuries treated in EDs) | ||||
|---|---|---|---|---|---|
| Number | (95% CI) | %a | Rateb | (95% CI) | |
| Total | 34,000 | (±6,800) | 100 | 2.6 | (±0.5) |
| Men | 30,100 | (±6,300) | 89 | 4 | (±0.2) |
| Women | 3,900 | (±1,300) | 11 | 0.7 | (±0.2) |
| 20–34 | 11,000 | (±2,500) | 32 | 2.7 | (±0.5) |
| 35–44 | 9,900 | (±2,500) | 29 | 3.3 | (±0.6) |
| 45–54 | 7,100 | (±2,500) | 21 | 2.2 | (±0.5) |
| 55–64 | 4,400 | (±1,500) | 13 | 2.1 | (±0.5) |
| ≥65 | — | — | — | ||
| White, non-Hispanic | 19,900 | (±6,100) | 59 | 2.2 | (±0.4) |
| Other, non-Hispanic | 2,000 | (±1,000) | 6 | 0.9 | (±0.5) |
| Hispanic | 5,800 | (±2,800) | 17 | 3.1 | (±1.3) |
| Unknown | — | — | — | ||
NOTE: CI, confidence interval; ED, emergency department.
a Percentages might not sum to 100 because of exclusions and rounding.
b Per 10,000 FTE workers. Each injury is only counted once, regardless of the number of ED visits. Rates were calculated by CDC based on the number of injuries and the number of primary employed FTE workers from the BLS Current Population Survey, 2011. Variances for NEISS-Work data and CPS data were pooled to estimate the variance for injury rates.
SOURCE: Socias et al., 2014.
wide range of health, employment, and economic data sources to provide information about health and safety in the construction industry. Findings are routinely updated and published in an online chart book widely used by industry stakeholders (CPWR, 2013). Given the increasing recognition of the contribution of workplace violence to the burden of occupational injuries, NIOSH is also working with the Bureau of Justice, which conducts the National Crime Victimization Survey to improve and report on data on work-related violence.
The agricultural sector poses unique challenges for surveillance given the range of work settings from large industrial farms relying on a migrant workforce to small family farms where family members are also at risk. Additionally, the agricultural industry is exempted from many labor protection laws in the United States. Data on all farm-related fatalities are collected
in the multisource CFOI, which shows agriculture to have one of highest fatality rates of any industry sector. Data on nonfatal injures among agriculture workers are collected in the SOII, however, as described, this survey excludes all farms with fewer than 11 employees. Also, the injury and illness experience of owner-operator farms and family members who work on these farms is not captured as these farms do not meet the BLS criteria for an employer. Despite limitations, the SOII indicates that agriculture has one of the highest rates of nonfatal injuries and illnesses.
In the past, to provide information not available through the SOII, NIOSH conducted surveillance of injuries and illnesses among agricultural workers through a series of surveys carried out in collaboration with U.S. Departments of Agriculture and Labor, which were discontinued in 2015 due to fiscal constraints. NIOSH is currently considering alternative approaches to conducting surveillance of health and safety of production agriculture workers, including the potential role that its extramural program, specifically, the NIOSH-funded regional Agricultural Centers, might play (NIOSH, 2016c). The new proposed BLS household survey will also need to be evaluated on its ability to identify agriculture-related injuries and illnesses. Legislative changes that allowed BLS to survey employers with less than 11 employees would be useful but only partially effective to identify nonfatal cases missed in its employer survey, since it would not address the issue of the owner-operated farm that relies on family members.
Conclusion: Agriculture is a high-risk industry sector where a legislative restriction and particular work arrangements reduce the ability to obtain accurate counts of nonfatal injuries and illnesses. Future evaluations will need to be conducted to determine if recommended changes are sufficient to address the current limitations in OSH surveillance in agriculture.
State-Based Surveillance of Nonfatal Occupational Injuries
As described in Chapter 3, a small number of states, have established expanded case- and population-based surveillance systems for select occupational injuries and illnesses. While most of these expanded state programs focus on occupational illnesses, several states conduct injury surveillance and prevention activities addressing targeted injury types, populations at risk, or industries. State-based work-related injury surveillance makes use of records from a wide array of data sources—hospitals, emergency departments, poison control centers, and workers’ compensation systems—to identify and track injuries and to target intervention and prevention activities (see examples in Box 4-3).
Several of these focused state systems combine data to get a more comprehensive picture of the condition under surveillance than would be possible with any single data source, and all include intervention and prevention activities. Half of the fundamental state surveillance programs, supported by NIOSH, use available state data sources to generate a standard set of over 20 occupational health indicators (Thomsen et al., 2007; CSTE, 2017a). These include several measures of work-related injury risk, such as the number and rate of work-related hospitalization for severe traumatic injuries (Appendix D). Some fundamental state programs include targeted efforts focused on specific types of injuries. As described, a significant advantage of these state-based programs is the ability to identify and address local concerns working with other government agencies, policy makers, trade associations, unions, and community partners.
Workers’ compensation data have been used extensively for surveillance of work-related injuries, including musculoskeletal disorders, in several states, particularly where a state agency is the sole insurer for workers’ compensation, most notably, Washington State and Ohio. In 2015, NIOSH established a Center for Workers’ Compensation Studies to promote the use of these data to improve workplace safety and health in additional states (see Chapter 6).
Additional Surveillance Systems Relevant to Nonfatal Occupational Injuries
Some of the other surveys and data systems used by NIOSH to conduct surveillance of chronic disease (described in Table 4-3) also provide information on nonfatal and fatal occupational injuries. An advantage of such information that is collected within broader public health data systems is that, unlike employer-based reporting, it allows for the assessment of the contribution of work-related injuries to the overall injury burden in the United States. For example, a question about activity at time of injury in
TABLE 4-3 Examples of Surveillance Systems for Nonfatal Occupational Injuries in the United States
| Surveillance System | Scopea | Typeb | Responsible Agency(ies) | Condition(s) under Surveillancec |
|---|---|---|---|---|
| Survey of Occupational Injuries and Illnesses (SOII) | National,e 41 states and the District of Columbia | P | BLS* States* | O: Nonfatal work-related injuries (95%) and acute illnesses (5%) |
| National Electronic Injury Surveillance System—Occupational Supplement | National | P | NIOSH* CPSC* CDC | O: Work-related injuries treated in emergency departments |
| Targeted State-Based Injury Surveillance Systems | 3 states | P, C, varies by system | States* NIOSH* | Og |
| Severe Injury Reporting | National, State | C | OSHA* | O: Severe injuries (hospitalizations, amputations, eye loss) |
NOTES: Asterisk indicates funding agency. BLS, Bureau of Labor Statistics; CDC, Centers for Disease Control and Prevention; CPSC, Consumer Product Safety Commission; NIOSH, National Institute for Occupational Safety and Health; OSHA, Occupational Safety and Health Administration.
a Geographic levels at which findings are publicly available.
b P, population based: data are collected on a census or representative sample of a defined population and allows for assessing extent of a health-related event and monitoring trends with this population over time/locale; C, case based: focus of data collection is on individual cases that require follow-up or immediate public health action. These approaches are not mutually exclusive.
the core module of the National Health Interview Survey (NHIS) allowed researchers to estimate that 29 percent of all injuries among the working-age population occurred at work. Among employed men age 55 to 64 years of age, this figure was 49 percent (Smith et al., 2005). The National Center for Health Statistics (NCHS) is currently revising the NHIS and it is not clear whether this and other questions relevant to OSH surveillance will be retained in the core module (see further discussion of NHIS below).
Administrative databases originating in the health care system are yet another important source of information on work-related injuries but their
| Data Source(s) | Population Coveredd | Approach | Time Frame for Report Release |
|---|---|---|---|
| Employer reports | Most workersf | Sample | Annual |
| Emergency department records | All workers Special follow-back studies | Sample of 67 emergency departments nationwide | Intermittent |
| Multiple sources, vary by system | Varies by system | Census and some case series, varies by system | Varies by system |
| Employer reports | All workers covered by federal or state OSHA | Case series | Ad hoc |
c O, outcome; H, hazard; E, exposure.
d The population covered may include active and former workers, retirees, and others depending on the system.
e Information for Guam, Puerto Rico, and the U.S. Virgin Islands is collected and public but not included in national estimates.
f Excludes self-employed, workers on small farms, domestic workers, U.S. postal workers, and federal workers, approximately 9 percent of the U.S. workforce.
g Massachusetts, young worker injuries, and hospital worker injuries; Michigan, amputation, burns, crushing injuries, farm injuries, and skull fractures; Washington, trucking industry worker injuries.
use is currently limited by lack of information on work-relatedness in these records. Payment information in these data systems indicating workers’ compensation as payer can be used to identify some but not all work-related cases, as not all workers are covered under workers’ compensation, and some injured workers who are may not file claims or their claims may be denied (Spieler and Burton, 2012; Groenewold and Baron, 2013; Sears and Bowman, 2016). The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) includes a supplemental External Cause of Injury code—“External Cause Status”—that indicates
if injury occurred while engaged in civilian activity for pay or income. ICD-10-CM was implemented in clinical settings in the fall of 2016 and the extent that these codes are being used in various health data sources remains to be evaluated.
Conclusion: The use of the supplemental External Cause of Injury codes has substantial potential to enhance the utility of hospital inpatient, emergency department, and outpatient data systems for OSH surveillance.
Work-Related Musculoskeletal Disorders
NIOSH’s prioritization of research and prevention resources based on burden, need, and impact directs attention toward the detrimental impact that work-related musculoskeletal disorders (WMSDs) have on workers and social insurance systems. Current estimates of the significant burden of WMSDs come from the BLS Survey of Occupational Injury and Illness—31% of all occupational injuries (BLS, 2016g), state-based surveillance programs usually using workers’ compensation data—43 percent of compensable claims in Washington State (Marcum and Adams, 2017), and the National Health Interview Survey Occupational Health Supplement (CDC, 2017e). WMSDs likely strain the U.S. Social Security Disability Insurance (SSDI) System as the expiration of limited benefits provided for long-term disability under workers’ compensation are “taken-up” by benefits offered under SSDI (Reville and Schoeni, 2004; O’Leary et al., 2012).
Throughout their history NIOSH and OSHA have recognized work as a risk to musculoskeletal health (NIOSH, 1997). A comprehensive review by the National Research Council and Institute of Medicine addressed the work-relatedness of musculoskeletal disorders (NRC, 2001). This review gave recommendations to BLS to revise their data collection and reporting systems for more comprehensive surveillance of WMSDs and recommended for NIOSH a lead role in “developing uniform definitions of musculoskeletal disorders for use in clinical diagnosis, epidemiologic research, and data collection for surveillance systems.” Some of these recommendations to BLS and NIOSH are reiterated in this report, such as “including details on non-lost-workday injuries or illnesses (as currently provided on lost workday injuries) to permit tracking of these events in terms of the variables now collected only for lost workday injuries (age, gender, race, occupation, event, source, nature, body part, time on the job)” (NRC, 2001). The report also supported a broader surveillance approach recommending collection of additional information on the worker’s use of tools and technology, the organizational conditions under which work is performed and development of exposure assessment tools which could be used for hazard surveillance.
Under current OSHA recordkeeping requirements, establishment level WMSD data are not easily available and OSHA’s efforts to improve estab-
lishment level recordkeeping requirements identifying WMSDs on OSHA logs have not been successful (GAO, 2016). The OSHA log prior to 2001 had included a column for “repeated trauma cases,” which was inclusive of some MSDs but not all (GAO, 2016). OSHA’s 2001 revised recordkeeping regulation included a column to identify MSD cases, but was deleted in a 2003 amendment to the standard. In 2010, OSHA proposed to modify the Log 300 form to include a specific column to identify which injuries are MSDs, which would provide more complete information on the extent of MSDs both in the workplace and in the SOII, but due to opposition and intervention by Congress, this proposed addition has not been finalized.
In the second decade of the National Occupational Research Agenda (from 2006-2016; NORA), industry sector councils included WMSD surveillance and prevention as part of their research agendas. In both the second and the third upcoming decade of NORA, NIOSH has included a Musculoskeletal Disorders Cross Sector Council, which reinforces the ubiquitous, pervasive nature of risk factors for WMSDs in all sectors of the U.S. economy.
Conclusion: Work-related musculoskeletal disorders represent a large physical and economic burden on the U.S. workforce demanding a continued emphasis on surveillance of these disorders.
OCCUPATIONAL DISEASE SURVEILLANCE
Surveillance of diseases in which an occupational hazard or hazards were the cause or contributing factor is especially challenging because the illnesses of interest (e.g., coronary artery disease, chronic obstructive pulmonary disease [COPD], lung cancer, and renal failure) can often have many potential risk factors, including work, that can contribute to disease development, and there is often substantial lag time between initial exposure and disease onset. Limited emphasis on occupational health in medical school curricula leaves most physicians ill equipped to assess work-relatedness of multifactorial conditions, which adds to the challenge (Michas and Iacono, 2008). The importance of work among the causes for these multifactorial conditions is underappreciated. Estimates of the preventable causes of these conditions generally ignore the impact of work resulting in incidence, prevalence, and mortality estimates that fail to identify primary prevention opportunities in the workplace. While the fraction of multifactorial illnesses that can be attributed to work may be small for common conditions such as lung cancer, workplace exposures may still account for a substantial human and economic burden. For example, consensus statements from the American Thoracic Society (ATS) based on the review of the medical literature have concluded that 15 percent of new-onset asthma among adults is caused by workplace exposures and that
another 25 percent of adult asthma is work aggravated (Balmes et al., 2003; Torén and Blanc, 2009; Henneberger et al., 2011; Blanc, 2012). Similarly, the ATS and others have estimated that work exposures contribute to at least 15 percent of COPD cases (Hnizdo et al., 2002; Balmes et al., 2003; Raherison and Girodet, 2009). Other estimates of the attributable risk of work have been developed: 6.3 to 18 percent of coronary artery disease deaths, and 8.2 to 14.5 percent of chronic renal failure deaths (Steenland et al., 2003). A recent systematic review that covered 46 years and 8,000 published studies found good evidence for the role of a variety of chemical exposures in heart disease, pulmonary heart disease, stroke, and high blood pressure (SBU, 2017).
In considering surveillance of long-latency conditions, it is useful to distinguish between diseases (such as silicosis and coal workers’ pneumoconiosis) that are almost invariably work related, and the diagnosis itself as an indicator for work-relatedness (pathognomonic occupational diseases) and multifactorial diseases for which occupational causes are only one of a number of contributing factors. Approaches to surveillance of the long-latency work-related pathognomonic diseases and common multifactorial diseases differ markedly. For pathognomonic diseases, data sources such as hospital discharge records that include diagnostic information can be used for surveillance to assess extent of the condition. Surveillance of multifactorial diseases is much more challenging. For conditions with known occupational etiology and a relatively high fraction attributed to work such as asthma or COPD, case-based approaches that involve follow-up with individuals or their providers to ascertain work-relatedness and sources of exposure are feasible. Also, surveillance of exposures can be a useful adjunct (see discussion of hazard and exposure surveillance below).
Surveillance of common multifactorial conditions, where the occupational contributions are less well studied but where the conditions are prevalent in the adult population (e.g., coronary artery disease, mental disorders) has generally been restricted to monitoring patterns of disease in relation to basic employment information (e.g., usual industry and occupation). Results from these efforts have been used to generate hypotheses about potential occupational associations that inform research priorities, and the approach may identify statistical aberrations (hot spots) that warrant follow-up. Research on cardiovascular disease (Fang et al., 2010; Costello et al., 2016; Du et al., 2016) and mental disorders (LaMontagne et al., 2008; Cohidon et al., 2012; Niedhammer et al., 2014; Theorell et al., 2015) has identified work-related risk factors that could be incorporated into surveillance efforts. For example, increased risk of cardiovascular disease among those exposed to fine particulates and of mental health problems among those working in stressful environments. In such efforts, disease and exposure information would need to be linked (see Chapter 6).
There are opportunities to advance knowledge about the importance of occupation as a contributor to many health conditions that have multifactor etiology with more extensive information about the employment history of individuals. The occupational medicine community has long advocated the collection of a more extensive occupational history in the individual patient’s medical record. These efforts have focused primarily on physician education but with little success. The potential of obtaining occupational information systematically through the electronic health record (EHR; see Chapter 6) offers a new opportunity to expand understanding of the relationship of work to chronic health conditions. Once in the EHR, current occupational information and, more importantly, the development of full occupational histories will permit examination of specific common conditions to seek important signals of occupational factors. Once noted, these can be tracked, hot spots can be identified, and formal etiologic studies can be planned.
It has been long recognized that the SOII is not an adequate source of information on occupational illnesses. The SOII captures only a limited percentage of acute illnesses such as dermatitis and few of the long-latency occupational illnesses with some relationship to work (Windau et al., 1991; Luckhaupt et al., 2013a; Alarcon, 2016). Although the 1987 NRC report recommended that NIOSH take the lead in occupational disease surveillance and develop a comprehensive national surveillance system using a wide variety of data, this funding to do so has not been provided to NIOSH. Rather, over the past several decades, NIOSH has taken more limited steps to advance surveillance of occupational disease.
The major strategies used by NIOSH have been to leverage use of existing health data sources and surveys and to support state health agencies in building case- and population-based surveillance systems for select occupational health conditions. Key systems and approaches currently in place are listed in Table 4-4 and described briefly below.
Death Certificate Data
Since 1980, NIOSH has partnered with up to 30 states and the NCHS to obtain death certificate data and to code the narratives in these records on usual industry and occupation according to the Census Bureau’s Industry and Occupation classification system. The death certificate data from these states (including underlying and contributory causes of death, demographic data, and usual industry and occupation information) serve as the basis for the NOMS system which is used by NIOSH to monitor trends in chronic disease and other causes of mortality by occupation and industry. Occupational diseases such as asbestosis or silicosis that are almost always work related can also be characterized. NIOSH and other researchers have
TABLE 4-4 Examples of Surveillance Systems for Occupational Illnesses in the United States
| Surveillance System | Scopea | Typeb | Responsible Agency(ies) | Condition(s) under Surveillancec |
|---|---|---|---|---|
| National Health Interview Survey Periodic (5-year) Occupational Health Supplement | National | P | NCHS* NIOSH* | O, H Multiple outcomes and hazards that vary with NIOSH supplement |
| Adult Blood Lead Evaluation and Surveillance Program | 26 states (and aggregated) | P, C | NIOSH* States* | E: Elevated blood levels |
| SENSOR Pesticide Surveillance | 12 states (and aggregated) | C, P | NIOSH* EPA* States | O: Occupational pesticide-related injury and illness |
| Work-related asthma surveillance | 5 states (and aggregated) | C, P | NIOSH* States | O: Asthma caused or exacerbated by work |
| Multisource silicosis surveillance | Michigan | C, P | NIOSH* State | O: Silicosis morbidity and mortality |
| Sharps injuries (blood-borne pathogen exposure) among hospital workers | Massachusetts | P | NIOSH* State* | E: Injuries due to contaminated needles and other sharp devices |
| National Occupational Mortality Surveillance (NOMS) | Aggregated data from 17 statesf | P | NIOSH* NCHS* | O: Chronic disease deaths by industry and occupation |
| Data Source(s) | Population Coveredd | Approach | Time Frame for Report Release |
|---|---|---|---|
| In-person household survey | Adult civilian population living in U.S.e | Sample | Intermittent |
| Clinical laboratory reports | All adults age *16 | Census | Annual |
| Multiple data sources | All workers | Case series | Intermittent |
| Multiple data sources: provider case reports, hospital, workers’ compensation records, etc. | All workers | Case series | Annual |
| Multiple data sources: provider case reports, hospital workers’ compensation records, death certificates | All workers | Census | Varies by state |
| Mandated sharps injury logs maintained by acute and chronic care hospitals | All workers in hospitals including students in training | Census | Annual |
| Death certificates | All workers | Census | Intermittent |
| Surveillance System | Scopea | Typeb | Responsible Agency(ies) | Condition(s) under Surveillancec |
|---|---|---|---|---|
| National Occupational Respiratory Mortality Surveillance (NORMS) | National and state, some county level data | P | NIOSH* NCHS* | O: Pneumoconiosis, hypersensitivity pneumonitis and mesothelioma deaths; other respiratory disease deaths by industry and occupation |
| Occupational Cancer Surveillance | 5 states aggregatedg | P | NIOSH* NIOSH* | O: Cancer incidence by industry and occupation |
| Hearing loss surveillance | National | P | NIOSH* | O: Hearing loss |
NOTES: Asterisk indicates funding agency. NCHS, National Center for Health Statistics; NIOSH, National Institute for Occupational Safety and Health; OSHA, Occupational Safety and Health Administration.
a Geographic levels at which findings are publicly available.
b P, population based: data are collected on a census or representative sample of a defined population and allows for assessing extent of a health related event and monitoring trends with this population over time/locale; C, case based: focus of data collection is on individual cases that require follow-up or immediate public health action. These approaches are not mutually exclusive.
published studies based on analyses of these data that have both confirmed previous risks and pointed to new associations that require further research (Dubrow et al., 1987; Blair et al., 1993; CDC, 1995; Burnett et al., 1997; Savitz et al., 1998; Colt et al., 2001; Luckhaupt and Calvert, 2008; Robinson et al., 2015). Findings are periodically updated and made available on an interactive NIOSH website (Box 4-2).
Electronic death registration systems, now implemented in most states, provide NIOSH with the opportunity to include more states and provide more timely coded industry and occupation data (PHII, 2016). NIOSH is planning to conduct a pilot effort with NCHS in 2018 to apply computer-assisted coding tools to code all industry and occupation data collected in real time from the 17 states now participating in NOMS. If successful, this
| Data Source(s) | Population Coveredd | Approach | Time Frame for Report Release |
|---|---|---|---|
| Death certificates | All workers | Census | Intermittent |
| State cancer registries | All workers | Census | Intermittent |
| Sample of audiometric service providers and U.S. Air Force | All workers | Case series | Peer-reviewed papers |
c O, outcome; H, hazard; E, exposure.
d The population covered may include active and former workers, retirees, and others depending on the system.
e Noninstitutionalized population.
f Number of participating states has varied over time.
g Previously one state; pilot under way expanding to five states.
partnership will provide the opportunity to analyze mortality patterns by industry and occupation in all 50 states.
The National Occupational Respiratory Mortality System (NORMS) is an interactive data system that is based on mortality data from death certificates provided to NIOSH annually by the NCHS (see Box 4-2). This national database contains information about deaths from 1968 forward with underlying or contributory causes of death from select respiratory conditions known to be associated with work: pneumoconiosis, hypersensitivity pneumonitis (since 1979), and mesothelioma (since 1999) (Figure 4-4). Counts, age-adjusted rates, and potential years of life lost for all U.S. residents and some states and counties by age, gender, and race are generated from the database for various time periods and included in NIOSH’s electronic Work-Related Lung Disease Surveillance System (eWoRLD), an
interactive web-based application that presents data on both occupational morbidity and mortality due to respiratory disease (NIOSH, 2017d; see Box 4-2). The national database does not include information about the usual industry and occupation of the decedent. To address this, data from states participating in NOMS (see above) are incorporated in the NORMS system and used to monitor mortality patterns of a broader range of respiratory diseases by industry and occupation. This “industry and occupation database” includes information on deaths due to chronic obstructive lung disease, asthma, influenza, lung cancer, mycobacterial infection, pleural plaques,
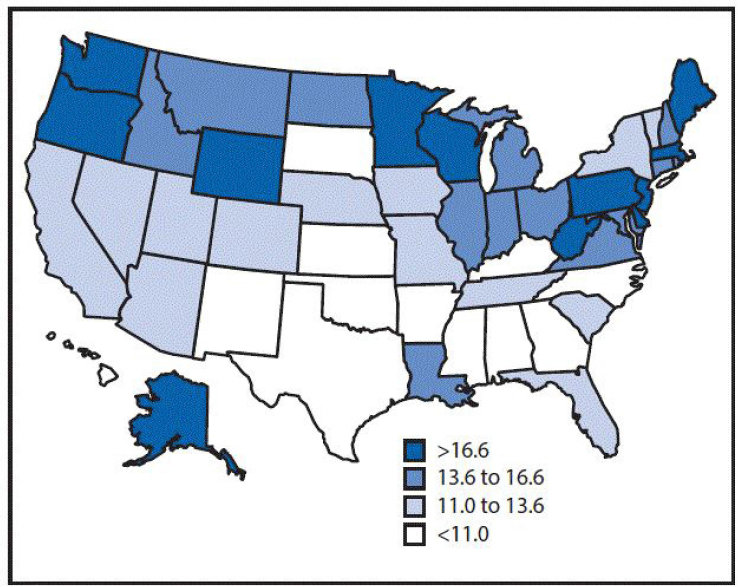
*Age-adjusted death rates were calculated by applying age-specific death rates to the 2000 U.S. standard population age distribution (CDC, 2017f). In two states (Maine and Washington), the age-adjusted death rate exceeded 20 per million per year. †Decedents aged ≥25 years for whom the International Classification of Diseases, 10th Revision, codes C45.0 (mesothelioma of pleura), C45.1 (mesothelioma of peritoneum), C45.2 (mesothelioma of pericardium), C45.7 (mesothelioma of other sites), or C45.9 (mesothelioma, unspecified) were listed on death certificates were identified using CDC multiple cause-of-death data for 1999-2015. SOURCE: Mazurek et al., 2017.
and tuberculosis in addition to the work-related respiratory diseases named above. Surveillance findings from this database, including proportionate mortality ratios for respiratory diseases by industry and occupation for several time periods, are likewise included in the eWoRLD. NORMS also includes tools for data users including crosswalks for comparing changes in the Census Bureau’s Industry and Occupation Classification System codes over time (1990 and 2000 revisions) and Census population estimates used by the system in calculating mortality rates.
Health Survey Data
The NHIS has been used by NIOSH and others to assess workers’ health. The NHIS is an ongoing annual household survey of approximately 35,000 households and 87,500 individuals conducted by the NCHS (NCHS, 2016). The survey is designed to represent the civilian noninstitutionalized population residing in the United States at the time of the interview. Its primary objective is to obtain national estimates of health care utilization, health conditions, health status, insurance coverage, and access, as well as to monitor trends in illness and disability in the nation. The NHIS consists of a core set of questions that have remained relatively unchanged along with supplemental questions that vary. Historically the core questions have collected basic employment information (employment status, current occupation, and industry) so that NHIS data from every year could be used to study general trends in chronic disease and other health conditions by industry and occupation. NIOSH has periodically analyzed data from this general health section to provide baseline information on the health status of the workforce in major industry sectors (see Table 4-5). As mentioned above, the NHIS is currently undergoing revision and the most recent proposal is to collect industry and occupation information on a rotating basis (NCHS, 2017). This would substantially reduce the utility of the data for examining not only health outcomes and disability but health care access and utilization as well as work-related health behaviors.
Periodically NIOSH funds occupational health supplements (NHIS-OSH) to collect national-level data on various occupational health outcomes and exposures, focusing on information not available in the SOII (NIOSH, 2016d).
An advantage of collecting supplemental OSH data through the NHIS is that the data can be used to provide current national estimates on the prevalence of common work-related health conditions and exposures by industry and occupation (CSTE, 2013a). NIOSH also uses such data to assess progress in meeting the Healthy People 2020 objective concerning patient-physician communication regarding asthma and work (HHS, 2017). Additionally, NIOSH researchers have used the data for topical research,
TABLE 4-5 Prevalence of Selected Health Conditions, Work Organization and Psychosocial Factors, and Physical and Chemical Exposures Among U.S. Workers (health care sector versus all U.S. workers, 2010), Occupational Health Supplement to the National Health Interview Survey
| Prevalence (%) | All U.S. Workers | Health Care Sector | |
|---|---|---|---|
| Prevalence (%) | Prevalence (%) | ||
| Health Conditions | In the past 12 Monthsa | ||
| Dermatitis | 9.8 | 11.7 | |
| Carpal tunnel syndrome | 3.1 | 3.3 | |
| Current asthma | 7.2 | 8.7 | |
| Injury or poisoning at work | 2.8 | 3.6* | |
| Work Organization Factors | Work ≥60 hours a weekb | 7.2 | 5.3 |
| Work ≥48 hours a weekb | 18.7 | 14.4 | |
| Nonstandard work arrangementsa | 18.7 | 10.7 | |
| Temporary employmenta | 7.2 | 3.9 | |
| Nonstandard shiftsa | 28.7 | 29.0 | |
| Psychosocial Exposures | Job insecurityc | 31.7 | 22.8 |
| Work-family imbalancec | 16.3 | 16.9 | |
| Hostile work environmentsa | 7.8 | 9.1 | |
| Physical/Chemical Exposures | Exposure to potential skin hazards at worka | 20.6 | 25.7 |
| Exposure to secondhand smoke at workd | 10.0 | 8.3 | |
| Exposure to outdoor worka | 24.7 | 6.9 | |
| Exposure to vapors, gas, dust, or fumese | 25.0 | 14.2 | |
a Among U.S. adults who have worked in the past 12 months.
b Among U.S. adults who have worked in the past 12 months, who only held one job.
c Among U.S. adults who were employed in the week prior to interview.
d Among nonsmoking U.S. adults who have worked in the past 12 months.
e Exposure during longest-held job (all other exposures refer to current or most recent job).
* These estimates have a relative standard error >30% and <50% and should be used with caution as they do not meet NCHS reliability/precision standards.
SOURCE: NIOSH, 2013.
including, for example, the congruence between current and usual occupation, and links between workplace mistreatment and sickness absenteeism (Luckhaupt et al., 2013b; Asfaw et al., 2014). The implementation of the OSH supplement on an ad hoc basis has been identified as problematic (CSTE, 2013a). There is a need for an ongoing NIOSH commitment to periodically incorporate the OSH supplement in the NHIS if this approach is to provide information about trends over time. With this recognition, NIOSH plans to support the supplement every 5 years; however, there is concern about funding as the survey costs are substantially increasing (Schnorr, 2016). Also, the wide range of potential questions related to occupational safety and health in light of the need to limit survey length raises challenges in consistently collecting data over time.
Conclusion: Pending the outcome of the proposed BLS pilot household survey, the periodic administration of the OHS supplement would need to be re-evaluated.
NIOSH is engaged in a number of additional activities to incorporate occupational information in existing health surveys and data systems. These are described in Chapter 6.
Medical Monitoring Program Data
Several ongoing programs that routinely monitor worker health in specific industries provide data useful for occupational health and safety surveillance. The NIOSH Coal Workers’ Health Surveillance Program is a medical monitoring program established by the Federal Coal Mine Health and Safety Act of 1969 (P.L. 91-173; NIOSH, 2017e). The intent is to prevent early coal workers’ pneumoconiosis from progressing to a disabling disease. From 1971-2014, the program provided surveillance services to active underground coal miners that included occupational histories and chest radiographs classified for chances of pneumoconiosis by physicians with special training and certification by NIOSH (B readers10). New miners were required to participate in the program when first employed (preplacement) and at 3 years after hire, they were able to participate on a voluntary
___________________
10 A “B reader” is a licensed physician who has passed a test classifying 125 chest films for the presence and severity of findings associated with pneumoconiosis, based on a standardized classification system maintained by the International Labour Organization (ILO). The B reader maintains certification by passing a test classifying 75 chest films for pneumoconiosis every 4 years. Although the testing/certification is part of regulations administered by NIOSH for providing medical examinations to coal miners, OSHA medical monitoring regulations for silica exposed workers require that a B reader classify the chest radiograph. For asbestos exposed workers, OSHA requires that a B reader, a board eligible/certified radiologist, or an experienced physician with known expertise in pneumoconiosis use the ILO system to classify the chest radiograph.
basis at about 5-year intervals thereafter. In 2014, the program expanded to provide services to active surface coal miners and to add spirometry and respiratory health questionnaires to surveillance services. NIOSH compiles the data to describe the prevalence of coal workers’ pneumoconiosis and disseminates findings through a data query system (see Box 4-2). Despite the success in using these B-reader reports to conduct surveillance for coal workers’ pneumoconiosis, no similar program has been set up for other common pneumoconiosis such as asbestosis or silicosis.
NIOSH has also encouraged large audiometry-testing firms to participate in a surveillance system for noise-induced hearing loss. These firms voluntarily submit audiometric hearing tests. The results have been published in peer-reviewed publications (Masterson et al., 2014). Results are analyzed by geographic regions and industry sector. NIOSH has used data from the National Health and Nutrition Examination Survey to examine the prevalence of hearing loss by occupation and industry (Tak et al., 2009); individual states have used the Behavioral Risk Factor Surveillance System (BRFSS) data (Stanbury et al., 2008) and case-based reporting by audiologists (MSU and MI DELEG, 2009).
OSHA requires medical monitoring of workers exposed to a number of hazards, including asbestos, noise, and silica. The asbestos and silica regulations require both chest radiographs and spirometry. The noise regulation requires audiometric testing. There is, however, no provision in these regulations to collect the results of the medical testing and use the data for surveillance of these conditions. In addition to mandatory medical monitoring programs, NIOSH, medical specialties and industry trade groups have developed recommended medical monitoring for individuals working with multiple substances, for example diacetyl and isocyanates.
Conclusion: NIOSH has effectively used the results from a mandatory medical monitoring program for coal miners and a voluntary program for noise exposed workers for occupational illness surveillance. Use of the results of mandatory medical monitoring required by OSHA and the recommended medical monitoring conducted by employers has the potential to improve surveillance data for selected occupational illnesses.
Infectious Disease Surveillance
Infectious diseases can be an important public health problem in many different work settings (Molinari et al., 2007; Keech and Beardsworth, 2008; Edwards et al., 2016). Some work environments present increased risk of select infectious diseases. For example, livestock workers have been shown to be at risk of methicillin-resistant Staphylococcus aureus infections, hepatitis, Q fever, leptospirosis, and antibiotic-resistant Escherichia coli (Klous et al., 2016). Child care workers are at risk of several infectious
diseases: cytomegalovirus through contact with toys or diaper changes, hepatitis B and C, and human immunodeficiency virus (HIV) transmitted through blood, and a variety of enteric pathogens such as hepatitis A, cryptosporidium, giardia, shigella, campylobacter, enteroviruses, and rotavirus transmitted by fecal-oral contamination through diaper changes or via sink faucets and the hands of child care workers or children (Reves and Pickering, 1992; Churchill and Pickering, 1997; Cordell et al., 2004). Health care workers can be exposed to several infectious agents through sharp injuries (e.g., HIV, hepatitis B virus, and hepatitis C virus; NIOSH, 2017f) as well as through direct patient care (e.g., pertussis and meningococcus) and the contaminated environment (e.g., Clostridium difficile) (Weber and Rutala, 2016). And both health care workers and corrections officers are at increased risk for tuberculosis (IOM, 2001; NIOSH, 2016e).
The workplace can also be a critical locus for transmission of infectious disease, regardless of initial causation. For example, the annual epidemics of influenza A that are tracked around the world impact workplaces of many types. Influenza can lead to pneumonia and dehydration and can worsen long-term medical conditions, such as congestive heart failure, asthma, or diabetes. Timely information about work-related transmission of infectious diseases can be strategically important to facilitate rapid assessment and intervention to control the spread of disease to other workers and the public, particularly workers in critical and public-related services such as health care, medical waste treatment, emergency response, postal and package delivery, utilities, and transportation.
In the United States, state, local, and territorial public health agencies take the lead on receiving cases of specified infectious conditions. The Council of State and Territorial Epidemiologists (CSTE) is responsible for defining and recommending which diseases and conditions are nationally notifiable and reported to the Centers for Disease Control and Prevention (CDC). All but five of the nationally notifiable diseases are infectious diseases. States voluntarily report these conditions to disease-specific CDC programs through the National Notifiable Diseases Surveillance System (NNDSS).
Of the 90 conditions included in the NNDSS, approximately 36 include some information on work largely because of one or more specific work relationships. As noted, information about work is important not only in identifying the exposure source for reported cases but to address the workplace as a locus of potential disease transmission. However, the occupational data collected currently are not harmonized across conditions nor coded using a standard coding system. CDC is undergoing an agency-wide effort both to harmonize the variables collected in its surveillance systems and to improve the NNDSS technological infrastructure by basing it on interoperable, standardized data and exchange mechanisms. CSTE has
recommended that CDC incorporate industry and occupation and other work information as appropriate in CDC surveillance systems as feasible (CSTE, 2014). This ongoing work provides an important opportunity for NIOSH and its state partners to influence collection and harmonization of industry and occupation information for conditions within the NNDSS. There appears to be increasing recognition that standardized collection and coding of industry and occupation information could substantially enhance surveillance of infectious diseases in relation to work, a significant gap in OSH surveillance. NIOSH and CSTE are currently engaged with colleagues at CDC to identify next steps to be taken to move this forward. In a related effort, they are also collaborating in the development of a Reportable Condition Knowledge Management System, a system designed by CSTE as a web portal for public health agencies to manage reporting criteria to facilitate automatic electronic case reporting of reportable and notifiable conditions documented in electronic health records (CSTE, 2017b).
On another front, given the multiple hazards, including exposure to infectious disease, faced by heath care workers, NIOSH has developed the Occupational Health Safety Network (OHSN). OHSN is a web-based application to collect standardized data from employers on common work-related injuries and illnesses among hospital workers, which includes a module to collect information on injuries from contaminated needles and other sharp devices (sharps injuries). A convenience sample of 114 hospital systems (2014 data) is currently reporting data through OHSN. As part of its state-funded activity, NIOSH also contributes to the support of the Sharps Injury Surveillance System in Massachusetts. State law in Massachusetts requires hospitals to report case-level data on all sharps injuries to the state health department annually. Sharps injury surveillance is essentially an exposure surveillance system, as the focus is not on the injury or the development of an infection but the sharp injury as an indicator of potential exposure to blood-borne pathogens.
OSH surveillance programs in state health agencies may also collaborate with their infectious disease programs to investigate and address clusters of infectious disease in the workplace. For example, occupational safety and health staff worked with infectious disease colleagues in California to identify, investigate, and prevent coccidioidomycosis among construction workers in the solar industry (Wilken et al., 2015).
Conclusion: Further work is needed to increase collaboration between infectious and occupational public health programs at the state and federal levels to ensure that information on work is regularly collected and considered as part of infectious disease surveillance activity, including investigations.
State-Based Surveillance Systems for Occupational Disease Surveillance
Approximately 10 states have built on mandatory state disease reporting requirements to implement case-based surveillance of selected occupational disease using a model initially developed by NIOSH—the Sentinel Event Notification System for Occupational Risks (SENSOR) (Rutstein et al., 1983; Baker, 1989). This model is based on the concept of a sentinel health event in which a single event is considered a sentinel or warning sign that the prevention system has failed and follow-up with the worker and/or the worksite may be warranted to prevent additional cases (Baker, 1989). Initially based primarily on case reporting by health care providers, the model has evolved over time to include use of multiple sources such as death certificates, administrative data sources such as statewide hospital data sets and worker’s compensation records, laboratory reports, and other sources such as calls to poison control centers and agricultural extension programs for case ascertainment, e.g., silicosis (Schleiff et al., 2016). NIOSH identifies national priorities for targeted funding and states have the option of proposing their own targets. Case definitions for surveillance, which have been developed by NIOSH and the states, are used to confirm cases. Case follow-up may include public health investigations of the worksite, referrals to OSHA or other agencies to control exposures and protect other workers at risk, and steps to ensure the affected individual has appropriate medical treatment. Follow-up also allows for collection of additional data to better understand the epidemiology of the disease. Summary data are used by states to target broader-based prevention efforts and have included, for example, dissemination of prevention recommendations; changes in state policies; and educational outreach to employers, workers, and health care providers. While data from case-based surveillance may or may not be complete or representative, summary findings can identify new hazards and provide important, otherwise, unavailable information to inform prevention efforts (Rosenman et al., 2003).
Currently state-based surveillance systems are in place for surveillance of work-related lung disease, with a focus on asthma and silicosis, and pesticide-related injury and illnesses. All use multiple data sources for case ascertainment and data to inform prevention efforts. Participating states also submit their data to NIOSH for aggregation and analysis to gain a broader understanding of the problems, fill gaps in national level surveillance, and foster prevention activities such as those described in the following examples. Findings of work-related asthma associated with cleaning products in multiple states have led to changes in national policies regarding certification of products as “green cleaners” only if they contain no known asthma-causing chemicals (Green Seal Institutional Cleaning Products, 2017). Data from multiple states on illness associated with the
use of pesticide-releasing foggers led the Environmental Protection Agency to issue new requirements for product labeling to improve user understanding of risks and safe use (CDC, 2008).
Additionally, 28 states participate in the NIOSH Adult Blood Lead Epidemiology and Surveillance (ABLES) program (2015 data). These states require clinical laboratories to submit reports of blood lead tests in both adults (and children) to a state health agency. Blood lead levels (BLLs) at or above the reference level of 5 µg/dL are considered an indicator of exposure (CSTE, 2015b). Laboratory reports generally do not contain information about the industry or occupation of the affected worker. States conduct follow-up of individual cases based on blood lead levels to ensure adequate medical treatment and removal from exposure and to identify the source of exposure, including industry of the affected worker, and to control exposures. Many state health agencies work with OSHA to conduct follow-up in workplaces where cases were exposed to lead. Summary data are used to monitor trends and to identify high-risk industries and communities for outreach. States participating in ABLES submit their data to NIOSH and summary findings are published annually (Alarcon, 2016). The NIOSH ABLES program, which provides resources for adult blood lead surveillance in most of the participating states, reports that the program has contributed to a greater than 60 percent decline in the prevalence of BLLs ≥25 μg/dL among adults in the United States from 1994 through 2013 (NIOSH, 2016f) (see Figure 4-5) A limited number of states have developed similar laboratory-based surveillance systems for other metals such as cadmium and mercury (e.g., Michigan and New York; MI DHHS, 2015; New York State Department of Health, 2016).
The occupational health indicators generated by NIOSH-funded OSH programs in about half the states include measures of several diseases almost always caused by work such as mesothelioma and asbestosis as well as elevated blood lead levels in adults and occupationally related calls to poison control centers (Appendix D).
Summary
In echoing the conclusions of the 1987 NRC committee, there are no modifications of the BLS employer survey that would enable it to measure the occurrence of occupational illnesses. Studies have documented that the SOII only captures a limited percentage of acute illnesses and is even less useful in counting long-latency occupational illnesses. Individual states and NIOSH collect occupational illness surveillance data but the data are not compiled and findings regularly released. Individual research publications, surveillance reports, and web applications are used to disseminate findings
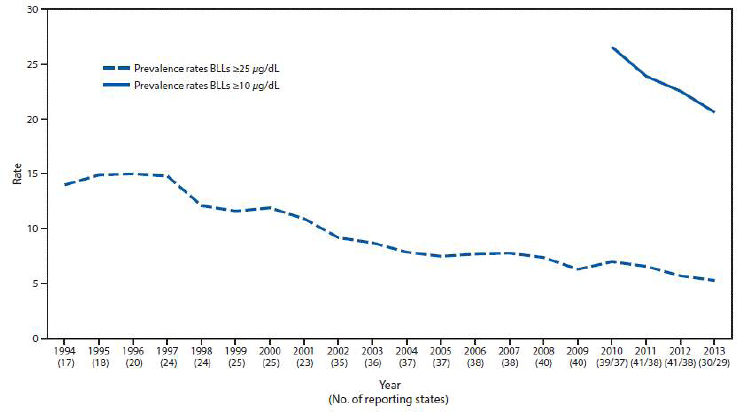
*Per 100,000 employed adults aged ≥16 years. Denominator data extracted from 2015 U.S. Department of Labor, Bureau of Labor Statistics Local Area Unemployment Statistics (LAUS) program (http://www.bls.gov/lau/staadata.txt).
†Since 2009, the case definition for an elevated blood lead level is a BLL ≥10 µg/dL. For historical comparisons, prevalence rates at the previous case definition (BLL ≥25 μg/dL) are provided.
NOTE: A total of 30 states submitted data in 2013 (down from 41 states in 2012): Alabama, Alaska, Arizona, California, Colorado, Connecticut, Florida, Georgia, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Missouri, Nebraska, New Jersey, New Mexico, New York, North Carolina, Oklahoma, Oregon, Pennsylvania, Vermont, Washington, Wisconsin, and Wyoming. Massachusetts provided data for BLLs ≥ 25 µg/dL. For 2013, the first number is the number of states reporting BLLs ≥ 25 µg/dL (i.e., 30 states in 2013), and the second number is the number of states reporting BLLs ≥ 10 µg/dL (i.e., 29 states in 2013).
but not with all occupational illnesses combined, not in conjunction with the release of the BLS SOII data, and not on a regularly scheduled basis.
Recommendation B: NIOSH, working with the state occupational safety and health surveillance programs and across divisions within the agency, should develop a methodology and coordinated system for surveillance of both fatal and nonfatal occupational disease using multiple data sources. The data should be analyzed, interpreted, and presented regularly in a comprehensive public report.
The data sources to be considered should include reporting by audiometric providers, disease registries (such as cancer and chronic renal failure), hospitals, laboratories, physicians, poison control centers, and health surveys as well as appropriate exposure databases. It is important that illness data collected by the states and NIOSH be analyzed and released in a timely manner. The data should be released in conjunction with BLS illness data in a manner that does not delay data released by BLS.
In the near term:
- NIOSH should combine information from the existing focused occupational disease surveillance systems (e.g., ABLES, pesticide illness, silicosis surveillance, and NORMS) and mesothelioma from cancer registries and other relevant occupational health indicators to provide a more comprehensive annual report on the extent of occupational illness morbidity and mortality that can be released in conjunction with information from the SOII. Methods for extrapolating from available data to generate national estimates should be explored.
- To enhance surveillance of occupational lung disease, NIOSH should require all B readers to report all chest radiographs interpreted to be positive for all types of pneumoconiosis.
- Increased collaboration between NIOSH and CDC infectious disease surveillance programs, with improved collection of occupational information, will be important to improve documentation of endemic and epidemic infectious disease related to work.
In the longer term:
- Gaps identified in the occupational illness surveillance system will need to be addressed through future developments that may involve
- New or modified state regulations, requiring close coordination with the states, many of which have already promulgated reporting regulations.
- Inference of occupational disease burden and trends that result from enhanced exposure assessment (Recommendation H, see Chapter 6).
- Updating the list of occupational sentinel health events, establishing additional criteria for establishing a link between workplace exposures and common diseases.
- Action on recommendations that address the inclusion of occupational information in medical records (Recommendation J, see Chapter 7), federal health surveys and public health surveillance systems (Recommendation M, Chapter 7), and automated coding of the industry and occupa-
- tion information (Recommendation L, see Chapter 7) will be important for ensuring the optimal implementation over time of this recommendation.
OCCUPATIONAL HAZARD AND EXPOSURE SURVEILLANCE
Occupational hazard surveillance is the systematic assessment of the occurrence of workplace risks with potential to contribute to health, disease, and injury among working populations. Exposure surveillance measures actual risk by including distribution of, and the secular trends in exposure to workplace risks. In a public health context, hazard or exposure surveillance identifies settings or individuals exposed to hazardous levels of specific agents allowing for intervention to reduce risk. While there is no comprehensive occupational exposure surveillance system in the United States, the concept has been discussed over the past several decades and was included in the 1987 NRC report.
Risk is defined as the combination of hazard and exposure. A hazard is a substance or condition with an inherent ability to harm; for example, in the case of chemicals, the material’s toxicity is the point of reference, while for radiant energy, the wavelength determines the hazard. Harm results when individuals or populations come into contact with, and are exposed to, the hazard. Both the intensity and the duration of exposure are important to determine. For some hazardous exposures the harm can just be acute (e.g., acute poisoning by carbon monoxide), for others the harms are cumulative or latent and cause or contribute to chronic disease (e.g., asbestos), and for others the harm may be both acute and chronic (e.g., lead).
The 1987 NRC report identified hazard and exposure surveillance as a priority and presented four recommendations:
- OSHA should include quantitative exposure information in its publicly available database.
- OSHA should require submission of all exposure measurements required by industry in complying with OSHA standards.
- NIOSH should compile and publish exposure data collected during health hazard evaluations as well as analyze these data to characterize the evaluated industries.
- NIOSH should include quantitative exposures in any future occupational hazard surveys.
Opportunities for creating systems to address these recommendations have been challenging; nevertheless, significant advances have been made. OSHA responded positively to the recommendations by including quantitative industrial hygiene measurements in their publicly available Integrated
Management Information System (IMIS), and these data are now being explored by researchers for quality and potential intervention research approaches. In addition, IMIS data are being used for surveillance purposes by NIOSH researchers that are focused on respiratory health and on surveillance. However, the specific goals and procedures for use of these data for ongoing surveillance have not been defined. In addition, NIOSH has compiled and created exposure-specific databases derived from the health hazard evaluation (HHE) investigations and to date has posted data for lead and noise (NIOSH, 2015b). Data on formaldehyde exposures are expected to be posted soon.
Large-scale hazard surveys, such as the National Occupational Hazard Survey (NOHS) and the National Occupational Exposure Survey (NOES) (see also Chapter 6), have not been conducted since the 1980s and those data, which were widely used, are now considered out of date and of limited utility (NIOSH, 1974; NIOSH, 2017g). In 2011, NIOSH conducted a web-based survey of health care workers—the Health and Safety Practices Survey of Healthcare Workers—to evaluate the extent of the use of well-known precautionary practices to minimize exposure to chemical hazards (NIOSH, 2017h). The primary lessons learned were that
- recommended exposure controls are not always implemented by the employer or employees;
- barriers to use of personal protective equipment (PPE) include that PPE is not provided or the perceived risk of exposure is underestimated, even for highly toxic chemicals such as chemotherapeutic drugs; and
- research is needed to evaluate factors preventing the use of safe handling practices.
Problems with a web-based survey were characterized and difficulty in reaching some of the health care worker component groups (housekeeping and environmental services) was noted. OSHA’s publicly available IMIS and Chemical Exposure Health Data (CEHD) include quantitative industrial hygiene measurements from a variety of sources.11 Assessment of IMIS data from the 1980s found that, despite the limitations in using exposure data from a compliance database, some surveillance objectives are met when examining exposures to airborne lead and airborne silica. An analysis of the airborne concentrations of lead collected during OSHA compliance in-
___________________
11 The CEHD, available since 2010 as part of the OSHA Information System, also contains quantitative industrial hygiene measurements but these are limited to those that are processed by the OSHA Salt Lake Technical Center. The CEHD and IMIS have a significant degree of overlap (about 50 percent) but each data set contains a substantial amount of unique data (Lavoue et al., 2013a,b).
spections from 1979 to 1985 identified 52 industries which had more than one-third of the median air lead levels measured that were greater than the permissible exposure limit (Froines et al., 1990). The data developed in this analysis also indicated the need to investigate certain industries with high exposures but few inspections. Methods were also developed that permit ranking of potentially hazardous industries in a geographic area using IMIS data.
Researchers have continued to explore the effective use of IMIS data for risk characterization. A systematic review of studies using or analyzing IMIS data identified 29 such studies, most of which focused on single analytes such as lead or silica (Lavoue et al., 2013a). These authors also identified potential biases due to underreporting of values under the limit of detection. However, despite the limitations of these data, their potential for ongoing hazard characterization was highlighted. Additional modeling of the IMIS data using ancillary information about the workplace and its history of inspection demonstrated additional utility of the IMIS data in understanding some workplace characteristics associated with higher exposure levels (Sarazin et al., 2016). A number of other studies examining specific issues, for instance isocyanate asthma, have used IMIS data to identify and characterize high-risk conditions (Lefkowitz et al., 2015).
Despite the above examples using IMIS data, the limitations of using compliance data for surveillance are well recognized. The data are not comprehensive or balanced with respect to the exposures characterized, the workplaces or jobs selected for monitoring, or the complete reporting of results. In addition, although making these data available to the public is a big step forward, they are not routinely disseminated in a simple way for use by the public or health agencies. Promising developments in the surveillance of occupational hazards and exposures is further discussed in Chapter 6.
CROSS-CUTTING ISSUES
This section provides a brief overview of several topics relevant across the different end points under surveillance: the role of state programs, surveillance research, and sources of information on populations at risk.
State-Based OSH Surveillance Programs
The 1987 NRC panel recognized the importance of the state-federal partnership and recommended that NIOSH continue and expand its efforts to develop the occupational health surveillance capability of state health departments through technical assistance and financial support. NIOSH responded positively to these recommendations and, even in the absence of
additional dedicated federal funding for surveillance, now supports some level of OSH surveillance activity in 27 of the states.12 Initially, in the late 1980s, state activities focused largely on exploring use of death certificate and cancer registry data to examine patterns of disease in relation to employment characteristics. Today, states are exploring many different data sources, in some instances as part of multisource surveillance systems, to meet state surveillance objectives and to inform action to improve worker safety and health, while helping to fill gaps in national surveillance.
There are many recognized benefits: the state programs have access to unique state data sources; they are in a position to conduct case- as well as population-based surveillance with the attendant responsibility to follow up in individual workplaces; and, because the states have legal access to key identifiers, they are able to link data sources to develop a more comprehensive understanding of the magnitude and distribution of the conditions under surveillance. The states have also demonstrated the critical position they are in to use the surveillance findings to promote practical actions to improve worker safety and health.
While important advances have been made in OSH surveillance at the state level, there are significant obstacles to building effective programs across the nation. As described in Chapter 3, worker safety and health is seen largely as a responsibility of the Department of Labor. As a result, occupational health and safety and OSH surveillance have remained relatively low priorities in the general public health community at both national and state levels. Occupational safety and health has not received strong support from the U.S. Department of Health and Human Services (HHS) or CDC, and OSH surveillance has not been funded by CDC as a core public health function. Consequently, whereas in some public health domains, such as infectious disease and cancer prevention, surveillance programs are in most if not all states, close to half of the states report having little or no OSH surveillance capacity. In a nationwide assessment of state health agencies regarding epidemiologic and surveillance capacity in eight public health domains, only 20 percent of states reported having substantial epidemiologic and surveillance capacity in occupational health, the lowest percentage of all domains assessed (CSTE, 2013b). This results not only in lack of attention to occupational safety and health but missed opportunities for collaboration across public health domains to address convergent public health concerns that affect workers as well as the general public.
Given limited resources for OSH surveillance, states with OSH pro-
___________________
12 Twenty-six states have funding from NIOSH for fundamental or expanded surveillance (detailed later in the chapter). Additionally, 5 states have NIOSH funding for work with workers’ compensation data (of these 1 state is not part of the 26 states with fundamental or expanded surveillance).
grams rely on transient federal funding allocated through a highly competitive application process. While this is not unique to occupational health, it substantially hinders continuity and strategic consistency (Burkom, 2017). State programs come and go over funding cycles leaving gaps in the nation’s OSH surveillance capacity. This problem is compounded by lack of a comprehensive national strategic plan for state-based surveillance identifying critical national priorities for expanded state-based surveillance. An additional “operational” barrier faced by states is the funding mechanism used by NIOSH to award funds for state OSH surveillance programs. In other public health domains, state-based surveillance activities are funded through applied public health practice mechanisms. However, NIOSH supports state surveillance activities through a competitive research application process (research cooperative agreements). This research application process introduces practical challenges for states. These include, for example, the inability of inexperienced states who wish to initiate OSH surveillance programs to meet research grant eligibility requirements such as innovation and the need for principal investigators with published research articles. For even experienced states, this has created hurdles—such as evaluation for ongoing funding based on innovation and the number of peer-reviewed publications—rather than success in collecting and using surveillance data to inform policy and practice. Additionally, these research applications require human-subjects review, which state institutional review boards are reluctant to conduct for ongoing surveillance programs, considered as applied public health practice.
Conclusion: State OSH programs play an essential role in a national OSH surveillance system and are especially well positioned to disseminate surveillance findings to those in positions to take action to protect worker safety and health. It is not necessary to conduct in-depth expanded programs for all conditions in all states in order to have an effective national surveillance system. However, contribution of such programs would be increased if implemented within the context of a comprehensive strategic surveillance plan developed by NIOSH in conjunction with the states as well as BLS and OSHA. Also, enhanced coordination among federally funded OSH and other public health programs at the state level have the potential to increase the effectiveness and efficiency of these state-based programs.
Recommendation C: NIOSH should lead a collaborative effort with BLS, OSHA, the states, and other relevant federal agencies to establish and strengthen state-based OSH surveillance programs. This should be carried out as part of a national coordinated effort to monitor priority conditions, hazards, and exposures; to identify emerging workplace risks; and to facilitate prevention programs that address these concerns. Furthermore, this
should be carried out with the full support of and assistance from other parts of HHS and CDC.
In the near term:
- OSH Agency Collaboration Within States: NIOSH, BLS, and OSHA should actively encourage and promote collaboration among their programs in the states to reflect the national commitment to interagency effectiveness for OSH surveillance and leverage surveillance and prevention expertise across agencies. This should include sharing data and taking advantage of unique state-level data sets and case-based surveillance capacities to identify and respond to emerging occupational safety and health hazards and conditions.
- Public Health Agency Collaboration Within States: NIOSH and other CDC centers that support state-based surveillance and prevention activities should promote collaboration among their state-level programs to monitor and address public health problems of shared concern, such as violence, asthma, infectious disease, traffic safety, and health inequities among vulnerable population groups.
- NIOSH should also
- Explore and implement, as appropriate, alternative approaches to funding ongoing surveillance in the states as applied public health programs rather than research programs.
- Foster increased coordination and communication between its intramural and extramural surveillance programs.
- Encourage NIOSH-funded Education Research and Training Centers and Agricultural Health and Safety Centers to provide technical and research support to state surveillance programs in their regions as part of their required outreach and education core activity.
Surveillance Research
Research is the process of systematic investigation to generate new facts, and it is important for all types of surveillance, including OSH surveillance. There are important distinctions, however, between research and surveillance (CDC, 2010). The most obvious distinction is that the primary goal of surveillance is to inform public health action, not necessarily to generate new knowledge. The dissemination of information produced by a surveillance system to guide action would be a central consideration in developing and evaluating surveillance systems. In contrast, research findings are usually disseminated through a process called knowledge translation, tending to be less well-structured and often ad hoc.
Another important distinction is that surveillance is an ongoing pro-
cess, whereas research is not necessarily so. Accordingly, surveillance is usually funded through the core operating funds of a public health organization, while research is usually funded through competitions, which may be targeted (i.e., strategic) or investigator initiated. Despite these differences, it can be difficult to make the distinction between surveillance and surveillance research. This can happen, for example, when states conduct surveillance to protect the health of the state population, but also analyze the state data together with a national data set to generate new knowledge.
Surveillance research can generally be divided into two broad categories. The first is research that uses data collected through surveillance to generate new knowledge. Generating data for research is a well-accepted objective for a surveillance system, although not the primary objective for most systems. The second type is research to develop or adapt methods for surveillance. This type of applied research is less common, although increasingly recognized as being important for improving the efficiency and effectiveness of all types of public health surveillance. Applied surveillance research will play an important role in developing new approaches and adapting new technologies to build a smart OSH surveillance system for the 21st century.
Research Using Surveillance Data to Generate New Knowledge About Occupational Health
Within a surveillance system, the data collected are usually limited to the minimum data necessary to accomplish the objectives. This limitation is imposed for multiple reasons, including cost, protection of privacy, and acceptability of the system by those who provide data. When supporting research is an objective of a surveillance system, then the scope of data collection may be greater than it otherwise would be (i.e., if supporting research were not an objective). In any event, even if supporting research is not an explicit objective of a surveillance system, the data collected by the system can usually support research. Examples range from descriptive analyses, hypothesis-driven research, and research to assess the impact of interventions, including more general policies both as natural experiments and as simulated scenario analysis (“what if”).
Given that research occurs under a different legal and ethical framework than public health surveillance, an important consideration in this type of research is to ensure that the researcher has the legal authority to use the data, that the necessary ethical approvals have been obtained, and that the necessary mechanisms are in place to ensure the protection of privacy. In practice, the same people conducting surveillance may also be conducting research, but this does not diminish, and may even augment, the
need to clearly distinguish between the use of surveillance data for public health practice and research.
Research to Develop and Evaluate Methods for Occupational Health Surveillance
Applied research aims to develop, implement, and evaluate methods and tools for conducting surveillance. It is considered applied because the focus is to improve aspects of the surveillance process. The following are examples of applied research in occupational safety and health:
- Development of novel technologies for measurement of exposure (e.g., accelerometers in helmets, clothing to measure repetitive movements), and collection of outcomes (e.g., social media, crowd sourcing);
- Development of data-coding technologies (e.g., natural language processing and statistical methods) to be shared;
- Application of or development of new statistical methods in occupational health for detection of events, clusters, or other outliers;
- Linking in data sets to join variables, to assess reporting, to get denominator for rates, and to triangulate;
- Assessment of data quality and new data sources for case ascertainment;
- Estimation of attributable fraction of COPD caused by exposures at work; and
- Evaluation of whether traditional approaches to capturing and coding occupation and industry cover new work arrangements and development of new approaches to capturing this information.
To be research, the results or methods need to be generalizable. Thus, periodic evaluation of surveillance data may be research if the findings are generalizable while periodic evaluation of a surveillance system would be part of ongoing surveillance programming.
Current Surveillance Research
BLS intramural researchers conduct surveillance research both using CFOI and SOII data and are developing new methods. These include, for example, development of coding software for assigning standard codes for occupation and event based on free text, and web-sweeping approaches for ascertaining fatal occupational injuries in publicly available data sets. As described above, the agency has processes in place for researchers to apply to use CFOI and SOII data for research purposes and is in the process of making these data available at their Federal Statistical Research Data
Centers (in a manner that preserves data confidentiality). In recent years, BLS has also supported a program of intramural and extramural research specifically aimed at better understanding the undercounting of injuries and acute illnesses in the SOII and factors that contribute to it. As will be described in Chapter 6, they are also supporting research to explore the feasibility of a worker survey.
NIOSH likewise conducts and supports surveillance research using surveillance data as well as applied research to develop new surveillance methods. Within NIOSH, investigators periodically compete with other researchers for funds to support investigator-initiated surveillance research projects using existing data sets. NIOSH also funds investigator-initiated research activities carried out by extramural researchers in universities and the states and other nonprofit organizations (for examples, see NIOSH, 2014b). With the exception of an extramural funding stream specifically designated for surveillance research in 2000, extramural applications for surveillance research are submitted to the general NIOSH extramural research funding competition. NIOSH does not appear to have a current research agenda for surveillance, although many of the NORA industry sectors have identified surveillance activities among their research goals.
Sources of Information on Populations at Risk
This chapter thus far has focused primarily on approaches used to collect data on health outcomes or hazards (numerator data). As mentioned in the 2009 Institute of Medicine (IOM) report Traumatic Injury Research at NIOSH, information about the “population at risk (denominator data) is also critical for surveillance and necessary to calculate injury and illness rates that allow for identification of disproportionate risks among segments of the population and subsequent priority setting” (IOM, 2009).
The SOII and some state workers’ compensation insurance programs collect data on numbers of workers and hours of work as part of ongoing data collection which allows for calculating injury and illness rates by industry (but not occupation and demographic characteristics such as age, gender, and race and ethnicity.) Other systems, such as ABLES, CFOI, and NEISS-Work, rely on external sources of denominator data to use in calculating incidence rates by employment and demographic characteristics. A number of different sources of employment data are collected by federal statistical agencies, each with strengths and limitations, and the choice depends upon the availability of robust data at the geographic level of interest and intended purpose. An important distinction is that between employee count and hours-based incidence rates. The denominator for hours-based incidence rates, which takes into account time persons are at
risk, is generally expressed as a full-time equivalent (FTE).13 As reported by BLS, count-based incidence rates underestimate risk among part-time workers, an important consideration in addressing the need to understand the injury and illness experience of the increasing numbers of workers in contingent employment situations (Ruser, 1998). BLS publishes hour-based rates in both the SOII and in CFOI (BLS, 2010).
One of the most widely used sources of employment information in generating injury or illness rates at the national and state levels is the Current Population Survey (CPS) conducted by BLS. BLS maintains a public use access file and NIOSH has developed a user-friendly query system—the Employed Labor Force query system—based on these data that provides employed worker population estimates of both counts of workers and FTEs (workers age 15 years or older) from 1980 through the present. A significant advantage of the CPS employment data is that this is a panel survey and data on employment and hours of work are collected from the same individual over time and aggregated to generate annual employment estimates. A disadvantage is that the sample size is often too small to generate robust rates for detailed segments of the population at the state or local level. The American Community Survey (ACS), conducted by the U.S. Census Bureau, is another important source of employment estimates with the advantage of a larger sample size. A disadvantage is that information about weeks and hours of employment is collected from individuals at a single point in time and thus subject to recall bias or error due to changes in work and work schedules over the course of the year. Also, the ACS reports employment data as a categorical rather than a continuous variable and offers no recommended method for computing FTEs. The Quarterly Census of Employment and Wages is yet another source of employment information. Unlike both the CPS and ACS, which are household surveys, the Quarterly Census of Employment and Wages Program at BLS provides data on the numbers of employed workers by industry provided by employers as part of the unemployment insurance system. This source may be expected to provide the most accurate count of workers but information about occupation hours of work or demographic characteristics is not provided. The BLS Current Employment Survey is another source of employment data based on data provided by a smaller sample of employers on a more frequent basis. BLS also generates monthly Local Area Unemployment (and employment) statistics for census areas and metropolitan regions combining data from employer-reported and household survey sources. Unemployment
___________________
13 An FTE is the number of hours worked by one employee on a full-time basis. The concept is used to convert the hours worked by several employees into hours worked by full-time employees. A full-time employee in generally considered to work 40 hours per week and 50 weeks per year, or 2,000 hours per year.
Insurance (UI) wage files maintained by states for purposes of determining eligibility of claimants for UI benefits are another source of employment data for potential use in OSH surveillance.
NIOSH is currently working in collaboration with state and academic partners to explore the use of alternative data sources alone and in combination for generating employment denominators for use in OSH surveillance. This important research needs to be conducted. Practical guidance tools for selecting appropriate denominators for state OSH surveillance programs and other researchers are also needed. With changes in the health care delivery system there is increasing emphasis on documenting health needs at the community level. For example, under the Patient Protection and Affordable Care Act (P.L. 111-148) all nonprofit hospitals are required to conduct community health needs assessments to qualify for Medicare and Medicaid reimbursement (IRS, 2016). Local health departments also prepare a community health assessment as part of the public health department accreditation process (PHAB, 2015). Alternatives for generating community-level OSH surveillance information need to be explored.
Accurate documentation of employment among the contingent workforce in light of the changing nature of work and work relationships is a significant challenge and has potentially important implications for generating estimates of health and safety risk. Between 1995 and 2005, BLS collected data on contingent and alternative employment arrangements in periodic supplements to the CPS (GAO, 2015). These supplements were discontinued due to insufficient funds. While BLS has often requested funding to repeat this survey every 2 years, Congress has not allocated funding to do so. BLS did field a contingent worker supplement again in 2017 with one-time DOL funding, but it is unclear when the survey will be repeated. These surveys are needed to provide critical information about the workforce. Additional research is also needed to assess the validity of information on alternative work arrangements collected in population surveys that has implications for OSH surveillance. Research on how to generate authoritative labor statistics in light of the many changes in the structure of work including the emergence of the on-demand economy is a critical area of research with relevance far beyond OSH surveillance (NASEM, 2017).
Another concern expressed by OSHA to the committee is the lack of comprehensive data on establishments in the United States by industry that could be used to inform outreach and dissemination efforts. Although this information is collected through the unemployment insurance system overseen by BLS, it is not available to OSHA. Public health access to unemployment insurance listings of establishments by North American Industry Classification System code is also limited and varies by state.
SUMMARY
While substantially improved since 1987, the current state of OSH surveillance continues to have gaps and lacks maturity across the end points under surveillance. A robust system for fatal injuries is in place. Advances have been made in surveillance of nonfatal injuries with some critical omissions or shortcomings remaining. There continues to be limited surveillance of most chronic occupational diseases. There is very limited surveillance of hazards and exposures necessary for informing effective approaches to prevention for long latency health outcomes. There is not a clear delineation of specific objectives for each component of the current surveillance system, and a comprehensive synthesis of findings across these systems is
lacking. Although there is some coordination across the multiple entities engaged in surveillance, the current “system” operates more as a collection of separate and sometimes fragmented data systems, rather than a coordinated national OSH surveillance system that effectively promotes use of the data for prevention.
Using the framework of the objectives of an ideal surveillance system outlined in Chapter 2 the committee identified the major gaps in surveillance (see Box 4-4). Agencies are well aware of current limitations and are engaged in a number of ongoing activities with potential to address many of these gaps. These are presented in Chapters 6 and 7.
REFERENCES
AFL-CIO. 2017. Death on the job: The toll of neglect. Available online at https://aflcio.org/sites/default/files/2017-04/2017Death-on-the-Job.pdf (accessed June 15, 2017).
Alarcon, W. A. 2016. Elevated blood lead levels among employed adults—United States, 1994–2013. Morbidity and Mortality Weekly Report 63(55):59-65.
Asfaw, A. G., C. C. Change, and T. K. Ray. 2014. Workplace mistreatment and sickness absenteeism from work: Results from the 2010 National Health Interview Survey. American Journal of Industrial Medicine 57(2):202-213.
Azaroff, L., C. Levenstein, and D. H. Wegman. 2002. Occupational injury and illness surveillance: Conceptual filters explain underreporting. American Journal of Public Health 92(9):1421-1429.
Azaroff, L., H. M. Nguyen, T. Do, R. Gore, and M. Goldstein-Gelb. 2011. Results of a community-university partnership to reduce deadly hazards in hardwood floor finishing. Journal of Community Health 36(4):358-368.
Baker, E. L. 1989. Sentinel Event Notification System for Occupational Risks (SENSOR): The concept. American Journal of Public Health 79(Suppl):18-20.
Balmes, J., M. Becklake, P. Blanc, P. Hennenberger, K. Kreiss, C. Mapp, D. Milton, D. Schwartz, K. Toren, and G. Viegi. 2003. American Thoracic Society statement: Occupational contribution to the burden of airway disease. American Journal of Respiratory Critical Care Medicine 167:787-797.
Bhandari, R., S. M. Marsh, A. A. Reichard, and T. R. Tonozzi. 2016. Characterizing emergency department patients who reported work-related injuries and illnesses. American Journal of Industrial Medicine 59(8):611-621.
Blair, A., M. Dosemeci, and E. F. Heineman. 1993. Cancer and other causes of death among male and female farmers from twenty-three states. American Journal of Industrial Medicine 23:729-742.
Blanc, P. D. 2012. Occupation and COPD: A brief review. Journal of Asthma 49(1):2-4.
BLS (Bureau of Labor Statistics). 2010. Census of fatal occupational injuries-hours-based rates. Available online at https://www.bls.gov/iif/oshnotice10.htm (accessed November 8, 2017).
BLS. 2012. Occupational Injury and illness classification manual Version 2.01. Available online at https://www.bls.gov/iif/oiics_manual_2010.pdf (accessed November 8, 2017).
BLS. 2015. Occupational injuries and illnesses: A pilot study of job-transfer or work-restricted cases, 2011-2015. Report 1056. Available online at https://www.bls.gov/iif/oshwc/osh/case/djtr2012.pdf (accessed November 8, 2017).
BLS. 2016a. Scope of the census of fatal occupational injuries. Available online at https://www.bls.gov/iif/cfoiscope.htm (accessed June 12, 2017).
BLS. 2016b. Fatal occupational injuries in 2015, charts. Available online at https://www.bls.gov/iif/oshwc/cfoi/cfch0014.pdf (accessed May 1, 2017).
BLS. 2016c. Survey of Occupational Injuries and Illnesses (SOII)—Information for respondents. Available online at https://www.bls.gov/respondents/iif (accessed April 4, 2017).
BLS. 2016d. 2015 Survey of occupational injuries & illnesses summary estimates charts package. October 27, 2016. Available online at https://www.bls.gov/iif/oshwc/osh/os/osch0057.pdf (accessed September 18, 2017)
BLS. 2016e. Employer-reported workplace injury and illness summary. Available online at https://www.bls.gov/news.release/osh.nr0.htm (accessed June 15, 2017).
BLS. 2016f. Table 2. Numbers of nonfatal occupational injuries and illnesses by case type and ownership, selected industries, 2015. Economic News Release. Available online at https://www.bls.gov/news.release/osh.t02.htm (accessed June 13, 2017).
BLS. 2016g. Nonfatal occupational injuries and illnesses requiring days away from work, 2015. Economic News Release. USDL-16-2130. Available online at https://www.bls.gov/news.release/osh2.nr0.htm (accessed November 8, 2017).
BLS. 2017a. Census of Fatal Occupational Injuries (CFOI)—Current and revised data. Available online at https://www.bls.gov/iif/oshcfoi1.htm (accessed April 4, 2017).
BLS. 2017b. Non-fatal occupational injuries and illnesses with days of job transfer or restriction, Survey of Occupational Injuries and Illnesses. Available online at https://www.bls.gov/iif/oshwc/osh/case/osch0059.pdf (accessed November 8, 2017).
BLS. 2018. Injuries, illnesses, and fatalities databases. Available online at https://www.bls.gov/iif/data.htm (accessed January 31, 2018).
Boden, L. I., and A. Ozonoff. 2008. Capture-recapture estimates of nonfatal workplace injuries and illnesses. Annals of Epidemiology 18(6):500-506.
Burkom, H. S. 2017. Evolution of public health surveillance: Status and recommendations. American Journal of Public Health 107(6):848-850.
Burnett, C., J. Maurer, H. M. Rosenberg, and M. Dosemeci. 1997. Mortality by occupation, industry, and cause of death, 24 reporting states (1984–1988). Cincinnati, OH: NIOSH. DHHS (NIOSH) Document No. 97-114. Available online at https://www.cdc.gov/niosh/docs/97-114/pdfs/97-114.pdf (accessed May 5, 2017).
Byler, C. 2013. Hispanic/Latino fatal occupational injury rates. Monthly Labor Review February:14-23. Available online at https://www.bls.gov/opub/mlr/2013/02/art2full.pdf (accessed April 4, 2017).
CDC (Centers for Disease Control and Prevention). 1995. Proportionate mortality from pulmonary tuberculosis associated with occupations—28 states, 1979–1990. Morbidity and Mortality Weekly Report 44:14-19.
CDC. 2008. Illnesses and injuries related to total release foggers: Eight states, 2001-2006. Morbidity and Mortality Weekly Report 57(41):1125-1129.
CDC. 2010. Distinguishing public health research and public health nonresearch. Available online at https://www.cdc.gov/od/science/integrity/docs/cdc-policy-distinguishing-public-health-research-nonresearch.pdf (accessed June 15, 2017).
CDC. 2016. Strategies for reducing health disparities; selected CDC sponsored intervention, US, 2016. Morbidity and Mortality Weekly Report Supplement 65(1). Available online at www.cdc.gov/mmwr/volumes/65/su/pdfs/su6501.pdf (accessed November 8, 2017).
CDC. 2017a. The work-related injury statistics query system. Available online at https://wwwn.cdc.gov/wisards/workrisqs/ (accessed April 5, 2017).
CDC. 2017b. Employed Labor Force (ELF) query system. Available online at https://wwwn.cdc.gov/wisards/cps/ (accessed December 1, 2017).
CDC. 2017c. Occupational injury and illness classification system. Available online at https://wwwn.cdc.gov/wisards/oiics/ (accessed December 1, 2017).
CDC. 2017d. Occupational injury and illness classification system: Coding selection rules. Available online at https://wwwn.cdc.gov/wisards/oiics/ (accessed December 1, 2017).
CDC. 2017e. NIOSH worker health charts: NHIS occupational health supplement. 2017. Available online at https://wwwn.cdc.gov/Niosh-whc/source/ohs (accessed November 8, 2017).
CDC. 2017f. Multiple cause of death 1999-2005. Available online at https://wonder.cdc.gov/wonder/help/mcd.html#Age-Adjusted Rates (accessed December 1, 2017).
Churchill, R. B., and L. K. Pickering. 1997. Infection control challenges in child-care centers. Infectious Disease Clinics of North America 11(2):347-365.
Cohidon C., G. Santin, J. Chastang, E. Imbernon, and I. Niedhammer. 2012. Psychosocial exposures at work and mental health potential utility of a job-exposure matrix. Journal of Occupational and Environmental Medicine 54:184-191.
Colt, J. S., L. Stallones, L. L. Cameron, M. Dosemeci, and S. H. Zahm. 2001. Proportionate mortality among U.S. migrant and seasonal farmworkers in twenty-four states. American Journal of Industrial Medicine 40:604-611.
Cordell, R., L. Pickering, F. W. Henderson, and J. Murph. 2004. Infectious diseases in childcare settings. Emerging Infectious Diseases 10(11):e9.
Costello, S., A. M. Neophytou, D. M. Brown, E. M. Noth, S. K.Hammond, M. R. Cullen, and E. A. Eisen. 2016. Incident ischemic heart disease after long-term occupational exposure to fine particulate matter: Accounting for 2 Forms of Survivor Bias. American Journal of Epidemiology 183(9): 861-868.
CPWR (Center for Construction Research and Training). 2013. The Construction Chart Book. Available online at http://www.cpwr.com/publications/construction-chart-book (accessed April 5, 2017).
CPWR. 2017. Fatality map. Available online at http://stopconstructionfalls.com/fatality-map/ (accessed April 4, 2017).
CSTE (Council of State and Territorial Epidemiologists). 2013a. Counting work-related injuries and illnesses: Taking steps to close the gaps. Available online at http://c.ymcdn.com/sites/ www.cste.org/resource/resmgr/OccupationalHealth/SummaryRecClosGapsMtg2013.pdf (accessed June 22, 2017).
CSTE. 2013b. National assessment of epidemiologic capacity, findings and recommendations. Available online at http://www.cste2.org/2013eca/CSTEEpidemiologyCapacityAssessment2014-final2.pdf (accessed September 4, 2017).
CSTE. 2014. Position Statement 14-OH-02. Inclusion of work information as data elements in CDC surveillance systems. Available online at www.cste.org/?page=Position Statements (accessed November 28, 2017).
CSTE. 2015a. Handicapped-accessible accelerator pedal redesigned based on fatality. Available online at http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/Occupational_Health_Success_Stories/KY_success_story-_handicappe.pdf (accessed July 18, 2017).
CSTE. 2015b. Public health reporting and national notification for elevated blood lead levels. Available online at http://c.ymcdn.com/sites/www.cste.org/resourceresmgr/2015PS/2015PSFinal/15-EH-01.pdf (accessed June 14, 2017).
CSTE. 2017a. Occupational health indicators. Available online at http://www.cste.org/members/group.aspx?id=106668 (accessed June 10, 2017).
CSTE. 2017b. Surveillance/informatics: Reportable Condition Knowledge Management System. Available online at http://www.cste.org/group/RCKMS (accessed May 8, 2017).
Davis, L., M. Standbury, B. Materna, and E. Simms. 2012. Putting data to work for worker safety and health, success stories in the states. Available online at https://c.ymcdn.com/sites/cste.site-ym.com/resource/resmgr/OccupationalHealth/OC_Health_Book_FINAL.pdf (accessed May 1, 2017).
Du Y., X. Xu, M. Chu, Y. Guo, and J. Wang. 2016. Air particulate matter and cardiovascular disease: The epidemiological, biomedical and clinical evidence. Journal of Thoracic Disease 8(1): E8-E19.
Dubrow, R., J. Sestito, N. Lalich, C. Burnett, and J. Salg. 1987. Death certificate-based occupational mortality surveillance in the United States. American Journal of Industrial Medicine 11:329-342.
Edwards, C. H., G. S. Tomba, and B. F. de Blasio. 2016. Influenza in workplaces: Transmission, workers’ adherence to sick leave advice and European sick leave recommendations. European Journal of Public Health 26(3):478-485.
Fagan, K. M., and M. J. Hodgson. 2017. Under-recording of work-related injuries and illnesses: An OSHA priority. Journal of Safety Research 60:79-83.
Fang, S. C., A. Cassidy, and D. C. Christiani. 2010. A systematic review of occupational exposure to particulate matter and cardiovascular disease. International Journal of Environmental Research and Public Health 7(4):1773-1806.
Froines, J. R., S. Baron, D. H. Wegman, and S. O’Rourke. 1990. Characterization of the airborne concentrations of lead in U.S. industry. American Journal of Industrial Medicine 18(1):1-17.
GAO (U.S. Government Accountability Office). 2015. Contingent workforce: Size, characteristics, earnings, and benefits. Available online at http://www.gao.gov/assets/670/669766.pdf (accessed June 14, 2017).
GAO. 2016. Workplace Safety and Health: Additional Data Needed to Address Continued Hazards in the Meat and Poultry Industry. GAO-16-337. Washington, DC: U.S. Government Printing Office.
Grattan K., L. K. Davis, M. Fiore, E. Pechter, and J. Laing. 2017. Employer Compliance with OSHA Requirement to Report Amputations, Updated Findings from a Massachusetts Study. CSTE Annual Conference, June, Boise, ID.
Green Seal Institutional Cleaning Products. 2017. Green seal. Available online at www.greenseal.org/FindGreenSealProductsandServices.aspx?vid=ViewProductDetail&cid=16 (accessed June 15, 2017).
Groenewold, M. R., and S. L. Baron. 2013. The proportion of work-related emergency department visits not expected to be paid by workers’ compensation: Implications for occupational health surveillance, research, policy, and health equity. Health Services Research 48(6 Pt 1):1939-1959.
Haddon, W. 1970. On the escape of tigers: An ecologic note. American Journal of Public Health 60(2):2229–2234.
Harris, R. 2016. Suicide in the workplace. Monthly Labor Review. Available online at https://www.bls.gov/opub/mlr/2016/article/suicide-in-the-workplace.htm (accessed May 5, 2017).
Henneberger, P. K., C. A. Redlich, D. B. Callahan, P. Harber, C. Lemiere, J. Martin, S. M. Tarlo, and O. Vandenplas. 2011. An official American Thoracic Society statement: Work-exacerbated asthma. American Journal of Respiratory Critical Care Medicine 184(3):368-378.
HHS (U.S. Department of Health and Human Services). 2017. Asthma. Available online at https://www.healthypeople.gov/2020/topics-objectives/topic/respiratory-diseases/objectives (accessed April 5, 2017).
Hnizdo, E., P. A. Sullivan, K. M. Bang, and G. Wagner. 2002. Association between chronic obstructive pulmonary disease and employment by industry and occupation in the U.S. population: A study of data from the Third National Health and Nutrition Examination Survey. American Journal of Epidemiology 156:738-746.
Huband, E. M., and P. Bobbit. 2013. Nonresponse bias in the survey of occupational injuries and illnesses. BLS Statistical Survey Papers. Available online at https://www.bls.gov/osmr/pdf/st130170.pdf (accessed November 8, 2017).
IOM (Institute of Medicine). 2001. Tuberculosis in the Workplace. Washington, DC: National Academy Press.
IOM. 2009. Traumatic Injury Research at NIOSH: Reviews of Research Programs of the National Institute for Occupational Safety and Health. Washington, DC: The National Academies Press.
IRS (Internal Revenue Service). 2016. New requirements for 501(c)(3) hospitals under the Affordable Care Act. Available online at https://www.irs.gov/charities-non-profits/charitable-organizations/new-requirements-for-501c3-hospitals-under-the-affordable-care-act (accessed June 14, 2017).
Jackson L. 2001. Non-fatal occupational injuries and illnesses treated in hospital emergency departments in the United States. Injury Prevention 7(Suppl I):i21-i26.
Keech, M., and P. Beardsworth. 2008. The impact of influenza on working days lost: A review of the literature. Pharmacoeconomics 26(11):911-924.
Kica, J., and K. D. Rosenman. 2012. Multi-source surveillance system for work-related burns. Journal of Occupational and Environmental Medicine 54(5):642-647.
Kica, J., and K. D. Rosenman. 2014. Multi-source surveillance system for work-related skull fractures in Michigan. Journal of Safety Research 51:49-56.
Klous, G., A. Huss, D. J. Heederik, and R. A. Coutinho. 2016. Human-livestock contacts and their relationship to transmission of zoonotic pathogens, a systematic review of literature. One Health 2:65-76.
Largo, T. W., and K. D. Rosenman. 2015. Surveillance of work-related amputations in Michigan using multiple data sources: Results for 2006-2012. Occupational and Environmental Medicine 72(3):171-176.
LaMontagne A.D., T. Keegel, D.A. Vallance, A. Ostry, and R. Wolfe. 2008. Job strain—Attributable depression in a sample of working Australians: Assessing the contribution to health inequalities. BMC Public Health 8(181).
Lavoue, J., M. Friesen, and I. Burstyn. 2013a. Workplace measurements by the U.S. Occupational Safety and Health Administration since 1979: Descriptive analysis and potential uses for exposure assessment. Annals of Occupational Hygiene 57(5):681-683.
Lavoue, J., M. Friesen, and I. Burstyn. 2013b. Workplace measurements by the U.S. Occupational Safety and Health Administration since 1979: Descriptive analysis and potential uses for exposure assessment. Annals of Occupational Hygiene 57(1):77-97.
Lefkowitz, D., E. Pechter, M. Lumia, A. Stephens, K. Fitzsimmons, L. Davis, J. Flattery, J. Weinberg, R. J. Harrison, M. J. Reilly, M. S. Filios, G. E. White, and K. D. Rosenman. 2015. Isocyanates and work-related asthma: Findings from California, Massachusetts, Michigan, and New Jersey, 1993-2008. American Journal of Industrial Medicine 58(11): 1138-1149.
Luckhaupt, S., and G. M. Calvert. 2008. Deaths due to blood-borne infections and their sequelae among health care workers. American Journal of Industrial Medicine 51(11): 812-824.
Luckhaupt, S. E., J. M. Dahlhamer, B. W. Ward, A. L. Sussell, M. H. Sweeney, J. P. Sestito, and G. M. Calvert. 2013a. Prevalence of dermatitis in the working population, United States, 2010 National Health Interview Survey. American Journal of Industrial Medicine 56(6):625-634.
Luckhaupt, S. E., M. A. Cohen, and G. M. Calvert. 2013b. Concordance between current job and usual job in occupational and industry groupings: Assessment of the 2010 National Health Interview Survey. Journal of Occupational and Environmental Medicine 55(9):1074-1090.
MA COSH (Massachusetts Coalition for Occupational Safety and Health). 2005. Protecting workers and homeowners from wood floor-finishing hazards in Massachusetts. Available online at http://www.masscosh.org/files/ProtectingFromFloorFinishingHazards.pdf (accessed April 4, 2017).
MA DPH (Massachusetts Department of Public Health). 2017. Fatal occupational injuries in Massachusetts: 2008-2013. Available online at http://www.mass.gov/eohhs/docs/dph/occupational-health/fatal-reports/work-related-fatalities-2008-2013.pdf (accessed June 15, 2017).
Marcum J. L., and D. Adams. 2017. Work-related musculoskeletal disorder surveillance using the Washington State workers’ compensation system: Recent declines and patterns by industry, 1999-2013. American Journal of Industrial Medicine 60(5):457-471.
Marsh, S. M., A. A. Reichard, R. Bhandari, and T. R. Tonozzi. 2016. Using emergency department surveillance data to assess occupational injury and illness reporting by workers. American Journal of Industrial Medicine 59(8):600-610.
Masterson, E. A., M. H. Sweeney, J. A. Deddens, C. L. Themann, and D. K. Wall. 2014. Prevalence of workers with shifts in hearing by industry: A comparison of OSHA and NIOSH hearing shift criteria. Journal of Occupational and Environmental Medicine 56(4):446-455.
Mazurek, J. M., G. Syamial, J. M. Wood, S. A. Hendricks, and A. Weston. 2017. Malignant mesothelioma mortality—United States, 1999-2015. Morbidity and Mortality Weekly Report 66:214-218.
Michaels, D. 2016. Year one of OSHA’s severe injury reporting program: An impact evaluation. Available online at https://www.osha.gov/injuryreport/2015.pdf (accessed April 4, 2017).
Michas, M. G., and C. U. Iacono. 2008. Overview of occupational medicine training among US family medicine residency programs Family Medicine 40(2):102-106.
MI DCH (Michigan Department of Community Health). 2013. Thirteen indicators of the health of Michigan’s workforce. Available online at http://www.michigan.gov/documents/Michigan_Indicator_Report_revised_41206_156036_7.pdf (accessed July 18, 2017).
MI DHHS (Michigan Department of Health and Human Services). 2015. Heavy metals surveillance in Michigan: Eighth annual report. Available online at http://www.oem.msu.edu/userfiles/file/Annual%20Reports/HeavyMetals/2014HeavyMetalsAnnualReport.pdf (accessed June 14, 2017).
MI FACE (Michigan Fatality Assessment and Control Evaluation). 2013. Methylene chloride causes death of three Michigan bathtub refinishers. Hazard alert. Available online at http://www.oem.msu.edu/userfiles/BathtubRefinishingHA14.pdf (accessed April 4, 2017).
Molinari, N. A., I. R. Ortega-Sanchez, M. L. Messonnier, W. W. Thompson, P. M. Wortley, E. Weintraub, and C. B. Bridges. 2007. The annual impact of seasonal influenza in the U.S.: Measuring disease burden and costs. Vaccine 25(27):5086-5096.
MSU and MI DELEG (Michigan State University and the Michigan Department of Energy, Labor, and Economic Growth). 2009. Annual report on work-related noise-induced hearing loss in Michigan. Available online at http://www.oem.msu.edu/userfiles/file/Annual%20Reports/Hearing/08NIHL_Report.pdf (accessed June 12, 2017).
NASEM (National Academies of Sciences, Engineering, and Medicine). 2017. Information Technology and the U.S. Workforce: Where Are We and Where Do We Go from Here? Washington, DC: The National Academies Press.
National COSH (Council for Occupational Safety and Health). 2017. U.S. worker fatality maps. Available online at http://www.coshnetwork.org/fatality-database-maps (accessed April 4, 2017).
NCHS (National Center for Health Statistics). 2016. About the National Health Interview Survey. Available online at https://www.cdc.gov/nchs/nhis/about_nhis.htm (accessed June 14, 2017).
NCHS. 2017. National Health Interview Survey 2018 questionnaire redesign: Proposed design. Available online at https://www.cdc.gov/nchs/nhis/2018_quest_redesign.htm (accessed November 27, 2017).
New York State Department of Health. 2016. Heavy metals surveillance: New York State heavy metals registry. Available online at https://www.health.ny.gov/environmental/workplace/heavy_metals_registry (accessed June 14, 2017).
Niedhammer I., H. Sultan-Taieb, J. F. Chastang, G. Vermeylen, and A. Parent-Thirion. 2014. Fractions of cardiovascular diseases and mental disorders attributable to psychosocial work factors in 31 countries in Europe. International Archives of Occupational and Environmental Health 87(4):403-411.
NIOSH (National Institute for Occupational Safety and Health). 1974. National Occupational Hazard Survey. Volume I: Survey Manual. Cincinnati, OH: NIOSH.
NIOSH. 1997. Musculoskeletal Disorders and Workplace Factors - A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back. Cincinnati, OH: NIOSH. Available online at https://www.cdc.gov/niosh/docs/97-141/pdfs/97-141.pdf (accessed November 8, 2017).
NIOSH. 2012. A Story of Impact: NIOSH Research Cited in Recommendations for Improving Commercial Fishing. NIOSH Publication No. 2012-129 March 2012. Available online at https://www.cdc.gov/niosh/docs/2012-129/pdfs/2012-129.pdf (accessed May 5, 2017).
NIOSH. 2013. 2010 occupational health supplement. Available online at https://www.cdc.gov/niosh/topics/nhis/healthcareocc/hcocctables.html (accessed December 1, 2017).
NIOSH. 2014a. Impact: PFD manufacturer adopts NIOSH research into product development process. Available online at https://www.cdc.gov/niosh/docs/2015-119/pdfs/2015-119.pdf (accessed May 6, 2017).
NIOSH. 2014b. NIOSH research projects. Available online at https://www.cdc.gov/niosh/programs/surv/projects2.html#ohd (accessed June 14, 2017).
NIOSH. 2015a. Washington occupational injury and illness surveillance program—Annual report. Available online at https://www.cdc.gov/niosh/oep/pdfs/annualreports/washington-occupational-injury-and-illnesssurveillance-program.pdf (accessed November 17, 2017).
NIOSH. 2015b. Health hazard evaluations. Available online at https://www.cdc.gov/niosh/hhe/resources.html (accessed May 8, 2017).
NIOSH. 2016a. Definitions of traumatic injuries and MSDs. Available online at https://www.cdc.gov/niosh/programs/msd/risks.html (accessed June 13, 2017).
NIOSH. 2016b. Coal Workers’ Health Surveillance Program (CWHSP) data query system. Available online at https://webappa.cdc.gov/ords/cwhsp-database.html (accessed December 1, 2017).
NIOSH. 2016c. National agriculture, forestry and fishing agenda. Available online at https://www.cdc.gov/niosh/nora/comment/agendas/agforfish/default.html (accessed June 13, 2017).
NIOSH. 2016d. National Health Interview Survey: Occupational health supplement. Available online at https://www.cdc.gov/niosh/topics/nhis/ (accessed April 5, 2017).
NIOSH. 2016e. Tuberculosis. Available online at https://www.cdc.gov/niosh/topics/tb/ (accessed May 8, 2017).
NIOSH. 2016f. Adult blood lead epidemiology and surveillance. Available online at http://www.cdc.gov/niosh/topics/ables/description.html (accessed November 21, 2016).
NIOSH. 2016g. NIOSH musculoskeletal disorders prevention programs. May. Available online at https://stacks.cdc.gov/view/cdc/39919 (accessed December 21, 2017).
NIOSH. 2017a. Fatality Assessment and Control Evaluation (FACE) program. Available online at https://www.cdc.gov/niosh/face/default.html (accessed April 4, 2017).
NIOSH. 2017b. Firefighter fatality investigation and prevention. Available online at https://www.cdc.gov/niosh/fire/default.html (accessed January 29, 2017).
NIOSH. 2017c. NIOSH and partners work to prevent worker deaths from exposures to hydrocarbon gases and vapors at oil and gas wellsites. Available online at https://www.cdc.gov/niosh/docs/2017-110 (accessed May 8, 2017).
NIOSH. 2017d. Welcome to eWORLD. Available online at https://wwwn.cdc.gov/eworld (accessed June 14, 2017).
NIOSH. 2017e. Coal workers’ health surveillance program. Available online at https://www.cdc.gov/niosh/topics/cwhsp (accessed April 5, 2017).
NIOSH. 2017f. Bloodborne infectious diseases: HIV/AIDS, hepatitis B, hepatitis C. Available online at https://www.cdc.gov/niosh/topics/bbp (accessed May 8, 2017).
NIOSH. 2017g. Health and safety practices survey of healthcare workers. Available online at https://www.cdc.gov/niosh/topics/healthcarehsps/aboutstudy.html (accessed June 14, 2017).
NIOSH. 2017h. National Occupational Exposure Survey (NOES). Available online at https://www.cdc.gov/noes/default.html (accessed November 8, 2017).
NRC (National Research Council). 1987. Counting Injuries and Illnesses in the Workplace: Proposals for a Better System. Washington, DC: National Academy Press.
NRC. 2001. Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities. Washington, DC: National Academy Press.
O’Leary P., L. I. Boden, S. A. Seabury, A. Ozonoff, and E. Scherer. 2012. Workplace injuries and the take-up of Social Security benefits. Social Security Bulletin 72(3).
OMB (Office of Management and Budget). 2007. Implementation Guidance for Title V of the E-Government Act, Confidential Information Protection and Statistical Efficiency Act of 2002 (CIPSEA). Notice of Decision. 72 Federal Register 33362-33377, June 15.
OSHA (Occupational Safety and Health Administration). 2001. Occupational Injury and Illness Recording and Reporting Requirements. Final Rule. 66 Federal Register 5921-5923, January 19.
OSHA. 2007. Hispanic outreach. Available online at www.osha.gov/OshDoc/data_Hispanic/hispanic_outreach.pdf (accessed June 12, 2017).
OSHA. 2013. Methylene chloride hazards for bathtub refinishers. Available online at https://www.osha.gov/dts/hazardalerts/methylene_chloride_hazard_alert.pdf (accessed May 8, 2017).
OSHA. 2014. Temporary Worker Initiative. TWI Bulletin 1. Available online at https://www.osha.gov/temp_workers/OSHA_TWI_Bulletin.pdf (accessed April 4, 2017).
OSHA. 2015. OSHA fact sheet: Preventing cuts and amputations from food slicers and meat grinders. Available online at https://www.osha.gov/Publications/OSHA3794.pdf (accessed June 13, 2017).
OSHA, 2016a. Improve Tracking of Workplace Injuries and Illnesses. Final Rule. 81 Federal Register 29637-29639, May 12.
OSHA. 2016b. Memorandum for regional administrators and state designees from Thomas Galassi, director, Directorate of Enforcement Programs, “Revised Interim Enforcement Procedures for Reporting Requirements under 29 CFR 1904.39,” March 4. Available online at https://www.osha.gov/dep/enforcement/Interm_Enforcement_Procedures.html (accessed April 5, 2017).
OSHA. 2017a. National safety stand-down to prevent falls in construction. Available online at https://www.osha.gov/StopFallsStandDown (accessed April 4, 2017).
OSHA. 2017b. Fatality and catastrophe investigation summaries. Available online at www.osha.gov/pls/imis/accidentsearch.html (accessed April 4, 2017).
OSHA. 2017c. Severe injury reports. Available online at https://www.osha.gov/severeinjury/index.html (accessed May 8, 2017).
Pegula, S. M. 2013. An analysis of fatal occupational injuries at road construction sites, 2003–2010. Monthly Labor Review November. Available online at https://www.bls.gov/opub/mlr/2013/article/an-analysis-of-fatal-occupational-injuries-at-road-construction-sites-2003-2010.htm (accessed April 4, 2017).
Pegula, S. M., and A. Measure. 2016. Web scraping and a timely repository for fatality data. Presentation to the Data Users Advisory Committee, Bureau of Labor Statistics. November 10.
PHAB (Public Health Accreditation Board). 2015. Guide to national public health department initial accreditation. Available online at http://www.phaboard.org/wp-content/uploads/Guide-to-Accreditation-final_LR2.pdf (accessed June 15, 2017).
PHII (Public Health Informatics Institute). 2016. Next generation electronic death registration system: Supporting improved quality and timeliness of vital records data. Available online at https://www.phii.org/sites/www.phii.org/files/resource/pdfs/20160316%20Next%20Generation%20EDRS%20Report%20FINAL%20WEBSITE.pdf (accessed June 13, 2017).
Raherison, C., and P. O. Girodet. 2009. Epidemiology of COPD. European Respiratory Review 18:213-221.
Rappin, C. L., S. E. Wuellner., and D. K. Bonauto. 2016. Employer reasons for failing to report eligible workers compensation claims in the BLS Survey of Occupational Injuries and Illnesses. American Journal of Industrial Medicine 59(5):343-356.
Reves, R. R., and L. K. Pickering. 1992. Impact of child day care on infectious diseases in adults. Infectious Disease Clinics of North America 6(1):239-250.
Reville, R. T. and R. F. Schoeni. 2004. The fraction of disability caused at work. Social Security Bulletin 65(4). Available online at https://www.ssa.gov/policy/docs/ssb/v65n4/v65n4p31.html (accessed November 8, 2017).
Robinson, C. F., J. T. Walker, M. H. Sweeney, R. Shen, G. M. Calvert, P. K. Schumacher, J. Ju, and S. Nowlin. 2015. Overview of the National Occupational Mortality Surveillance (NOMS) system: Leukemia and acute myocardial infarction risk by industry and occupation in 30 U.S. states 1985-1999, 2003-2004, and 2007. American Journal of Industrial Medicine 58(2):123-137.
Rosenman, K. D. 2016. OSHA, well past its infancy, but still learning how to count injuries and illnesses. American Journal of Industrial Medicine 59(8):595-599.
Rosenman, K. D., M. J. Reilly, D. P. Schill, D. Valiante, J. Flattery, R. Harrison, F. Reinisch, E. Pechter, L. Davis, C. M. Tumpowsky, and M. Fillios. 2003. Cleaning products and work-related asthma. Journal of Occupational and Environmental Medicine 45(5):556-563.
Rosenman, K. D., A. Kalush, M. J. Reilly, J. C. Gardiner, M. Reeves, and Z. Luo. 2006. How much work-related injury and illness is missed by the current national surveillance system? Journal of Occupational and Environmental Medicine 48(4):357-365.
Ruser, J. W. 1998. Denominator choice in the calculation of workplace fatality rates. American Journal of Industrial Medicine 33(2):151-156.
Ruser, J. W. 2008. Examining evidence on whether BLS undercounts workplace injuries and illnesses, Monthly Labor Review, August 2008. Available online at https://www.bls.gov/opub/mlr/2008/08/art2full.pdf (accessed November 17, 2017).
Rutstein, D. D., R. J. Mullan, T. M. Frazier, W. E. Halperin, J. M. Melius, and J. P. Sestito. 1983. Sentinel health events (occupational): A basis for physician recognition and public health surveillance. American Journal of Public Health 73(9):1054-1062.
Sabbath, E. L., L. I. Boden, J. A. Williams, D. Hashimoto, K. Hopcia, and G. Sorensen. 2017. Obscured by administrative data? Racial disparities in occupational injury. Scandinavian Journal of Work, Environment, and Health 43(2):155-162.
Sarazin, P., I. Burstyn, L. Kincl, and J. Lavoue. 2016. Trends in OSHA compliance monitoring data 1979-2011: Statistical modeling of ancillary information across 77 chemicals. Annals of Occupational Hygiene 60(4):432-452.
Savitz, D. A., D. P. Loomis, and C. K. Tse. 1998. Electrical occupations and neurodegenerative disease: Analysis of U.S. mortality data. Archives of Environmental Health 53:71-74.
SBU (Swedish Agency for Health Technology Assessment and Assessment of Social Services). 2017. Occupational health and safety–Chemical exposure. Available online at http://www.sbu.se/261e (accessed May 17, 2017).
Schleiff, P. L., J. M. Mazurek, M. J. Reilly, K. D. Rosenman, M. B. Yoder, M. E. Lumia, and K. Worthington. 2016. Surveillance for silicosis—Michigan and New Jersey, 2003–2011. Morbidity and Mortality Weekly Report 63(55):73-78.
Schnorr, T. 2016. Sponsor panel for follow-up questions and answers. Presentation to the National Academies Committee on Developing a Smarter National Surveillance System for Occupational Safety and Health in the 21st Century, September 21.
Sears, J. M., and S. M. Bowman. 2016. State trauma registries as a resource for occupational injury surveillance and research: Lessons from Washington State, 1998-2009. Public Health Reports 131(6):791-799.
Simpson, H. 2016. Sponsor panel for follow-up questions and answers. Presentation to the National Academies Committee on Developing a Smarter National Surveillance System for Occupational Safety and Health in the 21st Century, September 21.
Sincavage, J. R. 2005. Fatal occupational injuries among Asian workers. Monthly Labor Review October:49-55. Available online at https://www.bls.gov/opub/mlr/2005/10/art6full.pdf (accessed April 4, 2017).
Smith, G. S., H. M. Wellman, G. S. Sorock, M. Warner, T. K. Courtney, G. S. Pransky, and L. A. Fingerhut. 2005. Injuries at work in the U.S. adult population: Contributions to the total injury burden. American Journal of Public Health 95(7):1213-1219.
Socias, C. M., C. K. Chaumont Menendez, J. W. Collins, and P. Simeonov. 2014. Occupational ladder fall injuries—United States, 2011. Morbidity and Mortality Weekly Report 63(16):341-346.
Spieler, E. A., and J. F. Burton, Jr. 2012. The lack of correspondence between work-related disability and receipt of workers’ compensation benefits. American Journal of Industrial Medicine 55(6):487-505.
Spieler, E. A., and G. R. Wagner. 2014. Counting matters: Implications of undercounting in the BLS Survey of Occupational Injuries and Illnesses. American Journal of Industrial Medicine 57(10):1077-1084.
Stanbury, M., A. P. Rafferty, and K. D. Rosenman. 2008. Prevalence of hearing loss and work-related noise induced hearing loss in Michigan. Journal of Occupational and Environmental Medicine 50(1):72-79.
Steenland, K., C. Burnett, N. Lalich, E. Ward, and J. Hurrell. 2003. Dying for work: The magnitude of U.S. mortality from selected causes of deaths associated with occupation. American Journal of Industrial Medicine 43(5):461-482.
Tak, S., R. R. Davis, and G. M. Calvert. 2009. Exposure to hazardous workplace noise and use of hearing protection devices among U.S. workers—NHANES, 1999-2004. American Journal of Industrial Medicine 52(5):358-371.
Thacker, S. B., J. R. Qualters, and L. M. Lee. 2012. Public health surveillance in the United States: Evolution and challenges. Morbidity and Mortality Weekly Report 61(3):3-9.
Theorell T., A. Hammarström, G. Aronsson, L. T. Bendz, T. Grape, C. Hogstedt, I. Marteinsdottir, I. Skoog, and C. Hall. 2015. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 15:738.
Thomsen, C., J. McClain, K. Rosenman, and L. Davis. 2007. Indicators for occupational health surveillance. Morbidity and Mortality Weekly Report 56(RR-1):1-7.
Tonozzi, T. R., S. M. Marsh, A. A. Reichard, and R. Bhandari. 2016. Reported work-related injuries and illnesses among Hispanic workers: Results from an emergency department surveillance system follow-back survey. American Journal of Industrial Medicine 59(8):622-630.
Torén, K., and P. D. Blanc. 2009. Asthma caused by occupational exposures is common—a systematic analysis of estimates of the population-attributable fraction. BMC Pulmonary Medicine 9:7, doi: 10.1186/1471-2466-9-7.
Weber, D. J., and W. A. Rutala. 2016. Occupational health update: Focus on preventing the acquisition of infections with pre-exposure prophylaxis and postexposure prophylaxis. Infectious Disease Clinics of North America 30(3):729-757.
Weil, D. 2014. The Fissured Workplace: Why Work Became So Bad for So Many and What Can Be Done to Improve It. Cambridge, MA: Harvard University Press.
Weil, D. 2017. How to make employment fair in an age of contracting and temp work. Harvard Business Review, March 24. Available online at https://hbr.org/2017/03/making-employment-a-fair-deal-in-the-age-of-contracting-subcontracting-and-temp-work (accessed June 15, 2017).
Wiatrowski, W. J. 2005. Fatalities in the ornamental shrub and tree services industry. Compensation and Working Condition, July 25. Available online at https://www.bls.gov/opub/mlr/cwc/fatalities-in-the-ornamental-shrub-and-tree-services-industry.pdf (accessed April 4, 2017).
Wiatrowski, W. J. 2014. The BLS Survey of Occupational Injuries and Illnesses: A primer. American Journal of Industrial Medicine 57(10):1085-1089.
Wilken, J. A., G. Sondermeyer, D. Shusterman, J. McNary, D. J. Vugia, A. McDowell, P. Borenstein, D. Gilliss, B. Ancock, J. Prudhomme, D. Gold, G. C. Windham, L. Lee, and B. L. Materna. 2015. Coccidioidomycosis among workers constructing solar power farms, California, USA, 2011-2014. Emerging Infectious Diseases 21(11):1997-2005.
Windau, J. A. 1998. Worker fatalities from being caught in machinery. Compensation and Working Condition Winter:35-38. Available online at https://www.bls.gov/opub/mlr/cwc/worker-fatalities-from-being-caught-in-machinery.pdf (accessed June 12, 2017).
Windau, J., K. D. Rosenman, H. Anderson, L. Hanrahan, L. Rudolph, M. Stanbury, and A. Stark. 1991. The identification of occupational lung disease from hospital discharge data. Journal of Occupational Medicine 33(10):1061-1066.
Wuellner, S. E., and D. K. Bonauto. 2014. Exploring the relationship between employer recordkeeping and underreporting in the BLS Survey of Occupational Injury and Illness. American Journal of Industrial Medicine 57(10):1133-1143.
Wuellner, S., and P. Phipps. 2016. Identifying patterns in employer reporting errors in the BLS Survey of Occupational Injuries and Illnesses. Pp. 3322-3335 in JSM Proceedings, Statistical Computing Section. Alexandria, VA: American Statistical Association. Available online at https://www.bls.gov/osmr/pdf/st160200.pdf (accessed April 4, 2017).
Wuellner, S. E., D. A. Adams, and D. K. Bonauto. 2016. Unreported workers’ compensation claims to the BLS Survey of Occupational Injuries and Illnesses: Establishment factors. American Journal of Industrial Medicine 59(4):274-279.
Wuellner, S. E., D. A. Adams, and D. K. Bonauto. 2017. Workers’ compensation claims not reported in the Survey of Occupational Injury and Illnesses: Injury and claim characteristics. American Journal of Industrial Medicine 60(3):264-275.
WY DWS (Wyoming Department of Workforce Services). 2016. Wyoming state occupational epidemiologist releases most comprehensive report on workplace fatalities since program’s inception. Available online at http://www.wyomingworkforce.org/news/2016-10-25a (accessed May 8, 2017).






































































