Proceedings of a Workshop
INTRODUCTION1
Remarkable developments in health promotion and disease treatment and prevention have led to significant improvements in life expectancy throughout the 20th century and into the present. Concurrent with those improvements has been the reality that most Americans will experience a substantial period of time living with serious illness; an estimated 45 million Americans currently are living with one or more chronic conditions (IOM, 2015; NASEM, 2016). Those living with serious illness can be found across the age spectrum and in a broad range of care settings, from pre-birth to geriatric care.
Recognizing the need to thoughtfully consider and address the challenges and opportunities to improve care for people of all ages and all stages of a serious illness, the Roundtable on Quality Care for People with Serious Illness serves to convene stakeholders from government, academia, industry, professional associations, nonprofit advocacy organizations, and philan-
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop has been prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
thropies. Inspired by and expanding on the work of the 2014 Institute of Medicine consensus study report Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life (IOM, 2015),2 the Roundtable aims to foster ongoing dialogue about critical policy and research issues to accelerate and sustain progress in care for people of all ages experiencing serious illness.
As explored during the Roundtable’s first public workshop on Integrating the Patient and Caregiver Voice into Serious Illness Care, when asked what kind of care they prefer, most people living with serious illnesses want to focus on the quality of their life as they live with serious illness.3 Palliative care is the interdisciplinary specialty focused on improving quality of life for people with serious illness and their families. As defined by Diane Meier, director of the Center to Advance Palliative Care (CAPC) at the Icahn School of Medicine at Mount Sinai, palliative care is “specialized medical care for people with serious illness. This type of care focuses on providing relief from the symptoms and stress of a serious illness.” Such interdisciplinary care is provided by doctors, nurses, social workers, chaplains, and others who work together with the patient’s other doctors to provide an extra layer of support. Such care is appropriate for people at any age and at any stage in a serious illness, and can be provided together with curative treatment to address clinical, emotional, psychosocial, and spiritual concerns of the patient and their family4 (CAPC, 2015). To better understand how the principles of palliative care can be integrated into the overall provision of care and services to those facing serious illness, the Roundtable on Quality Care for People with Serious Illness of the National Academies of Sciences, Engineering, and Medicine held the public workshop Models and Strategies to Integrate Palliative Care Principles into Care for People with Serious Illness. The workshop was held on April 27, 2017, in Washington, DC.
In her introductory remarks to open the workshop, planning committee co-chair Brenda Nevidjon, chief executive officer of the Oncology Nurs-
___________________
2 As of March 2016, the Health and Medicine Division of the National Academies of Sciences, Engineering, and Medicine continues the consensus studies and convening activities previously carried out by the Institute of Medicine (IOM). The IOM name is used to refer to publications issued prior to July 2015.
3 See Integrating the Patient and Caregiver Voice into Serious Illness Care: Proceedings of a Workshop, available at http://www.nap.edu/catalog/24802 (accessed September 11, 2017).
4 Other organizations have developed definitions of palliative care as detailed in IOM (2015, pp. 55–60).
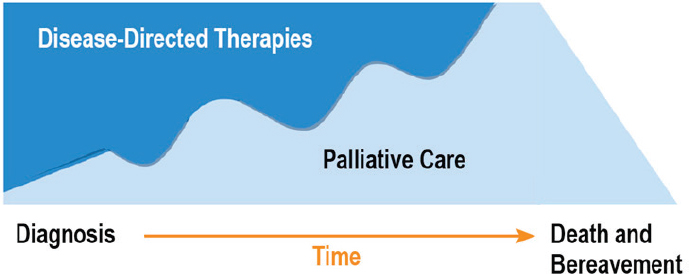
SOURCE: As presented by Diane Meier, April 27, 2017.
ing Society, noted that the goal for the workshop was to examine innovative care delivery models from concept to action and success, and to include the experiences of those who benefit from these models. “You will notice that we start broadly and then get very focused as the day goes on, with many exemplars of what people are doing out in the field,” noted Nevidjon as she previewed the day for workshop participants.
Planning committee co-chair Diane Meier set the stage for the workshop’s presentations by describing the conceptual shift that led to the inception of the field of palliative care. When Meier received her medical training, she explained, the idea was to keep treating patients with every available therapy until there was nothing left to do but send the patient to hospice. “Those of us who came up and were trained in that environment were increasingly uncomfortable with it,” she said. Meier noted that a person often gets sick, then better and sick again; the process “is not linear” she explained (see Figure 1). Palliative care, she pointed out, recognizes that there are “many quality-of-life challenges from the point of diagnosis of a serious illness and throughout the course of that illness,” whether or not it is cured, whether the individual lives with it for decades as a chronic condition, or whether it is progressive and leads to death.
The workshop format combined an interview of a patient, caregiver, and clinician in the first session with moderated panel presentations and interactive audience discussion exploring a range of topics, including
- Gaps, challenges, and potential strategies for providing community-based palliative care across the age spectrum;
- Examples of high-quality, community-based palliative care delivery models that are measurably improving value for very high-needs populations across the continuum of care throughout the trajectory of a serious illness;
- Essential elements of successful models in a broad range of patient populations, payment models, clinical settings, and geographic settings;
- Workforce needs and the key role of interdisciplinary teams in successful community-based palliative care models; and
- Policy changes to support and spread community-based palliative care for people living with serious illness.
Throughout the workshop’s five sessions, the panelists and audience members shared many examples of patient-centered palliative care improving the lives of individuals living with serious illness and benefiting their family and caregivers. The workshop’s first session featured patient, caregiver, and clinician perspectives, which served to present a human perspective on the benefits of palliative care. The second session focused on the challenges and benefits of applying the principles of palliative care across the age spectrum. The third and fourth sessions highlighted a variety of promising innovations and successful models of providing community-based palliative care in a range of settings. The final session discussed some of the policy options that would enable successful community-based palliative care models to scale and spread.
This Proceedings of a Workshop summarizes the presentations and discussions that presented a broad range of views and ideas. A summary of suggestions for potential actions from individual workshop participants is provided in Box 1. The workshop Statement of Task can be found in Appendix A, and the workshop agenda can be found in Appendix B. The workshop speakers’ presentations (as PDF and audio files) have been archived online.5
___________________
5 For additional information, see http://nationalacademies.org/hmd/Activities/HealthServices/QualityCareforSeriousIllnessRoundtable/2017-APR-27.aspx (accessed June 19, 2017).
FRAMING THE CHALLENGES AND OPPORTUNITIES TO PROVIDE HIGH-QUALITY CARE TO PEOPLE WITH SERIOUS ILLNESS
Meier opened the workshop with a brief overview of the current landscape of palliative care in the United States, explaining that such care is easily accessible in two settings: hospice and hospital. The problem with that, Meier explained, is that most people with serious illness who could benefit from palliative care are not within 6 months of dying and are not in hospitals. “Upwards of 99 percent of people with serious illness are in the community. They are at home. They may be in assisted living or nursing homes, or get care through their doctors’ offices, and that is a huge gap in
access to high-quality palliative care,” said Meier. Palliative care, she said, needs to be available across all settings in the community, offer an array of services in venues that matter most to patients and families, and provide care in ways that ensure smooth transitions among settings.
Meier noted that eligibility for hospice care is restricted by law to individuals who have a prognosis of 6 months or less, as agreed on by two doctors, and who agree to give up regular Medicare coverage for disease or curative treatment. According to the most recent data compiled by the National Hospice and Palliative Care Organization (NHPCO), the median length of time spent in hospice was 17 days in 2014. Meier pointed out that 35 percent of people are in hospice for less than a week and 10 percent
are in hospice less than 24 hours (NHPCO, 2014). Meier explained that “even though it is intended to be a 6-month benefit, in reality it is a 2-week benefit” for many people.
Meier explained that the vast majority of hospice recipients are Medicare beneficiaries over age 65. Overall, of those who do receive hospice care, 60 percent are cared for in their home, while 30 percent receive care in a nursing home, residential hospice, or hospital (NHPCO, 2014). According to Meier, for those in hospice, “outcomes consistently show better quality of life, not only for the person with serious illness, but also for their family, and significantly lower Medicare spending if the length of stay is less than 6 months.” Meier noted that although the number of hospices has nearly doubled from 2,255 in 2000 to nearly 4,200 in 2015 (MedPAC, 2017), there is enormous geographic variation in the use of hospice across the United States. For example, at least half of all Medicare decedents received hospice care in 2014 in states such as Florida and Texas, compared to 21 to 39 percent in states such as New York and Vermont, according to data compiled by CMS (see Figure 2).
In shifting to the hospital setting, Meier pointed to the nearly threefold increase in the availability of hospital-based palliative care since 2000 and explained that in 2015, hospital-based palliative care programs were serving more than 8 million patients each year. Meier noted that all of the U.S. News & World Report 2014–2015 Honor Roll Hospitals and all of the top 20 National Institutes of Health-funded hospitals have palliative care
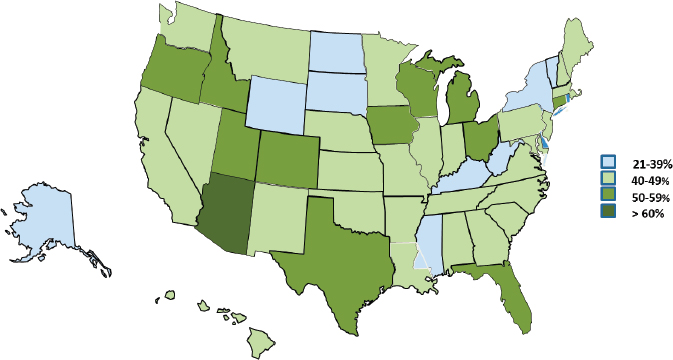
SOURCES: As presented by Diane Meier, April 27, 2017; CMS, 2016.
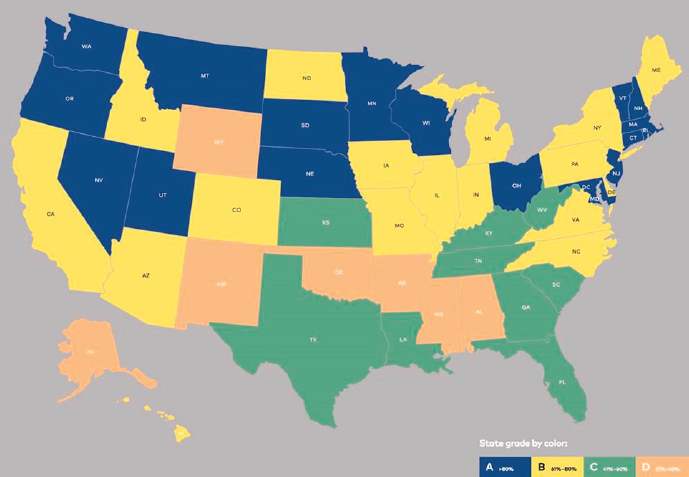
SOURCES: Meier presentation, April 27, 2017 (https://reportcard.capc.org). Copyright © Center to Advance Palliative Care—All Rights Reserved.
teams. Moreover, 97 percent of the Council of Teaching Hospitals member organizations and 87 percent of National Cancer Institute-designated Comprehensive Cancer Centers have palliative care programs. Although the number of hospitals with palliative care programs, as well as the total number of patients served, has tripled since 2000, significant variation remains in the availability of hospital-based palliative care across the United States (see Figure 3), said Meier. She explained that at least 80 percent of the hospitals in the blue states shown in the figure have palliative care teams, while only 20 to 40 percent of hospitals in the orange states have palliative care teams. “Your care depends on where you live in every possible way” noted Meier.
Meier pointed out that data about access to community-based care for people with serious illness is not available. She asked, “How do we get to a point where we say we have the same access to community-based serious illness care models as we do hospital palliative care or hospice?” Meier pointed out that the workshop sessions would demonstrate a number of creative and effective serious illness care models—the “bright lights”—that
shift care for patients out of emergency departments (EDs) and hospitals and into communities where they live.
Concluding her introductory remarks, Meier directed workshop participants to listen for key principles of palliative care that are common characteristics of the models of care featured by workshop presenters. These include 24/7 access to care, attention to social determinants of health, accurate identification of patients at risk, professional skill in managing pain and symptom management, use of interdisciplinary teams, and caregiver support. As Meier pointed out, the workshop presenters would provide proof that it can be done, as consistent outcomes are achieved by a broad range of models across care settings (see Table 1).
TABLE 1 Examples of Community-Based Palliative Care Models
| Program/Model Name | Summary of Key Features |
|---|---|
| PANDA Palliative Care Team Children’s National Health System, Washington, DC, and Bridges Palliative Care, OHSU Doernbecher Children’s Hospital, Portland, OR |
Pediatric palliative care for the preborn to young adults; programs aim to decrease hospital admissions, decrease ED visits, enable seriously ill children to remain at home to the extent possible. The programs work to equip acute care clinicians that have pediatric expertise with palliative care education and training and work with adult hospice partners to provide them with pediatric training through the development of a shared education and mentoring model; also work to expand community-based hospice outreach through in-person training and telehealth collaboration. Programs have demonstrated they can provide seamless coordinated care and provide patients and families better choices in terms of care and setting of care. |
| Transitions LifeCare Raleigh, NC |
Nonprofit, community-based hospice and palliative care organization takes part in the Medicare Care Choices model, a 5-year pilot effort in which hospice eligible patients can receive supportive hospice services and disease-directed treatments. Patients are Medicare or dual eligible with a prognosis of 6 months or less as determined by two physicians, and are in four diagnostic categories (heart failure, COPD, cancer, HIV/AIDS). Services provided include care coordination, shared decision making, symptom management, 24/7 access to nurses/ home visits. Payment is per person, per month rate. Challenges include being able to offer the program earlier, when people have a 12- or 18-month prognosis, limits on diagnostic groups, and sustainability of payment model. |
| Program/Model Name | Summary of Key Features |
|---|---|
| ProHEALTH New York City Metropolitan area |
Multispecialty, home-based palliative care program for seriously ill patients with an initial focus on the Medicare Shared Savings Program ACO; provides 24-hour telephonic support, telepalliative care/virtual visits, coordinates services, arranges home health aides, organizes food and transportation, also provides caregiver support. The program uses claims data such as recent hospitalizations, orders for a hospital bed, and use of home oxygen to identify high-risk patients; most of their patients have five or more chronic conditions. Outcomes of home-based palliative care program include per person per month savings, fewer hospital admissions, and an increased percentage of patients dying at home. |
| MedStar Total Elder Care-Medicare Independence at Home (IAH) Demonstration Washington, DC |
Home-based primary care teams implement palliative care principles such as treatment of symptoms and suffering, 24/7 access to care, establishing clear goals of care according to patient and family preferences, close communication among care team members, patients and family members, psychosocial support, coordination of care across the course of a patient’s life and illness and across all settings. Such home-based primary care has been shown to result in positive outcomes in terms of patient satisfaction and per capita cost of care. IAH Demonstration is a shared savings model; providers are paid within Medicare fee-for-service but also able to share savings if quality metrics are met and per patient costs are reduced by 5 percent compared to expected costs. Challenges include funding for time for travel, family meetings and coordination of services, attracting and retaining the right staff, and training in best practices. |
| ResolutionCare Humboldt County, CA |
Home and community-based palliative care initiative uses telemedicine to provide care for seriously ill patients in remote, rural areas; patients are primarily Medicaid beneficiaries. ResolutionCare partners with health insurers and plans with value-based payment arrangements for palliative care services. Program receives high patient satisfaction ratings. Challenges include attracting physicians willing to work in remote areas, lack of telemedicine parity and national licensure, and reciprocity across state lines. |
| Program/Model Name | Summary of Key Features |
|---|---|
| Commonwealth Care Alliance (CCA) Boston, MA |
Not-for-profit, full-spectrum care system, health plan, and delivery organization focused exclusively on beneficiaries dually eligible for Medicare and Medicaid. CCA serves more than 20,000 members with complex medical, behavioral, and social needs; administers and manages behavioral health, primary and specialty care, acute and post-acute, and long-term services and supports. CCA was the first in the United States to use risk-adjusted premium to create integrated payer and care delivery model. Clinical innovations include a community paramedicine program that responds to urgent care needs of seriously ill patients. |
| Landmark Health (LMH) CA with locations in MA, NY, OR, PA, WA |
LMH is a mobile medical group that provides risk-based intensive patient-centric 24/7 in-home care to the most complex and chronically ill patients. LMH’s interdisciplinary clinical model integrates behavioral, social, and palliative care and provides 24/7 triage capability, pre-911 call, in-home urgent visit when clinically indicated. LMH partners with health plans to share risk based on a prepayment/capitated model. LMH outcomes include high rankings in quality measures and patient satisfaction levels. LMH challenges include provider burnout and retention. |
| Midland Health, Midland, KS Program of All-Inclusive Care for the Elderly (PACE) |
PACE is a comprehensive, fully integrated community-based model of care including primary, palliative, and hospice for frail elderly adults at least 55 years old and certified at nursing home level of function. Payment is based on a capitated rate adjusted for the frailty of the patient population. Medicare requires a 6-month assessment and review of care plans and regular reporting and review of quality measures. Challenges include workforce recruitment and retention and inconsistent state and federal financial support. |
| CareMore Based in Downey, CA, with operations in nine states |
CareMore provides coordinated care through care teams and neighborhood care centers; focuses on three areas: prevention of disease through sub-acute services and fitness centers; chronic care through disease management programs; and acute care through case managers and “extensivists,” internists who see the patient in the hospital and follow them through post-discharge to ensure continuity of care. Clinical results include reduced hospital admissions, fewer hospital bed days, and fewer CHF and COPD admissions. Challenges include sustaining and scaling the culture of care across multiple areas. |
| Program/Model Name | Summary of Key Features |
|---|---|
| Tandem365 Grand Rapids, MI |
Five community-based organizations partnered to form Tandem365; provides comprehensive care services to patients age 55 and older with complex medical needs referred by health plans and insurers. Tandem365’s holistic approach to care focuses on the social determinants of health. Interdisciplinary teams provide 24/7 coverage through nurses and integrated care paramedics. Tandem receives per member per month payments and is in an at-risk contract with a health plan. Challenges include workforce recruitment and retention, expansion of geographic reach, and diversification of funding sources. |
NOTE: ACO = accountable care organization; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; ED = emergency department; OHSU = Oregon Health & Science University.
SOURCES: Adapted from De Jonge, Fratkin, Jain, LaFond, Le, Loughnane, Lustbader, Patel, Perko, Toland, and Wensel presentations, April 27, 2017.
Meier stated that the “data are very clear that palliative care and hospice improve the value equation, improve quality, and lead to reduced costs.” Palliative care, she emphasized, is not rationing. Rather, “It is meeting people’s needs so that they do not call 911 at 3 AM for a pain crisis, because there is no pain crisis,” she said. In closing, Meier asked workshop participants to consider “How do we get from ‘you have to be lucky’ to this is the standard of care?”
The Garrett Family’s Experience with Palliative Care
Building on the roundtable’s first workshop,6 a number of speakers highlighted the importance of hearing directly from patients and caregivers about the transformative impact of palliative care on how they live their lives in the face of serious illness. In this workshop, that critical perspective was provided by Vicki and David Garrett. As Meier reminded the workshop participants, “It always helps to think back to the real experiences of
___________________
6 See http://www.nationalacademies.org/hmd/Activities/HealthServices/QualityCareforSeriousIllnessRoundtable/2016-DEC-15.aspx (accessed August 3, 2017).
patients, people with serious illness in their families, to remind ourselves why this work matters so much.”
Colleen Tallen, medical director of palliative care at LeeHealth, introduced Vicki Garrett, a registered nurse, and her husband David, who together provided the perspective of how a patient and caregiver cope with the challenges of living with serious illness, in this case untreatable mesothelioma. Tallen, Vicki’s palliative care clinician, asked Vicki to share her story with the workshop audience. Vicki recounted how her journey living with serious illness began on a rainy autumn day when she and a colleague were walking to a meeting two blocks from the hospital where she worked. As Vicki described it, she pointed out: “I was healthy. There was no reason why I couldn’t walk two blocks.” She became increasingly short of breath as she walked, however, eventually reaching the point where she thought she was going to have to sit down on the sidewalk. When Vicki finally reached the meeting site, her supervisor took one look at her and declared that she was taking her to the ED immediately. After a preliminary exam failed to reveal any obvious cause of her difficulty in breathing, the attending physician decided to order an X-ray.
After the X-ray images were completed, the emergency room doctor asked Vicki to take a walk with her to see the images. “Being a nurse, and being a surgery nurse, I knew what I was looking at,” said Garrett. “The first words out of my mouth were, ‘Call the thoracic surgeon.’” Vicki added, “he was my friend.” Not surprisingly, Vicki was scared, and when her thoracic surgeon said he wanted to perform what is known as video-assisted thoracoscopic surgery (VATS) procedure to confirm the diagnosis, she agreed. In telling her story, she remarked that her surgeon did not mention any other options, and that she trusted him and was too scared at that point to ask any questions.
When the surgeon gave her the definitive diagnosis of mesothelioma, for which there is no known cure, he told her that she had approximately 18 months to live. His recommendation was to remove one of her lungs, but her pulmonologist said she had insufficient lung capacity and it would be too risky. After talking about her options, her pulmonologist sent her to a specialist, who said her only chance was to have her lung removed and that she had 2 days to decide what to do. She then called Tallen, who Vicki said has been with her throughout this journey. “It doesn’t matter what time of the day or weekends. When I need her, she has been there for me 100 percent of the time,” said Garrett. “She has never said it is an inconvenience. She has walked with me.”
Vicki shared the good news that two subsequent rounds of imaging have shown that her tumor is currently stable. Based on her experience, she and her husband have told others in her situation to look at their options and to not be afraid to ask questions. “Doctors can only tell you what they see on an X-ray, but they don’t know what you are capable of, the strength that you have. They don’t know about your family support. I couldn’t have done it without my family support,” Vicki said.
An important part of her story, Vicki pointed out, is what Tallen said to her when she went to Florida, where she and David spend half the year, not long after receiving her prognosis. Vicki explained that “When I came to Florida, I came to die. That is what the doctors said and I believed them.” Tallen, however, told her she did not come to Florida to die, but rather to live, whether that was going to be 10 days or 10 years. “So I took her advice,” said Vicki. Today, as a firm believer in palliative care, Vicki strongly affirms being honest with patients. “I do think you need to tell them the truth, but I think you can do it in a way that doesn’t scare them to death and doesn’t shut them down,” she explained.
For his part, David recalled the devastation he felt when the thoracic surgeon came to talk to him about Vicki’s condition. He explained that it made him think back to the time many years earlier when his mother was diagnosed with lung cancer and her surgeon wanted to keep the diagnosis a secret from his mother. “I could not believe I heard what I thought he said,” David recounted. “I looked at him and said, ‘You have got to be kidding me. This is her life we are talking about, and she has a right to know exactly what she is dealing with.’ And he was not very happy with me, but I didn’t care because I believed very strongly that my mother had the right to know. So we did tell her and I never regretted that,” David explained.
David felt the same way about talking to Vicki, and the two had long discussions and he was very honest with her. “As we talked, I shared with her that even though the news had not been very pleasant, there was still a part of me that believed that, as I referred to it, she was going to have a very positive testimony.” Some 29 months later, he still believes that. He described when he and Vicki first went to see Tallen, her response was to immediately throw her arms around his wife. He recalled “from the moment that Colleen presented this wonderful notion that we could choose to live, it made a huge difference for both of us.” In concluding his remarks, David thanked all members of the team that care for Vicki: “We are eternally grateful to Colleen, to the oncologist, and to the palliative care people in Michigan”
(where the Garretts reside the other half of the year), “because they truly have made a significant difference in the last 29 months for us.”
Filling in some details, Tallen explained that when Vicki was diagnosed with mesothelioma, it was early-stage disease. There was disagreement between the surgeon, who wanted to cut out the tumor, and the pulmonologist, who said doing so would leave her dependent upon supplemental oxygen. “My role in the case was to give her time to process and facilitate what it would look like to actually live through these decisions,” Tallen said. As a result of those discussions, Vicki decided not to have surgery because as Tallen pointed out, “she did not want to live oxygen-dependent in her home.” Tallen also spoke of the strong connection between Vicki’s palliative care teams in Florida and Michigan. Recently, for example, Vicki developed pneumonia, and a quick response from the team in Florida in conjunction with her oncologist in Michigan kept her from being hospitalized. What makes this possible, Tallen explained, is an infrastructure where people are on call 24 hours per day, 7 days per week. Tallen noted that Vicki knows she has 24/7 access to her care team, but the phone calls are not reimbursed. Tallen noted that shifting from episodic care to longitudinal care requires a change in how health care financial resources are distributed. She added: “Believe me, we have the money. We are just using it in the wrong places.”
Amy Berman, senior program officer at The John A. Hartford Foundation, thanked Vicki for her bravery in telling her story so eloquently. Berman explained that she too is a nurse, and that she, like Vicki, is seriously ill and appreciates all that palliative care does for her. She asked Vicki what she would say to the many people who do not understand palliative care and are frightened by the term. Vicki explained that at first she was also afraid. “I think I would say at some point you need to put your trust somewhere.” If you are fortunate to have a palliative care team, she said, give them a chance. “It took me a long time to come to the point where I was willing to trust that they had my best interest at heart.”
In concluding her remarks, Vicki shared that she has never received any treatment, either chemotherapy or radiation therapy, because it was not going to change her diagnosis. “We know there is no cure,” she said. Instead, Vicki’s care has been guided by her palliative care team. “They shared with me my options, but didn’t push me to make a decision,” she said. “What I did,” she explained, was “chose to just live my life.”
Community-Based Palliative Care: Population Health Management Perspective
Martha Twaddle, senior medical director for Aspire Health, began her presentation by thanking the Garretts for “grounding us in what matters most.” Twaddle shared that she has been working in the field of palliative care for 30 years and pointed out that this specialty was created to reinfuse into medicine the “bio-psychosocial-spiritual model of care, which is one of the deepest roots of allopathic7 medicine.” In Twaddle’s view, “this is where we came from” and where “we are trying to get back to.” She noted that one important reason for establishing palliative care as a formal subspecialty is that it then becomes a formal part of the medical education system that systematizes that way of thinking, reinforcing it through education, modeling, and mentoring. Twaddle underscored the importance of training health care professionals “to think in terms not just of the individual in front of us, but of populations and how to risk stratify and apply the right care to the right person at the right time, which is the hallmark of quality.”
The challenge, explained Twaddle, is to create a scalable system that does not require a patient to be lucky, as Vicki Garrett was, to find a palliative care team, but instead identifies those individuals who would benefit from palliative care as part of the systematic approach. In such a system, care becomes less about prognosis and more about need, noted Twaddle. And given the “silver tsunami” that the United States faces in the form of an aging population, Twaddle emphasized the importance of thinking about different ways to meet this need that engages others in the community. “It’s about the person, and it is about those that love and care for them,” she said.
Referring to her story of Eleanor (who is actually an aggregate of many patients) (see Box 2), Twaddle said it underscores the imperative of providing coordinated care, a system in which hospitals, nursing and rehabilitation facilities, and clinicians communicate with one another. Some may argue that creating such a system would be expensive, but in fact, noted Twaddle, the money spent today on wasted and duplicated services would more than cover the cost of establishing and operating a system that coordinates care to the benefit of patients with serious illness. Twaddle recalled that when she started her career as a primary care internist, she saw her patients
___________________
7 Allopathic medicine refers to a system in which medical doctors and other health care professionals (e.g., nurses, pharmacists, and therapists) treat symptoms and diseases using drugs, radiation, or surgery. It is also called biomedicine, conventional medicine, mainstream medicine, orthodox medicine, and Western medicine.
everywhere they went. As she put it, she was her patients’ electronic health record (EHR), and she spent at least half a day per week visiting her patients wherever they were. “That system works. When we fragmented and limited that system, guess what happened? Our costs escalated,” noted Twaddle.
Twaddle emphasized that palliative care is so effective because “we talk about the person and their family first, the relationships that are therapeutic over and above any medical model, and we emphasize communication, collaboration, and coordination of care.” These three pillars of palliative care are key to improved outcomes, such as reduction in symptom burden, care concordant with patient and family preferences, improved patient and fam-
ily satisfaction, and reduced costs. Put simply, “Palliative care is uniquely effective at addressing the Triple Aim,”8 according to Twaddle.
One challenge, observed Twaddle, is to determine when to integrate community-based support—ideally to identify what people need before they need it—in order to “shift the epicenter of care to the home envi-
___________________
8 According to the Institute for Healthcare Improvement, the Triple Aim refers to an approach to optimizing health system performance. It focuses on three dimensions: “improving the patient experience of care (including quality and satisfaction); improving the health of populations; and reducing the per capita cost of health care.” See http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx (accessed August 17, 2017).
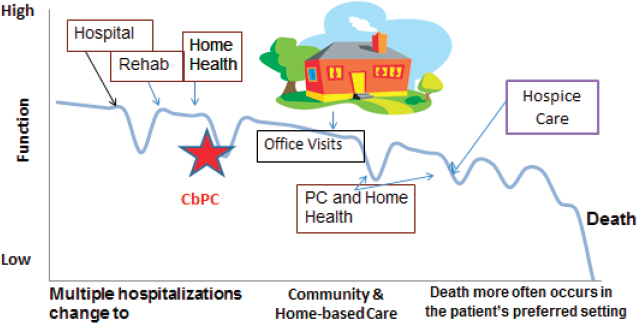
NOTE: CbPC = community-based palliative care; PC = palliative care.
SOURCE: As presented by Martha Twaddle, April 27, 2017.
ronment,” said Twaddle (see Figure 4). Indeed, she proposed that a great quality metric for those with serious illness could be days spent at home. Rather than providing care in the hospital, which comes with its own set of risks, community-based palliative care provides needed services in the home or ambulatory setting, depending on what care is needed. Twaddle underscored the importance of home-based care for people with multiple morbidities and limited mobility.
Twaddle noted that individuals receiving community-based palliative care typically spend a longer time in hospice, which again benefits the person, as well as their family members. Twaddle emphasized the importance of “thinking broader than just the person in front of us,” as well as “recognizing the impact that one life has on many, and how important that is,” noting that is the focus of population health.
Twaddle offered the medical home model as an example of a care system into which palliative care fits naturally. This model serves a population of people, and through risk stratification, identifies those individuals whose care needs to be managed proactively. The medical home care manager could help coordinate care in the community, which would break down silos, said Twaddle, and community services could be home-based primary care or home-based palliative care. Care coordination in this form would facilitate transitions among different components of the health care system
and help with acute care management that would enable those with serious illnesses to avoid the use of services that are not beneficial. As Twaddle pointed out, “We are refocusing care on what is beneficial and definitely coordinating the gaps of care.”
Twaddle shared that she has come to appreciate fully the importance of primary and palliative care working together to provide community-based care. “This is not about palliative care coming on one day and primary care coming the next day,” said Twaddle. “We create a team. We collaborate. We coordinate. And that allows us to scale.” She noted the critical role of telehealth in identifying which resources are required at the bedside. Being in the home also enables the health care professionals to be aware of any social issues that influence care delivery and remain up to date on all of its patients’ medical issues. “The days of EMRs [electronic medical records] not talking to each other, paper faxes when there is no fax machine that works, or it doesn’t have paper in it anymore, those need to go away,” said Twaddle. “We need to drive and insist on systems that coordinate so that we don’t repeat care.” Twaddle reinforced the key themes from the Roundtable’s first workshop,9 pointing out that “really, this comes back to the best care is care that is driven by a person’s preferences and those of their family, integrating information you would find helpful, and really working as a team.”
In summary, Twaddle said it is imperative to use risk stratification to target and identify those individuals who would benefit from coordinated primary and palliative care, to provide that care in a manner that matters most to the individual and that reflects the individual’s prognosis. “We need to be proactive and holistic in our care delivery,” said Twaddle. “Pain and symptom management is part of that, but it is much broader than just that because symptoms are not just physical.” She reminded workshop participants that the other key elements of quality care include 24/7 access to care, support for family and caregivers, and thinking about who is at risk in the future by targeting highest risk people.
Community-Based Palliative Care: Health System Perspective
Stacie Pinderhughes, chair of the division of palliative medicine at Banner Health, also began her presentation by thanking the Garretts, remarking that “it really helps the clinicians and the individuals in the field
___________________
9 See http://www.nationalacademies.org/hmd/Activities/HealthServices/QualityCareforSeriousIllnessRoundtable/2016-DEC-15.aspx (accessed August 3, 2017).
to hear from the voice of the patient.” Pinderhughes also shared a patient story (see Box 2), which she said “exemplifies the need to fundamentally change both our organizational and cultural thinking to really understand that we have responsibility for our patients wherever they are” in their health care journey.
Before focusing on her organization’s approach to value in health care, Pinderhughes presented an international perspective, reminding workshop participants that compared to all other nations with advanced economies, the United States spends more on health care, but fares significantly worse in terms of measures such as life expectancy.10 “This is shocking . . . in a country where you can get second and third and fourth line chemotherapy that is probably not going to help you. We still don’t live as long as other nations that provide health care to all their citizens. We still have work to do,” she observed.
Pinderhughes explained that Banner Health is trying to approach the transition from volume to value in a thoughtful, measured process, and like many health systems, is trying to figure out how the best way to do this from the perspective of population health. Banner Health is a large and growing health system of 28 acute care and critical access hospitals across six states, and recently purchased 23 urgent care centers.
Highlighting that the cost of care provided outside of the hospital setting is growing rapidly and now accounts for a significant portion of Medicare expenditures, Pinderhughes emphasized that “the imperative for health care systems is to figure out how to deliver consistent, safe, reliable, effective, and timely” care in the post-acute setting. For a population health–focused organization such as Banner Health, Pinderhughes said the focus is on changing the organizational structure from the transactional, “do more, get paid more” mentality and framework to reflect a fundamental shift in understanding that “we have responsibility for patients whether they are in front of us at the moment or not—responsibility for the totality of their care.”
Pinderhughes described her organization’s approach to facilitate the cultural transition from volume toward value. Banner Health created several so-called Imaginariums, which serve as innovation testing sites and launch pads for new ideas on how to deliver services to meet consumer needs. She explained that one of the Imaginariums, for example, is focused on design-
___________________
10 See http://www.oecd.org/els/health-systems/health-data.htm (accessed August 17, 2017).
ing the care delivery system that Medicare Advantage members want and expect, and it will endeavor to manage the total cost of care while providing superior quality and a great consumer experience, explained Pinderhughes. She noted that this Imaginarium has the potential to innovate because, as an independent entity separate from the business of Banner Health, it will be free of the “standard cumbersome structure of the health system” and long decision-making process. Pinderhughes pointed out that the Imaginarium will have distinct leadership and teams. Based in Sun City, Arizona, which has a high proportion of Medicare Advantage members enrolled in the Banner Health network, its mission will be to push the value imperative while improving the health of its members through coordination of care.
Pinderhughes summarized that health systems are trying to move from volume to value because the patient is what matters the most. For organizations like Banner Health, the value imperative is driven by the need to reduce health care costs while improving health outcomes and pursuing continuous quality improvement. Ultimately, she noted, the goal is to reduce fragmentation in health care delivery by driving toward an integrated health care system.
Pinderhughes concluded her remarks with some suggestions for working in the current disruptive environment as health care organizations gradually transition from a fee-for-service model to a value-based, population health model (see Box 3).
Reacting to Pinderhughes’ presentation, Meier asked about Banner’s “decision to separate out the innovation engine from the mainstream machinery of the health system.” Pinderhughes explained that as an organization, “Banner Health didn’t really know how to do population health in terms of a value-based approach,” and they realized that “they needed to do something drastic and different.” She explained that Banner is at the very beginning of the journey and the Imaginariums are not yet fully operational. Meier added that the states, Medicaid, and insurance companies are all part of the drive toward value. “Value is not going away,” concluded Meier, “because the rest of the health system is committed to it.”
PALLIATIVE CARE PRINCIPLES ACROSS THE AGE SPECTRUM
In introducing the second session’s panel speakers, Brenda Clarkson, executive director of the Virginia Association for Hospice and Palliative Care, noted that as a hospice nurse since the 1980s, she has witnessed the
birth of palliative care. She explained that the second workshop session was organized to examine palliative care principles across the lifespan. Clarkson referred to Diane Meier’s earlier comment that palliative care’s whole-person approach needs to be available to anyone regardless of age, state, disease, or prognosis. That does not mean, however, that palliative care programs for children and their families will be the same as those for a 40-year-old with cancer or an 80-year-old with chronic kidney disease and congestive heart failure.
Pediatric Palliative Care
Pediatric palliative care refers to programs that work with children from the pre-born to toddlers to young adults and their families, explained Kathy Perko, pediatric nurse practitioner and program director of the Bridges Palliative Care program at the Oregon Health & Science University Doernbecher Children’s Hospital. Perko emphasized that improving the care of children and their families through palliative care is critical because approximately 43,000 children ages 0 to 19 die every year, accounting for approximately 1.6 percent of all deaths in the United States (Osterman et
al., 2015). “Although it is a small number, it is a significant number. It is life changing for those families,” she said.
More than half of the children who die annually are infants, and half of those infants die within the first 30 days of life. In addition, at any one time, some 5,000 children are nearing the end of their lives (Feudtner et al., 2001), and 400,000 U.S. children have chronic health care conditions, including cystic fibrosis, Duchenne muscular dystrophy, cancer, cerebral palsy, and congenital heart disease, which can have a major effect on quality of life. Caring for these children accounts for as much as one-third of health care spending on children, or approximately $100 billion annually (Cohen et al., 2012; Kuo et al., 2011; Lassman et al., 2014). As is the case with adults, children with serious illness make more visits to the ED and hospital, and their hospitalizations tend to be lengthy. “We believe, and we have seen with good palliative care, we can decrease those hospital admissions. We can decrease those emergency department visits. We can keep those kids at home where they want to be and where their families want them to be,” said Perko.
Palliative care, explained Perko, “is not always about end-of-life care and pain and symptom management.” It is about “how do we meet these families where they are, and then help these families go through this process.” In some cases, she said, palliative care can be as simple as providing a child with two sets of books, one at home and one at school, so they do not have to carry their books between the two. One of the keys to good pediatric palliative care, she explained, is the interdisciplinary team approach, because “none of us can do this by ourselves. It is emotionally difficult” and requires a broad range of knowledge and expertise.
While the main principles of pediatric and adult palliative care are similar—relieve suffering, slow progression of the disease, and improve the individual’s quality of life at all stages of the disease—there are important differences (see Table 2). Perko pointed out, for example, that given the importance of play for children, pediatric palliative care emphasizes enabling children to play, as they move through their lives with chronic conditions, and even as they near the end of their lives. To meet that need, child life specialists have a key role in pediatric palliative care, helping not only the children, but also the members of the palliative care team, “to look at the big picture” and work with “every child, every infant, and every family to have this day be the best day they can have,” Perko explained.
Pediatric palliative care also differs from adult palliative care with regard to the primary decision maker, with parents and guardians, rather than the
TABLE 2 Adult Versus Pediatric Palliative Care
| Adult Palliative Care | Pediatric Palliative Care |
|---|---|
|
|
SOURCE: Lafond and Perko presentation, April 27, 2017.
patient, serving as the decision maker. That becomes a gray area, however, as children get older. “What about the 15-year-old?” asked Perko. “How are we addressing their needs? How are we talking to them? How do we engage the parents of the families, sometimes it is a grandparent, and the child, to look at advance care planning?”
Perko pointed out the increasing use of technology for pediatric patients, particularly newborns. As a result, some infants go home on ventilators or with gastric feeding tubes that require complex care by family members, and palliative care programs need to address that challenge. “We are asking families to do more and more with their children because of the increasing use of technology,” said Perko. “It is not right or wrong. It is a family decision, and it is different for every child.”
Developmental issues are a concern when caring for seriously ill children, particularly when there are other children in the family who have different understandings, depending on their ages, of what it means to have a serious illness and face death. “How do we, as a team, an interdisciplinary team with our social work colleagues, our child life specialists, our nurses, our physicians, our families, and our hospice teams that take care of these kids—how do we come together to really address the developmental issues of kids?” asked Perko.
To illustrate how the principles of palliative care can be applied in the pediatric setting, Perko recounted the story of Jody, who gave birth prematurely to twins Jack and Kate. At 24 weeks, after what had been an uneventful pregnancy to that point, Jody experienced some bleeding, so she left her 4-, 6-, and 7-year-old children with her husband and drove herself to the hospital. As Perko recounted, she and her team partnered with the neonatal intensive care unit (NICU) and obstetrics teams to talk to Jody
and her husband about what they wanted for their babies at that time. “They wanted everything done,” said Perko. When the twins were born 12 days later, it was clear within an hour that Jack was not going to survive. “Our palliative care team came together with Child Life and Social Work and arranged for that mom to go to the resuscitation room to spend that last bit of time with her son Jack and then spend 103 days in our NICU with Kate,” Perko explained. During that time, the palliative care team provided bereavement services and active childcare. They answered questions and sat next to Jody’s bedside when she needed to talk to someone. Today, Kate is 16 months old, and she is nearly walking and doing well. “That is what palliative care is for pediatrics,” said Perko. “It is a family experience.”
For many years, said Deborah Lafond, a nurse practitioner with the PANDA Palliative Care Team in the Division of Hospitalist Medicine at the Children’s National Health System in Washington, DC, families with seriously ill or dying children were forced to make a choice between potentially curative or life-prolonging treatments and improving quality of life through palliative care. “We asked them to make an almost impossible choice, a choice that can be perceived as being life or death,” explained Lafond. Consequently, she said, few parents chose to enroll their children in hospice, and if they did so, it was often at the very end of their child’s life. When that happened, a new set of caregivers would come into the home knowing nothing about the child or family, with little, if any, chance to develop a meaningful relationship with the family. Too often, the family would have to end their relationship with their primary care teams.
The ability to provide disease-directed treatment at the same time as palliative care was facilitated by passage of the Patient Protection and Affordable Care Act of 2010, which contained a specific provision on concurrent care for children, enabling palliative care services to be provided without being required to first discontinue curative therapy. However, explained Lafond, this provision only applies to children under age 21 who have Medicaid or who are enrolled in the Children’s Health Insurance Program and for whom a doctor certifies that the child is likely to die within 6 months.
Lafond pointed out that concurrent care reduces costs by 11 to 27 percent (Gans et al., 2012) and days spent in the hospital by nearly 50 percent (Gans et al., 2016). However, the most important benefit of concurrent pediatric palliative care is the continuity of care it provides noted Lafond. “It gives us time for the hospice to develop these relationships with patients and families, to know what is more important to them at the most vulnerable
times of their lives, and to be able to help guide them and prepare them as the end of life nears,” said Lafond.
As an example of ways to build on concurrent care to optimize care for children with serious illness, Perko described the Bridges Palliative Care program at her institution. This program started in 2003, she explained, after two parents whose children had died shared their experiences with a nurse in the Doernbecher Children’s Hospital oncology clinic. The parents explained that the clinic could improve continuity of care when children left the hospital to die at home. After conducting a survey of every hospice in Oregon and southwest Washington state to find out if they would be willing to take care of children, it was clear there were significant issues to address. “They wanted to know about developmental issues, and how to disclose information to kids, but mostly they wanted to know how to take care of themselves,” said Perko. In other words, she explained, hospice caregivers were unsure how they would deal with the emotional challenges of working with seriously ill and dying children when they went into the hospice field to take care of elderly adults who were dying.
To address those issues, Perko and her team created the Bridges Palliative Care program, which includes an interdisciplinary educational program, webinars, telehealth, support calls for nurses and other palliative and hospice care staff, and regular calls with families, as well as an annual conference. The goal of this program, explained Perko, is for families to turn to the local hospice or palliative care team in their community. She told a story of an 8-year-old with recurrent cancer who informed her hospice team that she was having trouble sleeping. The nurse and social worker in the hospice team asked the girl about it, and the girl replied that she was afraid of death, which she said she was dreaming about at night. When asked if there was anything that could help, the girl replied that she would not be afraid of death if she could have a pair of angel wings to wear when she slept. As Perko recalled, the hospice team got their art supplies together and with the help of the girl’s parents and siblings, made a pair of angel wings. “Then she put those wings on at night, and she was never afraid of death again. This is why pediatric palliative care and community hospice matters,” said Perko.
Lafond described the PANDA primary palliative care program she and her colleagues developed at the Children’s National Health System. There, primary palliative care pairs the clinicians in the acute care setting, including physicians and advanced practice nurses who have extensive pediatric experience, but limited hospice and palliative care training and experience, with adult community hospice providers who have hospice and palliative
care training but limited training and experience in pediatrics. Lafond noted that the year-long program, which includes individual and unit-based mentoring as well as didactic education, has had three cohorts with 149 participants from all of the disciplines involved in palliative care. She noted that the next cohort, scheduled to start in the fall of 2017, will include community-based primary care pediatricians and advanced practice nurses.
One measure of the program’s success, said Lafond, is that more than 92 percent of all pediatric oncology patients are referred to the program. In addition, there are now automatic referrals for every bone marrow transplant, heart failure patient, and brain tumor patient, and the program recently started working with the health system’s cystic fibrosis and muscular dystrophy programs. She noted that the program has produced a mobile device application called My Neighborhood©, which enables parents to find the resources they need to help manage their children’s pain and symptoms at home, and has an active telehealth program for mentoring adult hospice nurses who are providing pediatric palliative care in the child’s home.
To illustrate why this effort matters, Lafond told the story of Justice, a 14-year-old girl with cerebral palsy. At age 6, Justice had a significant intestinal problem that led to having nearly all of her intestines removed, and as a result, she required technology to help feed her. During the 2 years prior to connecting with the PANDA palliative care team, Justice’s family had noticed her change from a child who smiled and giggled frequently and was very engaged with her siblings, to one who had more bad days than good ones. Justice’s mother asked her primary medical team about palliative care, but the response was that Justice did not need it because she was not dying.
Justice’s mother knew better and called the PANDA program office herself. “So we sat down with the medical team. We sat down with the parents. We had a very open and honest discussion about what goals of care are,” said Lafond. Though Justice eventually died at home, her mother said that before that happened, the smiles and giggles came back and Justice was once again the center of her family. “So when she died, that is what the mother remembers,” said Lafond. “She does not remember the bad days.”
In closing, Lafond noted that both the pediatric palliative care programs she and Perko described have demonstrated the ability to provide seamless coordinated care and education to increase advance care planning conversations. Moreover, she pointed out that they have helped parents and families to have access to better choices in terms of the type and setting of care provided to their children.
When asked about institutional culture barriers that affect their two
programs, Perko said that one barrier is the attitude of not giving up, while another is the attitude that these programs are taking patients away from primary care. The challenge with the first barrier is that there are few pediatric palliative care programs in the United States and as a result there is very little knowledge among pediatric care providers about what hospice and palliative care can do for their patients. Both programs have taken the approach of engaging communities to spread the word about these programs. To address the latter issue, both programs have structured their programs as consultative services that augment what the primary care team is doing, which has the effect of supporting both the care team and the family.
Medicare Care Choices Model
Referring back to Meier’s earlier presentation, Laura Patel, chief medical officer at Transitions LifeCare, a nonprofit, community-based hospice and palliative care organization in Raleigh, North Carolina, pointed out that while the use of hospice care in the United States has increased overall, with fewer individuals dying in hospitals (Teno et al., 2013), the median length of stay in hospice is still only 17.4 days.
Citing one of the key barriers to hospice is the need to forgo curative or disease-directed treatment, Patel noted that “This is increasingly challenging as our medical culture and research are finding the latest new technologies, chemotherapies, and surgeries. It is very hard for patients to decide to give up those options.” Other barriers to hospice include the perception that going into hospice means giving up, and the belief that hospice is only for the last few days, when one is actively dying. Yet another barrier to hospice, explained Patel, is our health care culture, which views dying as a failure on the part of health care professionals. Finally, predicting the future course of disease is becoming increasingly difficult at a time of rapid medical progress, including new treatments, which poses another challenge for hospice.
In an effort to address these barriers, CMS introduced the Medicare Care Choices model in 2014 to enable patients to receive curative or disease-directed treatment, while simultaneously receiving hospice-like support. Patel explained that the model was designed to explore whether taking the word hospice out of the title of the program—while providing similar support without restrictions on treatment—would entice more people to select access to this support. CMS will evaluate whether providing these
services can improve the quality of life of patients facing serious illness, increase patient satisfaction, and reduce Medicare expenditures.11
Initially, Patel explained, the plan was to enroll 30 hospices over a 3-year period, but there was so much interest that 140 hospices are participating in two cohorts. Over the course of the 5-year pilot, CMS will evaluate access to hospice, overall Medicare expenditures, and quality-of-life and satisfaction scores. Patel explained that admission into the program is restricted to individuals who have had at least one hospital encounter and at least three office visits over the previous 12 months, live at home, are eligible for hospice, and have a diagnosis of congestive heart failure, chronic obstructive pulmonary disease (COPD), cancer, or HIV/AIDS. Individuals in Medicare Advantage and other managed care programs or who have received hospice are not eligible to participate.
The model, Patel explained, is based on the interdisciplinary framework of hospice and focuses on care coordination, shared decision making, and symptom management. “We like to call it hospice light or palliative care heavy because it does offer more than your traditional fee-for-service palliative care consultative approach, but is less comprehensive than hospice care,” said Patel. Participants receive round-the-clock access to nurses, including home visits in the middle of night if needed, using on-call hospice staff. She noted that her organization has developed some routine order sets for symptom management that primary care physicians can elect to sign when their patients enroll in this program, allowing its nurses to have some ability to manage these patients at home. Experience has shown, however, that triage nurses manage most of the calls because patients generally are looking for reassurance rather than needing a medical visit. “If they do need a visit, it is usually because they are in crisis,” said Patel.
Hospices participating in the program receive a per beneficiary, per month payment of $400, or $200 if the patient is enrolled for less than 15 days. This payment model, said Patel, differs from the typical daily rate that hospices receive and is meant to be all-encompassing with regard to providing all services patients need related to their terminal diagnoses. Medicare Parts A, B, or D cover therapies, medications, equipment, ambulances, and hospitalizations, and patients are subject to the standard 20 percent co-payments for those services.
Patel said her organization has been able to integrate this model into its
___________________
11 For detailed information, see https://innovation.cms.gov/initiatives/Medicare-Care-Choices (accessed September 11, 2017).
organization in part because it already had a strong infrastructure of using its nurse practitioners to provide community-based, non-hospice palliative care. “This program allowed us to kind of share staff and responsibilities and leverage them both to make both programs more successful,” she said. Nurses in Patel’s organization’s Care Choices Program, for example, help triage palliative care patients, and the medical director, social workers, and chaplains serve dual roles as well. The nurses in this program are not hospice nurses, though many were hospice nurses or hospice admission nurses at some point in their careers. Patel explained that the nurses have strong skill sets in communication, which is essential because they are the contact for patients and families, and in assessment, which is important because they are the ones in patients’ homes and identifying issues they can bring to the attention of the medical team.
Other programs having success with this model have integrated it successfully into their hospice teams, which ensure continuity of care according to Patel. One challenge for hospice nurses, Patel explained, is that they have to live in a “gray area” in which patients are accessing care while the goals of care are still being developed. “As an organization, we need to then support our hospice nurses to make sure they have the resources and skill sets to be able to support their patients,” said Patel.
Patel noted that collaboration with organizations in the community, such as Meals on Wheels, transportation services, and home delivery pharmacies, plays an important role in implementing this model successfully. One of her organization’s hospitals, for example, has a telephonic heart failure team that refers patients to the program because it believes the Care Choices nurses can be their eyes and ears in the home and help keep patients out of the hospital. The program’s palliative care nurse practitioners also follow the large majority of the patients, allowing for more active symptom management and assistance with complex decision making. Patel said she considers this one of the program’s strengths.
Patel explained that the oncologists in her community refer patients to her program frequently, and work with the team to provide insights into whether a patient’s treatment is still effective and discuss when it is time to transition to hospice. Patients with congestive heart failure and COPD have a more variable trajectory, said Patel, and many are elderly and have multiple other conditions. Often, when entering the program, they have just come from a stay in the hospital or rehabilitation facility and can look as though they are in their terminal decline. However, once some supports are in place, they can do better for an extended time, she added.
The common denominator among these patients, said Patel, is that though eligible for hospice, they have all chosen not to pursue it as an option. “There is a high likelihood that this group may never have come to hospice,” she said. Nevertheless, the majority of patients who do receive care from this program do die on hospice, which Patel said speaks to “the impact of this high-touch, interdisciplinary approach and its ability to develop trust and rapport” with people with serious illness and their families.
As with any pilot program, there is room for improvement, explained Patel. The limited ability to predict when patients with serious illness are nearing the end of life is perhaps the biggest obstacle, said Patel. “We feel that by the time we get in there, sometimes it is late. We want to be in there sooner. We would love to be able to offer this service for people who have a 12- or 18-month prognosis.” Another issue to resolve, she said, was how to adjust the payment model to account for the heavy care needs of these patients. While both patients and caregivers benefit tremendously from aide support, providing it on a frequent basis under the current payment model is not realistic or sustainable, she said. In her opinion, CMS needs to provide more clarity on how this program fits with other home support programs, such as home health, so that they can all be maximized. Patel said she would like to see the program expanded to other diagnostic groups with long periods of caregiving needs, such as dementia, amyotrophic lateral sclerosis, and end-stage renal disease.
The program’s strengths, according to Patel, include its ability to reach a patient population that may never have come to hospice. It does so, in large part, by reassuring people that they do not have to give up any treatment options. As a result, patients have more time for decision making while still receiving the supportive care that benefits them and their caregivers. Patel wondered if this program might benefit traditionally underserved communities, who as a whole tend to underuse hospice. Other strengths include providing some caregiver relief, round-the-clock access to support staff, and a smoother transition to hospice with little delay or disruption when the time is right. This last benefit, said Patel, is why she believes this type of model should be embedded in the hospice framework.
Patel recounted that a speaker at a local meeting described these types of programs as a way for people to “come sit on the porch for a while,” take their time, get to know the program staff, and eventually feel comfortable inviting them into their homes. “I think many people just need that extra little time, that extra little reassurance that hospice does not mean they are giving up,” she said.
Patel ended her presentation with the story of Brenda, a 68-year-old woman with end-stage COPD who had been receiving care in the community for several years from Care Choices nurses. Eventually, she had a crisis, was hospitalized, and was intubated in the intensive care unit. One of Brenda’s Care Choices nurses, who knew from previous conversations that she did not want long-term ventilator support, was able to confirm this with Brenda and talk to her family. She arranged for Brenda to be extubated and admitted to hospice in the hospital, where she died peacefully with her family by her side. Her family members are now receiving bereavement support from the program.
From a statistical view, this might seem to be a failure because Brenda went to the hospital several times during her last 3 months and died in the hospital. “That is why people are so much more than statistics,” said Patel. “This was what was right for her. This was the path she needed to go down.” Brenda and her family, she added, received much more support than they would have had otherwise without the Care Choices program. Even on Brenda’s last day, she and her family received guidance and reassurance from the team. In closing, Patel pointed out that “Ultimately, that is what this program is about: meeting the patient where they are at, wherever that is, providing whatever support we can for whatever time we can for these patients and families who have a great need.”
Adult Palliative Care in a Value-Based Payment Model
Dana Lustbader, chief of the department of palliative care at ProHEALTH, an Optum Company, described how she became interested in exploring how home-based palliative care could better support those with serious illness after working for 20 years as a hospital-based critical care physician. Her organization is a 900-physician multispecialty group that serves more than 1 million people in New York City metropolitan area, with 100,000 patients in a shared-savings arrangement. Lustbader explained that ProHEALTH developed a home-based palliative care program 3 years ago, as part of a Medicare Shared Savings Program accountable care organization (ACO), which currently has 35,000 enrolled members. The program was then expanded to other shared-savings contracts. Lustbader’s program provides in-home team-based palliative care and 24-hour-a-day telephonic support for both the patient and caregiver, and it works with community partners to coordinate other services, including coordination of care with
the patient’s other doctors, arranging home health aides, assisting with food and transportation when needed.
As an example of a typical patient, Lustbader told the story of Frank, an 87-year-old with dementia, heart failure, and kidney disease who uses a walker and is cared for by his son and 86-year-old wife, both of whom are overwhelmed. Frank has had multiple trips to the ED and, given the oversupply of hospital beds in New York, he typically gets admitted to the hospital and ends up in the intensive care unit. He is not terminally ill, so he is not eligible for hospice. However, with home-based palliative care, which provided 24/7 telephonic support, caregiver support and coordinated with Meals on Wheels and a friendly visitor program, Frank’s condition stabilized and he had no ED visits or hospitalizations in 9 months.
The space that the ProHEALTH Care program addresses is what Lustbader called pre-pre-hospice, a period spanning approximately 6 to 18 months before a person would be eligible for hospice, and the target population includes the so-called super users—those individuals with multiple chronic conditions that typically send them to the hospital. Rather than wait for referrals for the system’s clinicians, however, Lustbader and her colleagues actively search for these patients using an algorithm they developed to mine the claims data they have access to as a result of being a Medicare Shared Savings Program ACO. While there are limitations to using a claims-based algorithm to find people who would benefit from palliative care, Lustbader said the data provide important information. For example, having a hospital bed ordered for a patient was highly predictive of a patient dying within 1 year. Coupling that with other indicators, such as having COPD and being on home oxygen, enables Lustbader to identify and target patients with very high needs.
Once identified, engagement staff calls the individuals and asks if a nurse can come out to their homes to see how they are doing. “We don’t ever use words that might be a barrier to patients and their families; we do not use the words palliative care,” said Lustbader. She pointed out that “most people really welcome a nurse or doctor coming to the home to provide care.”
Lustbader and her colleagues also work with associated health plans using the approaches those plans have to identify high-risk patients, and she pointed out that the health plans provide their data within a day or two of discharge. In addition, they receive notifications when patients are discharged from the hospital and use a variety of methods, such as two or more recent hospitalizations, a high LACE index score and Charlson Comorbid-
ity Index12 to identify high-risk patients. Particular clinical triggers include having five or more chronic conditions, a high-risk score, chronic kidney disease with depression and other co-morbidities, and frailty or functional decline. She noted that in the Medicare population, patients who have cancer as their primary diagnosis requiring palliative care account for only 20 percent of her program’s clients, with those having multiple chronic conditions accounting for the remaining 80 percent. In the younger commercial population her organization serves, by contrast, 70 to 80 percent of the patients have cancer as their primary diagnosis requiring palliative care, Lustbader said.
Each palliative care team has three registered nurses, half to three-quarters of a palliative care physician or geriatric physician, and half of a social worker to serve approximately 250 patients. Patients receive a minimum of one visit at home per month, with more frequent visits determined by each patient’s specific needs. For example, a patient recently discharged from the hospital or rehabilitation facility might receive two visits the following week. Interdisciplinary teams meet twice weekly for 90 minutes to discuss difficult cases and to engage in educational activities. On occasion, these meetings include a virtual visit with a family member and patient and include teachings for the family member. In addition to the interdisciplinary team meetings, the individual team members—the nurses, doctor, and social worker—meet in person every week for an hour to discuss issues such as deprescribing drugs to reduce the pill burden on patients.
The program includes a telepalliative care component using a platform that complies with the Health Insurance Portability and Accountability Act (HIPAA) requirements. During a home visit, the nurse downloads the app onto the patient’s or family member’s smartphone. Using this app, the team can deliver care for acute issues, schedule follow-up visits, help with advance care planning that involves far-away family members, and provide caregiver support. Lustbader said this program uses the VIDYO app, though others such as Skype for Business and Zoom are also HIPAA-compliant.
Discussing the outcomes of her organization’s home-based palliative care program, Lustbader said that people who received home-based palliative care cost $12,000 less over the last 3 months of life than a control group
___________________
12 The Charlson Comorbidity Index (CCI) predicts 10-year survival in patients with multiple comorbidities. The LACE index, which incorporates four parameters (length of stay, acuity of admission, CCI, and number of emergency department visits in preceding 6 months) identifies patients who are at risk for readmission or death within 30 days of discharge.
of patients matched on 22 parameters by actuaries at Optum Health. For patients who do not die, savings reach $2,000 or more per enrolled member per month. In addition, 85 percent of those patients receiving home-based palliative care who died did so at home, compared to 25 percent of those receiving usual care. People who moved from home-based palliative care to hospice also spent more time in hospice—34 days on average compared to 7 for those receiving usual care (Lustbader et al., 2017).
In closing, Lustbader characterized fee-for-service payment as “an enemy” to good palliative care. “It drives churn and it rewards excessive care,” she said. “Innovative models of payment are really critical and would allow us to deliver the kind of care people need, which is that 24/7 care and primarily with a focus on care at home.” She noted that CAPC, which has a registry of inpatient palliative care programs and will be starting one for community and home-based palliative care, will become a good source of information on the benefits of these programs.13
The discussion following the speakers’ presentations began with a question from workshop participant Paige Bingham with Allina Health in Minneapolis. She asked about the idea of using community health workers as part of interdisciplinary teams providing home-based palliative care. Patel said the concept of employing community resources and training non-clinical professionals to provide additional support in the home is essential as “we build out these home-based palliative care models.” Lustbader pointed out that her program has an active volunteer force that it draws upon to provide additional services, such as Reiki therapy and massage therapy. These volunteers, she added, participate in the team meetings to discuss the patients they see. Home health aides also provide additional services to those families that can afford them—Medicare and private insurance plans do not cover them. Medicaid will pay for home health aides and her program helps patients apply for that help.
Rebecca Kirch of the National Patient Advocate Foundation thanked the presenters for their focus on the needs of infants, children, and their families, and highlighted the opportunity for cross-learning between adult and pediatric palliative care. She asked the speakers about their approach to garnering executive-level support for and financial investment in these types of programs. For Lustbader, the focus on patients enrolled in Medicare Shared Savings Plans made it easier to convince health system executives to
___________________
13 For more information, see https://palliativeinpractice.org/palliative-pulse/palliative-pulse-august-2017/mapping-community-palliative-care (accessed September 11, 2017).
approve a program that reduces hospitalizations and saves money. She said, though, that such financial alignment was not present several years earlier when she had tried to convince the large hospital where she was working to start a home-based palliative care program in an effort to reduce hospital usage.
Patel was able to show the impact of palliative care in terms of cost savings from reduced hospital readmissions. She also noted the importance of drawing on personal experience in discussions with executive decision makers. “People in the C-Suite have families. A lot of them have gone through an illness.” Perko and Lafond agreed that cost savings and the personal stories were critical when looking for executive-level support for their programs. Lafond noted that the patient and the family are best placed to tell their stories. “In pediatrics, in particular, having siblings talk about” the impact of serious illness for their family and “how palliative care helped them, tells a powerful story that we (as providers) can’t get across in a meaningful way.”
Pamela Hinds of the National Children’s Health System, referring to the expansion of the Triple Aim framework into the Quadruple Aim, wondered what programs can do to sustain the well-being of their health care providers. Lafond said her program is proactive in the interventions it runs for staff and has regular self-care activities. Doing so, she noted, can require creative approaches to budgeting, and she acknowledged budgeting for such activities is an area of weakness for her program. The chaplains in her program created a mobile room called the comfort corner that has music, art supplies, chocolate, and other things that make staff feel better. They also hold dance parties with the children. Perko said the nurses in her program have made their breakroom a “no complaining zone” and that her program has been working to incorporate more self-care activities and ways of reminding one another—and the rest of the health system—about the value of what they are doing. Lafond also noted the importance of supporting those providers such as oncologists and the team in the NICU who may not be part of the formal palliative or hospice care team, but who also mourn the loss of patients.
Patel noted that her health system created an escape room with beanbag chairs and giraffes in the window to provide an uplifting environment for staff. Lustbader said strategies she uses include fun Fridays at the end of every month that include competitive charades, and she also hosts quarterly wine and cheese parties. She also encourages staff to take pictures of something uplifting and include a humorous message to send in a text to
the entire group. The goal of all these activities is to incorporate self-care into care delivery, recognizing that providers will not be able to take care of patients and their families unless they take care of themselves as well.
PROMISING INNOVATIONS IN PROVIDING HIGH-QUALITY, COMPREHENSIVE PALLIATIVE CARE
The workshop’s first two afternoon sessions were devoted to learning about innovative, real-world applications of palliative care principles to provide person-centered care for individuals with serious illness. Speakers discussed programs that provide care in the home, care for the Medicare/ Medicaid dual-eligible population, and caring for patients in remote, underserved areas. Speakers discussed the challenges and opportunities presented by different models of care delivery. To illustrate why innovative palliative care programs, such as those discussed at the workshop, are so critical, Marian Grant, director of policy and professional engagement at the Coalition to Transform Advanced Care and a nurse practitioner, shared an example of what happens in the absence of such programs (see Box 4).
Home-Based Primary Care Through Independence at Home
K. Eric De Jonge, primary care geriatrician and executive director of the MedStar Total Elder Care program, began his presentation by encouraging workshop participants to believe they can change the system to provide better care for individuals with serious illness, citing his experience over the past nearly two decades as proof that it can be done. De Jonge described how MedStar Health provides services to some of its clients through CMS’s Independence at Home (IAH) Demonstration. The IAH Demonstration is designed to test the effectiveness of delivering comprehensive primary care services in the home setting. It also seeks to determine if providing such care at home improves care for Medicare beneficiaries with multiple chronic conditions, enhances patient and caregiver satisfaction, and results in reduced costs. Under the IAH Demonstration, providers that meet certain quality metrics share overall cost savings.14
The clinical model for De Jonge’s program is team- and home-based primary care employing palliative care principles for patients who have seri-
___________________
14 For more information, see https://innovation.cms.gov/initiatives/independence-at-home (accessed September 11, 2017).
ous illness and functional disabilities, have been high-cost in recent years, and have trouble getting out of the house to see a doctor. As an example of the type of patient his program focuses on, De Jonge described Ms. C., age 72, had liver and heart failure, suffered from depression, fell frequently, and was cared for by her daughter. In 2011, her daughter moved Ms. C. from Colorado, where she had six hospital admissions over the previous year, to Washington, DC, so that she could enroll in De Jonge’s program. Between 2011 and 2016, Ms. C. received more than 200 urgent and routine house calls from social workers, nurse practitioners, physicians, and other service providers, and even had X-rays, electrocardiograms, echocardiograms, and blood drawn for lab work in her home. The program provided her with a mobile EHR with a secure connection to the hospital’s EHR.
In 2014, Ms. C. had a major gastrointestinal bleed that was nearly fatal, but after a life-saving treatment in the medical intensive care unit, she was able to return home within 48 hours. In 2016, she began having respiratory failure and after consulting with family, her primary nurse practitioner, and MedStar Health’s hospice team, Ms. C. transitioned to inpatient hospice, where she passed away 10 days later. Over the course of the 5 years she was in the program, she had only three hospital admissions and spent more than 99 percent of her days at home with her family. Like Twaddle, De Jonge believes that “days spent at home is a very valuable metric.”
The key to the success of this program, said De Jonge, is that the clinical model revolves around the patient and family in the home. The care team is composed of a physician, a nurse practitioner, and a social worker who commits to coordinating the delivery of all of the services the patient and family need in the home, including social services and home aides, physical and occupational therapy, medications and equipment, diagnostics services, and rehabilitation services on a 24/7 basis. If needed, the program also coordinates emergency department and hospital care, including transport to and from the hospital.
This approach to care, De Jonge explained, encompasses major principles of palliative care outlined by Meier in her introductory remarks, including treating symptoms and suffering; establishing clear goals of care; engaging in close communications among the care team, patient, and caregivers; providing psychosocial support; and coordinating all aspects of care. “This is what we would want for all of our loved ones who have serious illness, and the home-based primary care approach tries to meet all of these principles using a primary care house call team that is very skilled in managing all of the symptoms and suffering of serious illness,” said De Jonge.
He added that this is not a consultative or specialty service; rather, it is true primary care that tries to execute these palliative care principles. De Jonge highlighted continuity of relationship of the primary care team over time and across settings as the linchpin, which has “a powerful effect on being able to establish and meet the goals of care” for seriously ill patients.
In terms of the program’s strengths, De Jonge said that the in-home visits have a “transformative effect on listening to and learning from the patient and the family and understanding their needs and goals, which in turn builds trust.” Such trust enables the care team to better navigate with the family the uncertainty that inevitably arises when caring for a seriously ill patient, noted De Jonge.
De Jonge identified other strengths of the program, including having one primary care team that has a relationship with the patient and family over time. The mobile EHR and 24-hour-a-day access enable the program’s 29 staff members to coordinate all services, including acute care. Such care coordination is critical, as De Jonge pointed out: “We manage those transitions in and out of the hospital with the same team that knows the patient and family, and I think that’s really powerful for the patient and family, but also affects metrics like cost of care,” he said.
De Jonge explained that the program’s payment is organized according to a shared-savings model. Medicare reimburses De Jonge’s program on a fee-for-service basis, but if his program meets six quality metrics and reduces total cost per capita by 5 percent compared to expected costs, they are able to share the savings. De Jonge pointed out that according to CMS, the national program saved an aggregate of nearly $33 million over the first 2 years of operation, and providers received incentive payments totaling $16.7 million (CMS, 2017). He added that the IAH Demonstration overall is very popular and that patients and families have been very interested in enrolling in his program, which is oversubscribed. In De Jonge’s opinion, home-based primary care is scalable when achieving quality metrics and savings. Caring for these individuals is still expensive, De Jonge acknowledged, but savings are possible while still providing high-quality care for this population of individuals with serious illness.
The main challenges for his program, explained De Jonge, include funding staff time for travel, family meetings, as well as all that is involved in care coordination. Attracting physicians is also difficult because hospitalist positions pay better, and the same is true for other interdisciplinary staff members. Another challenge is training staff on best practices, though
De Jonge noted that the Home Centered Care Institute is putting together a best practices curriculum for house call programs.15
Building new home-based primary care teams that have staff with the right attitudes, skills, and compassion is the key to successfully scaling this type of program, said De Jonge. Another key to success, he added, is establishing efficient and high-quality daily operations funded by diverse sources of revenue. “If one dries up or if health care reform gets repealed and replaced, you have to have something else to take its place,” said De Jonge.
De Jonge shared three “take-home messages” with workshop participants. The first is that home-based primary care is a team approach that implements palliative care principles as a major part of its work across the patient’s life and illness and across all settings. Second, this approach has proven value with positive results in terms of patient experience and lower costs. Finally, the IAH Demonstration is the subject of a bipartisan bill (S. 464)16 introduced in March 2017; the proposed legislation serves as one example of an effective policy lever to sustain the home-based primary care model.
Reaching Patients in Rural Underserved Areas: ResolutionCare
Michael Fratkin, chief executive officer of ResolutionCare, described his organization as “a people-powered, technology-enabled, home-based palliative care initiative” in rural Humboldt County, California. Fratkin explained that ResolutionCare is people centered in that it cares for the people providing the care as much as it cares for those needing care. In Fratkin’s opinion, this equal treatment is important to the sustainability, stability, and growth of his organization.
ResolutionCare’s interdisciplinary care team has specially trained palliative care physicians, registered nurses, social workers, chaplains, and community health workers, and the team has a flat organizational structure. “There is not a top-down, doctor-driven hierarchy,” said Fratkin, “and, in fact, the community health workers on the team bring a legacy of caregiving and wisdom as well as practical knowledge that tends to lead quite often to clinical discussions and treatment planning for people.”
ResolutionCare operates on a value-based payment model that com-
___________________
15 See http://www.hccinstitute.org (accessed August 17, 2017).
16 See https://www.congress.gov/bill/115th-congress/senate-bill/464 (accessed July 3, 2017).
pensates the full team to provide the right level of care at the right time, he added. Creating this model required an engaged and aligned relationship with health care financiers and health plans. The program receives value-based payment from California’s Medicaid program, in partnership with Partnership HealthPlan, under a program authorized by the state in 2014 that essentially mandates palliative care for all Medicaid recipients in the state. His organization also receives payment from insurers such as Blue Shield of California, which Fratkin described as a “catalytic leader” in value-based payment for palliative care services.
Fratkin said that because his program serves a largely rural, highly dispersed, and primarily Medicaid population, he and his colleagues think less about acuity and more about identifying the needs of individuals at any given moment and what resources they have to meet those needs in an adaptive and nimble manner. The team delivers care either in person or through video conferencing technology, supported on occasion by its community health workers. In-person meetings occur in the home or in the community at coffee shops, the grocery store, or other locations if that is what makes sense, he said. Approximately 8 percent of the program’s clients are in nursing homes or assisted living facilities, and because the program has a contract with the local community hospital, it can provide seamless continuity for its patients when they are hospitalized.
Fratkin described ResolutionCare’s use of telemedicine drawing on smartphones and cloud-based computing to provide relational and longitudinal care using secure platforms that meet HIPAA requirements. Approximately 20 percent of the people his program cares for use this technology to engage their health care team from their home or a non-clinical outpatient setting. Under a value-based payment model, his program can address various technology barriers when they exist. For example, it can lend wireless tablets to its clients or put a satellite dish on the roof to address a lack of connectivity. The large majority of patients in his program—88 percent—report that they like using these technologies and appreciate their value, particularly when it comes to delivering care quickly. “We can slide in an acute encounter in minutes for people and deal with whatever is on their plate at that particular moment,” said Fratkin.
Citing pilot data from Partnership Health Plan, Fratkin noted that 95 percent of the participants surveyed believed they received the best possible care from their palliative care team and would recommend the team to others. The cost of care fell by 33 to 55 percent for pilot participants during the 3 months after enrolling in the program and they experienced 40
percent fewer hospitalizations in the past 30 days of their lives compared to non-participants. The program also showed approximately $3 in hospital cost savings for every $1 spent on the palliative care program. Given that the goal of the pilot program was to make community-based palliative cost neutral, Fratkin said, “We have done that, and we have really knocked the ball out of the park.”
Going forward, Fratkin and his colleagues are working to build network capacity to include small hospitals and critical access hospitals that have no ability to invest in developing a robust palliative care team. His understanding from talking with California state health officials is that less than 25 percent of palliative care teams in the community are fully resourced. “There are many burned out docs out there and by wrapping around our model of care, we can enhance their ability to sustain themselves,” Fratkin explained.
Reiterating remarks by other speakers that staff recruitment is an ongoing challenge, Fratkin hopes to create a work environment that supports and sustains a remote workforce by giving people the freedom to work where they want, while at the same time making them feel integrated into care teams. “Imagine having health care providers and practitioners living exactly where they want to, providing care to people anywhere,” said Fratkin. He also noted that telemedicine offers the possibility of addressing the limited access to care experienced by many underserved communities.
In closing, Fratkin said that in the future, he hopes to establish a proactive system to identify patients who would benefit from his program rather than waiting for referrals from physicians. “We dream of an integrated platform where everything happens in one information ecosphere. Dream with me, please?” he asked, in closing.
Serving the Dual-Eligible Population: Commonwealth Care Alliance
John Loughnane, Commonwealth Care Alliance’s (CCA’s) chief of innovation and medical director of its Life Choices Palliative Care Program, described his organization as a “unique entity” that was formed in 2004 and was one of the “first in the country to use risk-adjusted premiums to create both a payer and care delivery model.” He shared CCA’s approach to taking on 100 percent of the financial risk of caring for “the sickest, most costly, most complicated patients” through two care models. CCA serves nearly 21,000 Massachusetts beneficiaries who are eligible for both Medicare and Medicaid—the so-called dual-eligible population—and it manages all of their covered benefits, including behavioral health, primary
and specialty care, acute and post-acute care, and long-term services and supports explained Loughnane.
Loughnane explained that CCA’s Senior Care Options plan treats dual-eligible individuals who are over age 65, 62 percent of whom speak a primary language other than English and two-thirds of whom did not complete high school. More than 75 percent of the approximately 8,000 members enrolled in this plan are nursing home certifiable, more than 65 percent report their general health status to be “poor” or “fair,” 70 percent have four or more chronic conditions, and 45 percent have three or more impairments affecting activities of daily living, noted Loughnane.
CCA’s One Care plan serves nearly 13,000 dual-eligible individuals under age 65, 70 percent of whom have a behavioral health diagnosis, and 7 percent of whom are homeless, with many more being marginally housed. Nearly 15 percent of this population has a substance abuse or alcohol dependency issue, and there are high rates of unmet needs, particularly in primary care and long-term supports and services, said Loughnane. He noted that the One Care program was designed specifically to address issues of limited access to care. In fact, community health workers and others go out and find people who are having access problems.
Before describing the palliative care program Loughnane developed, he noted the importance for sustainability of demonstrating that programs such as this have a positive return on investment and a good profit-to-loss ratio. “I know if palliative care is showing a good profit-and-loss ratio, my palliative care program is going to survive,” said Loughnane. “I cannot say it enough that it has to have a financial relevance that matches quality,” he stressed. One factor that contributes to the financial success of these programs, he explained, is that the disenrollment rate is low, which means the upfront investments it makes in improving the health of these patients, particularly those in the One Care program, pay off in terms of lower costs over time. “Bringing these patients in and doing the right medicine is expensive. The only way you can then maintain what you do is to care for them over time,” he said. “I think that has a real relevance to palliative care,” observed Loughnane.
CCA launched its palliative care program in 2009 with the goal of “freeing it from three constructs,” said Loughnane. The first construct was the dichotomous idea that patients are well one day and die the next, which, he pointed out in no way reflects human physiology. The second was to change the wording associated with palliative care from “end-of-life” care
to care for people with serious illness, and the third was to embed palliative care into individualized care plans as part of a menu of options.
Loughnane explained that an important component of CCA’s palliative care program is a community paramedicine pilot program funded by a grant from the Patient-Centered Outcomes Research Institute (PCORI) that responds to urgent care needs and provides highly intensive care in the member’s setting of choice at any time of day using specially trained paramedics. According to Loughnane, based on the experience of this program, which aims to provide cost-effective care and reduce ED visits, the state of Massachusetts is developing regulations designed to encourage more models of what he terms “community-powered medicine” across the state.
Concluding his presentation, Loughnane provided some provocative proposals for the health care system. The first is that health care reform should focus on accelerating the adoption of new models of care, based on today’s technologies, which would reduce the significant costs associated with serious illness and end-of-life care. Toward that end, CCA established a subsidiary, Winter Street Ventures, a for-profit health innovation accelerator that partners with early-stage entrepreneurs to take health care technology, devices, and services from concept to marketplace. As an example of such a disruptive use of technology, Loughnane asked the workshop to imagine providing seriously ill patients with access to on-demand home health aides and personal care attendants using the model that Uber and Lyft are using to provide on-demand driving. Not only would the structure make more efficient use of a limited workforce in some areas, but it would also provide a source of income for those in low-income and underserved communities. He also suggested that making more efficient use of community resources in this way could reduce provider burden and burnout.
His second proposal was for the health care sector to use technology to better coordinate care. As an example, he noted how he can buy virtually anything on Amazon and track where his order is whenever he wants, “but if I want to find out about a patient who was discharged from somewhere, it takes me way too long and I give up.”
Community-powered medicine, in Loughnane’s view, requires the realization that the system needs to be disrupted, that good work has to be supported by financial and other results based on data, and that the workforce needs to be engaged in a slightly different way. “I think there is a new dawn, but this new dawn only happens with these three realizations,” concluded Loughnane.
Transforming Care Delivery: Landmark Health’s Complexivist Model
Landmark Health, explained Michael Le, the organization’s co-founder and chief medical officer, is a mobile medical group that partners with risk-bearing entities in 10 markets in six states to deliver 24 hours per day, 7 days per week home care for the sickest, frailest patients. He noted that one advantage of delivering care in the homes of these seriously ill patients is that it provides a good view into the role of their home environments in the struggles they experience, a picture that is impossible to form in a 10-minute office visit. “In the home, there is nowhere for them to hide and you see all of the root causes,” said Le.
Landmark’s approach centers on the use of an interdisciplinary team of physicians, nurse practitioners, physician assistants, case managers, social workers, pharmacists, and dieticians that focuses on the social and behavioral health of the patient. The teams receive specialty training in palliative and end-of-life care. Le explained that Landmark has coined the term “complexivist” to refer to these expert medical teams that provide in-home care.
The financial model that makes this type of care possible, said Le, is one that aligns incentives with the risk associated with the total cost of care. Landmark Health partners with health plans to take both upside and downside risk using a prepayment, capitated model that calculates savings based on improvements in the medical loss ratio. Landmark Health assumes responsibility for the risk of caring for an entire cohort, regardless of whether the members of that cohort engage with Landmark Health. Patient selection, Le explained, is based on chronic conditions rather than hospitalizations or ED visits, which he said makes it easier to identify the real effects the care model is having on a population. If Landmark cannot reduce the cost of care for the selected cohort, it refunds the prepaid funds provided by the health plan. “In essence, these patients would get free concierge-level care in their home 24/7 and the health plans should be none the worse for that. If we are able to generate savings, then we share that with the health plans,” Le explained.
The complexivist model, noted Le, provides high-touch, high-intensive care by the interdisciplinary care team. Initial visits with a patient are 90 minutes long, and subsequent visits are 45 minutes, which provides time to get to know a patient well. “If you really know their baseline well, you may notice that today their color just does not look quite the same, or they are a little less verbal,” said Le. “You may not know what is going on, but you can investigate and really kind of figure out that urinary tract infection before it
becomes urosepsis or that early fluid weight gain before it becomes full heart failure.” Landmark’s teams provide 24/7 in-person care in the home, often performing procedures that would normally require a trip to the emergency department or hospitalization. Le pointed out that providing home-based care for a seriously ill elderly patient can prevent the complications associated with being admitted to the hospital. The complexivist team also works to educate patients and caregivers to improve their health literacy and their crisis management skills, noted Le.
Le explained that Landmark’s program is supported by four clinical pillars; the team-based complexivist team represents the first pillar. The second pillar is behavioral health, as an analysis of Landmark’s patient population showed that more than 50 percent have some behavioral health comorbidity that was often underdiagnosed and almost always undertreated. Given that community behavioral health resources are scarce, Landmark Health established a behavioral health team of psychiatrists, addiction specialists, nurse practitioners, and physician assistants with psychiatric specialty training. The behavioral health team, like the complexivist care team, is available all day, every day, and it works with Landmark Health’s social workers and other community resources to address various social determinants of health. Le noted that the program’s chief behavioral health officer put together a behavioral health assessment tool that is used to identify patients who would benefit from such health services.
The third pillar is represented by Landmark’s strong focus on palliative care, starting with the initial 90-minute visit. Le said that as someone trained as a hospitalist, he believes strongly that the worst place to have a discussion about palliative care is at 1 AM in the emergency department or intensive care unit. “There is really no better place than sitting in their living room surrounded by their family with an hour and a half to talk about all the issues that need to be addressed, answer all their questions, and get everyone onto the same page,” he said. Staff receives training on how to have these challenging conversations and fill out medical orders for sustaining life treatment forms and physician orders for life-sustaining treatment (POLST) forms. He said that Landmark Health’s EHR triggers an alert on a patient’s third visit requiring that the team document an advance care planning discussion in the EHR. The system also requires the plan to be updated annually. Steps such as these significantly increased the length of stay in hospice, and nearly doubled the percentage of patients dying in hospice, said Le. He added that patients who do not sign up for hospice still receive hospice-like care in their homes from the care team.
The fourth clinical pillar of the program is that it serves its clients in collaboration with, rather than as a replacement for, the patient’s primary care provider (PCP). “We communicate with the PCPs and we make sure that they’re getting all of the information, picking up the phone and calling them, but it is something where I think the PCPs can see value because sometimes these patients are the ones that are not getting into the office, or when they do, they need to call 911” because it is a crisis situation, said Le. His experience has been that most, though not all, of the primary care physicians are satisfied with this arrangement, and most do see the value of having a dedicated team to provide care for those patients who may not be able to get to their offices when they are in crisis. He noted, too, that Landmark schedules monthly to quarterly meetings with the health plans to make sure communication issues are resolved quickly.
Every member of the health care team, said Le, receives training in each of these four areas in a 3-week course, called the Landmark Academy, before they see their first client. New team members take part in “ride-alongs” with experienced care teams and receive additional advanced evidence-based training. Landmark Health also has local subject matter experts trained in end-of-life care and other situations that may arise in the most challenging patients. In general, the complexivist team sees every patient and the behavioral health care team attends to those who have more serious problems.
Le noted that Landmark Health is fortunate that health plans are open to innovation and to working with groups such as his that are willing to take on risk. Over the 4 years Landmark Health has been operating, Le explained, it has acquired some 45,000 members across multiple business lines, including Medicare Advantage, Medicaid, dual-eligible plans, and commercial and health insurance exchange plans. During that time, the program has made more than 94,000 house calls and more than 22,000 unscheduled urgent care visits, noted Le.
Le explained that when Landmark Health contracts with a health plan, it sets quality goals that are 5 percent above current plan performance. Le noted that Landmark Health’s performance often exceeds 5-star levels, despite care for highest risk patient populations (see Table 3). The program produced a significant reduction in inpatient admissions, which accounted for approximately 70 percent of the overall reductions in Medicare Part C utilization in the program’s first 18 months of operation, said Le. Use of skilled nurse facilities and outpatient specialists also fell, while use of hospice and palliative services increased. The medical loss ratio for Part C fell 25 percent below baseline in year one of the program, and 37 percent below
TABLE 3 Landmark Health’s Impact on Quality Metrics
| Measure | Actual (pre-LMH) | Target Performance | Actual (post-LMH) |
|---|---|---|---|
| Controlling high blood pressure; cardiovascular | 71.0% 4 stars |
76.0% 5 stars |
90.8% 5 stars |
| Nephropathy screening: diabetes | 88.0% 1 star |
93.0% 2 stars |
98.1% 5 stars |
| HbA1C controlled < 9 | 66.0% 3 stars |
71.0% 3 stars |
87.1% 5 stars |
| Retinal exam: diabetes | 70.0% 3 stars |
75.0% 4 stars |
81.6% 5 stars |
| Adult BMI assessment | 85.0% 3 stars |
90.0% 4 stars |
99.3% 5 stars |
| PHQ-9 annual screening | 85.0% | 90.0% | 92.4% |
| Member satisfaction | 75.0% | 80.0% | 96.6% |
NOTE: BMI = body mass index, LMH = Landmark Health, PHQ-9 = Patient Health Questionnaire-9.
SOURCE: As presented by Michael Le, April 27, 2017.
baseline in year two. “Patients that were starting at 110 percent medical loss ratio are now down in the 80s,” said Le, which means these high-risk, high-need patients become profitable for health plans that contract with Landmark Health. Le added that the annual mortality of engaged members improved by nearly 17 percent compared to cohort members who never engaged with Landmark Health, even though engaged members were sicker on average.
Le pointed out that patient satisfaction surveys have shown that patients are engaged and satisfied; 97 percent of the members surveyed said the program has helped them stay out of the ED or hospital, and 96 percent rate the plan as “excellent” or “good.” The one area in which the program struggles, Le explained, is retaining staff and preventing staff burnout. “I think it is not an easy job, and I think finding the right person is key for this sort of model,” said Le. Because the care teams are out in the community, they can experience a lack of connection, so he hosts in-person meetings once a week to help remind staff they are part of a team.
In closing, Le emphasized the great need for home-based care for people facing serious illness. He shared that for Landmark, “it is always going to be a work in progress.”
Responding to a question during the discussion session following the speaker presentations from Judith R. Peres, board member of the Social Work Hospice and Palliative Care Network, about the role of advance care planning, De Jonge responded that planning begins before they see the patient. He explained that when someone joins the program, staff has an initial intake discussion with the patient’s family or caregiver to find out from their perspective what the major issues are and why they want to be in the program. During the first home visit, the physician conducts an extensive medical, functional, and social assessment that goes into the mobile EHR and, together with the intake discussion, serves as a framework for the care plan. The program’s nurse practitioner and social workers follow up over multiple visits, building a living document within the EHR that is adjusted depending on the stage of illness and that includes advance care planning, goals of care, and power of attorney designations. Loughnane agreed that individualized care plans should not be static documents; rather, they should be revisited frequently. Fratkin explained that ResolutionCare’s teams work with patients to determine a care plan and discuss advance care planning over the course of several early visits. Within the first 4 weeks of joining the program, a new patient will meet with a physician, nurse practitioner, social worker, and someone who addresses the patient’s spiritual health. Conversations during these visits help develop the plans at a pace that is comfortable for the patient, said Fratkin.
Speakers were asked by a workshop participant about the ability of their programs to deal with problems related to unequal access to care. De Jonge said he believes the home care “mobile” approach “cuts the Gordian knot of access for this high-risk population” as his program’s care teams are going out to see patients across Washington, DC, and surrounding areas. Loughnane responded that CCA’s One Care program was expressly designed to address access issues and partner with community health workers to locate people in need who face difficulties in accessing care. Fratkin also noted that ResolutionCare providers reach patients in very rural and remote areas through home-based care and telemedicine.
PROVIDING HIGH-QUALITY COMPREHENSIVE CARE
The workshop’s fourth session featured care delivery models that provide comprehensive services. These models included the Program of All-Inclusive Services for the Elderly (PACE), as well as innovative approaches taken by CareMore and Tandem365.
PACE Model of Care
David Wensel, medical director of Midland Care, a nonprofit, community-based health organization located in Topeka, Kansas, shared his experience operating a PACE model, which provides every aspect of care for a frail elderly adult, including primary, palliative, and hospice, throughout the patient’s life. Since its formal inception in 1990, the community-based, capitated, and coordinated PACE model has been proven to benefit patients and reduce hospitalizations (Eng et al., 1997; Meret-Hanke, 2011), in large part because it uses a continuous process of assessment, treatment planning, service provision, and monitoring that focuses on primary, secondary, and tertiary prevention. Medicare, noted Wensel, requires PACE programs to conduct a complete reassessment of each patient’s care plan at least every 6 months.
According to Wensel, the average PACE program participant in 2016 in his program was 72, had 15 diagnoses submitted to Medicare, took more than 10 medications daily, had at least 2 deficits in activities of daily living, and lived 32 months from the time of enrollment. With regard to medication, Wensel said it is not uncommon for participants joining the program to be taking too many medications; in one instance, an 82-year-old woman who joined his program was taking 52 pills per day. He noted that his program, like all PACE programs, is the Medicare Part D provider for its participants, so the pharmacist on the interdisciplinary team plays a critical role in the care of PACE participants, monitoring every patient’s medications closely.
Like many models of care described at the workshop, an interdisciplinary team provides care. However, in PACE, the interdisciplinary team, rather than an individual case manager, manages and coordinates care. Wensel explained the difference in this way: He might send a patient to see the cardiologist, who may recommend a particular procedure. Before subjecting that patient to the procedure, the care team members will review that recommendation together during one of its twice-weekly care planning meetings and decide if it is appropriate for that particular patient. Wensel explained that the team meetings include not only the clinical members and chaplains, but also home health aides, transportation aides, community caseworkers, caregivers, and family members involved in the care of the specific patients who are the subjects of that day’s meeting. As he put it, the type of coordination goes beyond what is typical of even a hospice setting.
An important component of the PACE program is its capitated and
pooled financing model. Medicare capitation rates, said Wensel, are adjusted for the frailty of the PACE enrollees. In addition, Medicare, Medicaid, and private-pay payments are pooled for each program’s enrollees. Each PACE program assumes all risk for each enrollee as part of the capitated payments it receives, Wensel explained, which makes many providers reluctant to participate in the program given that they are wary of the financial risk associated with capitated payments. One barrier to starting a PACE program, he said, is that start-up costs run into the millions of dollars because of the requirement that they operate out of a defined center.
Addressing some of the other challenges to spreading and scaling the PACE model, Wensel explained that PACE enrollees are limited to those who are at least 55 and that the local area agency on aging has certified to be at a nursing home level of function. While regulations require there to be a designated PACE center, programs such as Wensel’s are now partnering with physicians and other service providers in rural areas, for example, to bring services directly to underserved communities. He added that only 25 to 30 percent of his program’s participants come into the PACE center regularly.
Another challenge is that there has been inconsistent support for PACE from state and federal programs, Wensel noted. He also pointed to the increasing number of PACE enrollees who do not have caregivers, are on the edge of homelessness and starvation, and go to the ED to be admitted so they can get a meal. Securing adequate resources to address these complex problems is a daunting challenge, Wensel added.
Echoing the message of a number of workshop speakers, Wensel explained that workforce issues are a major challenge, particularly in his organization’s home state of Kansas, where there is an extreme shortage of nurses and primary care providers. Wensel’s organization is collaborating with medical and nursing schools to bring students into its PACE program and its separate hospice, palliative care, and home health programs. This “grow your own” approach aims to introduce students to these interdisciplinary, collaborative forms of care early in their education. In his opinion, the workforce shortage situation is only going to get worse in the future.
PACE, according to Wensel, is the most regulated form of medical care in the United States. Every 2 years, CMS and state regulators conduct onsite reviews of every PACE center’s quality measures and patient medical charts. PACE organizations are required to report all Level I and Level II incidents (see Table 4), and in 2017, the National Quality Forum endorsed an additional set of PACE-specific quality measures that Econometrica had developed under a contract with CMS. These quality measures covered
TABLE 4 Types of Level I and Level II Incidents
| Level I Incidents | Level II Incidents |
|---|---|
|
|
SOURCE: As presented by David Wensel, April 27, 2017.
pressure ulcer and injury prevalence rates, fall rates, and falls with injury rates. Additional measures under development will assess the percentage of patients with depression who are receiving therapy, the percentage of participants not in nursing homes, and the percentage of participants with advance directives and whose advance directives are reviewed annually. Wensel noted that PACE organizations report on their quality measures through the CMS Health Plan Monitoring System, and as a result, data are available to compare the performance of PACE programs with one another as well as against the performance of nursing homes and other health care systems.
Palliative care is an integral part of the PACE model, Wensel pointed out, and every team member is cross-trained in palliative medicine and end-of-life care. The care team aggressively treats any symptoms that affect quality of life, in keeping with palliative care principles. The program requires every new enrollee and his or her caregiver to complete advance directives and to settle on the goals of care. These documents, as well as a completed POLST form, are reviewed every 6 months, and as part of a client’s annual assessment, or sooner if there is a change in the patient’s condition. A 2002 study found that for PACE participants, the probability of dying at home is twice as great as for the general population of older Americans
(Temkin-Greener and Mukamel, 2002). This study also revealed that 21 percent of PACE participants die in the hospital compared to 53 percent of Medicare beneficiaries. “Dying at home is not the objective, but it is where the patient wants to be,” said Wensel.
Wensel pointed out that the PACE Innovation Act, signed into law in 2015, authorized PACE pilot programs to serve an expanded range of populations, including those under age 55, and increase the number of patients these serve, which will improve their financial viability. Wensel also noted that there is heightened interest on the part of payers in developing capitated, provider-based solutions such as PACE for high-need patients.
CareMore’s Model of Comprehensive Care
The CareMore medical group came into existence 25 years ago with the goal of developing a different model of care for the sickest patients, said Sachin Jain, CareMore’s chief executive officer. Jain described CareMore’s founder Shelly Zinberg as a visionary health care thinker who, as a physician, had the observation that all patients are not equal—the sickest patients actually need more attention. Jain explained that Zinberg grew increasingly frustrated by what he saw as a disjointed care experience created by the fact that different people provide primary care, specialty care, and post discharge care, and that many mistakes were made at every point along the uncoordinated continuum of care.
Zinberg created the CareMore medical group as a different way to practice medicine. This required a new approach, explained Jain. First, Zinberg recognized the fundamental importance of preventing people with chronic disease from progressing, and that doing so requires a team of health professionals who can help patients manage their own health and disease. To enable this type of health and disease management approach, CareMore created medical home cooperatives, or care centers, which include dieticians, nurse practitioners trained to manage chronic disease, podiatrists, other health care professionals, and even a fitness center. “All of the sudden, there was this very vibrant neighborhood-based care center that had nothing to do with a person’s primary care specialists’ offices where we do chronic disease management,” said Jain.
In addition to developing care centers, Zinberg created a new role, that of a specialist who was an internist. The internist would see patients in the hospital and follow them to the skilled nursing facility (SNF), and see them in post discharge follow-up care. Having this one physician, which
CareMore termed an “extensivist,” in the hospital who knew the CareMore patient coming into the emergency department helped avoid the unnecessary hospitalizations and accompanying expenses that often occur when the ED attending physician sees a patient with serious illness for the first time. Similarly, because the same physician would then follow the patient, those who were hospitalized were moved along more quickly through the continuum of care, again reducing costs while meeting the ultimate goal of having the patient back in their home.
This approach has had a significant impact on hospital admissions and stays. According to Jain, CareMore members in 2016 had 37 percent fewer hospital bed days, 60 percent fewer inpatient days associated with end-stage renal disease, and 33 percent fewer congestive heart failure readmissions compared to the Medicare average.
An important lesson from the CareMore experience, explained Jain, concerned the importance of an organizational culture of caring that started with CareMore’s founder and permeated into every person who works there, starting with the member services representative who enrolls new clients. This culture enabled staff to practice at their highest level and care for their patients to the best of their abilities. “You cannot do this work unless you care,” said Jain. “You have to do it because it is what you want to do. You have to be super passionate about it.” An additional piece of the CareMore philosophy, said Jain, is a commitment to continuous improvement that extends throughout the organization. “We take a philosophical stance that every admission to the hospital is somehow a failure of what we are doing,” he said. “We take the view that medication adherence is our problem, not the patient’s problem.”
A guiding clinical philosophy at CareMore, explained Jain, is to never waste any clinical touches. As an example, he said that one of the services CareMore offers at its care centers is free monthly toenail clipping for every member. “This is not about toenail clipping. It is about creating more touches in the system,” said Jain. Getting members into the care centers for their monthly toenail clipping enables staff to better manage their chronic diseases and build stronger relationships with their patients.
This high-touch approach has translated into better health outcomes, said Jain, as well as lower disenrollment rates. “It has translated into a clinical culture that is about bonding with patients and doing what you can for them, whether it is giving them rides to come to and from their appointments, getting them an air conditioner if they are dehydrated in the
summer months, or building them a ramp for their home if they need it,” he said.
Referring to the workforce issue that came up throughout the day, Jain said there are many mission-oriented health care professionals, and programs such as the ones discussed during the workshop need to go out and actively recruit those people. He joked that he spends so much time recruiting people that some people in his organization think he runs human resources, not the entire company. “The product is the clinical care, and the ingredients are the people,” he noted. Jain cautioned against just hiring warm bodies to meet the need for capable staff. “If I can just pass one lesson on from my work,” said Jain, “it is to focus on the people and the culture, and making sure you have the right people seeing your patients, because when you start to scale, you are never going to be able to be in every single room, and you need to have people who you trust to make the right decisions by your patients every single day.”
CareMore’s ability to grow from one location in southern California to a health system that has more than 100,000 members in 8 states is due to its success in building, sustaining, and scaling its culture across multiple geographies, Jain said. CareMore became part of Anthem in 2012. It recently became a Medicaid provider for some 25,000 patients in Memphis and Des Moines, and has begun working with blind and disabled populations. In closing, Jain challenged workshop participants to think about how to make systems such as his and the others discussed at this workshop the norm rather than the exception.
Tandem365’s Model for Comprehensive Care Delivery
Teresa Toland, chief executive officer of Tandem365, began her presentation by clarifying that her organization is neither part of a health system nor part of an ACO. She explained that Tandem365 was formed in 2013, when five providers in Michigan—four faith-based continuing care retirement communities and an ambulance service—came together to form Tandem365, an independent collaborative venture assisting hospitals, doctors, family members, and individuals in need of health care services not traditionally provided as part of health system benefits. The four retirement community partners, explained Toland, were formerly competitors who operate independent living and assisted living facilities, nursing homes, and skilled nursing rehabilitation facilities, and offer certified home health and private-duty attendants. Though competitors, the eventual partners all had
strong reputations in the community for providing excellent care, an important factor when it came to convincing insurance companies to contract with them to provide services for their clients with complex medical needs.
Before describing Tandem365’s approach to care, Toland told the story of Larry, a 79-year-old developmentally delayed man who lived most of his life with his mother. After she died, he continued living in the same house, but as he aged he developed serious illness, fell often, and was a frequent user of the emergency department. The trustee his mother had appointed to watch over Larry did not have his best interests at heart, and the first thing Tandem365’s social work department did was appoint a pro bono attorney to get Larry a new trustee, one who is involved in his life and helps him access the services he needs. Toland also spoke about Laurie, a 60-year-old woman whose mental health issues made it difficult for her to manage her multiple health problems, let alone manage her household and pay her bills. Tandem365’s social workers helped her move to a house that she can better afford and manage. “They’re not going to be the outcomes, by the way, that are on the scorecard,” said Toland. However, “They are the outcomes that we know will make a difference.”
Tandem365 receives referrals from insurance companies for patients who are aged 55 and older and have complex medical needs. This population, said Toland, includes the most expensive 5 percent of patients. A key part of Tandem365’s comprehensive model of care is the holistic approach to health management based on the Neuman Systems Model (Neuman, 1980, 1996). In creating each patient’s care plan, Toland explained, “We make sure that we understand every dimension of their life. You have to get to the root of what these problems are, so that is what we do.” The goal of taking this approach, she said, is to improve patients’ lives in their homes while teaching them to manage their own health, become as independent as possible, and provide treatment for non-threatening situations in their homes to reduce the number of ED visits.
As with the other models discussed at the workshop, Tandem365 relies on a comprehensive, interdisciplinary team-based approach to care, which includes primary care physicians, nurses, social workers, chaplains, as well as integrated-care paramedics that provide 24/7 coverage. Toland explained that the 24/7 coverage is key to keeping patients out of the ED.
Tandem365 also includes advance care planning as part of its services on the premise that it cannot take care of its clients without knowing what they want in the future. This model has a strong focus on hospice and palliative care. Toland admitted that staff struggled initially with having those
difficult conversations with their patients until they realized those conversations were the only way patients could speak for themselves and convey what their goals are.
Community and provider partnership has been a key to the success of Tandem365. “We do not recreate or reinvent any wheels,” said Toland. “What we do is partner with other health care providers in our community.” She noted that Tandem365’s navigators, nurses, and social workers know their job is to connect the dots for their clients, which requires them to engage constantly with the community to arrange for supportive services. Tandem365 also recruits volunteers from the community, particularly from an individual’s church when appropriate, to provide additional support.
Tandem365 serves clients referred by health care plans and insurers, and it receives a per member, per month payment. She noted that Tandem365 is currently in an at-risk contract with Blue Care Network, which means they receive part of their payment now and the other part in a year, depending on the program’s outcomes. Carefully managing resources is critical to the organization’s sustainability, said Toland, as is its ability going forward to expand its client base beyond three counties in western Michigan.
Tandem365 is accountable for a number of utilization and quality measures, including emergency department visits, hospitalizations, days in SNFs, intensive care unit admissions, and care transitions. Toland noted that one client is asking her organization to improve its scores on the Healthcare Effectiveness Data and Information Set (HEDIS) and its performance regarding diagnostic procedures. While this is not in Tandem365’s core mission, she explained, “You have to create value to get past that first step, and if we do not create value with the physicians, we will not get anywhere and we all know that is how they are incentivized.”
Going forward, Toland’s goal is to enroll 2,000 or more clients by expanding its geographic reach to additional counties. She is seeking additional funding sources outside of payers to improve sustainability, and she hopes to conduct a pilot project with Blue Cross’s dual-eligible clients.
As a final note, Toland pointed out that Tandem365 has changed its model more than a dozen times since it started operations, but “the main thing is, we have not changed our goals,” said Toland. “The goal is still the same. We have to take care of these people, and the refreshing part is, look at all of us that are doing something about it today.” The challenge, she said, is to develop a strategic approach to scaling these programs so that they can be delivered to more people in need across the nation.
During the discussion session following the panel presentations, work-
shop participants asked about a common ongoing challenge for most programs: the workforce. Wensel reiterated that in an effort to address shortages of nurses and of primary care providers in general, his organization is partnering with medical schools and schools of nursing so that students and residents gain experience working with them in their hospice, palliative care, home health, and PACE programs.
Noting that her organization’s expansion plans will require additional staff, Toland pointed out that her goal will be to recruit the right people from the beginning. She noted that when her organization first started, it had trouble retaining nurses, many of whom were task oriented versus person focused. Today, Tandem365 has a robust selection and orientation process that includes embedding an instructor with new hires for 12 weeks. Retention rates, she said, are now stable. In addition, enabling staff to practice within the scope of their license helps everyone to be more invested in their patients’ care while increasing the number of touches a patient receives. Working out what that scope is, particularly for medical assistants and paramedics, was challenging and involved long discussions with state regulators and medical directors, she added.
Jain emphasized that although the workshop focused on the various innovative models of care delivery, “It’s about the people. The model is really only as good as the people who operate within the model.” Jain added that “the recruitment of passionate, mission-driven, highly capable, clinically competent, intrinsically motivated, excited clinicians is the secret sauce.”
Workshop participant Katrina Scott of the Association of Professional Chaplains asked the speakers about the role of outreach to faith communities in their holistic care models. Wensel noted that the chaplains and spiritual care are an integral part of the PACE model; “they are always at the table,” he said. Jain noted that CareMore’s care centers are neighborhood based so there is a strong connection between the care centers and the communities around them. Toland noted that four of Tandem’s retirement community partners are faith-based organizations. She said the question made her think about how her organizations could better capitalize on the use of chaplains. Scott responded that chaplains are “really well-kept secrets.”
Steve Clauser, program director at PCORI, asked Wensel about the potential for a “population-based strategy to think about PACE in the same way that we think about ACOs.” For Wensel, several key factors limit the expansion of PACE, including the upfront investment necessary to launch a PACE program. Joanne Lynn, director of Altarum Institute’s Center for Elder Care and Advanced Illness, added that there are many constraints on
the expansion of PACE. She also asked the speakers to consider ways to provide the full range of services that high-need patients require, such as housing, food, and transportation. Jain noted that the “marriage of payer and provider” is a theme that was raised throughout the day and might provide the answer to “unleashing the power of common sense to do the things you need to do to keep your patients out of the hospital and keep them well.” Jain noted that there is often limited knowledge about what is happening across health and non-health sectors and “that is a really important gap we can all help” to address.
POTENTIONAL POLICY STEPS TO SUPPORT HIGH-QUALITY CARE FOR PEOPLE WITH SERIOUS ILLNESS
Over the course of the workshop, a number of leaders of innovative programs that incorporate the principles of palliative care into the care of individuals with serious illness described the opportunities and challenges to spreading and scaling their programs. The workshop’s last session provided some insights into the potential that policy developments hold for spreading programs such as these more broadly across the nation.
Person-Centered Care for High-Need, High-Cost Medicare Patients
The final session of the day featured a presentation by William Hoagland, senior vice president of the Bipartisan Policy Center (BPC), a nonprofit organization that provides politically balanced policy making, advocacy, and research. Hoagland focused his remarks on BPC’s policy recommendations aimed at improving care for high-cost, high-need Medicare patients. Opening on an optimistic note, Hoagland said he believes that the nation’s policy makers have reached a consensus that improving the quality and availability of medical and social services for patients and their families will not only enhance quality of life through the end of life, but also contribute to a more sustainable health care system. “I believe policy makers get it,” said Hoagland. He also noted that the most important thing he had learned from the workshop’s presentations was that too many elderly spend the last years of their lives going in and out of hospitals, receiving high-tech, high-cost interventions while suffering from a lack of low-tech, high-touch services.
From a budgetary perspective, said Hoagland, policy makers tend to look at aggregate expenditures. In the aggregate, the rate of growth in
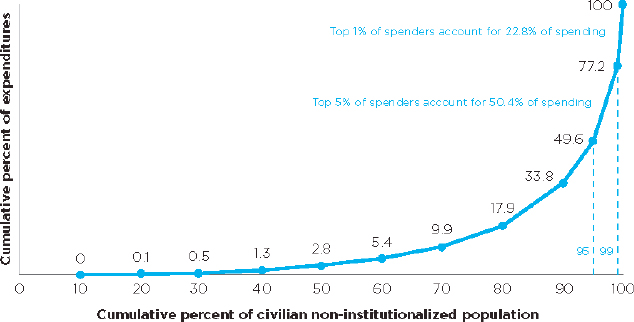
SOURCES: Hoagland presentation, April 27, 2017; Dzau et al., 2017.
Medicare and Medicaid spending is outstripping the rate of growth in the economy (CBO, 2017) leading policymakers to conclude such expenditures are not sustainable over the long term. Hoagland noted the importance of initiatives such as the National Academy of Medicine’s Vital Directions for Health and Health Care (Dzau et al., 2017), which included BPC long-term–care working group committee members Senators Frist and Daschle,17 in calling policy makers’ attention to the fact that high-need patients account for a disproportionate share of health care costs. Specifically, Hoagland pointed out that of total personal health care expenditures in 2014, the top 1 percent of health care spenders accounted for 22.8 percent of all health care spending, and the top 5 percent accounted for 50.4 percent, according to the Agency for Healthcare Research and Quality’s Medical Expenditure Panel Survey18 (see Figure 5).
A more fine-grained analysis of health care expenditures shows that the costliest 10 percent of Medicare fee-for-service beneficiaries account for 59 percent of Medicare fee-for-service spending, while the least costly 50 percent of beneficiaries account for only 4 percent of Medicare fee-
___________________
17 Senator William Frist (R-TN) served in the U.S. Senate from 1995–2007; Senator Thomas Daschle (D-SD) served in the U.S. Senate from 1987–2005 and in the U.S. House of Representatives from 1979–1987.
18 See https://meps.ahrq.gov/mepsweb (accessed July 5, 2017).
for-service expenses. This analysis also reveals that 36 percent of Medicare fee-for-service beneficiaries have four or more chronic conditions and they account for 76 percent of all Medicare fee-for-service spending (MedPAC, 2016). Hoagland noted that the average per capita spending for a Medicare beneficiary was $14,000 in 2016, but average costs rose to $30,000 annually if that beneficiary had three or more chronic conditions and functional or cognitive impairment (Fise et al., 2017) “I think it should be clear that if policy makers are concerned about cost, which they tend to be, they must focus their attention on those who contribute the most to those costs,” said Hoagland.
With that as background, Hoagland explained that BPC is focused on two distinct high-need, high-cost populations: Medicare/Medicaid dual-eligible individuals and the Medicare-only beneficiaries with three or more chronic conditions and functional/cognitive impairment. BPC, Hoagland explained, has issued four reports focusing on these two populations over the last year (Bipartisan Policy Center, 2016a,b, 2017a,b). “We concluded that while both populations had common features in terms of health status, behavioral health needs, and assistance required for activities of daily living, the policy challenges were definitely different,” said Hoagland. For the dual-eligible population, the main policy concern was how to better integrate Medicare and Medicaid benefits. For the Medicare-only population, the main policy issue was the lack of flexibility and financial incentives to provide non-Medicare–covered social services.
In their most recent report on the subject (Bipartisan Policy Center, 2017b), Hoagland and his colleagues noted that of the estimated 10.3 million dual-eligible beneficiaries in 2015, only slightly more than 2 million individuals, or 2.1 percent of this population, were enrolled in systems of organized care such as Dual-Eligible Special Needs Plans (D-SNPs), Medicare–Medicaid plans, or PACE programs. From a policy perspective, he noted, the substantial number of dual-eligible individuals still receiving benefits under traditional fee-for-service arrangements and such a limited number of individuals enrolled in coordinated care settings raise cost and quality concerns. Consequently, BPC put forward the following recommendations regarding the dual-eligible population:
- Permanently reauthorize the D-SNP program before its 2018 expiration, and in addition, D-SNPs should be fully integrated into a single managed care organization with clinical health care, behavioral services, and long-term supports and services;
- Modify the contracts for ongoing financial alignment demonstration projects to permit unanticipated infrastructure investment associated with starting up these special needs programs. These demonstration programs should be allowed to be deficit-neutral over a 5-year period, rather than the current requirement to be deficit-neutral every year. In addition, new states should be allowed to enter into demonstrations when they are ready, states should receive greater shared savings to incentivize them to integrate care, and these demonstrations should allow Medicare and Medicaid dollars to be combined for full financial integration;
- Combine the regulatory authority for reimbursement for Medicare and Medicaid into a single Medicare–Medicaid Coordination Office; and
- Establish a new regulatory structure to serve this particular population based on the proven results of the demonstration projects. This regulatory structure would use a model three-way contract and require plans to be seamless to beneficiaries, with a single enrollment process, claims forms, benefit cards, case managers, and plan point of contacts. The new regulatory structure should align Medicare and Medicaid grievance and appeals processes and overlapping benefits, and it would afford benefit flexibility based on a reasonable and necessary standard for patients with multiple chronic conditions and functional limitation or cognitive impairment.
The overall conclusion for the dual-eligible population is straightforward, said Hoagland. “If we are to be successful in integrating palliative care into services for the seriously ill and vice versa, we need to increase the availability of coordinated care in the system or it will never work,” he said.
With regard to the high-need, high-cost Medicare-only population, Hoagland and his colleagues first identified a number of regulatory and payment policy barriers to providing integrated care for this population, whether through Medicare Advantage plans, accountable care organizations, or patient-centered medical homes (Bipartisan Policy Center, 2017a). To address the barriers, BPC issued the following recommendations for policy changes relevant to the high-need, high-cost Medicare-only population (Bipartisan Policy Center, 2017b):
- Reform Medicare Advantage “uniform benefit” requirement to allow targeting of supplemental benefits on a per person basis rather than a uniform “one size fits all”;
- Allow Medicare Advantage plans to offer supplemental benefits that are not “primarily health-related,” as long as they are part of a person-centered plan for chronically ill beneficiaries;
- Allow Medicare Advantage plans to count costs of non-covered (non-supplemental benefit) supports toward the medical loss ratio, when supports are provided to a beneficiary at no charge;
- Reform Medicare’s risk adjustment model to account for a beneficiary’s frailty. The current risk model has been estimated to underpredict the medical costs of frail individuals by nearly 30 percent while overpredicting the costs of the lowest cost beneficiaries by nearly 60 percent;
- Develop new quality measures that will financially incentivize Medicare Advantage and accountable care organizations to provide non-Medicare–covered social supports; and
- Clarify program integrity rules to allow for accountable care organizations and medical homes to provide non-Medicare–covered supports to high-risk beneficiaries free of charge.
Each of these recommendations, said Hoagland, is designed to provide flexibility. This flexibility would allow Medicare Advantage plans and Medicare providers to furnish or finance non-Medicare–covered supports that are part of person-centered care plans for Medicare-only beneficiaries with three or more chronic conditions and functional or cognitive impairment.
As an illustrative example, the BPC team analyzed the cost implications of providing four potential supplemental benefits: in-home meal deliveries, non-emergent medical transportation, minor home modifications, and targeted case management. Hoagland said the average monthly cost of providing these benefits ranged from $50 per patient for transportation to $360 per recipient for daily home delivery of fresh meals, with the caveat that these amounts will vary by location. The analysis also found that if this cost for all beneficiaries with three or more chronic conditions and functional or cognitive impairment was spread across all enrollees in Medicare Advantage plans, the per person per month cost would be about $5 (Fise et al., 2017). Because the average per member per month rebate for Medicare Advantage plans in 2017 is nearly $90, Hoagland and his colleagues con-
cluded that providing these additional benefits could be financed within the existing Medicare Advantage payment structure without adding to the cost. In fairness, he added, BPC did not have data that would have allowed them to determine the potential savings to Medicare from reducing avoidable high-cost medical events by providing these “soft touch” benefits. “The point is that it can be done within the existing structure,” said Hoagland.
Hoagland noted that bipartisan legislation introduced in April 2017—the Creating High-Quality Results and Outcomes Necessary to Improve Chronic (CHRONIC) Care Act—included at least five of the recommendations BPC issued in its reports (see Table 5). Hoagland finds the most rewarding parts of this bill are the provisions that would allow Medicare Advantage plans to target supplemental benefits and to waive the restriction that Medicare Advantage benefits are primarily for health-related services. He noted that the 21st Century Cures Act, which received bipartisan support and was signed into law at the close of the Obama Administration, addresses issues with the current risk adjustment factor and allows Medicare-eligible individuals with end-stage renal disease to access Medicare Advantage programs.
As a final thought, Hoagland said, “despite the fireworks over the future of the Affordable Care [Act] in Congress, progress is being made, if so slightly, toward focusing on improving the quality and availability of medical and social services for patients and their families to enhance the quality of life for patients with serious illness.” In his opinion, those advances will not only benefit those individuals and their families through the end of their lives, but also “benefit the public purse.”
Additional Opportunities for Policy Changes
Throughout the day’s presentations, a number of workshop speakers offered policy recommendations of their own. In their presentations, both De Jonge and Le voiced support for Senate Bill 464,19 the Independence at Home Act, which was introduced at the end of February 2017 and was referred to the Senate Finance Committee. This bill would establish a permanent Independence at Home medical practice program in Medicare under which a primary care practice would be accountable for providing comprehensive, coordinated, continuous, and accessible care to applicable
___________________
19 See https://www.congress.gov/bill/115th-congress/senate-bill/464 (accessed July 3, 2017).
TABLE 5 Common Features Between BPC Recommendations and the Chronic Care Act of 2017
| CHRONIC Care Act | BPC April 2017 Recommendations | BPC September 2016 Recommendations | |
|---|---|---|---|
| Allowing MA plans to target supplemental benefits to chronically ill enrollees | |||
| Waiving the restriction that limits MA supplemental benefits to “primarily health-related” services | |||
| Clarifying that certain ACOs and medical homes can provide non-Medicare-covered social support services for free | |||
| Improving the accuracy of the Risk Adjustment Model for MA plans and ACOs | |||
| Establishing new quality measures to assess the integration of medical services with non-medical social supports | |||
| Making the CMS Medicare–Medicaid coordination office the focal point for dual-eligible issues | |||
| Permanently authorizing D-SNPs in conjunction with new requirements for D-SNPs to integrate certain Medicare/Medicaid benefits | |||
| Integrating Medicare/Medicaid grievance and appeals processes within D-SNPs | |||
| Revising and improving the structure of the financial alignment initiative for dual-eligible beneficiaries | |||
| Developing a new three-way contract model for integrated care for dual-eligible individuals |
NOTE: ACO = accountable care organization; CMS = Centers for Medicare & Medicaid Services; D-SNP = Dual-Eligible Special Needs Plan; MA = Medicare Advantage.
SOURCE: As presented by William Hoagland, April 27, 2017.
Medicare beneficiaries at home, and for coordinating health care across all treatment settings. The bill would also extend the existing IAH Demonstration program pending permanent implementation of the program and remove the limit on the number of beneficiaries allowed to participate in the current Demonstration program.
Le also offered three additional policy recommendations:
- Create a new Advanced Physician Group Model that would shift risk to physician groups, allow financially able provider groups to accept full risk, and allow consumers to opt in;
- Create full-risk, poly-chronic accountable care organizations that would allow attribution based on condition and need and would focus on fostering the most effective care models for fee-for-service patients with multiple chronic conditions; and
- Expand the PACE program and allow a PACE without Walls program as a means of reaching new and additional beneficiaries.
Hoagland, like Wensel, supports efforts to expand the PACE program, particularly to serve people under the age of 55. Wensel had several other policy recommendations relevant to the PACE program. The first was to enhance PACE affordability and access for Medicare-only beneficiaries at a private-pay premium rate reflecting their specific level of need, and offer a choice of affordable Part D plans for their prescription drug needs. He also called for CMS to release its Final Rule governing the PACE program and to issue PACE pilot program requests for proposals, both of which were authorized under the PACE Innovation Act that President Obama signed into law in November 2015. He also recommended that any reforms to Medicare and Medicaid undertaken by Congress should account for the needs of vulnerable populations, such as those served by PACE, and in particular should support integrated financing and care for dual-eligible individuals.
Fratkin offered two policy recommendations that he believes would increase the application of palliative care principles nationwide. The first is to create a federal version of California Senate Bill 1004,20 which would require CMS to establish standards and provide technical assistance for Medicare managed care plans to ensure the delivery of palliative care services. If enacted at the federal level, such a policy change would create a
___________________
20 See http://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201320140SB1004 (accessed July 3, 2017).
Medicare-mandated, value-based payment benefit for community-based palliative care at home. He also called for national licensure and reciprocity across state laws to support the widespread deployment of telemedicine technologies.
Jain called for new thinking about health and how health care legislation is developed. In Jain’s view, “It needs to explicitly write to the responsibilities of other agencies and explicitly prompt that cross-sector innovation, and explicitly prompt the structural reforms that are needed within agencies.” Jain pointed out that while we can continue to reform policy, much can be done within the existing policy structures, as was demonstrated by the workshop speakers. Building on these examples, Jain offered a final comment: “I would say that we should look at these organizations and try to figure out how we can enable them to do more of what they are doing.”
Bernard Lo, president and chief executive officer of the Greenwall Foundation, asked the speakers what workshop participants themselves could do to promote the type of policy proposals described over the course of the day. Hoagland said he believes the practitioners in the field have the most power to influence senators and representatives. “Bring them to your operations and show them what you are doing,” he said. He cautioned, however, that any discussions with elected officials should avoid focusing on return on investment because saving money is associated with limiting care in the minds of some members of Congress. Hoagland said there is a need to change the way elected officials think about this issue. “What this is, is dignity at the end of life that they have to better understand,” said Hoagland.
Jain had a number of suggestions for moving policies forward. The first suggestion called on foundations and other funders to organize a “dignitypalooza,” a large-scale national gathering at which these issues are raised and discussed and that would create a social movement to support better care for people with serious illness. His second suggestion was for health care system leaders to recognize that there are existing policy instruments, such as Medicare Advantage, which they could use to enact some of the innovative approaches discussed at the workshop. He pointed out that health care systems that operate their own Medicare Advantage plans receive 100 percent of the premium dollars from CMS, which provides a great deal of freedom and flexibility. Jain concluded that many organizations are not taking advantage of the opportunity for significant flexibility within Medicare Advantage.
Jain also encouraged workshop participants to reject incrementalism. “Start calling out when your organizations are trying to pilot things that we
know work,” said Jain. In his view, organizations retest things as a means of deferring real action and “kicking the can down the road on hard decisions.” Jain also encouraged honest discussions about the winners and losers from policy changes. “If we starting taking cost and waste out of the system, there will be some parts of the system that will shrink while others grow, and that is not a conversation we are comfortable having,” said Jain. By not acknowledging this fact, he believes the health care community is not defining the problem correctly, which makes it difficult to develop workable solutions. As a final point, Jain encouraged workshop participants to start having conversations with an agency or organization that feels oblique to the mission of their organizations to see if there is an opportunity to bridge a gap. For example, he has started conversations with the Red Cross and with the local Area Agency on Aging about ways to address the problem of alienation and loneliness among the elderly.
CONCLUDING THOUGHTS
In her remarks to conclude the workshop, Nevidjon thanked presenters for having “taken us from age 0 to the oldest of the old,” and described some innovative models across a range of care settings. Meier said she was “inspired by the success, impact, and spread of solutions” that organizations have developed “despite the perverse payment incentives and regulatory restraints that we work under. This is a very creative, entrepreneurial country, and we are out there solving problems,” said Meier.
Meier pointed out that policy can help scale and spread these programs and make health care more equitable, and she is optimistic that will happen. She called for the types of innovative programs featured in the workshop to represent the standard of care, not the exception. Meier predicted that the baby boom generation will create the social will to make that happen. “I think we are a strong political force and that we need to get mobilized, because it is our future and there are a lot of us,” said Meier, referring to the fact that 10,000 baby boomers turn 65 every day.
REFERENCES
Bipartisan Policy Center. 2016a. Delivery system reform: Improving care for individuals dually eligible for Medicare and Medicaid. Washington, DC: Bipartisan Policy Center.
Bipartisan Policy Center. 2016b. Initial recommendations to improve the financing of long-term care. Washington, DC: Bipartisan Policy Center.
Bipartisan Policy Center. 2017a. Challenges and opportunities in caring for high-need, high-cost Medicare patients. Washington, DC: Bipartisan Policy Center.
Bipartisan Policy Center. 2017b. Improving care for high-need, high-cost Medicare patients. Washington, DC: Bipartisan Policy Center.
CAPC (Center to Advance Palliative Care). 2015. About palliative care. https://www.capc.org/about/palliative-care (accessed September 12, 2017).
CBO (Congressional Budget Office). 2017. The budget and economic outlook: 2017 to 2027. Congressional Budget Office Website. https://www.cbo.gov/sites/default/files/115th-congress-2017-2018/reports/52370-outlookonecolumn.pdf (accessed July 17, 2017).
CMS (Centers for Medicare & Medicaid Services). 2016. CMS (Centers for Medicare & Medicaid Services) hospice PUF files, CY2014.https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Hospice.html (accessed July 17, 2017).
CMS. 2017. Independence at home demonstration corrected performance year 2 results. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017-01-19.html (accessed July 17, 2017).
Cohen, E., J. G. Berry, X. Camacho, G. Anderson, W. Wodchis, and A. Guttmann. 2012. Patterns and costs of health care use of children with medical complexity. Pediatrics 130(6):e1463–e1470.
Dzau, V. J., M. B. McClellan, J. M. McGinnis, S. P. Burke, M. J. Coye, A. Diaz, T. A. Daschle, W. H. Frist, M. Gaines, M. A. Hamburg, J. E. Henney, S. Kumanyika, M. O. Leavitt, R. M. Parker, L. G. Sandy, L. D. Schaeffer, G. D. Steele, Jr., P. Thompson, and E. Zerhouni. 2017. Vital directions for health and health care: Priorities from a National Academy of Medicine Initiative. Washington, DC: National Academy of Medicine. https://nam.edu/vital-directions-for-health-health-care-priorities-from-a-national-academy-of-medicine-initiative (accessed July 17, 2017).
Eng, C., J. Pedulla, G. P. Eleazer, R. McCann, and N. Fox. 1997. Program of all-inclusive care for the elderly (PACE): An innovative model of integrated geriatric care and financing. Journal of the American Geriatrics Society 45(2):223–232.
Feudtner, C., R. M. Hays, G. Haynes, J. R. Geyer, J. M. Neff, and T. D. Koepsell. 2001. Deaths attributed to pediatric complex chronic conditions: National trends and implications for supportive care services. Pediatrics 107(6):E99.
Fise, P., K. Hayes, G. W. Hoagland, M. McKearn, and M. Workman. 2017. Improving care for high-need, high-cost medicare patients.https://cdn.bipartisanpolicy.org/wp-content/uploads/2017/04/BPC-Health-Improving-Care-for-High-Need-High-Cost-Medicare-Patients.pdf (accessed July 17, 2017).
Gans, D., G. F. Kominski, D. H. Roby, A. L. Diamant, X. Chen, W. Lin, and N. Hohe. 2012. Better outcomes, lower costs: Palliative care program reduces stress, costs of care for children with life-threatening conditions. Policy Brief UCLA Center for Health Policy Research (Pb2012-3):1–8.
Gans, D., M. W. Hadler, X. Chen, S. H. Wu, R. Dimand, J. M. Abramson, B. Ferrell, A. L. Diamant, and G. F. Kominski. 2016. Cost analysis and policy implications of a pediatric palliative care program. Journal of Pain and Symptom Management 52(3):329–335.
IOM (Institute of Medicine). 2015. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: The National Academies Press.
Kuo, D. Z., E. Cohen, R. Agrawal, J. G. Berry, and P. H. Casey. 2011. A national profile of caregiver challenges among more medically complex children with special health care needs. Archives of Pediatrics and Adolescent Medicine 165(11):1020–1026.
Lassman, D., M. Hartman, B. Washington, K. Andrews, and A. Catlin. 2014. US health spending trends by age and gender: Selected years 2002–2010. Health Affairs 33(5):815–822.
Lustbader, D., M. Mudra, C. Romano, E. Lukoski, A. Chang, J. Mittelberger, T. Scherr, and D. Cooper. 2017. The impact of a home-based palliative care program in an accountable care organization. Journal of Palliative Medicine 20(1):23–28.
MedPAC (The Medicare Payment Advisory Commission). 2016. Health care spending and the Medicare program.http://www.medpac.gov/docs/default-source/data-book/june-2016-data-book-health-care-spending-and-the-medicare-program.pdf (accessed July 17, 2017).
MedPAC. 2017. Report to the Congress: Medicare payment policy.http://medpac.gov/docs/default-source/reports/mar17_entirereport.pdf (accessed July 17, 2017).
Meret-Hanke, L. A. 2011. Effects of the program of all-inclusive care for the elderly on hospital use. Gerontologist 51(6):774–785.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Families caring for an aging America. Washington, DC: The National Academies Press.
Neuman, B. 1980. The Betty Neuman health-care systems model: A total person approach to patient problems. Edited by J. P. Riehl and C. Roy. New York: Appleton-Century-Crofts.
Neuman, B. 1996. The Neuman systems model in research and practice. Nursing Science Quarterly 9(2):67–70.
NHPCO (National Hospice and Palliative Care Organization). 2014. NHPCO’s facts and figures: Hospice care in America 2014 edition.https://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf (accessed July 17, 2017).
Osterman, M. J., K. D. Kochanek, M. F. MacDorman, D. M. Strobino, and B. Guyer. 2015. Annual summary of vital statistics: 2012–2013. Pediatrics 135(6):1115–1125.
Temkin-Greener, H., and D. B. Mukamel. 2002. Predicting place of death in the program of all-inclusive care for the elderly (PACE): Participant versus program characteristics. Journal of the American Geriatrics Society 50(1):125–135.
Teno, J. M., P. L. Gozalo, J. P. Bynum, N. E. Leland, S. C. Miller, N. E. Morden, T. Scupp, D. C. Goodman, and V. Mor. 2013. Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 309(5):470–477.
This page intentionally left blank.












































































