3
Reaction Panel of Developers and Users
In the spirit of continuing the discussion that began the workshop, the second session featured four presentations that provided reactions to the commissioned paper. The four speakers were Cindy Brach, senior health care researcher at the AHRQ’s Center for Delivery, Organization, and Markets; Yolanda Robles, founder and president of CulturaLink; Marshall Chin, the Richard Parrillo Family Professor of Healthcare Ethics at The University of Chicago; and Michael Wright, vice president for diversity and health equity at Northwell Health. An open discussion followed the four short presentations.
QUESTIONS REGARDING AN INTEGRATED APPROACH TO MEASUREMENT1
Brach addressed five questions that had been posed to panelists. The first question asked was whether the idea of an integrated approach to measurement was useful. Brach responded, “Providing care that is health literate and culturally and linguistically competent is the hat trick of quality improvement for vulnerable populations. The idea of integrating measures is appealing, and as the [paper’s] authors discussed, it could reduce
___________________
1 This section is based on the presentation by Cindy Brach, senior health care researcher at the AHRQ Center for Delivery, Organization, and Markets, and the statements are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine and do not represent the views of the U.S. Department of Health and Human Services.
measurement burden” and would create a greater constituency for unified measurement sets.
Thinking about this question, however, prompted Brach to examine what integrating measures means. Brach observed that the proposed framework is more of an amalgamation across the three measurement domains rather than integration. She acknowledged that consolidation of measures would be beneficial, but noted that integration comes with some cost. “The level of detail you need to do quality improvement work will likely not appear when you start rolling up performance measures to cover the bigger terrain,” said Brach, “so as we hold organizations accountable for these measures, we may lose the spotlight on vulnerable populations, which is what we were striving to achieve in the first place.” She noted that the authors recognized this issue to some extent by recommending that there be a package of measures for vulnerable populations, but to her that seems counter to the idea of integration.
Brach suggested that rotating measurement sets could address the fact that integration usually produces long surveys with too many items. Rotating sets of measures could produce the same results while reducing the burden on individual survey respondents. She also commented on the need to make sure that the measures go beyond the typical “top-box” approaches that determine the percentage of people always receiving the best care. Such approaches, she said, tend to focus on helping those in the middle get better care as opposed to being concerned about those receiving the worst care. “Maybe we need to think about some bottom-box approaches,” said Brach. “We do not want organizations to deliver great care to 80 percent but totally fail the remaining 20 percent.”
Another way to think about integration, Brach reflected, was to look for the places where health literacy, cultural competence, and language access overlap. The example she gave was that misunderstanding is an issue for cross-cultural communication, language barriers, and health literacy concerns. “Looking for those sweet spots where you can get a three-for-one is another way to think about integrating measures,” said Brach. She suggested that another approach is to think about measuring whether integrated care is being delivered. “Rather than the parallel play approach of measuring health literacy and cultural and linguistic competence in coordination but separately, we would measure whether the care itself is being integrated,” she said, giving the example of a CHW who is bilingual, bicultural, and health literate.
The second question she addressed was whether the proposed framework can adequately address the issue of integration. She responded that the real question to ask is, “Will this approach get us closer to the goal of health equity and provide a foundation for organizations that serve vulnerable populations with the funds they need to deliver effective care?” Her
concern, echoing that expressed by Catina O’Leary in the opening session, is that patient-centeredness is more of a fourth topic with its own history rather than an overarching rubric for health literacy, cultural competence, and language access measures. “Unfortunately, [patient-centeredness] has not always been closely associated with providing health-literate and culturally and linguistically competent care,” said Brach.
She also expressed concern that while NCQA has been “fantastic” in terms of integrating those measures in its PCMH accreditation process, not all PCMH efforts do that. “It is very appealing, because if you are person centered then obviously you are taking care of language and culture. But there is a danger that if you just say ‘PCMH’ that you will lose the emphasis on these other important areas.” Her suggestion was to make sure that all PCMH efforts are addressing these measurement issues. “But I would say [that] about any patient safety or quality improvement initiative, that we [should] weave the concerns for vulnerable populations throughout.”
Addressing the third question, as to whether there were other things that should be included in the framework, Brach suggested a domain she believed to be missing: navigation. She explained that navigation, which is an issue for all three of the vulnerable populations the framework is addressing, deals with interacting with both the built and the electronic environment and negotiating the increasingly complex and fragmented health care system. She also suggested broadening the domain of patient engagement to include self-management. In her view, doing that would “bring home the idea that it is not just about engaging, it is also about empowering individuals and their families to be able to take care of themselves,” said Brach.
The fourth question asked was, “Even if the measures are integrated, do you think one of the domains could be used to drive the others forward?” Brach suggested that health literacy could be the concept that drives the framework forward. She noted that she comes from the cultural and linguistic competence area and so that suggestion does not come from the bias of being a health literacy scholar. “But I have found that health literacy has more universal appeal because it does not rely on altruism,” said Brach. “People see that we are all having struggles with understanding health information and negotiating these systems, and therefore [health literacy] has more legs.”
The fifth question asked what is needed to implement the framework. In Brach’s opinion, the commissioned paper did a good job of recognizing the barriers facing implementation of the framework. For example, with the possible exception of Spanish, there is a lack of culturally competent, easy-to-understand, and translated survey items. “If we are depending on patient experience surveys, we need them across the languages and cultures of the individuals we are concerned about,” said Brach. Another barrier is
that while oversampling vulnerable populations is a great idea, doing so can be extremely expensive.
Brach expressed some concern about the reliance on structural measures as opposed to performance and accountability measures. “Structural measures are fantastic for quality improvement, but none of the measures in the paper, which largely rely on staff and individuals in the organizations to give testimony about how their organizations are doing, are going to be good for accountability. Those measures can be gamed,” said Brach. She also noted that, to achieve success in improving care for vulnerable populations, the drivers for change in health care—such as payment, regulation, market forces, and accreditation standards—would need to be aligned. Despite her reservations, she encouraged everyone to take all opportunities to move this agenda forward. “If you get asked to train accreditation surveyors, say yes. If you get asked to be on an advisory panel around measurement, do it!” said Brach. She said she believes that it is important to take every opportunity to champion the collection of reliable race, ethnic, and language data; fund psychometric testing of surveys across cultures and languages; and any other action, because “it will take all of us make this happen.”
HELPING HEALTH CARE ORGANIZATIONS IMPROVE SERVICES TO DIVERSE POPULATIONS2
When Robles founded CulturaLink3 in 2006, her goal was to improve outcomes for diverse patient population services by working at the organizational level, and she approached that goal in three steps. First, she created an approach that assesses an organization’s strengths and weaknesses regarding how it worked with diverse populations. “When we think of assessments, we only think about gap analysis, but we do not think about what are some of the best practices that exist within a health care system that can be duplicated across the system,” said Robles. Second, she wanted to address all kinds of communication barriers, which led her to establish nationwide interpreter services to provide health care systems, community health organizations, and payers with a means of helping individuals to understand and be compliant with their care plans. The third step was to work with organizations to engage their workforces, educate their employees about the importance of delivering culturally competent,
___________________
2 This section is based on the presentation by Yolanda Robles, founder and president of CulturaLink, and the statements are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
3 See www.theculturalink.com (accessed June 14, 2017).
patient-centered care, and operationalize that in terms of making it easy for staff to access interpretation and culturally competent services for patients.
Reflecting on what separates those clients that have made progress from those that have not, Robles said that both successful and unsuccessful clients use performance measures, but those that are successful have the capacity to use the resulting data productively. “Many health care systems do not really understand what to do with those data,” said Robles. In her opinion, having an integrated framework that would allow a health care system to take action based on the framework as a whole, rather than on individual pieces, is a “great idea.” In fact, what she has seen in her work is that effective communication cannot be separated from cultural competence and health literacy. “All of those components tie together to provide the best experience for your patient,” said Robles.
Noting how often health literacy, cultural competence, and language services exist in silos, each managed separately, Robles said that treating these as distinct issues impedes an organization’s ability to promote culturally competent care and use its resources effectively. “When considering the provision of culturally competent care, care that is respectful and responsive, it is important to take all these pieces together,” she said. Having an integrated set of measures would, in her opinion, help organizations do just that and provide a roadmap for improvement. She believes, in fact, that the roadmap will be a key component of the framework because many organizations do not have the capacity to figure out how to deliver these services and then implement the changes needed to deliver them effectively. “Provision of domains and structural measures provides guidance that can help accomplish that change,” said Robles.
One strength of the framework, she noted, is the crosswalk that illustrates how the domains interact with one another and how they fit into the measures accreditation agencies are using. “Many times, hospitals live and die by these accreditation agencies making sure that they actually are working toward delivering the appropriate services or at least meeting those standards that are set by those organizations,” said Robles.
A suggestion she had with regard to implementing the framework was to call out a few key points in each domain so that health care systems will have a better understanding of why they are important. She also said she would like to see something in the framework on leadership and organizational culture, given how important those are to a successful change process, and on the competencies needed in terms of workforce skills.
Seconding Brach’s idea of adding navigation as a domain, Robles said that CulturaLink is working with a health care system to pilot a culturally and linguistically competent lay navigator program tied to community engagement. “Bringing that navigator back into the organization and educating the staff on what that navigator learned through the process I
think is extremely important,” said Robles. To illustrate the importance of culturally and linguistically competent navigation, she described one health system she worked with that only provided navigation to English-speaking patients. When she examined how English-speaking and non-English-speaking patients fared, there was a significant difference in outcomes, with the English-speaking patients doing significantly better.
Robles did suggest placing a stronger emphasis on data collection given her observation that data collection is a constant issue when she assesses a health care system. In her experience, staff are often uncomfortable asking questions about language preference and culture, so they do not feel data collection is that important. She also suggested that organizational readiness and capacity to deliver these services are factors that need to be measured.
One way the framework can get organizations to change is by providing payers with the means to create incentives based on how organizations do on these measures. One of her clients, for example, bases payments in part on whether providers are delivering culturally and linguistically competent care. The framework could be used to create a dashboard-type application to enable health care organizations to report on their performance and progress.
EQUITY PERFORMANCE MEASURES WITHIN PAYMENT AND DELIVERY SYSTEM REFORM4
The focus of Chin’s comments was on placing the framework within the broader context of efforts to reduce disparities, particularly with regard to payment and delivery system reform efforts. In his opinion, the proposed framework is “on the right track” because it is holistic and not siloed in its perspective. That perspective, he said, will enable integration of the framework into the broader efforts to reduce disparities. “There are some obvious links now with policy and change levers,” said Chin.
The broader framework that Chin believes this work fits into comes from a Robert Wood Johnson Foundation program on equity that he has run over the past decade. As part of this program, Chin and his colleagues developed a roadmap and set of best practices that organizations can follow to reduce racial and ethnic disparities in health care (Chin et al., 2012). One of the major lessons of this work, he said, is that there is no magic bullet for achieving equity. “You cannot roll out a model program and think it is going to solve the problem,” he said. While every solution involves raising
___________________
4 This section is based on the presentation by Marshall Chin, the Richard Parrillo Family Professor of Healthcare Ethics at The University of Chicago, and the statements are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
awareness that there is an equity problem and then prioritizing achieving equity, specific solutions must be tailored to fit the local context and involve an iterative quality improvement process that addresses specific barriers to change and uses the principles of implementation science.
In Chin’s experience, organizations do not like to hear that there is no magic bullet and that addressing disparities and equity is a systematic process. However, once an organization understands the change process, it then benefits from a menu of evidence-based interventions it can use as a starting point for developing its own solutions. As he noted, there is a good evidence base to support the effectiveness of these interventions
The roadmap Chin and his colleagues developed to reduce racial and ethnic disparities in care comprises six steps. The first step, as he mentioned earlier, is for an organization to recognize that disparities exist and commit to actions in two domains: prioritizing equity and reporting performance data stratified by race, ethnicity, language, and socioeconomic status. The second step is to implement a quality improvement infrastructure and process, and the third step is to make equity an integral part of quality. This third step is something that few organizations do well, he said. Equity is a dimension of quality that crosses all the other dimensions and something that should go beyond checking a box, he explained. Step four in creating the roadmap is to design interventions; step five is to implement, evaluate, and adjust the interventions; and step six is to sustain the interventions, which Chin said is a critical step. “Unless there is sustainability, this is all moot,” he said.
In reviewing the published literature on more than 400 equity interventions, Chin and his colleagues found a few common features that reduce disparities. The most common threads were that effective interventions were multifactorial, culturally tailored, and attacked different levers impacting disparities. Effective interventions relied on team-based care, involved families and community partners, employed CHWs, and included interactive skills-based training for patients as opposed to didactic lecturing.
Payment policy is perhaps the biggest barrier to change, one reported by even the most mission-driven safety net providers, such as federally qualified health centers. “They all say the same thing: that at a certain point, no matter how important the mission or goal such as equity, or how good an intervention program may be, there is only so much they can do because of the way they are paid,” said Chin. “They have to balance their bottom lines, ergo the importance of payment reform.”
Another barrier to a potential facilitator of change is motivation, both intrinsic and extrinsic. Intrinsic motivation has to do with professionalism and the desire to do things for the right reasons, Chin explained. The health care profession needs to do a better job of nurturing health equity as a priority across all levels. “Some of the most important parts of cultural
competency training build upon intrinsic motivation,” he said. However, he added, intrinsic motivation only goes so far if there is no economic case for change, a type of extrinsic motivation.
When Chin thinks about payment reform and value-based purchasing, he thinks about three buckets in terms of equity. One is pay for performance that incentivizes a specific action, such as providing mammography screening for underserved patients. The second bucket is for infrastructure to reduce disparities, for example, ensuring that enough of a global payment goes toward funding the preventive and primary care that currently is not incentivized to a great degree. The third bucket is addressing the social determinants of health and population health, an area in which Chin said there are emerging innovative programs.
The Medicare Access and Children’s Health Insurance Program Reauthorization Act, which includes quality payment programs such as MIPS and the Advanced Alternative Payment Model, is structured around requirements to meet various quality metrics, make more effective use of health information technologies, and achieve cost accountability. However, the regulations do not mention equity, said Chin. In his view, equity does not have a high enough priority at CMS despite the agency’s good intentions.
Regarding the need to create a business case for achieving equity in health care, Chin had several recommendations on how CMS and private payers can align financial incentives (Chin, 2016a). The first would be to require public reporting of stratified disparities data. The second would be to pay for reducing disparities and include equity accountability measures in payment programs, something that he believes is missing from most payment programs. “It still boggles my mind that there are no equity accountability measures,” said Chin. He noted that the framework Jessica French discussed includes these measures. His third recommendation was to strengthen incentives for prevention and primary care by updating the physician relative value unit payment schedule, moving toward global payments and shared savings plans, and developing intersectoral partnerships that address the social determinants of health.
Aligning financial incentives to promote equity, said Chin, will require aligning equity measures across public and private payers, as well as increasing payments to safety net providers such as by risk-adjusting performance measures or payment by patients’ social risk factors. The bottom line, he said, is to have an explicit equity lens when designing payment and quality improvement programs so that they reduce disparities intentionally rather than deal with them after the fact as unintended consequences.
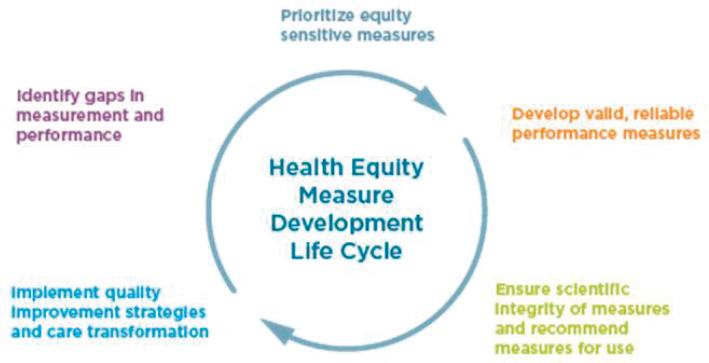
To address some of these recommendations, NQF has a Disparities Standing Committee. This committee has developed a health equity measure development life cycle (see Figure 3-1) that aims to incentivize reducing
disparities through measurement. Chin noted that the draft equity measures NQF has developed overlap with many of those in the draft framework, and they aim to help create a culture of equity within health care organizations. Such a culture would place a high priority on equity and cultural competency throughout an organization, and it would address workforce diversity and raise awareness of the cumulative structural disadvantages many individuals face. Chin noted that measures of equity in the NQF Disparities Standing Committee’s vision would promote advocacy and help build a safe and accessible environment for all.
Though a culture that supports equity is important, Chin said, organizational structures must also support equity. Organizational structures must have the capacity and resources to identify patients’ social risk factors, report and improve on stratified performance data, support a learning health system driven by quality improvement through an equity lens, and include population health management. A structure that supports equity would also conduct community needs assessments, include adequate policies and practices to support equity, and be transparent and accountable to the public.
The challenge, said Chin, is to develop measures that an organization can use to be accountable across the domains of providing equitable access, such as availability, accessibility, affordability, and convenience, and in delivering equitable high-quality care. These measures should drive both absolute attainment of equitable care and continuous improvements across structure, processes, and outcome performance stratified by social risk fac-
SOURCES: Presented by Chin on May 4, 2017; adapted from NQF, 2017.
tors. Fortunately, he added, there are many evidence-based interventions for reducing disparities. Many of these interventions rely on team-based care, use CHWs, are culturally tailored, and support self-care. They also include collaborations, partnerships, and linkages across health and nonhealth sectors that improve equity by integrating medical, behavioral, oral, and other health services; by building and sustaining social capital and social cohesion; and by addressing underlying social determinants of health.
In thinking about what the roundtable and NCQA are trying to accomplish, Chin said that education is necessary but not sufficient to produce the needed behavior change. Equity performance and accountability measures coupled with payment reform must also drive behavioral change. One word of caution, though, was not to let “perfect” be the enemy of “good” when thinking about performance metrics for use with payment and accountability programs.
As a final thought, Chin pondered the question of why health disparities persist. The simple answer, he said, is that the nation tolerates them (Chin, 2016b). “If there is a high enough priority, we would be making more progress,” he said. “The way we pay for medical care largely does not support efforts to achieve health equity.” In his opinion, movement advocacy can break down ingrained structural barriers and policies that impede health equity (Chin, 2017), and he suggested that the roundtable’s efforts to work on structural policies and regulations that impede equity can play an important role in breaking down those barriers. At the same time, clinicians, health organizations, and advocates need to build trusting relationships and resolve conflict with mutual respect and honesty at the front lines of care, he said. “We must combine advocacy and relationship-building to end disparities,” said Chin. “Achieving health equity will require policy changes and personalized clinical care and organizational transformation that are dependent on good will and trust. In other words, equity must be a priority in all health policy issues.” He noted in closing that the older he gets, the less patient he is regarding policy regulations that impede equity in health care and that fixing those regulations is not a high enough priority. “Leadership matters,” he said. “It is our professional responsibility as clinicians, administrators, and policy makers to improve the way we deliver care to diverse patients. We can do better.”
LEADERSHIP DEVELOPMENT, TALENT MANAGEMENT, ORGANIZATIONAL DEVELOPMENT, AND CHANGE5
Speaking from the perspective of Northwell Health’s journey to integrate health literacy, language access, and cultural competency as a means of helping its patients achieve better health outcomes by reducing health disparities and improving the overall patient experience, Wright noted that having an integrated approach to measurement is useful from the perspective of supporting improved patient understanding and engagement in health care. “Yet based upon the outcomes, it seems the overall approach has been challenging given the disconnected nature of the framework,” said Wright. Given that conclusion, he focused his remarks on strategies to address the gap in what he believes is fundamentally important for successfully implementing and sustaining the framework going forward.
Northwell Health, explained Wright, is “61,000 people looking at health care differently. We are many things, but every day we are one thing, dedicated to our communities.” Northwell Health is New York’s largest private employer, generating $11 billion in revenue, and is the nation’s 14th largest health system with 21 hospitals and more than 13,000 physicians and 15,000 nurses serving 8 million members in its network. In terms of community impact, Northwell Health contributes more than $878 million in community benefits and treats more than 2 million patients annually in 4.3 million patient encounters. Wright added that Northwell Health, which serves New York City and Long Island, operates in one of the most diverse communities in the United States. “We have always viewed diversity, inclusion, health literacy strategies, and principles as essential in transforming the health and wellness of all of our populations,” he said.
In 2010, Northwell Health created the Office of Diversity, Inclusion, and Health Literacy, formalizing its approach to diversity, inclusion, and health literacy across the organization. In 2011 and 2012, the organization embarked on a multiyear strategic plan to conduct a baseline assessment of several of its hospitals’ readiness to deliver effective, culturally competent communication in the context of patient-centered care. It also began a series of educational activities and other initiatives to strengthen the promotion of health, wellness, and the prevention and control of disease and illness and to enable people to live healthier lives by integrating the principles of equity, diversity, and health literacy in the community and in the delivery of health care. “We continue on this journey by way of operationalizing the tenets of diversity, inclusion, and health literacy into our fabric,” said Wright.
Today, Northwell Health is increasing its efforts to eliminate health
___________________
5 This section is based on the presentation by Michael Wright, vice president for diversity and health equity at Northwell Health, and the statements are not endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.
care disparities through inclusion, respect, and partnerships with the communities it serves. “Our ability to successfully deliver on this new chapter requires integrating the essential components of achieving health equity,” said Wright. “All of these essential components must work together, much like a well-oiled machine.” He supported the commissioned paper’s call for an integrated framework for quality and structure measures related to patient care, education, research, and governance, calling them necessary to support Northwell Health’s efforts. He noted that in 2016 the organization joined more than 1,400 hospitals in committing to the American Hospital Association’s #123forEquity Campaign to Eliminate Health Care Disparities.6 This campaign aims to make progress in three areas that provide opportunities for hospitals to increase the equity of care they deliver:
- Increase the collection and use of race, ethnicity, and language preference data and use the data to identify and solve health disparities
- Increase cultural competency training
- Increase diversity in leadership and governance
Northwell Health, he added, is leveraging the Institute for Healthcare Improvement’s framework to inform its priorities as it moves forward with its work in these three areas. This framework has five essential components:
- Make health equity a strategic priority
- Develop structure and processes to support health equity work
- Deploy specific strategies to address the multiple determinants of health on which health care organizations can have a direct impact
- Decrease institutional racism within the organization
- Develop partnerships with community organizations
The reason Northwell Health is taking these actions, said Wright, is that, despite the increases in American lifespan since 1900, there is still much work to do to protect the health of the communities it serves given the preponderance of chronic illnesses affecting the health of Americans. Toward that end, the organization has made patient-centeredness the essential foundation for quality and patient safety, and it is looking at patient-centeredness through total health. “We recognized that clinical care is only representing 20 percent of an individual’s health,” said Wright. “Clearly, we have to consider other factors.” As an example, he noted that poor medication adherence results from factors related to patients, physicians, and the health care system. This total health perspective, he added, requires
___________________
6 See http://www.equityofcare.org/pledge/index.shtml (accessed June 12, 2017).
looking at social and economic factors, health behaviors, and the physical environment in addition to clinical care.
To truly address the total health of the populations Northwell Health serves, it recognizes that it has to weave an understanding of the determinants of health into the very fabric of the organization and its financial commitment, its community outreach efforts, its community collaborations, and its accountability for outcomes in each of its service lines. “Underpinning all of this is the critical need for the integration of health care quality measures related to health literacy, language access, and cultural competence,” said Wright.
Creating a total health organization that emphasizes reducing the prevalence of chronic disease requires a new way of working with patients to address their health care, said Wright. “Although patient-centered approaches have contributed to significant advancements in care and to treatments that more fully respect patients’ preferences, values, and personal experiences, the reality is that health care professionals still hold a monopoly on the role of healer,” he explained. Northwell’s approach is not just to put patients at the center of care but to actively make them equal partners in their care. Patients, after all, are experts in their specific experiences of illness, and that expertise needs to be welcomed, valued, and fostered by other members of the care team, said Wright. Realizing this patient-as-partner approach requires leadership accountability to overcome the resistance associated with change and to support long-term sustainability of this change, he added.
In that regard, Wright said that a missing element in the framework, one that he believes is critical for its success going forward, is a disciplined and structured approach to managing change. Inserting change management strategies to support the shift to a patient-as-partner model could, in his opinion, achieve true breakthroughs in care. Without them, he added, the risk of failure, at huge cost to both industry and patients, is large. “The reality is that most of the factors impacting the success of change efforts are related not only to the soft side of change but also to the hard side of managing change, and so we need to get better at building our muscle around good change practice and integrating this into our change efforts and thinking how this fits into the integrated framework,” said Wright. Mismanaging change, as we know from our experiences, he added, can lead to the loss of valuable employees and their knowledge, a prolonged period of reduced productivity, lost opportunity for cost savings, and damaged relationships with service providers, among other consequences.
So how does this type of change look in the context of health care? Wright said that the process starts with a clear vision of change linked to specific outcomes. It requires identifying critical success factors that can be measured, involving stakeholders in supporting change, committing to
formal decision-making strategies and processes surrounding change, and dedicating resources to address the human aspects of change. The value of change management, he added, lies in its ability to improve management of stakeholder expectations and risks and provide a systematic approach to deliver business results. In addition, developing change management capacity improves overall management of complex strategic projects and programs that can accelerate an organization’s ability to change more rapidly and effectively in the future.
Unfortunately, he said, a large percentage of change projects fail for a variety of reasons. A failure to get buy-in across an organization is a major cause of failure, as is having unrealistic expectations about the change process. In Wright’s experience, a common mistake as evidenced across multiple industries is that organizations assume people go from awareness of the need for change to ownership even though they have not yet bought into the change. “Buy-in is a personal experience and it occurs at an individual level,” he noted. In his opinion, the change associated with the framework proposed in the discussion paper will be transformational. “We have to look at the scope, the sphere of influence, and the scale of change,” said Wright. “We are embarking on a complex change and, as such, we have to be thoughtful. We have to be intentional about how we are designing and applying methodologies to support a complex approach in addressing all the variables and the needs of our key stakeholders.”
Noting that there is a process methodology for effectively integrating change management activity streams within a project and ways to assess and measure outcomes related to good change practice, managing change effectively requires thinking about the impact of change from the stakeholders’ perspectives. “Our ability to be successful and to implement and sustain the measures we are suggesting in our proposed framework is ultimately dependent upon the consideration of fundamental questions impacting the targets of our change,” said Wright. Also important, he added, will be considering key behaviors for change leaders—how they take accountability for change, how they advocate for change, and how they provide the resources to support change and overcome obstacles.
He noted that sustaining change will require being mindful of intended impacts, establishing measures of short-term and longer-term progress, and being clear on desired targets. It will be important to track these change measures and make them available to stakeholders through dashboards as a means of involving them in the change process. “We need to bring people along on this journey, from being a target of change to a partner in the process, and not only our patients but even ourselves, as change agents and sponsors of this change,” said Wright.
Ensuring that implementation is lasting will require continued communication with stakeholders and building skill sets and incentives for the
partners in the process to keep people in the new state. Slippage, explained Wright, can be a factor in why change fails, and without a framework for sustaining change, organizations can go back to their old ways of behavior, which can have drastic impacts on patient health outcomes and the patient experience.
In closing, he noted the need to proactively address the risks and issues connected to organizational change and the transitions that individuals go through in the process of change. Change is hard, he said, and how an individual transitions is a choice. Creating change starts with articulating the rationale and goals for change, honoring what an organization has done up to the present, and making explicit the need for individuals to work differently in the future. While every individual and organization experiences change in unique ways and assimilates change at their own pace, a common language and standardized best practices, with clear, positive, value-oriented measures, can help individuals with change. Balancing pride for the past with the need to be future focused is an important message, as is the fact that the more someone experiences transformational change, the better they become at doing it. As a final thought, Wright quoted Charles Darwin, who said, “It is not the strongest species that survive, nor the most intelligent, but the ones most responsive to change.”
DISCUSSION
Jordan Sellers from Howard University asked Wright about the compromises Northwell Health made as it moved to integrate mental health care into the overall health care system. Wright replied that, although he was not at Northwell Health in 2012 when this integration occurred, he understood that the organization relied heavily on the Core Capacity Assessment Tool, an online, survey-based tool designed to collect information from key decision makers in an organization and create prioritized recommendations for building organizational capacity, to help develop a foundation on how to move forward around health literacy, cultural competency, and language access. Rosof, who was at Northwell Health at that time, commented that leadership was the focus of activity that moved the organization forward. “Leadership was so focused on moving forward, and the community was so important, that we really did not have to compromise much because there were resources that were given right from the very beginning,” said Rosof.
George Isham from HealthPartners asked Wright if the integration of these concepts into Northwell Health’s system could be applied to a federally qualified health center in New Mexico or an urban practice in central Los Angeles or if it needed to be tailored for each type of organization. Wright answered that it is a combination of both. “I think we have custom-
ized where it makes sense based on the audience and the need, but I think we also created a repeatable process that could be applied elsewhere for the most part. I would say it was taking the general tenets of cultural competency, health literacy, and language and customizing them to support unique needs within our communities and within our health system,” he explained.
Isham then asked if it would be helpful if NCQA or the federal government would specify the way integration should occur and require integration. Wright replied that any framework that has best practices, has been tested, and comes with supporting data that an organization can learn from would be helpful. He then noted that Northwell Health is always looking to use best practices from other health systems and industries outside of health care to improve its delivery of care. Brach added that she recently conducted a study of Northwell Health’s journey to becoming a health-literate organization and found certain structural elements that might lend themselves to being measured. “For example, we have been talking about community health workers as something we value, and we could say this is something that you need to have and we are going to measure it,” she explained. Similarly, having a language access coordinator and health literacy leader, as Northwell Health does at each of its facilities, could be required and measured.
Brach noted, though, that the issue of mandating those types of features is questionable because every organization has to adapt someone else’s best practices to fit its own context. “I think we want to tread softly in terms of mandates,” she said. The challenge will be to identify common denominators and identify measures and incentives to go along with those common features. Chin said, for example, that his institution is in the fourth year of a 5-year initiative to incorporate diversity and equity in all systems, and for some time he kept thinking that this should be a requirement for all institutions. However, as the initiative proceeded, he came to realize that an organization’s culture plays a large role in the specifics of how equity becomes institutionalized. The University of Chicago, for instance, uses the Lean7 method for its quality improvement process, but this may not be the right approach for every organization.
Terri Parnell from Health Literacy Partners noted that she was at Northwell Health when it launched its diversity, inclusion, and health literacy initiatives and that the organization found several documents helpful in its efforts. These included the roundtable’s Ten Attributes of Health Literate Health Care Organizations (Brach et al., 2012), the enhanced National Standards for Culturally and Linguistically Appropriate Services (enhanced CLAS standards), and numerous publications from the Joint Commission. That literature helped guide the development of new policies
___________________
7 See https://www.lean.org/WhatsLean (accessed November 13, 2017).
and procedures that served as the foundation for an organization-wide educational effort involving its entire workforce. One key for success was finding employees who had a passion for this work and having them help drive change among their coworkers. In addition, more formal, systemwide meetings at all 18 hospitals furthered the change process. Another important aspect of the change process, said Parnell, was having an overarching structure to which everyone was accountable, but at the same time allowing each hospital to be flexible in the way it implemented policies to reflect the different patient populations the hospitals served and the services they provided. “We had to give them that agility to be able to implement the health literacy, cultural competency, and language services in a way that worked for their organization,” she said. “That was a big key. It was not mandated but there was accountability.”
Wright added that, even today, Northwell Health still has site champions, as well as an executive-level council, focused on diversity and health equity issues. These site champions, he explained, report on the successes they have and synthesize many of the best practices developed throughout the Northwell Health system. “In many ways, they are the change agents in the field, but their success depends upon how well we are sponsoring and driving leadership accountability at the top of the organization,” said Wright. Fortunately, he added, the leadership team is deeply committed to this work and to health equity.
Jennifer Dillaha from the Arkansas Department of Health commented that a challenge her state has with implementing quality improvement strategies arises from the struggle that health care providers have in getting the data needed to drive these strategies from health information technology systems. Brach agreed that data collection is one of the main problems in the measurement domain. “We do not have good, reliable data on race, ethnicity, and language, and we have an even more difficult situation with health literacy, where a large cohort in the field does not feel that we should be doing individual assessments of health literacy,” said Brach. In addition, there is the burden on organizations to process and analyze those data that are available to drive quality improvement. Her “backdoor approach” has been to use the model for improvement that looks at small tests of change on the premise that working with a little bit of information is better than nothing when there is no infrastructure to support a data-driven, holistic strategy for quality improvement.
Chin also agreed that collecting data on race, ethnicity, and language preferences requires more work, and getting those data may require new regulations, incentives, and training. He recounted that when the Health Insurance Portability and Accountability Act (HIPAA) went into effect, the sentiment of patient advocates was that, although HIPAA required more work on the part of providers, patient privacy was so important that the
regulations were needed. In his opinion, health equity is critically important. “Some of this will require more work, but it is so important that it needs to be done,” said Chin. One challenge, he said, is that health information technology systems were designed for billing purposes rather than to drive quality improvement work. In that respect, the data collection and mining issue is part of a larger discussion on how to use health information technology and payment reform to drive systemwide quality improvement.
Wright noted that his group is working with Northwell Health’s information technology organization to determine how registration systems and electronic health records can collect these data. His sense is that the existing health information system is doing a good job at collecting data on race and ethnicity but is closing gaps with language preference. “We are looking at ways to standardize how that information is collected so that we can better report on it,” said Wright, who added that this effort is also examining how data on preferred gender are captured and integrated into equity reports. He also said that Northwell Health has more work to do on the training and education front to ensure that the organization is collecting the right data and that community members understand why they need to collect those data. The organization is currently embarking on a community campaign, “We Ask Because We Care,” to ensure that community members understand why the health system collects race, ethnicity, and language data. This campaign was modeled on a best practice from Henry Ford Hospital in Detroit, Michigan.
Ignatius Bau from Health Policy Consultation Services asked Brach if AHRQ had plans to integrate the concepts of health literacy and cultural competence into the CAHPS surveys and if the agency had a future vision of other ways of documenting and reporting on patient experience beyond CAHPS that might reflect the integrated approach described in the commissioned paper. Brach replied that questions relating to health literacy and cultural competence are available for several different CAHPS surveys. For example, there are separate item sets on health literacy and cultural competence, which includes language access, in the CAHPS surveys covering clinicians and group practices. In the survey for hospitals, language access questions are included in the health literacy item set and there is no separate item set for cultural competence. Brach said there is a schism within the CLAS community; some advocates argue that the language piece is most important, whereas others, particularly within the African American community, have other concerns they want organizations to address.
As far as looking beyond CAHPS, Brach said that there are other approaches that could be used, and she mentioned the patient tracer model. In this model, accreditation auditors follow patients through the time of their stay at a facility. “This can be a powerful information source for how an organization is performing,” she said. In fact, she added, the AHRQ
Health Literacy Universal Precautions Toolkit suggests that an organization shadow patients as part of its quality improvement activities.
Earnestine Willis from the Medical College of Wisconsin asked if Northwell Health was doing asset mapping as part of its community assessment work. She also asked if there are internal factors that influence a system or a community’s readiness to engage in quality metrics. Wright replied that one of his organization’s initiatives involves building an organization of CHWs. This initiative is developing the organization’s ability to identify and train CHWs who live where there are pockets of chronic disease in their communities. The idea here is that these individuals understand the needs of their communities, relate to the cultural values and beliefs of their communities, and are fluent in the languages spoken in those communities.
Allen asked if Robles had any take-away messages beyond the importance of leadership that would help the roundtable understand the most important on-the-ground issues. Robles replied that she advocates for the patient tracer method as an important tool for helping frontline staff understand the challenges around culture and language that their diverse clientele face in their interactions with the health care system. Another lesson has been the importance of including cultural competence and equity in an organization’s strategic plan. “If it is in your strategic plan then somebody is going to pay attention to it and somebody is going to do some kind of implementation associated with it,” said Robles.
She also noted that not only is addressing cultural issues and equity the right thing to do but there is also a business case for it given the demographic shift occurring in the United States that will have a majority of minorities by 2050. “Being able to create a welcoming environment for diverse populations produces results and especially produces good business results for organizations,” she said. “The loyalty factor is going to be with the health care systems that are providing the right types of services for the right types of patients.”
Chin added that another important lesson is that quality improvement is not a rigid linear process in which every organization goes from the same step one to the same step two and so on. Organizations should be prepared to take whatever steps are necessary in whatever order works for them to reach the desired end point. A second point he made was that cultural competency training is important but insufficient by itself to improve many clinical performance measures. Organizations need to include cultural competency training as part of their overall quality improvement and community engagement processes.
This page intentionally left blank.




















