5
Postcrash and Arrest Interventions
INTRODUCTION
While the two previous chapters discuss interventions aimed at influencing behaviors such as drinking to impairment and driving while impaired, this chapter focuses on reducing the likelihood or severity of negative outcomes of these behaviors: motor vehicle crashes and serious injuries and fatalities. As noted throughout the report, alcohol-impaired driving fatalities make up 28 percent of all traffic fatalities, and 10,497 people were killed in alcohol-impaired driving crashes in 2016. Because of data limitations, it can be difficult to obtain accurate arrest data on driving while impaired (DWI), accurate counts of how many offenders reoffend, and estimates of the number of DWI arrests that lead to a conviction (see Chapter 6 and Appendix A for more on data limitations). However, available data show that there were more than 1 million arrests for driving under the influence in 2015 (CDC, 2017; FBI, 2015). About 20 to 28 percent of first-time DWI offenders will repeat the offense (Lapham et al., 2006; Robertson et al., 2016), and recidivists are about 60 percent more likely to be involved in a fatal crash (Fell, 2014; Sloan et al., 2016).
This chapter begins with a section on the interventions (i.e., policies, systems, and programs) in the legal system that focus on deterring the general public (general deterrence) and those who have been previously arrested (specific deterrence) from driving while impaired. According to criminological theories, potential offenders balance risks and benefits when choosing whether to commit a crime (Nagin, 2013); deterrence theory relies on the perception of “swift, certain, and severe” detection
and punishment of criminal activity, including alcohol-impaired driving (Goodwin et al., 2015, p. 1-10; NIAAA, 2000; Nichols and Ross, 1989). This perception is built on a system of continued, publicized enforcement (IIHS, 2017a). This section also focuses on treatment of those convicted of alcohol-impaired driving to help modify their behaviors and decrease the likelihood that they will repeat the crime. There are many other points in the legal process that could be improved that are not discussed in this section. The interventions discussed are those the committee determined would have the greatest effect on the population, are feasible, are cost-effective, and target specific high-risk populations. The chapter’s second section includes information on how to improve emergency response after a motor vehicle crash, with a focus on rural areas. Although the committee did not focus on emergency response as an intervention, it is a promising area to help reduce fatalities in rural areas. As discussed in Chapter 2, rural areas are an important target population for alcohol-impaired driving because they account for a large proportion of fatal crashes, and many existing interventions are more relevant to urban areas. The interventions in this chapter engage the range of actors required to enforce laws and detect, prosecute, adjudicate, and treat alcohol-impaired drivers as well as respond to alcohol-impaired driving crashes.
LEGAL SYSTEM INTERVENTIONS: ENFORCEMENT
Law enforcement officers are trained to detect and arrest impaired drivers in three phases. The first phase is the law enforcement officer’s observation of the driver and any unsafe behaviors that draw the officer’s attention to the vehicle, such as lane swerving or failure to obey traffic signs and signals. After pulling over a potentially impaired driver, the second phase of detection involves the officer’s personal contact with the driver. Law enforcement officials are trained to use all senses when communicating with the driver. For example, the officer observes how the driver is speaking, any odors coming from the driver or vehicle, and any items visible in the vehicle. If the officer suspects the driver is impaired, he or she can then perform the third phase by requesting the driver to perform the standardized field sobriety tests (SFSTs). The officer will continue to observe the driver as he or she exits the vehicle, looking for additional indicators of impairment such as slurred speech or poor motor control. At this point the officer will also ask the driver if he or she has any medical conditions that would preclude the driver from performing the SFSTs. The SFSTs are made up of three validated parts: the walk and turn; the one-leg stand; and the horizontal gaze nystagmus (although some jurisdictions do not allow admission of testimony regarding the horizontal gaze nystagmus). In this phase, the officer may also administer
a preliminary, handheld breath test (PBT) (Voas and Fell, 2011). This device can be used to indicate the presence of alcohol, but the results cannot be used in court in most states. A drug recognition expert could also be summoned if the officer does not think alcohol is the sole cause of the driver’s impairment. Taken together, the observations of driving ability, communication with the driver, and performance on the SFSTs can lead an officer to conclude there is probable cause for arrest. Subsequent to arrest, officers will request the driver take a chemical test, such as a blood test, to determine blood alcohol concentration (BAC) (Voas and Fell, 2011). State laws vary with respect to policies criminalizing refusal to take chemical tests and license suspension at the point of arrest.
There are some barriers to the process of successfully detecting and arresting alcohol-impaired drivers. For example, law enforcement officers may not be adequately or consistently trained in the three phases or the agency might be understaffed. Additionally, some states have limited laboratories or personnel to complete tests, and tests are often expensive and resource intensive.
Furthermore, it is important to note that there is evidence of systematic discrimination and disproportionate targeting of people of color by the police in the United States (Aboelata et al., 2017; Ingraham, 2014; NASEM, 2017; President’s Task Force on 21st Century Policing, 2015). Implementing a unified approach to reducing alcohol-impaired driving in communities would require intensive officer training and community engagement to foster cooperation and avoid alienating residents as communities and police work toward a common goal of zero lives lost (Aboelata et al., 2017).
Breath and Blood Tests for Detecting Alcohol Impairment
Once an officer arrests a driver, the officer will ask the driver to provide a breath test, which may take place at a roadside location or at a police station (Berning et al., 2008). A driver may decline to provide a breath test. The refusal may significantly affect or hinder subsequent prosecution and sanctions, as the absence of a BAC test result precludes a suspected alcohol-impaired driver from being charged under a per se law (Berning et al., 2008).1 Driver refusal rates for tests vary greatly among states. In 2011, the range of state breath test refusal rates (of Puerto Rico and 33 states with adequate reporting data) was 1 percent to 82 percent, with a national average of 24 percent. Two states (Florida and New Hampshire) had breath test refusal rates above 70 percent, and two more states had rates above 40 percent. Puerto Rico and 21 states had breath
___________________
1 A per se law means that the act in question is illegal in and of itself.
test refusal rates below 25 percent, and of those, 6 states and Puerto Rico had rates of 10 percent or less (Namuswe et al., 2014).
Toxicologists can use a calculation (retrograde extrapolation) to determine an impaired driver’s BAC at the time of an offense using, for example, a later BAC result obtained at the police station after arrest (AAA, 2016). This calculation factors in details such as the driver’s weight, height, sex, number and type of drinks consumed, and time passed to establish a metabolism rate and estimated BAC while the person was driving (APRI, 2003). As an estimate based on assumptions, results of retrograde extrapolation are not as accurate as a BAC measured in real time. Results can be used in expert testimony in court; however, they may be challenged or excluded, which can disadvantage a prosecutor’s case (APRI, 2003; Robertson and Simpson, 2002).
Testing Alcohol Impairment—Practices and Policies
All 50 states and the District of Columbia have implied consent laws, meaning that drivers using state roads (or federally owned park roads) have “consented” to comply with sobriety testing if there is an indication that they are driving while impaired. In an effort to compel drivers to comply with sobriety testing, states have enacted laws that make it a criminal offense to refuse a chemical test (e.g., Minnesota and Nebraska, among 16 other states)2 (Goodwin et al., 2015). As discussed above, law enforcement officials have few tests at their disposal to identify and detect alcohol-impaired drivers, and each of these tests—the SFSTs, a handheld breath-testing device, and blood or urine tests—come with their own limitations and challenges. While the SFSTs and handheld breath-testing devices can be administered at the point of contact with a driver who is suspected of being alcohol impaired, blood, breath, or urine testing are generally administered by trained technicians at a hospital or police station. Some jurisdictions have introduced enforcement vans with evidentiary equipment, although these can be costly and are not available everywhere (DeMetrick, 2016; Hedlund and McCartt, 2002; NC Health and Human Services, 2017). SFSTs and blood, breath, and urine tests can all be used to facilitate the prosecution of DWI cases, although the extent to which they can be admissible in court varies from state to state.
One challenge that police officers face when it comes to administering alcohol-impairment tests is the possibility that drivers simply refuse to comply with their request for testing. Unless the penalty for refusing a chemical test exceeds the penalty that a driver could incur should they fail the test (e.g., being prosecuted for impaired driving), there is little
___________________
2 Number as of 2013 (Goodwin et al., 2015).
incentive for drivers to comply. See Chapter 4 for more information about no refusal enforcement. Without court-admissible tests results, however, it is difficult for police officers or court officials to prove whether a driver was indeed alcohol impaired at the time he or she was stopped.
In 2016, the Supreme Court ruled on a case involving the admissibility of breath and blood tests in states where drivers were told they were subject to criminal charges if they refused to comply with a police officer’s request to take a sobriety test.3 The defendants argued that their Fourth Amendment rights had been violated because they could not refuse the tests, and were not served a court-ordered warrant for the test, thus constituting an unreasonable search. In their ruling, the court determined that the Fourth Amendment rights of drivers were not violated and no warrant was necessary since the breath tests were not invasive, the tests only measured alcohol in the breath, and no biosamples were stored after the test was administered. In regard to blood tests, however, the court ruled that a warrant would be necessary since the act of drawing blood is invasive, an individual’s blood can yield additional information beyond the BAC, and biosamples could be saved or used for other purposes.
One strategy to increase BAC testing at the time of arrest, and to eliminate the need for retrograde extrapolation, is the use of electronic warrants. In many jurisdictions law enforcement officers are able to contact on-call judges remotely at the time of arrest and have an electronic warrant sent directly to their smartphones or computers to avoid a delay in testing. Traditional means of obtaining warrants could take hours. These systems link the officer, prosecutor, and judges and allow for the generation, review, approval, and filing of warrants. Potential challenges related to electronic warrants include the availability of judges to be on call, which could be especially difficult in smaller jurisdictions; organizing the needed services for the blood draws, including during evenings and weekends; training for those who obtain the blood samples (including training to minimize risk to oneself or others); transport of a driver to a hospital or clinic if a trained phlebotomist is not available; and the issue of the chain of evidence for the blood sample, as the assessment of the sample would not be performed by the nurse/practitioner who draws the blood, but would need to be taken or sent to a laboratory for analysis. While hospital laboratories are generally open 24/7, this type of testing is not generally performed on an emergency basis for someone who is not a patient in the emergency department (ED) or hospital. The blood would likely be sent to a state laboratory for processing, thereby not providing an immediate answer to the question related to BAC. In addition, if there are any questions during
___________________
3Birchfield v. North Dakota, 136 S. Ct. 2160 (2016) consolidated with Bernard v. Minnesota, 844 N.W.2d 41 (Minn. Ct. App. 2014) and Beylund v. North Dakota, 859 N.W.2d 403 (N.D. 2015).
the case about the chain of evidence, the person who draws the blood may need to appear in court to attest to the fact that s/he drew the blood and handed it directly to the police officer who was then responsible for getting it to the next destination. However, many law enforcement agencies need to address these issues regardless of when the blood sample is taken from the defendant. Hedlund (2017) notes that many law enforcement agencies are currently considering transitioning to an electronic warrant system to improve efficiency. While electronic warrants are a promising strategy for obtaining accurate BAC results, more guidance is needed on how to implement them and the required infrastructure and protocols.
A passive test, such as using a flashlight that is equipped with an alcohol sensor, can help police officers screen drivers who they suspect have been drinking. These have been shown to increase the arrest rate for police officers who do not normally make DWI arrests (Fell et al., 2008), but the tests do not aid in charging or prosecuting a driver who may have been driving under the influence of alcohol. A recent survey of law enforcement agencies found infrequent use of passive tests, mainly due to a lack of equipment (Eichelberger and McCartt, 2016), although past research has also documented officer aversion to passive tests because of personal safety concerns (e.g., using the device brings the officer in close contact with the driver and occupies one hand) (Goodwin et al., 2015; Leaf and Preusser, 1996).
LEGAL SYSTEM INTERVENTIONS: ADJUDICATION
The adjudication process begins after an alcohol-impaired driver has been arrested. An offender could be arraigned the same day as the arrest or released to come back to court another time. Before pleading guilty at a court appearance, hearing, or trial, defendants may undergo an alcohol evaluation by a trained, certified individual in some jurisdictions or states; the driver is often referred to a treatment program if he or she meets the criteria for alcohol use disorder (AUD, DSM-5)4 (SAMHSA, 2005a). Whether or not screening is mandatory and when screening takes place vary by state (Chang et al., 2002), but the results can inform the prosecutor’s proposal to the judge, along with other additional information such as performance on the SFSTs, chemical tests, observations of the driver,
___________________
4 Alcohol use disorder, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is based on the presence of at least two symptoms from a specific set of criteria, with subclassifications of mild, moderate, and severe, whereas the DSM-IV defined two different disorders (alcohol abuse and alcohol dependence) with separate criteria for each. This has implications for how the categories compare across various research studies. In this chapter these disorders will be defined as the study authors defined them in their methodology.
statements made by the offender during the arrest process and/or testing, the offender’s driving history, and the effect on the victim if a crash was involved. If the driver is found guilty of alcohol-impaired driving, penalties could include fines, restitution, license suspension or revocation, ignition interlock installation, serving time in a correctional facility, or probation (Goodwin et al., 2015; SAMHSA, 2005a). A driver convicted of DWI could also be sentenced to complete a treatment program, participate in a monitoring program, or attend a victim impact panel (Goodwin et al., 2015; SAMHSA, 2005a). Many states have enacted various vehicle and license plate sanctions, including vehicle immobilization, impoundment, or forfeiture, and license plate impoundment and marked license plates for offenders with revoked or suspended licenses (Goodwin et al., 2015). Implementation of these laws varies by state and the evidence base for individual measures is mixed, but in general these sanctions reduce DWI recidivism (Goodwin et al., 2015; TRB, 2013a). States have varying sanctions for convicted DWI offenders, such as the number of DWIs that raise the charge to a felony, as well as more severe penalties for higher BAC levels or for having a child in the car at the time of arrest or crash (Goodwin et al., 2015).
There are some challenges that can impede the adjudication process for ensuring offenders receive proper sentencing and treatment. For example, because blood test results can take a long time to be processed, a prosecutor may have to proceed to trial without those results and therefore potentially rely on less information when presenting the case. Furthermore, information on past DWI convictions in other states may not be available to inform the decision of whether an offense should be increased to a felony charge (AAA, 2016; Robertson and Simpson, 2002). Additionally, there can be discrepancies between arrest and conviction data since some arrests may lead to a lesser plea, and therefore a driver’s conviction may not reflect the initial reason for arrest (see Chapter 6 for more details and information gaps regarding these data sources). For example, someone could be charged with reckless driving in addition to a felony DWI but that driver might plead guilty to the felony and have other charges dropped as a result of a deal with the prosecutor. Moreover, alcohol-impaired driving offenses could be reduced to non-alcohol-impaired driving offenses, or a defendant’s record could be sealed.
Prosecution Process
Limits on Diversion and Plea Agreements
After an alcohol-impaired driving arrest, some offenders are given the option of participating in a diversion program or taking a plea agreement.
A diversion program usually takes the form of education or treatment, and if the program is successfully completed, then the defendant may be given the option to plead to a non-alcohol-impaired driving offense such as reckless driving, for example, or in some cases, charges may be dropped and the infraction erased from the offender’s record (Goodwin et al., 2015). There is variation in the types of education and treatment used in diversion programs, and as a result, the evidence on whether they are effective is mixed (Voas and Fisher, 2001). A plea agreement is an agreement in which the defendant agrees to plead guilty in return for a concession from the prosecutor. Restrictions on when prosecutors can offer plea agreements have been found to reduce alcohol-impaired driving recidivism (Goodwin et al., 2015; Surla and Koons, 1989). Survey results indicate that up to 75 percent of alcohol-impaired driving cases are resolved with a plea agreement, and the concession offered is most often a reduced penalty (Goodwin et al., 2015; Robertson and Simpson, 2002). Concessions, however, vary by state, and in some states plea agreements result in the elimination of penalties and a clean record (Goodwin et al., 2015). Or, lesser offenses could remain on the record, and at least one state (Washington) maintains a record of completed diversion programs (McCartt et al., 2013).
When the record of an alcohol-impaired driving offense is erased or reduced through participation in a diversion program or a plea agreement, then it becomes impossible to identify recidivist offenders, reducing the severity with which their crime is perceived and in turn, the severity of the consequences associated thereof (Hedlund and McCartt, 2002; NTSB, 2000; Robertson and Simpson, 2002; TRB, 2005a). Grunwald et al. (2001) found that approximately 40 percent of alcohol-impaired driving offenders in Rhode Island that were charged as a first-time offender had previous alcohol-impaired driving arrests that had been erased from their records. As of 2014, 13 states had anti-plea-bargaining statutes limiting when a plea bargain can be offered (NHTSA, 2016). The National Highway Traffic Safety Administration (NHTSA) rates limits on diversion and plea agreements as a four-star intervention (that is, demonstrated to be effective in certain situations) for reducing alcohol-impaired driving (Goodwin et al., 2015). The National Transportation Safety Board (NTSB, 2000), the Transportation Research Board (TRB, 2005a), and the Traffic Injury Research Foundation (Robertson and Simpson, 2002) have also recommended limits on diversion and plea agreements.
Many DWI cases do not proceed to trial and offenders are instead offered participation in diversion programs or plea agreements with reduced charges (AAA, 2016; Robertson and Simpson, 2002; Voas and Fisher, 2001). This section reviews limits on diversion and plea agreements, but notes evidence on diversion program effectiveness is mixed
because program components and studies of them vary substantially. The only study directly examining plea agreement restrictions found reduced recidivism in three communities in response to the restrictions (Surla and Koons, 1989). Eliminated offenses because of a diversion program or lessened charges as a result of a plea agreement have implications for the severity of punishment and subsequent offender interactions with the criminal justice system, such as later DWIs, and therefore, general and specific deterrent effects (Robertson and Simpson, 2002). Based on older and mixed evidence on plea agreement restrictions and diversion programs, the committee concludes:
Conclusion 5-1: Research is needed on the effects of restrictions on diversion programs that remove alcohol-impaired driving convictions from a driver’s record and on the content of plea agreements for alcohol-impaired driving offenders as strategies to reduce DWI recidivism.
Administrative License Suspension/Administrative License Revocation Laws
Administrative license suspension (ALS) laws permit law enforcement officials to suspend an alcohol-impaired driver’s license at the time of arrest for refusing to submit or failing (i.e., the driver’s BAC is over the limit set by state law) a chemical test to determine his or her BAC. Administrative license revocation (ALR) laws require driver’s license reapplication after a suspension concludes. These pre-conviction laws apply to both first-time and repeat offenders. These measures are separate from criminal convictions; drivers convicted of DWI may also lose their licenses and face additional criminal sanctions. A temporary license, which can be valid from 7 to 90 days, allows time for an administrative hearing and for the driver to obtain alternative transportation (Goodwin et al., 2015; IIHS, 2017a).
ALS laws are enacted in 41 states and the District of Columbia,5 but they vary in the length of temporary license validity, length of suspension, and whether limited driving privileges can be restored during the suspension period (IIHS, 2017b). For example, Virginia’s suspension period is 7 days. Mississippi suspends offenders’ licenses for 90 days, and while Arizona’s suspension is the same length of time, offenders in that state are allowed limited driving privileges after 30 days. At least 12 states allow driving during the suspension period if the driver agrees to an ignition interlock device (IIHS, 2017b). A recent study found suspension periods of at least 91 days to be more effective than shorter periods (Fell and Scherer,
___________________
5 Nine states do not have ALS/ALR laws: Kentucky, Michigan, Montana, New Jersey, Pennsylvania, Rhode Island, South Carolina, South Dakota, and Tennessee.
2017). NHTSA recommends an initial license suspension for at least 90 days for drivers with a BAC over 0.08% (or, 15 days followed by 75 days with a restricted license if the driver uses an ignition interlock device) and greater penalties for drivers who refuse a BAC test (NHTSA, 2006). Some states also allow a hardship provision, permitting the offender to drive to work or school (Goodwin et al., 2015). Although ALS laws have been challenged, court decisions have upheld these statutes, determining the laws ensure drivers’ due process as they provide a timely administrative hearing (IIHS, 2017c).
ALS and ALR laws are swift and certain; the consequences immediately follow the offending behavior, rather than following a conviction (Wagenaar and Maldonado-Molina, 2007). Many studies assessing the effectiveness of ALS and ALR laws were conducted as laws were enacted decades ago (Goodwin et al., 2015). These laws have been shown to affect alcohol-impaired driving crashes and fatalities (IIHS, 2017d; Talpins et al., 2014; Voas et al., 2000a). For example, one study found that alcohol-impaired driving crashes and first-time and repeat DWI convictions significantly declined after California’s ALS law was enacted (Rogers, 1997). Voas et al. (2000b) examined about 43,700 records of Ohio DWI offenders from 1990 to 1995. Compared to the time period before Ohio’s ALS law was enacted, the authors found reductions in DWI recidivism, moving violations, and crashes for first-time and multiple offenders after the law was implemented, although vehicle sanction legislation was also passed around the same time, which also could have affected driving outcomes. The recidivism rate within 24 months of arrest decreased from 15 to 5 percent for first-time offenders and from 25 to 7 percent among multiple offenders. Furthermore, crash involvement declined from 12 to 5 percent and from 14 to 7 percent among first-time and multiple offenders, respectively, in the 24 months after DWI arrest. Another large study that examined data in 38 states from 1976 to 2002 found a significant 5 percent reduction in alcohol-related fatal crash involvement and estimated the law(s) saved 800 lives per year (Wagenaar and Maldonado-Molina, 2007). This study found no significant effect of post-conviction suspension laws and concluded ALS policies are more effective in deterring alcohol-impaired driving than post-conviction license suspension or revocation (Wagenaar and Maldonado-Molina, 2007). While recent studies on cost-effectiveness of ALS and ALR laws have not been completed, a 1991 analysis of three states concluded that revenues generated from license reinstatement fees compensated for the laws’ operating expenses (Lacey et al., 1991).
License suspension or revocation does not, however, stop all DWI offenders from continuing to drive without a valid license (Goodwin et al., 2015; Lenton et al., 2010; McCartt et al., 2002), nor does it affect DWI
offenders’ alcohol consumption among those with AUD. Approximately half of first-time and repeat DWI offenders in one study delayed license reinstatement for at least 1 year (Voas et al., 2010a); those offenders who postpone license reinstatement are more likely to repeat the DWI offense compared to those drivers who reestablish their licenses (Voas et al., 2010b).
As described earlier in this chapter, the theory of deterrence relies on the perception of immediate, guaranteed, and severe punishment; well-implemented ALS and ALR laws ensure celerity and certainty of punishment (Goodwin et al., 2015; IIHS, 2017d). However, these laws are not in place in all states, and among those that have enacted laws, penalty severity varies among states. Although any suspension period is more effective than having no law, analyses favor ALS laws with longer suspension periods (Fell and Scherer, 2017). While there is a need for additional contemporary research, there is evidence from several studies that ALS and ALR laws have both general and specific deterrence effects, and the laws reduce alcohol-impaired driving crashes and convictions (Rogers, 1997; Voas et al., 2000a,b; Wagenaar and Maldonado-Molina, 2007). These effects can endure past the suspension period as well. In a recent study, Fell and Scherer (2017) found ALR laws had greater general deterrence effects than specific deterrence effects. This is an important finding because some offenders will continue to drive without a license, and these laws are one measure to deter alcohol-impaired driving among the general driving population. Other interventions, such as treatment, counseling, and ignition interlock devices (all discussed in more detail in this chapter), could complement ALS and ALR laws to prevent DWI recidivism (Goodwin et al., 2015; TRB, 2013a).
Conclusion 5-2: Nationwide adoption of effective administrative license suspension (ALS) and administrative license revocation (ALR) laws that provide for pre-conviction license suspension/revocation for refusing or failing a BAC test, that include an initial complete suspension, and that are based on updated model legislation would increase the effect of these laws.
Model legislation on ALS/ALR laws exists (NHTSA, 1986), but should be brought up-to-date. NHTSA could work with organizations that focus on state-level traffic laws and traffic safety to ensure that effective model laws (for example, full suspension for refusal to take a breath test) are in place and disseminated to states.
Treatment Related to the Adjudication Process
Different types of alcohol misuse necessitate the need for different, tailored types of interventions. Figure 5-1 shows a spectrum of problems related to alcohol misuse and the types of interventions that may be most beneficial for individuals suffering from each of these problems. The following sections describe some of these interventions and the individuals who may benefit the most from them, particularly among alcohol-impaired driving offenders. Although alcohol-impaired driving is a crime and law enforcement measures can be very effective, enforcement alone will not fully solve the problem of alcohol-impaired driving.
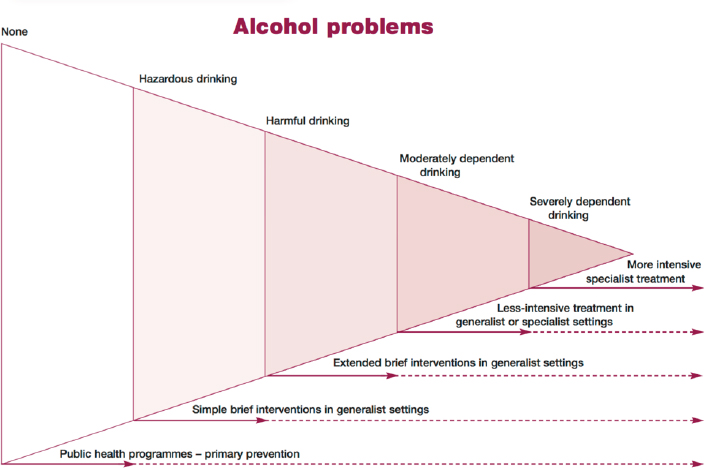
NOTES: Although the figure is not drawn to scale, the prevalence in the population of each of the categories of alcohol problem is approximated by the area of the triangle occupied; most people have no alcohol problems, a very large number show risky consumption but no current problems, many have risky consumption and less serious alcohol problems, some have moderate dependence and problems, and a few have severe dependence or complicated alcohol problems. In this figure, responses to alcohol problems include public health programs, brief interventions, and treatment. Each of these responses can differ with respect to the setting, duration, and intensity according to the problem.
SOURCE: Raistrick et al., 2006.
Alcohol Use Disorder (AUD) and Convictions for Driving While Impaired
There is a spectrum of reasons individuals drive while alcohol impaired. For those who do not suffer from AUD (DSM-5), swift and appropriate sanctions and penalties, or the use of screening, brief intervention, and referral to treatment (SBIRT) are generally effective. However, apprehension for DWI is an opportunity to identify and provide resources to people with AUD across the entire spectrum. When a convicted individual has AUD, treatment is a key part of the adjudication process to help modify his or her behavior and reduce the likelihood of driving while alcohol impaired again.
More than 15 million adults and 623,000 adolescents had AUD in 2015, according to results from the National Survey on Drug Use and Health (SAMHSA, 2016a). Furthermore, AUD is a highly comorbid condition; 2.7 million adults with AUD in 2015 also had an illicit drug use disorder (SAMHSA, 2016b). Data from the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions III showed both 12-month and lifetime AUD were significantly associated with other drug disorders, mood disorders including major depressive and bipolar I disorders, and antisocial and borderline personality disorders (Grant et al., 2015). There is no evidence whether interventions geared toward the general public (e.g., alternative transportation) will be as effective for DWI offenders with AUD. Furthermore, those who drink and drive may also drive while impaired by drugs (Talpins and Rogers, 2017; Talpins et al., 2015). For example, a study of 92 drivers arrested for DWI in Florida found that 41 percent tested positive for at least one of seven drug categories; the most prevalent drugs included cannabinoids, benzodiazepines, and cocaine (Logan et al., 2014).
Among those convicted of DWI, rates of alcoholism appear to increase as the number of DWI convictions increases (Cavaiola et al., 2003). A cohort study found that people with multiple DWIs are five times more likely than the general population to have an alcohol abuse or dependence diagnosis (DSM-IV) (Lapham et al., 2011). Brinkmann et al. (2002) found that more than 80 percent of individuals who drove with a BAC higher than 0.19% were alcoholics in a sample of alcohol-impaired drivers.6
Recent national estimates on how many DWI offenders are diagnosed with AUD in the general population are not available in the published literature. Hingson7 of the National Institute on Alcohol Abuse and Alco-
___________________
6 “Alcoholic” is defined in this study by Alc-Indices (calculated using methanol, acetone, 2-propanol, γ-GT, and CDT concentrations).
7 Personal communication with Ralph Hingson, National Institute on Alcohol Abuse and Alcoholism on April 13, 2017. Available by request from the National Academies of Sciences, Engineering, and Medicine’s Public Access Records Office (PARO@nas.edu).
holism (NIAAA) performed a descriptive analysis on data from the 2012 and 2013 National Epidemiology Survey and Related Conditions and found that among the 8 percent (n = 2,091) who reported driving after drinking in the past year, 25 percent met criteria for mild AUD, 21 percent moderate AUD, and 30 percent severe AUD. In the total population, 9 percent met criteria for mild AUD, 5 percent for moderate AUD, and 5 percent for severe AUD.8Stasiewicz et al. (2007) found 4.2 and 4.4 percent of convicted DWI offenders from a sample in Erie County, New York, were diagnosed with alcohol abuse and alcohol dependence, respectively (DSM-IV).
Screening DWI offenders for alcohol abuse problems is mandatory in most states, but not all; results can be used to inform treatment recommendations to the court (Chang et al., 2002). Sometimes formal screening methods involving testing and interviewing are used (Chang et al., 2001), but most courts use self-reported information from DWI offenders to screen for AUD, usually by having them complete a simple questionnaire about their alcohol use (NIAAA, 2004/2005). Offenders, however, often underreport their alcohol use for fear of punishment, judgment, or breach in confidentiality, resulting in a missed treatment opportunity for many (Center for Substance Abuse Treatment, 1995; Knight et al., 2002; Lapham et al., 2002, 2004). Although there are effective AUD screening guidelines available (Chang et al., 2002), courts generally cannot hire people specifically trained to screen for AUD because of financial limitations (Knight et al., 2002). The amount it would cost courts to screen and treat these individuals, however, is often much less than the cost of incarceration (Center for Substance Abuse Treatment, 1995; NIAAA, 2004/2005).
Court assessment, referral, intervention, and treatment strategies for DWI offenders vary substantially across the United States (Cavaiola and Wuth, 2014). Some forms of treatment for DWI offenders include motivational interviewing, brief interventions, cognitive behavioral therapy (CBT), and counseling (Robertson et al., 2008; SAMHSA, 2005a). Sentencing practices for driving under the influence of alcohol also vary by state. For example, courts in Washington provide a DWI sentencing grid based on BAC result and number of prior offenses to help judges determine appropriate punishments for DWI offenders. As noted, expanded alcohol assessment and treatment is deemed mandatory in the sentencing grid for any offender with two or three prior offenses (Washington Courts, 2016). A similar sentencing grid created by NHTSA in 2005 recommends alcohol use assessment and treatment for all repeat offenders (NHTSA, 2005).
___________________
8 Ibid.
Not all public court sentencing records are available electronically. In most states, court records are available on their website and are searchable by last name or court date, but only by county; they are often unreliable because all data are not routinely entered (see Chapter 6 for more information on data collection). For specific information, such as whether the offender was screened for AUD, one must often contact the court where an individual’s action was filed. The number of DWI arrests made per year by state is available through the Federal Bureau of Investigation’s Uniform Crime Reporting (UCR) program (FBI, 2010), but these data are neither comprehensive nor timely (Rosenfeld, 2007). The UCR program is made up of crime data reports submitted by police agencies across the country, but these crime rates are often underestimates because of barriers to monitoring and reporting such as financial restrictions, staffing changes, inadequate training, natural disasters, and new computers or crime reporting systems (Maltz and Targonski, 2002). Some states, like California, have been able to overcome these barriers and track not only arrest rates but also types of DWI convictions (Daoud et al., 2015).
DWI Courts
DWI courts are specialized courts aimed at changing DWI offenders’ behavior through comprehensive monitoring and substance abuse treatment. As a part of the DWI control system, these post-conviction courts are a systematic mechanism for holding offenders accountable for their actions while treating the underlying cause(s) of their impaired driving. They are a voluntary alternative to traditional probation (Fourth Judicial District Minnesota Judicial Branch, n.d.; Hawaii State Judiciary, n.d.). DWI courts are modeled after the successful drug court system (NADCP, n.d.) and are founded on 10 guiding principles (see Box 5-1).
Some DWI courts are a subset of drug courts; as of August 2014, there were 216 DWI courts across 31 states and 409 hybrid DWI/drug courts (Goodwin et al., 2015). In a 2016 survey, 40 percent of DWI courts reported primarily serving urban areas; more than one-third of programs indicated they mainly serve rural areas, but no respondents described principally serving tribal territory (Block, 2016). DWI courts reported predominantly white, fully employed participants (Block, 2016).
DWI courts are team-based, in which the judge, prosecuting and defense attorneys, probation officer, and treatment staff familiar with DWI laws and addiction issues work together to ensure an effective and individualized sentencing and treatment plan for the offender (Goodwin et al., 2015). Teams meet frequently to report program infractions, offer positive reinforcement, and modify restrictions when deemed appropriate. DWI courts’ intensive supervision involves observing the offender in public,
at home, and at work. This includes adherence to a treatment plan, use of ignition interlocks or car impounds, and alcohol and drug testing (using transdermal or breath test devices). Offender clinical assessments involve screening for alcohol triggers and drug abuse, evaluating physical and mental health, and considering employment and financial status. Motivation for change also plays a role in the treatment plan, which is usually multicomponent and incorporates effective medications (for a discussion of medications, see section on pharmacological treatments), behavioral therapies, peer support groups, and social skills training (NCDC, n.d.-a). Court programs typically last 1 to 3 years, and supervision can be lessened as participants move through a program’s different phases (Block, 2016; Goodwin et al., 2015; Hawaii State Judiciary, n.d.; NCDC, n.d.-b). Courts vary in requirements for serving jail time before entering the program; sentences usually do not change after program completion, although some programs reduce sentences (Block, 2016). Participants may be removed from programs for noncompliance or new charges (Block, 2016; Circuit Court of the State of Oregon, n.d.).
Evidence suggests that traditional court processes and sanctions are generally not effective in influencing the behavior of offenders with multiple DWIs (Goodwin et al., 2015; NCDC, n.d.-c). One-third of those arrested annually for driving impaired have a prior DWI conviction (NCDC, n.d.-b). Therefore, most DWI courts are aimed at offenders who have at least one prior DWI and/or who drove with a BAC of 0.15% or higher (NCDC, n.d.-c). DWI courts may disqualify offenders also convicted of felonies or violent crimes (Block, 2016; Hawaii State Judiciary, n.d.; NCDC, n.d.-a). Furthermore, 65 to 80 percent of first-time DWI offenders will not reoffend, and contact with the criminal justice system may offer enough deterrence for first-time offenders to avoid future impaired driving (Goodwin et al., 2015; NCDC, n.d.-b). DWI court resources are best directed toward repeat offenders with whom the treatment program can have the biggest effect. Only about 1 percent of those arrested for DWIs, however, are referred to a specialty court, and approximately half of those referred complete the program (Sloan et al., 2016).
A 2009 systematic review concluded DWI courts are an effective intervention in reducing recidivism, but found many studies were methodologically weak and encouraged additional future research (Marlowe et al., 2009). For example, one of the stronger studies in the review determined participants in an Oregon DWI court were less likely to be convicted of a DWI or other traffic violations (Lapham et al., 2006). Furthermore, 85 percent of studies in a 2012 meta-analysis favored DWI courts over traditional courts (Mitchell et al., 2012). Three of the four randomized studies reviewed in the meta-analysis found DWI courts reduced the odds of recidivism (Mitchell et al., 2012). The fourth experimental study, an
evaluation of a DWI court in Los Angeles County, did not find significant differences in drinking behavior or recidivism between the participants assigned to the DWI court and those assigned to a control group (traditional criminal court) during a 24-month follow-up period (MacDonald et al., 2007). The authors note limited jail time in the county for DWI offenders during the study period likely affected incentive to participate in the voluntary DWI court (MacDonald et al., 2007). However, this DWI court was created as an investigational program for a research study, and as such, was not pilot-tested or evaluated for compliance with DWI court guiding principles (Marlowe et al., 2009). Furthermore, aspects of the traditional court (control group) could be considered important elements of a DWI court (such as the number of status hearings in the first 6 months), so the two groups of participants received similar interventions (Marlowe et al., 2009).
Mitchell et al. (2012) found that more DWI court participants graduated from DWI programs compared to adult and juvenile drug court participants (Mitchell et al., 2012). DWI courts characterized by longer program duration and higher quantity of services usually have a higher completion rate, and graduates experience better outcomes, including increased educational fulfilment and enhanced employment status (Robertson et al., 2016; Sloan et al., 2013).
DWI courts have long-term effects on offenders as well. A study of DWI courts in North Carolina found reduced rates of recidivism over 4 years compared to people not referred to the specialty court (Sloan et al., 2016). Similar long-term, positive results were observed in an analysis of three Georgian DWI courts; recidivism rates of comparison groups matched by the number of previous DWI convictions, sex, and age were between 24 and 35 percent, while DWI court graduates’ recidivism rate was 9 percent (Fell et al., 2011; Goodwin et al., 2015; NCDC, 2015). Additionally, DWI courts may be more effective than hybrid DWI/drug courts in preventing DWI recidivism because drug courts enroll several types of participants and do not specifically target DWI offenders (Sloan et al., 2016).
Many DWI courts are funded through federal, state, and county grants as well as fees collected from offenders (Block, 2016). Participants often have to pay for program components such as alcohol monitoring and ignition interlocks, substance abuse treatment, and any imposed fines (Carey et al., 2008; Circuit Court of the State of Oregon, n.d.; Fourth Judicial District Minnesota Judicial Branch, n.d.). Although more resources (e.g., time and staff) are needed to provide DWI courts’ close monitoring, these courts do not cost more, and sometimes cost less, in up-front costs than traditional probation (Goodwin et al., 2015; NCDC, 2015). Additionally,
courts save money by reducing rearrests and total time offenders spend in jail (Carey et al., 2008; NCDC, 2015; NPC Research, 2014).
DWI courts are voluntary programs that couple offender supervision with individualized treatment; courts target high-need offenders who can benefit the most from these components. Characteristics of DWI court programs matter; analyses favor longer program duration and higher intensity contact between the participant and the DWI court (Sloan et al., 2013). Well-done studies by Fell et al. (2011), Lapham et al. (2006), and Sloan et al. (2016) demonstrate that DWI courts have short- and long-term specific deterrent effects. A meta-analysis (Mitchell et al., 2012) generally supports these individual findings, though some methodically weak studies of DWI courts (e.g., inadequately controlling for selection bias) and varying study designs result in different findings. The field could benefit from additional well-designed and executed studies that adhere to established standards. To improve health and safety outcomes and reduce recidivism of repeat offenders and high BAC offenders, the committee recommends:
Recommendation 5-1: Every state should implement DWI courts, guided by the evidence-based standards set by the National Center for DWI Courts, and all DWI courts should include available consultation or referral for evaluation by an addiction-trained clinician.
Screening, Brief Intervention, and Referral to Treatment (SBIRT)
SBIRT may serve to identify hazardous and harmful alcohol intake, as well as provide an opportunity for immediate intervention and referral to treatment, if necessary. DWI offenders are an important population to screen and treat for AUD (DSM-5). As noted earlier, there is not a reliable estimate of AUD among DWI offenders in the criminal justice system (Lapham et al., 2004). However, research suggests recidivists generally exhibit heavier and more frequent drinking behavior (Mullen et al., 2015). Additionally, only about a quarter of impaired drivers treated in EDs are convicted, so many of these offenders do not receive treatment through a court referral (Higgins-Biddle and Dilonardo, 2013). Importantly, many alcohol-impaired driving episodes are caused by binge drinkers, rather than heavy drinkers, so it is equally important to identify these patients and provide treatment before they are involved in an alcohol-impaired driving crash (Flowers et al., 2008; Higgins-Biddle and Dilonardo, 2013). It is clear then that SBIRT plays a role in the other phases of the committee’s framework (see Figure 1-5), but it is included in this chapter as it is
relevant to many of the treatment options that follow screening and brief intervention.
The main goal of SBIRT is to increase a patient’s awareness and understanding of the risks of excessive drinking and to motivate him or her to decrease his or her consumption (Agerwala and McCance-Katz, 2012). A range of health care workers can conduct SBIRT in a variety of settings, including the criminal justice system, EDs, primary care, behavioral health care, and college campuses. Screening, the first component of SBIRT, is usually done using one of several tools (e.g., AUDIT or CAGE) that have been tested and demonstrated to be effective in documenting alcohol consumption as well identifying at-risk alcohol consumption or possible AUD. This may be done in one of several ways: orally, in writing, via computer, or other electronic means (Agerwala and McCance-Katz, 2012; Higgins-Biddle and Dilonardo, 2013). If the screening results indicate at-risk alcohol consumption such as binge drinking or exceeding the recommended limits for low-risk consumption, a brief intervention is performed. In cases in which possible AUD is identified, a more thorough assessment may be done, and the brief intervention may focus on motivating the patient to begin treatment.
A brief intervention is a short, tailored, one-on-one counseling session, usually lasting between 5 and 30 minutes, that uses techniques from motivational interviewing, brief negotiated interviewing, and/or CBT to try to eliminate harmful drinking behaviors such as binge drinking and alcohol-impaired driving (NIAAA, 2005a; SAMHSA, n.d.). During the intervention, practitioners deliver the results of the screening, provide information on low-risk alcohol consumption, assess the patient’s motivation to change his or her alcohol consumption, and collaboratively set goals for decreasing consumption (Higgins-Biddle and Dilonardo, 2013). Brief interventions can vary considerably and may consist of one to four sessions depending on the severity of the patient’s alcohol problem, the setting, the clinician’s expertise, and time constraints (NIAAA, 2005a). Once the brief intervention is completed, the patient may receive follow-up in a primary care or behavioral health setting, or be referred for more extensive treatment if needed (NIAAA, 2005a). Treatment plans can vary in scope and duration, and they are tailored to the patient’s specific needs.
Several studies present strong evidence that brief interventions can effectively decrease harmful alcohol consumption (Dunn et al., 2001; Moyer et al., 2002; Vasilaki et al., 2006), especially when conducted in emergency care settings (D’Onofrio and Degutis, 2002; Nilsen et al., 2008), primary care settings (Ballesteros et al., 2004; Bertholet et al., 2005; Kaner et al., 2009; O’Donnell et al., 2014), and college settings (Carey et al., 2007; Larimer and Cronce, 2002). The evidence is inconclusive on whether brief alcohol interventions are effective in general hospital settings (Emmen et
al., 2004), among repeat DWI offenders (Brown et al., 2010; Miller et al., 2015; Ouimet et al., 2013), among heavy drinkers or those with alcohol dependence (Saitz, 2010), or among adolescent drivers (Steinka-Fry et al., 2015; Yuma-Guerrero et al., 2012); therefore, more research is needed in these areas. Current studies rely on self-reports of alcohol consumption and include participants who partake in SBIRT and then return for a follow-up assessment. To counteract self-reporting and self-selection bias, future research would benefit from analyzing population health effects in real-world settings. There is also evidence to suggest the positive effects of SBIRT wane over time, and further research is needed to determine the optimum frequency of interventions (O’Donnell et al., 2014). More investigation is also needed into whether brief interventions reduce alcohol-impaired driving (Dill et al., 2004), although at least one study has shown a brief intervention to be effective in decreasing drinking and driving (D’Onofrio et al., 2012).
The U.S. Preventive Services Task Force recommends all adults receive SBIRT at primary care visits (USPSTF, 2013). A recent study from the Centers for Disease Control and Prevention, however, found that only one in three self-reported binge drinkers were screened for alcohol misuse at their last checkup and told that their drinking was risky, and only one in six were screened and advised to reduce their drinking (McKnight-Eily et al., 2017). Primary care physicians have an opportunity to increase their use of SBIRT, allowing them to reach more patients engaging in risky drinking and reduce alcohol-impaired driving injuries. There are barriers, however, that make universal screening difficult. Beich et al. (2003) found approximately 9 percent of patients will screen positive for risky drinking behavior in primary care settings. Madras et al. (2009) found that when EDs and clinics are included, approximately 23 percent of patients screened will self-report risky drinking behavior. These low percentages cause some physicians, who are already strapped for time and resources, to discount SBIRT as an efficient use of their time (Beich et al., 2003). Staff training is also necessary before SBIRT can be effectively administered, which takes additional time and resources (Bernstein et al., 2009; Nilsen et al., 2006).
In addition to busy workloads and financial constraints, other barriers to administering SBIRT include
- underreporting of drinking by patients;
- health care professionals not seeing SBIRT as part of their job;
- more immediate, competing health problems (especially in the ED);
- lack of physician knowledge about alcohol guidelines;
- cultural differences in alcohol consumption; and
- that the topic of alcohol abuse can be a difficult one to discuss (Johnson et al., 2011).
Yokell et al. (2014) found that brief interventions were administered more often in rural EDs and less often in crowded, metropolitan EDs owing to time and financial constraints. In contrast, Colorado initiated a statewide SBIRT initiative over 10 years ago and has documented the strategies necessary for successful implementation of an SBIRT program, including clinical issues, training for health professionals, and reimbursement (Nunes et al., 2017). The Substance Abuse and Mental Health Services Administration (SAMHSA) funded a national initiative to implement SBIRT in general medicine and community settings. Evaluation of 11 of the programs demonstrated that the method used by SAMHSA was an effective way to implement the programs (Bray et al., 2017).
There are also legal reasons why a physician may be hesitant to screen a patient for alcohol misuse. Physicians are required to report “at-risk drivers” to their state Department of Motor Vehicles (DMV) in six states: California, Delaware, Nevada, New Jersey, Oregon, and Pennsylvania (AAA Foundation for Traffic Safety, 2016; State of Nevada, n.d.). The guidelines on which conditions physicians must report, however, are vague and vary by state. All states allow physicians to report medically at-risk patients to the DMV in good faith. Many physicians are more comfortable reporting an impaired driver to the DMV’s medical review board rather than to the police (Mello et al., 2003). The reported information is confidential in all states, but most states will release it if they receive a court order (AAA Foundation for Traffic Safety, 2016). Hesitant physicians may be concerned about patient confidentiality and the risk of civil action against the physician (Mello et al., 2003). Furthermore, the implementation of a law in Ontario, Canada, requiring physicians to warn medically at-risk drivers of the consequences of alcohol-impaired driving resulted in a reduced rate of crashes requiring emergency care, but the warning was also associated with increased depression and fewer subsequent doctor visits, suggesting that physicians should decide which patients would benefit most from a warning (Redelmeier et al., 2012). However, warning drivers of consequences without performing interventions to address risky drinking may be part of the difficulty with this approach.
Finally, insurance reimbursement policy may dissuade practitioners from administering SBIRT, although commercial insurance, Medicare, and Medicaid provide reimbursement for SBIRT (SAMHSA, 2017). The Uniform Accident and Sickness Policy Provision Law (UPPL) authorizes health insurance companies to deny claims for injuries sustained while intoxicated, including those that result from driving under the influence (Chezem, 2005). As of 2016, UPPL remains in place in 24 states (APIS,
2016). The National Conference of State Legislators worked to repeal UPPL laws and to ensure that states did not introduce new restrictions on insurance payments. O’Keeffe et al. (2009) assessed the costs associated with caring for patients who are intoxicated compared to those who are not and discussed the implications for costs borne by trauma centers in states with UPPL. The findings showed that alcohol consumption by minimally injured trauma patients is correlated with higher hospital charges, which are exacerbated in UPPL states, and, the authors conclude, are likely to increase with implementation of SBIRT. Gentilello et al. (2005a) analyzed survey data from trauma surgeons and identified UPPL as an important barrier to alcohol screening. The results indicated strong support for alcohol screening and intervention programs, yet the majority (51 percent) of surgeons reported not routinely measuring BAC. Furthermore, almost one-quarter of surgeons reported having a payment denied in the past 6 months based on alcohol screening results. Interestingly, SBIRT does not identify whether the visit at which SBIRT is being performed is for treatment of an alcohol-impaired driving injury, as the screening tool documents patterns of alcohol use, rather than report of use for a single incident. Because of this, SBIRT in itself may not contribute to denial of coverage for an injury.
It is important to note that SBIRT may be performed by a number of members of the health care team who have been trained in its use, which is one way to overcome the limitations of physician time and financial resources (Johnson et al., 2011). This includes nurses, social workers, health educators, and others who interact with patients on a regular basis. Education and training programs have been developed and disseminated through several initiatives by federal agencies, professional organizations such as the American College of Emergency Physicians and the Association for Medical Education and Research in Substance Abuse, and academic centers (ACEP, n.d.; AMERSA, n.d.). Studies have demonstrated that health promotion advocates, who do not have a professional license, can effectively perform SBIRT in the ED (Bernstein et al., 2009; D’Onofrio and Degutis, 2010). Carnegie et al. (1996) found that when provided with proper training, receptionists were open to helping with preventive medicine tasks. Several studies also suggest that SBIRT is cost-effective in the long term because it reduces health care costs by addressing risky alcohol behaviors before they lead to injury (Estee et al., 2010; Fleming et al., 2002; Gentilello et al., 2005b). A redistribution of ED resources that prioritizes SBIRT training and implementation may therefore make financial sense.
As discussed in this section, the evidence on SBIRT’s efficacy is strong, but it requires resources, training, and time. Many of the barriers outlined above could also be overcome through new technology that electronically administers screening and brief interventions to patients, such as at
computer kiosks, on tablets, or through smartphone applications and text messages. The Community Preventive Services Task Force9 recommends electronic screening and brief interventions to curtail harmful alcohol consumption (Community Preventive Services Task Force, 2012), and evidence suggests that electronic screening and brief interventions delivered through interactive, online programs and smartphones are effective (Donoghue et al., 2014; White et al., 2010).
Mobile health approaches have emerged as a promising strategy for expanding behavioral alcohol interventions (Kazemi et al., 2017; Muench et al., 2017). Recent studies by Suffoletto et al. (2014, 2015) found that brief interventions delivered by text messages were successful in reducing self-reported binge drinking among young adults discharged from the ED. In fact, findings from Suffoletto et al. (2015) suggested that an intervention consisting of an interactive text message with tailored feedback was more effective than self-monitoring without feedback and no text messaging or feedback (the control condition) in reducing alcohol consumption and related injury. These findings were consistent with a previous study, which also used text messaging to provide feedback to young adults who were identified as hazardous drinkers. The study findings showed that the text message intervention reduced heavy drinking; young adults who received the intervention reported about two fewer drinks per drinking day than they did at baseline and approximately three fewer heavy drinking days in the last month (Suffoletto et al., 2012).
A randomized controlled pilot study tested four types of alcohol-reduction themed text messages for problem drinkers. Participants significantly reduced their weekly drinking in response to loss-framed (i.e., conveys the consequences of harmful drinking) and tailored (i.e., conveys messages tailored to the individual’s baseline assessment and goal achievement) messages (Muench et al., 2017). There are many opportunities to reach more patients with alcohol problems as technology continues to develop, but further research is needed to identify which elements of electronic interventions are key to initiating behavioral changes (Bewick et al., 2008). The following sections discuss various treatment and program strategies for people who have AUD or engage in harmful drinking behaviors such as binge drinking.
___________________
9 The Community Preventive Services Task Force was formerly known as the Task Force on Community Preventive Services. Task Force publications prior to 2012 are cited as the latter, and those published after 2012 are cited as the former.
Use of Medications for Alcohol Use Disorders
There are four medications approved by the Food and Drug Administration (FDA) for the treatment of alcohol dependence: naltrexone (NTX), extended release naltrexone, acamprosate, and disulfiram (NIAAA, 2005b). NTX is an opioid receptor antagonist approved for the treatment of opioid addiction and AUD (SAMHSA, 2016c). It is taken as a 50 mg pill once per day and has been shown to reduce alcohol consumption and cravings in those with alcohol dependence (Lobmaier et al., 2011; SAMHSA, 2016c). NTX is effective because it blocks the feelings of euphoria associated with alcohol intoxication and has no abuse potential (O’Brien et al., 1996; Roozen et al., 2006). Oral NTX, however, is known for having poor adherence rates (Swift et al., 2011), possibly because of its initial side effects of nausea, vomiting, dizziness, and fatigue, or the patient belief that it is not effective (Carmen et al., 2004; Rohsenow et al., 2000; Srisurapanont and Jarusuraisin, 2005). Research also indicates that family history of alcohol dependence and genetic variations can influence the efficacy of NTX. Most notably, a polymorphism of the µ-opioid receptor gene may be positively associated with the efficacy of NTX (Chamorro et al., 2012; Garbutt et al., 2014; Oslin et al., 2006). Further research is needed to confirm these moderating effects. They have the potential to influence physician decision making by identifying subgroups that are more likely to respond positively to NTX.
Extended-release naltrexone requires intramuscular injection into the gluteus muscle at 380 mg per month (SAMHSA, 2016c). This schedule greatly improves adherence to treatment. The medication has the potential to increase compliance as it requires less frequent administration than NTX. Over 5 percent of users, however, experience complications at the injection site including induration, swelling, nodules, and itching (Walker et al., 2017). Injection site reactions can occur if the injection is made into fat rather than muscle. A recent study by Walker et al. (2017) suggests that a modified injection technique in which the needle is inserted at a 40 degree angle may help decrease injection site complications. Long-acting depot formulations or implants of NTX have also been under development and show promise in terms of increasing treatment efficacy and decreasing noncompliance rates (Goonoo et al., 2014). Although they are not yet approved by FDA, these new delivery systems have the potential to release NTX to the brain for up to 7 months after insertion (Goonoo et al., 2014). More research on the safety and tolerability of these medications is needed before they can be released for use by the general public (Goonoo et al., 2014). All FDA-approved addiction medications are covered by the Patient Protection and Affordable Care Act, and the high cost of naltrexone and extended-release naltrexone to prevent relapse is considered justified by the high cost of alcohol relapse.
Two pilot studies analyzed the specific effects of NTX on alcohol-impaired driving. The first study examined the efficacy of NTX on treating repeat DWI offenders. The researchers found that with NTX, participants’ daily drinks decreased by 77 percent and that vehicular failures to start because of an ignition interlock activation decreased from 3.1 to 1.29 percent of tests (Lapham and McMillan, 2011). The second study analyzed the feasibility and effectiveness of using extended-release NTX to treat alcohol dependence (DSM-IV) in three drug court settings. The researchers found that NTX treatment was associated with 57 percent fewer missed court sessions and a reduction in positive drug and alcohol tests (Finigan et al., 2011). An endpoint analysis found that 26 percent of standard-care clients were rearrested compared to 8 percent of clients treated with NTX (Finigan et al., 2011). Randomized, clinically-controlled trials that look specifically at NTX effects on alcohol-impaired driving are needed.
Acamprosate is a glutamate antagonist that is administered in two 333 mg tablets three times per day and is used to maintain abstinence of alcohol after withdrawal has occurred (SAMHSA, 2005b). A recent systematic review and meta-analysis of medications for treating AUD (DSM-5) found that oral NTX and acamprosate are equally effective in reducing rates of drinking relapse (Jonas et al., 2014). NTX has been shown to be more effective in reducing heavy drinking and craving, while acamprosate has been shown to be more effective in maintaining abstinence (Carmen et al., 2004; Maisel et al., 2013; Mann, 2004; Rösner et al., 2008). Research suggests that the combination of NTX and acamprosate is safe and more effective than treatment with either medication alone (Feeney et al., 2006; Kiefer and Wiedemann, 2004). The most common side effect from acamprosate is diarrhea, but this has not been shown to cause any problems in medication adherence (Carmen et al., 2004).
Disulfiram, the first medication approved by the FDA to treat alcohol dependence, is an alcohol-sensitizing agent that causes physical reactions such as sweating, hyperventilation, head and neck throbbing, nausea, vomiting, and weakness when the patient consumes any alcohol (Center for Substance Abuse Treatment, 2009). Once alcohol has been ingested it usually takes 10 to 30 minutes for this reaction to occur; the intensity shows individual variation (Center for Substance Abuse Treatment, 2009). Disulfiram is taken as a pill of 125 to 500 mg once per day (Center for Substance Abuse Treatment, 2009). Evidence on the effectiveness of disulfiram in treating alcohol dependence is mixed. There is compelling evidence to indicate that disulfiram decreases alcohol consumption when the drug is taken in a controlled laboratory setting (Fuller et al., 1986). In real-life settings, however, adherence is very difficult to maintain and ingestion of the medication must be supervised in order to be effective
(Brewer et al., 2000). In addition to compliance issues, high doses of alcohol and disulfiram can be life threatening, leading some physicians to dismiss it as a viable treatment option (Williams, 2005). Disulfiram is most effective and safe when used in substance abuse treatment programs where patients can be closely monitored (Schuckit, 2006).
Topiramate is an antiepileptic drug that was approved by FDA to prevent seizures. It can be used off-label to treat alcohol dependence as well (Kenna et al., 2009). It has been reported to decrease cravings and promote alcohol abstinence by mimicking the presence of alcohol in the brain (Ait-Daoud et al., 2006). Topiramate is taken as a 15 to 200 mg pill twice per day (Kenna et al., 2009). A meta-analysis of pharmacotherapy concluded there is moderate10 evidence to suggest that topiramate is associated with fewer drink days, fewer heavy drinking days, and fewer drinks per drinking day (Jonas et al., 2014). One review found oral naltrexone and topiramate were equally effective in increasing days of abstinence in those with alcohol dependence (DSM-IV), while acamprosate was only moderately effective (Miller et al., 2011). Topiramate has some side effects that may affect adherence including paresthesia, taste perversion, anorexia, and difficulty concentrating (Johnson et al., 2007). A study conducted on patients taking topiramate for long-term prevention of seizures found that cognitive slowing and dysphasia were the main reasons the medication was discontinued (Bootsma et al., 2004). Topiramate holds promise in producing self-efficacy to resist heavy drinking among a subset of heavy drinkers identified by a specific genotype (Kranzler et al., 2016),11 but further research is needed to understand how the drug affects alcohol-impaired driving.
Evidence suggests that most antipsychotics are not effective in reducing drinking or craving in patients with alcohol dependence (DSM-IV) (Kishi et al., 2013). While the antipsychotic quetiapine has shown some promising effects in treating alcohol dependence and abuse (DSM-IV) because of its effects on mood, anxiety, and sleep, more research is needed to determine its usefulness and to identify patients most likely to benefit from it (Ray et al., 2010).
Although psychopharmacological approaches to treating AUD have been shown to be cost-effective (Burton et al., 2016; Zarkin et al., 2010) and effective in reducing heavy drinking, medications are underused. In 2016, a survey of DWI courts reported that 31 courts used NTX for alcohol
___________________
10Jonas et al. (2014) based the strength of evidence on published guidance on comparing medical interventions from the Agency for Healthcare Research and Quality (Owens et al., 2008).
11 Heavy drinking was defined in this study as average weekly consumption of 18 and 24 standard drinks for women and men, respectively (Kranzler et al., 2016).
treatment services and 3 courts used acamprosate (Block, 2016). A 2008 study analyzed state-level policies and their association with the use of NTX in treatment facilities. They found that Medicaid policies that support the use of generic drugs were associated with higher NTX use while policies with preferred drug lists and restricted pharmacy network were not (Heinrich and Hill, 2008).
The quality of the evidence for the efficacy of anti-relapse medications is excellent. For NTX, the first such medication approved by FDA for efficacy in preventing relapse, the evidence is based on placebo-controlled, randomized clinical trials conducted in multiple countries throughout the world. The most reliable finding for success is not total abstinence from drinking, but rather a reduction in the number of heavy drinking days. This translates into fewer opportunities to drive a vehicle in an alcohol-impaired state. While there are reports from drug courts on the benefits of using medication as a means of preventing relapse to alcohol-impaired driving, the published controlled trials were not conducted among drug court participants. The evidence for NTX, acamprosate, and topiramate is mainly based on controlled trials and meta-analyses, while that for disulfiram is poor for efficacy because of high drop-out from treatment. NTX, extended-release NTX, acamprosate, disulfiram, and topiramate all appear to be effective in certain situations, but more research is needed to determine which medications are most beneficial for which patients. Most of the research on the effects of these medications has been done on adults; future research should analyze the effectiveness of pharmacotherapy for younger populations of driving age (Stockings et al., 2016). Although medication is a helpful tool in treating people with AUD, research indicates that psychosocial therapy given in conjunction is beneficial (Miller et al., 2011; Rohsenow, 2004; Roozen et al., 2006; Srisurapanont and Jarusuraisin, 2005).
Conclusion 5-3: Though effect sizes vary, medications in combination with other treatment modalities to treat individuals with alcohol use disorder who have been convicted of alcohol-impaired driving can reduce impaired-driving recidivism.
While a single DWI does not imply an illness, repeat offenders have a high probability of having an AUD. This, like other addictions, is a disease of the brain and requires long-term treatment to prevent relapse. The offender needs to be evaluated by a clinician with addiction training and, if medically indicated, placed in a program that includes relapse prevention medication and the requirement for an extended period of attendance in therapy (see the following section for a discussion of one such therapy—CBT). Because there are barriers to adherence to medication,
success in some DWI programs for repeat offenders has involved monthly injections of extended-release naltrexone. As explained above, this medication reduces reward from alcohol drinking, has minimal side effects, and often reduces craving for alcohol. The result reported in most studies is a reduction in heavy drinking, though not total abstinence. There are many barriers to AUD treatment, including stigma, comorbid conditions requiring treatment, lack of perceived need for treatment or motivation for change, lack of adequate training among health care professionals, and decreased access to or increased cost of medications or providers (Knudsen et al., 2011; NIAAA, 2010; Schuler et al., 2015). Furthermore, offenders could refuse to comply with compulsory treatment components of sentences, after which they would face additional punishment; motivational enhancement therapy could be helpful for these offenders (Dill and Wells-Parker, 2006).
Cognitive Behavioral Therapy (CBT)
CBT is a structured behavioral therapy that helps patients solve problems by changing their patterns of thought and therefore their behavior and coping strategies in response to daily situations. There are several effective approaches to CBT in addressing AUD. For example, motivational interventions are relatively brief and focus on readiness to change behavior (Magill and Ray, 2009; Miller and Rollnick, 2002). Contingency management involves the provision of some type of material reinforcement when an individual refrains from drinking alcohol (Petry et al., 2000; Prendergast et al., 2006). The community reinforcement approach is focused on making sobriety more rewarding than alcohol use. Behavioral couples therapy centers around the effects of alcohol use on the relationship (Epstein and McCrady, 1998; Powers et al., 2008). CBT can also be made available online or through other communication technologies, making it more accessible to patients in remote areas. For example, CBT has been adapted to interactive voice response for continuing care after AUD treatment (Rose et al., 2015) and other mobile or Internet-based tools for a variety of conditions (Blankers et al., 2011; Marsch et al., 2014; Vallury et al., 2015).
CBT may also be used in conjunction with other therapies, such as medications that have demonstrated effectiveness in the treatment of AUD. For example, a systematic review found that the community reinforcement approach combined with the medication disulfiram decreased the number of drinking days, but there was conflicting evidence of the impact of a community reinforcement approach on abstinence (Hunt and Azrin, 1973; Roozen et al., 2004). Studies have shown that CBT combined with naltrexone, alone or with acamprosate, is an effective treatment for
alcohol dependence (DSM-IV) (Anton et al., 2006; Feeney et al., 2006). However, the COMBINE study did not demonstrate any significant added effectiveness of the combination of naltrexone, acamprosate, and behavioral interventions (Anton et al., 2006). Another study found that while acamprosate was more effective in promoting abstinence, naltrexone had a slight advantage in reducing heavy drinking and craving, but this review did not examine the effect of the medications in conjunction with CBT (Maisel et al., 2013). The degree of effectiveness of CBT in combination with medications warrants further study, given the number of people with AUD and the consequences that can result from the disease for patients and the public.
Cost-Effectiveness of Treatment to Reduce Alcohol-Impaired Driving Crashes
The committee could not identify a study of alcohol treatment that specifically examined the cost-effectiveness related to alcohol-impaired driving crashes and/or fatalities as the single outcome. However, there are multiple studies of the cost-effectiveness of AUD treatment with respect to other outcomes, suggesting that AUD treatment can be cost-effective. Thus, while there are no studies evaluating whether AUD treatment is cost-effective when solely considering reducing alcohol-impaired driving crashes, there would likely be other important effects from AUD treatment to other socially desirable outcomes such that treatment could be cost-effective when considering a broader set of outcomes.
For example, the study by Fleming et al. (2002) included motor vehicle crashes, operating a vehicle while intoxicated, and operating while under the influence as components of the full set of benefits of a brief intervention. However, these were not separate endpoints, but rather they factored into the full benefits (measured as costs averted). The study found that motor vehicle crashes declined with the study’s specific brief intervention, which included two in-person physician visits followed up by two nurse calls and other related activities (e.g., a worksheet and an “agreement”). The high-quality study includes randomization to treatment arms, a large sample, and a long follow-up period (48 months). The extent to which the findings can be generalized to other brief interventions or to treatments more generally is not clear. However, a review of multiple screening and counseling studies found that brief intervention was one of the most cost-effective among a number of effective services (Solberg et al., 2008).
Gentilello et al. (2005b) conducted a cost-benefit analysis of alcohol interventions for patients treated in U.S. hospitals and EDs. The authors found that every $1.00 spent on screening and intervention saved $3.81 in health care costs. Net cost savings per patient for screening are $89, and for an intervention the savings are $330. It is important to note that
Gentilello et al. did not take into account societal costs or health care follow-up costs. A similar study by Purshouse et al. (2013) modeled the cost-effectiveness of brief intervention and alcohol screening within primary care in England, using quality-adjusted life years as the outcome. Study researchers found that screening patients upon registering with a general practitioner would be cost-effective, saving £120 million in health care costs over 30 years.
Zarkin et al. (2008) and Dunlap et al. (2010) both examined the cost-effectiveness of several combinations of medications and behavioral therapies for treating alcohol dependence (DSM-IV) that were examined in a large (1,383 patients) randomized clinical trial. However, neither study included alcohol-impaired driving or crashes in their analyses. Instead, the main outcomes of the study were the incremental costs per percentage point increase in percentage of days abstinent, as well as the incremental costs of avoiding heavy drinking and of achieving a good clinical outcome. A recent evidence review on treating alcohol dependence with medication found that it is cost-effective when compared to standard care (Burton et al., 2016). Treatment with medication and psychotherapy has also been found to result in decreased median social costs, such as those associated with motor vehicle crashes, arrests, and health care (Zarkin et al., 2010).
In summary, although cost-effectiveness analyses for alcohol-impaired driving as a primary outcome are not clear at this time, use of medications for AUD to prevent alcohol-impaired driving fatalities should not be discounted.
Conclusion
Assessment, treatment, and monitoring of alcohol-impaired driving offenders remain critical elements in reducing alcohol-impaired driving recidivism and fatal crashes. Therefore, the committee recommends the following:
Recommendation 5-2: All health care systems and health insurers should cover and facilitate effective evaluation, prevention, and treatment strategies for binge drinking and alcohol use disorders including screening, brief intervention, and referral to treatment (SBIRT), cognitive behavioral therapy, and medication-assisted therapy.
Alcoholics Anonymous
Alcoholics Anonymous (AA) is an international, self-help recovery program founded in the 1930s for “alcoholics” (now defined in DSM-5 as a spectrum of alcohol use disorder) to achieve sobriety (AA, 2017). The group frames the disorder as “a progressive illness which can never be ‘cured,’ but which, like some other illnesses, can be arrested” (AA World Services Inc., 1984, p. 9). It is a nonprofessional, nonclinical, peer-to-peer program based on 12 steps, which include an individual admitting a problem with alcohol, asking for help from a higher power, making amends with people who have been harmed by his or her drinking, and providing emotional support for others in the same situation (AA, n.d.). AA and other 12-step programs have become a common part of alcohol and drug treatment and aftercare (Gross, 2010). For example, DWI courts’ treatment component includes development of an individual treatment plan that can include participation in a 12-step program to maintain abstinence (NCDC, n.d.-d).
Peer support groups can be an important part of treating those with substance use disorders (Tracy and Wallace, 2016). AA has an estimated 2 million members worldwide and is frequently suggested as an intervention for people with alcohol use disorder (Ferri et al., 2006; Gross, 2010; Tracy and Wallace, 2016). Involvement in AA can be associated with the development of healthy coping mechanisms and increased self-efficacy, which are related to better outcomes (Tracy and Wallace, 2016). However, potential participants may be deterred by the program’s lack of treatment or its religious overtones (Tracy and Wallace, 2016).
Research into the effectiveness of AA can be controversial and produces mixed results (Dill and Wells-Parker, 2006; Kaskutas, 2009). For example, mandatory AA attendance as an intervention ranked low in efficacy in a review of 361 controlled trials of various alcohol use disorder treatments (Miller and Wilbourne, 2002). For this reason, the DWI court model compliance checklist cautions DWI courts against assigning AA participation, because forced AA attendance could modify its effectiveness, and because some people in DWI courts are not the target AA population (NCDC, n.d.-d). Additionally, the Cochrane Group reviewed eight trials including mandatory and voluntary participants of AA and other 12-step programs. The authors concluded there was no strong evidence from a number of studies that AA had an effect on therapy acceptance or duration compared to other interventions, nor were there conclusive studies with evidence of AA’s effectiveness in reducing alcohol dependence or realizing abstinence (Ferri et al., 2006).
Kaskutas (2009) reviewed additional AA literature and found varied results. Observational research generally associates AA with positive outcomes, but this could be due to self-selection bias (Humphreys et al., 2014;
Kaskutas, 2009). Alcohol abstinence was higher among a large sample of male Veterans Health Administration inpatients who attended AA compared to those who did not attend (Kaskutas, 2009). Sustained and frequent AA attendance was associated with higher alcohol abstinence rates across separate populations and lengths of follow-up, and components of the AA program are aligned with theories of behavioral change (such as adjustments in life outlook, strengthening positive social ties, and improving self-efficacy and relapse prevention skills) (Kaskutas, 2009). However, experimental studies in the sample produced the weakest evidence, and results were similarly wide ranging (indications of positive, negative, or null effects) after adjustment for confounders or flaws in study design (Kaskutas, 2009). Finally, few recent studies explore alcohol-impaired driving outcomes (Dill and Wells-Parker, 2006). One observational study found previously untreated DWI offenders who attended AA and received outpatient treatment were less likely to repeat the offense within 1 and 16 years of follow-up, although results could again be affected by self-selection bias (Timko et al., 2011).
The literature lacks robust, well-designed studies in which AA is compared to interventions where successful elements can be identified. Additional studies are needed to examine AA’s effect on alcohol-impaired driving outcomes; the program may be more effective in reducing DWI recidivism if combined with other interventions, although the effects of mandatory versus voluntary participation need further investigation as well (Dill and Wells-Parker, 2006).
Penalties and Sanctions
Offender Monitoring: The 24/7 Program and Continuous Alcohol Monitoring Devices
Close DWI offender monitoring can be accomplished through a variety of approaches, including intensive supervision programs such as DWI courts (discussed earlier in this chapter), staggered sentencing (allows offenders to serve a portion of his or her full sentence in jail followed by 3 to 6 years of additional monitoring and probation in which segments of the full sentence can be stayed), and the 24/7 program. Components of intensive supervision programs can include AUD screening and treatment, supervision (including continuous alcohol monitoring devices), license and/or vehicle sanctions, and punishment for noncompliance, depending on the program, its resources, and community needs (Wiliszowski et al., 2011). Such programs can be offered at state or local levels. There is evidence that close offender monitoring reduces DWI recidivism (AAA, 2016; Goodwin et al., 2015; Wiliszowski et al., 2011).
For example, a Minnesota staggered sentencing program significantly reduced the recidivism rate in program participants for up to 4 years when compared to age- and sex-matched nonparticipants (Wiliszowski et al., 2011).
In 2005, the State of South Dakota enacted the 24/7 Sobriety Program, a statewide program to reduce alcohol- or drug-related incarcerations by eliminating (or limiting) alcohol and drug use by repeat offenders. The 24/7 Program combines thorough alcohol and drug testing and monitoring with immediate and certain punishment for violations, and therefore provides an opportunity for repeat offenders to avoid incarceration and remain active in their communities as long as they abstain from alcohol or drug use. In participating counties, repeat offenders or offenders with BAC levels at or above 0.17% must participate in the 24/7 Program to get a work permit. Participation can also be mandated as a condition of certain court actions—such as sentencing, probation, parole, or court-ordered care or treatment—or may be required in child custody or visitation orders (Loudenburg et al., 2010; Nicosia et al., 2016). In 2009, 59 percent of all 24/7 Program participants were guilty of DWI offenses while the remainder of participants (41 percent) had drug or other alcohol offenses (Loudenburg et al., 2010).
The 24/7 Program’s focus on repeated alcohol (and drug) testing and the certainty of immediate consequences for a failed drug- or alcohol-detection test make it unique. Most program participants are subject to twice-daily PBTs, which are typically administered at the local sheriff’s office at 12-hour intervals (typically between the hours of 7–9 a.m. and 7–9 p.m.). To pass a test, participants must test negative for alcohol use or be officially excused from taking a test. Missing or failing a PBT (by having alcohol detected) results in immediate but modest jail time, usually lasting overnight or 1 to 2 days. While twice-daily PBTs are the most commonly used monitoring method, transdermal continuous alcohol monitoring and testing can also be conducted electronically through the use of ankle bracelet testing, once-per-day PBT, or urinalysis; occasionally these tests are administered contemporaneously or used in conjunction with ignition interlock devices (Loudenburg et al., 2010). The continuous alcohol monitoring devices use a transdermal sampling method every 30 minutes to detect ethanol vapor at the skin’s surface as perspiration evaporates, and wirelessly transmit sampling results from the ankle device to the monitoring agency at predetermined times, one to six times daily (SCRAM Systems, 2017). Continuous alcohol monitoring units are programmed to detect tampering and can also be used to monitor the movement of offenders who are under house arrest.
The use of transdermal devices is seen as an especially promising alternative for offenders who face special challenges securing transportation to
and from law enforcement agencies for twice-daily PBT tests, and for populations such as those who live in rural communities (MADD, 2013). 24/7 Sobriety Program participants are responsible for paying testing fees—$1 per PBT test, $10 for a urinalysis, $40 for each drug patch attached, $40 for the activation and deactivation of a mobile testing device, and $4 per day for use, as well as a program participation fee not to exceed $3 per day (South Dakota Legislature, 2017).
Evaluations of South Dakota’s 24/7 Sobriety Program have garnered positive results. Loudenburg et al. (2010) reviewed 24/7 Sobriety Program data from 17,874 participants, collected between the program’s inception in 2005 through January 2010, to evaluate testing results and recidivism rates for program participants. Researchers found that offenders who had one or two DWI offenses, 24 to 31 percent and 40 to 47 percent, respectively, made up the largest percentage of 24/7 Sobriety Program participants. The majority of offenders participated in the program for at least 31 to 60 days (n = 982) or 91 to 180 days (n = 963). Test results from 802,210 records showed that participants successfully passed 99.4 percent of PBT tests, and of the sample evaluated (n = 4,009), 54.5 percent (2,183 participants) passed all of their tests and only 8.8 percent (351 participants) had failed more than three tests. When compared to controls, participants who entered the program after their second DWI and were tested for at least 30 consecutive days had a statistically significant 74 percent reduction in recidivism for future DWI arrests (from 13.7 percent to 3.6 percent). Participants who had their third DWI when they entered the program and had similar testing had a 44 percent decrease in recidivism (from 15.3 to 8.6 percent) and these results improved when consecutive testing days were increased to 90 days.
Similar results were seen in differences-in-differences analyses conducted by Kilmer et al. (2013) and Nicosia et al. (2016). Using South Dakota county data collected between January 2001 and December 2010, Kilmer et al. (2013) made comparisons using pre- and post-24/7 Sobriety Program implementation data. The authors found a reduction in DWI incidence and reported crashes involving males between 18 and 40 years of age, as well as significant reductions in repeat arrests (12 percent) and domestic violence arrests (9 percent), in counties where the number of participants was at least one-quarter of all DWI arrests in the county. Nicosia et al. (2016) used 24/7 Program data from January 2000 through June 2011 to determine whether the program was associated with a reduction in mortality by evaluating total deaths as well as deaths caused by circulatory or digestive disorders, external injuries, or cancer. Based on 9,108 county-month observations, the authors found a 4.2 percent reduction in all-cause mortality since implementation of the 24/7 Sobriety Program. No deterrent effect for first-time DWI arrests was apparent.
Since being implemented in South Dakota, five other rural states have put the 24/7 Program into place: Alaska, Iowa, Montana, North Dakota, and Wyoming. Several additional states, including Florida, Illinois, New Mexico, Pennsylvania, Tennessee, Virginia, Washington, West Virginia, and Wisconsin, are considering the program as well (Sobering Up, 2016). (See Box 5-2 for how a rural sheriff’s department in Tennessee recently used monitoring devices as part of a comprehensive approach to reducing alcohol-impaired driving.) Of the new state programs that have been evaluated, results similar to South Dakota’s have been found in the evaluated new state programs. RAND evaluated the Montana program and found “suggestive evidence” that 24/7 participation reduced the probability of DWI rearrest (within 12 months) among second-time offenders by approximately 45 to 70 percent,12 although many limitations were noted, including missing data or information on the sample participants (Midgette and Kilmer, 2015). The program in North Dakota was found to have more of a deterrent effect on female repeat offenders than males, and the overall deterrent effect was strongest when the program had a mandatory 12-month enrollment period (Kubas et al., 2015).
Although not a 24/7 Sobriety program, a related Sobriety Tags pilot program has been implemented in London, United Kingdom, where ankle monitoring devices are being used for offenders who have committed crimes that can be attributed to the use of alcohol (Greater London Authority, 2016).
In this section, the committee reviews the evidence on the effectiveness of the 24/7 Sobriety Program and continuous alcohol monitoring devices. These are two examples of offender monitoring programs (DWI courts and ignition interlock devices also closely monitor offenders and are discussed elsewhere in this chapter). The 24/7 Program is targeted toward repeat or high-BAC DWI offenders. The PBTs, continuous alcohol monitoring devices, and other tests ensure a high probability of alcohol detection; immediate sanctions are enacted for failed tests. The 24/7 Sobriety Program analysis (Loudenburg et al., 2010) and peer-reviewed differences-in-differences study (Kilmer et al., 2013), both with large sample sizes, consistently found significantly reduced DWI recidivism among 24/7 Program participants; the differences-in-differences analysis by Nicosia et al. (2016) also identified a small reduction in all-cause adult mortality in South Dakota counties. There is also emerging, promising
___________________
12 The program was challenged in court for charging program fees to offenders as unconstitutional pretrial punishment, but the Montana Supreme Court upheld the program saying that the associated fees are not unconstitutional, and that judges must consider each case individually (i.e., prior alcohol-related arrests, risk to the community, financial standing) when determining whether to assign an offender to the program (State v. Spady, 2015 MT 218, 354 P.3d 590).
evidence from other states with large rural populations that have implemented 24/7 Sobriety Programs and alcohol consumption monitoring. However, the studies in this section report limitations such as failure to account for program fidelity, missing data, and reliance on aggregate analyses rather than individual-level data; additional research is needed using randomization or matched control groups to more completely assess the short- and long-term effects of the program among diverse jurisdictions and offenders.
Finding 5-1: The 24/7 monitoring program for high-risk offenders has been shown to be effective in some rural areas.
Conclusion 5-4: Systems alcohol monitoring programs are a promising intervention for reducing alcohol use and alcohol-impaired driving recidivism among high-risk offenders.
Successful implementation of these monitoring programs requires buy-in from law enforcement agencies and officials. Further investigation is required to see if similar programs could be implemented in other contexts.
Victim Impact Panels
Begun in 1982 by Mothers Against Drunk Driving (MADD), victim impact panels aim to reduce alcohol-impaired driving by exposing DWI offenders to the pain and suffering inflicted on victims of alcohol-impaired driving and their loved ones (Rojek et al., 2003). Victim impact panels follow a restorative justice model in which victims of alcohol-impaired driving and their loved ones are given the opportunity to speak about how the problem has affected their lives. The panels are not intended to condemn or shame audience members, nor are they a replacement for other sanctions (MADD, n.d.). Individuals convicted of alcohol-impaired driving, particularly first-time DWI offenders, are commonly court ordered to attend victim impact panels (AAA, 2016).
Evidence showing the effects of victim impact panels on alcohol-impaired driving and recidivism is mixed. While some studies have indicated that victim impact panels decrease recidivism, others have shown that recidivism rates are not significantly lower for those who attend victim impact panels than for those who do not. Much of the literature examining victim impact panels has not been updated; therefore, the following section presents the available evidence.
In a study measuring rearrest rates of DWI offenders who attended a victim impact panel in a southeastern county of the United States, 15.8 percent of offenders were rearrested over the following 5 years compared to 33.5 percent of the control group (Rojek et al., 2003). The analysis suggested that those who attended victim impact panels were 55.7 percent less likely to be rearrested and that victim impact panels were most effective in the first 2 years following arrest, after which their effectiveness decreased significantly. In an earlier study, rearrest rates during 0 to 6, 7 to 12, and 0 to 12 months after arrest were all found to be lower for those who attended a victim impact panel (Fors and Rojek, 1999). Differences in rearrest rates were most significant for white men, those between the
ages of 26 and 35, and those with one previous DWI arrest. The authors suggested that victim impact panels can be cost-effective in reducing rearrest rates of DWI offenders if implemented on a larger scale. An examination of a victim impact panel program in North Dakota demonstrated reduced odds of recidivism among male and female DWI offenders who participated when compared to those who did not. These findings were consistent for multiple DWI offenders (Joyce and Thompson, 2017).
Other studies have shown victim impact panels to be ineffective at reducing recidivism (C’de Baca et al., 2000; Crew and Johnson, 2011; Polacsek et al., 2001; Wheeler et al., 2002, 2004). Results of an unpublished randomized trial of convicted alcohol-impaired drivers in Bernalillo County, New Mexico, showed that victim impact panels potentially increased recidivism among those with multiple previous convictions, as the average number of subsequent convictions for those who attended a victim impact panel (1.81) was significantly higher than for those who did not (1.31) (Woodall et al., 2000). The average number of subsequent convictions for first-time DWI offenders who attended a victim impact panel in addition to DWI classes (0.87) was not significantly lower than for those who only attended DWI classes (1.09).
In a study of more than 2,000 DWI offenders in California and Oregon, recidivism rates following victim impact panel attendance were compared to rates in control groups of offenders matched by age and sex who were convicted of DWIs in the same states and in the same time periods (Shinar and Compton, 1995). Recidivism rates in the group that attended a victim impact panel were also compared with 683 offenders who were ordered to attend a panel but failed to show up. DWI offenders in Oregon who attended a victim impact panel had lower recidivism rates than those in their age-sex matched control group, but they did not have significantly different recidivism rates than those who were ordered to attend but failed to do so. However, DWI offenders in California who attended a victim impact panel did not have lower recidivism rates than those in the control groups and those who were ordered to attend but failed to do so. The authors noted, however, that analysis of more narrow age groups as well as by sex suggested that victim impact panels could be effective for DWI offenders aged 35 years and older.
A modified victim impact panel tailored to represent the local demographics of a community in New Mexico was also found to be ineffective. A randomized trial of first-time DWI offenders in San Juan County found that alcohol consumption, alcohol-impaired driving, and recidivism within 2 years were no different for those who attended a victim impact panel as part of a 28-day treatment program than for those in the treatment program who did not attend the panel (Wheeler et al., 2004). Nevertheless, San Juan County’s customized victim impact panel was not
found to increase the effectiveness of the treatment program in changing alcohol-impaired driving behavior among first-time DWI offenders.
Although attendees of victim impact panels often recall the experience as highly emotional, the emotional effect only seems to exert a temporary influence and is not influential enough to sustain long-term behavioral change (Lapham and England-Kennedy, 2012). Many court-ordered attendees have also reported that they felt out of place and/or burdened by attending a victim impact panel. Many also discounted the experience because they thought their own impaired driving was not bad enough to be responsible for a serious alcohol-impaired driving crash.
In summary, evidence on the effectiveness of victim impact panels with respect to reducing rearrest recidivism is mixed and needs to be updated. While a number of studies found victim impact panels to be effective at decreasing recidivism rates of DWI offenders (Fors and Rojek, 1999; Joyce and Thompson, 2017), particularly within the first 2 years after arrest (Rojek et al., 2003), several studies produced mixed results (Shinar and Compton, 1995) or found them to be ineffective (C’de Baca et al., 2000; Crew and Johnson, 2011; Polacsek et al., 2001; Wheeler et al., 2002, 2004). Based on its review of the available evidence, the committee offers the following finding:
Finding 5-2: While victim impact panels may have positive effects for victims and their families, the available evidence is insufficient to determine whether victim impact panels are effective in preventing alcohol-impaired driving recidivism.
Ignition Interlock Devices
An ignition interlock device is a breath alcohol analyzer that is connected to a vehicle’s ignition and requires the driver to provide a breath sample in order to start the vehicle’s engine (Marques and Voas, 2010; Sprattler, 2009). The device inhibits driving if the driver’s breath contains more than a preset alcohol concentration level, which is typically 0.02 g/dL or 0.02% (Goodwin et al., 2015). Interlocks generally have four basic features:
- breath alcohol sensor in the vehicle and a control unit under the hood;
- rolling retest system, which requires at least one retest once the trip is under way (for most interlocks, a retest is required every 20 to 30 minutes while driving);13
___________________
13 This feature can mitigate the potential harm associated with time to peak BAC. For example, if a driver’s BAC is ascending, but not yet at or above the limit set by the interlock,
- tamper-proof system for mounting the engine part of the unit with a system incorporated to detect attempts to bypass the interlock; and
- data-recording system that logs BAC results, tests compliance, and logs engine operation to determine if the offender is driving the vehicle regularly (Marques and Voas, 2010, p. 1).
Recent models of interlock devices feature an embedded camera, which takes the driver’s photograph when a breath sample is required. Facial imaging technology allows for better identification of the driver providing the breath sample (Voas, 2014) and helps prevent circumvention by having someone else provide a sample for an impaired driver. The use of ignition interlocks in the United States is generally managed in programs that are administered at the state level and aim to prevent alcohol-impaired driving recidivism among individuals arrested for alcohol-impaired driving.
History and legislation Interlock devices were first developed in the United States in 1969, and alcohol-detecting interlocks began to gain traction in the 1980s, when the public’s attention to the issue of impaired driving demanded solutions (AAMVA, 2015; Marques and Voas, 2010). The first national model standard for interlock devices was not issued until 1992 (Voas, 2014). The devices became more widespread once Congress passed legislation in 1998 that provided financial incentives to states that passed laws requiring interlocks for repeat offenders (AAMVA, 2015). More recently, the 2012 U.S. transportation reauthorization bill, Moving Ahead for Progress in the 21st Century Act, included incentives for states to pass and enforce mandatory interlock laws.14
While every state currently has some form of an ignition interlock law, the nature of the law, enforcement, structure, authority, and operational practices of the interlock programs vary (NCSL, 2016; NHTSA, 2013). For example, 30 states, the District of Columbia, and 4 counties in California require interlocks for all alcohol-impaired driving offenders, including first-time offenders (also called “all-offender” ignition interlock laws). Other states have different variations of interlock laws, including only requiring interlocks for repeat offenders and/or offenders with high BAC levels, mandatory interlocks for first-time offenders at the time of
___________________
then the vehicle may start after the driver provides a breath sample, but a retest would theoretically capture the driver’s peak or subsequent increased BAC and not allow further operation of the vehicle if it is above the limit. Best practices for retest requirements vary (see AAMVA, 2015).
14 Moving Ahead for Progress in the 21st Century Act, Public Law 112-141, 112th Cong. (July 6, 2012).
arrest (Illinois), or no requirements for first-time or repeat offenders (IIHS, 2017c). In some states where offenders are not required by law to install interlocks, there are still incentives for offenders to do so (e.g., avoiding a jail sentence) (Casanova-Powell et al., 2015). In Georgia, for example, first-time offenders are given the option of a limited driving permit if they install an ignition interlock, with the restriction that they can only drive to work, school, treatment, and monthly monitoring meetings (NCSL, 2016). These devices do not stop an offender from driving a car without the device installed. To help avoid this, in states such as Ohio and Oklahoma, the offender is required to obtain a specially marked driver’s license indicating that they can only drive a vehicle that is equipped with an interlock.
Additionally, state ignition interlock laws vary in the length of time for which offenders must have an ignition interlock device installed. For example, for a first offense, Arkansas requires 6 months with an ignition interlock, Arizona requires 12 months, and Delaware requires between 4 and 23 months (MADD, 2017). Comparatively, interlocks are not available for first-time offenders in Massachusetts (MADD, 2017). Ignition interlocks can also be purchased by anyone directly from the manufacturer, usually for voluntary personal use, for parents to monitor teen drivers, or for employers to install in company vehicles (Collier, 2013). A recent study conducted discussion groups with parents, teens, and young adults, as well as manufacturing and insurance companies, on the feasibility of using ignition interlocks to monitor young drivers (Kelley-Baker et al., 2017). All groups agreed that in order for ignition interlocks to be seen as a viable vehicle safety addition, they would first have to be destigmatized from their use as a punishment.
State interlock programs also vary in the extent to which compliance is monitored and how sanctions are tied to noncompliance. Evidence from a randomized controlled trial conducted in the state-wide ignition interlock program in Maryland (Zador et al., 2011), combined with evidence from multiple observation studies conducted in Texas (Marques et al., 2004, 2007) and Canada (Marques et al., 1998, 1999, 2000), indicates that dedicated monitoring can increase compliance with the requirements of an interlock program, and that increased compliance is associated with reductions in impaired driving recidivism after completing a period of interlock monitoring. Compliance is an important component of state interlock programs but is one that has received relatively little research attention in comparison to other program components.
Current use Interlock use in the United States has increased dramatically since the early 2000s. Installation of interlocks increased by about 15 percent per year from 2006 to 2012 (Marques and Voas, 2012). Since 2006
the number of interlocks in use has almost tripled, from 101,000 to about 318,714 in 2014 (Casanova-Powell et al., 2015; Roth, 2014). Despite this increase and the prevalence of ignition interlock laws and state monitoring programs throughout the country, research suggests that interlocks are underused relative to the number of eligible offenders. Goodwin et al. (2015) estimate a ratio of one installed interlock to five DWI arrests.
The interlock technology has also evolved over the past few decades, allowing for more accurate, frequent, and in-depth offender monitoring. While data from earlier models of interlocks were only available on a monthly basis, now interlock companies can provide daily and real-time data to monitoring agencies. The availability of GPS data also provides information on the offender’s driving patterns and location when a breath sample is being given (Voas, 2014).
Ignition interlocks can be administered through three general types of programs: administrative, judicial, and hybrid. Administrative programs are typically managed by state DMV agencies that require the ignition interlock installation as a condition of both licensing a suspended driver as well as of license reinstatement. These programs do not require a conviction. Judicial programs use the power of the court to mandate an interlock for an offender, either pretrial or post-conviction, and ensure program compliance. While administrative programs are managed uniformly throughout a jurisdiction, judicial programs allow the courts to have discretion and flexibility to tailor sanctions to program participants. Hybrid programs incorporate a combination of administrative and judicial requirements, which demand a great deal of coordination between judicial and administrative operations (AAMVA, 2015).
Fees for ignition interlocks are borne by the DWI offender. Offenders can pay approximately $65 to $90 per month for an interlock device, in addition to installation fees that can vary from $100 to $250 (Marques and Voas, 2010). Indigent funds are provided for low-income offenders based on specific unaffordability criteria in 30 states and Washington, DC (Goodwin et al., 2015; MADD, 2017); providing such funds in the states without them could help increase participation among low-income offenders there (Elder et al., 2011; Marques and Voas, 2010).
In 2013, NHTSA published a Model Guideline to State Ignition Interlock Programs, which provides practical strategies on key program features that are critical for effective delivery. These include legislation, education, program administration, and criminal and administrative sanctions (NHTSA, 2013). In 2015 the American Association of Motor Vehicle Administrators (AAMVA) published the Ignition Interlock Program Best Practices Guide, which provides recommendations for how ignition interlock programs should be administered, ranging from technical matters including alerts, device calibration, retests, and anti-circumvention measures including
cameras, to administrative matters including outlining program rules and the processes individuals must complete to participate (AAMVA, 2015).
Many countries outside the United States also use ignition interlocks including Australia, Belgium, Canada, Denmark, Finland, Ireland, the Netherlands, Sweden, and the United Kingdom (Martino et al., 2014; Schonfeld and Sheehan, 2004). In Sweden, alcohol-impaired driving offenders have the option of choosing between a 12-month license revocation and a 2-year alcohol ignition interlock program. A study found that those who chose the ignition interlock program were more likely to be relicensed 2 and 3 years after the DWI, had lower rates of harmful alcohol consumption, and were less likely to reoffend (Bjerre and Thorsson, 2008). Another study conducted in Québec, Canada, found that participation in their alcohol ignition interlock program reduced recidivism by 80 percent among first-time offenders during the first 12 months and by 74 percent among repeat offenders during the first 24 months (Vézina, 2002).
Evidence of interlocks as related to drinking and driving The benefits of ignition interlocks as they relate to the problem of drinking and driving have been evaluated with respect to several outcomes, including alcohol-impaired driving recidivism while devices are installed, alcohol-impaired motor vehicle crashes and crash fatalities while devices are installed, and alcohol-impaired driving after devices have been removed from drivers’ vehicles.
Considerable research has been dedicated to evaluating whether ignition interlocks have an impact on recidivism, defined as arrests for alcohol-impaired driving among individuals who have an ignition interlock device installed on their vehicle. The evidence from these studies is compelling and indicates that interlocks reduce alcohol-impaired driving recidivism by 50 to 90 percent while ignition interlock devices are installed (Beck et al., 1999; Bjerre, 2005; Casanova-Powell et al., 2015; Coben and Larkin, 1999; Fiedler et al., 2012; Roth et al., 2007; Willis et al., 2004). Also compelling, however, is the evidence that this effect is not observed among drivers after interlock devices are removed from drivers’ vehicles (Voas et al., 2016; Willis et al., 2004). Most of the studies evaluating how ignition interlocks relate to recidivism used observation designs. Many of those studies were subject to selection bias, as only subsets of offenders were included as interlock users rather than studying the effectiveness of interlocks among all individuals who are eligible for a given program (Willis et al., 2004). Also, based on the findings of their systematic review, Willis et al. (2004) note that some interlock programs are voluntary versus mandatory for offenders in a jurisdiction. Voas et al. (1999) note that interlock programs can only be effective to the extent that offenders participate. Hence, participation has implications both for how
research findings are interpreted and for whether interlock programs can be successful.
In 1991, Sweden was the first country to introduce ignition interlocks on commercial vehicles (buses, trucks, and taxis) on a voluntary basis (Bjerre and Kostela, 2008). A study found that the rates of alcohol-impaired driving were similar among professional drivers and general drivers and that although ignition interlocks prevented very few starts in commercial vehicles, the installation increased employer confidence in drivers (Bjerre and Kostela, 2008). A recent report released in Australia called for the universal use of ignition interlocks on commercial fleets and personal vehicles (Fitzharris et al., 2015). Ignition interlocks are not required on U.S. commercial vehicles or fleets, but they are available to interested employers, school districts, and public transportation officials (Intoxalock, n.d.). In 2017, two Rhode Island legislators sponsored a bill that would require ignition interlocks on all state school buses (O’Coin, 2017).
A separate matter is whether ignition interlocks affect alcohol-impaired driving crashes; a small number of studies have considered this outcome (Elder et al., 2011). Of these, a study in Sweden found decreased crashes in the interlock group compared to the control group, but there were low absolute numbers of crashes in both groups, limiting the interpretation of the findings (Bjerre, 2005; Elder et al., 2011). A study in California found that ignition interlocks installed on the vehicles of convicted drivers were effective at preventing alcohol-impaired driving crashes, but they were associated with increases in other types of crashes. However, this study found that interlocks appeared not to prevent alcohol-impaired driving crashes for first-time DWI offenders with high BAC levels (DeYoung et al., 2004). Another study analyzed relocating interlock order issuance to the driver licensing department from courts and expanding the ignition interlock requirement to first-time offenders with BACs below 0.15% in Washington (McCartt et al., 2013). The authors concluded that requiring interlocks for first-time offenders was associated with fewer reconvictions (despite low interlock use rates) and with reduced single-vehicle late-night crashes.
A recent study by Vanlaar et al. (2017) evaluated the ignition interlock program implemented in Nova Scotia to assess its effectiveness in reducing alcohol-impaired driving. The study was conducted by evaluating alcohol-impaired driving charges and convictions and fatal and serious crashes experienced by 929 offenders who had a voluntary or mandatory interlock device and a comparison group of 326 offenders who declined to participate in the interlock program and instead had their drivers’ licenses suspended for their revocation period. Over the course of approximately 12 months, the authors observed a conviction recidivism rate of 0.94 and 3.02 percent among the interlock-voluntary and interlock-mandatory
groups, respectively, compared to 8.93 percent among the control group, representing a 90 percent reduction in recidivism in the voluntary group and a 66 percent reduction in recidivism in the mandatory group. The recidivism rates increased to 1.89 percent in the voluntary group and 3.73 percent in the mandatory group after devices were removed from vehicles, but these rates were still lower than those observed among the control group. In addition to this evidence of a specific deterrent effect, the authors used an interrupted time series analysis and found evidence of a general deterrent effect among the entire population of Nova Scotia drivers, in the form of a temporary decrease in the number of alcohol-impaired driving charges (13.3 percent within the first month of the program) and the number of alcohol-impaired driving convictions (9.9 percent following the seventh month of program implementation). They also found a small but significant decrease in the number of fatal and serious-injury alcohol-impaired driving crashes. The authors concluded that the interlock program was more effective in preventing harm attributable to alcohol-impaired driving compared to what would have occurred had the interlock program not been implemented.
Barriers to implementing ignition interlock programs include delays to being eligible to install a device in one’s vehicle, low installation rates once individuals are eligible, and recidivism after devices are uninstalled. Ma et al. (2016) evaluated the Reduced Suspension with Ignition Interlock Conduct Review Program in Ontario, Canada. The program was implemented to change Ontario’s preexisting interlock policy, in which DWI offenders served at least a 12-month license suspension and then completed another 12 months with either an interlock or without driving at all, in an attempt to address these issues. The program shortened the license suspension period to 3 or 6 months if an offender agreed to install an interlock, followed by 9 or 12 months with the device installed. The new program also attempted to shorten the pretrial elapsed time and therefore required an “early” guilty plea within 90 days of the alcohol-impaired driving offense. Finally, the new program also included behavioral feedback and compliance-based removal to affect long-term recidivism rates. The authors analyzed records of first-time offenders (n = 30,200 in both the interlock installation and pretrial elapsed time investigations; n = 9,326 in the post-interlock recidivism assessments) from 2005 to 2014. The authors found positive effects of the incentive program on two outcomes of interest: interlock installation rates improved 54 percent and pretrial elapsed time shortened by 146 days. However, there was no positive effect on reoffense rate after interlocks were removed. The authors concluded ignition interlocks could be incentivized to bolster installation uptake.
Researchers have questioned whether integrating AUD treatment with ignition interlock programs could extend the effectiveness of these devices after their removal. Voas et al. (2016) studied a Florida policy that required AUD treatment for DWI offenders in an ignition interlock program. The program mandated treatment for offenders who committed three violations (a violation was defined as two lockouts within four hours). The authors conducted survival analyses to compare recidivism between offenders with multiple DWIs who received treatment while their vehicles had interlock devices (n = 640) and matched offenders not required to receive treatment while using interlocks (n = 806). In the 48 months after interlock removal, the DWI offenders who benefited from treatment experienced 32 percent lower recidivism compared to the offenders who did not receive treatment. AUD treatment of offenders was estimated to prevent 41 rearrests, 13 crashes, and 9 injuries from crashes among this group after interlock removal.
To the committee’s knowledge, no studies had investigated fatalities as outcomes in evaluations of ignition interlock programs or device installation until two such studies were published within the past 2 years. In 2016, Kaufman and Wiebe used a difference-in-differences design to compare U.S. states that introduced an all-offender ignition interlock law versus states that did not introduce such a law between 2004 and 2013. Eighteen states introduced an all-offender ignition interlock law during that period, making interlocks mandatory for all alcohol-impaired driving convictions. Evidence of an effect of the law was apparent 3 years after these laws were implemented, with an average alcohol-related crash death rate of 4.7 per 100,000 people in states with an all-offender interlock requirement, compared to a rate of 5.5 per 100,000 people in states without this requirement, suggesting an absolute reduction of 0.8 deaths per 100,000 people per year. The authors concluded that policies mandating ignition interlocks for all alcohol-impaired driving convictions were associated with 15 percent fewer alcohol-related driving fatalities; they estimated that 915 lives were saved in the universal interlock states during the period of study.
In 2016, McGinty et al. (2017) used a multilevel model to investigate the relationship between state ignition interlock laws and alcohol-impaired fatal crashes in the United States between 1983 and 2013. After accounting for between-state variation and autocorrelation within states over time, the authors found that state laws requiring interlocks for all alcohol-impaired driving convictions had a 7 percent lower rate of fatal crashes with a BAC greater than 0.08% and an 8 percent lower rate of fatal crashes with a BAC of at least 0.15%. The findings of this study, along with those of Kaufman and Wiebe (2016), provide evidence that
alcohol-impaired driving crash deaths are prevented through state all-offender ignition interlock laws.
Potential for primary prevention There are opportunities for more widespread implementation of ignition interlocks among offenders and nonoffenders. This has been a subject of discussion since the devices’ emergence as a prevention strategy. The use of ignition interlocks to prevent motor vehicle fatalities is not inherently limited to high-risk populations (i.e., people who have already been convicted of DWI). Public support, a major determinant of widespread implementation, has been studied as well. A nationally representative survey of the U.S. population revealed that 84 percent of participants supported mandating ignition interlocks for all convicted DWI offenders. In addition, if affordable, about 42 percent expressed interest in having advanced alcohol test technology in their vehicles (McCartt et al., 2010).15 See the section on cost-effectiveness data for information on the potential cost savings for interlocks in all new vehicles.
Bjerre (2005) describes a primary prevention pilot conducted in Sweden with three commercial transport companies (buses, trucks, and taxis). Professional drivers of commercial vehicles, as well as their employers and passengers, accepted ignition interlocks; interlocks as a primary prevention measure were reported to be quickly growing in Sweden at the time the 2005 article was written. Ultimately, the authors found the interlock stopped 3 of 1,000 ignition starts after the device detected a BAC above the lock point (and limit set by Swedish law) of 0.02%, providing some evidence of effectiveness.
Ignition interlock devices on motorcycles Opportunities to prevent alcohol-impaired driving crashes might be achieved through the use of ignition interlock devices on motorcycles. Motorcyclist fatalities, as a proportion of all traffic fatalities, increased from 11 percent in 2006 to 14 percent in 2015 (NCSA, 2016); there were 4,976 motorcyclist fatalities in 2015, which is the highest number since 2012 (NCSA, 2016). In 2011, 30 percent of motorcycle riders involved in fatal crashes had a BAC of 0.08% or higher, a proportion higher than for any other type of vehicle (NHTSA, 2017). NHTSA recently examined the feasibility of ignition interlocks for motorcycles by conducting interviews with ignition interlock manufacturers and installers, state officials, and motorcycle riders with interlocks installed on their motorcycles (NHTSA, 2017).
___________________
15 Of the other 58 percent of respondents, about 54 percent would not be interested in having such technology in their vehicles and 4 percent were undecided or refused to answer.
State laws vary on the extent to which motorcycles are addressed in operating standards for interlocks. For example, some states require DWI offenders who are owners of motorcycles to equip them with an interlock, other states disallow interlocks, and other states have laws that require motorcycle owners to install motorcycle interlocks but do not enforce them. Two interlock manufacturing companies currently permit their devices to be installed on motorcycles (NHTSA, 2017). These devices are designed for use on motor vehicles other than motorcycles, but they can be installed to work adequately on a motorcycle. A number of issues pose challenges for this practice, including exposure to weather and vibration, secure storage, power draw on the battery, and circumvention potential (NHTSA, 2017). A particular challenge with implications for safety is the requirement for performing retests while the motorcycle is being operated. These technical challenges can be overcome, however. NHTSA estimates that motorcycle interlocks likely represent less than 0.1 percent of all interlocks in service (NHTSA, 2017). However, interlock manufacturers reported being willing to install interlocks on motorcycles and to work on adapting or developing new technology for this purpose if states require a motorcycle option for interlocks in their laws.
Cost-effectiveness studies for ignition interlock devices Studies on ignition interlock devices can be divided into two types: studies that examine mandatory interlock device policies for high-risk offenders, and those that aim to predict the effect of mandating interlock devices on all new cars. The former typically involves an alcohol-impaired driving crash and a court mandating that the high-risk driver install an interlock device instead of a court-mandated fine and/or jail time. Also, the former can be studied with real-world data as several states have implemented such policies.
Studies on current interlock programs tend to find them to be cost-effective, but care needs to be taken in observing which costs are included. Interlock devices save the public $3 to $7 on every $1 spent on the devices for DWI offenders, and are cost-effective for this population (MADD, 2013). Similarly, a study of mandatory interlocks in New Mexico (Roth et al., 2007) found that the benefits of requiring interlocks for first offense is cost-effective, finding a $3 benefit (cost savings) for $1 spent for this population. First-time offenders are a high-risk population who might more easily be deterred from future offenses, when compared to repeat offenders. Ullman (2016) also focuses on first-time offenders, noting that interlock programs can prevent alcohol-impaired driving and crashes and provide benefits to society, especially when offenders bear the costs of installation and maintenance.
There are several studies that predict a universal ignition interlock policy would be cost-effective. A study by Carter et al. (2015) modeled the cost savings of interlock devices installed in new vehicles in the United States. The study predicted that, over a span of 15 years, 59,554 fatalities would be prevented and approximately 1.25 million injuries averted. The study further predicted that injury-related savings would outweigh the cost of device installation after 3 years, with savings related to fatal and nonfatal injuries estimated to be $342 billion over the 15-year time span. The study concluded that interlock devices are cost-effective in reducing alcohol-impaired driving crashes, most notably among drivers ages 21 to 29.
An Australian study by Lahausse and Fildes (2009) estimated that benefit-cost ratios for interlock devices can range between 0.6:1 and 3.4:1, depending on various factors including discount rates and time horizon. However, because effectiveness rates are not known, the authors assumed several different levels instead. Not surprisingly, the higher assumed level of effectiveness appeared to be cost-effective, while the lower level was not. This means that the results are rather speculative and may not be applicable to U.S. policy, as it was based in Australia and the alternative effectiveness rates were hypothesized and then compared.
In summary, there are relatively few studies examining the cost-effectiveness of interlock devices. The suggestive evidence is that requiring interlock devices for those arrested for alcohol-impaired driving, and specifically first-time offenders, is likely cost-effective. This conclusion is supported by evaluations of cost-effectiveness of implemented programs. However, there is some uncertainty in this conclusion, and more studies are needed.
The findings are less clear for universal ignition interlock devices on all new cars. These studies are necessarily hypothetical; the price of implementing these devices in the future is unknown. It is reasonable to think that requiring interlock devices for those identified as high risk for alcohol-impaired driving (e.g., arrested) would be more cost-beneficial for society when compared to requiring universal interlock devices and their payment even though only some devices would be used to prevent alcohol-impaired driving. The price is an important unknown factor. In contrast, the advantages of universal ignition interlock are that all high-risk individuals would be subject to the interlock whether they have been caught by law enforcement or not. Furthermore, there would be more alcohol-impaired driving prevention, and costs of law enforcement requiring implementation of interlock would be averted.
Conclusions This section provides a considerable body of research from the United States and other countries that have investigated ignition interlock laws and programs and their effects on alcohol-impaired driving
recidivism and related harm. There is strong evidence that individuals convicted of alcohol-impaired driving who have an interlock installed on their vehicle are less likely than others to be rearrested for alcohol-impaired driving or to crash while the device is installed. Evidence from a Cochrane systematic review including only randomized controlled trials and controlled trials also suggests that the benefits of an ignition interlock cease once the device is removed from a vehicle; additional randomized controlled trials are needed as nonrandomized studies do not adequately control for selection bias (Willis et al., 2004). Elder et al. (2011) used the Community Guide methodology to synthesize the research from the Cochrane review, in addition to four other studies, and found strong evidence for ignition interlocks’ effectiveness to reduce rearrest rates while interlocks are installed. As a result, the Community Preventive Services Task Force concludes that increased and sustained use of interlocks could significantly affect the rate of alcohol-related crashes. However, findings from at least one study suggest a benefit may be gained by pairing an ignition interlock program with a treatment program for AUD (Voas et al., 2016). States that have introduced all-offender ignition interlock laws appear to have experienced reductions in alcohol-related motor vehicle crash deaths (Kaufman and Wiebe, 2016). It is worth noting that there is evidence suggesting ignition interlock laws have general, as well as specific, deterrent effects. Given strong scientific evidence that individuals convicted of alcohol-impaired driving who have an interlock installed on their vehicle are less likely than others to be rearrested for alcohol-impaired driving or to crash while the device is installed, the committee finds ignition interlocks to be a beneficial technological intervention for reducing alcohol-impaired driving. This technology is affordable for many individuals, and made affordable for others through indigent funds for low-income offenders.
Recommendation 5-3: All states should enact all-offender ignition interlock laws to reduce alcohol-impaired driving fatalities. An ignition interlock should be required for all offenders with a blood alcohol concentration (BAC) above the limit set by state law. To increase effectiveness, states should consider increased monitoring periods based on the offender’s BAC or past recidivism.
Current monitoring periods vary by state. The monitoring period ranges from a minimum of 6 months (for example, Delaware and South Carolina) for a first offense to 2 to 5 or more years for second, third, and subsequent offenses (for example, Alabama, New Mexico, and Washington) (NCSL, 2016). Evidence indicates that a minimum monitoring period
of 2 years is effective for a first offense and 4 years for a second offense, such as the ignition interlock programs administered in Alabama, Illinois, Oklahoma, and Washington. The law should not have a BAC minimum. Furthermore, given the effectiveness of ignition interlock devices in reducing recidivism, additional research and development into the use of these devices for motorcycles is needed because of the high rates of alcohol-impaired driving fatalities for motorcyclists. Based on the limitations of ignition interlocks (e.g., dissipating effects after removal) and in light of the research that indicates most crash fatalities involve drivers who have never been convicted of a DWI, there is a need to integrate alcohol detection technology in all vehicles (see Chapter 4 for a discussion of the Driver Alcohol Detection System for Safety, a passive alcohol detection system for vehicles).
Education and Training of Law Enforcement and Judicial System Experts
For interventions related to law enforcement and the judicial system to be successful, it is important for those on the front lines to have adequate training and education on alcohol impairment, the law, and options during the adjudication process. Prosecutors can regularly be at a disadvantage during DWI cases because retained defense counsel is usually well funded, resource rich, and highly knowledgeable (AAA, 2016), and prosecutors assigned to DWI cases are often newer and less practiced. In fact, almost half of DWI prosecutors in one survey described insufficient training for DWI prosecution before trying cases, and 94 percent reported wanting additional training (Robertson and Simpson, 2002). Inadequate preparation can affect the outcome of a DWI case (Robertson and Simpson, 2002). Therefore, all prosecutors would benefit from training regarding the development of SFSTs, operation and certification procedures for breath-testing devices, toxicology testing and expert testimony, and procedures and protocols for blood and urine testing to determine BAC. State traffic safety resource prosecutors can be used to create and conduct trainings on these issues. Training courses and other educational resources including technical and trial assistance are also available through the National District Attorneys Association’s National Traffic Law Center on topics such as alcohol and drug toxicology, the admission of scientific evidence, and cross-examination of expert witnesses (NDAA, n.d.).
Law enforcement officers are the first to interact with impaired drivers as they make observations on roads and highways. As discussed earlier in this chapter, many of the procedures they regularly perform are essential elements in apprehending and processing an alcohol-impaired driver. Administering SFSTs; accurately assessing drivers based on observations of their driving behavior, speech, demeanor, and appearance;
administration of a breath test; collection of urine or blood for analysis; training on alcohol-related laws (Ramirez, 2017); and other evidence collection provide the basis for how DWI cases will move through the criminal justice system (Shrum, 2017; Woodward, 2017). Because of these crucial roles, timely training and education is important. The National Traffic Law Center also has courses and educational materials available to law enforcement officials involved in DWI cases (NDAA, n.d.).
Judges overseeing alcohol-impaired driving cases need to be knowledgeable about how impaired drivers proceed through the justice system and challenges confronting the judiciary in these cases (AAA, 2016; Shrum, 2017). For example, education for judges could include the signs and symptoms of impairment and the history and protocol regarding administration of the SFSTs by law enforcement officers. Additional education needs to center on how the scientific evidence is collected from the driver, on the operation and certification procedures for breath-testing devices, and on the procedures and protocols for blood and urine testing to determine BAC, the results of which may be submitted during a trial. In terms of post-conviction sanctions, judges could also receive education regarding the full range of effective treatment options for repeat offenders and for those with AUD (including the use of SBIRT, therapy, and medications). The National Judicial College offers training to traffic court judges, magistrates, and hearing officers and could be an important partner for expanding and disseminating the needed knowledge to judges (The National Judicial College, n.d.). State and regional judicial outreach liaisons can also be mobilized to create and conduct trainings on these issues.
Clinical staff who provide assessments of offenders and offer treatment suggestions to judges need to be aware of the various effective treatment options. Training for clinicians can include screening for alcohol and/or other drug use, identifying AUD, identifying binge drinking and the relationship of that behavior to alcohol-impaired driving fatalities and injuries, and implementing prevention strategies in the clinical setting.
Given the central role of law enforcement officers and the judicial system experts described above, as well as the Robertson and Simpson (2002) survey, agreement from national organizations (AAA, 2016; Goodwin et al., 2015; The National Judicial College, n.d.; NDAA, n.d.), and in large part based on information gathered during committee meetings (Ramirez, 2017; Shrum, 2017; Woodward, 2017) and committee expertise on this topic, the committee concludes:
Conclusion 5-5: To enhance the effectiveness of alcohol-impaired driving interventions, systematic and ongoing training of professionals in law enforcement, prosecution, the judiciary, clinicians, and public health is needed.
Law Enforcement Activities
As discussed throughout Chapters 3–5, law enforcement and the criminal justice system play a vital role in preventing alcohol-impaired driving fatalities in every phase outlined in the report’s conceptual framework (from precrash to postcrash). However, if supportive policies are not in place or data are not available to help target interventions, the effectiveness of enforcement activities and the ability to take a comprehensive approach to addressing alcohol-impaired driving becomes hampered.
Conclusion 5-6: With respect to DWI prevention and enforcement, the criminal justice and legal systems need to have supportive policies and resources at their disposal to do the following: publicize laws or enforcement activities, permit and conduct sobriety checkpoints, conduct other enforcement activities, administer preliminary breath tests, have strong penalties for refusal to take alcohol tests when warranted, conduct investigations, prosecute and adjudicate criminal charges to the fullest extent of the law (i.e., to reduce pleading down to lesser charges), access data monitoring systems to track and report outcomes of DWI-related charges, access place-of-last-drink data to prioritize enforcement activities, and use Alcoholic Beverage Control Commission enforcement agents to assist in conducting enforcement activities and compliance of alcohol licensees.
IMPROVING EMERGENCY MEDICAL AND TRAUMA SYSTEM SERVICES
Surviving injuries and minimizing the harm of crashes from alcohol-impaired driving require receiving definitive trauma care quickly (MacKenzie et al., 2006). Care in a designated level I or level II trauma center can reduce mortality by 25 percent in patients with severe injuries when compared with care in a nontrauma center hospital (MacKenzie et al., 2006). Alcohol-related crashes that occur in rural areas pose a particular concern given that crashes can occur in remote areas with less access to trauma center care. Using data from the 2000 Census and the 2005 American Hospital Association (AHA) annual survey, Hsia and Shen (2011) found two-thirds of Americans in urban areas have easy access to trauma centers (defined in the study as within 10 miles), compared to 24 percent of people living in rural areas. Furthermore, about one-third of Americans in rural areas have difficult access to trauma centers (defined as more than 30 miles away), compared to 12 percent of urban populations. Additionally, increased notification and response times of emergency care (Gonzalez et al., 2009) can lead to more severe disability after
injury (Sihler and Hemmila, 2009) and an increased number of fatalities (Muelleman et al., 2007; Zwerling et al., 2005).
As of 2010, the last year data are available, only 5 percent of the U.S. land area and 64 percent of the U.S. population could access a level I or level II trauma center by ground ambulance within 60 minutes of injury (Carr and Branas, n.d.). Increasing geographical access to trauma centers by locating new air medical helicopter services in rural and other under-covered areas could help reduce alcohol-impaired driving crash fatalities (Branas et al., 2013; Brown et al., 2017; Schiller et al., 2009). If existing air medical transport is used, 35 percent of U.S. land area and 90 percent of the U.S. population could access a level I or level II trauma center within 60 minutes of injury (Carr and Branas, n.d.).
Rural Areas
Delays to emergency care in rural areas may be increasing given that over the past several decades rural hospitals have been closing at a rapid rate (Pines and Ernst, 2017). Trauma centers are often safety-net hospitals, treating disproportionately high volumes of patients with Medicaid or no insurance and as a result are often underfunded, owing to poor reimbursement for their provision of lifesaving but expensive care. Because of this, many trauma center closures have occurred over the last 20 years (Hsia and Shen, 2011). As noted earlier, motivation for treatment of problematic drinking is often lacking. Time in the trauma center may be an opportunity for an offender with a history of problematic drinking to receive counseling and connection to a treatment program for AUD.
Emergency medical services (EMS) coverage and response, as well as geographical access to trauma centers, is especially challenging in rural tribal areas (Dernocoeur, 1988). This is likely a contributor to the disparities in fatal crash rates among American Indian/Alaska Native (AI/AN) populations. The AHA Task Force on Ensuring Access in Vulnerable Communities recommends several strategies to improve the capacity of the Indian Health Service (IHS) to provide care to AI/AN communities. These recommendations include ensuring technical expertise so IHS facilities can gain appropriate federal reimbursements, strengthening partnerships among IHS and non-IHS facilities to enhance coordination of care, and increasing IHS funding (AHA, 2017).
Coordinated efforts are needed to improve access to emergency and trauma care for individuals injured in alcohol-impaired driving crashes in rural areas. Some such efforts are described below. The National Cooperative Highway Research Program Guide for Enhancing Rural Emergency Services identifies four objectives (see bullets below) for improving emergency medical services in rural areas. Each objective is linked with a
number of strategies that can be pursued by local decision makers based on their level of need and resources.
- Integrate services to enhance emergency medical capabilities.
- Provide or improve management and decision-making tools.
- Provide better education opportunities for rural EMS.
- Proven strategy: Use technology-based instruction for rural EMS training.16
- Reduce time from injury to appropriate definitive care (TRB, 2005b, p. I-1).
Partnering Emergency Medicine and Primary Care
Many rural hospitals and EDs serve as rural patients’ source of primary care; these hospitals are often staffed by primary care and emergency medicine practitioners who can provide care in both disciplines. As rurality increases, a patient is seven times more likely to be treated by a primary care practitioner in an ED (versus an emergency physician). Rural health needs can be met by developing a partnership between primary care and emergency medicine in these areas (Greenwood-Ericksen et al., 2017). For example, a hospital leadership team in a rural county in North Carolina recently rebuilt their facility around “a community-focused care model” (Greenwood-Ericksen et al., 2017, p. 641). The new facility includes a primary care clinic, space for specialists, and an ED with a trauma room; there is no separation between components as all patient rooms are grouped in one bay. A physician assistant and ED nurse screen incoming patients so they can best direct them, and the facility employs patient navigators to help with coordinating care. The flexible care delivery supports the community, patients, and providers.
Mueller et al. (2014) conducted a systematic review to assess published tele-emergency models and their associated outcomes. The authors evaluated a large, Midwestern tele-emergency service through a survey sent to all 71 participating hospitals in addition to site visits and telephone interviews. The authors found tele-emergency services effectively enhance clinical quality by broadening and coordinating the clinical care team and amplifying available resources during events, which help reduce time to care. These attributes foster patient-centered care and help maintain rural hospitals’ patient bases while increasing family physician recruitment and retention. The study also found regulatory barriers to tele-emergency use such as varying reimbursement policies and cross-state licensure
___________________
16 This strategy is the only one listed in the report that is marked as “proven” (i.e., evidence based).
issues. Payment systems related to outcomes, rather than volume, such as value-based systems, could help alleviate these challenges and expand tele-emergency services.
Freestanding Emergency Centers
Unlike urgent care centers, freestanding emergency centers (either independent or as a hospital satellite of a regional health system) are full-service EDs that may provide a practical solution to the problem of decreasing time to treatment in rural settings in the context of the United States having experienced so many rural hospital closures (Pines and Ernst, 2017). Rural communities may not provide adequate demand for inpatient care and therefore may not be able to sustain a full hospital. Alternatively, freestanding emergency centers have a lower cost structure and higher patient volume, and facilitate sharing of electronic medical records and imaging, as well as faster transfers of those patients who need additional specialty or trauma care. Correctly triaging patients and improving interhospital transfer is important (Haas et al., 2010, 2012), as one study found that patients who were not transferred to trauma centers from nontrauma EDs but should have been were at risk of getting insufficient trauma care (Delgado et al., 2014).
Technological Advances
Automated crash notification (ACN), a vehicle safety technology designed to notify emergency responders of a crash and its location, has been shown to reduce crash to notification times to 1 minute or less, potentially reducing overall response time (Lahausse et al., 2008). It is estimated that a fully implemented ACN system in the United States could save between 400 and 1,600 lives per year by improving EMS response times (Clark and Cushing, 2002).
Advanced automatic crash notification (AACN) builds on the concept of ACN by including more detailed crash data, such as changes in speed, seat belt use, air bag deployment, and direction of impact, to provide an understanding of crash severity; however, data on how AACN affects patient outcomes are not yet available (TRB, 2013b).
Data Linkage
Samra et al. (2014) evaluated the rural transportation system components in South Dakota as they relate to EMS and ultimately recommended linking EMS data with crash data to “predict service
delivery more accurately and establish more specific, data-driven, and performance-based measures” (p. 25).
Beyond improving EMS response times, improving the systems of care for seriously injured crash victims would benefit from the development of a national, learning trauma system, as outlined in an NASEM report on the national trauma care system (NASEM, 2016). The report concluded that, despite past recommendations, the United States lacks a governmental civilian health lead agency for prehospital, in-hospital, and post-acute trauma care. Such leadership is needed to support a learning system for trauma care at the national level. The report recommended that
the White House should lead the integration of military and civilian trauma care to establish a national trauma care system. This initiative would include assigning a locus of accountability and responsibility that would ensure the development of common best practices, data standards, research, and workflow across the continuum of trauma care. (NASEM, 2016, pp. 16–17)
A critical role would be to enable the linking of current data sources (crash, EMS, nontrauma center and trauma center hospital discharge data, and longitudinal postdischarge data such as death certificates) in order to measure and improve system outcomes. Identifying best practices and learning from successes and failures, particularly in rural areas, has the potential to save lives from alcohol-impaired driving crashes as well as other traffic crashes. Trauma centers could be engaged to reduce time to care for rural areas.
This section reviews some of the challenges rural regions face in confronting alcohol-impaired driving fatalities, including longer distances to trauma centers and hospital closures. Several organizations (e.g., the National Cooperative Highway Research Program and the National Academies of Sciences, Engineering, and Medicine) have drawn attention to these issues and made recommendations to integrate services. Emergency response and trauma system improvement is a promising intervention for rural communities, which is particularly important given the large proportion of alcohol-impaired fatalities that occur there and because many other interventions in this report may be more relevant to urban areas. For example, Greenwood-Ericksen et al. (2017) provide a compelling example of how rural hospitals can effectively partner emergency medicine with primary care, and the Mueller et al. (2014) systematic review and survey illustrate ways in which tele-emergency services can positively affect rural health systems. As explained above, the United States lacks a national trauma care system that effectively integrates successful learning system processes from military settings with civilian trauma care; the National Academies report recommended that the White
House lead this effort (NASEM, 2016). Data linkage is a key component in reducing rural alcohol-impaired driving fatalities. Therefore, the committee concludes:
Conclusion 5-7: A coordinated and continuous learning trauma care system is lacking in the United States. Facilitating the linkage of crash, EMS, and hospital data to generate insights on areas for improvement in addition to greater coordination could substantially affect the number of deaths from alcohol-impaired driving, particularly in rural and tribal areas owing to longer response times to crashes and increased distances from trauma care facilities.
REFERENCES
AA (Alcoholics Anonymous). 2017. What is A.A.? https://www.aa.org/pages/en_US/what-is-aa (accessed October 3, 2017).
AA. n.d. The twelve steps of Alcoholics Anonymous. https://www.aa.org/assets/en_US/smf-121_en.pdf (accessed October 3, 2017).
AA World Services Inc. 1984. This is A.A.: An introduction to the A.A. recovery program. New York: Alcoholics Anonymous World Services, Inc.
AAA (American Automobile Association). 2016. DUI justice link: A resource to help reduce substance-impaired driving. http://duijusticelink.aaa.com/wp-content/uploads/2016/11/Bench-Book.pdf (accessed December 9, 2017).
AAA Foundation for Traffic Safety. 2016. Driver licensing policies and practices. http://lpp.seniordrivers.org/index.cfm?selection=reportingdrs1&orderby= (accessed June 2, 2017).
AAMVA (American Association of Motor Vehicle Administrators). 2015. Ignition interlock program: Best practices guide. Arlington, VA: American Association of Motor Vehicle Administrators.
Aboelata, M., E. Yanez, and R. Kharrazi. 2017. Vision Zero: A health equity road map for getting to zero in every community. Los Angeles, CA: Prevention Institute.
ACEP (American College of Emergency Physicians). n.d. Alcohol screening and brief intervention in the ED. https://www.acep.org/Clinical---Practice-Management/Alcohol-Screening-and-Brief-Intervention-in-the-ED/#sm.0001k2vlbre0odbbru92379zdg78p (accessed November 27, 2017).
Agerwala, S. M., and E. F. McCance-Katz. 2012. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs 44(4):307–317.
AHA (American Hospital Association). 2017. Emerging strategies to ensure access to health care services. http://www.aha.org/content/17/stategies-to-ensure-access.pdf (accessed October 10, 2017).
Ait-Daoud, N., R. J. Malcolm, and B. A. Johnson. 2006. An overview of medications for the treatment of alcohol withdrawal and alcohol dependence with an emphasis on the use of older and newer anticonvulsants. Addictive Behaviors 31(9):1628–1649.
AMERSA (Association for Medical Education and Research in Substance Abuse). n.d. Project Mainstream. https://amersa.org/resources/educational-resources/project-mainstream (accessed November 27, 2017).
Anton, R. F., S. S. O’Malley, D. A. Ciraulo, R. A. Cisler, D. Couper, D. M. Donovan, D. R. Gastfriend, J. D. Hosking, B. A. Johnson, J. S. LoCastro, R. Longabaugh, B. J. Mason, M. E. Mattson, W. R. Miller, H. M. Pettinati, C. L. Randall, R. Swift, R. D. Weiss, L. D. Williams, and A. Zweben. 2006. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The combine study: A randomized controlled trial. JAMA 295(17):2003–2017.
APIS (Alcohol Policy Information System). 2016. Health care services and financing: Health insurance: Losses due to intoxication (“UPPL”). https://alcoholpolicy.niaaa.nih.gov/Insurers_Liability_for_Losses_Due_to_Intoxication_UPPL.html (accessed June 9, 2017).
APRI (American Prosecutors Research Institute). 2003. Alcohol toxicology for prosecutors: Targeting hardcore impaired drivers. Alexandria, VA: American Prosecutors Research Institute.
Ballesteros, J., J. C. Duffy, I. Querejeta, J. Ariño, and A. González-Pinto. 2004. Efficacy of brief interventions for hazardous drinkers in primary care: Systematic review and meta-analyses. Alcoholism: Clinical and Experimental Research 28(4):608–618.
Beck, K. H., W. J. Rauch, E. A. Baker, and A. F. Williams. 1999. Effects of ignition interlock license restrictions on drivers with multiple alcohol offenses: A randomized trial in Maryland. American Journal of Public Health 89(11):1696–1700.
Beich, A., T. Thorsen, and S. Rollnick. 2003. Screening in brief intervention trials targeting excessive drinkers in general practice: Systematic review and meta-analysis. BMJ 327(7414):536–542.
Berning, A., R. Compton, M. Vegega, D. Beirness, J. Hedlund, R. Jones, and J. Nichols. 2008. Refusal of intoxication testing: A report to Congress. DOT HS 811 098. Washington, DC: National Highway Traffic Safety Administration.
Bernstein, E., D. Topp, E. Shaw, C. Girard, K. Pressman, E. Woolcock, and J. Bernstein. 2009. A preliminary report of knowledge translation: Lessons from taking screening and brief intervention techniques from the research setting into regional systems of care. Academic Emergency Medicine 16(11):1225–1233.
Bertholet, N., J.-B. Daeppen, V. Wietlisbach, M. Fleming, and B. Burnand. 2005. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Archives of Internal Medicine 165(9):986–995.
Bewick, B. M., K. Trusler, M. Barkham, A. J. Hill, J. Cahill, and B. Mulhern. 2008. The effectiveness of web-based interventions designed to decrease alcohol consumption—A systematic review. Preventive Medicine 47(1):17–26.
Bjerre, B. 2005. Primary and secondary prevention of drink driving by the use of alcolock device and program: Swedish experiences. Accident Analysis & Prevention 37(6):1145–1152.
Bjerre, B., and J. Kostela. 2008. Primary prevention of drink driving by the large-scale use of alcolocks in commercial vehicles. Accident Analysis & Prevention 40(4):1294–1299.
Bjerre, B., and U. Thorsson. 2008. Is an alcohol ignition interlock programme a useful tool for changing the alcohol and driving habits of drink-drivers? Accident Analysis & Prevention 40(1):267–273.
Blankers, M., M. W. Koeter, and G. M. Schippers. 2011. Internet therapy versus Internet self-help versus no treatment for problematic alcohol use: A randomized controlled trial. Journal of Consulting and Clinical Psychology 79(3):330–341.
Block, A. 2016. Survey of DWI courts. DOT HS 812 283. Washington, DC: National Highway Traffic Safety Administration.
Bootsma, H., F. Coolen, A. Aldenkamp, J. Arends, L. Diepman, J. Hulsman, D. Lambrechts, L. Leenen, M. Majoie, and A. Schellekens. 2004. Topiramate in clinical practice: Long-term experience in patients with refractory epilepsy referred to a tertiary epilepsy center. Epilepsy & Behavior 5(3):380–387.
Branas, C. C., C. S. Wolff, J. Williams, G. Margolis, and B. G. Carr. 2013. Simulating changes to emergency care resources to compare system effectiveness. Journal of Clinical Epidemiology 66(8 Suppl):S57–S64.
Bray, J. W., F. K. Del Boca, B. G. McRee, S. W. Hayashi, and T. F. Babor. 2017. Screening, brief intervention and referral to treatment (SBIRT): Rationale, program overview, and cross-site evaluation. Addiction 112(Suppl 2):3–11.
Brewer, C., R. J. Meyers, and J. Johnsen. 2000. Does disulfiram help to prevent relapse in alcohol abuse? CNS Drugs 14(5):329–341.
Brinkmann, B., J. Beike, H. Köhler, A. Heinecke, and T. Bajanowski. 2002. Incidence of alcohol dependence among drunken drivers. Drug and Alcohol Dependence 66(1):7–10.
Brown, J. B., M. R. Rosengart, T. R. Billiar, A. B. Peitzman, and J. L. Sperry. 2017. Distance matters: Effect of geographic trauma system resource organization on fatal motor vehicle collisions. Journal of Trauma and Acute Care Surgery 83(1):111–118.
Brown, T. G., M. Dongier, M. C. Ouimet, J. Tremblay, F. Chanut, L. Legault, N. Y. Kin, and N. M. Kwong. 2010. Brief motivational interviewing for DWI recidivists who abuse alcohol and are not participating in DWI intervention: A randomized controlled trial. Alcoholism: Clinical and Experimental Research 34(2):292–301.
Burton, R., C. Henn, D. Lavoie, R. O’Connor, C. Perkins, K. Sweeney, F. Greaves, B. Ferguson, C. Beynon, A. Belloni, V. Musto, J. Marsden, and N. Sheron. 2016. A rapid evidence review of the effectiveness and cost-effectiveness of alcohol control policies: An English perspective. The Lancet 389(10078):15–21.
Carey, K. B., L. A. Scott-Sheldon, M. P. Carey, and K. S. DeMartini. 2007. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors 32(11):2469–2494.
Carey, S. M., B. E. Fuller, K. Kissick, E. Taylor, and P. Zold-Kilbourn. 2008. Michigan DUI courts outcome evaluation: Final report. Portland, OR: NPC Research.
Carmen, B., M. Angeles, M. Ana, and A. J. María. 2004. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: A systematic review. Addiction 99(7):811–828.
Carnegie, M. A., M. K. Gomel, J. B. Saunders, H. Britt, and L. Burns. 1996. General practice receptionists’ attitudes and beliefs towards preventive medicine before and after training and support interventions. Family Practice 13(6):504–510.
Carr, B. G., and C. C. Branas. n.d. Traumamaps.org trauma center maps. http://www.traumamaps.org (accessed October 10, 2017).
Carter, P. M., C. A. C. Flannagan, C. R. Bingham, R. M. Cunningham, and J. D. Rupp. 2015. Modeling the injury prevention impact of mandatory alcohol ignition interlock installation in all new US vehicles. American Journal of Public Health 105(5):1028–1035.
Casanova-Powell, T., J. Hedlund, W. Leaf, and J. Tison. 2015. Evaluation of state ignition interlock programs: Interlock use analyses from 28 states, 2006–2011. Washington, DC: National Highway Traffic Safety Administration.
Cavaiola, A. A., and C. Wuth. 2014. Assessment and treatment of the DWI offender, edited by B. Carruth. New York: Routledge.
Cavaiola, A. A., D. B. Strohmetz, J. M. Wolf, and N. J. Lavender. 2003. Comparison of DWI offenders with non-DWI individuals on the MMPI-2 and the Michigan alcoholism screening test. Addictive Behaviors 28(5):971–977.
CDC (Centers for Disease Control and Prevention). 2017. Impaired driving: Get the facts. https://www.cdc.gov/motorvehiclesafety/impaired_driving/impaired-drv_factsheet.html (accessed January 30, 2017).
C’de Baca, J., S. C. Lapham, S. Paine, and B. J. Skipper. 2000. Victim impact panels: Who is sentenced to attend? Does attendance affect recidivism of first-time DWI offenders? Alcoholism: Clinical and Experimental Research 24(9):1420–1426.
Center for Substance Abuse Treatment. 1995. Substance abuse treatment for adults in the criminal justice system. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Center for Substance Abuse Treatment. 2009. Chapter 3 Disulfiram. In Incorporating alcohol pharmacotherapies into medical practice. Vol. 49. Rockville, MD: Substance Abuse and Mental Health Services Administration.
Chamorro, A. J., M. Marcos, J. A. Mirón-Canelo, I. Pastor, R. González-Sarmiento, and F. J. Laso. 2012. Association of µ-opioid receptor (OPRM1) gene polymorphism with response to naltrexone in alcohol dependence: A systematic review and meta-analysis. Addiction Biology 17(3):505–512.
Chang, I., S. C. Lapham, J. C’de Baca, and J. Davis. 2001. Alcohol use inventory: Screening and assessment of first-time driving-while-impaired offenders. II. Typology and predictive validity. Alcohol and Alcoholism 36(2):122–130.
Chang, I., C. Gregory, and S. C. Lapham. 2002. Review of screening instruments and procedures for evaluating DWI [driving while intoxicated/impaired] offenders. Washington, DC: AAA Foundation for Traffic Safety.
Chezem, L. 2005. Legal barriers to alcohol screening in emergency departments and trauma centers. Lafayette, IN: Purdue University.
Circuit Court of the State of Oregon. n.d. DISP participant handbook. Portland, OR: Multnomah County Courthouse.
Clark, D. E., and B. M. Cushing. 2002. Predicted effect of automatic crash notification on traffic mortality. Accident Analysis & Prevention 34(4):507–513.
Coben, J., and G. Larkin. 1999. Effectiveness of ignition interlock devices in reducing drunk driving recidivism. American Journal of Preventive Medicine 16(Suppl 1):81–87.
Collier, R. 2013. Ignition interlock devices in California. http://dmv-defenders.com/ignition-interlock-devices-california (accessed August 25, 2017).
Community Preventive Services Task Force. 2012. Alcohol—excessive consumption: Electronic screening and brief interventions (E-SBI). https://www.thecommunityguide.org/findings/alcohol-excessive-consumption-electronic-screening-and-brief-interventions-e-sbi (accessed May 30, 2017).
Crew, B. K., and S. E. Johnson. 2011. Do victim impact programs reduce recidivism for operating a motor vehicle while intoxicated? Findings from an outcomes evaluation. Criminal Justice Studies 24(2):153–163.
Daoud, S. O., H. N. Tashima, and R. Grippe. 2015. 2015 annual report of the California DUI management information system. Sacramento: California Department of Motor Vehicles.
Delgado, M. K., M. A. Yokell, K. L. Staudenmayer, D. A. Spain, T. Hernandez-Boussard, and N. E. Wang. 2014. Factors associated with the disposition of severely injured patients initially seen at non-trauma center emergency departments: Disparities by insurance status. JAMA Surgery 149(5):422–430.
DeMetrick, A. 2016. State police rolling out a mobile breathalyzer truck. http://baltimore.cbslocal.com/2016/12/15/state-police-rolling-out-a-mobile-breathalyzer-truck (accessed December 5, 2017).
Dernocoeur, K. 1988. The far limits of rural EMS. Challenges on indian reservations. Journal of Economics and Management Strategy 13(4):36–39.
DeYoung, D. J., H. N. Tashima, and S. Maston. 2004. An evaluation of the effectiveness of ignition interlock in California. Sacramento, CA: Office of Traffic Safety.
Dill, P. L., and E. Wells-Parker. 2006. Court-mandated treatment for convicted drinking drivers. Alcohol Research and Health 29(1):41–48.
Dill, P. L., E. Wells-Parker, and C. A. Soderstrom. 2004. The emergency care setting for screening and intervention for alcohol use problems among injured and high-risk drivers: A review. Traffic Injury Prevention 5(3):278–291.
D’Onofrio, G., and L. C. Degutis. 2002. Preventive care in the emergency department: Screening and brief intervention for alcohol problems in the emergency department: A systematic review. Academic Emergency Medicine 9(6):627–638.
D’Onofrio, G., and L. C. Degutis. 2010. Integrating project assert: A screening, intervention, and referral to treatment program for unhealthy alcohol and drug use into an urban emergency department. Academic Emergency Medicine 17(8):903–911.
D’Onofrio, G., D. A. Fiellin, M. V. Pantalon, M. C. Chawarski, P. H. Owens, L. C. Degutis, S. H. Busch, S. L. Bernstein, and P. G. O’Connor. 2012. A brief intervention reduces hazardous and harmful drinking in emergency department patients. Annals of Emergency Medicine 60(2):181–192.
Donoghue, K., R. Patton, T. Phillips, P. Deluca, and C. Drummond. 2014. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: A systematic review and meta-analysis. Journal of Medical Internet Research 16(6):e142.
Dunlap, L. J., G. A. Zarkin, J. W. Bray, M. Mills, D. R. Kivlahan, J. R. McKay, P. Latham, and J. S. Tonigan. 2010. Revisiting the cost-effectiveness of the combine study for alcohol-dependent patients. Medical Care 48(2):306–313.
Dunn, C., L. Deroo, and F. P. Rivara. 2001. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction 96(12):1725–1742.
Eichelberger, A. H., and A. T. McCartt. 2016. Impaired driving enforcement practices among state and local law enforcement agencies in the United States. Journal of Safety Research 58:41–47.
Elder, R. W., R. Voas, D. Beirness, R. A. Shults, D. A. Sleet, J. L. Nichols, R. Compton, and Task Force on Community Preventive Services. 2011. Effectiveness of ignition interlocks for preventing alcohol-impaired driving and alcohol-related crashes: A community guide systematic review. American Journal of Preventive Medicine 40(3):362–376.
Emmen, M. J., G. M. Schippers, G. Bleijenberg, and H. Wollersheim. 2004. Effectiveness of opportunistic brief interventions for problem drinking in a general hospital setting: Systematic review. BMJ 328(7435):318.
Epstein, E. E., and B. S. McCrady. 1998. Behavioral couples treatment of alcohol and drug use disorders: Current status and innovations. Clinical Psychology Review 18(6):689–711.
Estee, S., T. Wickizer, L. He, M. F. Shah, and D. Mancuso. 2010. Evaluation of the Washington State screening, brief intervention, and referral to treatment project: Cost outcomes for Medicaid patients screened in hospital emergency departments. Medical Care 48(1):18–24.
FBI (Federal Bureau of Investigation). 2010. Crime in the United States table 69: Arrests by state. https://ucr.fbi.gov/crime-in-the-u.s/2010/crime-in-the-u.s.-2010/tables/10tbl69.xls (accessed April 11, 2017).
FBI. 2015. Crime in the United States 2015: Table 29, estimated number of arrests. https://ucr.fbi.gov/crime-in-the-u.s/2015/crime-in-the-u.s.-2015/tables/table-29 (accessed November 15, 2017).
Feeney, G. F., J. P. Connor, R. Young, J. Tucker, and A. McPherson. 2006. Combined acamprosate and naltrexone, with cognitive behavioural therapy is superior to either medication alone for alcohol abstinence: A single centres’ experience with pharmacotherapy. Alcohol and Alcoholism 41(3):321–327.
Fell, J. C. 2014. Update: Repeat DWI offenders involvement in fatal crashes in 2010. Traffic Injury Prevention 15(5):431–433.
Fell, J. C., and M. Scherer. 2017. Administrative license suspension: Does length of suspension matter? Traffic Injury Prevention 18(6):577–584.
Fell, J. C., C. Compton, and R. B. Voas. 2008. A note on the use of passive alcohol sensors during routine traffic stops. Traffic Injury Prevention 9(6):534–538.
Fell, J. C., A. S. Tippetts, and E. A. Langston. 2011. An evaluation of the three Georgia DUI courts. Washington, DC: National Highway Traffic Safety Administration.
Ferri, M., L. Amato, and M. Davoli. 2006. Alcoholics Anonymous and other 12-step programmes for alcohol dependence. Cochrane Database of Systematic Reviews (3):CD005032.
Fiedler, K., C. Brittle, and S. Stafford. 2012. Case studies of ignition interlock programs. DOT HS 811 594. Washington, DC: National Highway Traffic Safety Administration.
Finigan, M. W., T. Perkins, P. Zold-Kilbourn, J. Parks, and M. Stringer. 2011. Preliminary evaluation of extended-release naltrexone in Michigan and Missouri drug courts. Journal of Substance Abuse Treatment 41(3):288–293.
Fitzharris, M., S. Liu, S. Peiris, A. Devlin, K. Young, M. Lenne, D. Bowman, and J. Gatof. 2015. Options to extend coverage of alcohol interlock programs. Sydney, Australia: Austroads.
Fleming, M. F., M. P. Mundt, M. T. French, L. B. Manwell, E. A. Stauffacher, and K. L. Barry. 2002. Brief physician advice for problem drinkers: Long-term efficacy and benefit-cost analysis. Alcoholism: Clinical and Experimental Research 26(1):36–43.
Flowers, N. T., T. S. Naimi, R. D. Brewer, R. W. Elder, R. A. Shults, and R. Jiles. 2008. Patterns of alcohol consumption and alcohol-impaired driving in the United States. Alcoholism: Clinical and Experimental Research 32(4):639–644.
Fors, S. W., and D. G. Rojek. 1999. The effect of victim impact panels on DUI/DWI rearrest rates: A twelve-month follow-up. Journal of Studies on Alcohol 60(4):514–520.
Fourth Judicial District Minnesota Judicial Branch. n.d. Adult DWI court. Minneapolis, MN: Fourth Judicial District.
Fuller, R. K., L. Branchey, D. R. Brightwell, R. M. Derman, C. D. Emrick, F. L. Iber, K. E. James, R. B. Lacoursiere, K. K. Lee, and I. Lowenstam. 1986. Disulfiram treatment of alcoholism: A Veterans Administration cooperative study. JAMA 256(11):1449–1455.
Garbutt, J. C., A. M. Greenblatt, S. L. West, L. C. Morgan, A. Kampov-Polevoy, H. S. Jordan, and G. V. Bobashev. 2014. Clinical and biological moderators of response to naltrexone in alcohol dependence: A systematic review of the evidence. Addiction 109(8):1274–1284.
Gentilello, L. M., A. Donato, S. Nolan, R. E. Mackin, F. Liebich, D. B. Hoyt, and R. A. LaBrie. 2005a. Effect of the uniform accident and sickness policy provision law on alcohol screening and intervention in trauma centers. Journal of Trauma Injury, Infection, and Critical Care 59(3):629–636.
Gentilello, L. M., B. E. Ebel, T. M. Wickizer, D. S. Salkever, and F. P. Rivara. 2005b. Alcohol interventions for trauma patients treated in emergency departments and hospitals: A cost benefit analysis. Annals of Surgery 241(4):541–550.
Gonzalez, R. P., G. R. Cummings, H. A. Phelan, M. S. Mulekar, and C. B. Rodning. 2009. Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis. American Journal of Surgery 197(1):30–34.
Goodwin, A., L. Thomas, B. Kirley, W. Hall, N. O’Brien, and K. Hill. 2015. Countermeasures that work: A highway safety countermeasure guide for state highway safety offices, 8th ed. DOT HS 812 202. Washington, DC: National Highway Traffic Safety Administration.
Goonoo, N., A. Bhaw-Luximon, R. Ujoodha, A. Jhugroo, G. K. Hulse, and D. Jhurry. 2014. Naltrexone: A review of existing sustained drug delivery systems and emerging nano-based systems. Journal of Controlled Release 183:154–166.
Grant, B. F., R. B. Goldstein, T. D. Saha, S. P. Chou, J. Jung, H. Zhang, R. P. Pickering, W. J. Ruan, S. M. Smith, B. Huang, and D. S. Hasin. 2015. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 72(8):757–766.
Greater London Authority. 2016. “Sobriety tags” rolled out across London. https://www.london.gov.uk/press-releases/mayoral/crackdown-against-alcohol-related-crime (accessed September 13, 2017).
Greenwood-Ericksen, M. B., R. Tipirneni, and M. Abir. 2017. An emergency medicine-primary care partnership to improve rural population health: Expanding the role of emergency medicine. Annals of Emergency Medicine 70(5):640–647.
Gross, M. 2010. Alcoholics Anonymous: Still sober after 75 years. American Journal of Public Health 100(12):2361–2363.
Grunwald, D., J. McDonald, and J. Galante. 2001. Drunk driving in Rhode Island: 1995–1997. Providence, RI: Brown University.
Haas, B., D. Gomez, B. Zagorski, T. A. Stukel, G. D. Rubenfeld, and A. B. Nathens. 2010. Survival of the fittest: The hidden cost of undertriage of major trauma. Journal of the American College of Surgeons 211(6):804–811.
Haas, B., T. A. Stukel, D. Gomez, B. Zagorski, C. De Mestral, S. V. Sharma, G. D. Rubenfeld, and A. B. Nathens. 2012. The mortality benefit of direct trauma center transport in a regional trauma system: A population-based analysis. Journal of Trauma and Acute Care Surgery 72(6):1510-1515; discussion 1515–1517.
Hawaii State Judiciary. n.d. DWI court program overview. http://www.courts.state.hi.us/docs/special_projects/DWI_Court_Info.pdf (accessed April 19, 2017).
Hedlund, J. 2017. Drug-impaired driving: A guide for what states can do. Washington, DC: Governors Highway Safety Association.
Hedlund, J. H., and A. T. McCartt. 2002. Drunk driving: Seeking additional solutions. Washington, DC: AAA Foundation for Traffic Safety.
Heinrich, C. J., and C. J. Hill. 2008. Role of state policies in the adoption of naltrexone for substance abuse treatment. Health Services Research 43(3):951–970.
Higgins-Biddle, J., and J. Dilonardo. 2013. Alcohol and highway safety: Screening and brief intervention for alcohol problems as a community approach to improving traffic safety. DOT HS 811 836. Washington, DC: National Highway Traffic Safety Administration.
Hsia, R., and Y. C. Shen. 2011. Possible geographical barriers to trauma center access for vulnerable patients in the United States: An analysis of urban and rural communities. Archives of Surgery 146(1):46–52.
Humphreys, K., J. C. Blodgett, and T. H. Wagner. 2014. Estimating the efficacy of Alcoholics Anonymous without self-selection bias: An instrumental variables re-analysis of randomized clinical trials. Alcoholism: Clinical and Experimental Research 38(11):2688–2694.
Hunt, G. M., and N. H. Azrin. 1973. A community-reinforcement approach to alcoholism. Behavior Research Therapy 11(1):91–104.
IIHS (Insurance Institute for Highway Safety). 2017a. Impaired driving: Deterrence and enforcement. http://www.iihs.org/iihs/topics/t/impaired-driving/qanda#alcohol-deterrence-and-enforcement (accessed November 27, 2017).
IIHS. 2017b. Impaired driving: DUI/DWI. http://www.iihs.org/iihs/topics/laws/dui?topicName=impaired-driving (accessed June 28, 2017).
IIHS. 2017c. Alcohol-impaired driving. http://www.iihs.org/iihs/topics/t/impaired-driving/qanda#alcohol--general (accessed June 19, 2017).
IIHS. 2017d. Impaired driving: Administrative license suspension. http://www.iihs.org/iihs/topics/t/impaired-driving/qanda#alcohol--administrative-license-suspension (ac cessed November 27, 2017).
Ingraham, C. 2014. You really can get pulled over for driving while black, federal statistics show. The Washington Post, September 9.
Intoxalock. n.d. Alcohol monitoring business solutions. https://www.intoxalock.com/drunk-driving-prevention/fleets (accessed August 28, 2017).
Johnson, B. A., N. Rosenthal, J. A. Capece, F. Wiegand, L. Mao, K. Beyers, A. McKay, N Ait-Daoud, R. F. Anton, and D. A. Ciraulo. 2007. Topiramate for treating alcohol dependence: A randomized controlled trial. JAMA 298(14):1641–1651.
Johnson, M., R. Jackson, L. Guillaume, P. Meier, and E. Goyder. 2011. Barriers and facilitators to implementing screening and brief intervention for alcohol misuse: A systematic review of qualitative evidence. Journal of Public Health 33(3):412–421.
Jonas, D. E., H. R. Amick, C. Feltner, G. Bobashev, K. Thomas, R. Wines, M. M. Kim, E. Shanahan, C. E. Gass, and C. J. Rowe. 2014. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: A systematic review and meta-analysis. JAMA 311(18):1889–1900.
Joyce, S., and K. M. Thompson. 2017. Do victim impact panels reduce drunk driving recidivism? Restorative Justice 5(2):251–266.
Kaner, E. F., H. O. Dickinson, F. Beyer, E. Pienaar, C. Schlesinger, F. Campbell, J. B. Saunders, B. Burnand, and N. Heather. 2009. The effectiveness of brief alcohol interventions in primary care settings: A systematic review. Drug and Alcohol Review 28(3):301–323.
Kaskutas, L. A. 2009. Alcoholics Anonymous effectiveness: Faith meets science. Journal of Addiction and Disease 28(2):145–157.
Kaufman, E. J., and D. J. Wiebe. 2016. Impact of state ignition interlock laws on alcohol-involved crash deaths in the United States. American Journal of Public Health 106(5):865–871.
Kazemi, D. M., B. Borsari, M. J. Levine, S. Li, K. A. Lamberson, and L. A. Matta. 2017. A systematic review of the mHealth interventions to prevent alcohol and substance abuse. Journal of Health Communication 22(5):413–432.
Kelley-Baker, T., E. Taylor, A. Berning, J. Yao, E. Lauer, and D. Watson. 2017. The feasibility of voluntary ignition interlocks as a prevention strategy for young drivers. Washington, DC: National Highway Traffic Safety Administration.
Kenna, G. A., T. L. Lomastro, A. Schiesl, L. Leggio, and R. M. Swift. 2009. Review of topiramate: An antiepileptic for the treatment of alcohol dependence. Current Drug Abuse Reviews 2(2):135–142.
Kiefer, F., and K. Wiedemann. 2004. Combined therapy: What does acamprosate and naltrexone combination tell us? Alcohol and Alcoholism 39(6):542–547.
Kilmer, B., N. Nicosia, P. Heaton, and G. Midgette. 2013. Efficacy of frequent monitoring with swift, certain, and modest sanctions for violations: Insights from South Dakota’s 24/7 sobriety project. American Journal of Public Health 103(1):e37–e43.
Kishi, T., S. Sevy, R. Chekuri, and C. U. Correll. 2013. Meta-analysis antipsychotics for primary alcohol dependence: A systematic review and meta-analysis. Journal of Clinical Psychiatry 74(7):e642–e654.
Knight, K., D. D. Simpson, M. L. Hiller, C. Leukefeld, F. Tims, and D. Farabee. 2002. Screening and referral for substance-abuse treatment in the criminal justice system. Washington, DC: Department of Justice.
Knudsen, H. K., A. J. Abraham, and C. B. Oser. 2011. Barriers to the implementation of medication-assisted treatment for substance use disorders: The importance of funding policies and medical infrastructure. Evaluation and Program Planning 34(4):375–381.
Kranzler, H. R., S. Armeli, R. Wetherill, R. Feinn, H. Tennen, J. Gelernter, J. Covault, and T. Pond. 2016. Self-efficacy mediates the effects of topiramate and GRIK1 genotype on drinking. Addiction and Biology 21(2):450–459.
Kubas, A., P. Kayabas, and K. Vachal. 2015. Assessment of the 24/7 sobriety program in North Dakota: Participant behavior during enrollment. Fargo, ND: North Dakota State University
Lacey, J. H., R. K. Jones, and J. R. Stewart. 1991. Cost-benefit analysis of administrative license suspensions. DOT HS 807 689. Washington, DC: National Highway Traffic Safety Administration.
Lahausse, J. A., and B. N. Fildes. 2009. Cost-benefit analysis of an alcohol ignition interlock for installation in all newly registered vehicles. Traffic Injury Prevention 10(6):528–537.
Lahausse, J. A., B. N. Fildes, Y. Page, and M. P. Fitzharris. 2008. The potential for automatic crash notification systems to reduce road fatalities. Paper presented at Annals of Advance in Automotive Medicine/Annual Scientific Conference, San Diego, CA, October 6–8.
Lapham, S., and E. England-Kennedy. 2012. Convicted driving-while-impaired offenders’ views on effectiveness of sanctions and treatment. Qualitative Health Research 22(1): 17–30.
Lapham, S. C., and G. P. McMillan. 2011. Open-label pilot study of extended-release naltrexone to reduce drinking and driving among repeat offenders. Journal of Addiction Medicine 5(3):163–169.
Lapham, S. C., J. C’de Baca, I. Chang, W. C. Hunt, and L. R. Berger. 2002. Are drunk-driving offenders referred for screening accurately reporting their drug use? Drug and Alcohol Dependence 66(3):243–253.
Lapham, S. C., J. C’de Baca, G. McMillan, and W. C. Hunt. 2004. Accuracy of alcohol diagnosis among DWI offenders referred for screening. Drug and Alcohol Dependence 76(2):135–141.
Lapham, S. C., L. R. Kapitula, J. C’de Baca, and G. P. McMillan. 2006. Impaired-driving recidivism among repeat offenders following an intensive court-based intervention. Accident Analysis & Prevention 38(1):162–169.
Lapham, S. C., R. Stout, G. Laxton, and B. J. Skipper. 2011. Persistence of addictive disorders in a first-offender driving while impaired population. Archives of General Psychiatry 68(11):1151–1157.
Larimer, M. E., and J. M. Cronce. 2002. Identification, prevention and treatment: A review of individual-focused strategies to reduce problematic alcohol consumption by college students. Journal of Studies on Alcohol (Suppl 14):148–163.
Leaf, W., and D. Preusser. 1996. Effectiveness of passive alcohol sensors. DOT HS 808 381. Washington, DC: National Highway Traffic Safety Administration.
Lenton, S., J. Fetherston, and R. Cercarelli. 2010. Recidivist drink drivers’ self-reported reasons for driving whilst unlicensed—A qualitative analysis. Accident Analysis & Prevention 42(2):637–644.
Lobmaier, P. P., N. Kunøe, M. Gossop, and H. Waal. 2011. Naltrexone depot formulations for opioid and alcohol dependence: A systematic review. CNS Neuroscience & Therapeutics 17(6):629–636.
Logan, B. K., A. L. A. Mohr, and S. K. Talpins. 2014. Detection and prevalence of drug use in arrested drivers using the Drager Drug Test 5000 and Affiniton DrugWipe oral fluid drug screening devices. Journal of Analytical Toxicology 38(7):444–450.
Loudenburg, R., G. Drube, and G. Leonardson. 2010. South Dakota 24/7 sobriety program evaluation findings report. Salem, SD: Mountain Plains Evaluation.
Ma, T., P. A. Byrne, J. A. Bhatti, and Y. Elzohairy. 2016. Program design for incentivizing ignition interlock installation for alcohol-impaired drivers: The Ontario approach. Accident Analysis & Prevention 95(Pt A):27–32.
MacDonald, J. M., A. R. Morral, B. Raymond, and C. Eibner. 2007. The efficacy of the Rio Hondo DUI court: A 2-year field experiment. Evaluation Review 31(1):4–23.
MacKenzie, E. J., F. P. Rivara, G. J. Jurkovich, A. B. Nathens, K. P. Frey, B. L. Egleston, D. S. Salkever, and D. O. Scharfstein. 2006. A national evaluation of the effect of trauma-center care on mortality. New England Journal of Medicine 354(4):366–378.
MADD (Mothers Against Drunk Driving). 2013. Ignition interlock institutes: Promoting the use of interlocks and improvements to interlock programs. DOT HS 811 815. Washington, DC: National Highway Traffic Safety Administration.
MADD. 2017. Ignition interlock laws in the United States of America: A look at how states implement ignition interlock laws. http://www.madd.org/laws/law-overview/Overview-of-first-offender-interlock-laws.pdf (accessed June 28, 2017).
MADD. n.d. How it works: Victim impact panel program. https://www.maddvip.org/how-it-works (accessed July 3, 2017).
Madras, B. K., W. M. Compton, D. Avula, T. Stegbauer, J. B. Stein, and H. W. Clark. 2009. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug and Alcohol Dependence 99(1):280–295.
Magill, M., and L. A. Ray. 2009. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs 70(4):516–527.
Maisel, N. C., J. C. Blodgett, P. L. Wilbourne, K. Humphreys, and J. W. Finney. 2013. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: When are these medications most helpful? Addiction 108(2):275–293.
Maltz, M. D., and J. Targonski. 2002. A note on the use of county-level UCR data. Journal of Quantitative Criminology 18(3):297–318.
Mann, K. 2004. Pharmacotherapy of alcohol dependence: A review of the clinical data. CNS Drugs 18(8):485–504.
Marlowe, D. B., D. S. Festinger, P. L. Arabia, J. R. Croft, N. S. Patapis, and K. L. Dugosh. 2009. A systematic review of DWI court program evaluations. Alexandria, VA: National Drug Court Institute.
Marques, P. R., and R. B. Voas. 2010. Key features for ignition interlock programs. DOT HS 811 262. Washington, DC: National Highway and Traffic Safety Administration.
Marques, P. R., and R. B. Voas. 2012. Are we near a limit or can we get more safety from vehicle alcohol interlocks? Addiction 108(4):657–658.
Marques, P. R., R. B. Voas, and D. Hodgins. 1998. Vehicle interlock programs: Protecting the community against the drunk driver. Journal of Prevention & Intervention in the Community 17(1):31–44.
Marques, P. R., R. B. Voas, A. S. Tippetts, and D. J. Beirness. 1999. Behavioral monitoring of DUI offenders with the alcohol ignition interlock recorder. Addiction 94(12):1861–1870.
Marques, P. R., A. S. Tippets, R. B. Voas, E. R. Danseco, and D. R. Beirness. 2000. Support services provided during interlock usage and post-interlock repeat DUI: Outcomes and processes. In Proceedings of the 15th International Conference on Alcohol, Drugs and Traffic Safety, edited by H. Laurell and F. Schlyter. Stockholm, Sweden: X-CD Technologies. Pp. 1127–1132.
Marques, P. R., R. B. Voas, and D. S. Timken. 2004. Preliminary outcomes from a Texas manual-based group motivational intervention supplement for court-stipulated interlock DUI offenders. In Proceedings of the 17th International Conference on Alcohol, Drugs and Traffic Safety, edited by J. Oliver, P. Williams, and A. Clayton. Glasgow, Scotland: X-CD Technologies.
Marques, P., R. Voas, S. Tippetts, K. Blackman, D. Timken, and C. Field. 2007. Motivational intervention keyed to interlock use reduces the rate of positive BAC tests. In Proceedings of the T2007 Joint International Meeting of TIAFT/ICADTS/IIS, edited by B. K. Logan, D. S. Isenschmid, J. M. Walsh, D. Beirness, and J. Morland. Seattle, WA: ICADTS.
Marsch, L. A., K. M. Carroll, and B. D. Kiluk. 2014. Technology-based interventions for the treatment and recovery management of substance use disorders: A JSAT special issue. Journal of Substance Abuse and Treatment 46(1):1–4.
Martino, A., A. Sitran, and C. Rosa. 2014. Technical development and deployment of alcohol interlocks in road safety policy. Brussels, Belgium: European Union.
McCartt, A. T., L. L. Geary, and W. J. Nissen. 2002. Observational study of the extent of driving while suspended for alcohol-impaired driving. Washington, DC: National Highway Traffic Safety Administration.
McCartt, A. T., J. K. Wells, and E. R. Teoh. 2010. Attitudes toward in-vehicle advanced alcohol detection technology. Traffic Injury Prevention 11(2):156–164.
McCartt, A. T., W. A. Leaf, C. M. Farmer, and A. H. Eichelberger. 2013. Washington State’s alcohol ignition interlock law: Effects on recidivism among first-time DUI offenders. Traffic Injury Prevention 14(3):215–229.
McGinty, E. E., G. Tung, J. Shulman-Laniel, R. Hardy, L. Rutkow, S. Frattaroli, and J. S. Vernick. 2017. Ignition interlock laws: Effects on fatal motor vehicle crashes, 1982–2013. American Journal of Preventive Medicine 52(4):417–423.
McKnight-Eily, L. R., C. A. Okoro, R. Mejia, C. H. Denny, J. Higgins-Biddle, D. Hungerford, D. Kanny, and J. E. Sniezek. 2017. Screening for excessive alcohol use and brief counseling of adults—17 states and the District of Columbia, 2014. Morbidity and Mortality Weekly Report 66(12):313–319.
Mello, M. J., T. D. Nirenberg, D. Lindquist, H. A. Cullen, and R. Woolard. 2003. Physicians’ attitudes regarding reporting alcohol-impaired drivers. Substance Abuse 24(4):233–242.
Midgette, G., and B. Kilmer. 2015. The effect of Montana’s 24/7 sobriety program on DUI rearrest: Insights from a natural experiment with limited administrative data. Santa Monica, CA: RAND.
Miller, P. G., A. Curtis, A. Sønderlund, A. Day, and N. Droste. 2015. Effectiveness of interventions for convicted DUI offenders in reducing recidivism: A systematic review of the peer-reviewed scientific literature. The American Journal of Drug and Alcohol Abuse 41(1):16–29.
Miller, P. M., S. W. Book, and S. H. Stewart. 2011. Medical treatment of alcohol dependence: A systematic review. International Journal of Psychiatry in Medicine 42(3):227–266.
Miller, W. R., and S. Rollnick. 2002. Motivational interviewing: Preparing people for change, 2nd ed. New York: Guilford Publications.
Miller, W. R., and P. L. Wilbourne. 2002. Mesa Grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction 97(3):265–277.
Mitchell, O., D. B. Wilson, A. Eggers, and D. L. MacKenzie. 2012. Assessing the effectiveness of drug courts on recidivism: A meta-analytic review of traditional and non-traditional drug courts. Journal of Criminal Justice 40(1):60–71.
Moyer, A., J. W. Finney, C. E. Swearingen, and P. Vergun. 2002. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction 97(3):279–292.
Muelleman, R. L., M. C. Wadman, T. P. Tran, F. Ullrich, and J. R. Anderson. 2007. Rural motor vehicle crash risk of death is higher after controlling for injury severity. Journal of Trauma 62(1):221–225; discussion 225–226.
Mueller, K. J., A. J. Potter, A. C. MacKinney, and M. M. Ward. 2014. Lessons from tele-emergency: Improving care quality and health outcomes by expanding support for rural care systems. Health Affairs (Millwood) 33(2):228–234.
Muench, F., K. van Stolk-Cooke, A. Kuerbis, G. Stadler, A. Baumel, S. Shao, J. R. McKay, and J. Morgenstern. 2017. A randomized controlled pilot trial of different mobile messaging interventions for problem drinking compared to weekly drink tracking. PLoS ONE 12(2):e0167900.
Mullen, J., S. R. Ryan, C. W. Mathias, and D. M. Dougherty. 2015. Feasibility of a computer-assisted alcohol screening, brief intervention and referral to treatment program for DWI offenders. Addiction Science and Clinical Practice 10:25.
NADCP (National Association of Drug Court Professionals). n.d. What are drug courts?: The most effective justice strategy addressing the drug-addicted and mentally ill. http://www.nadcp.org/learn/what-are-drug-courts (accessed April 19, 2017).
Nagin, D. 2013. Deterrence in the twenty-first century: A review of the evidence. In Heniz College Research Showcase. Pittsburgh, PA: Carnegie Mellon University.
Namuswe, E. S., H. L. Coleman, and A. Berning. 2014. Breath test refusal rates in the United States—2011 update. Traffic Safety Facts Report DOT HS 811 881. Washington, DC: National Highway Traffic Safety Administration.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. A national trauma care system: Integrating military and civilian trauma systems to achieve zero preventable deaths after injury. Washington, DC: The National Academies Press.
NASEM. 2017. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press.
The National Judicial College. n.d. Traffic courses and programs. http://www.judges.org/courses/courses-by-judge-type/traffic-courses-and-programs (accessed October 10, 2017).
NC (North Carolina) Health and Human Services. 2017. Forensic tests for alcohol: Breath alcohol testing (BAT) program awareness. http://publichealth.nc.gov/chronicdiseaseandinjury/fta/bataware.htm (accessed December 5, 2017).
NCDC (National Criminal Defense College). 2015. The bottom line: Research update on DWI courts. https://www.dwicourts.org/wp-content/uploads/The%20Bottom%20Line_0.pdf (accessed August 9, 2017).
NCDC. n.d.-a. The ten guiding principles of DWI courts. https://www.dwicourts.org/wp-content/uploads/Guiding_Principles_of_DWI_Court_0.pdf (accessed August 16, 2017).
NCDC. n.d.-b. The bottom line: DWI court: First-time offenders—In or out? https://www.dwicourts.org/wp-content/uploads/The%20Bottom%20Line_0.pdf (accessed August 9, 2017).
NCDC. n.d.-c. What is a DWI court? https://www.dwicourts.org/uncategorized/what-dwi-court (accessed April, 11, 2017).
NCDC. n.d.-d. DWI court model compliance checklist. https://www.dwicourts.org/wp-content/uploads/2011%20NCDC%20Checklist%20Final-Form_0.pdf (accessed August 9, 2017).
NCSA (National Center for Statistics and Analysis). 2016. Traffic safety facts 2015: A compilation of motor vehicle crash data from the Fatality Analysis Reporting System and General Estimates System. DOT HS 812 384. Washington, DC: National Highway Traffic Safety Administration.
NCSL (National Conference of State Legislators). 2016. State ignition interlock laws. http://www.ncsl.org/research/transportation/state-ignition-interlock-laws.aspx (accessed June 16, 2017).
NDAA (National District Attorneys Association). n.d. National Traffic Law Center: Resources. http://ndaa.org/ntlc_resources.html (accessed November 28, 2017).
NHTSA (National Highway Traffic Safety Administration). 1986. Reducing highway crashes through administrative license revocation. DOT HS 806 921. Washington, DC: National Highway Traffic Safety Administration.
NHTSA. 2005. A guide to sentencing DUI offenders. Washington, DC: National Highway Traffic Safety Administration.
NHTSA. 2006. Uniform guidelines for state highway safety programs: Highway safety program guideline no. 8: Impaired driving. Washington, DC: National Highway Traffic Safety Administration.
NHTSA. 2013. Model guideline for state ignition interlock programs. DOT HS 811 859. Washington, DC: National Highway Traffic Safety Administration.
NHTSA. 2016. Digest of impaired driving and selected beverage control laws. Washington, DC: National Highway Traffic Safety Administration.
NHTSA. 2017. Examining the feasibility of alcohol ignition interlocks for motorcycles. Traffic Tech Report DOT HS 812 406. Washington, DC: National Highway Traffic Safety Administration.
NIAAA (National Institute on Alcohol Abuse and Alcoholism). 2000. 10th special report to the U.S. Congress on alcohol and health. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism.
NIAAA. 2004/2005. Screening for alcohol use and alcohol related problems. Alcohol Alert 65.
NIAAA. 2005a. Brief interventions. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism.
NIAAA. 2005b. Helping patients who drink too much. Washington, DC: National Institute on Alcohol Abuse and Alcoholism.
NIAAA. 2010. Exploring treatment options for alcohol use disorders. Alcohol Alert 81.
Nichols, J., and H. L. Ross. 1989. The effectiveness of legal sanctions in dealing with drinking drivers. In Surgeon General’s Workshop on Drunk Driving: Background papers. Rockville, MD: Office of the Surgeon General. Pp. 93–112.
Nicosia, N., B. Kilmer, and P. Heaton. 2016. Can a criminal justice alcohol abstention programme with swift, certain, and modest sanctions (24/7 sobriety) reduce population mortality? A retrospective observational study. Lancet Psychiatry 3(3):226–232.
Nilsen, P., M. Aalto, P. Bendtsen, and K. Seppä. 2006. Effectiveness of strategies to implement brief alcohol intervention in primary healthcare: A systematic review. Scandinavian Journal of Primary Health Care 24(1):5–15.
Nilsen, P., J. Baird, M. J. Mello, T. Nirenberg, R. Woolard, P. Bendtsen, and R. Longabaugh. 2008. A systematic review of emergency care brief alcohol interventions for injury patients. Journal of Substance Abuse Treatment 35(2):184–201.
NPC (Northwest Professional Consortium, Inc.) Research. 2014. Collection of executive summaries: Evaluation findings in nine DWI court programs. http://www.mncourts.gov/Documents/0/Public/Drug_Court/DWI_Court_Evaluation_Collection_of_Statewide_and_Program_Summaries.pdf (accessed August 16, 2017).
NTSB (National Transportation Safety Board). 2000. Actions to reduce fatalities, injuries, and crashes involving the hard core drinking driver. Washington, DC: National Transportation Safety Board.
Nunes, A. P., M. K. Richmond, K. Marzano, C. Swenson, and J. Lockhart. 2017. Ten years of implementing SBIRT: Lessons learned. Substance Abuse 38(4):508–512.
O’Brien, C. P., L. A. Volpicelli, and J. R. Volpicelli. 1996. Naltrexone in the treatment of alcoholism: A clinical review. Alcohol 13(1):35–39.
O’Coin, T. 2017. Lawmakers propose ignition locks on school buses. WPRI, January 18.
O’Donnell, A., P. Anderson, D. Newbury-Birch, B. Schulte, C. Schmidt, J. Reimer, and E. Kaner. 2014. The impact of brief alcohol interventions in primary healthcare: A systematic review of reviews. Alcohol and Alcoholism 49(1):66–78.
O’Keeffe, T., S. Shafi, J. L. Sperry, and L. M. Gentilello. 2009. The implications of alcohol intoxication and the uniform policy provision law on trauma centers; A national trauma data bank analysis of minimally injured patients. Journal of Trauma 66(2):495–498.
Oslin, D. W., W. H. Berrettini, and C. P. O’Brien. 2006. Review: Targeting treatments for alcohol dependence: The pharmacogenetics of naltrexone. Addiction Biology 11(3–4):397–403.
Ouimet, M. C., M. Dongier, I. Di Leo, L. Legault, J. Tremblay, F. Chanut, and T. G. Brown. 2013. A randomized controlled trial of brief motivational interviewing in impaired driving recidivists: A 5-year follow-up of traffic offenses and crashes. Alcoholism: Clinical and Experimental Research 37(11):1979–1985.
Owens, D. K., K. N. Lohr, D. Atkins, J. R. Treadwell, J. T. Reston, E. B. Bass, S. Chang, and M. Helfand. 2008. Grading the strength of a body of evidence when comparing medical interventions. In Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality.
Petry, N. M., B. Martin, J. L. Cooney, and H. R. Kranzler. 2000. Give them prizes, and they will come: Contingency management for treatment of alcohol dependence. Journal of Consulting and Clinical Psychology 68(2):250–257.
Pines, J., and D. Ernst. 2017. Solving the rural health care access crisis with the freestanding emergency center care model. http://healthaffairs.org/blog/2017/02/21/solving-the-rural-health-care-access-crisis-with-the-freestanding-emergency-center-care-model (accessed October 10, 2017).
Polacsek, M., E. M. Rogers, W. G. Woodall, H. Delaney, D. Wheeler, and N. Rao. 2001. MADD victim impact panels and stages-of-change in drunk-driving prevention. Journal of Studies on Alcohol 62(3):344–350.
Powers, M. B., E. Vedel, and P. M. Emmelkamp. 2008. Behavioral couples therapy (BCT) for alcohol and drug use disorders: A meta-analysis. Clinical Psychology Review 28(6): 952–962.
Prendergast, M., D. Podus, J. Finney, L. Greenwell, and J. Roll. 2006. Contingency management for treatment of substance use disorders: A meta-analysis. Addiction 101(11): 1546–1560.
President’s Task Force on 21st Century Policing. 2015. Final report of the President’s Task Force on 21st Century Policing. Washington, DC: Office of Community Oriented Policing Services.
Purshouse, R. C., A. Brennan, R. Rafia, N. R. Latimer, R. J. Archer, C. R. Angus, L. R. Preston, and P. S. Meier. 2013. Modelling the cost-effectiveness of alcohol screening and brief interventions in primary care in England. Alcohol and Alcoholism 48(2):180–188.
Raistrick, D., N. Heather, and C. Godfrey. 2006. Review of the effectiveness of treatment for alcohol problems. London, UK: National Treatment Agency for Substance Misuse.
Ramirez, R. 2017. PowerPoint presentation to the Committee on Accelerating Progress to Reduce Alcohol-Impaired Driving Fatalities in Washington, DC, February 16, 2017. http://nationalacademies.org/hmd/~/media/Files/Activity%20Files/AcceleratingProgresstoReduceAlcoholImpairedDrivingFatalities/16%20FEB%202017/5%20Ramirez.pdf (accessed December 4, 2017).
Ray, L. A., A. Heydari, and T. Zorick. 2010. Quetiapine for the treatment of alcoholism: Scientific rationale and review of the literature. Drug and Alcohol Review 29(5):568–575.
Redelmeier, D. A., C. J. Yarnell, D. Thiruchelvam, and R. J. Tibshirani. 2012. Physicians’ warnings for unfit drivers and the risk of trauma from road crashes. New England Journal of Medicine 367(13):1228–1236.
Robertson, A., S. Gardner, C. S. Walker, and A. Tatch. 2016. DUI recidivism by intervention adherence: A multiple risk factor approach. American Journal of Drug and Alcohol Abuse 42(5):597–605.
Robertson, R. D., and H. M. Simpson. 2002. DWI system improvements for dealing with hard core drinking drivers: Prosecution. Executive summary. Ottawa, Canada: Traffic Injury Research Foundation.
Robertson, R., H. Simpson, and P. Parson. 2008. Screening, assessment and treatment of DWI offenders: A guide for justice professionals and policy makers. Ottawa, Ontario: Traffic Injury Research Foundation.
Rogers, P. N. 1997. Specific deterrent impact of California’s 0.08% blood alcohol concentration limit and administrative per se license suspension laws. Sacramento: California Department of Motor Vehicles.
Rohsenow, D. J. 2004. What place does naltrexone have in the treatment of alcoholism? CNS Drugs 18(9):547–560.
Rohsenow, D. J., S. M. Colby, P. M. Monti, R. M. Swift, R. A. Martin, T. I. Mueller, A. Gordon, and C. A. Eaton. 2000. Predictors of compliance with naltrexone among alcoholics. Alcoholism: Clinical and Experimental Research 24(10):1542–1549.
Rojek, D. G., J. E. Coverdill, and S. W. Fors. 2003. The effect of victim impact panels on DUI rearrest rates: A five-year follow-up. Criminology 41(4):1319–1340.
Roozen, H. G., J. J. Boulogne, M. W. van Tulder, W. van den Brink, C. A. De Jong, and A. J. Kerkhof. 2004. A systematic review of the effectiveness of the community reinforcement approach in alcohol, cocaine and opioid addiction. Drug and Alcohol Dependency 74(1):1–13.
Roozen, H. G., R. de Waart, D. A. van der Windt, W. van den Brink, C. A. de Jong, and A. J. Kerkhof. 2006. A systematic review of the effectiveness of naltrexone in the maintenance treatment of opioid and alcohol dependence. European Neuropsychopharmacology 16(5):311–323.
Rose, G. L., J. M. Skelly, G. J. Badger, T. A. Ferraro, and J. E. Helzer. 2015. Efficacy of automated telephone continuing care following outpatient therapy for alcohol dependence. Addictive Behavior 41:223–231.
Rosenfeld, R. 2007. Transfer the uniform crime reporting program from the FBI to the Bureau of Justice Statistics. Criminology & Public Policy 6(4):825–833.
Rösner, S., S. Leucht, P. Lehert, and M. Soyka. 2008. Acamprosate supports abstinence, naltrexone prevents excessive drinking: Evidence from a meta-analysis with unreported outcomes. Journal of Psychopharmacology 22(1):11–23.
Roth, R. 2014. 2014 survey of currently-installed interlocks in the U.S. http://www.rothinterlock.org/2014_survey_of_currently_installed_interlocks_in_the_us.pdf (accessed December 20, 2016).
Roth, R., R. Voas, and P. Marques. 2007. Interlocks for first offenders: Effective? Traffic Injury Prevention 8(4):346–352.
Saitz, R. 2010. Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug and Alcohol Review 29(6):631–640.
SAMHSA (Substance Abuse and Mental Health Services Administration). 2005a. Substance abuse treatment for adults in the criminal justice system: A treatment improvement protocol. Rockville, MD: Department of Health and Human Services.
SAMHSA. 2005b. Acamprosate: A new medication for alcohol use disorder. Washington, DC: Department of Health and Human Services.
SAMHSA. 2016a. Results from the 2015 National Survey on Drug Use and Health: Detailed tables. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm#tab2-41b (accessed March 31, 2017).
SAMHSA. 2016b. Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Washington, DC: Department of Health and Human Services.
SAMHSA. 2016c. Naltrexone. https://www.samhsa.gov/medication-assisted-treatment/treatment/naltrexone (accessed June 8, 2017).
SAMHSA. 2017. Coding for screening and brief intervention reimbursement. https://www.samhsa.gov/sbirt/coding-reimbursement (accessed November 28, 2017).
SAMHSA. n.d. SBIRT: Brief intervention. http://www.integration.samhsa.gov/clinical-practice/sbirt/brief-interventions#Brief_Intervention_Models (accessed June 1, 2017).
Samra, H., X. Qin, and H. Zhaoxiang. 2014. Improving rural emergency medical services (EMS) through transportation system enhancements. Brookings: South Dakota State University.
Schiller, J., J. E. McCormack, V. Tarsia, M. J. Shapiro, A. J. Singer, H. C. Thode, Jr., and M. C. Henry. 2009. The effect of adding a second helicopter on trauma-related mortality in a county-based trauma system. Prehospital Emergency Care 13(4):437–443.
Schonfeld, C., and M. Sheehan. 2004. Critical overview of alcohol ignition interlock programs in Australia. Paper presented at 17th International Conference on Alcohol, Drugs and Traffic Safety, Glasgow, Scotland, August 8–13.
Schuckit, M. A. 2006. Rehabilitation. In Drug and alcohol abuse: A clinical guide to diagnosis and treatment. New York: Springer.
Schuler, M. S., S. Puttaiah, R. Mojtabai, and R. M. Crum. 2015. Perceived barriers to treatment for alcohol problems: A latent class analysis. Psychiatric Services 66(11):1221–1228.
SCRAM (Secure Continuous Remote Alcohol Monitor) Systems. 2017. SCRAM continuous alcohol monitoring: Quick facts. https://www.scramsystems.com/images/uploads/general/media-pdf/media-kits/scram-mediakit-quickFacts.pdf (accessed September 3, 2017).
Shinar, D., and R. P. Compton. 1995. Victim impact panels: Their impact on DWI recidivism. Alcohol, Drugs and Driving 11(1):73–87.
Shrum, C. 2017. PowerPoint presentation to the Committee on Accelerating Progress to Reduce Alcohol-Impaired Driving Fatalities in Washington, DC, May 9, 2017. http://nationalacademies.org/hmd/Activities/PublicHealth/ReduceAlcoholImpairedDrivingFatalities/2017-MAY-09.aspx (accessed October 17, 2017).
Sihler, K. C., and M. R. Hemmila. 2009. Injuries in nonurban areas are associated with increased disability at hospital discharge. Journal of Trauma 67(5):903–909.
Sloan, F. A., L. M. Chepke, D. V. Davis, K. Acquah, and P. Zold-Kilbourn. 2013. Effects of admission and treatment strategies of DWI courts on offender outcomes. Accident Analysis & Prevention 53:112–120.
Sloan, F. A., E. J. Gifford, L. M. Eldred, and S. A. McCutchan. 2016. Does the probability of DWI arrest fall following participation in DWI and hybrid drug treatment court programs? Accident Analysis & Prevention 97:197–205.
Sobering Up. 2016. States make 24/7 sobriety legislation a top priority in 2016. https://www.scramsystems.com/blog/2016/02/states-make-247-sobriety-legislation-a-top-priority-in-2016 (accessed September 19).
Solberg, L. I., M. V. Maciosek, and N. M. Edwards. 2008. Primary care intervention to reduce alcohol misuse ranking its health impact and cost effectiveness. American Journal of Preventive Medicine 34(2):143–152.
South Dakota Legislature. 2017. 24/7 sobriety program, chapter 2:06:03: Fees. http://sdlegislature.gov/rules/DisplayRule.aspx?Rule=02:06:03 (accessed September 13, 2017).
Sprattler, K. 2009. Ignition interlocks—what you need to know: A toolkit for policy makers, highway safety professionals, and advocates. Washington, DC: National Highway Traffic Safety Administration.
Srisurapanont, M., and N. Jarusuraisin. 2005. Naltrexone for the treatment of alcoholism: A meta-analysis of randomized controlled trials. International Journal of Neuropsychopharmacology 8(2):267–280.
Stasiewicz, P. R., T. H. Nochajski, and D. L. Homish. 2007. Assessment of alcohol use disorders among court-mandated DWI offenders. Journal of Addictions & Offender Counseling 27(2):102–112.
State of Nevada. n.d. State regulations dementia and driving. Carson City, NV: Department of Health & Human Services.
Steinka-Fry, K. T., E. E. Tanner-Smith, and E. A. Hennessy. 2015. Effects of brief alcohol interventions on drinking and driving among youth: A systematic review and meta-analysis. Journal of Addiction & Prevention 3(1):11.
Stockings, E., W. D. Hall, M. Lynskey, K. I. Morley, N. Reavley, J. Strang, G. Patton, and L. Degenhardt. 2016. Prevention, early intervention, harm reduction, and treatment of substance use in young people. Lancet Psychiatry 3(3):280–296.
Suffoletto, B., C. Callaway, J. Kristan, K. Kraemer, and D. B. Clark. 2012. Text-message-based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcoholism: Clinical and Experimental Research 36(3):552–560.
Suffoletto, B., J. Kristan, C. Callaway, K. H. Kim, T. Chung, P. M. Monti, and D. B. Clark. 2014 A text message alcohol intervention for young adult emergency department patients: A randomized clinical trial. Annals of Emergency Medicine 64(6):664–672.
Suffoletto, B., J. Kristan, T. Chung, K. Jeong, A. Fabio, P. Monti, and D. B. Clark. 2015. An interactive text message intervention to reduce binge drinking in young adults: A randomized controlled trial with 9-month outcomes. PLoS One 10(11):e0142877.
Surla, Jr., L., and S. Koons. 1989. An evaluation of the elimination of plea bargaining for DWI offenders. Washington, DC: National Highway Traffic Safety Administration.
Swift, R., D. W. Oslin, M. Alexander, and R. Forman. 2011. Adherence monitoring in naltrexone pharmacotherapy trials: A systematic review. Journal of Studies on Alcohol and Drugs 72(6):1012–1018.
Talpins, S. K., and P. Rogers. 2017. Overcoming the plateau: Reducing impaired driving by addressing drug-impaired drivers. Global Journal of Addiciton & Rehabilitation Medicine 1(4):555–569.
Talpins, S. K., R. DuPont, R. Voas, E. Holmes, K. Sabet, and C. Shea. 2014. License revocation as a tool for combating drugged driving. Impaired Driving Update 19(2):29–41.
Talpins, S. K., R. L. DuPont, H. C. Walls, K. Sabet, and D. Wallace. 2015. The Miami-Dade protocol: Making drugged driving enforcement a reality. Journal of Alcoholism & Drug Dependence 3(4):212.
Timko, C., A. Desai, D. M. Blonigen, B. S. Moos, and R. H. Moos. 2011. Driving while intoxicated among individuals initially untreated for alcohol use disorders: One- and sixteen-year follow-ups. Journal of Studies on Alcohol and Drugs 72(2):173–184.
Tracy, K., and S. P. Wallace. 2016. Benefits of peer support groups in the treatment of addiction. Substance Abuse and Rehabilitation 7:143–154.
TRB (Transportation Research Board). 2005a. Guidance for implementation of the AASHTO strategic highway safety plan. Volume 16: A guide for reducing alcohol-related collisions. Washington, DC: The National Academies Press.
TRB. 2005b. Guidance for implementation of the AASHTO strategic highway safety plan. Volume 15: A guide for enhancing rural emergency medical services. Washington, DC: The National Academies Press.
TRB. 2013a. Countermeasures to address impaired driving offenders: Toward an integrated model. Washington, DC: The National Academies Press.
TRB. 2013b. Emergency medical services response to motor vehicle crashes in rural areas. Washington, DC: The National Academies Press.
Ullman, D. F. 2016. Locked and not loaded: First time offenders and state ignition interlock programs. International Review of Law and Economics 45:1–13.
USPSTF (U.S. Preventive Services Task Force). 2013. Alcohol misuse: Screening and behavioral counseling interventions in primary care. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/alcohol-misuse-screening-and-behavioral-counseling-interventions-in-primary-care (accessed June 2, 2017).
Vallury, K. D., M. Jones, and C. Oosterbroek. 2015. Computerized cognitive behavior therapy for anxiety and depression in rural areas: A systematic review. Journal of Medical Internet Research 17(6):e139.
Vanlaar, W. G., M. Mainegra Hing, and R. D. Robertson. 2017. An evaluation of Nova Scotia’s alcohol ignition interlock program. Accident Analysis & Prevention 100:44–52.
Vasilaki, E. I., S. G. Hosier, and W. M. Cox. 2006. The efficacy of motivational interviewing as a brief intervention for excessive drinking: A meta-analytic review. Alcohol and Alcoholism 41(3):328–335.
Vézina, L. 2002. The Québec alcohol ignition interlock program: Impact on recidivism and crashes. In Proceedings of Alcohol, Drugs and Traffic Safety—T2002: 16th International Conference on Alcohol, Drugs and Traffic Safety, edited by D. Mayhew and C. Dussault. Québec, Canada: Societe de L’assurance automobile du Québec. Pp. 97–104.
Voas, R. B. 2014. Enhancing the use of vehicle alcohol interlocks with emerging technology. Alcohol Research: Current Reviews 36(1):81–89.
Voas, R. B., and J. C. Fell. 2011. Preventing impaired driving opportunities and problems. Alcohol Research & Health 34(2):225–235.
Voas, R. B., and D. A. Fisher. 2001. Court procedures for handling intoxicated drivers. Alcohol Research and Health 25(1):32–42.
Voas, R. B., P. R. Marques, A. S. Tippetts, and D. J. Beirness. 1999. The Alberta interlock program: The evaluation of a province-wide program on DUI recidivism. Addiction 94(12):1849–1859.
Voas, R. B., A. S. Tippetts, and J. Fell. 2000a. The relationship of alcohol safety laws to drinking drivers in fatal crashes. Accident Analysis & Prevention 32(4):483–492.
Voas, R., A. S. Tippetts, and E. Taylor. 2000b. Effectiveness of the Ohio vehicle action and administrative license suspension laws. Washington, DC: National Highway Traffic Safety Administration.
Voas, R. B., A. S. Tippetts, and A. S. McKnight. 2010a. DUI offenders delay license reinstatement: A problem? Alcoholism: Clinical and Experimental Research 34(7):1282–1290.
Voas, R. B., S. S. Tippetts, D. Fisher, and M. Grosz. 2010b. Requiring suspended drunk drivers to install alcohol interlocks to reinstate their licenses: Effective? Addiction 105(8): 1422–1428.
Voas, R. B., A. S. Tippetts, G. Bergen, M. Grosz, and P. Marques. 2016. Mandating treatment based on interlock performance: Evidence for effectiveness. Alcoholism: Clinical and Experimental Research 40(9):1953–1960.
Wagenaar, A. C., and M. M. Maldonado-Molina. 2007. Effects of drivers’ license suspension policies on alcohol-related crash involvement: Long-term follow-up in forty-six states. Alcoholism: Clinical and Experimental Research 31(8):1399–1406.
Walker, J., D. Santos, C. Rowe, G.-M. Santos, S. Jung, and P. Coffin. 2017. A novel approach to naltrexone injections may reduce complications and increase adherence. Drug & Alcohol Dependence 171:e210.
Washington Courts. 2016. Current DUI sentencing grid. Olympia, WA: Administrative Office of the Courts.
Wheeler, D. R., G. Woodall, and E. Rogers. 2002. Victim impact panels. Do they impact drinking and driving behavior? Paper presented at 16th International Conference on Alcohol, Drugs and Traffic Safety, Montreal, Canada, August 4–9.
Wheeler, D. R., E. M. Rogers, J. S. Tonigan, and W. G. Woodall. 2004. Effectiveness of customized victim impact panels on first-time DWI offender inmates. Accident Analysis & Prevention 36(1):29–35.
White, A., D. Kavanagh, H. Stallman, B. Klein, F. Kay-Lambkin, J. Proudfoot, J. Drennan, J. Connor, A. Baker, and E. Hines. 2010. Online alcohol interventions: A systematic review. Journal of Medical Internet Research 12(5):e62.
Wiliszowski, C., J. Fell, S. McKnight, and S. Tippetts. 2011. An evaluation of intensive supervision programs for serious DWI offenders. DOT HS 811 446. Washington, DC: National Highway Traffic Safety Administration.
Williams, S. H. 2005. Medications for treating alcohol dependence. American Family Physician 72(9):1775–1780.
Willis, C., S. Lybrand, and N. Bellamy. 2004. Alcohol ignition interlock programmes for reducing drink driving recidivism. The Cochrane Library 18(4):CD004168.
Woodall, W. G., H. Delaney, E. Rogers, and D. Wheeler. 2000. A randomized trial of victim impact panels’ DWI deterrence effectiveness. Alcoholism: Clinical and Experimental Research 24(S5):113A.
Woodward, T. 2017. PowerPoint presentation to the Committee on Accelerating Progress to Reduce Alcohol-Impaired Driving Fatalities in Washington, DC, February 16, 2017. http://nationalacademies.org/hmd/~/media/Files/Activity%20Files/AcceleratingProgresstoReduceAlcoholImpairedDrivingFatalities/16%20FEB%202017/4%20Woodward.pdf (accessed December 4, 2017).
Yokell, M. A., C. A. Camargo, N. E. Wang, and M. K. Delgado. 2014. Characteristics of United States emergency departments that routinely perform alcohol risk screening and counseling for patients presenting with drinking-related complaints. Western Journal of Emergency Medicine 15(4):438–445.
Yuma-Guerrero, P. J., K. A. Lawson, M. M. Velasquez, K. von Sternberg, T. Maxson, and N. Garcia. 2012. Screening, brief intervention, and referral for alcohol use in adolescents: A systematic review. Pediatrics 130(1):115–122.
Zador, P. L., E. M. Ahlin, W. J. Rauch, J. M. Howard, and G. D. Duncan. 2011. The effects of closer monitoring on driver compliance with interlock restrictions. Accident Analysis & Prevention 43(6):1960–1967.
Zarkin, G. A., J. W. Bray, A. Aldridge, D. Mitra, M. J. Mills, D. J. Couper, R. A. Cisler, and COMBINE Cost-Effectiveness Research Group. 2008. Cost and cost-effectiveness of the COMBINE study in alcohol-dependent patients. Archives of General Psychiatry 65(10):1214–1221.
Zarkin, G. A., J. W. Bray, A. Aldridge, M. Mills, R. A. Cisler, D. Couper, J. R. McKay, and S. O’Malley. 2010. The impact of alcohol treatment on social costs of alcohol dependence: Results from the COMBINE study. Medical Care 48(5):396–401.
Zwerling, C., C. Peek-Asa, P. S. Whitten, S. W. Choi, N. L. Sprince, and M. P. Jones. 2005. Fatal motor vehicle crashes in rural and urban areas: Decomposing rates into contributing factors. Injury Prevention 11(1):24–28.
This page intentionally left blank.














































































