2
Microbiome Variation
Traditional notions in which microorganisms were viewed solely as pathogens or etiologic agents of acute infectious diseases have been challenged. Today, scientists recognize that such a “foe” view neglects the growing evidence that many microorganisms reside in a symbiotic and likely mutually beneficial relationship with the host. The Human Microbiome Project, which characterized the microbial composition of multiple body sites in healthy people of different ethnicities in two cities (St. Louis, MO, and Houston, TX) in the United States (HMP Consortium 2012a,b; Aagaard et al. 2013), has established a body of information that has sparked numerous investigations to understand the link between human health and disease. Research now suggests associations between microbial perturbations and such diseases as obesity, type II diabetes mellitus, ulcerative colitis, Crohn’s disease, and colorectal cancer (Mangin et al. 2004; Ley et al. 2005; Gophna et al. 2006; Manichanh et al. 2006; Turnbaugh et al. 2006, 2008, 2009; Bäckhed et al. 2007; Cani et al. 2007; Willing et al. 2009; Larsen et al. 2010; Schwiertz et al. 2010; Wu et al. 2010; Joossens et al. 2011; Lepage et al. 2011; Marchesi et al. 2011; Sobhani et al. 2011; Qin et al. 2012; Wang et al. 2012; Devaraj et al. 2013). Although associations have been reported, causal relationships have yet to be fully established in most cases, and environmental and host modifiers need to be defined. Furthermore, questions remain concerning when in the lifespan the host–microbial interactions that lead to various health or disease states are first established and to what extent they can be modified.
The Human Microbiome Project also demonstrated greater bacterial diversity and body-site specificity than expected on the basis of previous studies. Specifically, microbial community composition and function have been found to vary substantially over the human life span (Palmer et al. 2007; Aagaard et al. 2012; Yatsunenko et al. 2012; Bäckhed et al. 2015; Hollister et al. 2015) and to exhibit extensive body-site specificity with remarkable variation between sites but considerably less interindividual variation within given sites (Turnbaugh et al. 2007; Costello et al. 2009; Grice et al. 2009; HMP Consortium 2012a,b; Aagaard et al. 2013; Franzosa et al. 2015; Voigt et al. 2015). It is the variation in the human microbiome that is the primary focus of this chapter. General factors that contribute to variation in the human microbiome are discussed first and then variation specifically in the gut, skin, and respiratory microbiomes. The chapter concludes with a discussion of variation between human and animal microbiomes and implications for using animal models to study the human microbiome. It is important to note that the variation that is typically studied and is the focus of this report is not due to day-to-day fluctuations but actually measurable perturbations that are independent of circadian rhythm. Furthermore, some examples of variation or changes in the human microbiome that affect function or health are provided here, but a comprehensive review of the literature on the human microbiome and health and disease states is beyond the scope of this report.
FACTORS THAT CONTRIBUTE TO VARIATION IN THE HUMAN MICROBIOME
Population-based studies have identified multiple factors that relate to the observed variation in the composition, gene content, and function of the human microbiome. They include body site (Grice and Segre 2011; HMP Consortium 2012a,b; Costello et al. 2013), age (Yatsunenko et al. 2012), environmental exposures (chemical and microbiologic), disease state (Huang et al. 2015; Mar et al. 2016), genetics (Goodrich et al. 2014; Ma et al. 2014a; Imhann et al. in press), sex (Aagaard et al. 2013; Markle et al. 2013), socioeconomic status (Levin et al. 2016), geography (Yatsunenko et al. 2012), pregnancy status (Aagaard et al. 2012; Koren et al. 2012), and diet (Yatsunenko et al. 2012; David et al. 2014b).
Body site is a key factor in the variation observed in the human microbiome. Different body sites contain microbiomes that differ in microbial composition and function. As a result, each body site can be characterized by specific bacterial species and other microorganisms that have adapted to the site’s environment, and the differences in microbial composition yield differences in metabolic capacity and in aggregate function of the human microbiome. Specifically, no bacterial taxon has been found to be present in all body sites, and a given taxon might be absent from a specific body site in one person but dominate corresponding microbial communities in another person (Zoetendal et al. 2012). At higher levels of microbial classification, however, individual body sites do exhibit characteristic phylum-level distributions. Such sites as the skin, respiratory tract, and reproductive system that have a low biomass exhibit fewer taxa but often have microbial communities with diverse functions (Grice et al. 2009; Yatsunenko et al. 2012; Aagaard et al. 2014; David et al. 2014a; Ordiz et al. 2015). In light of the substantial variation in microbial composition and function between body sites, the following discussion of the human microbiome is organized according to body site.
THE GUT MICROBIOME
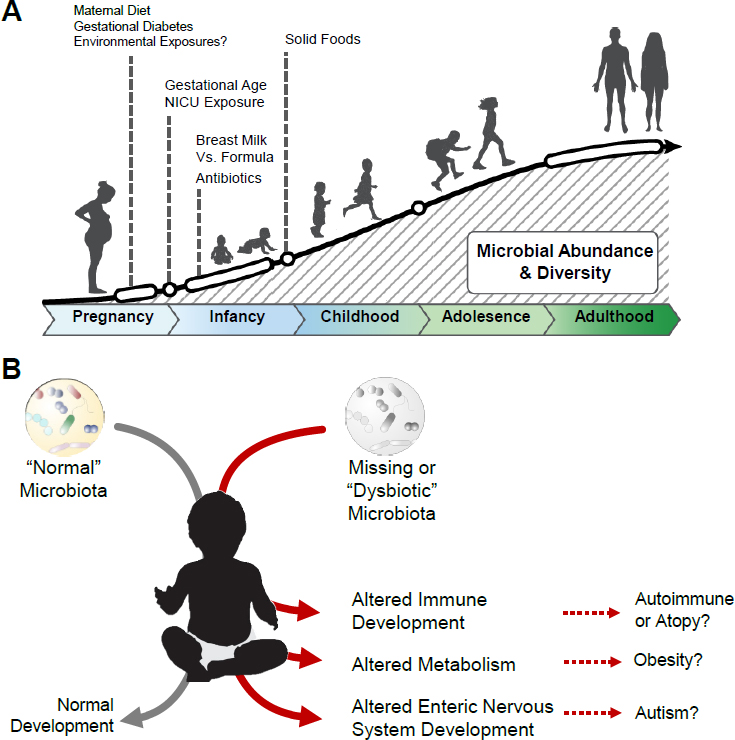
The greatest microbial biomass in humans is in the gastrointestinal tract (the gut). Colonization of the gut by microorganisms probably begins in utero, although the exact timing of colonization during development is not known (Jiménez et al. 2005; Steel et al. 2005; Dominguez-Bello et al. 2010; Gerritsen et al. 2011; Rautava et al. 2012; Aagaard et al. 2014; Ma et al. 2014a; Collado et al. 2016; Fallani 2016; Gibson et al. 2016; Yassour et al. 2016; Chu et al. 2017). As a result, the neonatal gut is not sterile but rather harbors pioneer species in a somewhat simplified community that expands by the age of 4–6 weeks (Chu et al. 2017). Early influential factors in gut microbiome development include gestational age at delivery (Gibson et al. 2016), infant feeding patterns (Graham-Rowe 2011; Walker et al. 2011), maternal dietary fat intake throughout gestation and lactation (Ma et al. 2014a; Chu et al. 2016), antibiotic use (Dethlefsen et al. 2008), and environmental exposures (MacFarlane and Cummings 1999; Roager et al. 2014).
Data on the effect of mode of delivery on neonatal and infant microbiome composition and function are mixed. Although initial small studies suggest a link between vaginal (vs cesarean) birth and neonatal gut microbiota (Dominguez-Bello et al. 2010), longer-term longitudinal studies conflict as to whether the robustness of the association holds true throughout infancy (Bäckhed et al. 2015; Yassour et al. 2016; Chu et al. 2017; Levin et al. 2016). Several studies have suggested that the underlying medical indication for a cesarean might be more influential than the cesarean surgery itself (Azad et al. 2013; Chu et al, 2016, 2017). In recognition of that suggestion, the American College of Obstetricians and Gynecologists (ACOG 2017) recently released an opinion that stated that “much of the research that exists regarding the link between cesarean delivery and incidence of allergies and autoimmune diseases has found an association with mode of delivery. However, there is still not enough evidence to prove causation due to the environmental, dietary and genetic factors that also impact the development of conditions, such
as asthma. Additionally, the microbiota of infants born by C-section will cause a variation in the research findings because some may have had contact with maternal vaginal bacteria if the procedure was performed after the onset of labor or rupture of membranes.”
Soon after birth, the neonatal gastrointestinal tract is exposed first to colostrum and then to breast milk, formula, or both; these exposures result in the development of microbial communities (Harmsen et al. 2000; Morelli 2008; Biesbroek et al. 2014). Over the first year of life, bacterial taxonomic diversity in the gut expands in parallel with contraction of fungal diversity in healthy infants (Fujimura et al. 2016). Several studies have indicated that at the age of about 3 years the phylum-level distribution of bacteria in the gut resembles that of adults (Palmer et al. 2007; Yatsunenko et al. 2012), but interindividual differences are substantial at lower taxonomic levels (Armugam et al. 2011). In addition to microbial composition, the functional attributes of the gut microbiome in infants, children, and adolescents differ substantially from those of adults (Lynch and Pedersen 2016). For example, infants, children, and adolescent gut microbiomes are richer than adult gut microbiomes in microbial pathways involved in microbial folate biosynthesis (Hollister et al. 2015). The compositional and functional differences indicate that the microbiome adapts as the human host develops and ages (see Figure 2-1).
Compared with the period of dynamic gut microbiome development in early life, healthy adults exhibit relatively stable gut microbiota composi-
tion and metagenomic content (Yatsunenko et al. 2012). Factors known to be associated with variation in the community and structure of the gut microbiome include age, environmental exposures, health status, genetics, socioeconomic status, geography, pregnancy, and diet. In addition, such other factors as exercise (O’Sullivan et al. 2015), antibiotic use (Dethlefsen and Relman 2011), and surgical interventions (Tremaroli et al. 2015) also play a role in shaping the gut microbiome. Of those factors, diet exerts a key and modifiable influence on the gut microbiome (Penders et al. 2006; Wu et al. 2011); both long-term and short-term eating habits have been shown to alter the microbiota of healthy adults (David et al. 2014b).
Dietary inputs provide nutritional substrates for the gut microbiota (Krajmalnik-Brown et al. 2012) and can also be a source of live microorganisms (David et al. 2014a,b). The amounts and composition of carbohydrates, proteins, and fats affect gut microbiota composition. Although all are important, resistant carbohydrate polymers—dietary fiber that is resistant to degradation by human enzymes—have been more widely accepted as an important microbiota-determining factor (Walker et al. 2011; David et al. 2014a). For example, De Filippo et al. (2010) showed that gut microbiota composition varied with dietary fiber consumption in children in Italian and African populations. Specifically, the high-fiber plant polysaccharide-based diet consumed by children who lived in Burkina Faso correlated with a greater diversity and relative abundance of cellulose-degrading Prevotella and Xylanibacter. In contrast, lower-fiber diets of children raised in Florence, Italy, were associated with lower abundances of Prevotella and increases in opportunistic gastrointestinal Enterobacteria (Shigella and Escherichia), which resulted in an increased capacity for simple-sugar uptake and metabolism. In a separate study, increased relative abundance of Prevotella species was also observed after a 10-day low-fat–high-fiber dietary intervention (Wu et al. 2011); a high-fat–low-fiber diet was correlated with increased relative abundance of Bacteroides. In addition to differences in composition, functional attributes of the gut microbiome are strongly influenced by diet, as evidenced by the enrichment of gut microbial genes that encode α-amylase (responsible for degradation of plant polysaccharides) in Malawian populations, whose primary dietary starch is maize, and the comparative enrichment of bacterial α-L-fucosidase in age-matched populations in the United States, where dietary simple sugars are abundant (Yatsunenko et al. 2012).
Rapid diet-related changes in gut microbiota have been detected after long-term and short-term intervention studies of healthy adults (Jumpertz et al. 2011; David et al. 2014b; Zeevi et al. 2015). Although changes in fiber intake constitute one of the most important factors in daily microbiota fluctuations, fat consumption and protein consumption are also related to microbiota composition (David et al. 2014a). High-fat diets increase the concentration of bile acids delivered to the colon, and a shift from a high-carbohydrate to a high-fat diet increased the abundance of bile-tolerant Alistipes, Bilophila, and Bacteroides; increased excretion of fecal short-chain fatty acids; and reduced the abundance of plant-polysaccharide degraders, such as Roseburia, Eubacterium rectale, and Ruminococcus bromii (Fava et al. 2013). Calorie content also influences the gut microbiome (Jumpertz et al. 2011); an increase by 1,000 kcal/day in caloric intake was associated with an increase in the relative abundance of Firmicutes and increased host-energy extraction (Jumpertz et al. 2011), a feature also associated with the gut microbiome of obese people (Ley et al. 2006; Turnbaugh et al. 2006).
Short-term and long-term dietary intervention studies have focused exclusively on healthy populations; however, in more heterogeneous and presumably more representative human populations, people exhibit distinct metabolic responses to identical meals (Zeevi et al. 2015). Using a machine-learning algorithm applied to blood glucose concentrations, dietary habits, and gut microbiome data, Zeevi et al. (2015) could predict a person’s postprandial glycemic response to specific meals. Their results indicate that the metabolic fate of dietary components is tightly linked to the activities of the gut microbiome. It has been demonstrated that chemicals ingested via the diet exert an effect on the gut microbiota and that consumption
of artificial sweeteners alters microbiota composition and can lead to insulin resistance (Suez et al. 2014).
Substantial differences in microbiome composition and function have been described among human populations distinguished by geography or ethnicity (De Filippo et al. 2010; Yatsunenko et al. 2012; Ma et al. 2014b). The differences have been attributed largely to distinct diets because diet clearly exerts a major selective pressure on the gut microbiome, as discussed above. However, confounding factors, such as host genetics and environmental microbial exposures, might also play a substantial role in the gut microbiome differences observed among populations of geographically segregated humans. Indeed, mounting evidence indicates that environmental microbiota exposures through residential house dust in early life (up to the age of 3 months) are related to development of or protection against allergy and asthma outcomes at the age of 3 or 7 years (Fujimura et al. 2010; Lynch et al. 2014; O’Connor et al. in press). Moreover, evidence from mouse models indicates that exposure to such microbiologically distinct residential house dusts differentially shapes gut microbiota composition and function in a manner that promotes or prevents development of protective airway and hematopoietic immune function after allergen or viral respiratory insult (Fujimura et al. 2014; Fonseca et al. 2017). For example, increased prevalence of allergic asthma in Hutterite children in the United States is associated with reduced exposure to environmental microorganisms in house dust, and nasal exposure of mice to house dust from Hutterite homes promoted proallergic responses after airway sensitization (Stein et al. 2016). The studies offer a plausible mechanism by which environmental microbial exposures in early life contribute to or protect against childhood disease development. Hence, the combination of environmental exposures and dietary selective pressure, particularly during the early-life period of microbiome development, appears to play a key role in determining how a person responds to later environmental exposures.
THE SKIN MICROBIOME
The skin makes up a vast and variable ecosystem that is comprised of about 1.8 m2 of discrete habitats that are both physically and chemically distinct (Grice and Segre 2011) and form a physical interface with the external environment. Using 10 healthy adult subjects, Grice et al. (2009) demonstrated that although microbial biomass is typically low on the skin surface, relatively reproducible patterns of bacterial and fungal microbial colonization are apparent at specific body sites. The site-specific community states are driven primarily by local ecologic conditions, particularly water availability and nutrition, which are relatively consistent in healthy humans at specific body sites but vary widely between body sites. Grice et al. (2009) also examined temporal stability of the skin microbiome by performing a repeat sampling of five subjects 4–6 months after the initial sampling. Microbiota composition was relatively stable at some sites—such as those associated with the ear canal, groin, and nose—but varied at others, including the armpit, forearm, and buttock. Those findings suggest that skin-associated microbiota compositional stability is site-specific.
On the healthy human skin surface, sites with high water availability are typically enriched in members of the Staphylococcus and Corynebacterium genera (Costello et al. 2009; Grice and Segre 2011), and sebaceous sites are selectively enriched in Propionibacterium (Leeming et al. 1984). The site-specific selective enrichment in Propionibacterium is due largely to its multiple encoded lipases that catalyze degradation of sebaceous lipids and provide this genus with a competitive colonization advantage. Degradation of sebaceous lipids produces free fatty acids (Marples et al. 1971), which both lower the microenvironmental pH (Elias 2007) and inhibit the growth of potentially pathogenic species, including Staphylococcus aureus and Streptococcus pyogenes, while promoting the growth of coagulase-negative species, such as some members of the Corynebacterium and Staphylococcus genera (Korting et al. 1990). Studies of fungal species that colonize the skin surface
are less common than bacterial investigations, but the studies that have been performed indicate that Malassezia forms a large portion (53–80%) of the skin-associated fungal biomass; variations in relative abundance depend on skin site (Gao et al. 2010).
A more recent metagenomic study of 18 skin sites in 15 healthy adults revealed that only about 30% of microbial functional gene content, primarily encoding processes essential to microbial growth and metabolism, was conserved (maintained) across body sites (Oh et al. 2014). The remaining functional gene content exhibited substantial variation between skin sites. Microbial metabolic diversity was lowest in sebaceous sites, which coincidentally exhibited lower taxonomic diversity than nonsebaceous skin sites (Oh et al. 2014). However, microbial communities in sebaceous sites exhibited a preponderance of fungal pathways, including those involved in the cell cycle, DNA replication, transcription, translation, protein degradation, and fungus-encoded vitamin D2 biosynthetic genes. Microbial communities in nonsebaceous sites exhibited increased capacity for sulfate, glutamate, aspartame, L- or branched amino acids, and sorbitol transport and putrescine or spermidine biosynthesis and transport. The results indicate that there is great chemical diversity, which the microorganisms in those anatomic niches use to their advantage.
Although most studies have examined topographic variation in the skin microbiome in healthy populations, studies that have examined site-specific dermal microbiomes in healthy and diseased states have demonstrated that disease is associated with perturbations of the composition of the microbiota and its metagenome—findings consistent with those in other anatomic sites (Barnard et al. 2016). Thus, although the prevailing conditions at a given skin habitat influence the microbial colonization pattern and the functional genetic capacity of the communities in a relatively predictable manner, individual skin-associated microbial signatures have a remarkable range. That observation suggests that the microbial potential to transform or sequester dermal environmental chemical exposures depends on the body site, the individual, and the individual’s health status.
Age, sex, and geography are also associated with skin microbiota heterogeneity. Microbial colonization of the skin is thought to begin during the perinatal and postnatal period. Costello et al. (2013) demonstrated in a small cohort of premature neonates that were sampled repeatedly over the first 3 weeks of life that of all the sites sampled (skin, saliva, and stool), the skin microbiota most resembled that of an adult. More recently, a study of mother–infant pairs demonstrated that the skin microbiota, although similar to the oral and fecal microbiota at birth, exhibits site-specific differentiation as early as the age of about 4–6 weeks (Chu et al. 2017). Culture-based studies have demonstrated that puberty-associated alterations in sebum production correspond with the quantity of skin-associated lipophilic bacteria (Somerville 1969). Moreover, sex-based differences in skin microbiota have been described and are associated with physiologic and anatomic differences in sweat, sebum, and hormone production that occur in males and females, particularly during puberty (Marples 1982; Fierer et al. 2008; Giacomoni et al. 2009). Exogenous factors that influence the skin microbiota include prevailing temperature and humidity, increases in which are associated with increased bacterial numbers on the underarms, back, and feet (McBride et al. 1977). Conversely, exposure to ultraviolet (UV) radiation is bactericidal; thus, gradients of UV exposure associated with longitude or latitude are thought to contribute to geographic variation in skin microbiota, although a large number of confounding factors co-vary with UV exposure in spatially separated geographic locales.
THE RESPIRATORY MICROBIOME
Research on the respiratory microbiome, particularly in the lungs, is still relatively sparse compared with investigation of the gut microbiome. In fact, knowledge regarding site-specific microbiota composition in both the upper respiratory tract and lower respiratory tract has increased rapidly in
the last 5 years.1 Invasive sampling of the lower airways for research studies is difficult to justify in otherwise healthy infants and children, so nasopharyngeal sampling that uses swabs, aspirates, or brushings has been pursued. Studies of healthy children reveal significant changes in nasopharyngeal bacterial composition related to age and delivery method (Biesbroek et al. 2014; Bosch et al. 2016); given age-related variation, age is an important factor to consider in the design of cross-sectional respiratory microbiome studies. The focus, however, has been largely on early life (such as up to 24 months), and the dynamics of the nasopharyngeal microbiota in healthy older children and adults are underexplored.
Recent studies that used bronchoscopy to sample the lower respiratory tract or lungs in healthy people and that used culture-independent analyses have consistently demonstrated the presence of a microbial community (Dickson et al. 2014, 2015, 2017; Bassis et al. 2015). However, the overall dynamics of community stability in the lower airways of healthy people without evident lung disease remains a matter of debate. Numerous physiologic and anatomic factors play a role in determining the composition of the respiratory microbiota and its regional variation in the respiratory tract (Dickson et al. 2014). Factors include differences in oxygen tension, airway luminal temperature, mucociliary clearance mechanisms, and other innate defenses. Moreover, microaspiration of upper airway and oropharyngeal secretions is common and often asymptomatic even in healthy persons and likely leads to microbial colonization of the respiratory tract (Huxley et al. 1978).
Given the much lower microbial biomass found in the lungs than in the oropharynx or intestinal tract, it is important to emphasize that substantial attention must be paid to study design, sample collection, processing protocols, and collection of reagent controls in analyzing and interpreting findings. In light of those considerations, researchers have conducted detailed topographic study of the microbiota along the tracheobronchial tree and demonstrated microanatomic variability (Bassis et al. 2015; Dickson et al. 2017). Bacterial load and ecologic measures of mouth–lung similarity peak at or near the tracheal bifurcation, and this finding supports the hypothesis that in healthy persons microaspiration is the most likely route by which the lower respiratory tract receives and becomes colonized by bacteria (Dickson et al. 2017). However, studies on bacterial burden, community diversity, and mouth–lung similarities can yield different results that depend on the sampling methods used; the varied results reflect differences in the sampled surface areas regardless of health or disease status and differences between the lower and upper respiratory tract (Denner et al. 2016; Perez-Losada et al. 2016; Dickson et al. 2017). The collective findings in healthy people highlight some of the intrinsic factors in the variability in data from studies of the respiratory microbiome that must be considered in developing study protocols and designs.
Emerging evidence suggests that bacteria commonly found as part of the “normal” lung microbiome might shape immune responses in the lung. For example, two recent studies suggest that a lung bacterial community that is enriched primarily in members of the Veillonella and Prevotella genera (supraglottic bacteria often found in the oropharynx) is associated with lung inflammation, as manifested by increased lymphocytes and neutrophils in bronchoalveolar-lavage fluid. Moreover, it is striking and somewhat counterintuitive that studies have not shown associations between cigarette-smoking history or smoking cessation and alterations in lower-airway bacterial microbiota composition; instead, changes are associated with the oral microbiota composition (Morris et al. 2013; Einarsson et al. 2016; Munck et al. 2016; Segal et al. 2016).
The composition of the microbiome in the lower respiratory tract of people who have chronic airway disease clearly differs from that of healthy people. Most studies have focused on patients who have cystic fibrosis, chronic obstructive pulmonary disease (COPD), or asthma. Those people all have impaired or dysregulated immune responses that might magnify the microbial perturbations ob-
___________________
1 As in clinical practice, the upper respiratory tract and lower respiratory tract are distinguished here by partitioning relative to the epiglottis.
served in studies that examine the respiratory microbiome in healthy and diseased people. Intrinsic airway defenses—such as mucociliary clearance, epithelial barrier function, and innate immune functions, including the secretion of antimicrobial peptides—all work to mitigate potentially detrimental inhaled exposures. Those mechanisms become impaired in chronic airway disease to various extents. It is also well recognized that chronic airway diseases are clinically heterogeneous. Indeed, differences in underlying immune-response profiles and molecular phenotypes distinguish some presentations of asthma and COPD. Thus, it is likely that complex interactions among a variety of factors—including environmental exposures, genetic risk, and immune phenotype—shape airway-disease susceptibility and clinical manifestations and prognosis (Han et al. 2010; Huang and Boushey 2015; Huang et al. 2017).
Adding to that knowledge base, recent studies of the respiratory microbiome in cohorts of airway-disease patients have revealed important interindividual heterogeneity in microbiota composition in the upper respiratory tract and the lower respiratory tract (Cox et al 2010; Bogaert et al. 2011; Erb-Downward et al. 2011; Biesbroek et al. 2014; Zhao et al. 2014; Huang et al. 2015; Einarsson et al. 2016; Durack et al. 2017). Moreover, significant associations between clinical features of host disease and patterns of microbiota composition and predicted microbial functions have been shown and suggest potential mechanistic links. Lower-airway enrichment in members of the Proteobacteria phylum, in particular, has consistently been associated with chronic airway disease and with clinical outcomes in COPD or asthma. Those relationships between the microbiome and disease phenotype include microbiota enrichment patterns linked to worse lung function, airway reactivity, and symptom control, and to different airway immune-response profiles, including type 2 and nontype 2 inflammatory responses (Huang et al. 2011, 2015; Denner et al. 2016; Wang et al. 2016; Durack et al. 2017). Moreover, different medications can have profoundly different effects on the airway microbiome, as has been reported with antibiotics and corticosteroid administration (Huang et al. 2014; Wang et al. 2016; Durack et al. 2017). In addition, the bronchial microbiome of asthmatic people who did not respond to a trial of inhaled corticosteroid therapy was enriched in predicted microbial pathways involved in chemical metabolism, and this finding suggests that the presence of some airway microorganisms could influence biotransformation of synthetic therapeutic drugs (Durack et al. 2017). The recent insights from studies of patients who have chronic respiratory diseases highlight the importance of understanding microorganism–host interactions in well-characterized clinical contexts because both the microbiome and the host phenotype can vary greatly.
VARIATION BETWEEN HUMAN AND ANIMAL MICROBIOMES
Animal models have long been a mainstay of experimental biology because of their intrinsic similarities to humans in anatomy, physiology, and genetics. They also provide genetically and microbiologically manipulable systems for studies that are untenable in humans. Most host–microbiome studies in animal models have been performed in mice. Their relatively short reproductive and life cycles make them an economical option for study of microbiome perturbations in a controlled experimental setup that allows the assessment of causality. A large number of mouse-based microbiome studies have contributed invaluable information on host–microbiome interactions. However, translation of results of microbiome studies from mouse to human systems can be difficult because of differences among mammalian species. For example, mouse and human skin surfaces clearly differ substantially. A recent genomewide transcriptomic study of skin-specific expression of human or mouse genes identified only a 30% overlap, which the authors offered as an explanation of why results generated with skin-associated mouse models fail to translate to humans (Gerber et al. 2014). Likewise, although the mouse gut and the human gut have similarities—for example, the ratio of mucosal to body-surface area is similar among species (Casteleyn et al. 2010)—distinct sections of the gut have substantial differences in this ratio.
There are other differences in human and mouse gut anatomy: the mouse gut lacks an appendix and has a nonglandular foregut and glandular stomach, taller villi, fermentative metabolism in the cecum, a smooth colon with no divisions, paneth cells only in the small intestine, and abundant goblet cells in the proximal colon (Casteleyn et al. 2010). In addition to spatial differences between the mouse gut and the human gut in the distribution of antimicrobial-producing paneth and mucin-secreting goblet cells, mice encode additional toll-like receptors (proteins on cell surfaces that sense and respond to microorganisms). Mouse immune development is also distinct from that of humans; for example, the CD4+ population in mice develops in the postnatal period (Landreth 2002), whereas human CD4+ populations begin to mature in utero (Zlotoff et al. 2008). Other established immunologic distinctions between humans and mice include the relative ratio of leukocytes (humans have relatively more neutrophils and fewer lymphocytes than mice); the types of antimicrobial defensins (humans express only two intestinal defensins whereas mice express more than 20); the induction of nitric oxide synthase, which is inconsistently induced from human macrophages but reproducibly induced by IFN-γ and LPS in mouse macrophages; and differences in signaling molecules and B-cell and T-cell development and regulation (Mestas and Hughes 2004).
Not surprisingly, the anatomic and immunologic distinctions are associated with important differences in the composition of the mouse and human microbiomes. Using 16S rRNA profiling, Frorath et al. (1991) found that about 85% of bacterial genera that were detected in the mouse gastrointestinal tract were not detected in humans. However, using a higher-resolution approach and 32 gut samples from 16 human subjects and 88 samples from three mouse strains, Krych et al. (2013) found that 89% (80 of 89) of the prevalent bacterial genera were present in both humans and mice. A more recent meta-analysis of mouse gut and human gut microbiotas identified 79 genera that were detected in both, but the study revealed that the relative abundances of many of the dominant organisms were distinct (Nguyen et al. 2015). Alterations in the relative quantities of distinct species affect microbial interspecies interactions, which rely on quorum signaling—the process of sensing and responding to concentrations of microbial-derived chemical signals that allow species to determine the burden and activities of the species in their immediate environment and alter their gene expression accordingly (Papenfort and Bassler 2016). Such compositional alterations in both the species and their relative distribution in microbial communities could have important effects on the functional output of the microbiome. It should be noted that no study has examined overlap in fungal or viral population among humans and mammalian model systems, nor have the functional attributes of these communities been assessed. Furthermore, because previous studies have compared only the taxonomic composition of mouse and human microbiomes, functional attributes of the microbial communities might be more similar than their taxonomic composition would suggest. Nonetheless, given the breadth of microbial diversity known to exist in humans and the differences between human and mouse models, observations made in mice, although informative and foundational, might not capture the full breadth of microbial interactions that exist in situ in the human host.
To overcome the issues of microbial differences between mice and humans, several studies have used “humanized” mice—previously germfree mice that have been inoculated with microbial species found in human stool (Chung et al. 2012; Smith et al. 2012; Ridaura et al. 2013). Personalized culture collections have been valuable in the experimental approach in validating the results of human-to-mouse fecal transfers and in providing a platform to determine which components are important (Ridaura et al. 2013). The studies also have been instrumental in, for example, understanding gut microbial responses to dietary changes. However, humanized mice, like bioreactor systems, do not fully recapitulate the microbial diversity of the human gut microbiome (Auchtung et al. 2015; Griffin et al. 2017). Therefore, although humanized model systems might be useful in promoting a fundamental understanding of causality or micro-
bial dynamics in response to perturbation, the relevance of such mouse models to microbiome responses in humans must be interpreted cautiously.
FINDINGS
- Population-based studies have identified multiple factors related to the observed life span and body-site variation in the composition, gene content, and function of the human microbiome. The factors include age, environmental exposures, disease state, genetics, sex, socioeconomic status, geography, pregnancy status, and diet.
- Body site is a key factor in the variation observed in the human microbiome, and each body site can be characterized by specific bacterial species and other microorganisms that have adapted to the specific environment. The site-specific differences in microbial composition yield differences in metabolic capacity and in aggregate function of the human microbiome.
- Age and diet play primary roles in the variation observed in the gut microbiome. However, the combination of environmental exposures and dietary selective pressure, particularly during the early-life period of gut microbiome development, might play a key role in determining how a person responds to later environmental exposures.
- The site-specific community states in the skin microbiome are driven primarily by local ecologic conditions, particularly water and nutrient availability, which are relatively consistent in healthy humans at a specific body site but vary widely between body sites. However, skin-associated microbiota compositional stability appears to be site-specific.
- Numerous physiologic and anatomic factors play a role in determining the composition of the respiratory microbiota and its regional variation within the respiratory tract. This field of study is relatively new, but research indicates that important factors include differences in oxygen tension, airway luminal temperature, mucociliary clearance mechanisms, and other innate defenses.
- Mice and other animal models have been useful in studying host–microbiome interactions, including “humanized” mice that allow researchers to test the effects of a specific human microbiome on host biology. However, differences between humans and mice in anatomy, immunology, and microbiome composition can present challenges for translating results between these hosts. Observations made in mice and other animal models, although informative and foundational, might not capture the full breadth of microbial interactions that occur in human hosts.
REFERENCES
Aagaard, K., K. Riehle, J. Ma, N. Segata, T.A. Mistretta, C. Coafa, S. Raza, S. Rosenbaum, I. Van den Veyver, A. Milosavljevic, D. Gevers, C. Huttenhower, J. Petrosino, and J. Versalovic. 2012. A metagenomics approach to characterization of the vaginal microbiome signature in pregnancy. PLoS ONE 7(6):e36466.
Aagaard, K., J. Petrosino, W. Keital, M. Watson, J. Katancik, N. Garcia, S. Patel, M. Cutting, T. Madden, H. Hamilton, E. Harris, D. Gevers, G. Simone, P. McInnes, and J. Versalovic. 2013. The Human Microbiome Project strategy for comprehensive sampling of the human microbiome and why it matters. FASEB J. 27(3):1012-1022.
Aagaard, K., J. Ma, K.M. Antony, R. Ganu, J. Petrosino, and J. Versalovic. 2014. The placenta harbors a unique microbiome. Sci. Transl. Med. 6:237ra65.
ACOG (American College of Obstetrician Gynecologists). 2017. Vaginal Seeding not Recommended for Infants. News: October 24, 2017 [online]. Available: https://www.acog.org/About-ACOG/News-Room/News-Releases/2017/Vaginal-Seeding-Not-Recommended-for-Infants {accessed November 13, 2017].
Armugam, M., J. Raes, E. Pelletier, D. Le Paslier, T. Yamada, D.R. Mende, G.R. Fernandes, J. Tap, T. Bruls, J.M. Batto, M. Bertalan, N. Borruel, F. Casellas, L. Fernandez, L. Gautier, T. Hansen, M. Hattori, T. Hayashi, M. Kleerebezem, K. Kurokawa, M. Leclerc, F. Levenez, C. Manichanh, H.B. Nielsen, T. Nielsen, N. Pons, J. Poulain, J. Qin, T. Sicheritz-Ponten, S. Tims, D. Torrents, E. Ugarte, E.G. Zoetendal, J. Wang, F. Guarner, O. Pedersen, W.M. De Vos, S. Brunak, J. Dore, Meta HITC, M. Antolin, M F. Artiguenave, H.M. Blottiere, M. Almeida, C. Brechot, C. Cara, C. Chervaux, A. Cultrone, C. Delorme, G. Denariaz, R. Dervyn, K.U. Foerstner, C. Friss, M. Van de Guchte, E. Guedon, F. Haimet, W. Huber, J. Van Hylckama-Vlieg, A. Jamet, C. Juste, G. Kaci, J. Knol, O.
Lakhdari, S. Layec, K. Le Roux, E. Maguin, A. Merieux, R.M. Minardi, C. M’Rini, J. Muller, R. Oozeer, J. Parkhill, P. Renault, M. Rescigno, N. Sanchez, S. Sunagawa, A. Torrejon, K. Turner, G. Vandemeulebrouck, E. Varela, Y. Winogradsky, G. Zeller, J. Weissenbach, S.D. Ehrlich, and P. Bork. 2011. Enterotypes of the human gut microbiome. Nature 473(7346):174-180.
Auchtung, J.M., C.D. Robinson, and R.A. Britton. 2015. Cultivation of stable, reproducible microbial communities from different fecal donors using minibioreactor arrays (MBRAs). Microbiome 3:42.
Azad, M.B. T. Konya, H. Maughan, D.S. Guttman, C.J. Field, R.S. Chari, M.R. Sears, A.B. Becker, J.A. Scott, and A.L. Kozyrskyj. 2013. Gut microbiota of healthy Canadian infants: Profiles by mode of delivery and infant diet at 4 months. CMAJ 185(5):385-394.
Bäckhed, F., J.K. Manchester, C.F. Semenkovich, and J.I. Gordon. 2007. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc. Natl. Acad. Sci. USA 104(3):979-984.
Bäckhed, F., J. Roswall, Y. Peng, Q. Feng, H. Jia, P. Kovatcheva-Datchary, Y. Li, Y. Xia, H. Xie, H. Zhong, M.T. Khan, J. Zhang, J. Li, L. Xiao, J. Al-Aama, D. Zhang, Y.S. Lee, D. Kotowska, C. Colding, V. Tremaroli, Y. Yin, S. Bergman, X. Xu, L. Madsen, K. Kristiansen, J. Dahlgren, and J. Wang. 2015. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe 17(5):690-703.
Barnard, E., B. Shi, D. Kang, N. Craft, and H. Li. 2016. The balance of metagenomic elements shapes the skin microbiome in acne and health. Sci. Rep. 6:39491.
Bassis, C.M., J.R. Erb-Downward, R.P. Dickson, C.M. Freeman, T.M. Schmidt, V.B. Young, J.M. Beck, J.L. Curtis, and G.B. Huffnagle. 2015. Analysis of the upper respiratory tract microbiotas as the source of the lung and gastric microbiotas in healthy individuals. mBio 6(2):e00037-15.
Biesbroek, G., A.A. Bosch, X. Wang, B.J. Keijser, R.H. Veenhoven, E.A. Sanders, and D. Bogaert. 2014. The impact of breastfeeding on nasopharyngeal microbial communities in infants. Am. J. Respir. Crit. Care Med. 190(3):298-308.
Bogaert, D., B. Keijser, S. Huse, J. Rossen, R. Veenhoven, E. van Glis, J. Bruin, R. Montijn, M. Bonten, and E. Sanders. 2011. Variability and diversity of nasopharyngeal microbiota in children: A metagenomic analysis. PLoS ONE 6(2):e17035.
Bosch, A.A., E. Levin, M.A. van Houten, R. Hasrat, G. Kalkman, G. Biesbroek, W.A. de Steenhuijsen Piters, P.K. de Groot, P. Pernet, B.J. Keijser, E.A. Sanders, and D. Bogaert. 2016. Development of upper respiratory tract microbiota in infancy is affected by mode of delivery. EBioMedicine 9:336-345.
Cani, P.D., A.M. Neyrinck, F. Fava, C. Knauf, R.G. Burcelin, K.M. Tuohy, G.R. Gibson, and N.M. Delzenne. 2007. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia 50(11):2374-2383.
Casteleyn, C., A. Rekecki, A. Van der Aa, P. Simoens, and W. Van den Broeck. 2010. Surface area assessment of the murine intestinal tract as a prerequisite for oral dose translation from mouse to man. Lab. Anim. 44(3):176-183.
Chu, D.M., K.M. Antony, J. Ma, A.L. Prince, L. Showalter, M. Moller, and K.M. Aagaard. 2016. The early infant gut microbiome varies in association with a maternal high-fat diet. Genome Med. 8(1):77.
Chu, D.M., J. Ma, A.L. Prince, K.M. Anthony, M.D. Seferovic, and K.M. Aagaard. 2017. Maturation of the infant microbiome community structure and function across multiple body sites and in relation to mode of delivery. Nat. Med. 23(3):314-326.
Chung, H., S.J. Pamp, J.A. Hill, N.K. Surana, S.M. Edelman, E.B. Troy, N.C. Reading, E.J. Villablanca, S. Wang, J.R. Mora, Y. Umesaki, D. Mathis, C. Benoist, D.A. Relman, and D.L. Kasper. 2012. Gut immune maturation depends on colonization with a host-specific microbiota. Cell 149(7):1578-1593.
Collado, M.C., S. Rautava, J. Aakko, E. Isolauri, and S. Salminen. 2016. Human gut colonization may be intitiated in utero by distinct microbial communities in the placenta and amniotic fluid. Sci. Rep. 6:23129.
Costello, E.K., C.L. Lauber, M. Hamady, N. Fierer, J.I. Gordon, and R. Knight. 2009. Bacterial community variation in human body habitats across space and time. Science. 326(5960):1694-1697.
Costello, E.K., E.M. Carlisle, E.M. Bik, M.J. Morowitz, and D.A. Relman. 2013. Microbiome assembly across multiple body sites in low-birthweight infants. MBio 4(6):e00782-13.
Cox, M.J., M. Allgaier, B. Taylor, M.S. Baek, Y.J. Huang, R.A. Daly, U. Karaoz, G.L. Andersen, R. Brown, K.E. Fujimura, B. Wu, D. Tran, J. Koff, M.E. Kleinhenz, D. Nielson, E.L. Brodie, and S.V. Lynch. 2010. Airway mi-
crobiota and pathogen abundance in age-stratified cystic fibrosis patients. PLoS ONE 5:e11044.
David, L., A. Materna, J. Friedman, M. Campos-Baptista, M. Blackburn, A. Perrotta, S. Erdman, and E. Alm. 2014a. Host lifestyle affects human microbiota on daily timescales. Genome Biol. 15(7): R89.
David, L.A., C.F. Maurice, R.N. Carmody, D.B. Gootenberg, J.E. Button, B.E. Wolfe, A.V. Ling, A.S. Devlin, Y. Varma, M.A. Fischbach, S.B. Biddinger, R.J. Dutton, and P.J. Turnbaugh. 2014b. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505(7484):559-563.
De Filippo, C., D. Cavalieri, M. Di Paola, M. Ramazzotti, J.B. Poullet, S. Massart, S. Collini, G. Pieraccini, and P. Lionetti. 2010. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA 107(33):14691-14696.
Denner, D.R., N. Sangwan, J.B. Becker, D.K. Hogarth, J. Oldham, J. Castillo, A. Sperling, J. Solway, E.T. Naureckas, J.A. Gilbert, and S.R. White. 2016. Corticosteroid therapy and airflow obstruction influence the bronchial microbiome, which is distinct from that of bronchoalveolar lavage in asthmatic airways. J. Allergy Clin. Immunol. 137(5):1398-1405.
Dethlefsen, L., and D.A. Relman. 2011. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc. Natl. Acad. Sci. USA 108(Suppl. 1):4554-4561.
Dethlefsen, L., S. Huse, M.L. Sogin, and D.A. Relman. 2008. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PloS Biol. 6(11):e280.
Devaraj, S., P. Hemarajata, and J. Versalovic. 2013. The human gut microbiome and body metabolism: Implications for obesity and diabetes. Clin. Chem. 59(4):617-628.
Dickson, R.P., J.R. Erb-Downward, H.C. Prescott, F. Martinez, J.L. Curtis, V.N. Lama, and G.B. Huffnagle. 2014. Cell-associated bacteria in the human lung microbiome. Microbiome 2:28.
Dickson, R.P., J.R. Erb-Downward, C.M. Freeman, L. McCloskey, J.M. Beck, G.B. Huffnagle, and J.L. Curtis. 2015. Spatial variation in the healthy human lung microbiome and the adapted island model of lung biogeography. Ann. Am. Thorac. Soc. 12(6):821-830.
Dickson, R.P., J.R. Erb-Downward, C.M. Freeman, L. McCloskey, N.R. Falkowski, G.B. Huffnagle, and J.L. Curtis. 2017. Bacterial topography of the healthy human lower respiratory tract. MBio 8(1):e02287-16.
Ding, T., and P.D. Schloss. 2014. Dynamics and associations of microbial community types across the human body. Nature 509(7500):357-360.
Dominguez-Bello, M.G., E.K. Costello, M. Contreras, M. Magris, G. Hidalgo, N. Fierer, and R. Knight. 2010. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc. Natl. Acad. Sci. USA 107(26):11971-11975.
Durack, J., S.V. Lynch, S. Nariya, N.R. Bhakta, A. Beigelman, M. Castro, A.M. Dyer, E.Israel, M. Kraft, R.J. Martin, D.T. Mauger, S.R. Rosenberg, T. Sharp-King, S.R. White, P.G. Woodruff, P.C. Avila, L.C. Denlinger, F. Holgun, S.C. Lazarus, N. Lugogo, W.C. Moore, S.P. Peters, L. Que, L.J. Smith, C.A. Sorkness, M.E. Wechsler, S.E. Wenzel, H.A. Boushey, and Y.J. Huang. 2017. Features of the bronchial bacterial microbiome associated with atopy, asthma and responsiveness to inhaled corticosteroid treatment. J. Allergy Clin. Immunol. 140(1):63-75.
Einarsson, G.G., D.M. Comer, L. McIlreavey, J. Parkhill, M. Ennis, M.M. Tunney, and J.S. Elborn. 2016. Community dynamics and the lower airway microbiota in stable chronic obstructive pulmonary disease, smokers and healthy non-smokers. Thorax 71(9):795-803.
Elias, P.M. 2007. The skin barrier as an innate immune element. Semin. Immunopathol. 29(1):3-14.
Erb-Downward, J.R., D.L Thompson, M.K Han, C.M. Freeman, L. McCloskey, L.A Schmidt, V.B Young, G.B Toews, J.L Curtis, B. Sundaram, F.J Martinez, and G.B Huffnagle. 2011. Analysis of the lung microbiome in the “healthy” smoker and in COPD. PLoS ONE 6(2):e16384.
Fallani, M., D. Young, E. Norin, S. Amarri, R. Adam, M. Aguilera, S. Khanna, A. Gil, C.A. Edwards, and J. Doré. 2010. Intestinal microbiota of 6-week-old infants across Europe: Geographic influence beyond delivery mode, breast-feeding, and antibiotics. J. Pediatr. Gastroenterol. Nutr. 51(1):77-84.
Fava, F., R. Gitau, B.A. Griffin, G.R. Gibson, K.M. Tuohy, and J.A. Lovegrove. 2013. The type and quantity of dietary fat and carbohydrate alter faecal microbiome and short-chain fatty acid excretion in a metabolic syndrome ‘at-risk’ population. Int. J. Obes. 37(2):216-223.
Fierer, N., M. Hamady, C.L. Lauber, and R. Knight. 2008. The influence of sex, handedness, and washing on the diversity of hand surface bacteria. Proc. Natl. Acad. Sci. USA 105(46):17994-17999.
Fonseca, W., K. Lucey, S. Jang, K.E. Fujimura, A. Rasky, H.A. Ting, J. Petersen, C.C. Johnson, H.A. Boushey, E. Zoratti, D.R. Ownby, A.M. Levine, K.R. Bobbit, S.V. Lynch, and N.W. Lukacs. 2017. Lactobacillus johnsonii supplementation attenuates respiratory viral infection via metabolic reprogramming and immune cell modulation. Mucosal. Immunol. 10(6):1569-1580.
Franzosa, E.A., T. Hsu, A. Sirota-Madi, A. Shafquat, G. Abu-Ali, X.C. Morgan, and C. Huttenhower. 2015. Sequencing and beyond: Integrating molecular ‘omics’ for microbial community profiling. Nat. Rev. Microbiol. 13(6):360-372.
Frorath, B., M. Scanarini, H.J. Netter, C.C. Abney, B. Liedvogel, H.J. Lakomek, and W. Northermann. 1991. Cloning and expression of antigenic epitopes of the human 68-kDa (U1) ribonucleoprotein antigen in Escherichia coli. Biotechniques 11(3):364-366.
Fujimura, K.E., C.C. Johnson, D.R. Ownby, M.J. Cox, E.L. Brodie, S.L. Havstad, E.M. Zoratti, K.J. Woodcroft, K.R. Bobbitt, G. Wegienka, H.A. Boushey, and S.V. Lynch. 2010. Man’s best friend? The effect of pet ownership on house dust microbial communities. J. Allergy Clin. Immunol. 126(2):410-412.
Fujimura, K.E., T. Demoor, M. Rauch, A.A. Faruqi, S. Jang, C.C. Johnson, H.A. Boushey, E. Zoratti, D. Ownby, N.W. Lukacs, and S.V. Lynch. 2014. House dust exposure mediates gut microbiome Lactobacillus enrichment and airway immune defense against allergens and virus infection. Proc. Natl. Acad. Sci. USA 111(2):805-810.
Fujimura, K.E., A.R. Sitarik, S. Havstad, D.L. Lin, S. Levan, D. Fadrosh, A.R. Panzer, B. LaMere, E. Rackaityte, N.W. Lukacs, G. Wegienka, H.A. Boushey, D.R. Ownby, E.M. Zoratti, A.M. Levin, C.C. Johnson, and S.V. Lynch. 2016. Neonatal gut microbiota associates with childhood multisensitized atopy and T-cell differentiation. Nat. Med. 22(10):1187-1191.
Gao, Z., G.I. Perez-Perez, Y. Chen, and M.J. Blaser. 2010. Quantitation of major human cutaneous bacterial and fungal populations. J. Clin. Microbiol. 48(10):3575-3581.
Gerber, P.A., B.A. Buhren, H. Schrumpf, B. Homey, A. Zlotnik, and P. Hevezi. 2014. The top skin-associated genes: A comparative analysis of human and mouse skin transcriptomes. Biol. Chem. 395(6):577-591.
Gerritsen, J., H. Smidt, G.T. Rijkers, and W.M. de Vos. 2011. Intestinal microbiota in human health and disease: The impact of probiotics. Genes Nutr. 6(3):209-240
Giacomoni, P.U., T. Mammone, and M. Teri. 2009. Gender-linked differences in human skin. J. Dermatol. Sci. 55(3):144-149.
Gibson, M.K., B. Wang, S. Ahmadi, C.A. Burnham, P.I. Tarr, B.B. Warner, and G. Dantas. 2016. Developmental dynamics of the preterm infant gut microbiota and antibiotic resistome. Nat. Microbiol. 1:16024.
Goodrich, J.K., J.L. Waters, A.C. Poole, J.L. Sutter, O. Koren, R. Blekhman, M. Beaumont, W. Van Treuren, R. Knight, J.T. Bell, T.D. Spector, A.G. Clark, and R.E. Ley. 2014. Human genetics shape the gut microbiome. Cell 159(4):789-799.
Gophna, U., K. Sommerfeld, S. Gophna, W.F. Doolittle, and S.J.O. Veldhuyzen van Zanten. 2006. Differences between tissue-associated intestinal microfloras of patients with Crohn’s disease and ulcerative colitis. J. Clin. Microbiol. 44(11):4136-4141.
Graham-Rowe, D. 2011. Lifestyle: When allergies go west. Nature 479(7374):S2-S4.
Grice, E.A., and J.A. Segre. 2011. The skin microbiome. Nat. Rev. Microbiol. 9(4):244-253.
Grice, E.A., H.H. Kong, S. Conlan, C.B. Deming, J. Davis, A.C. Young, NISC Comparative Sequencing Program, G.G. Bouffard, R.W. Blakesley, P.R. Murray, E.D. Green, M.L. Turner, and J.A. Segre. 2009. Topographical and temporal diversity of the human skin microbiome. Science 324(5931):1190-1192.
Griffin, N.W., P.P. Ahern, J. Cheng, A.C. Heath, O. Ilkayeva, C.B. Newgard, L. Fontana, and J.I. Gordon. 2017. Prior dietary practices and connections to a human gut microbial metacommunity alter responses to diet interventions. Cell Host Microbe 21(1):84-96.
Han, M.K., A. Agusti, P. Calverley, B.R. Celli, G. Criner, J.L. Curtis, L.M. Fabbri, J.G. Goldin, P.W. Jones, W. Mac-nee, B.J. Make, K.F. Rabe, S.I. Rennard, F.C. Sciurba, E.K. Silverman, J. Vestbo, G.R. Washko, E.F. Wouters, and F.J. Martinez. 2010. Chronic obstructive pulmonary disease phenotypes: The future of COPD. Am. J. Respir. Crit. Care Med. 182(5):598-604.
Harmsen, H.J.M., A.C.M. Wildeboer-Veloo, G.C. Raangs, A.A. Wagendorp, N. Klijn, J.G. Bindels, and G.W. Welling. 2000. Analysis of intestinal flora development in breast-fed and formula-fed infants by using molecular identification and detection methods. J. Pediatr. Gastroenterol. Nutr. 30(1):61-67.
HMP (Human Microbiome Project) Consortium. 2012a. Structure, function and diversity of the healthy human microbiome. Nature 486(7402):207-214.
HMP Consortium. 2012b. A framework for human microbiome research. Nature 486(7402):215-221.
Hollister, E.B., K. Riehle, R.A. Luna, E.M. Weidler, M. Rubio-Gonzales, T.A. Mistretta, S. Raza, H.V. Doddapaneni, G.A. Metcalf, D.M. Muzny, R.A. Gibbs, J.F. Petrosino, R.J. Shulman, and J. Versalovic. 2015. Structure and function of the healthy pre-adolescent pediatric gut microbiome. Microbiome 3:36.
Huang, Y.J., and H.A. Boushey. 2015. The microbiome in astma. J. Allergy Clin. Immunol. 135(1):25-30.
Huang, Y.J., C.E. Nelson, E.L. Brodie, T.Z. Desantis, M.S. Baek, J. Liu, T. Woyke, M. Allgaier, J. Bristow, J.P. Wiener-Kronish, E.R. Sutherland, T.S. King, N. Icitovic, R.J. Martin, W.J. Calhoun, M. Castro, L.C. Denlinger, E. Dimango, M. Kraft, S.P. Peters, S.I. Wasserman, M.E. Wechsler, H.A. Boushey, and S.V. Lynch. 2011. Airway microbiota and bronchial hyperresponsiveness in patients with suboptimally controlled asthma. J. Allergy Clin. Immunol. 127(2):372-381.
Huang, Y.J., S. Sethi, T. Murphy, S. Nariya, H.A. Boushey, and S.V. Lynch. 2014. Airway microbiome dynamics in exacerbations of chronic obstructive pulmonary disease. J. Clin. Microbiol. 52(8): 2813- 2823.
Huang, Y.J., S. Nariya, J.M. Harris, S.V. Lynch, D.F. Choy, J.R. Arron, and H. Boushey. 2015. The airway microbiome in patients with severe asthma: Associations with disease features and severity. J. Allergy Clin. Immunol. 136(4):874-884.
Huang, Y.J., J.R. Erb-Downward, R.P. Dickson, J.L. Curtis, G.B. Huffnagle, and M.K. Han. 2017. Understanding the role of the microbiome in chronic obstructive pulmonary disease: Principles, challenges, and future directions. Transl. Res. 179:71-83.
Huxley, E.J., J. Viroslav, W.R. Gray, and A.K. Pierce. 1978. Pharyngeal aspiration in normal adults and patients with depressed consciousness. Am. J. Med. 64(4):564-568.
Imhann, F., A. Vich Vila, M.J. Bonder, J. Fu, D. Gevers, M.C. Visschedijk, L.M. Spekhorst, R. Alberts, L. Franke, H.M. van Dullemen, R.W. Ter Steege, C. Huttenhower, G. Dijkstra, R.J. Xavier, E.A. Fsten, C. Wijmenga, A. Zhernakova, and R.K. Weersma. In press. Interplay of host genetics and gut microbiota underlying the onset and clinical presentation of inflammatory bowel disease. Gut
Jiménez, E., L. Fernández, M.L. Marín, R. Martín, J.M. Odriozola, C. Nueno-Palop, A. Narbad, M. Olivares, J. Xaus, and J.M. Rodríguez. 2005. Isolation of commensal bacteria from umbilical cord blood of healthy neonates born by cesarean section. Curr. Microbiol. 51(4):270-274.
Joossens, M., G. Huys, M. Cnockaert, V. De Preter, K. Verbeke, P. Rutgeerts, P. Vandamme, and S. Vermeire. 2011. Dysbiosis of the faecal microbiota in patients with Crohn’s disease and their unaffected relatives. Gut 60:631-637.
Jumpertz, R., D.S. Le, P.J. Turnbaugh, C. Trinidad, C. Bogardus, J.I. Gordon, and J. Krakoff. 2011. Energy-balance studies reveal associations between gut microbes, caloric load, and nutrient absorption in humans. Am. J. Clin. Nutr. 94(1):58-65.
Koren, O., J.K. Goodrich, T.C. Cullender, A. Spor, K. Laitinen, H.K. Bäckhed, A. Gonzalez, J.J. Werner, L.T. Angenent, R. Knight, F. Bäckhed, E. Isolauri, S. Salminen, and R.E. Ley. 2012. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 150(3):470-480.
Korting, H.C., K. Hubner, K. Greiner, G. Hamm, and O. Braun-Falco. 1990. Differences in the skin surface pH and bacterial microflora due to the long-term application of synthetic detergent preparations of pH 5.5 and pH 7.0. Results of a crossover trial in health volunteers. Acta. Derm. Venereol. 70(5):429-431.
Krajmalnik-Brown, R., Z.E. Ilhan, D.W. Kang, and J.K. DiBaise. 2012. Effects of gut microbes on nutrient absorption and energy regulation. Nutr. Clin. Pract. 27(2):201-214.
Krych, L., C.H. Hansen, A.K. Hansen, F.W. van den Berg, and D.S. Nielsen. 2013. Quantitatively different, yet qualitatively alike: A meta-analysis of the mouse core gut microbiome with a view towards the human gut microbiome. PLoS ONE 8(5):e62578.
Landreth, K.S. 2002. Critical windows in development of the rodent immune system. Hum. Exp. Toxicol. 21(9-10):493-498.
Larsen, N., F.K. Vogensen, F.W.J. van den Berg, D.S. Nielsen, A.S. Andreasen, B.K. Pedersen, W.A. Al-Soud, S.J. Sørensen, L.H. Hansen, and M. Jakobsen. 2010. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS ONE 5(2):e9085.
Leeming, J.P., K.T. Holland, and W.J. Cunliffe. 1984. The microbial ecology of pilosebaceous units isolated from human skin. J. Gen. Microbiol. 130(4):803-807.
Lepage, P., R. Häsler, M.E. Spehlmann, A. Rehman, A. Zvirbliene, A. Begun, S. Ott, L. Kupcinskas, J. Doré, A. Raedler, and S. Schreiber. 2011. Twin study indicates loss of interaction between microbiota and mucosa of patients with ulcerative colitis. Gastroenterology 141(1):227-236.
Levin, A.M., A.R. Sitarik, S.L. Havstad, K.E. Fujimura, G. Wegienka, A.E. Cassidy-Bushrow, H. Kim, E.M. Zoratti, N.W. Lukacs, H.A. Boushey, D.R. Ownby, S.V. Lynch, and C. C. Johnson. 2016. Joint effects of pregnancy, sociocultural, and environmental factors on early life gut microbiome structure and diversity. Sci. Rep. 6:31775.
Ley, R.E., F. Bäckhed, P. Turnbaugh, C.A. Lozupone, R.D. Knight, and J.I. Gordon. 2005. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. 102(31):11070-11075.
Ley, R.E., P.J. Turnbaugh, S. Klein, and J.I. Gordon. 2006. Microbial ecology: Human gut microbes associated with obesity. Nature 444(7122):1022-1023.
Lynch, S.V., and O. Pedersen. 2016. The human intestinal microbiome in health and disease. N. Engl. J. Med. 375(24):2369-2379.
Lynch, S.V., R.A. Wood, H. Boushey, L.B. Bacharier, G.R. Bloomberg, M. Kattan, G.T. O’Connor, M.T. Sandel, A. Calatroni, E. Matsui, C.C. Johnson, H. Lynn, C.M. Visness, K.F. Jaffee, P.J. Gergen, D.R. Gold, R.J. Wright, K. Fujimura, M. Rauch, W.W. Busse, and J.E. Gern. 2014. Effects of early-life exposure to allergens and bacteria on recurrent wheeze and atopy in urban children. J. Allergy Clin. Immunol. 134(3):593-601.
Ma, L., J. Kim, R. Hatzenpichler, M.A. Karymov, N. Hubert, I.M. Hanan, E.B. Chang, and R.F. Ismagilov. 2014a. Gene-targeted microfluidic cultivation validated by isolation of a gut bacterium listed in Human Microbiome Project’s Most Wanted taxa. Proc. Natl. Acad. Sci. USA. 111(27):9768-9773.
Ma, L., S.S. Datta, M.A. Karymov, Q. Pan, S. Begolo, and R.F. Ismagilov. 2014b. Individually addressable arrays of replica microbial cultures enabled by splitting SlipChips. Integr. Biol. (Camb.) 6(8):796-805.
MacFarlane, G.T., and J.H. Cummings. 1999. Probiotics and prebiotics: Can regulating the activities of intestinal bacteria benefit health? BMJ 318(7189):999-1003.
Mangin, I., R. Bonnet, P. Seksik, L. Rigottier-Gois, M. Sutren, Y. Bouhnik, C. Neut, M.D. Collins, J.F. Colombel, P. Marteau, and J. Doré. 2004. Molecular inventory of faecal microflora in patients with Crohn’s disease. FEMS Microbiol. Ecol. 50(1):25-36.
Manichanh, C., L. Rigottie-Gois, E. Bonnaud, K. Gloux, E. Pelletier, L. Frangeul, R. Nalin, C. Jarrin, P. Chardon, P. Marteau, J. Roca, and J. Dore. 2006. Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach. Gut 55(2):205-211.
Mar, J.S., B.J. LaMere, D.L. Lin, S. Levan, M. Nazareth, U. Mahadevan, and S.V. Lynch. 2016. Disease severity and immune activity relate to distinct interkingdom gut microbiome states in ethnically distinct ulcerative colitis patients. MBio 7(4):e01072-16.
Marchesi, J.R., B.E. Dutilh, N. Hall, W.H.M. Peters, R. Roelofs, A. Boleij, and H. Tjalsma. 2011. Towards the human colorectal cancer microbiome. PLoS ONE 6(5):e20447.
Markle, J.G., D.N. Frank, S. Mortin-Toth, C.E. Robertson, L.M. Feazel, U. Rolle-Kampczyk, M. von Bergen, K.D. McCoy, A.J. Macpherson, and J.S. Danska. 2013. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 339(6123):1084-1088.
Marples, R.R. 1982. Sex, constancy, and skin bacteria. Arch. Dermatol. Res. 272(3-4):317-320.
Marples, R.R., D.T. Downing, and A.M. Kigman. 1971. Control of free fatty acids in human surface lipids by Corynebacterium acnes. J. Invest. Dermatol. 56(2):127-131.
McBride, M.E., W.C. Duncan, and J.M. Knox. 1977. The environment and the microbial ecology of human skin. Appl. Environ. Microbiol. 33(3):603-608.
Mestas, J., and C.C. Hughes. 2004. Of mice and not men: Differences between mouse and human immunology. J. Immunol. 172(5):2731-2738.
Morelli, L. 2008. Postnatal development of intestinal microflora as influenced by infant nutrition. J. Nutr. 138(9):1791S-1795S.
Morris, A., J.M. Beck, P.D. Schloss, T.B. Campbell, K. Crothers, J.L. Curtis, S.C. Flores, A.P. Fontenot, E. Ghedin, L. Huang, K. Jablonski, E. Kleerup, S.V. Lynch, E. Sodergren, H. Twigg, V.B. Young, C.M. Bassis, A. Venkataraman, T.M. Schmidt, and G.M. Weinstock 2013. Comparison of the respiratory microbiome in healthy nonsmokers and smokers. Am. J. Respir. Crit. Care Med. 187(10):1067-1075.
Munck, C., J. Helby, C.G. Westergaard, C. Porsbjerg, V. Backer, and L.H. Hansen. 2016. Smoking cessation and the microbiome in induced sputum samples from cigarette smoking asthma patients. PLoS ONE 11(7):e0158622.
Nguyen, T.L., S. Vieira-Silva, A. Liston, and J. Raes. 2015. How informative is the mouse for human gut microbiota research?. Dis. Model. Mech. 8(1):1-16.
O’Connor, G.T., S.V. Lynch, G.R. Bloomberg, M. Kattan, R.A. Wood, P.J. Gergen, K.F. Jaffee, A. Calatroni, L.B. Bacharier, A. Beigelman, M.T. Sandel, C.C. Johnson, A. Faruqi, C. Santee, K.E. Fujimura, D. Fadrosh, H. Boushey, C.M. Visness, and J.E. Gern. In press. Early-life home environment and risk of asthma among inner-city children. J. Allergy Clin. Immunol.
Oh, J., A.L. Byrd, C. Deming, S. Conlan, NISC Comparative Sequencing Program, H.H. Kong, and J.A. Segre. 2014. Biogeography and individuality shape function in the human skin metagenome. Nature 514(7520):59-64.
Ordiz, M.I., T.D. May, K. Mihindukulasuriya, J. Martin, J. Crowley, P.I. Tarr, K. Ryan, E. Mortimer, G. Gopalsamy, K. Maleta, M. Mitreva, G. Young, and M.J. Manary. 2015. The effect of dietary resistant starch type 2 on the microbiota and markers of gut inflammation in rural Malawi children. Microbiome 3:37.
O’Sullivan, O., O. Cronin, S.F. Clarke, E.F. Murphy, M.G. Molloy, F. Shanahan, and P.D. Cotter. 2015. Exercise and the microbiota. Gut Microbes 6(2):131-136.
Palmer, C., E.M. Bik, D.B. Digiulio, D.A. Relman, and P.O. Brown. 2007. Development of the human infant intestinal microbiota. PLoS Biol. 5(7):e177.
Papenfort, K., and B.L. Bassler. 2016. Quorum sensing signal-response systems in Gram-negative bacteria. Nat. Rev. Microbiol. 14(9):576-588.
Penders, J., C. Thijs, C. Vink, F.F. Stelma, B. Snijders, I. Kummeling, P.A. van den Brandt, and E.E. Stobberingh. 2006. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics 118(2):511-521.
Pérez-Losada, M., K.A. Crandall, and R.J. Freishtat. 2016. Two sampling methods yield distinct microbial signatures in the nasopharynges of asthmatic children. Microbiome 4(1):25.
Qin, J., Y. Li, Z. Cai, S. Li, J. Zhu, F. Zhang, S. Liang, W. Zhang, Y. Guan, D. Shen, Y. Peng, D. Zhang, Z. Jie, W. Wu, Y. Qin, W. Xue, J. Li, L. Han, D. Lu, P. Wu, Y. Dai, X. Sun, Z. Li, A. Tang, S. Zhong, X. Li, W. Chen, R. Xu, M. Wang, Q. Feng, M. Gong, J. Yu, Y. Zhang, M. Zhang, T. Hansen, G. Sanchez, J. Raes, G. Falony, S. Okuda, M. Almeida, E. LeChatelier, P. Reneault, N. Pons, J.M. Batto, Z. Zhang, H. Chen, R. Yang, W. Zheng, S. Li, H. Yang, J. Wang, S.D. Ehrlich, R. Nielsen, O. Pedersen, K. Kristiansen, and J. Wang. 2012. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490(7418):55-60.
Rautava, S., M.C. Collado, S. Salminen, and E. Isolauri. 2012. Probiotics modulate host-microbe interaction in the placenta and fetal gut: A randomized, double-blind, placebo-controlled trial. Neonatology 102(3):178-184.
Ridaura, V.K., J.J. Faith, F.E. Rey, J. Cheng, A.E. Duncan, A.L. Kau, N.W. Griffin, V. Lombard, B. Henrissat, J.R. Bain, M.J. Muehlbauer, O. Ilkayeva, C.F. Semenkovich, K. Funai, D.K. Hayashi, B.J. Lyle, M.C. Martini, L.K. Ursell, J.C. Clemente, W. Van Treuren, W.A. Walters, R. Knight, C.B. Newgard, A.C. Heath, and J.I. Gordon. 2013. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341(6150):1241214.
Roager, H.M., T.R. Licht, S.K. Poulsen, T.M. Larsen, and M.I. Bahl. 2014. Enterotypes, inferred by the Prevotellato-Bacteroides ratio, remained stable during a 6-month randomized controlled diet intervention with the new Nordic diet. Appl. Environ. Microbiol. 80(3):1142-1149.
Schwiertz, A., D. Taras, K. Schäfer, S. Beijer, N.A. Bos, C. Donus, and P.D. Hardt. 2010. Microbiota and SCFA in lean and overweight healthy subjects. Obesity 18(1):190-195.
Segal, L.N., J.C. Clemente, J.C. Tsay, S.B. Koralov, B.C. Keller, B.G. Wu, Y. Li, N. Shen, E. Ghedin, A. Morris, P. Diaz, L. Huang, W.R. Wikoff, C. Ubeda, A. Artacho, W.N. Rom, D.H. Sterman, R.G. Collman, M.J. Blaser, and M.D. Weiden. 2016. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat. Microbiol. 1:16031.
Smith, M.I., T. Yatsunenko, M.J. Manary, I. Trehan, R. Mkakosya, J. Cheng, A.L. Kau, S.S. Rich, P. Concannon, J.C. Mychaleckyj, J. Liu, E. Houpt, J.V. Li, E. Holmes, J. Nicholson, D. Knights, L.K. Ursell, R. Knight, and J.I. Gordon. 2012. Gut microbiomes of Malawian twin pairs discordant for kwashiorkor. Science 339(6119):548-554.
Sobhani, I., J. Tap, F. Roudot-Thoraval, J.P. Roperch, S. Letulle, P. Langella, G. Corthier, J.T. Van Nhieu, and J.P. Furet. 2011. Microbial dysbiosis in colorectal cancer (CRC) patients. PLoS ONE 6(1):e16393.
Somerville, D.A. 1969. The normal flora of the skin in different age groups. Br. J. Dermatol. 81(4):248-258.
Steel, J.H., S. Malatos, N. Kennea, A.D. Edwards, L. Miles, P. Duggan, P.R. Reynolds, R.G. Feldman, and M.H. Sullivan. 2005. Bacteria and inflammatory cells in fetal membranes do not always cause preterm labor. Pediatr. Res. 57(3):404-411.
Stein, M.M., C.L. Hrusch, J. Gozdz, C. Igartua, V. Pivniouk, S.E. Murray, J.G. Ledford, M. Marques dos Santos, R.L. Anderson, N. Metwali, J.W. Neilson, R.M. Maier, J.A. Gilbert, M. Holbreich, P.S. Thorne, F.D. Martinez, E. von Mutius, D. Vercelli, C. Ober, and A.I. Sperling. 2016. Innate immunity and asthma risk in Amish and Hutterite farm children. N. Engl. J. Med. 375(5):411-421.
Suez, J., T. Korem, D. Zeevi, G. Zilberman-Schapira, C.A. Thaiss, O. Maza, D. Israeli, N. Zmora, S. Gilad, A. Weinberger, Y. Kuperman, A. Harmelin, I. Kolodkin-Gal, H. Shapiro, Z. Halpern, E. Segal, and E. Elinav. 2014. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514(7521):181-186.
Tremaroli, V., F. Karlsson, M. Weling, M. Stahlman, P. Kovatcheva-Datchary, T. Olbers, L. Fandriks, C.W. le Roux, J. Nielsen, and F. Bäckhed. 2015. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab. 22(2):228-238.
Turnbaugh, P.J., R.E. Ley, M.A. Mahowald, V. Margrini, E.R. Mardis, and J.I. Gordon. 2006. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 44(7122):1027-1031.
Turnbaugh, P., R. Ley, M. Hamady, C.M. Fraser-Ligett, R. Knight, and J. Gordon. 2007. The human microbiome project. Nature 449(7164):804-810.
Turnbaugh, P.J., F. Bäckhed, L. Fulton, and J.I. Gordon. 2008. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe 3(4):213-223.
Turnbaugh, P.J., V.K. Ridaura, J.J. Faith, F.E. Rey, R. Knight, and J.I. Gordon. 2009. The effect of diet on the human gut microbiome: A meta- genomic analysis in humanized gnotobiotic mice. Sci. Transl. Med. 6(1):6ra14.
Voigt, A.Y., P.I. Costea, J.R. Kultima, S.S. Li, G. Zeller, S. Sunagawa, and P. Bork. 2015. Temporal and technical variability of human gut metagenomes. Genome Biol. 16:73.
Walker, A.W., J. Ince, S.H. Duncan, L.M. Webster, G. Holtrop, X.L. Ze, D. Brown, M.D. Stares, P. Scott, A. Berger-at, P. Louis, F. McIntosh, A.M. Johnstone, G.E. Lobley, J. Parkhill, and H.J. Flint. 2011. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J. 5(2):220-230.
Wang, H.B., P.Y. Wang, X. Wang, Y.L. Wan, and Y.C. Liu. 2012. Butyrate enhances intestinal epithelial barrier function via up-regulation of tight junction protein Claudin-1 transcription. Dig. Dis. Sci. 57(12):3126-3135.
Wang, Z., M. Bafadhel, K. Haldar, A. Spivak, D. Mayhew, B.E. Miller, R. Tal-Singer, S.L. Johnson, M.Y. Ramsheh, M.R. Barer, C.E. Brightling, and J.R. Brown. 2016. Lung microbiome dynamics in chronic obstructive pulmonary disease exacerbations. Eur. Respir. J. 47:1082-1092.
Willing, B., J. Halfvarson, J. Dicksved, M. Rosenquist, G. Järnerot, L. Engstrand, C. Tysk, and J.K. Jansson. 2009. Twin studies reveal specific imbalances in the mucosa-associated microbiota of patients with ileal Crohn’s disease. Inflamm. Bowel Dis.15(5):653-660.
Wu, X., C. Ma, L. Han, M. Nawaz, F. Gao, X. Zhang, P. Yu, C. Zhao, L. Li, A. Zhou, J. Wang, J.E. Moore, B.C. Millar, and J. Xu. 2010. Molecular characterisation of the faecal microbiota in patients with type II diabetes. Curr. Microbiol. 61(1):69-78.
Wu, G.D., J. Chen, C. Hoffmann, K. Bittinger, Y.Y. Chen, S.A. Keilbaugh, M. Bewtra, D. Knights, W.A. Walters, R. Knight, R. Sinha, E. Gilroy, K. Gupta, R. Baldassano, L. Nessel, H.Z. Li, F.D. Bushman, and J.D. Lewis. 2011. Linking long-term dietary patterns with gut microbial enterotypes. Science 334(6052):05-108.
Yassour, M., T. Vatanen, H. Siljander, A. Hämäläinen, T. Härkönen, S.J. Ryhänen, E. Franzosa, H. Vlamakis, C. Huttenhower, D. Gevers, E.S. Lander, M. Knip, DIABIMMUNE Study Group, and R.J. Xavier. 2016. Natural history of the infant gut microbiome and impact of antibiotic treatment on bacterial strain diversity and stability. Sci. Transl. Med. 8(343):343ra81.
Yatsunenko, T., F.E. Rey, M.J. Manary, I. Trehan, M.G. Dominguez-Bello, M. Contreras, M. Magris, G. Hidalgo, R.N. Baldassano, A.P. Anokhin, A.C. Heath, B. Warner, J. Reeder, J. Kuczynski, J. G. Caporaso, C.A. Lozupone, C. Lauber, J.C. Clemente, D. Knights, R. Knight, and J.I. Gordon. 2012. Human gut microbiome viewed across age and geography. Nature 486(7402):222-227.
Zeevi, D., T. Korem, N. Zmora, D. Israeli, D. Rothschild, A. Weinberger, O. Ben-Yacov, D. Lador, T. Avnit-Sagi, M. Lotan-Pompan, J. Suez, J.A. Mahdi, E. Matot, G.
Malka, N. Kosower, M. Rein, G. Zilberman-Schapira, L. Dohnalová, M. Pevsner-Fischer, R. Bikovsky, Z. Halpern, E. Elinav, and E. Segal. 2015. Personalized nutrition by prediction of glycemic responses. Cell 163(5):1079-1094.
Zhao, J., S. Elborn, and J.J. LiPuma. 2014. Airway infection and the microbiome. Eur. Respir. Monogr. 64:32-46.
Zoetendal, E.G., J. Raes, B. Van den Bogert, M. Arumugam, C.C. Booijink, F.J. Troost, P. Bork, M. Wels, W.M. De Vos, and M. Kleerebezem. 2012. The human small intestinal microbiota is driven by rapid uptake and conversion of simple carbohydrates. ISME J. 6(7):1415-1426.
Zlotoff, D.A., B.A. Schwarz, and A. Bhandoola. 2008. The long road to the thymus: The generation, mobilization, and circulation of T-cell progenitors in mouse and man. Semin. Immunopathol. 30(4):371-382.


















