Proceedings of a Workshop
WORKSHOP OVERVIEW1
Graduate medical education (GME) is critical to the career development of individual physicians, to the functioning of many teaching institutions, and to the production of our physician workforce. However, recent reports have called for substantial reform of GME (IOM, 2014; Weinstein, 2011). The 2014 Institute of Medicine (IOM) consensus report Graduate Medical Education That Meets the Nation’s Health Needs offered recommendations intended to strengthen GME, but also highlighted concerns about the paucity of GME outcomes data (IOM, 2014), noting that concerns about GME are difficult to address without reliable, systematic data. The current lack of established GME outcome measures limits our ability to assess the impact of individual graduates, the performance of residency programs and teaching institutions, and the collective contribution of GME graduates to the physician workforce.
Much of GME is based on tradition, regulatory requirements, and hospitals’ care delivery needs rather than on evidence of effective education (IOM, 2014). Systematic data collection and analysis could help to improve the quality and efficiency of physician training, which is a key element in
___________________
1 The planning committee’s role was limited to planning the workshop, and the Proceedings of a Workshop was prepared by the workshop rapporteurs as a factual summary of what occurred at the workshop. Statements, recommendations, and opinions expressed are those of individual presenters and participants, and are not necessarily endorsed or verified by the National Academies of Sciences, Engineering, and Medicine, and they should not be construed as reflecting any group consensus.
improving the health of our nation. If national outcome data were available, large-scale observational studies could generate hypotheses for further research and innovation.
However, Debra Weinstein from the Partners HealthCare System and chair of the workshop planning committee stressed that defining and implementing GME outcome measures necessitate careful consideration about which GME outcomes are relevant, as well as clarification about what is actually measurable (now or in the foreseeable future). In addition, she said that the methods for data collection and analysis need to be considered, along with who should be responsible for tracking GME outcomes and with whom the data should be shared. The expanding use of health information technology (IT) and availability of big data could also facilitate large-scale tracking of GME outcome measures.
To examine these opportunities and challenges in measuring and assessing GME outcomes, the Board on Health Care Services of the National Academies of Sciences, Engineering, and Medicine held a workshop, Graduate Medical Education Outcomes and Metrics, on October 10–11, 2017, in Washington, DC.
Workshop participants discussed
- meaningful and measurable outcomes of GME;
- possible metrics that could be used to track these GME outcomes;
- possible mechanisms for collecting, collating, analyzing, and reporting these data; and
- further work to accomplish this ambitious goal.
These proceedings chronicle the presentations and discussions at the workshop. A broad range of views and ideas were presented. Box 1 highlights a number of suggestions from individual worshop participants to define and implement GME outcome measures. The workshop Statement of Task can be found in Appendix A, and the workshop agenda can be found in Appendix B. Speakers’ presentations (as PDF and video files) have been archived online.2
OPENING REMARKS: OPTIMIZING GME BY MEASURING OUTCOMES
Weinstein opened the workshop by articulating the overarching purpose of improving health by optimizing caregiver education. She noted that
___________________
2 See http://www.nationalacademies.org/hmd/Activities/Workforce/GMEoutcomesandmetrics/2017-OCT-10.aspx (accessed December 13, 2017).
this goal applies across the health professions and across the continuum of professional development, though the current (initial) focus is on GME.
Weinstein acknowledged that important improvements in GME have been made in recent decades, including an evolution from an immersive, unplanned “learn-by-doing” approach to curriculum-based education; graduation by default to a more careful assessment based on defined competencies; and informal oversight to an expectation of more explicit supervision. Yet, much has not changed, she continued: GME is still tethered to inpatient care, and resident activities are still heavily influenced by the service needs of teaching institutions. Concerns have been raised that today’s GME graduates are not prepared adequately for independent practice, and that the mix of graduates is not fulfilling national physician workforce needs, Weinstein explained. In addition, questions about funding persist—both about whether it is sufficient and whether it is justified, she said. These concerns were front and center when the IOM convened a committee in 2012 to examine the governance and financing of GME, resulting in the consensus report Graduate Medical Education That Meets the Nation’s Health Needs (IOM, 2014).
Insights from the 2014 Consensus Report: Graduate Medical Education That Meets the Nation’s Health Needs
Weinstein described three important realizations stemming from that committee’s deliberations:
- There is no shared understanding of what GME should accomplish. Historically, the sole expectation has been that GME programs produce competent physicians. However, additional goals need to be considered, including fulfilling national physician workforce needs and producing graduates who will advance biomedical science and health care delivery. There may also be expectations related to training programs’ contributions to the community, not just by producing local practitioners, but through impact of the GME programs themselves on care delivery.
- GME has not functioned as a system. Ten thousand GME residency programs and hundreds of institutions that sponsor them function within a common set of rules, are governed by the same group of oversight organizations, are funded largely by the same mechanism, and share a fundamental purpose. However, residency programs and teaching institutions are largely independent actors without coordination.
- No mechanism exists for comprehensive, ongoing, and consistent assessment of whether GME is meeting its goals. Believing that
GME is successful is not good enough: We need evidence that indicates what is succeeding, where improvements are needed, and how to make those improvements.
Why Measure GME Outcomes, and What Is Needed?
Measuring GME outcomes is essential for research aimed at enhancing GME and is needed to guide public policy, Weinstein asserted. Data related to the 130,000 residents who are in training at any time should be harnessed to continuously improve that training, she continued. Measuring GME outcomes with common metrics is needed to determine best educational practices and to measure the success of innovative pilots, she concluded.
Weinstein described a path to achieving this vision by (1) defining the relevant outcomes of GME, (2) identifying a system for ongoing tracking of common metrics, and (3) sharing data to facilitate large-scale research that could enable evidence-based education. Large-scale research is needed (versus single-program or single-institution studies) to provide evidence that is convincing enough to overcome entrenched processes, in which hospitals depend on residents continuing to do what they do now, she said. Large-scale research will also be more effective at influencing GME policy and regulations, and hopefully in demonstrating a significant return on the public investment in GME. She emphasized the importance of engaging all relevant stakeholders in the health care sector, including hospitals and other health care providers, regulatory groups, funders, and policy makers.
Weinstein described how, initially, observational data can be used to explore the relationship between educational processes and outcomes for graduates. For example, does the amount of ambulatory time during training correlate with the type or location of practice that graduates choose? Do physicians who have a deep experience with simulation during residency have different clinical outcomes than those that do not? Prospective interventional studies could then be used to compare different approaches to GME as long as common metrics are in place to assess the outcomes.
Measuring GME outcomes presents a number of challenges, Weinstein noted. Administrative burden is a major concern, so data collection would need to be efficient and streamlined. Some worry that common metrics would lead to a loss of autonomy, where all teaching institutions would be expected to demonstrate similar outcomes for graduates. Rather, Weinstein suggested that national goals should be met collectively, without each residency program and teaching institution being expected to contribute to every goal of GME. Privacy issues relating to data regarding individual physicians, residency programs, and teaching institutions would need careful consideration; these issues are the focus of a workshop session. Funding
is a challenge because the data collection and analysis would require some investment. Moreover, many stakeholders are reluctant to tinker with the status quo based on concerns about potential loss of current GME funding if a residency program or teaching institution demonstrates suboptimal outcomes. She acknowledged the risk of misinterpretation or overinterpretation of data, and noted the importance of meaningful, high-quality data within a responsible GME outcome measurement system.
Why Now?
Despite the obstacles and challenges, the time to develop metrics to measure GME outcomes is now for several reasons, Weinstein asserted, including the following:
- GME could capitalize on rapid advances in health information technology, big data, and data science.
- With a surging interest among medical school and academic health center faculty in education research, there are people who are willing and able to undertake this work.
- A number of the oversight organizations are shifting their focus from process to outcomes, with a corresponding willingness to relax rules and requirements for purposes of research. (Recent multi-institution studies of resident duty hours and the Education Across the Continuum project in pediatrics are examples.)
- Perpetual threats to federal funding for GME (along with greater constraints on institutional funds available for education) increase the urgency to demonstrate return on investment for taxpayers and to identify ways to use educational funds most effectively.
GME OUTCOMES: WHAT MATTERS?
David Asch from Penn Medicine Center for Health Care Innovation asked what GME should do better and for which areas GME should be accountable. Panelists responded by discussing the need to focus on clinical outcomes, community outcomes, and improving value in health care. Panelists and workshop participants also discussed perceived and real barriers imposed by the number of available GME positions, GME accreditation, and funding streams.
Good clinical training is important and necessary for the delivery of high-quality medical care, but it is not sufficient, said Gail Wilensky from Project HOPE. She added that GME has achieved excellence in the technical training provided to clinicians, and maintaining the excellence for which the U.S. training programs are known is essential. Humayun Chaudhry
from the Federation of State Medical Boards agreed, saying that one constant from his travels through South America, Europe, Africa, and Asia is an admiration for the way in which the United States educates and trains doctors. However, he said that in the 21st century GME also needs to focus on clinical outcomes and improved patient health. To achieve good clinical outcomes, Wilensky stressed, graduates should understand and be responsive to the needs of an ethnically diverse population.
An overarching challenge to GME progress is an overemphasis on inputs and insufficient focus on the outcomes for graduates, Wilensky continued. Despite discourse about value-based care focused on quality and efficiency, she said little progress has been made on this front; thus, GME activities should focus more on patient outcomes. Measuring outcomes is complicated, but GME needs to rise to the challenge and figure out what can be traced back to the clinical community, she said.
Several participants acknowledged that a fundamental challenge of focusing on clinical outcomes is identifying the most meaningful outcome metrics. For example, Donald Brady from the Vanderbilt University Medical Center noted that patient outcomes can be measured at different time points, but the longer the time frame, the less likely the outcome is to be directly associated with a particular clinician or program. Wilensky said that both the outcome of the individual being trained and the outcome for the patient should be measured to improve GME. Asch added that a set of outcomes for GME is a necessary requirement for a system of accountability for GME, and together those outcomes should more broadly reflect GME’s role in health care.
Fitzhugh Mullan from The George Washington University emphasized the need to focus on community outcomes in addition to individual clinical outcomes through more physician engagement in the community and programs to bridge the gaps in rural areas and in primary care. He said GME should consider its social mission beyond competencies and capabilities; the goal is not simply making GME better but also more equitable in the distribution of services that the graduates provide around the country. Advances in public health and medicine have contributed to dramatic increases in the average American life span in the past 100 years, from age 40 to age 70, but not without health disparities (CDC, 1999). The goal now should be to reduce the gaps in racial health disparities, and GME should be seen in that context, Mullan continued (Williams and Purdie-Vaughns, 2016).
Mullan stressed that physicians should play an important role in an “all hands on deck” effort to lift society as a whole. This means addressing social determinants of health and training mission-driven physicians, not just in family medicine, but also in other specialties, said Mullan. Currently, many health care training institutions are located in areas with significant poverty, but they often have little involvement in the community beyond
clinical care. GME could include an expectation of community engagement, defined in a variety of ways, with metrics measuring GME’s ultimate effect in the community, he said. One informative example is the concept of “communities of commitment” in undergraduate medical education, in which a medical school has a designated area in the community for which it takes some responsibility for making a measurable impact.
Although about 20 percent of the U.S. population lives in rural areas, less than 10 percent of physicians are in rural settings, said Mullan (IHS Markit, 2017). Residency is the staging ground for the workforce, where location, type, and style allegiances and values are formed. In some innovative GME approaches, teaching health centers address these workforce shortages by taking GME training to locations with physician deficits, but getting these programs off the ground is challenging. The current medical specialty mix does not represent U.S. health care needs, with 8,400 declared primary care shortages, Mullan added (IHS Markit, 2017). GME residency programs influence the specialty mix, but they are more focused on current hospital staffing needs than the national workforce needs. Addressing the social mission of GME would require metrics, data, and subsequent policy changes (CDC, 1999) for GME that are more accountable, responsible, and effective, Mullan stressed. Trying to separate GME from the entire remainder of what needs to be accomplished in health care would be a mistake, he concluded.
Mullan addressed the commonly raised issue of an upcoming GME shortfall—an insufficient number of GME positions for the number of medical school graduates. But Mullan said this notion is not supported by data. Each year, for the past two decades, more than 6,000 international medical graduates have undertaken GME training in the United States, meaning there have been about 6,000 excess GME slots (Mullan et al., 2015). However, the gap is closing; for the past 13 or 14 years, the number of U.S. medical school graduates entering residency programs has increased by about 2.4 percent annually (Mullan et al., 2015). Closing the gap could have a positive global impact, Mullan added, because currently the U.S. demand for international medical graduates is contributing to the brain drain in low- and middle-income countries, which is a destabilizing factor for those countries.
Marschall Runge from the University of Michigan introduced the concept of value-based outcomes, including a definition of value, as an important concept for GME programs. This has not been standardized across residency programs because of the challenge in measuring value. His comments focused on how to define and measure value in a meaningful way. What we want from GME is to optimize value in health care, said Runge. The term “value in health care” is broadly defined as a ratio of quality to cost. Our GME programs can and should embrace the goal that their
trainees graduate with the skill set and competency to practice and teach high-value health care at an appropriate cost, said Runge. To achieve this goal, residency programs should make value training a part of their common goals and learn from their collective experience, which has been the case for addressing so many different challenges over the past 20 years, Runge continued. At present, though, a focus on producing physicians who practice high-value health care across institutions is not commonly on the agenda for GME meetings.
Residency programs vary significantly, from academically oriented programs that include a goal of training practitioners across a broad spectrum of specialties, to physician scientists and others with unique expertise, to community-based programs that focus on training primary care physicians to serve the community. These are, and should be, very different programs with different training goals, but finding commonalities across these many programs in value-based health care could improve all residency programs, said Runge. As a simple example, physicians should have some familiarity with the kind of care that can be delivered in different settings as this can impact both the quality of care and the cost of care. He also proposed the concept of “precision education” to recognize that trainees start at different points and develop competency at different rates.
Emphasizing the importance of team-based care for improving value, Runge highlighted an example at the University of Michigan. He said the average cost to perform a joint replacement was $25,000, but Medicare reimbursement was $23,000. After bringing together a physician-led team that included experts in physical therapy, pharmacy, and home health, not only did they reduce the average cost to $19,000, but the length of inpatient stay and the use of opioids were both reduced significantly.3 Such pilots are important, said Runge, and they are likely scalable across institutions, but doing so involves collaboration, and a common denominator would be the orthopedic residents at each institution. Unfortunately, developing analogous processes for other specific causes of hospitalization often involves quite different factors. Ultimately, changing financial incentives can be leveraged to improve value, Runge also noted. In the past, many more physicians had loans repaid as an incentive to working in underserved areas. As a result of such loan repayment programs, about one quarter of these physicians remained in underserved areas.
Speaking to the challenges of measurement in GME, specifically measurement of value, Runge said the metrics currently required by regulatory agencies—payers and funders for GME—mostly fall into the category of being measurable, but not important. Despite this challenge, Runge offered some insights on strategies to measure value in GME. In terms of the most
___________________
3 See http://marcqi.org/about-marcqi/marcqi-goals (accessed January 9, 2018).
appropriate metrics available today at a very simplistic level, one possibility is to think about a way to measure how frequently trainees use evidence-based care guidelines, he said, noting that there are many good guidelines, but they are underused. He added that use of guidelines should consider the whole patient and allow for adjustments in care. A balanced approach to measuring use of physician guidelines could be a target metric of value. He also noted the recent rapid advances in artificial intelligence, and how that might change clinical practice and medical training in the future. The ability to analyze massive data sets would create new knowledge and may provide much more meaningful (albeit complex) metrics.
Another possibility might be to assess some aspects of training through feedback, said Runge, as he offered an example of investigators from Michigan using social media inputs from more than 40,000 residents across the United States to study depression and suicide in that population (Mata et al., 2016; Sen et al., 2010). The future is bright if we all are willing to innovate, take chances, and measure the success (or lack of it) for new interventions, said Runge.
Discussion of Challenges to Identifying, Measuring, and Achieving Optimal Outcomes
Several challenges to identifying, measuring, and achieving optimal GME outcomes were raised and discussed by the workshop participants. The panel had a robust discussion about whether the current requirements of residency programs are impeding progress in GME. Susan Skochelak from the American Medical Association (AMA) asked the panel whether requirements at the residency review committee level, including service obligations and location of training, which she said is often still limited to inpatient care, stifles innovation in GME. Mullan said that medical centers place a high priority on meeting accreditation standards and performing well in reviews by the Accreditation Council for Graduate Medical Education (ACGME) and the Liaison Committee on Medical Education (LCME). Thus, they are hesitant to try new strategies or to highlight novel things they are doing, but instead focus on “checking all the boxes,” he said.
Thomas Nasca from ACGME responded, saying that the barriers discussed are perceived but not real. ACGME is not only willing to innovate by waiving standards, but has funded research on important questions, Nasca continued. There has been a dramatic change in perspective on GME accreditation over the past 15 years, not only with the introduction of the competencies and measurable clinical outcomes of education that could be linked to patient outcomes, but also in the standards, he said. Regarding the distribution of inpatient versus outpatient training, he said that two-thirds
of the training in internal medicine could be undertaken in the ambulatory care setting if desired, according to ACGME standards. He added that ACGME’s goal in accreditation is no longer satisfaction of minimum standards, but rather to help residency programs achieve excellence. ACGME cannot do it alone, however, and cannot be the only entity to set standards, said Nasca. Reflecting on Nasca’s comments, Runge added that the risk of innovation versus crossing the t’s and dotting the i’s has held back many institutions that are concerned about the balance between innovation and documentation of standards ACGME has historically followed. Thus, there is less innovation in education than is optimal. Dan Burke from the Morgan County Rural Training Track agreed with Nasca, saying that based on his experience in Colorado, ACGME standards have not been a barrier to innovation.
Burke also raised a funding issue. A real challenge is that funding goes directly to the hospitals even when the innovators are educators and scientists, he said. Changing who receives the money was a recommendation of the 2014 report, responded Wilensky, although little progress has been made in that regard. Many other participants, such as teaching health centers, are important and should also be able to receive the funding, Wilensky said. Another funding stream challenge discussed is where the funding is received within an institution. At many teaching hospitals, Medicare GME dollars flow to the hospital and are under the purview of the hospital chief financial officer, who has many financial needs and may not prioritize support for education, Runge said. At the very least, this important funding stream has been conflated and complicated based on individual institutions’ approaches to GME, Runge continued. Michigan Medicine recently developed a single unified budget that encompasses the medical school and health system specifically to be able to make funding sources and expenditures transparent and rational. Other institutions, such as the University of Pennsylvania, have made similar budgetary changes for the same reasons, having a common view of GME funds. This does provide additional funding that positions these institutions to be innovators in GME, he said.
CURRENT METRICS: WHAT IS MEASURED NOW?
National Board of Medical Examiners (NBME) Measurements
Peter Katsufrakis from NBME discussed four types of data that NBME collects to assess medical school students, including U.S. Medical Licensing Examination (USMLE) performance data, NBME subject examinations, NBME clinical assessments, and data from exams that NBME also
administers for 15 health professional organizations.4 He concluded with lessons learned and a glimpse into future NBME data collection plans.
USMLE5 is made up of four elements, or four examinations in three steps, said Katsufrakis. Three of the four examinations include single best answer multiple-choice questions. Step 2 is divided into clinical knowledge (CK) and clinical skills (CS), with Step 2 CS consisting of 12 standardized patient stations, each of which lasts 15 minutes, followed by 10 minutes for the examinees to complete their postencounter note. Finally, Step 3 also includes clinical case simulations of managing a patient. To develop these examinations during any given year, more than 300 faculty members in various disciplines from medical schools across the country create items for the examinations, review the performance of items that have been created previously, and participate in the management and governance of the USMLE program.6 Although the USMLE’s primary purpose is as a licensing examination, most students consider it a residency placement examination because of the critical role USMLE scores play in the selection of candidates by residency programs. A significant number of medical students take USMLE exams, with approximately 40,000 examinees completing Step 1 and Step 2 CK, 35,000 students taking Step 2 CS, and nearly 30,000 students taking Step 3.7
Upon completion, examinees receive a detailed report of their scores, including performance gaps for which more focused training may be needed. Robert Phillips from the American Board of Family Medicine (ABFM) noted that at ABFM, residency training programs receive these competency reports and translate them into a personalized curriculum and education plan, an exercise that has been associated with significantly improved pass rates on the initial certification exam. In the coming year, Katsufrakis said the score reports would be presented in a new way to more clearly communicate examinees’ strengths and weaknesses in each subject area and relative to other examinees.
NBME also administers basic science and clinical science subject examination programs for students in medical schools, said Katsufrakis. In 2016, examinees took approximately 40,000 basic science subject exams.8 These numbers have declined in recent years as schools have opted for customized assessments. Five of the eight clinical subject exams, including medicine, obstetrics and gynecology, pediatrics, psychiatry, and surgery are taken by nearly 25,000 examinees.9
___________________
4 See http://www.nbme.org/about/index.html (accessed December 18, 2017).
5 See http://www.usmle.org (accessed December 19, 2017).
6 See http://www.usmle.org (accessed January 9, 2018).
7 See http://www.usmle.org/performance-data/default.aspx (accessed January 9, 2018).
8 Unpublished data.
9 Unpublished data.
Nasca pointed out that one clinical subject, ambulatory care, had fewer than 1,000 examinees, well below other subjects. Katsufrakis said some of the challenges faced in graduate medical education are similar to those faced in undergraduate medical education. For example, it is easier to organize medical education around an inpatient facility in a hospital, and more challenging to manage an educational program in which students are placed in different locations across the city or perhaps across the state or region. The result, Katsufrakis continued, is more uptake for traditional internal medicine examinations that are focused primarily on content from an inpatient setting, compared with outpatient specialties, such as ambulatory medicine.
Katsufrakis described several challenges and barriers to using each of these data sets for research, including varied organizational policies and ownership rights, and data isolation. Different data policies govern release of USMLE data and NBME data because of shared ownership with the Federation of State Medical Boards, said Katsufrakis. Health professional organization exam data are potentially even more restricted due to differences in ownership rights and data management. These access challenges within NBME are an example of what to expect as methods to pull data from different sources are developed.
Because the exam systems were all developed separately, collating data for an individual’s performance on the different steps of the USMLE examination and the subject examinations is not simple, Katsufrakis said. However, NBME is reinventing its system to allow researchers to combine data from multiple examination sets by 2022. However, even then, NBME would face the challenge of matching data without universal identifiers, he said.
Katsufrakis used the example of the Data Commons10 to illustrate the challenge of creating and sustaining tools for research using these data. The Data Commons was formed by NBME and several other organizations to create a simplified way of combining data that were held by these different organizations for the purposes of research, said Katsufrakis. However, after expending hundreds of thousands of dollars to create the Data Commons, there was not much demand to use the system. He said the cautionary lesson from the Data Commons example is the need to consider regulatory and market forces as both carrots and sticks to promote use of future systems.
The Pediatric Milestone Assessment Collaborative
An encouraging example of successfully measuring a resident’s progress, said Katsufrakis, is the Pediatric Milestone Assessment Collaborative
___________________
10 See https://www.nbme.org/PDF/Publications/Examiner-2013-SpringSummer.pdf (accessed July 31, 2019). This link was revised after release.
(PMAC), a collaboration among NBME, the American Board of Pediatrics, and the Association of Pediatric Program Directors. PMAC’s mission is to “uphold the public trust by creating a unified, longitudinal approach to assessment of Pediatricians” that verifies continued competence beyond medical knowledge, drives continuous performance improvement, facilitates lifelong learning, and recognizes and guides both personal and professional growth. PMAC’s current focus is on developing assessments that can measure a pediatric resident’s progress through the milestones. Presenting results from PMAC, Katsufrakis noted that historically, achieving a generalizability coefficient (a statistical measure of the reliability of the assessments) in the range of 0.7 to 0.8 requires drawing data from 12 to 15 different observers (Donnon et al., 2014). Furthermore, by reducing the number of instruments from 12 to 6, the PMAC’s pilot studies were able to dramatically reduce the administrative burden of collecting data and improve information collection.11 All three PMAC modules will be completed within 24 months, he noted.
ACGME Milestone Data Measurements
Eric Holmboe from ACGME provided background on the learning curves and professional development of residents before presenting findings from ACGME’s Milestones12 project and next steps. GME’s goal is proficiency as defined by the Dreyfus model of professional development, as most graduates would not yet be experts, said Holmboe. Medical student graduates enter residency with only 12 to 20 weeks of experience in their discipline, climb the steep curve into proficiency within 3 to 7 years during residency, and then (hopefully) continue developing their expertise after residency and throughout practice (Pusic et al., 2014). Based on the current U.S. GME training model, Holmboe described how the five Dreyfus levels (Dreyfus and Dreyfus, 1980) of the ACGME milestones translate for residency programs, including (1) expectations for a beginning resident; (2) milestones for a resident who has advanced beyond entry but is performing at a lower level than what is expected at midresidency; (3) key developmental milestones midresidency and well into a specialty; (4) knowledge, skills, and attitudes for a graduating resident; and (5) exceeding expectations. Holmboe emphasized that the ultimate goal of residency programs is to achieve level four—ensuring that all residency graduates are prepared for unsupervised practice. Readiness for unsupervised practice in each subcompetency is not a requirement, Holmboe added, but a goal.
___________________
11 Unpublished data.
12 See http://www.acgme.org/What-We-Do/Accreditation/Milestones/Overview (accessed December 20, 2017).
Holmboe also displayed a logic model to provide a conceptual framework that can be used to specify the goals of GME and to analyze how GME contributes to each goal (see Figure 1). The logic model provides the scaffolding that allows for the development of criteria for generating, selecting, and evaluating potential measures (see also Van Melle, 2016). It can be used to evaluate the purpose, resources needed (inputs), critical activities, and outcomes of a training program, he said.
ACGME’s Milestone project collects measurable outcome data for trainees in 144 specialties and subspecialties, said Holmboe (Hamstra et al., 2017). In June 2017, 133,335 residents and fellows entered the Milestone system, which generates 3.4 million data points every 6 months that can be used to analyze the performance of residents and programs (Hamstra et al., 2017). ACGME has generated evidence to demonstrate validity of the system, with national multi-institutional studies for internal medicine, emergency medicine, pediatrics, family medicine, and neurosurgery. Lawrence Smith from the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell raised a question about the reliability of measurements, asking if an assessment from one program is comparable to another program, and recognizing that the evaluator’s frame of reference may also differ. Holmboe responded that the assessment framework between residency programs is a challenge and that researchers are trying to identify ways to improve Milestone assessments. He also added that some evaluators may not be fully trained on the competency elements they are assessing. Currently, it is “messy,” said Holmboe, but residency programs can use ACGME feedback
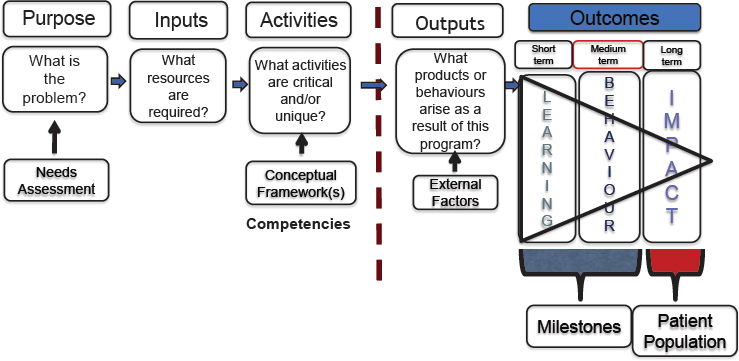
SOURCES: Holmboe Presentation, October 10, 2017; concept adapted from Van Melle, 2016.
data to help their faculty learn and adapt as a continuous quality improvement process.
Holmboe presented study results demonstrating how Milestone data are identifying gaps in the curriculum and providing evidence on the training trajectory that can help predict the likelihood of meeting level four proficiency targets. He said it can also help to identify workforce challenges, and longitudinal data would be used to assess how Milestones correlate with practice. For example, Holmboe said that in family medicine, residents are struggling with community medicine across the country, demonstrating that there is a likely deficit in the curriculum. These types of data can inform continuous quality improvement in training programs. Neurosurgery data analysis helped determine that a significant subset of residents were not meeting level four proficiency standards in Pain and Peripheral Nerve Surgery, and Surgical Treatment of Epilepsy and Movement Disorders. Reflecting on these data, the neurosurgery community realized these residents were likely not seeing enough patients to gain proficiency in their program for a number of reasons. These data helped to catalyze the neurosurgery community to revise their Milestones.
With multiple time points of assessment, Milestone data also allow ACGME to provide predictive feedback to residency training programs and to help identify residents with additional training needs. For example, Holmboe said ACGME recognized that progress slows for a subset of residents—a phenomenon called a plateau effect. Supplying this feedback metric to programs creates a potential opportunity for program leaders to provide an intervention for those residents.
Holmboe also provided an example of how ACGME is connecting with and using other longitudinal data, such as post-GME practice survey data. He said the Association of Family Medicine Residency Directors (AFMRD) implemented a survey of family medicine physicians, collected data on scope of practice, practice organization, preparation, and location, and had an excellent response rate. The AFMRD and ACGME team is hoping to conduct a longitudinal analysis connecting this survey data with Milestone data to potentially predict what happens when people enter practice. Thus, the Milestones data set is now reaching a level of maturity where it can begin to follow people out into practice, enabling correlation with Milestone data. These longitudinal studies are now possible because ACGME has longitudinal assessment data across all competencies, Holmboe concluded.
Edward Salsberg from The George Washington University Health Workforce Institute asked about the ability to share information in a national longitudinal database. The Milestones are co-branded, owned by both ACGME and the American Board of Medical Specialties (ABMS), Nasca responded, noting that they are working with LCME to provide Milestone data to medical schools for their graduates. Although data usage is limited
by the approvals, ACGME is currently engaged in discussions with the Accreditation Council for Continuing Medical Education and ABMS about the opportunity for creating a blinded national database for individual data and perhaps also institutional data. The next big challenge is to integrate those data with clinical information, he said.
GME Program Metrics of the Health Resources & Services Administration
Nasca said the innovative programs of the Health Resources & Services Administration (HRSA) provide clues on how to decentralize GME and move into community settings, as he introduced Candice Chen of HRSA. Chen provided an overview of HRSA’s Bureau of Health Workforce Vision & Mission. She described GME payment and grant programs, including the metrics that HRSA uses to measure residency training program components and outcomes, as required by law.
HRSA is the agency within the U.S. Department of Health and Human Services (HHS) that focuses on ensuring high-quality health care for all communities, and particularly for underserved communities, said Chen. The HRSA Bureau of Health Workforce is key to achieving that mission. The Bureau supports stipends and other payment costs associated with GME through two types of programs: GME grants for preventive medicine residency programs, and GME payment programs, including the Children’s Hospital GME (CHGME) and Teaching Health Center GME (THCGME).
The statutory reporting requirements provide a sense of congressional interest in GME outcomes and metrics, said Chen (see Box 2). The Preventive Medicine Residency Program, which grants awards every 5 years and supported the training of 115 residents in academic year (AY) 2015–2016, was established after passage of the Government Performance and Results Act (GPRA) enacted in 1993.13 GPRA required all agencies to engage in strategic planning, performance planning, and reporting. The GPRA Modernization Act of 2010, more specifically, required program goals to be objective, quantifiable, and measurable.14 Under Title VII of the Public Health Service Act, HRSA’s National Center for Health Workforce Analysis is tasked with annually evaluating, developing, and publishing the performance measures for the Title VII programs, including the GME grants program, said Chen.15 Finally, HRSA’s Council on Graduate Medical Education is also tasked explicitly with developing, publishing, and
___________________
13 Public Law 103-162.
14 Public Law 111-352.
15 Section 761(b)(2) of the Public Health Service Act.
implementing performance measures for the Title VII programs, as well as developing longitudinal evaluations.16
Reporting requirements are operationalized through performance measures, said Chen. In AY 2015–2016, CHGME and THCGME programs
___________________
16 Section 762(a)(3)(4) of the Public Health Service Act.
provided annual reports on training program characteristics, including types of partners/consortia and total number of accredited and filled positions.17 They reported on individual-level characteristics of the residents they are training, including demographics, whether they are from a rural or disadvantaged background, training hours and encounters in primary care, underserved and/or rural settings, employment outcomes after 1 year, and intention at graduation. CHGME programs also report hospital information, including the hospital discharges by payer type, zip code, and patient safety initiatives within the hospital.
Chen discussed outcomes of the HRSA GME payment programs and discussed future program goals. One in two pediatric specialists were trained under the CHGME program, said Chen.18 In AY 2015–2016, children’s hospitals across the country trained more than 6,800 full-time equivalent residents, of which 4,600 were supported by the CHGME Payment Program. Furthermore, the CHGME program is currently supporting the training of about 48 percent of general pediatric residents and 53 percent of all pediatric subspecialty residents.19 Highlighting program successes, Chen noted that more than 60 percent of THCGME graduates are practicing in medically underserved communities and in rural settings.20
Looking forward, HRSA is focused on reducing the administrative burden of reporting for the grantees, improving accuracy of the training data, increasing visibility, connecting programs to other databases to longitudinally track graduates, and tying payments to metrics, said Chen. HRSA hopes to improve the quality of the data by developing a data collection portal that would allow trainees to self-report on metrics such as demographics, and to increase visibility of the program by connecting directly with trainees who may not know they are funded by HRSA. In the past year, THCGME and CHGME programs began using National Provider Identifiers21 (NPIs) in data reporting. Ultimately, connecting NPI numbers with Medicare and Medicaid claims would allow longitudinal tracking and insight into whether individuals trained in these GME programs continue to provide care for these critical populations, Chen said.
Finally, there is currently no mechanism to link funding to GME metrics, she said. However, in 2013, Congress authorized a Children’s Hospital
___________________
17 See https://bhw.hrsa.gov/grants/reportonyourgrant (accessed January 9, 2018).
18 See https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/childrens-hospital-highlights.pdf (accessed January 9, 2018).
19 See https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/childrens-hospital-highlights.pdf (accessed January 9, 2018).
20 See https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/teaching-health-center-graduate-highlights.pdf (accessed January 9, 2018).
21 See https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/NationalProvIdentStand (accessed November 14, 2017).
Quality Bonus System, which HRSA will begin to implement in 2019.22 With this program, HRSA plans to address issues such as access, quality, and cost of care, as well as provider wellness.
Metrics of the American Board of Medical Specialties
Lois Margaret Nora from ABMS defined board certification, explained the process of certification and associated metrics, and discussed lessons learned and future trends in board certification assessments. ABMS23 is the umbrella organization for 24 independent member boards that oversee the standards through their assessment mechanisms in 39 specialties and 86 subspecialties, said Nora. The ABMS boards certify both allopathic and osteopathic physicians, and the American Osteopathic Association also certifies osteopathic physicians in the osteopathic medical specialties. ABMS board certification is distinct from medical licensure, which is a requirement for practicing medicine. Board certification credentials are grounded in the standards that define the specialty and are a statement that the physician meets the professionalism, knowledge, skills, and standards of the specialty board.
Initial board certification (which was the primary focus of this presentation) entails an ongoing assessment of knowledge, skills, and professionalism across an extended period of time, generally through completion of training in an ACGME-accredited residency or fellowship program, said Nora. Board certification requires a statement from the ACGME program director regarding the professionalism, ethical behavior, and readiness for independent practice of the trainees, in addition to successful performance on board-based assessment. Other requirements vary by board and may include oral examinations, practice requirements, professional recommendations from peers and hospital leadership, procedural case log books, hospital privileges, and elements of certification(s) examination administered during residency.
Providing evidence that board certification makes a difference, Nora cited research showing that patient outcomes across a wide variety of clinical conditions are better when care is provided by an ABMS board-certified physician (Hawkins et al., 2013; Sharp et al., 2002). There are also fewer disciplinary actions for board-certified physicians (Lipner et al., 2013). Board certification is an important distinguishing factor in clinical privilege and has been identified as important to patients and their families, Nora added.
___________________
22 See https://bhw.hrsa.gov/fundingopportunities/default.aspx?id=fa87b0b7-3538-43f4-af1d-55e3ba2f464b (accessed January 9, 2018).
23 See http://www.abms.org (accessed December, 19, 2017).
Nora highlighted current trends and lessons learned. First, ABMS is working to address the limited understanding of board certification among medical students. One lesson learned from a board that dropped oral examinations for a period of time is that they provide unique information regarding skills such as clinical reasoning and ethical analysis (personal communication from Robert H. Miller, American Board of Otolaryngology, 2017). Use of technology and simulation-style assessment is increasing, and all boards are looking at how to use the Milestones and better understand what information the Milestone system can provide. Looking forward, Nora noted three fundamental questions to address regarding board metrics: (1) What measures give us the most important information? (2) What measures give us unique information? and (3) What do measures say about length and style of training?
Several participants discussed the importance of applying board certification and other assessments of GME in practice. Several strategies to assess metrics throughout the career of a physician are being evaluated by some boards, such as registries and long-term Milestones, that could potentially provide important information back to GME educators, said Nora. However, GME is a relatively short time period compared to the career of a physician, so it is important to also consider how lessons learned from GME apply across the career of a physician. Nora provided an example of how the American Board of Urology (ABU) used data to reduce unnecessary patient testing and improve patient care (Pearle, 2013). ABU evaluates practice based on longitudinal Current Procedural Terminology (CPT) code data and noted, a number of years ago, that there were certain practices that were duplicative and redundant (e.g., urinalyses and urine creatinine tests). Through questions, discussion, and education from ABU, that trend changed and patient care was improved by reducing unnecessary testing, said Nora.
Certifying boards can play a helpful role in residency training and then look at different time points in practice to see how training is reflected in care quality and patient outcomes, added Phillips from ABFM. ABFM worked with the AFMRD to develop a survey of their graduates who are 3 years out of training. This survey provides feedback to residency programs about how prepared their graduates thought they were for practice, and what they are doing in practice. The Family Medicine Review Committee requires surveys of graduates, but Phillips said that this has not been done rigorously in the past; the ABFM–AFMRD partnership provides greater standardization through their survey, which had a 67 percent response rate in its first year. Katsufrakis said that perhaps the greatest value of this survey approach might be to provide feedback to individuals in clinical practice about how they could improve. Nora added that one of the most remarkable things happening within the board community, relative
to continuing certification, is the uptake of longitudinal assessments. The results of these assessments feed into a system that could provide summative conclusions, and thus allow for substantial modifications to improve the high-stakes decadal exam for maintenance of certification (MOC).
BLUE SKY: DATA IN THE FUTURE
A panel of data scientists and health services researchers presented data they have collected and analyzed in their fields, and discussed potential implications for future GME research.
Lessons from Measuring Provider Performance in Clinical Practice
Rachel Werner from the University of Pennsylvania spoke about measuring provider performance in clinical practice, and the implications for GME. Werner first described the qualities of good performance metrics, which she said should be correlated with something important. In the patient care setting, that often means clinical outcomes. The reason to focus on measurement is to improve quality of care; thus, quality metrics are only useful to the extent that providers can control what is being measured and thus have the opportunity to improve that quality. Furthermore, quality metrics should not unintentionally harm clinical care. A big challenge of measuring quality in any setting is ensuring that the data are current, and that the measures are relevant and important, Werner added.
Process measures, which assess whether the right care is delivered and whether care is concordant with clinical guidelines when they are available, have been very widely adopted across clinical quality measurement activities for a number of reasons, said Werner. Process measures are directly under the control of the providers and are less sensitive to the clinical and sociodemographic characteristics of patients. Process metrics are also measured in the short term, giving providers immediate feedback about the quality of care they are delivering and thus providing clinicians with the opportunity to change practice to improve quality of care. However, there is a need to validate these measures, which are surrogate outcomes, to ensure that they are related to patient outcomes.
Too often, process measures are not well correlated, at least at a provider level, with patient outcomes, said Werner. For example, when Medicare began rating hospitals on the quality of care they delivered, they did so using a series of process measures (Werner and Bradlow, 2006). For heart attack patients, Medicare used five measures (aspirin on admission, beta-blocker on admission, aspirin on discharge, beta-blocker on discharge, and angiotensin-converting enzyme inhibitor for left ventricular dysfunction) (Werner and Bradlow, 2006). However, although process-based
performance improved, the mortality trend did not change significantly (Ryan et al., 2012). Similarly, in a Medicare demonstration project, reimbursement for a small group of hospitals was partly determined by process metrics for heart attacks, but data showed that although process-based quality improved in participating hospitals, patient mortality at 30 days remained unchanged (Werner et al., 2011).
Measuring clinical outcomes directly is appealing both to policy makers and to patients because outcomes are clinically meaningful end points and have strong face validity, said Werner. However, she emphasized the importance of ensuring that provider-level outcomes are (1) valid measures by ensuring they truly reflect provider quality, as many factors influence patient outcomes and are not simply a measure of patient risk; and (2) under the provider’s control. Werner provided several examples of research results in which improved patient outcomes were linked to provider quality rather than patient characteristics. In one study, researchers investigated whether hip fracture mortality at a hospital was predictive of that hospital’s future outcome. Results indicated that hospitals with lower mortality for hip fracture patients in the past did much better with current hip fracture patients, indicating that the outcome was a result of hospital quality (Neuman et al., 2016). Another study demonstrated how researchers can use comparisons among the same set of patients to control for patient risk. Analyzing data from patients who were admitted to multiple hospitals within a relatively short period of time, researchers found that readmission rates at the historically higher-performing hospitals (hospitals with low readmission rates) were 2 percent lower than readmission rates at historically lower-performing hospitals (hospitals with higher readmission rates). Thus, this research provides evidence that providers’ past outcomes predict future outcomes, even after controlling for patient risk (Krumholz et al., 2017). In a third study, researchers used Medicare data to examine readmission rates for a group of conditions across all hospitals in the United States and found a significant reduction in readmission rates across hospitals with a focus on those conditions, said Werner (Zuckerman et al., 2016). This study demonstrated that outcomes are under provider control; in other words, hospitals can improve their outcomes.
Werner also emphasized the importance of monitoring for unintended effects of assessing quality metrics. Although quality metrics are always well meaning, the ways in which providers react to them or the ways in which care delivery changes in response to metrics can be surprising, said Werner. One risk to patients could result from “cream-skimming,” in which risk adjustment of patient outcomes is imperfect because providers treat patients who appear healthier, intending to maintain a high-quality rating on these outcome metrics, Werner continued. Because the patients receiving treatment are healthier to begin with, there is an appearance of improved
patient outcomes without true improvements in the quality of care provided (Konetzka et al., 2013; Werner et al., 2005). Thus, it is essential to construct metrics in a way that minimizes this bias.
In closing, Werner articulated lessons that could translate from clinical quality measurement to GME. First, data and methods for using patient outcomes to evaluate GME training programs are available; thus, using metrics based on patient outcomes is possible, although monitoring unintended consequences is a challenge. However, questions remain about whether patient outcomes occur over a time period that is short enough to make outcome-based metrics a feasible strategy to measure and improve GME. Finally, she said that leveraging policy and funding opportunities to identify ways to improve clinical quality measurement and influence provider behavior could benefit GME as well.
Linking Data Sources to Inform GME
Anupam Jena from Harvard Medical School provided several examples of research demonstrating how claims data, which includes physician NPIs, can be linked with other databases to better understand the characteristics of physicians who deliver high-quality care. The key is to take patient data that are already routinely collected, include information on the various providers that interact with each patient in the hospital, and then link that to information about those providers, said Jena. Data sources include claims data for Medicare or other major insurers, state inpatient data, Optum Labs,24 and Doximity,25 a medical professional network with detailed physician information.
In one study assessing the impact of resident duty hour reform on patients, researchers used Florida state inpatient data to compare patient mortality rates between newly practicing physicians who trained before versus after duty hour reform, using physicians who were 10 years out in practice as a control group. Results indicated that reductions in mortality were unrelated to duty hour reform, but rather to secular changes in hospital care (Jena et al., 2014). In another study evaluating how patient outcomes change with years of physician experience after residency, researchers linked Medicare claims data with Doximity data and found that hospital mortality increased with each year after internal medicine residency completion (Tsugawa et al., 2017). The opposite was true, however, in a similar unpublished study of surgeons, implying that a surgeon’s years of experience correlated with improved patient outcomes.26 To control for
___________________
24 See https://www.optumlabs.com (accessed December 20, 2017).
25 See https://www.doximity.com (accessed December 20, 2017).
26 Unpublished data.
selection bias in each of these studies, researchers studied hospitalist physicians and emergency weekend surgeries, both situations in which patients do not choose their physicians, and vice versa.
Jena emphasized the potential implications for using this type of research in accreditation and recertification. Assessing residency programs and medical schools on the basis of patient outcomes rather than processes is a useful avenue to consider, but there are challenges, he said. One challenge is determining whether the patient outcomes are due to residency training or to the types of doctors who choose particular residency programs. Werner had previously raised this concern, stating that a challenge for GME metrics includes separating selection effects from training effects, as high-performing physicians may cluster at particular programs. To address this question, Jena suggested using residency match data to study individuals at the cutoff between two residency programs, at which point the program they were admitted to was close to randomization, said Jena. Similarly, pairwise comparisons could be used together with linked residency match data and patient outcomes data to get a causal estimate of the impact of a particular training program on the long-term outcomes of patients who are treated by that program’s graduates, Jena continued.
A participant from Massachusetts General Hospital asked about strategies to account for the fact that multiple people provide care for patients. Jena answered that at the end of the day, even in team-based medicine, the attending physician always has primary responsibility. It is possible to see which other physicians are involved through claims data. Even with the involvement of students and nurses, whose data are not captured in claims data, one physician is responsible for the patient’s care, and that physician is billing Medicare (or other insurers) for the care.
Jena also provided examples of quality assessment using prescription data instead of mortality data. Researchers have demonstrated that within the same emergency department, the likelihood of a patient being prescribed an opioid by an emergency physician varies by nearly threefold across physicians (Barnett et al., 2017). Following these patients for 1 year after the original emergency department visit showed that patients who happened by chance to see a high-intensity opioid prescriber were 20 to 30 percent more likely to become a long-term user of prescription opioids, compared with patients treated by a low-intensity opioid prescriber (Barnett et al., 2017). Data on opioid prescribing can also be linked to Doximity data to see whether physicians training in specific residency programs or medical schools are more likely to prescribe opioids. The implication for GME is that specific programs could be identified with the goal of targeted educational interventions, which could subsequently be evaluated using similar data.
The keys, Jena emphasized, are obtaining support from organizations that hold necessary data to study questions related to GME outcomes,
linking multiple data sources, conducting robust empirical assessments that rely on quasi-experimental research strategies, and obtaining funding to conduct this research. He also stressed the need to train future researchers in these methods, and the importance of funding data acquisition and research methods.
Using Clinical Data for GME
Alvin Rajkomar from Google Brain and the University of California, San Francisco (UCSF), presented a series of studies he conducted at UCSF using both administrative and clinical data to guide how residents practice. He shared his thoughts on the kind of data to expect in the future. In his first study, Rajkomar created a program to analyze clinical notes in electronic health records (EHRs) to ascertain which diagnoses residents commonly see or rarely encounter (Rajkomar et al., 2017). In another study, Rajkomar wrote a program to provide interns with a list of patients for whom they had written notes while on rotation at UCSF to enable residents to follow their patients’ progress. This exercise showed that interns greatly valued the data, and he found that even when the interns had the wrong diagnosis, they learned from that, said Rajkomar. Some interns also noted moments of vindication where they had made the correct assessment. Finally, upon reading their own discharge summaries, interns realized how confusing some of their summaries were and subsequently improved on them (Narayana et al., 2017).
In a third study, Rajkomar emphasized that providing data feedback is not a trivial or simple exercise, and utility matters. He created a program that gave residents daily feedback on their identified quality improvement (QI) performance. In a randomized controlled trial, Rajkomar found this daily feedback on QI performance did increase resident performance; however, the residents disliked the feedback because they found it redundant (Patel et al., 2016). Rajkomar noted two other important lessons learned from these experiments. One is that attribution matters. Interns write notes, so finding their data is easier than it is for residents, whose contributions may not be reflected in the EHR. The second important lesson learned is that accuracy matters. If data are inaccurate for even a single patient, it is hard to win back the trust of the clinicians.
Future data will not come from clinicians entering data, said Rajkomar, but technology is going to capture the data that are generated in the course of clinical practice. For example, some hospitals are trying to collect data via Amazon’s Alexa27 or other kinds of voice dictation or assistants to document the clinical encounter (Singer, 2017). Other studies of “click
___________________
27 See https://developer.amazon.com/alexa (accessed December 20, 2017).
logs” that track what users are clicking on in the EHR could also provide valuable data (Arndt et al., 2017). Rajkomar also described a study using police body camera footage to understand how police officers are communicating with citizens, and noted that it just takes a small leap of logic to think about using this technology to assess communication between residents and patients, although it could become invasive (Voigt et al., 2017). In conclusion, Rajkomar stressed that it is imperative to use the data responsibly and reiterated the importance of having trainees access and analyze their own data in the future. Despite variations in resources in training programs, technologies to help trainees become better physicians should be democratized for all trainees, he added.
GME METRICS
Workshop participants divided into four breakout groups to discuss metrics that could be used to advance GME at four levels: (1) GME graduate level, (2) GME residency program level, (3) teaching institution level, and (4) regional and national levels (see Box 3).
GME Graduate-Level Metrics
Kelly Caverzagie from the University of Nebraska and Bridget McIlwee from ProPath and ACGME presented the top three metrics identified by the graduate-level metrics breakout group, with a focus on measuring outcomes expected of GME graduates. The first is competence, said Caverzagie, which could include individual performance, especially for procedural specialties, as well as team-based care and population management. A strength of this metric would be its orientation toward meeting public and professional expectations, but the metric is limited by the availability of valid assessment tools and the variability of standards across specialty boards, he noted.
Caverzagie said the second metric focuses on value of care (patient outcomes per cost of care) from the perspectives of both the public and the profession. The strength of value metrics is their focus on patient care. Value metrics would measure the actual care provided by graduates after they leave the residency or the fellowship program. A limitation is the difficulty in standardizing the assessment of a value-based outcome, said Caverzagie. Choosing Wisely28 could be used as a starting point for value metrics, Caverzagie added.
The third metric is professional engagement, said Caverzagie. A residency program fostering professional engagement puts the learner in an environment in which he or she can continue to evolve, grow, and engage
___________________
28 See http://www.choosingwisely.org (accessed November 14, 2017).
with the profession. Validated survey instruments exist to measure professional engagement and burnout, which are two sides of the same coin, he said. Taking into account the pressures of residency with an emphasis on clinician well-being is an important step to prevent and mitigate burnout, said McIlwee. When residents are burned out and choose in the end not to
practice, that reflects on the GME program’s value. The group discussed the possibility of creating a composite score of engagement and burnout to take both components into account. Several participants noted that challenges with measuring professional engagement include understanding what it means over the long term, parsing out all of the confounders of professional engagement, and tracing this metric back to the residency program.
GME Residency Program-Level Metrics
Furman McDonald from the American Board of Internal Medicine and Christina Al Malouf from Pennsylvania Hospital presented the top four metrics discussed during the GME residency program-level breakout discussion. The first category was workforce metrics that could be assessed at the institutional, regional, and national levels, said McDonald. Workforce measures connect to the societal need of training doctors. However, workforce metrics are challenging because residency program directors have limited ability to change GME to address workforce needs. Other challenges include a lack of clarity on how to define workforce needs, and the time lag between initial training and meeting workforce needs, he said.
The second focus was the quality of care delivered by the graduates of the residency program, said McDonald. Al Malouf added that this should include resident confidence and autonomy, as well as an aggregation of individual quality measures associated with a physician. Quality of care metrics have strong face validity and would be useful for public accountability but are limited by a lack of agreement on the definition of this metric. Furthermore, given the heterogeneity of quality metrics and patient populations, such assessments would require risk adjustment methodology, McDonald added.
Many group participants suggested specialty board certification rates as a third metric, which are already used in practice as a metric across most residency programs, said McDonald. Strengths of this metric include public accountability, easy measurability, availability, and connection to many other metrics of good care. The limitations of using board certification rate as a metric include variability across boards, lack of board certification for some specialties, and that board certification is a floor measurement, measuring basic competence, rather than a ceiling measurement of a program’s aspirational competence, he explained.
The fourth category of suggested residency program metrics was internal process measures, said McDonald, including the clinical learning environment, graduate data, professionalism measures, and patient outcome data. The strength of internal process measures is their ability to serve as a foundation for all the other metrics. McDonald emphasized the need for ACGME to benchmark internal process measures, moving toward
community standards. Al Malouf added that from a trainee perspective, such metrics should also include resident well-being. Limitations, however, include the subjectivity of some measures as well as the lack of standardization across institutions, he concluded.
Teaching Institution Metrics
Monica Lypson from the U.S. Department of Veterans Affairs (VA) and McKinley Glover from Massachusetts General Hospital presented five categories of teaching institution metrics discussed by the teaching institution–level breakout group, including graduate outcomes, communities of commitment, clinical learning environments, value, and evaluations for program accreditation. Marschall Runge of the University of Michigan previously explained that communities of commitment indicate an institution’s explicit declaration of commitment and responsibility for a specific area.
Regarding graduate outcome metrics at teaching institutions, Glover echoed previous comments, emphasizing a focus on graduate distribution metrics to meet workforce needs, including practicing in areas with a shortage of health professionals, and proportionately adjusting the distribution of trainees among needed specialties and subspecialties. He said another key metric is output of graduates, including their contribution to discovery science, community service, patient care, and so forth. Other key metrics include the quality and success of the training environment measured by the number of trainees who transfer across specialties, those who take additional years to complete their training, and drop-out rates, he continued. Additional important metrics include board certification rates and MOC. The strength of reporting these metrics, said Glover, includes implications for the public, especially because the residency programs are publicly funded. Graduate distribution and workforce metrics would necessitate reporting mechanisms that explicitly address needs in research, social health equity, and primary care. Glover and Lypson also discussed the potential unintended uses of such data as a challenge. Glover also emphasized the importance of process and outcome measures relating to the clinical learning environment, including evaluation of curriculum, knowledge of patient safety, and trainee outcomes in practice. However, creating a platform for these metrics could be a challenge, he said.
Finally, Lypson discussed the possibility of using currently available data, including the health care index (data sets covering changes in medical costs, employment, and education),29 and data on the last 6 months of life
___________________
29 See https://www.usnews.com/news/health-care-index/articles/2015/05/07/the-methodology-behind-the-us-news-health-care-index (accessed February, 8, 2018).
to measure value. The strengths of this approach are that data are available, and the metric is not specialty specific and reflects meaningful patient outcomes and cost. However, hospital culture may limit use of such value metrics, she said. Lypson also discussed the potential use of data from the Centers for Medicare & Medicaid Services (CMS) Merit-Based Incentive Payment System30 to drill down to the provider level. However, a challenge is linking to resident outcomes, Lypson noted.
National-, Regional-, or State-Level Metrics
John Norcini from the Foundation for Advancement of International Medical Education and Research and Jordan Warchol from The George Washington University addressed the topic of national-, regional-, and state-level metrics by presenting metrics that their breakout group suggested for four primary stakeholders, including self-regulators, such as boards and specialty societies, state and federal policy makers, patients, and trainees.
For self-regulators, Norcini and Warchol described five metrics, including board certification, patient outcomes, physician joy in practice, physician sociobehavioral skills, and professionalism and disciplinary action. Board certification shows breadth and depth of specialty and is a known standard, but it is limited in that it is knowledge heavy. They also noted that questions have been raised about the relevance and validity of MOC. Patient outcome metrics, as noted previously, are important to improve patient care and physician practice but are limited in GME assessment because of uncertainties concerning the appropriate timing and specific measurements. Metrics that assess joy in practice could lead to improved clinician well-being and thus improved patient outcomes, but it may be hard to modify and, because of its multifactorial nature, a challenge to measure. Most important to patients, Warchol argued, is physician sociobehavioral skills, which include team-based care, coordination of care, communication skills, partnering with patients, and understanding social determinants of health. However, challenges to such metrics include questions about validity, subjectivity, and expense. Finally, measuring professionalism and disciplinary actions could be important to protect patients. However, using these metrics appropriately is a challenge due to variability of sanctions across states, said Warchol.
For state and federal policy makers, the breakout group focused on metrics that could assess return on investment, including geographic distribution, specialty distribution, and provision of care to underserved populations after training, Warchol explained. Data are available to assess both geographic and specialty distribution metrics, but there are questions about
___________________
30 See https://qpp.cms.gov (accessed February 8, 2018).
whether the necessary clinical infrastructure is available where physicians are needed, or whether funding could incentivize physicians to move. Warchol added that requirements to provide care for underserved populations or to report related data are currently lacking.
Warchol discussed three metrics for patients: clinical outcomes, patient experience, and access to providers. Clinical outcome metrics may be challenging for patients to use if the personal relevance of the data is unclear. Patient experience metrics, on the other hand, which she said could be collected through programs such as Truth Point,31 may have limited utility if there is a lag time, or if all representative patient voices are not heard. Finally, Warchol identified access to providers as a key metric but noted the challenge of using the data to address gaps in a timely manner.
For trainees entering residency, understanding program characteristics, such as where graduates go and what they do (e.g., academics, community practice, caring for underserved populations) after training, is important. Warchol noted that assigning each trainee an NPI number could be beneficial in tracking this metric. Furthermore, she said that resident assessment of training is a critical metric for trainees, including whether the residents feel both confident and competent upon graduation, and whether they would choose their program again. Such data would provide a good assessment of the residency programs on a national level, but are limited by their inherent subjectivity, Warchol said.
CAN OUTCOME MEASUREMENT PROVIDE A PATH TOWARD EVIDENCE-BASED EDUCATION?
In discussing how outcome measurements could guide evidence-based education going forward, panelists provided examples of how they are using or could use data to modify their curricula, create innovative educational programs, and guide and assess how residency programs are meeting society’s medical workforce needs.
Answering GME Questions Using “Big Data” at New York University
Marc Triola from New York University Langone Health (NYU Langone) summarized some of the key questions regarding medical education, and how NYU Langone is using big data to address those questions. He said there are fundamental unanswered questions about the effectiveness and impact of medical school and graduate training programs. For example, are graduates prepared for independent practice? What specialties do they choose? What clinical conditions and procedures do they see and experience? What
___________________
31 See http://truth-point.com/our-solutions/rapidrounds (accessed December 19, 2017).
impact does medical education have on patients across the country? How does one medical school’s performance compare with that of others? Triola said the majority of educational impact lies in independent practice, yet few data beyond GME training exist. Current surveys of graduates and residency program directors help but suffer from a lack of depth and breadth. Furthermore, learners crisscross institutional boundaries, and there is a minimal feedback loop connecting graduates in practice and a school’s curriculum, advising, and mentoring. However, he said medicine is potentially the most data-rich specialty of all areas in higher education. The challenge is to collect and aggregate the measurement data across the medical education continuum (see Figure 2).
Over the past 3 years, said Triola, the NYU Langone School of Medicine has focused on building a rich and interconnected educational data warehouse, visualized in Figure 2 below. First, Triola and his team integrated data available from undergraduate medical education, GME, and continued professional development, including evaluations, assessment, and simulation data. The education data warehouse was merged with NYU Langone’s EHR clinical data warehouse, allowing real-time, seamless links between medical education data and the inpatient and NYU practice network, said Triola. For example, the system can link a first-year medical student’s multiple-choice answer with the clinical orders the student later
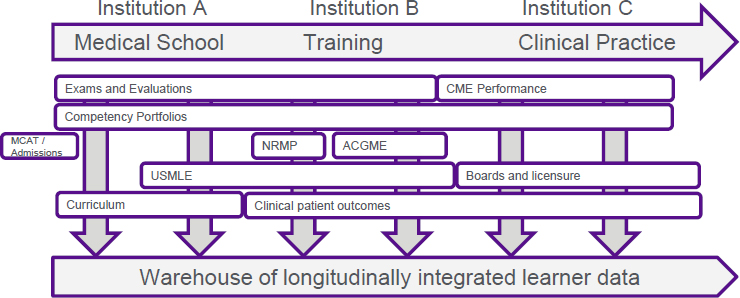
NOTE: ACGME = Accreditation Council for Graduate Medical Education; CME = continuing medical education; MCAT = Medical College Admission Test; NRMP = National Resident Matching Program; USMLE = U.S. Medical Licensing Examination.
SOURCES: Triola presentation, October 11, 2017; Triola M. M., Pusic M. V. The Education Data Warehouse: A Transformative Tool for Health Education Research. Journal of Graduate Medical Education. 2012:4(1):113–115.
placed and the subsequent clinical outcomes. As a result, the integrated data can be used for reporting, analytics, and dashboards, and for creating deidentified data to support medical education research endeavors. However, these analyses are limited to the 20–30 percent of students remaining at NYU after residency, Triola added.
To track graduates after they leave NYU, Triola and his team integrated several databases, including the AMA Masterfile32 for NYU, a database containing identifiable data for 8,500 current and former NYU medical students and 12,000 NYU GME graduates; CMS Physician Compare,33 an open database of doctors participating in Medicare that includes their NPI, medical school, and graduation year; the NPI database34; CMS Part D prescription database35; CMS usage and payment database36; and New York State SPARCS (Statewide Planning and Research Cooperative System),37 a database allowing for the reidentification of inpatient data, including data on quality of care, for every hospital in New York (see Figure 3).
Analyzing the combined data provides information about factors such as practice environment for NYU graduates, and the common diagnoses graduates are seeing compared with those across New York State. Furthermore, usage and payment data provide insights on the impact of graduates, including the number of Medicare outpatient visits nationwide and in New York State, and orders for statins, electrocardiograms, and chest X-rays for Medicare patients. In one analysis, Triola presented benzodiazepine prescription drug data from Physician Compare and CMS Part D data, and found a linear trend with the rate of prescriptions being lower for more recent graduates. However, looking specifically at NYU medical student data, improvements in prescription rates correlated with the year of NYU medical school curricular reform38—compelling data that deserve more investigation, added Triola. In another analysis, Triola demonstrated how AMA Masterfile and New York State SPARCS data can be used to assess differences in the value of care provided by NYU graduates. By looking at the number of high-cost procedures and death rates associated with NYU
___________________
32 See https://www.ama-assn.org/life-career/ama-physician-masterfile (accessed December 19, 2017).
33 See https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/physician-compare-initiative (accessed December 19, 2017).
34 See https://npiregistry.cms.hhs.gov (accessed December 19, 2017).
35 See https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Part-D-Prescriber.html (accessed December 19, 2017).
36 See https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier.html (accessed December 19, 2017).
37 See https://www.health.ny.gov/statistics/sparcs (accessed December 19, 2017).
38 Unpublished data.
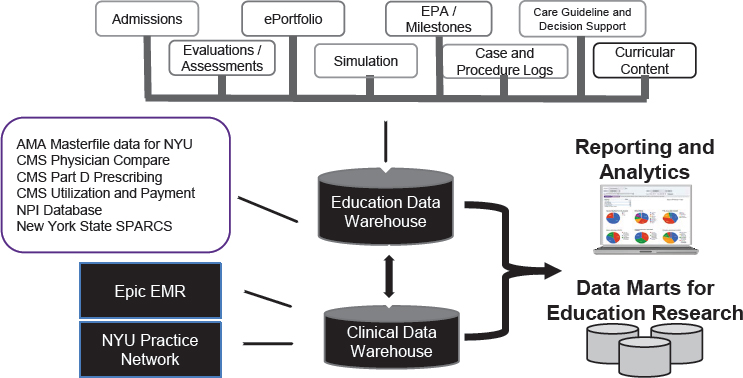
NOTE: AMA = American Medical Association; CMS = Centers for Medicare & Medicaid Services; EMR = electronic medical record; EPA = Entrustable Professional Activity; NPI = National Provider Identifier; NYU = New York University; SPARCS = Statewide Planning and Research Cooperative System.
SOURCE: Triola presentation, October 11, 2017.
graduates compared with other physicians, the combined data sets inform the potential need to revise a program’s curriculum.
Limitations to this approach, said Triola, include confounders, such as the possibility that the data are not measuring individual physicians but rather a team of care providers; the long lag time—it takes 8 to 10 years from when an individual starts medical school until his or her outcome data appear in public data sets; the diversity of GME versus clinical outcomes that can be measured—the outcomes are not focused on specific programs and may not be equally meaningful for each specialty; and, though vast, the data are still myopic, with gaps in Medicaid and Medicare data for specific specialties, the lack of VA data, and so forth. Responding to a participant’s question about the challenge of persuading the hospital to release EHR data, Triola responded that medical centers are going to get so much more value from the hundreds of millions of dollars they are spending on EHR systems if they are open to the world of innovation as opposed to just driving reimbursement and clinical operations.
In summary, Triola emphasized the opportunities for using currently available data to support evidence-based education. These data can inform curricular planning, transition to residency programs, mentoring and
coaching, and predictive analysis. Most importantly, said Triola, these data allow alignment of medical education outcomes with health care delivery system-level outcomes that matter to patients. To replicate the success of NYU in other programs, Triola stressed the importance of encouraging authorities at the regional, state, and federal levels to allow more data sharing where appropriate, and of sharing methods and models through consortia, such as the Accelerating Change in Medical Education Consortium at the AMA.39 The data exist and the opportunity is there, Triola concluded.
Outcomes-Based Education in Surgery
Rachel Kelz from the University of Pennsylvania described how national-quality data can be used to create innovative educational programs. The goal of GME, said Kelz, is to provide a safe learning environment, access to a meaningful clinical experience, and appropriate supervision for physicians to learn the skills and practices necessary to achieve optimal patient outcomes after the transition to independent practice, in order to meet the care needs of the U.S. population. Kelz emphasized the importance of targeting residency programs to implement improved surgical practice because targeting the 268 surgical residency programs is more efficient than attempting to reach more than 135,000 surgeons who practice at more than 5,000 hospitals40 (see Figure 4).
Kelz stressed the importance of asking the right questions and introduced Donabedian’s Quality Framework (Donabedian, 1966), which focuses on the structure, process, and outcomes of clinical care, as a relevant model for identifying meaningful questions to ask and answer about GME. Examples of questions include Does the program type affect the level of residency proficiency? How does resident work affect patient outcomes? Does the quality of GME vary across training programs? Kelz also presented a Framework for the Assessment of Graduate Medical Education (see Figure 5). The framework, Kelz explained, can help to guide the selection of balanced and comprehensive metrics to evaluate GME. She said that an assessment of GME should prioritize patient outcomes while also incorporating the personal effects of training and practice on physicians in a systematic fashion. She emphasized the need to examine the attainment of typical adult developmental milestones among trainees. Examples of such Milestones for trainees include financial independence and the development
___________________
39 See https://www.ama-assn.org/education/creating-medical-school-future (accessed December 19, 2017).
40 See http://www.aha.org/research/rc/stat-studies/fast-facts.shtml (accessed January 10, 2018).
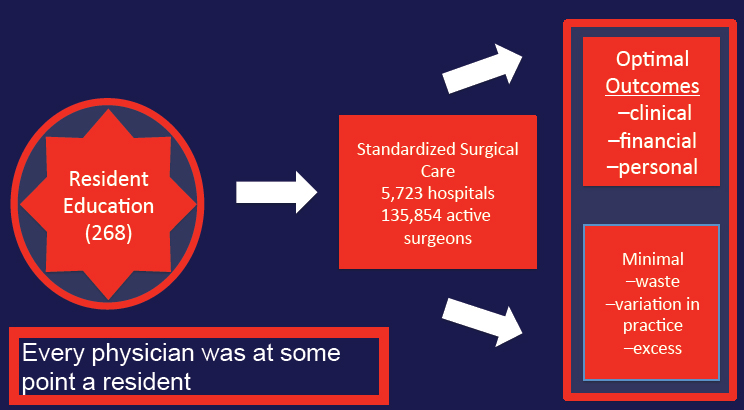
SOURCE: Kelz presentation, October 11, 2017.
of long-term, meaningful relationships, which she said are important measures for the system of GME (Sellers et al., 2017).
More data are available now than ever before to answer these GME questions, Kelz said. She emphasized the opportunity to use data linked by NPIs, including CMS data, state-based claims, registries, and data from EHRs, AMA, ABMS, and ACGME. In addition, a wealth of barely explored information exists on social media, Kelz added. She provided several examples of studies using such data to answer meaningful GME questions. In two studies, researchers compared surgical outcomes for physicians from different residency programs. One study showed a 30 percent difference across the low-performing and high-performing programs in obstetrics (Asch et al., 2009). Another study focused on general surgery found a 10 percent difference between low- and high-ranking surgical residency programs but also found significantly greater variation among surgeons with 5 years in practice compared to those with 10 to 20 years in practice (Bansal et al., 2016). These results imply that residency training effects are more relevant during the time of transition to independent practice than at later time points in the career trajectory, said Kelz. Highlighting the importance of careful methodology and statistical analysis for meaningful results, Kelz noted an ongoing study investigating surgical outcomes before and after reform of resident duty hours. Researchers used an analytical strategy with data matching designed to overcome the bias of changes in
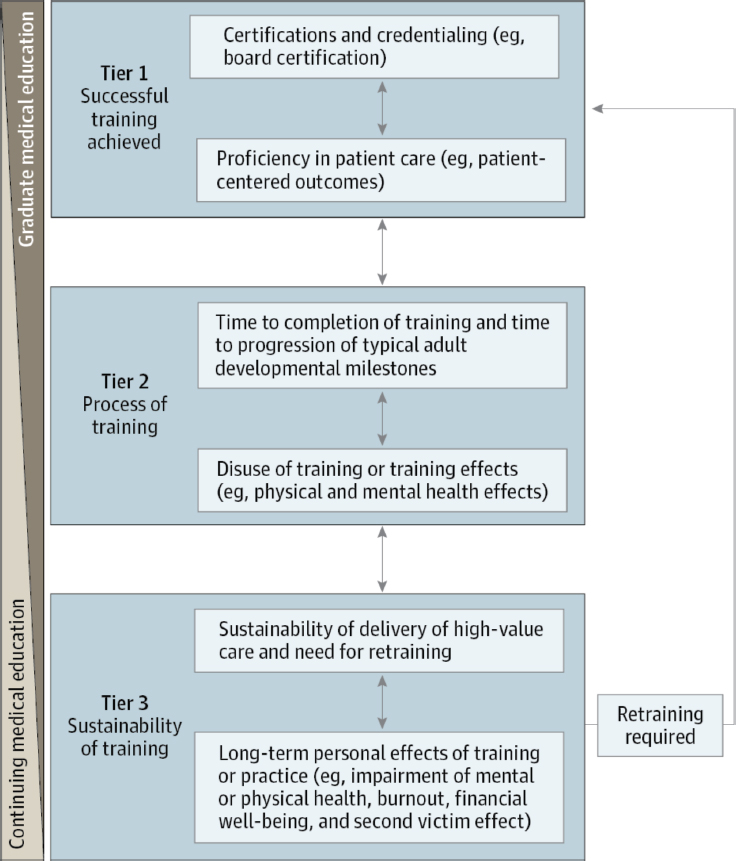
NOTES: Tier 1 includes standard outcome measures of residency training programs, such as certification and credentialing. Tier 2 includes measures of the physical and mental health effects of training and the opportunity costs (financial and otherwise) incurred by trainees. Tier 3 tracks the sustainability of training.
SOURCES: Kelz presentation, October 11, 2017; Sellers et al., 2017. © 2017 American Medical Association. May not be reproduced without permission.
practice over time and other confounding factors. Results from a pilot study showed that after appropriate matching and control for all of the measured confounders, there was no difference in patient mortality between new and experienced surgeons (Pimentel et al., 2015).
Highlighting the possibilities of translating clinical outcome data to evidence-based education, Kelz described the Quality In-Training Initiative (QITI).41 A collaborative under the umbrella of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP),42 QITI aims to provide residents with their outcome data, develop a curriculum for quality and safety, and improve data sharing with trainees across the country. Trained chart reviewers enter four pieces of information into a web portal to provide 30-day outcome data to residents on their patients. The concepts applied by QITI can be used for any surgical specialty and could be expanded for nonsurgical specialties as well. With the proper partnerships, it is surprisingly easy to execute, Kelz said.
To achieve evidence-based education using QITI data, Kelz and her team designed a study comparing outcomes associated with structural elements of surgical residency programs and resident actions. One study found that residents who discuss colorectal surgery procedures with the attending surgeon the day before a procedure were more likely to participate in the procedure and consider themselves a teacher. The study concluded that this advance discussion should be considered as a best practice in surgical education (Bailey et al., 2017).
Kelz also noted her experience with developing a program that sent residents and medical students into the community with surgical faculty to conduct educational campaigns. One program focused on early detection of colorectal cancer (Hoffman et al., 2016). In that program, residents and medical students found the program extremely beneficial. As a result, a self-sustaining community program run through the surgical interest group at the Perelman School of Medicine now brings health care–related information focused on surgical problems into community centers, houses of worship, and high schools to improve the health of the population that they serve. There are real opportunities like this to get physicians into the community and into safety net hospitals through undergraduate medical education and GME programs to improve care through patient and caregiver education before health services are needed, Kelz said.
In closing, Kelz noted that cost information should also be included in research, medical education, and clinical care. She emphasized that
___________________
41 See http://bulletin.facs.org/2013/11/the-acs-nsqip-quality-in-training-initiative-educating-residents-to-ensure-the-future-of-optimal-surgical-care/#.WiimwBiZM6g (accessed December 19, 2017).
42 See https://www.facs.org/quality-programs/acs-nsqip (accessed January 10, 2018).
although the possibilities for outcomes-based education are endless, with more data available now than ever before, questions need to be defined carefully to ensure that results are actionable and can be applied to improve education and, ultimately, clinical care.
Workforce Data and Metrics Based on Residency Program Outputs
Phillips from ABFM demonstrated how databases can be used to guide or assess GME program outputs relative to society’s medical workforce needs, including sufficiency, specialty and geographical distribution, and quality of care. Although the total number of graduating physicians is growing, he said, geographic distribution is uneven, resulting in underserved populations in many areas, including much of rural America. GME is not purposefully addressing population workforce needs, he reiterated. The community health needs assessment requirements of public hospitals (under Internal Revenue Service [IRS] regulation), including academic medical centers, require assessment of community needs and demonstration of related benefit provided. At least one major academic medical center reported its GME payments as a community benefit, and in 2012 GME funding was two-thirds of its reported benefit. However, GME funding is really just a pass-through of dollars, Phillips said, and many would have difficulty justifying their GME outputs as effectively meeting community needs. For example, one study found that changes in primary care and mental health graduate medical education do not correlate with changes in community need indicators (Coutinho et al., 2017).
Phillips described the GME Mapper,43 a tool to track GME programs, the production of physicians in primary care and rural environments, and data informing which student and program characteristics yield improved outputs in primary and rural care. The GME Mapper allows every institution to see its primary care and rural physician outputs over time, and provides a ranking of residency programs. For example, data from the GME Mapper shows major differences in two hospitals in Manhattan; at Mount Sinai, 26 percent and 7.6 percent of graduates went into primary care and rural settings, respectively, compared with only 8.6 percent and 1.4 percent at New York Presbyterian.
Phillips and his team linked graduate questionnaire data from the Association of American Medical Colleges (AAMC) with institutional, training, and student factors. The results highlighted the importance of rural birth, said Phillips. Students born in rural areas are 2.5 times more likely to end up practicing in rural settings, and two times more likely to practice
___________________
43 See https://www.graham-center.org/rgc/maps-data-tools/interactive/gme-outcomes.html (accessed December 19, 2017).
family medicine. Furthermore, students affirming interest in practicing in underserved areas in their medical school graduation questionnaires were three and four times more likely to serve in community health centers and rural health clinics, respectively (Phillips et al., 2009). Similar data from AAMC can be used to assess the impact of inner city, rural, and primary care clerkships and electives. In rural training track programs, 48 percent train in safety net settings, and 41 percent serve shortage areas; yet, these rural training tracks are “the ones that are dying on the vine right now,” said Phillips (Patterson et al., 2012). Finally, research using Medicare claims data and tracking physicians with their NPI demonstrates that the location of training matters. GME graduates whose training included service in a federally qualified health center (FQHC), or a rural health clinical or critical access hospital, were more likely to practice in such settings upon completion of training. Specifically, 38 percent practiced in a rural health clinic, 31 percent in an FQHC, and more than half in a critical access hospital (Phillips et al., 2013). Kelz also noted her experience with developing a program that sent residents in the community to do educational campaigns on early detection of colorectal cancer. Those residents found the program to be so beneficial that it evolved into a self-sustaining community program.
The impact of training programs on physician practice patterns is also relevant to quality care and competency, Phillips reiterated. Two studies found that those who trained in high-cost areas became high-cost physicians (Chen et al., 2014; Phillips et al., 2017). This imprint lasted more than 16 years, said Phillips, explaining that it took 16 years for physicians trained in high-cost settings to regress to the mean for their practice setting. Furthermore, there was no relationship between cost and quality, said Phillips, countering the argument that physicians producing higher costs might provide higher-quality care. Residency programs should take advantage of this powerful and potent imprinting potential to improve training, Phillips said. With future studies, Phillips and his team hope to identify training program components with these effects, and create interventions to make positive changes to residency programs.
Phillips emphasized the opportunities to make evidence-based changes to GME through purposeful faculty development and team-based training. For example, ABFM currently funds studies of residency programs along with the Macy Foundation. The boards have many roles, including stimulating innovation, and are willing to work with partners to do that, Phillips added.
PUBLIC POLICY IMPLICATION
Panelists described the role of federal and state policy in addressing physician workforce needs. Janis Orlowski from AAMC discussed the
importance of articulating which workforce goals to pursue and described potential implications of different goals. Carmen Hooker Odom, former president of the Milbank Memorial Fund, discussed the lack of alignment between GME goals and public policy priorities. Finally, Erin Fraher from the University of North Carolina (UNC) at Chapel Hill presented lessons learned from a study investigating state-based approaches to reforming Medicaid-funded GME.
Implications of Workforce Goals
What is the goal? Orlowski emphasized the importance of understanding the goal before developing the metric. A substantial amount of data is available on the physician workforce, but the key questions pertain to future planning. She said one potential goal is to address predicted physician shortfalls, noting that AAMC uses data on the effects of managed care, millennial recruitment, and physician retirement to project physician shortfalls. Reaching agreement on how many physicians are needed in the United States is an important step preceding the identification of appropriate metrics. However, the number of physicians needed depends partly on national public health goals, especially as the population demographics are shifting to older ages (see Figure 6), Orlowski said. For example, in one population health–focused scenario, 6.3 million more people could avoid a premature death between 2015 and 2030 if current public health goals are met. Initially, this improved population health translates to fewer hospitalizations and a reduced health care demand. However, by 2030, the addition of these 6.3 million elderly people would increase demands on the medical system, with projections of more than 6 million additional hospital inpatient days, 1.7 million more emergency department visits, and 16,500 additional doctors needed (IHS Markit, 2017).
Orlowski described the scale of the workforce implication of a goal focused on achieving equity in the use of health care, emphasizing that equity is understudied from a workforce perspective, and, currently, there is no national goal on equity in health care use. Orlowski described two ways to define workforce equity goals, and the implications for workforce needs. First, if everyone in the United States had access to health insurance and similar access to health care compared with populations in urban environments, 34,800 additional physicians would have been needed in 2015 (assuming that all care currently provided by physicians would be provided by them in the future) (IHS Markit, 2017). The second scenario is more troubling from a public health point of view, Orlowski noted. If the conditions of the prior scenario were met, and there was no difference in access based on race and ethnicity, so that underrepresented minorities could access health care at the same rate that the white population can, 96,800 more
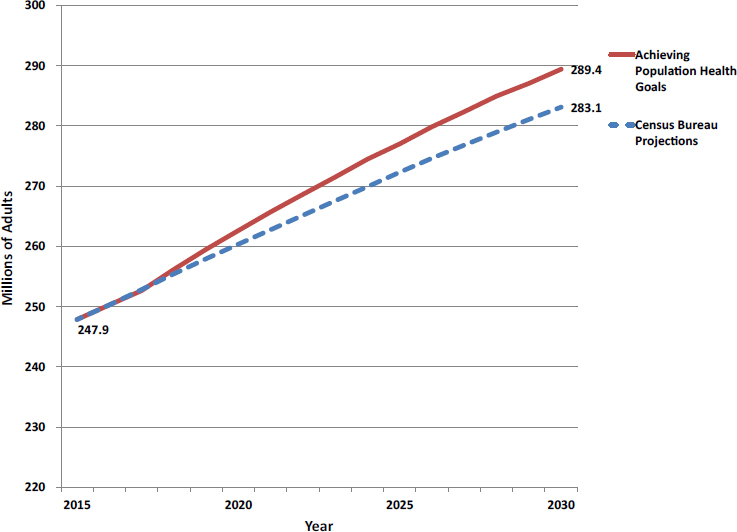
SOURCES: Orlowsky presentation, October 11, 2017; IHS Markit, 2017. © 2017 Association of American Medical Colleges. May not be reproduced without permission.
physicians would have been needed in a single year (IHS Markit, 2017). Even after accounting for overuse, currently estimated at 5–18 percent, there is still a significant need for physicians to achieve usage equity across the United States. Orlowski stressed the importance of applying these data to public policy.
Certain geographic areas have significant deficits, said Orlowski. She highlighted two examples emphasizing the important role of states in addressing such deficits. Nevada had the lowest GME to undergraduate medical education ratio in AY 2013–2014. They had 814 students, but only 373 residents (AAMC, 2017). These data suggest that physician shortages in the area will continue, as many residents stay within the geographic area of their training. The state holds a very critical role, in addition to the federal government, in the discussion of how to deal with the physician workforce in that particular state. Orlowski also provided an example of a state with effective statewide collaboration efforts to meet workforce needs. In northern Wisconsin, the state collaborated with the Medical College of
Wisconsin to create new GME programs in primary care and in psychiatry to meet the needs of the rural population (Boulton, 2016).
Orlowski concluded by noting that in the early 2000s, AAMC called for an increase of 30 percent in the number of matriculates in medical schools, and undergraduate medical education will exceed that goal (AAMC, 2017). However, whether or not the physician workforce meets the demands of public health, national, and regional equity goals should be a part of the national discussion, she said.
Alignment Between GME Goals and Public Policy Priorities
Hooker Odom, former president of the Milbank Memorial Fund, highlighted the need to align GME goals and public policy priorities. She discussed the importance of the clinical learning environment, specifically, the need for standardization across learning institutions in order to produce physicians who can provide effective and high-quality care. She also said that the 2014 GME report documented a lack of skills and knowledge needed for 21st-century health care, such as a lack of proficiency in care coordination and team-based care (IOM, 2014). She said many of these challenges could be addressed through policy changes that enable more skill building within the clinical learning environment in order to improve health care delivery. Finally, she highlighted the finding that lower spending on social services, relative to higher spending in health care, is associated with poorer health outcomes (Bradley and Taylor, 2013). She urged public policy makers to take these findings into consideration when developing health care policies and making funding decisions. Hooker Odom also outlined several important considerations from a public policy maker’s perspective. These include the racial and ethnic diversity of clinicians, a challenge that is exacerbated by the lack of socioeconomic mobility (Reeves, 2017), fiscal transparency, and accountability within GME institutions and health care organizations, and gaps in physicians’ knowledge and skills, GME faculty and staff development and compensation, and workforce specialty mix and geographic distribution.
Lessons Learned from State-Based Approaches to Reforming Medicaid-Funded Graduate Medical Education
Fraher from UNC said that action at the federal level has stalled on GME, so states are developing their own strategies. She said states are actively seeking to use data and metrics to determine where to invest in GME and how to evaluate the return on investment. Fraher described results from a qualitative research study UNC conducted from December 2015 to July 2016 to investigate how states are using Medicaid dollars to
reform GME and identify innovations and challenges. The study included two interviews with HHS officials, governors, staff, medical school faculty, residency program directors, primary care associations, and others in each of 10 states across the country (Michigan, Minnesota, Montana, Nebraska, Nevada, New Mexico, New York, Ohio, South Carolina, and Virginia). Two interviews were conducted in each state. States were selected based on having undertaken efforts to reform Medicaid GME.
One finding was that the impetus for GME reform stems from multiple sources, said Fraher, and included maldistribution of physicians by specialty, geography, and setting; ensuring that there are enough GME slots to match medical school expansions; potential loss of Teaching Health Center funds; and disparities in GME funding received by different training institutions in the state. Most states had a champion who articulated the vision, coalesced stakeholders, and worked with executive/legislative branches, as well as an implementer, often located in the Medicaid office. The role of the implementer was to determine how to change a GME Medicaid payment, modify the state plan, and apply for a 1115 waiver.44
Reforming GME financing is harder than it looks, said Fraher, noting that state GME reform actions center around several related strategies. One is to figure out how to better leverage existing Medicaid funds, including pursuing 1115 waivers to modify federal rules for allocating GME funds.45 States are also trying to delink GME funding from Medicaid claims, which is particularly important as declining inpatient admissions will result in a smaller Medicaid GME funding pool. Rather than redistributing existing funds, which often encounters resistance from teaching hospitals, states often seek new appropriations. These funds are sometimes used to create innovation funding pools, Fraher said. States are also investing in innovation by providing seed money for new training programs and by funding rural rotations. Dan Burke from the University of Colorado added that state-based initiatives supporting primary care and rural programs are more vulnerable than the CMS funds. When there is an economic downturn, he said Medicaid is one of the first things to be cut in a state budget because it is one of the larger components of the budget.
Fraher noted that oversight bodies had an important role in GME reform. Oversight bodies play a critical role, she said, in educating legislators about state workforce needs. Oversight bodies can use data to determine where GME funds should be targeted and help navigate competing
___________________
44 See https://www.medicaid.gov/medicaid/section-1115-demo/demonstration-and-waiver-list/index.html (accessed January 23, 2018).
45 See https://www.medicaid.gov/medicaid/section-1115-demo/about-1115/index.html (accessed November 14, 2017).
interests of stakeholders. These oversight bodies included a range of GME stakeholders and were always advisory rather than authoritative, she said.
State officials interviewed in the study highlighted the current lack of transparency and called for increased transparency to better understand what they are paying for with GME funds, said Fraher. In some states, publishing how much money individual institutions received stimulated reform. The study also found calls for more accountability. States currently focus on fiscal accountability for Medicaid funds, not workforce outcomes, Fraher said, while training institutions focused on quality of training. Thus, the idea of accountability for workforce outcomes represented a paradigm shift. Interviewees voiced a strong desire to move toward a system that better aligned funding with population health needs, but they were cautious about how much training programs could be held accountable for workforce outcomes.
States need metrics to assess return on investment to justify appropriations for Medicaid, Fraher noted. Data collection and analysis were seen as critical components to aligning GME spending with population health needs, Fraher reported. However, interviewees said they needed financial and technical support to collect workforce data and to develop and operationalize metrics and analytical capacity. She noted that many states lack the analytical capacity to use available workforce data to help inform GME policy decisions. To help fill this gap, UNC has created a data visualization tool called DocFlows,46 Fraher said. DocFlows allows users to query, download, and share maps showing interstate moves by residents and actively practicing physicians in 36 specialties. UNC is also in the process of creating a GME policy toolkit for state policy makers that will describe how to use different data sources to inform state-level GME policy discussion.
In closing, Fraher said state efforts to develop and operationalize metrics will likely evolve, but slowly. As one interviewee put it, “This is a simmer process. This isn’t a microwave process.” Finally, despite limited progress, she said states have much to learn from each other, and federal policy makers also have much to learn from states in GME reform.
Several participants discussed the idea of targeting GME funding to places in need. Craig Lisk from Craig K. Lisk Health Policy Analysis asked about the need to differentiate how residency programs are funded. Funds should be targeted, said Orlowski. But Fraher added that it is a challenge, noting that even after transferring some GME positions to rural areas and primary care, expansion of that workforce did not occur. The workforce for rural health care, primary care, psychiatry, and general surgery is not expanding, she said. Kathleen Klink from the Office of Academic Affiliations at the VA noted that the VA has increased its workforce by 750 physicians,
___________________
46 See docflows.unc.edu (accessed November 14, 2017).
and through legislation, has placed GME positions in low-resource areas. But infrastructure support is needed in these situations, Klink emphasized, including faculty support, faculty development, space, transportation, and, in some cases, housing.
PRIVACY VERSUS TRANSPARENCY
Panelists considered the potential trade-offs between privacy and transparency and discussed when public reporting is appropriate, the potential risks and benefits of transparency, and the potential uses of data by stakeholders, beginning with the ethical argument for sharing or withholding data from the public. When people are in training, their formative assessments, as they strive to become proficient, should not be available to the public, said Smith from Hofstra/Northwell. However, careful analyses of good summative metrics that correlate with quality of care at the end of training could benefit patients, Smith continued. David Hoyt from the American College of Surgeons said that information about a provider’s competency is important to informed consumers and is a component of informed consent. Several participants noted the importance of balancing privacy versus transparency. However, to justify potential privacy risks, the data shared have to be meaningful, said Al Steinman from Saint Joseph Hospital in Denver.
Participants emphasized the value of sharing deidentified data with researchers to assess GME. Salsberg asked whether people in organizations are willing to collect and share data for research purposes, which is critical to inform GME and the health care system. Hoyt responded that the American College of Surgeons currently has deidentified databases associated with each of its 2,700 surgical training programs.47 Research and focused feedback of information valuable to individual residency programs is a reward for providing those data to a consortium, said Smith, as he expressed support for making data available for research purposes.
Several participants discussed the benefits of data sharing and transparency from the perspective of stimulating quality improvement and reducing cost. Smith advocated for the public release and scrutiny of data on residency program and teaching institutions, not to punish, but to stimulate competition and improvement. Hoyt agreed that sharing data can stimulate quality improvement. For example, an American College of Surgeons study with 150 hospitals showed that by simply sharing data publicly and with the physicians, complications were reduced by 82 percent. This study showed that mortality was also reduced, which, in combination with complication reduction, then translates into cost savings (Hall et al., 2009). Smith said hospitals and practices would benefit from data on transitioning
___________________
47 See https://www.facs.org/quality-programs (accessed January 12, 2018).
new physicians because it would highlight their strengths, weaknesses, and capabilities and thus make the orientation process of new physicians safer. It could also enable a more positive experience for the new physicians, he added. Chaudhry raised the potential for overmeasurement, which could pose a potential risk to quality care by overburdening people with unnecessary metrics. Smith agreed that too much measurement is a potential risk, emphasizing that measurement should be meaningful and carefully implemented.
Regulators also want data, said Smith. They probably could do positive things with the data, but they also could inadvertently do something disruptive or harmful, Smith continued, highlighting a potential risk of data transparency. Payers are also interested in performance data, Smith said, but many care providers are concerned about how such data would be used. For example, if data are shared too widely or misused, the willingness to report data will decline, said Hoyt. It is important to establish a culture that is nonpunitive and fosters learning and improvement, he continued.
Panelists also noted that not all metrics will apply equally in all care settings. For example, it may be more difficult to meet benchmarks for clinical outcomes when providing care to disadvantaged populations because the social determinants of health can affect clinical outcomes and other metrics.
Residency program applicants would also benefit from GME data by potentially gaining insights on what happens to program graduates—if they are “good doctors with good job prospects, and if they get the great fellowships,” said Smith.
IMPLEMENTATION
Deborah Powell from the University of Minnesota Medical School asked workshop participants to consider next steps—to begin to implement some of the ideas heard and discussed throughout the workshop. Powell discussed the need for balanced approaches in educational innovation and suggested that pilot projects are a good way to achieve this balance. For educational innovations of this magnitude, said Powell, a key issue to consider is the pace of innovation; there is a risk of doing too much too quickly and then finding that the desired results are not being achieved, as well as a risk of doing too little so that the efforts are not relevant.
Powell described two examples of pilot projects relevant to GME innovation that could potentially be scaled into larger-scale projects for testing new paradigms. Pilot projects are relatively flexible, allowing learning and modification as the project progresses, which can help inform the design of larger subsequent projects, she said. For example, the ACGME Milestone Project started out as a pilot, beginning with only three residency programs and then adding another four to enable learning over time before including
all residency programs (Swing et al., 2013). She added that multiple data sources were used to develop the GME Milestones. The pilot project on Education in Pediatrics Across the Continuum (EPAC) is testing a model of true competency-based education at four sites, with variable time to advancement through medical school and GME into practice. In the first cohort, 8 of 12 students met competency thresholds in the first semester of their fourth year of medical school and advanced to GME a full year ahead of the remainder of their classmates (Andrews et al., 2018). The most important lesson learned from these pilots, said Powell, is that the learners (medical students in the case of EPAC) and the faculty are essential to the project’s success, and without their buy-in and support, projects like EPAC will fail. She also noted that more data were collected than expected, necessitating a data repository, and that data can be used in multiple ways and in a variety of projects. In addition, she said an institutional sponsor is needed for credibility, and she cautioned that a project never unfolds exactly as planned, so program implementers should expect the unexpected. For example, the cost of pilot projects is often higher than anticipated, so additional funding sources may be required. Finally, she emphasized that regulatory bodies can offer a lot of flexibility with a pilot.
Powell instructed participants to break into groups to discuss implementation challenges and four key questions: (1) How can “buy-in” be achieved? (2) Should providing data be a requirement? (3) How should a national database be maintained and funded? and (4) What infrastructure is required?
Achieving Buy-In and Requiring Data Reporting
Dave Conklin from the Vanderbilt University Medical Center and Lisa Nash from the University of North Texas Health Science Center highlighted two key strategies to achieving buy-in for GME metrics, based on the remarks made by their discussion group. The first is defining the purpose of a national GME database and making sure that purpose is effectively communicated to all stakeholders, including trainees, programs, and institutions, said Conklin. The other major element to achieving buy-in is adequately addressing privacy concerns. Defining what level of aggregation is sufficient to protect privacy, but still granular enough to support initiatives and quality improvement and other aims, will be critical, said Nash. The data should be protected to prevent misuse of data, and pilot projects could help mitigate unintended consequences, said Conklin. He added that some data sharing would likely need to be mandatory and global, while other data could be selected as relevant to the mission of the teaching institution or residency program.
Deborah Driscoll from the Hospital of the University of Pennsylvania and Laura Higginbotham from UNC summarized the discussions of the breakout group they led, saying that mandatory reporting requirements for publicly funded GME programs should be put in place but limited to well-defined core metrics. Initially, residency programs and teaching institutions would be encouraged to voluntarily report on specialty-specific metrics, Driscoll said. Driscoll also emphasized that distrust related to the risk of data misuse is a potential barrier to data sharing.
Several discussion group leaders highlighted the need to minimize the administrative burden and cost of reporting data, especially for under-resourced institutions, to increase buy-in and promote initial voluntary data reporting. To achieve that goal, reporting needs to be simple and budget neutral, said Driscoll. Some institutions are going to be better equipped than others to engage in this process and collect data, Conklin said. He added that using data that are already available could help relieve the administrative burden of establishing a common GME database.
Discussion group leaders also highlighted access to data as a key component of achieving buy-in and encouraging voluntary data contributions. If residency programs could access aggregated data and benchmark their program against others, that would be an incentive to participate, said Driscoll. Conklin agreed that identifying feedback loops for the data should be a key component to achieve buy-in. He also noted that linking metrics to funding provides a fiduciary interest in participating.
Several participants discussed the possibility of using data to rank institutions. Nash said her discussion group was opposed to a system that would enable ranking across institutions because it might impede buy-in, and instead proposed a system with customized dashboards that would allow one institution to compare themselves with others on various metrics. For example, such dashboards could enable individual trainees to access and compare their own data to those of their peers, and residency programs could compare their performance to others, said Nash. However, Eric Anderson, a public participant, said that if quantitative data are collected, they will be used to rank. Anderson recommended a system in which data are objective and valuable to the reader, rather than the ranker. For example, rankings about which residency programs generate the most physicians who go into rural practice or which programs have the most contact with low-income urban patient populations should be available because such data could influence residency selection and funding decisions, said Anderson.
How Should a National Database Be Maintained and Funded?
Salsberg from The George Washington University Health Workforce Institute and Laura Ostapenko from Brigham and Women’s Hospital
summarized the discussion of the breakout group focused on maintaining and funding a national database.
Salsberg emphasized the importance of building on existing data sets, noting that an inventory of current GME databases would be helpful. Several organizations already have extensive data, said Salsberg, so it would be far more cost-effective to build on those. Furthermore, increasing the transparency of existing databases might, in itself, encourage change, said Ostapenko. Recognizing that various stakeholders have different interests in the data, Ostapenko said that conducting a needs assessment could help to ensure optimal design of a national database.
Salsberg described potential options for the governance of a national database. One option for governance is through HHS, including CMS and the Center for Medicare & Medicaid Innovation, because they are paying for GME through Medicare and Medicaid. CMS also already manages extensive data on GME programs, but it is a different role to develop a database that would be shared with the community, Salsberg noted. Powell said finalizing the specific details, including where within the agency it would be governed and how it would be managed, is a bigger challenge.
Several participants suggested that governance should remain within the GME community. However, it would likely require a broad coalition of existing organizations, as well as individuals who could champion this approach within those organizations to move it forward. Noting a challenge to this approach, Salsberg added that collection and analysis of high-quality data would be required along with broad participation and access.
To minimize costs, several participants suggested building on existing data sets using the Data Commons model. That model, said Salsberg, could bring together data from many existing organizations, including the AAMC, ACGME, and AMA, who have data in their Master File for physicians in training and in practice over the long term. Katsufrakis commented that the primary goal in the development of the Data Commons was not to create a database but rather to create a system that would allow real-time access to the existing databases. The individual data owners maintained the authority to release or not provide information for various different uses.
What Infrastructure Is Required?
John Duval from ACGME and Medhanit Tekle from the Institute for Family Health in Harlem summarized the discussion of the breakout group focused on infrastructure, and outlined five important elements of an infrastructure for GME metrics, including a collaborative learning community, an honest broker, a hosting center, a granting organization, and leveraging of current efforts. Duval said the infrastructure has to be scalable and flexible enough to promote local, regional, and state engagement along the way,
and he added that development of a GME database would need to begin with dialogue among the various stakeholders to inform whatever ultimate structures are assembled. Powell noted that many organizations have a long history of working together.
Tekle noted that the breakout group members described “infrastructure” broadly, to include people, widgets, hardware, systems, a process, control, and collaborations among many teams and networks, and she noted the importance of a collaborative learning community to create best practices. One lesson learned from the experience with ACGME was the importance of being informative rather than authoritative, Tekle said. Duval said the group advocated for a quasi-independent organization to serve as the role of an honest broker.
Discussion group members suggested setting up a hosting center with an aggregated group of technical experts that could help participating organizations to report and use the data, Tekle said. To incentivize innovation, funding would be needed for pilot tests. Finally, Tekle said the group emphasized the importance of leveraging current efforts, perhaps including large data aggregators such as Vizient,48 to realize a shared benefit. She also said the breakout group members revisited the need to be mindful about how these data are used to ensure continued engagement by all participants.
ORGANIZATIONAL REACTIONS
Malcolm Cox from the University of Pennsylvania asked panelists to consider the next steps toward achieving a common systemwide approach to collecting consistent data that could be used to assess the quality of GME, with the ultimate goal of improving health care, including how to bring together disparate constituencies and identify resources. Panelists representing several stakeholder organizations provided their reactions to the workshop’s presentations and discussions.
Several panelists emphasized that the next step should be to convene key leaders within the medical profession to discuss the various potential strategies and decide what would work best (with minimal unintended consequences) and to evaluate resources. One critical challenge, noted William Pinsky from the Educational Commission for Foreign Medical Graduates and the Foundation for Advancement of International Medical Education and Research, is to identify a neutral body to convene the organizations. Cox also noted that some data are already rapidly accumulating, and he emphasized that if the medical community does not move quickly, other entities will use the available data in ways the profession may not want.
___________________
48 See https://www.vizientinc.com (accessed November 14, 2017).
Several panelists emphasized the need to shift the focus from inputs to outputs and outcomes. Those outputs bring a different dimension to the discussion, said Cox, and he also stressed the need to look beyond learning outcomes to patient population and system outcomes. Nonetheless, assessing patient outcomes is challenging because they are confounded by complexities such as patient risk and the clinical learning environment, he said. Steven Shannon from the American Association of Schools of Osteopathic Medicine emphasized the importance of workforce outcomes in relation to the societal support provided to GME and the need to look at both team-based and individual learning outcomes. Carolyn Clancy from the VA agreed with the need to focus on outcomes of care and helping people manage their own chronic illnesses. Timothy Brigham from ACGME noted that accreditation is resolutely moving toward a more outcomes-oriented approach, but Mira Irons from ABMS cautioned against tying GME to long-term patient outcomes until methods are developed to clearly define the individual physician’s contribution to the care of the patient and subsequent outcome. Clancy highlighted the increasing demand to use data to anticipate the future needs of education as well as those of the health care delivery system. Cox also emphasized the importance of a systems approach and how the different components of the educational and delivery systems interact to shape the clinical learning environment (IOM, 2015).
The need for and challenges of data sharing were emphasized by many participants throughout the panel discussion. Pinsky said his cynicism about the willingness to share data stems from the lack of progress of the Data Commons, with no participants beyond the six founding members. The Data Commons, he continued, is a good way to protect one’s database but still facilitate appropriate data sharing. He added that he hoped the interest and enthusiasm expressed by workshop participants would translate into a willingness to share data. Irons said that any system of data sharing should include an agreement on transparency aligned with the purpose and use of the shared data. Clancy agreed that data sharing should be targeted for a specific purpose; it will not be easy, she said, but it is worth the effort.
One challenge to sharing and providing data, noted by several panelists, is the relatively fragmented U.S. system of specialty boards and accreditation. In other countries, certification and accreditation are overseen by the same organization, said Brigham and Irons. Stephen Shannon from the American Association of Colleges of Osteopathic Medicine added that there is further fragmentation between D.O. and M.D. training programs, and he recommended including osteopathic physicians in discussions of GME metrics.
Finally, Clancy said that creating efficiencies in the system could liberate resources that could be devoted to shared efforts. The collective resources that go into credentialing and privileging as well as ongoing training and
professional evaluation just at the VA are substantial, and that is multiplied many times over throughout the country and for physicians who are affiliated with more than one system, she added.
CLOSING REMARKS
George Thibault of The Josiah Macy Jr. Foundation said that GME reform has been on the national agenda since the 1950s, but the conversation has now reached a turning point. Six regional conferences recently co-sponsored by academic medical centers focused on innovation and creativity rather than governance and finance, and that, coupled with this workshop, has changed the tenor, with a focus that is now more meaningful to the trainees and the public, he said.
Thibault summarized seven themes from the workshop discussions. First, he said that measuring and reporting GME outcomes are important for professional accountability and to justify public funding. There was a resounding consensus on this point, and that is a very important outcome of this meeting. However, many details need to be addressed to achieve this goal.
Second, many data are already available, and there are many opportunities to use those data in novel ways. For example, presentations at the workshop noted that data are currently collected by AAMC, ABMS, ACGME, AMA, CMS, HRSA, NBME, the VA, and state databases. Thibault noted that conversations are ongoing about how to aggregate existing data to enable new analyses and uses. Presentations by people engaged in research described novel use of EHRs and big data to assess clinical outcomes, said Thibault, and innovative leaders in the GME community should embrace this approach.
Third, Thibault reviewed the need for meaningful metrics at the level of trainees, residency programs, and teaching institutions, as well as at the national level. This includes information about what graduates are doing and how they are performing across clinical and academic settings. Patient outcomes should be tracked to assess the quality and value of care provided. It is also important to monitor the well-being of trainees and clinicians by addressing such factors as commitment and engagement in the medical profession and the joy of practice.
Fourth, Thibault said the workshop discussions demonstrated the challenges associated with assessing and guiding the physician workforce distribution and composition. Where residents train makes a difference, he said, and the experiences residents have during their training influence their decisions, the type of care they provide, and their capabilities. However, Thibault noted that state and local initiatives can make a difference and have already made some progress in addressing workforce gaps. He
suggested that the GME community develop a commitment to address physician workforce challenges.
The fifth theme that Thibault highlighted is that challenges to gathering and using data are complicated, but not insurmountable. Complexities include the need to ensure the quality and relevance of data, ownership, privacy issues, and the potential for unintended uses and unanticipated consequences. Effectively addressing such issues will require resources, input from data experts, and involvement by the people most affected, he said.
The sixth theme to emerge was the need to fund and conduct GME research, Thibault said. He also highlighted the need to invest in the careers of individuals who conduct such research. For example, the National Center for Interprofessional Practice and Education49 is a unique partnership that was initiated by a grant from HRSA with additional contributions from four foundations and the hosting academic institution, the University of Minnesota. That could be a model, he said, to fund research and serve as a repository for best practices. Thibault also described his work with the Macy Faculty Scholars Program,50 which promotes the careers of innovators in nursing and medical education.
Finally, the seventh theme of the discussions focused on the concept of a data repository for assessing GME outcomes, said Thibault, noting that two questions came up repeatedly: Where and how should a repository be established? and Who is responsible for the data? He said there is generally a strong preference in the profession for self-regulation. However, Thibault challenged that perhaps the medical and GME communities are not fulfilling all of their responsibilities and that it is time to consider values other than self-regulation. The GME community may not be able to do this alone, and it may need to accept the idea that it needs to partner with government and regulatory bodies, said Thibault. He provided several suggestions for potential next steps:
- First of all, he said it is important to maintain momentum and to capitalize on the energy and enthusiasm displayed at the workshop.
- As a follow-up to the workshop, Thibault recommended convening four expert groups, each with a separate focus, including metrics, policy, research, and funding.
- He also suggested convening all of the organizations with relevant data to talk about the rules of engagement for a data repository in a neutral setting.
___________________
49 See https://nexusipe.org (accessed December 19, 2017).
50 See http://macyfoundation.org/macy-scholars (accessed December 19, 2017).
- Next, Thibault emphasized the role of institutions and encouraged them to pilot innovative ways to provide feedback to residency programs and trainees.
- The boards and professional organizations also need to be engaged, said Thibault, as he recommended that each of the boards and other professional organizations develop their own pilots.
Thibault reminded the workshop participants that trainees need to be a part of the discussions going forward. Trainees add so much to the discussion, he said. He congratulated participants on a “fantastic, stimulating, and uplifting meeting,” but added, “it has only just begun.”
REFERENCES
AAMC (Association of American Medical Colleges). 2017. 2017 State Physician Workforce Data Report. https://members.aamc.org/eweb/upload/2017%20State%20Physician%20Workforce%20Data%20Report.pdf (accessed February 9, 2018).
Andrews, J. S., J. F. Bale, Jr., J. B. Soep, M. Long, C. Carraccio, R. Englander, and D. Powell. 2018. Education in Pediatrics Across the Continuum (EPAC): First steps towards realizing the dream of competency-based education. Academic Medicine 93(3):414–420.
Arndt, B. G., J. W. Beasley, J. L. Watkinsson, W. T. Temte, C. A. Sinsky, and V. J. Gilchrist. 2017. Tethered to the EHR: Primary care physician workload assessment using EHR event log data and time-motion observations. Annals of Family Medicine 15(5):419–426.
Asch, D., S. Nicholson, and S. Srinivas. 2009. Evaluating obstetrical residency programs using patient outcomes. JAMA 302(12):1277–1283.
Bailey, E. A., A. P. Johnson, I. L. Leeds, R. L. Medbery, V. Ahuja, T. VanderMeer, E. C. Wick, B. Irojah, and R. R. Kelz. 2017. Quantification of resident work on colorectal surgery. Journal of Surgical Education. pii: S1931-7204(17)30445-2. Epub ahead of print. https://www.ncbi.nlm.nih.gov/pubmed/28986275 (accessed April 23, 2018).
Bansal, N., K. D. Simmons, and A. J. Epstein. 2016. Using patient outcomes to evaluate general surgery residency program performance. JAMA Surgery 151(2):111–119.
Barnett, M. L., A. R. Olenski, and A. B. Jena. 2017. Opioid-prescribing patterns of emergency physicians and risk of long-term use. New England Journal of Medicine 376:663–673.
Boulton, G. 2016 (August 23). Medical residency programs expanding. Online. Milwaukee Journal Sentinel. https://www.jsonline.com/story/money/business/health-care/2016/08/23/medical-residency-programs-expanding/89121480 (accessed March 8, 2018).
Bradley, E. H., and L. A. Taylor. 2013. The American health care paradox: Why spending more is getting us less. New York: PublicAffairsTM.
CDC (Centers for Disease Control and Prevention). 1999 (April 2). Ten great public health achievements—United States, 1900–1999.https://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm (accessed January 4, 2018).
Chen, C., S. Patterson, R. Phillips, A. Bazemore, and F. Mullan. 2014. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA 312(22):2385–2393.
Coutinho, A. J., K. Klink, P. Wingrove, S. Petterson, R. L. Phillips, Jr., and A. Bazemore. 2017. Changes in primary care graduate medical education are not correlated with indicators of need: Are states missing an opportunity to strengthen their primary care workforce? Academic Medicine 92(9):1280–1286.
Donabedian, A. 1966. Evaluating the quality of medical care. Milbank Memorial Fund Quarterly 44(3):166–206.
Donnon, T., A. Al Ansari, S. Al Alawi, and C. Violato. 2014. The reliability, validity, and feasibility of multisource feedback physician assessment: A systematic review. Academic Medicine 89(3):511–516.
Dreyfus, S., and H. Dreyfus. 1980. A five stage model of the mental activities involved in directed skill acquisition. California University Berkeley Operations Research Center [monograph on the Internet]. http://www.dtic.mil/dtic/tr/fulltext/u2/a084551.pdf (accessed February 9, 2018).
Hall, B. L., B. H. Hamilton, K. Richards, K. Y. Bilimoria, M. E. Cohen, and C. Y. Ko. 2009. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: An evaluation of all participating hospitals. Annals of Surgery 250(3):363–376.
Hamstra, S. J., L. Edgar, K. Yamazaki, and E. S. Holmboe. 2017. Milestones annual report. Accreditation Council for Graduate Medical Education. http://www.acgme.org/Portals/0/PDFs/Milestones/MilestonesAnnualReport2017.pdf?ver=2017-10-26-092443-267 (accessed December 21, 2017).
Hawkins, R. E., R. S. Lipner, H. P. Ham, R. Wagner, and E. S. Holmboe. 2013. American Board of Medical Specialties Maintenance of Certification: Theory and evidence regarding the current framework. Journal of Continuing Education in the Health Professions 33(S1):S7–S19.
Hoffman, R. L., B. Bryant, S. R. Allen, M. K. Lee, C. B. Aarons, and R. R. Kelz. 2016. Using community outreach to explore health-related beliefs and improve surgeon–patient engagement. Journal of Surgical Research 206(2):411–417.
IHS Markit. 2017. The complexities of physician supply and demand: Projections from 2015 to 2030. Association of American Medical Colleges Report. Last modified February 28, 2017. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565-14ec-48fb-974b-99fafaeecb00/aamc_projections_update_2017.pdf (accessed March 8, 2018).
IOM (Institute of Medicine). 2014. Graduate medical education that meets the nation’s health needs. Washington, DC: The National Academies Press.
IOM. 2015. Measuring the impact of interprofessional education on collaborative practice and patient outcomes. Washington, DC: The National Academies Press.
Jena, A. B., L. Schoemaker, and J. Bhattacharya. 2014. Exposing physicians to reduced residency work hours did not adversely affect patient outcomes after residency. Health Affairs 33(10):1832–1840.
Konetzka, R. T., D. Polsky, and R. M. Werner. 2013. Shipping out instead of shaping up: Re-hospitalization from nursing homes as an unintended effect of public reporting. Journal of Health Economics 32:341–352.
Krumholz, H. M., K. Wang, Z. Lin, K. Dharmarajan, L. I. Horwitz, J. S. Ross, E. E. Drye, S. M. Bernheim, and S. T. Normand. 2017. Hospital-readmission risk—isolating hospital effects from patient effects. New England Journal of Medicine 377:1055–1064.
Lipner, R. S., B. J. Hess, and R. L. Phillips. 2013. Specialty board certification in the United States: Issues and evidence. Journal of Continuing Education in the Health Professions 33(Suppl 1):S20–S35.
Mata, D. A., M. A. Ramos, N. Bansal, R. Khan, C. Guille, E. Di Angelantonio, and S. Sen. 2016. Prevalence of depression and depressive symptoms among resident physicians. JAMA 314(22):2373–2383.
Mullan, F., E. Salsberg, and K. Weider. 2015. Why a GME squeeze is unlikely. New England Journal of Medicine 373:2397–2399.
Narayana, S., A. Rajkomar, J. D. Harrison, V. Valencia, G. Dhaliwal, and S. R. Ranji. 2017. What happened to my patient? An educational intervention to facilitate postdischarge patient follo-up. Journal of Graduate Medical Education 9(5):627–633.
Neuman, M. D., M. R. Passarella, and R. M. Werner. 2016. The relationship between historical risk-adjusted 30-day mortality and subsequent hip fracture outcomes: Retrospective cohort study. Healthcare (Amsterdam, Netherlands) 4(3):192–199.
Patel, S., J. D. Harris, V. Valencia, M. Mourad, S. Ranji, and A. R. Rajkomar. 2016. The feedback bundle: A novel method of inpatient audit and feedback. Journal of Hospital Medicine 11(Suppl 1).
Patterson, D. G., R. Longenecker, D. Schmitz, I. M. Xierali, R. L. Phillips, S. M. Skillman, and M. P. Doescher. 2012. Rural Health Research Center. http://depts.washington.edu/uwrhrc/uploads/RTT_Grad_Outcomes_PB.pdf (accessed March 8, 2018).
Pearle, M. S. 2013. Message from the President. A Newsletter for Diplomates and Candidates from the American Board of Urology. ABU Report 1(21):1–15.
Phillips, R. L., M. S. Dodoo, S. Petterson, I. Xierali, A. Bazemore, B. Teevan, K. Bennett, C. Legagneur, J. Rudd, and J. Phillips. 2009. Specialty and geographic distribution of the physician workforce: What influences medical student & resident choices? Washington, DC: The Robert Graham Center. Policy Studies in Family Medicine and Primary Care.
Phillips, R. L., S. Petterson, and A. Bazemore. 2013. Do residents who train in safety net settings return for practice? Academic Medicine 88(12):1934–1940.
Phillips, R. L., S. M. Petterson, A. W. Bazemore, P. Wingrove, and J. C. Puffer. 2017. The effects of training institution practice costs, quality, and other characteristics on future practice. Annals of Family Medicine 15(2):140–148.
Pimentel, S. D., R. R. Kelz, J. H. Silber, and P. R. Rosenbaum. 2015. Large, sparse optimal matching with refined covariate balance in an observational study of the health outcomes produced by new surgeons. Journal of the American Statistical Association 110(510):515–527.
Pusic, M. V., K. Boutis, R. Hatala, and D. A. Cook. 2014. Learning curves in health professions education. Academic Medicine 90(8):1034–1042.
Rajkomar, A., S. R. Ranji, and B. Sharpe. 2017. Using the electronic health record to identify educational gaps for internal medicine interns. Journal of Graduate Medical Education 9(1):109–112.
Reeves, R. V. 2017. Dream hoarders: How the American upper middle class is leaving everyone else in the dust, why that is a problem, and what to do about it. Washington, DC: Brookings Institution Press.
Ryan, A. M., B. K. Nallamothu, and J. B. Dimick. 2012. Medicare’s public reporting initiative on hospital quality had modest or no impact on mortality from three key conditions. Health Affairs 31(3):585–592.
Sellers, M. M., B. A. Niknam, and R. Kelz. 2017. A framework for the assessment of graduate medical education. JAMA Surgery 152(8):715–716.
Sen, S., H. R. Kranzler, J. H. Krystal, H. Speller, G. Chan, J. Gelernter, and C. Guille. 2010. A prospective cohort study investigating factors associated with depression during medical internship. Archives of General Psychiatry 67(6):557–565.
Sharp, L. K., P. G. Bashook, M. S. Lipsky, S. D. Horowitz, and S. H. Miller. 2002. Specialty board certification and clinical outcomes: The missing link. Academic Medicine 77:534–542.
Singer, N. 2017. How big tech is going after your health care. The New York Times. https://www.nytimes.com/2017/12/26/technology/big-tech-health-care.html (accessed March 8, 2018).
Swing, S. R., M. S. Beeson, C. Carraccio, M. Coburn, W. Iobst, N. R. Selden, P. J. Stern, and K. Vydareny. 2013. Educational milestone development in the first 7 specialties to enter the next accreditation system. Journal of Graduate Medical Education 5(1):98–106.
Triola, M. M., M. V. Pusic. 2012. The Education Data Warehouse: A Transformative Tool for Health Education Research. Journal of Graduate Medical Education 4(1):113–115.
Tsugawa, Y., J. P. Newhouse, J. D. MacArthur, A. M. Zaslavsky, D. M. Blumenthal, A. B. Jena, and R. L. Newhouse. 2017. Physician age and outcomes in elderly patients in hospital in the U.S.: Observational study. BMJ 375:j1797.
Van Melle, E. 2016. Using a logic model to assist in the planning, implementation and evaluation of educational programs. Academic Medicine 91(10):1464.
Voigt, R., C. P. Nicholas, V. Prabhakaran, W. L. Hamilton, R. C. Hetey, C. M. Griffiths, D. Jurgens, D. Jurafsky, and J. L. Eberhardt. 2017. Language from police body camera footage shows racial disparities in officer respect. Proceedings of the National Academy of Sciences 114(25):6521–6526.
Weinstein, D. 2011. Ensuring an effective physician workforce for the United States. Recommendations for reforming graduate medical education to meet the needs of the public. The Second of Two Conferences—the Content and Format of GME. New York: The Josiah Macy Jr. Foundation.
Werner, R. M., and E. T. Bradlow. 2006. Relationship between Medicare’s Hospital Compare performance measures and mortality rates. JAMA 296:2694–2702.
Werner, R. M., D. A. Asch, and D. Polsky. 2005. Racial profiling: The unintended consequences of coronary artery bypass graft report cards. Circulation 111:1257–1263.
Werner, R. M., J. T. Kolstad, E. A. Stuart, and D. Polsky. 2011. The effect of pay-for-performance in hospitals: Lessons for quality improvement. Health Affairs 30(4):690–698.
Williams, D. R., and V. Purdie-Vaughns. 2016. Needed interventions to reduce racial/ethnic disparities in health. Journal of Health Politics, Policy & Law 41(4):627–651.
Zuckerman, R. B., S. H. Sheingold, E. J. Orav, J. Ruhter, and A. Epstein. 2016. Readmissions, observation, and the hospital readmissions reduction program. New England Journal of Medicine 374:1543–1551.




























































