Roger Crystal, chief executive officer of Opiant Pharmaceuticals, Inc., noted that the United States is somewhat unique in that opioids are the first line of analgesia in hospital-based and dental settings. Furthermore, he said that systems in the United States incentivize the broader use of opioids, adding that even if opioid prescriptions were halted, there would still be millions of opioid addicts who need better treatment. Moreover, while overdose levels from opioid painkillers appear to be tapering off, they are being replaced by even greater overdoses from synthetic opioids such as fentanyl, said Crystal. Fentanyl is not only much more potent than heroin,
it gets into the brain quickly and lasts longer, and is cheaper and easier to produce, he said. It is also easy to derivatize.
Opioid use disorder is a chronic relapsing brain disease that is expressed as compulsive behavior and that is accompanied by robust physical dependence, said Sharon Walsh. The diagnostic criteria for a substance use disorder, according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) (American Psychiatric Association, 2013), includes 11 behavioral characteristics with the level of severity based on the number of behaviors present (see Figure 5-1). Walsh noted that physical dependence is not required to meet the criteria for opioid use disorder, although distinguishing those who do or do not have physical dependence would be important for drug development studies.
Three treatments are currently available for treating opioid use disorder by targeting opioid receptors, said Walsh. Methadone was introduced in the 1970s, followed by oral naltrexone in 1984, sublingual buprenorphine (SUBOXONE®) in 2002, injectable naltrexone (VIVITROL®) in 2010, and most recently, buprenorphine implants (Probuphine®) in 2016. Methadone is a full agonist, buprenorphine a partial agonist, and naltrexone an antagonist of the opioid receptor, said Walsh. She noted that buprenorphine is on the World Health Organization’s list of essential medicines—highlighting the importance of treating this disorder, according to Walsh—and development of the buprenorphine implant was facilitated by a partnership between Titan and Braeburn Pharmaceuticals, with some support from the National Institute on Drug Abuse (NIDA).
None of these drugs are a panacea, said Walsh, because more than half of patients relapse within 6 to 11 months. But this is far better than the 100 percent relapse in the first month among people who try to stop the drug without treatment, said Walsh. Treatment with these drugs decreases opioid use, overdose deaths, criminal activity, and infectious disease transmission, while increasing social functioning, she said.
According to Walsh, the clinical studies that were required to gain approval of drugs to treat opioid use disorders indicate that the FDA is willing to think creatively about its expectations for different types of medication. For example, only one pivotal study was required to file a New Drug Application for Probuphine; and for two other long-acting injectable formulations of buprenorphine, sponsors used the 505(b)(2) pathway, which required them only to do bridging studies, a blockade study, and a Phase III efficacy and safety study. Both of these drugs were also granted priority review by the FDA.
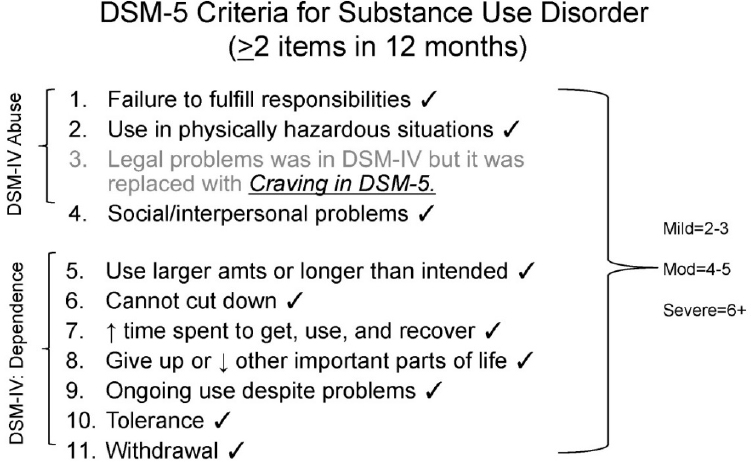
SOURCES: Presented by Sharon Walsh, October 11, 2017; APA, 2013.
Buprenorphine, a high-affinity μ-opioid receptor partial agonist, received FDA approval as a sublingual tablet, either alone or in combination with naloxone, for the treatment of opioid addiction in 2002.1 It works through several different mechanisms to suppress opioid withdrawal symptoms, reduce craving, and produce opioid blockade, said Walsh. Opioid blockade is a phenomenon whereby a drug blocks the response to an opioid such as hydromorphone. While several preclinical models exist, Walsh illustrated opioid blockade with data from a recent study she conducted with colleagues at the University of Kentucky’s Center on Drug and Alcohol Research. In this randomized clinical trial of CAM2038, a subcutaneous buprenorphine depot formulation, individuals were enrolled who were physically dependent on opioids and not seeking treatment for their disorder. In five 3-day sessions, participants were given one of three doses of hydromorphone and were asked to rate how much they liked it on
___________________
1 For more information, go to https://www.fda.gov/Drugs/DrugSafety/ucm191521.htm (accessed December 27, 2017).
a visual analog scale. Following the first test session, participants were randomized to receive different doses of CAM2038, along with the hydromorphone. As expected, there was a dose-related increase in liking for hydromorphone, but when they were dosed with the CAM2038, there was a complete and automatic suppression of this response (Walsh et al., 2017).
This outcome indicates that the drug may be able to prevent relapse, Walsh said. Nora Volkow noted that buprenorphine and naltrexone also have the effect of improving mood, possibly by blockade of kappa receptors, which could contribute to their therapeutic effect. However, Walsh said that what patients want is a drug that will treat the symptoms of withdrawal—they want to feel well, have their cravings go away, and they want to stop thinking about using drugs every day. For this to happen, other types of drugs are needed, she said.
NEW TREATMENTS IN DEVELOPMENT FOR OPIOID USE DISORDERS
Novel approaches to treating opioid use disorders are in development, said Walsh. One such drug is lofexidine, an α-adrenergic agonist, which is being developed for the treatment of withdrawal symptoms by a small company called World Meds, with substantial support from NIDA. In a recent Phase III trial of this medication conducted by Walsh and colleagues, lofexidine was shown to significantly suppress the symptoms of opioid withdrawal (compared with placebo) in patients who had opioid use disorder, were physically dependent, and were willing to undergo spontaneous withdrawal (Gorodetzky et al., 2017).
Walsh stressed, however, that detoxification alone is not an efficacious treatment for opioid use disorder and, in fact, is highly predictive of overdose and death. She cited a study from Sweden that compared patients who received a short 7-day taper off buprenorphine (the detoxification arm) to those who received buprenorphine for 1 year (Kakko et al., 2003). Both groups also received counseling and psychosocial services. After 60 days, no one in the detoxification arm remained in the study, and 4 of the 20 people randomized to that arm died. Similarly, people are entering very expensive 90-day residential treatment programs that prohibit medication, and 1 week after getting out they are overdosing and dying, said Walsh.
Nonetheless, she said there is an important application for drugs such as lofexidine because they can provide a bridge to manage symptoms for people transitioning from opioids or agonist therapies to antagonists like
naltrexone. They are also useful for people seeking a medication-free status so they can meet work requirements or enter a residential program, and for chronic pain patients who want to transition from opioid to non-opioid treatments or discontinue agonist treatment.
Long-acting formulations of buprenorphine are also in development. According to Christian Heidbreder, chief scientific officer of Indivior, Inc., these drugs are needed because with daily dosing of a drug such as buprenorphine, the plasma level of drug at the end of the dosing interval is subtherapeutic (Greenwald et al., 2007). If patients are not covered for the entire dosing interval, he said, there can be reemergence of opioid-like effects, craving, and withdrawals. In addition, there is a potential for diversion and misuse with oral medications such as these, he said.
Heidbreder described the clinical development of an alternative buprenorphine formulation (RBP-6000), which uses an extended release drug delivery platform that combines buprenorphine with a biodegradable polymer and a biocompatible solvent and is delivered once a month by subcutaneous (SC) injection with a prefilled syringe. A Phase II clinical study conducted by Heidbreder and colleagues showed that 12 weeks of treatment with RBP-6000 (300 mg) completely blocked the subjective drug-liking effects of a full opioid agonist such as hydromorphone (Nasser et al., 2016). Modeling and simulation based on positron emission tomography (PET) data suggested that 300 mg of RBP-6000 in subjects with opioid use disorder would translate into plasma concentrations of buprenorphine ≥ 2 ng/mL and 75 to 92 percent occupancy of the µ-opioid receptors in the brain.
This led to a Phase III 24-week multicenter trial in treatment-seeking patients who met the DSM-5 criteria for moderate or severe opioid use disorder, followed by an open-label safety extension study. Patients were first inducted with SUBOXONE® (buprenorphine/naloxone) sublingual film over a period of 7 to 14 days and then randomized to one of following dosing regimens: 6 once-monthly 300 mg doses, 2 once-monthly 300 mg doses followed by 4 once-monthly 100 mg doses, or 6 once-monthly SC injections of placebo. In addition to study medication, all subjects received manual-guided psychosocial support at least once a week. The Phase III study showed that the mean percentage abstinence was significantly higher in both RBP-6000 groups (approximately 40 percent) compared with placebo (5 percent). Exposure-response analyses confirmed a relationship between buprenorphine plasma concentrations, predicted brain µ-opioid receptor occupancy, abstinence, opioid craving, and withdrawal
signs and symptoms. In conclusion, treatment with RBP-6000 significantly reduced illicit opioid use compared to placebo with an acceptable safety and tolerability profile in adults with opioid use disorder, said Heidbreder.
Basic research is also needed to identify new targets for opioid use disorders that are not based on the μ-opioid receptor but that modulate endogenous opioids or that address neurocircuitry disruption by addiction, said Volkow. Other strategies, including the development of vaccines that target heroin, oxycodone, and fentanyl are also in development, said Walsh, noting that nearly all this work is supported by NIDA rather than industry. For example, researchers at the University of Minnesota have developed a vaccine to induce serum antibodies that bind to oxycodone and hydrocodone, preventing these drugs from getting into the brain, she said. In rodents, the vaccine has been shown to reduce the amount of oxycodone self-administration, suggesting that the vaccine may reduce opioid abuse (Pravetoni et al., 2014).
Special Considerations for Conducting Trials for Opioid Use Disorder Treatments
Enrolling participants in trials for opioid use disorder treatments can be challenging because of the unique characteristics of the intended population, said Walsh. Among the inclusion and exclusion criteria that will need to be carefully considered are poly-substance abuse, liver function, venous access, and co-morbid mental health disorders and infectious diseases such as hepatitis C and HIV, which are common in this population, she said. Other important considerations include the possibility of deception when using self-report measures; preparing for adverse events, including unplanned pregnancies, overdose, and seroconversion (time period in which HIV antibodies become detectable); and planning for adherence issues related to transportation, arrests, and other reasons for impairment. Walsh added that enrolling patients in grave danger of death because of their untreated opioid use disorder into studies of extended-release formulations (e.g., young people who endure long hospitalizations for conditions such as endocarditis or osteomyelitis) might improve the efficiency of studies while potentially reducing relapses and saving lives.
In addition, some trial design considerations include whether to use a placebo or active comparator as a control. Given that there are some partially effective treatments available, Walsh said she favors active comparator controls, although these require use of non-inferiority designs.
Selecting the appropriate outcome measures can also be challenging, and the FDA is thinking creatively about the expectations for different types of drugs, said Walsh. For example, urine drug toxicology levels may be appropriate for assessing whether abstinence is achieved or if a relapse has occurred, although there are no fixed criteria to determine this. Moreover, Walsh suggested that more attention should be paid to other measures such as improvement of quality of life and psychosocial factors such as maintaining employment and mending relationships with family members. She also noted that substance use disorder patients are recognized as a protected population under the Code of Federal Regulations (CFR Title 42: Part 2), which requires drug developers to take into account state laws regarding reporting and other issues related to confidentiality.
THERAPEUTIC DEVELOPMENT TO REVERSE OVERDOSE
Naloxone has been around for a long time to address the immediate emergency issue of treating opioid overdose, said Roger Crystal. It was originally approved as an injectable that required trained personnel to administer. An autoinjector was recently made available, but remains expensive and still involved needles; therefore, less suitable for lay bystanders. The concept of the nasal spray began when some first-responder and harm-reduction groups began using improvised nasal kits. These were not FDA approved, the absorption of naloxone was poor (Dowling et al., 2008), and they required an eight-step process to prepare them for use. What was needed, said Crystal, was a product that could be easily delivered by a lay bystander with sufficient efficacy to deliver naloxone into the brain quickly to prevent hypoxia.
Recognizing the urgent need to develop a product that could be easily and quickly delivered by anyone to people in the midst of an overdose, Opiant partnered with NIDA to develop a nasal spray formulation that would deliver a high dose of naloxone in a small volume quickly and easily. Opiant had previously developed a nasal spray formulation of naloxone to treat binge eating disorder, said Crystal. The data from the pilot study conducted in collaboration with NIDA showed that both 2 mg and 4 mg intranasal doses were rapidly absorbed and produced higher blood levels compared to the standard 0.4 mg intramuscular dose (Krieter et al., 2016). The product, NARCAN® nasal spray, was licensed to Adapt Pharma in December 2014 and received FDA approval in November 2015, and was on the market by the first quarter of 2016. Crystal noted that the
device can be used in all directions and does not need priming, easing delivery even in a crisis situation.
This page intentionally left blank.










