5
Research Directions, Policy Initiatives, and Potential Ways Forward
This chapter features presentations on research directions, policy initiatives, and potential ways forward in addressing the opioid epidemic and its infectious disease consequences. William Powderly, Dr. J. William Campbell Professor of Medicine and Larry J. Shapiro Director of the Institute for Public Health at Washington University in St. Louis, offered an overview of the Infectious Disease Society of America. Elisabeth (Els) Houtsmuller described the work of the Patient-Centered Outcomes Research Institute (PCORI), where she is associate director in the Healthcare Delivery and Disparities Research program. Anika Alvanzo, assistant professor of medicine at the Johns Hopkins University School of Medicine, presented some of the advocacy work done by the American Society of Addiction Medicine (ASAM).
RESEARCH DIRECTIONS AND POLICY INITIATIVES
Infectious Disease Society of America
William Powderly provided an overview of the Infectious Disease Society of America (IDSA), which currently represents more than 11,000 physicians, scientists, and other health care professionals who specialize in infectious diseases. IDSA’s purpose is to improve the health of individuals, communities, and society by promoting excellence in patient care, education, research, public health, and prevention relating to infectious diseases. Around 19 years ago, IDSA created the HIV Medicine Associa-
tion to represent the diversity of human immunodeficiency virus (HIV) health care providers and promote quality HIV care by advocating for policies that ensure a comprehensive and humane response to the AIDS pandemic.
For years, IDSA has partnered with the American Association for the Study of Liver Disease to maintain current hepatitis C virus (HCV) guidelines, which are updated on an ongoing basis.1 Guidelines on chronic pain management for HIV patients were published in October 2017. IDSA also advocates for federal funding for infectious disease and HIV prevention, care, treatment, and research and for other types of evidence-based prevention, including syringe services programs and safe consumption sites. IDSA also provides clinical updates on managing opioid-related infections at IDWeek. During its annual meeting several years ago, it became clear that opioid-related infections were a key concern of members, who were asked to list their top priorities. It revealed that infective endocarditis rates were doubling in many places and it was a major issue across the country. Other top priorities included issues related to skin infection, bone infection, and the transmissible viral infections, HCV and HIV. He noted that the response of members to the question of what they needed most were all around practice-related issues—that is, the need to focus on prevention related not to the infection per se, but prevention related to the cause of that infection. Survey respondents said they needed syringe exchanges, safe injection areas and education on safe injection practices, increased access to medication for addiction treatment (MAT) and integration of MAT into primary care and specialty care, and more supportive inpatient facilities to treat endocarditis and addiction.
Key Policy Issues
Powderly explained that IDSA created a working group on the intersection of infectious diseases and opioid use to develop its policy as a professional society. The working group identified five key policy issues:
- heightening prevention;
- increasing epidemiological data and enhancing surveillance;
- building health care provider capacity through telehealth and provider training;
- expanding access to HIV, HCV, and other infectious disease treatment and to addiction treatment; and
- researching and supporting models to co-treat addiction and infections.
___________________
1 The guidance is available at www.hcvguidelines.org (accessed April 14, 2018).
In terms of prevention, Powderly recommended investing new resources in the Centers for Disease Control and Prevention (CDC) to build state and local health department capacity to respond to their local opioid epidemics, as well as expanding access to syringe services programs and supporting jurisdictions implementing safe consumption sites. National HIV, hepatitis B virus (HBV), and HCV screening guidelines also need to be fully implemented. He pointed to the disconnection between developing guidelines, laws, and policies and then actually implementing them; the same holds true for existing technology that has not yet been fully implemented. Funding should be increased to expand surveillance for HCV and to generate and track national epidemiologic data (including morbidity and mortality) on infectious endocarditis and other infections associated with opioid use, he recommended. He warned that putting this into policy without resources to support it will just generate bad data that are done poorly, or not at all—yet another unfunded mandate will just cause problems.
Building health care provider capacity is critical, Powderly said. More than half of the hospitals in the United States do not have an infectious disease specialist, including 70 percent of hospitals in rural areas hardest hit by the epidemic. He suggested leveraging telehealth or other technologies to expand access to infectious disease and addiction treatment. Training is an important policy initiative, which could be supported by increased funding at the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Health Resources and Services Administration (HRSA) for addiction training for clinicians—including infectious disease specialists—on the frontlines of the opioid epidemic. Resources should also be provided for support of frontline clinicians prescribing MAT, such as case managers and onsite counselors. To provide physicians in the places where they are needed most, he suggested attracting addiction and infectious disease or HIV specialists to underserved areas by expanding loan forgiveness opportunities to create a market.
IDSA is advocating for expanded access to addiction treatment and for treatment of HIV, HCV, and other infectious diseases. In addition to building capacity on the provider side, patients should be able to access the therapies they need. Barriers to treatment include insufficient access to MAT nationwide and lack of integration with the delivery of other services. In countries that have integrated health care systems, addiction specialists and infectious disease specialists perform rounds together on patients with active infections and have an integrated treatment plan with patients referred immediately for methadone therapy. They receive the remainder of their infectious disease treatment in methadone clinics. Powderly said, “It is not rocket science. No new technologies, and it doesn’t require precision medicine investment. It just requires us to be sensible.” He pointed to
opportunities within existing programs around HIV that work well and are well resourced, such as fully leveraging HRSA’s Ryan White HIV/AIDS Program to improve access to prevention and treatment for people with HIV who also have opioid use disorder. He noted that the rate of substance use (both alcohol and drug) in the HIV population is significantly greater than the general population, for many reasons. Therefore, leveraging what is already in place—and that already works—would be relatively straightforward. Barriers to HCV treatment that must be addressed include coverage restrictions, such as requiring sobriety and limiting the types of providers who can prescribe HCV treatment.
Inpatient and outpatient clinics need to be better integrated, Powderly said, particularly for vulnerable populations of patients who are interacting with the criminal justice system. Better integration is also needed across the realms of addiction specialists, psychiatrists, primary care clinicians, surgeons, and infectious diseases physicians. He offered suggestions for addressing research gaps in service delivery, harm reduction, and treatment. In the context of implementation science, he called for more effective models for co-treating and integrating addiction and treatment for infectious diseases such as endocarditis. A practical issue in the treatment of staphylococcal endocarditis is that long-acting antibiotics have not been approved for anything other than skin or soft tissue infections; there is tremendous interest in their potential to treat patients with endocarditis out of the hospital in the context of integrated addiction treatment. Finally, he recommended that research should prioritize vulnerable populations who are disproportionately affected and face unique prevention and treatment challenges. This requires recognizing that significant poverty-related issues pervade the urban cores and also rural populations. Involving the infectious disease community in advocacy is important because “the language of epidemics is the language of infectious diseases,” he said.
Patient-Centered Outcomes Research Institute
Els Houtsmuller provided an overview of PCORI, an independent research institute authorized by Congress in 2010 and governed by a 21-member board of governors representing the entire health care community. PCORI funds comparative clinical effectiveness research (CER) that engages patients and other stakeholders throughout the research process. Funded studies are required to have two or more comparators (e.g., treatments, diagnostic tools, approaches). PCORI has a unique focus on engaging patients and other stakeholders in the research to seek answers to real-world questions—not purely academic questions—about what works best for patients based on their circumstances and concerns.
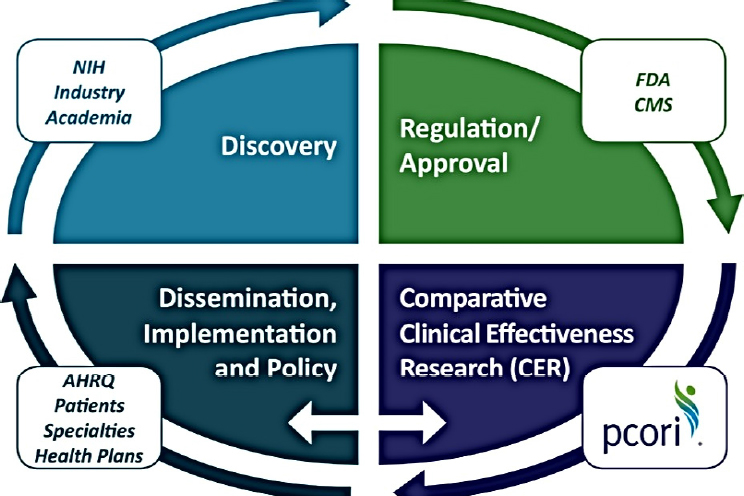
NOTE: AHRQ = Agency for Healthcare Research and Quality; CER = clinical effectiveness research; CMS = Centers for Medicare & Medicaid Services; FDA = Food and Drug Administration; NIH = National Institutes of Health; PCORI = Patient-Centered Outcomes Research Institute.
SOURCE: As presented by Elisabeth Houtsmuller at the workshop Integrating Infectious Disease Considerations with Response to the Opioid Epidemic on March 13, 2018.
Figure 5-1 illustrates how PCORI complements ongoing efforts. PCORI is not focused on discovery nor is it involved in any regulation or approval. It becomes involved after that process, working closely with institutes such as the Agency for Healthcare Research and Quality and CDC to disseminate results.
Houtsmuller explained that PCORI works somewhat differently than other institutions in that it funds research on which care options work, for whom, and under which circumstances. It focuses on answering questions that are most important to patients and those who care for them and aims to produce evidence that can be easily applied in real-world settings. Stakeholders are engaged throughout the research process, including patients and consumers, payors, clinicians, caregivers and family members, purchasers, policy makers, industry, hospitals and health systems, training institutions, and patient and caregiver advocacy organizations.
Pain and Opioid-Related Research
Houtsmuller reported that as of November 2017, PCORI had awarded $252 million to fund 65 CER studies related to aspects of noncancer pain, including opioid use, and had awarded $74 million to fund 13 CER studies related to opioid use through projects involving 105,000 patients. PCORI’s approach spans the entire care continuum. It has funded studies regarding the prevention of unsafe prescribing as well as nonopioid treatment options for pain. Studies on the latter have suggested that opioids are no more effective for either acute or chronic pain than just nonsteroidal anti-inflammatory drugs. It also funds studies in the management of long-term prescription opioid use, looking at patient-centered interventions for people who are on very high doses of opioids, such as dose reduction of opioids or switching from a full agonist to a partial agonist, like buprenorphine, which has a better safety profile. Other studies are funded to look at treatments for opioid use disorder. One study is looking at whether outcomes are improved through personalized MAT delivered in Federally Qualified Health Centers and complemented by a menu of services such as cognitive behavioral therapy and contingency management to increase treatment retention. To ensure that positive study outcomes are implemented, PCORI engages with relevant stakeholders, including payors, before the study even begins. A recent round of funding was announced to look at delivery of MAT specifically for pregnant women.
Houtsmuller provided more detail on studies PCORI has funded on HCV in the context of the opioid epidemic. The incidence of HCV in patients who have substance use disorders (SUDs) is higher than in patients who do not, she said, but access to treatment is especially challenging for this population. New medications are costly, and there are concerns about medication adherence and linkage to care for this population. Two PCORI-funded studies are looking at patient-centered models of HCV care. In the first study of people who inject drugs (PWID), one arm of the study was randomized to have a patient navigator meet with them to talk about their care, remind them to take their medications, and so forth. Because it is very difficult to meet somebody in person every day for medication, patients are given a phone with which they take a picture of themselves taking the medication that they then send to their patient navigator (i.e., teledelivery). In the other arm of the study, PWID receiving methadone take the medication through directly observed treatment and receive integrated care in the methadone clinic. The study will demonstrate which model works better for which patients. The second study is being carried out in New York at multiple sites to investigate another teledelivery approach. Among patients with HCV who come to a methadone clinic to receive MAT, half get referred to a specialist (usual care) and half get a teleconnection in the clinic to an HCV infectious disease specialist.
That study is both an access and an integration study, she noted, that will demonstrate what actually improves outcomes for which patients.
American Society of Addiction Medicine
Alvanzo described ASAM, which was founded in 1954, as the nation’s oldest and largest medical specialty organization representing more than 5,500 physicians and clinicians in the field of addiction medicine. Although primarily a physician-led organization, it also has associate memberships including licensed professionals in addiction care (including but not limited to licensed clinical psychologists, licensed clinical alcohol drug counselors, social workers, nurses, and pharmacists) to facilitate a multidisciplinary team-based approach.
A primary focus of ASAM is increasing access to treatment, said Alvanzo. Prior to the Patient Protection and Affordable Care Act (ACA), approximately 34 percent of enrollees in individual market plans did not have coverage that included addiction treatment services. Medicaid accounts for about one-fifth of all SUD treatment and about one-fourth of spending specifically on medications for treatment of opiate addiction. Medicaid expansion has also been associated with an 18.3 percent reduction in unmet need for SUD treatment. Given the attempted repeal of the ACA and reduction in Medicaid expansion, ASAM is continuing to advocate for continued expansion of the treatment and maintenance of coverage gains. ASAM is also working to ensure that whatever subsequent models are proposed would not allow states to waive the essential health benefits and thus does not support any efforts to move toward block grant funding.
Despite overwhelming evidence that supports the use of Food and Drug Administration–approved medications, said Alvanzo, there continue to be limitations placed on access to those medications, such as prior authorizations and fail-first policies. Therefore, ASAM is a proponent of removing any such policies that will limit people’s access to evidence-based medications for the treatment of opioid use disorders. The Mental Health Parity and Addiction Equity Act of 2008 continues to have gaps in enforcement, so ASAM is supporting local efforts to enforce the Parity Act and ensure that patients have equal access to addiction and mental health treatment, along with physical health treatment. In terms of products for support, ASAM has released National Practice Guidelines for the use of medications in the treatment of addiction involving opioid use.2 ASAM criteria is a research-validated set of guidelines that provide outcome-
___________________
2 For more information, see https://www.asam.org/resources/guidelines-and-consensusdocuments/npg (accessed May 30, 2018).
oriented and results-based care for the treatment of addiction, and ASAM has also developed CONTINUUM, a Web-based decision-support system that guides health care providers through a structured interview to help them with placement based on the ASAM criteria.3
Alvanzo said that ASAM is currently targeting workforce expansion such as including nurse practitioners and physician assistants. ASAM has been an advocate for Congressman Paul D. Tonko’s Addiction Treatment Act, which would codify in statute that addiction specialist physicians may prescribe buprenorphine up to the 275 patient limit and eliminate the sunset date. Coverage would be expanded by allowing nurse practitioners and physician assistants to prescribe buprenorphine, but with a sunset date attached that ASAM wants to eliminate for that prescribing authority. ASAM also supports this bill because it will expand prescribing authority to nurse anesthetists, clinical nurse specialists, and nurse midwives. The society is also in support of expanding the workforce by increasing the number of addiction medicine fellowships across the country, with ASAM working as a leader in the recent recognition of addiction medicine as a medical specialty (the first exam was administered by the American Board of Preventive Medicine in 2017). ASAM is also interested in developing a pathway for physicians who do not have a primary specialty board.
As part of its recent strategic planning process, said Alvanzo, ASAM has included the voices of the patient and the family in its programming and its advocacy efforts. “We realize that addiction is a family disease, so we need to get the voice of the family and the patient. We think that will go a long way to reducing stigma related to not only the disease of addiction, but to the treatment associated with it,” she said. Funding initiatives are urgently needed for both the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism, she added, whose research are critical to better understanding addiction and specifically the intersection between pain and addiction. To engage at the local level, ASAM has added a liaison in its national office who works directly with the state chapters on different policy issues. As president of the Maryland-DC chapter, she vouched that ASAM’s support in writing testimony and providing policy information has been hugely beneficial to local chapters.
ROUNDTABLE DISCUSSION
Benjamin Linas, associate professor of medicine at Boston University, commented that for certain patients, it seems appropriate to pre-
___________________
3 For more information, see https://www.asamcontinuum.org (accessed May 30, 2018).
scribe buprenorphine in infectious disease clinics; he asked if IDSA would consider incorporating that into infectious disease fellowship programs. Powderly said that it would be complicated because nationally accredited fellowship programs have both their core and optional components examined; training every infectious disease fellow in an area they are not likely to practice in would not make sense. However, there are opportunities to look at expanding skills and specifically ensuring that fellows who have particular interest in treating vulnerable patients with addiction, for example, can get those skills without having 2 extra years of training. IDSA is looking into dual boarding in both critical care medicine and infectious diseases, for example, with interest from fellows and trainees. IDSA is also addressing antimicrobial stewardship, an example of something that is core infectious disease business and now part of core specialty training. He added that an entire generation of providers came out of infectious disease fellowships before the advent of antimicrobial stewardship, so increasing capability needs to be provided for those interested who cannot take time off work or do a new fellowship. It is a matter of being creative and working with the partner specialty to find ways to train infectious disease physicians to be safe, appropriate providers focused on the interests of patients, but this should not create new bureaucracy.
Sandy Springer, associate professor at the Yale School of Medicine, asked if there are ways to help infectious disease and primary care doctors access training quickly to get their waivers if they are interested, as the 8-hour training session poses a barrier. Alvanzo could not speak to ASAM’s position on eliminating the 8-hour requirement, but there is no training required for opiate prescribing. In terms of pharmacology, buprenorphine is safer than full agonist opiates. ASAM is a leader in terms of training physicians who are looking to get waivers and offers a number of different opportunities for that training, including adding core sessions at their annual meetings. This addition for workforce development and expansion is 8 hours for physicians, but it is 24 hours for physician-extended colleagues such as nurse practitioners and physician assistants.
A workshop participant asked the panelists to highlight changes in action, policy, or procedures that would make a meaningful difference at this intersection of infectious diseases and the opioid crisis. The panelists responded as follows:
- Enact straightforward policy interventions to improve access, such as preventing gaps in care and addressing Medicaid restrictions. (Powderly)
- Create more training opportunities to increase the number of providers. (Powderly)
- Ensure that new technology such as telemedicine is financially reasonable, such as remove barriers to reimbursement. (Powderly)
- Address barriers administratively rather than legislatively to the degree possible. (Powderly)
- Conduct research on long-acting glycopeptides. (Powderly)
- Integrate care among HCV specialists, HIV specialists, and addiction specialists in settings where the patients already are. (Houtsmuller)
- Use every interaction with a health provider as an opportunity to get people engaged in treatment. (Houtsmuller)
- Start patients with opioid use disorder in emergency departments and hospitals on buprenorphine treatment, and link the patient to treatment in an active way, not simply via referral. (Houtsmuller)
- Remove barriers to effective evidence-based treatment by working with payors to eliminate prior authorizations for addiction treatment. (Alvanzo)
- Expand Medicare coverage to include addiction treatment for the aging population. (Alvanzo)
Springer suggested leveraging the HIV model of care to expand MAT and behavioral services. If MAT is conceived of as prevention of HIV, HCV, and overdoses, then other models of care could be used to help reach rural communities. The Conference on Retroviruses and Opportunistic Infections has good examples from resource-limited countries doing successful work in home-based HIV testing, he said, and the same could be done to expand MAT using community health care workers, especially in areas like West Virginia. Providers can learn from what has been done in other countries and bring those strategies to the United States. Todd Korthuis, program director for the Oregon Health & Science University’s Addiction Medicine Fellowship, agreed that many of the lessons learned in the HIV epidemic are directly translatable to the opioid epidemic, and mused that “the country is ripe for a Ryan White for opioid use disorder.” He noted that the research priority of the Office of AIDS Research focuses exclusively on viral suppression and transmission as outcomes for HIV research, and it misses the opportunity to better understand HIV as an infectious disease consequence of opioid use disorder—“It doesn’t help patients to have virologic suppression if they die of an opioid overdose. . . . Research outcomes should incorporate those as high-priority targets,” he said. He added that the Rural Opioid Initiative was recently funded as a collaborative project among CDC, the National Institutes of Health (NIH), and the Appalachian Regional Authority to increase
surveillance of HCV and other infectious consequences of opioid use disorder in rural American states.
PRESENTATIONS BY SESSION RAPPORTEURS
During the final session of the workshop, participants who had been designated as rapporteurs provided brief summaries of the presentations and discussions that took place over the preceding three sessions. The rapporteurs’ summaries were intended to stimulate discussion during the final question-and-answer session of the workshop. Jonathan Colasanti, assistant professor of medicine at Emory University’s School of Medicine and Rollins School of Public Health, served as the rapporteur for the first session, which explored the scope of the problem. Anika Alvanzo, assistant professor of medicine at the Johns Hopkins University School of Medicine, offered her reflections on the second session: opportunities for, and barriers to, treatment and prevention. The rapporteur for the third session—which focused on law, enforcement, and research and policy initiatives—was Ellen Eaton, assistant professor of medicine at the University of Alabama at Birmingham School of Medicine. A summary of selected points highlighted by each of the session rapporteurs is provided in Box 5-1.
POTENTIAL WAYS FORWARD
Carlos del Rio, Hubert Professor and chair of the Department of Global Health at the Rollins School of Public Health and professor of medicine at the Emory University School of Medicine, acknowledged that the epidemic is not going to be solved quickly, but he asked participants for their suggestions about potential integration points, policy issues that need to be immediately addressed, or other cross-cutting interventions that could have a short-term effect in mitigating the challenges ahead. A workshop participant suggested that in terms of implementation, SSPs and HCV surveillance are desperately needed yet woefully underfunded, so working with Congress to approve funding should be the top priority (e.g., additional Ryan White funding). CDC also needs additional funding, the participant added. The president’s budget included a $40 million program for CDC to address infectious diseases, opioid use, and injection drug use, said the participant, but it was at the $40 million expense from HIV funding. Interventions must span across disease groups. Any PWID tested for HIV should also be tested for HCV and other diseases. The infectious disease aspect of the opioid epidemic is being debated in Congress; SAMHSA should have an infectious disease component (not necessarily entirely new programs) and may be able to provide more money for local and state health departments and community-based organizations to work on this epidemic if things go well. The participant also noted that relevant funding is often contained in siloed funding streams, which impedes proposing programs that cut across diseases.
Sharon Morgan from the American Nurses Association commented that these conversations around the opioid epidemic among the national agencies reminded her of the steps that had to be taken to change seatbelt laws. The three-point seatbelt system was developed in 1955, but it only became a national agenda issue in the mid-1960s and in 2017, Wyoming became the last state to enact seatbelt regulations for children. It took 60 years to change the dialogue and similarly, it will take work to connect the dots to show the complexity of the issue to providers, so they can cohesively work to change the dialogue around the epidemic. She suggested starting that process by developing a template of potential points for intervention as a person passes through the system after visiting a provider.
del Rio noted that the intersections of poverty, lack of education, and lack of opportunity recurred during the workshop, highlighting the importance of considering social determinants of health and the structural interventions needed in communities to address the epidemic. Linas agreed that primary prevention, social determinants of health, and structural interventions are all crucially important in addressing the epidemic. But if the overdose curve is going to be bent now, it will require secondary
and tertiary prevention, more research, more funding, and more service provision. What will save someone tomorrow is treating people with opioid use disorder and having naloxone on site. Prevention work, prescription drug monitoring programs (PDMPs), and other work is crucial, he said, but the 5-year outcomes are going to be affected by secondary and tertiary prevention.
In the HIV model, people can access home-based HIV testing through which patients who are positive are immediately given antiretroviral therapy and patients who are negative are immediately given preexposure prophylaxis, remarked Springer. Opiate overdose is an obvious indication of an opiate use disorder, and patients need to be linked with opiate medication treatment, counseling services, and harm reduction services, so she asked if a similar model could be used for opiate addiction. del Rio contended that the entry point should be the patient coming in with an infectious complication clearly related to injection drug use—an overdose should not be the threshold for intervention. Springer agreed that in the hospital setting, people who come in with endocarditis or infections related to an opiate use disorder should be immediately screened for opiate use disorder and offered medical and behavioral treatment as needed.
del Rio remarked that in many hospitals, multiple best practices are due to Centers for Medicare & Medicaid Services (CMS) measures which are linked to outcomes; he suggested creating a CMS measure for hospitals around opiate use disorder, such as the percentage of patients with opiate use disorder linked to services. Springer suggested that preventing reinfection and rehospitalization could serve as a powerful incentive.
Nickolas Zaller, associate professor of public health and director of the University of Arkansas for Medical Sciences Office of Global Health, commended the Massachusetts model, but argued that there is no single compelling, rational, viable explanation as to why naloxone still requires a prescription, which is the single barrier limiting access. He also suggested that the debate on health care access and health care reform cannot be emphasized enough in an election year, and the counties experiencing the greatest proportion of death and destruction from these epidemics are supporting the very lawmakers who are dismantling the ACA. As these things are debated in their home states and communities, they should be applying significant pressure on our lawmakers to work seriously toward ending an epidemic. CDC and NIH grant funding are not sufficient; insurance companies must step up, take responsibility, and cover addiction treatment, and the only way to do that is to have mandated insurance coverage. Regarding naloxone access, del Rio mentioned that getting permission to stock naloxone in schools is another barrier because they may require that every prescription medication in the nurse’s office be linked to a student. He also highlighted the value of co-prescribing naloxone
with opioids, even at significant effort and cost. Linas noted that naloxone is available without a prescription in Massachusetts, per standing order.
Korthuis highlighted the opportunity for professional society recommendations regarding quality metrics. For example, ASAM has recently released quality-of-care recommendations for specialty addiction treatment centers linked to various metrics, SAMHSA has similar metrics, and there are metrics related to Ryan White funding to which HRSA’s HIV/AIDS Bureau encourages providers to adhere for HIV care. He suggested that IDSA, ASAM, and other organizations come together around policy measures recommending that everyone who is a willing person with opioid use disorder receives a dose of medication before they leave for treatment. Patients should be started with a referral to care and provided with naloxone rescue kits as they leave, he said. Tuberculosis testing should also be added while patients are hospitalized because it facilitates entry into methadone and residential treatment, which is often a barrier.
Powderly agreed that quality metrics are very important, but they need to be measurable and changeable. For example, if a measurement is the responsibility of an infectious disease doctor who has no ability to control the system that delivers it, then the doctor is penalized for the fault of the system. If quality metrics that CMS would enforce around hospitals are brought in, then hospitals must have the ability to measure that metric so there is a true opportunity to avoid a penalty. The process is complicated and lengthy, he added. If CMS wants to change any rule, it must go up for public review through a federal process. He emphasized that the desired outcome must be achievable, otherwise it creates bureaucracy and “noise for the sake of creating noise.” These discussions about fixes on the edges of a broken health care system, he said, make it easiest for hospitals in conservative, nonexpansion states to transfer complicated patients to other hospitals that can actually care for them. Rural hospitals are under a huge threat in this country, he added. If metrics are imposed without adding resources to follow those metrics, it will only increase the burden, resulting in more hospital closures and even less access to quality health care for people in rural America. It is only worthwhile to collect the data about meaningful metrics that can be acted on, he said.
del Rio remarked that metrics have impacted many providers, such as timed antibiotics in the emergency room following pneumonia. He suggested determining what represents a good outcome, for example, in terms of the percentage of patients who come to the emergency room with an overdose and leave the emergency room with medication-assisted therapy. Leaving with that prescription is so simple and would contribute to reducing the number of overdoses, although resources would be required. A participant noted that pregnant women with opioid use disorders face unique issues that need to be considered. For example, judges
have refused to let pregnant women off probation until they are in an abstinence-based program, despite the standard practice of providing MAT during pregnancy and starting detox from the day of delivery. There are issues for pregnant women that should be considered.
Veda Moore, Johns Hopkins Health Care community care coordinator, remarked that in Baltimore, the health department trains individuals on naloxone administration by going out into the community and providing naloxone supplies and education in areas where drugs are being sold and used. She reminded the group to consider the stigma faced by the lesbian, gay, bisexual, transgender, and questioning (LGBTQ) community, many of whom are shunned by their families and are forced to live on the street doing whatever they can to survive. They often are addicted to drugs and at risk of contracting HIV and HCV. She then read aloud a poem she had written as she listened to the workshop’s proceedings, titled “What Is This All About?” (see Box 5-2).
FINAL REMARKS
Corinna Dan of the Department of Health and Human Services (HHS) remarked that the Office of HIV/AIDS and Infectious Disease Policy (OHAIDP) and the Office on Women’s Health (OWH) asked the National Academies of Sciences, Engineering, and Medicine to develop this workshop on such a condensed schedule because of extreme concerns about the emerging trends related to the opioid epidemic. Every day and every week, increasing numbers of people are being exposed to preventable but potentially life-threatening infections.
She thanked the workshop’s organizers and participants and urged them to continue building new partnerships to support, enhance, and sustain these collective efforts to respond to the opioid epidemic. Jessica Tytel, HHS’s OWH, also offered thanks and praise to all participants for their efforts. She asked the group to continue to explore the specific effects of the opioid epidemic on women with respect to the differences in biology, physiology, social determinants of health, and lived experiences that affect every aspect of women’s physical and mental health, including their experiences with opioid use and the resulting infectious disease implications. She highlighted the need for more data on the specific effects of the opioid epidemic and infectious diseases on women, as well as the importance of providing programs and services that meet people where they are, including those that address women’s specific needs. This requires acknowledging the relationships between drug use, violence, and trauma and providing services to address those co-occurring realities of women’s lives, Tytel said.
Richard Wolitski, director of the HHS OHAIDP, concluded the workshop by reflecting on opportunities that exist to turn the tide of the opioid epidemic, which he called “the public health crisis of this generation,” in a collaborative way. Beyond calls for funding and establishing new programs, these opportunities should leverage existing available resources to transform the way systems work and make a huge difference in people’s lives. To illustrate, he described the Ryan White program, which has set the goal to cure all people who are co-infected with HCV in that program. They have used funding from the Minority AIDS Initiative Fund to build demonstration projects that show that how this might be achievable with existing resources. The program is actively planning how best to work toward that goal. The opportunity is at hand to disrupt systems and to fundamentally change them, he said. This will require close scrutiny of processes, implementation, and funding streams, as well as how policies, procedures, systems, and structures are organized in alignment with funding. He discussed the need to think about how issue-specific funding, programs, delivery of services, and accountability for implementation and
results change the way we approach people and the problems that affect their lives.
A minimum need is more braiding of funding at the local level, Wolitski said. Models already exist for doing this, he continued. This does require extra effort that reduces the funds available for direct services. Other opportunities may also exist to implement novel solutions such as braiding funding at the federal level so the local agencies receiving the funding will not bear the burden of counting separate funding streams. He indicated that there is a need to determine what options for providing flexibility are viable and what would be needed to realize the potential of these innovations and integrate funding provided to grantees. For example, CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention allows 5 percent of disease-specific funds to be used to address cross-cutting issues. These are the types of models that can shift the system toward putting the patient at the center of everything, regardless of what door the person enters.
Wolitski called on participants to step out of their own self-interests and think beyond their academic training and professional positions about how to generate the largest benefit. The opioid epidemic is a national crisis that can be a catalyst for innovation and more fully integrated delivery systems or we could remain focused on individual threats and fail to create the systems changes that are needed to be more efficient and effective in public health and medical care programs. History has shown that focus on the emergence of one problem, like crack cocaine, can turn things around. It has also shown, however, that when we focus narrowly on one issue and other related issues are not addressed, or we let up on our efforts once we have achieved some or all of the progress that was sought, we allow for other issues to emerge or reemerge that can be as bad or worse than the problem with which we started out.
There is an opportunity here to broaden the perspective about the constellation of SUDs, including and beyond opioids, Wolitski said. He concluded the workshop by recommending that the overall dynamics of SUDs should be addressed from a higher-level perspective, taking into account addictions and the systems that allow them to grow unchecked. “A whole-person approach and putting the person at the center are the keys to improving individual health, keeping families together, and building strong and healthy communities,” Wolitski concluded.


















