CHAPTER 4
HUMAN HEALTH CONSIDERATIONS
INTRODUCTION
Review of Human Health Considerations in Previous National Research Council Reports
Part of the committee’s task is to evaluate factors that could affect the decision about the use of dispersants in oil spill response. One of these many factors is the potential impact of dispersant use on human health. While much of the present report builds on the National Research Council’s (NRC’s) reports (NRC, 1989, 2005), we note that human health considerations were not a focus of these previous studies. The 1989 NRC report recognized the need to consider health hazards in oil spill response decision making, but it did not address the impacts of dispersants specifically. Similarly, one of the limited mentions of human health in the 2005 report identified human health as the first decision point in the dispersant use flowchart (NRC, 2005). In addition, both a mention of potential health effects from 2-butoxyethanol exposure during the Exxon Valdez oil spill response1 and a study assessing the potential for mammalian toxicity were reviewed in that previous report (NRC, 2005).
Overview of Human Health Considerations During and After Oil Spills
While the environmental consequences of marine oil spills has been an important topic of investigation since at least the Torrey Canyon and Santa Barbara oil spills in 1967 and 1969, respectively, research on the direct and indirect human health impacts of oil spills is relatively recent, whether dispersants were used or not, with some research conducted following the Exxon Valdez and Sea Empress oil spills but much more initiated after the Prestige oil spill in 2002 (Goldstein et al., 2011; Laffon et al., 2016; see Table 4.2 later in this chapter). Furthermore, human health
___________________
1 The 2005 NRC report contains a comment on page 56 indicating that health effects were found during a previous use of Corexit® 9527. Follow-up by the current committee with a previous committee member indicated that the concern referred to 2-butoxyethanol, a component of Inipol EAP22, a product that was used to promote biodegradation during the Exxon Valdez oil spill response. 2-butoxyethanol is also a component of Corexit® 9257.
considerations, which include physical, mental, and social well-being, with regard to dispersant use during oil spills only became a topic of epidemiological investigation during and following the Deepwater Horizon (DWH) oil spill (also referred to as the Macondo spill) in 2010 (Kwok et al., 2017a,b; McGowan et al., 2017; Rusiecki et al., 2017). As is emphasized frequently in this report, every oil spill is unique, and decisions about dispersant use that might impact human health will need to take local factors into account for any future spill.
The key questions addressed in this chapter are identified in Box 4.1. In the case of direct adverse effects to response workers, a critical component of the question is whether or not those direct effects can be mitigated through a proper worker health and safety program that focuses on worker training, personal protective equipment, and health and safety monitoring. The committee noted no evidence that the worker health and safety approach would differ for crude oil components whether or not dispersants were present.
With regard to exposure to crude oil, the components of particular concern are the carcinogenic constituents such as the polycyclic aromatic hydrocarbons (PAHs), which are known to cause human lung, bladder, and skin cancer. Additionally, benzene, a volatile component of fresh oil, is known to cause human hematological cancer and is a particular risk to workers who are nearby and may present some concern to downwind communities in close proximity to fresh oil.
A spill can also have an extensive effect in that the presence of surface sheen or of PAHs in seafood can result in prolonged closure of fisheries, which may contribute to secondary effects on community psychological and socioeconomic health and well-being. Worker health and safety is a primary concern during spill response in the United States, and community health, safety, and well-being have also received attention after more recent oil spills. If a response tool such as dispersants can shorten the intensity and duration of response activities, and if the proper worker health and safety and community health and safety measures can be implemented, it would be expected to lessen worker and community health risk. These issues must be examined and weighed as part of the response trade-off decision for dispersant use.
DIRECT HUMAN HEALTH CONSIDERATIONS
The environmental behavior and composition of the spilled oil will largely determine the primary exposure pathways and potential for toxicity in humans, as in other species (see Chapter 3). Primary oil constituents of concern for human health include volatile organic compounds (VOCs), benzene, toluene, ethylbenzene, and xylene (BTEX) in particular, and PAHs. The carcinogenicity of benzene and PAHs, particularly benzo(a)pyrene, are well characterized. In addition, exposure and toxicity of VOC and PAH oil constituents have been reviewed elsewhere (EPA, 1998, 2017; IARC, 2012a,b; Laffon et al., 2016). The use of dispersants may affect the pathways of exposure to oil and oil constituents relevant to human health via changes in the fate, transport, and biodegradation
of these oil constituents (see Chapter 2). Here we will focus on published research evaluating the effects of dispersants alone and how they may affect exposure or toxicity of oil constituents most relevant for human health. The committee first covers potential exposure pathways and evidence of exposure, followed by the toxicological evidence that provides information about the intrinsic hazard of a substance (whether, at any dose, the substance could cause an adverse effect) as well as epidemiological evidence from the DWH spill. Risk, a combination of hazard and exposure, is then discussed where sufficient evidence was available (e.g., see the section related to seafood below).
Exposure Pathways for Oil, Dispersant, and Dispersant Oil Mixtures
Dermal and Inhalation Pathways
During an oil spill response, primary response worker exposure pathways of concern are inhalational and dermal exposure to VOC components of oil, including benzene, and potential inhalational and dermal exposure to dispersants or dispersed oil. In addition, air transport of VOCs released from an oil spill can contribute to formation of secondary air pollutants, such as ozone (de Gouw et al., 2011), which could contribute to inhalational exposure to responder and nonresponder populations downwind of the oil spill. For future spills, downwind ozone formation might need to be taken into account during summer months, particularly in regions that are exceeding, or close to exceeding, the primary air quality standard for ozone. Results of modeling of subsea use of dispersants during the DWH spill response suggest a reduction in the VOC inhalational exposure pathway by enhancing the formation of small oil droplets and increasing the dissolution of VOCs within the water column, which also could potentially decrease downwind ozone formation (Gros et al., 2017; see Chapter 2). Aerosolization of oil-containing particles is another potential pathway to both inhalation and dermal exposures (Ehrenhauser et al., 2014; Middlebrook et al., 2012).
Dermal exposure to oil constituents has been shown to cause skin irritation and skin cancer (EPA, 2017), and transdermal absorption will also be an important route in chronic toxicity risk for oil components, particularly related to cancer risk estimates for benzene. Although it is conceivable that the surfactant properties of dispersants may increase transdermal absorption (Subedi et al., 2010), there is limited evidence to determine the effect of dispersants on the transdermal absorption of crude oil components. The likelihood of workers being exposed to a mixture of dispersants and crude oil may be unknown, but it is expected to be low because few responders are in the immediate vicinity when dispersants are applied to surface slicks, either by vessel or aircraft. For responders who could be in the area performing specific tasks, it is expected that appropriate personal protective equipment (PPE) will be used.
While not related to dispersant use, mechanical cleaning of oiled vessels and equipment may splash oil back onto workers; this could result in both inhalation and dermal exposures of oil components and cleaning agents used in the decontamination of oiled vessels or shorelines, particularly if PPE is not used properly.
Ingestion Pathways
Exposure via ingestion could occur through consumption of seafood that may have elevated PAH or dispersant components during or after an oil spill, although protocols for fisheries closures and reopening of waters to fisheries during and after an oil spill are designed to protect public health from this exposure route. These protocols have been in use since the 1989 Exxon Valdez oil spill (Yender et al., 2002) and are presented in more detail in the section regarding seafood below; however, how dispersants modulate exposures via this pathway versus the no dispersant alternative has not been systematically evaluated. Another possible route for ingestion of oil components is
through poor responder hygiene and possible contamination of food during a response, although this can be addressed by proper training. The use of dispersants could serve to reduce the presence of surface oil and obviate this possible exposure route.
Finally, ingestion by children of dispersed oil that reaches the shore may occur through their hand to mouth habits. Beach closures are designed to minimize this exposure route, although there may be residual oil after reopening. Dispersant exposure, however, is less likely because current policies in the United States restrict dispersant use to beyond 3 nautical miles from shore or in water column depths greater than 10 m. Few field measures exist, but concentrations of dioctyl sodium sulfosuccinate (DOSS) were low (non-detectable to 19 parts per billion [ppb]) in seawater samples taken at beaches during DWH, and spatiotemporal patterns suggested to authors a non-dispersant-related source of DOSS (Hayworth and Clement, 2012). Samples taken at depth during and following DWH (ranging from non-detectable [< 67 ng/L]) to 71 ng/L at 90 m depth to 13,000 ng/L at 1,180 m depth) as well as in weathered oil washed ashore 25-46 months following DWH were also low (~1-260 ng/g) (Place et al., 2016; White et al., 2014). Concentrations of nonionic surfactants in Corexit® dispersants, including sorbitan monooleate (Span 80), sorbitan monooleate polyethoxylate (Tween 80), and sorbitan trioleate polyethoxylate (Tween 85), were found infrequently and at low concentrations (840 to 9,100 ng/L) in seawater (Place et al., 2016).
Exposure Assessment and Guidelines
To date, exposure assessment during oil spills has been hampered by the lack of protocol development for dispersants and, to a lesser extent, for oil component concentrations at baseline and during response activities. Development and validation of an analytical chemistry protocol upfront for monitoring the levels of dispersant (i.e., dispersant components) and chemically dispersed oil in biota, including humans, could allow for monitoring of baseline conditions as well as levels during and post–oil spill, thereby providing a dataset for a more accurate exposure assessment to dispersants and dispersed oil. There would be value in expanding and improving protocols for measuring exposure during a response for oil spill workers (with potential dermal, ingestion, and inhalation exposure routes associated with dispersant application and oil spill response activities) as well as for residents in general (via dermal, ingestion, and inhalation exposure routes from beach activities and/or consumption of seafood). Previous reports have noted the need for emergency responder exposure monitoring and health surveillance (Decker et al., 2013; Reissman and Howard, 2008). The Centers for Disease Control and Prevention (CDC) developed a framework for worker monitoring and disaster research response (CDC, 2018).
A Good Practice Guide was developed to provide very specific, detailed recommendations for worker health and safety as they relate to surface dispersant operations. Protection measures detailed in the guide cover exposures related to breathing aerosol mist, ingestion, absorption through the skin, and splashes to the eyes (IPIECA-IOGP, 2012).
Evidence of Exposure to Crude Oil, Dispersant, and Dispersant Oil Mixtures
Evidence of Exposure to Crude Oil
The human health effects of crude oil are relatively well understood due to occupational health studies of drillers, including those heavily exposed during accidental discharge, in the petroleum refinery workforce, and in industries using crude oil and its components (e.g., EPA, 2017; Macys, 1992). In recent years, studies of workers involved in response after marine oil spills in the United States and elsewhere have reported, with reasonable consistency, respiratory and dermal effects
as well as other concerns (see Table 4.2). The committee notes that past studies of petrochemical industry workers have largely been of males, and they likely included fewer women of reproductive age than have been present among the population of oil spill response workers (Bingham et al., 1979). Relatively little information is available concerning other possible vulnerable populations.
Evidence of Exposure to Dispersants
In addition to understanding the impacts of dispersant use on exposure to oil, it is also important to consider whether and how direct exposure to dispersants has implications for human health. Workers involved in dispersant operations, or otherwise in the pathway of dispersant exposure, are presumably most at risk, although the use of appropriate PPE is expected to mitigate this risk (IPIECA-IOGP, 2012). PPE compliance is an important variable and was likely affected in the DWH response due to high ambient temperatures contributing to the discomfort of wearing PPE. While the institution of appropriate workplace protective measures can greatly minimize worker exposure, it is important to understand the potential health consequences of inadequate or inappropriate use of such measures, including unforeseen accidents that lead to human exposure.
Available information about the potential effects (or hazard) of direct dispersant exposure is derived primarily from standard toxicological studies of specific dispersants and of their individual components. Traditionally, one would also look for studies of workers involved in the manufacture of dispersants, but the committee could find no such information.
Two studies of DWH response workers have attempted to disentangle the direct effects of dispersants from other worker health risks. While both studies have noted adverse effects associated with self-reported dispersant exposures, both have significant problems in validating the accuracy of the workers’ identification of dispersant exposures (see below). During the DWH spill, personal breathing zone and area air samples were collected on a vessel during and following application of 50 gallons of Corexit® EC9500A. Aerial application of 125 gallons of Corexit® EC9500A co-occurred with the vessel application on the same slick. All substances monitored (including propylene glycol as the component monitored from the dispersant) had either non-detectable concentrations or concentrations well below occupational exposure limits (King and Gibbons, 2011).
Outside of direct exposure through handling or accidental release of dispersants by response workers, contact with the formulated dispersant (i.e., all the components in the ratio present in the product prior to application) is unlikely due to rapid dilution, dissolution, biodegradation, and photodegradation processes.
A more thorough discussion of the fate and transport of dispersants in the marine environment is presented in Chapter 2. The relevant aspects for human health are highlighted here. Dispersant formulations are mixtures of solvents and nonionic and anionic surfactants that have different properties and therefore potential fates in the environment. Once introduced to open ocean waters, dispersant mixtures will be quickly diluted (Lee et al., 2013a) and the various components subjected to degradation processes. Research examining the long-term fate of dispersant mixtures in the environment, however, indicates that DOSS is not always completely degraded. Studies have shown that DOSS persisted for up to 4 years following the DWH spill in oil-sand patties collected from beaches; however, the concentrations of DOSS observed have been extremely low (McDaniel et al., 2015; Perkins et al., 2017; White et al., 2014).
Evidence of Exposure to Chemically Dispersed Oil
In addition to potential direct exposure to dispersants, offshore response personnel working directly with or near dispersant application are the most likely group to be exposed to mixtures of dispersants and crude oil (chemically dispersed oil) via inhalation and dermal pathways, although
direct evidence of exposure is lacking. Broader community exposure is significantly less likely, although there may be rare and isolated instances that could lead to ingestion, inhalation, and dermal routes. Again, direct evidence of exposure to chemically dispersed oil is not available from previous oil spill investigations.
Hazard Related to Exposure to Oil, Dispersant, and Chemically Dispersed Oil
Risk is a function not just of exposure but of hazard as well. This section covers the hazard component of risk. Exposure is discussed above briefly and also is covered in subsequent sections. In considering the potential implications of using dispersants in an oil spill, the primary toxicological agents of concern are (1) the individual chemicals in oil and dispersant formulations; (2) the dispersant formulation as a mixture; (3) the mixture of dispersants and crude oil (referred to as chemically dispersed oil here and in Chapter 3); and (4) the weathered chemically dispersed oil.
Toxicological Evidence of Hazard
Crude Oil Toxicity
The potential for acute and subacute dermal toxicity and for the acute central nervous system effects of crude oil components, particularly BTEX, are discussed below. Chronic toxicity concerns of oil constituents are primarily driven by the carcinogenicity of benzene and PAHs via inhalation and ingestion exposure routes, respectively. While the BTEX components have similar acute central nervous system effects, it is only benzene that is a known human carcinogen, causing cancers of the hematological system such as leukemia and lymphoma (ATSDR, 2007; Bingham et al., 1979; Goldstein, 2010a; IARC, 2012a).
Weathered crude oil could account for a substantial part of the exposure of workers and the potential exposures of community members following a marine oil spill if it comes ashore near populations. Far less is known about the potential for human toxicity of weathered crude oil, although lower molecular weight components, including benzene, will be at lower concentrations; and, in the case of extremely weathered crude oils, no bioavailable components may remain. Examination of the effect of weathering on toxicity has been evaluated in other vertebrates relevant to ecological risk assessment (see Chapter 3) and may be relevant for predicting mammalian toxicity.
For comparison, the committee notes that burning of surface oil, another method used in oil spill response, produces pyrogenic PAHs or unsubstituted parent compounds, whereas PAHs found in crude oil are more likely to be alkylated. Jaligama et al. (2015) exposed mice to particulate matter from in situ surface burning of oil during the DWH response and showed induction of pulmonary inflammation. Whether the pyrogenic PAHs provide more or less risk than PAHs naturally present in crude oil is uncertain and warrants further study (Wickliffe et al., 2014; see also Chapter 3).
Dispersant Toxicity
Previous reviews describe the use of dispersant constituents in common household and pharmaceutical agents and summarize available toxicity information, identifying skin, eye, and respiratory tract irritation as the primary acute toxicity endpoints of concern (Dickey and Dickhoff, 2011; Fabisiak and Goldstein, 2011; Fiume et al., 2016; Popovech, 2017). These are similar to symptoms reported in workers and community members following significant oil spills irrespective of dispersant use (see epidemiological evidence section and Table 4.2).
After the DWH oil spill, the National Institute for Occupational Safety and Health (NIOSH) examined respiratory, cardiovascular, and neurotoxicity endpoints following exposure to Corexit®
EC9500A via inhalation and dermal exposure routes in mice and rats. Direct dermal or inhalation exposure may occur over brief periods in the field to workers who venture into spray areas before aerial or boat spray hit the water or to responders spraying dispersants from vessels, particularly if PPE is not worn correctly. Direct dermal exposure to Corexit® EC9500A, including the surfactant DOSS, resulted in allergic contact sensitization in the Organisation for Economic Co-operation and Development standardized Local Lymph Node Assay (EC3 = 0.4% and 3.9%, respectively) and Mouse Ear Swelling Test (Anderson et al., 2011). Acute inhalation exposure (27 mg/m3, 5 hour) resulted in transient increases in heart rate and blood pressure (Krajnak et al., 2011) as well as changes in biomarkers of neural dysfunction (Sriram et al., 2011); however, breathing rate, airway resistance, and lung inflammation were not altered in these rodent models (Roberts et al., 2011). Repeated inhalation exposures at similar concentrations resulted in no significant long-term changes in cardiovascular or respiratory endpoints (Roberts et al., 2014). George et al. (2001) found gut microbial differences in Fischer rats following a 5-week daily oral exposure to Corexit® 9527, Nigerian crude oil, and a Corexit® 9527 Nigerian crude oil mixture (daily dose volume equal to 0.1% of body weight, 1:20 dilution of crude oil or a 1:50 dilution of Corexit® 9527, or mixture, in peanut oil). No differences in body or organ weight were found across treatment and control groups, and mutagenicity tests were negative. This study was described in detail in the previous 2005 NRC report (NRC, 2005). Limitations of this study include small sample size and unclear relevance of the doses and oral gavage exposure route to expected worst-case doses and exposure routes for humans in field conditions during an oil spill response.
When subsea dispersant use was authorized during DWH, the U.S. Environmental Protection Agency (EPA) Computational Toxicology Program performed rapid toxicity screening to determine which dispersants were least toxic to mysid shrimp and silverside minnow as well as to human cell lines (Judson et al., 2010). For human cell line studies, the LC50 (the concentration that is lethal to half of the cells in culture) for Corexit® EC9500A (120 parts per million [ppm]) was lower than that for several other dispersants but higher than the LC50 determined for another dispersant formulation, Dispersit SPC 1000 (see Table 4.1). It should be noted that the concentrations reported in these studies (the HepG2 assay value of 100+ ppm) are at least one order of magnitude greater than expected field concentrations of dispersant alone (3-10 mg/L depending on application rates; see Chapter 3), and exposures in the field would be expected to be brief. Additional human cell-based studies have examined markers associated with human disease: for example, oxidative stress, mitochondrial dysfunction (Bandele et al., 2012), and chromosomal aberrations in sperm whale skin fibroblasts (Wise et al., 2014). Some dispersant formulations have been evaluated for endocrine-related endpoints: The dispersants Nokomis 3-F4 and ZI-400 had weak estrogenic activity (Judson et al., 2010), and DOSS activated adipocyte (fat cell) differentiation and gene expression in mice, suggesting potential obesogenic activity (Temkin et al., 2016).
During DWH, significant controversy resulted from a comparison of the U.S. Product Schedule dispersant being used to a dispersant approved for use outside the United States. EPA directed studies to compare dispersants. While some other dispersants had lower acute toxicity, they either contained endocrine disrupters or lacked effectiveness in spill response (Coelho et al., 2011a; Hemmer et al., 2011).
Note that dispersant effectiveness varies by formulation and oil composition. Additionally, comparison of dispersant toxicity metrics with those of cleaning agents used in the decontamination of vessels by oil spill response workers may be useful, because surface washing agents, like dispersants, contain surfactants and solvents. As an example, ecotoxicity of cleaning agents used in decontamination, such as PES-51 and Simple Green, has been evaluated by EPA (EPA, 2018). Screening tests in human cell lines, however, as described in Judson et al. (2010) and Table 4.1, were not found for these formulations.
TABLE 4.1 In Vitro LC50s (ppm) for a Variety of Dispersant Formulations and Mammalian Cell Types
| Reference | Cell Line | Exposure Time | Corexit® EC9500A | Corexit® EC9527A | Corexit® 9550 | ZI-400 | Dispersit SPC 1000 | Nokomis 3-F4 | Nokomis 3-AA | Sea Brat #4 | SAF-FRON GOLD | JD 2000 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bandele et al., 2012 | Hep2G | 72 hr | 275 | 250 | — | > 400 | — | — | — | — | — | — |
| Shi et al., 2013 | BEAS-2B | 24 hr | 200 | 100 | > 300 | — | — | — | — | — | — | — |
| Zheng et al., 2014 | Multiple w/FBS (w/out FBS) |
48 hr | 150 ≥ 200 (16-95) |
— | — | — | — | — | — | — | — | — |
| Judson et al., 2010 | HepG2 | 24 hr | 120 | — | — | 420 | 28 | 180 | 200 | 410 | — | > 1,000 |
| Judson et al., 2010 | HEK-298 (AR) | 5 hr | 410 | — | — | 670 | 170 | 370 | 200 | 560 | 1,400 | 3,200 |
| Wise et al., 2014 | Sperm whale skin cells | 24 hr | 350 | 700 | — | — | — | — | — | — | — | — |
NOTES: Corexit® 9550 is no longer on the NCP Product Schedule. Dashes reflect no data available. SOURCE: J. Fabisiak, presentation to the committee.
Chemically Dispersed Oil Toxicity
Limited toxicity studies have been conducted to examine chemically dispersed oil in human cells. These few studies found that cytotoxicity in human lung epithelial cells was greater and gene expression was differentially altered after exposure to chemically enhanced (either by Corexit® EC9500A or Corexit® EC9527) water-accommodated fraction (CEWAF) versus WAF mixtures using Macondo crude oil (Liu et al., 2016, 2017b; Major et al., 2012, 2016; Wang et al., 2012). While important to follow up, these cell culture experiments are difficult to interpret because (1) there is variation in the preparation of the WAFs; (2) the duration of exposures (up to 3 months) is long; (3) the concentrations of dissolved oil constituents were not measured; and (4) there are potential complexities arising from the effects of detergents in the dispersant preparations on cell permeability (Gerhard and Anello, 1969; Jamur and Oliver, 2010; Vinardell and Infante, 1999). Comparing dissolved concentrations of oil constituents is an important component to determining toxicity, as discussed in detail in Chapter 3.
During an oil spill, PAH degradation occurs, in part, through oxygenation at the seawater surface. The extent to which surface application of dispersants could affect the relative uptake into seafood and potential toxicity of oxygenated PAHs is unknown, although a recent study suggested that a relatively persistent PAH, chrysene, when oxygenated, may contribute to the developmental toxicity (heart, circulation, spine, and eye defects, among others, when exposure occurs during development) of weathered oil (Diamante et al., 2017). The net risk is unclear. Similarly, burning of hydrocarbons also leads to formation of benzene, but perhaps not at levels that would counteract the pyrolysis of benzene by the burning of the crude oil.
Epidemiological Evidence from Deepwater Horizon
Standard toxicological testing data were available for dispersant components prior to the DWH oil spill. These data, along with the general use of dispersant components in common household and pharmaceutical agents, gave some assurance that the use of a large volume of dispersants in response to DWH could be done safely. However, two studies published in 2017, based on epidemiological analysis of DWH, reported that oil spill response workers who self-reported possible exposure to dispersants had a higher level of symptoms as compared to those who self-reported they were not exposed to dispersants. Both of these studies are described below, and some of the methodological issues that complicate their interpretation are identified.
National Institute of Environmental Health Sciences Gulf Long-Term Follow-Up Study (GuLF) and the Deepwater Horizon Oil Spill Coast Guard Cohort Study
As part of an extensive health study of DWH response workers, investigators from the National Institute of Environmental Health Sciences (NIEHS) and collaborative programs attempted to specifically disentangle the impact of potential exposure to dispersants on the previously reported respiratory, dermal, and eye irritation symptoms (McGowan et al., 2017). Between March 2011 and March 2013, 32,608 individuals involved in the oil spill response completed a detailed telephone interview. Of those responses, between 25,659 and 29,648 were judged suitable for further evaluation of the respondents’ self-reports of dispersant and oil exposure and contained information about individual symptoms. Less than 10% of the participants claimed exposure to dispersants. Although each respondent was interviewed only once, the authors consider the study to be prospective in nature because the respondents were separately asked about symptoms associated with their oil spill response work and about symptoms within 30 days of the interview period. The adjusted prevalence ratio for all respiratory and eye symptoms was statistically significantly higher during both periods
for eye symptoms and for all respiratory symptoms except cough, which was not higher at the time of enrollment. Dermal irritation was reported to be statistically significantly higher for the time of the oil spill response and statistically significantly lower for the interview period. A follow-up study did not find a statistically significant association between lung function at 1 and 3 years after the spill and estimated total petroleum hydrocarbon exposure (Gam et al., 2018a,b).
A somewhat different approach was taken by investigators from the U.S. Coast Guard (USCG) and their colleagues in their cross-sectional evaluation of 4,855 USCG personnel involved in the DWH response (55.8% of total) (Alexander et al., 2018). Of the total responders, 22% were reported to be exposed to dispersant. Each USCG member involved in the oil spill response activity was asked to complete an exit survey, including exposure-related information and symptoms. Using a five-point Likert scale, respondents were asked to quantify how often they were exposed to crude oil/oily water or to dispersants. As in the NIEHS study, the response workforce had a statistically significant greater association for oil plus dispersants as compared with oil alone for the symptoms of coughing, shortness of breath, and wheezing. The USCG survey, though with fewer participants than the number in the NIEHS cohort, consisted of a more uniform group of presumably healthy and trained individuals who filled out a questionnaire in a more proximal time frame (June and November 2010) than did the NIEHS cohort. In addition, one might argue that they were more likely to be knowledgeable about their tasks and the possibility of dispersant exposure. However, valid concerns about recall bias remain as do potential problems related to the unexpectedly low response rate for a uniformed service.
Although the findings would seem to corroborate each other, both sets of investigators recognized that there were many potentially serious confounding issues that could affect their results. This led them to do sensitivity analyses which gave added credence to their findings. However, neither study was able to fully dispel significant concerns about recall bias nor the other problems described below.
Problems Interpreting DWH Dispersant Health Effects Studies
The major problem with these two studies is their limitations in the exposure assessment for dispersants. It was difficult to determine whether, how often, and how much a response worker was exposed to dispersant. Ideally, there would be direct information through biological markers of the extent of exposure, but this was not feasible. Using a questionnaire in which workers were asked to provide information about their exposure is a relatively standard approach, but it requires a reasonable degree of validation. NIEHS has appropriately worked to develop a job exposure matrix for the response workers involved in the GuLF study (Stewart et al., 2018). Unfortunately, they did not have sufficient quantitative information about dispersant exposures. In contrast with total hydrocarbons, for which they developed arithmetic means for the exposure groups and were able to assign ordinal values, for dispersants they depended solely on questionnaire responses (Stewart et al., 2018). The questionnaire used in McGowan et al. (2017) to estimate dispersant exposure of DWH response workers was further complicated by a number of factors.
- The complex response process. The inherent complexity of the response inevitably led to a confusing set of jobs for the individual worker, many of whom had no previous training. Supervisors were appropriately focused on getting the oil spill response job done quickly and safely, rather than specifically informing the workers as to whether they were potentially exposed to dispersants. Furthermore, there would be little or no difference in what was known about the safe approach to response activities for crude oil whether or not dispersants were present.
- Delays. Impediments to initiating a human study led the worker response to the questionnaire about dispersant exposure to be significantly delayed, particularly for the NIEHS cohort. This delay eliminated any possibility for the development or use of biological markers of dispersant exposure and complicated worker recall.
- Recall bias. Recall bias, sometimes called response bias, is inherent in studies of this nature (Coughlin, 1990). It reflects the very human propensity to say yes to questions about potential exposure when experiencing symptoms that are not explained by other exposures, particularly in situations where there is negative publicity about a potential for risk. Concern about recall bias has led many occupational health epidemiologists to avoid discussing potential exposures with those workers who have the adverse effect under study.
Other Studies Potentially Related to Dispersant Exposure
Data from the NIEHS GuLF worker study were also used in studies that further explored mental health indicators (Kwok et al., 2017a) and lung function (Gam et al., 2018a). As each of these studies was dependent for assessment of dispersant exposure on the same questionnaire used in the studies reporting symptoms, the concerns expressed above also apply. As discussed below, there is an opportunity for reanalysis if improved exposure information is forthcoming.
Among those who participated in the oil spill response there was a statistically significant increase in depression (prevalence ratio 1.22, 95% confidence interval [CI] 1.08-1.37) and posttraumatic stress disorder (PTSD) (prevalence ratio 1.35, 95% CI 1.07-1.71). However, no statistically significant increase was observed in the group labeled as “any self-reported work with dispersants” (depression prevalence ratio 1.04, 95% CI 0.92-1.19; PTSD prevalence ratio 1.15, 95% CI 0.91-1.45) (Kwok et al., 2017a).
Lung function was studied by spirometry during home visits occurring between May 2011 and May 2013. No differences were found between workers and nonworkers. Among response workers there were small but statistically significant reductions in lung function among those involved in decontamination or with high exposure to burning oil. In comparison to other workers, those who were believed likely to have had exposure to dispersants had modestly lower forced expiratory volume 1 (FEV1), forced vital capacity (FVC), and FEV1/FVC measurements. The subcohort that reported personally using dispersants (in contrast to being on a vessel that used dispersant) was reported to have a suggestive inverse association with FEV1/FVC (Beta –0.76%; 95% CI –1.33 to –0.18). But no difference in lung function measurements was found across tertiles of dispersant exposures (Gam et al., 2018a).
A series of studies by D’Andrea and Reddy (2013, 2018) claim longer-term effects on a variety of organ systems in workers exposed to crude oil and to dispersants as compared to a control group. Insufficient information is available to fully assess the implications of these studies as they do not conform to standard epidemiological methodology (Piacentino et al., 2014). Questions about these studies are also raised by internal inconsistencies in the hematologic findings in relation to the potential for the alleged benzene effects as well as by the reported presence of an increase in a benzene biomarker (urinary phenol) well past the time that this biomarker would persist in the body following the cessation of response work.
Next Steps for DWH Analyses and Considerations for Future Work
The information from studies of DWH response workers suggests the need for continued diligence in avoiding dispersant exposure during any future use. An impressive amount of exposure analysis has been performed, but there may be existing data sources that could help pinpoint who was exposed and under what conditions, thereby improving an understanding of the potential role of dispersants in producing the health effects reported in DWH responders.
Such continual evaluation, alone and together, of the USCG and NIEHS cohorts merits consideration, as it may help future decision makers determine whether to use dispersants. Furthermore, lessons learned from the methodological limitations of the DWH studies could be applied to future studies of dispersant use. Also, it appears that public health advice would be helpful to the On-Scene Coordinator. The Safety Officer position has historically been filled by someone who has occupational health and safety expertise, and this position remains a critical part of the response for worker health and safety. The Assistant Safety Officer for Public Health position is key to developing liaisons with local public health authorities in complex oil spills (USCG, 2014). However, the human health complexities in events such as the DWH oil spill go beyond the response workers and communities impacted by the event. Approaches such as a Spill Impact Mitigation Assessment are available to assess potential trade-offs associated with such a wide-ranging emergency response (see Chapter 6).
Additional information from the two existing studies associating self-reported exposure to dispersants with symptoms in response workers could be acquired through coordination and exchange of information among USCG and NIEHS scientists. As some workers appear to have been included in both studies, the two groups of investigators could assess the extent to which their findings for these workers corroborate each other. After-action reports related to dispersant usage, including releases, provide information useful to identifying workers potentially exposed to dispersants (Houma ICP Aerial Dispersant Group, 2010). Appropriately designed exposure-related studies require and may deserve significant research funding.
Workers involved in a large-scale crisis response effort start with the initial response group who have a certain level of experience in spill response and may have been screened for health-related requirements of the job. The remainder of the response pool are pulled from a general population who may have no previous experience in spill response work. They are provided with preemployment training, such as the Occupational Safety and Health Administration’s (OSHA’s) Hazardous Waste and Emergency Response standard or other just-in-time training and deployed to the scene of the event. Some of these workers may have preexisting health conditions that are not evident because there is no requirement for a preemployment physical or no baseline health data was collected or made available by the worker (NIEHS, 2012). In considering dispersant use, proper exposure assessment and toxicological evaluation would recognize that response workers may not be from a healthy worker population and may not know how to minimize exposure.
The two recently released DWH worker health studies have suggested that exposure to dispersants contributes to the symptoms of oil spill responders, particularly of the respiratory tract. If confirmed after more detailed exposure assessment, or in subsequent studies of response workers, it is important to determine whether longer-term consequences will follow, as has occurred, for example, in the 9/11 response group (Mauer et al., 2010). Relevant agencies, including the National Academies Gulf Research Program, could consider a request for applications aimed at understanding how a dispersant, as differentiated from crude oil components alone, might potentiate the effects of a pulmonary irritant or otherwise be responsible for the observed association.
The committee briefly considered possible biophysical mechanisms that might account for the seeming greater effect on respiratory symptoms of dispersant plus oil than oil alone, if in fact such occurs. These potential mechanisms ranged from a dispersant effect on airway protective systems, allowing greater penetration of irritants derived from oil, to an interactive effect with the salt-induced cough not uncommon in workers in coastal beach areas during summer. Research into understanding these mechanisms conceivably could have the benefit of identifying a characteristic of dispersants that is responsible for toxicity, if it occurs, but not of particular value for its desired dispersant effect, thus allowing the formulation of a less toxic dispersant.
Improving the exposure analysis for the NIEHS and USCG studies could be emphasized by both the NIEHS and USCG groups. This could include meeting together to understand the extent
to which individual workers may be enrolled in both studies and, if feasible, the extent to which the exposure estimates are replicable. Continued analysis of data sources allowing better location of workers in relation to sources—including better understanding of who was exposed and under what circumstances and duration—would be useful. Further clarification as to whether subcontractors responsible for dispersant applications are part of either study—and, perhaps, could be singled out as a high dose comparison group—could be a next step. In view of the uncertainties surrounding identification of workers exposed to dispersants by the NIEHS and USCG groups, consideration could be given to reevaluating the available information concerning dispersant usage in relation to the reports of these same workers’ symptoms available to those conducting the NIEHS and USCG epidemiological studies of dispersants.
Epidemiological Evidence from Studies of Other Previous Oil Spills
Previous Oil Spills (Exxon Valdez, MT Braer, Sea Empress, MT Erika, Prestige, MT Hebei Spirit)
Studies evaluating human health outcomes during and following previous oil spills have been reviewed (Aguilera et al., 2010; Goldstein et al., 2011; Gräbsch, 2016; Laffon et al., 2016). Here the committee provides a summary table of human health studies conducted following oil spills when dispersants were used versus when they were not.
In general, studies published on physiological effects have identified a broad spectrum of acute health symptoms (respiratory, dermal, eye and throat irritation, headache, nausea, vomiting/dizziness, and injuries and back pain) associated with exposure and/or response to oil spills (see Table 4.2). In addition, studies published following the Prestige accident also found increases in airway injury and in chromosomal damage in fishermen who participated in response activities versus fishermen who did not participate (Rodríguez-Trigo et al., 2010). Gräbsch (2016) presents a comparison of human health study findings following the Prestige and Hebei Spirit oil spills as two relatively well-studied oil spills, where chemical dispersants were applied (Hebei Spirit) versus not applied (Prestige). Direct exposure to dispersants was not evaluated. Frequency of acute symptoms—including eye (14% versus 20%), respiratory tract irritation (23% versus 39%), and headache (13% versus 36%)—self-reported by oil spill workers within the first 2 weeks after the spills were lower during the Prestige versus Hebei Spirit, respectively. Dispersant use was only one of many differences between these oil spills, and the type of oil and differences in the response population are also likely important explanatory factors for the differences in health symptoms experienced (Gräbsch, 2016).
In 2015, the German Federal Institute for Risk Assessment held a workshop to address the potential for dispersant use as an oil spill response in German waters. A publication derived from the workshop in its review of the evidence related to health effect concludes: “A reliable assessment of the overall impact of dispersant use on human exposure and potential health impairment is still needed,” which describes the goal of this chapter (Grote et al., 2018).
Seafood Exposure Considerations
Alteration in PAH Uptake in Fish, Crustaceans, and Bivalves
PAHs are a chemical class that contains known human carcinogens, and they are present in varying amounts in crude oil. The uptake of PAHs in fish and shellfish and subsequent ingestion is an important route of potential human exposure during and after an oil spill. Fisheries are generally closed if an oil sheen is detected at the surface, in part because navigation through this area may
TABLE 4.2 Studies Examining Human Health Outcomes During and After Oil Spillsa
| Oil Spill | Year | Amount (Kt) and Type of Oil Released | Amount (T) of Chemical Dispersant Used | Human Health Outcomes Evaluated | Methods | Findings | References |
|---|---|---|---|---|---|---|---|
| Oil spills in which chemical dispersants were used and human health outcomes were evaluated | |||||||
| Exxon Valdez | 1989 | 37, crude oil | Aerial application trials only took place over several days shortly after the spill and before the majority of response workers were on scene (Gilson, 2006) | Mental health | Cross-sectional and longitudinal, survey | Increased generalized anxiety disorder, depression, PTSD, heightened effect on Alaskan Natives and subsistence lifestyle | Arata et al. (2000); Gilson (2006); Palinkas et al. (1993a,b); Picou et al. (1992) |
| MV Braer | 1993 | 85, crude oil | 120 Although most of the dispersion that occurred was due to sea state and the type of oil | Lung function, VOC exposure, acute illness symptoms, liver and renal function | Cross-sectional, survey, spirometry, urinary biomarkers of exposure, blood liver and renal function, DNA damage in peripheral blood | Increased headache, sore throat, itchy eyes, no significant difference in lung, renal or liver function, toluene urinary metabolite heightened, no differences in DNA damage measures | Campbell et al. (1993, 1994); Cole et al. (1997) |
| Sea Empress | 1996 | 72, light crude oil | 445 | Acute illness and mental symptoms | Cross-sectional survey, retrospective cohort | Increased headache, sore throat, anxiety, depression | Gallacher et al. (2007); Lyons et al. (1999) |
| Nakhodka | 1997 | 6, heavy oil | Limited amounts sprayed by helicopter | VOC exposure, acute illness symptoms | Survey, personal air monitoring, urinary biomarkers | Increase in urinary marker for toluene exposure, headache, eye and throat irritation increased | Morita et al. (1999) |
| Tasman Spirit | 2003 | 35, light crude oil | 16 | Acute illness symptoms, lung function | Cross-sectional, spirometry, and survey | Lower lung function, increased ocular and respiratory symptoms | Janjua et al. (2006); Meo et al. (2008, 2009a,b) |
| Hebei Spirit | 2007 | 10, Middle Eastern crude oils | 298 | Acute illness symptoms, lung function, VOC and PAH exposure, oxidative stress biomarkers | Longitudinal, cross-sectional, survey, urinary biomarkers | Headache, eye and throat irritation increased, lung function decreased, some differences in urinary exposure biomarkers after spill response versus before, but no association with physical symptoms, oxidative stress biomarkers increased and correlated with PAH exposure biomarker 1 year after cessation of response efforts | Cheong et al. (2011); Ha et al. (2012); Jung et al. (2013); Lee et al. (2010); Noh et al. (2015) |
| Deepwater Horizon | 2010 | 500-750, LA sweet crude oil | ~4,050 surface ~2,900 subsea | Acute illness symptoms, VOC exposure | Longitudinal, survey | See above detailed summary | See summary above |
| Oil spills in which chemical dispersants were not used and human health outcomes were evaluated | |||||||
| Erika | 1999 | 20, heavy fuel oil | N/A | Acute illness symptoms | Cross-sectional survey | No control group | Schvoerer et al., 2000 |
| Prestige | 2002 | 63, heavy fuel oil | N/A | Acute illness and injury symptoms, lung function, biomarkers of airway injury, mental health, DNA damage in peripheral blood | Cross-sectional survey, cohort of response workers | Increased headache, sore throat, dizziness; elevated markers of airway injury at 2 years but not 6 years after response work; conflicting reports on mental health; increased micronuclei (indicator of DNA damage) in peripheral blood | Carrasco et al. (2007); Pérez-Cadahía et al. (2008a,b); Rodrigues-Trigo et al. (2010); Sbucedo et al. (2009, 2010); Suarez et al. (2005); Zock et al. (2012, 2014) |
a Table was developed based on compilation of information in similar tables found in CRRC Dispersant Initiative Final Report (CRRC et al., 2012), Goldstein et al. (2011), Gräbsch (2016), and Laffon et al. (2016),. Different sources may give somewhat different amounts of oil spilled or dispersants used.
result in contamination of fishing gear on vessels (nets, holding tanks, etc.). Reopening waters to fisheries typically requires seafood tissue analysis of PAH levels, ensuring that they do not exceed exposure limits based on cancer risk levels (NOAA/FDA, 2010; Yender et al., 2002). Cessation of fishery activities can have a significant effect on the overall economic, psychosocial, and health impacts of any major oil spill. The extent to which PAH concentrations in seafood can be altered by the use of a dispersant is central to any decision about its use or about comparing its use with other response methods.
Dispersant Constituents in Seafood
Because analytical strategies had not been developed, reports of dispersant constituents found in seafood were not compiled during and following oil spills prior to DWH. Due to public concern over the use of dispersants during the DWH response, the National Oceanic and Atmospheric Administration (NOAA) and the U.S. Food and Drug Administration (FDA) developed a protocol using LC MS/MS for determination of DOSS (CAS 577-11-7)—a component of Corexit® EC9500A, Corexit® EC9527A, and other commercially available products—in seafood samples (Flurer et al., 2010). FDA and NOAA finalized methods for detection of DOSS on October 27, 2010, approximately 6 months after the initial blowout. DOSS was chosen in part because it could be distinguished from oil-related compounds and because of its bioactivity, low volatility, and potential to persist in the environment compared to other dispersant components (Lubchenco et al., 2012; Ylitalo et al., 2012). DOSS is widely used in over-the-counter medications and other products to which humans are frequently exposed, suggesting that it is generally harmless at ingestion doses of up to 0.1 mg/kg body weight per day, which is based on weanling weight loss in reproductive toxicity studies conducted in rodent models (FAO/WHO, 1991, 1995). Petroleum-derived solvent components (e.g., petroleum distillates, CASRN 64742-47-8) of dispersants could also be considered in toxicity evaluations. A full component list of Corexit® EC9500A and EC9527A, the two dispersants used during the DWH response, can be found in Chapter 1.
Results from subsequent laboratory testing of a variety of commercially relevant species (Benner et al., 2010) and in field testing following DWH suggest minimal potential for bioaccumulation in seafood or exposure to DOSS via ingestion of seafood (Ylitalo et al., 2012). Of the > 8,000 seafood samples (including oysters, shrimp, crab, and finfish) that were submitted for chemical analysis by NOAA/FDA between June 2010 and March 2011, 393 were retrospectively tested for DOSS and 14 had detectable levels of DOSS which ranged from 0.011 to 0.41 µg/g (Dickey and Dickhoff, 2011). The concentrations detected were well below the derived level of concern (LOC) of 100-500 µg/g, which assumes a 70 kg person eating approximately 10-50 g of seafood per day for 5 years. Additional analyses of finfish and shrimp after reopening of waters to fisheries after DWH did not detect DOSS in seafood samples, and risk estimates, even for high consumers, were low (Fitzgerald and Gohlke, 2014; Sathiakumar et al., 2017; Wickliffe et al., 2014; Xia et al., 2012).
The additional step of developing methods for dispersant detection during an active emergency response resulted in a lack of baseline information and estimates of exposure during the spill; this could be avoided by moving this activity to the preplanning phases of oil spill response efforts. It is uncertain whether findings would be similar for other dispersant components or formulations or for an oil spill response that relies more or less on surface versus subsurface dispersant application, because detection would be dependent on potential differences in fate, transport, biodegradation, metabolism capabilities, and other factors.
Polycyclic Aromatic Hydrocarbons Concentrations in Seafood
Closure of federal waters to fisheries during and following an oil spill requires coordination between FDA, which is responsible for regulation of contamination or taint of seafood destined for interstate commerce, and the National Marine Fisheries Service of NOAA, which is responsible for regulation of fisheries commerce. Visible presence of surface sheen and oil trajectory modeling is used to make closure decisions. Direct toxicity of oil and dispersant to marine life is discussed in Chapter 3. Following a fisheries closure based on an environmental assessment (NMFS, 2010), agencies develop risk-based reopening criteria for species of concern and implement a seafood tissue sampling and analysis plan (Yender et al., 2002).
Protocols for reopening fisheries after closure from an oil spill have been based on cancer and noncancer human health risks associated with PAH concentrations in muscle tissue of a variety of seafood evaluated through sensory testing (Reilly and York, 2001) and chemical analysis via gas chromatography–mass spectrometry or liquid chromatography-fluorescence (Gratz et al., 2010; Sloan et al., 2004). More rapid analytical techniques are under development (Rusina et al., 2017). As described above, during the reopening of fisheries after DWH, an additional risk-based criterion for the dispersant component DOSS was developed.
Standard risk assessment calculations are completed to determine the acceptable concentration in seafood tissue and are referred to as the LOC. A variety of assumptions are made considering average and high-end consumption rates of each type of seafood, acceptable risk level for carcinogens, exposure duration, and age sensitivity (Dickey, 2012; Gohlke et al., 2011; Klasing and Brodberg, 2013; NOAA/FDA, 2010; Rotkin-Ellman et al., 2012). Calculated LOCs have varied considerably across oil spills primarily driven by differences in the choice of risk level and exposure duration (Gohlke et al., 2011).
The following 13 PAHs and their alkylated homologs have been considered in the risk evaluations during previous oil spills: naphthalene, fluorene, anthracene, phenanthrene, pyrene, fluoranthene, chrysene, benzo[b]fluoranthene, benzo[k]fluoranthene, benz[a]anthracene, indeno[1,2,3-cd]pyrene, dibenz[a,h]anthracene, and benzo[a]pyrene. Similar to the toxic unit dose metric described in Chapter 3 (Equation 2), the cancer LOCs are based on the summation of benzo[a]pyrene equivalents (BaPE) for 7 PAHs (chrysene [0.001], benzo[b]fluoranthene [0.1], benzo[k]fluoranthene [0.01], benz[a]anthracene [0.1], indeno[1,2,3-cd]pyrene [0.1], dibenz[a,h]anthracene [1], and benzo[a] pyrene [1]); the following equation is used to establish a LOC in seafood:
LOC (BaPE) = (RL × BW × AT × CF) ÷ (CSF × CR × ED),
where the risk level (RL) has been set at 1 × 10–6 or 1 × 10–5; body weight (BW) is 12 to 80 kg based on average child or adult body weight; averaging time (AT) has been set at 70 or 78 years based on average life expectancy; and the unit conversion factor (CF) = 1,000 µg/mg. The cancer slope factor (CSF) has been set at 1.7 or 7.3 mg/kg/day based on EPA’s BaP risk assessment for oral exposure (EPA, 1994) and are derived from dose-response data on gastrointestinal cancers in rodent models. The seafood consumption rate (CR) has been set at various levels for different oil spills. For example, for the DWH spill, 13 g/day for shrimp and crab, 12 g/day for oysters, and 49 g/day for finfish were used based on 90th percentile seafood consumers in the 2005-2006 National Health and Nutrition Examination Survey study. It is important to note that PAH exposure via consumption of seafood will also vary based on culinary practices and preparation methods (dos Santos Fogaca et al., 2018). The exposure duration (ED) has been previously set to 2, 5, 10, or 70 years, based on estimates of the retention period of PAH contamination in seafood.
These exposure duration estimates are conservative and generally based on retentions seen in those species that cannot readily metabolize PAHs, such as oysters, which have less efficient
metabolic capabilities for PAHs when compared to fish or crustaceans (Varanasi, 1989). As an example, the last reopening of Louisiana state waters in Barataria Basin after the DWH spill was in June 2015, more than 5 years after the blowout, due primarily to the entrainment in sediments and retention of PAHs in oysters (LDWF, 2015).2 The calculated LOCs for the DWH spill were 35 ng/g (ppb) BaPE for finfish, 132 ng/g (ppb) BaPE for shrimp/crab, and 143 ng/g (ppb) BaPE for oysters. In addition, one area off the Louisiana coast was reopened, then closed again to fishing for red royal shrimp, due to a shrimper reporting tarballs in his nets while trawling for this sediment dwelling species.
Determination of noncancer risks has been based on EPA reference dose calculations (RfD; an estimate of a daily exposure of each chemical that likely has no significant risk during a lifetime) for the six additional PAHs (naphthalene, fluorene, anthracene, phenanthrene, pyrene, and fluoranthene) using the following equation:
LOC = (RfD)(BW)(CF) ÷ CR.
Oral RfDs used are from EPA’s Integrated Risk Information System: 0.02 mg/kg/day naphthalene, 0.04 mg/kg/day fluorene, 0.30 mg/kg/day anthracene/phenanthrene, 0.03 mg/kg/day pyrene, and 0.04 mg/kg/day fluoranthene, and they are based on neurotoxicity and developmental toxicity. BW, CF, and CR are defined as above for the cancer risk assessment. The calculated LOCs ranged between 49.0 µg/g (pyrene in finfish) and 2,000 µg/g (anthracene/phenanthrene in oysters) for DWH. Because noncancer LOCs are much higher than those calculated for carcinogenic PAHs, LOCs derived from the carcinogenic PAHs typically drive the assessment.
Considerable uncertainty exists in RfDs, cancer classifications, CSFs, and equivalency factors, creating variation in risk-based criteria for fisheries reopenings seen across state and federal agencies and over time (Gohlke et al., 2011). For example, the calculated acceptable concentration of BaPE for finfish required for reopening following the Exxon Valdez oil spill were set a 0.5 ppb; whereas the LOCs set for finfish after more recent spills, including Cosco Buscan, Dubai Star, and DWH, were almost two orders of magnitude higher (35-44 ppb). Application of different acceptable risk levels (1 in 1 million versus 1 in 100,000 or 10,000) and different exposure durations (5 to 70 years) accounts for a large portion of the variation; however, differences in other parameters are also notable. For example, the California Environmental Protection Agency considers naphthalene and its alkylated homologues in their cancer risk determination. In addition, equivalency factors and CSFs have changed over time as the toxicological and epidemiological data are reassessed. Moving forward, as the body of evidence becomes more refined, risk-based criteria for fisheries reopenings should become more consistent in the evaluation of health risk associated with chemically dispersed oil and inclusion of seafood contamination risks into integrated models.
Additional Considerations in Comparing Toxicity Across Response Methods
The ultimate decision to use dispersants will be made by an agency different from the one with statutory responsibility for evaluating seafood safety and closure decisions. Therefore, close coordination would be useful to provide valuable information about consideration of the various factors.
If dispersants are used, the reopening protocol could be modified to include risk-based criteria for dispersant components, such as DOSS, in addition to PAHs. In addition, use of dispersants may affect the species of concern determined in the reopening protocol, because species in the water column may have increased exposure. The sampling and analysis plan may be altered to
___________________
2 See https://web.archive.org/web/20190801090052/http://www.wlf.louisiana.gov/news/39225.
reflect differences in the species of concern, potential for more rapid biodegradation, and increased complexity of the distribution of the dispersed oil. The estimated exposure duration may be altered by dispersant use and could be considered in the risk-based LOC calculations once further information is gathered. The waiting period that was used following the DWH was set at 30 days of no visible surface oil. A more effective reopening protocol may consider subsurface and sediment measurements in addition to tissue samples; for example, following the DWH spill there was a closure for red royal shrimp, then reopening, and then reclosure (NOAA, 2011).
Whether dispersant use alters the fate and transport of trace metals found in oil and, ultimately, concentrations found in seafood, is not well understood (Joung and Shiller, 2013; Liu et al., 2012; Steffy et al., 2016). Oil-related trace metal (vanadium, mercury, nickel) concentrations in oysters and sediment were found to be within historically observed ranges for most sites evaluated post-DWH as part of NOAA’s National Status and Trends Program (Apeti et al., 2013). Vanadium and nickel concentrations were elevated in sediment and oysters post–oil spill at some sites, and concentrations were below human health levels of concern. An analysis of whale tissue showed elevated chromium and nickel concentrations post-DWH (Wise et al., 2014). FDA surveillance of shrimp, crab, and oysters and an analysis of reef fish did not indicate elevated mercury, cadmium, lead, or arsenic tissue concentrations post-DWH (FDA, 2011; Fitzgerald and Gohlke, 2014).
Alteration in Benzene, Toluene, Ethylbenzene, and Xylene Exposure
Neurological and carcinogenic impacts from inhalation of VOCs are a primary consideration in establishing acute and chronic inhalation exposure guidelines to protect response workers. Volatile aromatic hydrocarbons, often considered together as BTEX, all have similar central nervous system anesthetic-like effects that are additive. Studies demonstrating more subtle effects on coordination—akin to mild alcohol intoxication (Benignus et al., 2011)—suggest that VOC exposures can affect coordination and judgment in ways that might increase the likelihood of injuries and accidents among response workers. Benzene is a known human carcinogen present in crude oil. It causes acute myelogenous leukemia and other hematological cancers (ATSDR, 2007; Goldstein, 2010a; IARC, 2012a). The NIOSH Immediately Dangerous to Life or Health (IDLH) value, usually based only on a 15-minute averaging time, is 500 ppm for both benzene and toluene, 800 ppm for ethyl benzene, and 900 ppm for xylenes. For example, at 300 ppm some decrease in central nervous system function that could impair safe decision making could be expected, particularly as BTEX blood levels would accumulate during the 1-hour period. Without effective PPE, it would not be particularly surprising if response workers were “woozy” after a few minutes of exposure. Contributing to the central nervous system effect would be aliphatics, which presumably would be a significant part of the VOC measurement: for instance, the IDLH for octane is 1,000 ppm and for pentane 1,500 ppm.
Based on carcinogenicity, the permissible occupational exposure limit for benzene is 1 ppm as an 8-hour time weighted average, with a maximum short-term exposure limit of 5 ppm for any 15-minute period (Substance Safety Data Sheet, Benzene, Standard Number 1910.1028 App A). The benzene standard also outlines under what conditions workers are required to wear and be trained in the use of PPE. As has been recognized by OSHA, their standards for other volatile aromatic hydrocarbons, including toluene, ethylbenzene, and xylene, are out of date, and they often exceed industry and state guidelines The NIOSH Recommended Exposure Levels (100 ppm), which are also published by OSHA, are those that are generally followed and are listed in the Annotated OSHA Z-2 Table along with the Cal/OSHA Permissible Exposure Limit (10 ppm) and the American Conference of Governmental Industrial Hygienists’ Threshold Limit Value (20 ppm) (OSHA, 2018).
In contrast to PAHs, BTEX chemicals are highly volatile, possess some solubility in seawater, and degrade relatively rapidly in the atmosphere—with the rate of degradation being dependent on temperature and on the presence of active species of oxygen generated in the atmosphere, through sunlight at the water surface, or through biological processes. Benzene is readily measurable in air or water.
Public concern about the potential for leukemia due to an oil spill can be anticipated to result in a focus on benzene measurements, as occurred following DWH, which leads to estimation of the extent to which a marine oil spill results in worker and community exposure to benzene. Using standard risk assessment techniques, benzene in air can readily be converted into lifetime risk estimates of leukemia for exposed workers or community members.
In the DWH response, one rationale for subsea dispersant injection (SSDI) at the crude oil release point and surface application at the wellhead was that they would increase dispersion and enhance dissolution of the more volatile portion of the crude within the water column, thereby reducing potential VOC exposure and fire hazards for response workers at the surface near the wellhead (USCG, 2011). Indeed, subsequent modeling suggests that SSDI may decrease overall VOC levels at the surface (Gros et al., 2017). Personal samplers worn by response workers during DWH response (from late May through July 2010) and analyzed for BTEX resulted in very few samples above detectable limits, and none approached the health limits (King and Gibbons, 2011; OSHA, 2018). These data suggest that response workers were not subjected to high-exposure conditions during SSDI; however, no published personal exposure data were available to the committee to assess exposure prior to initiation of SSDI in mid-May 2010 beyond what is mentioned above. The On Scene Coordinator Report also mentions recorded VOC levels above 200 ppm (USCG, 2011).
Field trial studies of surface application suggest that the dispersant Corexit® EC9500A and the surfactant Span 80 may increase aerosolization of less volatile oil constituents, such as PAHs, which would also need to be considered in evaluating exposure to response workers, although atmospheric concentrations at relevant distances away from dispersant application exclusion zones are expected to be low (Ehrenhauser et al., 2014; see Chapter 2, aerosolization section).
INDIRECT HUMAN HEALTH CONSIDERATIONS
The literature from various oil spills around the world, including DWH-related studies, consistently report adverse health effects among response workers and, more infrequently, have measured adverse health consequences in affected community members (see Table 4.2). Adverse community health effects often, but not always, have been associated with psychosocial and socioeconomic impacts on the community rather than toxicity associated with direct exposure to chemicals or crude oil. Communities at particular risk are those that already have relatively poor health and a past history of possible environmental injustice, which characterizes many members of the communities affected by the DWH oil spill (Hansel et al., 2017). These various health impacts in workers and community members are likely at least partly dependent on the duration of the oil spill recovery period. To the extent that dispersants fulfill expectations and shorten this duration, this presumably would lessen the overall impacts on worker and community health. A more detailed discussion of response worker injury risk from the DWH spill and duration of response activities is below.
As one reviews the extensive data collected during DWH, there is injury and illness information by time period, location, and type of injury, but there is no specific breakdown of the difference between injuries and illnesses associated with dispersant use versus without dispersant use (see Figure 4.1). Of the 2,129 total response worker injuries and illnesses recorded between April 23 and July 27, 2010, 32% were offshore. The most common injuries reported were sprains and
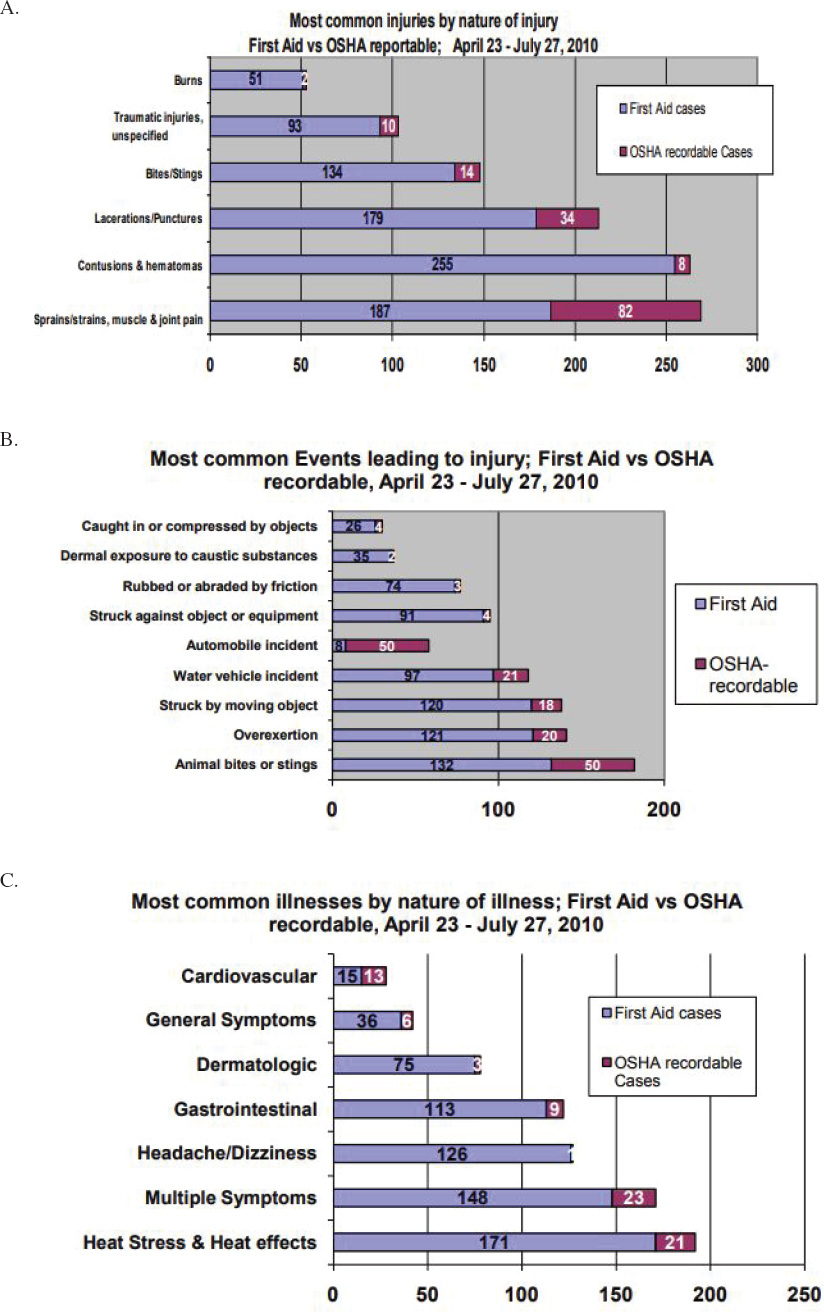
strains, contusions, and lacerations or punctures. The most common events leading to injury included animal bites and stings, whereas dermal exposure to caustic agents accounted for a small portion of reported events leading to injury (see Figure 4.1B). For illness reporting, dermatologic and headache/dizziness were commonly reported, with multiple symptoms and heat stress being the most common reported illnesses (see Figure 4.1C). While the data suggest that exposure to chemicals (e.g., from dispersants, oil, or other agents used in response work) may account for at least some of the reported injuries and illnesses (see Figures 4.1B and 4.1C), the lack of details in this dataset makes it challenging to draw any conclusions for comparing dispersant use as a response tool compared with other response tools, such as in situ burning or mechanical removal. Many response methods were employed simultaneously during the spill. There is also potential for exposure to many different chemicals during oil spill response, and specific chemical exposures are not identified in this dataset.
This lack of detail in responder health surveillance is not specific to oil spill response. The National Response Team Emergency Responder Health Monitoring and Surveillance Technical Assistant Document dated January 26, 2012, notes that even though lessons learned from previous emergency events continue to be applied, “there are still significant gaps and deficiencies in health monitoring and surveillance for emergency response workers.” The report further points out a need “for a coherent, comprehensive approach to protecting these groups of workers and for detailed, practical guidance on implementing such an approach.”
Oil spill response carries certain risk for workers, especially in the emergency response phase. Large and complex spills generally require a large number of people and, depending on the situation, may require long work hours. In a recent nationwide study, working in jobs that require overtime was associated with a 61% higher injury hazard rate relative to jobs that do not require overtime (Dembe et al., 2005).
If the use of dispersants might alter the response time and duration of the response, this risk-benefit analysis and possible change in injury hazard reduction rate can be part of the decision analysis. Duration of the hazard is a major determinant of risk. A question central to determining the impact of dispersant use on human health risk is whether and to what extent it shortens the response period and the return to normal. If use of dispersants shortens the number of days needed for response and/or number of workers needed for response, then theoretically this would result in less occupational injury risk (e.g., less likelihood of slips and falls in a tired group of response workers) associated with an oil spill response. In the case of DWH, the committee did not have sufficient information available to determine whether or not the use of dispersant altered the duration of the effects.
Weighing occupational health risks and benefits associated with use of dispersants during oil spill response should include an examination of the value of dispersant application subsea in improving the occupational safety of response workers working in the vicinity of the source control. Although the most appropriate goal for occupational health and safety is zero adverse events, it is not unreasonable to utilize comparative data on adverse health and safety events to help evaluate health and safety activities. During the DWH spill and response activities, the illnesses and injuries were coded and categorized using the Bureau of Labor Statistics Occupational Injury and Illness Classification System (NIOSH Illness and Injury Data3). However, more directly relevant record-keeping on worker health and safety related to the spill response itself, with the possibility of more direct evaluation of potential exposure to dispersant and dispersed oil, should serve as the baseline metric for evaluation of response for future oil spills.
Improving on the details of injury and illness reporting for worker health and safety would be useful for the next oil spill, including a clear focus on whether workers were exposed to disper-
___________________
3 See https://www.cdc.gov/niosh/topics/oilspillresponse/data.html.
sant. To that end, publication and ready availability of well-defined DWH worker health and safety statistics would be helpful.
Duration of Oil Spill Response Activities
Several previous studies have characterized significant economic, psychosocial, and mental health effects during and after oil spills in coastal communities (see Table 4.2). It is reasonable to expect that should there be a shortening of a spill response, then improvements in community resilience would be expected. The economy and community well-being would be improved with people getting back to their normal work and leisure routine, fisheries and related industries reopening, and tourism returning to its normal state. The positive impacts of more rapid response periods vary, and may include a shorter duration of direct economic impact, should fisheries closure times be shortened (NMFS, 2010). Other potential positive impacts may include the value of a restored natural environment and improved mental and behavioral health.
An effort could be made to compute the value of use of dispersants versus nonuse as it relates to the duration of the spill response. This should include the impact on the estimated time component of the risk of seafood PAH contamination. If the use of dispersants is shown to shorten the duration, then presumably this would lessen the impact on overall community health and well-being and provide a significant benefit from a Spill Impact Mitigation Assessment perspective (see Chapters 1 and 6).
Risk Communication and Transparency
Impact of Dispersant Information Availability
The importance of the transparent availability of information to the public has been increasingly emphasized in many U.S. and international environmental or public health documents, including EPA’s Mission Statement, the Rio Declaration on Environment and Development, the Aarhus Convention, and a recent review by the then head of CDC, Thomas Frieden, who in enumerating the public health actions of a responsive government, listed the first as “(p)romoting free and open information” (see Goldstein, 2016, for review). Major oil spills inherently are stressful to affected communities. Lack of transparency enhances the stress levels and psychosocial impact of any risk-related situation. As occurred during DWH, the choice of a dispersant that has a proprietary component contributes to this problem and also may limit the extent of toxicological information immediately available (Goldstein, 2010b). Lack of transparency also contributes to the “social amplification of risk,” a phenomenon highly dependent on how much trust is accorded by individuals and communities to the information source (Kasperson et al., 1988; Slovic, 1987). Secrecy, whether justified or not, unfailingly decreases trust and the willingness of the public to follow recommendations or to be involved in the stakeholder engagement processes, which are central to risk communication (Walker, 2016; Walker et al., 2015). Loss of trust also increases the amount of time that decision makers must devote to responding to public concerns. Accordingly, the presence or absence of undisclosed, and potentially proprietary components in a dispersant formulation could be considered among the determinants in choosing a dispersant in response to an oil spill. This could be extended to include the cleaning agents used in decontamination activities during a spill.
Wherever possible, full disclosure of a confidential business information agent could accompany initial use. If the authorities are not willing to strongly reassure the concerned public in the midst of a disaster such as the DWH oil spill that a secret ingredient in a dispersant is harmless, it would be best not to use that dispersant.
After the DWH oil spill, CDC disseminated a useful document aimed at local health professionals: “Gulf Oil Spill 2010: Deep Water Horizon Human Health Interim Clinical Guidance.” The CDC document did not provide health guidance on dispersants, however. In order to facilitate early dissemination of guidance to local health professionals after the next oil spill, CDC could update its guidance document to include appropriate information about dispersants in the near future.
Integrating Human Health Considerations into Modeling Efforts
Ultimately, each one of the direct and indirect dispersant-related scenarios described above must be considered in a comparative risk context. For example, mechanical (booming and skimming) and controlled burning of surface oil are among the other techniques available to decision makers for responding to an oil spill. A reasonable question is how each of these alternative methods compares with dispersant use in terms of the potential for human health effects. For example, burning of a complex hydrocarbon mixture such as crude oil could lead to greater inhalational exposure to PAHs and benzene for the worker population. As discussed in the toxicological evidence section, the PAHs produced by combustion are somewhat different in chemical structure and in component mixture than are those naturally present in crude oil and likely have different toxicological properties. Air emissions after in situ burning have been characterized (e.g., Gullett et al., 2016; Ross et al., 1996; Schaum et al., 2010); however, it is difficult to estimate occupational exposure from these studies. There are also direct risks of fire that can and should be fully containable but are not zero.
Chapters 6 and 7 discuss more fully the current efforts to make comparisons across oil spill control techniques using integrated models. The integration of human health effects into these models are just beginning, and some interesting initial findings are worth noting. Gros et al. (2017) modeled the ascent of DWH oil from the seafloor to the surface and validated their model by comparing hydrocarbon concentrations at various levels in the water column to observations during the DWH response. They found that SSDI reduced VOC atmospheric concentrations by 28% overall, with a benzene estimated reduction of 2,000 times. These results assume a dispersant injection of 0.4%, the average for the DWH time period (Spaulding et al., 2017). Had a 1% injection been used, subsequent calculations by Socolofsky and Gros (see Appendix E) and described in Chapter 7 suggest a greater reduction in benzene concentration at the surface. Crowley et al. (2018) also suggest that SSDI can substantially reduce VOCs at the surface. Using model simulations of a deepwater blowout under varying conditions (described in further detail in Chapter 7), they evaluate how SSDI affects the spatiotemporal pattern of VOC concentrations in the atmosphere above the blowout. Simulations suggest that SSDI reduces VOC concentrations within a 2 km radius of the release site. This reduction in VOC levels around the wellhead would conceivably lead to better access and hence quicker response as well as reduced exposures for well-control responders, because responders often move out of areas when measured levels are a health concern. However, current oil spill fate models do not explicitly model dispersant components and do not include aerosols, which could be an important exposure route for both occupational and community exposure scenarios (Afshar-Mohajer et al., 2019). In addition, integrated models that include risk estimates from ingestion of seafood would also be useful.
Until analysis of the impact of dispersant use focuses not just on the hazard component of risk but also on the spill duration and number of people involved in the response, computing the value of shortening the response period by using dispersants as compared to other response approaches is not possible. Future work could consider whether or not dispersant use results in a shortened duration and subsequent alteration in occupational injury and illness risk related to tasks performed as well as seafood safety closure periods, when dispersants are used versus when they are not used.
FINDINGS AND RECOMMENDATIONS
Finding: Epidemiological studies examining the association between dispersant exposure and health outcomes after the Deepwater Horizon (DWH) oil spill have reported respiratory and dermal effects in responders; however, drawing conclusive results from these studies is hindered by limitations inherent to the DWH response. In particular, the protracted initiation of the studies and the lack of a dispersant/dispersed oil biomarker necessitated reliance on self-reporting, making it difficult to accurately estimate exposures and hence effects of dispersant/dispersed oil versus oil alone in response workers and the general community.
Recommendation: Selection of biomarkers to improve human exposure assessment should consider the toxicity of dispersant and oil components and degradation products (produced by both biological and photodegradation), persistence in the environment, and bioaccumulation potentials. Biomarkers and analytical protocols should be established for each dispersant formulation listed on the U.S. Environmental Protection Agency’s National Contingency Plan Product Schedule.
Recommendation: In advance of the next significant oil spill, the reporting requirements for details of injury and illness reporting for worker health and safety should be improved, with a clear focus on whether workers were exposed to dispersant. To that end, publication and ready availability of well-defined DWH worker health and safety statistics is needed. Exposure assessment and toxicological evaluation should recognize that response workers may not be from a healthy worker population and may not know how to minimize exposure.
Recommendation: Consideration should be given for ongoing evaluation, alone and together, of the U.S. Coast Guard and the National Institute of Environmental Health Sciences cohorts, and lessons learned from the methodological limitations of the DWH studies should be applied to future studies of dispersant use. As some workers appear to have been included in both studies, the committee recommends that the two groups of investigators assess the extent to which their findings for these workers corroborate each other.
Recommendation: Approaches such as a Spill Impact Mitigation Assessment should be used to assess potential trade-offs associated with such a wide-ranging emergency response. If the use of dispersants might change the response time and duration of the response—and hence, person-hours worked—the potential impact on the injury hazard rate should be part of the risk-benefit decision analysis.
Finding: Tracking oil in the water column and sediment may be more informative for determining locations in which fisheries may be affected and for initiating fishery closures than observing oil at the surface. The protocol for reopening fisheries after DWH was criticized for not including testing for potential contamination from dispersants and for not accounting for the range of seafood consumption rates and meal preparation methods in local communities. There is inadequate information to determine whether dispersant use alters polycyclic aromatic hydrocarbon (PAH) uptake in fish or shellfish such that it would change the length of time before fisheries are reopened. Concentrations of dioctyl sodium sulfosuccinate (DOSS) measured in fish and shellfish tissue during and following DWH were low or nondetectable, suggesting negligible human health risk associated with dispersant exposure via ingestion of seafood.
Recommendation: During the pre-event planning phase, the National Response Team and Regional Response Teams should engage with the U.S. Food and Drug Administration, the National Oceanic and Atmospheric Administration, and state agencies with statutory authority for ensuring seafood safety to develop national, regional, and locally appropriate protocols that involve engagement of local communities for closing and reopening waters to fisheries. Such protocols should rely on direct measurement and projection of subsurface oil movement and potential for exposure (e.g., through integrated modeling). These protocols should also involve analytical methods to determine dispersant component concentrations within seafood. Furthermore, better understanding of whether dispersant use changes the length of time of fishery closures by altering PAH uptake could help in predicting its impact on community economic and psychosocial effects.
Finding: Large-scale oil spills result in mental and behavioral effects in community members. During the spill response following the DWH oil spill, the use of an unprecedented volume of chemical dispersant contributed to these effects. Furthermore, the publicity related to the lack of publicly available information on the chemical constituents of the dispersant formulations contributed to concerns.
Recommendation: Wherever possible, full disclosure of a confidential business information agent should accompany initial use. If the authorities are not willing to strongly reassure the concerned public in the midst of a disaster such as the DWH oil spill that a secret ingredient in a dispersant is harmless, it would be best not to use that dispersant. Furthermore, disclosure of real-time dispersant use information and up-to-date health risk information or guidance should be publicly available. Actively engaging public health authorities at the national and state levels early on to provide risk communications will improve transparency, and it may increase trust and understanding of health risks, assisting in mitigating the overall psychosocial impact of dispersant use during an oil spill.


























