5
The Cost Dimensions of Antimicrobial Resistance
Session I, part C, of the workshop explored the different dimensions of cost of antimicrobial resistance (AMR). The session was moderated by Keiji Fukuda, director and clinical professor at The University of Hong Kong School of Public Health. In his opening remarks, he stated that while the global community has recognized the severity of AMR, there has been inadequate action against the problem. To bolster effective action, he said, the costs of AMR as well as the costs of the interventions to counter it are critical to understand, as they are among the major factors that policy makers consider in their decision-making process.
The session began with a discussion on the direct and indirect costs of AMR by Mukesh Chawla, advisor for health, nutrition, and population at the World Bank. Mark Pearson, deputy director of employment, labor, and social affairs for the Organisation for Economic Co-operation and Development (OECD), followed with an evaluation of the cost-effectiveness of interventions to counter AMR. Ramanan Laxminarayan, director and senior fellow of the Center for Disease Dynamics, Economics & Policy, concluded the session with a presentation on reconceptualizing the issue of AMR to build the investment case.
CONSIDERATIONS FOR ESTIMATING THE COST OF ANTIMICROBIAL RESISTANCE: DIRECT VERSUS INDIRECT COSTS
Mukesh Chawla, advisor for health, nutrition, and population at the World Bank, discussed the methodologies and modeling results of the
World Bank’s efforts to assess the economic cost of AMR. He noted that his presentation draws on various studies, including two recent ones from the World Bank (Adeyi et al., 2017; Ahmed et al., 2017). Before delving into his presentation, Chawla cautioned that costing analyses are based on various assumptions, but they can be made robust by narrowing the variability of these inputs.
Direct and Indirect Costs of Antimicrobial Resistance
According to Chawla, AMR affects the economy through four channels that lead to either direct or indirect costs: increase in human mortality and morbidity, increase in livestock mortality and morbidity, and the “fear factor.” Direct costs of AMR include health care expenditures and resources used to treat the disease, such as hospitalization expenses and medications. Indirect costs of AMR are derived from present and future costs to society from the loss of outputs caused by a reduced labor supply and lower productivity attributable to increased morbidity and mortality. In addition, Chawla noted that the fear factor of infectious disease outbreaks could lead to border restrictions, which may increase trade and transport margins that cause a fall in exports. In sum, he highlighted that these types of channels of disruption need to be considered when calculating the economic impacts of AMR.
Chawla reviewed the methodology that the modeling team at the World Bank used to calculate the economic impacts of AMR (Ahmed et al., 2017). While the modeling team at the World Bank drew inspiration from a KPMG study that looked at the global economic impact of AMR (KPMG, 2014), the team employed different methods—namely using the GLOBE_DYN, which is a multisectoral, multicountry, and multiagent recursive dynamic computational general equilibrium model that uses the Global Trade Analysis Project.1 Through this modeling technique, a range of AMR incidence scenarios were compared to the base case scenario of a world without AMR, with marginal effects of AMR measured as the difference in the progression of economic variables (including gross domestic product [GDP], exports, and health care expenditures) between the scenarios. The analyses compared AMR severity across four income regions based on the current World Bank country classifications—low-income, lower middle-income, higher middle-income, and high-income (Adeyi et al., 2017; Ahmed et al., 2017). These AMR scenarios included possibilities of low case (5 percent resistance rate), middle case (current resistance rate until year 15 and then
___________________
1 Recursive dynamic computational general equilibrium models are solved sequentially and assume that behavior depends only on current and past states of the economy. For more information about GLOBAL_DYN, see McDonald et al., 2013.
40 percent onward), and high case (current resistance rate until year 15 and then 100 percent onward), drawing from a study conducted by the RAND Corporation (Taylor et al., 2014).
Economic Cost of Antimicrobial Resistance
Chawla highlighted some of the findings from the model simulations. In terms of direct costs of AMR, health care expenditures would increase in tandem with rising cases of AMR (see Figure 5-1). Results also show that additional health care expenses in 2050 would be $0.33 trillion in the low AMR scenario, while in the high AMR scenario they would amount to $1.2 trillion annually (Ahmed et al., 2017).
For indirect costs, Chawla stated that AMR makes a significant negative impact on GDP (see Figure 5-2). Compared to the base case, GDP
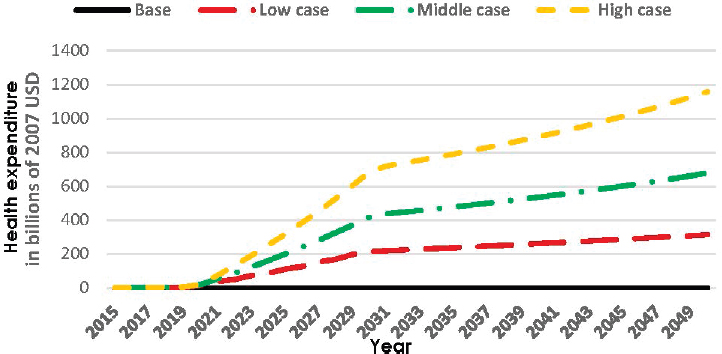
NOTES: USD = U.S. dollars. Health expenditure (in terms of an additional direct household tax) is represented on the y-axis and time is represented on the x-axis. Projected costs are for three scenarios of AMR: Low case assumes 5 percent resistance rate, middle case assumes current resistance rate until year 15 and then 40 percent onward, high case assumes current resistance rate until year 15 and then 100 percent onward.
SOURCES: Chawla presentation, June 12, 2018; Ahmed et al., 2017. Ahmed, Syud Amer; Baris, Enis; Go, Delfin S.; Lofgren, Hans; Osorio-Rodarte, Israel; and Thierfelder, Karen. 2017. Assessing the Global Economic and Poverty Effects of Antimicrobial Resistance. © World Bank. https://elibrary.worldbank.org/doi/abs/10.1596/1813-9450-8133 Creative Commons Attribution CC BY 3.0 IGO.
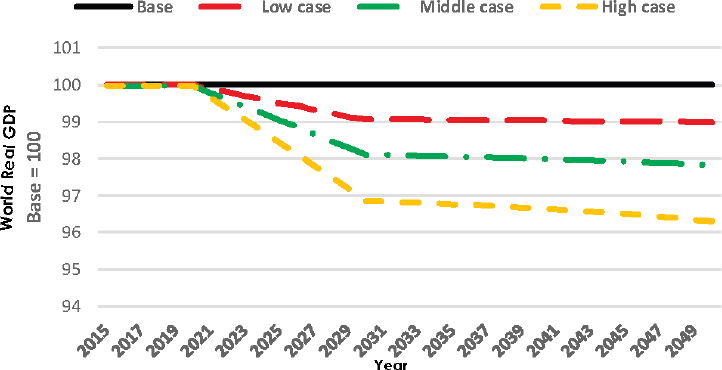
NOTES: GDP = gross domestic product. The global economic output is represented on the y-axis and time is represented on the x-axis. Projected declines are for three scenarios of AMR: Low case assumes 5 percent resistance rate, middle case assumes current resistance rate until year 15 and then 40 percent onward, high case assumes current resistance rate until year 15 and then 100 percent onward.
SOURCES: Chawla presentation, June 12, 2018; Ahmed et al., 2017. Ahmed, Syud Amer; Baris, Enis; Go, Delfin S.; Lofgren, Hans; Osorio-Rodarte, Israel; and Thierfelder, Karen. 2017. Assessing the Global Economic and Poverty Effects of Antimicrobial Resistance. © World Bank. https://elibrary.worldbank.org/doi/abs/10.1596/1813-9450-8133 Creative Commons Attribution CC BY 3.0 IGO.
would be 1.1 percent lower in 2050 under the low AMR scenario and 3.8 percent lower in 2050 under the high AMR scenario (Ahmed at al., 2017). He pointed out that the GDP decline stabilizes after people and economies adjust to the new circumstances as resources are reallocated with different patterns of new investments. Similar effects of decline are seen with regard to global exports and livestock exports.
After highlighting the individual direct and indirect costs, Chawla presented the cumulative economic cost of AMR. To calculate this, the modeling team derived the present values for the differences for GDP, exports, and extra health expenditures between the AMR scenarios and the base case at four social discount rates (see Table 5-1).2 At the intermediate dis-
___________________
2 A social discount rate is “typically used to derive a net present value as a summary measure of the effect of projects with streams of economic benefits and costs that are uneven over time” (Ahmed et al., 2017).
TABLE 5-1 Cumulative Costs of Antimicrobial Resistance (AMR) in Trillions (in 2007 U.S. dollars)
| Social Discount Rate | ||||
|---|---|---|---|---|
| Scenario | 0% | 1.4% | 3.5% | 5.5% |
| GDP | ||||
| Low case | –40.4 | –29.3 | –18.7 | –12.7 |
| Middle case | –74.5 | –53.7 | 34.0 | –22.7 |
| High case | –118.6 | 85.4 | –53.7 | –35.7 |
| Exports | ||||
| Low case | –10.8 | –7.8 | –5.0 | –3.4 |
| Middle case | –19.9 | –14.3 | –9.0 | –6.0 |
| High case | –31.7 | –22.8 | –14.3 | –9.5 |
| Household tax to finance extra health expenditure | ||||
| Low case | 8.0 | 5.8 | 3.8 | 2.6 |
| Middle case | 14.8 | 10.7 | 6.8 | 4.6 |
| High case | 23.6 | 17.14 | 10.8 | 7.2 |
NOTE: GDP = gross domestic product.
SOURCES: Chawla presentation, June 12, 2018; adapted from Ahmed et al., 2017. Ahmed, Syud Amer; Baris, Enis; Go, Delfin S.; Lofgren, Hans; Osorio-Rodarte, Israel; and Thierfelder, Karen. 2017. Assessing the Global Economic and Poverty Effects of Antimicrobial Resistance. © World Bank. https://elibrary.worldbank.org/doi/abs/10.1596/1813-9450-8133 Creative Commons Attribution CC BY 3.0 IGO.
count rate of 3.5 percent, the costs associated with the high AMR scenario amount to $53.7 trillion in lost GDP, $14.3 trillion in lost exports, and $10.8 trillion in additional health expenditures, amounting to a total loss of $80 to $90 trillion (Ahmed et al., 2017). Chawla pointed out that this figure is larger than previous costing studies by a factor of 20 and should motivate deliberate global action to minimize future global impact.
COST-EFFECTIVENESS OF INTERVENTIONS TO LIMIT THE SPREAD OF ANTIMICROBIAL RESISTANCE: A PERSPECTIVE FROM OECD
Mark Pearson, deputy director of employment, labor, and social affairs for OECD, discussed the cost-effectiveness of interventions aimed at countering AMR. He noted that his presentation focuses on human health and draws on data from the European Centre for Disease Prevention and Control and the World Bank. He first presented on the country-specific AMR
rates in OECD and Group of Twenty (G20) countries. He then described simulations estimating the cost-effectiveness of efforts to address AMR.
Antimicrobial Resistance in OECD and the G20
Pearson described projections of AMR by predicting country-level drug resistance rates in OECD and G20 countries through the year 2030 based on eight bacteria-antibacterial drug combinations. OECD used a machine learning approach to predict AMR by not applying the same rates of increase across all countries but rather forecasting partial correlates of drug resistance in human health, such as health spending and out-of-pocket expenses.3 These datasets were used to develop an ensemble model that includes linear mixed-effects regression, exponential smoothing, and random forest techniques. He noted that a drawback of the machine learning approach is that it enters numbers into a “black box,” making it impossible to determine why some countries are doing better than others. Despite this drawback, the model is capable of providing more reliable estimates compared to using a single technique, he said. While the patterns vary across countries, the model estimates that generally AMR will increase to approximately 25 percent between 2015 and 2030. Some countries, including Iceland, the Netherlands, and Norway, will see a more modest rise in AMR, and other countries, including Indonesia, the Russian Federation, and Turkey, will experience more severe outcomes. The relationship between antibiotic use and resistance is not one to one, he added.
Pearson also described the difference in resistance trends for first-, second-, and third-line treatments. Resistance to first-line antibiotic therapies in OECD countries is projected to decline, though resistance to second- and third-line therapies will rise. In G20 countries, including China, India, and Russia, resistance will likely rise for all first-, second-, and third-line therapies, he said. He cautioned that as third-line therapies are used more frequently, the resistance also increases more quickly for them than with any other lines of therapy for both OECD and G20 countries.
Cost-Effectiveness of Efforts to Address Antimicrobial Resistance in OECD and European Union Countries
Pearson described a cost-effectiveness analysis that used a dynamic microsimulation model to calculate the impact of AMR in OECD and
___________________
3 Machine learning approach is a method of data analysis that automates analytical model building, allowing computer systems the ability to learn from data, identify patterns, and make decisions, without explicit programming. Partial correlation measures the degree of association between two variables, while controlling or adjusting the effect of one or more additional variables.
European Union countries by 2050 depending on a series of transition probabilities of relevant diseases in a population that might become resistant to antibiotics.4 Then from a literature review, the researchers examined the factors that might affect those transition probabilities, and identified six policy approaches that could tackle inappropriate use of antimicrobials: (1) delayed prescriptions, (2) mass media campaigns, (3) enhanced environmental hygiene, (4) improved hand hygiene, (5) rapid diagnostic tests, and (6) antibiotic stewardship programs (OECD, 2017).
Pearson revealed that the selected AMR interventions were associated with significant reductions in deaths, particularly improved hand hygiene. He then compared the cost of implementing these interventions with their projected cost savings, focusing only on direct costs borne by hospitals. The hospital sector was specifically chosen, as it is motivated to take action to reduce resistance in order to reduce associated patient care costs. By highlighting the probabilistic estimates of the interventions’ likelihood of cost-effectiveness and savings, Pearson stated that mass media campaigns and delayed prescription programs are associated with low costs but also have low levels of associated savings; meanwhile hand hygiene was associated with low costs and high savings. Improved hand hygiene demonstrated a 95 percent likelihood of being cost saving. He added that nearly all the interventions described had a high probability of being not only cost-effective, but also cost saving within the hospital sector. Pearson concluded that the implementation of a combination of hospital-based AMR interventions could lead to savings of more than 2 million disability-adjusted life years by 2050.
RECONCEPTUALIZING ANTIMICROBIAL RESISTANCE TO BUILD THE INVESTMENT CASE
Ramanan Laxminarayan, director and senior fellow of the Center for Disease Dynamics, Economics & Policy, discussed building the investment case for controlling AMR. He addressed the distinctive aspects of AMR and how its understanding must be reshaped and enhanced in not only health, but also other sectors including livestock and the environment.
___________________
4 Dynamic microsimulation models are frequently used in health policy to predict or study the effects of intervention strategies over time, using microlevel data such as an individual’s development of a disease. Costs (e.g., health care expenditures) and outcomes (e.g., avoided deaths) are attached to each health status (e.g., healthy, sick, or dead) to estimate the cost and effectiveness expected for each intervention studied. Transition probabilities are calculations of health changes over time between health statuses.
Reconceptualizing the Impact of Antimicrobial Resistance on Human Health
Laxminarayan began by highlighting the unique nature of AMR. He said that the issue of AMR is often framed similarly to common diseases when, in fact, it is fundamentally different because it underlies both infectious and chronic diseases. Antibiotics are crucial to address both, as many infectious diseases are not vaccine preventable and antibiotics represent the only treatment option, and for many chronic diseases antibiotics are part of the treatment approaches needed to control these diseases. The medical community’s experience with antibiotics is relatively short—antibiotic treatment was only discovered in the early 20th century—and its experience with resistance to these drugs is even shorter. While concern for AMR has existed for decades, the recent increase in resistance from 1 percent to more than 40 percent occurred after the year 2000 (Review on Antimicrobial Resistance, 2014).
Another unique aspect he noted was that although antibiotic use patterns have contributed to present-day rates of AMR, antibiotics have also saved many lives and advanced the field of medical care. Laxminarayan stated that while the global community is focused on the costs of AMR today, the innumerable benefits of antibiotics to humans all over the world need to be recognized, as is the case with fossil fuel. He explained that oil has become increasingly depleted but not before allowing societies to build entire economies and roads on the back of oil—and that should be the approach to thinking about AMR. Moving forward, he added, the global community needs to think about how to get the best value out of antibiotics in the best possible way. Laxminarayan said this involves investing in the replenishment of the stock of effective antibiotics and conservation of existing ones through infection preventive measures (e.g., improved hand hygiene and vaccination) or prioritizing antibiotic use in certain conditions (e.g., restricting the use of antibiotics for acne treatment).
Laxminarayan also pointed out that the way to think about AMR’s consequences on human health needs to go beyond only focusing on the death tolls from drug-resistant pathogens. He highlighted that AMR deeply affects care-seeking behaviors. He described a scenario in which an elderly patient might forgo a hip replacement surgery because of the higher associated risk of a postoperative infection and has to live with a bad hip for several more years. He reiterated that behavioral adaptations in response to not having access to effective antibiotics or any antibiotics at all are likely to be significant, and he urged the audience to think about these often overlooked ramifications.
Antimicrobial Resistance Beyond the Health Sector
Laxminarayan argued for the need to focus on the effects of AMR beyond the health sector, especially as the majority of antibiotics are used on animals. China consumes more than half of the world’s antibiotics, and the majority of these medications are used for livestock (Zhang et al., 2015). While the use of these antibiotics has boosted the productivity of livestock and helped reduce the price of meat, Laxminarayan noted that protein production has negative environmental impacts related to air emissions, water, and climate.
He specifically argued that antibiotics have a direct impact on the environment when they affect the microbiome of public spaces. A study of the Ganges river, for example, suggested a twentyfold increase in circulating NDM-1 proteins—a marker of antibiotic-resistant organisms—during the annual pilgrimage season when there is mass bathing of 10 million people (Ahammad et al., 2014). He also noted the lack of appreciation for the consequences of dumping tons of antibiotics into concentrated ecosystems such as rivers in China, where there might be tens of thousand times more concentration of resistance genes than found in typical groundwater. He stated that the overall consequences of circulating antibiotics in the environment is poorly understood.
Laxminarayan concluded with his perspectives on investing in AMR mitigation efforts. He emphasized that current thinking around the benefits of new antibiotics is mainly focused on the health sector, but more analysis is needed to understand the effect of AMR on other sectors. He also noted that though funding for AMR response from the global community has risen over recent years, the majority of this funding goes toward antibiotic discovery. He urged that a higher proportion of these funds should be directed toward strategies related to diagnostics, vaccines, and conservation of existing effective antimicrobials.
DISCUSSION
Because a key theme of the workshop is how to influence policy and decision makers to invest in countering microbial threats, Fukuda asked the three speakers to share how they would like to see future funding targeted to reduce the threat of AMR.
- Pearson highlighted the need to focus on two issues: the livestock sector and discovery of new antimicrobials. He specifically argued the importance of identifying credible alternatives that will help reduce the massive use of antibiotics while not heavily disrupting the livestock sector. He shared experiences from Europe where
-
the production model has moved away from antibiotic use while maintaining competitiveness in the livestock sector, and believed that these experiences can be used to convince other countries like China and Brazil to follow a similar path. On his second point, he expressed his concerns regarding the inadequate pipeline of new antimicrobials. He called for more efforts directed toward developing new antibiotics as well as vaccines, rapid diagnostics, and conservation strategies.
- Chawla reiterated Pearson’s point that more attention is needed on the livestock sector. Chawla highlighted the challenge of higher production costs for farmers, and the resistance from some governments that are not readily committing to reduce the use of antibiotics in livestock. He suggested that a fund to counter AMR could be set up to pay for costs associated with new policies to incentivize low- and middle-income countries.
- Laxminarayan urged for fundamental changes in the way the global community manages antibiotics and infectious diseases in both humans and animals. He argued that while he is not opposed to funds going to research and development, there is a strong need to invest in conservation and prevention measures.
Fukuda opened the discussion to the audience, starting with questions on the viability of specific interventions to reduce the threat of AMR. Mary Wilson, clinical professor of epidemiology and biostatistics in the School of Medicine at the University of California, San Francisco, asked about the potential benefit of vaccines as a prevention measure for both humans and livestock to reduce antibiotic use. Laxminarayan responded that there is huge potential for both existing and potentially new vaccines to prevent infections as well as to reduce antibiotic use. He stated that current research is evaluating how vaccines can reduce antibiotic consumption.
Martin Meltzer, senior economist and distinguished consultant at the U.S. Centers for Disease Control and Prevention, asked about the sustainability of interventions that aim to reduce AMR but have short life spans and need continuous monitoring for effectiveness—such as hand washing. He asked the panelists to reflect on actions that will change antibiotic use not only in the short term but also in the long term, before a new set of tools such as novel antibiotics are introduced. Laxminarayan noted that current tools, such as the pneumococcal conjugate vaccine prevent the need for antibiotics and reduces both antibiotic-susceptible and antibiotic-resistant diseases. He argued that a tuberculosis (TB) vaccine would prevent both TB-resistant and TB-susceptible infections. On the sustainability of behavioral interventions, he agreed that the effect can wane with time unless a new social norm is created. Pearson responded that the declining success of
behavioral interventions, like hand washing, was integrated in the models he presented, but the interventions were nonetheless demonstrated to be cost-effective. He pointed out that some interventions are more structural, like delayed prescription policies, where the patients have to wait for 3 days before being prescribed the antibiotics and at which point the patients may not need the drugs because they have recovered in that time frame.
Carlos Castillo-Chavez, professor of mathematical biology at Arizona State University, asked how to reduce resistance of antimicrobials by effectively managing hospital-acquired infections and methods to appropriately treat and deliver the drugs to patients in ways that are not cost-prohibitive. He noted the practice of cycling or mixing antibiotics to prevent resistant nosocomial infections, which can have limitations, versus isolation of these cases, which can be more effective but expensive.5 Laxminarayan responded by noting that a large body of research has recently been published, establishing heterogeneity of antibiotics as a superior strategy to cycling. Castillo-Chavez acknowledged this literature, particularly stemming from the agriculture sector, but emphasized that there are still issues of resistance even with heterogeneity and that the crux of the question is the need to redesign how and where to deliver antibiotics to reduce resistance within hospital settings. Laxminarayan agreed that this is a question to consider and that part of the answer depends on the various costs of isolation.
The discussion turned to AMR in the context of low- and middle-income countries. Anas El Turabi, Frank Knox fellow in health policy at Harvard University, reflected on the equity dimension of AMR. He noted that economic loss from health in low- and middle-income countries typically point to mortality and morbidity from diseases like HIV, TB, and malaria, yet much of the discussions on AMR often focus on hospital-acquired infections, which are not always the biggest driver of mortality and morbidity in these countries. He asked the panelists to comment on this divergence, and on whether the interventions that are likely to work in high-income settings will also work for the AMR challenges of low-income countries. Laxminarayan noted that AMR has become an engine for many types of health interventions and is now tied to the universal health care agenda. Chawla stated that interventions taken from high-income countries to reduce AMR will be particularly difficult in countries with fragmented health systems, since the issue can be political, and it is difficult to manage prescriptions and antibiotic use by individual health care providers.
___________________
5 Similar to crop rotation, cycling prioritizes a set of antibiotics to use against specific diseases during a determined time period before rotating to a period of restriction. The aim is that one particular drug would not be encountered by the pathogen during restriction cycles to prevent a mechanism of resistance from developing. Alternatively, a mixing strategy randomly allocates an appropriate antibiotic to patients within the same patient cohort, and is also referred to as a heterogeneity strategy (Beardmore et al., 2017).
Peter Daszak, president of EcoHealth Alliance, also asked about the status of AMR in low- and middle-income countries, specifically about the scalability and feasibility of antibiotic-free livestock in these locations. Laxminarayan noted that removing antimicrobial growth promoters and replacing them with more labor effort would cost about $1.50 per pig, and paying this amount is a choice that producers and consumers are able to make (Laxminarayan et al., 2015). He stated that livestock facilities in China and India are becoming state of the art, so it would be possible for them to transition to antibiotic-free livestock production. Pearson agreed that livestock production in China and India is characterized by high technology factories that can be regulated, making it feasible to change their production model. Chawla offered a different view, not fully agreeing that production facilities in these countries have become totally modern and concentrated for a feasible introduction of measures to reduce antibiotics.
Highlighting another issue from the livestock sector, Dennis Carroll, director of the Global Health Security and Development Unit at the U.S. Agency for International Development, noted that the biggest policy makers of livestock production are in the private sector as they make decisions about how investments are made. He added that many multinational livestock producers are making their own conclusions to move toward greater antibiotic stewardship in the interest of future profit concerns and their economic bottom line. He asked the panelists to share ideas on how to expand this type of thinking to incentivize the private sector as catalysts for change in the general fight against AMR but relying on the perceived economic benefits. Pearson responded by describing the motivations for the private sector as seeking first-mover advantage. After the first-mover advantage has been used, Pearson explained that it is difficult to rely on the private sector because they might fear incurred costs from taking further action while not reaping any benefits. Therefore, he stated that public–private partnerships are needed to catalyze industry-wide changes.
Kimberly Thompson, president of Kid Risk, Inc., commented that antibiotics should be considered as a global public good and suggested that there is a need for a public management strategy and a shared realization that all stakeholders are implicated in AMR. She asked how incentives can be created to unite interest groups to take society-level interventions to address AMR. Pearson responded that it is necessary to involve civil society to create social movements, and pointed out that some infectious diseases like HIV have strongly associated civil society embedded in the population. In contrast, civil society seems virtually nonexistent for AMR beyond the usual stakeholders who interact with the United Nations agencies. He argued that the lack of connection with the wider population and civil society has made it difficult to develop a movement around AMR to push for investments and policies that restrict antibiotic use.
Finally, the discussion ended on the participants reflecting on the enormous costs of AMR. Dean Jamison, professor emeritus of global health at the University of California, San Francisco, highlighted the complexities of defining the billion or trillion dollar cost associated with past and forthcoming use of antibiotics. Ed Whiting, chief of staff and director of policy of the Wellcome Trust, noted that the large estimates of impact have been helpful to create a political narrative for raising the issue on the global agenda. Laxminarayan responded by arguing that overstating the problem does not help, and large estimates require further unpacking. He added that calculations relying on past AMR trends and costs of antibiotics do not necessarily translate to future costing estimates, as the role of antibiotics will likely evolve. Pearson argued that the numbers associated with the future cost of AMR (estimated to be as large as the global financial crisis) helped raise the issue to the level of national policy makers, but big numbers do not always help to find solutions. He stated that breaking down the costs faced by different actors, and comparing these costs with interventions to evaluate their cost-effectiveness, will help to identify potential investments. Chawla reiterated that all costing exercises are limited by their underlying assumptions, but that these costing studies are nevertheless helpful as a starting point for an evaluation of market incentives. The field of economics has the potential to generate insights into the incentives around antibiotic use and research and reveal future solutions, he said.
This page intentionally left blank.














