6
Designing Mobile Technologies for Research and Clinical Practice That Reflect Patient Attitudes and Preferences
Mobile technologies have the potential to impact health care through monitoring, therapeutic intervention, participant recruitment for clinical trials, and more, but only if there is widespread adoption and use by consumers, and only if the information collected is useful for physicians, said
Magali Haas, CEO and president of Cohen Veterans Bioscience. Consumer attitudes vary with regard to data ownership, access, and privacy; the usability of different types of devices; and the utility of their data, said Haas. Whether they have a disease or are well but worried about the future may impact their decisions about monitoring as well as their propensity to use certain technologies and adhere to protocols, she said.
For example, Haas cited the case of an app called PTSD Coach,1 which was developed by the Department of Veterans Affairs to help people learn about and manage symptoms resulting from trauma. Despite being one of the most successful apps available in terms of demonstrated validity and number of downloads, an analysis by the developers revealed that actual adoption and usage rates were low, said Haas. This raises questions about the design of the devices, how the devices are implemented in research studies or marketed to consumers, how easy the devices are to set up and use, and the cost of using these devices, she said. In addition, if the devices are intended to be used for self-management, the quality of the data comes into question, as well as the appropriateness of providing direct feedback to people without any physician review of the data or regulatory approval of the device.
A recent review of initial experience with Apple’s open-source smartphone platform, ResearchKit, demonstrated a similarly dramatic dropoff in use after initial enthusiasm for five smartphone apps developed in 2015 (Dorsey et al., 2017), said Jeffrey Kaye, Layton Professor of Neurology and Biomedical Engineering and director of the Oregon Center for Aging and Technology (ORCATECH) at the Oregon Health & Science University (OHSU). Kaye suggested that one reason for low adoption rates may be the introduction of a novel technology without first developing a full understanding of why and how the data collected will provide value and why a person would want to become involved in the study. Theories of adoption, including the Unified Theory of Acceptance and Use of Technology (Venkatesh et al., 2003) and the Technology Acceptance Model (Holden and Karsh, 2010), have been around for many years, said Kaye. Essentially, he said, they propose that acceptance of a technology requires developers to “know their customers;” that is, to understand the attitudes, beliefs, and experiences of the people who will be using it.
Age is a particularly important factor for technology developers to consider, said Kaye, noting that advanced age is a crucial factor in neurological disorders, with most of the people affected by dementia over the
___________________
1 To learn more about PTSD Coach, see https://www.ptsd.va.gov/public/materials/apps/ptsdcoach.asp (accessed July 18, 2018).
age of 80. A recent Pew Research Center survey found that while use of digital technologies is high even among adults over the age of 65, only about 17 percent of those over age 80 own a smartphone, said Kaye (Pew Research Center, 2017). Thus, technologies developed for the “oldest old” may achieve limited adoption if they rely on use of a smartphone. Moreover, he said, as people age, even the digitally mature will become naïve to the next new technology. Older people with cognitive decline may also have trouble making sense of technology, added Deborah Estrin.
SURVEYING CONSUMER ATTITUDES ABOUT MOBILE TECHNOLOGY
Focus groups and surveys such as those conducted by the Pew Research Center are critical to understanding peoples’ preferences and attitudes about a range of issues related to the use of digital technologies, said Kaye. For example, to learn about what multiple sclerosis (MS) patients think about the collection and sharing of health-related data through mobile technology, the Accelerated Cure Project for Multiple Sclerosis surveyed their community of more than 4,600 members, according to Sara Loud, COO of the Accelerated Cure Project. They were able to push this survey to members through iConquerMS.org, an online portal designed to help patients drive MS research by providing personal health information as well as their experiences and opinions, she said.2 About 650 members responded to the survey. Most respondents (91 percent) own a smartphone or tablet and 28 percent own a wearable. Only about one-quarter of them use their smartphone to track their own health, but 71 percent of those with wearables use them to track their health. These numbers are similar to those seen in the general population, said Loud.
About half of those with wearables share their data, mostly with family and friends through social media, but also with health care providers, device manufacturers, and researchers, said Loud. The survey did not assess how receptive health care providers were to the shared data, and Loud noted that health care systems may not have the means to accept these data in a format that fits within the constructs of the providers’ jobs. Only a few respondents reported sharing data with employers or insurance companies. The primary reason people are not sharing data, according to the survey, is the belief that others are not interested. Other reasons included a lack of
___________________
2 To learn more about iConquerMS, see https://www.iconquerms.org (accessed July 29, 2018).
knowledge about how to share data and fear of being judged or otherwise negatively impacted.
Loud said the survey also asked participants to imagine how they would feel about using an implantable device designed to help with symptom management if it was offered in a clinical trial setting. The device, they were told, would collect not only symptom-specific data, but also other biological and health activity information, location, etc. Eighty-five percent of respondents said they would consider participating in such a trial, and 39 percent said they would be willing to share any data collected. Some said they would be willing to share only certain information, and 17 percent said they wanted to be able to select what they would share. Respondents were most willing to share data with MS and device researchers, as well as with their health care providers, demonstrating their interest in driving research and improving their health, said Loud. “They want to see that their data can have a manageable and tangible effect on what happens in the understanding of the disease,” she said.
Not surprisingly, respondents also expressed concerns about data sharing. These concerns mostly related to fear of losing insurance or health care coverage and loss of privacy, said Loud. She said a few also raised concerns about the reliability of the data.
Respondents also expressed strong feelings about having access to their own information, although Loud acknowledged some reluctance in the research community to provide participants with large amounts of data that may not be actionable. The issue of data return to participants should be addressed in the consent process, with provisos that those returned data are understandable, meaningful, actionable, and accessible, said Loud. She advocated a co-design paradigm where study participants and patient communities are involved both in the design of the study and the crafting of the informed consent.
ASSESSING FUNCTION IN REAL-LIFE SETTINGS
Kaye also uses surveys and focus groups as a first step in an iterative research process for studies aimed at developing technologies to assess real-world functional changes associated with aging (Kaye et al., 2011) (see Figure 6-1). Taking the time to understand the views of all stakeholders involved in the research enterprise is yeoman’s work, but necessary to ensure that the research is carried out properly, he said.
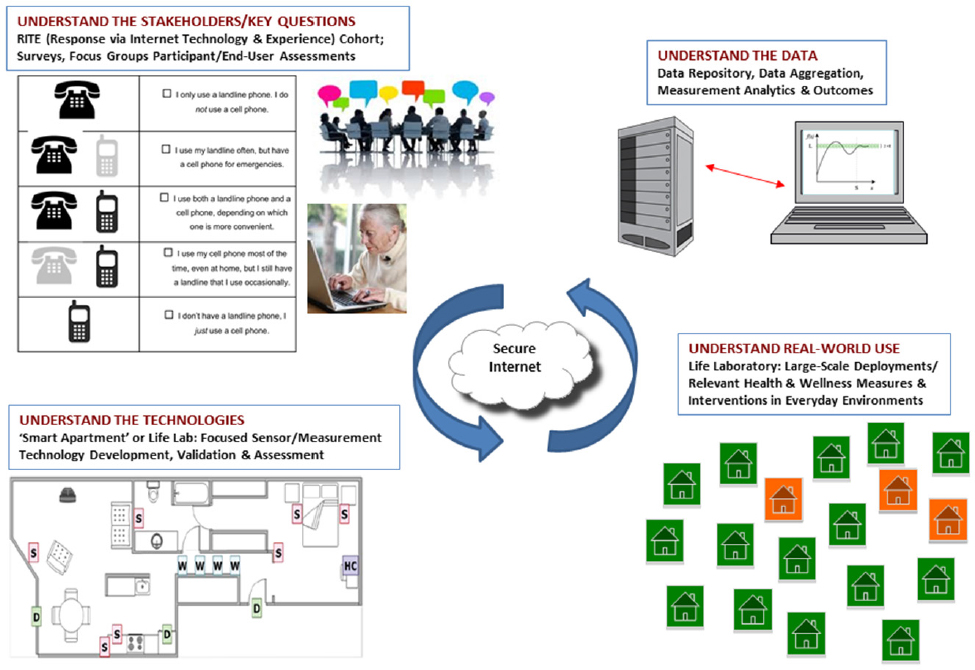
SOURCE: Presented by Kaye, June 6, 2018.
To understand how technologies can work in real-world settings, Kaye and his ORCATECH colleagues created the Life Laboratory, where multiple sensors and devices are deployed in people’s homes to assess a multitude of functions—activity, mobility, sleep, cognition, social engagement, medication adherence, etc. (Kaye et al., 2011; Lyons et al., 2015). These rich data are stored in a secured data repository and made available for sharing with other researchers, said Kaye. His lab’s focus is not about any specific technology, he said. Rather, it is about being able to plug in different technologies to test these functions in a real-life context and compare the data over time.
For example, Kaye’s team has used the Life Laboratory to test people’s attitudes about using a remote-controlled robot in an older person’s homes to facilitate communication between the senior and a “remote collateral individual” (e.g., an adult child or other family member). Both the older adult participants and the remote collaterals gave the robot high marks in terms of both usability and acceptability, commenting that the robot improved communication, provided a sense of safety, and gave fam-
ily members peace of mind, said Kaye (Seelye et al., 2012). Only one participant with some cognitive impairment rated the robot unfavorably, he said. Another study conducted by Kaye and colleagues used video chats to boost social engagement in people with normal cognition and mild cognitive impairment (Dodge, 2015). Very high acceptance and adherence to this protocol suggested that isolation among participants made them highly motivated, said Kaye. “They had a reason to want to use the technology, and the technology didn’t get in the way,” he said.
Developing user-focused technologies also requires consideration of cultural factors, said Kaye. For example, his team collaborated with OHSU’s Raina Croff on the Sharing History through Active Reminiscence and Photo-imagery study, which aimed to motivate aging African Americans to walk more by using technology to enhance the culturally relevant experience of walking around historically Black neighborhoods that have been gentrified. As groups of participants walk along a prescribed path, memory markers relevant to their lives are delivered over their smartphones to stimulate discussion (Croff et al., 2018). Kaye said the program has been very popular.
Kaye noted that some of research studies have been less successful despite employing user-centered design principles. For example, he had hoped to show that continuous functional data could be used by decision makers to delay the transition to higher levels of care in retirement communities. However, despite initial enthusiasm, adoption of the technology was poor, and exit interviews suggested that decision makers were not sure how to use the trend data they were provided, said Kaye. Additionally, the technology was not integrated well enough into the systems that already existed at the facility. Nonetheless, Kaye noted that the technology itself worked well and provided a great deal of natural history data from the cohort.
INTEGRATING DIGITAL TECHNOLOGIES INTO CLINICAL TRIALS: BENEFITS TO PATIENTS
Digital technologies can speed up trials, reduce the number of participants required and thus their exposure to potentially harmful treatments, and potentially allow assessments to be conducted remotely, thus reducing participant burden, said William Marks. As a result, future trials that employ digital technologies may be much more decentralized and diverse in
terms of the characteristics of participants, said Vaibhav Narayan. Moreover, said Iain Simpson, they have the potential to provide more precise measures of real-world function. Indeed, Stephen Arnerić predicted that digital technologies will transform the way clinical trials are done.
If designed well, digital technology platforms enable trialists to communicate very clearly with research participants what they are signing up for in the trial and what data they do or do not want to contribute, said Marks. Kaye and Loud agreed, noting that people participate in clinical studies for different reasons. For example, some people participate out of a sense of altruism, while others believe they are going to get information that is meaningful or useful to them, including information that will allow them to self-manage their disease, said Kaye. Various incentives can be used to encourage participation by a broad population.
INFORMED CONSENT
Obtaining informed consent for studies conducted online and using digital devices requires special considerations to ensure that people are truly informed, said Loud. In addition to clear language, she suggested that infographics and other visualizations, as well as quizzes at the end of the consent process, may be needed to be certain that participants fully understand their agreements. The iConquerMS cohort wants a tiered approval process, she said, where they can select who gets the data and be provided full disclosure of the ramifications of their choice to share their data.
Kristen Rosati added that building platforms that enable leveraging data collected for one purpose to be used for other clinical research activities would require structuring the consent to allow this. This should be addressed at the beginning of a study, she said.
DIGITAL TECHNOLOGIES AS INTERVENTIONS
Interventions are the next frontier for digital technologies, said Munmun De Choudhury; however, there are many unresolved research questions about how to move from sensing and predicting to intervening. For example, if an algorithm suggests someone may be at high risk of a health event, what should the intervention look like and how should it be communicated to the individual? Should the messages point to available resources? De Choudhury emphasized that humans—both clinicians and patients—
should be involved in the intervention delivery process loop to ensure that incorrect assessments are circumvented and inappropriate interventions reduced.
Tanzeem Choudhury added that developers of these technologies should think about measurement and intervention simultaneously, including consideration of individuals’ acceptance, willingness, and motivation to act on their data and change behaviors. To marry sensing and intervention, she suggested that it will be important to make behavioral interventions fit into the person’s routine and lifestyle with low effort. In her experience, individuals with behavioral health problems have been overwhelmingly accepting of digital sensing technologies, which she hypothesized is because they know how debilitating these conditions can be and readily accept anything that keeps them functioning at a healthy level.








