H
Fact Sheet: Coding Guidance for Traumatic Brain Injury
 Health Information Management Office of Informatics and Analytics
Health Information Management Office of Informatics and Analytics
IMPORTANT NOTE: This Fact Sheet denotes use of International Classification of Diseases, Tenth Revision (ICD-10) codes effective October 1, 2015. ALL PREVIOUS VERSIONS OF THIS FACT SHEET ARE RESCINDED.
BACKGROUND: The Veterans Health Administration (VHA) has a need, to the best of its ability, to uniquely identify and report on Traumatic Brain Injury (TBI), its conditions, syndrome, and symptoms resulting from such injuries. VHA in conjunction with Department of Defense (DOD) have championed the development of TBI codes to more accurately capture and reflect TBI and its effects.
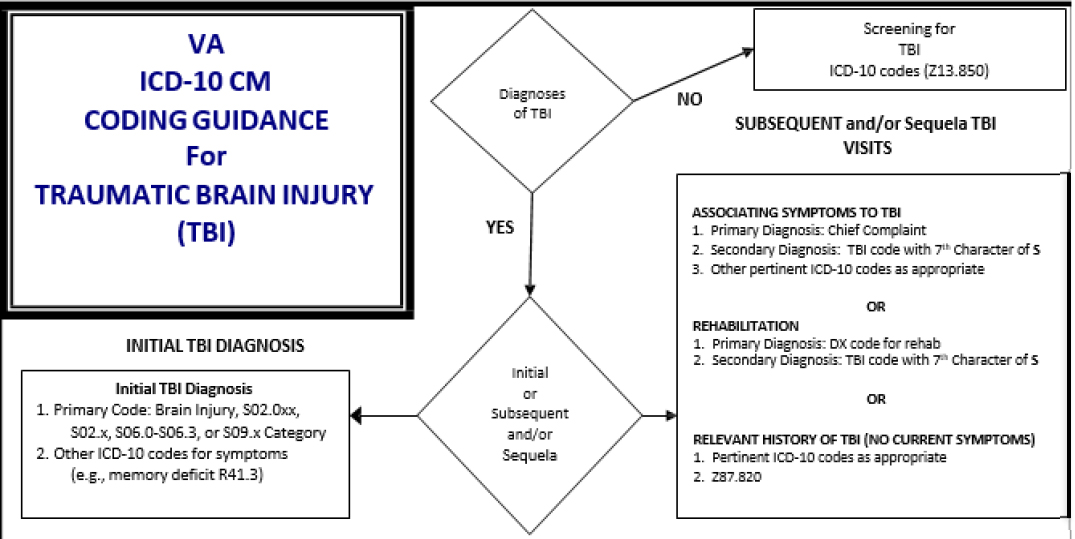
CODING THE INITIAL ENCOUNTER: The ICD-10-CM codes will now provide the specificity of initial, subsequent, and/or sequela to describe the injury; however the seventh character of A will be used to identify the first time the patient is seen for the injury, regardless of when the injury took place. If an injury occurred in the past several months or even years prior but the patient has never sought treatment for the injury previously, the first time the patient is SEEN for the injury is considered the initial treatment.
An initial encounter does not refer to the first time the patient is seen by each clinician for that particular TBI. Rather, an initial encounter is defined as the first time the patient is seen by any medical professional for the TBI, regardless of when the injury took place even if it occurred several weeks, months or years prior to the encounter, and for additional encounters where the patient is receiving “active treatment” as defined in the ICD-10-CM Official Guidelines for Coding and Reporting. Clinical documentation must clearly indicate that the encounter coded is the initial encounter for that particular injury.
For ICD-10-CM the appropriate 7th character will be added to the code to indicate the type of encounter:
- A initial encounter will be used while the patient is receiving active treatment for the condition
- D subsequent encounter will be used for encounters after the patient has received active treatment of the condition and receiving routine care for the condition during the healing or recovery phase
- S sequela will be used for complications that arise as a direct result of the condition
Initial Encounter: Veteran is seen for the first time at a VA facility for memory problems, as well as any additional encounters where the patient is receiving “active treatment”. During the history the practitioner determines, on the basis of Veteran’s self-report, that there was brief loss of consciousness less than 30 minutes due to an Improvised Explosive Device (IED) blast. There is no evidence in the record of skull fracture. The Veteran reports that he has never sought treatment for the condition which is now causing significant problems at work. The practitioner selects the codes TBI Not Otherwise Specified (NOS) with loss of consciousness of 30 minutes or less, initial encounter (S06.9X1A) and the codes the for memory loss NOS (R41.3), and war operations involving explosion of improvised explosive device (IED), military personnel (Y36.230A).
ICD-10 now codes based on loss of consciousness (LOC) time after the injury. In order to ensure the most accurate and appropriate level of coding, documentation must clearly state if there was an LOC due to the injury and the duration of the LOC. If documentation does not clearly define the LOC then unspecified state of consciousness must be coded. Please refer to your Health Information Management Coding Department for further guidance.
FOLLOW UP CARE (Subsequent/Sequela Encounter): Subsequent encounter designation will be used for encounters after the patient has received active treatment of the condition and is receiving routine care for the condition during the healing or recovery phase, and sequela (late effect) designation will be used for complications that arise as a direct result of the condition. For follow up visits for late effects directly related to a previous TBI, the symptom code(s) that best represents the patient’s chief complaint or symptom(s) (e.g., headache, insomnia, vertigo) are coded, followed by the appropriate late effect code or sequela code. This will be the initial TBI injury code with the seventh character of S for sequela. Late effects include any symptom or sequelae of the injury specified as such, which may occur at any time after the onset of the injury. The External Causes of Morbidity (V01-Y99) code will also need to be added with a seventh character of S.
The pairing of the symptom code and the late effect code is the ONLY WAY that symptoms can be causally and uniquely associated with TBI and is essential to the accurate classification of TBI.
REHABILITATION: For TBI patients who receive inpatient or outpatient rehabilitation, the first-entered diagnosis is the purpose of the appropriate condition for which the rehabilitation service is being performed (e.g. neurological deficits, hemiparesis, etc.) and then the appropriate TBI code with the seventh character of D for subsequent encounter or S for sequela (S06.2, S06.3, or S06.9). The External Causes of Morbidity (V01-Y99) code will also need to be added with a seventh character of S.
USE of Z87.820 CODE: Z87.820 Personal history of traumatic brain injury was developed to indicate that previous TBI occurred and may impact current care. The Z87.820 code is not used in conjunction with the late effect codes; rather the Z code is used when no other code is available to reflect a previous TBI. Normally, the Z87.820 code is used to identify a personal history of injury with or without a confirmed diagnosis. A history of an illness, even if no longer present, is important information that may alter the type of treatment ordered.
TBI SCREENING: Code Z13.850 should be used if TBI screening occurs at a visit, whether or not the screening is positive. A TBI diagnosis code should not be entered for a positive screen since a positive TBI screen does not indicate a TBI diagnosis. A TBI diagnosis code can only be entered for the encounter at which the diagnosis is made.
Examples of ICD-10-CM Codes Typically Associated with TBI
Acute Injuries
| Series Code | Description |
|---|---|
| S02.0xx | Fractures of vault of skull—requires a seventh character for type of encounter and healing |
| S02.1 | Fractures of base of skull—requires two digits and a seventh character |
| S06.0 | Concussion—requires two digits and a seventh character |
| S06.1 | Traumatic cerebral edema—requires two digits and a seventh character |
| S06.2 | Diffuse traumatic brain injury—requires two digits and a seventh character |
| S06.30 | Focal traumatic brain injury—requires an additional digit and a seventh character |
| S06.31 | Contusion and laceration of right cerebrum—requires an additional digit and a seventh character |
| S06.32 | Contusion and laceration of left cerebrum—requires an additional digit and a seventh character |
| S06.33 | Contusion and laceration of cerebrum, unspecified—requires an additional digit and a seventh character |
| S09.x | Unspecified intracranial injury (TBI NOS)—requires an additional digit and a seventh character |
Late Effect Codes or Sequela
| Series Code | Description |
|---|---|
| S06.2 | Diffuse traumatic brain injury—requires two digits and a seventh character of S |
| S06.30 | Focal traumatic nrain injury—requires an additional digit and a seventh character of S |
| S09.x | Unspecified intracranial injury (TBI NOS)—requires an additional digit and a seventh character of S |
Symptoms Involving Emotional State
| ICD-10 Code | Symptom |
|---|---|
| R45.0 | Nervousness |
| R45.4 | Irritability and anger |
| R45.87 | Impulsiveness |
| R45.86 | Emotional lability |
| R45.3 | Demoralization and apathy |
| R45.89 | Other signs and symptoms involving emotional state |
Symptoms Involving Cognitive Function and Awareness
| ICD-10 Code | Symptom |
|---|---|
| R41.840 | Attention and concentration deficit |
| R41.841 | Cognitive communication deficit |
| R41.842 | Visuospatial deficit |
| R41.843 | Psychomotor deficit |
| R41.844 | Frontal lobe and executive function deficit |
| R41.89 | Other signs and symptoms involving cognitive functions and awareness |
Note: Memory deficits will be coded as R41.3.
Physical Effects of TBI
| ICD-10 Code | Description |
|---|---|
| G44.301 | Posttraumatic headache, unspecified, intractable |
| G44309 | Posttraumatic headache, unspecified, not intractable |
| G44.321 | Chronic posttraumatic headache, unspecified, intractable |
| G44.329 | Chronic posttraumatic headache, unspecified, not intractable |
| R42. | Dizziness |
| R43.0 | Loss of smell (anosmia) |
| R43.8 | Other disturbance of smell and taste |
| R47.82 | Fluency disorder conditions classified elsewhere |
| R47.81 | Slurred speech |
| R56.1 | Posttraumatic seizures |
 |
|
| Review all existing documentation, including that from outside sources, to ensure that a previous TBI code has not been assigned. Clarify the patient’s documented symptoms by answering the below questions | Severity of TBI |
| Duration: Has the symptom existed for days, weeks, or months? Has the symptom occurred only intermittently? Are there times of the day when the symptom(s) is worse? Particularly with regard to pain and fatigue, can the patient define if these symptoms occur 2 or 3 days per month or constantly? | The below diagnostic criteria does not predict functional or rehabilitative outcome of the patient. The level of injury is based on the status of the patient at the time of injury, based on observable signs such as level of consciousness, posttraumatic amnesia and coma scaling. |
| Onset: Can the patient recall exactly how the symptoms began? Were the triggering events, either physical or emotional? Was the onset subtle and gradual, or are there changing patterns? | 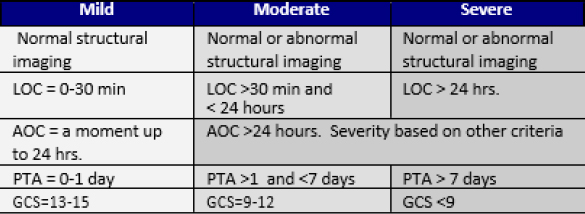 |
| Location: Is the symptom localized or diffuse? Can the patient localize the symptom by pointing to it? If the pain is diffuse, does it involve more than one body area or quadrant? | AOC – Alteration of consciousness/mental state LOC – Loss of consciousness PTA – Post-traumatic amnesia GCS – Glasgow Coma Scale |
| Comorbidity: Does the patient have any diagnosed co-existing diagnoses? What is the relationship between the onset and severity of the co-existing illnesses and the symptoms of fatigue and/or pain? Are there co-morbid diagnoses? Are there new changes to the patient’s weight, mood, or diet? | |
| Previous Episodes: If the symptoms are episodic, what is the pattern with regard to timing, intensity, triggering events, and response to treatment? | Additional Procedure Coding for TBI Care |
| Intensity and Impact: How severe are the symptoms (1–10 rating scale)? Ask the patient to describe any new limitations they have experience compared to their usual life-style, such as limitations in physical endurance or strength (e.g. climbing stairs, shopping, or sleep quality). | If the psychomotor Neurobehavioral Status Exam is completed, the provider should also utilize the CPT code 96116. This code includes the time for testing, interpreting, and a written report must be prepared. Coding is completed in 1-hr units but anything less than an hour is claimed as 1 unit. Documentation must include clinically indicated portions of an assessment of thinking, reasoning and judgment (e.g., attention, acquired knowledge, language, memory and problem solving). |
| Previous Treatment and Medications: Request that patient bring copies of previous medical records regarding treatment of injury, or have patient authorize VA to receive copies and/or discuss medical history with previous clinician. Ask that the patient bring their medications bottles with them and document them within CPRS. Discuss with the patient which mediations have or have not been helpful. | Documentation Questions retrieved from the tables in the VA/DoD Clinical Practice Guidelines for Management of Concussion/mTBI 2.0, Retrieved August 5, 2015, from VA/DoD Clinical Practice Guidelines |






